Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 665-672 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yasamani K, Khalkhali H, Farrokh Eslamlou H, Didarloo A. Determinants of COVID-19 Preventive Behaviors among Women of Reproductive Age in Urmia using a Behavioral Change Model in 2021. Health Educ Health Promot 2022; 10 (4) :665-672
URL: http://hehp.modares.ac.ir/article-5-59074-en.html
URL: http://hehp.modares.ac.ir/article-5-59074-en.html
1- Department of Public Health, School of Health, Urmia University of Medical Sciences, Urmia, Iran
2- Department of Epidemiology and Biostatistics, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
2- Department of Epidemiology and Biostatistics, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
Keywords: Health Belief Model [MeSH], COVID-19 [MeSH], Preventive Health Services [MeSH], Women [MeSH]
Full-Text [PDF 1346 kb]
(955 Downloads)
| Abstract (HTML) (779 Views)
Full-Text: (93 Views)
Introduction
COVID-19 is an infectious disease caused by a new type of coronavirus as the third most common zoonotic coronavirus in the current century, and it can cause respiratory infections, from a simple cold to Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS) [1]. The disease was first reported in Wuhan, China, and has become a pandemic of the century due to its spread throughout the world [2]. Up to January 1, 2022, 288548655 cases of the disease were confirmed worldwide, among which 5453460 resulted in death. In Iran, 6194401 cases and 131606 deaths were reported up to that date [3]. Most people infected with the virus experience mild to moderate respiratory illness and recover without the need for special treatment [4]. Common symptoms include fever, dry cough, shortness of breath, and extreme tiredness. Symptoms such as sputum, headache, vomiting, diarrhea, and runny nose have been reported in some people. In severe cases, the disease can cause systemic reactions and even death [1]. The disease is transmitted through coughing and sneezing, contact with an infected person or touching infected surfaces, and then touching the mouth, nose, and eyes of both groups of symptomatic and asymptomatic people. The time interval between exposure to the disease and the onset of symptoms varies between 2 and 14 days [2].
Due to the lack of access to proven effective antiviral treatment, the inability of existing vaccines to prevent definitive infection, as well as the possibility of resistance to new species resulting from various mutations [5], the World Health Organization (WHO) has recommended preventive behaviors to control the disease based on previous experience of managing SARS and MERS infections [6], and such behaviors can be classified into two levels: Social level that is often enforced by legal policies (e.g. social distance), and individual level that is often by performed by people and based on their beliefs to protect themselves or others (e.g. regular hand washing and wearing a mask) [7].
Studies have indicated that the virus characteristics in high pathogenicity and the reduction of individuals' adherence to preventive behaviors in society are the reasons for the high reproductive capacity of the COVID-19 epidemic in society [8]. Therefore, identifying and eliminating cognitive-social causes related to the cause of reduced adherence to health guidelines seems to be essential [9]. In this regard, models and theories of behavioral change can be helpful. The health belief model (HBM) considers behavior as a function of individual knowledge and attitude and causes people to perceive a health threat, thereby leading their behaviors towards health [10]. According to this model, a person should first feel at risk for COVID-19 (perceived susceptibility), and then perceive the severity and seriousness of its complications (perceived severity), and according to positive symptoms from the environment (cues to action) believe the feasibility of the COVID-19 prevention program (perceived benefits) and find the barriers to action less costly than its benefits (perceived barriers) to ultimately perform COVID-19 preventive behavior. Finally, positive judgment about the individual ability to adopt preventive behaviors (perceived self-efficacy) is also an accelerating force that necessitates adopting these behaviors [2].
The results of a study in Sudan indicated that the constructs of the health belief model could predict 43% of the variance of COVID-19 preventive behaviors [11]. Khafaie et al. also reported that perceived sensitivity, perceived severity, perceived benefits, and self-efficacy were the strongest predictors of COVID-19 preventive behaviors [12].
Due to the vulnerability of women in crises, and lack of access to equal opportunities in the allocation of information and health resources, the special needs of women are often ignored and it is expected that in addition to children, they should take care of men, the elderly, the sick, and disabled family members. Furthermore, women are often addressed in educational messages on health issues, due to more responsibility [13]. Therefore, the present study aimed to investigate the determinants of COVID-19 preventive behaviors among women of reproductive age using a behavioral change model to utilize its results in health interventions and planning to promote COVID-19 preventive behaviors.
Instrument and Methods
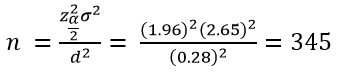
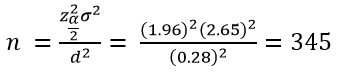
This cross-sectional descriptive-analytical study examined women of reproductive age in Urmia in 2021. The sample size was 345 based on estimating the mean COVID-19 preventive behavior according to the results of a study [2], in which the mean score of total COVID-19 preventive behaviors was 4.19±2.65 at a 95% confidence level, and the measurement precision of 0.28 using the following formula for estimating the mean of a trait in the population:
COVID-19 is an infectious disease caused by a new type of coronavirus as the third most common zoonotic coronavirus in the current century, and it can cause respiratory infections, from a simple cold to Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS) [1]. The disease was first reported in Wuhan, China, and has become a pandemic of the century due to its spread throughout the world [2]. Up to January 1, 2022, 288548655 cases of the disease were confirmed worldwide, among which 5453460 resulted in death. In Iran, 6194401 cases and 131606 deaths were reported up to that date [3]. Most people infected with the virus experience mild to moderate respiratory illness and recover without the need for special treatment [4]. Common symptoms include fever, dry cough, shortness of breath, and extreme tiredness. Symptoms such as sputum, headache, vomiting, diarrhea, and runny nose have been reported in some people. In severe cases, the disease can cause systemic reactions and even death [1]. The disease is transmitted through coughing and sneezing, contact with an infected person or touching infected surfaces, and then touching the mouth, nose, and eyes of both groups of symptomatic and asymptomatic people. The time interval between exposure to the disease and the onset of symptoms varies between 2 and 14 days [2].
Due to the lack of access to proven effective antiviral treatment, the inability of existing vaccines to prevent definitive infection, as well as the possibility of resistance to new species resulting from various mutations [5], the World Health Organization (WHO) has recommended preventive behaviors to control the disease based on previous experience of managing SARS and MERS infections [6], and such behaviors can be classified into two levels: Social level that is often enforced by legal policies (e.g. social distance), and individual level that is often by performed by people and based on their beliefs to protect themselves or others (e.g. regular hand washing and wearing a mask) [7].
Studies have indicated that the virus characteristics in high pathogenicity and the reduction of individuals' adherence to preventive behaviors in society are the reasons for the high reproductive capacity of the COVID-19 epidemic in society [8]. Therefore, identifying and eliminating cognitive-social causes related to the cause of reduced adherence to health guidelines seems to be essential [9]. In this regard, models and theories of behavioral change can be helpful. The health belief model (HBM) considers behavior as a function of individual knowledge and attitude and causes people to perceive a health threat, thereby leading their behaviors towards health [10]. According to this model, a person should first feel at risk for COVID-19 (perceived susceptibility), and then perceive the severity and seriousness of its complications (perceived severity), and according to positive symptoms from the environment (cues to action) believe the feasibility of the COVID-19 prevention program (perceived benefits) and find the barriers to action less costly than its benefits (perceived barriers) to ultimately perform COVID-19 preventive behavior. Finally, positive judgment about the individual ability to adopt preventive behaviors (perceived self-efficacy) is also an accelerating force that necessitates adopting these behaviors [2].
The results of a study in Sudan indicated that the constructs of the health belief model could predict 43% of the variance of COVID-19 preventive behaviors [11]. Khafaie et al. also reported that perceived sensitivity, perceived severity, perceived benefits, and self-efficacy were the strongest predictors of COVID-19 preventive behaviors [12].
Due to the vulnerability of women in crises, and lack of access to equal opportunities in the allocation of information and health resources, the special needs of women are often ignored and it is expected that in addition to children, they should take care of men, the elderly, the sick, and disabled family members. Furthermore, women are often addressed in educational messages on health issues, due to more responsibility [13]. Therefore, the present study aimed to investigate the determinants of COVID-19 preventive behaviors among women of reproductive age using a behavioral change model to utilize its results in health interventions and planning to promote COVID-19 preventive behaviors.
Instrument and Methods
This cross-sectional descriptive-analytical study examined women of reproductive age in Urmia in 2021. The sample size was 345 based on estimating the mean COVID-19 preventive behavior according to the results of a study [2], in which the mean score of total COVID-19 preventive behaviors was 4.19±2.65 at a 95% confidence level, and the measurement precision of 0.28 using the following formula for estimating the mean of a trait in the population:
Considering the 15% loss, 400 individuals were included in the study. The samples were selected by the convenience and snowball sampling method, and the questionnaires were completed online by sending links to individuals via WhatsApp channels. At the beginning of the questionnaires, sufficient explanations were given about the research purpose, inclusion criteria, and individuals' voluntary participation, and they were assured that their information would be kept confidential by the researcher so that their names and contact numbers were not requested. Inclusion criteria were as follows: willingness to participate in the study, being a woman, and resident of Urmia, age of 15 to 49 years, access to the internet, and the ability to complete the questionnaire physically and mentally. Exclusion criteria: The unwillingness to continue cooperation, and the incomplete questionnaires.
The research tool included the researcher-made questionnaire consisting of four sections: First, demographic information (age, marital status, education level, job status, and the number of family members). The second section was about knowledge consisting of 14 questions with a score range of 0-28 under which the answers “yes” received a score of 2, “I do not know” scored 1, and “no” scored zero. The third section included questions about constructs of the health belief model as follows: perceived susceptibility, benefits, barriers, and self-efficacy dimensions each of which had five questions with a score range of 5-25, and scoring was based on the five-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) scored from 1 to 5, The questions 4 and 5 of perceived susceptibility and all questions of perceived barriers were scored in reverse. The perceived severity included seven questions with a range of 7-35 and was also based on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, and strongly agree) ranging from 1 to 5 (never, rarely, sometimes, often, and always). The “cues to action” dimension included eight questions with a range of 8-40, and 5 options (never, rarely, sometimes, often, and always) were considered for responding to the questions and each answer was scored from 1 to 5. The fourth section also included 5 questions about preventive behaviors such as social distancing, mask use, hand hygiene (washing hands with soap and water or disinfecting with 70% alcohol solution), and disinfecting surfaces with a score range of 5-25, which like the cues to action dimension, it was assessed using 5 options (never, rarely, sometimes, often, and always). The face and content validity methods were used in both quantitative and qualitative ways to evaluate the validity of the scale. To determine the face validity of the questionnaire by the qualitative method, it was given to about 10 experts in fields related to research and instrumentation (4 specialists in health education and promotion, 2 specialists in infectious diseases, 2 nurses, 1 psychologist, and 1 expert in instrumentation) to examine the questions according to the desirability of the terms and their clarity. To receive the opinions of the target group, interviews were conducted with about 20 of them, and their opinions were applied to the questionnaire. In the quantitative method, the impact score was calculated for each question by multiplying the percentage of the number of people who gave the questions a score of 4 or 5 by the average score of each question [14]. If the question effect score was greater than 1.5, the item was retained and otherwise deleted. To determine the content validity by the qualitative method, the questionnaires were given to about 10 experts to provide their corrective views in writing after careful study of the questions. Finally, their opinions were included in the questionnaire. The content validity ratio using the necessity criterion, and the content validity index using the relevance, clarity, and simplicity criteria were utilized to determine the content validity by the quantitative method. Therefore, the questionnaires were given to about 10 experts to score each question in terms of necessity, relevance, clarity, and simplicity. The first item was calculated by the content validity ratio (CVR), and the second item was calculated by the content validity index (CVI). Questions, in which the CVR values were at least 0.62 and higher, and the CVI values were above 0.79, were retained and the rest were omitted. For reliability, a pilot study was conducted on 30 individuals, and the Cronbach's alpha was measured for perceived susceptibility (0.86), perceived severity (0.85), perceived benefits (0.89), perceived barriers (0.84), perceived self-efficacy (0.87), cues to action (0.81), behavior (0.83), and knowledge (0.9), and the instrument reliability was confirmed since Cronbach's alpha values were greater than 0.7 for all constructs.
To analyze the data, descriptive indices such as frequency, and mean were utilized to report the demographic variables. Kolmogorov-Smirnov test was performed to check the data normality. Pearson correlation was applied to examine the association between variables. Linear regression was used to determine effective factors in the behavior based on the HBM variable. The analyses were performed by SPSS software with version 16. All analyses were statistically considered at a significance level of 0.05.
Findings
Data obtained from 400 questionnaires were analyzed in this study. The mean age of participants was 36.64±11.82 years. Most participants were in the age groups of 45-49 years and 35-39 years respectively. Most people were married, with a bachelor's degree, and were housewives (Table 1).
The mean scores of perceived severity, knowledge, and cues to action were higher than other constructs (Table 2).
The results of the correlation coefficient table indicated that preventive behaviors had a significant positive correlation with self-efficacy (p<0.001), perceived benefits (p<0.001), perceived susceptibility (p=0.002), perceived severity (p<0.001), cues to action (p<0.001), and knowledge (p<0.001), and a significant negative correlation with perceived barriers (p<0.001); and the strongest correlation belonged to self-efficacy construct. Among the constructs, the strongest correlation belonged to self-efficacy and perceived benefits (Table 3).
According to Table 3, official Internet news
agencies, the media, and finally physicians and healthcare personnel were the most important sources of information about COVID-19. The
printed media played the least role in receiving information (Table 4).
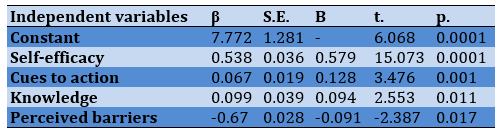
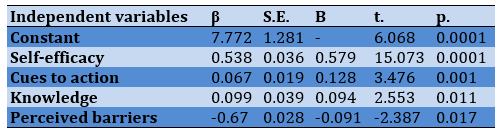
In regression analysis using the forward method, self-efficacy, cues to action, knowledge, and perceived barriers remained in the final model as predictors of COVID-19 preventive behaviors. Based on the results of the regression analysis table, the constructs of the health belief model could predict 50% of the variance of preventive behaviors and self-efficacy was the strongest predictor (Table 5).
The research tool included the researcher-made questionnaire consisting of four sections: First, demographic information (age, marital status, education level, job status, and the number of family members). The second section was about knowledge consisting of 14 questions with a score range of 0-28 under which the answers “yes” received a score of 2, “I do not know” scored 1, and “no” scored zero. The third section included questions about constructs of the health belief model as follows: perceived susceptibility, benefits, barriers, and self-efficacy dimensions each of which had five questions with a score range of 5-25, and scoring was based on the five-point Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) scored from 1 to 5, The questions 4 and 5 of perceived susceptibility and all questions of perceived barriers were scored in reverse. The perceived severity included seven questions with a range of 7-35 and was also based on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, and strongly agree) ranging from 1 to 5 (never, rarely, sometimes, often, and always). The “cues to action” dimension included eight questions with a range of 8-40, and 5 options (never, rarely, sometimes, often, and always) were considered for responding to the questions and each answer was scored from 1 to 5. The fourth section also included 5 questions about preventive behaviors such as social distancing, mask use, hand hygiene (washing hands with soap and water or disinfecting with 70% alcohol solution), and disinfecting surfaces with a score range of 5-25, which like the cues to action dimension, it was assessed using 5 options (never, rarely, sometimes, often, and always). The face and content validity methods were used in both quantitative and qualitative ways to evaluate the validity of the scale. To determine the face validity of the questionnaire by the qualitative method, it was given to about 10 experts in fields related to research and instrumentation (4 specialists in health education and promotion, 2 specialists in infectious diseases, 2 nurses, 1 psychologist, and 1 expert in instrumentation) to examine the questions according to the desirability of the terms and their clarity. To receive the opinions of the target group, interviews were conducted with about 20 of them, and their opinions were applied to the questionnaire. In the quantitative method, the impact score was calculated for each question by multiplying the percentage of the number of people who gave the questions a score of 4 or 5 by the average score of each question [14]. If the question effect score was greater than 1.5, the item was retained and otherwise deleted. To determine the content validity by the qualitative method, the questionnaires were given to about 10 experts to provide their corrective views in writing after careful study of the questions. Finally, their opinions were included in the questionnaire. The content validity ratio using the necessity criterion, and the content validity index using the relevance, clarity, and simplicity criteria were utilized to determine the content validity by the quantitative method. Therefore, the questionnaires were given to about 10 experts to score each question in terms of necessity, relevance, clarity, and simplicity. The first item was calculated by the content validity ratio (CVR), and the second item was calculated by the content validity index (CVI). Questions, in which the CVR values were at least 0.62 and higher, and the CVI values were above 0.79, were retained and the rest were omitted. For reliability, a pilot study was conducted on 30 individuals, and the Cronbach's alpha was measured for perceived susceptibility (0.86), perceived severity (0.85), perceived benefits (0.89), perceived barriers (0.84), perceived self-efficacy (0.87), cues to action (0.81), behavior (0.83), and knowledge (0.9), and the instrument reliability was confirmed since Cronbach's alpha values were greater than 0.7 for all constructs.
To analyze the data, descriptive indices such as frequency, and mean were utilized to report the demographic variables. Kolmogorov-Smirnov test was performed to check the data normality. Pearson correlation was applied to examine the association between variables. Linear regression was used to determine effective factors in the behavior based on the HBM variable. The analyses were performed by SPSS software with version 16. All analyses were statistically considered at a significance level of 0.05.
Findings
Data obtained from 400 questionnaires were analyzed in this study. The mean age of participants was 36.64±11.82 years. Most participants were in the age groups of 45-49 years and 35-39 years respectively. Most people were married, with a bachelor's degree, and were housewives (Table 1).
The mean scores of perceived severity, knowledge, and cues to action were higher than other constructs (Table 2).
The results of the correlation coefficient table indicated that preventive behaviors had a significant positive correlation with self-efficacy (p<0.001), perceived benefits (p<0.001), perceived susceptibility (p=0.002), perceived severity (p<0.001), cues to action (p<0.001), and knowledge (p<0.001), and a significant negative correlation with perceived barriers (p<0.001); and the strongest correlation belonged to self-efficacy construct. Among the constructs, the strongest correlation belonged to self-efficacy and perceived benefits (Table 3).
According to Table 3, official Internet news
agencies, the media, and finally physicians and healthcare personnel were the most important sources of information about COVID-19. The
printed media played the least role in receiving information (Table 4).
In regression analysis using the forward method, self-efficacy, cues to action, knowledge, and perceived barriers remained in the final model as predictors of COVID-19 preventive behaviors. Based on the results of the regression analysis table, the constructs of the health belief model could predict 50% of the variance of preventive behaviors and self-efficacy was the strongest predictor (Table 5).
Table 1) Frequency distribution of demographic characteristics of the participants (n= 400)
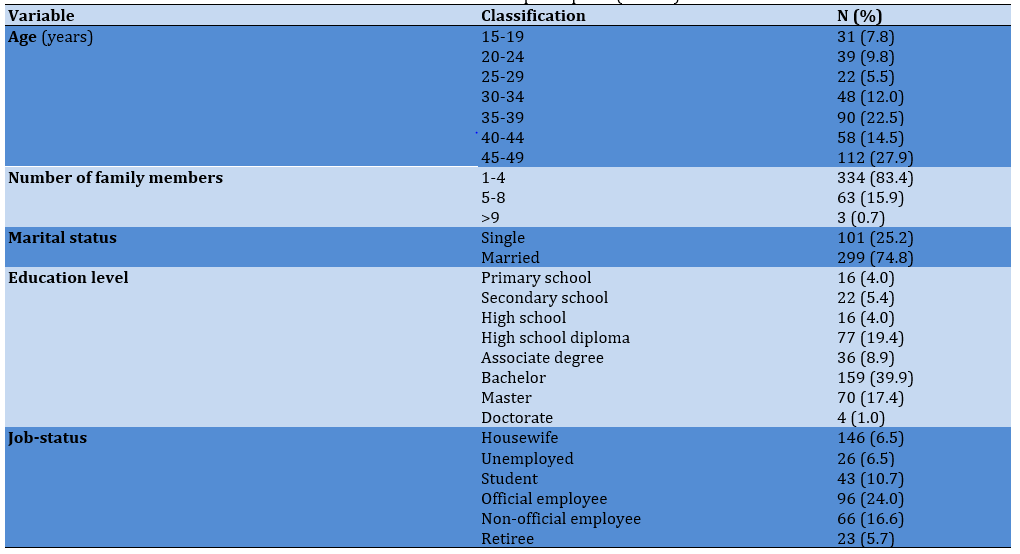
Table 2) Mean results of health belief model constructs
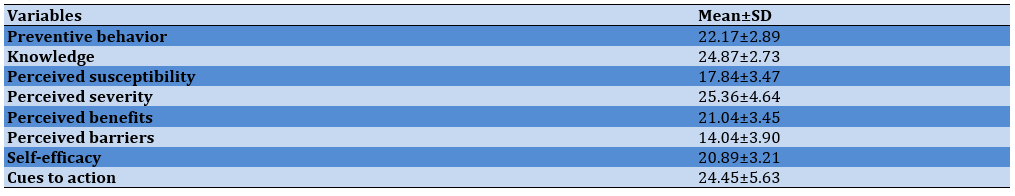
Table 3) Correlation between health belief model constructs
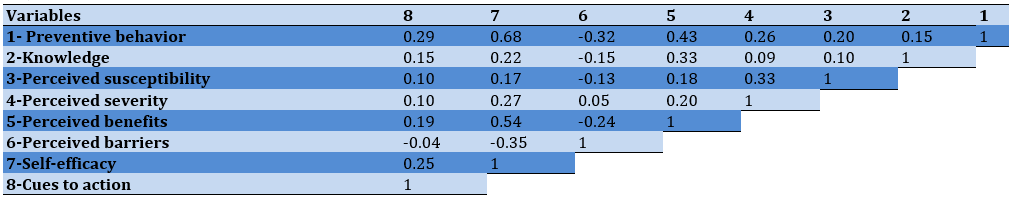
Table 4) Frequency distribution of information sources about COVID-19
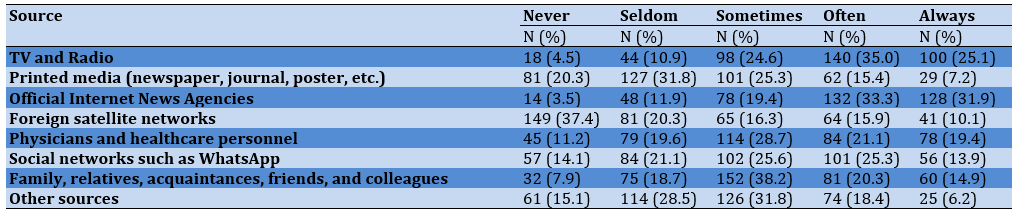
Table 5) Results of predictors of COVID-19 preventive behavior (R2=0.500)
Discussion
The present study aimed to investigate the determinants of COVID-19 preventive behaviors among women of reproductive age in Urmia using a behavioral change model. The mean score of knowledge of most participants was relatively high, and the result was consistent with Albaqawi's findings in Saudi female students and Aly SA in Malaysian pregnant women [15, 16]. Investigating four generations of Hungarian women, Marschalko et al. found a high level of knowledge of the third generation about COVID-19 and acknowledged that even though high knowledge was necessary to follow preventative behaviors, it was insufficient to change health behavior and manage the disease [17]. A study in India indicated that despite the high knowledge of most women, they were less likely than men to recognize all main symptoms of the disease [18] probably due to the challenge of equal access to information. Therefore, sufficient knowledge about COVID-19 can ensure women's readiness to respond to similar public health crises in the future. However, the caution of the relevant agencies is very important to prevent the dissemination of incorrect and misleading information.
The results indicated that the mean scores of women's preventive behaviors were at a desirable level. Yue et al. found that most Chinese pregnant women took protective measures such as wearing masks (97.4%), frequent hand-washing (88.3%), and staying at home (76.3%) [19]. Anderson also indicated that women in the United States performed better at staying home (except for essential activities), physical distancing, and wearing masks in public places [20]. However, a low percentage of the population studied by Tadesse et al. adopted COVID-19 preventive behaviors [21], and their result was inconsistent with the present study probably due to differences in the perception of risk in different societies and cultures. Since women can be behavior models and their participation in prevention is very important, and also preventive behaviors are vital to minimize the transmission of COVID-19 and ultimately reduce the health, social, and economic burden of society, government participation in promoting measures to increase the convenience of staying at home, teleworking support, and adapting the public space to facilitate and enhance the physical distance. The high preventive performance of women in the study can be due to the high prevalence of COVID-19 and the increase in hospitalizations and deaths in a short time in the world, and Iran, especially Urmia.
The mean perceived susceptibility score was relatively proper in most female participants. The research findings also indicated a high level of perceived severity in the majority of them, and the result was consistent with a study by Rattay et al. on German women [22]. In a study in Turkey, 52% of women felt vulnerable to COVID-19, and 80% of them were mainly concerned about complications of the disease [23]. Furthermore, about one-third (36.4%) of Chinese pregnant women considered themselves or their family members susceptible to the disease, and about 78% believed that the disease would have serious consequences [24]. In a Smail et al.'s study, in which more than half of the participants were American women, perceived susceptibility values were zero, low, and high in 17.7%, 42.8%, and 39.5% of the participants respectively, and their perceived severity values were zero, low, and high in 20.7%, 55.6%, and 23.7% of the participants [25]. Given that perceived susceptibility is a person's mental belief in illness or possible injury, its high level indicates individuals' perception of susceptibility to the disease; hence, they are more likely to take measures such as taking preventative behaviors to prevent the occurrence of the disease. In this regard, Sim et al. considered perceived susceptibility necessary to increase the use of masks in people [26]. Perceived severity also refers to individuals' beliefs about the mental effects of the disease and its impact on life. Due to the high perceived severity of women in this study, the higher hospitalization and severe complications of the disease make individuals perceive the disease severity after assessing the pain level, mortality, and social consequences of the disease (impact on work, impact on family life, and social relationships), and accept preventive behavior. Given that the combination of severity with susceptibility constitutes a perceived threat, perceiving the severity of complications of a disease without perceiving the susceptibility to it alone cannot lead to preventive behavior. A study in the United States found that a high perceived threat led to adherence to COVID-19 reduction strategies [27] but Yue reported a moderate level of perceiving the risk of COVID-19 in Chinese pregnant women [19], and the result was inconsistent with the present study.
In this study, the most important sources of information about COVID-19 were the official Internet news agencies, radio and television, physicians, and healthcare personnel. Important sources of information reported in Khafaei's study were radio and television, physicians, health workers, and social media [28]. Hashemi et al. reported health personnel, family, and the mass media as external cues and stimuli used by pregnant women [28]. Lin et al. also found that the mean scores of health belief model constructs were significantly higher in social media users [29]. Given the importance of mass media, especially virtual networks in transmitting health messages and the lack of gatherings to reduce the transmission of COVID-19, their high potential can be used to increase awareness and encourage people to exhibit COVID-19 preventive behaviors.
The mean scores of perceived benefits of most participating women were high. According to the individual's belief in the usefulness of adopting appropriate behaviors in this construct, these women believe that personal hygiene, social distancing, and the use of masks decreased the probability of COVID-19. The findings of the present study were consistent with the results of studies [2, 12]. In a study by Sim et al., most women had a high understanding of the benefits of preventive behaviors, especially the use of masks, in respiratory infections [25] probably due to continuous education and promotion of wearing masks as an effective tool in disease prevention. In the general population of northern Ethiopia, it was found that 72% of the participants believed in the usefulness of COVID-19 preventive behaviors [30]. It seems that appropriate information can lead women's beliefs and attitudes towards a higher perception of the benefits of preventive behaviors. Furthermore, widespread social media coverage and the World Health Organization's emphasis on personal hygiene in its slogans as the only way to overcome this disease can also be effective in increasing perceived benefits in women.
Perceived barriers to preventive behaviors were almost low in this study, and the result was consistent with the findings of Jose's study in which 60% of the participants were women in India [31]. Low perceived barriers were a plus as participants believed that they faced fewer barriers to engaging in preventative behaviors. In the Shahnazi et al. study, in which almost half of the respondents were female, there were fewer barriers to individual preventive behaviors such as hand washing, but environmental barriers such as lack of masks and disinfectants strongly affected participants [32]. A study in China also indicated the lack of masks for the public as the main reason for not adopting COVID-19 preventative behavior [33]. Understanding more benefits versus fewer barriers provides a better way to perform the behavior. Therefore, measures can be taken to minimize barriers to performing COVID-19 preventive behaviors by designing and implementing appropriate interventions.
The research findings indicated that the mean self-efficacy scores were high in most women, and the result was consistent with studies [2, 12] but only slightly more than half of the pregnant women reported high levels of self-efficacy in a study in China [23]. The results of a study by Wahyuni et al. also indicated that 80% of pregnant Malaysian women had poor self-efficacy [34] and the result was inconsistent with the results of the present study probably due to specific pregnancy conditions. Self-efficacy is the individuals' judgment of their ability to perform particular actions and can be considered the most important precondition for behavioral change. According to the Ministry of Health and Social Media, women's knowledge seems to have increased compared to the early onset of the pandemic, and the women's self-efficacy has increased, and eventually, their level of adoption of these behaviors has also increased with the increased perceived susceptibility and severity of COVID-19 infection, perceived benefits, and barriers of preventive behaviors.
The results of the correlation coefficient indicated that preventive behaviors were positively correlated with perceived knowledge, susceptibility, severity, benefits, and self-efficacy, and negatively correlated with perceived barriers. Khafaie's findings also indicated that COVID-19 preventive behaviors were positively correlated with perceived sensitivity, perceived severity, perceived benefits, and self-efficacy, and negatively correlated with perceived barriers [12]. However, the level of correlation was not high in the present study, and the strongest correlation was between self-efficacy and perceived benefits, indicating a high perception of the benefits of preventive behaviors, and a positive belief in the effectiveness of these behaviors. Pellymonter reported a negative correlation between social distancing with barriers and a positive correlation with perceived benefits and susceptibility [35].
Based on the results of regression analysis, the constructs of the health belief model could predict a total of 50% of the variance of COVID-19 preventive behaviors, among which self-efficacy was the strongest predictor. In Noghabi's study, in which about 60% of the participants were women, the health belief model was responsible for 73.3% of the variance of COVID-19 preventive behaviors, and self-efficacy and cues to action constructs were the strongest predictors [36]. According to Mehanna's findings, 43% of the variance of COVID-19 preventive behaviors was predicted by the Health Belief Model [11] but Mirzaei and Khazaee-Pool reported 29.9% and 26% of the predictive the ability of the model for preventive behaviors respectively [2, 37].
The strengths of the present study included the selection of women as the target group and they could be received special attention in pandemic conditions due to their important roles in society and family. A limitation of the study was the nature of the self-report and online completion of the questionnaire which could affect the data reliability and quality. Given that only people with access to smartphones and the Internet could participate, other people's chances of completing the questionnaire were lost. Due to the difference in perception of risk in different societies and cultures, it is recommended to conduct similar studies and use other models of behavioral change in different regions of Iran.
Conclusion
According to the effective role of the research model in explaining the determinants of COVID-19 preventive behaviors, the health belief model and effective constructs in educational planning and interventions can be used to promote preventive behaviors.
Acknowledgments: The authors are grateful to the Research Deputy of Urmia University of Medical Sciences, and women of reproductive age in this city for their cooperation in the present research.
Ethical Permissions: The present study was taken from a master's thesis approved by Urmia University of Medical Sciences with an ethical code (IR.UMSU.REC.1400, 109).
Conflicts of Interests: The authors declared no conflict of interest.
Authors’ Contributions: Yasamani K (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Khalkhali H (Second Author), Statistical Analyst (15%); Farrokh Eslamlou H (Third Author), Methodologist/Assistant Researcher (5%); Didarlou A (Forth Author), Methodologist/Main Researcher/Discussion Writer (40%)
Funding/Support: Urmia University of Medical Sciences funded the present study.
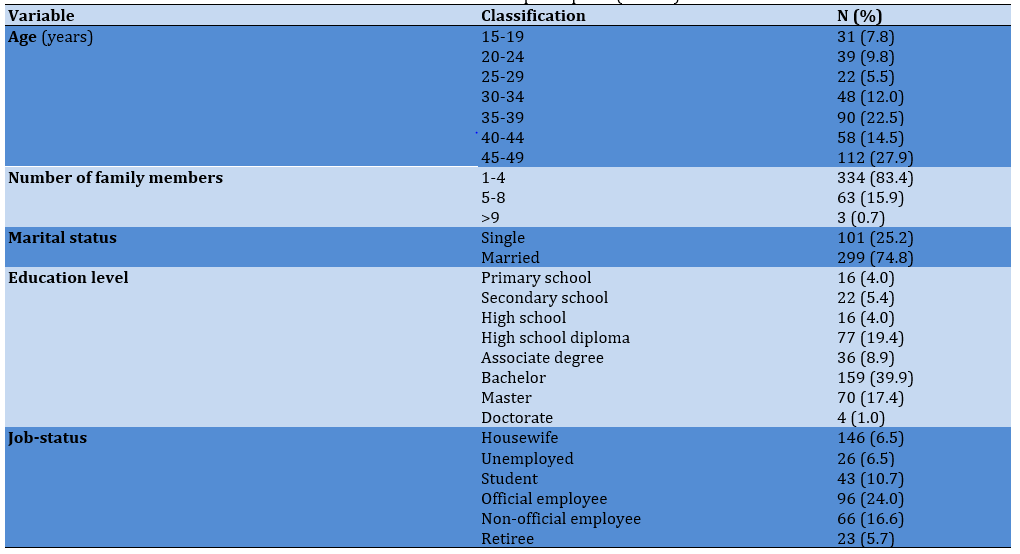
Table 2) Mean results of health belief model constructs
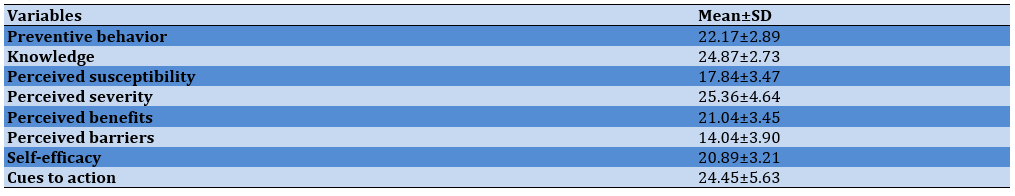
Table 3) Correlation between health belief model constructs
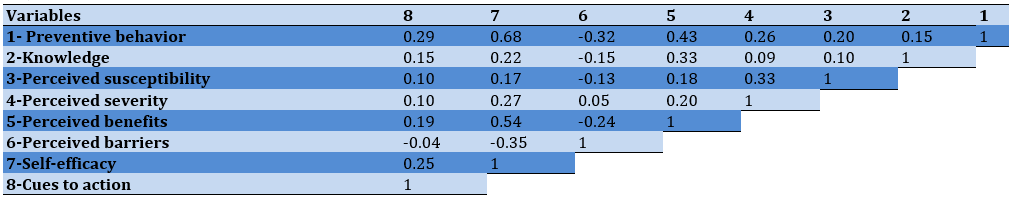
Table 4) Frequency distribution of information sources about COVID-19
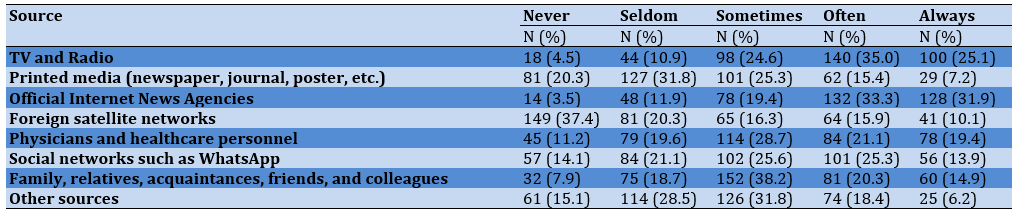
Table 5) Results of predictors of COVID-19 preventive behavior (R2=0.500)
Discussion
The present study aimed to investigate the determinants of COVID-19 preventive behaviors among women of reproductive age in Urmia using a behavioral change model. The mean score of knowledge of most participants was relatively high, and the result was consistent with Albaqawi's findings in Saudi female students and Aly SA in Malaysian pregnant women [15, 16]. Investigating four generations of Hungarian women, Marschalko et al. found a high level of knowledge of the third generation about COVID-19 and acknowledged that even though high knowledge was necessary to follow preventative behaviors, it was insufficient to change health behavior and manage the disease [17]. A study in India indicated that despite the high knowledge of most women, they were less likely than men to recognize all main symptoms of the disease [18] probably due to the challenge of equal access to information. Therefore, sufficient knowledge about COVID-19 can ensure women's readiness to respond to similar public health crises in the future. However, the caution of the relevant agencies is very important to prevent the dissemination of incorrect and misleading information.
The results indicated that the mean scores of women's preventive behaviors were at a desirable level. Yue et al. found that most Chinese pregnant women took protective measures such as wearing masks (97.4%), frequent hand-washing (88.3%), and staying at home (76.3%) [19]. Anderson also indicated that women in the United States performed better at staying home (except for essential activities), physical distancing, and wearing masks in public places [20]. However, a low percentage of the population studied by Tadesse et al. adopted COVID-19 preventive behaviors [21], and their result was inconsistent with the present study probably due to differences in the perception of risk in different societies and cultures. Since women can be behavior models and their participation in prevention is very important, and also preventive behaviors are vital to minimize the transmission of COVID-19 and ultimately reduce the health, social, and economic burden of society, government participation in promoting measures to increase the convenience of staying at home, teleworking support, and adapting the public space to facilitate and enhance the physical distance. The high preventive performance of women in the study can be due to the high prevalence of COVID-19 and the increase in hospitalizations and deaths in a short time in the world, and Iran, especially Urmia.
The mean perceived susceptibility score was relatively proper in most female participants. The research findings also indicated a high level of perceived severity in the majority of them, and the result was consistent with a study by Rattay et al. on German women [22]. In a study in Turkey, 52% of women felt vulnerable to COVID-19, and 80% of them were mainly concerned about complications of the disease [23]. Furthermore, about one-third (36.4%) of Chinese pregnant women considered themselves or their family members susceptible to the disease, and about 78% believed that the disease would have serious consequences [24]. In a Smail et al.'s study, in which more than half of the participants were American women, perceived susceptibility values were zero, low, and high in 17.7%, 42.8%, and 39.5% of the participants respectively, and their perceived severity values were zero, low, and high in 20.7%, 55.6%, and 23.7% of the participants [25]. Given that perceived susceptibility is a person's mental belief in illness or possible injury, its high level indicates individuals' perception of susceptibility to the disease; hence, they are more likely to take measures such as taking preventative behaviors to prevent the occurrence of the disease. In this regard, Sim et al. considered perceived susceptibility necessary to increase the use of masks in people [26]. Perceived severity also refers to individuals' beliefs about the mental effects of the disease and its impact on life. Due to the high perceived severity of women in this study, the higher hospitalization and severe complications of the disease make individuals perceive the disease severity after assessing the pain level, mortality, and social consequences of the disease (impact on work, impact on family life, and social relationships), and accept preventive behavior. Given that the combination of severity with susceptibility constitutes a perceived threat, perceiving the severity of complications of a disease without perceiving the susceptibility to it alone cannot lead to preventive behavior. A study in the United States found that a high perceived threat led to adherence to COVID-19 reduction strategies [27] but Yue reported a moderate level of perceiving the risk of COVID-19 in Chinese pregnant women [19], and the result was inconsistent with the present study.
In this study, the most important sources of information about COVID-19 were the official Internet news agencies, radio and television, physicians, and healthcare personnel. Important sources of information reported in Khafaei's study were radio and television, physicians, health workers, and social media [28]. Hashemi et al. reported health personnel, family, and the mass media as external cues and stimuli used by pregnant women [28]. Lin et al. also found that the mean scores of health belief model constructs were significantly higher in social media users [29]. Given the importance of mass media, especially virtual networks in transmitting health messages and the lack of gatherings to reduce the transmission of COVID-19, their high potential can be used to increase awareness and encourage people to exhibit COVID-19 preventive behaviors.
The mean scores of perceived benefits of most participating women were high. According to the individual's belief in the usefulness of adopting appropriate behaviors in this construct, these women believe that personal hygiene, social distancing, and the use of masks decreased the probability of COVID-19. The findings of the present study were consistent with the results of studies [2, 12]. In a study by Sim et al., most women had a high understanding of the benefits of preventive behaviors, especially the use of masks, in respiratory infections [25] probably due to continuous education and promotion of wearing masks as an effective tool in disease prevention. In the general population of northern Ethiopia, it was found that 72% of the participants believed in the usefulness of COVID-19 preventive behaviors [30]. It seems that appropriate information can lead women's beliefs and attitudes towards a higher perception of the benefits of preventive behaviors. Furthermore, widespread social media coverage and the World Health Organization's emphasis on personal hygiene in its slogans as the only way to overcome this disease can also be effective in increasing perceived benefits in women.
Perceived barriers to preventive behaviors were almost low in this study, and the result was consistent with the findings of Jose's study in which 60% of the participants were women in India [31]. Low perceived barriers were a plus as participants believed that they faced fewer barriers to engaging in preventative behaviors. In the Shahnazi et al. study, in which almost half of the respondents were female, there were fewer barriers to individual preventive behaviors such as hand washing, but environmental barriers such as lack of masks and disinfectants strongly affected participants [32]. A study in China also indicated the lack of masks for the public as the main reason for not adopting COVID-19 preventative behavior [33]. Understanding more benefits versus fewer barriers provides a better way to perform the behavior. Therefore, measures can be taken to minimize barriers to performing COVID-19 preventive behaviors by designing and implementing appropriate interventions.
The research findings indicated that the mean self-efficacy scores were high in most women, and the result was consistent with studies [2, 12] but only slightly more than half of the pregnant women reported high levels of self-efficacy in a study in China [23]. The results of a study by Wahyuni et al. also indicated that 80% of pregnant Malaysian women had poor self-efficacy [34] and the result was inconsistent with the results of the present study probably due to specific pregnancy conditions. Self-efficacy is the individuals' judgment of their ability to perform particular actions and can be considered the most important precondition for behavioral change. According to the Ministry of Health and Social Media, women's knowledge seems to have increased compared to the early onset of the pandemic, and the women's self-efficacy has increased, and eventually, their level of adoption of these behaviors has also increased with the increased perceived susceptibility and severity of COVID-19 infection, perceived benefits, and barriers of preventive behaviors.
The results of the correlation coefficient indicated that preventive behaviors were positively correlated with perceived knowledge, susceptibility, severity, benefits, and self-efficacy, and negatively correlated with perceived barriers. Khafaie's findings also indicated that COVID-19 preventive behaviors were positively correlated with perceived sensitivity, perceived severity, perceived benefits, and self-efficacy, and negatively correlated with perceived barriers [12]. However, the level of correlation was not high in the present study, and the strongest correlation was between self-efficacy and perceived benefits, indicating a high perception of the benefits of preventive behaviors, and a positive belief in the effectiveness of these behaviors. Pellymonter reported a negative correlation between social distancing with barriers and a positive correlation with perceived benefits and susceptibility [35].
Based on the results of regression analysis, the constructs of the health belief model could predict a total of 50% of the variance of COVID-19 preventive behaviors, among which self-efficacy was the strongest predictor. In Noghabi's study, in which about 60% of the participants were women, the health belief model was responsible for 73.3% of the variance of COVID-19 preventive behaviors, and self-efficacy and cues to action constructs were the strongest predictors [36]. According to Mehanna's findings, 43% of the variance of COVID-19 preventive behaviors was predicted by the Health Belief Model [11] but Mirzaei and Khazaee-Pool reported 29.9% and 26% of the predictive the ability of the model for preventive behaviors respectively [2, 37].
The strengths of the present study included the selection of women as the target group and they could be received special attention in pandemic conditions due to their important roles in society and family. A limitation of the study was the nature of the self-report and online completion of the questionnaire which could affect the data reliability and quality. Given that only people with access to smartphones and the Internet could participate, other people's chances of completing the questionnaire were lost. Due to the difference in perception of risk in different societies and cultures, it is recommended to conduct similar studies and use other models of behavioral change in different regions of Iran.
Conclusion
According to the effective role of the research model in explaining the determinants of COVID-19 preventive behaviors, the health belief model and effective constructs in educational planning and interventions can be used to promote preventive behaviors.
Acknowledgments: The authors are grateful to the Research Deputy of Urmia University of Medical Sciences, and women of reproductive age in this city for their cooperation in the present research.
Ethical Permissions: The present study was taken from a master's thesis approved by Urmia University of Medical Sciences with an ethical code (IR.UMSU.REC.1400, 109).
Conflicts of Interests: The authors declared no conflict of interest.
Authors’ Contributions: Yasamani K (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Khalkhali H (Second Author), Statistical Analyst (15%); Farrokh Eslamlou H (Third Author), Methodologist/Assistant Researcher (5%); Didarlou A (Forth Author), Methodologist/Main Researcher/Discussion Writer (40%)
Funding/Support: Urmia University of Medical Sciences funded the present study.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2022/01/27 | Accepted: 2022/07/25 | Published: 2022/09/17
Received: 2022/01/27 | Accepted: 2022/07/25 | Published: 2022/09/17
References
1. Zorriehzahra M J, Dadar M, Ziarati M, Seidgar M, Hassantabar F, Rashidi Monfared S, et al. A perspective on the origin of COVID-19 and its epidemic situation in Iran and the world. J Mar Med. 2020;2(1):41-52. [Link]
2. Khazaee-Pool M, Shahrvsand S, Naghibi SA. Predicting COVID-19 preventive behaviors based on health belief model: an internet-based study in Mazandaran province, Iran. J Mazandaran Univ Med Sci. 2020;30(190):56-66. [Link]
3. Worldometer. WHO: Novel Coronavirus [Internet]. Worldometer; 2021 [cited 2022 Jan 1]. Available from: https://www.worldometers.info/coronavirus/who-coronavirus/ [Link]
4. Jafari S, Farshid R, Jabbari L. Thematic analysis of COVID-19 studies in five large continents. Scientometr Res J. 2020;6(11):277-97. [Persian] [Link]
5. Jalali Farahani A, Ashourzadeh Fallah S, Khashei Z, Heidarzadeh F, Sadeghi F, Masoudi P, et al. Available effective vaccines in preventing COVID-19: a narrative review. J Mar Med. 2021;3(4):153-62. [Persian] [Link]
6. Farnoosh G, Alishiri G, Hosseini Zijoud SR, Dorostkar R, Jalali Farahani A. Understanding the severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus disease (COVID-19) based on available evidence-a narrative review. J Mil Med. 2020;22(1):1-11. [Persian] [Link]
7. Lin CY, Imani V, Majd NR, Ghasemi Z, Griffiths MD, Hamilton K, et al. Using an integrated social cognition model to predict COVID‐19 preventive behavior. Br J Health Psychol. 2020;25(4):981-1005. [Link] [DOI:10.1111/bjhp.12465]
8. Bagheri Lankarani K, Khayamzadeh M. Points for improving the COVID-19 national control program. 2021;5(2):143-51. [Persian] [Link]
9. Thoma V, Weiss-Cohen L, Filkuková P, Ayton P. Cognitive predictors of precautionary behavior during the COVID-19 pandemic. Front Psychol. 2021;12:325. [Link] [DOI:10.3389/fpsyg.2021.589800]
10. Sadeghi R, Mazloomy S, Hashemi M, Rezaeian M. The effects of an educational intervention based on the health belief model to enhance HIV-preventive behaviors among male barbers in Sirjan. J Rafsanjan Univ Med Sci. 2016;15(3):235-46. [Persian] [Link]
11. Mehanna A, Elhadi YAM, Lucero-Prisno DE. Factors influencing intention to adhere to precautionary behavior in times of COVID-19 pandemic in Sudan: an application of the health belief model. medRxiv. 2020 June. [Link] [DOI:10.1101/2020.12.25.20248859]
12. Khafaei M, Mahjoub B, Mojaddam M. Evaluation of preventive behaviors of Corona Virus (COVID-2019) among family health ambassadors of Ahvaz Jundishapur university of medical sciences in 2020 using the health belief model. Jundishapur Sci Med J. 2021;20(2):150-61. [Persian] [Link] [DOI:10.32598/JSMJ.20.2.7]
13. Mirhossieni Z. Qualitative evaluation of women's problems and life challenges during the COVID-19 pandemic. Soc Probl Iran. 2021;12(1):197-219. [Persian] [Link]
14. Taghizadeh Z, Ebadi A, Montazeri A, Shahvari Z, Tavousi M, Bagherzadeh R. Psychometric properties of health-related measures, part 1: translation, development, content, and face validity. PAYESH. 2017;16(3):343-57. [Persian] [Link]
15. Albaqawi HM, Alquwez N, Balay-Odao E, Bajet JB, Alabdulaziz H, Alsolami F, et al. Nursing students' perceptions, knowledge, and preventive behaviors toward COVID-19: a multi-university study. Front Public Health. 2020;8:573390. [Link] [DOI:10.3389/fpubh.2020.573390]
16. Syed Anwar Aly SA, Abdul Rahman R, Sharip S, Shah SA, Abdullah Mahdy Z, Kalok A. Pregnancy and COVID-19 pandemic perception in Malaysia: a cross-sectional study. Intl J Environ Res Public Health. 2021;18(11):5762. [Link] [DOI:10.3390/ijerph18115762]
17. Marschalko EE, Kotta I, Kalcza-Janosi K, Szabo K, Jancso-Farcas S. Psychological predictors of COVID-19 prevention behavior in Hungarian women across different generations. Front Psychol. 2021;12:596543. [Link] [DOI:10.3389/fpsyg.2021.596543]
18. Pinchoff J, Santhya KG, White C, Rampal S, Acharya R, Ngo TD. Gender-specific differences in COVID-19 knowledge, behavior and health effects among adolescents and young adults in Uttar Pradesh and Bihar, India. PloS One. 2020;15(12):e0244053. [Link] [DOI:10.1371/journal.pone.0244053]
19. Yue C, Liu C, Wang J, Zhang M, Wu H, Li C, et al. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: the mediating effect of risk perception. Int J Soc Psychiatry. 2021;67(2):120-7. [Link] [DOI:10.1177/0020764020941567]
20. Anderson KM, Stockman JK. Staying home, distancing, and face masks: COVID-19 prevention among U.S. women in The COPE study. Int J Environ Res Public Health. 2021;18(1):180. [Link] [DOI:10.3390/ijerph18010180]
21. Tadesse T, Alemu T, Amogne G, Endazenaw G, Mamo E. Predictors of Coronavirus disease 2019 (COVID-19) prevention practices using health belief model among employees in Addis Ababa, Ethiopia, 2020. Infect Drug Resist. 2020;13:3751-61. [Link] [DOI:10.2147/IDR.S275933]
22. Rattay P, Michalski N, Domanska OM, Kaltwasser A, de Bock F, Wieler LH, et al. Differences in risk perception, knowledge and protective behavior regarding COVID-19 by education level among women and men in Germany. Results from the COVID-19 snapshot monitoring (COSMO) study. Plos One. 2021;16(5):e0251694. [Link] [DOI:10.1371/journal.pone.0251694]
23. Yassa M, Birol P, Yirmibes C, Usta C, Haydar A, Yassa A, et al. Near-term pregnant women's attitude toward, concern about, and knowledge of the COVID-19 pandemic. J Matern Fetal Neonat Med. 2020;33(22):3827-34. [Link] [DOI:10.1080/14767058.2020.1763947]
24. Mo PKH, Fong VWI, Song B, Di J, Wang Q, Wang L. Association of perceived threat, negative emotions, and self-efficacy with mental health and personal protective behavior among chinese pregnant women during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. 2021;23(4):e24053. [Link] [DOI:10.2196/24053]
25. Smail E, Schneider KE, DeLong SM, Willis K, Arrington-Sanders R, Yang C, et al. Health beliefs and preventive behaviors among adults during the early COVID-19 pandemic in the United States: a latent class analysis. Prevent Sci. 2021;22(8):1013-22. [Link] [DOI:10.1007/s11121-021-01273-0]
26. Sim SW, Moey KSP, Tan NC. The use of facemasks to prevent respiratory infection: a literature review in the context of the health belief model. Singapore Med J. 2014;55(3):160-7. [Link] [DOI:10.11622/smedj.2014037]
27. Badr H, Oluyomi A, Woodard L, Zhang X, Raza SA, Fahmideh MA, et al. Sociodemographic and Health Belief Model Factors Associated with Nonadherence to COVID-19 Mitigation Strategies in the United States. Ann Behav Med. 2021;55(7):677-85. [Link] [DOI:10.1093/abm/kaab038]
28. Hashemi M, Sadeghi R, Shamsi M. An investigation of educational intervention impact on pregnant women for promoting preventive behaviors of influenza H1N1: using health belief model. KOOMESH. 2017;19(3):603-10. [Persian] [Link]
29. Lin Y, Hu Z, Alias H, Wong LP. Influence of mass and social media on psychobehavioral responses among medical students during the downward trend of COVID-19 in Fujian, China: a cross-sectional study. J Med Internet Res. 2020;22(7):e19982. [Link] [DOI:10.2196/19982]
30. Shewasinad Yehualashet S, Asefa KK, Mekonnen AG, Gemeda BN, Shiferaw WS, Aynalem YA, et al. Predictors of adherence to COVID-19 prevention measure among communities in North Shoa Zone, Ethiopia based on health belief model: a cross-sectional study. PLoS One. 2021;16(1):e0246006. [Link] [DOI:10.1371/journal.pone.0246006]
31. Jose R, Narendran M, Bindu A, Beevi N, Manju L, Benny P. Public perception and preparedness for the pandemic COVID-19: a health belief model approach. Clin Epidemiol Glob Health. 2021;9:41-6. [Link] [DOI:10.1016/j.cegh.2020.06.009]
32. Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID-19: a cross-sectional study with health belief model in Golestan province, northern of Iran. Infect Dis Poverty. 2020;9(1):157. [Link] [DOI:10.1186/s40249-020-00776-2]
33. Mahase E. Novel Coronavirus: Australian GPs raise concerns about the shortage of face masks. Br Med J; 2020;368:m477. [Link] [DOI:10.1136/bmj.m477]
34. Wahyuni S, Rahayu T. Self efficacy of pregnant women in areas affected by COVID-19. Enfermería Clínica. 2021;31(S4):601-4. [Link] [DOI:10.1016/j.enfcli.2021.04.021]
35. Pellymonter K, Butler A, Dethlefs T. Predicting COVID-19 health behaviors using the health belief model. 2020;22. [Link]
36. Delshad Noghabi A, Yoshany N, Mohammadzadeh F, Javanbakht S. Predictors of COVID-19 preventive behaviors in Iranian population over 15 years old: an application of health belief model. J Mazandaran Univ Med Sci. 2020;30(191):13-21. [Persian] [Link]
37. Mirzaei A, Kazembeigi F, Kakaei H, Jalilian M, Mazloomi S, Nourmoradi H. Application of health belief model to predict COVID-19-preventive behaviors among a sample of Iranian adult population. J Educ Health Promot. 2021;10(69). [Link] [DOI:10.4103/jehp.jehp_747_20]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |