Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 179-186 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Arab-Borzu Z, Shahraki-Mohammadi A, Mollazehi-Bakhshan M. Mental Health Literacy and Quality of Life in Iranian Medical Students. Health Educ Health Promot 2025; 13 (1) :179-186
URL: http://hehp.modares.ac.ir/article-5-79795-en.html
URL: http://hehp.modares.ac.ir/article-5-79795-en.html
1- Department of Biostatistics and Epidemiology, School of Health, Zahedan University of Medical Sciences, Zahedan, Iran
2- Department of Medical Library and Information Sciences, School of Allied Medical Sciences, Zahedan University of Medical Sciences, Zahedan, Iran
3- “Student Research Committee” and “School of Medicine”, Zahedan University of Medical Sciences, Zahedan, Iran
2- Department of Medical Library and Information Sciences, School of Allied Medical Sciences, Zahedan University of Medical Sciences, Zahedan, Iran
3- “Student Research Committee” and “School of Medicine”, Zahedan University of Medical Sciences, Zahedan, Iran
Full-Text [PDF 640 kb]
(451 Downloads)
| Abstract (HTML) (533 Views)
Full-Text: (47 Views)
Introduction
The long-term health and well-being of all members of society are significantly correlated with the educational level and literacy they acquire throughout their lives, particularly in terms of health and mental health [1]. Mental health literacy refers to the knowledge and beliefs that contribute to the recognition, management, and prevention of mental disorders. It encompasses six dimensions: recognizing symptoms of psychiatric disorders, maintaining positive attitudes that encourage seeking help, understanding the causes and risk factors, knowledge of available treatments, awareness of accessible self-help strategies, and knowing how to seek mental health information [2]. An individual’s mental health can be shaped by various environments [3]. Recent studies indicate a gradual increase in the prevalence of mental health disorders among students worldwide [4]. This underscores the critical importance of assessing mental health literacy among students. Throughout their education, medical students should acquire the necessary knowledge, skills, and professional attitudes to address lifelong challenges in their profession [5]. Previous studies have shown that pursuing medical studies can impact students’ mental health [6]. Depression, anxiety, and stress have been reported to be excessively prevalent among medical students [7]. Moreover, these conditions tend to escalate during their studies [8].
Paying attention to students’ quality of life during their studies, a period marked by significant stress is of paramount importance [9]. Leaving the family environment, experiencing peer pressure, and facing a new setting challenge students’ mental health and well-being [10]. University, with no guaranteed future, demands a substantial investment of time and resources from students [11]. Psychological stress deteriorates various aspects of individuals’ quality of life, including physical, psychological, and environmental health. Health literacy, particularly mental health literacy, is a critical factor in the recognition and understanding of mental health disorders. It is essential for diagnosing, managing, and preventing mental health problems, as well as for improving quality of life [12]. In a study examining mental health literacy and quality of life among physicians, nurses, and other hospital staff, Su et al. concluded that both quality of life and mental health literacy were poor across all occupational groups within hospitals [13].
Quality of life and mental health literacy are among the factors influencing the daily lives, efficiency, job satisfaction, and academic satisfaction of students, as well as their future performance as healthcare providers. Therefore, mental health literacy, defined as understanding the signs and symptoms of mental disorders and recognizing the necessity of consulting an appropriate specialist, is a crucial factor in believing in and identifying mental health disorders to diagnose, manage, and prevent mental health problems, ultimately improving quality of life.
Many individuals, especially students, do not receive accurate information about mental disorders, and misinformation can deprive them of appropriate medical care and support [14]. Consequently, it has a significant effect on students’ quality of life. Thus, examining the relationship between mental health literacy and students’ quality of life and subsequently providing appropriate solutions to their problems can contribute to the advancement of a university’s educational objectives. Although numerous studies have investigated the relationship between general health literacy and quality of life, few studies have explored the connection between mental health literacy and quality of life. Given the importance and prevalence of this topic, this study aimed to investigate the dimensions of mental health literacy and its relationship with quality of life among students at Zahedan University of Medical Sciences.
Instrument and Methods
This study was a cross-sectional descriptive study conducted in 2024 at Zahedan University of Medical Sciences. Considering a significance level of α=0.05 and a power of 80%, and given r=0.43 from previous studies [15], the sample size was calculated using the formulas w=1/2(log(1+r/1-r)) and n=(z1-B+Z1-a/2)²/w². Accounting for a 10% attrition rate, 220 individuals were enrolled in the study.
The sampling method employed was proportional stratified random sampling. Each educational level (undergraduate, graduate, and general medicine) was considered a stratum. Given the population sizes for each stratum (bachelor’s, master’s, and doctoral) as 1971, 1858, and 260 respectively, the sample sizes for the bachelor’s, master’s, and doctoral groups were 105, 100, and 15, proportional to the population of each stratum, and participants were randomly selected from each group.
To collect data, researchers visited Zahedan University of Medical Sciences and introduced themselves to the students. They explained the research objectives and provided detailed information about the confidentiality of the data. After obtaining informed consent, questionnaires (comprising a mental health literacy questionnaire and a quality of life questionnaire) were distributed to the students. The participants were requested to complete the questionnaires honestly. The inclusion criterion for this study was the willingness and consent of Zahedan University of Medical Sciences students to participate.
Data were collected using the personal information form, the Mental Health Literacy Scale (MHLS) and the Quality of Life Scale.
The personal information form included questions about age, gender, education level, occupation, marital status, family history of mental illness, previous referrals to psychologists/psychiatrists, sources of information on mental health, and completion of psychology courses.
The MHLS was developed by O’Connor & Casey in 2015 [16]. O’Connor & Casey reported an internal consistency of 0.873 using Cronbach’s alpha in their study. The validity and reliability of this questionnaire were evaluated in Iran by Noroozi et al. [17]. The Cronbach’s alpha and the content validity ratio (CVR) for the questionnaire were 0.72 and 0.90, respectively. This scale consists of 35 items and measures six dimensions of mental health literacy, including the ability of individuals to recognize mental disorders, knowledge of risk factors and causes, knowledge of self-treatment, knowledge of professional help available, knowledge of where to seek information, and attitudes that recognize help-seeking behavior. A higher score for each attribute indicates a higher literacy rate for that attribute. The total MHLS score is calculated by summing the scores of all the attributes, with a minimum score of 35 and a maximum score of 160. Higher scores reflect a more favorable MHLS status.
The Quality of Life Questionnaire (SF-12) is a shortened version of a questionnaire developed by Ware et al. and is widely used in various studies [18]. The validity and reliability of this 12-item questionnaire have been confirmed by Montazeri et al. [19]. Cronbach’s alpha values for the physical health subscale and the mental health subscale were 0.73 and 0.72, respectively. These 12 items are divided into two subscales; physical health with six items and mental health with six items. The minimum and maximum scores on the physical health subscale range from 6 to 20, while the minimum and maximum scores on the mental health subscale range from 6 to 27. Higher scores on each subscale indicate a better quality of life. The total quality of life score is obtained by summing the scores of the two subscales (physical health and mental health).
