Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 375-381 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohsenipouya H, Hashemi A, Hosseinnataj A, Roy N, Mamun M. Strengths, Weaknesses, Opportunities, and Threats Analysis of an Electronic Health Record in Iran. Health Educ Health Promot 2024; 12 (3) :375-381
URL: http://hehp.modares.ac.ir/article-5-75487-en.html
URL: http://hehp.modares.ac.ir/article-5-75487-en.html
1- Department of Health Education and Promotion, Faculty of Nursing, Mazandaran University of Medical Sciences, Behshahr, Iran
2- “Students Research Committee” and “Department of Nursing, Faculty of Nursing, Mazandaran University of Medical Sciences, Behshahr, Iran
3- Department of Biostatistics, Faculty of Health, Mazandaran University of Medical Sciences, Sari, Iran
4- Department of Biochemistry and Food Analysis, Patuakhali Science and Technology University, Patuakhali, Bangladesh
5- Department of Public Health and Informatics, Jahangirnagar University, Dhaka, Bangladesh
2- “Students Research Committee” and “Department of Nursing, Faculty of Nursing, Mazandaran University of Medical Sciences, Behshahr, Iran
3- Department of Biostatistics, Faculty of Health, Mazandaran University of Medical Sciences, Sari, Iran
4- Department of Biochemistry and Food Analysis, Patuakhali Science and Technology University, Patuakhali, Bangladesh
5- Department of Public Health and Informatics, Jahangirnagar University, Dhaka, Bangladesh
Full-Text [PDF 674 kb]
(798 Downloads)
| Abstract (HTML) (667 Views)
Full-Text: (7 Views)
Introduction
According to the World Health Organization (WHO), “eHealth” refers to the safe and efficient use of information and communication technologies (ICTs) in healthcare, including activities, such as health surveillance, health literature, health education, and knowledge and research [1]. Considering the rapid progress of information technology (IT) and the vast capabilities of electronic health records (EHRs), it is inevitable that EHRs will soon prevail in medical treatment, supplanting conventional paper records and becoming the principal method of communication for patient-related matters [2, 3]. An EHR is a systematic collection of health data about individuals and populations, stored in a digital format [4, 5]. EHRs may include a range of information, including demographic details, medical history, medication and allergy records, immunization status, laboratory test results, radiographic images, vital signs, personal attributes such as age and weight, and billing data [4, 6].
EHRs offer many advantages, including enhanced healthcare quality [7-9], heightened customer satisfaction [10], timely access to data [11, 12], availability of diverse clinical data [13], efficient storage and retrieval of medical history, improved healthcare system efficiency [13, 14], cost reductions, decreased medication errors, improved data accessibility and tracking, and enhanced clinical outcomes [7, 11, 15]. The literature has described the problems related to the adoption and implementation of EHRs, despite their numerous merits [16, 17]. The challenges pertain to the integrity and availability of healthcare data, as well as the potential risks to patient safety, information privacy, user resistance, limited technological knowledge, and inadequate computer skills [18]. These challenges may also contribute to the disparity between developing and developed countries [19].
Iran’s healthcare system has seen significant progress with a focus on providing widespread access to healthcare services. In 2007, the Ministry of Health introduced SEPAS, a national initiative aimed at developing a comprehensive EHR system and creating a unified health information network across the country. SEPAS serves as an extensive EHR system used nationwide in Iran, centralizing patient information from various hospital visits into a unified database [20]. Hospital information systems transmit patient data to SEPAS, encompassing demographic details, diagnoses, procedures, para-clinical findings, and financial information. The Ministry of Health’s databases retain this data for future reference. The software infrastructure is decentralized, with SEPAS nodes situated at various medical university facilities nationwide. Hospitals affiliated with these universities share health information through their respective SEPAS nodes [21]. Presently, around 15 years after 2008, Iran has successfully shifted from lacking an electronic EHR system to attaining comprehensive coverage across the entire nation. However, the extent of success achieved by this project remains uncertain [20].
Previous research examining the efficacy of EHRs has identified a necessity for enhancing the EHR system [22]. There is a limited number of studies that have been carried out to thoroughly assess EHRs in Iran. Asadi et al. [23] analyzed the SEPAS project and concluded that it lacked adequate consideration of essential resources and requirements, leading to an inability to meet its intended goals. Despite this, there has been minimal exploration of viewpoints regarding the effectiveness of EHRs, even though potential deficiencies could impact decisions on their implementation. Therefore, there is a research gap in evaluating the efficacy of SEPAS within hospital environments. With the increasing importance of the SEPAS system in Iran and the substantial financial investments made by the Ministry of Health for its advancement, it is vital to assess the success of SEPAS.
The strengths, weaknesses, opportunities, and threats (SWOT) analysis is a valuable tool that healthcare organizations can utilize for any health-related project. This is because different groups within the organization often have varying goals, interests, and needs. Healthcare providers use SWOT analysis for strategic planning in all areas of healthcare. This form of analysis is now considered an essential component of situational analysis due to its simplicity, comprehensibility, and relevance in all types of organizations [24].
Iran must understand the SWOT elements related to the deployment of EHRs as it aims to align its healthcare infrastructure with global norms [25]. In recent years, Iran’s EHR system has been implemented; however, there is a lack of detailed information on its effectiveness, especially in the northern regions of the country. This study examined the SEPAS project from two viewpoints, including strengths and weaknesses, and opportunities and threats related to EHR implementation as perceived by healthcare practitioners and managers. The study outcomes are expected to assist policymakers, managers, and healthcare professionals in identifying obstacles, areas for improvement, opportunities, and strengths. Through this initiative, despite limited staffing and financial resources, enhanced efficiency and quality improvements in healthcare services are anticipated.
Instrument and Methods
Sampling and participants
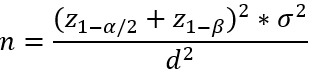
This cross-sectional study was conducted from May to September 2023, involving managers (n=63) and practitioners (n=110) of EHRs. Using purposive sampling methods, the participants were selected from the health centers of Mazandaran province. The inclusion criteria for participation in this study included familiarity with EHRs, having at least five years of clinical or administrative work experience, and knowledge of the process of recording and processing hospital information. Managers and practitioners were excluded if they answered less than 100% of the questionnaire questions. Mirani et al.[26] showed that the mean importance level of technical obstacles in the creation and implementation of the electronic health file was higher than that of all other obstacles (71.00±20.31). Considering the measurement error (d) of five units, the first type error (α) of 5%, the test power (1-β) of 90%, and using the following formula, at least 173 samples were considered.
Data collection
Sociodemographic characteristics
This study collected socio-demographic characteristics, including age, gender, work history, education level, and familiarity with EHRs.
SWOT Scale
The SWOT Scale developed by Shahmoradi et al. [6, 25] was used for data collection. The validity of the questionnaire was confirmed based on content validity and face validity, respectively, by using valid scientific texts and obtaining the opinions of ten experts in the fields of health information management and technology and medical informatics. The reliability of the scale was determined by calculating the internal consistency (α=0.93). This questionnaire consists of 30 Likert-type questions with five possible answers. There are eight questions about strengths, seven questions about weaknesses, seven questions about opportunities, and 8 questions about threats [6, 25]. The reliability of the scale was determined to be 0.89 for the present study.
Data analysis
Data were analyzed using SPSS version 23 p<0.05. Descriptive statistics were employed to report the frequency, percentages, and means for summarizing the characteristics of the individuals. To assess each question a scale ranging from one to ten was used to evaluate the significance of each question in relation to the EHR, with one indicating a lack of importance and ten denoting utmost importance. The weight of each factor was derived by summing the scores of one question across all questionnaires and dividing that total by the score of all factors. The responses were measured on a five-point scale, with a score of one indicating basic weakness and a score of five indicating excellence. The mean score was determined by calculating the average of these numbers. The weighted score was calculated by multiplying the weight by the mean. Ultimately, through the implementation of a weighted score, questions with higher scores are considered to have a greater level of importance.
The data are available upon reasonable request from the corresponding author.
Findings
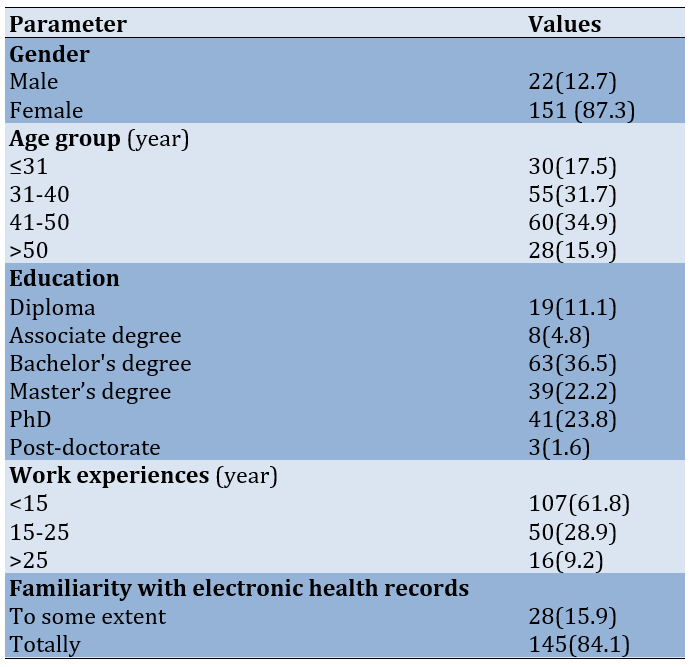
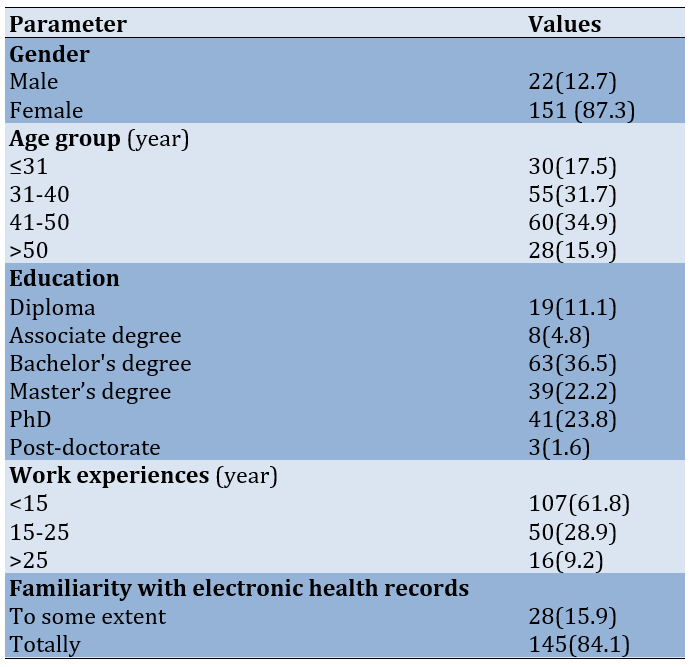
The majority (87.3%) of interviewees were female, and most (34.9%) were between the ages of 41 and 50, with a bachelor’s degree (36.5%). In terms of work experience, 61.8% of participants had fewer than 15 years of experience, and 84.1% reported a high level of familiarity with EHRs (Table 1).
Table 1. Frequency of the demographic characteristics of participants
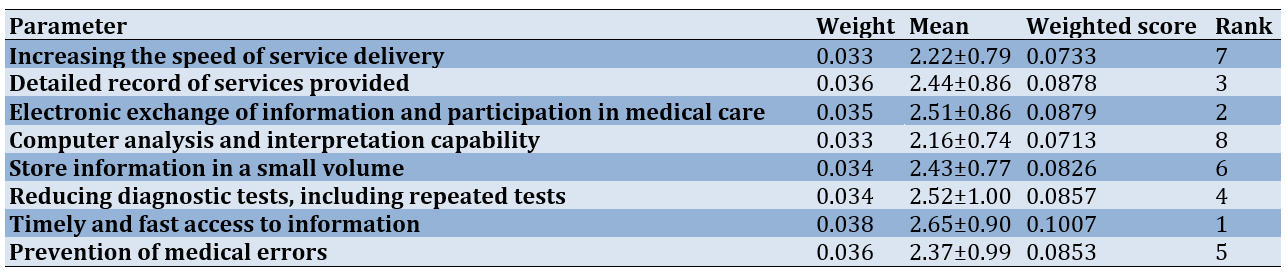
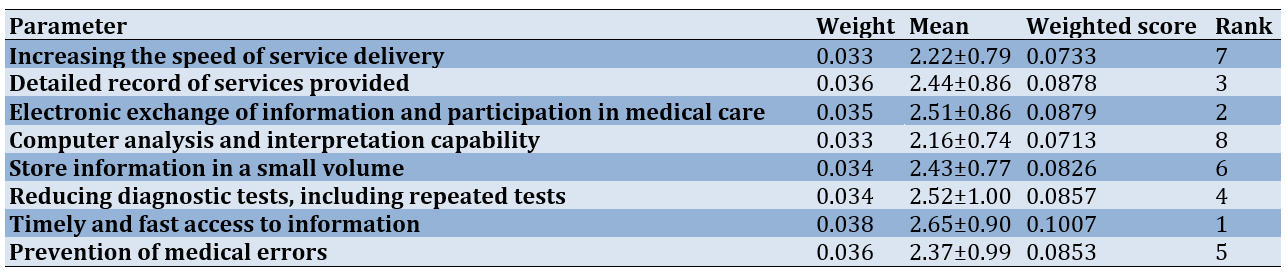
The most important issues were “timely and fast access to information” (weight score=0.1007) and “electronic exchange of information and participation in medical care” (weight score=0.0879), while the least important strength was “ability of computer analysis and interpretation” (weight score=0.0713; Table 2).
Table 2. Strengths of implementing electronic health records
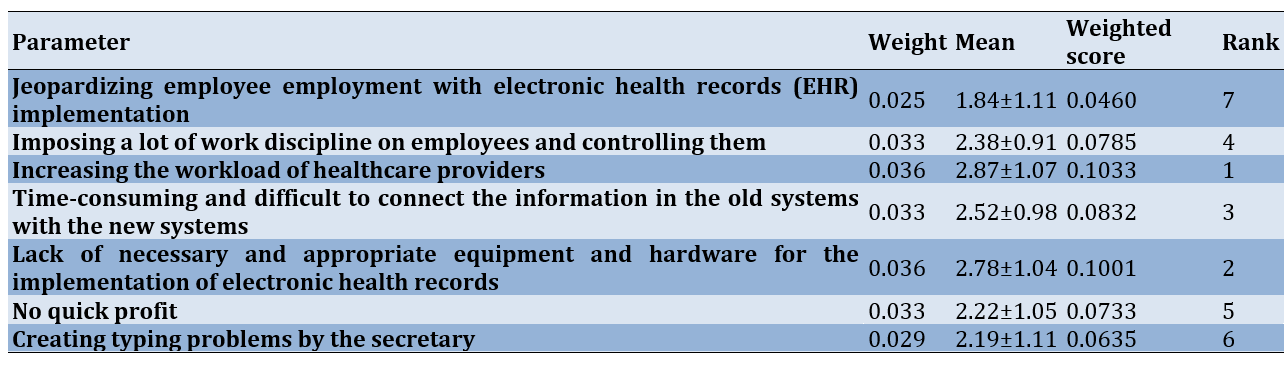
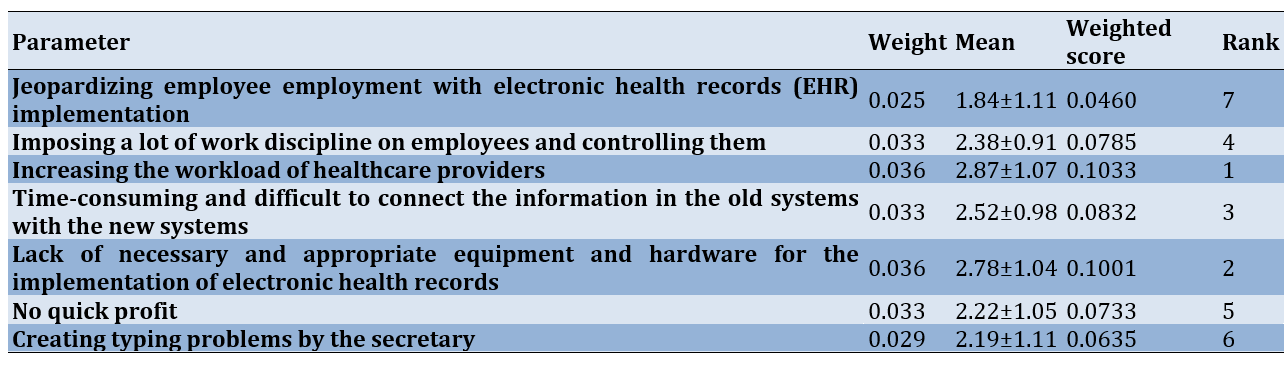
The most significant weaknesses were “increasing the workload of healthcare providers” (weight score=0.1033) and “lack of necessary and suitable equipment and hardware for the implementation of EHRs” (weight score=0.1001), while the least important weakness was “putting the job positions of employees at risk with the implementation of EHR” (weight score=0.0460; Table 3).
Table 3. Weaknesses of implementing electronic health records
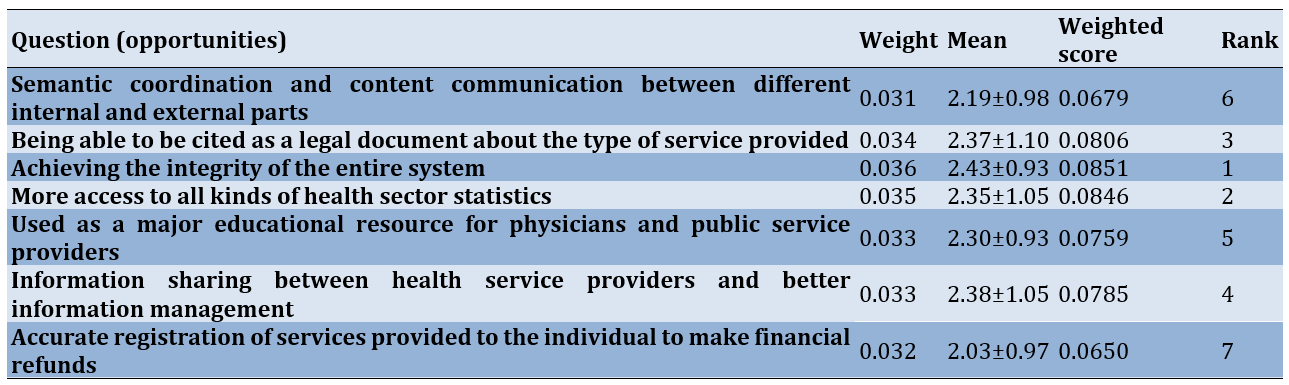
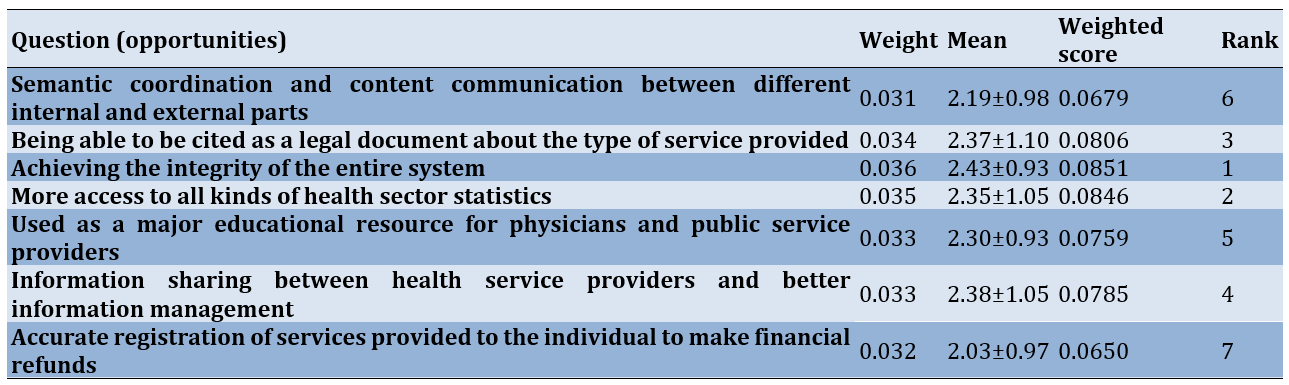
The most important opportunities included “achieving integration in the entire system” (weight score=0.0851) and “greater access to all types of statistics in the health sector” (weight score=0.0846), while the least important opportunity was “accurately recording the services provided to individuals to facilitate financial reimbursements” (weight score=0.0650; Table 4).
Table 4. Opportunities to implement electronic health records
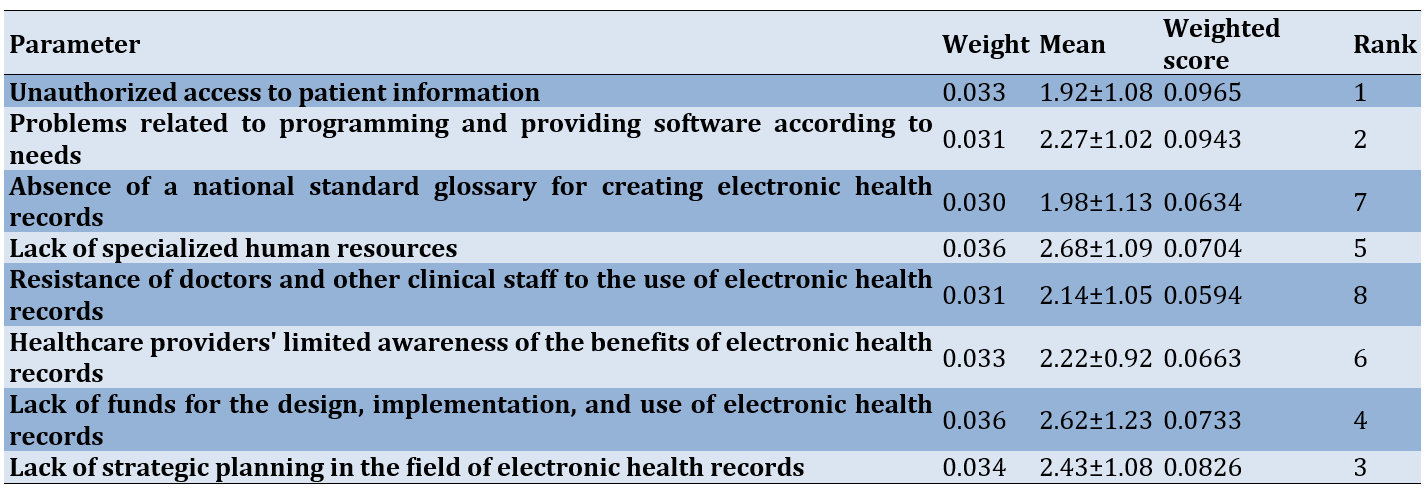
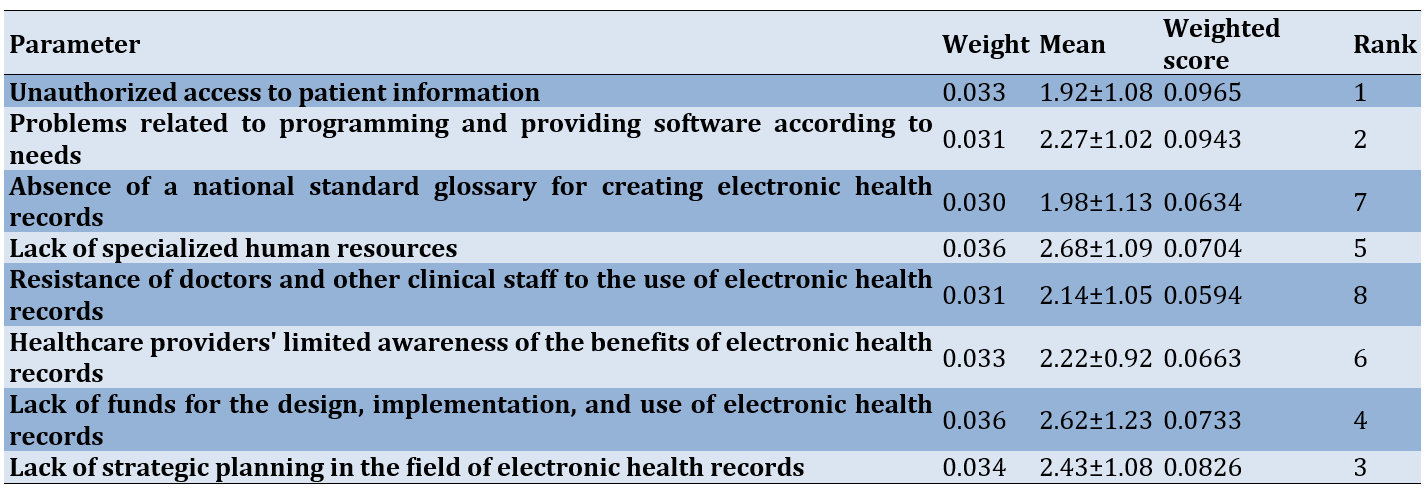
The most significant threats included “unauthorized access to patient information” (weight score=0.0965) and “problems related to programming and providing software according to needs” (weight score=0.0943), while the least important threat was “resistance of doctors and other clinical staff to the use of EHRs” (weight score=0.0594; Table 5).
Table 5. Threats of implementing electronic health records
Discussion
This study examined the use of SWOT analysis in EHR systems in hospitals affiliated with the Mazandaran University of Medical Sciences. The results highlighted the importance of evaluating various administrative, technical, financial, and organizational aspects when planning for EHR system implementation.
The most important strengths of implementing the EHRs were “timely and fast access to information” and “electronic exchange of information and participation in medical care.” Consistent with the results of our study, the authors of a study conducted in hospitals affiliated with the Tehran University of Medical Sciences [25] reported that timely and fast information access is the most significant strength. In line with our study, another recent systematic analysis of the literature revealed that the primary factors promoting the adoption and utilization of EHRs are access to comprehensive information and the availability of accurate, error-free data [11]. Shahmoradi et al. found that preventing medical errors is the lowest strength; however, in our study, the ability to analyze and interpret information using computers was identified as the lowest strength [25]. Therefore, training programs should focus on teaching healthcare professionals how to effectively analyze and interpret information using computer systems so that they can confidently navigate and extract valuable insights from EHR platforms.
Shahmoradi et al. [25] reported that a notable limitation of the EHR program implementation is the lack of a suitable infrastructure for EHR implementation. Our study highlighted several areas that require attention, including the heavy workload on healthcare providers and the insufficient equipment and hardware for EHR implementation. In Abbasi et al.'s research, the majority of users emphasize the importance of addressing technical infrastructure, data security, and system support before implementation. The current system lacks adequate facilities for interfacing with other information systems, potentially impacting its efficiency. Additionally, there is a lack of developed programs to support the system or ensure data security [27]. Consistent with this study, another study [28] has also discovered that physicians remain greatly concerned about the usability and workload associated with EHRs. Furthermore, Abbasi et al. reported that some users identify an excessive workload as a primary factor for the non-utilization of the system [27]. Therefore, it is crucial to prioritize investments in robust technological infrastructure and provide healthcare facilities with the necessary hardware and equipment. Additionally, strategies should be developed to address design flaws and promote innovation, ultimately improving the usability of EHR systems and reducing physician workload [29]. These efforts could lead to the successful implementation of EHRs in Iran.
We discovered that enhancing integration across the entire system and improving access to various healthcare statistics presented significant opportunities. Conversely, the precise recording of services for financial reimbursements was considered less crucial. In contrast to our results, Shahmoradi et al. [25] reported that information sharing among healthcare providers and improved information management are key opportunities in EHR implementation. Participants also emphasized the EHR’s potential as a training tool for medical professionals and the importance of accessing diverse health data. Moreover, other studies indicate that physicians serve as important facilitators and gatekeepers by motivating patients and enhancing their awareness of EHRs [30, 31]. By integrating the key opportunities identified in our research, healthcare systems can optimize EHR implementation, promoting enhanced integration, effective information management, and customization to meet their unique needs.
Shahmoradi et al. [25] have highlighted the challenges faced in the implementation of EHRs, such as the absence of strategic planning and resistance from clinical staff, while the lack of national standard terminology is a lesser concern. In our study, issues, like unauthorized access to patient information and software that does not meet user needs were identified as crucial challenges. Patient privacy risks due to the expansion of e-health technology were also noted, causing increased patient concern. Griesser et al. declared that certain French participants raise concerns about data security at different stages, including collection, transmission, and storage. According to one participant, “I am unable to safeguard my data privacy. I cannot control the exposure of my personal information; we witness instances, like the Facebook scandal daily, and it seems unstoppable” [32]. Policymakers are working toward enhancing security and privacy measures, including the requirement for audit trails in EHR systems to effectively monitor access to patient records [3, 13].
One limitation of this study is the paucity of previous research in this area, making it difficult to benchmark our findings. Self-reported data were used in this study, potentially introducing bias related to memory lapses or participant preferences in their responses. Furthermore, as this research was conducted in a single province, there is a need for more extensive national-level studies in the future to provide broader insights. This study highlights the significance of various factors in achieving success in implementing EHRs in Mazandaran University hospitals. Therefore, increased support in managing personnel workload, maintaining infrastructure, and organizing essential training workshops for medical staff and personnel in this field could potentially lead to greater success.
Conclusion
The success of HER implementation depends on a thorough understanding of its various aspects, including strengths, weaknesses, threats, and opportunities.
Acknowledgments: The authors thank all the study participants.
Ethical Permissions: The researchers followed the Declaration of Helsinki guidelines and obtained approval from the Ethics Committee of Mazandaran University of Medical Sciences (reference: IR.MAZUMS.REC.1401.466). Participants were provided with detailed information about the study’s objectives, potential risks and benefits, and their right to refuse participation. They were assured of voluntary participation and the freedom to withdraw at any point. Each participant signed an informed consent form indicating their agreement to participate. Ethical considerations focused on protecting the privacy and confidentiality of participant information, ensuring that data would be used for research purposes only, and maintaining participant anonymity in the questionnaire.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Mohsenipouya H (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Hashemi AH (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Hosseinnataj A (Third Author), Statistical Analyst (10%); Roy N (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Mamun MA (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: The study did not receive any funding.
According to the World Health Organization (WHO), “eHealth” refers to the safe and efficient use of information and communication technologies (ICTs) in healthcare, including activities, such as health surveillance, health literature, health education, and knowledge and research [1]. Considering the rapid progress of information technology (IT) and the vast capabilities of electronic health records (EHRs), it is inevitable that EHRs will soon prevail in medical treatment, supplanting conventional paper records and becoming the principal method of communication for patient-related matters [2, 3]. An EHR is a systematic collection of health data about individuals and populations, stored in a digital format [4, 5]. EHRs may include a range of information, including demographic details, medical history, medication and allergy records, immunization status, laboratory test results, radiographic images, vital signs, personal attributes such as age and weight, and billing data [4, 6].
EHRs offer many advantages, including enhanced healthcare quality [7-9], heightened customer satisfaction [10], timely access to data [11, 12], availability of diverse clinical data [13], efficient storage and retrieval of medical history, improved healthcare system efficiency [13, 14], cost reductions, decreased medication errors, improved data accessibility and tracking, and enhanced clinical outcomes [7, 11, 15]. The literature has described the problems related to the adoption and implementation of EHRs, despite their numerous merits [16, 17]. The challenges pertain to the integrity and availability of healthcare data, as well as the potential risks to patient safety, information privacy, user resistance, limited technological knowledge, and inadequate computer skills [18]. These challenges may also contribute to the disparity between developing and developed countries [19].
Iran’s healthcare system has seen significant progress with a focus on providing widespread access to healthcare services. In 2007, the Ministry of Health introduced SEPAS, a national initiative aimed at developing a comprehensive EHR system and creating a unified health information network across the country. SEPAS serves as an extensive EHR system used nationwide in Iran, centralizing patient information from various hospital visits into a unified database [20]. Hospital information systems transmit patient data to SEPAS, encompassing demographic details, diagnoses, procedures, para-clinical findings, and financial information. The Ministry of Health’s databases retain this data for future reference. The software infrastructure is decentralized, with SEPAS nodes situated at various medical university facilities nationwide. Hospitals affiliated with these universities share health information through their respective SEPAS nodes [21]. Presently, around 15 years after 2008, Iran has successfully shifted from lacking an electronic EHR system to attaining comprehensive coverage across the entire nation. However, the extent of success achieved by this project remains uncertain [20].
Previous research examining the efficacy of EHRs has identified a necessity for enhancing the EHR system [22]. There is a limited number of studies that have been carried out to thoroughly assess EHRs in Iran. Asadi et al. [23] analyzed the SEPAS project and concluded that it lacked adequate consideration of essential resources and requirements, leading to an inability to meet its intended goals. Despite this, there has been minimal exploration of viewpoints regarding the effectiveness of EHRs, even though potential deficiencies could impact decisions on their implementation. Therefore, there is a research gap in evaluating the efficacy of SEPAS within hospital environments. With the increasing importance of the SEPAS system in Iran and the substantial financial investments made by the Ministry of Health for its advancement, it is vital to assess the success of SEPAS.
The strengths, weaknesses, opportunities, and threats (SWOT) analysis is a valuable tool that healthcare organizations can utilize for any health-related project. This is because different groups within the organization often have varying goals, interests, and needs. Healthcare providers use SWOT analysis for strategic planning in all areas of healthcare. This form of analysis is now considered an essential component of situational analysis due to its simplicity, comprehensibility, and relevance in all types of organizations [24].
Iran must understand the SWOT elements related to the deployment of EHRs as it aims to align its healthcare infrastructure with global norms [25]. In recent years, Iran’s EHR system has been implemented; however, there is a lack of detailed information on its effectiveness, especially in the northern regions of the country. This study examined the SEPAS project from two viewpoints, including strengths and weaknesses, and opportunities and threats related to EHR implementation as perceived by healthcare practitioners and managers. The study outcomes are expected to assist policymakers, managers, and healthcare professionals in identifying obstacles, areas for improvement, opportunities, and strengths. Through this initiative, despite limited staffing and financial resources, enhanced efficiency and quality improvements in healthcare services are anticipated.
Instrument and Methods
Sampling and participants
This cross-sectional study was conducted from May to September 2023, involving managers (n=63) and practitioners (n=110) of EHRs. Using purposive sampling methods, the participants were selected from the health centers of Mazandaran province. The inclusion criteria for participation in this study included familiarity with EHRs, having at least five years of clinical or administrative work experience, and knowledge of the process of recording and processing hospital information. Managers and practitioners were excluded if they answered less than 100% of the questionnaire questions. Mirani et al.[26] showed that the mean importance level of technical obstacles in the creation and implementation of the electronic health file was higher than that of all other obstacles (71.00±20.31). Considering the measurement error (d) of five units, the first type error (α) of 5%, the test power (1-β) of 90%, and using the following formula, at least 173 samples were considered.
Data collection
Sociodemographic characteristics
This study collected socio-demographic characteristics, including age, gender, work history, education level, and familiarity with EHRs.
SWOT Scale
The SWOT Scale developed by Shahmoradi et al. [6, 25] was used for data collection. The validity of the questionnaire was confirmed based on content validity and face validity, respectively, by using valid scientific texts and obtaining the opinions of ten experts in the fields of health information management and technology and medical informatics. The reliability of the scale was determined by calculating the internal consistency (α=0.93). This questionnaire consists of 30 Likert-type questions with five possible answers. There are eight questions about strengths, seven questions about weaknesses, seven questions about opportunities, and 8 questions about threats [6, 25]. The reliability of the scale was determined to be 0.89 for the present study.
Data analysis
Data were analyzed using SPSS version 23 p<0.05. Descriptive statistics were employed to report the frequency, percentages, and means for summarizing the characteristics of the individuals. To assess each question a scale ranging from one to ten was used to evaluate the significance of each question in relation to the EHR, with one indicating a lack of importance and ten denoting utmost importance. The weight of each factor was derived by summing the scores of one question across all questionnaires and dividing that total by the score of all factors. The responses were measured on a five-point scale, with a score of one indicating basic weakness and a score of five indicating excellence. The mean score was determined by calculating the average of these numbers. The weighted score was calculated by multiplying the weight by the mean. Ultimately, through the implementation of a weighted score, questions with higher scores are considered to have a greater level of importance.
The data are available upon reasonable request from the corresponding author.
Findings
The majority (87.3%) of interviewees were female, and most (34.9%) were between the ages of 41 and 50, with a bachelor’s degree (36.5%). In terms of work experience, 61.8% of participants had fewer than 15 years of experience, and 84.1% reported a high level of familiarity with EHRs (Table 1).
Table 1. Frequency of the demographic characteristics of participants
The most important issues were “timely and fast access to information” (weight score=0.1007) and “electronic exchange of information and participation in medical care” (weight score=0.0879), while the least important strength was “ability of computer analysis and interpretation” (weight score=0.0713; Table 2).
Table 2. Strengths of implementing electronic health records
The most significant weaknesses were “increasing the workload of healthcare providers” (weight score=0.1033) and “lack of necessary and suitable equipment and hardware for the implementation of EHRs” (weight score=0.1001), while the least important weakness was “putting the job positions of employees at risk with the implementation of EHR” (weight score=0.0460; Table 3).
Table 3. Weaknesses of implementing electronic health records
The most important opportunities included “achieving integration in the entire system” (weight score=0.0851) and “greater access to all types of statistics in the health sector” (weight score=0.0846), while the least important opportunity was “accurately recording the services provided to individuals to facilitate financial reimbursements” (weight score=0.0650; Table 4).
Table 4. Opportunities to implement electronic health records
The most significant threats included “unauthorized access to patient information” (weight score=0.0965) and “problems related to programming and providing software according to needs” (weight score=0.0943), while the least important threat was “resistance of doctors and other clinical staff to the use of EHRs” (weight score=0.0594; Table 5).
Table 5. Threats of implementing electronic health records
Discussion
This study examined the use of SWOT analysis in EHR systems in hospitals affiliated with the Mazandaran University of Medical Sciences. The results highlighted the importance of evaluating various administrative, technical, financial, and organizational aspects when planning for EHR system implementation.
The most important strengths of implementing the EHRs were “timely and fast access to information” and “electronic exchange of information and participation in medical care.” Consistent with the results of our study, the authors of a study conducted in hospitals affiliated with the Tehran University of Medical Sciences [25] reported that timely and fast information access is the most significant strength. In line with our study, another recent systematic analysis of the literature revealed that the primary factors promoting the adoption and utilization of EHRs are access to comprehensive information and the availability of accurate, error-free data [11]. Shahmoradi et al. found that preventing medical errors is the lowest strength; however, in our study, the ability to analyze and interpret information using computers was identified as the lowest strength [25]. Therefore, training programs should focus on teaching healthcare professionals how to effectively analyze and interpret information using computer systems so that they can confidently navigate and extract valuable insights from EHR platforms.
Shahmoradi et al. [25] reported that a notable limitation of the EHR program implementation is the lack of a suitable infrastructure for EHR implementation. Our study highlighted several areas that require attention, including the heavy workload on healthcare providers and the insufficient equipment and hardware for EHR implementation. In Abbasi et al.'s research, the majority of users emphasize the importance of addressing technical infrastructure, data security, and system support before implementation. The current system lacks adequate facilities for interfacing with other information systems, potentially impacting its efficiency. Additionally, there is a lack of developed programs to support the system or ensure data security [27]. Consistent with this study, another study [28] has also discovered that physicians remain greatly concerned about the usability and workload associated with EHRs. Furthermore, Abbasi et al. reported that some users identify an excessive workload as a primary factor for the non-utilization of the system [27]. Therefore, it is crucial to prioritize investments in robust technological infrastructure and provide healthcare facilities with the necessary hardware and equipment. Additionally, strategies should be developed to address design flaws and promote innovation, ultimately improving the usability of EHR systems and reducing physician workload [29]. These efforts could lead to the successful implementation of EHRs in Iran.
We discovered that enhancing integration across the entire system and improving access to various healthcare statistics presented significant opportunities. Conversely, the precise recording of services for financial reimbursements was considered less crucial. In contrast to our results, Shahmoradi et al. [25] reported that information sharing among healthcare providers and improved information management are key opportunities in EHR implementation. Participants also emphasized the EHR’s potential as a training tool for medical professionals and the importance of accessing diverse health data. Moreover, other studies indicate that physicians serve as important facilitators and gatekeepers by motivating patients and enhancing their awareness of EHRs [30, 31]. By integrating the key opportunities identified in our research, healthcare systems can optimize EHR implementation, promoting enhanced integration, effective information management, and customization to meet their unique needs.
Shahmoradi et al. [25] have highlighted the challenges faced in the implementation of EHRs, such as the absence of strategic planning and resistance from clinical staff, while the lack of national standard terminology is a lesser concern. In our study, issues, like unauthorized access to patient information and software that does not meet user needs were identified as crucial challenges. Patient privacy risks due to the expansion of e-health technology were also noted, causing increased patient concern. Griesser et al. declared that certain French participants raise concerns about data security at different stages, including collection, transmission, and storage. According to one participant, “I am unable to safeguard my data privacy. I cannot control the exposure of my personal information; we witness instances, like the Facebook scandal daily, and it seems unstoppable” [32]. Policymakers are working toward enhancing security and privacy measures, including the requirement for audit trails in EHR systems to effectively monitor access to patient records [3, 13].
One limitation of this study is the paucity of previous research in this area, making it difficult to benchmark our findings. Self-reported data were used in this study, potentially introducing bias related to memory lapses or participant preferences in their responses. Furthermore, as this research was conducted in a single province, there is a need for more extensive national-level studies in the future to provide broader insights. This study highlights the significance of various factors in achieving success in implementing EHRs in Mazandaran University hospitals. Therefore, increased support in managing personnel workload, maintaining infrastructure, and organizing essential training workshops for medical staff and personnel in this field could potentially lead to greater success.
Conclusion
The success of HER implementation depends on a thorough understanding of its various aspects, including strengths, weaknesses, threats, and opportunities.
Acknowledgments: The authors thank all the study participants.
Ethical Permissions: The researchers followed the Declaration of Helsinki guidelines and obtained approval from the Ethics Committee of Mazandaran University of Medical Sciences (reference: IR.MAZUMS.REC.1401.466). Participants were provided with detailed information about the study’s objectives, potential risks and benefits, and their right to refuse participation. They were assured of voluntary participation and the freedom to withdraw at any point. Each participant signed an informed consent form indicating their agreement to participate. Ethical considerations focused on protecting the privacy and confidentiality of participant information, ensuring that data would be used for research purposes only, and maintaining participant anonymity in the questionnaire.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Mohsenipouya H (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Hashemi AH (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Hosseinnataj A (Third Author), Statistical Analyst (10%); Roy N (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Mamun MA (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: The study did not receive any funding.
Article Type: Descriptive & Survey |
Subject:
Health Communication
Received: 2024/06/5 | Accepted: 2024/08/20 | Published: 2024/09/5
Received: 2024/06/5 | Accepted: 2024/08/20 | Published: 2024/09/5
References
1. WHO. eHealth [Internet]. Geneva: The World Health Organization; 2024 [cited 2024, 3, 15]. Available from: https://www.emro.who.int/health-topics/ehealth/. [Link]
2. Singh HP, Kumari R. Digital technologies in healthcare management: A study of influence of national culture for adoption of electronic health records in India and Australia. Arch Bus Res. 2023;11(8):206-17. [Link] [DOI:10.14738/abr.118.15354]
3. Ahmad GI, Singla J, Giri KJ. Security and privacy of e-health data. In: Multimedia security. Singapore: Springer; 2021. p. 199-214. [Link] [DOI:10.1007/978-981-15-8711-5_10]
4. Ayala Solares JR, Diletta Raimondi FE, Zhu Y, Rahimian F, Canoy D, Tran J, et al. Deep learning for electronic health records: A comparative review of multiple deep neural architectures. J Biomed Inform. 2020;101:103337. [Link] [DOI:10.1016/j.jbi.2019.103337]
5. Tertulino R, Antunes N, Morais H. Privacy in electronic health records: A systematic mapping study. J Public Health. 2024;32(3):435-54. [Link] [DOI:10.1007/s10389-022-01795-z]
6. Shahmoradi L, Darrudi A, Shamsi F, Norouzinejad-Dastenayi A, Nasrolahbeigi F. Strategy formulation of electronic health record implementation using SWOT analysis. Health Inf Manag. 2017;14(1):9-15. [Persian] [Link]
7. Gatiti P, Ndirangu E, Mwangi J, Mwanzu A, Ramadhani T. Enhancing healthcare quality in hospitals through electronic health records: A systematic review. J Health Inform Dev Ctries. 2021;15(2). [Link]
8. Ayaad O, Alloubani A, ALhajaa EA, Farhan M, Abuseif S, Al Hroub A, et al. The role of electronic medical records in improving the quality of health care services: Comparative study. Int J Med Inform. 2019;127:63-7. [Link] [DOI:10.1016/j.ijmedinf.2019.04.014]
9. Campanella P, Lovato E, Marone C, Fallacara L, Mancuso A, Ricciardi W, et al. The impact of electronic health records on healthcare quality: A systematic review and meta-analysis. Eur J Public Health. 2016;26(1):60-4. [Link] [DOI:10.1093/eurpub/ckv122]
10. Wali R, Alqahtani R, Alharazi S, Bukhari S, Quqandi S. Patient satisfaction with the implementation of electronic medical records in the western region, Saudi Arabia, 2018. BMC Fam Pract. 2020;21(1):37. [Link] [DOI:10.1186/s12875-020-1099-0]
11. Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inform Health Soc Care. 2021;46(2):192-204. [Link] [DOI:10.1080/17538157.2021.1879810]
12. Ehrenstein V, Kharrazi H, Lehmann H, Taylor CO. Obtaining data from electronic health records. In: Tools and technologies for registry interoperability, registries for evaluating patient outcomes: A user's guide, 3rd edition, Addendum 2. Rockville: Agency for Healthcare Research and Quality; 2019. [Link]
13. Keshta I, Odeh A. Security and privacy of electronic health records: Concerns and challenges. Egypt Inform J. 2021;22(2):177-83. [Link] [DOI:10.1016/j.eij.2020.07.003]
14. Uslu A, Stausberg J. Value of the electronic medical record for hospital care: Update from the literature. J Med Internet Res. 2021;23(12):e26323. [Link] [DOI:10.2196/26323]
15. Boyle DK, Baernholdt M, Adams JM, McBride S, Harper E, Poghosyan L, et al. Improve nurses' well-being and joy in work: Implement true interprofessional teams and address electronic health record usability issues. Nurs Outlook. 2019;67(6):791-7. [Link] [DOI:10.1016/j.outlook.2019.10.002]
16. Bani Issa W, Al Akour I, Ibrahim A, Almarzouqi A, Abbas S, Hisham F, et al. Privacy, confidentiality, security and patient safety concerns about electronic health records. Int Nurs Rev. 2020;67(2):218-30. [Link] [DOI:10.1111/inr.12585]
17. Tayefi M, Ngo P, Chomutare T, Dalianis H, Salvi E, Budrionis A, et al. Challenges and opportunities beyond structured data in analysis of electronic health records. WIREs Comput Stat. 2021;13(6):e1549. [Link] [DOI:10.1002/wics.1549]
18. Els F, Cilliers L. A privacy management framework for personal electronic health records. Afr J Sci Technol Innov Dev. 2018;10(6):725-34. [Link] [DOI:10.1080/20421338.2018.1509489]
19. Al-Aswad AM, Brownsell S, Palmer R, Nichol JP. A review paper of the current status of electronic health records adoption worldwide: The gap between developed and developing countries. J Health Inform Dev Ctries. 2013;7(2). [Link]
20. Abbasi R, Khajouei R, Mirzaee M. Evaluating the demographic and clinical minimum data sets of Iranian National Electronic Health Record. BMC Health Serv Res. 2019;19(1):450. [Link] [DOI:10.1186/s12913-019-4284-x]
21. Sheikhtaheri A, Tabatabaee Jabali SM, Bitaraf E, TehraniYazdi A, Kabir A. A near real-time electronic health record-based COVID-19 surveillance system: An experience from a developing country. Health Inf Manag. 2024;53(2):145-54. [Link] [DOI:10.1177/18333583221104213]
22. Khajouei R, Abbasi R, Mirzaee M. Errors and causes of communication failures from hospital information systems to electronic health record: A record-review study. Int J Med Inform. 2018;119:47-53. [Link] [DOI:10.1016/j.ijmedinf.2018.09.004]
23. Asadi F, Moghaddasi H, Rabiei R, Rahimi F, Mirshekarlou SJ. The evaluation of SEPAS national project based on electronic health record system (EHRS) coordinates in Iran. Acta Inform Med. 2015;23(6):369-73. [Link] [DOI:10.5455/aim.2015.23.369-373]
24. Benzaghta MA, Elwalda A, Mousa MM, Erkan I, Rahman M. SWOT analysis applications: An integrative literature review. J Glob Bus Insights. 2021;6(1):55-73. [Link] [DOI:10.5038/2640-6489.6.1.1148]
25. Shahmoradi L, Darrudi A, Arji G, Nejad AF. Electronic health record implementation: A SWOT analysis. Acta Med Iran. 2017;55(10):642-9. [Link]
26. Mirani N, Ayatollahi H, Haghani H. A survey on barriers to the development and adoption of electronic health records in Iran. J Health Adm. 2013;15(50):65-75. [Persian] [Link]
27. Abbasi H, Rahimi B, Jebraeily M, Nourani A. End-users' perspectives on factors affecting implementation and utilization of the Iranian electronic health record system: A qualitative study in a developing country. BMC Health Serv Res. 2023;23(1):1064. [Link] [DOI:10.1186/s12913-023-10033-5]
28. Tajirian T, Stergiopoulos V, Strudwick G, Sequeira L, Sanches M, Kemp J, et al. The influence of electronic health record use on physician burnout: Cross-sectional survey. J Med Internet Res. 2020;22(7):e19274. [Link] [DOI:10.2196/19274]
29. Sieck CJ, Pearl N, Bright TJ, Yen PY. A qualitative study of physician perspectives on adaptation to electronic health records. BMC Med Inform Decis Mak. 2020;20:25. [Link] [DOI:10.1186/s12911-020-1030-6]
30. Lee WW, Alkureishi ML, Isaacson JH, Mayer M, Frankel RM, London DA, et al. Impact of a brief faculty training to improve patient-centered communication while using electronic health records. Patient Educ Couns. 2018;101(12):2156-61. [Link] [DOI:10.1016/j.pec.2018.06.020]
31. Hazra NC, Rudisill C, Gulliford MC. Developing the role of electronic health records in economic evaluation. Eur J Health Econ. 2019;20(8):1117-21. [Link] [DOI:10.1007/s10198-019-01042-5]
32. Griesser A, Mzoughi M, Bidmon S, Cherif E. How do opt-in versus opt-out settings nudge patients toward electronic health record adoption? An exploratory study of facilitators and barriers in Austria and France. BMC Health Serv Res. 2024;24(1):439. [Link] [DOI:10.1186/s12913-024-10929-w]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |