Volume 10, Issue 1 (2022)
Health Educ Health Promot 2022, 10(1): 115-122 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ravari A, Hoseinzadeh F, Mirzaei T, Sayadi A, Hassanshahi E. Effectiveness of Cognitive-Behavioral Therapy and Tai Chi Exercise on the Fear of Falling: a Clinical Trial Study. Health Educ Health Promot 2022; 10 (1) :115-122
URL: http://hehp.modares.ac.ir/article-5-54010-en.html
URL: http://hehp.modares.ac.ir/article-5-54010-en.html
1- Department of Medical-Surgical Nursing, School of Nursing and Midwifery, Geriatric Care Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
2- “Department of Medical Surgical Nursing, School of Nursing and Midwifery”, and “Student Research Committee”, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
3- “Department of Psychiatric Nursing and Mental Health, School of Nursing and Midwifery”, and “Social Determinants of Health Research Center”, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
4- Geriatric Care Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
2- “Department of Medical Surgical Nursing, School of Nursing and Midwifery”, and “Student Research Committee”, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
3- “Department of Psychiatric Nursing and Mental Health, School of Nursing and Midwifery”, and “Social Determinants of Health Research Center”, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
4- Geriatric Care Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran
Keywords: Fear [MeSH], Falling [MeSH], Cognitive-Behavioral Therapy [MeSH], Tai Chi [MeSH], Aged [MeSH]
Full-Text [PDF 550 kb]
(874 Downloads)
| Abstract (HTML) (1042 Views)
Full-Text: (483 Views)
Introduction
The phenomenon of aging is a serious and challenging issue for families and society [1]. Various factors have been considered as a threat to the health of the elderly [2]. Among these factors, which are more likely to occur with age, is the fall of the elderly. In addition to countless physical and psychological injuries and complications in the elderly, the problem of falls imposes a lot of financial costs on responsible institutions and organizations [3]. Fear of falling is one of the most important psychological effects of falling in old age [4]. The prevalence of fear of falling was 26.9% and 43.3% among men and women, respectively [5]. It is also reported that 33.2% of elderly Indians are afraid of falling [6]. However, accurate statistics on the fear of falling in Iran have not been reported. Low levels of fear of falling cause caution in the elderly, and this level of fear is desirable as long as it does not lead to functional limitations [7]. In contrast, high fear of falling in the elderly can lead to loss of independence and reduce their physical function [8]. Therefore, any intervention that can reduce the fear of falling in the elderly can help improve their quality of life by reducing these complications [9]. Cognitive-behavioral therapy (CBT) is one of several interventions that can be considered to reduce the fear of falling. CBT changes the way people think and relate to their world. This type of treatment involves exposure to stimuli and stressful situations. Thus, people can overcome their anxiety in any situation by creating new thoughts [10]. Although CBT is the first step in treating chronic diseases, a study has shown that CBT can play a role in treating chronic diseases and their complications [11]. Parry et al. showed that CBT training could effectively reduce the fear of falling in the elderly [12].
Exercise is another intervention that is widely used [13]. Kumar reviewed 36 exercise interventions and concluded that exercise interventions slightly reduced the fear of falling immediately post-intervention [14]. Gusi et al. showed that balance exercises reduce the fear of falling in the elderly [15]. Elderly participation in a structured exercise program improves balance and motor function, reduces the fear of falling, and increases self-confidence and social activity [16]. Among the structured exercises, we can mention the Tai Chi exercise [17]. The therapeutic effects of Tai Chi are considered complementary medicine, and it is referred to as a mobile drug [18]. Unlike other martial arts that have hard and violent movements, the techniques in the martial art of Tai Chi are soft and floating. Some of these exercises can even be done in hospitals and sanatoriums [19]. Positive effects of Tai Chi have been reported in treating chronic diseases such as hypertension, stress, insomnia, increased respiratory volume, body flexibility, The exchange of oxygen and carbon dioxide, and strengthening bones, muscles, and joints [19- 22]. Hung et al. showed that Tai Chi affects balance, sleep quality, and mental and cognitive aspects of the elderly [23]. Li et al. reported the positive effect of Tai Chi exercise on balance and the risk of falls in patients with Parkinson's disease [24]. Hosseini et al. also showed that Tai Chi exercise effectively improves balance and fear of falling in the Iranian elderly [25]. Given the high prevalence of aging and the problem of fear of falling, as well as the duties of nurses (including minimizing the fear of falling, raising self-esteem and social participation of the elderly hospitalized in hospitals, etc.) [12], practical interventions should be emphasized in this age group.
Considering the positive effect and non-comparison of CBT and tai chi exercises on improving the fear of falling in the elderly in previous studies, it is hypothesized that the two CBT and Tai Chi methods do not have the same effect on reducing the fear of falling in the elderly. A comparison of common interventions in reducing the fear of falling can introduce a more appropriate intervention. For this reason, the research team decided to compare two safe and uncomplicated methods of CBT training and Tai Chi exercise.
Materials and Method
The present study is a randomized clinical trial that was conducted on elderly retirees who were referred to the Retirees Association at Kerman University of Medical Sciences in Kerman, Iran from December 2018 to October 2019. There were more than 5,000 cases related to retirees; of whom 200 were selected by the simple random sampling and were contacted, 35 lacked the inclusion criteria, 30 were unwilling to participate in the study, and 15 did not participate in the study. The remaining 120 retirees announced their readiness and were selected. Then, they were randomly divided into Tai Chi, CBT, and control groups (40 retirees per group). To estimate the sample size, we used type one (α) and type two errors (β) of 0.05 and 0.10. Assuming 15% dropouts in each group, the final sample size was determined to be 40 elderlies per group:
n= 2(z 1-a/2 + z 1-b )2 s2 / d2
Inclusion criteria were including age over 60 years, not living in a nursing home or other institution, ability to read and write, a score on the Abbreviated Mental Test (AMT) be 8 or higher, a score on the Survey of Activities and Fear of Falling in the Elderly (SAFFE) be 10 or higher, no diseases such as stroke, dementia, multiple sclerosis, and orthopedic problems. Participants were excluded from the study if they didn't attend more than three sessions of exercises or training, unwillingness to continue the program, occurrence of orthopedic problems. The study flowchart is also presented in Diagram 1.
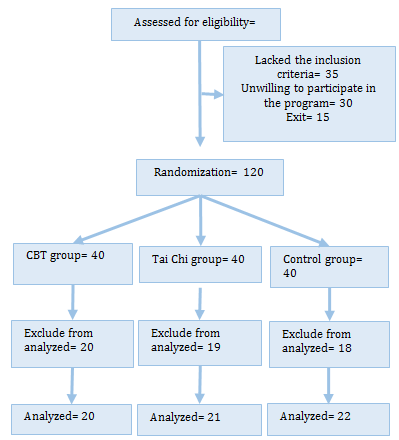
Diagram 1) Flowchart of the study participants
A trained researcher conducted all personal interviews after explaining the purpose of the study and obtaining informed consent from the elderly. Before entering the study, all retirees were asked to complete the Demographic Questionnaire, AMT, and the SAFFE. The demographic form included age, sex, marriage, and level of education. Hodkinson introduced the AMT in 1972 to assess elderly patients for the possibility of dementia rapidly. It constitutes a very quick screening test because the administration is estimated at 3 min for each patient. It consists of 10 questions, with a 10-point scale that evaluates short-term and long-term memory, orientation, as well as attention abilities. Each question scores 1 point, and the total score ranges from 0 (incorrect answer) to 10 (10 correct answers) [26]. Previous validations have shown it to have good levels of sensitivity [27, 28]. Validation of a Spanish version in a rural community showed a sensitivity of 100% and a specificity of 53% for a cut-off point of 7/8 [28]. The same cut-off point in a clinical sample in a London population gave 91 and 85% sensitivity and specificity, respectively [27]. Also, Jitapunkul showed that AMT reliability is satisfactory in terms of internal consistency (Cronbach B=0.80), and a score <8 indicates a significant cognitive deficit [27]. We used the Persian version of AMT. It is shown that the Persian version has a validity of 92.15% and reliability of 81.5% [29]. The SAFFE, a reliable (0.95) and valid (0.91) instrument was developed by Margine et al. and assesses fear of falling during eleven activities of daily living, mostly focusing on the negative aspects of the fear of falling, such as avoiding activities. 3 SAFFE subscales (fear, activity participation, and activity restriction) are determined from the responses. The SAFFE fear subscale score is determined based on the average fear ratings (0-3) across each of the 11 activities performed. A score of 0 indicates no fear, 1 indicates a little fearful, two indicates somewhat fearful, and three indicates very frighteningly while performing each respective activity. For each activity, the range of scores is 0 to 3, and the total score is 33 [30]. We used the Persian version of the SAFFE. Zarei et al. Reported that the Persian version of SAFFE has excellent content validity (based on the scores of Content Validity Ratio (CVI) and Content Validity Index (CVR)) and internal consistency of items (Cronbach's alpha coefficient= 0.93) [31].
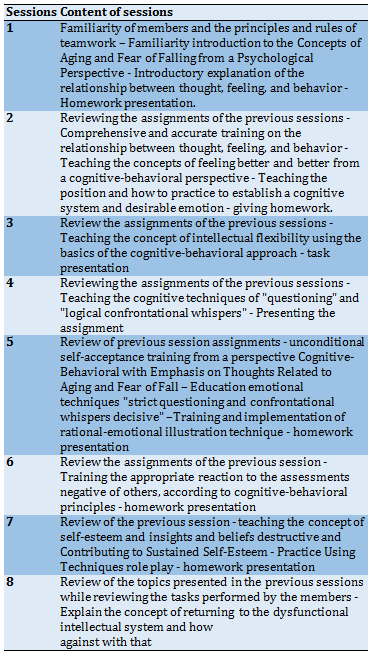
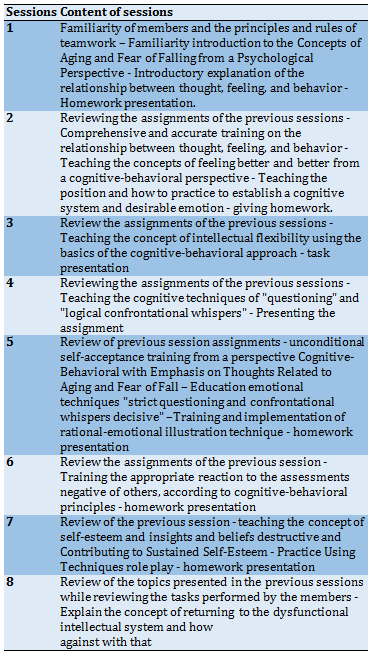
This research was approved by the Rafsanjan University of Medical Sciences Ethics Committee. The objectives of the study were outlined at the beginning of the study. Written informed consent was obtained from participants, the confidentiality of information was ensured, and participants were given authority to withdraw from the study if they were exposed to problems that might have hindered their participation. Participants in the CBT group received sixteen 60-70 minute group counseling sessions which were held and managed by a Master's holder in Psychology. The CBT programs were developed based on the related books. CBT group members attended CBT sessions twice a week for eight weeks. In order to intervene more effectively, sessions with individual assignments were conducted. The last 10 minutes of each session were devoted to reviewing the reports related to these assignments and answering questions. CBT sessions were held at the health center on Saturday and Tuesday (at 10-11:30 AM) for the CBT group (Table 1).
The Tai Chi group was then supervised by a trainer experienced with elderly people with a valid degree. Tai Chi was performed in two sessions of 45-60 minutes per week for eight weeks in one of the gyms in Kerman on Sunday and Wednesday (at 10-11:30 AM) for the Tai Chi group. At the beginning of each session, 7–10 min were used to warm up, and the last 7–10 min were spent cooling down. Ten movements extracted from the 24 simple forms of Tai Chi Chuan (Yang style) were selected as the main motions for the intervention protocol. In the first week, the exercise program emphasized the initial learning of movements. In subsequent sessions, the focus was on increasing motor performance and improving balance with increased attention to the individual's performance gestures. Light music was played during the exercise. The subjects were allowed to sit on a chair for short rest periods and, if needed, could use a walker or cane. The researcher guided participants in the control group to receive routine interventions in old age (such as controlling blood pressure and blood sugar). At the end of the study, educational booklets related to the topics discussed in the intervention groups were provided to the retirees in the control group. Questionnaires were completed three times, before, one month after the intervention (first month), and one month after the end of the intervention (second month). At the end of the training sessions, a fear of falling questionnaire was distributed again among the intervention and control groups to measure the effect of CBT training and Tai Chi exercise on their fear of falling before and after training.
The collected data were entered into SPSS 18 software. Quantitative data were presented as mean±SD, while qualitative data were presented as frequency and percentage (%). ANOVA test was used to compare the three groups, and repeated measurement ANOVA was used to compare the mean fear of falling in the first and second months compared to before the start of the study in each group.
Table 1) A summary of the content of cognitive-behavioral therapy sessions
Findings
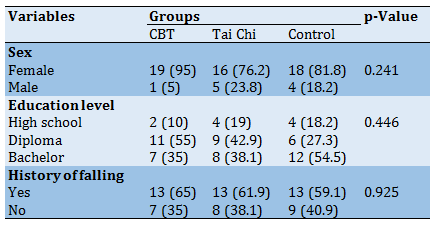
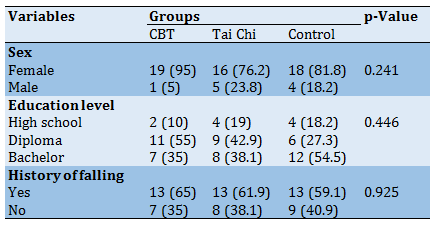
The mean age of the three groups was more than 66 years (CBT=66.55±5.02; Ti Chi=67.47±4.68; Control=69.31±6.56), and there was no significant difference (p=0.258). Most of the participants were women. Most of the people in the CBT and Tai Chi groups had a diploma education level, while most people in the control group had a university education level. About 60% of participants in the three groups had a history of falls. ANOVA and Chi-square test did not show a significant difference between the three groups regarding sex, history of falling, and education (Table 2).
Table 2) Demographic characteristics and History of falling in intervention and control groups
Before and in the first month after the intervention, there was no significant difference between the three groups regarding fear of falling components and total score, and ANOVA did not show a significant difference between the three groups (p>0.05). Before and in the first month after the intervention, the most significant difference in the total score was between the control group and Tai Chi. In the second month after the intervention, there was a significant difference between the three groups regarding the total score and component of the activity. The most significant difference in the total score was between the Tai Chi group and the control group. Despite the higher total score in the Tai Chi group, there was no significant difference between the Tai Chi group and the CBT group in terms of the total score (Table 3).
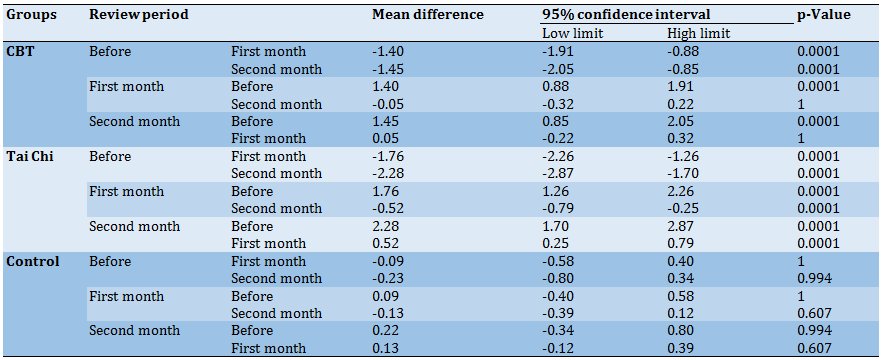
In terms of the total score in the Tai Chi and CBT groups, the t-test showed a significant difference between the second and first months compared to before the intervention, which was not significant in the control group (Table 4).
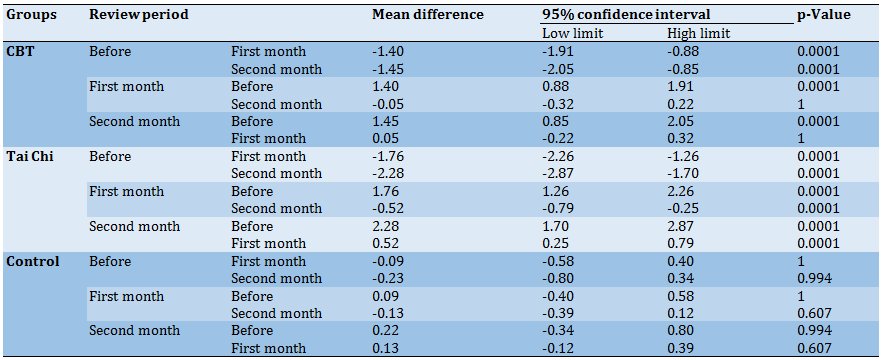
The most significant difference in terms of the total score in the intervention groups was between the second month compared before the intervention. There was no significant difference between the first and second months in the intervention groups. There was no significant difference in the control group between the second and first months compared to the beginning of the study (Table 5).
Table 3) The mean±SD of the total score of fear of falling and its subscales scores before and in the first and second months after interventions between groups
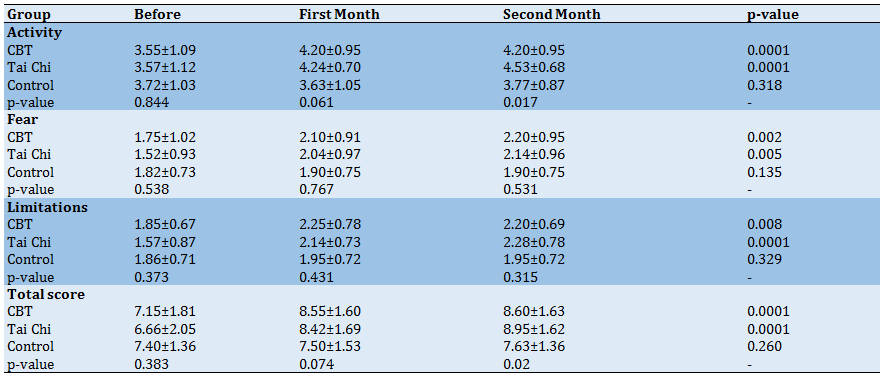
Table 4) Comparison of the mean differences between the groups studied before, the first month, and the second month after the intervention compared to each other
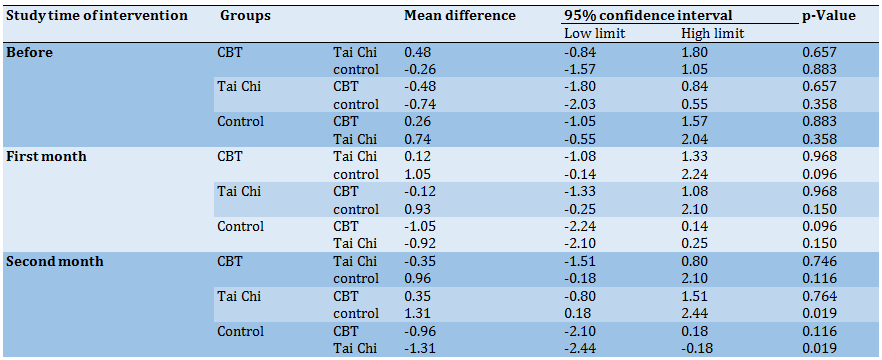
Table 5) Comparison of the mean differences of each study group in the first and second months compared to before the study
Discussion
Falls are one of the most common issues among the elderly. Many studies have shown the effective role of CBT and Tai Chi exercise in reducing the fear of falling in the elderly [12, 25]. The present study was conducted to compare the effects of CBT and Tai Chi on the fear of falling of retirement affiliated with Kerman University of Medical Sciences. The findings of this study showed that end of the second month of the CBT training and Tai Chi exercise, the mean score of fear of falling increased in the intervention groups compared to the control group, indicating the positive effect of CBT and Tai Chi on the reduction of the fear of falling in elderly. This finding agrees with several previous studies that showed that CBT and Tai Chi improve the fear of falling in the elderly [12, 25].
In this study, 59 to 65% of participants in three groups had a history of falls. In many studies [32-34], a history of falls in the elderly has been reported at 66 to 70%. Also, in the study of Ghezeljeh et al., it was reported that all elderly participants in this study had a history of falls in the six months before the intervention [35].
In the present study, the fear of falling in the elderly decreased but was not statistically significant in the first month. However, as Tai Chi exercise and CBT sessions continued, the mean scores of fear of falling in the intervention groups increased. The fear of falling in the intervention groups decreased compared to the control group. At the end of the second month, the activity component was significant among all components of fear of falling. Previous studies have compared CBT with Tai Chi. For example, a study by Huang et al. compared CBT with Tai Chi in the elderly over 60 years of age. The results of this study showed that the mean score of fear of falling in the two intervention groups compared to the control group had decreased after the intervention and five months after the intervention. Still, there was no statistically significant difference between the two intervention groups [23]. Also, in the present study, there was no significant difference between the two intervention groups at the end of the second month. There was no difference between the CBT and control groups, while there was a difference between the Tai Chi and the control groups. This may be due to differences in the method of intervention in the studies. Because in the study of Huang et al. [23], CBT sessions were performed in combination with Tai Chi, whereas in the present study, CBT sessions were performed alone. Also, in the study of Liu et al., Tai Chi with and without CBT was performed to assess the reduction of fear of falling in the elderly. The results of this study showed that Tai Chi, both with and without CBI, has a similar effect on reducing elderly people's fear of falling [36]. In Huang et al. and Liu's studies, no significant difference was reported between Tai Chi and CBT methods, which is consistent with the present study. Although the method of performing the two interventions and the instrument for measuring the fear of falling in the present study were different from the mentioned studies, a similar finding was obtained, indicating no difference between the two methods. It could be due to the characteristics of the study population.
In Huang et al. and Liu's studies, components of fear of falling have not been reported. However, in this study, the retirees were trained in the CBT group for two months. The findings showed that scores increased between before and the first month, and the fear of falling decreased. But in the second month compared to the first month, no increasing trend was observed, so there was no significant difference between the second month and the first month. The study by Dorresteijn et al. examined the effectiveness of a home-based CBT program for managing the fear of falling in the elderly. The results of this study showed that at 12 and 5 months, the intervention group had a lower fear of falling than the control group [37]. It could be due to the age of the study population.
In the Tai Chi group, there was a significant difference between the first and second months. Also, the score of fear of falling in the second month has increased compared to the first month, indicating the decreasing trend of fear of falling in this group. In the study of Mortazavi et al., the effect of Tai Chi exercise on the risk and fear of falling in older adults was investigated. The results of this study showed that after the fourth week, the risk of falling in the intervention and control groups did not decrease, while after the eighth and tenth weeks in the intervention group decreased [38]. Therefore, based on the findings of this study and the present study, it can be acknowledged that Tai Chi exercise has little effect on the fear of falling in the short term and should be done for a longer time for its effects to appear.
Among the limitations of this study, we can mention the individual differences between the participants in the Tai Chi group in terms of doing sports exercises and in the behavioral cognitive group, the differences in understanding the provided trainings, which were tried to minimize with more supervision. It is suggested that the effect of the combined intervention of cognitive-behavioral therapy and tai chi exercise on reducing the fear of falling in the elderly be investigated.
Conclusion
The findings of this study showed that the two interventions had a positive effect on the mean score of fear of falling and reducing this fear, but were not observed between the two groups in the first and second months. There was no significant difference in the CBT group in the second month compared to the first month. Still, in the Tai Chi group, the trend of increasing the mean score in the second month compared to the first month was continuous, which shows that this method is more effective in the second month.
Acknowledgments: We would like to thank the responsible authorities of the Geriatric Care Research Center and the Vice Chancellery for Research and Technology of Rafsanjan University of Medical Sciences. The participation and collaboration of the study participants are acknowledged.
Ethical Permissions: Approval for this research was acquired through the Rafsanjan University of Medical Sciences Ethics Committee (IR.RUMS.REC.1397.128).
Conflicts of Interests: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript
Authors’ Contributions: Ravari A. (First Author), Main Researcher/Methodologist/Discussion Writer (30%); Hoseinzadeh F. (Second Author), Main Researcher/Introduction Writer (20%); Mirzaei T. (Third Author), Main Researcher/Introduction Writer/Discussion Writer (30%); Sayadi A.R. (Forth author), Assistant Researcher/Statistical Analyst (10%); Hasanshahi E. (Fifth author), Assistant Researcher/Finding Writer (10%).
Funding/Sources: This research was funded by a grant from the Vice Chancellery for Research & Technology of Rafsanjan University of Medical Sciences.
The phenomenon of aging is a serious and challenging issue for families and society [1]. Various factors have been considered as a threat to the health of the elderly [2]. Among these factors, which are more likely to occur with age, is the fall of the elderly. In addition to countless physical and psychological injuries and complications in the elderly, the problem of falls imposes a lot of financial costs on responsible institutions and organizations [3]. Fear of falling is one of the most important psychological effects of falling in old age [4]. The prevalence of fear of falling was 26.9% and 43.3% among men and women, respectively [5]. It is also reported that 33.2% of elderly Indians are afraid of falling [6]. However, accurate statistics on the fear of falling in Iran have not been reported. Low levels of fear of falling cause caution in the elderly, and this level of fear is desirable as long as it does not lead to functional limitations [7]. In contrast, high fear of falling in the elderly can lead to loss of independence and reduce their physical function [8]. Therefore, any intervention that can reduce the fear of falling in the elderly can help improve their quality of life by reducing these complications [9]. Cognitive-behavioral therapy (CBT) is one of several interventions that can be considered to reduce the fear of falling. CBT changes the way people think and relate to their world. This type of treatment involves exposure to stimuli and stressful situations. Thus, people can overcome their anxiety in any situation by creating new thoughts [10]. Although CBT is the first step in treating chronic diseases, a study has shown that CBT can play a role in treating chronic diseases and their complications [11]. Parry et al. showed that CBT training could effectively reduce the fear of falling in the elderly [12].
Exercise is another intervention that is widely used [13]. Kumar reviewed 36 exercise interventions and concluded that exercise interventions slightly reduced the fear of falling immediately post-intervention [14]. Gusi et al. showed that balance exercises reduce the fear of falling in the elderly [15]. Elderly participation in a structured exercise program improves balance and motor function, reduces the fear of falling, and increases self-confidence and social activity [16]. Among the structured exercises, we can mention the Tai Chi exercise [17]. The therapeutic effects of Tai Chi are considered complementary medicine, and it is referred to as a mobile drug [18]. Unlike other martial arts that have hard and violent movements, the techniques in the martial art of Tai Chi are soft and floating. Some of these exercises can even be done in hospitals and sanatoriums [19]. Positive effects of Tai Chi have been reported in treating chronic diseases such as hypertension, stress, insomnia, increased respiratory volume, body flexibility, The exchange of oxygen and carbon dioxide, and strengthening bones, muscles, and joints [19- 22]. Hung et al. showed that Tai Chi affects balance, sleep quality, and mental and cognitive aspects of the elderly [23]. Li et al. reported the positive effect of Tai Chi exercise on balance and the risk of falls in patients with Parkinson's disease [24]. Hosseini et al. also showed that Tai Chi exercise effectively improves balance and fear of falling in the Iranian elderly [25]. Given the high prevalence of aging and the problem of fear of falling, as well as the duties of nurses (including minimizing the fear of falling, raising self-esteem and social participation of the elderly hospitalized in hospitals, etc.) [12], practical interventions should be emphasized in this age group.
Considering the positive effect and non-comparison of CBT and tai chi exercises on improving the fear of falling in the elderly in previous studies, it is hypothesized that the two CBT and Tai Chi methods do not have the same effect on reducing the fear of falling in the elderly. A comparison of common interventions in reducing the fear of falling can introduce a more appropriate intervention. For this reason, the research team decided to compare two safe and uncomplicated methods of CBT training and Tai Chi exercise.
Materials and Method
The present study is a randomized clinical trial that was conducted on elderly retirees who were referred to the Retirees Association at Kerman University of Medical Sciences in Kerman, Iran from December 2018 to October 2019. There were more than 5,000 cases related to retirees; of whom 200 were selected by the simple random sampling and were contacted, 35 lacked the inclusion criteria, 30 were unwilling to participate in the study, and 15 did not participate in the study. The remaining 120 retirees announced their readiness and were selected. Then, they were randomly divided into Tai Chi, CBT, and control groups (40 retirees per group). To estimate the sample size, we used type one (α) and type two errors (β) of 0.05 and 0.10. Assuming 15% dropouts in each group, the final sample size was determined to be 40 elderlies per group:
n= 2(z 1-a/2 + z 1-b )2 s2 / d2
Inclusion criteria were including age over 60 years, not living in a nursing home or other institution, ability to read and write, a score on the Abbreviated Mental Test (AMT) be 8 or higher, a score on the Survey of Activities and Fear of Falling in the Elderly (SAFFE) be 10 or higher, no diseases such as stroke, dementia, multiple sclerosis, and orthopedic problems. Participants were excluded from the study if they didn't attend more than three sessions of exercises or training, unwillingness to continue the program, occurrence of orthopedic problems. The study flowchart is also presented in Diagram 1.
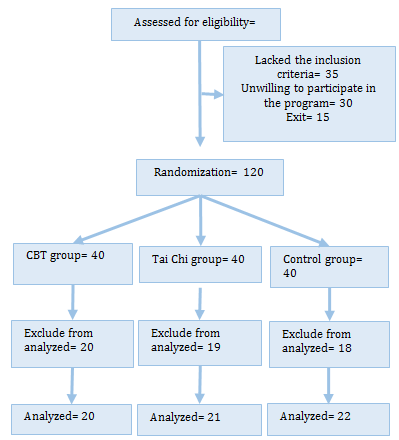
Diagram 1) Flowchart of the study participants
A trained researcher conducted all personal interviews after explaining the purpose of the study and obtaining informed consent from the elderly. Before entering the study, all retirees were asked to complete the Demographic Questionnaire, AMT, and the SAFFE. The demographic form included age, sex, marriage, and level of education. Hodkinson introduced the AMT in 1972 to assess elderly patients for the possibility of dementia rapidly. It constitutes a very quick screening test because the administration is estimated at 3 min for each patient. It consists of 10 questions, with a 10-point scale that evaluates short-term and long-term memory, orientation, as well as attention abilities. Each question scores 1 point, and the total score ranges from 0 (incorrect answer) to 10 (10 correct answers) [26]. Previous validations have shown it to have good levels of sensitivity [27, 28]. Validation of a Spanish version in a rural community showed a sensitivity of 100% and a specificity of 53% for a cut-off point of 7/8 [28]. The same cut-off point in a clinical sample in a London population gave 91 and 85% sensitivity and specificity, respectively [27]. Also, Jitapunkul showed that AMT reliability is satisfactory in terms of internal consistency (Cronbach B=0.80), and a score <8 indicates a significant cognitive deficit [27]. We used the Persian version of AMT. It is shown that the Persian version has a validity of 92.15% and reliability of 81.5% [29]. The SAFFE, a reliable (0.95) and valid (0.91) instrument was developed by Margine et al. and assesses fear of falling during eleven activities of daily living, mostly focusing on the negative aspects of the fear of falling, such as avoiding activities. 3 SAFFE subscales (fear, activity participation, and activity restriction) are determined from the responses. The SAFFE fear subscale score is determined based on the average fear ratings (0-3) across each of the 11 activities performed. A score of 0 indicates no fear, 1 indicates a little fearful, two indicates somewhat fearful, and three indicates very frighteningly while performing each respective activity. For each activity, the range of scores is 0 to 3, and the total score is 33 [30]. We used the Persian version of the SAFFE. Zarei et al. Reported that the Persian version of SAFFE has excellent content validity (based on the scores of Content Validity Ratio (CVI) and Content Validity Index (CVR)) and internal consistency of items (Cronbach's alpha coefficient= 0.93) [31].
This research was approved by the Rafsanjan University of Medical Sciences Ethics Committee. The objectives of the study were outlined at the beginning of the study. Written informed consent was obtained from participants, the confidentiality of information was ensured, and participants were given authority to withdraw from the study if they were exposed to problems that might have hindered their participation. Participants in the CBT group received sixteen 60-70 minute group counseling sessions which were held and managed by a Master's holder in Psychology. The CBT programs were developed based on the related books. CBT group members attended CBT sessions twice a week for eight weeks. In order to intervene more effectively, sessions with individual assignments were conducted. The last 10 minutes of each session were devoted to reviewing the reports related to these assignments and answering questions. CBT sessions were held at the health center on Saturday and Tuesday (at 10-11:30 AM) for the CBT group (Table 1).
The Tai Chi group was then supervised by a trainer experienced with elderly people with a valid degree. Tai Chi was performed in two sessions of 45-60 minutes per week for eight weeks in one of the gyms in Kerman on Sunday and Wednesday (at 10-11:30 AM) for the Tai Chi group. At the beginning of each session, 7–10 min were used to warm up, and the last 7–10 min were spent cooling down. Ten movements extracted from the 24 simple forms of Tai Chi Chuan (Yang style) were selected as the main motions for the intervention protocol. In the first week, the exercise program emphasized the initial learning of movements. In subsequent sessions, the focus was on increasing motor performance and improving balance with increased attention to the individual's performance gestures. Light music was played during the exercise. The subjects were allowed to sit on a chair for short rest periods and, if needed, could use a walker or cane. The researcher guided participants in the control group to receive routine interventions in old age (such as controlling blood pressure and blood sugar). At the end of the study, educational booklets related to the topics discussed in the intervention groups were provided to the retirees in the control group. Questionnaires were completed three times, before, one month after the intervention (first month), and one month after the end of the intervention (second month). At the end of the training sessions, a fear of falling questionnaire was distributed again among the intervention and control groups to measure the effect of CBT training and Tai Chi exercise on their fear of falling before and after training.
The collected data were entered into SPSS 18 software. Quantitative data were presented as mean±SD, while qualitative data were presented as frequency and percentage (%). ANOVA test was used to compare the three groups, and repeated measurement ANOVA was used to compare the mean fear of falling in the first and second months compared to before the start of the study in each group.
Table 1) A summary of the content of cognitive-behavioral therapy sessions
Findings
The mean age of the three groups was more than 66 years (CBT=66.55±5.02; Ti Chi=67.47±4.68; Control=69.31±6.56), and there was no significant difference (p=0.258). Most of the participants were women. Most of the people in the CBT and Tai Chi groups had a diploma education level, while most people in the control group had a university education level. About 60% of participants in the three groups had a history of falls. ANOVA and Chi-square test did not show a significant difference between the three groups regarding sex, history of falling, and education (Table 2).
Table 2) Demographic characteristics and History of falling in intervention and control groups
Before and in the first month after the intervention, there was no significant difference between the three groups regarding fear of falling components and total score, and ANOVA did not show a significant difference between the three groups (p>0.05). Before and in the first month after the intervention, the most significant difference in the total score was between the control group and Tai Chi. In the second month after the intervention, there was a significant difference between the three groups regarding the total score and component of the activity. The most significant difference in the total score was between the Tai Chi group and the control group. Despite the higher total score in the Tai Chi group, there was no significant difference between the Tai Chi group and the CBT group in terms of the total score (Table 3).
In terms of the total score in the Tai Chi and CBT groups, the t-test showed a significant difference between the second and first months compared to before the intervention, which was not significant in the control group (Table 4).
The most significant difference in terms of the total score in the intervention groups was between the second month compared before the intervention. There was no significant difference between the first and second months in the intervention groups. There was no significant difference in the control group between the second and first months compared to the beginning of the study (Table 5).
Table 3) The mean±SD of the total score of fear of falling and its subscales scores before and in the first and second months after interventions between groups
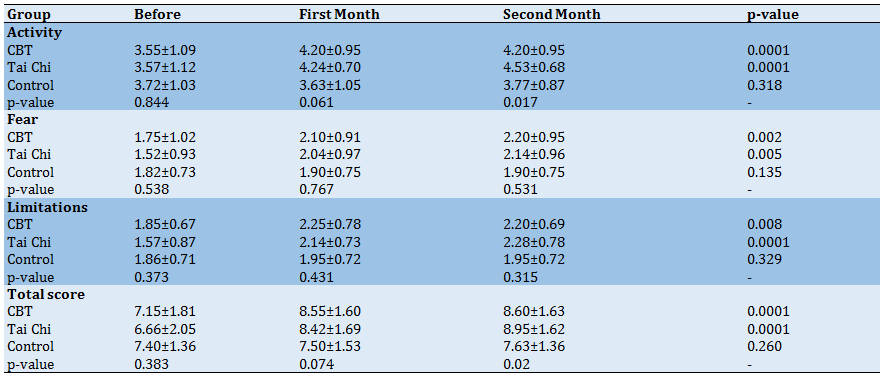
Table 4) Comparison of the mean differences between the groups studied before, the first month, and the second month after the intervention compared to each other
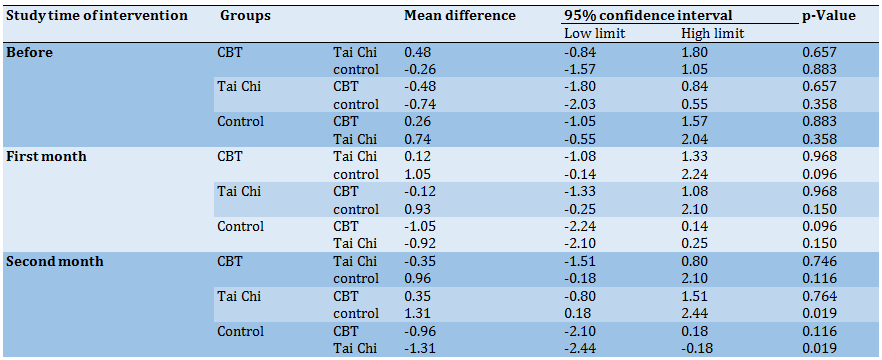
Table 5) Comparison of the mean differences of each study group in the first and second months compared to before the study
Discussion
Falls are one of the most common issues among the elderly. Many studies have shown the effective role of CBT and Tai Chi exercise in reducing the fear of falling in the elderly [12, 25]. The present study was conducted to compare the effects of CBT and Tai Chi on the fear of falling of retirement affiliated with Kerman University of Medical Sciences. The findings of this study showed that end of the second month of the CBT training and Tai Chi exercise, the mean score of fear of falling increased in the intervention groups compared to the control group, indicating the positive effect of CBT and Tai Chi on the reduction of the fear of falling in elderly. This finding agrees with several previous studies that showed that CBT and Tai Chi improve the fear of falling in the elderly [12, 25].
In this study, 59 to 65% of participants in three groups had a history of falls. In many studies [32-34], a history of falls in the elderly has been reported at 66 to 70%. Also, in the study of Ghezeljeh et al., it was reported that all elderly participants in this study had a history of falls in the six months before the intervention [35].
In the present study, the fear of falling in the elderly decreased but was not statistically significant in the first month. However, as Tai Chi exercise and CBT sessions continued, the mean scores of fear of falling in the intervention groups increased. The fear of falling in the intervention groups decreased compared to the control group. At the end of the second month, the activity component was significant among all components of fear of falling. Previous studies have compared CBT with Tai Chi. For example, a study by Huang et al. compared CBT with Tai Chi in the elderly over 60 years of age. The results of this study showed that the mean score of fear of falling in the two intervention groups compared to the control group had decreased after the intervention and five months after the intervention. Still, there was no statistically significant difference between the two intervention groups [23]. Also, in the present study, there was no significant difference between the two intervention groups at the end of the second month. There was no difference between the CBT and control groups, while there was a difference between the Tai Chi and the control groups. This may be due to differences in the method of intervention in the studies. Because in the study of Huang et al. [23], CBT sessions were performed in combination with Tai Chi, whereas in the present study, CBT sessions were performed alone. Also, in the study of Liu et al., Tai Chi with and without CBT was performed to assess the reduction of fear of falling in the elderly. The results of this study showed that Tai Chi, both with and without CBI, has a similar effect on reducing elderly people's fear of falling [36]. In Huang et al. and Liu's studies, no significant difference was reported between Tai Chi and CBT methods, which is consistent with the present study. Although the method of performing the two interventions and the instrument for measuring the fear of falling in the present study were different from the mentioned studies, a similar finding was obtained, indicating no difference between the two methods. It could be due to the characteristics of the study population.
In Huang et al. and Liu's studies, components of fear of falling have not been reported. However, in this study, the retirees were trained in the CBT group for two months. The findings showed that scores increased between before and the first month, and the fear of falling decreased. But in the second month compared to the first month, no increasing trend was observed, so there was no significant difference between the second month and the first month. The study by Dorresteijn et al. examined the effectiveness of a home-based CBT program for managing the fear of falling in the elderly. The results of this study showed that at 12 and 5 months, the intervention group had a lower fear of falling than the control group [37]. It could be due to the age of the study population.
In the Tai Chi group, there was a significant difference between the first and second months. Also, the score of fear of falling in the second month has increased compared to the first month, indicating the decreasing trend of fear of falling in this group. In the study of Mortazavi et al., the effect of Tai Chi exercise on the risk and fear of falling in older adults was investigated. The results of this study showed that after the fourth week, the risk of falling in the intervention and control groups did not decrease, while after the eighth and tenth weeks in the intervention group decreased [38]. Therefore, based on the findings of this study and the present study, it can be acknowledged that Tai Chi exercise has little effect on the fear of falling in the short term and should be done for a longer time for its effects to appear.
Among the limitations of this study, we can mention the individual differences between the participants in the Tai Chi group in terms of doing sports exercises and in the behavioral cognitive group, the differences in understanding the provided trainings, which were tried to minimize with more supervision. It is suggested that the effect of the combined intervention of cognitive-behavioral therapy and tai chi exercise on reducing the fear of falling in the elderly be investigated.
Conclusion
The findings of this study showed that the two interventions had a positive effect on the mean score of fear of falling and reducing this fear, but were not observed between the two groups in the first and second months. There was no significant difference in the CBT group in the second month compared to the first month. Still, in the Tai Chi group, the trend of increasing the mean score in the second month compared to the first month was continuous, which shows that this method is more effective in the second month.
Acknowledgments: We would like to thank the responsible authorities of the Geriatric Care Research Center and the Vice Chancellery for Research and Technology of Rafsanjan University of Medical Sciences. The participation and collaboration of the study participants are acknowledged.
Ethical Permissions: Approval for this research was acquired through the Rafsanjan University of Medical Sciences Ethics Committee (IR.RUMS.REC.1397.128).
Conflicts of Interests: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript
Authors’ Contributions: Ravari A. (First Author), Main Researcher/Methodologist/Discussion Writer (30%); Hoseinzadeh F. (Second Author), Main Researcher/Introduction Writer (20%); Mirzaei T. (Third Author), Main Researcher/Introduction Writer/Discussion Writer (30%); Sayadi A.R. (Forth author), Assistant Researcher/Statistical Analyst (10%); Hasanshahi E. (Fifth author), Assistant Researcher/Finding Writer (10%).
Funding/Sources: This research was funded by a grant from the Vice Chancellery for Research & Technology of Rafsanjan University of Medical Sciences.
Article Type: Original Research |
Subject:
Health Promotion Approaches
Received: 2021/07/11 | Accepted: 2021/09/30 | Published: 2022/04/10
Received: 2021/07/11 | Accepted: 2021/09/30 | Published: 2022/04/10
References
1. Ravari A, Mirzaei T, Salamizadeh A, Majdabadi HA. Effect of the spiritual care training on anxiety reduction in home caregivers of the elderly with alzheimer disease. KOOMESH. 2017;19(2):467-74. [Persian] [Link]
2. Mohammadi Shahrokhi V, Ravari A, Mirzaei T, Zare-Bidaki M, Asadikaram G, Kazemi Arababadi M. IL-17A and IL-23: plausible risk factors to induce age-associated inflammation in Alzheimer's disease. Immunol Invest. 2018;47(8):812-22. [Link] [DOI:10.1080/08820139.2018.1504300]
3. Alsaif AA, Ahmed Alsenany S. Balance and prevention of fall among elderly. MOJ Gerontol Ger. 2018;3(1):65-9. [Link] [DOI:10.15406/mojgg.2018.03.00087]
4. Lopes K, Costa D, Santos L, Castro D, Bastone A. Prevalence of fear of falling among a population of older adults and its correlation with mobility, dynamic balance, risk and History of falls. Braz J Physic Ther. 2009;13(3):223-9. [Link]
5. Tomita Y, Arima K, Tsujimoto R, Kawashiri SY, Nishimura T, Mizukami S, et al. Prevalence of fear of falling and associated factors among Japanese community-dwelling older adults. Med. 2018;97(4):e9721. [Link] [DOI:10.1097/MD.0000000000009721]
6. Mane AB, Sanjana T, Patil PR, Sriniwas T. Prevalence and correlates of fear of falling among elderly population in urban area of Karnataka, India. J Midlife Health. 2014;5(3):150-5. [Link] [DOI:10.4103/0976-7800.141224]
7. Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23(1):3-23. [Link] [DOI:10.1177/0898264310378039]
8. Schone D, Freiberger E, Sieber CC. Influence of skeletal muscles on the risk of falling in old age. Internist (Berl). 2017;58(4):359-70. [German] [Link] [DOI:10.1007/s00108-017-0212-5]
9. Rahimi A, Balouchi R, Eslami R, Shahrokhi M. The relationship between back extensor muscle strength with dynamic balance and fear of falling in elderly people. J Practi Stud Biosci Sport. 2016;4(7):114-24. [Persian] [Link]
10. Yousefy A, KhayamNekouei Z. Basis of cognitive-behavioral trainings and its applications in recovery of chronic diseases. Iranian J Med Educ. 2011;10(5):792-800. [Persian] [Link]
11. Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153-66. [Link] [DOI:10.1037/a0035747]
12. Parry SW, Bamford C, Deary V, Finch TL, Gray J, MacDonald C, et al. Cognitive-behavioural therapy-based intervention to reduce fear of falling in older people: therapy development and randomised controlled trial - the Strategies for Increasing Independence, Confidence and Energy (STRIDE) study. Health Technol Assess. 2016;20(56):1-206. [Link] [DOI:10.3310/hta20560]
13. Ravari A, Mirzaei T, Bahremand R, Raeisi M, Kamiab Z. The effect of pilates exercise on the happiness and depression of elderly women: A clinical trial study. J Sports Med Physic Fitness. 2021;61(1):131-9. [Link] [DOI:10.23736/S0022-4707.20.10730-8]
14. Kumar A, Delbaere K, Zijlstra GAR, Carpenter H, Iliffe S, Masud T, et al. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age Ageing. 2016;45(3):345-52. [Link] [DOI:10.1093/ageing/afw036]
15. Gusi N, Adsuar JC, Corzo H, del Pozo-Cruz B, Olivares PR, Parraca JA. Balance training reduces fear of falling and improves dynamic balance and isometric strength in institutionalised older people: a randomised trial. J Physiother. 2012;58(2):97-104. [Link] [DOI:10.1016/S1836-9553(12)70089-9]
16. Solloway MR, Taylor SL, Shekelle PG, Miake-Lye IM, Beroes JM, Shanman RM, et al. An evidence map of the effect of Tai Chi on health outcomes. Syst Rev. 2016;5(1):126. [Link] [DOI:10.1186/s13643-016-0300-y]
17. Sungkarat S, Boripuntakul S, Chattipakorn N, Watcharasaksilp K, Lord SR. Effects of Tai Chi on cognition and fall risk in older adults with mild cognitive impairment: a randomized controlled trial. J Am Geriatr Soc. 2017;65(4):721-7. [Link] [DOI:10.1111/jgs.14594]
18. You T, Ogawa EF, Thapa S, Cai Y, Zhang H, Nagae S, et al. Tai Chi for older adults with chronic multisite pain: a randomized controlled pilot study. Aging Clin Exp Res. 2018;30(11):1335-43. [Link] [DOI:10.1007/s40520-018-0922-0]
19. Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010;24(6):e1-e25. [Link] [DOI:10.4278/ajhp.081013-LIT-248]
20. Zou L, Sasaki JE, Wei GX, Huang T, Yeung AS, Barbosa Neto O, et al. Effects of mind-body exercises (Tai Chi/Yoga) on heart rate variability parameters and perceived stress: A systematic review with meta-analysis of randomized controlled trials. J Clin Med. 2018;7(11):404. [Link] [DOI:10.3390/jcm7110404]
21. Nguyen MH, Kruse A. A randomized controlled trial of Tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging. 2012;7:185-90. [Link] [DOI:10.2147/CIA.S32600]
22. Sun Z, Chen H, Berger MR, Zhang L, Guo H, Huang Y. Effects of tai chi exercise on bone health in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Osteoporos Int. 2016;27(10):2901-11. [Link] [DOI:10.1007/s00198-016-3626-3]
23. Huang TT, Yang LH, Liu CY. Reducing the fear of falling among community-dwelling elderly adults through cognitive-behavioural strategies and intense Tai Chi exercise: A randomized controlled trial. J Adv Nurs. 2011;67(5):961-71. [Link] [DOI:10.1111/j.1365-2648.2010.05553.x]
24. Li F, Harmer P, Fitzgerald K, Eckstrom E, Stock R, Galver J, et al. Tai chi and postural stability in patients with Parkinson's disease. N Engl J Med. 2012;366(6):511-9. [Link] [DOI:10.1056/NEJMoa1107911]
25. Hosseini L, Kargozar E, Sharifi F, Negarandeh R, Memari AH, Navab E. Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: a randomized control trial. J Exerc Rehabil. 2018;14(6):1024-31. [Link] [DOI:10.12965/jer.1836488.244]
26. Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972;1(4):233-8. [Link] [DOI:10.1093/ageing/1.4.233]
27. Jitapunkul S, Pillay I, Ebrahim S. The abbreviated mental test: its use and validity. Age Ageing. 1991;20(5):332-6. [Link] [DOI:10.1093/ageing/20.5.332]
28. Gomez de Caso JA, Rodriguez-Artalejo F, Claveria LE, Coria F. Value of Hodkinson's test for detecting dementia and mild cognitive impairment in epidemiological surveys. Neuroepidemiology. 1994;13(1-2):64-8. [Link] [DOI:10.1159/000110360]
29. Bakhtiyari F, Foroughan M, Fakhrzadeh H, Nazari N, Najafi B, Alizadeh M, et al. Validation of the persian version of abbreviated mental test (AMT) in elderly residents of kahrizak charity foundation. Iranian J Diabetes Metab. 2014;13(6):487-94. [Link]
30. Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci. 1998;53(1):P43-50. [Link] [DOI:10.1093/geronb/53B.1.P43]
31. Zarei M, Lajevardi L, Zarei MA, Mollazadeh E. Translation, content validity, and internal consistency of the persian version of the survey of activities and fear of falling in the elderly with parkinson's disease. Sci J Rehabil Med. 2017;6(1):93-103. [Persian] [Link]
32. Hee J. The effects of body mechanics training on fear of falling in community-dwelling older adults [dissertation]. Tacoma: University of Puget Sound; 2011. [Link]
33. Pighills AC, Torgerson DJ, Sheldon TA, Drummond AE, Bland JM. Environmental assessment and Modification to prevent falls in older people. J compilation, J Am Geriatr Soc. 2011;59(1):26-33. [Link] [DOI:10.1111/j.1532-5415.2010.03221.x]
34. Torkaman Gholami J, Mohamadi Shahbolaghi F, Norouzi K, Reza soltani P. The relationship between fear of falling and activity limitations among seniors of Ghaem Shahr city in 2013. Iranian J Rehabil Res Nurs. 2015;2(1):45-52. [Persian] [Link]
35. Ghezeljeh TN, Yekta ZP, Mehran A, Oori MJ. Effect of a multidimensional fall prevention program on incidence of falling and quality of life among elderly. HAYAT. 2014;20(2). [Link]
36. Liu Y, Tsui C. A randomized trial comparing Tai Chi with and without cognitive-behavioral intervention (CBI) to reduce fear of falling in community-dwelling elderly people. Arch Gerontol Geriatr. 2014;59(2):317-25. [Link] [DOI:10.1016/j.archger.2014.05.008]
37. Dorresteijn TAC, Rixt Zijlstra GA, Ambergen AW, Delbaere K, Vlaeyen JWS, Kempen GIJM. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial BMC Geriatr. 2016;16:2. [Link] [DOI:10.1186/s12877-016-0278-2]
38. Mortazavi H, Tabatabaeichehr M, Golestani A, Armat MR, Yousefi MR. The effect of Tai Chi exercise on the risk and fear of falling in older adults: a randomized clinical trial. Mater Sociomed. 2018;30(1):38-42. [Link] [DOI:10.5455/msm.2018.30.38-42]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |