Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 805-812 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi E, Pournamdar Z, Vahedparast H, Kazemnejad A. Effect of the Continuity Self-Preservation Model on Compliance with the Care-treatment Regimen and Its Consequences in Patients with Type 2 Diabetes. Health Educ Health Promot 2022; 10 (4) :805-812
URL: http://hehp.modares.ac.ir/article-5-65226-en.html
URL: http://hehp.modares.ac.ir/article-5-65226-en.html
1- Department of Nursing, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran
3- Department of Biostatistics, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
Keywords: Self Care [MeSH], Diabetes Type 2 [MeSH], Treatment Adherence and Compliance [MeSH], Quality of Life [MeSH]
Full-Text [PDF 1826 kb]
(856 Downloads)
| Abstract (HTML) (1385 Views)
Table 2) Comparison of the mean variables in the two groups before, 1, 3 and 6 months after the intervention

Table 3) Results of repeated measures analysis of variance in the two groups at different stages of the intervention

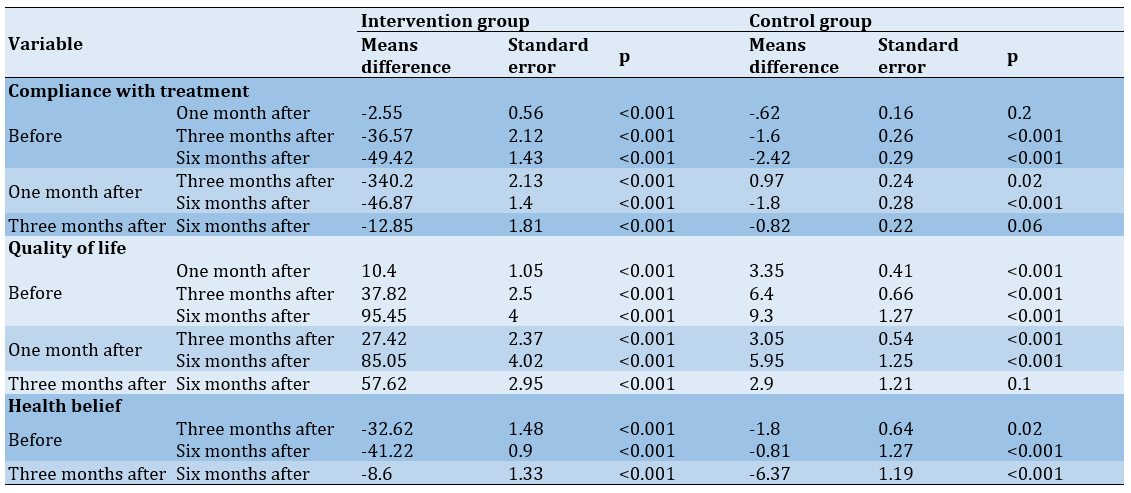
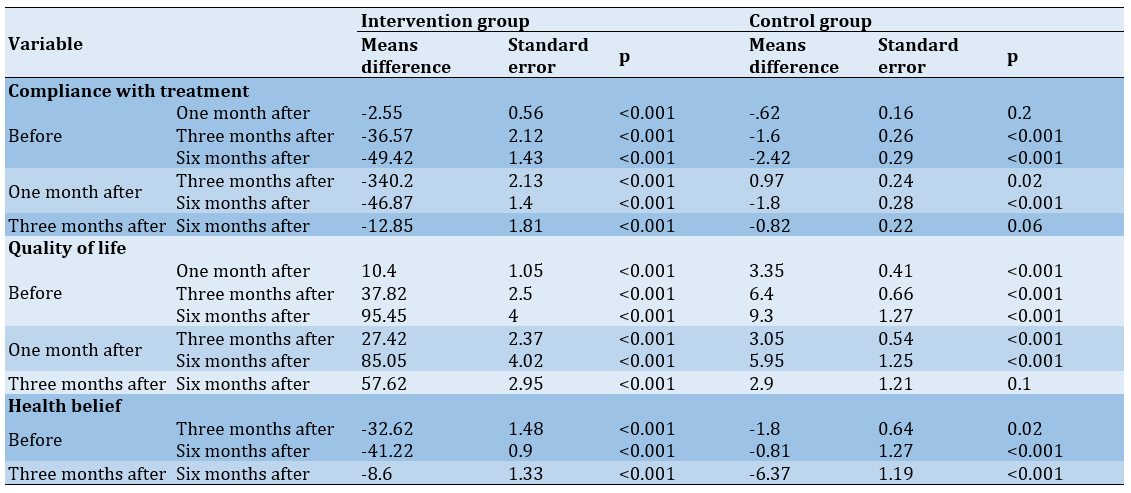
Table 4) Examining the differences in scores of compliance with treatment, quality of life and health beliefs in intervention and control groups in 4 stages using Bonferroni post hoc test
Full-Text: (287 Views)
Introduction
Diabetes mellitus is one of the most important metabolic diseases worldwide by an alarming prevalence, which has increased by 50% over the past 10 years [1]. The global prevalence of diabetes in 2019 was 9.3% (463 million people) which it is estimated to reach 10.2% (578 million people) in 2030 and 10.9% (700 million people) by 2045 [2]. In a study conducted from 2014 to 2020 on participants aged 35 to 70 years among different Iranian races, 15% of the adult population were diabetic, and more than 25% of them were pre-diabetic [2].
Diabetes patients often do not follow their treatment plan, which makes blood sugar management challenging [3]. The interplay of numerous elements or dimensions determines treatment adherence, which is a multidimensional phenomenon [4]. The ultimate goal of any recommended treatment is to achieve the desired outcome for the patient. While despite all the attention and efforts made by the healthcare team, if the patient does not adhere to the treatment, this will not be achieved [5].
Despite the scientific efforts and application of various theories and programs of professional interventions, nursing, and non-nursing, it has been reported that there is still a lack of adherence, as a challenge and problem, to control chronic diseases, which is a major expanding obstacle to achieving therapeutic goals. On the other hand, although non-compliance is a universal phenomenon, it does not have a fixed, common, and equal nature, as it is unique for individuals and social and is a completely contextual phenomenon, and even has a different nature and function in different diseases and patients, so that it cannot be explained and addressed by fixed and uniform theory, model or formula and program all over the world [3].
Thus, Vahedparast [6] conducted a study to design an effective model and intervention based on this model to promote compliance with care-treatment regimens in the patient's social life. They developed an emergency-based self-protection approach in which patients with chronic illness used to live, which is the leading cause of noncompliance with care-treatment regimens among individuals with chronic diseases. Considering that most cases of this disease have no obvious symptoms or consequences, patients do not feel threatened. This fear is superficial and periodic, which could be the main identified root causes of hesitation and failure in accepting adjusted behaviors and failure to comply with care-treatment regimens. According to these findings, they designed and presented a “continuity of self-preservation model”. They argue that self-preservation is not static, but a dynamic process and should be initiated at the beginning of a person's awareness of their chronic illness and be accompanied by a conscious and active search for the patient and the support and participation of nurses and other health professionals in the process of compliance with care-treatment regimens, leading to the best behavior in line with care-treatment regimens compliance. This model introduces the idea of a mediator notion termed a motivator, which is crucial for sustaining behavioral stimulus and motivation. It is possible to identify and use the support resources of their living environment (spouse, family, supportive spouses, peers and role models, and care-treatment team) to further advance the process of continuing self-protection.
The ultimate goal of this model is to continue the self-preservation of individuals with chronic diseases in compliance with care-treatment regimens, and strategies to optimize and maintain the recommended regimens are presented [6]. Therefore, this research aimed to design and evaluate an intervention program to improve compliance with treatment in patients with diabetes (one of the most common chronic diseases) based on the self-preservation continuity model.
Materials and Methods
Study design
This study is a quasi-experimental clinical trial in which the study population was patients with type 2 diabetes admitted to the internal wards of two hospitals in Zahedan (Iran) from 2020 to 2021. Randomization was not possible due to the limited number of specific treatment centers for this disease (two centers).
Samples and research environment
The sample size was determined based on the findings of a prior research [7]. With a 95% confidence interval and a 95% test power, 40 individuals were identified for each group, totaling 80 individuals. One treatment center was selected as the research environment for the intervention group, and another center was selected for the control group. Inclusion criteria were as follows: having at least a compliance with the treatment-care regimen using a questionnaire and blood test, age of at least 30, access to smart phone for patient or informal caregiver (family).
Collecting data
Data collection tools in this study included the following:
Summary of Diabetes Self-Care Activities (SDSCA) Scale: This scale was first designed by Toobert and Glasgow, and then Toobert et al. [8] modified it. Numerous studies in different countries, including Iran, used this tool to examine the compliance with self-care behaviors and treatment regimen in patients with diabetes [7, 9-21].
This scale is an accurate 12-item self-report instrument that looks at five aspects of a diabetes treatment plan (diet, exercise, proper tablet intake, self-monitoring blood sugar levels, foot care, and smoking). This tool is scored on a seven-choice scale from 0 to 7. The total score on the scale is 0 to 77. A score of 0 to 22 is considered a poor score. The internal consistency method was used to calculate the reliability, and Cronbach's alpha for the self-care activity scale was 91%.
Diabetes – Mellitus Specific Quality Of Life (DMQOL): This questionnaire was first developed to assess health-related quality of life in patients with diabetes in Taiwan based on the World Health Organization Quality of Life Scale Brief Version (WHOQOL) [22]. Saffari et al. [23] translated it into Persian, and based on its psychometric properties, they concluded that it is an appropriate instrument for evaluating the quality of life of diabetic patients in Iran. This questionnaire has four dimensions, including Satisfaction with one's condition, the impact of diabetes on a person's life, concerns related to diabetes and social and occupational concerns. A higher score on this instrument, which bases its options on the Likert scale, implies more unhappiness with life quality [23]. The researcher evaluated the reliability of this questionnaire with Cronbach's alpha of 84%.
Diabetes Specific Health Beliefs Scale: This scale is used to assess the perceived sensitivity and severity of complications of diabetes. This tool was used by Sharifabad and Rouhani [24], which is a translation of the Lewis and Bradley Diabetes Specific Health Beliefs Scale. This scale contains 20 questions. The achievable score in these structures is from 0 to 40 [24]. Cronbach's alpha was estimated in the perceived sensitivity section as 85%, for the perceived severity section was 92%, and for the total questionnaire was 73%.
Glycosylated hemoglobin: Glycosylated hemoglobin levels in the patient were measured twice, before and after the intervention. In a regulated and certified laboratory, HbA1C was also determined using a specific test kit.
Procedure
Following obtaining the necessary permits, the researcher implemented the designed program (based on the model) to improve the cognitive structure of the nurses working in the ward.
The approach of cognitive structure improvement is performed in three dimensions: 1) health care providers (nurses), 2) patients, and 3) patients' families. In this regard, first, a training program for nurses working in the intervention group was held in 3 sessions. Nurses were asked to consider the issues raised during the hospitalization of patients in the ward, discharge time, and during education programs. Patients were sampled once the nurses had finished their training. Blood was drawn with the patient's permission to test for glycosylated hemoglobin. The patient's treatment compliance questionnaire was filled out, and based on the predetermined criteria, patient was assigned to either the intervention group or the control group. The purpose of this stage in the intervention group was to modify the cognitive structure of patients to keep them sensitive in symptomatic and asymptomatic conditions and to create sensitivity to the hidden long-term effects of diabetes (such as heart attacks, strokes, wounds, amputations, blindness, etc.). For this purpose, first, a WhatsApp group of participants in the intervention group was by the researcher.
During the research, at least two educational messages containing educational items on diabetes self-care in the areas of diet, physical activity, medication use, related complications to diabetes, and its management were sent to the group by the researcher daily. Furthermore, warning messages related to complications (text or video messages) were sent every day both in groups and individually to the participants to keep them alert and sensitive to continue. The development of self-preservation skills in patients is a dimension related to the modification of the cognitive structure in this model. So in the following stage, training materials, including information about diabetes and self-care activities for disease control were held separately for patients in the group. To improve the cognitive structure of the family (one of the dimensions of the self-protection model), virtual groups of caregivers were formed, and educational materials and messages were sent to this group. During this time, the control group, from another hospital, received routine care. To assess the effect of the intervention, the scales of diabetes-related self-care activities and quality of life was completed 1, 3, and 6 months after the intervention, and the Health Belief Questionnaire 3 and 6 months after the intervention was completed again for both groups. Moreover, a blood sample for HbA1C was taken 6 months after the intervention.
Statistical analysis
Descriptive statistics, Chi-square test, repeated measures analysis of variance, Bonferroni post hoc test, independent t-test, and paired t-test were all used to examine the data. Data analysis was performed using SPSS 9 software.
Findings
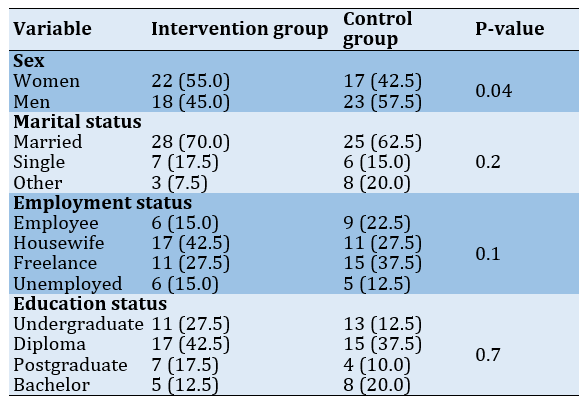
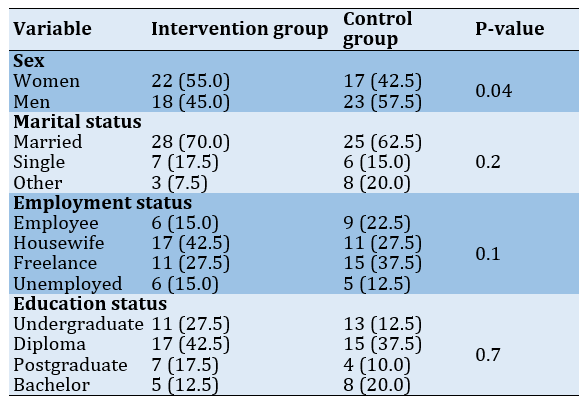
The mean age of the patients in the intervention and control groups was 46.17±10.44 and 47.02±8.6 years, respectively. The mean duration of diagnosis in the intervention and control groups was 7.6±4.6 and 8.1±3.5 years, respectively. There was no significant difference between the two groups before the intervention in age and disease duration (p>0.05). Also, there was no significant difference in the frequency distribution of the participants in terms of demographic characteristics in the intervention and control groups (Table 1).
Table 1) Comparison of frequency distribution of demographic variables in the intervention and control groups using chi-square test
Before the intervention, there was no significant difference between the two groups of intervention and control in the variables of compliance with treatment, quality of life, and health beliefs (p>0.05). However, one month after the intervention, there was a significant difference in the means of compliance with treatment in the two groups, and the score of compliance with treatment in the intervention group increased. The quality of life was also significantly impacted by this disparity. Although both groups' quality-of-life scores dropped (a lower score implies a higher quality of life), the intervention group's mean change was greater. On the other hand, the levels of treatment compliance, quality of life, and health beliefs significantly varied between the two groups three months and six months following the intervention. Compliance with treatment and health beliefs increased, and quality of life decreased (a lower score indicates a higher quality of life). The mean score of HbA1C in the two groups significantly reduced six months after the intervention. Moreover, the coefficient effect of 1.55 showed the high positive impact of the intervention (Table 2).
Besides, the inter-group and intra-group effects in different phases of the intervention are shown in Table 3. According to the results of an intergroup and intragroup analysis of variance with repeated measures of four measurements (before the intervention, 1, 3, and 6 months after the intervention) in the intervention and control groups, there was a significant difference in the factor scores, the groups' scores for treatment compliance, and the overall quality of life score (p<0.001). Repeated measurements of three measurements (before the intervention, 3, and 6 months after the intervention) in the intervention and control groups showed that there is a significant relationship between the scores and the groups in the total score of health belief (p<0.001).
These results indicated that the intervention was effective in increasing the score of compliance with treatment and decreasing the quality of life scores (according to the tools used, the lower score indicates a higher quality of life) (p<0.001). There was a significant difference among the mean scores of compliance with treatment, quality of life, and health belief in the two groups with a strong effect according to the Cohen coefficient of 0.9.
There was a statistically significant difference between the scores of compliance with treatment, quality of life, and health beliefs in four time periods in the intervention group before and six months after the intervention (Table 4).
Diabetes mellitus is one of the most important metabolic diseases worldwide by an alarming prevalence, which has increased by 50% over the past 10 years [1]. The global prevalence of diabetes in 2019 was 9.3% (463 million people) which it is estimated to reach 10.2% (578 million people) in 2030 and 10.9% (700 million people) by 2045 [2]. In a study conducted from 2014 to 2020 on participants aged 35 to 70 years among different Iranian races, 15% of the adult population were diabetic, and more than 25% of them were pre-diabetic [2].
Diabetes patients often do not follow their treatment plan, which makes blood sugar management challenging [3]. The interplay of numerous elements or dimensions determines treatment adherence, which is a multidimensional phenomenon [4]. The ultimate goal of any recommended treatment is to achieve the desired outcome for the patient. While despite all the attention and efforts made by the healthcare team, if the patient does not adhere to the treatment, this will not be achieved [5].
Despite the scientific efforts and application of various theories and programs of professional interventions, nursing, and non-nursing, it has been reported that there is still a lack of adherence, as a challenge and problem, to control chronic diseases, which is a major expanding obstacle to achieving therapeutic goals. On the other hand, although non-compliance is a universal phenomenon, it does not have a fixed, common, and equal nature, as it is unique for individuals and social and is a completely contextual phenomenon, and even has a different nature and function in different diseases and patients, so that it cannot be explained and addressed by fixed and uniform theory, model or formula and program all over the world [3].
Thus, Vahedparast [6] conducted a study to design an effective model and intervention based on this model to promote compliance with care-treatment regimens in the patient's social life. They developed an emergency-based self-protection approach in which patients with chronic illness used to live, which is the leading cause of noncompliance with care-treatment regimens among individuals with chronic diseases. Considering that most cases of this disease have no obvious symptoms or consequences, patients do not feel threatened. This fear is superficial and periodic, which could be the main identified root causes of hesitation and failure in accepting adjusted behaviors and failure to comply with care-treatment regimens. According to these findings, they designed and presented a “continuity of self-preservation model”. They argue that self-preservation is not static, but a dynamic process and should be initiated at the beginning of a person's awareness of their chronic illness and be accompanied by a conscious and active search for the patient and the support and participation of nurses and other health professionals in the process of compliance with care-treatment regimens, leading to the best behavior in line with care-treatment regimens compliance. This model introduces the idea of a mediator notion termed a motivator, which is crucial for sustaining behavioral stimulus and motivation. It is possible to identify and use the support resources of their living environment (spouse, family, supportive spouses, peers and role models, and care-treatment team) to further advance the process of continuing self-protection.
The ultimate goal of this model is to continue the self-preservation of individuals with chronic diseases in compliance with care-treatment regimens, and strategies to optimize and maintain the recommended regimens are presented [6]. Therefore, this research aimed to design and evaluate an intervention program to improve compliance with treatment in patients with diabetes (one of the most common chronic diseases) based on the self-preservation continuity model.
Materials and Methods
Study design
This study is a quasi-experimental clinical trial in which the study population was patients with type 2 diabetes admitted to the internal wards of two hospitals in Zahedan (Iran) from 2020 to 2021. Randomization was not possible due to the limited number of specific treatment centers for this disease (two centers).
Samples and research environment
The sample size was determined based on the findings of a prior research [7]. With a 95% confidence interval and a 95% test power, 40 individuals were identified for each group, totaling 80 individuals. One treatment center was selected as the research environment for the intervention group, and another center was selected for the control group. Inclusion criteria were as follows: having at least a compliance with the treatment-care regimen using a questionnaire and blood test, age of at least 30, access to smart phone for patient or informal caregiver (family).
Collecting data
Data collection tools in this study included the following:
Summary of Diabetes Self-Care Activities (SDSCA) Scale: This scale was first designed by Toobert and Glasgow, and then Toobert et al. [8] modified it. Numerous studies in different countries, including Iran, used this tool to examine the compliance with self-care behaviors and treatment regimen in patients with diabetes [7, 9-21].
This scale is an accurate 12-item self-report instrument that looks at five aspects of a diabetes treatment plan (diet, exercise, proper tablet intake, self-monitoring blood sugar levels, foot care, and smoking). This tool is scored on a seven-choice scale from 0 to 7. The total score on the scale is 0 to 77. A score of 0 to 22 is considered a poor score. The internal consistency method was used to calculate the reliability, and Cronbach's alpha for the self-care activity scale was 91%.
Diabetes – Mellitus Specific Quality Of Life (DMQOL): This questionnaire was first developed to assess health-related quality of life in patients with diabetes in Taiwan based on the World Health Organization Quality of Life Scale Brief Version (WHOQOL) [22]. Saffari et al. [23] translated it into Persian, and based on its psychometric properties, they concluded that it is an appropriate instrument for evaluating the quality of life of diabetic patients in Iran. This questionnaire has four dimensions, including Satisfaction with one's condition, the impact of diabetes on a person's life, concerns related to diabetes and social and occupational concerns. A higher score on this instrument, which bases its options on the Likert scale, implies more unhappiness with life quality [23]. The researcher evaluated the reliability of this questionnaire with Cronbach's alpha of 84%.
Diabetes Specific Health Beliefs Scale: This scale is used to assess the perceived sensitivity and severity of complications of diabetes. This tool was used by Sharifabad and Rouhani [24], which is a translation of the Lewis and Bradley Diabetes Specific Health Beliefs Scale. This scale contains 20 questions. The achievable score in these structures is from 0 to 40 [24]. Cronbach's alpha was estimated in the perceived sensitivity section as 85%, for the perceived severity section was 92%, and for the total questionnaire was 73%.
Glycosylated hemoglobin: Glycosylated hemoglobin levels in the patient were measured twice, before and after the intervention. In a regulated and certified laboratory, HbA1C was also determined using a specific test kit.
Procedure
Following obtaining the necessary permits, the researcher implemented the designed program (based on the model) to improve the cognitive structure of the nurses working in the ward.
The approach of cognitive structure improvement is performed in three dimensions: 1) health care providers (nurses), 2) patients, and 3) patients' families. In this regard, first, a training program for nurses working in the intervention group was held in 3 sessions. Nurses were asked to consider the issues raised during the hospitalization of patients in the ward, discharge time, and during education programs. Patients were sampled once the nurses had finished their training. Blood was drawn with the patient's permission to test for glycosylated hemoglobin. The patient's treatment compliance questionnaire was filled out, and based on the predetermined criteria, patient was assigned to either the intervention group or the control group. The purpose of this stage in the intervention group was to modify the cognitive structure of patients to keep them sensitive in symptomatic and asymptomatic conditions and to create sensitivity to the hidden long-term effects of diabetes (such as heart attacks, strokes, wounds, amputations, blindness, etc.). For this purpose, first, a WhatsApp group of participants in the intervention group was by the researcher.
During the research, at least two educational messages containing educational items on diabetes self-care in the areas of diet, physical activity, medication use, related complications to diabetes, and its management were sent to the group by the researcher daily. Furthermore, warning messages related to complications (text or video messages) were sent every day both in groups and individually to the participants to keep them alert and sensitive to continue. The development of self-preservation skills in patients is a dimension related to the modification of the cognitive structure in this model. So in the following stage, training materials, including information about diabetes and self-care activities for disease control were held separately for patients in the group. To improve the cognitive structure of the family (one of the dimensions of the self-protection model), virtual groups of caregivers were formed, and educational materials and messages were sent to this group. During this time, the control group, from another hospital, received routine care. To assess the effect of the intervention, the scales of diabetes-related self-care activities and quality of life was completed 1, 3, and 6 months after the intervention, and the Health Belief Questionnaire 3 and 6 months after the intervention was completed again for both groups. Moreover, a blood sample for HbA1C was taken 6 months after the intervention.
Statistical analysis
Descriptive statistics, Chi-square test, repeated measures analysis of variance, Bonferroni post hoc test, independent t-test, and paired t-test were all used to examine the data. Data analysis was performed using SPSS 9 software.
Findings
The mean age of the patients in the intervention and control groups was 46.17±10.44 and 47.02±8.6 years, respectively. The mean duration of diagnosis in the intervention and control groups was 7.6±4.6 and 8.1±3.5 years, respectively. There was no significant difference between the two groups before the intervention in age and disease duration (p>0.05). Also, there was no significant difference in the frequency distribution of the participants in terms of demographic characteristics in the intervention and control groups (Table 1).
Table 1) Comparison of frequency distribution of demographic variables in the intervention and control groups using chi-square test
Before the intervention, there was no significant difference between the two groups of intervention and control in the variables of compliance with treatment, quality of life, and health beliefs (p>0.05). However, one month after the intervention, there was a significant difference in the means of compliance with treatment in the two groups, and the score of compliance with treatment in the intervention group increased. The quality of life was also significantly impacted by this disparity. Although both groups' quality-of-life scores dropped (a lower score implies a higher quality of life), the intervention group's mean change was greater. On the other hand, the levels of treatment compliance, quality of life, and health beliefs significantly varied between the two groups three months and six months following the intervention. Compliance with treatment and health beliefs increased, and quality of life decreased (a lower score indicates a higher quality of life). The mean score of HbA1C in the two groups significantly reduced six months after the intervention. Moreover, the coefficient effect of 1.55 showed the high positive impact of the intervention (Table 2).
Besides, the inter-group and intra-group effects in different phases of the intervention are shown in Table 3. According to the results of an intergroup and intragroup analysis of variance with repeated measures of four measurements (before the intervention, 1, 3, and 6 months after the intervention) in the intervention and control groups, there was a significant difference in the factor scores, the groups' scores for treatment compliance, and the overall quality of life score (p<0.001). Repeated measurements of three measurements (before the intervention, 3, and 6 months after the intervention) in the intervention and control groups showed that there is a significant relationship between the scores and the groups in the total score of health belief (p<0.001).
These results indicated that the intervention was effective in increasing the score of compliance with treatment and decreasing the quality of life scores (according to the tools used, the lower score indicates a higher quality of life) (p<0.001). There was a significant difference among the mean scores of compliance with treatment, quality of life, and health belief in the two groups with a strong effect according to the Cohen coefficient of 0.9.
There was a statistically significant difference between the scores of compliance with treatment, quality of life, and health beliefs in four time periods in the intervention group before and six months after the intervention (Table 4).
Table 2) Comparison of the mean variables in the two groups before, 1, 3 and 6 months after the intervention

In addition, the paired t-test revealed a significant difference in the mean Hb1AC before and six months after the intervention in the two groups (Table 2).
Table 3) Results of repeated measures analysis of variance in the two groups at different stages of the intervention

Table 4) Examining the differences in scores of compliance with treatment, quality of life and health beliefs in intervention and control groups in 4 stages using Bonferroni post hoc test
Discussion
Regarding the findings, the intervention program based on the self-protection continuity model improved compliance with treatment and its consequences, including quality of life, health beliefs, and HbA1C in patients with type 2 diabetes.
Various studies showed that the main problem of patients with chronic disease, especially diabetic patients, is the lack of continuity and failure of patients to accompany and comply with care and treatment standards [25-30]. Previous research has also shown that patients and even service providers' inadequate awareness of the need for ongoing monitoring and care in the absence of symptoms and disease complications, as well as their inappropriate mentalities, are the main causes of this lack of continuity and compliance [27, 29, 31-34]. Meanwhile, it is not enough to just increase awareness, it is necessary to change and continue the behavior and provide the necessary mechanism for this work. Macido [35] evaluated the knowledge and adherence to the treatment of type 2 diabetic patients using self-management and support training program. After the intervention, the patients' awareness in the intervention group increased, but there was no significant change in treatment adherence behaviors in the two groups, which was probably due to the short duration of training. However, it seems that self-sufficiency and lack of continuous intervention are the more important reason. Also, the training program was still available to patients in the intervention group until the end of the study, and after the training program, communication with the patients via discussion in the virtual group, telephone communication and sending messages was available to motivate and increase sensitivity in patients, which it was effective to promote the treatment compliance among these patients.
Farmer et al. [36], in a study to determine the effect of a counseling-oriented nursing intervention on the support of diabetic patients to follow using the hypoglycemic medications showed that the specialized counseling of the nurse in the intervention group caused patients did not discontinue the medication during the period of study, but there was no significant difference between the intervention and control groups in secondary outcomes (quality of life and satisfaction with treatment). Counseling-oriented intervention emphasize on the correct and timely use of medications by patients, which is one of the dimensions of treatment.
Patients were motivated to adhere to these suggestions as they received suitable feedback after complying with therapy and were aware of the improvement in their quality of life. In line with the findings of the present study, Rezai Asl et al. [32], who investigated the effect of family-centered empowerment model on adherence to treatment regimen in the patients with type 2 diabetes, reported that the rate of adherence of patients with diabetes in the family-centered care group was significantly increased after the intervention. Although care was family-centered, the patient’s primary caregiver did not participate directly in the training program. Moreover, the effect of the intervention program was evaluated only one month later. The family actively participated in the intervention and the group, and messages were sent to inform and warn them. Also, the effect of the intervention program was observed even up to six months later, which indicates the continuation of self-care behaviors.
Faramarzi et al. [37] conducted a study to investigate the effect of education based on the health belief model in promoting kidney care behaviors in type 2 diabetic patients, which patients' performance in the intervention group showed a substantial improvement three months after the educational intervention, and fasting blood sugar index marginally dropped. In this investigation, increased scores were seen in the health beliefs-related aspects but not in the perceived severity and sensitivity [37]. The intervention was performed in the form of three training sessions for patients. Although educational intervention could increase some aspects of health belief, to continue self-care behaviors, it is necessary to constantly stimulate the patient and create sensitivity among them and their family to increase perceived severity and sensitivity to complications. In order to create fear and increase sensitivity in patients, the complications of the disease and the problems caused by the lack of blood sugar control and its complications were emphasized by regularly sending messages in groups and personally and by phone. This fear promoted health idea in two dimensions of perceived severity and sensitivity. The model of self-preservation continuity arises from the views, experiences and perceptions of chronic patients and is based on Iranian culture and society. Therefore, this model, considering the influential factors, offers solutions based on which the researcher designed and implemented the interventions.
The implementation of a continuum and self-preservation model can be recommended to improve compliance with treatment and its consequences among patients with chronic disease.
The limitation of this research is the patients' differences in terms of religion, spirituality, social and culture, beliefs, and economic issues, which may have caused differences in the implementation of the recommended items for the patients, and the complete control of these items was beyond the responsibility of the researcher.
It is suggested that the effect of the used model on treatment concordance in other chronic diseases such as high blood pressure, heart disease, asthma, etc., and in patients with type 1 diabetes also be investigated.
Conclusion
The self-preservation continuity model can be implemented even in the Covid-19 pandemic and is more effective in metabolic control and compliance with the treatment of diabetic patients than interventions based on other models that are purely educational.
Acknowledgements: The authors would like to thank the Vice Chancellor for Education and Research of the Faculty of Medical Sciences and Tarbiat Modares University, Zahedan University of Medical Sciences and its affiliated hospitals, the patients, and the nurses participating in this study.
Ethical Permission: This article was approved by the Ethics Committee of the Faculty of Medical Sciences with
code IR.MODARES.REC.1398.138. Before the study, the objectives of the study and ensuring the confidentiality of information were explained to the patients, and they entered the study with the necessary knowledge and consent. Considering the ethical considerations, after the study, educational materials and messages were sent to patients in the control group. The educational program designed based on the model was given to the control group for nurses to use after the research.
Conflict of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Mohammadi E (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Pournamdar Z (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Vahedparast H (Third Author), Methodologist/Assistant Researcher (20%); Kazemnejad A (Fourth Author), Statistical Analyst/Discussion Writer (20%)
Funding: This study is a part of the doctoral dissertation on Nursing in the Faculty of Medical Sciences of Tarbiat Modares University.
Regarding the findings, the intervention program based on the self-protection continuity model improved compliance with treatment and its consequences, including quality of life, health beliefs, and HbA1C in patients with type 2 diabetes.
Various studies showed that the main problem of patients with chronic disease, especially diabetic patients, is the lack of continuity and failure of patients to accompany and comply with care and treatment standards [25-30]. Previous research has also shown that patients and even service providers' inadequate awareness of the need for ongoing monitoring and care in the absence of symptoms and disease complications, as well as their inappropriate mentalities, are the main causes of this lack of continuity and compliance [27, 29, 31-34]. Meanwhile, it is not enough to just increase awareness, it is necessary to change and continue the behavior and provide the necessary mechanism for this work. Macido [35] evaluated the knowledge and adherence to the treatment of type 2 diabetic patients using self-management and support training program. After the intervention, the patients' awareness in the intervention group increased, but there was no significant change in treatment adherence behaviors in the two groups, which was probably due to the short duration of training. However, it seems that self-sufficiency and lack of continuous intervention are the more important reason. Also, the training program was still available to patients in the intervention group until the end of the study, and after the training program, communication with the patients via discussion in the virtual group, telephone communication and sending messages was available to motivate and increase sensitivity in patients, which it was effective to promote the treatment compliance among these patients.
Farmer et al. [36], in a study to determine the effect of a counseling-oriented nursing intervention on the support of diabetic patients to follow using the hypoglycemic medications showed that the specialized counseling of the nurse in the intervention group caused patients did not discontinue the medication during the period of study, but there was no significant difference between the intervention and control groups in secondary outcomes (quality of life and satisfaction with treatment). Counseling-oriented intervention emphasize on the correct and timely use of medications by patients, which is one of the dimensions of treatment.
Patients were motivated to adhere to these suggestions as they received suitable feedback after complying with therapy and were aware of the improvement in their quality of life. In line with the findings of the present study, Rezai Asl et al. [32], who investigated the effect of family-centered empowerment model on adherence to treatment regimen in the patients with type 2 diabetes, reported that the rate of adherence of patients with diabetes in the family-centered care group was significantly increased after the intervention. Although care was family-centered, the patient’s primary caregiver did not participate directly in the training program. Moreover, the effect of the intervention program was evaluated only one month later. The family actively participated in the intervention and the group, and messages were sent to inform and warn them. Also, the effect of the intervention program was observed even up to six months later, which indicates the continuation of self-care behaviors.
Faramarzi et al. [37] conducted a study to investigate the effect of education based on the health belief model in promoting kidney care behaviors in type 2 diabetic patients, which patients' performance in the intervention group showed a substantial improvement three months after the educational intervention, and fasting blood sugar index marginally dropped. In this investigation, increased scores were seen in the health beliefs-related aspects but not in the perceived severity and sensitivity [37]. The intervention was performed in the form of three training sessions for patients. Although educational intervention could increase some aspects of health belief, to continue self-care behaviors, it is necessary to constantly stimulate the patient and create sensitivity among them and their family to increase perceived severity and sensitivity to complications. In order to create fear and increase sensitivity in patients, the complications of the disease and the problems caused by the lack of blood sugar control and its complications were emphasized by regularly sending messages in groups and personally and by phone. This fear promoted health idea in two dimensions of perceived severity and sensitivity. The model of self-preservation continuity arises from the views, experiences and perceptions of chronic patients and is based on Iranian culture and society. Therefore, this model, considering the influential factors, offers solutions based on which the researcher designed and implemented the interventions.
The implementation of a continuum and self-preservation model can be recommended to improve compliance with treatment and its consequences among patients with chronic disease.
The limitation of this research is the patients' differences in terms of religion, spirituality, social and culture, beliefs, and economic issues, which may have caused differences in the implementation of the recommended items for the patients, and the complete control of these items was beyond the responsibility of the researcher.
It is suggested that the effect of the used model on treatment concordance in other chronic diseases such as high blood pressure, heart disease, asthma, etc., and in patients with type 1 diabetes also be investigated.
Conclusion
The self-preservation continuity model can be implemented even in the Covid-19 pandemic and is more effective in metabolic control and compliance with the treatment of diabetic patients than interventions based on other models that are purely educational.
Acknowledgements: The authors would like to thank the Vice Chancellor for Education and Research of the Faculty of Medical Sciences and Tarbiat Modares University, Zahedan University of Medical Sciences and its affiliated hospitals, the patients, and the nurses participating in this study.
Ethical Permission: This article was approved by the Ethics Committee of the Faculty of Medical Sciences with
code IR.MODARES.REC.1398.138. Before the study, the objectives of the study and ensuring the confidentiality of information were explained to the patients, and they entered the study with the necessary knowledge and consent. Considering the ethical considerations, after the study, educational materials and messages were sent to patients in the control group. The educational program designed based on the model was given to the control group for nurses to use after the research.
Conflict of Interests: The authors declare no conflict of interests.
Authors’ Contribution: Mohammadi E (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Pournamdar Z (Second Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (30%); Vahedparast H (Third Author), Methodologist/Assistant Researcher (20%); Kazemnejad A (Fourth Author), Statistical Analyst/Discussion Writer (20%)
Funding: This study is a part of the doctoral dissertation on Nursing in the Faculty of Medical Sciences of Tarbiat Modares University.
Article Type: Original Research |
Subject:
Health Promotion Approaches
Received: 2022/09/24 | Accepted: 2022/12/1 | Published: 2022/12/13
Received: 2022/09/24 | Accepted: 2022/12/1 | Published: 2022/12/13
References
1. Khamseh ME, Sepanlou SG, Hashemi-Madani N, Joukar F, Mehrparvar AH, Faramarzi E, et al. Nationwide prevalence of diabetes and prediabetes and associated risk factors among Iranian adults: Analysis of data from Persian cohort study. Diabetes Ther. 2021;12(11):2921-38. [Link] [DOI:10.1007/s13300-021-01152-5]
2. Sharma T, Kalra J, Dhasmana D, Basera H. Poor adherence to treatment: A major challenge in diabetes. J Indian Acad Clin Med. 2014;15(1):26-9. [Link]
3. van Dulmen S, Sluijs E, van Dijk L, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res. 2007;7(1):55. [Link] [DOI:10.1186/1472-6963-7-55]
4. Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry. 2001;158(1):29-35. [Link] [DOI:10.1176/appi.ajp.158.1.29]
5. Sluijs E, Dulmen Sv, Dijk Lv, de Ridder D, Heerdink R, Bensing J. Patient adherence to medical treatment: a meta review. Nivel. 2006. [Link]
6. Vahedparast H. The process of concordance with care - treatment regimens in patients affected by chronic diseases and designing of promoting its model [Dissertation]. Tehran: Tarbiat Modares University; 2016. [Persian] [Link]
7. Zheng F, Liu S, Liu Y, Deng L. Effects of an outpatient diabetes self-management education on patients with type 2 diabetes in China: a randomized controlled trial. J Diabetes Res. 2019;2019:1073131. [Link] [DOI:10.1155/2019/1073131]
8. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943-50. [Link] [DOI:10.2337/diacare.23.7.943]
9. Michels MJ, Coral MHC, Sakae TM, Damas TB, Furlanetto LM. Questionnaire of diabetes self-care activities: translation, cross-cultural adaptation and evaluation of psychometric properties. Arq Bras Endocrinol Metabol. 2010;54(7):644-51. [Portuguese] [Link] [DOI:10.1590/S0004-27302010000700009]
10. Roos AC, Baptista DR, de Miranda RC. Compliance with the treatment of patients with type 2 Diabetes Mellitus. Demetra Food Nutr Health. 2015;10(2):329-47. [Link] [DOI:10.12957/demetra.2015.13990]
11. Claude JAJ. An application of health behaviour models to diabetic treatment adherence: A comparison of protection motivation theory and the theory of planned behaviour [Dissertation]. Canada: The University of Regina: 2011. [Link]
12. Anbari K, Ghanadi K, Kaviani M, Montazeri R. The self-care and its related factors in diabetic patients of khorramabad city. Yafteh. 2012;14(4):49-57. [Persian] [Link]
13. Chamany S, Walker EA, Schechter CB, Gonzalez JS, Davis NJ, Ortega FM, et al. Telephone intervention to improve diabetes control: a randomized trial in the New York City A1c Registry. Am J Prev Med. 2015;49(6):832-41. [Link] [DOI:10.1016/j.amepre.2015.04.016]
14. Mahmoud NM, yousef Mohammed N, Essa RM. The relationship between health belief model and compliance with therapeutic regimen among diabetic pregnant women. Int J for Res in Health Sci Nurs. 2018;4(2):40-63. [Link]
15. Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med. 2009;32(4):349-59. [Link] [DOI:10.1007/s10865-009-9209-4]
16. Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Ann Behav Med. 2004;27(3):148-54. [Link] [DOI:10.1207/s15324796abm2703_2]
17. Ung SK. Role of cultural and psychological factors influencing diabetes treatment adherence [Dissertation]. Loma Linda, California, United States: Loma Linda University; 2017. [Link]
18. Wu SF. Effectiveness of self-management for persons with type 2 diabetes following the implementation of a self-efficacy enhancing intervention program in Taiwan [Dissertation]. Australia: Queensland University of Technology; 2007. [Link]
19. Turan B, Osar Z, Damci T, Ilkova H. The role of coping with disease in adherence to treatment regimen and disease control in type 1 and insulin treated type 2 diabetes mellitus. Diabetes Metab. 2002;28(3):186-93. [Link]
20. Kanapathy J. Illness perception of Type 2 Diabetic patients in Malaysia [Dissertation]. London: City University London; 2015. [Link]
21. Kamradt M, Bozorgmehr K, Krisam J, Freund T, Kiel M, Qreini M, et al. Assessing self-management in patients with diabetes mellitus type 2 in Germany: validation of a German version of the Summary of Diabetes Self-Care Activities measure (SDSCA-G). Health Qual Life Outcomes. 2014;12(1):185. [Link] [DOI:10.1186/s12955-014-0185-1]
22. Lin C-Y, Lee T-Y, Sun Z-J, Yang Y-C, Wu J-S, Ou H-T. Development of diabetes-specific quality of life module to be in conjunction with the World Health Organization quality of life scale brief version (WHOQOL-BREF). Health Qual Life Outc. 2017;15(1):167. [Link] [DOI:10.1186/s12955-017-0744-3]
23. Saffari M, Lin C-Y, O'Garo K, Koenig HG, Sanaeinasab H, Pakpour AH. Psychometric properties of Persian Diabetes-Mellitus Specific Quality of Life (DMQoL) questionnaire in a population-based sample of Iranians. Int J Diabetes Dev Ctries. 2019;39(1):218-27. [Link] [DOI:10.1007/s13410-018-0648-8]
24. Morowaty Sharifabad M, Rouhani Tonekaboni N. Perceived severity and susceptibility of diabetes complications and its relation to self-care behaviors among diabetic patients. Armaghan-e-Danesh. 2007;12(3):59-68. [Persian] [Link]
25. Hashemi SM, Bouya S. Treatment adherence in diabetic patients: an important but forgotten issue. J Diabetes Nurs. 2018;6(1):341-51. [Persian] [Link]
26. Gholamaliei B, Karimi-Shahanjarini A, Roshanaei G, Rezapour-Shahkolaei F. Medication adherence and its related factors in patients with type II diabetes. J Educ Community Health. 2016;2(4):3-12. [Persian] [Link] [DOI:10.21859/jech-02042]
27. Tanharo D, Ghods R, Pourrahimi M, Abdi M, Aghaei S, Vali N. Adherence to treatment in diabetic patients and its affecting factors. Pajouhan Sci J. 2018;17(1):37-44. [Persian] [Link] [DOI:10.21859/psj.17.1.37]
28. Harvey J, Lawson V. The importance of health belief models in determining self‐care behaviour in diabetes. Diabet Med. 2009;26(1):5-13. [Link] [DOI:10.1111/j.1464-5491.2008.02628.x]
29. Hamadzadeh S, Ezatti Z, Abedsaeidi Z, Nasiri N. Coping styles and self-care behaviors among diabetic patients. Iran J Nurs (2008-5923). 2013;25(80):24-33. [Persian] [Link]
30. Sweileh WM, Zyoud SeH, Abu Nab'a RJ, Deleq MI, Enaia MI, Nassar SaM, et al. Influence of patients' disease knowledge and beliefs about medicines on medication adherence: findings from a cross-sectional survey among patients with type 2 diabetes mellitus in Palestine. BMC Public Health. 2014;14(1):94. [Link] [DOI:10.1186/1471-2458-14-94]
31. Goli Roshan A, Hosseinkhani SN, Norouzadeh R. The relationship between health literacy of elderly diabetics and adherence to treatment, Babol, Iran, 2021. Qom Univ Med Sci J. 2021;14(12):70-80. [Persian] [Link] [DOI:10.52547/qums.14.12.70]
32. Rezai Asl H, Pishgooi SAH, Alhani F. The effectiveness of "Family-Centered Empowerment Model" on the treatment adherence of patients with type II diabetes and heart disorder admitted to AJA Hospitals, during year 2015. Mil. Caring Sci J. 2017;4(1):58-69. [Persian] [Link] [DOI:10.29252/mcs.4.1.58]
33. Wens J, Vermeire E, Hearnshaw H, Lindenmeyer A, Biot Y, Van Royen P. Educational interventions aiming at improving adherence to treatment recommendations in type 2 diabetes: a sub-analysis of a systematic review of randomised controlled trials. Diabetes Res Clin Pract. 2008;79(3):377-88. [Link] [DOI:10.1016/j.diabres.2007.06.006]
34. Smaje A, Weston‐Clark M, Raj R, Orlu M, Davis D, Rawle M. Factors associated with medication adherence in older patients: A systematic review. Aging Med. 2018;1(3):254-66. [Link] [DOI:10.1002/agm2.12045]
35. Macido A. A nurse-led inpatient diabetes self-management education and support program to improve patient knowledge and treatment adherence. J Health Educ Teach. 2019;10(1):1-10. [Link]
36. Farmer A, Hardeman W, Hughes D, Prevost AT, Kim Y, Craven A, et al. An explanatory randomised controlled trial of a nurse-led, consultation-based intervention to support patients with adherence to taking glucose lowering medication for type 2 diabetes. BMC Fam Pract. 2012;13(1):30. [Link] [DOI:10.1186/1471-2296-13-30]
37. Faramarzi M, Shamsi M, Khorsandi M, Almasi HA. The role of education underpinned by health belief model in promoting kidney care behaviors in type 2 diabetic patients. Iran J Evdocrinol Metabol. 2021;22(6):469-77. [Persian] [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





