Volume 11, Issue 4 (2023)
Health Educ Health Promot 2023, 11(4): 635-640 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Barkati H, Rakhshanderou S, Mehrabi Y, Nikbakht Nasrabadi A, Hosseinzadeh H, Daneshvar S, et al . Psychological Determinants of Hand Hygiene Intentions and Behaviors of Nursing Staff Using the Theory of Planned Behavior. Health Educ Health Promot 2023; 11 (4) :635-640
URL: http://hehp.modares.ac.ir/article-5-71341-en.html
URL: http://hehp.modares.ac.ir/article-5-71341-en.html
H. Barkati1, S. Rakhshanderou2, Y. Mehrabi3, A. Nikbakht Nasrabadi4, H. Hosseinzadeh5, S. Daneshvar2, A. Safari-Moradabadi6, M. Ghaffari *2
1- Department of Community Health and Geriatric Nursing, School of Nursing & Midwifery, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3- “Department of Epidemiology, School of Public Health and Safety” and “Endocrine Research Center, Research Institute for Endocrine Sciences”, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4- “Department of Medical-Surgical Nursing and Basic Sciences, School of Nursing & Midwifery” and “Brain and Spinal Cord Injury Research Center, Neuroscience Institute”, Tehran University of Medical Sciences, Tehran, Iran
5- Department of Health Promotion, School of Health and Society, University of Wollongong, Wollongong, Australia
6- Department of Health Promotion and Education, School of Health, Alborz University of Medical Sciences, Tehran, Iran
2- Department of Public Health, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3- “Department of Epidemiology, School of Public Health and Safety” and “Endocrine Research Center, Research Institute for Endocrine Sciences”, Shahid Beheshti University of Medical Sciences, Tehran, Iran
4- “Department of Medical-Surgical Nursing and Basic Sciences, School of Nursing & Midwifery” and “Brain and Spinal Cord Injury Research Center, Neuroscience Institute”, Tehran University of Medical Sciences, Tehran, Iran
5- Department of Health Promotion, School of Health and Society, University of Wollongong, Wollongong, Australia
6- Department of Health Promotion and Education, School of Health, Alborz University of Medical Sciences, Tehran, Iran
Full-Text [PDF 607 kb]
(3098 Downloads)
| Abstract (HTML) (1420 Views)
Full-Text: (267 Views)
Introduction
Hand hygiene is the simplest and most effective measure for preventing healthcare-associated infections (HAIs) [1, 2]. Hand hygiene, which includes washing hands, using alcohol-based hand sanitizers, and changing gloves when examining different parts of the patient's body, is essential to prevent the spread of nosocomial infections [3]. Improving hand hygiene among healthcare workers is an essential measure to reduce the risk of nosocomial infections in hospitals. High compliance rates of hand hygiene practice assist in the significant cost of healthcare-associated infections on patient health and the economic burden on healthcare systems [2].
In 2009, the World Health Organization (WHO) adopted new global hand hygiene guidelines that included compliance with the five critical moments for hand hygiene in patient care, which Hand Hygiene Australia [4] has specifically identified as: before touching a patient (Moment 1), before a procedure (Moment 2), after a procedure (Moment 3), after touching a patient (Moment 4), and after touching a patient’s surroundings (Moment 5).
Despite the simplicity of this procedure and advances made in infection control, hospital healthcare workers’ compliance with hand hygiene recommendations is generally low [5, 6]. According to investigations conducted by WHO, physicians and nurses, adhere to hand hygiene in less than 50% of cases. In busy hospitals, hand hygiene is only observed in 10% of required cases [7]. In general, reviewing previous studies related to adherence to hygienic protocols shows that hand Hygiene in special care units (30-40%) is less observed than in other units (50-60%). In addition, adherence rates of 32% and 48% have been consequently reported for physicians and nurses, respectively. Previous studies have also reported the efficiency of hand hygiene before making contact with the patient as 45% [6].
In the proper observance of hand hygiene, there are many determinative factors, such as belief, attitude, personnel awareness of the relationship between hand microorganisms and increased hospital infection, awareness of how to observe the effectiveness of hand hygiene, the role of superiors’ visions concerning hygiene, the presence of a colleague or supervisor as a role model in observing hand hygiene, access and availability of hand rub, and the number of patients and human resources [8-10].
Also, studies have shown that compliance with hand hygiene guidelines is inadequate and remains suboptimal even after interventions to improve compliance [6]. Therefore, significant effort has been expended to understand the factors underlying hand hygiene behaviors, particularly as the WHO has called for more theory-informed research to support the design of more effective interventions [11].
Theories result in guidance and improvement of the performance of healthcare instructors and can be used during the planning, execution, and or evaluation phases of a program [12]. The theory of planned behavior (TPB) evaluates the predictors of healthcare-related behaviors [13]. So far, various studies have been conducted on the clinical behaviors of health sector employees, including following guidelines, prescribing different drugs, including antibiotics, and observing hand hygiene using this theory [14-16].
TPB is a cognitive theory proposed by Ajzen and Fishbeen (1988). It is a subset of cognitive theories and based on current evidence, it is one of the most applied theories in the domain of anticipation or prediction of behavior of healthcare practitioners [17].
TPB proposes that an individual’s behavior is driven by behavior intentions, which are determined by individuals’ attitudes toward a given behavior and subjective norms as well as perceived behavioral control. Behavioral intention is used as a proxy for behavior and indicates an individual’s motivation to perform a certain behavior. Attitude toward behavior represents an individual’s positive or negative feelings toward a certain behavior. Subjective norm requires a person's perception of the social environment, which shows whether important people approve of his behavior or not. Perceived behavioral control refers to an individual’s perception of his/her resources and confidence to perform a behavior [18, 19].
Regarding the great importance of adherence to hand hygiene among healthcare practitioners, reviewing previous documents shows that only a few limited studies have been performed in Iran to investigate hand hygiene behavior among practitioners of healthcare. Also, concerning the intention for designing theory-based interventions and the necessity of recognition of determinants at the initiation of every phase, and considering the fitness of TPB for the subject of hand hygiene, the aim of this study was to use the TPB to identify predictors of hand hygiene intentions and behaviors of nurses. The results of this study can have implications in designing infection rate reduction interventions, propagation of adherence to hand hygiene in healthcare systems, and persuasion of practitioners toward adherence to hand hygiene principles.
Materials and Methods
This cross-sectional study was conducted in Tehran on working nurses in public hospitals of Tehran University of Medical Sciences. The sample size was calculated by Cochran's formula (Z=1.96, P=0.05, and d=0.07). In total, 196 nurses were enrolled in this study and selected through random sampling.
Inclusion criteria included the willingness to participate in the study and the group of nurses who have been employed for more than one year. Exclusion criteria included unwillingness to continue attending the study and less than one year of work experience.
Data collection tools included a researcher-made questionnaire based on TPB and included variables of attitude, subjective norms, perceived behavioral control, intention, and behavior. Attitude, subjective norms, and perceived behavioral control sections included 14, 24, and 6 questions, respectively, and the intention section included five questions according to a five-point Likert scale. Nonetheless, the section on behavior also adopted the same five-point Likert scale. The questionnaire included also 11 demographic questions.
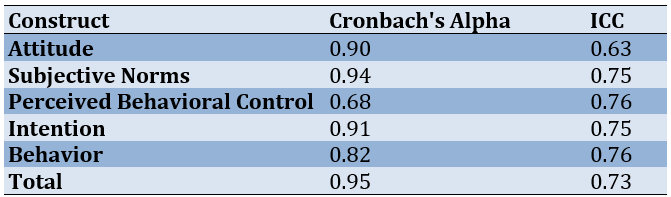
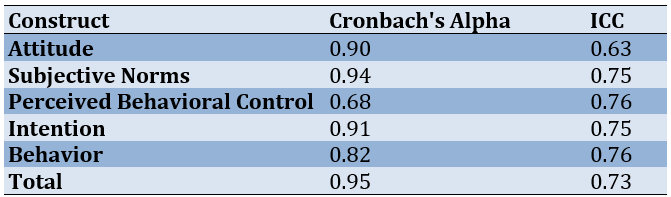
The validity of the questionnaire was confirmed by face and content validity methods and using the ideas of scholars and professors. For face validity, 40 nurses were provided with the questionnaire to assess ambiguity, relativity, proper terms, and grammar of items. For content validity, questions were given to 14 specialists in health education and health promotion, nursing, social medicine, and vital statistics. The content validity ratio (CVR) of the instrument was calculated as 0.57-1.0. Also, the content validity index (CVI) was obtained as 0.9-1 (average scale CVI=0.95). These values showed a suitable content validity of the tool. In addition, the test-retest method and internal consistency were used to determine the reliability of the questionnaire, which was also found to be sufficient (Table 1).
Table 1. Internal consistency and intraclass correlation coefficient (ICC) of the theory of planned behavior (TPB)-based questionnaire (n=40)
In order to obtain the required permissions, the authors contacted the hospitals. Two hospitals were randomly selected from the hospitals affiliated with the Tehran University of Medical Sciences. Afterward, the questionnaires were distributed among the samples. After collecting the inventories back, the driven data were subjected to statistical analyses using SPSS 16 software and statistical tests, including multiple regression analysis. In order to investigate the predictors of intention for hand hygienic behavior, we used multiple regression analysis in a stepwise manner. The variable of behavioral intention was fed to the regression equation as the dependent variable and then, the effects of other variables were evaluated on it. Also, to investigate the predictors of hand hygienic behavior, we used multiple regression analysis in a stepwise manner. In this regard, the variable of hand washing behavior was fed to the regression equation as the dependent variable and afterward, the effects of other variables were evaluated on it.
Findings
The mean age of respondents was 34.76±7.48 years with S a range of 20-50 years. Also, 85.7% of the respondents were females and most participants had an undergraduate degree and were married. The demographic characteristics of the participants are presented in Table 2.
Table 2. Frequency of demographic characteristics
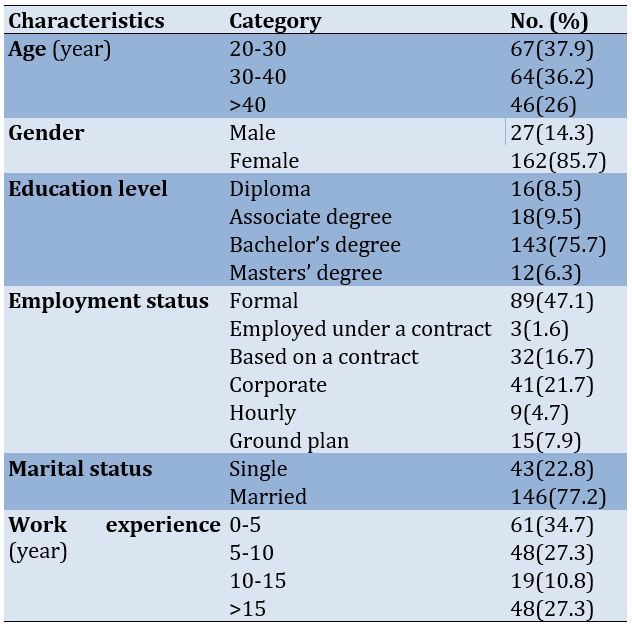
Table 3 shows the correlation between the constructs of TPB regarding adherence to hand hygiene. A significant and positive correlation was observed between the constructs of attitude, subjective norms, perceived behavioral control, and behavioral intention and hand hygiene behavior (p<0.001).
Table 3. Correlation between the constructs of the theory of planned behavior (TPB) and hand hygiene behavior (all correlations were significant at p<0.01)
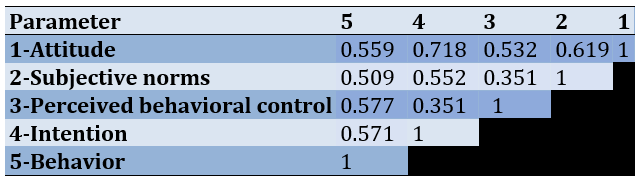
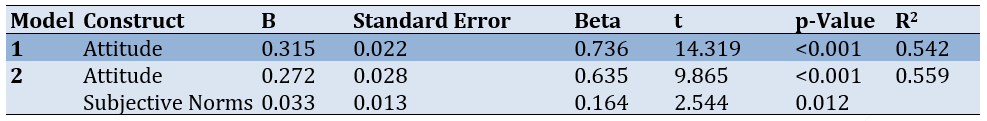
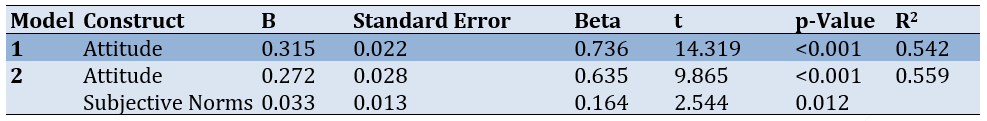
Table 4 shows that attitude (p<0.001) and subjective norms (p=0.012) are the predictors of behavioral intention, which together determined 56% of the total variance. On the other hand, attitude toward hand hygiene was identified as the strongest predictor of intention for adherence to hand hygiene in the TPB.
Table 4. Relationship between the theory of planned behavior (TPB) constructs and behavioral intention using regression analysis
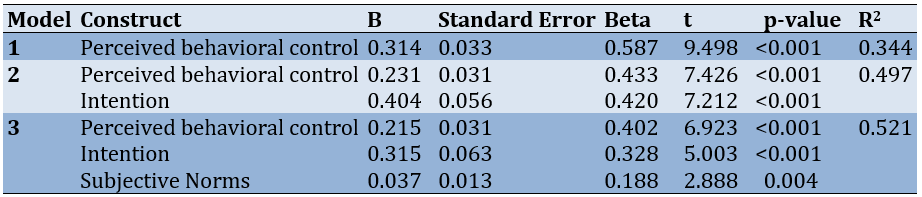
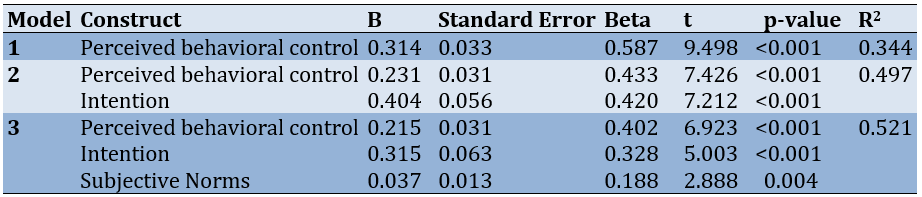
As seen in Table 5, the constructs of behavioral intention, perceived behavioral control, and subjective norms were the predictors of hand hygiene behavior, which together determined 52% of the total variance. In the first regression model, the variable of perceived behavioral control was able to anticipate 0.34% of the total variance. Based on three regression models and especially according to model 3, the constructs of perceived behavioral control (β=0.402) and subjective norms (β=0.188) were considered the strongest and the weakest predictors of hand hygiene behavior, respectively.
Table5. Relationship between the theory of planned behavior (TPB) constructs and behavioral intention using regression analysis
Discussion
Hand hygiene is very important to reduce healthcare-associated infections, but hand hygiene compliance is often low [20]. However, it seems necessary to study the factors affecting hand hygiene. Also, considering the role of nurses in preventing hospital infections and their direct relationship with patients, the purpose of this study was to use the theory of planned behavior to identify predictors of nurses' hand hygiene intentions and behaviors.
Our results showed that attitude toward hand washing and subjective norms were the strongest predictors for behavior intention, of which attitude had a higher predictability power. This result is consistent with that of Sin and Rochelle who used the TPB to explain hand washing among nurses [21]. In addition, McLaws et al. [22] and Wollast et al. [23] showed attitude and intention as the strongest predictors.
If the hospital staff has a positive attitude toward hand hygiene, and on the other hand, people who are important to them (including colleagues, the hospital director, supervisor, family, etc.) accept hand hygiene, they will show more serious intentions than adopting it.
Perceived behavioral control refers to the degree of simplicity or difficulty and investigates the current states and statuses of the person [24]. The results of this study showed that perceived behavioral control was significantly and positively related to hand hygiene behavior through intentions. The study performed by Luszczynska et al. titled "Predictors of asking healthcare practitioners about washing hands: Monitoring role of patients in the condition of MRSA infection" was conducted among 171 individuals. This research reported belief in the ability to control behavior and intention as the best predictor [25].
Among other results of this research, it can be referred to the point that among the different models, perceived behavioral control was the strongest predictor of behavior. In several studies, perceived behavioral control has been considered as the predictor of behavior in terms of adherence to hand hygiene. For example, Nicol et al. reported perceived behavioral control as the boldest phenomenon for helping understand the relations between the multiplicity of effects and intentional factors resulting from analyses. This research determined that control or self-efficacy, which is defined as belief in perceived simplicity or difficulty of performance is one of the strongest predictors of behavior [26].
Hugonnet et al. conducted a large-scale study on the determinants of favorable hand hygiene with 2,961 healthcare workers. This study found that pressure from friends and a high understanding of self-efficacy were respectively more effective than reasoning about the effect of hand hygiene on the safety of patients [27].
In some situations, prevention of crowdedness of care units can be effective. Therefore, it is recommended to enforce the required interventions for the removal of barriers to the occurrence of intended hygienic behaviors in order to be able to observe a higher rate of adherence to hand hygienic behavior.
Among the limitations of this study, it can be referred to the gender distribution of the research, as most participants were female and only a few male subjects responded to the questionnaires. Also, using self-report questionnaires was another limitation of the present study. Another issue that could limit the findings of this research is that only hospitals of Tehran University of Medical Sciences were considered because of their accessibility to the research team. The results could not be generalized to all hospitals in Tehran.
Conclusion
The constructs of the TPB have predictability regarding hand hygiene behavior. Specially, among these constructs, perceived behavioral control is of great importance. It is recommended to design and implement health education and health promotion interventions with regard to the important effects, especially the constructs of the TPB among nurses and other healthcare-related practitioners.
Acknowledgments: This paper was extracted from a PhD thesis on Health Education & Health Promotion. The authors thank all nursing staff who participated in the present study.
Ethical Permissions: Required permissions were obtained from the Vice-Chancellor of Research Affairs of the university for entering healthcare centers. In addition, the samples were assured that questionnaires were anonymous and would be analyzed in groups rather than in person. Furthermore, the purpose and nature of the study were explained to hospital authorities in detail. This paper was approved and supported as a research project by the Environmental and Occupational Hazards Control Research Center at Shahid Beheshti University of Medical Sciences, Tehran, Iran (SBMU.RAM.REC.1394.540).
Author’s Contribution: Barkati H (First Author) Main researcher/Introduction Writer (20%); Rakhshanderou S (Second Author) Statistical analysis/Methodology (10%); Mehrabi Y (Third Author) Statistical Analyst/Methodologist (10%); Nikbakht Nasrabadi A (Fourth Author) Introduction Writer/Statistical Analyst (10%); Hosseinzadeh H (Fifth Author) Methodologist/Discussion Writer/Statistical Analyst (10%); Daneshvar S (Sixth Author) Discussion Writer/Assistant Researcher/Statistical Analyst (10%); Safari-Moradabadi A (Seventh Author) Discussion Writer/Introduction Writer/Assistant Researcher/Statistical Analyst (10%); Ghaffari M (Eighth Author) Main Researcher/Methodologist/Discussion Writer (20%)
Conflicts of Interests: No potential conflicts of interests were reported.
Funding/Support: None.
Hand hygiene is the simplest and most effective measure for preventing healthcare-associated infections (HAIs) [1, 2]. Hand hygiene, which includes washing hands, using alcohol-based hand sanitizers, and changing gloves when examining different parts of the patient's body, is essential to prevent the spread of nosocomial infections [3]. Improving hand hygiene among healthcare workers is an essential measure to reduce the risk of nosocomial infections in hospitals. High compliance rates of hand hygiene practice assist in the significant cost of healthcare-associated infections on patient health and the economic burden on healthcare systems [2].
In 2009, the World Health Organization (WHO) adopted new global hand hygiene guidelines that included compliance with the five critical moments for hand hygiene in patient care, which Hand Hygiene Australia [4] has specifically identified as: before touching a patient (Moment 1), before a procedure (Moment 2), after a procedure (Moment 3), after touching a patient (Moment 4), and after touching a patient’s surroundings (Moment 5).
Despite the simplicity of this procedure and advances made in infection control, hospital healthcare workers’ compliance with hand hygiene recommendations is generally low [5, 6]. According to investigations conducted by WHO, physicians and nurses, adhere to hand hygiene in less than 50% of cases. In busy hospitals, hand hygiene is only observed in 10% of required cases [7]. In general, reviewing previous studies related to adherence to hygienic protocols shows that hand Hygiene in special care units (30-40%) is less observed than in other units (50-60%). In addition, adherence rates of 32% and 48% have been consequently reported for physicians and nurses, respectively. Previous studies have also reported the efficiency of hand hygiene before making contact with the patient as 45% [6].
In the proper observance of hand hygiene, there are many determinative factors, such as belief, attitude, personnel awareness of the relationship between hand microorganisms and increased hospital infection, awareness of how to observe the effectiveness of hand hygiene, the role of superiors’ visions concerning hygiene, the presence of a colleague or supervisor as a role model in observing hand hygiene, access and availability of hand rub, and the number of patients and human resources [8-10].
Also, studies have shown that compliance with hand hygiene guidelines is inadequate and remains suboptimal even after interventions to improve compliance [6]. Therefore, significant effort has been expended to understand the factors underlying hand hygiene behaviors, particularly as the WHO has called for more theory-informed research to support the design of more effective interventions [11].
Theories result in guidance and improvement of the performance of healthcare instructors and can be used during the planning, execution, and or evaluation phases of a program [12]. The theory of planned behavior (TPB) evaluates the predictors of healthcare-related behaviors [13]. So far, various studies have been conducted on the clinical behaviors of health sector employees, including following guidelines, prescribing different drugs, including antibiotics, and observing hand hygiene using this theory [14-16].
TPB is a cognitive theory proposed by Ajzen and Fishbeen (1988). It is a subset of cognitive theories and based on current evidence, it is one of the most applied theories in the domain of anticipation or prediction of behavior of healthcare practitioners [17].
TPB proposes that an individual’s behavior is driven by behavior intentions, which are determined by individuals’ attitudes toward a given behavior and subjective norms as well as perceived behavioral control. Behavioral intention is used as a proxy for behavior and indicates an individual’s motivation to perform a certain behavior. Attitude toward behavior represents an individual’s positive or negative feelings toward a certain behavior. Subjective norm requires a person's perception of the social environment, which shows whether important people approve of his behavior or not. Perceived behavioral control refers to an individual’s perception of his/her resources and confidence to perform a behavior [18, 19].
Regarding the great importance of adherence to hand hygiene among healthcare practitioners, reviewing previous documents shows that only a few limited studies have been performed in Iran to investigate hand hygiene behavior among practitioners of healthcare. Also, concerning the intention for designing theory-based interventions and the necessity of recognition of determinants at the initiation of every phase, and considering the fitness of TPB for the subject of hand hygiene, the aim of this study was to use the TPB to identify predictors of hand hygiene intentions and behaviors of nurses. The results of this study can have implications in designing infection rate reduction interventions, propagation of adherence to hand hygiene in healthcare systems, and persuasion of practitioners toward adherence to hand hygiene principles.
Materials and Methods
This cross-sectional study was conducted in Tehran on working nurses in public hospitals of Tehran University of Medical Sciences. The sample size was calculated by Cochran's formula (Z=1.96, P=0.05, and d=0.07). In total, 196 nurses were enrolled in this study and selected through random sampling.
Inclusion criteria included the willingness to participate in the study and the group of nurses who have been employed for more than one year. Exclusion criteria included unwillingness to continue attending the study and less than one year of work experience.
Data collection tools included a researcher-made questionnaire based on TPB and included variables of attitude, subjective norms, perceived behavioral control, intention, and behavior. Attitude, subjective norms, and perceived behavioral control sections included 14, 24, and 6 questions, respectively, and the intention section included five questions according to a five-point Likert scale. Nonetheless, the section on behavior also adopted the same five-point Likert scale. The questionnaire included also 11 demographic questions.
The validity of the questionnaire was confirmed by face and content validity methods and using the ideas of scholars and professors. For face validity, 40 nurses were provided with the questionnaire to assess ambiguity, relativity, proper terms, and grammar of items. For content validity, questions were given to 14 specialists in health education and health promotion, nursing, social medicine, and vital statistics. The content validity ratio (CVR) of the instrument was calculated as 0.57-1.0. Also, the content validity index (CVI) was obtained as 0.9-1 (average scale CVI=0.95). These values showed a suitable content validity of the tool. In addition, the test-retest method and internal consistency were used to determine the reliability of the questionnaire, which was also found to be sufficient (Table 1).
Table 1. Internal consistency and intraclass correlation coefficient (ICC) of the theory of planned behavior (TPB)-based questionnaire (n=40)
In order to obtain the required permissions, the authors contacted the hospitals. Two hospitals were randomly selected from the hospitals affiliated with the Tehran University of Medical Sciences. Afterward, the questionnaires were distributed among the samples. After collecting the inventories back, the driven data were subjected to statistical analyses using SPSS 16 software and statistical tests, including multiple regression analysis. In order to investigate the predictors of intention for hand hygienic behavior, we used multiple regression analysis in a stepwise manner. The variable of behavioral intention was fed to the regression equation as the dependent variable and then, the effects of other variables were evaluated on it. Also, to investigate the predictors of hand hygienic behavior, we used multiple regression analysis in a stepwise manner. In this regard, the variable of hand washing behavior was fed to the regression equation as the dependent variable and afterward, the effects of other variables were evaluated on it.
Findings
The mean age of respondents was 34.76±7.48 years with S a range of 20-50 years. Also, 85.7% of the respondents were females and most participants had an undergraduate degree and were married. The demographic characteristics of the participants are presented in Table 2.
Table 2. Frequency of demographic characteristics
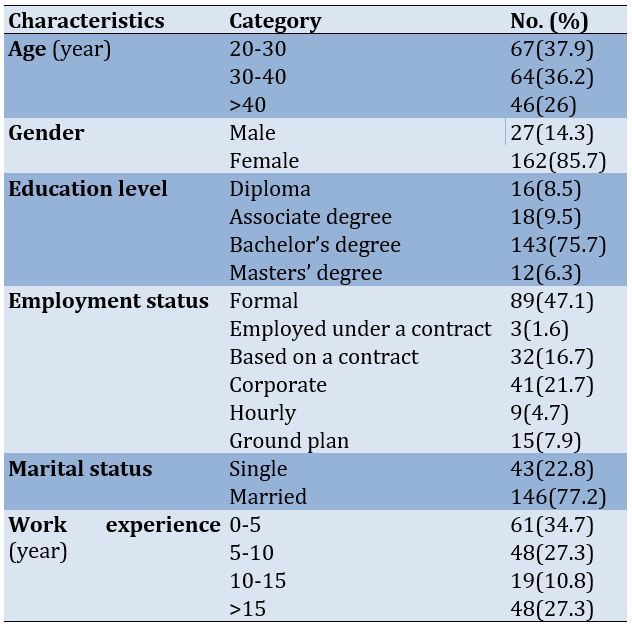
Table 3 shows the correlation between the constructs of TPB regarding adherence to hand hygiene. A significant and positive correlation was observed between the constructs of attitude, subjective norms, perceived behavioral control, and behavioral intention and hand hygiene behavior (p<0.001).
Table 3. Correlation between the constructs of the theory of planned behavior (TPB) and hand hygiene behavior (all correlations were significant at p<0.01)
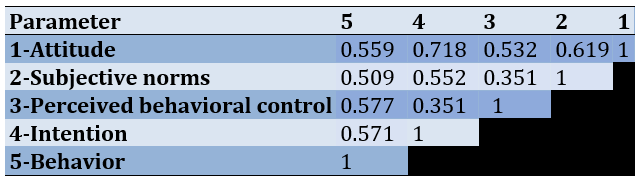
Table 4 shows that attitude (p<0.001) and subjective norms (p=0.012) are the predictors of behavioral intention, which together determined 56% of the total variance. On the other hand, attitude toward hand hygiene was identified as the strongest predictor of intention for adherence to hand hygiene in the TPB.
Table 4. Relationship between the theory of planned behavior (TPB) constructs and behavioral intention using regression analysis
As seen in Table 5, the constructs of behavioral intention, perceived behavioral control, and subjective norms were the predictors of hand hygiene behavior, which together determined 52% of the total variance. In the first regression model, the variable of perceived behavioral control was able to anticipate 0.34% of the total variance. Based on three regression models and especially according to model 3, the constructs of perceived behavioral control (β=0.402) and subjective norms (β=0.188) were considered the strongest and the weakest predictors of hand hygiene behavior, respectively.
Table5. Relationship between the theory of planned behavior (TPB) constructs and behavioral intention using regression analysis
Discussion
Hand hygiene is very important to reduce healthcare-associated infections, but hand hygiene compliance is often low [20]. However, it seems necessary to study the factors affecting hand hygiene. Also, considering the role of nurses in preventing hospital infections and their direct relationship with patients, the purpose of this study was to use the theory of planned behavior to identify predictors of nurses' hand hygiene intentions and behaviors.
Our results showed that attitude toward hand washing and subjective norms were the strongest predictors for behavior intention, of which attitude had a higher predictability power. This result is consistent with that of Sin and Rochelle who used the TPB to explain hand washing among nurses [21]. In addition, McLaws et al. [22] and Wollast et al. [23] showed attitude and intention as the strongest predictors.
If the hospital staff has a positive attitude toward hand hygiene, and on the other hand, people who are important to them (including colleagues, the hospital director, supervisor, family, etc.) accept hand hygiene, they will show more serious intentions than adopting it.
Perceived behavioral control refers to the degree of simplicity or difficulty and investigates the current states and statuses of the person [24]. The results of this study showed that perceived behavioral control was significantly and positively related to hand hygiene behavior through intentions. The study performed by Luszczynska et al. titled "Predictors of asking healthcare practitioners about washing hands: Monitoring role of patients in the condition of MRSA infection" was conducted among 171 individuals. This research reported belief in the ability to control behavior and intention as the best predictor [25].
Among other results of this research, it can be referred to the point that among the different models, perceived behavioral control was the strongest predictor of behavior. In several studies, perceived behavioral control has been considered as the predictor of behavior in terms of adherence to hand hygiene. For example, Nicol et al. reported perceived behavioral control as the boldest phenomenon for helping understand the relations between the multiplicity of effects and intentional factors resulting from analyses. This research determined that control or self-efficacy, which is defined as belief in perceived simplicity or difficulty of performance is one of the strongest predictors of behavior [26].
Hugonnet et al. conducted a large-scale study on the determinants of favorable hand hygiene with 2,961 healthcare workers. This study found that pressure from friends and a high understanding of self-efficacy were respectively more effective than reasoning about the effect of hand hygiene on the safety of patients [27].
In some situations, prevention of crowdedness of care units can be effective. Therefore, it is recommended to enforce the required interventions for the removal of barriers to the occurrence of intended hygienic behaviors in order to be able to observe a higher rate of adherence to hand hygienic behavior.
Among the limitations of this study, it can be referred to the gender distribution of the research, as most participants were female and only a few male subjects responded to the questionnaires. Also, using self-report questionnaires was another limitation of the present study. Another issue that could limit the findings of this research is that only hospitals of Tehran University of Medical Sciences were considered because of their accessibility to the research team. The results could not be generalized to all hospitals in Tehran.
Conclusion
The constructs of the TPB have predictability regarding hand hygiene behavior. Specially, among these constructs, perceived behavioral control is of great importance. It is recommended to design and implement health education and health promotion interventions with regard to the important effects, especially the constructs of the TPB among nurses and other healthcare-related practitioners.
Acknowledgments: This paper was extracted from a PhD thesis on Health Education & Health Promotion. The authors thank all nursing staff who participated in the present study.
Ethical Permissions: Required permissions were obtained from the Vice-Chancellor of Research Affairs of the university for entering healthcare centers. In addition, the samples were assured that questionnaires were anonymous and would be analyzed in groups rather than in person. Furthermore, the purpose and nature of the study were explained to hospital authorities in detail. This paper was approved and supported as a research project by the Environmental and Occupational Hazards Control Research Center at Shahid Beheshti University of Medical Sciences, Tehran, Iran (SBMU.RAM.REC.1394.540).
Author’s Contribution: Barkati H (First Author) Main researcher/Introduction Writer (20%); Rakhshanderou S (Second Author) Statistical analysis/Methodology (10%); Mehrabi Y (Third Author) Statistical Analyst/Methodologist (10%); Nikbakht Nasrabadi A (Fourth Author) Introduction Writer/Statistical Analyst (10%); Hosseinzadeh H (Fifth Author) Methodologist/Discussion Writer/Statistical Analyst (10%); Daneshvar S (Sixth Author) Discussion Writer/Assistant Researcher/Statistical Analyst (10%); Safari-Moradabadi A (Seventh Author) Discussion Writer/Introduction Writer/Assistant Researcher/Statistical Analyst (10%); Ghaffari M (Eighth Author) Main Researcher/Methodologist/Discussion Writer (20%)
Conflicts of Interests: No potential conflicts of interests were reported.
Funding/Support: None.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2023/09/1 | Accepted: 2023/11/8 | Published: 2023/11/16
Received: 2023/09/1 | Accepted: 2023/11/8 | Published: 2023/11/16
References
1. Sands M, Aunger R. Determinants of hand hygiene compliance among nurses in US hospitals: A formative research study. PLOS One. 2020;15(4):e0230573. [Link] [DOI:10.1371/journal.pone.0230573]
2. World Health Organization. WHO guidelines in hand hygiene in health care. Geneva: WHO Press: 2009. [Link]
3. Samraj S, Westbury J, Pallett A, Rowen D. Compliance with hand hygiene in a genitourinary medicine department. Int J STD AIDS. 2008;19(11):782-3. [Link] [DOI:10.1258/ijsa.2008.008183]
4. Hand Hygiene Australia. 5 moments for hand hygiene [Internet]. Melbourne: Hand Hygiene Australia. 2014- [cited 2023 Jan 16]. Available from: http://www.hha.org.au/home/5-moments-for-hand-hygiene.aspx. [Link]
5. Sharma S, Sharma S, Puri S, Whig J. Hand hygiene compliance in the intensive care units of a tertiary care hospital. Indian J Community Med. 2011;36(3):217-21. [Link] [DOI:10.4103/0970-0218.86524]
6. Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31(3):283-94. [Link] [DOI:10.1086/650451]
7. Zahraei M, Pezeshki P. Surveillance Guideline in Promotion of Hand Hygiene. 1th ed. Tehran: Center Of Disease Management; 2010. [Link]
8. Haenen A, de Greeff S, Voss A, Liefers J, Hulscher M, Huis A. Hand hygiene compliance and its drivers in long-term care facilities; observations and a survey. Antimicrob Resist Infect Control. 2022;11(1):50. [Link] [DOI:10.1186/s13756-022-01088-w]
9. Handiyani H, Ikegawa M, Hariyati RTS, Ito M, Amirulloh F. The determinant factor of nurse's hand hygiene adherence in Indonesia. Enfermeria Clin. 2019;29:257-61. [Link] [DOI:10.1016/j.enfcli.2019.04.031]
10. Engdaw GT, Gebrehiwot M, Andualem Z. Hand hygiene compliance and associated factors among health care providers in Central Gondar zone public primary hospitals, Northwest Ethiopia. Antimicrobial Resist Infect Control. 2019;8(1):190. [Link] [DOI:10.1186/s13756-019-0634-z]
11. World Health Organization. Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level [Internet]. Geneva: WHO. 2016- [cited 2023 Jan 16]. Available from: https://www.who.int/gpsc/core. [Link]
12. Ikeda S, Tokuda K, Kanamori H, Hirai Y, Endo S, Kunishima H, et al. Hand hygiene compliance among nurses in a Japanese tertiary hospital emergency department. Antimicrob Resist Infect Control. 2013;2(Suppl 1):P119. [Link] [DOI:10.1186/2047-2994-2-S1-P119]
13. Masomi-e-Asl H, Zahraei SM, Majidpour A, Nategian AR, Afhami Sh, Rahbar M, et al. National guideline of nosocomial infection surveillance. 2th ed.Tehran: Ministry of Health; 2007. [Persian] [Link]
14. Liu C, Liu C, Wang D, Deng Z, Tang Y, Zhang X. Determinants of antibiotic prescribing behaviors of primary care physicians in Hubei of China: a structural equation model based on the theory of planned behavior. Antimicrobial Resist Infect Control. 2019;8:23. [Link] [DOI:10.1186/s13756-019-0478-6]
15. White KM, Jimmieson NL, Obst PL, Graves N, Barnett A, Cockshaw W, et al. Using a theory of planned behaviour framework to explore hand hygiene beliefs at the '5 critical moments' among Australian hospital-based nurses. BMC Health Serv Res. 2015;15:59. [Link] [DOI:10.1186/s12913-015-0718-2]
16. Kortteisto T, Kaila M, Komulainen J, Mäntyranta T, Rissanen P. Healthcare professionals' intentions to use clinical guidelines: a survey using the theory of planned behaviour. Implementat Sci. 2010;5:51. [Link] [DOI:10.1186/1748-5908-5-51]
17. Guo R, Berkshire S, Fulton L, Hermanson P. Predicting intention to use evidence based management among U.S. healthcare administrators: Application of the theory of planned behavior and structural equation modeling. Int J Healthc Manag. 2017;12(1):32-25. [Link] [DOI:10.1080/20479700.2017.1336856]
18. Ajzen I. The theory of planned behavior. Organization Behav Human Decision Proc. 1991;50(2):179-211. [Link] [DOI:10.1016/0749-5978(91)90020-T]
19. Madden TJ, Ellen PS, Ajzen I. A comparison of the theory of planned behavior and the theory of reasoned action. Personality Soc Psychol Bulletin. 1992;18(1). [Link] [DOI:10.1177/0146167292181001]
20. Sadeghi L, Khodadadi E, Sadeghi R, Mansour Bavani S, Almasi KH, Fooladi M. Investigating the factors affecting on hand hygiene compliance from the viewpoints of Iranian nurses who working in intensive care units. J Res Med Dental Sci. 2018;6(5):93-8. [Link]
21. Sin CS, Rochelle TL. Using the theory of planned behaviour to explain hand hygiene among nurses in Hong Kong during COVID-19. J Hosp Infect. 2022;123:119-25. [Link] [DOI:10.1016/j.jhin.2022.01.018]
22. McLaws ML, Maharlouei N, Yousefi F, Askarian M. Predicting hand hygiene among Iranian health care workers using the theory of planned behavior. Am J Infect Control. 2012;40(4):336-9. [Link] [DOI:10.1016/j.ajic.2011.04.004]
23. Wollast R, Schmitz M, Bigot A, Luminet O. The theory of planned Behavior during the COVID-19 pandemic: A comparison of health behaviors between Belgian and French residents. PLOS One. 2021;16(11):e0258320. [Link] [DOI:10.1371/journal.pone.0258320]
24. Safari MSD, Ghofranipour F, Heydarnia A, Pakpour A. Health education and promotion theories, models and methods. 2th ed. Tehran: Sobhan Pub; 2019. [Persian] [Link]
25. Luszczynska A, Gunson KS. Predictors of asking medical personnel about handwashing: the moderating role of patients' age and MRSA infection status. Patient Educ Counsel. 2007;68(1):79-85. [Link] [DOI:10.1016/j.pec.2007.05.008]
26. Nicol PW, Watkins RE, Donovan RJ, Wynaden D, Cadwallader H. The power of vivid experience in hand hygiene compliance. J Hosp Infect. 2009;72(1):36-42. [Link] [DOI:10.1016/j.jhin.2009.01.021]
27. Hugonnet S, Chevrolet JC, Pittet D. The effect of workload on infection risk in critically ill patients. Crit Care Med. 2007;35(1):76-81. [Link] [DOI:10.1097/01.CCM.0000251125.08629.3F]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