Data analysis
Quantitative parameters were expressed as mean±standard deviation (SD), while qualitative parameters were expressed in terms of frequency and percentage. Independent samples t-tests and one-way analysis of variance (ANOVA) were used to examine the differences between groups. To determine the relationship between the effect of parameters and family history of mental illness, as well as referrals to psychologists or psychiatrists, logistic regression analysis was employed. Parameters with a p-value less than 0.2 in the univariate logistic regression analysis were included in the multiple logistic regression analysis. We also used Pearson’s correlation test to examine the relationship between attributes of mental health literacy and quality of life. The data were analyzed using SPSS software version 24. The significance level for all tests in this study was set at p<0.05.
Findings
A total of 220 participants were included in this study, of which 120 (54.5%) were male. The average age of the participants was 22.20 ± 2.69 years. Among these participants, 27(12.3%) were employed students. Regarding educational level, 105 cases (47.7%) held bachelor’s degrees, and 100 cases (45%) were pursuing doctoral studies (in general medicine).
There was a significant relationship between mental health literacy and gender, educational level, family history of mental illness, and place of residence. Specifically, women, those with a master’s degree, individuals with a family history of mental illness, and those living in dormitories reported significantly greater levels of mental health literacy than their counterparts. There was a significant association between quality of life and sex, education level, and history of mental illness. Specifically, males, individuals with a master’s degree, and those without a history of mental illness reported higher levels of quality of life (p-value<0.05; Table 1).
Table 1. Frequency of demographic factors (N=220)

There was a significant correlation between mental health literacy and its dimensions. Additionally, a significant correlation was found between quality of life and its dimensions. Furthermore, there was a significant correlation between quality of life and its psychological health dimension. Finally, a significant relationship was observed between mental health literacy and quality of life (p<0.001; Table 2).
Table 2. Pearson correlation between the attributes of mental health literacy and quality of life

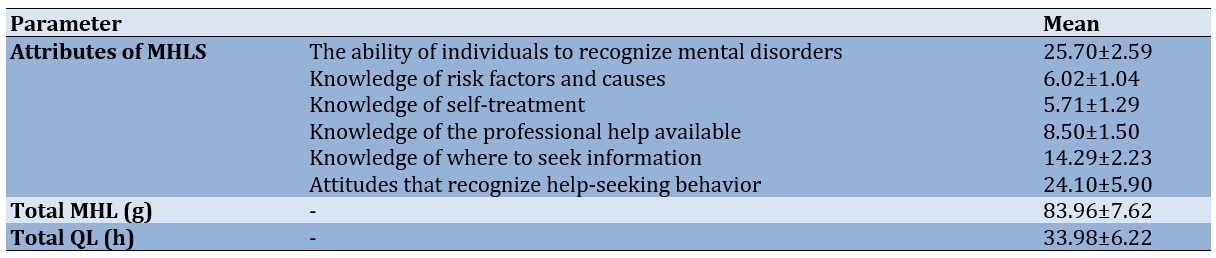
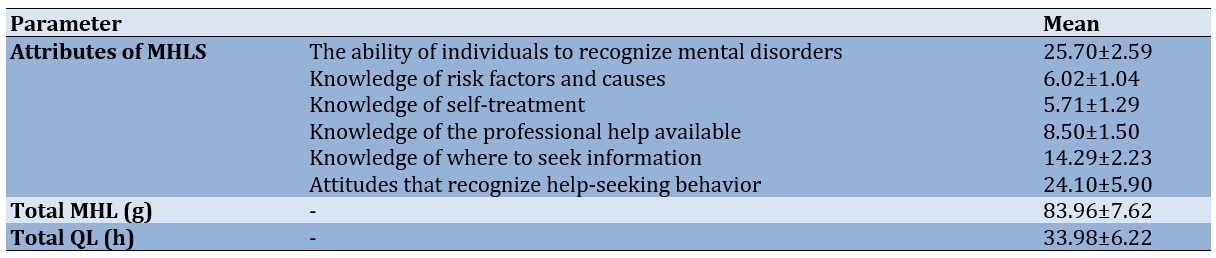
The average scores for different dimensions of mental health literacy and quality of life were measured (Table 3).
Table 3. Mean scores of mental health literacy and quality of life
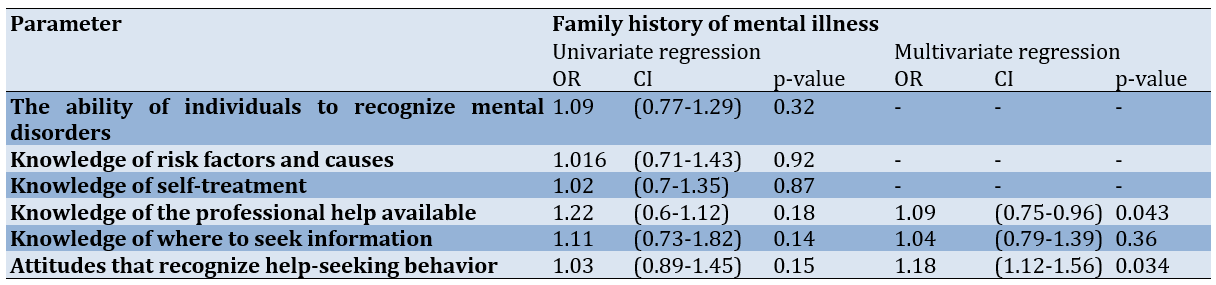
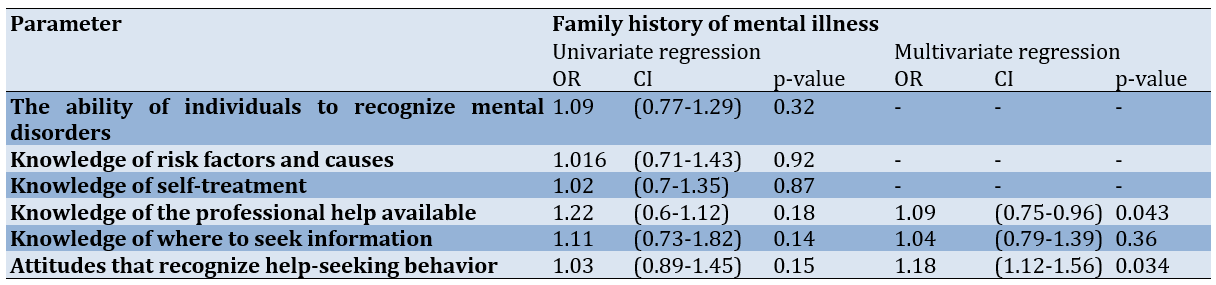
The multiple logistic regression showed a significant relationship between knowledge of the professional help available and attitudes that recognize help-seeking behavior with a family history of mental illness (p-value<0.05; Table 4).
Table 4. Relationship between a family history of mental illness and mental health literacy
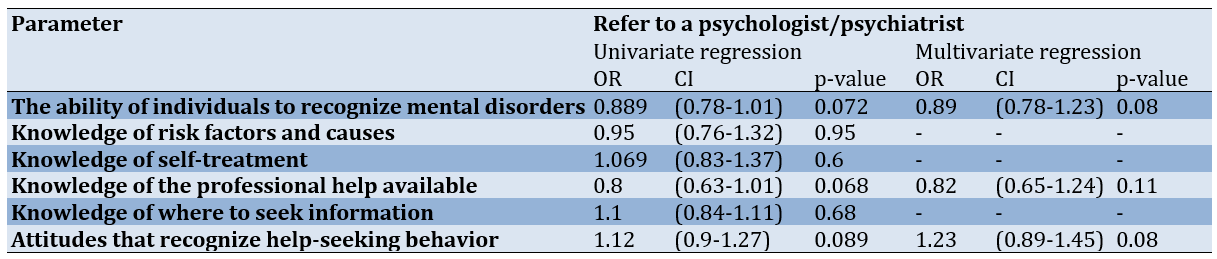
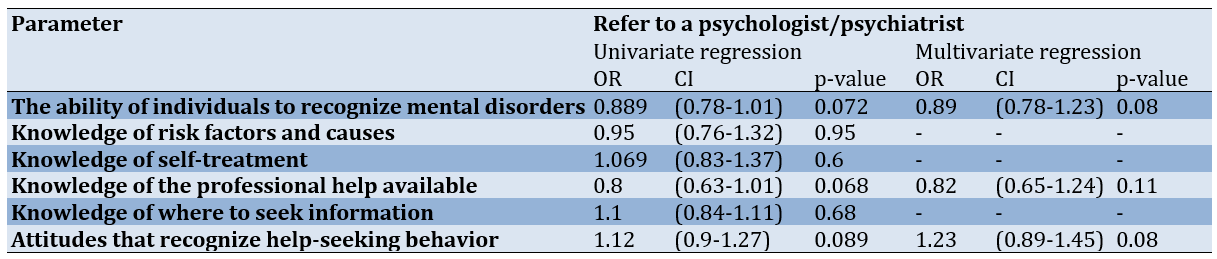
Furthermore, there was no significant relationship between referrals to a psychologist or psychiatrist and the dimensions of mental health in the multiple logistic regression model (p-value>0.05; Table 5).
Table 5. Relationship between previous referral to a psychologist/psychiatrist and mental health literacy
Discussion
This study aimed to investigate the dimensions of health literacy and its relationship with quality of life among students at Zahedan University of Medical Sciences. Among the levels of mental health literacy, the highest average was related to the ability of individuals to recognize mental disorders and attitudes that promote help-seeking behavior. The level of mental health literacy among students was not high. In a survey conducted by Nguyen Thai & Nguyen [20], the students examined have not demonstrate a high level of mental health literacy regarding depression, and these findings were consistent with ours. The results of Bahrami et al. [21] are also consistent with those of the present study, indicating that the mental health literacy level of female students is not high. In a study conducted by Dessauvagie et al. [22], university students from Vietnam and Cambodia are found to have lower levels of mental health literacy than their counterparts in Western countries. The most prevalent concerns among these students were the fear of stigma associated with mental illness and a reluctance to seek professional help. Syafitri [23] reported that students exhibit low levels of mental health literacy and hold negative attitudes toward seeking professional help. Low mental health literacy among students can significantly impact their academic progress, as mental health issues can directly affect their performance and motivation [24]. Furthermore, low mental health literacy among students, particularly those struggling with mental health issues, can lead to delayed recognition of these problems and a reluctance to seek professional help, which, in the long term, can result in irreversible consequences such as suicide.
The mean quality of life was 33.98±6.22 out of 47. Furthermore, there was a significant correlation between the total mental health literacy score and quality of life. Jafari et al. [15] report a positive correlation between mental health literacy and quality of life, noting that individuals who receive mental health information report a greater quality of life. Tehrani et al. [25] have found a significant correlation between depression literacy and quality of life, suggesting that depression literacy is a potential factor for improving mental health and enhancing the quality of life within communities. In the study by Rababah et al. [26], there is a positive impact of health literacy on quality of life. A systematic review exploring the relationship between health literacy and quality of life has revealed a moderate correlation between these two parameters among university students [27]. In the study by Barati et al. [28], the quality of life is correlated with health literacy, and as the evaluation and use of health information increase, a greater quality of life is reported. Increased health literacy can lead to more preventive behaviors and timely treatment of diseases, particularly mental health issues. According to the available evidence, an increase in health-related knowledge can significantly improve the quality of life for individuals in a community [28, 29].
There was a significant correlation between students’ mental health literacy and gender, with female students demonstrating higher levels of mental health literacy. In studies conducted by Baklola et al. [30], Gorczynski & Sims-Schouten [31], Dessauvagie et al. [22], and Reichel et al. [32], examining mental health literacy among students, a significant correlation has been found between gender and mental health literacy, with females exhibiting higher levels of mental health literacy than males, which is consistent with those of the present study. Furthermore, previous studies have indicated that females show a greater capacity for recognizing mental disorders [33, 34] and are more likely than males to seek professional help when confronted with mental health issues [35]. Additionally, females tend to be more inclined to acquire information about mental health and to interact with individuals who suffer from mental health problems [19]. This inclination can help increase knowledge and awareness in the field of mental disorders.
There was a significant relationship between gender and medical students’ quality of life, with men reporting a higher quality of life. A study conducted by Popov & Melikhova [36] reveals that male medical students report a higher quality of life than their female counterparts. However, as students gain more educational experience and progress through their studies, the impact of gender on medical students’ quality of life diminishes. In the study by Jafari et al. [15], men report a higher quality of life score than women. In the study by Gilan et al. [37], conducted in the general population, the women have reported a greater quality of life than men. The reason for this difference from the present study may be that female medical students experience stressful conditions due to the pressures of studying and being away from their families, which can adversely affect their quality of life.
Doctoral and master’s degree students presented significantly higher mental health literacy levels than undergraduate students and this correlation was statistically significant. Picco et al. [34] also have found a significant correlation between medical students’ ability to recognize mental disorders and their level of education, with higher-year students demonstrating a greater capacity for recognizing mental disorders. In the study by Miles et al. [38], fourth-year undergraduate students have a higher mental health literacy level than students in lower years. Lee et al. [39] also demonstrate that individuals with higher levels of education exhibit a greater propensity to enhance their mental health literacy. Students likely gain more knowledge and life experience with increasing years of education, especially in higher grades. They become familiar with the university setting and gain increased exposure to mental health services, which potentially contributes to the improvement of their mental health literacy.
A significant relationship was found between educational level and the quality of life of students. Master’s and doctoral students reported a higher quality of life than undergraduate students. Gil-Lacruz et al. [40] also report a significant correlation between educational level and health-related quality of life among young adults, indicating that young people with university degrees reported higher health-related quality of life. Jafari et al. [15] also report a significant correlation between education level and quality of life, revealing that individuals with higher levels of academic education reported a greater quality of life. One of the factors that can influence the improvement of quality of life is educational level; as educational level increases, the quality of life of individuals significantly improves [41].
The relationship between passing psychology courses and the level of mental health literacy was significant, with the average score of mental health literacy reported to be higher among students who took these courses. This finding is consistent with those of Reichel et al. [32]. Due to their psychology coursework, medical students exhibit higher levels of mental health literacy regarding depression. Miles et al. [38] report that taking a psychology course or studying psychology as a major significantly impacts students’ mental health literacy. In a study conducted by Miles et al. [42] on the relationship between the field of study and mental health literacy among undergraduate students, students majoring in psychology possess higher mental health literacy than those in other fields, such as biology and nursing. Since mental health literacy is a crucial life skill for students, it is recommended that suitable educational interventions be designed and implemented to improve mental health literacy, especially in educational environments.
There was a significant correlation between place of residence and mental health literacy. Individuals residing in dormitories reported higher levels of mental health literacy but lower quality of life. Sobhanifar et al. [43] reveal a significant relationship between place of residence and mental health literacy, with students living in dormitories reporting a higher level of mental health literacy, which is consistent with our findings. Collective living environments, such as student dormitories, facilitate increased interaction among students in informal settings, which may provide a foundation for the transfer of knowledge and experiences in the fields of health and mental health.
Individuals with a family history of mental disorders demonstrated a greater level of mental health literacy in terms of knowledge of the professional help available and attitudes that recognize help-seeking behavior. Similarly, in Gorczynski & Sims-Schouten's study [31], individuals reporting a prior history of mental health disorders present greater mental health literacy than those without such experiences. In the study conducted by Dessauvagie et al. [22] students reporting personal experiences with mental disorders (self or family) demonstrate greater mental health literacy than their peers did. Jafari et al.'[15] reveal a significant correlation between a family history of mental disorders and knowledge about available professional help. For patients suffering from a mental disorder, having a family member with a basic understanding of mental health can significantly impact their social support and the pursuit of appropriate professional help [44]. On the other hand, people who have experienced mental health problems in themselves or their families probably have a high level of mental health literacy due to increased knowledge and experience in this field.
There was a significant relationship between a family history of mental illness and quality of life. Students with no family history of illness reported a higher quality of life. Vaingankar et al. [45] demonstrate that a history of any mental disorder is associated with lower levels of general health and quality of life. Dhungana et al. [46] reveal that psychological disorders, such as anxiety and depression significantly impact the quality of life of patients affected by trauma. Jafari et al. [15] report a significant correlation between family history of illness and quality of life in the general population, indicating that individuals who do not report a family history of mental illness experience a higher quality of life.
A significant correlation was found between participants’ previous referrals to a psychologist or psychiatrist for psychological problems and their ability to recognize mental disorders. Individuals with prior referrals to a psychologist or psychiatrist demonstrated a greater ability to recognize mental health disorders. Miles et al. [38] also reveal that students’ prior experiences with mental health services (i.e., the diagnosis or treatment of mental health problems) significantly influence their mental health literacy. In Tehrani et al.’s study [25], which was conducted in a general population, significant correlations are found between referrals to a psychologist or psychiatrist and mental health literacy, and the results are consistent with ours. Consistent with the findings of the present study, Mahmoodi et al. [47] also report a significant correlation between students’ mental health literacy and a history of using mental health services. Mental health professionals are considered reliable sources for obtaining mental health information; thus, prior referrals to a psychologist or psychiatrist and the subsequent knowledge and experience gained in this field can help improve individuals’ mental health literacy.
One limitation of this study was that the data were collected through a questionnaire, which raises the possibility of self-reporting bias among participants. Another limitation of the present study was that, since the sample was selected from students at Zahedan University of Medical Sciences, the results cannot be generalized to all medical students.
The results of the present study revealed that the level of mental health literacy among medical students was not high and that there was a significant relationship between mental health literacy and quality of life among students at Zahedan University of Medical Sciences. Medical students are likely to face significant stress and psychological pressure during their studies, which can lead to the development of mental disorders and a decrease in quality of life. Therefore, discussions related to mental health literacy should be included in the educational curriculum of high schools and the early semesters of university for all learners across all fields of study. Additionally, the implementation of educational interventions such as workshops and seminars aimed at improving students’ mental health literacy is recommended. Furthermore, considering the increasing inclination of the younger generation to utilize advanced technologies such as applications, social networks, and virtual spaces, it seems essential to make greater use of these tools to design and implement programs that enhance the mental health literacy of young people, especially students.
Conclusion
There is a significant relationship between mental health literacy and quality of life among students at Zahedan University of Medical Sciences.
Acknowledgments: This study is part of a general medicine thesis conducted at Zahedan University of Medical Sciences. The researchers from Zahedan University of Medical Sciences express their gratitude for the financial support of this research.
Ethical Permissions: Ethical code: IR.ZAUMS.REC.1402.435.
Conflicts of Interests: The authors declared no competing interests.
Authors' Contribution: Arab-Borzu Z (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Shahraki-Mohammadi A (Second Author), Introduction Writer/Main Researcher/Discussion Writer (60%); Mollazehi-Bakhshan M (Third Author), Introduction Writer/Assistant Researcher (15%)
Funding/Support: This study was funded by Zahedan University of Medical Sciences (N0. 4103).
The long-term health and well-being of all members of society are significantly correlated with the educational level and literacy they acquire throughout their lives, particularly in terms of health and mental health [1]. Mental health literacy refers to the knowledge and beliefs that contribute to the recognition, management, and prevention of mental disorders. It encompasses six dimensions: recognizing symptoms of psychiatric disorders, maintaining positive attitudes that encourage seeking help, understanding the causes and risk factors, knowledge of available treatments, awareness of accessible self-help strategies, and knowing how to seek mental health information [2]. An individual’s mental health can be shaped by various environments [3]. Recent studies indicate a gradual increase in the prevalence of mental health disorders among students worldwide [4]. This underscores the critical importance of assessing mental health literacy among students. Throughout their education, medical students should acquire the necessary knowledge, skills, and professional attitudes to address lifelong challenges in their profession [5]. Previous studies have shown that pursuing medical studies can impact students’ mental health [6]. Depression, anxiety, and stress have been reported to be excessively prevalent among medical students [7]. Moreover, these conditions tend to escalate during their studies [8].
Paying attention to students’ quality of life during their studies, a period marked by significant stress is of paramount importance [9]. Leaving the family environment, experiencing peer pressure, and facing a new setting challenge students’ mental health and well-being [10]. University, with no guaranteed future, demands a substantial investment of time and resources from students [11]. Psychological stress deteriorates various aspects of individuals’ quality of life, including physical, psychological, and environmental health. Health literacy, particularly mental health literacy, is a critical factor in the recognition and understanding of mental health disorders. It is essential for diagnosing, managing, and preventing mental health problems, as well as for improving quality of life [12]. In a study examining mental health literacy and quality of life among physicians, nurses, and other hospital staff, Su et al. concluded that both quality of life and mental health literacy were poor across all occupational groups within hospitals [13].
Quality of life and mental health literacy are among the factors influencing the daily lives, efficiency, job satisfaction, and academic satisfaction of students, as well as their future performance as healthcare providers. Therefore, mental health literacy, defined as understanding the signs and symptoms of mental disorders and recognizing the necessity of consulting an appropriate specialist, is a crucial factor in believing in and identifying mental health disorders to diagnose, manage, and prevent mental health problems, ultimately improving quality of life.
Many individuals, especially students, do not receive accurate information about mental disorders, and misinformation can deprive them of appropriate medical care and support [14]. Consequently, it has a significant effect on students’ quality of life. Thus, examining the relationship between mental health literacy and students’ quality of life and subsequently providing appropriate solutions to their problems can contribute to the advancement of a university’s educational objectives. Although numerous studies have investigated the relationship between general health literacy and quality of life, few studies have explored the connection between mental health literacy and quality of life. Given the importance and prevalence of this topic, this study aimed to investigate the dimensions of mental health literacy and its relationship with quality of life among students at Zahedan University of Medical Sciences.
Instrument and Methods
This study was a cross-sectional descriptive study conducted in 2024 at Zahedan University of Medical Sciences. Considering a significance level of α=0.05 and a power of 80%, and given r=0.43 from previous studies [15], the sample size was calculated using the formulas w=1/2(log(1+r/1-r)) and n=(z1-B+Z1-a/2)²/w². Accounting for a 10% attrition rate, 220 individuals were enrolled in the study.
The sampling method employed was proportional stratified random sampling. Each educational level (undergraduate, graduate, and general medicine) was considered a stratum. Given the population sizes for each stratum (bachelor’s, master’s, and doctoral) as 1971, 1858, and 260 respectively, the sample sizes for the bachelor’s, master’s, and doctoral groups were 105, 100, and 15, proportional to the population of each stratum, and participants were randomly selected from each group.
To collect data, researchers visited Zahedan University of Medical Sciences and introduced themselves to the students. They explained the research objectives and provided detailed information about the confidentiality of the data. After obtaining informed consent, questionnaires (comprising a mental health literacy questionnaire and a quality of life questionnaire) were distributed to the students. The participants were requested to complete the questionnaires honestly. The inclusion criterion for this study was the willingness and consent of Zahedan University of Medical Sciences students to participate.
Data were collected using the personal information form, the Mental Health Literacy Scale (MHLS) and the Quality of Life Scale.
The personal information form included questions about age, gender, education level, occupation, marital status, family history of mental illness, previous referrals to psychologists/psychiatrists, sources of information on mental health, and completion of psychology courses.
The MHLS was developed by O’Connor & Casey in 2015 [16]. O’Connor & Casey reported an internal consistency of 0.873 using Cronbach’s alpha in their study. The validity and reliability of this questionnaire were evaluated in Iran by Noroozi et al. [17]. The Cronbach’s alpha and the content validity ratio (CVR) for the questionnaire were 0.72 and 0.90, respectively. This scale consists of 35 items and measures six dimensions of mental health literacy, including the ability of individuals to recognize mental disorders, knowledge of risk factors and causes, knowledge of self-treatment, knowledge of professional help available, knowledge of where to seek information, and attitudes that recognize help-seeking behavior. A higher score for each attribute indicates a higher literacy rate for that attribute. The total MHLS score is calculated by summing the scores of all the attributes, with a minimum score of 35 and a maximum score of 160. Higher scores reflect a more favorable MHLS status.
The Quality of Life Questionnaire (SF-12) is a shortened version of a questionnaire developed by Ware et al. and is widely used in various studies [18]. The validity and reliability of this 12-item questionnaire have been confirmed by Montazeri et al. [19]. Cronbach’s alpha values for the physical health subscale and the mental health subscale were 0.73 and 0.72, respectively. These 12 items are divided into two subscales; physical health with six items and mental health with six items. The minimum and maximum scores on the physical health subscale range from 6 to 20, while the minimum and maximum scores on the mental health subscale range from 6 to 27. Higher scores on each subscale indicate a better quality of life. The total quality of life score is obtained by summing the scores of the two subscales (physical health and mental health).
Data analysis
Quantitative parameters were expressed as mean±standard deviation (SD), while qualitative parameters were expressed in terms of frequency and percentage. Independent samples t-tests and one-way analysis of variance (ANOVA) were used to examine the differences between groups. To determine the relationship between the effect of parameters and family history of mental illness, as well as referrals to psychologists or psychiatrists, logistic regression analysis was employed. Parameters with a p-value less than 0.2 in the univariate logistic regression analysis were included in the multiple logistic regression analysis. We also used Pearson’s correlation test to examine the relationship between attributes of mental health literacy and quality of life. The data were analyzed using SPSS software version 24. The significance level for all tests in this study was set at p<0.05.
Findings
A total of 220 participants were included in this study, of which 120 (54.5%) were male. The average age of the participants was 22.20 ± 2.69 years. Among these participants, 27(12.3%) were employed students. Regarding educational level, 105 cases (47.7%) held bachelor’s degrees, and 100 cases (45%) were pursuing doctoral studies (in general medicine).
There was a significant relationship between mental health literacy and gender, educational level, family history of mental illness, and place of residence. Specifically, women, those with a master’s degree, individuals with a family history of mental illness, and those living in dormitories reported significantly greater levels of mental health literacy than their counterparts. There was a significant association between quality of life and sex, education level, and history of mental illness. Specifically, males, individuals with a master’s degree, and those without a history of mental illness reported higher levels of quality of life (p-value<0.05; Table 1).
Table 1. Frequency of demographic factors (N=220)

There was a significant correlation between mental health literacy and its dimensions. Additionally, a significant correlation was found between quality of life and its dimensions. Furthermore, there was a significant correlation between quality of life and its psychological health dimension. Finally, a significant relationship was observed between mental health literacy and quality of life (p<0.001; Table 2).
Table 2. Pearson correlation between the attributes of mental health literacy and quality of life

The average scores for different dimensions of mental health literacy and quality of life were measured (Table 3).
Table 3. Mean scores of mental health literacy and quality of life
The multiple logistic regression showed a significant relationship between knowledge of the professional help available and attitudes that recognize help-seeking behavior with a family history of mental illness (p-value<0.05; Table 4).
Table 4. Relationship between a family history of mental illness and mental health literacy
Furthermore, there was no significant relationship between referrals to a psychologist or psychiatrist and the dimensions of mental health in the multiple logistic regression model (p-value>0.05; Table 5).
Table 5. Relationship between previous referral to a psychologist/psychiatrist and mental health literacy
Discussion
This study aimed to investigate the dimensions of health literacy and its relationship with quality of life among students at Zahedan University of Medical Sciences. Among the levels of mental health literacy, the highest average was related to the ability of individuals to recognize mental disorders and attitudes that promote help-seeking behavior. The level of mental health literacy among students was not high. In a survey conducted by Nguyen Thai & Nguyen [20], the students examined have not demonstrate a high level of mental health literacy regarding depression, and these findings were consistent with ours. The results of Bahrami et al. [21] are also consistent with those of the present study, indicating that the mental health literacy level of female students is not high. In a study conducted by Dessauvagie et al. [22], university students from Vietnam and Cambodia are found to have lower levels of mental health literacy than their counterparts in Western countries. The most prevalent concerns among these students were the fear of stigma associated with mental illness and a reluctance to seek professional help. Syafitri [23] reported that students exhibit low levels of mental health literacy and hold negative attitudes toward seeking professional help. Low mental health literacy among students can significantly impact their academic progress, as mental health issues can directly affect their performance and motivation [24]. Furthermore, low mental health literacy among students, particularly those struggling with mental health issues, can lead to delayed recognition of these problems and a reluctance to seek professional help, which, in the long term, can result in irreversible consequences such as suicide.
The mean quality of life was 33.98±6.22 out of 47. Furthermore, there was a significant correlation between the total mental health literacy score and quality of life. Jafari et al. [15] report a positive correlation between mental health literacy and quality of life, noting that individuals who receive mental health information report a greater quality of life. Tehrani et al. [25] have found a significant correlation between depression literacy and quality of life, suggesting that depression literacy is a potential factor for improving mental health and enhancing the quality of life within communities. In the study by Rababah et al. [26], there is a positive impact of health literacy on quality of life. A systematic review exploring the relationship between health literacy and quality of life has revealed a moderate correlation between these two parameters among university students [27]. In the study by Barati et al. [28], the quality of life is correlated with health literacy, and as the evaluation and use of health information increase, a greater quality of life is reported. Increased health literacy can lead to more preventive behaviors and timely treatment of diseases, particularly mental health issues. According to the available evidence, an increase in health-related knowledge can significantly improve the quality of life for individuals in a community [28, 29].
There was a significant correlation between students’ mental health literacy and gender, with female students demonstrating higher levels of mental health literacy. In studies conducted by Baklola et al. [30], Gorczynski & Sims-Schouten [31], Dessauvagie et al. [22], and Reichel et al. [32], examining mental health literacy among students, a significant correlation has been found between gender and mental health literacy, with females exhibiting higher levels of mental health literacy than males, which is consistent with those of the present study. Furthermore, previous studies have indicated that females show a greater capacity for recognizing mental disorders [33, 34] and are more likely than males to seek professional help when confronted with mental health issues [35]. Additionally, females tend to be more inclined to acquire information about mental health and to interact with individuals who suffer from mental health problems [19]. This inclination can help increase knowledge and awareness in the field of mental disorders.
There was a significant relationship between gender and medical students’ quality of life, with men reporting a higher quality of life. A study conducted by Popov & Melikhova [36] reveals that male medical students report a higher quality of life than their female counterparts. However, as students gain more educational experience and progress through their studies, the impact of gender on medical students’ quality of life diminishes. In the study by Jafari et al. [15], men report a higher quality of life score than women. In the study by Gilan et al. [37], conducted in the general population, the women have reported a greater quality of life than men. The reason for this difference from the present study may be that female medical students experience stressful conditions due to the pressures of studying and being away from their families, which can adversely affect their quality of life.
Doctoral and master’s degree students presented significantly higher mental health literacy levels than undergraduate students and this correlation was statistically significant. Picco et al. [34] also have found a significant correlation between medical students’ ability to recognize mental disorders and their level of education, with higher-year students demonstrating a greater capacity for recognizing mental disorders. In the study by Miles et al. [38], fourth-year undergraduate students have a higher mental health literacy level than students in lower years. Lee et al. [39] also demonstrate that individuals with higher levels of education exhibit a greater propensity to enhance their mental health literacy. Students likely gain more knowledge and life experience with increasing years of education, especially in higher grades. They become familiar with the university setting and gain increased exposure to mental health services, which potentially contributes to the improvement of their mental health literacy.
A significant relationship was found between educational level and the quality of life of students. Master’s and doctoral students reported a higher quality of life than undergraduate students. Gil-Lacruz et al. [40] also report a significant correlation between educational level and health-related quality of life among young adults, indicating that young people with university degrees reported higher health-related quality of life. Jafari et al. [15] also report a significant correlation between education level and quality of life, revealing that individuals with higher levels of academic education reported a greater quality of life. One of the factors that can influence the improvement of quality of life is educational level; as educational level increases, the quality of life of individuals significantly improves [41].
The relationship between passing psychology courses and the level of mental health literacy was significant, with the average score of mental health literacy reported to be higher among students who took these courses. This finding is consistent with those of Reichel et al. [32]. Due to their psychology coursework, medical students exhibit higher levels of mental health literacy regarding depression. Miles et al. [38] report that taking a psychology course or studying psychology as a major significantly impacts students’ mental health literacy. In a study conducted by Miles et al. [42] on the relationship between the field of study and mental health literacy among undergraduate students, students majoring in psychology possess higher mental health literacy than those in other fields, such as biology and nursing. Since mental health literacy is a crucial life skill for students, it is recommended that suitable educational interventions be designed and implemented to improve mental health literacy, especially in educational environments.
There was a significant correlation between place of residence and mental health literacy. Individuals residing in dormitories reported higher levels of mental health literacy but lower quality of life. Sobhanifar et al. [43] reveal a significant relationship between place of residence and mental health literacy, with students living in dormitories reporting a higher level of mental health literacy, which is consistent with our findings. Collective living environments, such as student dormitories, facilitate increased interaction among students in informal settings, which may provide a foundation for the transfer of knowledge and experiences in the fields of health and mental health.
Individuals with a family history of mental disorders demonstrated a greater level of mental health literacy in terms of knowledge of the professional help available and attitudes that recognize help-seeking behavior. Similarly, in Gorczynski & Sims-Schouten's study [31], individuals reporting a prior history of mental health disorders present greater mental health literacy than those without such experiences. In the study conducted by Dessauvagie et al. [22] students reporting personal experiences with mental disorders (self or family) demonstrate greater mental health literacy than their peers did. Jafari et al.'[15] reveal a significant correlation between a family history of mental disorders and knowledge about available professional help. For patients suffering from a mental disorder, having a family member with a basic understanding of mental health can significantly impact their social support and the pursuit of appropriate professional help [44]. On the other hand, people who have experienced mental health problems in themselves or their families probably have a high level of mental health literacy due to increased knowledge and experience in this field.
There was a significant relationship between a family history of mental illness and quality of life. Students with no family history of illness reported a higher quality of life. Vaingankar et al. [45] demonstrate that a history of any mental disorder is associated with lower levels of general health and quality of life. Dhungana et al. [46] reveal that psychological disorders, such as anxiety and depression significantly impact the quality of life of patients affected by trauma. Jafari et al. [15] report a significant correlation between family history of illness and quality of life in the general population, indicating that individuals who do not report a family history of mental illness experience a higher quality of life.
A significant correlation was found between participants’ previous referrals to a psychologist or psychiatrist for psychological problems and their ability to recognize mental disorders. Individuals with prior referrals to a psychologist or psychiatrist demonstrated a greater ability to recognize mental health disorders. Miles et al. [38] also reveal that students’ prior experiences with mental health services (i.e., the diagnosis or treatment of mental health problems) significantly influence their mental health literacy. In Tehrani et al.’s study [25], which was conducted in a general population, significant correlations are found between referrals to a psychologist or psychiatrist and mental health literacy, and the results are consistent with ours. Consistent with the findings of the present study, Mahmoodi et al. [47] also report a significant correlation between students’ mental health literacy and a history of using mental health services. Mental health professionals are considered reliable sources for obtaining mental health information; thus, prior referrals to a psychologist or psychiatrist and the subsequent knowledge and experience gained in this field can help improve individuals’ mental health literacy.
One limitation of this study was that the data were collected through a questionnaire, which raises the possibility of self-reporting bias among participants. Another limitation of the present study was that, since the sample was selected from students at Zahedan University of Medical Sciences, the results cannot be generalized to all medical students.
The results of the present study revealed that the level of mental health literacy among medical students was not high and that there was a significant relationship between mental health literacy and quality of life among students at Zahedan University of Medical Sciences. Medical students are likely to face significant stress and psychological pressure during their studies, which can lead to the development of mental disorders and a decrease in quality of life. Therefore, discussions related to mental health literacy should be included in the educational curriculum of high schools and the early semesters of university for all learners across all fields of study. Additionally, the implementation of educational interventions such as workshops and seminars aimed at improving students’ mental health literacy is recommended. Furthermore, considering the increasing inclination of the younger generation to utilize advanced technologies such as applications, social networks, and virtual spaces, it seems essential to make greater use of these tools to design and implement programs that enhance the mental health literacy of young people, especially students.
Conclusion
There is a significant relationship between mental health literacy and quality of life among students at Zahedan University of Medical Sciences.
Acknowledgments: This study is part of a general medicine thesis conducted at Zahedan University of Medical Sciences. The researchers from Zahedan University of Medical Sciences express their gratitude for the financial support of this research.
Ethical Permissions: Ethical code: IR.ZAUMS.REC.1402.435.
Conflicts of Interests: The authors declared no competing interests.
Authors' Contribution: Arab-Borzu Z (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%); Shahraki-Mohammadi A (Second Author), Introduction Writer/Main Researcher/Discussion Writer (60%); Mollazehi-Bakhshan M (Third Author), Introduction Writer/Assistant Researcher (15%)
Funding/Support: This study was funded by Zahedan University of Medical Sciences (N0. 4103).
Article Type: Descriptive & Survey |
Subject:
Health Literacy
Received: 2025/03/5 | Accepted: 2025/04/8 | Published: 2025/04/11
Received: 2025/03/5 | Accepted: 2025/04/8 | Published: 2025/04/11
References
1. Turunen H, Sormunen M, Jourdan D, Von Seelen J, Buijs G. Health promoting schools-a complex approach and a major means to health improvement. Health Promot Int. 2017;32(2):177-84. [Link] [DOI:10.1093/heapro/dax001]
2. Sharifi V, Amin-Esmaeili M, Hajebi A, Motevalian A, Radgoodarzi R, Hefazi M, et al. Twelve-month prevalence and correlates of psychiatric disorders in Iran: The Iranian mental health survey, 2011. Arch Iran Med. 2015;18(2):76-84. [Link]
3. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392-407. [Link] [DOI:10.3109/09540261.2014.928270]
4. Hussain R, Guppy M, Robertson S, Temple E. Physical and mental health perspectives of first year undergraduate rural university students. BMC Public Health. 2013;13(1):848. [Link] [DOI:10.1186/1471-2458-13-848]
5. Kulsoom B, Afsar NA. Stress, anxiety, and depression among medical students in a multiethnic setting. Neuropsychiatr Dis Treat. 2015;11:1713-22. [Link] [DOI:10.2147/NDT.S83577]
6. Farahangiz S, Mohebpour F, Salehi A. Assessment of mental health among Iranian medical students: A cross-sectional study. Int J Health Sci. 2016;10(1):49-55. [Link] [DOI:10.12816/0031216]
7. Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141(3):354-7. [Link] [DOI:10.4103/0971-5916.156571]
8. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354-73. [Link] [DOI:10.1097/00001888-200604000-00009]
9. Ribeiro Í, Pereira R, Freire I, De Oliveira B, Casotti A, Boery E. Stress and quality of life among university students: A systematic literature review. Health Prof Educ. 2018;4(2):70-7. [Link] [DOI:10.1016/j.hpe.2017.03.002]
10. Jaspal R, Lopes B, Wignall L. The coping with identity threat scale: Development and validation in a university student sample. Identity. 2020;20(4):225-38. [Link] [DOI:10.1080/15283488.2020.1808469]
11. Geirdal AØ, Ruffolo M, Leung J, Thygesen H, Price D, Bonsaksen T, et al. Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. J Ment Health. 2021;30(2):148-55. [Link] [DOI:10.1080/09638237.2021.1875413]
12. Lam LT. Mental health literacy and mental health status in adolescents: A population-based survey. Child Adolesc Psychiatry Ment Health. 2014;8:26. [Link] [DOI:10.1186/1753-2000-8-26]
13. Su J, Weng H, Tsang HY, Wu JL. Mental health and quality of life among doctors, nurses and other hospital staff. Stress Health. 2009;25(5):423-30. [Link] [DOI:10.1002/smi.1261]
14. Sayarifard A, Ghadirian L. Mental health literacy in Iran: An urgent need for a remedy. Int J Prev Med. 2013;4(7):741-3. [Link]
15. Jafari A, Nejatian M, Momeniyan V, Barsalani FR, Tehrani H. Mental health literacy and quality of life in Iran: A cross-sectional study. BMC Psychiatry. 2021;21(1):499. [Link] [DOI:10.1186/s12888-021-03507-5]
16. O'Connor M, Casey L. The mental health literacy scale (MHLS): A new scale-based measure of mental health literacy. Psychiatry Res. 2015;229(1-2):511-6. [Link] [DOI:10.1016/j.psychres.2015.05.064]
17. Noroozi A, Khademolhosseini F, Lari H, Tahmasebi R. The mediator role of mental health literacy in the relationship between demographic variables and health-promoting behaviours. Iran J Psychiatry Behav Sci. 2018;12(2):e12603. [Link] [DOI:10.5812/ijpbs.12603]
18. Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-33. [Link] [DOI:10.1097/00005650-199603000-00003]
19. Montazeri A, Vahdaninia M, Mousavi SJ, Omidvari S. The Iranian version of 12-item short form health survey (SF-12): Factor structure, internal consistency and construct validity. BMC Public Health. 2009;9:341. [Link] [DOI:10.1186/1471-2458-9-341]
20. Nguyen Thai QC, Nguyen TH. Mental health literacy: Knowledge of depression among undergraduate students in Hanoi, Vietnam. Int J Ment Health Syst. 2018;12:19. [Link] [DOI:10.1186/s13033-018-0195-1]
21. Bahrami MA, Bahrami D, Chaman-Ara K. The correlations of mental health literacy with psychological aspects of general health among Iranian female students. Int J Ment Health Syst. 2019;13(1):59. [Link] [DOI:10.1186/s13033-019-0315-6]
22. Dessauvagie A, Dang HM, Truong T, Nguyen T, Nguyen H, Cao H, et al. Mental health literacy of university students in Vietnam and Cambodia. Int J Ment Health Promot. 2022;24(3):439-56. [Link] [DOI:10.32604/ijmhp.2022.018030]
23. Syafitri DU. Mental health literacy among university students in Semarang city. Psychosophia. 2022;4(1):19-35. [Link] [DOI:10.32923/psc.v4i1.1851]
24. Segar PG, Kosnin AM. Influencing factors, academic impacts, and effective evidence-based interventions for university and college students' mental health: A systematic review. Int J Acad Res Bus Soc. 2024;14(9). [Link] [DOI:10.6007/IJARBSS/v14-i9/22707]
25. Tehrani H, Vali M, Nejatian M, Moshki M, Charoghchian Khorasani E, Jafari A. The status of depression literacy and its relationship with quality of life among Iranian public population: A cross sectional study. BMC Psychiatry. 2022;22(1):607. [Link] [DOI:10.1186/s12888-022-04251-0]
26. Rababah JA, Al-Hammouri MM, Drew BL. The impact of health literacy on college students' psychological disturbances and quality of life: A structural equation modeling analysis. Health Qual Life Outcomes. 2020;18(1):292. [Link] [DOI:10.1186/s12955-020-01541-7]
27. Zheng M, Jin H, Shi N, Duan C, Wang D, Yu X, et al. The relationship between health literacy and quality of life: A systematic review and meta-analysis. Health Qual Life Outcomes. 2018;16(1):201. [Link] [DOI:10.1186/s12955-018-1031-7]
28. Barati M, Bijari S, Taherpour M, Afshari M. Investigating the relationship between staff health literacy and quality of life in Famennian County: A cross-sectional study. J Health Lit. 2019;4(3):46-55. [Link]
29. Zhang S, Xiang W. Income gradient in health-related quality of life-the role of social networking time. Int J Equity Health. 2019;18(1):44. [Link] [DOI:10.1186/s12939-019-0942-1]
30. Baklola M, Terra M, Taha A, Elnemr M, Yaseen M, Maher A, et al. Mental health literacy and help-seeking behaviour among Egyptian undergraduates: A cross-sectional national study. BMC Psychiatry. 2024;24(1):202. [Link] [DOI:10.1186/s12888-024-05620-7]
31. Gorczynski P, Sims-Schouten W. Evaluating mental health literacy amongst US college students: A cross sectional study. J Am Coll Health. 2024;72(3):676-9. [Link] [DOI:10.1080/07448481.2022.2063690]
32. Reichel JL, Dietz P, Sauter C, Schneider F, Oenema A. Is mental health literacy for depression associated with the intention toward preventive actions? A cross-sectional study among university students. J Am Coll Health. 2023;71(5):1530-7. [Link] [DOI:10.1080/07448481.2021.1942883]
33. Ghadirian L, Sayarifard A. Depression literacy in urban and suburban residents of Tehran, the capital of Iran; Recognition, help seeking and stigmatizing attitude and the predicting factors. Int J Prev Med. 2019;10:134. [Link] [DOI:10.4103/ijpvm.IJPVM_166_18]
34. Picco L, Seow E, Chua BY, Mahendran R, Verma S, Chong SA, et al. Recognition of mental disorders: Findings from a cross-sectional study among medical students in Singapore. BMJ Open. 2017;7(12):e019038. [Link] [DOI:10.1136/bmjopen-2017-019038]
35. Yu Y, Liu ZW, Hu M, Liu HM, Yang JP, Zhou L, et al. Mental health help-seeking intentions and preferences of rural Chinese adults. PLoS One. 2015;10(11):e0141889. [Link] [DOI:10.1371/journal.pone.0141889]
36. Popov VI, Melikhova EP. Study and methodology for research of the life quality in students. GIGIENA I SANITARIIA. 2016;95(9):879-84. [Russian] [Link] [DOI:10.18821/0016-9900-2016-95-9-879-884]
37. Gilan R, Mohamadi J, Zardoshtian S, Sarabi N, Palangard N, Khezeli M. Predicting perceived quality of life through social trust, physical activity, and sense of happiness in Iran: Moderating role of gender. Health Sci Rep. 2024;7(5):e2121. [Link] [DOI:10.1002/hsr2.2121]
38. Miles R, Rabin L, Krishnan A, Grandoit E, Kloskowski K. Mental health literacy in a diverse sample of undergraduate students: Demographic, psychological, and academic correlates. BMC Public Health. 2020;20(1):1699. [Link] [DOI:10.1186/s12889-020-09696-0]
39. Lee HY, Hwang J, Ball JG, Lee J, Albright DL. Is health literacy associated with mental health literacy? Findings from Mental Health Literacy Scale. Perspect Psychiatr Care. 2020;56(2):393-400. [Link] [DOI:10.1111/ppc.12447]
40. Gil-Lacruz M, Gil-Lacruz AI, Gracia-Pérez ML. Health-related quality of life in young people: The importance of education. Health Qual Life Outcomes. 2020;18(1):187. [Link] [DOI:10.1186/s12955-020-01446-5]
41. Zarezadeh Y, Eskandari N, Moradi M, Abdi N. The relationship between health literacy and quality of life of employees in campus of Kurdistan university of medical sciences. J Health Lit. 2020;4(4):38-45. [Link]
42. Miles RT, Krishnan A, Rabin LA, Brandt SA, Crispino ML. Does major make a difference? Mental health literacy and its relation to college major in a diverse sample of undergraduate students. Discov Ment Health. 2024;4(1):42. [Link] [DOI:10.1007/s44192-024-00099-w]
43. Sobhanifar F, Javanbakht S, Ahmadi Jirandeh R, Rahgoi A, Vahedi M. Mental health literacy and related factors in undergraduate students of university social welfare and rehabilitation sciences. Ment Health Sch. 2025;3(1):48-55. [Persian] [Link]
44. White M, Casey L. Helping older adults to help themselves: The role of mental health literacy in family members. Aging Ment Health. 2017;21(11):1129-37. [Link] [DOI:10.1080/13607863.2016.1206513]
45. Vaingankar JA, Chong SA, Abdin E, Siva Kumar FD, Chua BY, Sambasivam R, et al. Understanding the relationships between mental disorders, self-reported health outcomes and positive mental health: Findings from a national survey. Health Qual Life Outcomes. 2020;18(1):55. [Link] [DOI:10.1186/s12955-020-01308-0]
46. Dhungana S, Koirala R, Ojha SP, Thapa SB. Quality of life and its association with psychiatric disorders in outpatients with trauma history in a tertiary hospital in Kathmandu, Nepal: A cross-sectional study. BMC Psychiatry. 2021;21(1):98. [Link] [DOI:10.1186/s12888-021-03104-6]
47. Mahmoodi SMH, Ahmadzad-Asl M, Eslami M, Abdi M, Hosseini Kahnamoui Y, Rasoulian M. Mental health literacy and mental health information-seeking behavior in Iranian university students. Front Psychiatry. 2022;13:893534. [Link] [DOI:10.3389/fpsyt.2022.893534]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |