Volume 10, Issue 1 (2022)
Health Educ Health Promot 2022, 10(1): 183-191 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Osman Ali S, Kamel N, Holmes S, Abdelfatah Arafat A. Effect of Benson's Relaxation Technique on Psychological Distress and Sleep Quality among Elderly. Health Educ Health Promot 2022; 10 (1) :183-191
URL: http://hehp.modares.ac.ir/article-5-58542-en.html
URL: http://hehp.modares.ac.ir/article-5-58542-en.html
1- Department of Psychiatric and Mental Health Nursing, Faculty of Nursing, Suez Canal University, Ismailia, Egypt
2- Department of Psychiatric and Mental Health Nursing, Alexandria University, Alexandria, Egypt
3- Nursing Researcher-King Fahad Specialist Hospital, Dammam, Saudi Arabia
4- Department of Psychiatric and Mental Health Nursing, Faculty of Nursing, Zagazig University, Zagazig, Egypt
2- Department of Psychiatric and Mental Health Nursing, Alexandria University, Alexandria, Egypt
3- Nursing Researcher-King Fahad Specialist Hospital, Dammam, Saudi Arabia
4- Department of Psychiatric and Mental Health Nursing, Faculty of Nursing, Zagazig University, Zagazig, Egypt
Keywords: Anxiety [MeSH], Relaxation Technique [MeSH], Depression [MeSH], Elderly [MeSH], Sleep [MeSH], Quality Stress [MeSH]
Full-Text [PDF 511 kb]
(4347 Downloads)
| Abstract (HTML) (2836 Views)
The Research Ethics Committee of Zagazig University's Faculty of Nursing permitted the researchers to perform the study. After an explanation of the study's goal, the Director of the Faculty of Nursing, Zagazig University, issued letters to the Directors of the geriatric social club in Zagazig City, El-Resala geriatric home in Zagazig City, and Met-Ghamr geriatric home in Met-Ghamr city, obtaining official approval to conduct the study. After a thorough description of the study's goal, all elderly people signed a written consent form. The elderly were informed that all obtained data would be treated with strict confidentiality and would only be utilized for the study's purposes and that the study procedures would not hurt the participants. The researchers stressed that participation in the study is completely voluntary and that the elderly's anonymity was ensured by data coding. They were also told that they might leave the study at any time and without giving a reason. As a result, the study subjects' privacy and the confidentiality of the data obtained were guaranteed. The original authors also granted official permission for the use of the DASS and PSQI scales. A pilot study was conducted on 10% (10 elders) of the population to assess the content and clarity of the tools, as well as to estimate the time required to fill it out. The most important suggested adjustments were implemented, primarily restating and simplifying the semantic language used in the claims. The pilot study's sample was not included in the main study's sample.
Before the administration of the survey, the investigators interacted with the elderly in the study sample, introduced themselves, and discussed the study's purpose and benefits, as well as its processes, to secure their consent, build trust, and earn their cooperation and confidence. Upon obtaining their informed oral consent, the investigators started to fill out the questionnaire form through personal interviewing. They read and explained each item to the elderly and recorded their responses to each item. It was difficult to gather all elderly at the same time; so they were divided into 9 groups and each group consisted of 9-10 elderly. The investigators implemented the BRT for each group on scheduled times and days. The elderly in the study sample were exposed to twelve / one-hour-long sessions of BRT, for a total period of three months, Saturdays for the first, second, third, fourth, and fifth group, Tuesdays for the 6th and 7th group, and Wednesdays for 8th and 9th group from 10 Am to 2 pm in the hall of geriatric club and homes. The instruction of BRT included the following steps:
- Take a seat in a restful posture.
- Keep your eyes closed.
- Relax all muscles, starting at the feet and working up to the top of the head, and relax all regions of the body.
- Take a deep breath through your nose. When exhaling, exhale from the lips, repeat one word or number (as Allah), inhale, and exhale with ease and confidence.
- Do this for a total of 20 minutes. Try to keep their body and muscles relaxed while mentally repeating the desired word. Then slowly open your eyes and remain motionless for a few minutes.
- Through an attractive colored booklet developed by the researchers, as well as demonstration, re-demonstration, and videos, the elderly learned about the benefits of the method and learned about the relaxation technique. Their caregivers were asked to watch and guide elders in their geriatric homes/clubs to correctly execute the technique twice a day, in the morning and evening, for 20 minutes for two months.
- The same topic was presented utilizing the same teaching methods, conversations, and handouts to guarantee that all of the seniors in the five groups were exposed to the same information and learning experiences.
- To ensure that the elderly understood the BRT content, each session began with a review of what had been covered in the previous session and the goals of the new one, using basic language appropriate for the participants' educational level.
- During the sessions, motivation and reinforcement strategies such as praise and recognition were utilized to increase engagement and learning.
- During sessions, the investigators asked the elders to perform BRT in front of them to ensure that they elderly person completed it correctly.
- To get the elders' attention and motivate them, various instructional methods were tried. Interactive lectures, group discussions, brainstorming, demonstration re-demonstration, and role-playing were among the activities. PowerPoint presentations, YouTube videos, and a guidebook were among the training materials.
- The study was completed between the beginning of June and the end of October 2020.
- Evaluation: all elderly in the study sample were interviewed using the same data collection form to reassess their level of stress, anxiety, depression, and sleep quality (post-test) immediately after implementation of BRT.
- As a result of pandemic covid-19, it is necessary of taking safety precautions such as physical distancing, wearing a mask, keeping hales well ventilated, avoiding crowds, and cleaning hands.
The statistical package for social science (SPSS), version 20.0 for Windows, was used to gather, tabulate, and statistically analyze all data. The mean, SD, and range were used to convey quantitative data, while absolute and relative frequencies were used to express qualitative data (percentage). To compare two dependent groups of non-normally distributed variables, the Wilcoxon signed-rank test was utilized. The Chi-square test was used to compare the percentages of categorical variables. To assess the relationship between various study variables, the Spearman correlation coefficient was calculated, with the plus (+) sign indicating direct correlation and the minus (-) sign indicating inverse correlation. Furthermore, numbers close to 1 suggest a significant connection, whereas values close to 0 indicate a weak correlation. All of the tests were conducted in pairs. Statistical significance was defined as a p-value of less than 0.05.
Findings
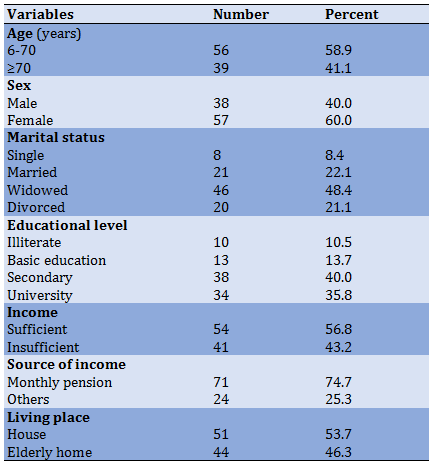
A total of 95 elderly people (Mean±SD=68.84±4.69) took part in the study, including 50 from the Geriatric social club in Zagazig City, 20 from El-Resala geriatric home in Zagazig City, and 25 from the Geriatric home at Met-Ghamr City, Egypt. Most of them were less than 70 years old, female, and widowed (Table 1).
Almost three-quarters of elders in the study sample didn't practice regular physical exercise. The majority of elders had chronic diseases, as well, and the majority of them take regular treatment for chronic diseases. Slightly more than three-fifths of elders did not have a disability (Table 2).
The majority of elders in the study had unsatisfactory knowledge about BRT during the pre-intervention phase (1.24±1.99). This score increased in the post-intervention phase (4.79±1.39). Additionally, the change in knowledge score was 2.85% (Table 3, p<0.001).
About two-thirds of elders in the study group had severe depression during the pre-intervention phase (45.14±9.9), and this was decreased in the post-intervention phase (27.16±7.55); the improvement in depression score was 39.38%. Slightly less than two-thirds of elders had severe anxiety in the pre-intervention phase (44.61±10.41), and this was decreased in the post-intervention phase (26.6±8.32); while the improvement of anxiety score was 0.40%. Less than three-quarters of elders had severe stress in the pre-intervention phase (47.13±8.95), this decreased in the post-intervention phase (28.64±7.97); the improvement of stress score was 0.39% (Table 4; p<0.001).
The majority of elders in the study sample had poor sleep quality in the pre-intervention phase, which decreased in the post-intervention phase to 50.5%. Sleep quality was enhanced following the implementation of the BRT (Diagram 1).
There was a negative significant correlation between stress and BRT, and between anxiety, depression, and stress and sleep quality, while there was a positive significant correlation between BRT and sleep quality (Table 5).
Table 1) Demographic characteristics of studied elderly (n=95)
Full-Text: (827 Views)
Introduction
Fear and uncertainty of the unknown, along with challenges from rapid changes and limitations are potential causes of stress and other mental health issues. The Covid-2019 pandemic sparked worldwide distress when the World Health Organization (WHO) confirmed [1]. The virus affected all segments of the population, with morbidity and mortality in the elderly being disproportionately affected [2-4].
Elderly individuals already affected by physical aging, declining health, the emergence of chronic diseases, loss of income or financial insecurity, and reduced social support or interactions from family members and friends, and are susceptible to anxiety, stress, depression, sleep problems, in addition to fear from COVID-19 infections [2, 5, 6].
Psychological distress is a concept that does not have an absolute definition [7, 8]. It used to cover everything from mild ailments to major illnesses [9]. In this study, the term psychological distress is measured using the Depression, Anxiety and Stress Scale (DASS), which includes several emotional components, the most notable of which are despair and anxiety. However, distress is one of the disturbing but predictable psychological disorders that may occur to the elderly and may be an inevitable reaction to feeling insecure or threatened. Increased and persistent feelings of anxiety and depression interfere with the daily functions and activities of older adults. In addition, distress may lead to negative mental health effects for older adults in the form of feelings of stress, anxiety or tension, a sense of impending danger, difficulty concentrating, and poor sleep quality [10].
Poor sleep quality is another problem that may occur to the elderly. It is defined as difficulty initiating sleep or waking up early, or difficulty that occurs despite adequate opportunities and conditions to fall asleep. Sleep deprivation has been linked to several forms of daytime impairment, such as fatigue, low energy, mood disturbances, and excessive worry or anxiety [11]. It is caused by sympathetic activation, the hypothalamic-pituitary-adrenal axis is also disrupted (HPA). Therefore, high blood pressure can have devastating effects on the health of older adults. Poor sleep quality has been linked to several undesirable outcomes including cognitive and functional impairment [12]. So managing stress and anxiety is important for overall health. Older adults with insomnia are more likely to develop depression and anxiety [13]. Thus, managing poor sleep quality and getting enough sleep through relaxation techniques is important for improving the well-being of the elderly [14].
Relaxation techniques are a type of complementary alternative therapy (CAT) known as anxiety reduction interventions. The use of relaxation techniques has shown significant effects on both the physical and psychological state of the elderly. These interventions help the elderly deal with anxiety by slowing down the body and calming the mind. One relaxation technique is Benson's Relaxation Technique (BRT) developed by Benson et al. [15]. BRT is an easy and effective method of nursing intervention that has been shown to produce significant changes in physical and emotional responses to distress. It includes directed breathing, relaxation sessions, and the use of progressive muscle relaxation, controlled breathing, and images to induce a relaxation response [16].
So, supporting good health is important to prevent the consequences of aging and fear of COVID-19. Programs to improve or maintain the health of elderly individuals are needed to achieve this goal, as frail elderly have been reported to be more likely to die from COVID-19 [17]. Once a person's vulnerability is identified, best practices support the implementation of a comprehensive plan to support and improve care [18]. Elderly persons who live in nursing homes or long-term care facilities and who are under the care of health care workers at all times may be more involved and supervised in these programs.
Nurses have an essential role in this matter. The scope of nursing is to meet the basic needs of the human being and to promote sleep as one of these needs. Improving older adults' knowledge and use of BRT is vital. Including health education guidelines and practices such as managing physical activity, exercises that increase immunity and reduce stress, anxiety, and depression and improve sleep quality can improve the physical and psychological health of older adults and their outcomes [19]. Accordingly, this study was conducted to assess the effect of BRT on psychological distress and sleep quality among the elderly during the COVID-19 pandemic.
The importance of this study is that by applying BRT to older adults at increased risk of contracting COVID-19, they will have fewer symptoms and be better able to manage or reduce the negative impact of stress, anxiety, depression, or sleep disturbances, enjoy a higher quality of sleep, and more fulfilling life and overall sense of security and high quality of life (QOL). The better the QOL of the elderly is the better their well-being. So, we wish the elderly well despite the challenges during this pandemic period.
This study aimed to assess the impact of BRT on psychological distress and sleep quality among older people during COVID 19 pandemic.
Methods
To fulfill the study's aim, a one-group pre/posttest was used in a quasi-experimental research design. The research was carried out in three locations: a senior social club in Zagazig City, the El-Resala geriatric home in Zagazig City, and the Geriatric home in Met Ghamr City, Egypt. For the elderly, these places provide recreational and social services as well as some low-cost medical care. samples included elderly people from the geriatric social club and geriatric homes in the above-mentioned settings. Open Epi [20], Version 3, and an open-source calculator were used to calculate the sample size. Using a 95% two-sided confidence level and a minimum of 80% study power, 95 senior adults were chosen randomly from the Geriatric Social Club in Zagazig City, the El-Resala geriatric residence in Zagazig City, and the geriatric home in Met Ghamr City. Purposive sampling was employed in the recruitment of this study's individuals who are 60 years old and older, with no cognitive or psychiatric disorders.
For data collection, three tools were used:
The interview questionnaire sheet consists of 2 sections:
-Part I: Age, sex, educational level, marital status, income, source of current income, living place, physical activity, smoking status, presence of chronic diseases, presence of disabilities, and use of assistance methods are among the demographic features.
-Part II: The investigators prepared the study subject's relaxation technique knowledge after a thorough evaluation of current literature and expert opinions for content validity to assess geriatric knowledge of BRT [15]. This tool asked three questions about BRT's definition, benefits, instructions, and impact on stress, anxiety, depression, and sleep quality. For each knowledge area, a completely correct response was scored two points, one point was given when the response was correct and incomplete, and zero point was given when the response was incorrect. The scores of the items were added together for each area of knowledge, and the total was divided by the number of items, yielding a mean score for the section. These results were converted to a percentage score. The elders' knowledge was deemed satisfactory if the score was 50% or higher, and unsatisfactory if the score was less than 50%.
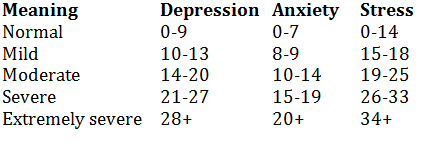
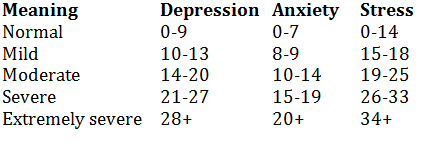
Depression Anxiety Stress Scales (DASS): This scale was constructed by Lovibond & Lovibond [21], and translated into Arabic by Taouk et al. [22]. It is intended to measure the three correlated negative emotional states (depression, anxiety, and stress). The scale consists of 42 self-report items rated on a 4-point Likert scale: “always”, “often”, “sometimes”, and “never”, reflecting the frequency or severity of the participant's experience. Each of the three negative emotional states has 14 items. Higher summed score items indicate more severe symptoms of depression, anxiety, and stress. The responses "always, " "often, " "occasionally, " and "never" were all given a score ranging from 4 to 1. The overall score is calculated by adding the scores of each of the negative emotional states' items. The total scores were divided by the number of items for each state, yielding a mean score for the component, and means and standard deviations were calculated. These results were converted to a percentage score. According to the percentile of the score received, the state was classified as mild, moderate, severe, or extreme:
The Pittsburgh Sleep Quality Index (PSQI): This tool, which was adapted from Buysse et al. [23], consists of a 19-item self-report questionnaire designed to measure sleep quality and disturbances over one month, resulting in seven sleep components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. The initial PSQI questions inquire about respondents' normal bedtime, length of time to fall asleep, usual wake-up time, and definite sleep duration. The remaining 15 Likert-type questions concern the frequency of sleep disruptions and subjective sleep quality in the previous month. Each item is graded on a scale of 0 to 3, with 0 denoting little difficulty and 3 denoting extreme difficulty. Subjective sleep quality (item 6), sleep latency (items 2 and 5a), sleep duration (item 4), habitual sleep efficiency (items 1, 3, and 4), sleep disturbances (items 5b to 5j), use of sleep medications (item 7) and daytime dysfunction (item 8) are the seven component scores or subscales derived from the 19 items (items 8 and 9). Component scores vary from 0 to 3, with 0 representing no difficulty and 3 indicating extreme difficulty. Furthermore, the seven component scores are added together to produce a single universal score ranging from 0 to 21, with larger values indicating lower sleep quality. The global score has a threshold of >5, which has been used to distinguish between good and bad sleepers. Good sleepers have a score of 5 or less, whereas poor sleepers have a score of more than 5. In this study, the Arabic version of this instrument [24] was used.
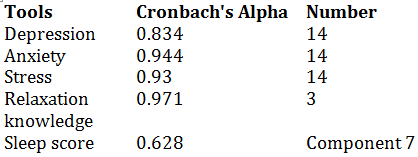
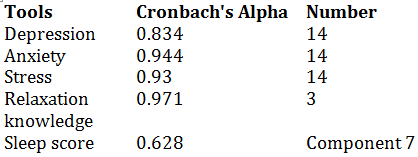
To meet the study's criteria for data collection tool reliability, a panel of three nursing experts from psychiatric and mental health nursing, gerontological nursing, and geriatric medicine tested and evaluated the tools for face and content validity, as well as relevance and comprehensiveness, clarity, applicability, and ease of implementation. The tools' reliability was determined by calculating the Cronbach alpha coefficient and measuring their internal consistency:
Fear and uncertainty of the unknown, along with challenges from rapid changes and limitations are potential causes of stress and other mental health issues. The Covid-2019 pandemic sparked worldwide distress when the World Health Organization (WHO) confirmed [1]. The virus affected all segments of the population, with morbidity and mortality in the elderly being disproportionately affected [2-4].
Elderly individuals already affected by physical aging, declining health, the emergence of chronic diseases, loss of income or financial insecurity, and reduced social support or interactions from family members and friends, and are susceptible to anxiety, stress, depression, sleep problems, in addition to fear from COVID-19 infections [2, 5, 6].
Psychological distress is a concept that does not have an absolute definition [7, 8]. It used to cover everything from mild ailments to major illnesses [9]. In this study, the term psychological distress is measured using the Depression, Anxiety and Stress Scale (DASS), which includes several emotional components, the most notable of which are despair and anxiety. However, distress is one of the disturbing but predictable psychological disorders that may occur to the elderly and may be an inevitable reaction to feeling insecure or threatened. Increased and persistent feelings of anxiety and depression interfere with the daily functions and activities of older adults. In addition, distress may lead to negative mental health effects for older adults in the form of feelings of stress, anxiety or tension, a sense of impending danger, difficulty concentrating, and poor sleep quality [10].
Poor sleep quality is another problem that may occur to the elderly. It is defined as difficulty initiating sleep or waking up early, or difficulty that occurs despite adequate opportunities and conditions to fall asleep. Sleep deprivation has been linked to several forms of daytime impairment, such as fatigue, low energy, mood disturbances, and excessive worry or anxiety [11]. It is caused by sympathetic activation, the hypothalamic-pituitary-adrenal axis is also disrupted (HPA). Therefore, high blood pressure can have devastating effects on the health of older adults. Poor sleep quality has been linked to several undesirable outcomes including cognitive and functional impairment [12]. So managing stress and anxiety is important for overall health. Older adults with insomnia are more likely to develop depression and anxiety [13]. Thus, managing poor sleep quality and getting enough sleep through relaxation techniques is important for improving the well-being of the elderly [14].
Relaxation techniques are a type of complementary alternative therapy (CAT) known as anxiety reduction interventions. The use of relaxation techniques has shown significant effects on both the physical and psychological state of the elderly. These interventions help the elderly deal with anxiety by slowing down the body and calming the mind. One relaxation technique is Benson's Relaxation Technique (BRT) developed by Benson et al. [15]. BRT is an easy and effective method of nursing intervention that has been shown to produce significant changes in physical and emotional responses to distress. It includes directed breathing, relaxation sessions, and the use of progressive muscle relaxation, controlled breathing, and images to induce a relaxation response [16].
So, supporting good health is important to prevent the consequences of aging and fear of COVID-19. Programs to improve or maintain the health of elderly individuals are needed to achieve this goal, as frail elderly have been reported to be more likely to die from COVID-19 [17]. Once a person's vulnerability is identified, best practices support the implementation of a comprehensive plan to support and improve care [18]. Elderly persons who live in nursing homes or long-term care facilities and who are under the care of health care workers at all times may be more involved and supervised in these programs.
Nurses have an essential role in this matter. The scope of nursing is to meet the basic needs of the human being and to promote sleep as one of these needs. Improving older adults' knowledge and use of BRT is vital. Including health education guidelines and practices such as managing physical activity, exercises that increase immunity and reduce stress, anxiety, and depression and improve sleep quality can improve the physical and psychological health of older adults and their outcomes [19]. Accordingly, this study was conducted to assess the effect of BRT on psychological distress and sleep quality among the elderly during the COVID-19 pandemic.
The importance of this study is that by applying BRT to older adults at increased risk of contracting COVID-19, they will have fewer symptoms and be better able to manage or reduce the negative impact of stress, anxiety, depression, or sleep disturbances, enjoy a higher quality of sleep, and more fulfilling life and overall sense of security and high quality of life (QOL). The better the QOL of the elderly is the better their well-being. So, we wish the elderly well despite the challenges during this pandemic period.
This study aimed to assess the impact of BRT on psychological distress and sleep quality among older people during COVID 19 pandemic.
Methods
To fulfill the study's aim, a one-group pre/posttest was used in a quasi-experimental research design. The research was carried out in three locations: a senior social club in Zagazig City, the El-Resala geriatric home in Zagazig City, and the Geriatric home in Met Ghamr City, Egypt. For the elderly, these places provide recreational and social services as well as some low-cost medical care. samples included elderly people from the geriatric social club and geriatric homes in the above-mentioned settings. Open Epi [20], Version 3, and an open-source calculator were used to calculate the sample size. Using a 95% two-sided confidence level and a minimum of 80% study power, 95 senior adults were chosen randomly from the Geriatric Social Club in Zagazig City, the El-Resala geriatric residence in Zagazig City, and the geriatric home in Met Ghamr City. Purposive sampling was employed in the recruitment of this study's individuals who are 60 years old and older, with no cognitive or psychiatric disorders.
For data collection, three tools were used:
The interview questionnaire sheet consists of 2 sections:
-Part I: Age, sex, educational level, marital status, income, source of current income, living place, physical activity, smoking status, presence of chronic diseases, presence of disabilities, and use of assistance methods are among the demographic features.
-Part II: The investigators prepared the study subject's relaxation technique knowledge after a thorough evaluation of current literature and expert opinions for content validity to assess geriatric knowledge of BRT [15]. This tool asked three questions about BRT's definition, benefits, instructions, and impact on stress, anxiety, depression, and sleep quality. For each knowledge area, a completely correct response was scored two points, one point was given when the response was correct and incomplete, and zero point was given when the response was incorrect. The scores of the items were added together for each area of knowledge, and the total was divided by the number of items, yielding a mean score for the section. These results were converted to a percentage score. The elders' knowledge was deemed satisfactory if the score was 50% or higher, and unsatisfactory if the score was less than 50%.
Depression Anxiety Stress Scales (DASS): This scale was constructed by Lovibond & Lovibond [21], and translated into Arabic by Taouk et al. [22]. It is intended to measure the three correlated negative emotional states (depression, anxiety, and stress). The scale consists of 42 self-report items rated on a 4-point Likert scale: “always”, “often”, “sometimes”, and “never”, reflecting the frequency or severity of the participant's experience. Each of the three negative emotional states has 14 items. Higher summed score items indicate more severe symptoms of depression, anxiety, and stress. The responses "always, " "often, " "occasionally, " and "never" were all given a score ranging from 4 to 1. The overall score is calculated by adding the scores of each of the negative emotional states' items. The total scores were divided by the number of items for each state, yielding a mean score for the component, and means and standard deviations were calculated. These results were converted to a percentage score. According to the percentile of the score received, the state was classified as mild, moderate, severe, or extreme:
The Pittsburgh Sleep Quality Index (PSQI): This tool, which was adapted from Buysse et al. [23], consists of a 19-item self-report questionnaire designed to measure sleep quality and disturbances over one month, resulting in seven sleep components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. The initial PSQI questions inquire about respondents' normal bedtime, length of time to fall asleep, usual wake-up time, and definite sleep duration. The remaining 15 Likert-type questions concern the frequency of sleep disruptions and subjective sleep quality in the previous month. Each item is graded on a scale of 0 to 3, with 0 denoting little difficulty and 3 denoting extreme difficulty. Subjective sleep quality (item 6), sleep latency (items 2 and 5a), sleep duration (item 4), habitual sleep efficiency (items 1, 3, and 4), sleep disturbances (items 5b to 5j), use of sleep medications (item 7) and daytime dysfunction (item 8) are the seven component scores or subscales derived from the 19 items (items 8 and 9). Component scores vary from 0 to 3, with 0 representing no difficulty and 3 indicating extreme difficulty. Furthermore, the seven component scores are added together to produce a single universal score ranging from 0 to 21, with larger values indicating lower sleep quality. The global score has a threshold of >5, which has been used to distinguish between good and bad sleepers. Good sleepers have a score of 5 or less, whereas poor sleepers have a score of more than 5. In this study, the Arabic version of this instrument [24] was used.
To meet the study's criteria for data collection tool reliability, a panel of three nursing experts from psychiatric and mental health nursing, gerontological nursing, and geriatric medicine tested and evaluated the tools for face and content validity, as well as relevance and comprehensiveness, clarity, applicability, and ease of implementation. The tools' reliability was determined by calculating the Cronbach alpha coefficient and measuring their internal consistency:
The Research Ethics Committee of Zagazig University's Faculty of Nursing permitted the researchers to perform the study. After an explanation of the study's goal, the Director of the Faculty of Nursing, Zagazig University, issued letters to the Directors of the geriatric social club in Zagazig City, El-Resala geriatric home in Zagazig City, and Met-Ghamr geriatric home in Met-Ghamr city, obtaining official approval to conduct the study. After a thorough description of the study's goal, all elderly people signed a written consent form. The elderly were informed that all obtained data would be treated with strict confidentiality and would only be utilized for the study's purposes and that the study procedures would not hurt the participants. The researchers stressed that participation in the study is completely voluntary and that the elderly's anonymity was ensured by data coding. They were also told that they might leave the study at any time and without giving a reason. As a result, the study subjects' privacy and the confidentiality of the data obtained were guaranteed. The original authors also granted official permission for the use of the DASS and PSQI scales. A pilot study was conducted on 10% (10 elders) of the population to assess the content and clarity of the tools, as well as to estimate the time required to fill it out. The most important suggested adjustments were implemented, primarily restating and simplifying the semantic language used in the claims. The pilot study's sample was not included in the main study's sample.
Before the administration of the survey, the investigators interacted with the elderly in the study sample, introduced themselves, and discussed the study's purpose and benefits, as well as its processes, to secure their consent, build trust, and earn their cooperation and confidence. Upon obtaining their informed oral consent, the investigators started to fill out the questionnaire form through personal interviewing. They read and explained each item to the elderly and recorded their responses to each item. It was difficult to gather all elderly at the same time; so they were divided into 9 groups and each group consisted of 9-10 elderly. The investigators implemented the BRT for each group on scheduled times and days. The elderly in the study sample were exposed to twelve / one-hour-long sessions of BRT, for a total period of three months, Saturdays for the first, second, third, fourth, and fifth group, Tuesdays for the 6th and 7th group, and Wednesdays for 8th and 9th group from 10 Am to 2 pm in the hall of geriatric club and homes. The instruction of BRT included the following steps:
- Take a seat in a restful posture.
- Keep your eyes closed.
- Relax all muscles, starting at the feet and working up to the top of the head, and relax all regions of the body.
- Take a deep breath through your nose. When exhaling, exhale from the lips, repeat one word or number (as Allah), inhale, and exhale with ease and confidence.
- Do this for a total of 20 minutes. Try to keep their body and muscles relaxed while mentally repeating the desired word. Then slowly open your eyes and remain motionless for a few minutes.
- Through an attractive colored booklet developed by the researchers, as well as demonstration, re-demonstration, and videos, the elderly learned about the benefits of the method and learned about the relaxation technique. Their caregivers were asked to watch and guide elders in their geriatric homes/clubs to correctly execute the technique twice a day, in the morning and evening, for 20 minutes for two months.
- The same topic was presented utilizing the same teaching methods, conversations, and handouts to guarantee that all of the seniors in the five groups were exposed to the same information and learning experiences.
- To ensure that the elderly understood the BRT content, each session began with a review of what had been covered in the previous session and the goals of the new one, using basic language appropriate for the participants' educational level.
- During the sessions, motivation and reinforcement strategies such as praise and recognition were utilized to increase engagement and learning.
- During sessions, the investigators asked the elders to perform BRT in front of them to ensure that they elderly person completed it correctly.
- To get the elders' attention and motivate them, various instructional methods were tried. Interactive lectures, group discussions, brainstorming, demonstration re-demonstration, and role-playing were among the activities. PowerPoint presentations, YouTube videos, and a guidebook were among the training materials.
- The study was completed between the beginning of June and the end of October 2020.
- Evaluation: all elderly in the study sample were interviewed using the same data collection form to reassess their level of stress, anxiety, depression, and sleep quality (post-test) immediately after implementation of BRT.
- As a result of pandemic covid-19, it is necessary of taking safety precautions such as physical distancing, wearing a mask, keeping hales well ventilated, avoiding crowds, and cleaning hands.
The statistical package for social science (SPSS), version 20.0 for Windows, was used to gather, tabulate, and statistically analyze all data. The mean, SD, and range were used to convey quantitative data, while absolute and relative frequencies were used to express qualitative data (percentage). To compare two dependent groups of non-normally distributed variables, the Wilcoxon signed-rank test was utilized. The Chi-square test was used to compare the percentages of categorical variables. To assess the relationship between various study variables, the Spearman correlation coefficient was calculated, with the plus (+) sign indicating direct correlation and the minus (-) sign indicating inverse correlation. Furthermore, numbers close to 1 suggest a significant connection, whereas values close to 0 indicate a weak correlation. All of the tests were conducted in pairs. Statistical significance was defined as a p-value of less than 0.05.
Findings
A total of 95 elderly people (Mean±SD=68.84±4.69) took part in the study, including 50 from the Geriatric social club in Zagazig City, 20 from El-Resala geriatric home in Zagazig City, and 25 from the Geriatric home at Met-Ghamr City, Egypt. Most of them were less than 70 years old, female, and widowed (Table 1).
Almost three-quarters of elders in the study sample didn't practice regular physical exercise. The majority of elders had chronic diseases, as well, and the majority of them take regular treatment for chronic diseases. Slightly more than three-fifths of elders did not have a disability (Table 2).
The majority of elders in the study had unsatisfactory knowledge about BRT during the pre-intervention phase (1.24±1.99). This score increased in the post-intervention phase (4.79±1.39). Additionally, the change in knowledge score was 2.85% (Table 3, p<0.001).
About two-thirds of elders in the study group had severe depression during the pre-intervention phase (45.14±9.9), and this was decreased in the post-intervention phase (27.16±7.55); the improvement in depression score was 39.38%. Slightly less than two-thirds of elders had severe anxiety in the pre-intervention phase (44.61±10.41), and this was decreased in the post-intervention phase (26.6±8.32); while the improvement of anxiety score was 0.40%. Less than three-quarters of elders had severe stress in the pre-intervention phase (47.13±8.95), this decreased in the post-intervention phase (28.64±7.97); the improvement of stress score was 0.39% (Table 4; p<0.001).
The majority of elders in the study sample had poor sleep quality in the pre-intervention phase, which decreased in the post-intervention phase to 50.5%. Sleep quality was enhanced following the implementation of the BRT (Diagram 1).
There was a negative significant correlation between stress and BRT, and between anxiety, depression, and stress and sleep quality, while there was a positive significant correlation between BRT and sleep quality (Table 5).
Table 1) Demographic characteristics of studied elderly (n=95)
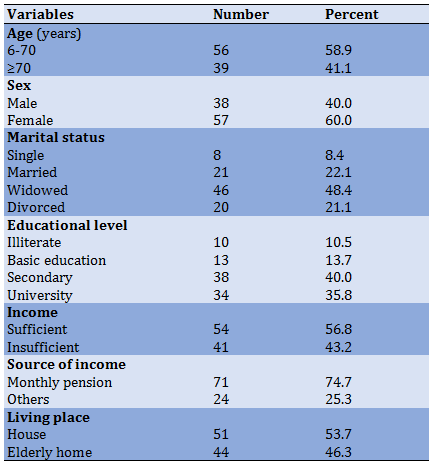
Table 2) Health characteristics of studied elders (n=95)
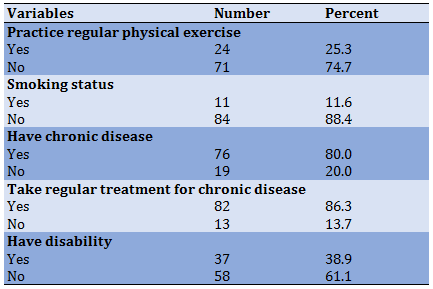
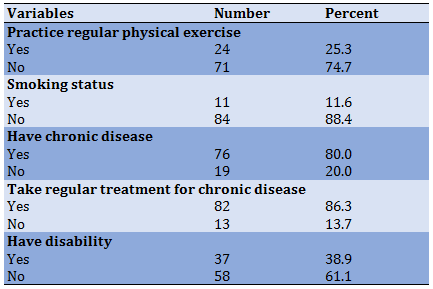
Table 3) Comparison between a score of relaxation knowledge about BRTs and its application to studied elderly throughout the study phases (n=95)
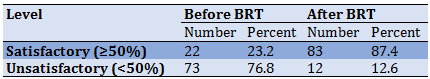
Table 4) Comparison between psychological distress scores of studied elderly throughout the study phases (n=95)
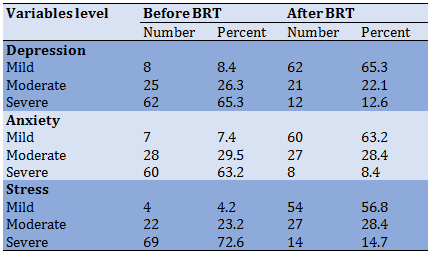
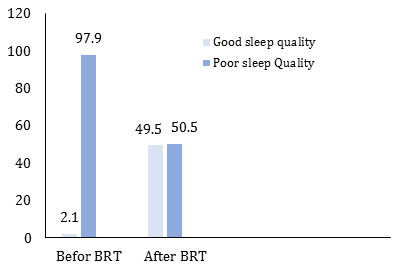
Diagram 1) Total score of sleep quality levels among studied elderly throughout the study phases (n=95)
Table 5) Correlation Matrix between BRT and both Depression, Anxiety, Stress, and Sleep quality Score post-intervention Phase (n=95)

Discussion
BRTs are beneficial in improving physical and mental functions and in enhancing the sleep quality of the elder. BRT can be used at home to decrease the time it takes to fall asleep and increase sleep duration in older adults with poor sleep quality. It is an intervention that is easy to learn and when incorporated into daily practice provides medium and long-term improvements in well-being and sleep quality for older adults.
The current study was conducted on a sample of the elderly representing both the social club for the elderly and the elderly homes in Egypt. Their demographic characteristics were those of typical older adults, aged 60-85 years, and a higher proportion of females, widowed, and those with secondary education. Identical results were reported by a study in Malaysia [20]. This group of elderly people may experience some additional burdens and psychological distress, being alone in charge of the family.
Concerning the health characteristics of the elders, the results of the current study indicated that a massive percent of the sample suffer from chronic diseases and regularly take medications for these chronic diseases that may interfere with the state of sleep. Therefore, sleep difficulties were not only due to aging itself, but were also related to medical and psychological disorders and health burdens [25]. Physical impairment seems to be another concern that shows a loss of independence in the elderly since it becomes more difficult to execute activities required for independent life [26].
Another indicator of a predominantly high psychological distress and a low level of sleep quality for the elderly in the current study, regardless of age, is the gender of the elderly, in post-test a meaningful difference between psychological distress and sleep quality (p<0.001). The result of this study is in agreement with those of Cybulski et al. [27], in Poland, who reported that a positive relationship between socio-demographic factors and prevalence of sleep disturbance was observed in the examined group. Physical impairment is another issue that signals a loss of independence in the elderly, as the difficulty in doing activities required for independent living rises.
The current study showed significant improvements in the knowledge gained for older adults about BRT after applying this technique. This indicates that they needed the information and that BRT was successful in meeting their needs. This may be attributed to the characteristics of BRT which is specifically designed to meet the specific real needs of elderly individuals. In addition, it was emphasized that during the COVID 19 pandemic, older adults need personalized educational materials that include suggestions on how to maintain their physical and mental health. Presenting such techniques in a way that is easy to understand and encouraging older people to practice them on an ongoing basis has increased confidence in them. In addition, the handbook provided to the elderly in this study aided their acquisition and retention of knowledge. Furthermore, the majority of the elders in the study had a medium or high educational level, which could have a substantial impact on their knowledge.
The results of the previous research by Reaves [28] showed that the average overall knowledge score increased significantly after applying the Benson relaxation technique (p≤0.01). This may be attributed to the fact that the majority of participants had incomplete knowledge about the BRT application and its benefits at the start of the study. The study provided older adults with the necessary techniques, which resulted in lower levels of stress, anxiety, and depression. The results of the current study found a significant positive difference in the mean scores of psychological distress for the elderly after BRT application. This showed that BRT is more effective in reducing stress and its manifestations in older adults, who feel positive and peaceful emotions rather than negative emotions, such as anger, anxiety, and sadness. Moreover, BRT as a non-pharmacological method can reduce stress among the elderly due to its function in reducing negative emotions by harmonizing the energy system of the human body along with the spiritual aspect to produce positive thinking as well. Physiologically, it helps control blood pressure by decreasing the stress hormone and creating relaxation.
In agreement with the previous finding, Habibollahpour et al. [29], reported that the progressive muscle relaxation technique could have a significant reduction in stress levels in the study group compared to the control group. Surprisingly, Reaves [28] highlighted that exercising BRT in one minute can create relaxation in 45 minutes for the human body. In addition, performing 5-20 minutes of relaxation exercises in one session can increase the energy of the elders (similar to one hour of sleep), and actions to generate facial muscles in creating a happy expression can have a positive effect on the nervous system. The movement of the facial muscles is closely related to the autonomic nervous system in regulating heartbeat, breathing, and subconscious bodily functions.
The results of the current study revealed a significant difference in the average anxiety scores of the elderly surveyed after the BRT application. This can be explained by the Benson technique being a simple, effective, safe, cost-effective relaxation technique that is easy to learn and does not require any additional equipment or resources. Gradual increases in intensity and biomechanical movements during BRT sessions may reduce anxiety as it stimulates the parietal lobe and provides somatosensory input. This may lead to an increase in the neurotropic factor that improves physical and psychological functions. These results are consistent with those of Amini et al. [30], who previously studied the effect of progressive muscle relaxation and aerobic exercise on anxiety, sleep quality, and fatigue. It has been said that BRT causes an increase in oxygen intake and an intensification of the energy production process. This plays an important role in reducing anxiety levels and thus affecting sleep quality.
A positive significant improvement in the total depression score of the studied elderly was revealed after applying the Benson relaxation technique. The reason for this large statistical difference may be the use of BRT for two- months. Relaxation and regular exercise can improve the health of older adults by regulating the autonomic nervous system and controlling emotions in stressful situations. The use of these exercises can change the hemodynamic variables, which may be the cause of the progression of the condition of the elderly. The result of this study is consistent with that of Safi [31], who concluded that the progressive muscle relaxation technique is effective in reducing stress and depression. In addition, Barati & Sarjuei [32] reported a significant difference in depression levels between elderly patients before and after BRT application.
Contrasting with previous findings, Reig-Ferrer et al. [33], the study showed no significant difference between the mean scores of depression values in the study group before and after the implementation of BRT. This discrepancy may be explained by the higher prevalence of depression among participants and may be due to the limited period practiced using the Benson technique.
The goal of this study was to see how effective BRT is at improving sleep quality in the elderly. At week eight of the study intervention, big variations in the scores of the Pittsburgh Sleep Quality Index subscales, such as sleep disturbance, daytime dysfunction, use of sleep medication, and subjective sleep quality, as well as their universal scores, were found between the two pre/post-intervention stages (p=0.001). In older persons, poor sleep quality was found to be connected with higher levels of psychological discomfort. The current study's findings emphasize the role of deep breathing exercises in enhancing sleep quality in older people receiving home care. It is critical to provide primary health care services to the elderly to improve their sleep quality. For those with poor sleep quality, these simple at-home treatments enhance sleep time, sleepover time in bed, and sleep duration.
This result was consistent with the previous study by Ahmed & Masry [34], who found an improvement in sleep quality scores among study group subjects compared to the control group after applying the BRT. When BRT is practiced continuously, the parasympathetic nervous system is stimulated and the release of endorphins produces an emotional state of happiness and calmness and can release pain. Collectively, these feelings can make it easier to fall asleep.
Other studies by Byomi & Shark away [35]; Abd Allah et al. [36] revealed that the sleep quality of the elderly improved significantly after applying for an educational training program on sleep disorders in the elderly.
The correlation analysis of this study showed that gaining knowledge about BRT improves sleep quality, while anxiety, depression, and stress lower it. These can be considered as mediating factors through which the intervention had a positive effect on the sleep quality of the elderly. For example, elderly people with sleep disturbances are more likely to develop hypertension, depression, cardiovascular disease, and cerebrovascular disease. Conversely, elderly people with any of these diseases are at greater risk of developing sleep problems than usual [37]. It appears that BRT can improve sleep duration resulting inadequate sleep at night, which in turn increases the ability to achieve daily activities. BRT can affect the stages of sleep.
The results of the current study revealed that there is a moderately positive, statistically significant relationship between elderly depression, anxiety, degree of stress, and knowledge about BRT on the one hand and before/after sleep quality scores on the other hand. These results are consistent with the results of a study by Ahmed & Masry [34], who reported statistically significant associations between demographic characteristics, knowledge about BRT, sleep quality, anxiety, stress, and depression. These results may be attributed to the fact that BRT is a simple and easy-to-apply technique that can be learned by anyone, regardless of age or education level.
According to the findings, More studies are required with a larger sample size and focus on social and demographic variables, and the distribution of BRT to other social clubs for the elderly and homes in several governorates of Egypt to further confirm the results; Gero-psychiatric nurses should encourage all elders' people to apply BRT for enhancement of their psychological wellbeing.
Conclusion
Increasing the application of BRT decreases stress, and enhances sleep quality.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Osman Ali SA (First Author), Methodologist/Main Researcher (25%); Kamel N (Second Author), Assistant Researcher/Statistical Analyst (25%); Holmes SL (Third Author), Introduction Writer/Statistical Analyst/Discussion Writer (25%); Abdelfatah Arafat AE (Forth Author), Assistant Researcher (25%)
Funding/Support: None declared.
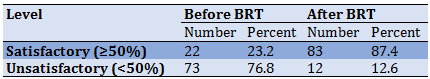
Table 4) Comparison between psychological distress scores of studied elderly throughout the study phases (n=95)
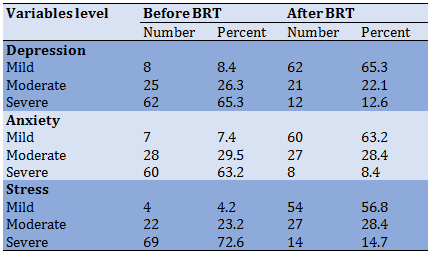
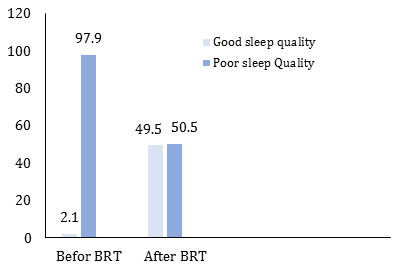
Diagram 1) Total score of sleep quality levels among studied elderly throughout the study phases (n=95)
Table 5) Correlation Matrix between BRT and both Depression, Anxiety, Stress, and Sleep quality Score post-intervention Phase (n=95)

Discussion
BRTs are beneficial in improving physical and mental functions and in enhancing the sleep quality of the elder. BRT can be used at home to decrease the time it takes to fall asleep and increase sleep duration in older adults with poor sleep quality. It is an intervention that is easy to learn and when incorporated into daily practice provides medium and long-term improvements in well-being and sleep quality for older adults.
The current study was conducted on a sample of the elderly representing both the social club for the elderly and the elderly homes in Egypt. Their demographic characteristics were those of typical older adults, aged 60-85 years, and a higher proportion of females, widowed, and those with secondary education. Identical results were reported by a study in Malaysia [20]. This group of elderly people may experience some additional burdens and psychological distress, being alone in charge of the family.
Concerning the health characteristics of the elders, the results of the current study indicated that a massive percent of the sample suffer from chronic diseases and regularly take medications for these chronic diseases that may interfere with the state of sleep. Therefore, sleep difficulties were not only due to aging itself, but were also related to medical and psychological disorders and health burdens [25]. Physical impairment seems to be another concern that shows a loss of independence in the elderly since it becomes more difficult to execute activities required for independent life [26].
Another indicator of a predominantly high psychological distress and a low level of sleep quality for the elderly in the current study, regardless of age, is the gender of the elderly, in post-test a meaningful difference between psychological distress and sleep quality (p<0.001). The result of this study is in agreement with those of Cybulski et al. [27], in Poland, who reported that a positive relationship between socio-demographic factors and prevalence of sleep disturbance was observed in the examined group. Physical impairment is another issue that signals a loss of independence in the elderly, as the difficulty in doing activities required for independent living rises.
The current study showed significant improvements in the knowledge gained for older adults about BRT after applying this technique. This indicates that they needed the information and that BRT was successful in meeting their needs. This may be attributed to the characteristics of BRT which is specifically designed to meet the specific real needs of elderly individuals. In addition, it was emphasized that during the COVID 19 pandemic, older adults need personalized educational materials that include suggestions on how to maintain their physical and mental health. Presenting such techniques in a way that is easy to understand and encouraging older people to practice them on an ongoing basis has increased confidence in them. In addition, the handbook provided to the elderly in this study aided their acquisition and retention of knowledge. Furthermore, the majority of the elders in the study had a medium or high educational level, which could have a substantial impact on their knowledge.
The results of the previous research by Reaves [28] showed that the average overall knowledge score increased significantly after applying the Benson relaxation technique (p≤0.01). This may be attributed to the fact that the majority of participants had incomplete knowledge about the BRT application and its benefits at the start of the study. The study provided older adults with the necessary techniques, which resulted in lower levels of stress, anxiety, and depression. The results of the current study found a significant positive difference in the mean scores of psychological distress for the elderly after BRT application. This showed that BRT is more effective in reducing stress and its manifestations in older adults, who feel positive and peaceful emotions rather than negative emotions, such as anger, anxiety, and sadness. Moreover, BRT as a non-pharmacological method can reduce stress among the elderly due to its function in reducing negative emotions by harmonizing the energy system of the human body along with the spiritual aspect to produce positive thinking as well. Physiologically, it helps control blood pressure by decreasing the stress hormone and creating relaxation.
In agreement with the previous finding, Habibollahpour et al. [29], reported that the progressive muscle relaxation technique could have a significant reduction in stress levels in the study group compared to the control group. Surprisingly, Reaves [28] highlighted that exercising BRT in one minute can create relaxation in 45 minutes for the human body. In addition, performing 5-20 minutes of relaxation exercises in one session can increase the energy of the elders (similar to one hour of sleep), and actions to generate facial muscles in creating a happy expression can have a positive effect on the nervous system. The movement of the facial muscles is closely related to the autonomic nervous system in regulating heartbeat, breathing, and subconscious bodily functions.
The results of the current study revealed a significant difference in the average anxiety scores of the elderly surveyed after the BRT application. This can be explained by the Benson technique being a simple, effective, safe, cost-effective relaxation technique that is easy to learn and does not require any additional equipment or resources. Gradual increases in intensity and biomechanical movements during BRT sessions may reduce anxiety as it stimulates the parietal lobe and provides somatosensory input. This may lead to an increase in the neurotropic factor that improves physical and psychological functions. These results are consistent with those of Amini et al. [30], who previously studied the effect of progressive muscle relaxation and aerobic exercise on anxiety, sleep quality, and fatigue. It has been said that BRT causes an increase in oxygen intake and an intensification of the energy production process. This plays an important role in reducing anxiety levels and thus affecting sleep quality.
A positive significant improvement in the total depression score of the studied elderly was revealed after applying the Benson relaxation technique. The reason for this large statistical difference may be the use of BRT for two- months. Relaxation and regular exercise can improve the health of older adults by regulating the autonomic nervous system and controlling emotions in stressful situations. The use of these exercises can change the hemodynamic variables, which may be the cause of the progression of the condition of the elderly. The result of this study is consistent with that of Safi [31], who concluded that the progressive muscle relaxation technique is effective in reducing stress and depression. In addition, Barati & Sarjuei [32] reported a significant difference in depression levels between elderly patients before and after BRT application.
Contrasting with previous findings, Reig-Ferrer et al. [33], the study showed no significant difference between the mean scores of depression values in the study group before and after the implementation of BRT. This discrepancy may be explained by the higher prevalence of depression among participants and may be due to the limited period practiced using the Benson technique.
The goal of this study was to see how effective BRT is at improving sleep quality in the elderly. At week eight of the study intervention, big variations in the scores of the Pittsburgh Sleep Quality Index subscales, such as sleep disturbance, daytime dysfunction, use of sleep medication, and subjective sleep quality, as well as their universal scores, were found between the two pre/post-intervention stages (p=0.001). In older persons, poor sleep quality was found to be connected with higher levels of psychological discomfort. The current study's findings emphasize the role of deep breathing exercises in enhancing sleep quality in older people receiving home care. It is critical to provide primary health care services to the elderly to improve their sleep quality. For those with poor sleep quality, these simple at-home treatments enhance sleep time, sleepover time in bed, and sleep duration.
This result was consistent with the previous study by Ahmed & Masry [34], who found an improvement in sleep quality scores among study group subjects compared to the control group after applying the BRT. When BRT is practiced continuously, the parasympathetic nervous system is stimulated and the release of endorphins produces an emotional state of happiness and calmness and can release pain. Collectively, these feelings can make it easier to fall asleep.
Other studies by Byomi & Shark away [35]; Abd Allah et al. [36] revealed that the sleep quality of the elderly improved significantly after applying for an educational training program on sleep disorders in the elderly.
The correlation analysis of this study showed that gaining knowledge about BRT improves sleep quality, while anxiety, depression, and stress lower it. These can be considered as mediating factors through which the intervention had a positive effect on the sleep quality of the elderly. For example, elderly people with sleep disturbances are more likely to develop hypertension, depression, cardiovascular disease, and cerebrovascular disease. Conversely, elderly people with any of these diseases are at greater risk of developing sleep problems than usual [37]. It appears that BRT can improve sleep duration resulting inadequate sleep at night, which in turn increases the ability to achieve daily activities. BRT can affect the stages of sleep.
The results of the current study revealed that there is a moderately positive, statistically significant relationship between elderly depression, anxiety, degree of stress, and knowledge about BRT on the one hand and before/after sleep quality scores on the other hand. These results are consistent with the results of a study by Ahmed & Masry [34], who reported statistically significant associations between demographic characteristics, knowledge about BRT, sleep quality, anxiety, stress, and depression. These results may be attributed to the fact that BRT is a simple and easy-to-apply technique that can be learned by anyone, regardless of age or education level.
According to the findings, More studies are required with a larger sample size and focus on social and demographic variables, and the distribution of BRT to other social clubs for the elderly and homes in several governorates of Egypt to further confirm the results; Gero-psychiatric nurses should encourage all elders' people to apply BRT for enhancement of their psychological wellbeing.
Conclusion
Increasing the application of BRT decreases stress, and enhances sleep quality.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Osman Ali SA (First Author), Methodologist/Main Researcher (25%); Kamel N (Second Author), Assistant Researcher/Statistical Analyst (25%); Holmes SL (Third Author), Introduction Writer/Statistical Analyst/Discussion Writer (25%); Abdelfatah Arafat AE (Forth Author), Assistant Researcher (25%)
Funding/Support: None declared.
Article Type: Original Research |
Subject:
Health Communication
Received: 2022/01/9 | Accepted: 2022/04/1 | Published: 2022/04/10
Received: 2022/01/9 | Accepted: 2022/04/1 | Published: 2022/04/10
References
1. World Health Organization. Coronavirus disease (COVID-19) pandemic [Internet]. Geneva: World Health Organization; 2020 [cited 2021 Aug 1]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Link]
2. Centers for Disease Control and Prevention. COVID-19 [Internet]. Centers for Disease Control and Prevention; 2020 [cited 2021 Aug 1]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/index.html. [Link]
3. Hwang J, Ryu HS, Kim HA, Hyun M, Lee JY, Yi HA. Prognostic factors of COVID-19 infection in elderly patients: a multicenter study. J Clin Med. 2020;9(12):3932. [Link] [DOI:10.3390/jcm9123932]
4. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35(12):1123-38. [Link] [DOI:10.1007/s10654-020-00698-1]
5. Al-Zahrani J. SARS-CoV-2 associated COVID-19 in geriatric population: A brief narrative review. Saudi J Biol Sci. 2021;28(1):738-43. [Link] [DOI:10.1016/j.sjbs.2020.11.001]
6. Khademi F, Moayedi S, Golitaleb M, Karbalaie N. The COVID‐19 pandemic and death anxiety in the elderly. Int J Men Health Nurs. 2020 Dec. [Link] [DOI:10.1111/inm.12824]
7. Couture M, Larivière N, Lefrançois R. Psychological distress in older adults with low functional independence: A multidimensional perspective. Arch Gerontol Geriatr. 2005;41(1):101-11. [Link] [DOI:10.1016/j.archger.2004.12.004]
8. Santini ZI, Jose PE, Cornwell EY, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62-70. [LinkLink] [DOI:10.1016/S2468-2667(19)30230-0]
9. Riedel‐Heller SG, Busse A, Angermeyer MC. The state of mental health in old‐age across the 'old'European :union:-a systematic review. Acta Psychiatrica Scand. 2006;113(5):388-401. [Link] [DOI:10.1111/j.1600-0447.2005.00632.x]
10. Henning-Smith C. Quality of life and psychological distress among older adults: the role of living arrangements. J Appl Gerontol. 2016;35(1):39-61. [Link] [DOI:10.1177/0733464814530805]
11. Kamal M, Herawati T. The effect of sleep hygiene and relaxation Benson on improving the quality of sleep among health failure patients: A literature review. Int J Nurs Health Serv. 2019;2:101-7. [Link] [DOI:10.35654/ijnhs.v2i1.69]
12. Tranah GJ, Stone KL, Ancoli-Israel S. Circadian rhythms in older adults. In: Kryger MH, Roth T and Dement WC, editors. Principles and practice of sleep medicine. 6th Edition. Philadelphia: Elsevier Inc; 2017. [Link] [DOI:10.1016/B978-0-323-24288-2.00154-9]
13. Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28(11):1457-64. [Link] [DOI:10.1093/sleep/28.11.1457]
14. Zargarani F, Kamkar M, Maghsoudlou A. The effect of progressive muscle relaxation technique on the quality of sleep and fatigue in patients with multiple sclerosis. Nurs Midwifery J. 2018;15(12):911-20. [Persian] [Link]
15. Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37(1):37-46. [Link] [DOI:10.1080/00332747.1974.11023785]
16. Elsayed EB, Radwan EH, Elashri NI, El-Gilany H. The effect of Benson's relaxation technique on anxiety, depression and sleep quality of elderly patients undergoing hemodialysis. Int J Nurs Didactics. 2019;9:23-31. [Link] [DOI:10.15520/ijnd.v9i02.2443]
17. Marengoni A, Zucchelli A, Vetrano DL, Armellini A, Botteri E, Nicosia F, et al. Beyond chronological age: Frailty and multimorbidity predict in-hospital mortality in patients with coronavirus disease 2019. J Gerontol A Biol Sci Med Sci. 2021;76(3):e38-45. [Link] [DOI:10.1093/gerona/glaa291]
18. Turner G, Clegg A. Best practice guidelines for the management of frailty: a British Geriatrics Society, Age UK and Royal College of General Practitioners report. Age Ageing. 2014;43(6):744-7. [Link] [DOI:10.1093/ageing/afu138]
19. Smeltzer, S., Bare, B., Hinkle, J, Cheever, K. Biophysical and psychological concepts in nursing practice, Introduced by Herbert Benson Brunner & Suddarths text book of medical surgical nursing. Philadelphia: Woltres; 2010. [Link]
20. Adam D, Ramli A, Shahar S. Effectiveness of a combined dance and relaxation intervention on reducing anxiety and depression and improving quality of life among the cognitively impaired elderly. Sultan Qaboos Univ Med J. 2016;16(1):e47-53. [Link] [DOI:10.18295/squmj.2016.16.01.009]
21. Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335-43. [Link] [DOI:10.1016/0005-7967(94)00075-U]
22. Moussa MT, Lovibond P, Laube R, Megahead HA. Psychometric properties of an arabic version of the depression anxiety stress scales (DASS). Rese Soc Work Pract. 2017;27(3):375-86. [Link] [DOI:10.1177/1049731516662916]
23. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [Link] [DOI:10.1016/0165-1781(89)90047-4]
24. Suleiman K, Al-Hadid L, Duhni A. Psychometric testing of the Arabic version of the Pittsburgh Sleep Quality Index (A-PSQI) among coronary artery disease patients in Jordan. J Nat Sci Res. 2012;2(8):15-20. [Link]
25. Dangol M, Shrestha S, Rai Koirala SK. Insomnia and its associated factors among older people of selected ward of Banepa municipality, Nepal. Nurs Open. 2020;7(1):355-63. [Link] [DOI:10.1002/nop2.396]
26. Gulia KK, Kumar VM. Sleep disorders in the elderly: a growing challenge. Psychogeriatrics. 2018;18(3):155-65. [Link] [DOI:10.1111/psyg.12319]
27. Cybulski M, Cybulski L, Krajewska-Kulak E, Orzechowska M, Cwalina U, Kowalczuk K. Sleep disorders among educationally active elderly people in Bialystok, Poland: A cross-sectional study. BMC Geriatric. 2019;19:225. [Link] [DOI:10.1186/s12877-019-1248-2]
28. Reaves C. Benson's relaxation response: psychological and physiological responses among patients with COPD [Dissertation]. Unknown Publisher; 2019. [Link]
29. Habibollahpour M, Ranjkesh F, Motalebi SA, Mohammadi F. The Impact of Benson's relaxation technique on the quality of sleep in the elderly. Topic Geriatric Rehabil. 2019;35(1):88-94. [Link] [DOI:10.1097/TGR.0000000000000204]
30. Amini E, Goudarzi I, Masoudi R, Ahmadi A, Momeni A. Effect of progressive muscle relaxation and aerobic exercise on anxiety, sleep quality, and fatigue in patients with chronic renal failure undergoing hemodialysis. Int J Pharmaceut Clin Res. 2016;8(12):1634-9. [Persian] [Link]
31. Safi SZ. A fresh look at the potential mechanisms of progressive muscle relaxation therapy on depression in female patients with multiple sclerosis. Iran J Psychiatry Behav Sci. 2015;9(1):e340. [Link] [DOI:10.17795/ijpbs340]
32. Barati S, Sarjuei Z. The effects of Benson & Jacobson combined relaxation techniques on the elderly's depression & life quality. J Chem Pharmaceut Res. 2016;8(6):100-3. [Link]
33. Reig-Ferrer A, Ferrer-Cascales R, Santos-Ruiz A, Campos-Ferrer A, Prieto-Seva A, Velasco-Ruiz I, et al. A relaxation technique enhances psychological well-being and immune parameters in elderly people from a nursing home: a randomized controlled study. BMC Complement Altern Med. 2014;14:311. [Link] [DOI:10.1186/1472-6882-14-311]
34. Ahmed NA, Masry SE. Effect of Benson's relaxation technique on night pain and sleep quality among adults and elderly patients undergoing joints replacement surgery. Int J Nurs Didactics. 2017;7:1-8. [Link] [DOI:10.15520/ijnd.2017.vol7.iss4.205.01-08]
35. Byomi SS, Sharkaway SA. The impact of nursing intervention about sleep disturbance among elderly patient. J Am Sci. 2013;9(5):193-202. [Link]
36. Abd Allah ES, Abdel-Aziz HR, Ali SA, El-Seoud AR. Cognitive behavioral intervention to improve sleep quality in older adults. IOSR J Nursing and Health Science. 2016. [Link]
37. Bloom HG, Ahmed I, Alessi CA, Ancoli‐Israel S, Buysse DJ, Kryger MH, et al. Evidence‐based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc. 2009;57(5):761-89. [Link] [DOI:10.1111/j.1532-5415.2009.02220.x]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





