Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 707-714 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Wibowo Y, Priyanto E, Mulyanto J, Munfiah S, Rujito L, Roestijawati N. Prevalence of Common Mental Disorders in Indonesian Pregnant Women on Pandemic Situation and its Influencing Factors. Health Educ Health Promot 2023; 11 (5) :707-714
URL: http://hehp.modares.ac.ir/article-5-72008-en.html
URL: http://hehp.modares.ac.ir/article-5-72008-en.html
1- Department of Public Health and Community Medicine, Faculty of Medicine, Jenderal Soedirman University, Purwokerto, Indonesia
2- Department of Obstetrics and Gynecology, Faculty of Medicine, Jenderal Soedirman University, Purwokerto, Indonesia
3- Department of Genetics and Molecular Medicine, Faculty of Medicine, Jenderal Soedirman University, Purwokerto, Indonesia
2- Department of Obstetrics and Gynecology, Faculty of Medicine, Jenderal Soedirman University, Purwokerto, Indonesia
3- Department of Genetics and Molecular Medicine, Faculty of Medicine, Jenderal Soedirman University, Purwokerto, Indonesia
Full-Text [PDF 604 kb]
(2800 Downloads)
| Abstract (HTML) (962 Views)
Full-Text: (203 Views)
Introduction
Typically, about 10% of pregnant women globally go through mental health challenges, predominantly depression. This figure tends to be even higher in developing nations, reaching approximately 16%. The prevalence of these mental health disorders may escalate due to the impact of the COVID-19 pandemic. Adopting precise and suitable strategies to address this trend is crucial. So, besides being vulnerable to physical health issues, expectant mothers face an increased risk of experiencing psychological issues, a consequence of public health management like minimizing social interactions and quarantine [1-3]. Everyone may be contaminated by the virus, and pregnant women are an at-risk population. Pregnant women are in a state of compromised immunity, and biological adaptive changes occur during pregnancy, which makes them vulnerable to contracting respiratory viruses such as SARS and MERS. The COVID-19 pandemic has resulted in increased levels of stress and anxiety in pregnant women [2-6].
Isolation measures frequently lead to an unfavorable ordeal for individuals subjected to them, resulting in psychological impacts like irritability. Concerns about infection transmission to loved ones make feelings of heightened anxiety, anger, confusion, frustration, loneliness, denial, depressive feelings, sleep disturbances, and, in severe cases, thoughts of self-harm or suicide. Individuals in isolation due to suspected cases often experience heightened anxiety stemming from uncertainty about their health status. This uncertainty may manifest in obsessive-compulsive behaviors, like frequently checking their temperature and maintaining rigorous sterilization practices. Furthermore, enforcing quarantine and isolation measures raises the potential for legal implications and the prospect of litigation [7-10]. Post-quarantine psychological impacts include socio-economic pressure, psychological symptoms from financial problems, social stigma and rejection, discrimination, property insecurity, and continued withdrawal from social events even after pandemic control [7].
The COVID-19 pandemic has indeed had a significant impact on the mental health of pregnant women. Research has shown that the pandemic has imposed a major mental health burden on pregnant and postpartum women, increasing the risk of depression, anxiety, and sleep disturbances [11]. Specific stressors faced by pregnant women during the pandemic include disruptions to prenatal care, fears of contracting the virus, social isolation, income loss, and anxiety about altered labor and delivery protocols [12]. These stressors, along with the limitations on recovery resources and support networks during the postpartum period, highlight the critical need to monitor and safeguard maternal mental health during public health crises [13].
Studies have also evaluated the associations between COVID-19-related experiences and mental health outcomes among pregnant women, indicating a significant impact on depressive symptoms, thoughts of self-harm, and anxiety. Coping strategies have been identified as mediators between COVID-19 experiences and mental health outcomes in pregnancy, emphasizing the importance of effective coping mechanisms during the pandemic. Furthermore, the pandemic has posed significant challenges associated with mental health, quality of life, and lifestyle changes among pregnant women, underscoring the need for comprehensive support and intervention efforts [14].
The impact of the COVID-19 pandemic on maternal mental health has been observed globally, with studies reporting worsening mental health symptoms, especially among mothers experiencing economic disadvantage [15]. It is crucial to closely monitor the prevalence and predictors of common mental disorders (CMDs) among pregnant women to guide intervention efforts during and after the pandemic. Additionally, the pandemic has raised concerns about the potential detrimental effects on maternal-fetal bonding and infant development [16].
Banyumas district is one of the largest districts in Central Java Province, Indonesia, with approximately 1.8 million people. Until July 2022, 37,638 confirmed cases of COVID-19 were reported, with 2,099 deaths. Findings from previous studies showed that 21% of the general population experienced anxiety related to COVID-19. Being a COVID-19 survivor and having unmarried status have been identified as the main risk factors. However, no studies have been conducted to investigate the prevalence of CMDs and the associated risk factors in vulnerable groups such as pregnant women after the pandemic situation. Therefore, this study aimed to estimate the prevalence of CMDs among Indonesian pregnant women as well as assess its associated risk factors.
Instrument and Methods
Study design
This is a cross-sectional study involving 1,543 participants of pregnant women who lived in Banyumas District, Central Java Province, Indonesia, from January to August 2022.
Sampling
The minimum sample size was 454 individuals, which were calculated based on the assumptions of (I) the anxiety prevalence in the population is 16%, (II) the level of significance is 5%, and (III) the design effect of two levels. Samples were recruited from the population using the snowball sampling method. Eligibility criteria include individuals who can access online questionnaires, are mentally competent, can read and write, and are willing to participate in the study by signing an informed consent form. Subjects who provided incomplete questionnaire data or resigned during the questionnaire's completion were excluded.
Data collecting tools
Basic covariates were demographic characteristics (age, type of family), socioeconomic characteristics (educational level, family income, employment status), place of residence, and body mass index (BMI) during pregnancy.
Self-Reported Questionnaire-20 (SRQ-20)
This questionnaire comprises 20 yes/no questions that encompass a range of psychological symptoms commonly observed in the general population, such as anxiety, depression, and psychosomatic complaints, to measure CMDs. The scoring of the SRQ-20 is straightforward; each "yes" response is scored as 1, and each "no" response is 0, leading to a total score ranging from 0 to 20. Higher scores suggest a greater likelihood of CMDs, with a specific cut-off point determined to identify at-risk individuals adapted to our study's population and setting. The SRQ-20's brevity and simplicity made it an ideal instrument for our research, allowing for efficient and effective data collection without overwhelming the participants, who were already dealing with pregnancy's physical and emotional stresses during a challenging time. To ensure cultural relevance and comprehension among the Indonesian participants, the SRQ-20 was translated into Bahasa Indonesia. This translation process included back-translation to maintain the integrity of the original questions. It was followed by a pilot test to confirm the questionnaire's reliability and validity in the Indonesian context, particularly among pregnant women.
Social Support Questionnaire-6 (SSQ-6)
The SSQ-6 is a brief and efficient tool consisting of six items, each designed to assess various dimensions of social support, including emotional, instrumental, and informational support. Respondents are asked to list the individuals who provide them with support in specific situations and then rate their satisfaction with the support received on a scale. In our context, the SSQ-6 was instrumental in assessing how social networks and the perceived adequacy of support influenced the mental well-being of pregnant women during a period marked by social isolation and heightened stress due to the pandemic. To ensure cultural appropriateness and clarity for our Indonesian participants, the SSQ-6 was carefully translated into Bahasa Indonesia, with attention to maintaining the essence of each item. The translated version underwent a pilot testing phase to confirm its effectiveness in capturing the intricacies of social support within the Indonesian cultural context, particularly among the pregnant population facing unique challenges during the pandemic.
Quality Marriage Index (QMI)
Marital satisfaction items inquire about the degree of happiness, level of agreement, overall satisfaction with the marriage, and the extent to which partners confide in each other. The respondents rate their agreement with these statements on a Likert scale, quantitatively measuring marital quality. This scale is particularly valuable in our study for understanding how the quality of marital relationships impacts the mental health of pregnant women. To suit the cultural and linguistic context of our Indonesian participants, the QMI was translated into Bahasa Indonesia. This meticulous translation process ensured that the nuances of the marital relationship as perceived in Indonesian culture were accurately captured. The translated QMI was then piloted among a small group to verify its reliability and validity in effectively measuring marital satisfaction in the Indonesian setting, especially during the tumultuous period of the pandemic.
Procedure
This study underwent an institutional review board and received ethics approval.
Statistical analysis
A statistical software was used for data analysis. The associations between risk factors and covariates with CMDs were tested using simple logistic regression, and crude odd ratios (OR) with 95% confidence interval (95%CI) were calculated to indicate the risk estimates of each main risk factor. The significant risk factors and covariates in the bivariate analysis were included in the final model and tested using multiple logistic regression to obtain the fully adjusted risk estimate. The risk estimates of each risk factor were indicated by adjusted OR with 95%CI.
Findings
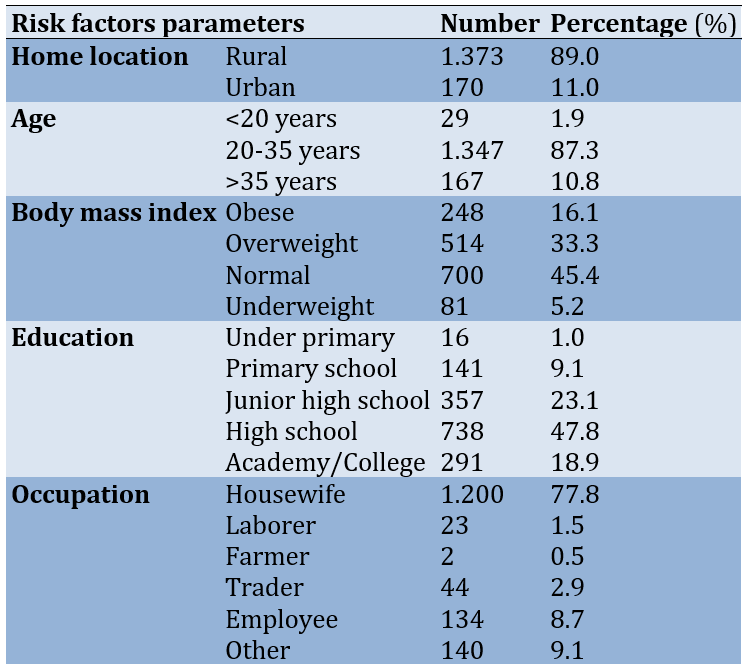
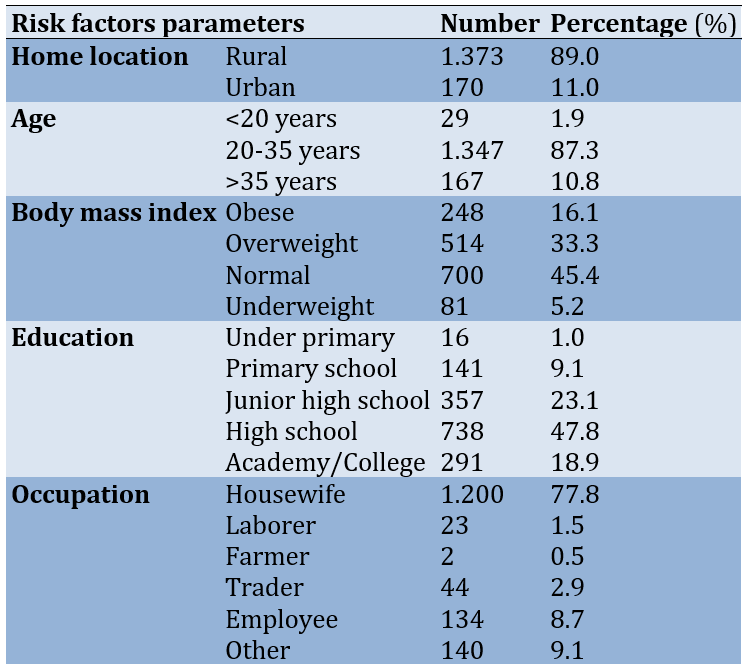
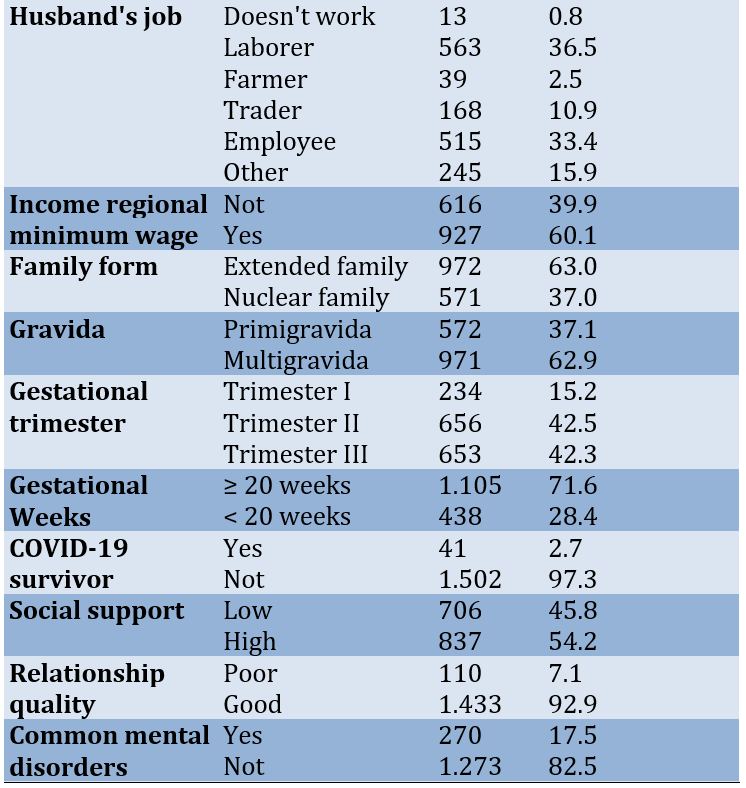
Most studied pregnant women lived in rural areas (89.0%), were between 20-35 years old (87.3%), had normal BMI (45.4%), completed high school education (47.8%), were not working or housewives (77.8%), had husbands working as laborers (36.5%), and had income above the regional minimum wage (60.1%). Over 60% were multigravida and in the second trimester of pregnancy (42.5%). Most were ≥20 weeks gestation (71.6%), did not have COVID-19 previously (97.3%), and had high social support (54.2%). The vast majority reported having a good relationship quality with their partner (92.9%; Table 1).
Table 1. Characteristics of the research subjects
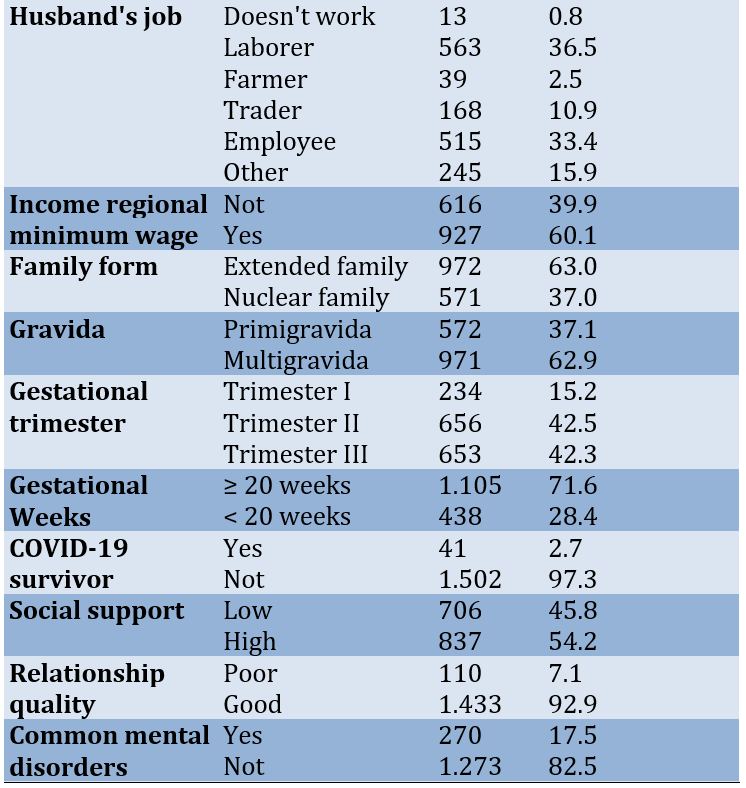
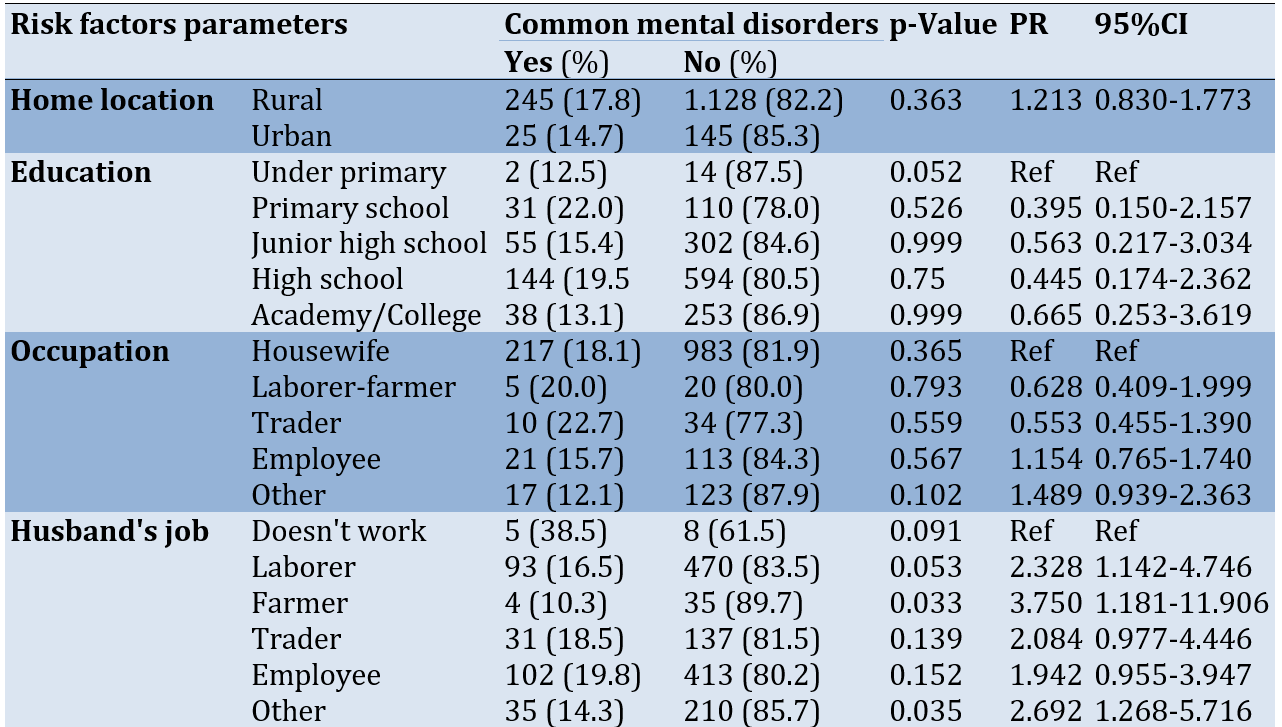
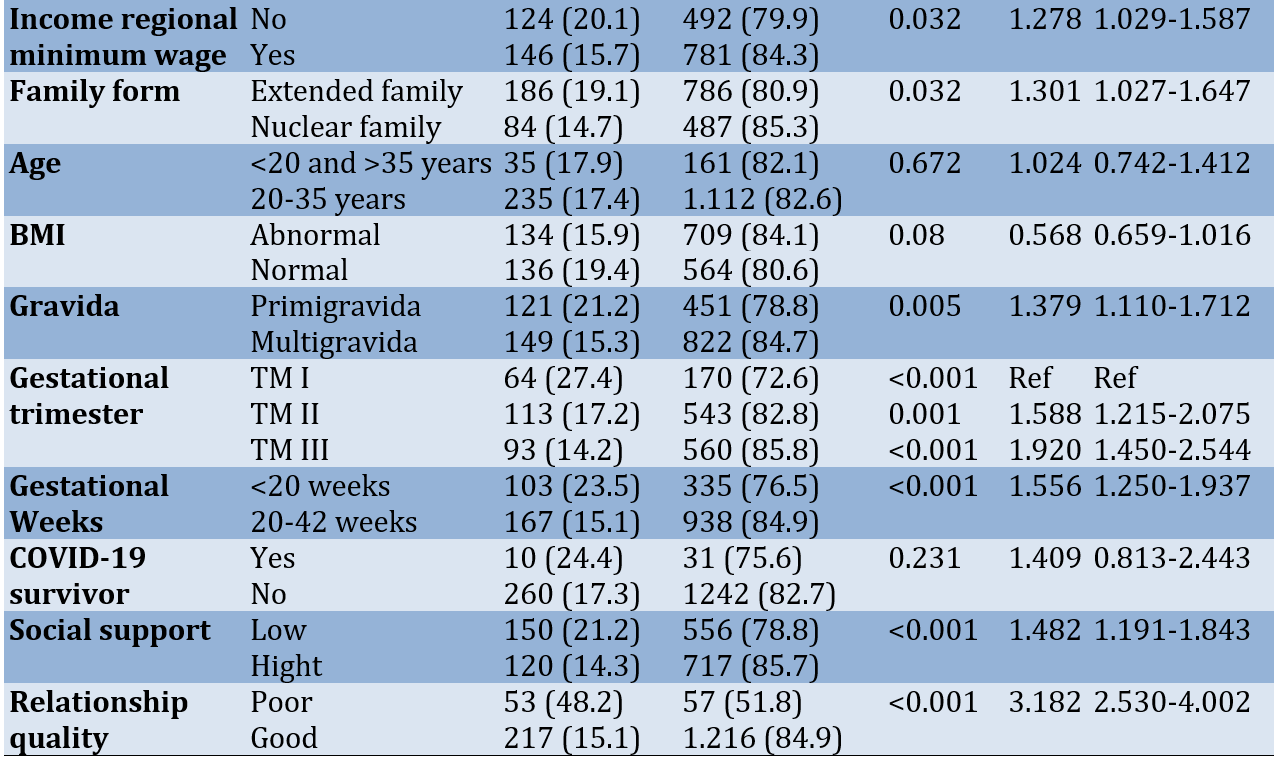
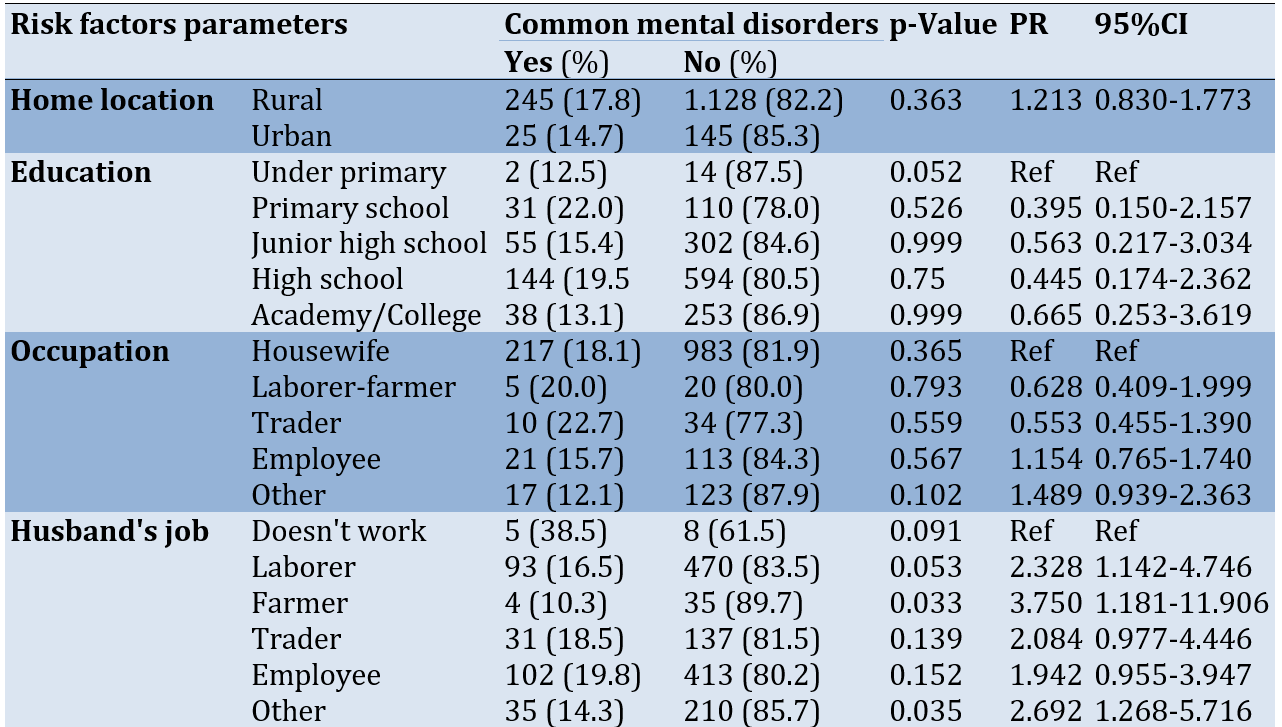
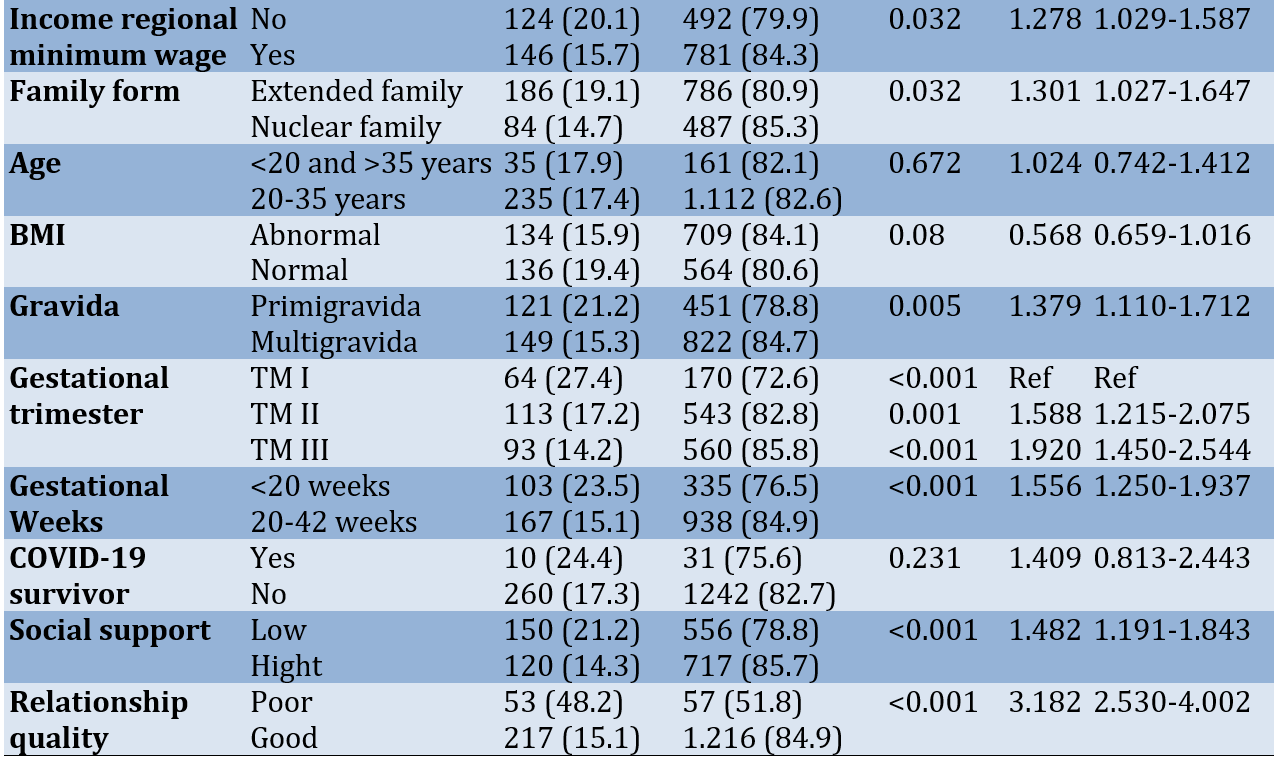
There were significant associations in between having and not having CMDs according to income regional minimum wage (p=0.032), family form (p=0.032), gravida (p=0.005), gestational week (p<0.001), gestational age (p<0.001), social support (p<0.001), and relationship quality (p<0.001; Table 2).
Table 2. The relationship between common mental disorders and risk factors parameters
Poor relationship quality had the highest odds ratio, with women having over 5 times higher odds than those with good relationship quality (OR=5.109; 95%CI=3.334-7.828; p<0.001). Lower maternal education level remained significantly associated with over 2 times higher odds of common mental disorders (OR=2.081; 95%CI=1.196-3.621; p=0.010). Primigravidity also had an independent association, with primigravida women having 1.7 times higher odds than multigravida women (OR=1.708; 95%CI=1.284-2.272; p<0.001). Finally, gestational age <20 weeks retained its significant association, with 1.8 times higher odds versus ≥20 weeks gestation (OR=1.812; 95%CI=1.360-2.414; p<0.001).
Discussion
The prevalence of common mental disorders among pregnant women in the Indonesian study was 17.5%, aligning with rates reported in comparable studies conducted in low and middle-income countries. A systematic review focusing on perinatal mental disorders among women in low and lower-middle-income countries found a weighted mean prevalence of 15.6% during pregnancy. This consistency in prevalence rates across diverse studies emphasizes the global nature of the issue and the need for widespread attention [17, 18].
Furthermore, additional systematic reviews have reported a wide range of prevalence estimates for antepartum anxiety and depression among women in non-western cultures, varying from 5.2% to 32.9% [19, 20]. These findings illustrate the significant variability in mental health challenges faced by pregnant women in different cultural contexts. In terms of gravidity, the majority of the sample in the Indonesian study were multigravida (62.9%), aligning with findings from Ethiopia, where multigravida women constituted 61.5% of the study population [21]. However, contrasting proportions were reported in studies from Turkey and Nepal, indicating potential cultural or regional differences in reproductive behaviors and experiences [22, 23].
The mean maternal age in the Indonesian study was 26 years old, comparable to mean ages ranging from 25-27 years reported in studies from various low and middle-income countries (LMICs) such as Brazil, Ethiopia, and Turkey. This consistency in maternal age across different LMICs underscores a common demographic trend among pregnant women in these settings. Regarding education levels, nearly half of the women in the Indonesian sample had completed high school education (47.8%), and 18.9% had a college education. This education distribution is notably higher than observed in Ethiopian and Nepali studies [22, 23], where the majority had only completed primary education. The upward trend in educational attainment among women in the Indonesian setting suggests advancements in educational opportunities and access for women [24, 25].
Economically, a substantial portion of the pregnant women in the Indonesian study were not formally employed (77.8%), resembling findings from India, where 90% were unemployed housewives. Conversely, studies from Turkey and Brazil reported higher proportions of formally employed pregnant women. These variations likely reflect socioeconomic disparities among different populations and underscore local economic conditions' influence on pregnant women's employment rates [22, 26].
Using the sociodemographic profiles, the data closely resembles other LMIC populations. The prevalence of antepartum mental disorders in this context aligns with rates observed in developing regions, emphasizing the critical need to prioritize mental healthcare for vulnerable pregnant women globally. This unified perspective emphasizes the importance of comprehensive mental health support for pregnant women, regardless of geographical or cultural differences, to ensure the well-being of both mothers and their unborn children [27, 28].
Income level was found to be a significant factor influencing the prevalence of common mental disorders. Women with incomes below the regional minimum wage exhibited a higher prevalence of common mental disorders (20.1%) compared to those with incomes above the minimum wage (15.7%), showing a statistically significant difference (p=0.032). This finding is consistent with prior research in low and middle-income countries (LMICs), where economic disparities have been linked to heightened levels of maternal mental health challenges during pregnancy [28]. This financial fact relates to daily need stress, reduced access to care, fewer social supports, and nutrition/health factors. The pandemic has significantly impacted the economy, with many people losing their jobs or experiencing financial instability [29].
Moreover, the family structure also displayed a significant association with the prevalence of common mental disorders. Women residing in extended families had a higher prevalence of common mental disorders (19.1%) compared to those in nuclear families (14.7%), demonstrating a statistically significant relationship (p=0.032). This aligns with previous studies in LMICs, indicating that extended family dynamics may present unique stressors affecting maternal mental health [30]. In many cultures, extended families are expected to support and care for pregnant women and new mothers. However, this support may come with expectations and obligations that can be stressful for women. For example, women may feel pressure to conform to traditional gender roles and expectations, which can limit their autonomy and increase their stress levels. Additionally, conflicts and tensions within extended families can create stress and strain on relationships, which can negatively impact maternal mental health [31].
Gravidity, or the number of pregnancies a woman has experienced, emerged as another significant factor influencing the prevalence of common mental disorders. Primigravida women exhibited a higher prevalence (21.2%) compared to multigravida women (15.3%), showcasing a statistically significant difference (p=0.005). This trend is consistent with research from similar socio-economic contexts, emphasizing the heightened vulnerability of first-time pregnant women to mental health challenges [32]. The COVID-19 pandemic has likely exacerbated this vulnerability, as first-time pregnant women may have experienced greater stress and anxiety due to the pandemic's impact on their social support systems and healthcare access [33, 34]. The pandemic has highlighted the need for interventions that address the unique mental health challenges faced by first-time pregnant women, particularly during the pandemic. These interventions may include telehealth services, online support groups, and community-based initiatives that promote social connectedness and relationship building [35, 36].
Furthermore, gestational age was significantly associated with the prevalence of common mental disorders. Prevalence decreased with increasing gestational age, with 27.4% in the first, 17.2% in the second, and 14.2% in the third (p<0.001). Notably, women with a gestational age of less than 20 weeks had a higher prevalence (23.5%) compared to those with a gestational age of 20 weeks or more (15.1%), emphasizing the potential vulnerability during the earlier stages of pregnancy. This finding aligns with studies indicating a higher risk of mental health disorders in early pregnancy due to various biological and psychosocial factors [37].
Primigravidity, representing first-time pregnancies, also exhibited an independent association, with primigravida women facing 1.7 times higher odds of experiencing common mental disorders compared to multigravida women (OR=1.708; 95%CI=1.284-2.272; p<0.001). This finding aligns with previous studies indicating increased vulnerability and stress associated with first-time pregnancies [37]. The COVID-19 pandemic has likely exacerbated this vulnerability by disrupting the impact on their social support systems and healthcare access. This may include telehealth services, online support groups, and community-based initiatives that promote social connectedness and relationship building [38]. Mental health service providers should mitigate disruptions by delivering care via alternative routes, including digital technologies and community-based initiatives [36]. It emphasizes the importance of tailored support and mental health interventions for women experiencing their first pregnancy.
Social support and relationship quality were also found to be significant factors impacting the prevalence of common mental disorders. Women with low social support demonstrated a significantly higher prevalence of common mental disorders (21.2%) compared to those with high support (14.3%), indicating the protective role of social support during pregnancy (p<0.001). Similarly, women with poor relationship quality exhibited a markedly higher prevalence (48.2%) compared to those with good relationship quality (15.1%), underscoring the importance of a supportive and positive relationship environment (p<0.001). These results are consistent with previous research highlighting the critical influence of social support and relationship quality on maternal mental health during pregnancy [39]. The pandemic has also disrupted social support systems and created feelings of loneliness and isolation among pregnant women [40]. The pandemic has highlighted the critical influence of social support and relationship quality on maternal mental health during pregnancy [41]. Supportive partner relationships have been found to contribute to maternal and infant well-being. Conversely, low social support has been associated with a higher prevalence of common mental disorders among pregnant women [42].
One of the most striking findings from the multivariate analysis is the profound impact of relationship quality on the odds of experiencing common mental disorders. Poor relationship quality exhibited the highest odds ratio, with women experiencing over 5 times higher odds than those with good relationship quality (OR=5.109; 95%CI=3.334-7.828; p<0.001). This underlines the critical role that the quality of relationships plays in maternal mental health, emphasizing the need for interventions addressing relationship dynamics to mitigate the risk of common mental disorders during pregnancy.
Moreover, lower maternal education level emerged as a significant factor independently associated with over 2 times higher odds of common mental disorders (OR=2.081; 95%CI=1.196-3.621; p=0.010). This finding resonates with existing research, emphasizing the adverse impact of limited education on maternal mental health [28]. It underscores the necessity for targeted educational interventions to improve mental health outcomes for pregnant women, particularly those with lower educational attainment.
Lastly, a gestational age of less than 20 weeks retained its significant association, showing 1.8 times higher odds of common mental disorders compared to the gestational age of 20 weeks or more (OR=1.812; 95%CI=1.360-2.414; p<0.001). This echoes previous research highlighting the heightened risk of mental health challenges in early pregnancy due to various physiological and psychosocial factors [43]. It underscores the importance of early mental health assessment and support for pregnant women, especially during the initial stages of pregnancy.
Conclusion
The number of common mental disorders in Indonesian pregnant women is relatively high. Poor relationship quality is the highest risk factor for having common mental disorders. Addressing social and educational determinants is vital for enhancing maternal mental health.
Acknowledgments: None declared by the authors.
Ethical Permissions: This study underwent an institutional review board and received ethics approval from the Health Research Ethics Committee, Faculty of Medicine, Jenderal Soedirman University, Indonesia, with reference number 001/KEPK/PE/V/2022.
Conflicts of Interests: None declared by the authors.
Authors’ Contributions: Wibowo Y (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Priyanto E (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Mulyanto J (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Munfiah S (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Rujito L (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Roestijawati N (Sixth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%)
Funding/Support: None declared by the authors.
Typically, about 10% of pregnant women globally go through mental health challenges, predominantly depression. This figure tends to be even higher in developing nations, reaching approximately 16%. The prevalence of these mental health disorders may escalate due to the impact of the COVID-19 pandemic. Adopting precise and suitable strategies to address this trend is crucial. So, besides being vulnerable to physical health issues, expectant mothers face an increased risk of experiencing psychological issues, a consequence of public health management like minimizing social interactions and quarantine [1-3]. Everyone may be contaminated by the virus, and pregnant women are an at-risk population. Pregnant women are in a state of compromised immunity, and biological adaptive changes occur during pregnancy, which makes them vulnerable to contracting respiratory viruses such as SARS and MERS. The COVID-19 pandemic has resulted in increased levels of stress and anxiety in pregnant women [2-6].
Isolation measures frequently lead to an unfavorable ordeal for individuals subjected to them, resulting in psychological impacts like irritability. Concerns about infection transmission to loved ones make feelings of heightened anxiety, anger, confusion, frustration, loneliness, denial, depressive feelings, sleep disturbances, and, in severe cases, thoughts of self-harm or suicide. Individuals in isolation due to suspected cases often experience heightened anxiety stemming from uncertainty about their health status. This uncertainty may manifest in obsessive-compulsive behaviors, like frequently checking their temperature and maintaining rigorous sterilization practices. Furthermore, enforcing quarantine and isolation measures raises the potential for legal implications and the prospect of litigation [7-10]. Post-quarantine psychological impacts include socio-economic pressure, psychological symptoms from financial problems, social stigma and rejection, discrimination, property insecurity, and continued withdrawal from social events even after pandemic control [7].
The COVID-19 pandemic has indeed had a significant impact on the mental health of pregnant women. Research has shown that the pandemic has imposed a major mental health burden on pregnant and postpartum women, increasing the risk of depression, anxiety, and sleep disturbances [11]. Specific stressors faced by pregnant women during the pandemic include disruptions to prenatal care, fears of contracting the virus, social isolation, income loss, and anxiety about altered labor and delivery protocols [12]. These stressors, along with the limitations on recovery resources and support networks during the postpartum period, highlight the critical need to monitor and safeguard maternal mental health during public health crises [13].
Studies have also evaluated the associations between COVID-19-related experiences and mental health outcomes among pregnant women, indicating a significant impact on depressive symptoms, thoughts of self-harm, and anxiety. Coping strategies have been identified as mediators between COVID-19 experiences and mental health outcomes in pregnancy, emphasizing the importance of effective coping mechanisms during the pandemic. Furthermore, the pandemic has posed significant challenges associated with mental health, quality of life, and lifestyle changes among pregnant women, underscoring the need for comprehensive support and intervention efforts [14].
The impact of the COVID-19 pandemic on maternal mental health has been observed globally, with studies reporting worsening mental health symptoms, especially among mothers experiencing economic disadvantage [15]. It is crucial to closely monitor the prevalence and predictors of common mental disorders (CMDs) among pregnant women to guide intervention efforts during and after the pandemic. Additionally, the pandemic has raised concerns about the potential detrimental effects on maternal-fetal bonding and infant development [16].
Banyumas district is one of the largest districts in Central Java Province, Indonesia, with approximately 1.8 million people. Until July 2022, 37,638 confirmed cases of COVID-19 were reported, with 2,099 deaths. Findings from previous studies showed that 21% of the general population experienced anxiety related to COVID-19. Being a COVID-19 survivor and having unmarried status have been identified as the main risk factors. However, no studies have been conducted to investigate the prevalence of CMDs and the associated risk factors in vulnerable groups such as pregnant women after the pandemic situation. Therefore, this study aimed to estimate the prevalence of CMDs among Indonesian pregnant women as well as assess its associated risk factors.
Instrument and Methods
Study design
This is a cross-sectional study involving 1,543 participants of pregnant women who lived in Banyumas District, Central Java Province, Indonesia, from January to August 2022.
Sampling
The minimum sample size was 454 individuals, which were calculated based on the assumptions of (I) the anxiety prevalence in the population is 16%, (II) the level of significance is 5%, and (III) the design effect of two levels. Samples were recruited from the population using the snowball sampling method. Eligibility criteria include individuals who can access online questionnaires, are mentally competent, can read and write, and are willing to participate in the study by signing an informed consent form. Subjects who provided incomplete questionnaire data or resigned during the questionnaire's completion were excluded.
Data collecting tools
Basic covariates were demographic characteristics (age, type of family), socioeconomic characteristics (educational level, family income, employment status), place of residence, and body mass index (BMI) during pregnancy.
Self-Reported Questionnaire-20 (SRQ-20)
This questionnaire comprises 20 yes/no questions that encompass a range of psychological symptoms commonly observed in the general population, such as anxiety, depression, and psychosomatic complaints, to measure CMDs. The scoring of the SRQ-20 is straightforward; each "yes" response is scored as 1, and each "no" response is 0, leading to a total score ranging from 0 to 20. Higher scores suggest a greater likelihood of CMDs, with a specific cut-off point determined to identify at-risk individuals adapted to our study's population and setting. The SRQ-20's brevity and simplicity made it an ideal instrument for our research, allowing for efficient and effective data collection without overwhelming the participants, who were already dealing with pregnancy's physical and emotional stresses during a challenging time. To ensure cultural relevance and comprehension among the Indonesian participants, the SRQ-20 was translated into Bahasa Indonesia. This translation process included back-translation to maintain the integrity of the original questions. It was followed by a pilot test to confirm the questionnaire's reliability and validity in the Indonesian context, particularly among pregnant women.
Social Support Questionnaire-6 (SSQ-6)
The SSQ-6 is a brief and efficient tool consisting of six items, each designed to assess various dimensions of social support, including emotional, instrumental, and informational support. Respondents are asked to list the individuals who provide them with support in specific situations and then rate their satisfaction with the support received on a scale. In our context, the SSQ-6 was instrumental in assessing how social networks and the perceived adequacy of support influenced the mental well-being of pregnant women during a period marked by social isolation and heightened stress due to the pandemic. To ensure cultural appropriateness and clarity for our Indonesian participants, the SSQ-6 was carefully translated into Bahasa Indonesia, with attention to maintaining the essence of each item. The translated version underwent a pilot testing phase to confirm its effectiveness in capturing the intricacies of social support within the Indonesian cultural context, particularly among the pregnant population facing unique challenges during the pandemic.
Quality Marriage Index (QMI)
Marital satisfaction items inquire about the degree of happiness, level of agreement, overall satisfaction with the marriage, and the extent to which partners confide in each other. The respondents rate their agreement with these statements on a Likert scale, quantitatively measuring marital quality. This scale is particularly valuable in our study for understanding how the quality of marital relationships impacts the mental health of pregnant women. To suit the cultural and linguistic context of our Indonesian participants, the QMI was translated into Bahasa Indonesia. This meticulous translation process ensured that the nuances of the marital relationship as perceived in Indonesian culture were accurately captured. The translated QMI was then piloted among a small group to verify its reliability and validity in effectively measuring marital satisfaction in the Indonesian setting, especially during the tumultuous period of the pandemic.
Procedure
This study underwent an institutional review board and received ethics approval.
Statistical analysis
A statistical software was used for data analysis. The associations between risk factors and covariates with CMDs were tested using simple logistic regression, and crude odd ratios (OR) with 95% confidence interval (95%CI) were calculated to indicate the risk estimates of each main risk factor. The significant risk factors and covariates in the bivariate analysis were included in the final model and tested using multiple logistic regression to obtain the fully adjusted risk estimate. The risk estimates of each risk factor were indicated by adjusted OR with 95%CI.
Findings
Most studied pregnant women lived in rural areas (89.0%), were between 20-35 years old (87.3%), had normal BMI (45.4%), completed high school education (47.8%), were not working or housewives (77.8%), had husbands working as laborers (36.5%), and had income above the regional minimum wage (60.1%). Over 60% were multigravida and in the second trimester of pregnancy (42.5%). Most were ≥20 weeks gestation (71.6%), did not have COVID-19 previously (97.3%), and had high social support (54.2%). The vast majority reported having a good relationship quality with their partner (92.9%; Table 1).
Table 1. Characteristics of the research subjects
There were significant associations in between having and not having CMDs according to income regional minimum wage (p=0.032), family form (p=0.032), gravida (p=0.005), gestational week (p<0.001), gestational age (p<0.001), social support (p<0.001), and relationship quality (p<0.001; Table 2).
Table 2. The relationship between common mental disorders and risk factors parameters
Poor relationship quality had the highest odds ratio, with women having over 5 times higher odds than those with good relationship quality (OR=5.109; 95%CI=3.334-7.828; p<0.001). Lower maternal education level remained significantly associated with over 2 times higher odds of common mental disorders (OR=2.081; 95%CI=1.196-3.621; p=0.010). Primigravidity also had an independent association, with primigravida women having 1.7 times higher odds than multigravida women (OR=1.708; 95%CI=1.284-2.272; p<0.001). Finally, gestational age <20 weeks retained its significant association, with 1.8 times higher odds versus ≥20 weeks gestation (OR=1.812; 95%CI=1.360-2.414; p<0.001).
Discussion
The prevalence of common mental disorders among pregnant women in the Indonesian study was 17.5%, aligning with rates reported in comparable studies conducted in low and middle-income countries. A systematic review focusing on perinatal mental disorders among women in low and lower-middle-income countries found a weighted mean prevalence of 15.6% during pregnancy. This consistency in prevalence rates across diverse studies emphasizes the global nature of the issue and the need for widespread attention [17, 18].
Furthermore, additional systematic reviews have reported a wide range of prevalence estimates for antepartum anxiety and depression among women in non-western cultures, varying from 5.2% to 32.9% [19, 20]. These findings illustrate the significant variability in mental health challenges faced by pregnant women in different cultural contexts. In terms of gravidity, the majority of the sample in the Indonesian study were multigravida (62.9%), aligning with findings from Ethiopia, where multigravida women constituted 61.5% of the study population [21]. However, contrasting proportions were reported in studies from Turkey and Nepal, indicating potential cultural or regional differences in reproductive behaviors and experiences [22, 23].
The mean maternal age in the Indonesian study was 26 years old, comparable to mean ages ranging from 25-27 years reported in studies from various low and middle-income countries (LMICs) such as Brazil, Ethiopia, and Turkey. This consistency in maternal age across different LMICs underscores a common demographic trend among pregnant women in these settings. Regarding education levels, nearly half of the women in the Indonesian sample had completed high school education (47.8%), and 18.9% had a college education. This education distribution is notably higher than observed in Ethiopian and Nepali studies [22, 23], where the majority had only completed primary education. The upward trend in educational attainment among women in the Indonesian setting suggests advancements in educational opportunities and access for women [24, 25].
Economically, a substantial portion of the pregnant women in the Indonesian study were not formally employed (77.8%), resembling findings from India, where 90% were unemployed housewives. Conversely, studies from Turkey and Brazil reported higher proportions of formally employed pregnant women. These variations likely reflect socioeconomic disparities among different populations and underscore local economic conditions' influence on pregnant women's employment rates [22, 26].
Using the sociodemographic profiles, the data closely resembles other LMIC populations. The prevalence of antepartum mental disorders in this context aligns with rates observed in developing regions, emphasizing the critical need to prioritize mental healthcare for vulnerable pregnant women globally. This unified perspective emphasizes the importance of comprehensive mental health support for pregnant women, regardless of geographical or cultural differences, to ensure the well-being of both mothers and their unborn children [27, 28].
Income level was found to be a significant factor influencing the prevalence of common mental disorders. Women with incomes below the regional minimum wage exhibited a higher prevalence of common mental disorders (20.1%) compared to those with incomes above the minimum wage (15.7%), showing a statistically significant difference (p=0.032). This finding is consistent with prior research in low and middle-income countries (LMICs), where economic disparities have been linked to heightened levels of maternal mental health challenges during pregnancy [28]. This financial fact relates to daily need stress, reduced access to care, fewer social supports, and nutrition/health factors. The pandemic has significantly impacted the economy, with many people losing their jobs or experiencing financial instability [29].
Moreover, the family structure also displayed a significant association with the prevalence of common mental disorders. Women residing in extended families had a higher prevalence of common mental disorders (19.1%) compared to those in nuclear families (14.7%), demonstrating a statistically significant relationship (p=0.032). This aligns with previous studies in LMICs, indicating that extended family dynamics may present unique stressors affecting maternal mental health [30]. In many cultures, extended families are expected to support and care for pregnant women and new mothers. However, this support may come with expectations and obligations that can be stressful for women. For example, women may feel pressure to conform to traditional gender roles and expectations, which can limit their autonomy and increase their stress levels. Additionally, conflicts and tensions within extended families can create stress and strain on relationships, which can negatively impact maternal mental health [31].
Gravidity, or the number of pregnancies a woman has experienced, emerged as another significant factor influencing the prevalence of common mental disorders. Primigravida women exhibited a higher prevalence (21.2%) compared to multigravida women (15.3%), showcasing a statistically significant difference (p=0.005). This trend is consistent with research from similar socio-economic contexts, emphasizing the heightened vulnerability of first-time pregnant women to mental health challenges [32]. The COVID-19 pandemic has likely exacerbated this vulnerability, as first-time pregnant women may have experienced greater stress and anxiety due to the pandemic's impact on their social support systems and healthcare access [33, 34]. The pandemic has highlighted the need for interventions that address the unique mental health challenges faced by first-time pregnant women, particularly during the pandemic. These interventions may include telehealth services, online support groups, and community-based initiatives that promote social connectedness and relationship building [35, 36].
Furthermore, gestational age was significantly associated with the prevalence of common mental disorders. Prevalence decreased with increasing gestational age, with 27.4% in the first, 17.2% in the second, and 14.2% in the third (p<0.001). Notably, women with a gestational age of less than 20 weeks had a higher prevalence (23.5%) compared to those with a gestational age of 20 weeks or more (15.1%), emphasizing the potential vulnerability during the earlier stages of pregnancy. This finding aligns with studies indicating a higher risk of mental health disorders in early pregnancy due to various biological and psychosocial factors [37].
Primigravidity, representing first-time pregnancies, also exhibited an independent association, with primigravida women facing 1.7 times higher odds of experiencing common mental disorders compared to multigravida women (OR=1.708; 95%CI=1.284-2.272; p<0.001). This finding aligns with previous studies indicating increased vulnerability and stress associated with first-time pregnancies [37]. The COVID-19 pandemic has likely exacerbated this vulnerability by disrupting the impact on their social support systems and healthcare access. This may include telehealth services, online support groups, and community-based initiatives that promote social connectedness and relationship building [38]. Mental health service providers should mitigate disruptions by delivering care via alternative routes, including digital technologies and community-based initiatives [36]. It emphasizes the importance of tailored support and mental health interventions for women experiencing their first pregnancy.
Social support and relationship quality were also found to be significant factors impacting the prevalence of common mental disorders. Women with low social support demonstrated a significantly higher prevalence of common mental disorders (21.2%) compared to those with high support (14.3%), indicating the protective role of social support during pregnancy (p<0.001). Similarly, women with poor relationship quality exhibited a markedly higher prevalence (48.2%) compared to those with good relationship quality (15.1%), underscoring the importance of a supportive and positive relationship environment (p<0.001). These results are consistent with previous research highlighting the critical influence of social support and relationship quality on maternal mental health during pregnancy [39]. The pandemic has also disrupted social support systems and created feelings of loneliness and isolation among pregnant women [40]. The pandemic has highlighted the critical influence of social support and relationship quality on maternal mental health during pregnancy [41]. Supportive partner relationships have been found to contribute to maternal and infant well-being. Conversely, low social support has been associated with a higher prevalence of common mental disorders among pregnant women [42].
One of the most striking findings from the multivariate analysis is the profound impact of relationship quality on the odds of experiencing common mental disorders. Poor relationship quality exhibited the highest odds ratio, with women experiencing over 5 times higher odds than those with good relationship quality (OR=5.109; 95%CI=3.334-7.828; p<0.001). This underlines the critical role that the quality of relationships plays in maternal mental health, emphasizing the need for interventions addressing relationship dynamics to mitigate the risk of common mental disorders during pregnancy.
Moreover, lower maternal education level emerged as a significant factor independently associated with over 2 times higher odds of common mental disorders (OR=2.081; 95%CI=1.196-3.621; p=0.010). This finding resonates with existing research, emphasizing the adverse impact of limited education on maternal mental health [28]. It underscores the necessity for targeted educational interventions to improve mental health outcomes for pregnant women, particularly those with lower educational attainment.
Lastly, a gestational age of less than 20 weeks retained its significant association, showing 1.8 times higher odds of common mental disorders compared to the gestational age of 20 weeks or more (OR=1.812; 95%CI=1.360-2.414; p<0.001). This echoes previous research highlighting the heightened risk of mental health challenges in early pregnancy due to various physiological and psychosocial factors [43]. It underscores the importance of early mental health assessment and support for pregnant women, especially during the initial stages of pregnancy.
Conclusion
The number of common mental disorders in Indonesian pregnant women is relatively high. Poor relationship quality is the highest risk factor for having common mental disorders. Addressing social and educational determinants is vital for enhancing maternal mental health.
Acknowledgments: None declared by the authors.
Ethical Permissions: This study underwent an institutional review board and received ethics approval from the Health Research Ethics Committee, Faculty of Medicine, Jenderal Soedirman University, Indonesia, with reference number 001/KEPK/PE/V/2022.
Conflicts of Interests: None declared by the authors.
Authors’ Contributions: Wibowo Y (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Priyanto E (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Mulyanto J (Third Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Munfiah S (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Rujito L (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Roestijawati N (Sixth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%)
Funding/Support: None declared by the authors.
Article Type: Descriptive & Survey |
Subject:
Social Determinants of Health
Received: 2023/10/16 | Accepted: 2023/12/10 | Published: 2024/05/15
Received: 2023/10/16 | Accepted: 2023/12/10 | Published: 2024/05/15
References
1. Ali NA, Shahil Feroz A. Maternal mental health amidst the COVID-19 pandemic. Asian J Psychiatr. 2020;54:102261. [Link] [DOI:10.1016/j.ajp.2020.102261]
2. Fakari FR, Simbar M. Coronavirus pandemic and worries during pregnancy. Arch Acad Emerg Med. 2020;8(1):e21. [Link]
3. Luo Y, Yin K. Management of pregnant women infected with COVID-19. Lancet Infect Dis. 2020;20(5):513-4. [Link] [DOI:10.1016/S1473-3099(20)30191-2]
4. Buekens P, Alger J, Bréart G, Cafferata ML, Harville E, Tomasso G. A call for action for COVID-19 surveillance and research during pregnancy. Lancet Glob Health. 2020;8(7):e877-8. [Link] [DOI:10.1016/S2214-109X(20)30206-0]
5. Topalidou A, Thomson G, Downe S. COVID-19 and maternal mental health: Are we getting the balance right?. Pract Midwife. 2020;23(7). [Link] [DOI:10.55975/ZYUT2405]
6. Zeng LN, Chen LG, Yang CM, Zeng LP, Zhang LY, Peng TM. Mental health care for pregnant women in the COVID-19 outbreak is urgently needed. Women Birth. 2021;34(3):210-1. [Link] [DOI:10.1016/j.wombi.2020.03.009]
7. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912-20. [Link] [DOI:10.1016/S0140-6736(20)30460-8]
8. Jeong H, Yim HW, Song YJ, Ki M, Min JA, Cho J, et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38:e2016048. [Link] [DOI:10.4178/epih.e2016048]
9. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732-8. [Link] [DOI:10.7150/ijbs.45120]
10. Miles SH. Kaci hickox: Public health and the politics of fear. Am J Bioeth. 2015;15(4):17-9. [Link] [DOI:10.1080/15265161.2015.1010994]
11. Tauqeer F, Ceulemans M, Gerbier E, Passier A, Oliver A, Foulon V, et al. Mental health of pregnant and postpartum women during the third wave of the COVID-19 pandemic: A European cross-sectional study. BMJ Open. 2023;11;13(1):e063391. [Link] [DOI:10.1136/bmjopen-2022-063391]
12. Liu J, Hung P, Alberg AJ, Hair L, Whitaker KM, Simon J, et al. Mental health among pregnant women with COVID‐19-related stressors and worries in the United States. Birth. 2021;48(4):470-9. [Link] [DOI:10.1111/birt.12554]
13. Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. Coping strategies mediate the associations between COVID-19 experiences and mental health outcomes in pregnancy. Arch Womens Ment Health. 2021;24(6):1007-17. [Link] [DOI:10.1007/s00737-021-01135-2]
14. Ma J, Wang A, Zhou H. Impact of the COVID-19 lockdown on quality of life in pregnant women. Front Public Health. 2022;10:785383. [Link] [DOI:10.3389/fpubh.2022.785383]
15. Thompson SF, Shimomaeda L, Calhoun R, Moini N, Smith MR, Lengua LJ. Maternal mental health and child adjustment problems in response to the COVID-19 pandemic in families experiencing economic disadvantage. Res Child Adolesc Psychopathol. 2022;50(6):695-708. [Link] [DOI:10.1007/s10802-021-00888-9]
16. Kokkinaki T, Hatzidaki E. COVID-19 pandemic-related restrictions: Factors that may affect perinatal maternal mental health and implications for infant development. Front Pediatr. 2022;10:846627. [Link] [DOI:10.3389/fped.2022.846627]
17. Kalra H, Tran TD, Romero L, Chandra P, Fisher J. Prevalence and determinants of antenatal common mental disorders among women in India: A systematic review and meta-analysis. Arch Womens Ment Health. 2021;24(1):29-53. [Link] [DOI:10.1007/s00737-020-01024-0]
18. Waqas A, Koukab A, Meraj H, Dua T, Chowdhary N, Fatima B, et al. Screening programs for common maternal mental health disorders among perinatal women: Report of the systematic review of evidence. BMC Psychiatry. 2022;22(1):54. [Link] [DOI:10.1186/s12888-022-03694-9]
19. Sari DN, Diatri H, Siregar K, Pratomo H. The prevalence of depression symptoms among pregnant women during the second wave of COVID-19. Maced J Med Sci. 2022;10(E):546-9. [Link] [DOI:10.3889/oamjms.2022.8255]
20. Sun F, Zhu J, Tao H, Ma Y, Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynecol. 2021;42(2):91-9. [Link] [DOI:10.1080/0167482X.2020.1857360]
21. Tamiru D, Misgana T, Tariku M, Tesfaye D, Alemu D, Weldesenbet AB, et al. Prevalence and associated factors of common mental disorders among pregnant mothers in rural Eastern Ethiopia. Front Psychiatry. 2022;13:843984. [Link] [DOI:10.3389/fpsyt.2022.843984]
22. Kahyaoglu Sut H, Kucukkaya B. Anxiety, depression, and related factors in pregnant women during the COVID-19 pandemic in Turkey: A web-based cross-sectional study. Perspect Psychiatr Care. 2021;57(2):860-8. [Link] [DOI:10.1111/ppc.12627]
23. Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS One. 2019;14(4):e0214992. [Link] [DOI:10.1371/journal.pone.0214992]
24. Rujito L, Nandhika T, Lestari DWD, Ferine M, Muhaimin A. Genetic literacy levels and genetic screening attitudes on medical students in Indonesia: A national survey. Malays J Public Health Med. 2020;20(3):1-8. [Link] [DOI:10.37268/mjphm/vol.20/no.3/art.407]
25. Baihaqi BS, Hidayah AN, Rujito L. Awareness of non-health students about premarital genetic screening; A study in Indonesia. Health Educ Health Promot. 2023;11(2):189-94. [Link]
26. Machado MMT, Rocha HAL, Castro MC, Sampaio EGM, Oliveira FA, Da Silva JPF, et al. COVID-19 and mental health of pregnant women in Ceará, Brazil. Rev Saude Publica. 2021;55:37. [Link] [DOI:10.11606/s1518-8787.2021055003225]
27. Howard LM, Khalifeh H. Perinatal mental health: A review of progress and challenges. World Psychiatry. 2020;19(3):313-27. [Link] [DOI:10.1002/wps.20769]
28. Maselko J, Bates L, Bhalotra S, Gallis JA, O'Donnell K, Sikander S, et al. Socioeconomic status indicators and common mental disorders: Evidence from a study of prenatal depression in Pakistan. SSM-Popul Health. 2018;4:1-9. [Link] [DOI:10.1016/j.ssmph.2017.10.004]
29. Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62(9):686-91. [Link] [DOI:10.1097/JOM.0000000000001962]
30. Eales L, Ferguson GM, Gillespie S, Smoyer S, Carlson SM. Family resilience and psychological distress in the COVID-19 pandemic: A mixed methods study. Dev Psychol. 2021;57(10):1563-81. [Link] [DOI:10.1037/dev0001221]
31. Amah OE. Managing the negative effects of work-to-family and family-to-work conflicts on family satisfaction of working mothers' in Nigeria: The role of extended family support. Commun Work Fam. 2021;24(3):257-71. [Link] [DOI:10.1080/13668803.2019.1697646]
32. Devi NS, Shinde P, Shaikh G, Khole S. Level of anxiety towards childbirth among primigravida and multigravida mothers. Int J Appl Res. 2018;4(5):221-4. [Link]
33. McMillan IF, Armstrong LM, Langhinrichsen-Rohling J. Transitioning to parenthood during the pandemic: COVID-19 related stressors and first-time expectant mothers' mental health. Couple Fam Psychol Res Pract. 2021;10(3):179-89. [Link] [DOI:10.1037/cfp0000174]
34. Schwartz DA. The effects of pregnancy on women with COVID-19: Maternal and infant outcomes. Clin Infect Dis. 2020;71(16):2042-4. [Link] [DOI:10.1093/cid/ciaa559]
35. Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package. Int J Environ Res Public Health. 2020;17(9):2997. [Link] [DOI:10.3390/ijerph17092997]
36. Grussu P, Jorizzo GJ, Alderdice F, Quatraro RM. Preventing, mitigating, and treating women's perinatal mental health problems during the COVID-19 pandemic: A scoping review of reviews with a qualitative narrative synthesis. Behav Sci. 2023;13(5):358. [Link] [DOI:10.3390/bs13050358]
37. Farrell T, Reagu S, Mohan S, Elmidany R, Qaddoura F, Ahmed EE, et al. The impact of the COVID-19 pandemic on the perinatal mental health of women. J Perinat Med. 2020;48(9):971-6. [Link] [DOI:10.1515/jpm-2020-0415]
38. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr Clin Res Rev. 2020;14(5):779-88. [Link] [DOI:10.1016/j.dsx.2020.05.035]
39. Rahman F, Wibowo Y, Riana P. Relationship between social support and COVID-related common mental disorders incidence in pregnant women in Banyumas, Central Java. Indones J Med. 2022;8(2):142-9. [Link] [DOI:10.26911/theijmed.2023.08.02.03]
40. Giallonardo V, Sampogna G, Del Vecchio V, Luciano M, Albert U, Carmassi C, et al. The impact of quarantine and physical distancing following COVID-19 on mental health: Study protocol of a multicentric italian population trial. Front Psychiatry. 2020;11:533. [Link] [DOI:10.3389/fpsyt.2020.00533]
41. Fan S, Guan J, Cao L, Wang M, Zhao H, Chen L, et al. Psychological effects caused by COVID-19 pandemic on pregnant women: A systematic review with meta-analysis. Asian J Psychiatr. 2021;56:102533. [Link] [DOI:10.1016/j.ajp.2020.102533]
42. Chivers BR, Garad RM, Boyle JA, Skouteris H, Teede HJ, Harrison CL. Perinatal distress during COVID-19: Thematic analysis of an online parenting forum. J Med Internet Res. 2020;22(9):e22002. [Link] [DOI:10.2196/22002]
43. Mimouni F, Lakshminrusimha S, Pearlman SA, Raju T, Gallagher PG, Mendlovic J. Perinatal aspects on the covid-19 pandemic: A practical resource for perinatal-neonatal specialists. J Perinatol. 2020;40(5):820-6. [Link] [DOI:10.1038/s41372-020-0665-6]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |