Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 365-373 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nouri Khaneghah Z, Sohrabi Z, Bigdeli S, Khoddam H, Kamali M. Knowledge Sharing in the Healthcare System; A Systematized Review. Health Educ Health Promot 2024; 12 (2) :365-373
URL: http://hehp.modares.ac.ir/article-5-75469-en.html
URL: http://hehp.modares.ac.ir/article-5-75469-en.html
1- “Center for Educational Research in Medical Sciences (CERMS)” and “Department of Medical Education, School of Medicine”, Iran University of Medical Sciences, Tehran, Iran
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Center for Educational Research in Medical Sciences (CERMS), Iran University of Medical Sciences, Tehran, Iran
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Center for Educational Research in Medical Sciences (CERMS), Iran University of Medical Sciences, Tehran, Iran
Keywords: Healthcare System [MeSH], Knowledge [MeSH], Knowledge Management [MeSH], Review article [MeSH]
Full-Text [PDF 663 kb]
(2869 Downloads)
| Abstract (HTML) (891 Views)
Full-Text: (137 Views)
Introduction
Knowledge is an organization's most important asset, empowering individuals to create and expand a productive work environment [1]. Knowledge management activities include acquiring, encoding, storing, transferring, applying, and sharing knowledge. Knowledge sharing is considered a key process in knowledge management [2].
Knowledge sharing, tacit and explicit, holds particular importance in the healthcare system, especially in hospitals, compared to other industries. In such environments, knowledge sharing among healthcare staff improves the quality of patient services, impacting their lives and health [3, 4]. Many studies have highlighted the significance and benefits of knowledge sharing among healthcare professionals. These benefits include having an informed medical team capable of accurate diagnosis and treatment [5], reducing medical errors, increasing evidence-based medicine utilization, controlling healthcare costs, improving employee performance [6-8], enhancing the quality of services, fostering inter-professional collaboration, and promoting innovation and learning. Therefore, knowledge sharing in the healthcare system is crucial [9].
Nevertheless, researchers define knowledge sharing in various ways, particularly in the healthcare system, with definitions differing in specific or broader contexts [10]. For instance, Rehman et al. consider knowledge sharing an essential process for knowledge management. It defines it as a culture and social interaction through which knowledge, including information, skills, and specialized insight, is exchanged among individuals, communities, and organizations [11]. Olan et al. describe knowledge sharing as transferring organizational experience and knowledge in business processes through communication channels among individuals [12]. Doronin et al. defines knowledge sharing as the dissemination and transfer of explicit and tacit knowledge at the individual level to enhance the recipients' knowledge, whether individuals, groups, organizations, or communities. Their study results indicate that knowledge sharing has a dual nature, with knowledge as input and knowledge sharing as a process [13].
While reviewing articles on knowledge sharing in the healthcare system, it was observed that the focus on clarifying knowledge sharing in the healthcare system needed to be more prominent. Instead, more attention was given to the importance of knowledge sharing in this context. For example, Omotayo & Orimolade, in their research on knowledge sharing among Nigerian physicians, defined it as "individuals' willingness and readiness to share their knowledge with others" without elaborating on details such as the types of knowledge shared or the methods used. This definition indicates a need for more clarity on this concept in their article [1]. Similarly, in his study on knowledge sharing among healthcare providers, Morrow noted that knowledge sharing among healthcare workers is highly abstract [14]. Based on these varied definitions, it is evident that knowledge sharing in the healthcare system needs more clarity. Since individuals from different healthcare fields come together for various purposes, such as providing patient care or planning research, the terminology used by all participants must be clearly understood. Although they may use similar terms to refer to healthcare concepts, communication inconsistencies can arise, leading to misunderstandings and differing interpretations. Therefore, clear communication is essential for collaborative efforts, ensuring members comprehend what others are articulating [15].
As far as we know, studies have yet to clarify knowledge sharing within the healthcare system. Given the importance of knowledge sharing in healthcare, our study aims to clarify this concept by examining the nature of shared knowledge, how knowledge is shared, the individual and organizational components involved in the process, and the resulting outcomes. These findings can provide significant evidence for health managers, policymakers, professionals, and hospital and university heads, guiding them in planning and, if necessary, implementing interventions to improve the knowledge-sharing process within the healthcare system. This could enhance the efficiency of healthcare staff and offer valuable insights into knowledge sharing in the healthcare system. The information gathered could also serve as a foundation for future education and research. However, achieving a common understanding of knowledge sharing in healthcare is a prerequisite for these actions. Thus, this research was conducted to clarify knowledge sharing in the healthcare system.
Information and Methods
In this systematized review, appropriate keywords were selected based on the MeSH (Medical Subject Headings) and relevant articles on knowledge sharing in the healthcare system, in collaboration with the research team and an expert librarian ("Medical system", "Health system", "Clinical system", "Biomedical system", "Health care system", "Healthcare system", "Knowledge management", "Knowledge sharing", "Knowledge brokering", "Knowledge transmission", "Knowledge dissemination", "Knowledge exchange", "Knowledge transfer", and "Knowledge distribution"). A search strategy was developed with team members and an expert librarian ("Medical system*", "Health system*", "Clinical system*", "Biomedical system*", "Health care system*", "Healthcare system*", "Knowledge management", "Knowledge sharing", "Knowledge brokering", "Knowledge transmission", "Knowledge dissemination", "Knowledge exchange", "Knowledge transfer", and "Knowledge distribution").
The search strategy was tested in the PubMed database and reevaluated or confirmed for use in other databases. Based on the research objectives and questions, databases such as MEDLINE (via PubMed), WOS, Scopus, Embase, ERIC, and ProQuest were selected to identify relevant evidence. The search strategy was developed with consultation from team members and a specialized librarian. The six mentioned databases were searched without time restrictions up to 2023. Search results from all databases were imported into the EndNote reference management software, where duplicates were removed (Figure 1).
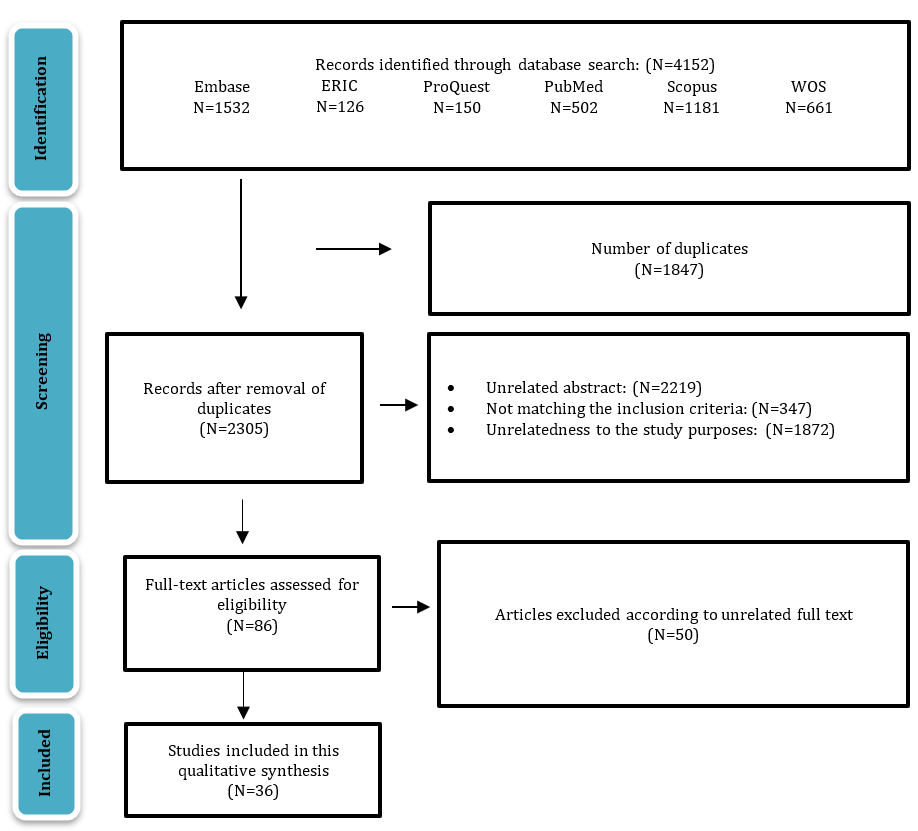
Figure 1. Flow diagram showing the entire search process
English quantitative and qualitative original and review articles, master's theses, and doctoral dissertations related to knowledge sharing in the healthcare system were included in the study without any time constraints. Letters to the editor, book chapters, editors’ notes, corrections, meeting abstracts, and conference proceedings were not included. The selected articles were screened in the reference management software.
Qualitative content analysis is a versatile method of analyzing various textual data sources, including verbal, visual, printed, and electronic sources. In their article titled "Three Approaches to Qualitative Content Analysis," Hsiu-Fang and Shannon differentiated between three main approaches: conventional, directional, and summative content analysis. This study utilized the conventional content analysis method [16]. The analysis was conducted to code the articles’ texts using the Graneheim and Lundman qualitative content analysis model (2004). The process began with a thorough review of each article's entire text, which was repeated several times to grasp the overall content. After this review, meaning units were identified, and corresponding codes were assigned. Once each article was coded, similar initial codes were merged into subcategories These subcategories were then grouped to form main categories. This process was repeated for 36 articles by two researchers, resulting in the final subcategories and categories [17].
The four criteria of Guba & Lincoln [18] were utilized to assess rigor. For credibility, the codes extracted from the articles were reviewed by a third researcher. To ensure transferability, complete explanations regarding the work process and code extraction were provided in the respective article. All information about retrieving articles, decision-making processes, and analyses was accurately recorded and maintained. Code extraction was performed by the second researcher, following the initial coding by the first researcher. The third researcher scrutinized and monitored all stages of the systematized review process, ensuring dependability and confirmability [18, 19].
Findings
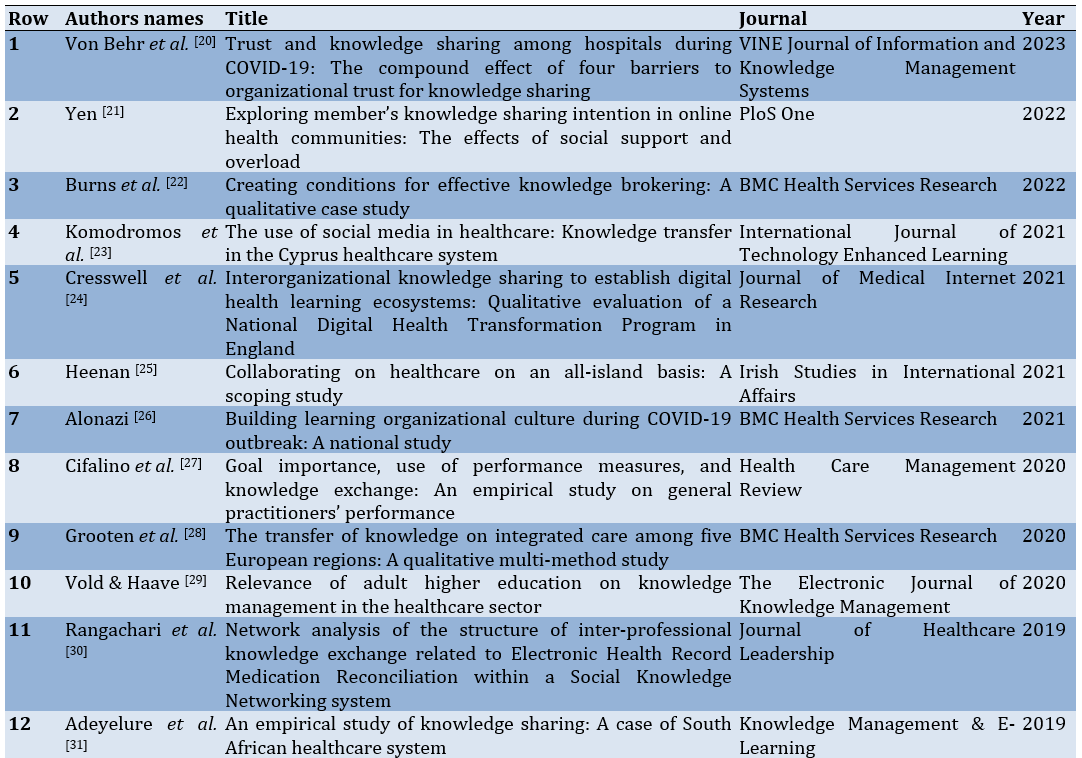
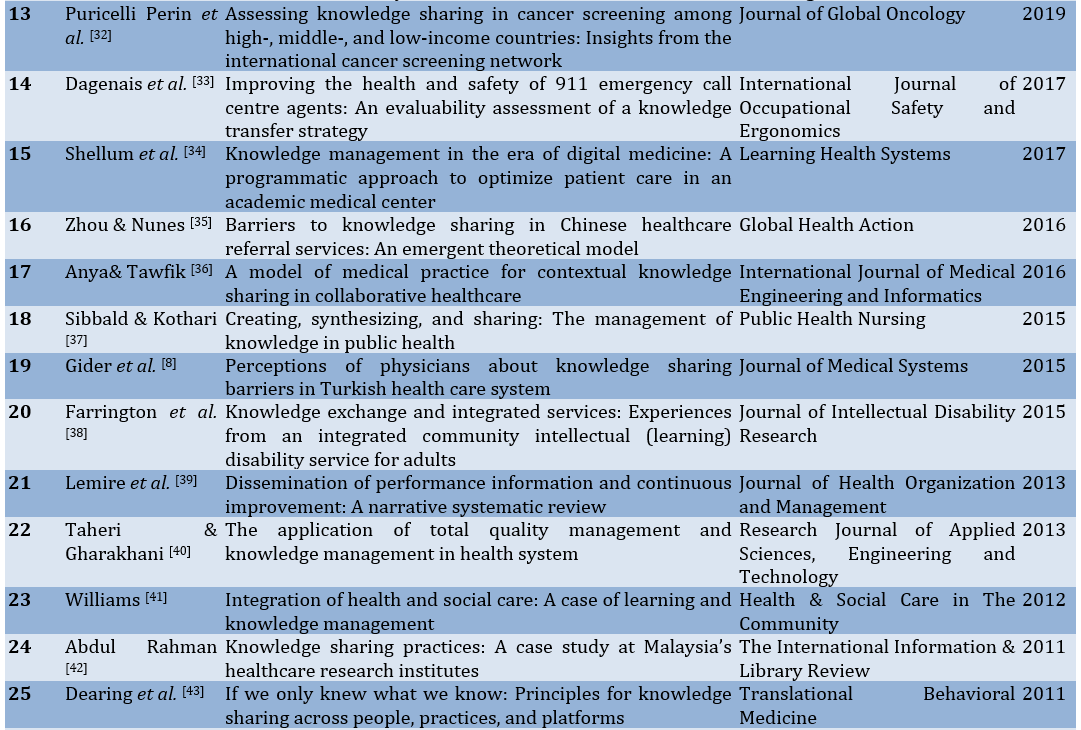
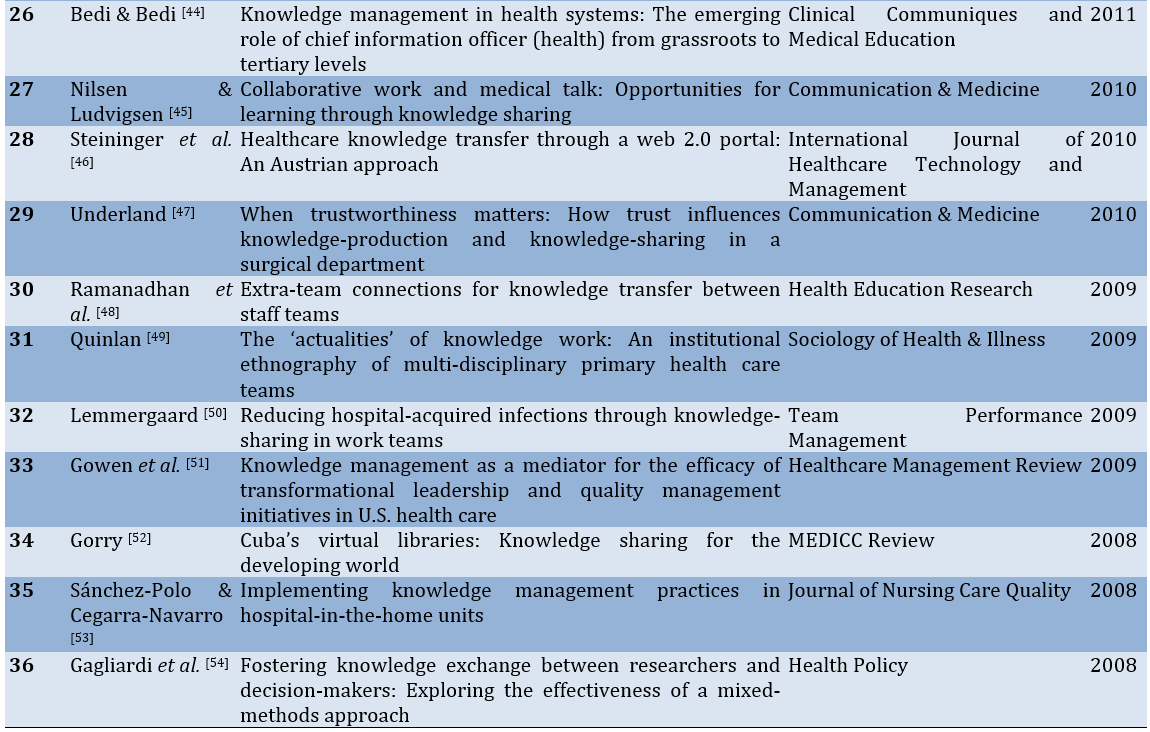
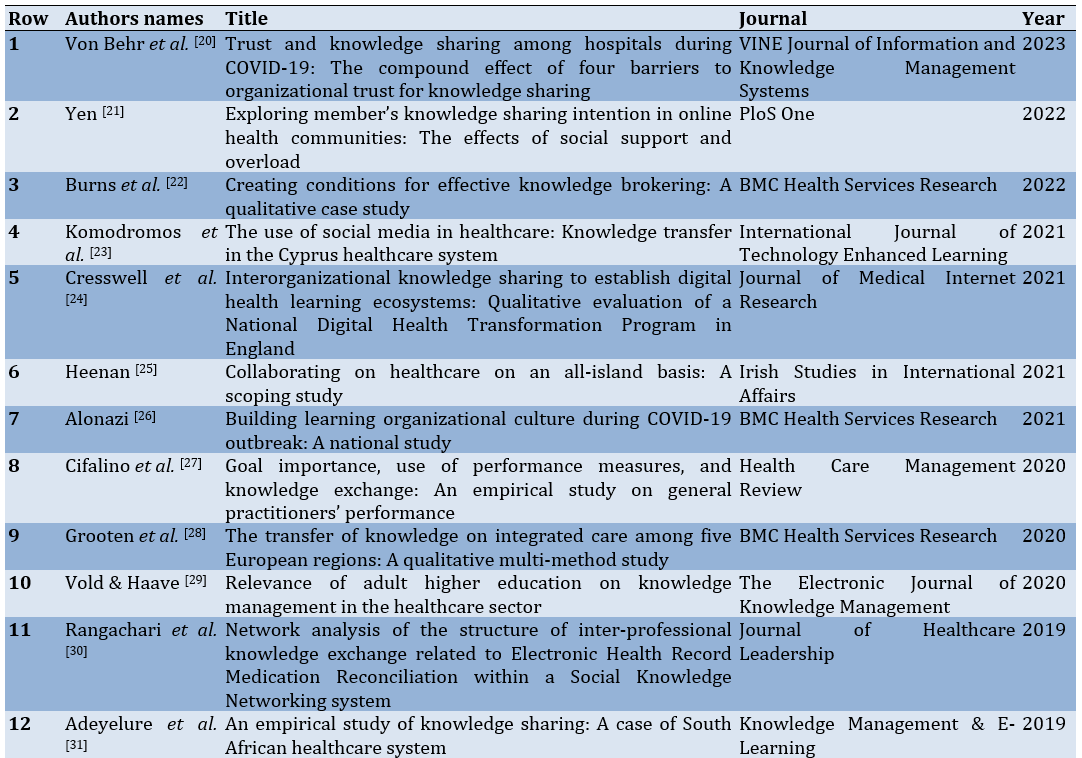
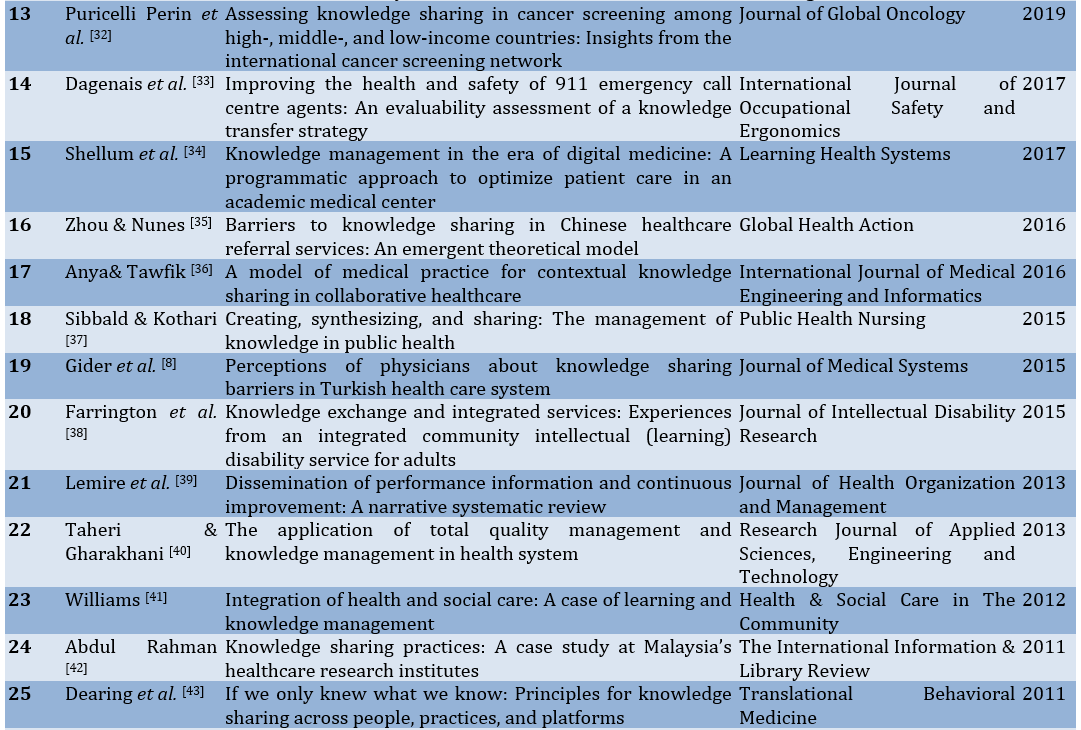
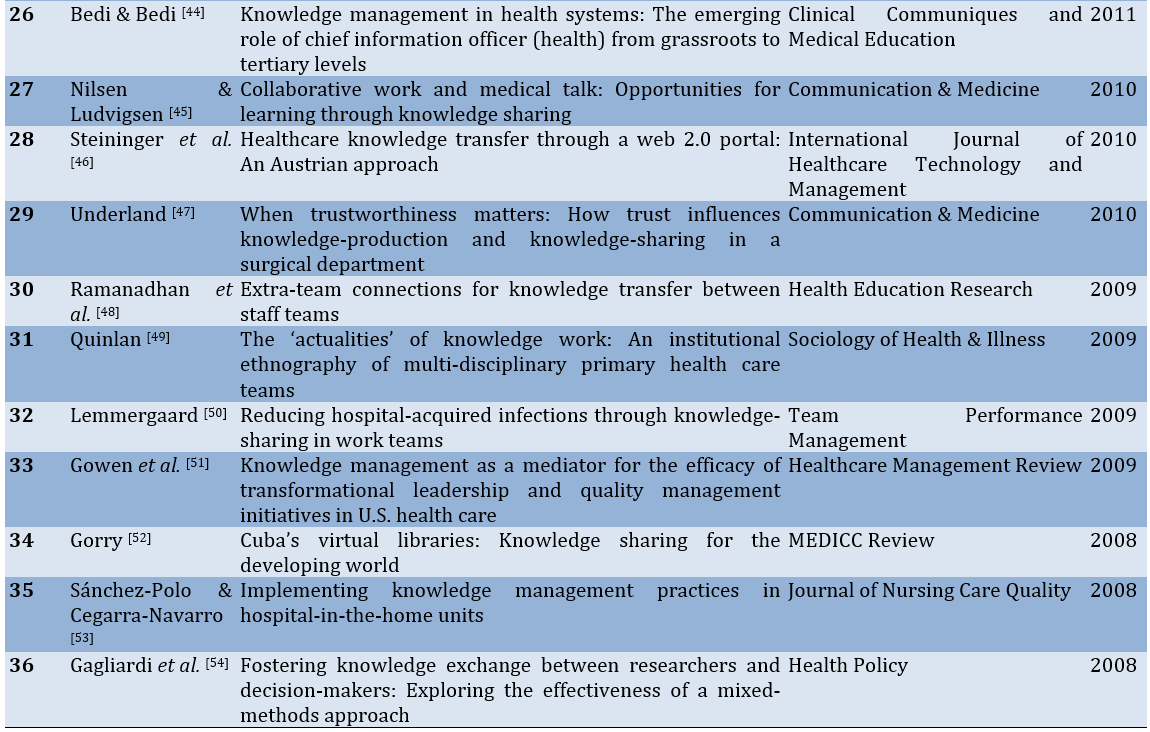
Based on the systematized review, 4,152 articles were retrieved. After removing duplicates and screening at three levels, including title, abstract, and full text, 36 articles were selected for qualitative content analysis (Table 1).
Table 1. Bibliographic information of retrieved articles on the concept of knowledge sharing in the health system
After merging and classifying the codes resulting from the article analysis, five main categories were identified:
1- Nature of shared knowledge
Article analysis revealed that in the healthcare system, knowledge encompasses not only clinical findings [8] but also specialized and theoretical knowledge of physicians, knowledge about factors influencing clinical work [31], practical tips and “how-know” [43], documents in electronic and paper medical records of patients [31, 35, 47], knowledge gained from consultations [8], acquired knowledge from individuals outside the organization, and knowledge about the hospital's organizational structure [8, 26]. In addition, it includes individual experiences [8, 20, 23, 24, 31, 32, 35, 37, 42], opinions [27, 31, 46], and suggestions, ideas, and innovations [23, 31, 42, 43], which are shared both tacitly and explicitly [8, 24, 31, 35, 37, 40, 42].
2- Ways of knowledge sharing
Knowledge sharing based on the web
Knowledge sharing based on the web has expanded beyond traditional face-to-face interactions to include technological factors. It now occurs through various means such as email [37], online clinical training courses [23], telemedicine [8, 45], online forums [21, 23, 43], and social media platforms among patients, healthcare professionals, and others in the healthcare system [23, 31, 37, 41].
Formal and informal knowledge sharing
Whether implicit or explicit, knowledge is shared through formal and informal channels, utilizing human communication bridges and non-human channels [31, 34, 35, 37, 38]. Tacit knowledge is shared through apprenticeship, imitation, observation, socialization, storytelling, analogy, consultation, negotiation, and teaching [8, 42, 49]. Explicit knowledge is shared through documents, personal portals in hospitals, discussions, group sessions, and educational services, including face-to-face classes, rounds, clinical sessions, workshops, symposiums, conferences, and webinars [8, 24, 27, 37, 42, 45, 47].
3-Factors involved in organizational and inter-organizational knowledge-sharing events
Organizational components
Organizational factors significantly influence knowledge sharing within and between healthcare organizations. These factors include efforts for survival and competition [31], the increasing need to formalize the knowledge-sharing process [24, 37], patient referral processes among hospitals, and financial alignment between healthcare organizations [35, 45].
Provision of technology-information system and infrastructure
With technological advancements, knowledge sharing is no longer limited to in-person interactions within an organization; Individuals can now share knowledge virtually across different organizations within the healthcare system. A crucial aspect of this shift is providing the necessary infrastructure and establishing robust information technology and communication systems. In addition to ensuring access to technology that enables unrestricted knowledge sharing regardless of location and time [8, 25, 31, 37, 45, 52], enhancing the technological literacy of healthcare staff is also essential [42].
4- Barriers to knowledge sharing
Individual barriers
One barrier to knowledge sharing among healthcare professionals is the fear of losing power through knowledge sharing, along with a lack of training in knowledge sharing [42], high workload in the healthcare team [35], and individuals' perspective on the lack of priority for knowledge sharing [37].
Organizational and political obstacles
In organizational knowledge sharing within healthcare institutions, challenges such as lack of trust in experiments and evidence presented by other hospitals [35], distrust in hospital management [42], lack of leadership for knowledge sharing [35], differences in organizational needs [24], and absence of managerial policies at national and local levels hinder inter-organizational knowledge sharing [35].
5- Consequences of knowledge sharing
Increasing organizational responsibility
Based on the article's analysis results, knowledge sharing positively affects the healthcare system. One such implication is the increased accountability in providing medical services to patients, treatment policy-making, planning, and enhancing the responsiveness of healthcare organizations to medical outcomes. Therefore, knowledge sharing in hospitals and among healthcare staff is crucial [31, 40].
Improving the quality of services and treatment outcomes
Knowledge sharing has numerous positive therapeutic outcomes, such as reducing medical errors, preventing misdiagnosis, lowering patient mortality rates [8, 31], and avoiding repeating medical mistakes [24, 32]. As a result, patients will receive higher-quality healthcare services at all levels of care, ultimately leading to the establishment of a quality healthcare system [8, 24, 31, 35, 45, 47, 52, 53].
Increasing the use of research and evidence
Knowledge sharing leads to evidence-based medical decision-making, provides research-oriented and innovative care, and advances therapeutic research strategies [8, 32].
Discussion
Knowledge shared among individuals or groups can be either explicit or tacit. Explicit knowledge can be codified, documented, and easily disseminated among individuals, groups, and organizations. It includes various forms such as documents, textbooks, and scientific articles [55]. In contrast, tacit knowledge refers to skills, ideas, and experiences that reside in the minds of individuals, making access to them challenging. People often do not recognize their tacit knowledge or how to leverage it to assist others [56]. In the study by Gider et al., various types of knowledge were referenced, including consulting knowledge, clinical findings about cases, work experiences, new medical knowledge, and knowledge about technology, as well as knowledge related to the work environment or organizational structure that physicians share with their colleagues or other healthcare professionals [8]. Abdul Rahman also examined methods of knowledge sharing, indicating that knowledge about 'know-how' and skills is shared tacitly [42]. Therefore, in the healthcare system across different hospital departments, tacit and explicit knowledge is shared, and these two types continually interact. Adeyelure et al. noted that interactions between tacit and explicit knowledge occur within meetings held among healthcare staff [31].
Knowledge can be shared formally or informally. Raven & El Sawy classified formal and informal knowledge-sharing methods, noting that each method can involve two or more participants. Formal sharing is typically planned, while informal sharing is spontaneous [57]. In the healthcare system, knowledge sharing occurs through various formal methods, such as workshops, symposiums, conferences, and webinars. Informally, it takes place through observation, imitation, and apprenticeship. With advancements in technology and communication, knowledge is increasingly shared online in addition to in-person interactions.
In addition to knowledge sharing within organizations, inter-organizational knowledge sharing occurs through referring patients to specialists from different hospitals [35]. Various factors contribute to knowledge sharing among organizations, such as the need for an organization to survive [1]—however, more than this factor is required. Effective inter-organizational knowledge sharing also necessitates infrastructure provision, especially when knowledge is shared virtually [42].
To facilitate the easy sharing of knowledge, individual, organizational, and political barriers must be addressed or managed as much as possible. Given the hierarchical nature of hospitals [10], it is not surprising that healthcare personnel may fear losing their positions of power, which can hinder knowledge sharing [42]. Some barriers, such as the overload of healthcare staff [35], can be mitigated with appropriate management. Since the primary focus of providing care to patients is to ensure their safety and well-being, healthcare workers sometimes do not prioritize knowledge sharing. Zhou & Nunes [35] noted that physicians are often overwhelmed with work and tend to focus more on addressing immediate patient needs, which may lower knowledge sharing on their priorities [35].
One of the significant barriers to knowledge sharing is the need for more trust at both the individual and organizational levels. As Zhou & Nunes noted in their study, a recurring theme in the interviewees' statements was the issue of distrust between parties during the referral process. This distrust pertained to healthcare professionals in primary care settings during referrals and to the tacit knowledge shared by peer specialists and patient medical records involved in the referral process [35]. Abdul Rahman also stated in his study that 45.5% of respondents identified peer distrust, and 43.3% identified distrust in management as an obstacle to knowledge sharing [42]. Underland [47] further indicated that when new information is shared in clinical meetings, surgeons must regard it as reliable; Otherwise, the clinical meeting serves no purpose as a venue for knowledge sharing and decision-making. Appropriate knowledge-sharing policies are needed to effectively manage these individual and organizational barriers, as the absence of such policies constitutes a barrier to knowledge-sharing [35].
Since knowledge is considered an important organizational asset and should not be confined, its sharing has positive implications when facilitated. Tetroe et al. asserted that knowledge sharing is vital for the healthcare sector, as it can enhance accountability and evidence-based performance in health planning, policy-making, and service delivery [58]. Jabr identified the benefits of knowledge sharing in his study as follows: 1) reduction of medical errors, 2) improvement in the quality of healthcare, 3) enhancement of patient health and safety, 4) support for the promotion of evidence-based medical practices, 5) encouragement of patient-centered technologies, and 6) provision of better health outcomes through improved training and education for health professionals [7].
One limitation of this study was the need for more access to the full text of certain articles and theses. Establishing clear policies is essential to facilitate effective knowledge sharing among individuals and organizations.
Conclusion
Tacit and explicit forms of knowledge (such as experiences and patient records) are shared among healthcare staff within the health system through formal, informal, in-person, and virtual means. Knowledge is shared at the individual level and within and between organizations. Both organizational and individual factors play a role in this process. Consequently, knowledge sharing in the health system has positive implications for its stakeholders, including organizations, patients, and healthcare staff.
Acknowledgments: The authors express their gratitude to Dr. Neda Mehrdad for her support in conducting this research, and The authors acknowledge the substantial contributions of all who shared their knowledge through published papers.
Ethical Permissions: This research was approved by the Ethics Committee of Iran University of Medical Sciences with the ethics code IR.IUMS.FMD.REC.1401.358.
Conflicts of Interests: The authors of this research have no conflicts of interest. This research, approved by Iran University of Medical Sciences, is being published with the consent and collaboration of all authors.
Authors' Contribution: Nouri Khaneghah Z (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Sohrabi Z (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Bigdeli S (Third Author), Introduction Writer/Methodologist/Original Researcher/Discussion Writer/Statistical Analyst (15%); Khoddam H (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (15%); Kamali M (Fifth Author), Methodologist/Main Researcher/Statistical Analyst (10%)
Funding/Support: The Vice-Chancellor for Research of Iran University of Medical Sciences granted and supported this research.
Knowledge is an organization's most important asset, empowering individuals to create and expand a productive work environment [1]. Knowledge management activities include acquiring, encoding, storing, transferring, applying, and sharing knowledge. Knowledge sharing is considered a key process in knowledge management [2].
Knowledge sharing, tacit and explicit, holds particular importance in the healthcare system, especially in hospitals, compared to other industries. In such environments, knowledge sharing among healthcare staff improves the quality of patient services, impacting their lives and health [3, 4]. Many studies have highlighted the significance and benefits of knowledge sharing among healthcare professionals. These benefits include having an informed medical team capable of accurate diagnosis and treatment [5], reducing medical errors, increasing evidence-based medicine utilization, controlling healthcare costs, improving employee performance [6-8], enhancing the quality of services, fostering inter-professional collaboration, and promoting innovation and learning. Therefore, knowledge sharing in the healthcare system is crucial [9].
Nevertheless, researchers define knowledge sharing in various ways, particularly in the healthcare system, with definitions differing in specific or broader contexts [10]. For instance, Rehman et al. consider knowledge sharing an essential process for knowledge management. It defines it as a culture and social interaction through which knowledge, including information, skills, and specialized insight, is exchanged among individuals, communities, and organizations [11]. Olan et al. describe knowledge sharing as transferring organizational experience and knowledge in business processes through communication channels among individuals [12]. Doronin et al. defines knowledge sharing as the dissemination and transfer of explicit and tacit knowledge at the individual level to enhance the recipients' knowledge, whether individuals, groups, organizations, or communities. Their study results indicate that knowledge sharing has a dual nature, with knowledge as input and knowledge sharing as a process [13].
While reviewing articles on knowledge sharing in the healthcare system, it was observed that the focus on clarifying knowledge sharing in the healthcare system needed to be more prominent. Instead, more attention was given to the importance of knowledge sharing in this context. For example, Omotayo & Orimolade, in their research on knowledge sharing among Nigerian physicians, defined it as "individuals' willingness and readiness to share their knowledge with others" without elaborating on details such as the types of knowledge shared or the methods used. This definition indicates a need for more clarity on this concept in their article [1]. Similarly, in his study on knowledge sharing among healthcare providers, Morrow noted that knowledge sharing among healthcare workers is highly abstract [14]. Based on these varied definitions, it is evident that knowledge sharing in the healthcare system needs more clarity. Since individuals from different healthcare fields come together for various purposes, such as providing patient care or planning research, the terminology used by all participants must be clearly understood. Although they may use similar terms to refer to healthcare concepts, communication inconsistencies can arise, leading to misunderstandings and differing interpretations. Therefore, clear communication is essential for collaborative efforts, ensuring members comprehend what others are articulating [15].
As far as we know, studies have yet to clarify knowledge sharing within the healthcare system. Given the importance of knowledge sharing in healthcare, our study aims to clarify this concept by examining the nature of shared knowledge, how knowledge is shared, the individual and organizational components involved in the process, and the resulting outcomes. These findings can provide significant evidence for health managers, policymakers, professionals, and hospital and university heads, guiding them in planning and, if necessary, implementing interventions to improve the knowledge-sharing process within the healthcare system. This could enhance the efficiency of healthcare staff and offer valuable insights into knowledge sharing in the healthcare system. The information gathered could also serve as a foundation for future education and research. However, achieving a common understanding of knowledge sharing in healthcare is a prerequisite for these actions. Thus, this research was conducted to clarify knowledge sharing in the healthcare system.
Information and Methods
In this systematized review, appropriate keywords were selected based on the MeSH (Medical Subject Headings) and relevant articles on knowledge sharing in the healthcare system, in collaboration with the research team and an expert librarian ("Medical system", "Health system", "Clinical system", "Biomedical system", "Health care system", "Healthcare system", "Knowledge management", "Knowledge sharing", "Knowledge brokering", "Knowledge transmission", "Knowledge dissemination", "Knowledge exchange", "Knowledge transfer", and "Knowledge distribution"). A search strategy was developed with team members and an expert librarian ("Medical system*", "Health system*", "Clinical system*", "Biomedical system*", "Health care system*", "Healthcare system*", "Knowledge management", "Knowledge sharing", "Knowledge brokering", "Knowledge transmission", "Knowledge dissemination", "Knowledge exchange", "Knowledge transfer", and "Knowledge distribution").
The search strategy was tested in the PubMed database and reevaluated or confirmed for use in other databases. Based on the research objectives and questions, databases such as MEDLINE (via PubMed), WOS, Scopus, Embase, ERIC, and ProQuest were selected to identify relevant evidence. The search strategy was developed with consultation from team members and a specialized librarian. The six mentioned databases were searched without time restrictions up to 2023. Search results from all databases were imported into the EndNote reference management software, where duplicates were removed (Figure 1).
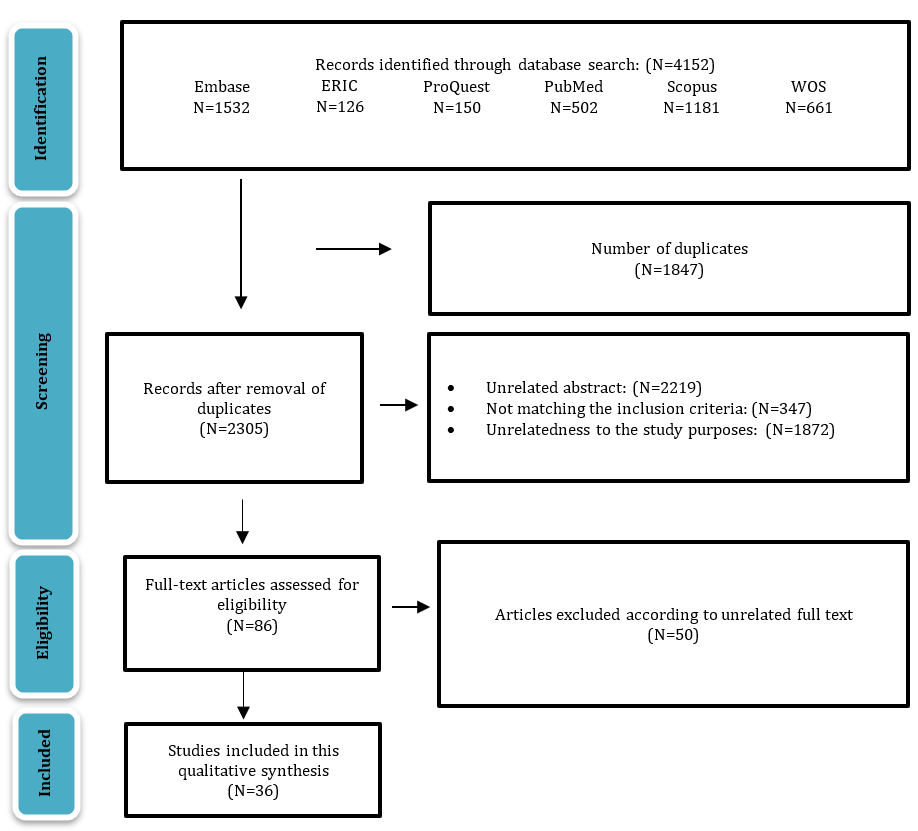
Figure 1. Flow diagram showing the entire search process
English quantitative and qualitative original and review articles, master's theses, and doctoral dissertations related to knowledge sharing in the healthcare system were included in the study without any time constraints. Letters to the editor, book chapters, editors’ notes, corrections, meeting abstracts, and conference proceedings were not included. The selected articles were screened in the reference management software.
Qualitative content analysis is a versatile method of analyzing various textual data sources, including verbal, visual, printed, and electronic sources. In their article titled "Three Approaches to Qualitative Content Analysis," Hsiu-Fang and Shannon differentiated between three main approaches: conventional, directional, and summative content analysis. This study utilized the conventional content analysis method [16]. The analysis was conducted to code the articles’ texts using the Graneheim and Lundman qualitative content analysis model (2004). The process began with a thorough review of each article's entire text, which was repeated several times to grasp the overall content. After this review, meaning units were identified, and corresponding codes were assigned. Once each article was coded, similar initial codes were merged into subcategories These subcategories were then grouped to form main categories. This process was repeated for 36 articles by two researchers, resulting in the final subcategories and categories [17].
The four criteria of Guba & Lincoln [18] were utilized to assess rigor. For credibility, the codes extracted from the articles were reviewed by a third researcher. To ensure transferability, complete explanations regarding the work process and code extraction were provided in the respective article. All information about retrieving articles, decision-making processes, and analyses was accurately recorded and maintained. Code extraction was performed by the second researcher, following the initial coding by the first researcher. The third researcher scrutinized and monitored all stages of the systematized review process, ensuring dependability and confirmability [18, 19].
Findings
Based on the systematized review, 4,152 articles were retrieved. After removing duplicates and screening at three levels, including title, abstract, and full text, 36 articles were selected for qualitative content analysis (Table 1).
Table 1. Bibliographic information of retrieved articles on the concept of knowledge sharing in the health system
After merging and classifying the codes resulting from the article analysis, five main categories were identified:
1- Nature of shared knowledge
Article analysis revealed that in the healthcare system, knowledge encompasses not only clinical findings [8] but also specialized and theoretical knowledge of physicians, knowledge about factors influencing clinical work [31], practical tips and “how-know” [43], documents in electronic and paper medical records of patients [31, 35, 47], knowledge gained from consultations [8], acquired knowledge from individuals outside the organization, and knowledge about the hospital's organizational structure [8, 26]. In addition, it includes individual experiences [8, 20, 23, 24, 31, 32, 35, 37, 42], opinions [27, 31, 46], and suggestions, ideas, and innovations [23, 31, 42, 43], which are shared both tacitly and explicitly [8, 24, 31, 35, 37, 40, 42].
2- Ways of knowledge sharing
Knowledge sharing based on the web
Knowledge sharing based on the web has expanded beyond traditional face-to-face interactions to include technological factors. It now occurs through various means such as email [37], online clinical training courses [23], telemedicine [8, 45], online forums [21, 23, 43], and social media platforms among patients, healthcare professionals, and others in the healthcare system [23, 31, 37, 41].
Formal and informal knowledge sharing
Whether implicit or explicit, knowledge is shared through formal and informal channels, utilizing human communication bridges and non-human channels [31, 34, 35, 37, 38]. Tacit knowledge is shared through apprenticeship, imitation, observation, socialization, storytelling, analogy, consultation, negotiation, and teaching [8, 42, 49]. Explicit knowledge is shared through documents, personal portals in hospitals, discussions, group sessions, and educational services, including face-to-face classes, rounds, clinical sessions, workshops, symposiums, conferences, and webinars [8, 24, 27, 37, 42, 45, 47].
3-Factors involved in organizational and inter-organizational knowledge-sharing events
Organizational components
Organizational factors significantly influence knowledge sharing within and between healthcare organizations. These factors include efforts for survival and competition [31], the increasing need to formalize the knowledge-sharing process [24, 37], patient referral processes among hospitals, and financial alignment between healthcare organizations [35, 45].
Provision of technology-information system and infrastructure
With technological advancements, knowledge sharing is no longer limited to in-person interactions within an organization; Individuals can now share knowledge virtually across different organizations within the healthcare system. A crucial aspect of this shift is providing the necessary infrastructure and establishing robust information technology and communication systems. In addition to ensuring access to technology that enables unrestricted knowledge sharing regardless of location and time [8, 25, 31, 37, 45, 52], enhancing the technological literacy of healthcare staff is also essential [42].
4- Barriers to knowledge sharing
Individual barriers
One barrier to knowledge sharing among healthcare professionals is the fear of losing power through knowledge sharing, along with a lack of training in knowledge sharing [42], high workload in the healthcare team [35], and individuals' perspective on the lack of priority for knowledge sharing [37].
Organizational and political obstacles
In organizational knowledge sharing within healthcare institutions, challenges such as lack of trust in experiments and evidence presented by other hospitals [35], distrust in hospital management [42], lack of leadership for knowledge sharing [35], differences in organizational needs [24], and absence of managerial policies at national and local levels hinder inter-organizational knowledge sharing [35].
5- Consequences of knowledge sharing
Increasing organizational responsibility
Based on the article's analysis results, knowledge sharing positively affects the healthcare system. One such implication is the increased accountability in providing medical services to patients, treatment policy-making, planning, and enhancing the responsiveness of healthcare organizations to medical outcomes. Therefore, knowledge sharing in hospitals and among healthcare staff is crucial [31, 40].
Improving the quality of services and treatment outcomes
Knowledge sharing has numerous positive therapeutic outcomes, such as reducing medical errors, preventing misdiagnosis, lowering patient mortality rates [8, 31], and avoiding repeating medical mistakes [24, 32]. As a result, patients will receive higher-quality healthcare services at all levels of care, ultimately leading to the establishment of a quality healthcare system [8, 24, 31, 35, 45, 47, 52, 53].
Increasing the use of research and evidence
Knowledge sharing leads to evidence-based medical decision-making, provides research-oriented and innovative care, and advances therapeutic research strategies [8, 32].
Discussion
Knowledge shared among individuals or groups can be either explicit or tacit. Explicit knowledge can be codified, documented, and easily disseminated among individuals, groups, and organizations. It includes various forms such as documents, textbooks, and scientific articles [55]. In contrast, tacit knowledge refers to skills, ideas, and experiences that reside in the minds of individuals, making access to them challenging. People often do not recognize their tacit knowledge or how to leverage it to assist others [56]. In the study by Gider et al., various types of knowledge were referenced, including consulting knowledge, clinical findings about cases, work experiences, new medical knowledge, and knowledge about technology, as well as knowledge related to the work environment or organizational structure that physicians share with their colleagues or other healthcare professionals [8]. Abdul Rahman also examined methods of knowledge sharing, indicating that knowledge about 'know-how' and skills is shared tacitly [42]. Therefore, in the healthcare system across different hospital departments, tacit and explicit knowledge is shared, and these two types continually interact. Adeyelure et al. noted that interactions between tacit and explicit knowledge occur within meetings held among healthcare staff [31].
Knowledge can be shared formally or informally. Raven & El Sawy classified formal and informal knowledge-sharing methods, noting that each method can involve two or more participants. Formal sharing is typically planned, while informal sharing is spontaneous [57]. In the healthcare system, knowledge sharing occurs through various formal methods, such as workshops, symposiums, conferences, and webinars. Informally, it takes place through observation, imitation, and apprenticeship. With advancements in technology and communication, knowledge is increasingly shared online in addition to in-person interactions.
In addition to knowledge sharing within organizations, inter-organizational knowledge sharing occurs through referring patients to specialists from different hospitals [35]. Various factors contribute to knowledge sharing among organizations, such as the need for an organization to survive [1]—however, more than this factor is required. Effective inter-organizational knowledge sharing also necessitates infrastructure provision, especially when knowledge is shared virtually [42].
To facilitate the easy sharing of knowledge, individual, organizational, and political barriers must be addressed or managed as much as possible. Given the hierarchical nature of hospitals [10], it is not surprising that healthcare personnel may fear losing their positions of power, which can hinder knowledge sharing [42]. Some barriers, such as the overload of healthcare staff [35], can be mitigated with appropriate management. Since the primary focus of providing care to patients is to ensure their safety and well-being, healthcare workers sometimes do not prioritize knowledge sharing. Zhou & Nunes [35] noted that physicians are often overwhelmed with work and tend to focus more on addressing immediate patient needs, which may lower knowledge sharing on their priorities [35].
One of the significant barriers to knowledge sharing is the need for more trust at both the individual and organizational levels. As Zhou & Nunes noted in their study, a recurring theme in the interviewees' statements was the issue of distrust between parties during the referral process. This distrust pertained to healthcare professionals in primary care settings during referrals and to the tacit knowledge shared by peer specialists and patient medical records involved in the referral process [35]. Abdul Rahman also stated in his study that 45.5% of respondents identified peer distrust, and 43.3% identified distrust in management as an obstacle to knowledge sharing [42]. Underland [47] further indicated that when new information is shared in clinical meetings, surgeons must regard it as reliable; Otherwise, the clinical meeting serves no purpose as a venue for knowledge sharing and decision-making. Appropriate knowledge-sharing policies are needed to effectively manage these individual and organizational barriers, as the absence of such policies constitutes a barrier to knowledge-sharing [35].
Since knowledge is considered an important organizational asset and should not be confined, its sharing has positive implications when facilitated. Tetroe et al. asserted that knowledge sharing is vital for the healthcare sector, as it can enhance accountability and evidence-based performance in health planning, policy-making, and service delivery [58]. Jabr identified the benefits of knowledge sharing in his study as follows: 1) reduction of medical errors, 2) improvement in the quality of healthcare, 3) enhancement of patient health and safety, 4) support for the promotion of evidence-based medical practices, 5) encouragement of patient-centered technologies, and 6) provision of better health outcomes through improved training and education for health professionals [7].
One limitation of this study was the need for more access to the full text of certain articles and theses. Establishing clear policies is essential to facilitate effective knowledge sharing among individuals and organizations.
Conclusion
Tacit and explicit forms of knowledge (such as experiences and patient records) are shared among healthcare staff within the health system through formal, informal, in-person, and virtual means. Knowledge is shared at the individual level and within and between organizations. Both organizational and individual factors play a role in this process. Consequently, knowledge sharing in the health system has positive implications for its stakeholders, including organizations, patients, and healthcare staff.
Acknowledgments: The authors express their gratitude to Dr. Neda Mehrdad for her support in conducting this research, and The authors acknowledge the substantial contributions of all who shared their knowledge through published papers.
Ethical Permissions: This research was approved by the Ethics Committee of Iran University of Medical Sciences with the ethics code IR.IUMS.FMD.REC.1401.358.
Conflicts of Interests: The authors of this research have no conflicts of interest. This research, approved by Iran University of Medical Sciences, is being published with the consent and collaboration of all authors.
Authors' Contribution: Nouri Khaneghah Z (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Sohrabi Z (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (30%); Bigdeli S (Third Author), Introduction Writer/Methodologist/Original Researcher/Discussion Writer/Statistical Analyst (15%); Khoddam H (Fourth Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (15%); Kamali M (Fifth Author), Methodologist/Main Researcher/Statistical Analyst (10%)
Funding/Support: The Vice-Chancellor for Research of Iran University of Medical Sciences granted and supported this research.
Article Type: Systematic Review |
Subject:
Health Promotion Setting
Received: 2024/06/4 | Accepted: 2024/08/28 | Published: 2024/08/30
Received: 2024/06/4 | Accepted: 2024/08/28 | Published: 2024/08/30
References
1. Omotayo FO, Orimolade TA. Exploring the knowledge sharing practices among medical doctors in Ibadan metropolis, Nigeria. Covenant J Commun. 2021;7(2). [Link] [DOI:10.1504/IJKMS.2021.116407]
2. Deng P, Lu H. Transnational knowledge transfer or indigenous knowledge transfer: Which channel has more benefits for China's high-tech enterprises?. Eur J Innov Manag. 2022;25(2):433-53. [Link] [DOI:10.1108/EJIM-07-2020-0269]
3. Sabeeh Z, Syed Mustapha S, Mohamad R. Healthcare knowledge sharing among a community of specialized physicians. Cogn Technol Work. 2018;20:105-24. [Link] [DOI:10.1007/s10111-017-0453-z]
4. Wills MJ, Sarnikar S, El-Gayar OF, Deokar A. Information systems and healthcare XXXIV: Clinical knowledge management systems-literature review and research issues for information systems. Commun Assoc Inf Syst. 2010;26:565-98. [Link] [DOI:10.17705/1CAIS.02626]
5. Adler-Milstein J, Daniel G, Grossmann C, Mulvany C, Nelson R, Pan E, et al. Return on information: A standard model for assessing institutional return on electronic health records. NAM Perspectives. Washington, DC: National Academy of Medicine; 2014. [Link]
6. Waring JJ, Bishop S. "Water cooler" learning: Knowledge sharing at the clinical "backstage" and its contribution to patient safety. J Health Organ Manag. 2010;24(4):325-42. [Link] [DOI:10.1108/14777261011064968]
7. Jabr NH. Physicians' attitudes towards knowledge transfer and sharing. Competit Rev. 2007;17(4):248-60. [Link] [DOI:10.1108/10595420710844334]
8. Gider Ö, Ocak S, Top M. Perceptions of physicians about knowledge sharing barriers in Turkish health care system. J Med Syst. 2015;39(5):42. [Link] [DOI:10.1007/s10916-015-0230-6]
9. Bolarinwa O, Salaudeen A, Akande T. Overview of knowledge management applications in health care delivery of developing countries. Acad Res Int. 2012;3(3):38-45. [Link]
10. Al Shamsi A. An investigation into knowledge sharing in crossprofessional teams in healthcare a multi-method, qualitative case study design [dissertation]. Sheffield: University of Sheffield; 2020. [Link]
11. Rehman WU, Ilyas M, Asghar N. Knowledge sharing, knowledge management strategy and performance a knowledge based view. Pak Econ Soc Rev. 2015;53(2):177-202. [Link]
12. Olan F, Liu S, Neaga I, Alkhuraiji A. How knowledge sharing and business process contribute to organizational performance: Using the fsQCA approach. J Bus Res. 2016;69(11):5222-7. [Link] [DOI:10.1016/j.jbusres.2016.04.116]
13. Doronin D, Lei S, Shah SHH. Reconsidering concept of knowledge sharing: search for quality dimensions. Kybernetes. 2021;50(5):1058-74. [Link] [DOI:10.1108/K-11-2019-0767]
14. Morrow S. A study of knowledge sharing practices between healthcare workers [dissertation]. Canada: Royal Roads University; 2006. [Link]
15. Bonis SA. Concept analysis: Method to enhance interdisciplinary conceptual understanding. ANS Adv Nurs Sci. 2013;36(2):80-93. [Link] [DOI:10.1097/ANS.0b013e318290d86e]
16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-88. [Link] [DOI:10.1177/1049732305276687]
17. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105-12. [Link] [DOI:10.1016/j.nedt.2003.10.001]
18. Guba EG, Lincoln YS. Competing paradigms in qualitative research. In: Handbook of qualitative research. Washington DC: Sage Publications; 1994. p. 105-17. [Link]
19. Tabatabaee A, Hasani P, Mortazavi H, Tabatabaeichehr M. Strategies to enhance rigor in qualitative research. J North Khorasan Univ Med Sci. 2013;5(3):663-70. [Persian] [Link] [DOI:10.29252/jnkums.5.3.663]
20. Von Behr CM, Cleaver I, Minshall T, Clarkson PJ. Trust and knowledge sharing among hospitals during COVID-19: The compound effect of four barriers to organisational trust for knowledge sharing. VINE J Inf Knowl Manag Syst. 2023;53(2):315-34. [Link] [DOI:10.1108/VJIKMS-05-2022-0170]
21. Yen C. Exploring member's knowledge sharing intention in online health communities: The effects of social support and overload. PloS One. 2022;17(3):e0265628. [Link] [DOI:10.1371/journal.pone.0265628]
22. Burns P, Currie G, McLoughlin I, Robinson T, Sohal A, Teede H. Creating conditions for effective knowledge brokering: A qualitative case study. BMC Health Serv Res. 2022;22(1):1303. [Link] [DOI:10.1186/s12913-022-08559-1]
23. Komodromos M, Nicoli N, Papacharalambous C. The use of social media in healthcare: Knowledge transfer in the Cyprus healthcare system. Int J Technol Enhanc Learn. 2021;13(3):253-65. [Link] [DOI:10.1504/IJTEL.2021.115976]
24. Cresswell K, Sheikh A, Franklin BD, Krasuska M, The Nguyen H, Hinder S, et al. Interorganizational knowledge sharing to establish digital health learning ecosystems: Qualitative evaluation of a National Digital Health Transformation Program in England. J Med Internet Res. 2021;23(8):e23372. [Link] [DOI:10.2196/23372]
25. Heenan D. Collaborating on healthcare on an all-island basis: A scoping study. Ir Stud Int Aff. 2021;32(2):413-47. [Link] [DOI:10.1353/isia.2021.0007]
26. Alonazi WB. Building learning organizational culture during COVID-19 outbreak: A national study. BMC Health Serv Res. 2021;21(1):422. [Link] [DOI:10.1186/s12913-021-06454-9]
27. Cifalino A, Mascia D, Vendramini EA. Goal importance, use of performance measures, and knowledge exchange: An empirical study on general practitioners' performance. Health Care Manag Rev. 2020;45(2):117-29. [Link] [DOI:10.1097/HMR.0000000000000206]
28. Grooten L, Vrijhoef HJM, Alhambra-Borrás T, Whitehouse D, Devroey D. The transfer of knowledge on integrated care among five European regions: A qualitative multi-method study. BMC Health Serv Res. 2020;20:11. [Link] [DOI:10.1186/s12913-019-4865-8]
29. Vold AT, Haave HM. Relevance of adult higher education on knowledge management in the healthcare sector. Electron J Knowl Manag. 2020;18(3):236-54. [Link] [DOI:10.34190/EJKM.18.03.004]
30. Rangachari P, Dellsperger KC, Rethemeyer RK. Network analysis of the structure of inter-professional knowledge exchange related to Electronic Health Record Medication Reconciliation within a Social Knowledge Networking system. J Healthc Leadersh. 2019;11:87-100. [Link] [DOI:10.2147/JHL.S211109]
31. Adeyelure TS, Kalema BM, Motlanthe BL. An empirical study of knowledge sharing: A case of South African healthcare system. Knowl Manag E-Learn. 2019;11(1):114-28. [Link] [DOI:10.34105/j.kmel.2019.11.007]
32. Puricelli Perin DM, Vogel AL, Taplin SH. Assessing knowledge sharing in cancer screening among high-, middle-, and low-income countries: Insights from the international cancer screening network. J Glob Oncol. 2019;5:1-8. [Link] [DOI:10.1200/JGO.19.00202]
33. Dagenais C, Plouffe L, Gagné C, Toulouse G, Breault AA, Dupont D. Improving the health and safety of 911 emergency call centre agents: An evaluability assessment of a knowledge transfer strategy. Int J Occup Saf Ergon. 2017;23(1):50-9. [Link] [DOI:10.1080/10803548.2016.1216355]
34. Shellum JL, Nishimura RA, Milliner DS, Harper Jr CM, Noseworthy JH. Knowledge management in the era of digital medicine: A programmatic approach to optimize patient care in an academic medical center. Learn Health Syst. 2017;1(2):e10022. [Link] [DOI:10.1002/lrh2.10022]
35. Zhou L, Nunes MB. Barriers to knowledge sharing in Chinese healthcare referral services: An emergent theoretical model. Glob Health Action. 2016;9:29964. [Link] [DOI:10.3402/gha.v9.29964]
36. Anya O, Tawfik H. A model of medical practice for contextual knowledge sharing in collaborative healthcare. Int J Med Eng Inform. 2016;8(4):360-89. [Link] [DOI:10.1504/IJMEI.2016.079364]
37. Sibbald SL, Kothari A. Creating, synthesizing, and sharing: The management of knowledge in public health. Public Health Nurs. 2015;32(4):339-48. [Link] [DOI:10.1111/phn.12184]
38. Farrington C, Clare I, Holland A, Barrett M, Oborn E. Knowledge exchange and integrated services: Experiences from an integrated community intellectual (learning) disability service for adults. J Intellect Disabil Res. 2015;59(3):238-47. [Link] [DOI:10.1111/jir.12131]
39. Lemire M, Demers‐Payette O, Jefferson‐Falardeau J. Dissemination of performance information and continuous improvement: A narrative systematic review. J Health Organ Manag. 2013;27(4):449-78. [Link] [DOI:10.1108/JHOM-08-2011-0082]
40. Taheri M, Gharakhani D. The application of total quality management and knowledge management in health system. Res J Appl Sci Eng Technol. 2013;5(9):2681-5. [Link] [DOI:10.19026/rjaset.5.4791]
41. Williams PM. Integration of health and social care: A case of learning and knowledge management. Health Soc Care Community. 2012;20(5):550-60. [Link] [DOI:10.1111/j.1365-2524.2012.01076.x]
42. Abdul Rahman R. Knowledge sharing practices: A case study at Malaysia's healthcare research institutes. Int Inf Library Rev. 2011;43(4):207-14. [Link] [DOI:10.1080/10572317.2011.10762902]
43. Dearing JW, Greene SM, Stewart WF, Williams AE. If we only knew what we know: Principles for knowledge sharing across people, practices, and platforms. Transl Behav Med. 2011;1(1):15-25. [Link] [DOI:10.1007/s13142-010-0012-0]
44. Bedi S, Bedi M. Knowledge management in health systems: The emerging role of chief information officer (health) from grassroots to tertiary levels. Clin Commun Med Educ. 2011;1(2):105-9. [Link]
45. Nilsen LL, Ludvigsen SR. Collaborative work and medical talk: Opportunities for learning through knowledge sharing. Commun Med. 2010;7(2):143-53. [Link] [DOI:10.1558/cam.v7i2.143]
46. Steininger K, Ruckel D, Dannerer E, Roithmayr F. Healthcare knowledge transfer through a web 2.0 portal: An Austrian approach. Int J Healthc Technol Manag. 2010;11(1-2):13-30. [Link] [DOI:10.1504/IJHTM.2010.033272]
47. Underland G. When trustworthiness matters: How trust influences knowledge-production and knowledge-sharing in a surgical department. Commun Med. 2010;7(2):187-96. [Link] [DOI:10.1558/cam.v7i2.187]
48. Ramanadhan S, Wiecha JL, Emmons KM, Gortmaker SL, Viswanath K. Extra-team connections for knowledge transfer between staff teams. Health Educ Res. 2009;24(6):967-76. [Link] [DOI:10.1093/her/cyp030]
49. Quinlan E. The 'actualities' of knowledge work: An institutional ethnography of multi‐disciplinary primary health care teams. Sociol Health Illn. 2009;31(5):625-41. [Link] [DOI:10.1111/j.1467-9566.2009.01167.x]
50. Lemmergaard J. Reducing hospital‐acquired infections through knowledge‐sharing in work teams. Team Perform Manag. 2009;15(1/2):63-77. [Link] [DOI:10.1108/13527590910937720]
51. Gowen CR 3rd, Henagan SC, McFadden KL. Knowledge management as a mediator for the efficacy of transformational leadership and quality management initiatives in U.S. health care. Health Care Manag Rev. 2009;34(2):129-40. [Link] [DOI:10.1097/HMR.0b013e31819e9169]
52. Gorry C. Cuba's virtual libraries: Knowledge sharing for the developing world. MEDICC Rev. 2008;10(1):9-12. [Link] [DOI:10.37757/MR2008.V10.N1.6]
53. Sánchez-Polo MT, Cegarra-Navarro JG. Implementing knowledge management practices in hospital-in-the-home units. J Nurs Care Qual. 2008;23(1):18-22. [Link] [DOI:10.1097/01.NCQ.0000303801.30327.a4]
54. Gagliardi AR, Fraser N, Wright FC, Lemieux-Charles L, Davis D. Fostering knowledge exchange between researchers and decision-makers: Exploring the effectiveness of a mixed-methods approach. Health Policy. 2008;86(1):53-63. [Link] [DOI:10.1016/j.healthpol.2007.09.002]
55. Stevens RH, Millage J, Clark S. Waves of knowledge management: The flow between explicit and tacit knowledge. Am J Econ Bus Adm. 2010;2(1):129-35. [Link] [DOI:10.3844/ajebasp.2010.129.135]
56. Holste JS, Fields D. Trust and tacit knowledge sharing and use. J Knowl Manag. 2010;14(1):128-40. [Link] [DOI:10.1108/13673271011015615]
57. Raven A, El Sawy OA. Silence or knowing in IT-facilitated face-to-face meetings. J Organ Comput Electron Commer. 2012;22(2):111-31. [Link] [DOI:10.1080/10919392.2012.667693]
58. Tetroe JM, Graham ID, Foy R, Robinson N, Eccles MP, Wensing M, et al. Health research funding agencies' support and promotion of knowledge translation: An international study. Milbank Q. 2008;86(1):125-55. [Link] [DOI:10.1111/j.1468-0009.2007.00515.x]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






