Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 103-110 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Akbarzadeh O, Golzad H, Moshashaei P. Health Promotion Model Insights on Determinants of Personal Protective Equipment Use in Occupational Settings. Health Educ Health Promot 2025; 13 (1) :103-110
URL: http://hehp.modares.ac.ir/article-5-79043-en.html
URL: http://hehp.modares.ac.ir/article-5-79043-en.html
1- Department of Occupational Health and Safety, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran
2- Department of Design and Built Environment, School of Design and Built Environment, University of Canberra, Canberra, Australia
2- Department of Design and Built Environment, School of Design and Built Environment, University of Canberra, Canberra, Australia
Keywords: Personal Protective Equipment [MeSH], Health Promotion [MeSH], Occupational Exposure [MeSH], Patient Compliance [MeSH]
Full-Text [PDF 777 kb]
(470 Downloads)
| Abstract (HTML) (847 Views)
Full-Text: (35 Views)
Introduction
In hazardous work environments, workers prioritize their protection against potential risks. At the same time, they develop a heightened sense of vulnerability due to prolonged exposure to these risks. This refers to increased awareness of potential dangers, which may lead to greater caution or stress over time [1]. Their behaviors and decision-making processes reflect this heightened risk awareness, underscoring the need for effective protective measures [2]. Additionally, the perception of safety is crucial in influencing workers’ well-being, productivity, and adherence to safety protocols [3]. Therefore, creating environments where workers feel safe and healthy is essential. By providing appropriate training and support, perceptions of safety risks stemming from exposure to health and safety hazards can be mitigated, leading to safer and more productive workplaces [4, 5].
Working in hazardous situations, such as extreme noise, heat stress, and radioactivity, can put workers at risk of developing severe occupational diseases. In recent years, the number of occupational disease cases has increased, with noise-induced deafness, musculoskeletal disorders, and skin diseases being among the most prevalent. These rising cases highlight the critical role of personal protective equipment (PPE) in mitigating occupational health risks [6-8]. Such alarming statistics emphasize the importance of PPE as a preventive measure in reducing the prevalence of occupational diseases, particularly in high-risk industrial sectors. Despite the availability of preventive measures, including PPE, occupational diseases continue to pose a significant challenge in high-risk industries [9]. This underscores the necessity of identifying key determinants influencing PPE adherence and addressing barriers to its proper use.
Previous research has extensively examined workplace hazards and the importance of PPE; however, significant gaps remain in understanding the specific factors affecting compliance in different occupational settings. Additionally, exposure to multiple workplace hazards, such as heat stress and chemical agents, can amplify health risks, emphasizing the necessity of effective control measures and PPE usage [10, 11].
While risk management measures, like elimination and engineering controls, are preferred, their implementation is often limited by budget constraints, poor supervision, and workplace restrictions. In such cases, PPE is the last defense against occupational diseases [12-14]. Although PPE may not be as effective as engineering controls, it offers a significant layer of protection when other safety procedures fail [15, 16]. These essential tools act as a shield, protecting workers from potential hazards and decreasing the likelihood of injury or illness. Depending on the risks present in a workplace, PPE can consist of a range of items tailored to those risks [17, 18].
Despite existing studies on PPE compliance, there is still a need for deeper investigation into the specific personal, organizational, and situational determinants influencing its utilization. In many workplaces, while production workers may use PPE, it is not uncommon to see some of them using equipment unsuitable for the specific risks they are exposed to [19]. This could be due to a lack of appropriate training [20], misinterpretation of the hazards involved [21], or even the inaccessibility of the right type of PPE [22]. Moreover, using inappropriate PPE can significantly diminish its effectiveness, leaving employees vulnerable to the health and safety risks they encounter [23].
PPE compliance is influenced by workers’ perceptions of safety, personal attitudes, and social factors such as peer support and organizational policies [24]. Common barriers include discomfort, poor fit, and the belief that PPE interferes with work [25, 26]. However, many previous studies have not provided comprehensive solutions to these challenges, underscoring the necessity for further research that identifies practical strategies to enhance PPE compliance.
Some workers might even think PPE is unnecessary if they do not perceive immediate risks or believe the benefits do not justify the hassle [27]. Wong et al. [17] suggest that by understanding and addressing these obstacles, we can encourage more regular use of PPE, ultimately leading to a safer work environment for everyone [28]. Additionally, when workers perceive that PPE makes their workplace safer and helps prevent incidents, they are more likely to be motivated to use it regularly. However, if they find the PPE uncomfortable or inconvenient, they may be less inclined to use it [29].
Furthermore, using PPE is shaped by several other key issues that can significantly influence workplace safety, including how employees perceive risk, their age and experience, and whether the employer provides the proper PPE. When businesses ensure that their workforce has access to appropriate protective gear, it becomes easier for them to adhere to safety regulations. Ultimately, these elements all work together to improve workplace safety. Beyond worker-related factors, a study by Larson & Liverman [30] demonstrates that organizational factors are also significant in the level of PPE usage among workers. A study by Sarfraz et al. shows that factors such as PPE availability, gear quality, workplace safety policies, and safety training all play a significant role [31].
Experienced workers are more aware of the importance of PPE due to their familiarity with workplace hazards. In contrast, younger or new employees often require additional training and supervision to enhance compliance [32]. This underscores the need for tailored safety programs that address the varying levels of awareness and compliance across different experience levels within the workforce [33, 34]. By exploring these multifaceted influences, this study aims to provide a deeper understanding of the determinants of PPE utilization, ultimately guiding the development of tailored interventions for diverse workplace settings. By explicitly addressing the gaps in previous studies, this research aims to provide new insights into the determinants of PPE utilization, ultimately guiding the development of targeted interventions to improve adherence in high-risk workplaces.
Many studies have highlighted a strong association between wearing PPE and the health promotion model (HPM). Items like masks and gloves protect hazardous materials and infectious agents, reducing the risk of illness or injury. The HPM focuses on encouraging preventive health behaviors by emphasizing the importance of PPE usage as a key strategy in mitigating health risks. Whether in healthcare settings, workplaces, or daily routines, PPE is a fundamental component of the HPM’s approach to proactive health management, ensuring individual and societal well-being. By promoting consistent and proper PPE use, the HPM helps reduce exposure to hazardous conditions, preventing illness and injury. This approach enhances workplace safety and fosters a culture of prevention and resilience in public health [35-37].
Several research studies have investigated the use of the HPM in improving PPE adherence among workers, especially in industrial settings. Khoshakhlag et al., involving small and medium enterprises found that workers’ attitudes toward PPE and workplace safety training are strong predictors of PPE use. Workers with safety training are significantly more likely to use PPE consistently. The primary barriers to PPE utilization include lack of availability, poor comfort, and inadequate training [38]. In another study conducted among construction workers, factors such as government oversight, the provision of safety briefs, and PPE training substantially increase the likelihood of PPE use [39]. Thus, applying the HPM through targeted interventions, such as workplace safety education and regular training, can effectively increase PPE adherence and reduce occupational hazards.
In another study, the application of the HPM is linked to better PPE usage in hazardous industries, such as mining. In the mentioned study, the model was used to develop interventions focusing on perceived barriers and benefits, risk perception, and self-efficacy [40]. Additionally, the COVID-19 pandemic led to increased focus on PPE usage in healthcare settings [41]. La Torre et al.'s study indicates that the use of PPE is associated with a 70% reduction in SARS-CoV-2 infections among healthcare workers, reinforcing the need for proper education and behavioral interventions based on the HPM to improve consistent PPE use in various industries [42].
Studies have shown that the HPM improves workers’ understanding, attitudes, and behaviors toward safety and PPE use, highlighting knowledge, perceived benefits, and self-efficacy [43]. A study conducted in small and medium-sized enterprises (SMEs) found that workers’ attitudes and risk perceptions significantly affect PPE usage. The study emphasized the significance of training interventions to enhance knowledge and positively shape workers’ perspectives toward PPE, merging these factors to achieve higher compliance rates [44]. Additionally, a study on construction employees in Addis Ababa, Ethiopia, underlined that elements, such as the availability of safety training and knowledge of PPE use, are crucial in boosting usage rates. Employees who receive safety training are up to four times more likely to use PPE than those who do not. This study also highlighted the role of external enforcement, such as government supervision, in reinforcing PPE compliance [39]. A study conducted by Alinejad et al. applies the health belief model (HBM) to examine how training can improve PPE compliance in healthcare settings. The HBM is introduced here because it highlights psychological factors, such as the perceived severity of health risks and perceived barriers to compliance, which influence individuals’ decisions to use PPE. This contrasts with the HPM, which takes a broader approach by promoting preventive health behaviors as a proactive and structured strategy. While the HBM focuses on personal risk perception and motivational barriers, the HPM emphasizes systematic and organizational measures to embed PPE use within daily routines [45]. These studies highlight health models' practical and theoretical applications in improving PPE adherence, which is crucial for understanding its determinants in various industries [46, 47].
The HPM provides a practical framework for addressing the research gap and understanding the integrated influence of personal and situational factors on PPE usage across various workplace settings. While previous studies focus narrowly on individual compliance or organizational safety practices, few investigate how these factors shape PPE utilization. This study uniquely bridges the gap by examining individual, interpersonal, and organizational dynamics, offering a holistic understanding of the factors influencing PPE adherence in complex workplace environments.
Guided by the main elements of the HPM, this study examined the interplay between employees’ characteristics (such as experience and risk perception) and organizational factors (like PPE availability and safety training), offering an integrated perspective. The originality of this study also lies in its focus on workers in major companies that have established international standards for safety and health, such as ISO 45000, ISO 45001, ISO 14001, and HSE-MS. This provides a unique perspective on PPE usage in settings with progressive occupational health protocols where workers are exposed to highly hazardous chemical materials such as BTEX (Benzene, Toluene, Ethylbenzene, and Xylene) compounds.
Focusing on organizations with advanced safety standards highlights best practices and uncovers persistent challenges, providing valuable lessons for less-regulated settings. By investigating PPE compliance within companies that are already committed to high safety and health measures, this research presented insights into how even well-regulated environments face challenges related to interpersonal and organizational characteristics. This context enhances our understanding of PPE usage beyond regulatory adherence, underscoring the nuanced factors of employee behavior and interaction that can affect safety and health practices even in optimal circumstances.
The findings are expected to inform policymakers and industry leaders in designing more effective, tailored interventions that enhance PPE adherence, even in high-risk and well-regulated industries. Through this approach, the study aims to identify targeted procedures to improve PPE adherence by considering interpersonal, situational, and organizational dynamics across different industries.
Instrument and Methods
Theoretical framework
The HPM [48] provided a theoretical framework for our study, which includes three main stages, including modifying factors, cognitive-perceptual factors, and health-related behaviors (using PPE). These stages are particularly relevant to our study, as they offer a structured approach to understanding how various influences shape PPE compliance in occupational settings. The model suggests that modifying characteristics, including demographic factors, peer support, and organizational culture, indirectly shape health-related behaviors by influencing cognitive-perceptual factors, such as perceived benefits, barriers, self-efficacy, and susceptibility. These cognitive-perceptual factors are central to individual decision-making, as they determine whether a worker believes PPE use is beneficial, whether they perceive significant obstacles to its use, how confident they feel in using PPE correctly, and how vulnerable they think they are to workplace hazards [49]. This is crucial in our context, as PPE compliance is not only a matter of knowledge but also depends on workplace culture, individual motivation, and perceived risks. By incorporating external influences and individual decision-making processes, the HPM provides a more comprehensive approach than other frameworks, such as the knowledge, attitude, and practice (KAP) model [50] or the contextual framework. Unlike the KAP model, the HPM integrates organizational and personal factors, making it well-suited for evaluating health-related behaviors, like PPE use in occupational settings [51]. In addition, organizational factors, such as workplace policies, safety climate, and managerial support, create an environment that either facilitates or hinders PPE compliance [52]. Simultaneously, personal factors, including perceived self-efficacy, perceived risk, and individual motivation, directly influence a worker’s willingness to adhere to PPE guidelines [53]. The interaction between these factors is critical, as PPE use is not solely an individual decision but is shaped by the broader organizational culture [54]. By incorporating both levels of influence, the HPM provides a comprehensive understanding of the determinants of PPE adherence, making it a more robust framework for analyzing workplace health behaviors.
Procedure and participants
This descriptive-analytical study, conducted in 2024, was based on a positivist research philosophy, carried out with samples selected from three industrial businesses with higher exposure rates to occupational diseases. Furthermore, these companies strictly comply with internationally recognized occupational safety and health standards, such as OHSAS 18001, ISO 45003, and HSE-MS, ensuring a strong framework for managing workplace hazards. Compliance with these standards indicates a commitment to sustaining high levels of safety and health management, providing a consistent approach across industries to decrease occupational risks and enhance worker well-being. In addition, positivism was applied to systematically analyze the quantitative factors influencing PPE usage [55]. By employing a structured methodological approach, we used measurable data to examine the associations between personal and situational factors and PPE compliance. The positivist approach ensures objectivity in data collection and analysis, reducing bias and enabling the generation of replicable and generalizable findings [56]. This methodological framework allows for the identification of key determinants affecting PPE use, providing empirical insights that can inform workplace health and safety policies [57]. This approach supports the study’s objective of determining reliable predictors of PPE adherence that can be applied across diverse industrial environments, offering precise, actionable insights to enhance workplace safety. Green’s advocacy [58] for incorporating transformative perspectives highlights the importance of investigating not only individual compliance but also the social and organizational contexts that shape safety behaviors. This process complements the HPM by suggesting that promoting supportive interpersonal and organizational environments may play an equally crucial role in improving PPE adherence. The data collection process was informed by the results of a pilot study survey [59]. Before the main study, the questionnaire was pilot-tested with a small group of workers from similar industries to evaluate its clarity and comprehension. This pilot test involved 40 participants who were asked to complete the questionnaire, provide feedback, and comment on the wording and structure of the questions.
The feedback highlighted several areas for improvement. Some technical terms were simplified to ensure accessibility for participants with varying education levels, and ambiguous phrasing in a few questions was clarified. Additionally, response scales were adjusted to enhance consistency and ease of interpretation. Based on these insights, adjustments were made to improve the clarity of the questions, ensuring participants with different levels of education and language proficiency easily understood them. These refinements helped enhance the questionnaire’s reliability and validity for the main study.
This pilot testing procedure not only improved the reliability of the questionnaire but also helped ensure that the questions effectively captured the intended information regarding PPE usage. Therefore, the final version of the questionnaire was refined and used for data collection in the main study. Considering a confidence level of 95%, d=0.05, and SD=0.47, using Z2α/2=(1.96)2 formula, the sample size was estimated at 340 persons.
This is the Z-score associated with a 95% confidence level. The Z-score corresponds to the number of standard deviations a data point is from the mean. For a 95% confidence level, the Z-score is 1.96, meaning that 95% of the data lies within 1.96 standard deviations from the mean in a normal distribution. The confidence level was 95%, indicating that 95% of the confidence intervals generated would contain the true population parameter if the same study were repeated numerous times. It is a common standard in research, reflecting a high degree of certainty. We regarded d=0.05 as the margin of error (denoted as d). In this case, it is 0.05, meaning the results are expected to be within ±5 percentage points of the true population value. It sets an acceptable level of precision for your estimate. The standard deviation (SD) measures how spread the data points are around the mean. A value of 0.47 indicates moderate variability in the data. Standard deviation is essential for understanding the variation in the data, which influences sample size requirements. The formula offers simplicity and accuracy in calculating sample size for quantitative studies by directly accounting for the confidence level, data variability, and desired precision. It ensures flexibility, allowing researchers to adjust the sample size based on study requirements while maintaining the desired confidence level. Additionally, it helps optimize resources by determining a sample size large enough to produce reliable results without being unnecessarily large.
The selection of participants from each company was based on the relative size of their workforces. The number of employees chosen from each organization reflects the number of workers in those companies, ensuring that our sample is representative of the broader workforce dynamics. Specifically, 120 employees were selected from the paint industrial plant, 100 from the plastic production company, and 120 from the petrochemical company. This distribution was designed to capture diverse experiences and exposure to PPE use in different manufacturing environments. By maintaining proportional representation, we aimed to ensure that the findings accurately reflect workers' practices and challenges in each sector. Additionally, this approach allows for a more comprehensive understanding of how PPE usage may vary across different industries, enhancing the study's overall validity.
The random sampling method was conducted systematically to ensure that each worker had an equal opportunity to participate. A comprehensive list of all employees from each company was obtained, and a random number generator was employed to choose participants from this list.
For the paint industrial plant and the petrochemical company, which had larger worker counts, we first ensured that the total number of workers was well-documented. After obtaining the worker list, we assigned a unique identification number to each worker. Then, using the random number generator, we established the required number of participants—120 from the paint plant and 120 from the petrochemical company.
In the case of the plastic production company, which had a smaller workforce, we directly randomized the employee IDs using the same random number generator until we achieved the target of 100 participants. This process provided an unbiased selection and ensured that our sample was representative of the workforce across the three industries.
By employing this random sampling method, we aimed to eliminate selection bias and improve the generalizability of our results across various manufacturing settings.
The participants were selected from workers working on the production line for over a year. As a selection criterion, participants must have worked on the production line for more than one year to ensure adequate experience, knowledge, and familiarity with the workplace environment, safety regulations, and potential hazards in their workplace. They had consistent exposure to organic solvents. This consistent exposure ensured that the study focuses on workers who face relevant occupational risks, providing a significant context for examining PPE usage and adherence. By choosing participants with regular contact with hazardous materials, the study could more accurately evaluate the factors that affect protective equipment utilization in high-risk environments. They also completed the research consent form and had access to the required PPE, indicating that workers were required to use PPE appropriate for their specific working and ergonomic conditions. However, this requirement was always observed in all companies adhering to international safety and health standards.
The study excluded workers who could not read or answer the questionnaire due to poor language skills. For those with lower levels of education, the research team read the questionnaire clearly to ensure that all participants fully understood the questions.
Before data collection, we received ethical approval from the Tabriz University of Medical Sciences. This approval ensured that all research activities adhered to ethical standards and protected the rights of participants.
To ensure participant confidentiality, responses were anonymized by removing identifying information and assigning unique ID numbers. All data were securely stored in a password-protected database accessible only to the research team. Reports and publications will present aggregated data to further protect individual identities. Participants were required to sign an informed consent document clearly outlining their rights, including the option to withdraw from the research at any time without repercussions. These ethical considerations were integral to the study design, ensuring that participant rights were respected and that the research adhered to ethical research practices.
At the sampling sites, the authors clarified the study’s purpose in clear and simple terms. They then distributed the questionnaires to the employees and collected them once completed. This careful and respectful approach guaranteed that every worker understood the study and contributed their experiences, leading to more accurate and meaningful results.
Measures
The primary data collection method was a questionnaire survey designed to assess PPE adherence among workers. The questionnaire was developed based on the studies of Lu et al. [60] and Nichol et al. [61] and was structured to evaluate various factors influencing PPE usage. To ensure its accuracy and consistency, researchers assessed its validity and reliability, confirming that the tool effectively measures PPE adherence while maintaining stable results across different instances.
The questionnaire consisted of five sections, including personal demographic information, additional individual factors, interpersonal influences, organizational or situational elements, and the usage of PPE. The first section collected demographic details, such as gender, age, work experience, marital status, education level, and exposure duration to organic solvents.
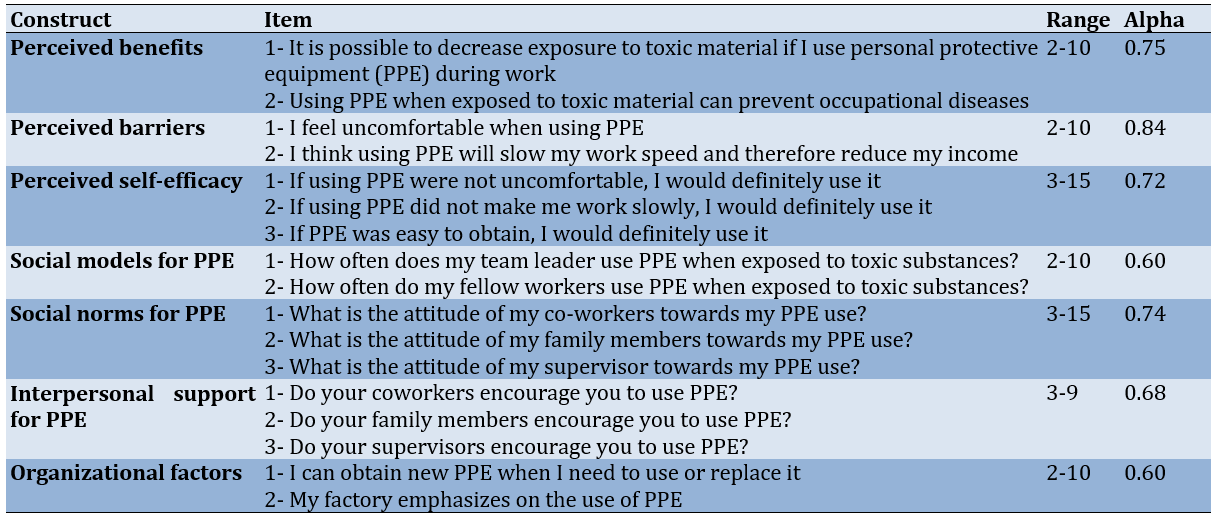
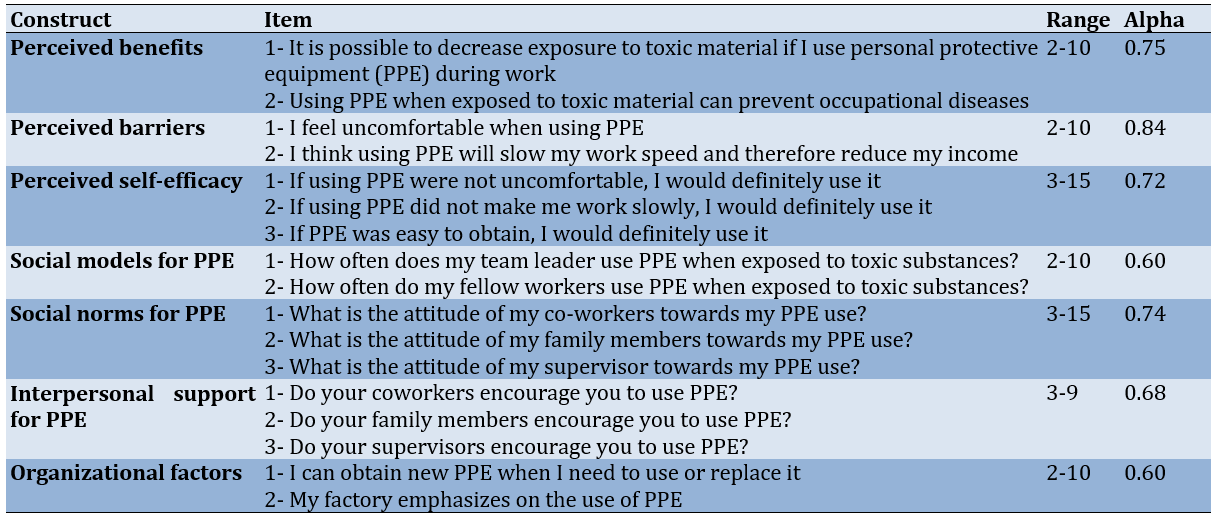
The remaining four sections (Table 1) were grounded in the HPM (Figure 1), which served as the theoretical foundation for this study. These sections explored personal, social, and organizational factors influencing PPE adherence, offering a broader perspective on occupational safety decision-making. According to the HPM, modifying factors, such as demographic characteristics and interpersonal influences, indirectly shape cognitive-perceptual elements, which ultimately drive health-related behaviors [62]. The second section of the questionnaire examined personal factors influencing PPE compliance, including perceived benefits of PPE use (two questions), barriers to PPE adherence (two questions), and self-efficacy in PPE use (three questions). Participants responded using a five-point Likert scale. The third section focused on social influences, assessing how role models (two questions), social norms (three questions), and peer support (three questions) impact PPE adherence. Participants also responded using a five-point Likert scale for consistency. The fourth section evaluated organizational factors affecting PPE compliance, particularly PPE accessibility and the organization’s commitment to enforcing PPE use.
Finally, the last section assessed actual PPE adherence, specifically using protective face masks and gloves. Participants answered questions such as, “How often do you wear a protective face mask during work?” and “How often do you wear protective gloves while working?” to measure their compliance with PPE guidelines.

Figure 1. Conceptual framework of the health promotion model (HPM)
Table 1. Questionnaire construct items
Statistical analysis
We examined the reliability of the questionnaire by assessing its internal consistency using Cronbach’s Alpha. According to Sørensen and Slater’s study, an alpha coefficient of 0.60 or higher indicates that the measure is reliable [63]. Our scales for perceived benefits (Table 1), barriers, self-efficacy, social modeling, social norms, interpersonal support, and organizational factors all met this standard, with alpha coefficients ranging from 0.60 to 0.84. We also evaluated the normality of our numeric variables using the Kolmogorov-Smirnov test. We presented our data as means and standard deviations for normally distributed numeric variables and medians with ranges for non-normal ones. In contrast, categorical data were shown as frequencies and percentages. To associate health promotion measures between those who wear PPE (like face masks or gloves) and those who do not, we used chi-square tests for categorical data and t-tests for normally distributed continuous data. A p-value of 0.05 or less was considered statistically significant [64].
Finally, we used a two-level logistic regression model to identify how different factors affected the use of PPE in the workplace while adjusting for individual demographics. In the current research, we employed a two-level logistic regression model because it accounts for the hierarchical structure of the data, such as individuals nested within groups (e.g., patients in clinics). This model captures individual and group-level variations, handling unobserved heterogeneity at the group level while accounting for clusters' correlations. Using logistic regression is suitable for binary outcomes (e.g., health behaviors), providing more accurate estimates and improving the model’s fit compared to single-level approaches. This results in more reliable and interpretable outcomes in contexts where individual and group-level elements affect results [65]. We considered results with p-values under 0.05 significant [66].
Cronbach’s alpha values were calculated, as presented in Table 1, to assess the reliability of the scales used in this study. Cronbach’s alpha is widely used to measure internal consistency, reflecting the degree to which items within a scale correlate with each other, thereby demonstrating that they collectively assess the same underlying construct. Typically, alpha values above 0.5 are considered acceptable, suggesting adequate reliability, whereas values exceeding 0.7 are considered a solid reliability indicator. In this context, Cronbach’s alpha values help confirm that the variables included are suitable for further analysis and reliably represent factors influencing PPE usage.
For the analysis of categorical variables, we employed logistic regression, a statistical method designed to model binary outcomes. Logistic regression is particularly useful in this study as it allows us to estimate the probability of PPE compliance as influenced by various predictor variables, such as interpersonal and organizational factors. This approach provides an understanding of how each independent variable contributes to the likelihood of PPE usage, yielding insights that can support targeted interventions to improve compliance in industrial settings. Data analysis was done using SPSS 26.
Findings
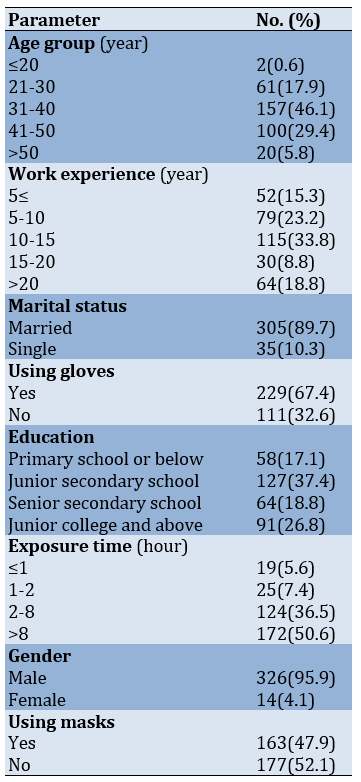
Most workers were men (95.9%), and most were married (89.7%). Approximately half were in their 30s, particularly aged 31 to 40 (46.1%), and had been employed for 10 to 15 years, indicating a fairly experienced group. In terms of education, a significant portion had completed junior secondary school (37.4%), providing insight into their academic situation. Over half were exposed to their work environment for over 8 hours daily (50.6%), indicating extended work shifts. While most workers took precautions by wearing protective gloves (67.4%), more than half did not use face masks (52.1%). This pattern indicates a gap in protective practices, especially concerning safeguarding against airborne hazards. These findings emphasize the need for continued attention to safety measures in the workplace (Table 2).
Table 2. Frequency of samples’ characteristics
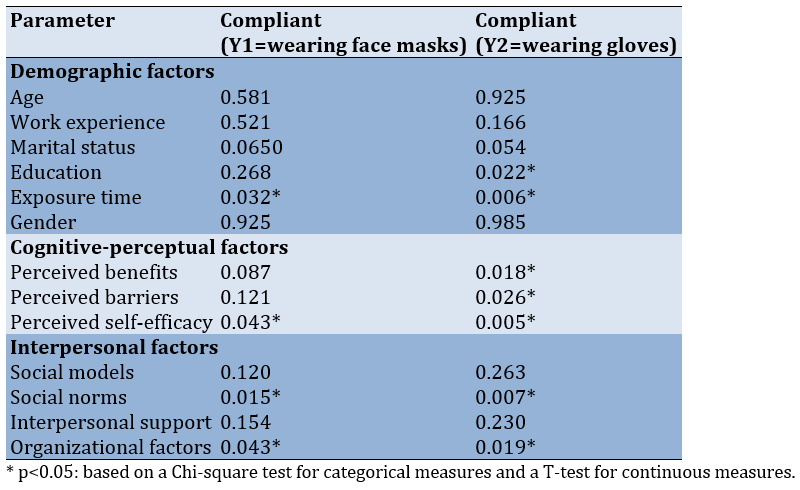
The Chi-square test and t-test revealed that the education level was closely associated with the probability of wearing protective gloves. Moreover, the time workers are exposed to hazards played a significant role in whether they used face masks and gloves (p<0.05). Regarding cognitive and perceptual factors, individuals who perceived clear benefits and encountered barriers in their work environment were more likely to use gloves. Additionally, those who felt confident in their ability to protect themselves were more inclined to use both types of PPE (p<0.05). Social norms, commonly accepted in one’s social circle, were particularly influential in encouraging the use of face masks and gloves. Lastly, organizational factors significantly influenced PPE usage (p<0.05; Table 3).
Table 3. Relationship between compliance with the use of personal protective equipment (PPE) and individual demographics, cognitive-perceptual, interpersonal, and situational factors
In the next stage, we developed a two-level logistic regression model that involved several explanatory variables. Gender affected whether workers were likely to wear face masks and protective gloves. After considering differences in demographics, the interpersonal factors from the HPM emerged as the most important drivers for PPE use. In contrast, cognitive-perceptual factors did not appear to have much impact. Upon closer examination, interpersonal support and organizational factors were only associated with using gloves. For face mask use, workers with higher scores in social support networks were significantly more likely to use them, with an odds ratio of 3.51 (95% CI: 1.23-1.50). On the other hand, regarding gloves, organizational factors were a powerful predictor, with a higher score in this area leading to an odds ratio of 3.15 (95% CI: 1.12-1.15) for increased use. Individuals’ PPE habits were influenced differently depending on the type of PPE. Social factors enhanced face mask usage, while workplace or organizational support had a greater effect on whether someone wore protective gloves (Table 4).
Table 4. Factors associated with personal protective equipment (PPE) use

Discussion
This study assessed how the HPM model can help predict workers’ attitudes toward using PPE. By examining specific factors, we demonstrated that the model could predict and provide a deep understanding of how PPE is being used in the workplace. Similar studies have verified these findings [25, 67, 68], in which the HPM model has also been employed to understand PPE use among workers. These studies emphasize the importance of using predictive models to improve workers’ safety and health.
When the right PPE is chosen and used properly, it can help reduce workplace accident rates, occupational exposure, and the severity of potential risks. Properly using PPE is imperative to improving worker safety and decreasing the likelihood of serious harm on the job [25, 69]. There is little information about the use of PPE among workers, but our findings show that only a few workers use PPE. Shamsi et al.'s study on attitudes and behaviors related to using PPE among subway construction station employees showed that using PPE by the staff is not desirable [70]. This study provides practical insights into the attitudes and behaviors affecting PPE usage among construction workers, underscoring the significance of audience analysis for developing effective behavior change interventions. Their findings emphasize that organizational culture, perceived risk, and the availability of PPE significantly impact compliance, aligning with the elements of the HPM in our study. Additionally, another study by Moshashaei et al. showed that clothing components and other PPE, such as masks, with a score below 20%, among the most undesirable components of safety and health [18]. Another study conducted by Sehsah et al. among construction workers demonstrated that safety and health training can improve workers’ attitudes and beliefs toward using PPE, which can subsequently affect occupational accidents and injuries. Furthermore, the authors noted that the main reasons for not using PPE are a lack of knowledge and fitting problems related to worker posture [71]. The results of this study are in line with our findings. Mahmood et al.'s study emphasizes the importance of proper training for healthcare workers in donning, doffing, and safely handling PPE to minimize the risk of self-contamination [72]. The results of their study align with our findings regarding the use of the HPM to adopt proper training to promote PPE usage among employees.
Many workers have stated that PPE tends to decrease efficiency and slow down work. In some cases, they find PPE annoying or restrictive, which makes it difficult for workers to move easily and reduces their performance. This view demonstrates the ongoing challenge of ensuring safety while also improving productivity. Several studies have confirmed these findings [68, 73, 74]. About 25% of academic workers had inadequate access to PPE due to economic and financial limitations. This issue is prevalent in many companies with limited financial margins; nevertheless, they still try to provide sufficient safety equipment [75]. Not only does this put workers’ health at risk, but it also highlights the broader challenge of ensuring worker safety in the face of economic pressures. These findings are consistent with several studies [76-78]. Here, utilization rates for face masks were 47.9%, while gloves were 67.4%. Previous studies have found the compliance rate for PPE use to be between 40% and 70% [79, 80]. Additionally, Lu et al.'s research showed that 54% of individuals use face masks and 77% use gloves, similar to our utilization rates. Face masks are used less than gloves due to the inadequate supply of face masks and presumably the discomfort associated with wearing one [60]. While our findings indicate high compliance with glove usage, the relatively lower face mask compliance warrants further exploration.
Several factors may contribute to this gap in face mask usage. First, the perceived risk associated with the tasks performed may affect employees’ attitudes toward PPE. For instance, if employees believe that their primary exposure risks are linked to skin contact rather than inhalation of hazardous substances, they may prioritize gloves over masks. This perception could arise from insufficient education or communication regarding hazardous organic solvents' specific health and safety hazards [81, 82].
Second, comfort and convenience play a vital role in PPE compliance. Face masks can often be perceived as uncomfortable, particularly during prolonged use, leading employees to forgo them in favor of gloves, which are generally easier to wear and adjust. Employers should consider evaluating the types of masks provided to ensure they are comfortable and appropriate for the tasks [83].
Finally, social influences and workplace culture may impact PPE adherence [84]. If managers or supervisors do not visibly reinforce face mask usage, employees may feel less compelled to wear them [85]. Cultivating a workplace culture that prioritizes comprehensive PPE usage, including face masks, is crucial for bridging this compliance gap [86].
We demonstrated the effect of interpersonal factors on forecasting acceptance of PPE usage. The parameter of social norms questioned workers about how much their colleagues, family, and supervisors believed that respondents should use PPE. The parameter of social models involved questions about how much workers believed their team leaders and colleagues used PPE when exposed to hazardous agents. The parameter of interpersonal support questioned workers regarding whether their colleagues, family, and supervisors advised them to use PPE. Workers’ interpersonal factors were more strongly associated with their use of PPE than any personal or organizational characteristics [37, 67]. Neves et al. underscore that ensuring the safety of nursing staff requires more than just the provision of PPE; it also involves addressing interpersonal, organizational, and educational determinants of PPE use. The study advocates for a holistic approach to improve adherence, ensuring the well-being of healthcare workers while minimizing occupational risks [87]. This finding is in line with the results of our study.
Interpersonal support requires more management effort than other parameters; therefore, it is practical to state that interpersonal support is related to the agreement on PPE use. However, some studies report that self-efficacy is important in PPE use [88-90]. This indicates that the user’s ability and comfort with PPE significantly affect its usage.
Cognitive-perceptual factors (perceived benefits, barriers, and self-efficacy) did not significantly predict PPE adherence. This may be due to workers’ reliance on external influences, such as workplace policies, peer behaviors, and organizational support, rather than personal beliefs. Additionally, inadequate training and awareness of occupational hazards may limit the impact of cognitive-perceptual factors on PPE use. Lu et al. showed that some cognitive parameters, such as perceived benefits and barriers to PPE use and self-efficacy, have no significant association with wearing PPE. They suggest that interventions should focus more on strengthening interpersonal and organizational support rather than solely addressing individual perceptions [60]. Workers may lack the confidence and persistence to use PPE, which may be due to a lack of awareness of workplace hazards and the benefits and barriers of PPE use resulting from insufficient occupational health and safety education and training. Our findings align with the results of Budhathoki et al.'s study [91], showing that while many workers are aware of various occupational hazards, their actual use of safety measures 0s inadequate. Elements affecting safety practices include education status, training on occupational safety and health, and access to appropriate PPE. The study concludes that improving awareness and providing adequate access to safety training and PPE are vital for enhancing the health and safety of workers.
Several solutions can be proposed to improve workers' use of PPE. These include increased mutual supervision, providing training programs to enhance peer-group support and supervision of PPE use, and developing occupational health and safety policies [92, 93]. This study summarized several key recommendations for implementing organizational modifications to enhance and promote PPE usage. These recommendations address critical areas, such as training, accessibility, policy evaluation, and fostering interpersonal support (Figure 2).
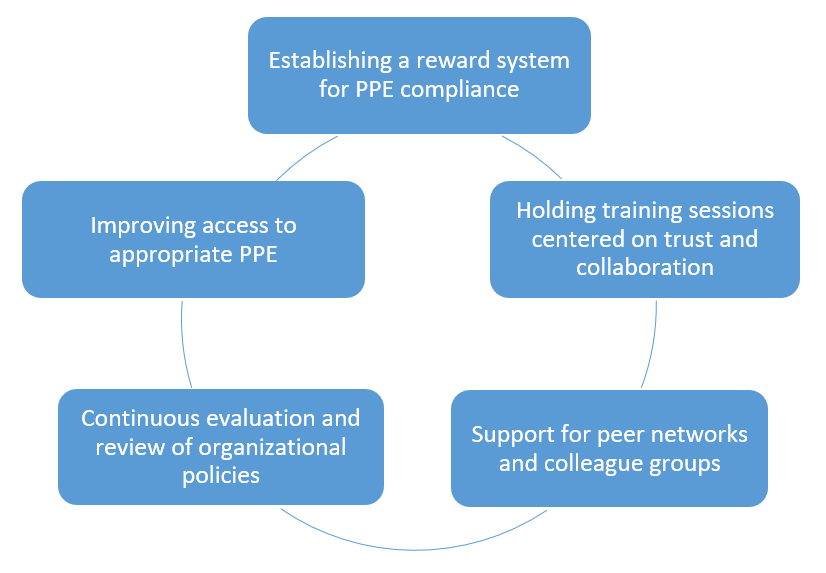
Figure 2. Recommendations for improving and promoting personal protective equipment (PPE) usage
Our study is one of the first in Iran to apply the HPM model to analyze potential determinants of PPE use among workers in major industrial companies exposed to organic solvent hazards.
PPE usage revealed gaps, with only 47.9% of workers wearing face masks compared to 67.4% for gloves, underscoring a disparity in PPE compliance, especially for airborne hazards. Higher education levels correlated with better glove use due to increased awareness about the nature of hazards, while longer exposure to hazards was linked to increased PPE usage. Also, perceived benefits, barriers, and self-efficacy played a role in glove use. Confidence in self-protection was significant for both gloves and masks. Social norms and organizational characteristics significantly affected PPE adherence, particularly mask use, demonstrating how workplace culture shapes protective behavior. Interpersonal and organizational characteristics were the most effective in promoting PPE use, specifically social models for mask use (odds ratio of 3.51) and organizational factors for gloves (odds ratio of 3.15). Organizations and managers should encourage a safety culture through continuous evaluations, policy reviews, and supervisor-led reinforcement. To improve PPE adherence, peer-group support, training programs, establishing reward systems, and ensuring easy access to appropriate PPE can enhance PPE usage.
This study indicated the application and potential of the HPM in predicting and understanding workers’ perspectives on safety and the use of. The model effectively underscores how personal beliefs, perceived benefits and barriers, self-efficacy, and interpersonal influences shape workers’ safety behaviors. This study emphasized the critical role of supportive environments in enhancing PPE compliance by determining key interpersonal and organizational factors, such as peer support, management commitment to safety, and access to training. Promoting a workplace culture that prioritizes safety through leadership involvement and collaborative efforts can significantly improve the likelihood of workers adhering to safety protocols. Like many other studies, ours has its limitations. One of the significant challenges of this study was the restricted access to certain companies, as some managers refused to permit research activities and data collection within their facilities. This issue reduced the number of potential study sites and the diversity of organizational settings that could have enriched the findings. The reluctance of some managers may be rooted in concerns about confidentiality, potential disruptions to workflow, or apprehension about revealing workplace procedures. This barrier highlights the significance of building trust and transparent communication with management in future research, ensuring that companies understand the value of such studies in improving occupational safety and health. This limitation naturally restricts the range of associations we could discover within the model. Moving forward, future research should consider including a wider range of variables so that we can better understand the different factors at play. Another significant point is that because our study was cross-sectional, we cannot draw firm conclusions about cause and effect. We were able to classify the relationships among variables, but it is difficult to determine what is driving what or if there are other unmeasured influences at work. One of the limitations of this study is that the questionnaire does not explicitly assess the role of necessary training, the establishment of mandatory rules, and the provision of PPE by companies. While organizational factors related to PPE accessibility were considered, aspects such as formal training programs, regulatory enforcement, and company policies were not directly measured. These factors are crucial in shaping workers’ adherence to PPE usage, as proper training enhances awareness, mandatory rules reinforce compliance, and PPE availability ensures accessibility. Future research should incorporate these elements to gain a more comprehensive understanding of PPE adherence. Qualitative methods like interviews or focus groups could provide deeper insights into how company policies and training initiatives influence workers’ behavior. Additionally, including specific survey items on training frequency, enforcement of PPE regulations, and company-provided PPE resources would help capture these dimensions more effectively.
Future studies could use a longitudinal approach to truly understand these relationships. This would allow researchers to track changes over time, providing a clearer picture of cause and effect. Furthermore, focusing on specific interventions, whether through programs or policies, could help pinpoint what improves workers’ use of PPE. However, it does not stop there. Evaluating these interventions and conducting thorough policy analyses could provide valuable insights that help individual organizations and shape broader policy decisions.
By addressing these limitations through more data, following individuals over time, and experimenting with targeted strategies, we can better understand how to improve PPE use in the workplace. Ultimately, this will help create safer work environments where workers are better protected, and health outcomes significantly improve. By taking these steps, future research can play a critical role in shaping theory and practical workplace safety solutions.
Despite these limitations, our study demonstrates that the HPM framework is relevant in different cultural contexts. Additionally, our study highlights the importance of interpersonal and organizational factors concerning other variables influencing the use of PPE. We hope organizations will focus on these important variables to enhance PPE usage further.
Future studies should adopt more comprehensive variables and designs to strengthen the understanding of cause-and-effect relationships. Increasing PPE through targeted interventions and policy support can lead to safer work environments and better health outcomes for workers.
Conclusion
The health promotion model can be utilized to understand compliance with personal protective equipment in industrial settings.
Acknowledgments: We are very grateful to the managers and officials of Color Pars, Azar Plast, and Tabriz Petrochemical Companies for their assistance with this study and to the workers who completed the questionnaires.
Ethical Permissions: The Ethics Committee of Tabriz University of Medical Sciences reviewed and approved this study (5/D/35916).
Conflicts of Interests: The authors declare no conflicts of interests.
Authors' Contribution: Akbarzadeh O (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (60%); Golzad H (Second Author), Introduction Writer/Assistant Researcher/Discussion Writer (15%); Moshashaei P (Third Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: Nothing to be reported.
In hazardous work environments, workers prioritize their protection against potential risks. At the same time, they develop a heightened sense of vulnerability due to prolonged exposure to these risks. This refers to increased awareness of potential dangers, which may lead to greater caution or stress over time [1]. Their behaviors and decision-making processes reflect this heightened risk awareness, underscoring the need for effective protective measures [2]. Additionally, the perception of safety is crucial in influencing workers’ well-being, productivity, and adherence to safety protocols [3]. Therefore, creating environments where workers feel safe and healthy is essential. By providing appropriate training and support, perceptions of safety risks stemming from exposure to health and safety hazards can be mitigated, leading to safer and more productive workplaces [4, 5].
Working in hazardous situations, such as extreme noise, heat stress, and radioactivity, can put workers at risk of developing severe occupational diseases. In recent years, the number of occupational disease cases has increased, with noise-induced deafness, musculoskeletal disorders, and skin diseases being among the most prevalent. These rising cases highlight the critical role of personal protective equipment (PPE) in mitigating occupational health risks [6-8]. Such alarming statistics emphasize the importance of PPE as a preventive measure in reducing the prevalence of occupational diseases, particularly in high-risk industrial sectors. Despite the availability of preventive measures, including PPE, occupational diseases continue to pose a significant challenge in high-risk industries [9]. This underscores the necessity of identifying key determinants influencing PPE adherence and addressing barriers to its proper use.
Previous research has extensively examined workplace hazards and the importance of PPE; however, significant gaps remain in understanding the specific factors affecting compliance in different occupational settings. Additionally, exposure to multiple workplace hazards, such as heat stress and chemical agents, can amplify health risks, emphasizing the necessity of effective control measures and PPE usage [10, 11].
While risk management measures, like elimination and engineering controls, are preferred, their implementation is often limited by budget constraints, poor supervision, and workplace restrictions. In such cases, PPE is the last defense against occupational diseases [12-14]. Although PPE may not be as effective as engineering controls, it offers a significant layer of protection when other safety procedures fail [15, 16]. These essential tools act as a shield, protecting workers from potential hazards and decreasing the likelihood of injury or illness. Depending on the risks present in a workplace, PPE can consist of a range of items tailored to those risks [17, 18].
Despite existing studies on PPE compliance, there is still a need for deeper investigation into the specific personal, organizational, and situational determinants influencing its utilization. In many workplaces, while production workers may use PPE, it is not uncommon to see some of them using equipment unsuitable for the specific risks they are exposed to [19]. This could be due to a lack of appropriate training [20], misinterpretation of the hazards involved [21], or even the inaccessibility of the right type of PPE [22]. Moreover, using inappropriate PPE can significantly diminish its effectiveness, leaving employees vulnerable to the health and safety risks they encounter [23].
PPE compliance is influenced by workers’ perceptions of safety, personal attitudes, and social factors such as peer support and organizational policies [24]. Common barriers include discomfort, poor fit, and the belief that PPE interferes with work [25, 26]. However, many previous studies have not provided comprehensive solutions to these challenges, underscoring the necessity for further research that identifies practical strategies to enhance PPE compliance.
Some workers might even think PPE is unnecessary if they do not perceive immediate risks or believe the benefits do not justify the hassle [27]. Wong et al. [17] suggest that by understanding and addressing these obstacles, we can encourage more regular use of PPE, ultimately leading to a safer work environment for everyone [28]. Additionally, when workers perceive that PPE makes their workplace safer and helps prevent incidents, they are more likely to be motivated to use it regularly. However, if they find the PPE uncomfortable or inconvenient, they may be less inclined to use it [29].
Furthermore, using PPE is shaped by several other key issues that can significantly influence workplace safety, including how employees perceive risk, their age and experience, and whether the employer provides the proper PPE. When businesses ensure that their workforce has access to appropriate protective gear, it becomes easier for them to adhere to safety regulations. Ultimately, these elements all work together to improve workplace safety. Beyond worker-related factors, a study by Larson & Liverman [30] demonstrates that organizational factors are also significant in the level of PPE usage among workers. A study by Sarfraz et al. shows that factors such as PPE availability, gear quality, workplace safety policies, and safety training all play a significant role [31].
Experienced workers are more aware of the importance of PPE due to their familiarity with workplace hazards. In contrast, younger or new employees often require additional training and supervision to enhance compliance [32]. This underscores the need for tailored safety programs that address the varying levels of awareness and compliance across different experience levels within the workforce [33, 34]. By exploring these multifaceted influences, this study aims to provide a deeper understanding of the determinants of PPE utilization, ultimately guiding the development of tailored interventions for diverse workplace settings. By explicitly addressing the gaps in previous studies, this research aims to provide new insights into the determinants of PPE utilization, ultimately guiding the development of targeted interventions to improve adherence in high-risk workplaces.
Many studies have highlighted a strong association between wearing PPE and the health promotion model (HPM). Items like masks and gloves protect hazardous materials and infectious agents, reducing the risk of illness or injury. The HPM focuses on encouraging preventive health behaviors by emphasizing the importance of PPE usage as a key strategy in mitigating health risks. Whether in healthcare settings, workplaces, or daily routines, PPE is a fundamental component of the HPM’s approach to proactive health management, ensuring individual and societal well-being. By promoting consistent and proper PPE use, the HPM helps reduce exposure to hazardous conditions, preventing illness and injury. This approach enhances workplace safety and fosters a culture of prevention and resilience in public health [35-37].
Several research studies have investigated the use of the HPM in improving PPE adherence among workers, especially in industrial settings. Khoshakhlag et al., involving small and medium enterprises found that workers’ attitudes toward PPE and workplace safety training are strong predictors of PPE use. Workers with safety training are significantly more likely to use PPE consistently. The primary barriers to PPE utilization include lack of availability, poor comfort, and inadequate training [38]. In another study conducted among construction workers, factors such as government oversight, the provision of safety briefs, and PPE training substantially increase the likelihood of PPE use [39]. Thus, applying the HPM through targeted interventions, such as workplace safety education and regular training, can effectively increase PPE adherence and reduce occupational hazards.
In another study, the application of the HPM is linked to better PPE usage in hazardous industries, such as mining. In the mentioned study, the model was used to develop interventions focusing on perceived barriers and benefits, risk perception, and self-efficacy [40]. Additionally, the COVID-19 pandemic led to increased focus on PPE usage in healthcare settings [41]. La Torre et al.'s study indicates that the use of PPE is associated with a 70% reduction in SARS-CoV-2 infections among healthcare workers, reinforcing the need for proper education and behavioral interventions based on the HPM to improve consistent PPE use in various industries [42].
Studies have shown that the HPM improves workers’ understanding, attitudes, and behaviors toward safety and PPE use, highlighting knowledge, perceived benefits, and self-efficacy [43]. A study conducted in small and medium-sized enterprises (SMEs) found that workers’ attitudes and risk perceptions significantly affect PPE usage. The study emphasized the significance of training interventions to enhance knowledge and positively shape workers’ perspectives toward PPE, merging these factors to achieve higher compliance rates [44]. Additionally, a study on construction employees in Addis Ababa, Ethiopia, underlined that elements, such as the availability of safety training and knowledge of PPE use, are crucial in boosting usage rates. Employees who receive safety training are up to four times more likely to use PPE than those who do not. This study also highlighted the role of external enforcement, such as government supervision, in reinforcing PPE compliance [39]. A study conducted by Alinejad et al. applies the health belief model (HBM) to examine how training can improve PPE compliance in healthcare settings. The HBM is introduced here because it highlights psychological factors, such as the perceived severity of health risks and perceived barriers to compliance, which influence individuals’ decisions to use PPE. This contrasts with the HPM, which takes a broader approach by promoting preventive health behaviors as a proactive and structured strategy. While the HBM focuses on personal risk perception and motivational barriers, the HPM emphasizes systematic and organizational measures to embed PPE use within daily routines [45]. These studies highlight health models' practical and theoretical applications in improving PPE adherence, which is crucial for understanding its determinants in various industries [46, 47].
The HPM provides a practical framework for addressing the research gap and understanding the integrated influence of personal and situational factors on PPE usage across various workplace settings. While previous studies focus narrowly on individual compliance or organizational safety practices, few investigate how these factors shape PPE utilization. This study uniquely bridges the gap by examining individual, interpersonal, and organizational dynamics, offering a holistic understanding of the factors influencing PPE adherence in complex workplace environments.
Guided by the main elements of the HPM, this study examined the interplay between employees’ characteristics (such as experience and risk perception) and organizational factors (like PPE availability and safety training), offering an integrated perspective. The originality of this study also lies in its focus on workers in major companies that have established international standards for safety and health, such as ISO 45000, ISO 45001, ISO 14001, and HSE-MS. This provides a unique perspective on PPE usage in settings with progressive occupational health protocols where workers are exposed to highly hazardous chemical materials such as BTEX (Benzene, Toluene, Ethylbenzene, and Xylene) compounds.
Focusing on organizations with advanced safety standards highlights best practices and uncovers persistent challenges, providing valuable lessons for less-regulated settings. By investigating PPE compliance within companies that are already committed to high safety and health measures, this research presented insights into how even well-regulated environments face challenges related to interpersonal and organizational characteristics. This context enhances our understanding of PPE usage beyond regulatory adherence, underscoring the nuanced factors of employee behavior and interaction that can affect safety and health practices even in optimal circumstances.
The findings are expected to inform policymakers and industry leaders in designing more effective, tailored interventions that enhance PPE adherence, even in high-risk and well-regulated industries. Through this approach, the study aims to identify targeted procedures to improve PPE adherence by considering interpersonal, situational, and organizational dynamics across different industries.
Instrument and Methods
Theoretical framework
The HPM [48] provided a theoretical framework for our study, which includes three main stages, including modifying factors, cognitive-perceptual factors, and health-related behaviors (using PPE). These stages are particularly relevant to our study, as they offer a structured approach to understanding how various influences shape PPE compliance in occupational settings. The model suggests that modifying characteristics, including demographic factors, peer support, and organizational culture, indirectly shape health-related behaviors by influencing cognitive-perceptual factors, such as perceived benefits, barriers, self-efficacy, and susceptibility. These cognitive-perceptual factors are central to individual decision-making, as they determine whether a worker believes PPE use is beneficial, whether they perceive significant obstacles to its use, how confident they feel in using PPE correctly, and how vulnerable they think they are to workplace hazards [49]. This is crucial in our context, as PPE compliance is not only a matter of knowledge but also depends on workplace culture, individual motivation, and perceived risks. By incorporating external influences and individual decision-making processes, the HPM provides a more comprehensive approach than other frameworks, such as the knowledge, attitude, and practice (KAP) model [50] or the contextual framework. Unlike the KAP model, the HPM integrates organizational and personal factors, making it well-suited for evaluating health-related behaviors, like PPE use in occupational settings [51]. In addition, organizational factors, such as workplace policies, safety climate, and managerial support, create an environment that either facilitates or hinders PPE compliance [52]. Simultaneously, personal factors, including perceived self-efficacy, perceived risk, and individual motivation, directly influence a worker’s willingness to adhere to PPE guidelines [53]. The interaction between these factors is critical, as PPE use is not solely an individual decision but is shaped by the broader organizational culture [54]. By incorporating both levels of influence, the HPM provides a comprehensive understanding of the determinants of PPE adherence, making it a more robust framework for analyzing workplace health behaviors.
Procedure and participants
This descriptive-analytical study, conducted in 2024, was based on a positivist research philosophy, carried out with samples selected from three industrial businesses with higher exposure rates to occupational diseases. Furthermore, these companies strictly comply with internationally recognized occupational safety and health standards, such as OHSAS 18001, ISO 45003, and HSE-MS, ensuring a strong framework for managing workplace hazards. Compliance with these standards indicates a commitment to sustaining high levels of safety and health management, providing a consistent approach across industries to decrease occupational risks and enhance worker well-being. In addition, positivism was applied to systematically analyze the quantitative factors influencing PPE usage [55]. By employing a structured methodological approach, we used measurable data to examine the associations between personal and situational factors and PPE compliance. The positivist approach ensures objectivity in data collection and analysis, reducing bias and enabling the generation of replicable and generalizable findings [56]. This methodological framework allows for the identification of key determinants affecting PPE use, providing empirical insights that can inform workplace health and safety policies [57]. This approach supports the study’s objective of determining reliable predictors of PPE adherence that can be applied across diverse industrial environments, offering precise, actionable insights to enhance workplace safety. Green’s advocacy [58] for incorporating transformative perspectives highlights the importance of investigating not only individual compliance but also the social and organizational contexts that shape safety behaviors. This process complements the HPM by suggesting that promoting supportive interpersonal and organizational environments may play an equally crucial role in improving PPE adherence. The data collection process was informed by the results of a pilot study survey [59]. Before the main study, the questionnaire was pilot-tested with a small group of workers from similar industries to evaluate its clarity and comprehension. This pilot test involved 40 participants who were asked to complete the questionnaire, provide feedback, and comment on the wording and structure of the questions.
The feedback highlighted several areas for improvement. Some technical terms were simplified to ensure accessibility for participants with varying education levels, and ambiguous phrasing in a few questions was clarified. Additionally, response scales were adjusted to enhance consistency and ease of interpretation. Based on these insights, adjustments were made to improve the clarity of the questions, ensuring participants with different levels of education and language proficiency easily understood them. These refinements helped enhance the questionnaire’s reliability and validity for the main study.
This pilot testing procedure not only improved the reliability of the questionnaire but also helped ensure that the questions effectively captured the intended information regarding PPE usage. Therefore, the final version of the questionnaire was refined and used for data collection in the main study. Considering a confidence level of 95%, d=0.05, and SD=0.47, using Z2α/2=(1.96)2 formula, the sample size was estimated at 340 persons.
This is the Z-score associated with a 95% confidence level. The Z-score corresponds to the number of standard deviations a data point is from the mean. For a 95% confidence level, the Z-score is 1.96, meaning that 95% of the data lies within 1.96 standard deviations from the mean in a normal distribution. The confidence level was 95%, indicating that 95% of the confidence intervals generated would contain the true population parameter if the same study were repeated numerous times. It is a common standard in research, reflecting a high degree of certainty. We regarded d=0.05 as the margin of error (denoted as d). In this case, it is 0.05, meaning the results are expected to be within ±5 percentage points of the true population value. It sets an acceptable level of precision for your estimate. The standard deviation (SD) measures how spread the data points are around the mean. A value of 0.47 indicates moderate variability in the data. Standard deviation is essential for understanding the variation in the data, which influences sample size requirements. The formula offers simplicity and accuracy in calculating sample size for quantitative studies by directly accounting for the confidence level, data variability, and desired precision. It ensures flexibility, allowing researchers to adjust the sample size based on study requirements while maintaining the desired confidence level. Additionally, it helps optimize resources by determining a sample size large enough to produce reliable results without being unnecessarily large.
The selection of participants from each company was based on the relative size of their workforces. The number of employees chosen from each organization reflects the number of workers in those companies, ensuring that our sample is representative of the broader workforce dynamics. Specifically, 120 employees were selected from the paint industrial plant, 100 from the plastic production company, and 120 from the petrochemical company. This distribution was designed to capture diverse experiences and exposure to PPE use in different manufacturing environments. By maintaining proportional representation, we aimed to ensure that the findings accurately reflect workers' practices and challenges in each sector. Additionally, this approach allows for a more comprehensive understanding of how PPE usage may vary across different industries, enhancing the study's overall validity.
The random sampling method was conducted systematically to ensure that each worker had an equal opportunity to participate. A comprehensive list of all employees from each company was obtained, and a random number generator was employed to choose participants from this list.
For the paint industrial plant and the petrochemical company, which had larger worker counts, we first ensured that the total number of workers was well-documented. After obtaining the worker list, we assigned a unique identification number to each worker. Then, using the random number generator, we established the required number of participants—120 from the paint plant and 120 from the petrochemical company.
In the case of the plastic production company, which had a smaller workforce, we directly randomized the employee IDs using the same random number generator until we achieved the target of 100 participants. This process provided an unbiased selection and ensured that our sample was representative of the workforce across the three industries.
By employing this random sampling method, we aimed to eliminate selection bias and improve the generalizability of our results across various manufacturing settings.
The participants were selected from workers working on the production line for over a year. As a selection criterion, participants must have worked on the production line for more than one year to ensure adequate experience, knowledge, and familiarity with the workplace environment, safety regulations, and potential hazards in their workplace. They had consistent exposure to organic solvents. This consistent exposure ensured that the study focuses on workers who face relevant occupational risks, providing a significant context for examining PPE usage and adherence. By choosing participants with regular contact with hazardous materials, the study could more accurately evaluate the factors that affect protective equipment utilization in high-risk environments. They also completed the research consent form and had access to the required PPE, indicating that workers were required to use PPE appropriate for their specific working and ergonomic conditions. However, this requirement was always observed in all companies adhering to international safety and health standards.
The study excluded workers who could not read or answer the questionnaire due to poor language skills. For those with lower levels of education, the research team read the questionnaire clearly to ensure that all participants fully understood the questions.
Before data collection, we received ethical approval from the Tabriz University of Medical Sciences. This approval ensured that all research activities adhered to ethical standards and protected the rights of participants.
To ensure participant confidentiality, responses were anonymized by removing identifying information and assigning unique ID numbers. All data were securely stored in a password-protected database accessible only to the research team. Reports and publications will present aggregated data to further protect individual identities. Participants were required to sign an informed consent document clearly outlining their rights, including the option to withdraw from the research at any time without repercussions. These ethical considerations were integral to the study design, ensuring that participant rights were respected and that the research adhered to ethical research practices.
At the sampling sites, the authors clarified the study’s purpose in clear and simple terms. They then distributed the questionnaires to the employees and collected them once completed. This careful and respectful approach guaranteed that every worker understood the study and contributed their experiences, leading to more accurate and meaningful results.
Measures
The primary data collection method was a questionnaire survey designed to assess PPE adherence among workers. The questionnaire was developed based on the studies of Lu et al. [60] and Nichol et al. [61] and was structured to evaluate various factors influencing PPE usage. To ensure its accuracy and consistency, researchers assessed its validity and reliability, confirming that the tool effectively measures PPE adherence while maintaining stable results across different instances.
The questionnaire consisted of five sections, including personal demographic information, additional individual factors, interpersonal influences, organizational or situational elements, and the usage of PPE. The first section collected demographic details, such as gender, age, work experience, marital status, education level, and exposure duration to organic solvents.
The remaining four sections (Table 1) were grounded in the HPM (Figure 1), which served as the theoretical foundation for this study. These sections explored personal, social, and organizational factors influencing PPE adherence, offering a broader perspective on occupational safety decision-making. According to the HPM, modifying factors, such as demographic characteristics and interpersonal influences, indirectly shape cognitive-perceptual elements, which ultimately drive health-related behaviors [62]. The second section of the questionnaire examined personal factors influencing PPE compliance, including perceived benefits of PPE use (two questions), barriers to PPE adherence (two questions), and self-efficacy in PPE use (three questions). Participants responded using a five-point Likert scale. The third section focused on social influences, assessing how role models (two questions), social norms (three questions), and peer support (three questions) impact PPE adherence. Participants also responded using a five-point Likert scale for consistency. The fourth section evaluated organizational factors affecting PPE compliance, particularly PPE accessibility and the organization’s commitment to enforcing PPE use.
Finally, the last section assessed actual PPE adherence, specifically using protective face masks and gloves. Participants answered questions such as, “How often do you wear a protective face mask during work?” and “How often do you wear protective gloves while working?” to measure their compliance with PPE guidelines.

Figure 1. Conceptual framework of the health promotion model (HPM)
Table 1. Questionnaire construct items
Statistical analysis
We examined the reliability of the questionnaire by assessing its internal consistency using Cronbach’s Alpha. According to Sørensen and Slater’s study, an alpha coefficient of 0.60 or higher indicates that the measure is reliable [63]. Our scales for perceived benefits (Table 1), barriers, self-efficacy, social modeling, social norms, interpersonal support, and organizational factors all met this standard, with alpha coefficients ranging from 0.60 to 0.84. We also evaluated the normality of our numeric variables using the Kolmogorov-Smirnov test. We presented our data as means and standard deviations for normally distributed numeric variables and medians with ranges for non-normal ones. In contrast, categorical data were shown as frequencies and percentages. To associate health promotion measures between those who wear PPE (like face masks or gloves) and those who do not, we used chi-square tests for categorical data and t-tests for normally distributed continuous data. A p-value of 0.05 or less was considered statistically significant [64].
Finally, we used a two-level logistic regression model to identify how different factors affected the use of PPE in the workplace while adjusting for individual demographics. In the current research, we employed a two-level logistic regression model because it accounts for the hierarchical structure of the data, such as individuals nested within groups (e.g., patients in clinics). This model captures individual and group-level variations, handling unobserved heterogeneity at the group level while accounting for clusters' correlations. Using logistic regression is suitable for binary outcomes (e.g., health behaviors), providing more accurate estimates and improving the model’s fit compared to single-level approaches. This results in more reliable and interpretable outcomes in contexts where individual and group-level elements affect results [65]. We considered results with p-values under 0.05 significant [66].
Cronbach’s alpha values were calculated, as presented in Table 1, to assess the reliability of the scales used in this study. Cronbach’s alpha is widely used to measure internal consistency, reflecting the degree to which items within a scale correlate with each other, thereby demonstrating that they collectively assess the same underlying construct. Typically, alpha values above 0.5 are considered acceptable, suggesting adequate reliability, whereas values exceeding 0.7 are considered a solid reliability indicator. In this context, Cronbach’s alpha values help confirm that the variables included are suitable for further analysis and reliably represent factors influencing PPE usage.
For the analysis of categorical variables, we employed logistic regression, a statistical method designed to model binary outcomes. Logistic regression is particularly useful in this study as it allows us to estimate the probability of PPE compliance as influenced by various predictor variables, such as interpersonal and organizational factors. This approach provides an understanding of how each independent variable contributes to the likelihood of PPE usage, yielding insights that can support targeted interventions to improve compliance in industrial settings. Data analysis was done using SPSS 26.
Findings
Most workers were men (95.9%), and most were married (89.7%). Approximately half were in their 30s, particularly aged 31 to 40 (46.1%), and had been employed for 10 to 15 years, indicating a fairly experienced group. In terms of education, a significant portion had completed junior secondary school (37.4%), providing insight into their academic situation. Over half were exposed to their work environment for over 8 hours daily (50.6%), indicating extended work shifts. While most workers took precautions by wearing protective gloves (67.4%), more than half did not use face masks (52.1%). This pattern indicates a gap in protective practices, especially concerning safeguarding against airborne hazards. These findings emphasize the need for continued attention to safety measures in the workplace (Table 2).
Table 2. Frequency of samples’ characteristics
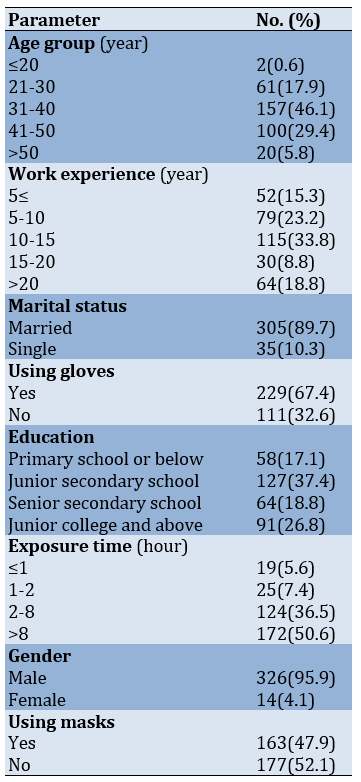
The Chi-square test and t-test revealed that the education level was closely associated with the probability of wearing protective gloves. Moreover, the time workers are exposed to hazards played a significant role in whether they used face masks and gloves (p<0.05). Regarding cognitive and perceptual factors, individuals who perceived clear benefits and encountered barriers in their work environment were more likely to use gloves. Additionally, those who felt confident in their ability to protect themselves were more inclined to use both types of PPE (p<0.05). Social norms, commonly accepted in one’s social circle, were particularly influential in encouraging the use of face masks and gloves. Lastly, organizational factors significantly influenced PPE usage (p<0.05; Table 3).
Table 3. Relationship between compliance with the use of personal protective equipment (PPE) and individual demographics, cognitive-perceptual, interpersonal, and situational factors
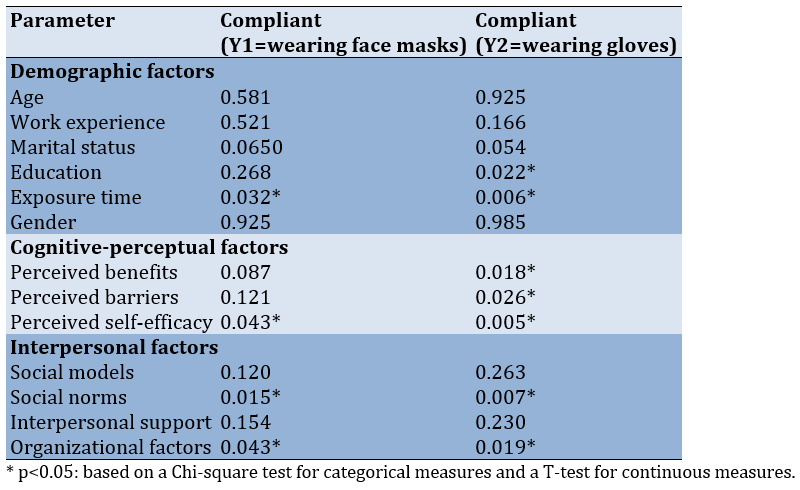
In the next stage, we developed a two-level logistic regression model that involved several explanatory variables. Gender affected whether workers were likely to wear face masks and protective gloves. After considering differences in demographics, the interpersonal factors from the HPM emerged as the most important drivers for PPE use. In contrast, cognitive-perceptual factors did not appear to have much impact. Upon closer examination, interpersonal support and organizational factors were only associated with using gloves. For face mask use, workers with higher scores in social support networks were significantly more likely to use them, with an odds ratio of 3.51 (95% CI: 1.23-1.50). On the other hand, regarding gloves, organizational factors were a powerful predictor, with a higher score in this area leading to an odds ratio of 3.15 (95% CI: 1.12-1.15) for increased use. Individuals’ PPE habits were influenced differently depending on the type of PPE. Social factors enhanced face mask usage, while workplace or organizational support had a greater effect on whether someone wore protective gloves (Table 4).
Table 4. Factors associated with personal protective equipment (PPE) use

Discussion
This study assessed how the HPM model can help predict workers’ attitudes toward using PPE. By examining specific factors, we demonstrated that the model could predict and provide a deep understanding of how PPE is being used in the workplace. Similar studies have verified these findings [25, 67, 68], in which the HPM model has also been employed to understand PPE use among workers. These studies emphasize the importance of using predictive models to improve workers’ safety and health.
When the right PPE is chosen and used properly, it can help reduce workplace accident rates, occupational exposure, and the severity of potential risks. Properly using PPE is imperative to improving worker safety and decreasing the likelihood of serious harm on the job [25, 69]. There is little information about the use of PPE among workers, but our findings show that only a few workers use PPE. Shamsi et al.'s study on attitudes and behaviors related to using PPE among subway construction station employees showed that using PPE by the staff is not desirable [70]. This study provides practical insights into the attitudes and behaviors affecting PPE usage among construction workers, underscoring the significance of audience analysis for developing effective behavior change interventions. Their findings emphasize that organizational culture, perceived risk, and the availability of PPE significantly impact compliance, aligning with the elements of the HPM in our study. Additionally, another study by Moshashaei et al. showed that clothing components and other PPE, such as masks, with a score below 20%, among the most undesirable components of safety and health [18]. Another study conducted by Sehsah et al. among construction workers demonstrated that safety and health training can improve workers’ attitudes and beliefs toward using PPE, which can subsequently affect occupational accidents and injuries. Furthermore, the authors noted that the main reasons for not using PPE are a lack of knowledge and fitting problems related to worker posture [71]. The results of this study are in line with our findings. Mahmood et al.'s study emphasizes the importance of proper training for healthcare workers in donning, doffing, and safely handling PPE to minimize the risk of self-contamination [72]. The results of their study align with our findings regarding the use of the HPM to adopt proper training to promote PPE usage among employees.
Many workers have stated that PPE tends to decrease efficiency and slow down work. In some cases, they find PPE annoying or restrictive, which makes it difficult for workers to move easily and reduces their performance. This view demonstrates the ongoing challenge of ensuring safety while also improving productivity. Several studies have confirmed these findings [68, 73, 74]. About 25% of academic workers had inadequate access to PPE due to economic and financial limitations. This issue is prevalent in many companies with limited financial margins; nevertheless, they still try to provide sufficient safety equipment [75]. Not only does this put workers’ health at risk, but it also highlights the broader challenge of ensuring worker safety in the face of economic pressures. These findings are consistent with several studies [76-78]. Here, utilization rates for face masks were 47.9%, while gloves were 67.4%. Previous studies have found the compliance rate for PPE use to be between 40% and 70% [79, 80]. Additionally, Lu et al.'s research showed that 54% of individuals use face masks and 77% use gloves, similar to our utilization rates. Face masks are used less than gloves due to the inadequate supply of face masks and presumably the discomfort associated with wearing one [60]. While our findings indicate high compliance with glove usage, the relatively lower face mask compliance warrants further exploration.
Several factors may contribute to this gap in face mask usage. First, the perceived risk associated with the tasks performed may affect employees’ attitudes toward PPE. For instance, if employees believe that their primary exposure risks are linked to skin contact rather than inhalation of hazardous substances, they may prioritize gloves over masks. This perception could arise from insufficient education or communication regarding hazardous organic solvents' specific health and safety hazards [81, 82].
Second, comfort and convenience play a vital role in PPE compliance. Face masks can often be perceived as uncomfortable, particularly during prolonged use, leading employees to forgo them in favor of gloves, which are generally easier to wear and adjust. Employers should consider evaluating the types of masks provided to ensure they are comfortable and appropriate for the tasks [83].
Finally, social influences and workplace culture may impact PPE adherence [84]. If managers or supervisors do not visibly reinforce face mask usage, employees may feel less compelled to wear them [85]. Cultivating a workplace culture that prioritizes comprehensive PPE usage, including face masks, is crucial for bridging this compliance gap [86].
We demonstrated the effect of interpersonal factors on forecasting acceptance of PPE usage. The parameter of social norms questioned workers about how much their colleagues, family, and supervisors believed that respondents should use PPE. The parameter of social models involved questions about how much workers believed their team leaders and colleagues used PPE when exposed to hazardous agents. The parameter of interpersonal support questioned workers regarding whether their colleagues, family, and supervisors advised them to use PPE. Workers’ interpersonal factors were more strongly associated with their use of PPE than any personal or organizational characteristics [37, 67]. Neves et al. underscore that ensuring the safety of nursing staff requires more than just the provision of PPE; it also involves addressing interpersonal, organizational, and educational determinants of PPE use. The study advocates for a holistic approach to improve adherence, ensuring the well-being of healthcare workers while minimizing occupational risks [87]. This finding is in line with the results of our study.
Interpersonal support requires more management effort than other parameters; therefore, it is practical to state that interpersonal support is related to the agreement on PPE use. However, some studies report that self-efficacy is important in PPE use [88-90]. This indicates that the user’s ability and comfort with PPE significantly affect its usage.
Cognitive-perceptual factors (perceived benefits, barriers, and self-efficacy) did not significantly predict PPE adherence. This may be due to workers’ reliance on external influences, such as workplace policies, peer behaviors, and organizational support, rather than personal beliefs. Additionally, inadequate training and awareness of occupational hazards may limit the impact of cognitive-perceptual factors on PPE use. Lu et al. showed that some cognitive parameters, such as perceived benefits and barriers to PPE use and self-efficacy, have no significant association with wearing PPE. They suggest that interventions should focus more on strengthening interpersonal and organizational support rather than solely addressing individual perceptions [60]. Workers may lack the confidence and persistence to use PPE, which may be due to a lack of awareness of workplace hazards and the benefits and barriers of PPE use resulting from insufficient occupational health and safety education and training. Our findings align with the results of Budhathoki et al.'s study [91], showing that while many workers are aware of various occupational hazards, their actual use of safety measures 0s inadequate. Elements affecting safety practices include education status, training on occupational safety and health, and access to appropriate PPE. The study concludes that improving awareness and providing adequate access to safety training and PPE are vital for enhancing the health and safety of workers.
Several solutions can be proposed to improve workers' use of PPE. These include increased mutual supervision, providing training programs to enhance peer-group support and supervision of PPE use, and developing occupational health and safety policies [92, 93]. This study summarized several key recommendations for implementing organizational modifications to enhance and promote PPE usage. These recommendations address critical areas, such as training, accessibility, policy evaluation, and fostering interpersonal support (Figure 2).
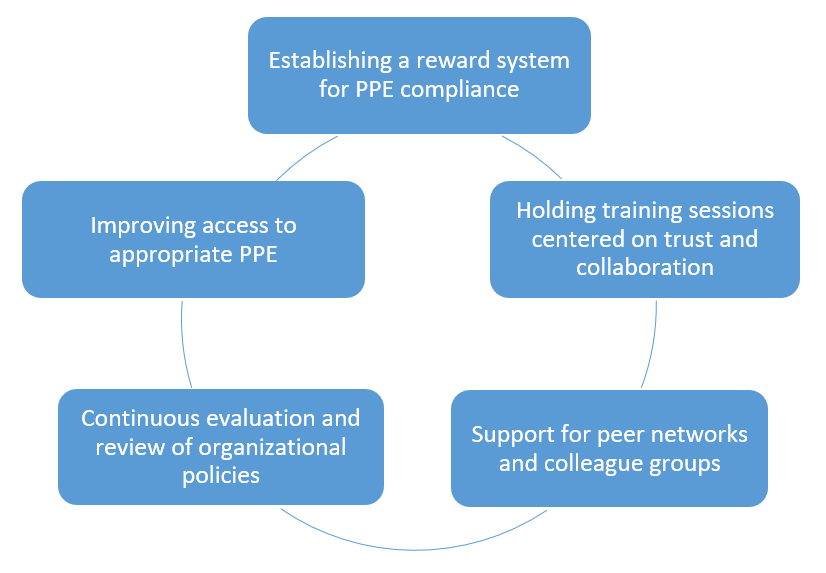
Figure 2. Recommendations for improving and promoting personal protective equipment (PPE) usage
Our study is one of the first in Iran to apply the HPM model to analyze potential determinants of PPE use among workers in major industrial companies exposed to organic solvent hazards.
PPE usage revealed gaps, with only 47.9% of workers wearing face masks compared to 67.4% for gloves, underscoring a disparity in PPE compliance, especially for airborne hazards. Higher education levels correlated with better glove use due to increased awareness about the nature of hazards, while longer exposure to hazards was linked to increased PPE usage. Also, perceived benefits, barriers, and self-efficacy played a role in glove use. Confidence in self-protection was significant for both gloves and masks. Social norms and organizational characteristics significantly affected PPE adherence, particularly mask use, demonstrating how workplace culture shapes protective behavior. Interpersonal and organizational characteristics were the most effective in promoting PPE use, specifically social models for mask use (odds ratio of 3.51) and organizational factors for gloves (odds ratio of 3.15). Organizations and managers should encourage a safety culture through continuous evaluations, policy reviews, and supervisor-led reinforcement. To improve PPE adherence, peer-group support, training programs, establishing reward systems, and ensuring easy access to appropriate PPE can enhance PPE usage.
This study indicated the application and potential of the HPM in predicting and understanding workers’ perspectives on safety and the use of. The model effectively underscores how personal beliefs, perceived benefits and barriers, self-efficacy, and interpersonal influences shape workers’ safety behaviors. This study emphasized the critical role of supportive environments in enhancing PPE compliance by determining key interpersonal and organizational factors, such as peer support, management commitment to safety, and access to training. Promoting a workplace culture that prioritizes safety through leadership involvement and collaborative efforts can significantly improve the likelihood of workers adhering to safety protocols. Like many other studies, ours has its limitations. One of the significant challenges of this study was the restricted access to certain companies, as some managers refused to permit research activities and data collection within their facilities. This issue reduced the number of potential study sites and the diversity of organizational settings that could have enriched the findings. The reluctance of some managers may be rooted in concerns about confidentiality, potential disruptions to workflow, or apprehension about revealing workplace procedures. This barrier highlights the significance of building trust and transparent communication with management in future research, ensuring that companies understand the value of such studies in improving occupational safety and health. This limitation naturally restricts the range of associations we could discover within the model. Moving forward, future research should consider including a wider range of variables so that we can better understand the different factors at play. Another significant point is that because our study was cross-sectional, we cannot draw firm conclusions about cause and effect. We were able to classify the relationships among variables, but it is difficult to determine what is driving what or if there are other unmeasured influences at work. One of the limitations of this study is that the questionnaire does not explicitly assess the role of necessary training, the establishment of mandatory rules, and the provision of PPE by companies. While organizational factors related to PPE accessibility were considered, aspects such as formal training programs, regulatory enforcement, and company policies were not directly measured. These factors are crucial in shaping workers’ adherence to PPE usage, as proper training enhances awareness, mandatory rules reinforce compliance, and PPE availability ensures accessibility. Future research should incorporate these elements to gain a more comprehensive understanding of PPE adherence. Qualitative methods like interviews or focus groups could provide deeper insights into how company policies and training initiatives influence workers’ behavior. Additionally, including specific survey items on training frequency, enforcement of PPE regulations, and company-provided PPE resources would help capture these dimensions more effectively.
Future studies could use a longitudinal approach to truly understand these relationships. This would allow researchers to track changes over time, providing a clearer picture of cause and effect. Furthermore, focusing on specific interventions, whether through programs or policies, could help pinpoint what improves workers’ use of PPE. However, it does not stop there. Evaluating these interventions and conducting thorough policy analyses could provide valuable insights that help individual organizations and shape broader policy decisions.
By addressing these limitations through more data, following individuals over time, and experimenting with targeted strategies, we can better understand how to improve PPE use in the workplace. Ultimately, this will help create safer work environments where workers are better protected, and health outcomes significantly improve. By taking these steps, future research can play a critical role in shaping theory and practical workplace safety solutions.
Despite these limitations, our study demonstrates that the HPM framework is relevant in different cultural contexts. Additionally, our study highlights the importance of interpersonal and organizational factors concerning other variables influencing the use of PPE. We hope organizations will focus on these important variables to enhance PPE usage further.
Future studies should adopt more comprehensive variables and designs to strengthen the understanding of cause-and-effect relationships. Increasing PPE through targeted interventions and policy support can lead to safer work environments and better health outcomes for workers.
Conclusion
The health promotion model can be utilized to understand compliance with personal protective equipment in industrial settings.
Acknowledgments: We are very grateful to the managers and officials of Color Pars, Azar Plast, and Tabriz Petrochemical Companies for their assistance with this study and to the workers who completed the questionnaires.
Ethical Permissions: The Ethics Committee of Tabriz University of Medical Sciences reviewed and approved this study (5/D/35916).
Conflicts of Interests: The authors declare no conflicts of interests.
Authors' Contribution: Akbarzadeh O (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (60%); Golzad H (Second Author), Introduction Writer/Assistant Researcher/Discussion Writer (15%); Moshashaei P (Third Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: Nothing to be reported.
Article Type: Descriptive & Survey |
Subject:
Health Promotion Setting
Received: 2025/01/13 | Accepted: 2025/02/15 | Published: 2025/02/27
Received: 2025/01/13 | Accepted: 2025/02/15 | Published: 2025/02/27
References
1. Scharf T, Vaught C, Kidd P, Steiner L, Kowalski K, Wiehagen B, et al. Toward a typology of dynamic and hazardous work environments. Hum Ecol Risk Assess. 2001;7(7):1827-41. [Link] [DOI:10.1080/20018091095429]
2. Hajat S, O'Connor M, Kosatsky T. Health effects of hot weather: From awareness of risk factors to effective health protection. Lancet. 2010;375(9717):856-63. [Link] [DOI:10.1016/S0140-6736(09)61711-6]
3. Olukolajo MA, Oyetunji AK, Oluleye IB. Covid-19 protocols: Assessing construction site workers compliance. J Eng Des Technol. 2022;20(1):115-31. [Link] [DOI:10.1108/JEDT-03-2021-0131]
4. Mearns K, Whitaker SM, Flin R. Safety climate, safety management practice and safety performance in offshore environments. Saf Sci. 2003;41(8):641-80. [Link] [DOI:10.1016/S0925-7535(02)00011-5]
5. Burke MJ, Sarpy SA, Smith-Crowe K, Chan-Serafin S, Salvador RO, Islam G. Relative effectiveness of worker safety and health training methods. Am J Public Health. 2006;96(2):315-24. [Link] [DOI:10.2105/AJPH.2004.059840]
6. OSHA. Workplace injury statistics [Internet]. Washington, DC: Occupational Safety and Health Administration; 2022 [cited 2023, October, 1]. Available from: https://www.osha.gov/data/commonstats. [Link]
7. Bonfiglioli R, Caraballo-Arias Y, Salmen-Navarro A. Epidemiology of work-related musculoskeletal disorders. Curr Opin Epidemiol Public Health. 2022;1(1):18-24. [Link] [DOI:10.1097/PXH.0000000000000003]
8. Govaerts R, Tassignon B, Ghillebert J, Serrien B, De Bock S, Ampe T, et al. Prevalence and incidence of work-related musculoskeletal disorders in secondary industries of 21st century Europe: A systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):751. [Link] [DOI:10.1186/s12891-021-04615-9]
9. Golzad H, Teimoory A, Mousavi SJ, Bayramova A, Edwards DJ. Mental health causation in the construction industry: A systematic review employing a psychological safety climate model. Buildings. 2023;13(10):2442. [Link] [DOI:10.3390/buildings13102442]
10. Falzone L, Marconi A, Loreto C, Franco S, Spandidos DA, Libra M. Occupational exposure to carcinogens: Benzene, pesticides and fibers (Review). Mol Med Rep. 2016;14(5):4467-74. [Link] [DOI:10.3892/mmr.2016.5791]
11. Shalili A, Mahabadi HA, Variani AS. Investigating the effects of co-exposure to noise and benzene on serum oxidative stress in rat. Toxicol Rep. 2024;13:101849. [Link] [DOI:10.1016/j.toxrep.2024.101849]
12. Manuele FA. Risk assessment & hierarchies of control. Prof Saf. 2005;50(5):33-9. [Link]
13. Olive C, O'Connor TM, Mannan MS. Relationship of safety culture and process safety. J Hazard Mater. 2006;130(1-2):133-40. [Link] [DOI:10.1016/j.jhazmat.2005.07.043]
14. Akbarzadeh O, Rasoulzadeh Y, Haghighi M, Talati A, Golzad H. Investigation of synergistic influence of ultrasound and co-doping to degrade toluene from polluted air in construction sites-An experimental approach. Buildings. 2024;14(9):2876. [Link] [DOI:10.3390/buildings14092876]
15. Gershon RR, Karkashian CD, Grosch JW, Murphy LR, Escamilla-Cejudo A, Flanagan PA, et al. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am J Infect Control. 2000;28(3):211-21. [Link] [DOI:10.1067/mic.2000.105288]
16. Neitzel R, Seixas N. The effectiveness of hearing protection among construction workers. J Occup Environ Hyg. 2005;2(4):227-38. [Link] [DOI:10.1080/15459620590932154]
17. Wong TKM, Man SS, Chan AHS. Critical factors for the use or non-use of personal protective equipment amongst construction workers. Safe Sci. 2020;126:104663. [Link] [DOI:10.1016/j.ssci.2020.104663]
18. Moshashaei P, Nazari J, Alizadeh SS. Surveying health and safety conditions of street sweepers in Tabriz city, Iran (case study). J Health Saf Work. 2017;7(3):203-18. [Persian] [Link]
19. Rafindadi AD, Napiah M, Othman I, Alarifi H, Musa U, Muhammad M. Significant factors that influence the use and non-use of personal protective equipment (PPE) on construction sites-Supervisors' perspective. Ain Shams Eng J. 2022;13(3):101619. [Link] [DOI:10.1016/j.asej.2021.10.014]
20. Ayton D, Soh SE, Berkovic D, Parker C, Yu K, Honeyman D, et al. Experiences of personal protective equipment by Australian healthcare workers during the COVID-19 pandemic, 2020: A cross-sectional study. PLoS One. 2022;17(6):e0269484. [Link] [DOI:10.1371/journal.pone.0269484]
21. Tamene A, Afework A, Mebratu L, Al-Khatib IA. A qualitative study of barriers to personal protective equipment use among laundry workers in government hospitals, Hawassa, Ethiopia. J Environ Public Health. 2020;2020(1):1-8. [Link] [DOI:10.1155/2020/5146786]
22. Barratt R, Wyer M, Hor SY, Gilbert GL. Medical interns' reflections on their training in use of personal protective equipment. BMC Med Educ. 2020;20(1):328. [Link] [DOI:10.1186/s12909-020-02238-7]
23. Ahmed J, Malik F, Bin Arif T, Majid Z, Chaudhary MA, Ahmad J, et al. Availability of personal protective equipment (PPE) among US and Pakistani doctors in COVID-19 pandemic. Cureus. 2020;12(6):e8550. [Link]
24. Mashia MS, Subramaniama C, Joharia J. The effect of safety training and workers involvement on healthcare workers safety behavior: The moderating role of consideration of future safety consequences. Int J Bus Manag. 2016;1(2):46-81. [Link]
25. Lombardi DA, Verma SK, Brennan MJ, Perry MJ. Factors influencing worker use of personal protective eyewear. Accid Anal Prev. 2009;41(4):755-62. [Link] [DOI:10.1016/j.aap.2009.03.017]
26. Brangier E, Barcenilla J. Benefits of combining social influence and ergonomics to improve the use of personal protective equipment (PPE). In: Advances in social and organizational factors. Boca Raton: CRC Press; 2012. p. 366-75. [Link]
27. Savoia E, Argentini G, Gori D, Neri E, Piltch-Loeb R, Fantini MP. Factors associated with access and use of PPE during COVID-19: A cross-sectional study of Italian physicians. PLoS One. 2020;15(10):e0239024. [Link] [DOI:10.1371/journal.pone.0239024]
28. Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q. 1984;11(1):1-47. [Link] [DOI:10.1177/109019818401100101]
29. MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17(2):144-58. [Link] [DOI:10.1177/0193841X9301700202]
30. Larson EL, Liverman CT, editors. Using PPE: Individual and organizational issues. In: Preventing transmission of pandemic influenza and other viral respiratory diseases: Personal protective equipment for healthcare personnel. Washington, DC: National Academies Press; 2011. [Link]
31. Sarfraz A, Sarfraz Z, Anwer A, Sarfraz M, Siddiq J. Availability, use, and satisfaction of personal protective equipment among healthcare workers: A cross-sectional assessment of low- and middle-income countries. J Occup Environ Med. 2020;62(11):e657-64. [Link] [DOI:10.1097/JOM.0000000000002028]
32. Wong TKM, Man SS, Chan AHS. Exploring the acceptance of PPE by construction workers: An extension of the technology acceptance model with safety management practices and safety consciousness. Saf Sci. 2021;139:105239. [Link] [DOI:10.1016/j.ssci.2021.105239]
33. Huang YH, Chen PY, Grosch JW. Safety climate: New developments in conceptualization, theory, and research. Accid Anal Prev. 2010;42(5):1421-2. [Link] [DOI:10.1016/j.aap.2009.12.007]
34. Probst TM, Brubaker TL. The effects of job insecurity on employee safety outcomes: Cross-sectional and longitudinal explorations. J Occup Health Psychol. 2001;6(2):139-59. [Link] [DOI:10.1037/1076-8998.6.2.139]
35. Ronis DL, Hong O, Lusk SL. Comparison of the original and revised structures of the Health Promotion Model in predicting construction workers' use of hearing protection. Res Nurs Health. 2006;29(1):3-17. [Link] [DOI:10.1002/nur.20111]
36. Lusk SL, Ronis DL, Hogan MM. Test of the health promotion model as a causal model of construction workers' use of hearing protection. Res Nurs Health. 1997;20(3):183-94.
https://doi.org/10.1002/(SICI)1098-240X(199706)20:3<183::AID-NUR2>3.0.CO;2-E [Link] [DOI:10.1002/(SICI)1098-240X(199706)20:33.0.CO;2-E]
37. Shin Y, Yun S, Pender NJ, Jang H. Test of the health promotion model as a causal model of commitment to a plan for exercise among Korean adults with chronic disease. Res Nurs Health. 2005;28(2):117-25. [Link] [DOI:10.1002/nur.20060]
38. Khoshakhlagh AH, Malakoutikhah M, Park J, Kodnoueieh MD, Boroujeni ZR, Bahrami M, et al. Assessing personal protective equipment usage and its correlation with knowledge, attitudes, performance, and safety culture among workers in small and medium-sized enterprises. BMC Public Health. 2024;24(1):1987. [Link] [DOI:10.1186/s12889-024-19517-3]
39. Alemu AA, Yitayew M, Azazeh A, Kebede S. Utilization of personal protective equipment and associated factors among building construction workers in Addis Ababa, Ethiopia, 2019. BMC Public Health. 2020;20(1):794. [Link] [DOI:10.1186/s12889-020-08889-x]
40. Aram SA, Saalidong BM, Appiah A, Utip IB. Occupational health and safety in mining: Predictive probabilities of Personal Protective Equipment (PPE) use among artisanal goldminers in Ghana. PLoS One. 2021;16(9):e0257772. [Link] [DOI:10.1371/journal.pone.0257772]
41. Rowan NJ, Laffey JG. Unlocking the surge in demand for personal and protective equipment (PPE) and improvised face coverings arising from coronavirus disease (COVID-19) pandemic-Implications for efficacy, re-use and sustainable waste management. Sci Total Environ. 2021;752:142259. [Link] [DOI:10.1016/j.scitotenv.2020.142259]
42. La Torre G, Marte M, Previte CM, Barone LC, Picchioni F, Chiappetta M, et al. The synergistic effect of time of exposure, distance and no use of personal protective equipment in the determination of SARS-CoV-2 infection: Results of a contact tracing follow-up study in healthcare workers. Int J Environ Res Public Health. 2021;18(18):9456. [Link] [DOI:10.3390/ijerph18189456]
43. Stoia M, Oancea S. Workplace health promotion program on using dietary antioxidants (anthocyanins) in chemical exposed workers. Procedia Eng. 2012;42:1989-96. [Link] [DOI:10.1016/j.proeng.2012.07.595]
44. Boakye MK, Adanu SK, Coffie GH, Adzivor EK, Ayimah JC. Building construction artisans' level of access to personal protective equipment (PPE) and the perceived barriers and motivating factors of adherence to its use. J Environ Public Health. 2022;2022:4870731. [Link] [DOI:10.1155/2022/4870731]
45. Alinejad N, Bijani M, Malekhosseini M, Nasrabadi M, Harsini PA, Jeihooni AK. Effect of educational intervention based on health belief model on nurses' compliance with standard precautions in preventing needle stick injuries. BMC Nurs. 2023;22(1):180. [Link] [DOI:10.1186/s12912-023-01347-0]
46. Sorensen G, McLellan D, Dennerlein JT, Pronk NP, Allen JD, Boden LI, et al. Integration of health protection and health promotion: Rationale, indicators, and metrics. J Occup Environ Med. 2013;55(12 Suppl):S12-8. [Link] [DOI:10.1097/JOM.0000000000000032]
47. Cooklin A, Joss N, Husser E, Oldenburg B. Integrated approaches to occupational health and safety: A systematic review. Am J Health Promot. 2017;31(5):401-12. [Link] [DOI:10.4278/ajhp.141027-LIT-542]
48. Pender NJ. Health promotion model manual. Ann Arbor: The University of Michigan; 2011. [Link]
49. Yun SN, Kim JH. Health-promoting behaviors of the women workers at the manufacturing industry-based on the Pender's health promotion model. Korean J Occup Health Nurs. 1999;8(2):130-40. [Link]
50. Luo YF, Chen LC, Yang SC, Hong S. Knowledge, attitude, and practice (KAP) toward COVID-19 pandemic among the public in Taiwan: A cross-sectional study. Int J Environ Res Public Health. 2022;19(5):2784. [Link] [DOI:10.3390/ijerph19052784]
51. Sakraida TJ. Health promotion model. Nurs Theor Their Work. 2010;7:434-53. [Link]
52. Aqtam I, Darawwad M. Health promotion model: An integrative literature review. Open J Nurs. 2018;8(7):485-503. [Link] [DOI:10.4236/ojn.2018.87037]
53. Galloway RD. Health promotion: Causes, beliefs and measurements. Clin Med Res. 2003;1(3):249-58. [Link] [DOI:10.3121/cmr.1.3.249]
54. Donaghy J. Organisational support improves adherence to infection prevention and control guidelines. Evid Based Nurs. 2022;25(1):10. [Link] [DOI:10.1136/ebnurs-2020-103305]
55. Crossan F. Research philosophy: Towards an understanding. Nurse Res. 2003;11(1):46-55. [Link] [DOI:10.7748/nr2003.10.11.1.46.c5914]
56. Paré G. Investigating information systems with positivist case research. Commun Assoc Inf Syst. 2004;13(1):18. [Link] [DOI:10.17705/1CAIS.01318]
57. Park YS, Konge L, Artino AR. The positivism paradigm of research. Acad Med. 2020;95(5):690-4. [Link] [DOI:10.1097/ACM.0000000000003093]
58. Green WM. Moving beyond positivism: Integrating transformative perspectives in health professions education and evaluation. In: Assessment, evaluation, and accountability in adult education. London: Routledge; 2020. p. 149-63. [Link] [DOI:10.4324/9781003443117-12]
59. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180-91. [Link] [DOI:10.1002/nur.20247]
60. Lu L, Shi L, Han L, Ling L. Individual and organizational factors associated with the use of personal protective equipment by Chinese migrant workers exposed to organic solvents. Saf Sci. 2015;76:168-74. [Link] [DOI:10.1016/j.ssci.2014.11.025]
61. Nichol K, Bigelow P, O'Brien-Pallas L, McGeer A, Manno M, Holness DL. The individual, environmental, and organizational factors that influence nurses' use of facial protection to prevent occupational transmission of communicable respiratory illness in acute care hospitals. Am J Infect Control. 2008;36(7):481-7. [Link] [DOI:10.1016/j.ajic.2007.12.004]
62. Bottorff JL, Johnson JL, Ratner PA, Hayduk LA. The effects of cognitive-perceptual factors on health promotion behavior maintenance. Nurs Res. 1996;45(1):30-6. [Link] [DOI:10.1097/00006199-199601000-00006]
63. Sørensen HE, Slater SF. Development and empirical validation of symmetric component measures of multidimensional constructs: customer and competitor orientation. Psychol Rep. 2008;103(1):199-213. [Link] [DOI:10.2466/pr0.103.1.199-213]
64. Greenland S, Senn SJ, Rothman KJ, Carlin JB, Poole C, Goodman SN, et al. Statistical tests, p values, confidence intervals, and power: A guide to misinterpretations. Eur J Epidemiol. 2016;31(4):337-50. [Link] [DOI:10.1007/s10654-016-0149-3]
65. Cain KC, Breslow NE. Logistic regression analysis and efficient design for two-stage studies. Am J Epidemiol. 1988;128(6):1198-206. [Link] [DOI:10.1093/oxfordjournals.aje.a115074]
66. Murtaugh PA. In defense of p values. Ecology. 2014;95(3):611-7. [Link] [DOI:10.1890/13-0590.1]
67. McCullagh M, Lusk SL, Ronis DL. Factors influencing use of hearing protection among farmers: A test of the pender health promotion model. Nurs Res. 2002;51(1):33-9. [Link] [DOI:10.1097/00006199-200201000-00006]
68. Edelson J, Neitzel R, Meischke H, Daniell W, Sheppard L, Stover B, et al. Predictors of hearing protection use in construction workers. Ann Occup Hyg. 2009;53(6):605-15. [Link]
69. Forst L, Noth IM, Lacey S, Bauer S, Skinner S, Petrea R, et al. Barriers and benefits of protective eyewear use by Latino farm workers. J Agromedicine. 2006;11(2):11-7. [Link] [DOI:10.1300/J096v11n02_04]
70. Shamsi M, Shams M, Nilipour Tabatabaei A. Attitude and behaviors related to using personal protective equipments: Audience analysis to design a behavior change intervention for employees in constructing underground stations in Esfahan. Iran Occup Health. 2013;10(3):20-8. [Persian] [Link]
71. Sehsah R, El-Gilany AH, Ibrahim AM. Personal protective equipment (PPE) use and its relation to accidents among construction workers. LA MEDICINA DEL LAVORO. 2020;111(4):285-95. [Link] [DOI:10.23749/mdl.v111i4.9398]
72. Mahmood SU, Crimbly F, Khan S, Choudry E, Mehwish S. Strategies for rational use of personal protective equipment (PPE) among healthcare providers during the COVID-19 crisis. Cureus. 2020;12(5):e8248. [Link] [DOI:10.7759/cureus.8248]
73. Situmeang L, Sulistiyani, Trianingsih NKA, Kismiyati. Analysis of factors affecting compliance of health workers using personal protective equipment. Sci Midwifery. 2023;10(6):4908-15. [Link]
74. Duan X, Sun H, He Y, Yang J, Li X, Taparia K, et al. Personal protective equipment in COVID-19: Impacts on health performance, work-related injuries, and measures for prevention. J Occup Environ Med. 2021;63(3):221-5. [Link] [DOI:10.1097/JOM.0000000000002123]
75. Patel R, Ali M, Bleasdale SC, Mena Lora AJ. Cost of personal protective equipment during the first wave of the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol. 2023;44(11):1897-9. [Link] [DOI:10.1017/ice.2023.115]
76. Ganczak, M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect. 2007;66(4):346-51. [Link] [DOI:10.1016/j.jhin.2007.05.007]
77. Drouard SHP, Ahmed T, Amor Fernandez P, Baral P, Peters M, Hansen P, et al. Availability and use of personal protective equipment in low-and middle-income countries during the COVID-19 pandemic. PLoS One. 2023;18(7):e0288465. [Link] [DOI:10.1371/journal.pone.0288465]
78. Balkhyour MA, Ahmad I, Rehan M. Assessment of personal protective equipment use and occupational exposures in small industries in Jeddah: Health implications for workers. Saudi J Biol Sci. 2019;26(4):653-9. [Link] [DOI:10.1016/j.sjbs.2018.06.011]
79. Wu Chuan An WC, Cai MiaoSen CM, Liu KaiQian LK. Survey of knowledge of occupational hazards and pretection in foreign funded enterprises. 2008. [Link]
80. Liu S, Shuai Z, Ye F, Mo Z. Survey of occupational health supervision for enterprises utilizing organic solvents in one county of Dongguan city in 2004. Chin J Ind Hyg Occup Dis. 2006;24(6):368-9. [Chinese] [Link]
81. Chia SE, Koh D, Fones C, Qian F, Ng V, Tan BH, et al. Appropriate use of personal protective equipment among healthcare workers in public sector hospitals and primary healthcare polyclinics during the SARS outbreak in Singapore. Occup Environ Med. 2005;62(7):473-7. [Link] [DOI:10.1136/oem.2004.015024]
82. Andonian J, Kazi S, Therkorn J, Benishek L, Billman C, Schiffhauer M, et al. Effect of an intervention package and teamwork training to prevent healthcare personnel self-contamination during personal protective equipment doffing. Clin Infect Dis. 2019;69(Suppl 3):S248-55. [Link] [DOI:10.1093/cid/ciz618]
83. Çiriş Yildiz C, Ulaşli Kaban H, Tanriverdi FŞ. COVID-19 pandemic and personal protective equipment: Evaluation of equipment comfort and user attitude. Arch Environ Occup Health. 2022;77(1):1-8. [Link] [DOI:10.1080/19338244.2020.1828247]
84. Olson R, Grosshuesch A, Schmidt S, Gray M, Wipfli B. Observational learning and workplace safety: The effects of viewing the collective behavior of multiple social models on the use of personal protective equipment. J Safety Res. 2009;40(5):383-7. [Link] [DOI:10.1016/j.jsr.2009.07.004]
85. George J, Shafqat N, Verma R, Patidar AB. Factors influencing compliance with personal protective equipment (PPE) use among healthcare workers. Cureus. 2023;15(2):e35269. [Link] [DOI:10.7759/cureus.35269]
86. Okello TR, Kansime K, Odora J, Apio JA, Pecorella I. Barriers and factors affecting personal protective equipment usage in St. Mary's Hospital Lacor in Northern Uganda. East Cent Afr J Surg. 2017;22(1):59-65. [Link] [DOI:10.4314/ecajs.v22i1.8]
87. Neves HC, Souza AC, Medeiros M, Munari DB, Ribeiro LC, Tipple AF. Safety of nursing staff and determinants of adherence to personal protective equipment. REVISTA LATINO-AMERICANA DE ENFERMAGEM. 2011;19(2):354-61. [Link] [DOI:10.1590/S0104-11692011000200018]
88. Lusk SL, Ronis DL, Kerr MJ, Atwood JR. Test of the health promotion model as a causal model of workers' use of hearing protection. Nurs Res. 1994;43(3):151-7. [Link] [DOI:10.1097/00006199-199405000-00005]
89. Melamed S, Rabinowitz S, Feiner M, Weisberg E, Ribak J. Usefulness of the protection motivation theory in explaining hearing protection device use among male industrial workers. Health Psychol. 1996;15(3):209-15. [Link] [DOI:10.1037/0278-6133.15.3.209]
90. White MC, Baker EL, Larson MB, Wolford R. The role of personal beliefs and social influences as determinants of respirator use among construction painters. Scand J Work Environ Health. 1988;14(4):239-45. [Link] [DOI:10.5271/sjweh.1926]
91. Budhathoki SS, Singh SB, Sagtani RA, Niraula SR, Pokharel PK. Awareness of occupational hazards and use of safety measures among welders: A cross-sectional study from Eastern Nepal. BMJ Open. 2014;4(6):e004646. [Link] [DOI:10.1136/bmjopen-2013-004646]
92. Liang Y, Xiang Q. Occupational health services in PR China. Toxicology. 2004;198(1-3):45-54. [Link] [DOI:10.1016/j.tox.2004.01.018]
93. Chen X, Yang F, Cheng S, Yuan S. Occupational health and safety in China: A systematic analysis of research trends and future perspectives. Sustainability. 2023;15(19):14061. [Link] [DOI:10.3390/su151914061]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






