Volume 11, Issue 1 (2023)
Health Educ Health Promot 2023, 11(1): 173-180 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yaaqoob B, Kadhem S. Evaluating the Level of Knowledge of University Students about Diabetes Mellitus. Health Educ Health Promot 2023; 11 (1) :173-180
URL: http://hehp.modares.ac.ir/article-5-55911-en.html
URL: http://hehp.modares.ac.ir/article-5-55911-en.html
B.Y. Yaaqoob *1, S.A. Kadhem1
1- College of Health and Medical Technology, Middle Technical University, Baghdad, Iraq
Full-Text [PDF 926 kb]
(661 Downloads)
| Abstract (HTML) (608 Views)
Full-Text: (241 Views)
Introduction
Diabetes mellitus is a metabolic group of diseases characterized by the chronic increase of glucose in the blood. It ascends because the body is unable to yield enough insulin for its requests, either because of weakened insulin secretion, impaired insulin action, or both. Diabetes upsets about 300 million people worldwide and is on the upturn [1]. The major clinical manifestation of the diabetic state is hyperglycemia. However, insulin deficiency and/or insulin resistance also are associated with abnormalities in lipid and protein metabolism and with mineral and electrolyte disturbances. The vast majority of diabetic patients are classified into one of two broad categories: type 1 diabetes mellitus, which is caused by an absolute or near absolute deficiency of insulin, or type 2 diabetes mellitus, which is characterized by the presence of insulin resistance with an inadequate compensatory increase in insulin secretion. In addition, women who develop diabetes during their pregnancy are classified as having gestational diabetes. Finally, there are a variety of uncommon and diverse types of diabetes, which are caused by infections, drugs, endocrinopathies, pancreatic destruction, and genetic defects. These unrelated forms of diabetes are included in the “Other Specific Types” and classified separately [2].
Chronic exposure to high blood glucose is a prominent cause of renal failure, visual loss, and other types of tissue destruction. Diabetes is also biased to arterial disease because it is often accompanied by hypertension, lipid disorders, and obesity. Although the cause of chronic complications in diabetic patients is not exactly clear, it is thought that its main reason is the spontaneous attachment of glucose to the key proteins. Glycosylation of proteins (glucose attachment to proteins) is a non-enzymatic process and occurs in small amounts in healthy people. In diabetic patients, due to the continuous high concentration of glucose in body fluids, the glycosylation process is intensified, and the corresponding proteins lose their physiological functions. The appropriate way to prevent the chronic complications of diabetes is to control the blood glucose concentration in these patients through medicine therapy or diet [3, 4].
The incidence, prevalence, and controllability of diabetes are different in various geographical areas, and factors such as genetic background, lifestyle, and diet play a considerable role in it [5]. Importantly, the prevalence of diabetes mellitus is not equally shared among ethnic/racial groups, with blacks, Hispanics, and Native Americans having a higher prevalence. In addition to the tremendous health toll attributed to diabetes mellitus, the US economic impact of diabetes mellitus is staggering, as the cost of caring for diabetes mellitus is greater than $327 billion annually [6].
Diabetes is the fifth cause of death in the world. A recent report by the World Health Organization (WHO) shows that the adult population (over 20 years old) will increase by 64% in the world from 1995 to 2025, and the prevalence of diabetes will increase from 4% in 1995 to 45% in 2025. The number of diabetics will increase dramatically, and in developed countries, it will reach 72 million from 51 million people, and in developing countries, it will reach 228 million people from 84 million people [7]. However, in 2025, more than 75% of the total diabetic population will be in developing countries [5].
Though genetics play an important role in the development of diabetes, monozygotic twin studies have certainly shown the importance of environmental influences [8]. Individuals with diabetes have been shown to make a dramatic impact on the progression and development of their disease by participating in their own care [9]. This participation can succeed only if those with diabetes and their health care providers are informed about taking effective care for the disease. It is expected that those with the greatest knowledge will have a better understanding of the disease and have a better impact on the progression of the disease and complications [10].
The level of patients' knowledge of diabetes plays an important role in the self-management of the disease. It is considered that patients with good disease knowledge have a better understanding of the nature and consequences of diabetes and are less prone to various complications and severe exacerbations of diabetes [11, 12]. Diabetes self-care, which includes activities such as healthful eating, regular physical activity, foot care, medication adherence, and self-monitoring of blood glucose, is very important to keep the disease under control.8,9 The American Diabetic Association underlined that diabetic self-care is necessary to limit potential organ damage, and it can reduce the likelihood of hospitalizations and emergency visits.10 Patient knowledge concerning disease and self-care practices for patients is important to achieve the desired treatment targets and for the appropriate management of their disease [13].
According to preliminary research, a gap or lack of knowledge of chronic diseases can increase morbidity and mortality rates [14]. According to published studies, adequate knowledge and awareness and strict adherence and self-care measures would have a significant impact on morbidity and mortality rates, thereby aiding in disease control [15].
Sufficient knowledge about the disease and its effective factors is necessary for preventing and controlling diseases [16]. Knowledge is essential for adequate diabetes management, and self-management education is the cornerstone of treatment for all people with diabetes. Patients need the knowledge and skills to make informed choices and facilitate self-directed changes in behavior and ultimately reduce the risk of the associated complications [17]. Behavior and lifestyle changes are the keys to successful self-management of diabetes [18].
Several studies report that the knowledge of diabetes is poor in developing and under-developed countries [19-21], and the knowledge should be improved through continuous education by healthcare professionals like pharmacists, nurses, and physicians. Public knowledge about diabetes not only helps to fight the disease but also its complications and medical and socio-economic consequences [22]. Simple lifestyle modifications, such as a healthy diet that includes reduced sugar intake, are necessary to prevent and reduce the incidence of diabetes mellitus [22, 23]. Several studies in different countries have shown that age, gender, education level, socio-economic status, and family history of diabetes are related to good knowledge of diabetes [24-26].
The youth are the future of a country and are considered dynamic human capital that plays a vital role in nation-building. If students adopt sedentary lifestyles and are inclined to fast food and irregular eating habits, then there is a lot of probability of suffering from being overweight, obese, and, consequently, diabetes mellitus at a young age [27]. The level of awareness and knowledge regarding the disease among the population helps a community manage it properly both on the prevention and management front. It is very important to target the sections of society who are or would be involved in the care of diseased persons because if we succeed in creating good awareness and positive attitudes towards the difficulties and miseries of the patient in our future health care professionals, then we can expect positive trends both in planning and management side [28].
This study aimed to investigate the knowledge level about diabetes and its relationship with demographic factors in students of Health and Medical Technology University in Baghdad City.
Instruments and Methods
This cross-sectional study is a descriptive study, which was carried out on the students of Health and Medical Technology University in Baghdad City, Iraq, during 2021-2022.
Among these students, 119 subjects were studied, so at first, they were selected by simple random sampling method, and then those who were affected by diabetes and followed medicine therapy for diabetes entered into the study. The exclusion criteria were smoking, addiction to special medicine except for diabetes medicine, and no attendance to continue to participate in the study.
Data were collected using a research-made questionnaire consisting of two sections: The first section included demographic information (age, gender, marital status, occupation, habitat, and family history of diabetes), and the second section included diabetes information (cause of diabetes, diabetes type, sign and symptoms, complication of hyperglycemia, diagnosis method, mode of transmission, treatment, and prevention).
Data were presented as frequency and percentage. The levels of knowledge were classified into three classes, including adequate, acceptable and inadequate, in such a way that a response of more than 50% was considered as an adequate level of knowledge, a response between 30% and 50% was considered as an acceptable level of knowledge, and a response of less than 30% was considered as an inadequate level of knowledge.
A logistic regression test was used to investigate the contribution of demographic variables in the knowledge level of subjects. The collected data were analyzed using SPSS 22 software.
Findings
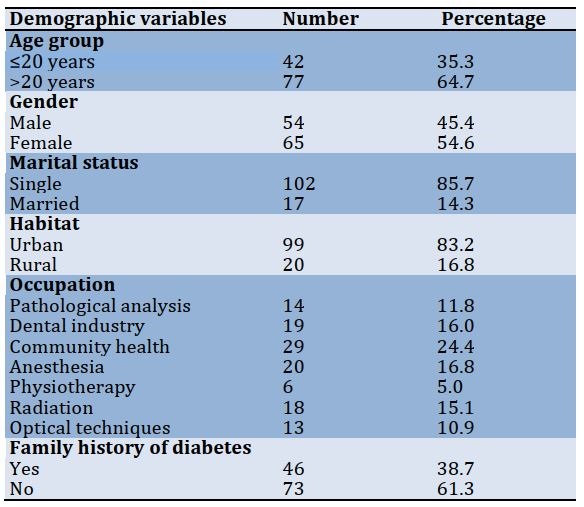
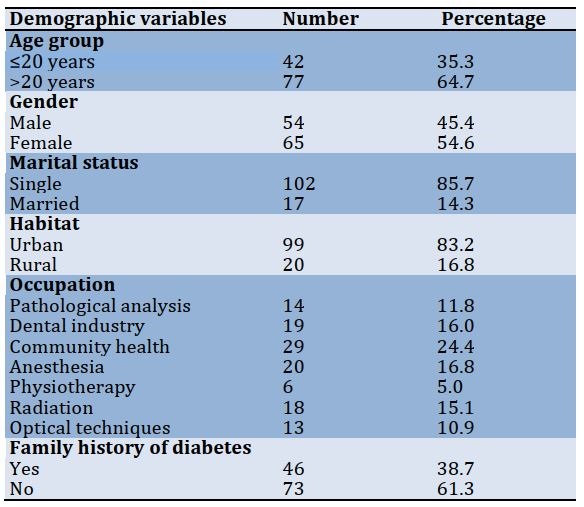
Out of 119 respondents, 45.4% were male, and 54.6% were female. The highest frequency was related to the age group of more than 20 years (64.7%), single people (85.7%), urban habitat (83.2%), and occupation of community health (24.4%). Also, 61.3% had no family history of diabetes (Table 1).
Table 1) Frequency distribution of demographic variables in students of Health and Medical Technology University in Baghdad City (n=119)
The frequency distribution of diabetes information in the studied students is presented in Table 2.
Table 2) Frequency distribution of diabetes information in students of Health and Medical Technology University in Baghdad City (n=119)

56 respondents (47.1%) had adequate knowledge, 33 respondents (27.7%) had acceptable knowledge, and 30 respondents (25.2%) had inadequate knowledge (Diagram 1).
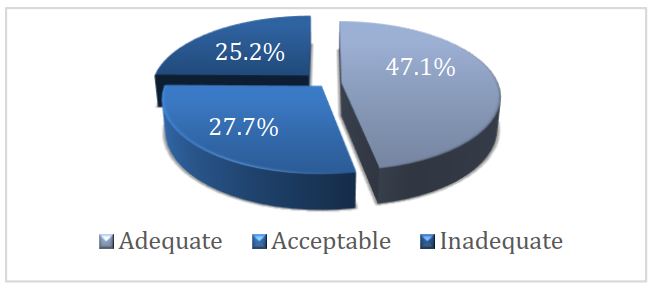
Diagram 1) Distribution of subject’s knowledge level
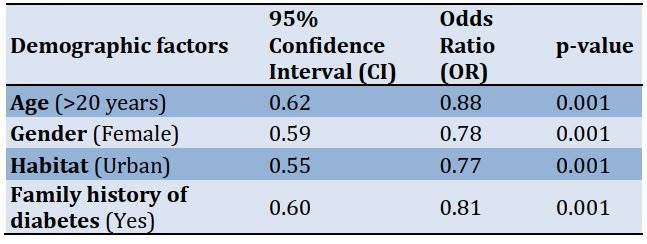
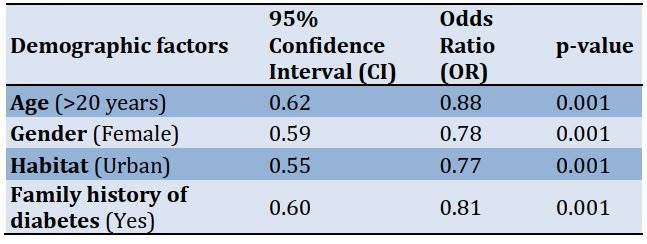
The contribution of four demographic factors, including age, gender, habitat, and family history of diabetes, in the adequate knowledge level of the subjects, was 88%, 78%, 77%, and 81%, respectively (Table 3).
Table 3) The results of the logistic regression test about the contribution of demographic factors in the knowledge level of the subjects
Discussion
Diabetes is a chronic disease affecting people of both genders and across all age groups. This disease is currently considered a major public health challenge worldwide, and raising awareness of risk factors and complications associated with diabetes has been a common strategy for controlling disease incidence [14]. Preparing future physicians for the great task that lies ahead starts with medical education during undergraduate years. Satisfactory knowledge of diabetes diagnosis, management, and patient education is crucial and pivotal. Studies showed that medical students possessed shortcomings in certain aspects of diabetes management that included insulin treatment options [29], diabetic dietary counseling [30], and management of hypoglycemia and perioperative diabetes management guidelines [31]. Therefore, appropriate knowledge of the diagnosis and accurate management of diabetes is of great importance. This study aimed to investigate the knowledge level about diabetes and its relationship with demographic factors in students of Health and Medical Technology University in Baghdad City during 2021-2022.
Studies have shown that increasing patient knowledge regarding disease and its complications has significant benefits concerning patient compliance to treatment and decreasing complications associated with the disease [32].
The results showed that the 47.1% of students had an adequate knowledge level (a response of more than 50%), and 25.2% had an inadequate knowledge level (a response of less than 30%). So, the knowledge of the students about diabetes was in a sufficient range.
This result is inconsistent with the findings by Ikizek [33] and Alanazi et al. [34]. Ikizek assessed the diabetes knowledge level of students studying in the field of health in Turkey and observed that the diabetes knowledge level of the students was limited. Therefore, he suggested that improvements should be made in the education curriculum to increase the knowledge and awareness of students about diabetes [33]. Alanazi et al. also investigated the knowledge and awareness of diabetes mellitus and its risk factors among the population of Saudi Arabia by summarizing available peer-reviewed publications about this topic. This review highlighted the need for increased knowledge and awareness of diabetes mellitus among the Saudi population [34]. However, our result is consistent with the findings by Alamri [35], which showed an encouraging knowledge level of diabetes among the students of Tabuk University.
Kwiendacz et al. evaluated diabetes-related knowledge among medicine students from all of the medical universities in Poland and proved that knowledge about diabetes mellitus among surveyed medical students in Poland is insufficient. Therefore, persistent improvement in transmitting it during the course of medical education is essential [36].
Gazzaz, in a study that investigated knowledge, attitudes, and practices regarding diabetes mellitus among university students in Jeddah, Saudi Arabia, showed that the students’ knowledge score was not up to the mark. Interestingly, participants had positive attitudes and practiced adequately for preventing diabetes mellitus, and the female gender was associated with good knowledge scores and positive attitudes [28].
The results of the logistic regression test about the contribution of demographic factors in the knowledge level of the subjects showed that the contribution of four demographic factors, including age, gender, habitat, and family history of diabetes, in the adequate knowledge level of the subjects, was 88%, 78%, 77%, and 81%, respectively. Older experienced students were more knowledgeable about diabetes than young students. Also, the knowledge level of students, who lived in an urban area, was more than that of students who lived in a rural area. These findings are in accordance with the findings of the study of Balla et al. [37], which showed that the prevalence of diabetes is increasing in the rural population of Sudan, and knowledge about diabetes is low. In addition, Bella et al. [37] showed the considerable contribution of the demographic factors of age (more than 30 years old), education level, a positive family of diabetes, gender (male), and smoking to the sufficient level of diabetes. Although, the contribution of male respondents was more than females, and it is not in accordance with the findings of this study.
Xu et al. carried out a cross-sectional study about self-reported knowledge of diabetes and its related factors among Chinese college students. This study indicated that the college students had low levels of knowledge about type 2 diabetes, with the rates of correct answers being <50% in the following areas: its chronic onset, sedentary lifestyles associated with the risk of diabetes, the monitoring index of blood glucose fluctuations, healthy dietary and exercise habits for treatment and its complications with eye problems and diabetic peripheral neuropathy. Additionally, gender was significantly associated with the level of knowledge, and female students had more general knowledge of diabetes than male students [38].
It was known that family history could induce the perception of disease risk. Those with a family history of diabetes tried to reduce or control the familial risk by adopting certain lifestyles or behaviors. This finding is consistent with the findings by Choi et al. [39]. Their study showed that participants with a diabetes-affected family member were living more actively and had healthier dietary habits but were less likely to have a normal body composition, which is a key factor for determining behavioral patterns [39].
In the last few decades, it has been established that diabetes can run in families, and people with a family history of diabetes are at a higher risk for developing diabetes. Behavioural change is the best-known modifiable risk factor, and healthy behaviors are known to be associated with a 40%–80% reduction in the risk of developing diabetes [40, 41]. It has been reported that family history can cause a perception of disease risk, and those who have a family history were more likely to have a greater perceived risk for diabetes [42, 43].
Also, Aldkhail [44] found significant knowledge about diabetes in men compared to women, which is different from our study. The differences may be due to the different studied communities. In the study of Gulabani et al. in India, the role of gender on knowledge regarding diabetes was evident, with women scoring significantly lower than men even after regulating other confounders [45].
Sahile et al. assessed diabetic self-care knowledge and its associated factors among adult diabetes mellitus patients. This study identified that being employed, having an urban residence, and having prior diabetic self-care knowledge were factors significantly associated with the diabetic self-care knowledge of the study participants [46].
In Sękowsk et al.'s study [47], females, those with higher education, respondents diagnosed with diabetes as well as those with a history of diabetes in the family were more likely to correctly indicate knowledge of diabetes. It should be noted that this study had been conducted among the public population.
Many studies conducted in very diverse populations have shown that girls and women performed better than boys and men regarding knowledge on diabetes mellitus, and the female gender had higher diabetes mellitus knowledge scores than the males [48-51].
Mohsen et al. assessed diabetes mellitus knowledge among Syrian medical students and reported that the knowledge and awareness of medical students about diabetes mellitus were found to have some gaps. In addition, this study identified old age, obesity, and a family history of diabetes as risk factors for diabetes mellitus [52].
Sabri et al. conducted a study in four selected regions of India and reported that overall urban residents had significantly higher awareness rates about diabetes (58.4%) compared to rural residents (36.8%). Thus, there is an urgent need to improve the awareness level of diabetes mellitus in rural areas [53].
According to the results of the present study, it can be said that conducting studies that evaluate the knowledge of medical students is essential to evaluate current curricula, experiential education, and clinical experience offered to medical students. Identifying gaps and possible predictors of poor knowledge will help members of educational boards and policymakers to develop and implement changes in the curricula. These modifications will enhance knowledge in areas where the deficit is detected and reflect on the quality of patient care and health care services provided to individuals with diabetes.
Conclusion
The knowledge of the students of Health and Medical Technology University in Baghdad City about diabetes is at a sufficient level. Four demographic factors, including age, gender, habitat, and family history of diabetes, play a role in the adequate knowledge level so that the older students, living in the city, with female gender, and with a positive family history of diabetes has adequate knowledge about diabetes mellitus.
Acknowledgements: We would like to thank all students who cooperated with us through their answers to our questions.
Ethical Permission: Nothing was reported by the authors.
Conflict of Interests: Nothing was reported by the authors.
Authors’ Contribution: Yaaqoob BY (First Author), Introduction Writer/Main Researcher/Statistical Analyst/Discussion Writer (50%); Kadhem SA (Second Author), Methodologist/Assistant Researcher/Discussion Writer (50%)
Funding: Nothing was reported by the authors.
Diabetes mellitus is a metabolic group of diseases characterized by the chronic increase of glucose in the blood. It ascends because the body is unable to yield enough insulin for its requests, either because of weakened insulin secretion, impaired insulin action, or both. Diabetes upsets about 300 million people worldwide and is on the upturn [1]. The major clinical manifestation of the diabetic state is hyperglycemia. However, insulin deficiency and/or insulin resistance also are associated with abnormalities in lipid and protein metabolism and with mineral and electrolyte disturbances. The vast majority of diabetic patients are classified into one of two broad categories: type 1 diabetes mellitus, which is caused by an absolute or near absolute deficiency of insulin, or type 2 diabetes mellitus, which is characterized by the presence of insulin resistance with an inadequate compensatory increase in insulin secretion. In addition, women who develop diabetes during their pregnancy are classified as having gestational diabetes. Finally, there are a variety of uncommon and diverse types of diabetes, which are caused by infections, drugs, endocrinopathies, pancreatic destruction, and genetic defects. These unrelated forms of diabetes are included in the “Other Specific Types” and classified separately [2].
Chronic exposure to high blood glucose is a prominent cause of renal failure, visual loss, and other types of tissue destruction. Diabetes is also biased to arterial disease because it is often accompanied by hypertension, lipid disorders, and obesity. Although the cause of chronic complications in diabetic patients is not exactly clear, it is thought that its main reason is the spontaneous attachment of glucose to the key proteins. Glycosylation of proteins (glucose attachment to proteins) is a non-enzymatic process and occurs in small amounts in healthy people. In diabetic patients, due to the continuous high concentration of glucose in body fluids, the glycosylation process is intensified, and the corresponding proteins lose their physiological functions. The appropriate way to prevent the chronic complications of diabetes is to control the blood glucose concentration in these patients through medicine therapy or diet [3, 4].
The incidence, prevalence, and controllability of diabetes are different in various geographical areas, and factors such as genetic background, lifestyle, and diet play a considerable role in it [5]. Importantly, the prevalence of diabetes mellitus is not equally shared among ethnic/racial groups, with blacks, Hispanics, and Native Americans having a higher prevalence. In addition to the tremendous health toll attributed to diabetes mellitus, the US economic impact of diabetes mellitus is staggering, as the cost of caring for diabetes mellitus is greater than $327 billion annually [6].
Diabetes is the fifth cause of death in the world. A recent report by the World Health Organization (WHO) shows that the adult population (over 20 years old) will increase by 64% in the world from 1995 to 2025, and the prevalence of diabetes will increase from 4% in 1995 to 45% in 2025. The number of diabetics will increase dramatically, and in developed countries, it will reach 72 million from 51 million people, and in developing countries, it will reach 228 million people from 84 million people [7]. However, in 2025, more than 75% of the total diabetic population will be in developing countries [5].
Though genetics play an important role in the development of diabetes, monozygotic twin studies have certainly shown the importance of environmental influences [8]. Individuals with diabetes have been shown to make a dramatic impact on the progression and development of their disease by participating in their own care [9]. This participation can succeed only if those with diabetes and their health care providers are informed about taking effective care for the disease. It is expected that those with the greatest knowledge will have a better understanding of the disease and have a better impact on the progression of the disease and complications [10].
The level of patients' knowledge of diabetes plays an important role in the self-management of the disease. It is considered that patients with good disease knowledge have a better understanding of the nature and consequences of diabetes and are less prone to various complications and severe exacerbations of diabetes [11, 12]. Diabetes self-care, which includes activities such as healthful eating, regular physical activity, foot care, medication adherence, and self-monitoring of blood glucose, is very important to keep the disease under control.8,9 The American Diabetic Association underlined that diabetic self-care is necessary to limit potential organ damage, and it can reduce the likelihood of hospitalizations and emergency visits.10 Patient knowledge concerning disease and self-care practices for patients is important to achieve the desired treatment targets and for the appropriate management of their disease [13].
According to preliminary research, a gap or lack of knowledge of chronic diseases can increase morbidity and mortality rates [14]. According to published studies, adequate knowledge and awareness and strict adherence and self-care measures would have a significant impact on morbidity and mortality rates, thereby aiding in disease control [15].
Sufficient knowledge about the disease and its effective factors is necessary for preventing and controlling diseases [16]. Knowledge is essential for adequate diabetes management, and self-management education is the cornerstone of treatment for all people with diabetes. Patients need the knowledge and skills to make informed choices and facilitate self-directed changes in behavior and ultimately reduce the risk of the associated complications [17]. Behavior and lifestyle changes are the keys to successful self-management of diabetes [18].
Several studies report that the knowledge of diabetes is poor in developing and under-developed countries [19-21], and the knowledge should be improved through continuous education by healthcare professionals like pharmacists, nurses, and physicians. Public knowledge about diabetes not only helps to fight the disease but also its complications and medical and socio-economic consequences [22]. Simple lifestyle modifications, such as a healthy diet that includes reduced sugar intake, are necessary to prevent and reduce the incidence of diabetes mellitus [22, 23]. Several studies in different countries have shown that age, gender, education level, socio-economic status, and family history of diabetes are related to good knowledge of diabetes [24-26].
The youth are the future of a country and are considered dynamic human capital that plays a vital role in nation-building. If students adopt sedentary lifestyles and are inclined to fast food and irregular eating habits, then there is a lot of probability of suffering from being overweight, obese, and, consequently, diabetes mellitus at a young age [27]. The level of awareness and knowledge regarding the disease among the population helps a community manage it properly both on the prevention and management front. It is very important to target the sections of society who are or would be involved in the care of diseased persons because if we succeed in creating good awareness and positive attitudes towards the difficulties and miseries of the patient in our future health care professionals, then we can expect positive trends both in planning and management side [28].
This study aimed to investigate the knowledge level about diabetes and its relationship with demographic factors in students of Health and Medical Technology University in Baghdad City.
Instruments and Methods
This cross-sectional study is a descriptive study, which was carried out on the students of Health and Medical Technology University in Baghdad City, Iraq, during 2021-2022.
Among these students, 119 subjects were studied, so at first, they were selected by simple random sampling method, and then those who were affected by diabetes and followed medicine therapy for diabetes entered into the study. The exclusion criteria were smoking, addiction to special medicine except for diabetes medicine, and no attendance to continue to participate in the study.
Data were collected using a research-made questionnaire consisting of two sections: The first section included demographic information (age, gender, marital status, occupation, habitat, and family history of diabetes), and the second section included diabetes information (cause of diabetes, diabetes type, sign and symptoms, complication of hyperglycemia, diagnosis method, mode of transmission, treatment, and prevention).
Data were presented as frequency and percentage. The levels of knowledge were classified into three classes, including adequate, acceptable and inadequate, in such a way that a response of more than 50% was considered as an adequate level of knowledge, a response between 30% and 50% was considered as an acceptable level of knowledge, and a response of less than 30% was considered as an inadequate level of knowledge.
A logistic regression test was used to investigate the contribution of demographic variables in the knowledge level of subjects. The collected data were analyzed using SPSS 22 software.
Findings
Out of 119 respondents, 45.4% were male, and 54.6% were female. The highest frequency was related to the age group of more than 20 years (64.7%), single people (85.7%), urban habitat (83.2%), and occupation of community health (24.4%). Also, 61.3% had no family history of diabetes (Table 1).
Table 1) Frequency distribution of demographic variables in students of Health and Medical Technology University in Baghdad City (n=119)
The frequency distribution of diabetes information in the studied students is presented in Table 2.
Table 2) Frequency distribution of diabetes information in students of Health and Medical Technology University in Baghdad City (n=119)

56 respondents (47.1%) had adequate knowledge, 33 respondents (27.7%) had acceptable knowledge, and 30 respondents (25.2%) had inadequate knowledge (Diagram 1).
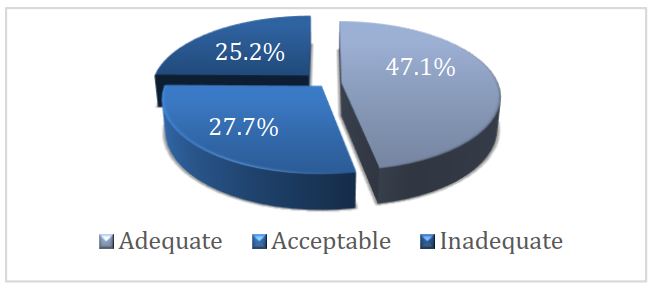
Diagram 1) Distribution of subject’s knowledge level
The contribution of four demographic factors, including age, gender, habitat, and family history of diabetes, in the adequate knowledge level of the subjects, was 88%, 78%, 77%, and 81%, respectively (Table 3).
Table 3) The results of the logistic regression test about the contribution of demographic factors in the knowledge level of the subjects
Discussion
Diabetes is a chronic disease affecting people of both genders and across all age groups. This disease is currently considered a major public health challenge worldwide, and raising awareness of risk factors and complications associated with diabetes has been a common strategy for controlling disease incidence [14]. Preparing future physicians for the great task that lies ahead starts with medical education during undergraduate years. Satisfactory knowledge of diabetes diagnosis, management, and patient education is crucial and pivotal. Studies showed that medical students possessed shortcomings in certain aspects of diabetes management that included insulin treatment options [29], diabetic dietary counseling [30], and management of hypoglycemia and perioperative diabetes management guidelines [31]. Therefore, appropriate knowledge of the diagnosis and accurate management of diabetes is of great importance. This study aimed to investigate the knowledge level about diabetes and its relationship with demographic factors in students of Health and Medical Technology University in Baghdad City during 2021-2022.
Studies have shown that increasing patient knowledge regarding disease and its complications has significant benefits concerning patient compliance to treatment and decreasing complications associated with the disease [32].
The results showed that the 47.1% of students had an adequate knowledge level (a response of more than 50%), and 25.2% had an inadequate knowledge level (a response of less than 30%). So, the knowledge of the students about diabetes was in a sufficient range.
This result is inconsistent with the findings by Ikizek [33] and Alanazi et al. [34]. Ikizek assessed the diabetes knowledge level of students studying in the field of health in Turkey and observed that the diabetes knowledge level of the students was limited. Therefore, he suggested that improvements should be made in the education curriculum to increase the knowledge and awareness of students about diabetes [33]. Alanazi et al. also investigated the knowledge and awareness of diabetes mellitus and its risk factors among the population of Saudi Arabia by summarizing available peer-reviewed publications about this topic. This review highlighted the need for increased knowledge and awareness of diabetes mellitus among the Saudi population [34]. However, our result is consistent with the findings by Alamri [35], which showed an encouraging knowledge level of diabetes among the students of Tabuk University.
Kwiendacz et al. evaluated diabetes-related knowledge among medicine students from all of the medical universities in Poland and proved that knowledge about diabetes mellitus among surveyed medical students in Poland is insufficient. Therefore, persistent improvement in transmitting it during the course of medical education is essential [36].
Gazzaz, in a study that investigated knowledge, attitudes, and practices regarding diabetes mellitus among university students in Jeddah, Saudi Arabia, showed that the students’ knowledge score was not up to the mark. Interestingly, participants had positive attitudes and practiced adequately for preventing diabetes mellitus, and the female gender was associated with good knowledge scores and positive attitudes [28].
The results of the logistic regression test about the contribution of demographic factors in the knowledge level of the subjects showed that the contribution of four demographic factors, including age, gender, habitat, and family history of diabetes, in the adequate knowledge level of the subjects, was 88%, 78%, 77%, and 81%, respectively. Older experienced students were more knowledgeable about diabetes than young students. Also, the knowledge level of students, who lived in an urban area, was more than that of students who lived in a rural area. These findings are in accordance with the findings of the study of Balla et al. [37], which showed that the prevalence of diabetes is increasing in the rural population of Sudan, and knowledge about diabetes is low. In addition, Bella et al. [37] showed the considerable contribution of the demographic factors of age (more than 30 years old), education level, a positive family of diabetes, gender (male), and smoking to the sufficient level of diabetes. Although, the contribution of male respondents was more than females, and it is not in accordance with the findings of this study.
Xu et al. carried out a cross-sectional study about self-reported knowledge of diabetes and its related factors among Chinese college students. This study indicated that the college students had low levels of knowledge about type 2 diabetes, with the rates of correct answers being <50% in the following areas: its chronic onset, sedentary lifestyles associated with the risk of diabetes, the monitoring index of blood glucose fluctuations, healthy dietary and exercise habits for treatment and its complications with eye problems and diabetic peripheral neuropathy. Additionally, gender was significantly associated with the level of knowledge, and female students had more general knowledge of diabetes than male students [38].
It was known that family history could induce the perception of disease risk. Those with a family history of diabetes tried to reduce or control the familial risk by adopting certain lifestyles or behaviors. This finding is consistent with the findings by Choi et al. [39]. Their study showed that participants with a diabetes-affected family member were living more actively and had healthier dietary habits but were less likely to have a normal body composition, which is a key factor for determining behavioral patterns [39].
In the last few decades, it has been established that diabetes can run in families, and people with a family history of diabetes are at a higher risk for developing diabetes. Behavioural change is the best-known modifiable risk factor, and healthy behaviors are known to be associated with a 40%–80% reduction in the risk of developing diabetes [40, 41]. It has been reported that family history can cause a perception of disease risk, and those who have a family history were more likely to have a greater perceived risk for diabetes [42, 43].
Also, Aldkhail [44] found significant knowledge about diabetes in men compared to women, which is different from our study. The differences may be due to the different studied communities. In the study of Gulabani et al. in India, the role of gender on knowledge regarding diabetes was evident, with women scoring significantly lower than men even after regulating other confounders [45].
Sahile et al. assessed diabetic self-care knowledge and its associated factors among adult diabetes mellitus patients. This study identified that being employed, having an urban residence, and having prior diabetic self-care knowledge were factors significantly associated with the diabetic self-care knowledge of the study participants [46].
In Sękowsk et al.'s study [47], females, those with higher education, respondents diagnosed with diabetes as well as those with a history of diabetes in the family were more likely to correctly indicate knowledge of diabetes. It should be noted that this study had been conducted among the public population.
Many studies conducted in very diverse populations have shown that girls and women performed better than boys and men regarding knowledge on diabetes mellitus, and the female gender had higher diabetes mellitus knowledge scores than the males [48-51].
Mohsen et al. assessed diabetes mellitus knowledge among Syrian medical students and reported that the knowledge and awareness of medical students about diabetes mellitus were found to have some gaps. In addition, this study identified old age, obesity, and a family history of diabetes as risk factors for diabetes mellitus [52].
Sabri et al. conducted a study in four selected regions of India and reported that overall urban residents had significantly higher awareness rates about diabetes (58.4%) compared to rural residents (36.8%). Thus, there is an urgent need to improve the awareness level of diabetes mellitus in rural areas [53].
According to the results of the present study, it can be said that conducting studies that evaluate the knowledge of medical students is essential to evaluate current curricula, experiential education, and clinical experience offered to medical students. Identifying gaps and possible predictors of poor knowledge will help members of educational boards and policymakers to develop and implement changes in the curricula. These modifications will enhance knowledge in areas where the deficit is detected and reflect on the quality of patient care and health care services provided to individuals with diabetes.
Conclusion
The knowledge of the students of Health and Medical Technology University in Baghdad City about diabetes is at a sufficient level. Four demographic factors, including age, gender, habitat, and family history of diabetes, play a role in the adequate knowledge level so that the older students, living in the city, with female gender, and with a positive family history of diabetes has adequate knowledge about diabetes mellitus.
Acknowledgements: We would like to thank all students who cooperated with us through their answers to our questions.
Ethical Permission: Nothing was reported by the authors.
Conflict of Interests: Nothing was reported by the authors.
Authors’ Contribution: Yaaqoob BY (First Author), Introduction Writer/Main Researcher/Statistical Analyst/Discussion Writer (50%); Kadhem SA (Second Author), Methodologist/Assistant Researcher/Discussion Writer (50%)
Funding: Nothing was reported by the authors.
Article Type: Original Research |
Subject:
Health Communication
Received: 2022/09/25 | Accepted: 2023/01/28 | Published: 2023/04/4
Received: 2022/09/25 | Accepted: 2023/01/28 | Published: 2023/04/4
References
1. Shi Y, Hu FB. The global implications of diabetes and cancer. Lancet. 2014;7(383):1947-8. [Link] [DOI:10.1016/S0140-6736(14)60886-2]
2. Solis-Herrera C, Triplitt C, Reasner C, DeFronzo RA, Cersosimo E. Classification of diabetes mellitus. In: Feingold KR, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, et al., editors. Endotext. South Dartmouth (MA): MDText.com, Inc.; 2018. [Link]
3. Bell KJ, Smart CE, Steil GM, Brand Miller J, King B, Wolpert HA. Impact of fat, protein, and glycemic index on postprandial glucose control in type 1 diabetes: implications for intensive diabetes management in the continuous glucose monitoring era. Diabetes Care. 2015;38(6):1008-15. [Link] [DOI:10.2337/dc15-0100]
4. Masoudi R, Kheiri S, Ali Akbari F, Eslami AA, Rabie L. Psychometrics and validation of the Iranian version of the diabetes health literacy assessment questionnaire. Iran J Diabetes Metab. 2020;19(6):353-45. [Persian] [Link]
5. Bayat F, Shojaeezadeh D, Baikpour M, Heshmat R, Baikpour M, Hosseini M. The effects of education based on extended health belief model in type 2 diabetic patients: a randomized controlled trial. J Diabetes Metab Disord. 2013;12(1):45 [Link] [DOI:10.1186/2251-6581-12-45]
6. American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-28. [Link] [DOI:10.2337/dci18-0007]
7. Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al. Effectiveness of the diabetes education and self-management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336(7642):491-5. [Link] [DOI:10.1136/bmj.39474.922025.BE]
8. Poulsen P, Kyvik KO, Vaag A, Nielsen-Beck H. Heritability of type II diabetes mellitus and abnormal glucose tolerance - a population-based twin study. Diabetologia. 1999;42(2):139-45. [Link] [DOI:10.1007/s001250051131]
9. UKPDS. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-53. [Link] [DOI:10.1016/S0140-6736(98)07019-6]
10. Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12:14. [Link] [DOI:10.1186/2251-6581-12-14]
11. Waheedi M, Awad A, Hatoum HT, Enlund H. The relationship between patients' knowledge of diabetes therapeutic goals and self-management behaviour, including adherence. Int J Clin Pharm. 2017;39(1):45-51. [Link] [DOI:10.1007/s11096-016-0375-5]
12. Chavan GM, Waghachavare VB, Gore AD, Chavan VM, Dhobale RV, Dhumale GB. Knowledge about diabetes and relationship between compliance to the management among the diabetic patients from Rural Area of Sangli District, Maharashtra, India. J Family Med Prim Care. 2015;4(3):439-43. [Link] [DOI:10.4103/2249-4863.161349]
13. Okonta HI, Ikombele JB, Ogunbanjo GA. Knowledge, attitude, and practice regarding lifestyle modification in type 2 diabetic patients. Afr J Prim Health Care Amp Fam Med. 2014;6(1):E1-6. [Link] [DOI:10.4102/phcfm.v6i1.655]
14. Wajid S, Samreen S, Sales I, Bawazeer G, Mahmoud MA, Aljohani MA. What has changed in the behaviors of the public after the COVID-19 pandemic? a cross-sectional study from the Saudi community perspective. Front Public Health. 2022;10:723229. [Link] [DOI:10.3389/fpubh.2022.723229]
15. Syed W, Alharbi MK, Samarkandi OA, Alsadoun A, Al-Rawi MBA, Iqbal A, et al. Evaluation of knowledge, awareness, and factors associated with diabetes: a cross-sectional community-based study. Int J Endocrinol. 2022;2022;1921010. [Link] [DOI:10.1155/2022/1921010]
16. Murugesan NSC, Shobhana R, Roglic G, Ramachandran A. Awareness about diabetes and its complications in the general and diabetic population in a city in Southern India. Diabetes Res Clin Pract. 2007;77(3):433-7. [Link] [DOI:10.1016/j.diabres.2007.01.004]
17. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al. National standard for diabetes self-management education and support. Diabetes Care. 2014;37 Suppl 1(Suppl 1):S144-53. [Link] [DOI:10.2337/dc14-S144]
18. Nehad MH, Istabraq DAA, Jyothi V, Hussain Y, Umar FU. Assessment of knowledge and awareness of diabetic and non-diabetic population towards diabetes mellitus in Kaduna, Nigeria. J Adv Sci Res. 2012;3(3):46-50 [Link]
19. Palanisamy S, ArulKumaran KSG, Rajasekaran A. Knowledge assessment in adverse drug reactions and reporting. Arch Pharm Pract. 2014;4(3):104-19. [Link] [DOI:10.4103/2045-080X.119063]
20. Singh A, Shenoy S, Sandhu JS. Prevalence of type 2 diabetes mellitus among urban Sikh population of Amritsar. Ind J Community Med. 2016;41(4):263-7. [Link] [DOI:10.4103/0970-0218.193338]
21. Acharya KG, Shah KN, Solanki ND, Rana DA. Evaluation of antidiabetic prescriptions, cost, and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospital. J Basic Clin Pharm. 2013;4(4):82-7. [Link] [DOI:10.4103/0976-0105.121653]
22. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetesmellitus by changes in lifestyle among subjects with impairedglucose tolerance. N Engl J Med. 2001;344(18):1343-50. [Link] [DOI:10.1056/NEJM200105033441801]
23. American Diabetes Association. The prevention or delay of type 2 diabetes. Diabetes care. 2002;25(4):742-9. [Link] [DOI:10.2337/diacare.25.4.742]
24. Asmamaw A, Asres G, Negese D, Fekadu A, Assefa G. Knowledge and attitude about diabetes mellitus and its associated factors among people in Debre Tabor town, Northwest Ethiopia: Cross sectional study. Sci J Public Health. 2015;3(2):199-209. [Link] [DOI:10.11648/j.sjph.20150302.17]
25. Islam FMA, Chakrabarti R, Dirani M, Islam MT, Ormsby G, Wahab M, et al. Knowledge, attitudes, and practice of diabetes in rural Bangladesh: the Bangladesh Population based Diabetes and Eye Study (BPDES). PLoS One 2014;9(10):e110368 [Link] [DOI:10.1371/journal.pone.0110368]
26. Kiberenge MW, Ndegwa ZM, Njenga EW, Muchemi EW. Knowledge, attitude, and practices related to diabetes among community members in four provinces in Kenya: a cross-sectional study. Pan Afr Med J. 2010;7:2. [Link] [DOI:10.4314/pamj.v7i1.69095]
27. Gazzaz ZJ. Knowledge, attitudes, and practices regarding diabetes mellitus among university students in Jeddah, Saudi Arabia. Diabetes Metab Syndr Obes. 2020;13:5071-8. [Link] [DOI:10.2147/DMSO.S287459]
28. Ahmed IB, Binnwejim MS, Alnahas TM, et al. Level of diabetic patients' knowledge of diabetes mellitus, its complications and management. Arch Pharm Pract. 2019;39:981-9. [Link]
29. Cheekati V, Osburne RC, Jameson KA, Cook CB. Perceptions of resident physicians about management of inpatient hyperglycemia in an urban hospital. J Hosp Med. 2009;4(1):E1-83. [Link] [DOI:10.1002/jhm.383]
30. Tang JW, Freed B, Baker T, Kleczek J, Tartaglia K, Laiteerapong N, et al. Internal medicine residents' comfort with and frequency of providing dietary counseling to diabetic patients. J Gen Intern Med. 2009;24(10):1140-3. [Link] [DOI:10.1007/s11606-009-1084-8]
31. Rubin DJ, Moshang J, Jabbour SA. Diabetes knowledge: are resident physicians and nurses adequately prepared to manage diabetes? Endocr Pract. 2007;13(1):17-21. [Link] [DOI:10.4158/EP.13.1.17]
32. Heisler M, Pietee JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28(4):816-22. [Link] [DOI:10.2337/diacare.28.4.816]
33. Ikizek M. Assessment of diabetes knowledge levels in university students. J Soc Analyt Health. 2022;2(2). [Link]
34. Alanazi F, Alotaibi J, Paliadelis P, Alqarawi N, Alsharari A, Albagawi B. Knowledge and awareness of diabetes mellitus and its risk factors in Saudi Arabia. Saudi Med J. 2018;39:981-9. [Link] [DOI:10.15537/smj.2018.10.22938]
35. Alamri O. Knowledge of diabetes characteristics by students at university of Tabuk, Saudi Arabia. Health. 2021;13(4):393-404. [Link] [DOI:10.4236/health.2021.134032]
36. Kwiendacz H, Nabrdalik K, Brzoza Z, Stokłosa I, Stokłosa M, Bugajski M, et al. Knowledge about diabetes mellitus among Polish medical students. Clin Diabetol. 2020;9(4):245-52. [Link] [DOI:10.5603/DK.2020.0023]
37. Balla SA, Abu Ahmed H, Awadelkareem MA. Prevalence of diabetes, knowledge and attitude of rural population towards diabetes and hypoglycaemic event, Sudan 2013. Am J Health Res. 2021;2(6):356-60. [Link] [DOI:10.11648/j.ajhr.20140206.16]
38. Xu Y, Zhang D, Liu K, Guo Y, Yang Y. Self-reported knowledge on diabetes and its related factors among Chinese college students: a cross-sectional study. BMJ Open. 2016;6:e011963. [Link] [DOI:10.1136/bmjopen-2016-011963]
39. Choi J, Choi JY, Lee SA, Lee KM, Shin A, Oh J, et al. Association between family history of diabetes and clusters of adherence to healthy behaviors: cross-sectional results from the health examinees-gem (hexa-g) study. Public Health Res. 2019;9(6):e025477. [Link] [DOI:10.1136/bmjopen-2018-025477]
40. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403. [Link] [DOI:10.1056/NEJMoa012512]
41. Lv J, Yu C, Guo Y, Bian , Yang L, Chan Y, et al. Adherence to a healthy lifestyle and the risk of type 2 diabetes in Chinese adults. Int J Epidemiol. 2017;46(5):1410-20. [Link] [DOI:10.1093/ije/dyx074]
42. Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85-9. [Link] [DOI:10.1016/j.copsyc.2015.03.012]
43. Darlow S, Goodman MS, Stafford JD, Lachance CR, Kaphingst KA. Weight perceptions and perceived risk for diabetes and heart disease among overweight and obese women, Suffolk County, New York, 2008. Prev Chronic Dis. 2012;9:E81. [Link] [DOI:10.5888/pcd9.110185]
44. Aldekhayel G. An assessment of the diabetic knowledge, attitude, and practice of school teachers in Riyadh, Kingdom of Saudi Arabia. J Diabetes Mellitus. 2020;10(3);132-53. [Link] [DOI:10.4236/jdm.2020.103012]
45. Gulabani M, John M, Isaac R. Knowledge of diabetes, its treatment and complications amongst diabetic patients in a Tertiary Care Hospital. Indian J Community Med. 2008;33(3):204-6. [Link] [DOI:10.4103/0970-0218.42068]
46. Sahile LZ, Shifraew MR, Sahile MZ. Diabetic self-care knowledge and associated factors among adult diabetes mellitus patients on follow-up care at North Shewa Zone Government Hospitals, Oromia Region, Ethiopia, 2020. Diabetes Metab Syndr Obes. 2021;14:2111-9. [Link] [DOI:10.2147/DMSO.S298336]
47. Sękowski K, Grudziąż-Sękowska J, Pinkas J, Jankowski M. Public knowledge and awareness of diabetes mellitus, its risk factors, complications, and prevention methods among adults in Poland-A 2022 nationwide cross-sectional survey. Front. Public Health. 2022;10:1029358. [Link] [DOI:10.3389/fpubh.2022.1029358]
48. Al-Mahrooqi B, Al-Hadhrami R, Al-Amri A, Al-Tamimi S, Al-Shidhani A, Al-Lawati H, et al. Self-reported knowledge of diabetes among high school students in Al-Amerat and Quriyat, Muscat Governate, Oman. Sultan Qaboos Med J. 2013;13(3):392-8. [Link] [DOI:10.12816/0003261]
49. Borges TT, Rombaldi AJ, Knuth AG, Hallal PC. Knowledge on risk factors for chronic diseases: a population-based study. Cad Saude Publica. 2009 Jul;25(7):1511-20. [Portuguese] [Link] [DOI:10.1590/S0102-311X2009000700009]
50. dos Santos PF, dos Santos PR, Ferrari GSL, Fonseca GAA, Ferrari CKB. Knowledge of diabetes mellitus: Does gender make a difference? Osong Public Health Res Perspect. 2014;5(4):199-203. [Link] [DOI:10.1016/j.phrp.2014.06.004]
51. Demaio AR, Otgontuya D, de Courten M, Bygbjerg IC, Enkhtuya P, Oyunbileg J, et al. Exploring knowledge, attitudes and practices related to diabetes in Mongolia: a national population-based survey. BMC Public Health. 2013;13:236. [Link] [DOI:10.1186/1471-2458-13-236]
52. Mohsen F, Safieh H, Shibani M, Ismail H, Alzabibi MA, Armashi H, et al. Assessing diabetes mellitus knowledge among Syrian medical students: A cross-sectional study. Heliyon. 2021;7(9):e08079. [Link] [DOI:10.1016/j.heliyon.2021.e08079]
53. Sabri AA, Qayyum MA, Saigol NU, Zafar K, Aslam F. Comparing knowledge of diabetes mellitus among rural and urban diabetics. Mcgill J Med. 2007;10(2):87-9. [Link] [DOI:10.26443/mjm.v10i2.741]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |