Volume 10, Issue 3 (2022)
Health Educ Health Promot 2022, 10(3): 609-615 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rabiei M, Pakkhesal M, Sobhi P, Masoudi Rad H. Geriatric Oral Health-Related Quality of Life in the Retired Elderly Population. Health Educ Health Promot 2022; 10 (3) :609-615
URL: http://hehp.modares.ac.ir/article-5-61764-en.html
URL: http://hehp.modares.ac.ir/article-5-61764-en.html
1- Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran
2- Community Oral Health Department, School of Dentistry, Golestan University of Medical Sciences, Gorgan, Iran
3- Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran
4- Department of Endodontics, School of Dentistry, Guilan University of Medical Sciences, Guilan, Iran
2- Community Oral Health Department, School of Dentistry, Golestan University of Medical Sciences, Gorgan, Iran
3- Faculty of Dentistry, Guilan University of Medical Sciences, Rasht, Iran
4- Department of Endodontics, School of Dentistry, Guilan University of Medical Sciences, Guilan, Iran
Full-Text [PDF 858 kb]
(3837 Downloads)
| Abstract (HTML) (1792 Views)
Full-Text: (402 Views)
Introduction
A significant demographic transition has been experienced worldwide due to declining birth rates and increasing life expectancy, which led to an increase in the elderly population [1]. The population of the elderly over 60 years will reach 2 billion by 2050 [2]. This demographic change produces heavy challenges to health authorities and social planners due to the fast rate burden of chronic diseases including oral diseases among the elderly [3].
The elderly who has lost most teeth suffer from serious functional limitations, leading to nutritional problems [4]. The chief component of an elderly person’s life which affects his/her lifestyle, and physical, emotional, and mental happiness is oral health status [5]. Oral health is essential to individual general health and quality of life [6]. The American Dental Association defines oral health as a functional, structural, aesthetic, physiologic, and psychosocial state of well-being [6]. With aging, a significant decline in oral health may be observed, making older adults more frail, dependent, and disabled [6].
Assessment of oral health-related quality of life (OHRQoL) has an important role in clinical practice. OHRQoL refers to the subjective thoughts and beliefs of an individual regarding his oral conditions. The OHRQoL provides a complete assessment of oral function and health [7]. A variety of measures of the subjective impact of oral conditions on quality of life have been developed and used in oral health surveys during the last decades. One of the most well-established instruments is Geriatric Oral Health Assessment Index (GOHAI), introduced in 1990 and included 12 items in physical function, psychosocial function, and pain and discomfort domains [8].
However, in recent years, many investigations have assessed the quality of life-related to oral health in the elderly population. However, most of the studies were conducted on elderly living in nursing homes [9], institutionalized seniors [10], or elderly who were referred to dental clinics [11]. Based on these documents, there is no adequate information about the elderly who have relative health status, such as retired elderly. In addition, people with different cultural backgrounds may respond differently to GOHAI items. For instance, being edentulous (missing teeth) may have different levels of importance in various cultures. Therefore, the GOHAI must be tested in diverse cultures, languages, and geography.
Likewise, Guilan province in the North of Iran has the highest percentage of the elderly population in this country [12]. Given the high rate of aging in the population, it is necessary to pay attention to this part of society so that they will have a comfortable and high‑quality life. In Guilan, tooth loss is the most important oral change that occurs in the elderly. Over half of the elderly are edentulous, and a large percentage of them do not wear a denture. The mean number of remaining teeth in the elderly often ranges from 4 to 8 [10, 11]. Thus, the present study was conducted to determine oral health status and the OHRQoL among independently elderly members of retirement centers in the northern region of Iran.
Material and Methods
This descriptive-analytical cross-sectional study was conducted on retired elderlies between April and September of 2018. The participants were members of the Civil Servants Pension Organization (CSPO), which has covered more than 1,471,000 retirees and government employees in Iran. This organization is an independent legal entity under the governance of the Ministry of Welfare and Social Security and runs an insurance company. Also, Civil Servants Pension Organization had around 10,000 members in Guilan city. The sample size was calculated to be 196 according to the result of Daradkeh et al. [13], considering 95% CI, mean of 40.9±10.7, and d=1.5 score. Subjects were entered into the study consecutively daily and referred to the only available retirement center. The target population included retired elderly, without physical and mental disabilities, 60 years and older of both sexes, willing to participate in research, ability to answer questions, and communication.
The Geriatric Oral Health Assessment Index (GOHAI) is a 12-item instrument with three domains: physical function (eating, speech, and swallowing), psychosocial function (worry or concern regarding oral health, dissatisfaction with appearance, self-consciousness regarding oral health, and avoidance of social interaction because of oral problems), and pain or discomfort (medication used to relieve oral pain or discomfort). Each item in the GOHAI was rated on a 5-point Likert scale ranging from 1 (always) to 5 (never). The total score ranged from 12 to 60 points, with a higher score indicating a more favorable OHRQoL. Consequently, a total score between 12 and 36 indicated a poor quality of life, between 36 and 48 indicated a moderate quality of life, and between 48 and 60 indicated a good quality of life. The Persian version of the GOHAI exhibited acceptable reliability and validity to evaluate OHRQoL in the Iranian elderly population [14-16]. According to the results of a study about the reliability of the Persian version of GOHAI, Cronbach’s α (0.78) showed a high degree of internal consistency and homogeneity between items [14]. Also, regarding the discriminant validity, the respondents with higher GOHAI scores were associated with a lower number of carious and missing teeth [14].
Subjects were ensured that they could leave the study whenever they wished to do so. Hence written informed consent was obtained before the start of the study. As well as, the aim of the study and research procedures were explained to participants initially. The oral examination of the subjects took place in an appropriate room of the retirement center using a disposable mirror, a wooden spatula, and a flashlight. In the present study, a single examiner was trained under the supervision of an oral & Maxillofacial Medicine specialist to standardize the oral lesions diagnostic as much as possible. A single trained examiner calculated data that intra-examiner agreement (kappa coefficient=0.87) was considered excellent. First, an examiner recorded sociodemographic information such as age, gender, marital status, economic status, and smoking due to face-to-face interviews. Then, the oral health status was rated (good, moderate, poor) according to the participant's response to the question, “How would you describe the health of your mouth, teeth, and gums?”. Also, the researcher asked about the subjects’ perceptions of their need for dental treatment. Besides, subjects were asked about their oral hygiene frequency per day (twice a day or more, once a day, and sometimes), and their last dental visit one year ago. The main reason for seeking dental treatment at the last dental appointment was also asked and divided based on the problem (dental pain, oral and gingival problems, or routine check-ups). Moreover, dental and prosthetic status was assessed based on the number of remaining teeth in the mouth and partial/ complete dentures usage. Data on the presence of systemic diseases were asked directly from the subjects. Consequently, the researcher sequentially read GOHAI questionnaire items, and participants' responses were entered directly into the forms on the same day.
Data were analyzed using Statistical Package for Social Sciences software (SPSS, version 21). The independent t-test and ANOVA were used to compare the OHRQoL based on qualitative variables such as age, gender, and dental visits. If the assumptions were not met, non-parametric tests such as the Mann-Whitney U test and the Kruskal-Wallis test were used for comparisons. A significance level of P<0.05 was the criterion for a statistically significant effect.
Findings
A total of 196 retired elderly consisting of 115 (58.7%) males and 81 (41.3%) females were included in the present study. The mean age of participants was 67.7±6.2 years, with an age range of 60 to 86 years. The following characteristics were predominant: married (92.3%), a university education level (47.4%), visiting a dentist only when experiencing pain (77.6%), the last dental visit one year ago (59.2%), not smoking (94.4%). The financial status of the majority of participants (48.5%) was moderate. The majority (66.3%) stated that they had poor or moderate oral health status, and 75% believed they needed dental treatment; 44.9% rinsed their mouth at least once a day.
As shown in Diagram 1, the most common oral mucosal lesions in the participants were xerostomia, fissured tongue and dorsal tongue base varies, and denture stomatitis. The most common systemic diseases were hypertension, cardiac disease, diabetes mellitus and pulmonary diseases with equal prevalence, neurologic diseases, dementia, and cerebrovascular conditions. The study participants' mean number of remaining teeth was 15.9±9.7 (range 0 to 29).
Of all, 17.9% were edentulous, 100 51% had less than 20 teeth in their mouth, and 31.1% had more than 20 teeth in their mouth. Out of all participants, 35 were completely edentulous and had complete dentures, 79 did not have posterior teeth, 41 did not have any prosthesis, and 38 had partial dentures. Of all, 8 did not have the anterior teeth; out of which, 3 did not have any prosthesis, and 5 had partial dentures. Thirteen subjects (6.6%) did not have anterior or posterior teeth and had a partial denture. Sixty-one subjects had over 20 teeth, out of which 12 had dental implants.
Moreover, Diagram 2 presents the median score and percentile of the subjects’ answers to each item on the GOHAI questionnaire. According to the findings in the physical domain, 45% of the elderly had limitations in having a variety of foods (Q1), 37.8% had problems in biting or chewing the food (Q2), 16 had problems with deglutition (Q3), and 20 (0.5%) had problems with speech (Q4); 38.8% had difficulty in eating (Q5). In the psychosocial domain, 15 had limited their social encounters with others due to oral and dental problems (Q6); 60% were not satisfied with the appearance of their teeth (Q7), 45.5% were worried about their teeth or gingiva (Q9), 33.7% were over-concerned about their dental or gingival status (Q10) and 227 were embarrassed about eating in front of others (Q11). In the pain and discomfort domain, 21.9% used analgesics to alleviate pain (Q8), and 36.2% stated that their teeth or gingiva were hypersensitive to hot, cold, and sweet foods and drinks (Q12).
As illustrated in Table 1, there was a significant difference among the three domains' scores on the GOHAI questionnaire (p<0.001). In general, according to the qualitative analysis, the OHRQoL score was qualitatively suitable or moderate in 95 (48.5%) subjects, good in 91 (46.4%), and poor in 10 (5.1%). According to the Kruskal-Wallis test and Mann-Whitney U test, the quality of life score of those living alone (51.1±5.0) was higher than married individuals (47.2±6.3; p=0.013). Subjects with good (50.7±4.6) or excellent (55.0±1.4) self-rated oral health had higher OHRQoL than those with poor (44.7±6.8) self-rated oral health (p<0.001). The elderly with a self-perceived need for treatment had shown lower quality of life scores (46.8±6.4) than those with no self-perceived need for treatment (48.9±5.8) and those with no opinion in this respect (50.3±5.5; P=0.03).
The OHRQoL score was not significantly different based on the objective social status of participants, such as their age, sex, level of education, socioeconomic status, dental status, and prosthetic status. Table 2 presents the dental status and prosthetic status of subjects in general and separately for each domain of the GOHAI questionnaire.

Diagram 1) Frequency of oral mucosal lesions in participants
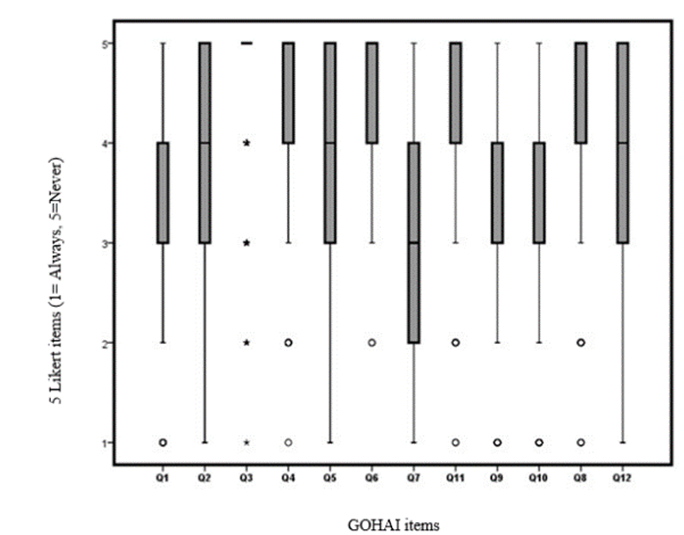
Diagram 2) Distribution of median scores and percentile of the subjects’ responses to GOHAI items
Table 1) The mean and standard deviation of total GOHAI score and domains scores
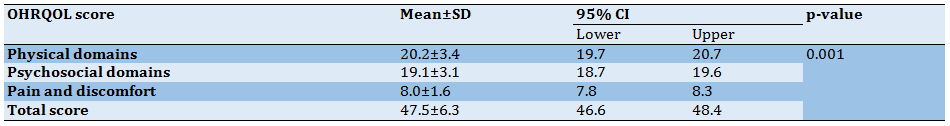
Table 2) Mean±SD of quality of life domains based on dental and prosthetic status
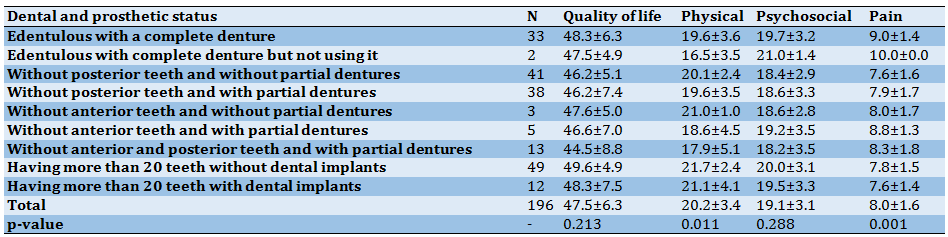
Table 3) OHRQoL score in presence of some oral conditions (Mean±SD)
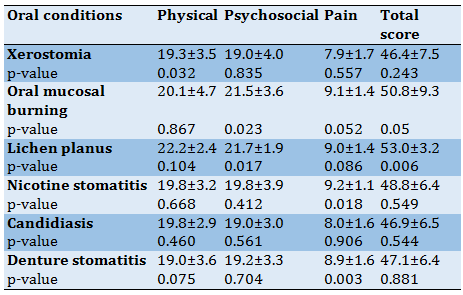
According to the Mann-Whitney U test, individuals with oral mucosal burning sensation and lichen planus acquired higher scores on the quality of life (Table 3).
In the physical domain, singles (living alone) compared to married individuals (coupled) (odds ratio=3.3, 95% CI:1-11.3) and those sought dental treatment only if they had pain compared to those with irregular dental visits (odds ratio=3.8, 95% CI:1.1-13) and those with over 20 teeth (odds ratio:5.36, 95% CI=2-14) compared to completely edentulous patients had higher quality of life in the physical domain. In the psychosocial domain, singles compared to married individuals (p=0.021, odds ratio=6.1-28.2) had higher quality of life scores, and those with a few teeth compared to completely edentulous patients (p=0.02, odds ratio=0.375, 95% CI: 0.1-1) had lower relative odds of quality of life median score in the psychosocial domain. In the pain and discomfort domain, those without self-perceived need for dental treatment (P=0.017, odds ratio=1.9, 95% CI:1.1-3.5), those with more than 20 teeth (odds ratio=0.243, 95% CI:0.1-0.7) and patients with fewer than 20 teeth compared to completely edentulous patients (p=0.011, odds ratio=0.261, 95% CI=0.1-0.7) had a higher median score of quality of life in pain and discomfort domain. In other words, completely edentulous patients had less pain and discomfort compared to dentate patients.
Discussion
The present study aimed to determine the oral health-related quality of life (OHRQoL) in the retired elderly population. The mean and standard deviation of GOHAI scores in the present study participants were 47.5±6.3. Similar results were reported in Malaysia, Lebanon, China, and France [17-20], while a lower quality of life has been reported in Jordan and India [13, 21]. However, the elderly in the Netherlands and Germany had a higher level of quality of life than those in our study (52.5 in the Netherlands, 53 in Germany) [22, 23]. It appears that the OHRQoL in southeast Asia is lower than that in West Asia and Europe [18].
Along with this, evidence suggests that experiences, expectations, and personal beliefs regarding oral conditions vary among different populations due to cultural differences [16, 24]. Besides, countries with a higher gross national product have a higher quality of life, and increased gross national product is related to higher life expectancy in different countries [25-27]. There is a gradient between income and health, and a higher level of health is often associated with higher income [25]. It shows that there is a gradient between the oral health of the elderly and objective (level of education, occupation, household income, and household wealth) and social subjective status (such as social position and socioeconomic status during childhood) as well as sociodemographic confounders such as age, gender and marital status [25, 28]. Some studies have emphasized that financial status, age, sex, and level of education are the most important predictors of quality of life and are even related to self-rated oral health [28].
A significant demographic transition has been experienced worldwide due to declining birth rates and increasing life expectancy, which led to an increase in the elderly population [1]. The population of the elderly over 60 years will reach 2 billion by 2050 [2]. This demographic change produces heavy challenges to health authorities and social planners due to the fast rate burden of chronic diseases including oral diseases among the elderly [3].
The elderly who has lost most teeth suffer from serious functional limitations, leading to nutritional problems [4]. The chief component of an elderly person’s life which affects his/her lifestyle, and physical, emotional, and mental happiness is oral health status [5]. Oral health is essential to individual general health and quality of life [6]. The American Dental Association defines oral health as a functional, structural, aesthetic, physiologic, and psychosocial state of well-being [6]. With aging, a significant decline in oral health may be observed, making older adults more frail, dependent, and disabled [6].
Assessment of oral health-related quality of life (OHRQoL) has an important role in clinical practice. OHRQoL refers to the subjective thoughts and beliefs of an individual regarding his oral conditions. The OHRQoL provides a complete assessment of oral function and health [7]. A variety of measures of the subjective impact of oral conditions on quality of life have been developed and used in oral health surveys during the last decades. One of the most well-established instruments is Geriatric Oral Health Assessment Index (GOHAI), introduced in 1990 and included 12 items in physical function, psychosocial function, and pain and discomfort domains [8].
However, in recent years, many investigations have assessed the quality of life-related to oral health in the elderly population. However, most of the studies were conducted on elderly living in nursing homes [9], institutionalized seniors [10], or elderly who were referred to dental clinics [11]. Based on these documents, there is no adequate information about the elderly who have relative health status, such as retired elderly. In addition, people with different cultural backgrounds may respond differently to GOHAI items. For instance, being edentulous (missing teeth) may have different levels of importance in various cultures. Therefore, the GOHAI must be tested in diverse cultures, languages, and geography.
Likewise, Guilan province in the North of Iran has the highest percentage of the elderly population in this country [12]. Given the high rate of aging in the population, it is necessary to pay attention to this part of society so that they will have a comfortable and high‑quality life. In Guilan, tooth loss is the most important oral change that occurs in the elderly. Over half of the elderly are edentulous, and a large percentage of them do not wear a denture. The mean number of remaining teeth in the elderly often ranges from 4 to 8 [10, 11]. Thus, the present study was conducted to determine oral health status and the OHRQoL among independently elderly members of retirement centers in the northern region of Iran.
Material and Methods
This descriptive-analytical cross-sectional study was conducted on retired elderlies between April and September of 2018. The participants were members of the Civil Servants Pension Organization (CSPO), which has covered more than 1,471,000 retirees and government employees in Iran. This organization is an independent legal entity under the governance of the Ministry of Welfare and Social Security and runs an insurance company. Also, Civil Servants Pension Organization had around 10,000 members in Guilan city. The sample size was calculated to be 196 according to the result of Daradkeh et al. [13], considering 95% CI, mean of 40.9±10.7, and d=1.5 score. Subjects were entered into the study consecutively daily and referred to the only available retirement center. The target population included retired elderly, without physical and mental disabilities, 60 years and older of both sexes, willing to participate in research, ability to answer questions, and communication.
The Geriatric Oral Health Assessment Index (GOHAI) is a 12-item instrument with three domains: physical function (eating, speech, and swallowing), psychosocial function (worry or concern regarding oral health, dissatisfaction with appearance, self-consciousness regarding oral health, and avoidance of social interaction because of oral problems), and pain or discomfort (medication used to relieve oral pain or discomfort). Each item in the GOHAI was rated on a 5-point Likert scale ranging from 1 (always) to 5 (never). The total score ranged from 12 to 60 points, with a higher score indicating a more favorable OHRQoL. Consequently, a total score between 12 and 36 indicated a poor quality of life, between 36 and 48 indicated a moderate quality of life, and between 48 and 60 indicated a good quality of life. The Persian version of the GOHAI exhibited acceptable reliability and validity to evaluate OHRQoL in the Iranian elderly population [14-16]. According to the results of a study about the reliability of the Persian version of GOHAI, Cronbach’s α (0.78) showed a high degree of internal consistency and homogeneity between items [14]. Also, regarding the discriminant validity, the respondents with higher GOHAI scores were associated with a lower number of carious and missing teeth [14].
Subjects were ensured that they could leave the study whenever they wished to do so. Hence written informed consent was obtained before the start of the study. As well as, the aim of the study and research procedures were explained to participants initially. The oral examination of the subjects took place in an appropriate room of the retirement center using a disposable mirror, a wooden spatula, and a flashlight. In the present study, a single examiner was trained under the supervision of an oral & Maxillofacial Medicine specialist to standardize the oral lesions diagnostic as much as possible. A single trained examiner calculated data that intra-examiner agreement (kappa coefficient=0.87) was considered excellent. First, an examiner recorded sociodemographic information such as age, gender, marital status, economic status, and smoking due to face-to-face interviews. Then, the oral health status was rated (good, moderate, poor) according to the participant's response to the question, “How would you describe the health of your mouth, teeth, and gums?”. Also, the researcher asked about the subjects’ perceptions of their need for dental treatment. Besides, subjects were asked about their oral hygiene frequency per day (twice a day or more, once a day, and sometimes), and their last dental visit one year ago. The main reason for seeking dental treatment at the last dental appointment was also asked and divided based on the problem (dental pain, oral and gingival problems, or routine check-ups). Moreover, dental and prosthetic status was assessed based on the number of remaining teeth in the mouth and partial/ complete dentures usage. Data on the presence of systemic diseases were asked directly from the subjects. Consequently, the researcher sequentially read GOHAI questionnaire items, and participants' responses were entered directly into the forms on the same day.
Data were analyzed using Statistical Package for Social Sciences software (SPSS, version 21). The independent t-test and ANOVA were used to compare the OHRQoL based on qualitative variables such as age, gender, and dental visits. If the assumptions were not met, non-parametric tests such as the Mann-Whitney U test and the Kruskal-Wallis test were used for comparisons. A significance level of P<0.05 was the criterion for a statistically significant effect.
Findings
A total of 196 retired elderly consisting of 115 (58.7%) males and 81 (41.3%) females were included in the present study. The mean age of participants was 67.7±6.2 years, with an age range of 60 to 86 years. The following characteristics were predominant: married (92.3%), a university education level (47.4%), visiting a dentist only when experiencing pain (77.6%), the last dental visit one year ago (59.2%), not smoking (94.4%). The financial status of the majority of participants (48.5%) was moderate. The majority (66.3%) stated that they had poor or moderate oral health status, and 75% believed they needed dental treatment; 44.9% rinsed their mouth at least once a day.
As shown in Diagram 1, the most common oral mucosal lesions in the participants were xerostomia, fissured tongue and dorsal tongue base varies, and denture stomatitis. The most common systemic diseases were hypertension, cardiac disease, diabetes mellitus and pulmonary diseases with equal prevalence, neurologic diseases, dementia, and cerebrovascular conditions. The study participants' mean number of remaining teeth was 15.9±9.7 (range 0 to 29).
Of all, 17.9% were edentulous, 100 51% had less than 20 teeth in their mouth, and 31.1% had more than 20 teeth in their mouth. Out of all participants, 35 were completely edentulous and had complete dentures, 79 did not have posterior teeth, 41 did not have any prosthesis, and 38 had partial dentures. Of all, 8 did not have the anterior teeth; out of which, 3 did not have any prosthesis, and 5 had partial dentures. Thirteen subjects (6.6%) did not have anterior or posterior teeth and had a partial denture. Sixty-one subjects had over 20 teeth, out of which 12 had dental implants.
Moreover, Diagram 2 presents the median score and percentile of the subjects’ answers to each item on the GOHAI questionnaire. According to the findings in the physical domain, 45% of the elderly had limitations in having a variety of foods (Q1), 37.8% had problems in biting or chewing the food (Q2), 16 had problems with deglutition (Q3), and 20 (0.5%) had problems with speech (Q4); 38.8% had difficulty in eating (Q5). In the psychosocial domain, 15 had limited their social encounters with others due to oral and dental problems (Q6); 60% were not satisfied with the appearance of their teeth (Q7), 45.5% were worried about their teeth or gingiva (Q9), 33.7% were over-concerned about their dental or gingival status (Q10) and 227 were embarrassed about eating in front of others (Q11). In the pain and discomfort domain, 21.9% used analgesics to alleviate pain (Q8), and 36.2% stated that their teeth or gingiva were hypersensitive to hot, cold, and sweet foods and drinks (Q12).
As illustrated in Table 1, there was a significant difference among the three domains' scores on the GOHAI questionnaire (p<0.001). In general, according to the qualitative analysis, the OHRQoL score was qualitatively suitable or moderate in 95 (48.5%) subjects, good in 91 (46.4%), and poor in 10 (5.1%). According to the Kruskal-Wallis test and Mann-Whitney U test, the quality of life score of those living alone (51.1±5.0) was higher than married individuals (47.2±6.3; p=0.013). Subjects with good (50.7±4.6) or excellent (55.0±1.4) self-rated oral health had higher OHRQoL than those with poor (44.7±6.8) self-rated oral health (p<0.001). The elderly with a self-perceived need for treatment had shown lower quality of life scores (46.8±6.4) than those with no self-perceived need for treatment (48.9±5.8) and those with no opinion in this respect (50.3±5.5; P=0.03).
The OHRQoL score was not significantly different based on the objective social status of participants, such as their age, sex, level of education, socioeconomic status, dental status, and prosthetic status. Table 2 presents the dental status and prosthetic status of subjects in general and separately for each domain of the GOHAI questionnaire.

Diagram 1) Frequency of oral mucosal lesions in participants
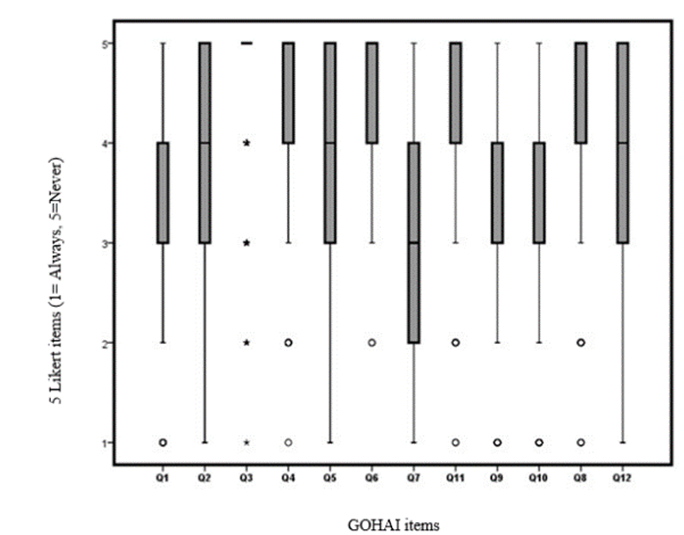
Diagram 2) Distribution of median scores and percentile of the subjects’ responses to GOHAI items
Table 1) The mean and standard deviation of total GOHAI score and domains scores
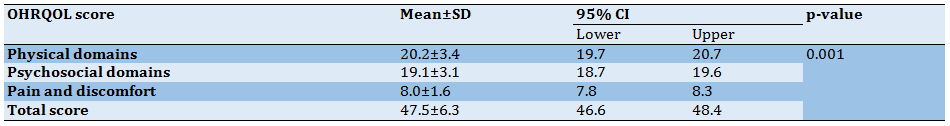
Table 2) Mean±SD of quality of life domains based on dental and prosthetic status
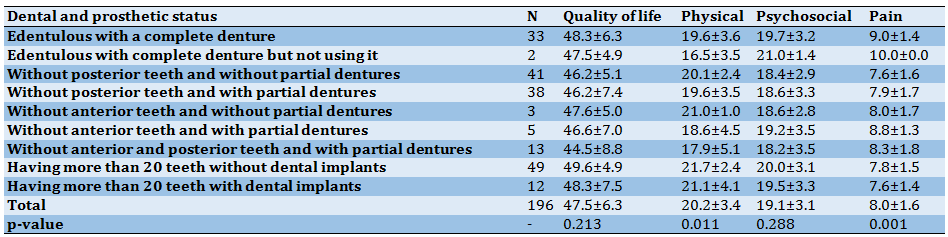
Table 3) OHRQoL score in presence of some oral conditions (Mean±SD)
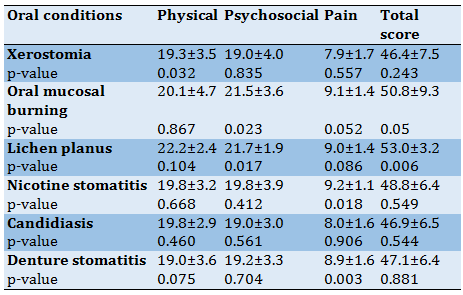
According to the Mann-Whitney U test, individuals with oral mucosal burning sensation and lichen planus acquired higher scores on the quality of life (Table 3).
In the physical domain, singles (living alone) compared to married individuals (coupled) (odds ratio=3.3, 95% CI:1-11.3) and those sought dental treatment only if they had pain compared to those with irregular dental visits (odds ratio=3.8, 95% CI:1.1-13) and those with over 20 teeth (odds ratio:5.36, 95% CI=2-14) compared to completely edentulous patients had higher quality of life in the physical domain. In the psychosocial domain, singles compared to married individuals (p=0.021, odds ratio=6.1-28.2) had higher quality of life scores, and those with a few teeth compared to completely edentulous patients (p=0.02, odds ratio=0.375, 95% CI: 0.1-1) had lower relative odds of quality of life median score in the psychosocial domain. In the pain and discomfort domain, those without self-perceived need for dental treatment (P=0.017, odds ratio=1.9, 95% CI:1.1-3.5), those with more than 20 teeth (odds ratio=0.243, 95% CI:0.1-0.7) and patients with fewer than 20 teeth compared to completely edentulous patients (p=0.011, odds ratio=0.261, 95% CI=0.1-0.7) had a higher median score of quality of life in pain and discomfort domain. In other words, completely edentulous patients had less pain and discomfort compared to dentate patients.
Discussion
The present study aimed to determine the oral health-related quality of life (OHRQoL) in the retired elderly population. The mean and standard deviation of GOHAI scores in the present study participants were 47.5±6.3. Similar results were reported in Malaysia, Lebanon, China, and France [17-20], while a lower quality of life has been reported in Jordan and India [13, 21]. However, the elderly in the Netherlands and Germany had a higher level of quality of life than those in our study (52.5 in the Netherlands, 53 in Germany) [22, 23]. It appears that the OHRQoL in southeast Asia is lower than that in West Asia and Europe [18].
Along with this, evidence suggests that experiences, expectations, and personal beliefs regarding oral conditions vary among different populations due to cultural differences [16, 24]. Besides, countries with a higher gross national product have a higher quality of life, and increased gross national product is related to higher life expectancy in different countries [25-27]. There is a gradient between income and health, and a higher level of health is often associated with higher income [25]. It shows that there is a gradient between the oral health of the elderly and objective (level of education, occupation, household income, and household wealth) and social subjective status (such as social position and socioeconomic status during childhood) as well as sociodemographic confounders such as age, gender and marital status [25, 28]. Some studies have emphasized that financial status, age, sex, and level of education are the most important predictors of quality of life and are even related to self-rated oral health [28].
Consequently, the GOHAI score in the present study was higher than it was reported in Hamadan [16]. Also, the GOHAI score in the current study was similar to the results of a study which was conducted in Babol [14]. It should be noted that the age of the participants in our study was higher than mentioned study. A higher level of literacy and better adherence to oral hygiene measures among individuals evaluated in our study and better access to dental care services for the members of the retirement centers can play a role in a higher quality of life of the elderly evaluated in our study to other studies. Along with this, older adults who participated in senior centers showed a better perception of OHRQoL in the Machado et al. study [6].
Similar to other studies, living alone affected both the physical and psychosocial domains, with single people having higher OHRQoLs than married individuals [28]. Studies that specifically evaluated the effect of marital status on oral, dental, and periodontal conditions have discussed that low marital quality can have significant adverse effects on the couple and their children. Evidence shows that the frequency of edentulous is lower in married individuals. There is a hypothesis that psychosocial factors, including marital quality, affect the immune system and significantly impact the host's response to oral diseases. Also, it affects the saliva flow, and by its reduction, the degradation of oral tissues occurs [29].
On the other hand, the lowest GOHAI score belonged to the psychosocial domain, which indicates that the main problem of the elderly is related to their concerns regarding oral health, dissatisfaction with their appearance, and avoiding social contact due to oral and dental conditions, which can explain the lower quality of life in married individuals [30]. Also, most participants were males, which raises a question regarding the significance of esthetic appearance for males [21]. Evidence shows that one's perception of his own oral and dental status is related to his mood, individual perception of life stresses, life satisfaction, marriage, self-perceived need for dental treatment, and self-respect [31, 32]. Besides, concerning the quality of life score of the elderly, those with a complete denture acquired a higher mean GOHAI score in the psychosocial domain compared to dentate patients with/without removable partial dentures [33]. Thus, the weight of questions in the psychosocial domain regarding having teeth and marriage can significantly affect the quality of life. The number of teeth more than 20 increases the quality of life in the physical domain [31].
Nevertheless, in the psychosocial domain, having a complete denture resulted in a higher quality of life than those with more than 20 teeth in their mouth. This issue may be due to the effect of the esthetic appearance of the teeth, which is highly important.
In contrast, among those with fewer than 20 teeth in their mouth, subjects without posterior teeth and no removable partial denture had a higher level of pain and discomfort and lower quality of life compared to those without anterior teeth and no removable partial denture [33]. Less number of teeth for mastication and the absence of anterior teeth have a great impact on OHRQoL and a further lower score of the physical domain in this index [34, 35].
The self-rated oral health of the majority of participants was poor or moderate in this study. Most subjects had the self-perceived need for dental treatment, but most stated that they would visit a dentist only if they had pain. This finding was expected considering the high frequency of patients with complete or partial edentulous [26, 31, 33]. Poor financial status and the insurance systems not covering dental services are mainly responsible for patients not seeking dental treatment.
In our study, most of the participants were retired teachers and had university or high-school levels of education. Previous studies have mainly reported that the level of education determines socioeconomic status and subsequently affects health status [19, 25, 26, 29-33]. Similar to other studies, the present study also showed that level of education affects the quality of life.
Conclusion
The findings indicated that the retired elderly who were members of the retirement centers had a moderate level of OHRQoL. The impact of oral health on the quality of life in the elderly population broadens the sources of information as epidemiological research beyond just clinical indicators. The obtained data on OHRQoL in the elderly can help decision-makers in the planning of oral health programs for the elderly.
Acknowledgments: We would like to thank the present study subjects for their participation in this research study and their willingness to share their experiences.
Ethical Permissions: The present study was commenced upon receiving approval from the Research Ethics Committee of Guilan University of Medical Sciences (IR. GUMS.1396.361).
Conflicts of Interests: The authors have no conflicts of interest to declare that are relevant to the content of this article.
Authors’ Contribution: Rabiei M (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Pakkhesal M (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (40%); Sobhi P (Third Author), Assistant Researcher/Statistical Analyst (10%); Masoudi Rad H (Fourth Author) Assistant Researcher/ Statistical Analyst (10%)
Funding/Support: No funding was received for conducting this study.
Similar to other studies, living alone affected both the physical and psychosocial domains, with single people having higher OHRQoLs than married individuals [28]. Studies that specifically evaluated the effect of marital status on oral, dental, and periodontal conditions have discussed that low marital quality can have significant adverse effects on the couple and their children. Evidence shows that the frequency of edentulous is lower in married individuals. There is a hypothesis that psychosocial factors, including marital quality, affect the immune system and significantly impact the host's response to oral diseases. Also, it affects the saliva flow, and by its reduction, the degradation of oral tissues occurs [29].
On the other hand, the lowest GOHAI score belonged to the psychosocial domain, which indicates that the main problem of the elderly is related to their concerns regarding oral health, dissatisfaction with their appearance, and avoiding social contact due to oral and dental conditions, which can explain the lower quality of life in married individuals [30]. Also, most participants were males, which raises a question regarding the significance of esthetic appearance for males [21]. Evidence shows that one's perception of his own oral and dental status is related to his mood, individual perception of life stresses, life satisfaction, marriage, self-perceived need for dental treatment, and self-respect [31, 32]. Besides, concerning the quality of life score of the elderly, those with a complete denture acquired a higher mean GOHAI score in the psychosocial domain compared to dentate patients with/without removable partial dentures [33]. Thus, the weight of questions in the psychosocial domain regarding having teeth and marriage can significantly affect the quality of life. The number of teeth more than 20 increases the quality of life in the physical domain [31].
Nevertheless, in the psychosocial domain, having a complete denture resulted in a higher quality of life than those with more than 20 teeth in their mouth. This issue may be due to the effect of the esthetic appearance of the teeth, which is highly important.
In contrast, among those with fewer than 20 teeth in their mouth, subjects without posterior teeth and no removable partial denture had a higher level of pain and discomfort and lower quality of life compared to those without anterior teeth and no removable partial denture [33]. Less number of teeth for mastication and the absence of anterior teeth have a great impact on OHRQoL and a further lower score of the physical domain in this index [34, 35].
The self-rated oral health of the majority of participants was poor or moderate in this study. Most subjects had the self-perceived need for dental treatment, but most stated that they would visit a dentist only if they had pain. This finding was expected considering the high frequency of patients with complete or partial edentulous [26, 31, 33]. Poor financial status and the insurance systems not covering dental services are mainly responsible for patients not seeking dental treatment.
In our study, most of the participants were retired teachers and had university or high-school levels of education. Previous studies have mainly reported that the level of education determines socioeconomic status and subsequently affects health status [19, 25, 26, 29-33]. Similar to other studies, the present study also showed that level of education affects the quality of life.
Conclusion
The findings indicated that the retired elderly who were members of the retirement centers had a moderate level of OHRQoL. The impact of oral health on the quality of life in the elderly population broadens the sources of information as epidemiological research beyond just clinical indicators. The obtained data on OHRQoL in the elderly can help decision-makers in the planning of oral health programs for the elderly.
Acknowledgments: We would like to thank the present study subjects for their participation in this research study and their willingness to share their experiences.
Ethical Permissions: The present study was commenced upon receiving approval from the Research Ethics Committee of Guilan University of Medical Sciences (IR. GUMS.1396.361).
Conflicts of Interests: The authors have no conflicts of interest to declare that are relevant to the content of this article.
Authors’ Contribution: Rabiei M (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Pakkhesal M (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (40%); Sobhi P (Third Author), Assistant Researcher/Statistical Analyst (10%); Masoudi Rad H (Fourth Author) Assistant Researcher/ Statistical Analyst (10%)
Funding/Support: No funding was received for conducting this study.
Article Type: Original Research |
Subject:
Oral Health Education/Promotion
Received: 2022/04/23 | Accepted: 2022/07/2 | Published: 2022/08/20
Received: 2022/04/23 | Accepted: 2022/07/2 | Published: 2022/08/20
References
1. Silva e Farias IP, Montenegro LD, Wanderley RL, de Pontes JC, Pereira AC, de Almeida LD, et al. Physical and psychological states interfere with health-related quality of life of institutionalized elderly: a cross-sectional study. BMC Geriatr. 2020;20(1):386-96. [Link] [DOI:10.1186/s12877-020-01791-6]
2. Azami-Aghdash S, Pournaghi-Azar F, Moosavi A, Mohseni M, Derakhshani N, Kalajahi RA. Oral health and related quality of life in older people: a systematic review and meta-analysis. Iran J Public Health. 2021;50(4):689-700. [Link] [DOI:10.18502/ijph.v50i4.5993]
3. Shokry AA, Adel MR, Rashad AE. Educational program to improve quality of life among elderly regarding oral health. Future Dent J. 2018;4(2):211-5. [Link] [DOI:10.1016/j.fdj.2018.07.002]
4. Motallebnejad M, Mehdizadeh S, Najafi N, Sayyadi F. The evaluation of oral health-related factors on the quality of life of the elderly in Babol. Contemp Clin Dent. 2015;6(3):313-7. [Link] [DOI:10.4103/0976-237X.161867]
5. Naik SP, Hota S, Bhushan P, Sam G, Kumari VV, Shetty N. Evaluation of oral health-related quality of life in patient with removable prosthesis: a cross-sectional study. J Pharm Bioallied Sci. 2020;12(Suppl 1):S210-3. [Link] [DOI:10.4103/jpbs.JPBS_63_20]
6. Machado Luz FW, Ribeiro Silva AE, Perroni AP, Goettems ML, Boscato N. Impact of seniors centers on oral health-related quality of life of older adults. Revista de Saúde Pública. 2020;54:7. [Link] [DOI:10.11606/s1518-8787.2020054001648]
7. Locker D, Allen F. What do measures of 'oral health‐related quality of life' measure?. Community Dent Oral Epidemiol. 2007;35(6):401-11. [Link] [DOI:10.1111/j.1600-0528.2007.00418.x]
8. Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. J Dent Educ. 1990;54(11):680-7. [Link] [DOI:10.1002/j.0022-0337.1990.54.11.tb02481.x]
9. Klotz AL, Tauber B, Schubert AL, Hassel AJ, Schröder J, Wahl HW, et al. Oral health‐related quality of life as a predictor of subjective well‐being among older adults- A decade‐long longitudinal cohort study. Community Dent Oral Epidemiol. 2018;46(6):631-8. [Link] [DOI:10.1111/cdoe.12416]
10. Rabiei M, Kasemnezhad E, Masoudi rad H, Shakiba M, Pourkay H. Prevalence of oral and dental disorders in institutionalised elderly people in Rasht, Iran. Gerodontology. 2010;27(3):174-7. [Link] [DOI:10.1111/j.1741-2358.2009.00313.x]
11. Rabiei M, Shakiba M, Masoudirad H, Javadinia A. Dental status among urban and rural elderly of Talesh (2009). J Inflamm Dis. 2011;15(3):69-75. [Link]
12. Hatamzadeh Y, Hosseinzadeh A. Toward a deeper understanding of elderly walking for transport: an analysis across genders in a case study of Iran. J Transp Health. 2020 September. [Link] [DOI:10.1016/j.jth.2020.100949]
13. Daradkeh S, Khader YS. Translation and validation of the Arabic version of the geriatric oral health assessment index (GOHAI). J Oral Sci. 2008;50(4):453-9. [Link] [DOI:10.2334/josnusd.50.453]
14. Motallebnejad M, Mottaghi K, Mehdizadeh S, Alaeddini F, Bijani A. Reliability and validity of the Persian version of the general oral health assessment index (GOHAI). Casp J Dent Res. 2013;2(1):8-17. [Persian] [Link]
15. Navabi N, Salahi S. Assessment of oral health assessment index (GOHAI) validity in Iranian elderly population. Res Dent Sci. 2012;9(3):161-9. [Persian] [Link]
16. Rezaei M, Rashedi V, Khedmati Morasae E. A Persian version of geriatric oral health assessment index. Gerodontology. 2016;33(3):335-41. [Link] [DOI:10.1111/ger.12161]
17. El Osta N, Tubert-Jeannin S, Hennequin M, Naaman NBA, El Osta L, Geahchan N. Comparison of the OHIP-14 and GOHAI as measures of oral health among elderly in Lebanon. Health Qual Life Outcomes. 2012;10:131. [Link] [DOI:10.1186/1477-7525-10-131]
18. Othman WNW, Muttalib KA, Bakri R, et al. Validation of the geriatric oral health assessment index (GOHAI) in the Malay language. J Public Health Dent. 2006;66(3):199-204. [Link] [DOI:10.1111/j.1752-7325.2006.tb02580.x]
19. Tubert‐Jeannin S, Riordan PJ, Morel‐Papernot A, Porcheray S, Saby‐Collet S. Validation of an oral health quality of life index (GOHAI) in France. Community Dent Oral Epidemiol. 2003;31(4):275-84. [Link] [DOI:10.1034/j.1600-0528.2003.t01-1-00006.x]
20. Wong MC, Liu JK, Lo EC. Translation and validation of the Chinese version of GOHAI. J Public Health Dent. 2002;62(2):78-83. [Link] [DOI:10.1111/j.1752-7325.2002.tb03426.x]
21. Deshmukh SP, Radke UM. Retracted: translation and validation of the Hindi version of the Geriatric Oral Health Assessment Index. Gerodontology. 2012;29(2):e1052-8. [Link] [DOI:10.1111/j.1741-2358.2011.00609.x]
22. Hassel AJ, Rolko C, Koke U, Leisen J, Rammelsberg P. A German version of the GOHAI. Community Dent Oral Epidemiol. 2008;36(1):34-42. [Link]
23. Niesten D, Witter D, Bronkhorst E, Creugers N. Validation of a Dutch version of the geriatric oral health assessment index (GOHAI-NL) in care-dependent and care-independent older people. BMC Geriatr. 2016;16:53. [Link] [DOI:10.1186/s12877-016-0227-0]
24. Tajvar M, Arab M, Montazeri A. Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health. 2008;8:323. [Link] [DOI:10.1186/1471-2458-8-323]
25. Marmot M. The influence of income on health: views of an epidemiologist. Health Aff. 2002;21(2):31-46. [Link] [DOI:10.1377/hlthaff.21.2.31]
26. Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: the role of subjective social status. Soc Sci Med. 2008;67(2):330-40. [Link] [DOI:10.1016/j.socscimed.2008.03.038]
27. Tsakos G, Demakakos P, Breeze E, Watt RG. Social gradients in oral health in older adults: findings from the English longitudinal survey of aging. Am J Public Health. 2011;101(10):1892-9. [Link] [DOI:10.2105/AJPH.2011.300215]
28. Tsakos G, Sabbah W, Chandola T, et al. Social relationships and oral health among adults aged 60 years or older. Psychosom Med. 2013;75(2):178-86. [Link] [DOI:10.1097/PSY.0b013e31827d221b]
29. Marcenes W, Sheiham A. The relationship between marital quality and oral health status. Psychol Health. 1996;11(3):357-69. [Link] [DOI:10.1080/08870449608400264]
30. Sanders AE, Slade GD, Turrell G, John Spencer A, Marcenes W. The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol. 2006;34(4):310-9. [Link] [DOI:10.1111/j.1600-0528.2006.00286.x]
31. Benyamini Y, Leventhal H, Leventhal EA. Self-rated oral health as an independent predictor of self-rated general health, self-esteem and life satisfaction. Soc Sci Med. 2004;59(5):1109-16. [Link] [DOI:10.1016/j.socscimed.2003.12.021]
32. Locker D, Gibson B. Discrepancies between self‐ratings of and satisfaction with oral health in two older adult populations. Community Dent Oral Epidemiol. 2005;33(4):280-8. [Link] [DOI:10.1111/j.1600-0528.2005.00209.x]
33. Atchison KA, Gift HC. Perceived oral health in a diverse sample. Adv Dent Res. 1997;11(2):272-80. [Link] [DOI:10.1177/08959374970110021001]
34. Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126. [Link] [DOI:10.1186/1477-7525-8-126]
35. Heydecke G, Locker D, Awad MA, Lund JP, Feine JS. Oral and general health‐related quality of life with conventional and implant dentures. Community Dent Oral Epidemiol. 2003;31(3):161-8. [Link] [DOI:10.1034/j.1600-0528.2003.00029.x]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |