Volume 9, Issue 4 (2021)
Health Educ Health Promot 2021, 9(4): 309-315 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chupradit S, Widjaja G, Khasanah U, Tondok S, Samal A, Rahman F et al . Prevalence of Diabetes and Sedentary Lifestyle: A Review of Diabetes Self-Management Education. Health Educ Health Promot 2021; 9 (4) :309-315
URL: http://hehp.modares.ac.ir/article-5-54875-en.html
URL: http://hehp.modares.ac.ir/article-5-54875-en.html
1- Department of Occupational Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand , supat.c@cmu.ac.th
2- Faculty of Public Health, Krisnadwipayana University, Jatiwaringin, Indonesia
3- Faculty of Nursing, Muhammadiyah Jakarta University, Banten, Indonesia
4- Department of Nursing, Faculty of Politeknik Kesehatan, Kementerian Kesehatan University, Jayapura, Indonesia
5- Faculty of Hospitality & Tourism Management, Siksha O Anusandhan University, Bhubaneswar, India
6- Faculty of Public Health, Muhammadiyah Kalimantan Timur University, Kalimantan Timur, Indonesia
7- Department of Pharmacology, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India
2- Faculty of Public Health, Krisnadwipayana University, Jatiwaringin, Indonesia
3- Faculty of Nursing, Muhammadiyah Jakarta University, Banten, Indonesia
4- Department of Nursing, Faculty of Politeknik Kesehatan, Kementerian Kesehatan University, Jayapura, Indonesia
5- Faculty of Hospitality & Tourism Management, Siksha O Anusandhan University, Bhubaneswar, India
6- Faculty of Public Health, Muhammadiyah Kalimantan Timur University, Kalimantan Timur, Indonesia
7- Department of Pharmacology, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Chennai, India
Full-Text [PDF 408 kb]
(1091 Downloads)
| Abstract (HTML) (2159 Views)
Full-Text: (551 Views)
Introduction
The incidence of diabetes continues to increase at an alarming rate [1-3]. The incidence of diabetes increases gradually due to the advancement of technology and the change in sedentary lifestyle and diet [4-6]. The number of individuals with diabetes globally, which was 171 million in 2000, reached 347 million in 2013 [7, 8]. In Turkey, the prevalence of diabetes in adults 20 years and older was 7.2% in 2002; this amount increased to 13.7% only in 5 years [9, 10].
The main problem in people with diabetes is uncontrollable blood glucose levels [11, 12]. Therefore, in the management of diabetes, the goal is to achieve glycemic control and prevention of complications [13, 14]. Diabetes treatment includes medical, physical nutrition activity, blood sugar monitoring, diabetes self-management education (DSME), and oral diabetes/insulin [15-17].
Diabetes treatment, which should be applied throughout life, requires the individual to manage his/her treatment and make a lifestyle change [17, 18]. DSME is important for individuals with diabetes to make lifestyle changes [19]. DSME is a collaborative process for individuals with diabetes or at risk of diabetes to acquire the necessary knowledge and skills to successfully manage their disease and disease-related conditions and make behavioral changes [20-22].
It has been found that DSME reduces the HbA1c level of individuals with diabetes and lowers fasting glucose level and blood pressure. Many studies indicated that increasing the knowledge of diabetes reduces the need for medication and improves the quality of life also; It is also emphasized that the positive results of DSME enable the patient to focus on self-management, and cultural characteristics are taken into account in plans and practices [23-25].
DSME is a theory that is recommended to be based on a model that active participation and self-efficacy of models in diabetic patients, encouraging development increase the effectiveness and results of self-management skills. In the study of Piatt et al. [26], it was shown that DSME based on the chronic care model improves the clinical and behavioral outcomes of individuals with diabetes. In the study of Brown et al. [27], it was determined that DSME improves the health outcomes of individuals with diabetes, especially those with an HbA1c level below 10%. In the study of Gucciardi et al. [28], it was determined that DSME based on Planned Behavior Theory increased the compliance of individuals with diabetes to medical nutrition behaviors and decreased HbA1c levels. In study [29] randomized controlled study, it was determined that patients who received DSME based on the Self-Care Deficiency Nursing Theory increased after six months of follow-up.
Although there are many studies on DSME, it is still debated whether group education as an education method is superior to individual education or which education method should be preferred. In this article, in the light of the literature about the DSME, how DSME is done, individual and group education as DSME is mentioned, and "Is group education superior to individual education?"
Diabetes self-management education (DSME)
Diabetes education: Since the discovery of insulin in 1920, over the years, Dr. Elliott P. Jocelyn, until the 1960s in several centers, systematically tried to understand information about the patient. Joslin & Kahn [30] emphasized the importance of education by saying, "Education is not a part of diabetes treatment; on the contrary, it is the treatment itself" [31]. The World Health Organization reported in 1980 that education is a cornerstone of diabetes treatment. Joslin & Kahn [30] advocated that individuals with diabetes should be responsible for their care and advocated the concept of DSME, which is recommended in diabetes education today. They emphasized the importance of education for an individual with diabetes to manage diabetes and stated that nurses have an important role in diabetes education and treatment.
Between 1970 and 1980, the American Association of Diabetes Educators and the Diabetes Education Study Group (DESG) took important steps in establishing organizations that aimed to structure, standardize and disseminate education programs. These organizations continue their studies on planning the diabetes education program, determining the principles of patient education with diabetes, and evaluating the education results. Principles of DSME are [32]:
The incidence of diabetes continues to increase at an alarming rate [1-3]. The incidence of diabetes increases gradually due to the advancement of technology and the change in sedentary lifestyle and diet [4-6]. The number of individuals with diabetes globally, which was 171 million in 2000, reached 347 million in 2013 [7, 8]. In Turkey, the prevalence of diabetes in adults 20 years and older was 7.2% in 2002; this amount increased to 13.7% only in 5 years [9, 10].
The main problem in people with diabetes is uncontrollable blood glucose levels [11, 12]. Therefore, in the management of diabetes, the goal is to achieve glycemic control and prevention of complications [13, 14]. Diabetes treatment includes medical, physical nutrition activity, blood sugar monitoring, diabetes self-management education (DSME), and oral diabetes/insulin [15-17].
Diabetes treatment, which should be applied throughout life, requires the individual to manage his/her treatment and make a lifestyle change [17, 18]. DSME is important for individuals with diabetes to make lifestyle changes [19]. DSME is a collaborative process for individuals with diabetes or at risk of diabetes to acquire the necessary knowledge and skills to successfully manage their disease and disease-related conditions and make behavioral changes [20-22].
It has been found that DSME reduces the HbA1c level of individuals with diabetes and lowers fasting glucose level and blood pressure. Many studies indicated that increasing the knowledge of diabetes reduces the need for medication and improves the quality of life also; It is also emphasized that the positive results of DSME enable the patient to focus on self-management, and cultural characteristics are taken into account in plans and practices [23-25].
DSME is a theory that is recommended to be based on a model that active participation and self-efficacy of models in diabetic patients, encouraging development increase the effectiveness and results of self-management skills. In the study of Piatt et al. [26], it was shown that DSME based on the chronic care model improves the clinical and behavioral outcomes of individuals with diabetes. In the study of Brown et al. [27], it was determined that DSME improves the health outcomes of individuals with diabetes, especially those with an HbA1c level below 10%. In the study of Gucciardi et al. [28], it was determined that DSME based on Planned Behavior Theory increased the compliance of individuals with diabetes to medical nutrition behaviors and decreased HbA1c levels. In study [29] randomized controlled study, it was determined that patients who received DSME based on the Self-Care Deficiency Nursing Theory increased after six months of follow-up.
Although there are many studies on DSME, it is still debated whether group education as an education method is superior to individual education or which education method should be preferred. In this article, in the light of the literature about the DSME, how DSME is done, individual and group education as DSME is mentioned, and "Is group education superior to individual education?"
Diabetes self-management education (DSME)
Diabetes education: Since the discovery of insulin in 1920, over the years, Dr. Elliott P. Jocelyn, until the 1960s in several centers, systematically tried to understand information about the patient. Joslin & Kahn [30] emphasized the importance of education by saying, "Education is not a part of diabetes treatment; on the contrary, it is the treatment itself" [31]. The World Health Organization reported in 1980 that education is a cornerstone of diabetes treatment. Joslin & Kahn [30] advocated that individuals with diabetes should be responsible for their care and advocated the concept of DSME, which is recommended in diabetes education today. They emphasized the importance of education for an individual with diabetes to manage diabetes and stated that nurses have an important role in diabetes education and treatment.
Between 1970 and 1980, the American Association of Diabetes Educators and the Diabetes Education Study Group (DESG) took important steps in establishing organizations that aimed to structure, standardize and disseminate education programs. These organizations continue their studies on planning the diabetes education program, determining the principles of patient education with diabetes, and evaluating the education results. Principles of DSME are [32]:
- Being a good listener,
- Instead of providing trained instruction, it is based on empowerment and problem-based models
- Diabetes educators; Identify their needs
- Collaboration with patients,
- Involvement of people with diabetes in decisions
- Consider the experiences of people with diabetes and their economic, social, cultural, and psychological characteristics
- How to evaluate patients, ongoing training, and support?
How is DSME done?
DSME is done in cooperation with the patient, taking into account the patient's priorities, interests, and concerns [33]. Collaboration role is used to empower patients about what they understand and expect
from health care. With the collaborative role, the patient's participation in their care increases, and they become stronger in managing their health conditions [34]. Considering the evidence-based recommendations regarding DSME to be applied according to the American Association of Diabetes Educators (AADE);
from health care. With the collaborative role, the patient's participation in their care increases, and they become stronger in managing their health conditions [34]. Considering the evidence-based recommendations regarding DSME to be applied according to the American Association of Diabetes Educators (AADE);
- All people with diabetes should have access to DSME (Evidence A).
- To increase the effectiveness of self-management, as defined by self-care behaviors in AADE, DSME should focus primarily on supporting behaviors (Evidence B).
- DSME should be provided by competent/qualified persons (Evidence A).
- DSME should follow a comprehensive five-step process. This process includes the steps of diagnosis (assessment), goal-setting, planning, implementation, and evaluation (Evidence C).
According to the American Association of Diabetes Educators, DSME is a problem-solving process [34]. For this reason, in the implementation process of DSME, the steps of diagnosis, goal setting, planning, implementation, and evaluation, which are the problem-solving process, should be applied [35].
Diagnosis: It is the stage of collecting and interpreting data from the patient about the problems and affecting factors. The diagnostic step in the training process depends on the skill level of the diabetes educator. To diagnose the patient's condition, the diabetes educator collects data from the patient, the patient's family, the patient's social environment, current medical records, and the referral healthcare team in a systematic and organized manner [34, 36].
Goal Setting: The goals of DSME are to strengthen the individual with diabetes, increase self-confidence, improve problem-solving skills and coping behaviors. Therefore, theoretical approaches should facilitate goal-setting regarding patient behavior change, patient empowerment, and patient-centered communication. Theoretical approaches used in DSME include Social Cognitive Theory, Theory of Reasoned Action, Transtheoretical Model, and Theory of Planned Behavior. These theories and models support the patients about the behaviors that patients want to change in diagnosis and help the diabetes educator create the patient's behavior change plan [34]. To achieve the goals in DSME, the cooperation of the patient and the diabetes educator and the participation of the person with diabetes in decisions are important.
Planning: The diabetes educator and the person with diabetes decide together how to reach the set goals. The existing diabetes education practices are integrated into the principles of education and behavior change developed. This plan is coordinated among the diabetes health care team members, the individual with or at risk of diabetes, their families, social support, and referrer [34].
Implementation: During the implementation process, diabetes educators apply diabetes self-management training according to the prepared plan. The diabetes educator counsels patients and their caregivers on the implementation of the DSME plan. Implementation can also be carried out in collaboration with other community and professional services [34].
Assessment: Continuous monitoring and evaluation of the implementation of the prepared plan are important for behavior change. For this reason,
both the training process and whether the predetermined goals have been achieved are evaluated periodically [34].
Individuals with diabetes need to set goals and make daily decisions to manage their diabetes successfully. Individuals with diabetes should be developed to make decisions about their goals, therapeutic options, and self-care behaviors and take responsibility for daily diabetes care to be effective in their care [37].
An example of a protocol for behavioral change in individuals with diabetes, developed by Funnell & Anderson [37], is presented in Table 1.
Table 1) Behavior changes protocol [37]
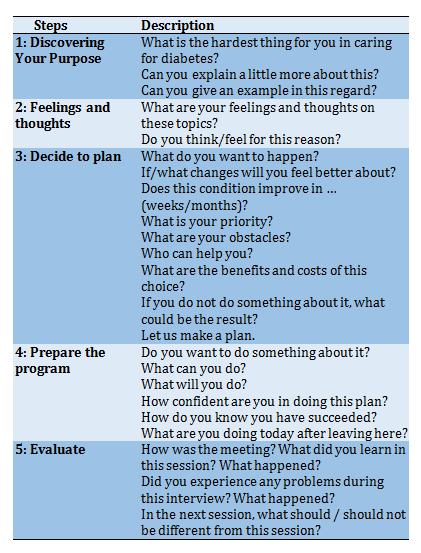
The problem-solving process applied in the behavior change protocol; provides information about diabetes to individuals with diabetes, develops goals related to diabetes and lifestyle, and aims to reach goals [38]. This process consists of five steps. The first two steps describe the problems of individuals with diabetes and their feelings and thoughts about the problems. In the third step, the goals and the patient's preferences are discussed. The patient promises to make behavioral changes that will help them achieve their goals. The fourth step discusses what the patients can do to achieve the goals and evaluate the results. In the fifth step, the educational process is evaluated. In this process, more information about the true nature of the problem will be gained, effective strategies will be developed for individuals with diabetes to cope with, and the barriers and emotions of individuals with diabetes will be learned [37].
Educational strategies can range from simple telephone contact to a comprehensive program, depending on the nature of the situation [39]. There is no single training method and material. Brochures, telephone, posters, slides, books or magazines, the internet, and visual and written media can be used to educate the target audience. However, none of them can replace the one-on-one training provided by diabetes educators. Different methods are used in the education of individuals with diabetes. Individual or group education of health professionals or diabetes educators is the most important education method used in the education of the target group. It should be noted that the DSME can be done by individual education and/or group education method.
Individual Education: Individual education is defined as one-on-one education or face-to-face education. In individual education, it is aimed to provide the appropriate education for the current needs of the individual with diabetes [40]. Communication is more intense in individual education. It is stated that individuals with diabetes express their economic-sexual-social problems and needs more clearly in individual education [40].
Group Education: Teaching people in groups has been an effective form of education for diabetes education since 1970. A group is defined as gathering people with a common interest, such as DSME. The number of participants participating in the groups can vary between 2 and 20. The number of groups depends on the person/organization making the payment, the subject to be discussed, the training method, and the trainers. Studies have found that forming groups of 6-10 people is effective in group education [41].
Why Group Education?
Group education is of great interest among educators and politicians [42]. Some educators prefer group education for their education and recommend using group education as a primary approach to improve outcomes of diabetes [43]. DSME states that it is more effective to do it through group education because it is supportive and encouraging, effective in time and cost, provides sharing experiences, and increases learning with peer interaction. In addition, it is stated that the group education environment supports certain educational activities such as social modeling and problem-based learning better than individual education.
Group education is recommended because it is more suitable for adults' learning styles and has positive results [42, 44]. Considering the principles of adult education, adults need to determine what they want to learn and meet their needs. Adults enjoy small group interaction and practical problem-solving processes, benefiting from other people's experiences. Adults learn as long as they actively participate in the sessions, and if they find the program suitable for them, they will be motivated. Adults are affected by their past experiences in the learning process/behavior change. Therefore, it is difficult for them to change. While physical comfort is important for adults, a pleasant environment and a dynamic environment are important. They enjoy receiving awards such as certificates and gain the courage to learn.
Effectiveness of group education
When we look at the studies comparing group education and individual education to evaluate the effectiveness of group education, it is seen that there are experimental and compilation studies on the subject. In the study of Rickheim et al. [45], in which group education and individual education were compared, the effectiveness of the education program prepared according to DSME standards was evaluated. In both forms of education, the study found that improvements in diabetes knowledge, BMI, quality of life and attitude towards diabetes, and mental health were similar. A decrease in HbA1c levels was detected in the six-month follow-up period in those who received individual and group training. When individual training versus group training was compared, the difference in HbA1c levels was of low statistical significance (marginally greater; p=0.05). In the study, the authors stated the study's limitations as the high losses in their study, the follow-up period of only six months, and the possibility of the results being open to bias because the randomization was not confidential.
Campbell et al. [46] implemented four different interventions in educating individuals with Type 2 diabetes: a minimal group program, an individual program, a comprehensive group program, and an individualized behavior program. The decrease in HbA1c and body mass index was not statistically significant between the groups in the study. However, it has been found that individual and group education have similar effects on the self-care management of individuals with diabetes. The systematic review study of Norris et al. [47] emphasized that group education on lifestyle (physical activity and diet) may have more positive effects than individual education. DSME was found to be effective in both individual and group education. In the meta-analysis study of Norris et al. [48], the effectiveness of diabetes education interventions was examined. The difference between the HbA1c levels of individuals with diabetes who received individual education and group education was not statistically significant.
In a study [49] comparing group education and individual education, the patients who received group education compared to those who received individual education, it was observed that HbA1c level, body mass index, drug dose decreased, retinopathy was less common. HDL cholesterol level increased [49]. In the study of Vadstrup et al. [50], although positive improvements were observed in the quality of life and diabetes symptoms in the groups given individual and group education, this improvement was not statistically significant. No difference was found between the groups. In the study of Llorca et al. [51], diabetes knowledge level improved, HbA1c, body mass index, and systolic blood pressure levels were decreased in groups that received individual and group education. The effects of individual and group training applied in the study were evaluated equally. In the study of Steinsbekk et al. [52] comparing group education with individual education, it was found that group education significantly improved HbA1c, blood glucose levels, lifestyle changes, and psychosocial outcomes of individuals with type 2 diabetes. On the other hand, it was found that there was no statistically significant change in mortality rates, body mass indexes, blood pressure, and lipid profiles of individuals with type 2 diabetes.
Numerous factors affect a patient's achievement of self-management. A review of the present study reveals that various factors, from the effect of age and sex and beliefs of the patient to the attitude, knowledge, skills, and performance of the caregiver, can positively and negatively affect the effectiveness of DSME. Awareness of these factors means that educators, on the one hand, must consider the limitations and potential and actual capabilities of the patient in planning. It should be noted that DSME is based on group and individual education. The choice of educating form is suggested according to the benefits of the education form and the program's target by examining the selected items.
Conclusion
DSME is an important building block of diabetes treatment. DSME is necessary for diabetes management and behavior change in individuals with diabetes. The results of the studies have found that group education is superior or not different from individual education. DSME should be chosen according to the characteristics of the individuals with diabetes, the purpose of the education, and the advantages and disadvantages of the education method to be selected.
Acknowledgments: -
Ethical Permissions: -
Conflicts of Interests: -
Authors’ Contributions: Chupradit S. (First Author), Methodologist/Main Researcher (20%); Widjaja G. (Second Author), Statistical Analyst/Main Researcher (15%); Khasanah U. (Third Author), Discussion Writer/Assistant Researcher (15%); Tondok S.B. (Forth Author), Introduction Writer/Assistant Researcher (13%); Samal A. (Fifth Author), Assistant Researcher/Discussion Writer (12%); Rahman F.F. (Sixth Author), Introduction Writer/Methodologist (12%); Aravindhan S. (Seventh Author), Statistical Analyst/Assistant Researcher (13%).
Funding/Sources: -
Diagnosis: It is the stage of collecting and interpreting data from the patient about the problems and affecting factors. The diagnostic step in the training process depends on the skill level of the diabetes educator. To diagnose the patient's condition, the diabetes educator collects data from the patient, the patient's family, the patient's social environment, current medical records, and the referral healthcare team in a systematic and organized manner [34, 36].
Goal Setting: The goals of DSME are to strengthen the individual with diabetes, increase self-confidence, improve problem-solving skills and coping behaviors. Therefore, theoretical approaches should facilitate goal-setting regarding patient behavior change, patient empowerment, and patient-centered communication. Theoretical approaches used in DSME include Social Cognitive Theory, Theory of Reasoned Action, Transtheoretical Model, and Theory of Planned Behavior. These theories and models support the patients about the behaviors that patients want to change in diagnosis and help the diabetes educator create the patient's behavior change plan [34]. To achieve the goals in DSME, the cooperation of the patient and the diabetes educator and the participation of the person with diabetes in decisions are important.
Planning: The diabetes educator and the person with diabetes decide together how to reach the set goals. The existing diabetes education practices are integrated into the principles of education and behavior change developed. This plan is coordinated among the diabetes health care team members, the individual with or at risk of diabetes, their families, social support, and referrer [34].
Implementation: During the implementation process, diabetes educators apply diabetes self-management training according to the prepared plan. The diabetes educator counsels patients and their caregivers on the implementation of the DSME plan. Implementation can also be carried out in collaboration with other community and professional services [34].
Assessment: Continuous monitoring and evaluation of the implementation of the prepared plan are important for behavior change. For this reason,
both the training process and whether the predetermined goals have been achieved are evaluated periodically [34].
Individuals with diabetes need to set goals and make daily decisions to manage their diabetes successfully. Individuals with diabetes should be developed to make decisions about their goals, therapeutic options, and self-care behaviors and take responsibility for daily diabetes care to be effective in their care [37].
An example of a protocol for behavioral change in individuals with diabetes, developed by Funnell & Anderson [37], is presented in Table 1.
Table 1) Behavior changes protocol [37]
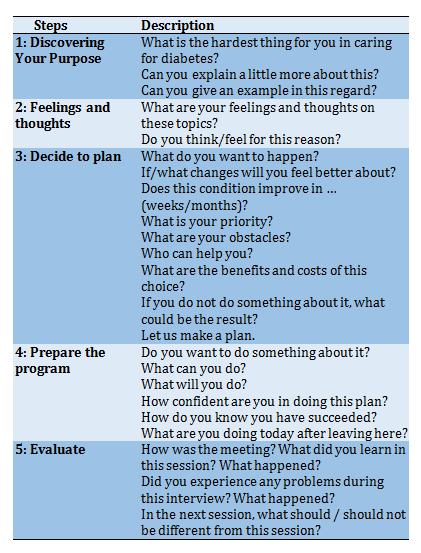
The problem-solving process applied in the behavior change protocol; provides information about diabetes to individuals with diabetes, develops goals related to diabetes and lifestyle, and aims to reach goals [38]. This process consists of five steps. The first two steps describe the problems of individuals with diabetes and their feelings and thoughts about the problems. In the third step, the goals and the patient's preferences are discussed. The patient promises to make behavioral changes that will help them achieve their goals. The fourth step discusses what the patients can do to achieve the goals and evaluate the results. In the fifth step, the educational process is evaluated. In this process, more information about the true nature of the problem will be gained, effective strategies will be developed for individuals with diabetes to cope with, and the barriers and emotions of individuals with diabetes will be learned [37].
Educational strategies can range from simple telephone contact to a comprehensive program, depending on the nature of the situation [39]. There is no single training method and material. Brochures, telephone, posters, slides, books or magazines, the internet, and visual and written media can be used to educate the target audience. However, none of them can replace the one-on-one training provided by diabetes educators. Different methods are used in the education of individuals with diabetes. Individual or group education of health professionals or diabetes educators is the most important education method used in the education of the target group. It should be noted that the DSME can be done by individual education and/or group education method.
Individual Education: Individual education is defined as one-on-one education or face-to-face education. In individual education, it is aimed to provide the appropriate education for the current needs of the individual with diabetes [40]. Communication is more intense in individual education. It is stated that individuals with diabetes express their economic-sexual-social problems and needs more clearly in individual education [40].
Group Education: Teaching people in groups has been an effective form of education for diabetes education since 1970. A group is defined as gathering people with a common interest, such as DSME. The number of participants participating in the groups can vary between 2 and 20. The number of groups depends on the person/organization making the payment, the subject to be discussed, the training method, and the trainers. Studies have found that forming groups of 6-10 people is effective in group education [41].
Why Group Education?
Group education is of great interest among educators and politicians [42]. Some educators prefer group education for their education and recommend using group education as a primary approach to improve outcomes of diabetes [43]. DSME states that it is more effective to do it through group education because it is supportive and encouraging, effective in time and cost, provides sharing experiences, and increases learning with peer interaction. In addition, it is stated that the group education environment supports certain educational activities such as social modeling and problem-based learning better than individual education.
Group education is recommended because it is more suitable for adults' learning styles and has positive results [42, 44]. Considering the principles of adult education, adults need to determine what they want to learn and meet their needs. Adults enjoy small group interaction and practical problem-solving processes, benefiting from other people's experiences. Adults learn as long as they actively participate in the sessions, and if they find the program suitable for them, they will be motivated. Adults are affected by their past experiences in the learning process/behavior change. Therefore, it is difficult for them to change. While physical comfort is important for adults, a pleasant environment and a dynamic environment are important. They enjoy receiving awards such as certificates and gain the courage to learn.
Effectiveness of group education
When we look at the studies comparing group education and individual education to evaluate the effectiveness of group education, it is seen that there are experimental and compilation studies on the subject. In the study of Rickheim et al. [45], in which group education and individual education were compared, the effectiveness of the education program prepared according to DSME standards was evaluated. In both forms of education, the study found that improvements in diabetes knowledge, BMI, quality of life and attitude towards diabetes, and mental health were similar. A decrease in HbA1c levels was detected in the six-month follow-up period in those who received individual and group training. When individual training versus group training was compared, the difference in HbA1c levels was of low statistical significance (marginally greater; p=0.05). In the study, the authors stated the study's limitations as the high losses in their study, the follow-up period of only six months, and the possibility of the results being open to bias because the randomization was not confidential.
Campbell et al. [46] implemented four different interventions in educating individuals with Type 2 diabetes: a minimal group program, an individual program, a comprehensive group program, and an individualized behavior program. The decrease in HbA1c and body mass index was not statistically significant between the groups in the study. However, it has been found that individual and group education have similar effects on the self-care management of individuals with diabetes. The systematic review study of Norris et al. [47] emphasized that group education on lifestyle (physical activity and diet) may have more positive effects than individual education. DSME was found to be effective in both individual and group education. In the meta-analysis study of Norris et al. [48], the effectiveness of diabetes education interventions was examined. The difference between the HbA1c levels of individuals with diabetes who received individual education and group education was not statistically significant.
In a study [49] comparing group education and individual education, the patients who received group education compared to those who received individual education, it was observed that HbA1c level, body mass index, drug dose decreased, retinopathy was less common. HDL cholesterol level increased [49]. In the study of Vadstrup et al. [50], although positive improvements were observed in the quality of life and diabetes symptoms in the groups given individual and group education, this improvement was not statistically significant. No difference was found between the groups. In the study of Llorca et al. [51], diabetes knowledge level improved, HbA1c, body mass index, and systolic blood pressure levels were decreased in groups that received individual and group education. The effects of individual and group training applied in the study were evaluated equally. In the study of Steinsbekk et al. [52] comparing group education with individual education, it was found that group education significantly improved HbA1c, blood glucose levels, lifestyle changes, and psychosocial outcomes of individuals with type 2 diabetes. On the other hand, it was found that there was no statistically significant change in mortality rates, body mass indexes, blood pressure, and lipid profiles of individuals with type 2 diabetes.
Numerous factors affect a patient's achievement of self-management. A review of the present study reveals that various factors, from the effect of age and sex and beliefs of the patient to the attitude, knowledge, skills, and performance of the caregiver, can positively and negatively affect the effectiveness of DSME. Awareness of these factors means that educators, on the one hand, must consider the limitations and potential and actual capabilities of the patient in planning. It should be noted that DSME is based on group and individual education. The choice of educating form is suggested according to the benefits of the education form and the program's target by examining the selected items.
Conclusion
DSME is an important building block of diabetes treatment. DSME is necessary for diabetes management and behavior change in individuals with diabetes. The results of the studies have found that group education is superior or not different from individual education. DSME should be chosen according to the characteristics of the individuals with diabetes, the purpose of the education, and the advantages and disadvantages of the education method to be selected.
Acknowledgments: -
Ethical Permissions: -
Conflicts of Interests: -
Authors’ Contributions: Chupradit S. (First Author), Methodologist/Main Researcher (20%); Widjaja G. (Second Author), Statistical Analyst/Main Researcher (15%); Khasanah U. (Third Author), Discussion Writer/Assistant Researcher (15%); Tondok S.B. (Forth Author), Introduction Writer/Assistant Researcher (13%); Samal A. (Fifth Author), Assistant Researcher/Discussion Writer (12%); Rahman F.F. (Sixth Author), Introduction Writer/Methodologist (12%); Aravindhan S. (Seventh Author), Statistical Analyst/Assistant Researcher (13%).
Funding/Sources: -
Article Type: Analytic Review |
Subject:
Social Health
Received: 2021/08/15 | Accepted: 2021/09/1 | Published: 2021/11/6
Received: 2021/08/15 | Accepted: 2021/09/1 | Published: 2021/11/6
References
1. Williams R, Karuranga S, Malanda B, Saeedi P, Basit A, Besancon S, et al. Global and regional estimates and projections of diabetes-related health expenditure: Results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2020;162:108072. [Link] [DOI:10.1016/j.diabres.2020.108072] [PMID]
2. Karimian M, Gholami A, Farzaei MH, Stefanucci A, Mollica A, Mahmoudi Y, et al. The effect of angipars™ on wound healing in patients with diabetes: A systematic review. J Chem Health Risks. 2020;10(3):195-202. [Persian] [Link]
3. Sharifi A, Shafiei E, Hoseinzadeh M. The study of the effectiveness of a mixture of Arnebia Euochroma and gum extract in animal oils and comparing it with honey in diabetic foot ulcer. J Chem Health Risks. 2019;9(2):167-72. [Persian] [Link]
4. Hu FB. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes Care. 2011;34(6):1249-57. [Link] [DOI:10.2337/dc11-0442] [PMID] [PMCID]
5. Goveia P, Canon-Montanez W, Santos DDP, Lopes GW, Ma RC, Duncan BB, et al. Lifestyle intervention for the prevention of diabetes in women with previous gestational diabetes mellitus: A systematic review and meta-analysis. Front Endocrinol. 2018;9:583. [Link] [DOI:10.3389/fendo.2018.00583] [PMID] [PMCID]
6. Magkos F, Hjorth MF, Astrup A. Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2020;16:545-55. [Link] [DOI:10.1038/s41574-020-0381-5] [PMID]
7. World health organization. Diabetes [Internet]. Geneva: World Health Organization; 2013 [cited 2020, 15 June]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/diabetes. [Link]
8. Al-Mofarji ST, Hussien HK, Mohamed NS, Hantoosh SF, Abass MK, Ali A. The association between gastric bacterial infection and low level of vitamin D among patients with type 2 diabetes mellitus. Baghdad J Biochem Appl Biol Sci. 2021;2(1):38-46. [Link] [DOI:10.47419/bjbabs.v2i01.32]
9. Sonmez A, Demirci I, Haymana C, Tasci I, Dagdelen S, Salman S, et al. Clinical characteristics and outcomes of COVID‐19 in patients with type 2 diabetes in Turkey: A nationwide study (TurCoviDia). J Diabetes. 2021;13(7):585-95. [Link] [DOI:10.1111/1753-0407.13171] [PMID] [PMCID]
10. Mhlanga D, Dunga SH. Determinants of demand for health insurance in South Africa. Int J Soc Sci Hum Stud. 2020;12(2):238-54. [Link]
11. Alkhatatbeh MJ, Abdul Razzak KK. Association between serum 25 hydroxyvitamin D, hemoglobin A1c and fasting blood glucose levels in adults with diabetes mellitus. Biomed Rep. 2018;9(6):523-30. [Link] [DOI:10.3892/br.2018.1159] [PMID] [PMCID]
12. Paul R, Mukkadan JK. Modulation of blood glucose, oxidative stress, and anxiety level by controlled vestibular stimulation in prediabetes. J Nat Sci Biol Med. 2020;11:111-7. [Link]
13. Fasil A, Biadgo B, Abebe M. Glycemic control and diabetes complications among diabetes mellitus patients attending at university of Gondar hospital, northwest Ethiopia. Diabetes Metab Syndr Obes. 2018;12:75-83. [Link] [DOI:10.2147/DMSO.S185614] [PMID] [PMCID]
14. Subber Z, Al-Shamma G, Hashim H. The total and free vitamin D in type 2 diabetes mellitus patients in Baghdad city: Free and total vitamin D. Baghdad J Biochem Appl Biol Sci. 2021;2(2):79-93. [Link] [DOI:10.47419/bjbabs.v2i02.41]
15. Greenwood DA, Gee PM, Fatkin KJ, Peeples M. A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. J Diabetes Sci Technol. 2017;11(5):1015-27. [Link] [DOI:10.1177/1932296817713506] [PMID] [PMCID]
16. Cappon G, Acciaroli G, Vettoretti M, Facchinetti A, Sparacino G. Wearable continuous glucose monitoring sensors: a revolution in diabetes treatment. Electronics. 2017;6(3):65. [Link] [DOI:10.3390/electronics6030065]
17. Powers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, et al. Diabetes self-management education and support in adults with type 2 diabetes: A consensus report of the American diabetes association, the association of diabetes care & education specialists, the academy of nutrition and dietetics, the American academy of family physicians, the American academy of PAs, the American association of nurse practitioners, and the American pharmacists association. J Acad Natr Diet. 2021;121(4):773-88. [Link] [DOI:10.1016/j.jand.2020.04.020]
18. Andersen MB, Bjorkman ASD, Pedersen M, Ekholm O, Molsted S. Social inequality in lifestyle, motivation to change lifestyle and received health advice in individuals with diabetes: A nationwide study. Scand J Public Health. 2020;48(8):847-54. [Link] [DOI:10.1177/1403494819885727] [PMID]
19. Ezenwaka C, Onuoha P, Sandy D, Isreal-Richardson D. Diabetes self-management education in a high-income developing country: Survey of the opinion of nurses and dietitians. Int J Diabetes Dev Ctries. 2013;34(3):163-8. [Link] [DOI:10.1007/s13410-013-0174-7]
20. Strawbridge LM, Lloyd JT, Meadow A, Riley GF, Howell BL. One-year outcomes of diabetes self-management training among medicare beneficiaries newly diagnosed with diabetes. Med Care. 2017;55(4):391-7. [Link] [DOI:10.1097/MLR.0000000000000653] [PMID]
21. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ. 2018;43(5):449-64. [Link] [DOI:10.1177/0145721717722968] [PMID]
22. Felix HC, Narcisse MR, Long CR, English E, Haggard-Duff L, Purvis RS, et al. The effect of family diabetes self-management education on self-care behaviors of marshallese adults with type 2 diabetes. Am J Health Behave. 2019;43(3):490-7. [Link] [DOI:10.5993/AJHB.43.3.4] [PMID]
23. Kueh YC, Morris T, Ismail AAS. The effect of diabetes knowledge and attitudes on self-management and quality of life among people with type 2 diabetes. Psychol Health Med. 2017;22(2):138-44. [Link] [DOI:10.1080/13548506.2016.1147055] [PMID]
24. Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: A narrative review and current innovations. Lancet Diabetes Endocrinol. 2018;6(2):130-42. [Link] [DOI:10.1016/S2213-8587(17)30239-5]
25. Sundaram G, Theagarajan R, Gopalakrishnan K, Babu GR, Murthy GD. Effect of fenugreek consumption with metformin treatment in improving plaque index in diabetic patients. J Nat Sci Biol Med. 2020;11(1):55. [Link] [DOI:10.4103/jnsbm.JNSBM_96_19]
26. Piatt GA, Orchard TJ, Emerson S, Simmons D, Songer TJ, Brooks MM, et al. Translating the chronic care model into the community: Results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006;29(4):811-7. [Link] [DOI:10.2337/diacare.29.04.06.dc05-1785] [PMID]
27. Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: The Starr county border health initiative. Diabetes Care. 2002;25(2):259-68. [Link] [DOI:10.2337/diacare.25.2.259] [PMID] [PMCID]
28. Gucciardi E, DeMelo M, Lee RN, Grace SL. Assessment of two culturally competent diabetes education methods: Individual versus individual plus group education in Canadian Portuguese adults with type 2 diabetes. Ethn Health. 2007;12(2):163-87. [Link] [DOI:10.1080/13557850601002148] [PMID]
29. Surucu HA, Kizilci S, Ergor G. The impacts of diabetes education on self-care agency, self-care activities and hbA1c levels of patients with type 2 diabetes: A randomized controlled study. Int J Caring Sci. 2017;10(1):479. [Link]
30. Joslin EP, Kahn CR. Joslin's Diabetes Mellitus. Philadelphia: Lippincott Williams & Wilkins; 2005. [Link]
31. Dunning T. The complex and constantly evolving role of diabetes educators. Diabetes Voice. 2007;52:9-11. [Link]
32. Reagan L, Pereira K, Jefferson V, Evans Kreider K, Totten S, D'Eramo Melkus G, et al. Diabetes self-management training in a virtual environment. Diabetes Educ. 2017;43(4):413-21. [Link] [DOI:10.1177/0145721717715632] [PMID]
33. Hessler DM, Fisher L, Bowyer V, Dickinson LM, Jortberg BT, Kwan B, et al. Self-management support for chronic disease in primary care: Frequency of patient self-management problems and patient reported priorities, and alignment with ultimate behavior goal selection. BMC Fam Pract. 2019;20(1):120. [Link] [DOI:10.1186/s12875-019-1012-x] [PMID] [PMCID]
34. Parkin C, Ms D, Hinnen V, Valentine C, Cde BA, Rice D, et al. AADE guidelines for the practice of diabetes self-management education and training (DSME/T). Diabetes Educ. 2009;35 Suppl 3:1-63. [Link] [DOI:10.1177/0145721709352436]
35. Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS. Users' preferences and design recommendations to promote engagements with mobile apps for diabetes self-management: Multi-national perspectives. Plos One. 2018;13(12):0208942. [Link] [DOI:10.1371/journal.pone.0208942] [PMID] [PMCID]
36. Chow CK, Ramasundarahettige C, Hu W, AlHabib KF, Avezum Jr A, Cheng X, et al. Availability and affordability of essential medicines for diabetes across high-income, middle-income, and low-income countries: A prospective epidemiological study. Lancet Diabetes Endocrinol. 2018;6(10):798-808. [Link] [DOI:10.1016/S2213-8587(18)30233-X]
37. Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clin Diabetes. 2004;22(3):123-7. [Link] [DOI:10.2337/diaclin.22.3.123]
38. Oster E. Diabetes and diet: Purchasing behavior change in response to health information. Am Econ J Appl Econ. 2018;10(4):308-48. [Link] [DOI:10.1257/app.20160232] [PMID] [PMCID]
39. Phillips BE, Kelly BM, Lilja M, Ponce-Gonzalez JG, Brogan RJ, Morris DL, et al. A practical and time-efficient high-intensity interval training program modifies cardio-metabolic risk factors in adults with risk factors for type II diabetes. Front Endocrinol. 2017;8:229. [Link] [DOI:10.3389/fendo.2017.00229] [PMID] [PMCID]
40. Vandenbosch J, Van Den Broucke S, Schinckus L, Schwarz P, Doyle G, Pelikan J, et al. The impact of health literacy on diabetes self-management education. Health Educ J. 2018;77(3):349-62. [Link] [DOI:10.1177/0017896917751554]
41. Adam L, O'Connor C, Garcia AC. Evaluating the impact of diabetes self-management education methods on knowledge, attitudes and behaviours of adult patients with type 2 diabetes mellitus. Can J Diabetes. 2018;42(5), 470-7. [Link] [DOI:10.1016/j.jcjd.2017.11.003] [PMID]
42. Mensing CR, Norris SL. Group education in diabetes: effectiveness and implementation. Diabetes Spectr. 2003;16(2):96-103. [Link] [DOI:10.2337/diaspect.16.2.96]
43. Adolfsson ET, Smide B, Gregeby E, Fernstrom L, Wikblad K. Implementing empowerment group education in diabetes. Patient Educ Couns. 2004;53(3):319-24. [Link] [DOI:10.1016/j.pec.2003.07.009] [PMID]
44. Deakin TA, McShane CE, Cade JE, Williams R. Group based training for self‐management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2(2):3417. [Link] [DOI:10.1002/14651858.CD003417.pub2] [PMID]
45. Rickheim PL, Weaver TW, Flader JL, Kendall DM. Assessment of group versus individual diabetes education: A randomized study. Diabetes Care. 2002;25(2):269-74. [Link] [DOI:10.2337/diacare.25.2.269] [PMID]
46. Campbell EM, Redman S, Moffitt P, Sanson-Fisher RW. The relative effectiveness of educational and behavioral instruction programs for patients with NIDDM: A randomized trial. Diabetes Educ. 1996;22(4):379-86. [Link] [DOI:10.1177/014572179602200412] [PMID]
47. Norris SL, Engelgau MM, Narayan KV. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561-87. [Link] [DOI:10.2337/diacare.24.3.561] [PMID]
48. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159-71. [Link] [DOI:10.2337/diacare.25.7.1159] [PMID]
49. Trento M, Passera P, Bajardi M, Tomalino M, Grassi G, Borgo E, et al. Lifestyle intervention by group care prevents deterioration of Type II diabetes: A 4-year randomized controlled clinical trial. Diabetologia. 2002;45(9):1231-9. [Link] [DOI:10.1007/s00125-002-0904-8] [PMID]
50. Vadstrup ES, Frolich A, Perrild H, Borg E, Roder M. Health-related quality of life and self-related health in patients with type 2 diabetes: Effects of group-based rehabilitation versus individual counselling. Health Qual Life Outcomes. 2011;9:110. [Link] [DOI:10.1186/1477-7525-9-110] [PMID] [PMCID]
51. Llorca MR, Bernal GG, Martin CA, Galindo PA. Group versus individual education for type-2 diabetes patients. Aten Primaria. 2003;32(1):36-41. [Spanish] [Link] [DOI:10.1016/S0212-6567(03)78854-4]
52. Steinsbekk A, Rygg L, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res. 2012;12:213. [Link] [DOI:10.1186/1472-6963-12-213] [PMID] [PMCID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |