Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 55-60 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nomiko D, Bar A, Monalisa M, Eliezer B. Effectiveness of Risk Detection Application in Breast Cancer Prevention in Women of Childbearing Age. Health Educ Health Promot 2025; 13 (1) :55-60
URL: http://hehp.modares.ac.ir/article-5-78855-en.html
URL: http://hehp.modares.ac.ir/article-5-78855-en.html
Effectiveness of Risk Detection Application in Breast Cancer Prevention in Women of Childbearing Age
1- Department of Nursing, Health Polytechnic of Ministry of Health Jambi, Jambi, Indonesia
Full-Text [PDF 577 kb]
(243 Downloads)
| Abstract (HTML) (419 Views)
Full-Text: (20 Views)
Introduction
Breast cancer is a malignancy originating from breast cells that grow and develop uncontrollably, eventually spreading to surrounding tissues or other parts of the body [1-3]. It is one of the most prevalent types of cancer in Indonesia [4]. According to Globocan data from 2020, breast cancer accounted for 11.5% of all cancer cases worldwide, ranking as the second most common cancer globally, with a mortality rate of 6.9%. In Indonesia, the mortality rate was reported at 16.6 per 100,000 population. If left unchecked, it is projected that by 2030, 26 million individuals will be diagnosed with breast cancer, and 17 million will succumb to the disease [5].
In Indonesia, 80% of breast cancer cases are diagnosed at an advanced stage, with approximately 40% of patients treated at Dharmais Hospital Jakarta already in stages III or IV. The mortality rate for advanced-stage (III-IV) breast cancer is high, with life expectancy rates of 72% and 22%, respectively, leading to a poorer prognosis. Cases diagnosed at this stage are categorized as late-stage breast cancer [6].
Early detection is a crucial first step in identifying the possibility of breast cancer. This process begins with self-examination of the breasts [7, 8]. When early detection efforts are followed by clinical breast examinations, the proportion of advanced-stage cancer cases can be reduced by 50%. Methods for early breast cancer detection include breast self-examination (SADARI), clinical breast examination (SADANIS), and mammography. Among these, SADARI is highly recommended, as 86% of breast lumps are discovered by patients themselves. It is also the most affordable and accessible method, particularly for women of reproductive age [9, 10].
Early detection of breast cancer is strongly recommended to raise awareness among women in their 20s about the risks of breast cancer. Therefore, it is crucial to enhance promotive and preventive efforts through early education programs targeted at women of reproductive age. These initiatives aim to facilitate early intervention and ultimately reduce breast cancer mortality rates [11, 12].
In 2022, researchers conducted a study on the development of a breast cancer education model, which included materials on the concept of breast cancer and strategies for its prevention. Building on this, in 2023, an application was developed that incorporated a breast cancer risk detection feature, named the Deriskara Application. The initial development focused solely on creating and conducting basic field tests of the educational model; however, the evaluation phase has not yet been undertaken. In 2024, researchers plan to proceed to the evaluation stage to assess the application’s effectiveness in enhancing respondents’ cognitive abilities regarding breast cancer prevention. This will be conducted through a quasi-experimental design employing a pre-test-post-test control group approach. This research is particularly critical due to the increasing prevalence of breast cancer, which remains the second leading cause of cancer-related deaths among women worldwide. Early risk assessment for breast cancer is therefore essential. The findings from studies utilizing breast cancer risk assessment tools have proven highly beneficial in clinical management, aiding in service delivery for screening and prevention, as well as predicting an individual’s risk of developing breast cancer. Such tools also support the implementation of risk-based screening policies. The development of a web-based application allows for early detection of potential breast cancer risks, ensuring that women are promptly aware of their condition. This enables them to take timely action before cancer cells spread further in the body [13-15].
Early detection of breast cancer risk and staying informed about the latest advancements in cancer treatment are crucial components of an effective strategy to prevent breast cancer-related deaths. The earlier breast cancer is identified (when the tumor is smaller and less likely to have spread), the higher the chances of successful treatment. Regular screening examinations remain one of the most reliable methods for early detection.
This study aligns with the government’s policy and commitment to controlling non-communicable diseases by promoting innovations in health information technology (e-health and m-health) in Indonesia. To contribute to breast cancer prevention efforts, a readily accessible health information system is essential. In this study, an Android-based breast cancer risk assessment application was developed to address this need.
Materials and Methods
Study design and participants
This quasi-experimental study, conducted in 2024, employed a pre-test-post-test control group approach. The intervention group consisted of women of reproductive age residing in the service area of Puskesmas Simpang Kawat, while the control group included women of reproductive age from the service area of Puskesmas Pakuan Baru. The study population consisted of all women of reproductive age residing in the service areas of Pakuan Baru Health Center and Simpang Kawat Health Center in Jambi City. The sampling method used was random sampling. The total population was determined to be 76 individuals. Using a margin of error of 5% (0.05), the required sample size was calculated using the Slovin formula. Based on the calculation, the sample size for a population of 76 individuals with a 5% margin of error was approximately 64 participants. Thus, a total of 64 respondents were included, with 32 participants in the intervention group and 32 in the control group.
Inclusion and exclusion criteria
The inclusion criteria were respondents who owned and were capable of operating Android-based smartphones, were literate, were willing to participate as respondents, and were able to cooperate. The study was conducted at two different sites, namely Puskesmas Simpang Kawat and Puskesmas Pakuan Baru in Jambi City. Puskesmas Simpang Kawat served as the location for testing the application with the intervention group, while Puskesmas Pakuan Baru was used to evaluate the effectiveness of breast cancer education using a pocketbook with the control group.
Data collection
The research process involved several key stages, including obtaining licensing and ethical clearance, developing the application, mapping and selecting the sample, obtaining informed consent, providing education on how to use the application, conducting a pre-test, performing breast cancer screening, delivering breast cancer education, and administering a post-test.
Data collected included respondents’ demographic information and knowledge about breast cancer, which were gathered through interviews and observations. The tools used included questionnaires, pocketbooks, and smartphones. During the data collection phase, two enumerators, who had been trained to ensure data quality and consistency, assisted the researcher.
Research tools
The Knowledge Questionnaire consisted of 15 items, designed to measure respondents’ knowledge about breast cancer prevention in women of reproductive age. The questionnaire was the same for both study groups, ensuring consistent comparison between the groups. Some examples of questions included in the questionnaire were risk factors that can increase the likelihood of breast cancer, the correct way to perform breast self-examination (BSE), the ideal frequency of performing BSE, early signs of breast cancer to watch out for, and the benefits of regular clinical breast examinations (CBE). Additionally, the questionnaire covered topics, such as a healthy lifestyle to prevent cancer, the relationship between high-fat diets and cancer risk, the contribution of physical activity to cancer prevention, as well as the benefits of breastfeeding and early cancer detection. Other questions addressed the impact of family history, alcohol consumption, smoking, chemical exposure, and the importance of breast health education. The questionnaire was developed based on relevant literature, underwent validity and reliability testing, and demonstrated excellent reliability with a Cronbach’s Alpha score of 0.87.
The control group was provided with education using a pocketbook containing material on breast cancer prevention, while the intervention group received education through a smartphone equipped with an application that provided information on breast cancer prevention. The material presented in the pocketbook and the smartphone application was designed to deliver comprehensive and relevant information related to breast cancer prevention. Both the pocketbook and the smartphone application served as the primary sources for developing the knowledge questionnaire used to assess respondents’ understanding. This approach ensured that the educational material provided was aligned with the knowledge assessment instrument, allowing the results to accurately reflect the effectiveness of each educational method.
Data analysis
Data analysis was performed in two descriptive and inferential analysis stages. Descriptive analysis was used to examine changes in knowledge scores before and after the intervention in both study groups.
Inferential analysis began with a data distribution test using the Kolmogorov-Smirnov test to confirm that the data were normally distributed. Once normality was established, a paired t-test was used to assess the difference in scores before and after the intervention within each group. Additionally, an independent t-test was conducted to compare the mean post-intervention scores between the intervention and control groups. Data processing and analysis were conducted using SPSS version 23.0.
Findings
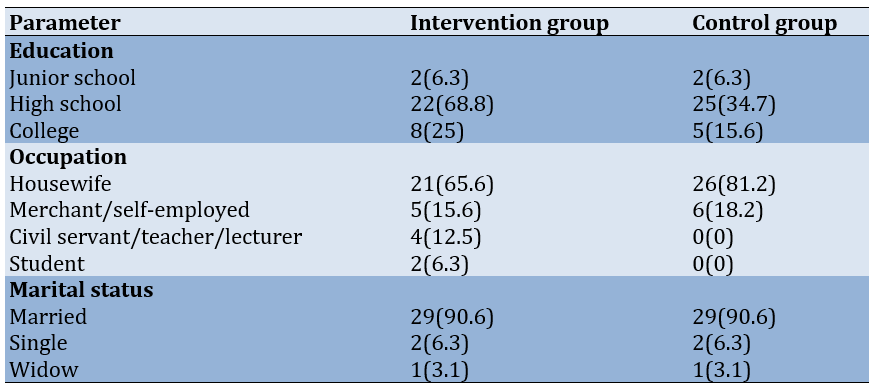
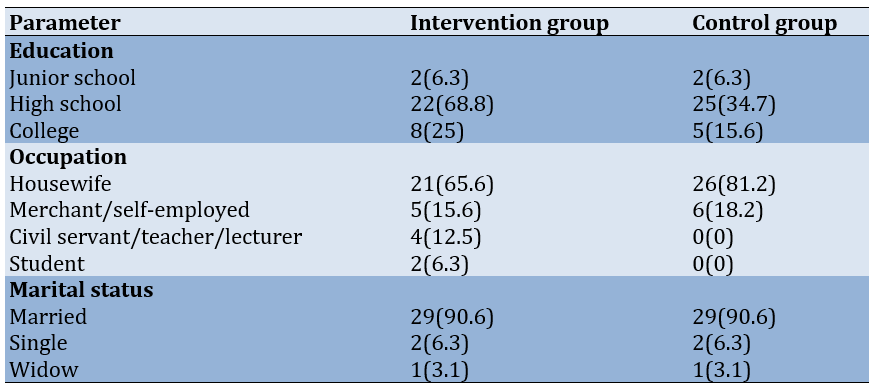
The majority of participants in both groups were approximately the same average age, around 36 years (intervention and control groups: 35.720±8.803 and 35.970±8.499 years, respectively). Most participants had a high school education, with a higher proportion in the intervention group (68.8%) compared to the control group (34.7%). Regarding occupation, the majority were housewives, particularly in the control group (81.2%), while the intervention group had a broader range of occupations, including traders/self-employed individuals (15.6%) and civil servants/teachers/lecturers (12.5%). Most participants in both groups were married (90.6%; Table 1).
Table 1. Frequency of respondents’ characteristics
In the control group, the pre-test mean knowledge level score was 10.750±1.344, which increased to 11.500±1.368 in the post-test (p=0.0001), indicating a statistically significant improvement. In the intervention group, the pre-test mean score was 10.940±1.865, which rose more substantially to 13.380±1.314 at the post-test (p=0.0001). Also, the mean knowledge score in the intervention group was 13.380±1.314, with a 95% confidence interval of 1.205-2.545. In contrast, the control group had a lower mean knowledge score of 11.500±1.368. The difference in knowledge scores between the two groups was statistically significant (p=0.0001).
Discussion
This study aimed to assess the effectiveness of an Android-based breast cancer risk assessment application in enhancing the knowledge of women of reproductive age regarding breast cancer prevention. Breast cancer is a disease characterized by uncontrolled changes in breast tissue cells, often originating from the milk lobules in the ducts. Risk factors for breast cancer are classified into non-modifiable and modifiable factors [16]. Non-modifiable factors include age, gender, race, and family history, while modifiable factors include pregnancy and breastfeeding, hormone therapy, obesity, physical activity, oral contraceptive use, exposure to radiation during breast development, a history of benign tumors, alcohol consumption, smoking, and the intake of fat and red meat [17, 18].
Breast cancer prevention and control programs focus on identifying risk factors and implementing strategies to avoid them through three levels of prevention: primary, secondary, and tertiary. Screening and early detection fall under secondary prevention, which aims to identify pre-cancerous conditions and cancer at an early stage [19, 20]. Early detection of breast cancer involves identifying the disease at its earliest stages, enabling treatment with techniques that have less physical impact and offer a greater chance of recovery. When treated appropriately, the cure rate for breast cancer is quite high (80%-90%), whether through screening or early detection [21].
The principles of screening include, first, that the disease should be severe, relatively common, and recognized as a public health issue by the community. Second, screening should be safe and acceptable to the public [22, 23]. The screening process requires the participation of individuals who are considered appropriate candidates for screening. Third, screening must be accurate and reliable [24].
Early detection of breast cancer aims to identify the disease at its earliest stages, allowing for treatment with techniques that have less physical impact and offer a greater chance of recovery. When treated appropriately, the cure rate for breast cancer is relatively high (80%-90%), whether through screening or early detection. Early discovery is also a strategy for downstaging the disease, beginning with raising public awareness about changes in breast shape or abnormalities. Promoting the SADARI program is essential, as 85% of breast abnormalities are first recognized by the patients themselves [25].
One approach used in the intervention program is the incorporation of technology for breast cancer prevention. The research team developed a breast cancer risk detection application module, targeting women of childbearing age as the primary users. This social network mobile application delivers educational materials about breast cancer through videos, texts, and images, thereby increasing awareness of the disease [26-28].
Various studies have highlighted the benefits of using health technology, particularly through m-Health applications. These studies demonstrate that the use of technology in breast cancer prevention primarily aims to increase awareness about cancer, provide relevant information, and assist in early detection. One study, for example, showed a substantial increase in the average knowledge score, suggesting that mobile applications can be effective tools for disseminating health information.
The use of technology in breast cancer prevention has been explored in several related studies. For example, according to Prochaska et al. [29], the application of technology through m-Health applications in breast cancer typically aims to raise awareness about the disease, provide cancer-related information, and assist in early detection. Other specific research findings have shown that the use of mobile health applications in breast cancer has significantly contributed to early detection programs while also improving accessibility to information and education for ongoing cancer care. Mobile applications offer a mechanism for enhancing education on both the prevention and treatment of cancer [30, 31].
Several studies have examined the knowledge and behavior of women of reproductive age regarding breast self-examination (SADARI), revealing differences in respondents’ knowledge levels about the routine early detection of breast cancer and the actual implementation of screening behaviors. Respondents who participated in health education programs were more likely to adhere to guidelines for breast cancer detection and screening [32]. Additionally, education level was found to be a significant predictor of self-breast care practices, supported by other research that indicates the influence of health education on women’s knowledge, attitudes, and behaviors related to SADARI in breast cancer prevention [33]. Furthermore, Yusuf et al. [34] highlighted that mobile applications have a positive impact on enhancing women’s knowledge about breast cancer risk factors, awareness of warning signs, and self-confidence regarding breast cancer.
Another specific study on nursing students indicated that knowledge about breast cancer and breast self-examination behaviors is significantly influenced by their trust in the healthcare system [35]. Therefore, it is crucial to enhance preventive intervention programs for all women of reproductive age regarding all aspects of breast cancer, including symptoms and the importance of early detection.
One such intervention program that has been implemented involves the use of technology in breast cancer prevention. Various findings related to the benefits of health technology use have been presented in several studies, including one by Timothy et al. [36], which stated that m-Health applications for breast cancer generally aim to increase awareness, provide cancer-related information, and assist in early detection. Other specific studies have shown that the use of mobile health applications for breast cancer contributes to prevention programs for early detection, as well as improving accessibility to information and education for continuous cancer care.
In another study, the use of breast cancer early detection applications in the intervention group has caused an increase in knowledge and behavior among women of reproductive age. A significant difference in knowledge before and after the intervention in the intervention group, compared to the control group using leaflets, is found to be 44.01%. Additionally, the behavioral analysis indicates its significant effect [37].
Our findings emphasize the importance of using intervention approaches as a method that can positively impact participants’ knowledge enhancement.
This study has several limitations. First, the sample size may not be large enough to represent the broader population of women of reproductive age, which limits the generalizability of the findings. Second, although the mobile application has proven effective in increasing knowledge, this study did not assess long-term knowledge retention or sustained behavioral changes. Future research should consider larger and more diverse sample groups to enhance the external validity of the findings. Additionally, implementing a longitudinal design could help evaluate the long-term impact of the mobile application on behavior change and adherence to breast cancer prevention practices.
Conclusion
The breast cancer risk assessment detection application effectively enhances the knowledge of women of reproductive age regarding breast cancer prevention.
Acknowledgments: We express our gratitude to the Directorate General of the Ministry of Health of the Republic of Indonesia for funding this research, to the Director of Poltekkes Kemenkes Jambi, and the Puskesmas Pakuan Baru and Puskesmas Simpang Kawat in Jambi City for facilitating the study, as well as to all parties involved in this research.
Ethical Permissions: Participants’ privacy is protected, there is no incentive to engage in the study, and registered prospective respondents have signed an informed consent form. The researcher obtained ethical permission before beginning data collection. According to the authors, this study was authorized by the Health Polytechnic of the Ministry of Health in Jambi, under approval number: LB.02.06/2/301/2024.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Nomiko D (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (40%); Bar A (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Monalisa M (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Eliezer B (Fourth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: This research was funded by a grant from the Ministry of Health of the Republic of Indonesia. The funding body had no role in the study’s design, data collection, analysis, interpretation, or manuscript preparation.
Breast cancer is a malignancy originating from breast cells that grow and develop uncontrollably, eventually spreading to surrounding tissues or other parts of the body [1-3]. It is one of the most prevalent types of cancer in Indonesia [4]. According to Globocan data from 2020, breast cancer accounted for 11.5% of all cancer cases worldwide, ranking as the second most common cancer globally, with a mortality rate of 6.9%. In Indonesia, the mortality rate was reported at 16.6 per 100,000 population. If left unchecked, it is projected that by 2030, 26 million individuals will be diagnosed with breast cancer, and 17 million will succumb to the disease [5].
In Indonesia, 80% of breast cancer cases are diagnosed at an advanced stage, with approximately 40% of patients treated at Dharmais Hospital Jakarta already in stages III or IV. The mortality rate for advanced-stage (III-IV) breast cancer is high, with life expectancy rates of 72% and 22%, respectively, leading to a poorer prognosis. Cases diagnosed at this stage are categorized as late-stage breast cancer [6].
Early detection is a crucial first step in identifying the possibility of breast cancer. This process begins with self-examination of the breasts [7, 8]. When early detection efforts are followed by clinical breast examinations, the proportion of advanced-stage cancer cases can be reduced by 50%. Methods for early breast cancer detection include breast self-examination (SADARI), clinical breast examination (SADANIS), and mammography. Among these, SADARI is highly recommended, as 86% of breast lumps are discovered by patients themselves. It is also the most affordable and accessible method, particularly for women of reproductive age [9, 10].
Early detection of breast cancer is strongly recommended to raise awareness among women in their 20s about the risks of breast cancer. Therefore, it is crucial to enhance promotive and preventive efforts through early education programs targeted at women of reproductive age. These initiatives aim to facilitate early intervention and ultimately reduce breast cancer mortality rates [11, 12].
In 2022, researchers conducted a study on the development of a breast cancer education model, which included materials on the concept of breast cancer and strategies for its prevention. Building on this, in 2023, an application was developed that incorporated a breast cancer risk detection feature, named the Deriskara Application. The initial development focused solely on creating and conducting basic field tests of the educational model; however, the evaluation phase has not yet been undertaken. In 2024, researchers plan to proceed to the evaluation stage to assess the application’s effectiveness in enhancing respondents’ cognitive abilities regarding breast cancer prevention. This will be conducted through a quasi-experimental design employing a pre-test-post-test control group approach. This research is particularly critical due to the increasing prevalence of breast cancer, which remains the second leading cause of cancer-related deaths among women worldwide. Early risk assessment for breast cancer is therefore essential. The findings from studies utilizing breast cancer risk assessment tools have proven highly beneficial in clinical management, aiding in service delivery for screening and prevention, as well as predicting an individual’s risk of developing breast cancer. Such tools also support the implementation of risk-based screening policies. The development of a web-based application allows for early detection of potential breast cancer risks, ensuring that women are promptly aware of their condition. This enables them to take timely action before cancer cells spread further in the body [13-15].
Early detection of breast cancer risk and staying informed about the latest advancements in cancer treatment are crucial components of an effective strategy to prevent breast cancer-related deaths. The earlier breast cancer is identified (when the tumor is smaller and less likely to have spread), the higher the chances of successful treatment. Regular screening examinations remain one of the most reliable methods for early detection.
This study aligns with the government’s policy and commitment to controlling non-communicable diseases by promoting innovations in health information technology (e-health and m-health) in Indonesia. To contribute to breast cancer prevention efforts, a readily accessible health information system is essential. In this study, an Android-based breast cancer risk assessment application was developed to address this need.
Materials and Methods
Study design and participants
This quasi-experimental study, conducted in 2024, employed a pre-test-post-test control group approach. The intervention group consisted of women of reproductive age residing in the service area of Puskesmas Simpang Kawat, while the control group included women of reproductive age from the service area of Puskesmas Pakuan Baru. The study population consisted of all women of reproductive age residing in the service areas of Pakuan Baru Health Center and Simpang Kawat Health Center in Jambi City. The sampling method used was random sampling. The total population was determined to be 76 individuals. Using a margin of error of 5% (0.05), the required sample size was calculated using the Slovin formula. Based on the calculation, the sample size for a population of 76 individuals with a 5% margin of error was approximately 64 participants. Thus, a total of 64 respondents were included, with 32 participants in the intervention group and 32 in the control group.
Inclusion and exclusion criteria
The inclusion criteria were respondents who owned and were capable of operating Android-based smartphones, were literate, were willing to participate as respondents, and were able to cooperate. The study was conducted at two different sites, namely Puskesmas Simpang Kawat and Puskesmas Pakuan Baru in Jambi City. Puskesmas Simpang Kawat served as the location for testing the application with the intervention group, while Puskesmas Pakuan Baru was used to evaluate the effectiveness of breast cancer education using a pocketbook with the control group.
Data collection
The research process involved several key stages, including obtaining licensing and ethical clearance, developing the application, mapping and selecting the sample, obtaining informed consent, providing education on how to use the application, conducting a pre-test, performing breast cancer screening, delivering breast cancer education, and administering a post-test.
Data collected included respondents’ demographic information and knowledge about breast cancer, which were gathered through interviews and observations. The tools used included questionnaires, pocketbooks, and smartphones. During the data collection phase, two enumerators, who had been trained to ensure data quality and consistency, assisted the researcher.
Research tools
The Knowledge Questionnaire consisted of 15 items, designed to measure respondents’ knowledge about breast cancer prevention in women of reproductive age. The questionnaire was the same for both study groups, ensuring consistent comparison between the groups. Some examples of questions included in the questionnaire were risk factors that can increase the likelihood of breast cancer, the correct way to perform breast self-examination (BSE), the ideal frequency of performing BSE, early signs of breast cancer to watch out for, and the benefits of regular clinical breast examinations (CBE). Additionally, the questionnaire covered topics, such as a healthy lifestyle to prevent cancer, the relationship between high-fat diets and cancer risk, the contribution of physical activity to cancer prevention, as well as the benefits of breastfeeding and early cancer detection. Other questions addressed the impact of family history, alcohol consumption, smoking, chemical exposure, and the importance of breast health education. The questionnaire was developed based on relevant literature, underwent validity and reliability testing, and demonstrated excellent reliability with a Cronbach’s Alpha score of 0.87.
The control group was provided with education using a pocketbook containing material on breast cancer prevention, while the intervention group received education through a smartphone equipped with an application that provided information on breast cancer prevention. The material presented in the pocketbook and the smartphone application was designed to deliver comprehensive and relevant information related to breast cancer prevention. Both the pocketbook and the smartphone application served as the primary sources for developing the knowledge questionnaire used to assess respondents’ understanding. This approach ensured that the educational material provided was aligned with the knowledge assessment instrument, allowing the results to accurately reflect the effectiveness of each educational method.
Data analysis
Data analysis was performed in two descriptive and inferential analysis stages. Descriptive analysis was used to examine changes in knowledge scores before and after the intervention in both study groups.
Inferential analysis began with a data distribution test using the Kolmogorov-Smirnov test to confirm that the data were normally distributed. Once normality was established, a paired t-test was used to assess the difference in scores before and after the intervention within each group. Additionally, an independent t-test was conducted to compare the mean post-intervention scores between the intervention and control groups. Data processing and analysis were conducted using SPSS version 23.0.
Findings
The majority of participants in both groups were approximately the same average age, around 36 years (intervention and control groups: 35.720±8.803 and 35.970±8.499 years, respectively). Most participants had a high school education, with a higher proportion in the intervention group (68.8%) compared to the control group (34.7%). Regarding occupation, the majority were housewives, particularly in the control group (81.2%), while the intervention group had a broader range of occupations, including traders/self-employed individuals (15.6%) and civil servants/teachers/lecturers (12.5%). Most participants in both groups were married (90.6%; Table 1).
Table 1. Frequency of respondents’ characteristics
In the control group, the pre-test mean knowledge level score was 10.750±1.344, which increased to 11.500±1.368 in the post-test (p=0.0001), indicating a statistically significant improvement. In the intervention group, the pre-test mean score was 10.940±1.865, which rose more substantially to 13.380±1.314 at the post-test (p=0.0001). Also, the mean knowledge score in the intervention group was 13.380±1.314, with a 95% confidence interval of 1.205-2.545. In contrast, the control group had a lower mean knowledge score of 11.500±1.368. The difference in knowledge scores between the two groups was statistically significant (p=0.0001).
Discussion
This study aimed to assess the effectiveness of an Android-based breast cancer risk assessment application in enhancing the knowledge of women of reproductive age regarding breast cancer prevention. Breast cancer is a disease characterized by uncontrolled changes in breast tissue cells, often originating from the milk lobules in the ducts. Risk factors for breast cancer are classified into non-modifiable and modifiable factors [16]. Non-modifiable factors include age, gender, race, and family history, while modifiable factors include pregnancy and breastfeeding, hormone therapy, obesity, physical activity, oral contraceptive use, exposure to radiation during breast development, a history of benign tumors, alcohol consumption, smoking, and the intake of fat and red meat [17, 18].
Breast cancer prevention and control programs focus on identifying risk factors and implementing strategies to avoid them through three levels of prevention: primary, secondary, and tertiary. Screening and early detection fall under secondary prevention, which aims to identify pre-cancerous conditions and cancer at an early stage [19, 20]. Early detection of breast cancer involves identifying the disease at its earliest stages, enabling treatment with techniques that have less physical impact and offer a greater chance of recovery. When treated appropriately, the cure rate for breast cancer is quite high (80%-90%), whether through screening or early detection [21].
The principles of screening include, first, that the disease should be severe, relatively common, and recognized as a public health issue by the community. Second, screening should be safe and acceptable to the public [22, 23]. The screening process requires the participation of individuals who are considered appropriate candidates for screening. Third, screening must be accurate and reliable [24].
Early detection of breast cancer aims to identify the disease at its earliest stages, allowing for treatment with techniques that have less physical impact and offer a greater chance of recovery. When treated appropriately, the cure rate for breast cancer is relatively high (80%-90%), whether through screening or early detection. Early discovery is also a strategy for downstaging the disease, beginning with raising public awareness about changes in breast shape or abnormalities. Promoting the SADARI program is essential, as 85% of breast abnormalities are first recognized by the patients themselves [25].
One approach used in the intervention program is the incorporation of technology for breast cancer prevention. The research team developed a breast cancer risk detection application module, targeting women of childbearing age as the primary users. This social network mobile application delivers educational materials about breast cancer through videos, texts, and images, thereby increasing awareness of the disease [26-28].
Various studies have highlighted the benefits of using health technology, particularly through m-Health applications. These studies demonstrate that the use of technology in breast cancer prevention primarily aims to increase awareness about cancer, provide relevant information, and assist in early detection. One study, for example, showed a substantial increase in the average knowledge score, suggesting that mobile applications can be effective tools for disseminating health information.
The use of technology in breast cancer prevention has been explored in several related studies. For example, according to Prochaska et al. [29], the application of technology through m-Health applications in breast cancer typically aims to raise awareness about the disease, provide cancer-related information, and assist in early detection. Other specific research findings have shown that the use of mobile health applications in breast cancer has significantly contributed to early detection programs while also improving accessibility to information and education for ongoing cancer care. Mobile applications offer a mechanism for enhancing education on both the prevention and treatment of cancer [30, 31].
Several studies have examined the knowledge and behavior of women of reproductive age regarding breast self-examination (SADARI), revealing differences in respondents’ knowledge levels about the routine early detection of breast cancer and the actual implementation of screening behaviors. Respondents who participated in health education programs were more likely to adhere to guidelines for breast cancer detection and screening [32]. Additionally, education level was found to be a significant predictor of self-breast care practices, supported by other research that indicates the influence of health education on women’s knowledge, attitudes, and behaviors related to SADARI in breast cancer prevention [33]. Furthermore, Yusuf et al. [34] highlighted that mobile applications have a positive impact on enhancing women’s knowledge about breast cancer risk factors, awareness of warning signs, and self-confidence regarding breast cancer.
Another specific study on nursing students indicated that knowledge about breast cancer and breast self-examination behaviors is significantly influenced by their trust in the healthcare system [35]. Therefore, it is crucial to enhance preventive intervention programs for all women of reproductive age regarding all aspects of breast cancer, including symptoms and the importance of early detection.
One such intervention program that has been implemented involves the use of technology in breast cancer prevention. Various findings related to the benefits of health technology use have been presented in several studies, including one by Timothy et al. [36], which stated that m-Health applications for breast cancer generally aim to increase awareness, provide cancer-related information, and assist in early detection. Other specific studies have shown that the use of mobile health applications for breast cancer contributes to prevention programs for early detection, as well as improving accessibility to information and education for continuous cancer care.
In another study, the use of breast cancer early detection applications in the intervention group has caused an increase in knowledge and behavior among women of reproductive age. A significant difference in knowledge before and after the intervention in the intervention group, compared to the control group using leaflets, is found to be 44.01%. Additionally, the behavioral analysis indicates its significant effect [37].
Our findings emphasize the importance of using intervention approaches as a method that can positively impact participants’ knowledge enhancement.
This study has several limitations. First, the sample size may not be large enough to represent the broader population of women of reproductive age, which limits the generalizability of the findings. Second, although the mobile application has proven effective in increasing knowledge, this study did not assess long-term knowledge retention or sustained behavioral changes. Future research should consider larger and more diverse sample groups to enhance the external validity of the findings. Additionally, implementing a longitudinal design could help evaluate the long-term impact of the mobile application on behavior change and adherence to breast cancer prevention practices.
Conclusion
The breast cancer risk assessment detection application effectively enhances the knowledge of women of reproductive age regarding breast cancer prevention.
Acknowledgments: We express our gratitude to the Directorate General of the Ministry of Health of the Republic of Indonesia for funding this research, to the Director of Poltekkes Kemenkes Jambi, and the Puskesmas Pakuan Baru and Puskesmas Simpang Kawat in Jambi City for facilitating the study, as well as to all parties involved in this research.
Ethical Permissions: Participants’ privacy is protected, there is no incentive to engage in the study, and registered prospective respondents have signed an informed consent form. The researcher obtained ethical permission before beginning data collection. According to the authors, this study was authorized by the Health Polytechnic of the Ministry of Health in Jambi, under approval number: LB.02.06/2/301/2024.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Nomiko D (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (40%); Bar A (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Monalisa M (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (20%); Eliezer B (Fourth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: This research was funded by a grant from the Ministry of Health of the Republic of Indonesia. The funding body had no role in the study’s design, data collection, analysis, interpretation, or manuscript preparation.
Article Type: Original Research |
Subject:
Technology of Health Education
Received: 2025/01/1 | Accepted: 2025/01/30 | Published: 2025/02/3
Received: 2025/01/1 | Accepted: 2025/01/30 | Published: 2025/02/3
References
1. Sant M, Bernat-Peguera A, Felip E, Margelí M. Role of ctDNA in breast cancer. Cancers. 2022;14(2):310. [Link] [DOI:10.3390/cancers14020310]
2. Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, et al. Breast cancer. Nat Rev Dis Primers. 2019;5(1):66. [Link] [DOI:10.1038/s41572-019-0111-2]
3. Moo TA, Sanford R, Dang C, Morrow M. Overview of breast cancer therapy. PET Clin. 2018;13(3):339-54. [Link] [DOI:10.1016/j.cpet.2018.02.006]
4. Lestari P, Wulansari W. The importance of breast self-examination (be aware) as an effort to detect breast cancer early. Indones J Community Empower. 2019;1(2). [Indonesian] [Link]
5. UICC. GLOBOCAN 2020: New global cancer data [Internet]. Geneva: :union: for International Cancer Control; 2020 [cited 2024, November, 20]. Available from: https://www.uicc.org/news/globocan-2020-global-cancer-data. [Link]
6. RSK DHARMAIS. Is it important to detect breast cancer early? [Internet]. Jakarta: KEMENKES RSK DHARMAIS; 2024 [cited 2024, November, 20]. Available from: https://dharmais.co.id/news/653/Pentingkah-Deteksi-Dini-Kanker-Payudara. [Indonesian] [Link]
7. Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biol Res. 2017;50(1):33. [Link] [DOI:10.1186/s40659-017-0140-9]
8. Amila A, Sinuraya E, Gulo ARB. Awareness education (breast self-examination) for early detection of breast cancer in Medan high school students. JURNAL ABDIMAS MUTIARA. 2020;1(2):29-40. [Indonesian] [Link]
9. Ginsburg O, Yip C, Brooks A, Cabanes A, Caleffi M, Dunstan Yataco JA, et al. Breast cancer early detection: A phased approach to implementation. Cancer. 2020;126(Suppl 10):2379-93. [Link] [DOI:10.1002/cncr.32887]
10. Milosevic M, Jankovic D, Milenkovic A, Stojanov D. Early diagnosis and detection of breast cancer. Technol Health Care. 2018;26(4):729-59. [Link] [DOI:10.3233/THC-181277]
11. Provencher L, Hogue JC, Desbiens C, Poirier B, Poirier E, Boudreau D, et al. Is clinical breast examination important for breast cancer detection?. Curr Oncol. 2016;23(4):e332-9. [Link] [DOI:10.3747/co.23.2881]
12. Migowski A, Dias MBK, Diz MDPE, Sant'Ana DR, Nadanovsky P. Guidelines for early detection of breast cancer in Brazil. II-New national recommendations, main evidence, and controversies. CADERNOS DE SAUDE PUBLICA. 2018;34(6):e00074817. [Portuguese] [Link] [DOI:10.1590/0102-311x00074817]
13. Manjuri S, Gill SS. Machine learning-based web application for breast cancer prediction. In: Applications of AI for interdisciplinary research. Boca Raton: CRC Press; 2024. [Link] [DOI:10.1201/9781003467199-6]
14. Nugroho A, Fauzi A, Sunarko B, Wibawanto H, Mulwinda A, Iksan N. Web based application system for cancerous object detection in ultrasound images. AIP Conf Proc. 2023;2727(1):040023. [Link] [DOI:10.1063/5.0141519]
15. Ma Z, Shi Y, Yao S, Lu N, Cheng F. Effectiveness of telemedicine-based psychosocial intervention for breast cancer patients: A systematic review and meta-analysis. Support Care Cancer. 2023;31(10):595. [Link] [DOI:10.1007/s00520-023-08052-3]
16. Maas P, Barrdahl M, Joshi AD, Auer PL, Gaudet MM, Milne RL, et al. Breast cancer risk from modifiable and nonmodifiable risk factors among white women in the United States. JAMA Oncol. 2016;2(10):1295-302. [Link] [DOI:10.1001/jamaoncol.2016.1025]
17. Hashemi SM, Rafiemanesh H, Aghamohammadi T, Badakhsh M, Amirshahi M, Sari M, et al. Prevalence of anxiety among breast cancer patients: A systematic review and meta-analysis. Breast Cancer. 2020;27(2):166-78. [Link] [DOI:10.1007/s12282-019-01031-9]
18. Rojas K, Stuckey A. Breast cancer epidemiology and risk factors. Clin Obstet Gynecol. 2016;59(4):651-72. [Link] [DOI:10.1097/GRF.0000000000000239]
19. Niell BL, Freer PE, Weinfurtner RJ, Arleo EK, Drukteinis JS. Screening for breast cancer. Radiol Clin North Am. 2017;55(6):1145-62. [Link] [DOI:10.1016/j.rcl.2017.06.004]
20. McKinney SM, Sieniek M, Godbole V, Godwin J, Antropova N, Ashrafian H, et al. International evaluation of an AI system for breast cancer screening. Nature. 2020;577(7788):89-94. [Link] [DOI:10.1038/s41586-019-1799-6]
21. Da Costa Vieira RA, Biller G, Uemura G, Ruiz CA, Curado MP. Breast cancer screening in developing countries. Clinics. 2017;72(4):244-53. [Link] [DOI:10.6061/clinics/2017(04)09]
22. Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. Breast cancer screening and diagnosis: A synopsis of the European breast guidelines. Ann Intern Med. 2020;172(1):46-56. [Link] [DOI:10.7326/M19-2125]
23. Seely JM, Alhassan T. Screening for breast cancer in 2018-what should we be doing today?. Curr Oncol. 2018;25(Suppl 1):115-24. [Link] [DOI:10.3747/co.25.3770]
24. Waks AG, Winer EP. Breast cancer treatment: A review. JAMA. 2019;321(3):288-300. [Link] [DOI:10.1001/jama.2018.19323]
25. Chetlen A, Mack J, Chan T. Breast cancer screening controversies: Who, when, why, and how?. Clin Imaging. 2016;40(2):279-82. [Link] [DOI:10.1016/j.clinimag.2015.05.017]
26. Al Husaini MAS, Hadi Habaebi M, Gunawan TS, Islam MR. Self-detection of early breast cancer application with infrared camera and deep learning. Electronics. 2021;10(20):2538. [Link] [DOI:10.3390/electronics10202538]
27. Suprapto, Anita KW. Breast cancer screening application based on Android with the certainty factor method. IAIC Int Conf Ser. 2023;4(1):88-96. [Link] [DOI:10.34306/conferenceseries.v4i1.633]
28. Peristiowati Y, Hariyono, Arantrinita. Socialization and early detection of breast cancer using the Android application "MamoApp". J Community Engagem Health. 2024;7(2):131-40. [Link] [DOI:10.30994/jceh.v7i2.617]
29. Prochaska JJ, Coughlin SS, Lyons EJ. Social media and mobile technology for cancer prevention and treatment. Am Soc Clin Oncol Educ Book. 2017;37:128-37. [Link] [DOI:10.1200/EDBK_173841]
30. Gatuha G, Jiang T. Android based naive Bayes probabilistic detection model for breast cancer and mobile cloud computing: Design and implementation. Int J of Eng Res Afr. 2016;21:197-208. [Link] [DOI:10.4028/www.scientific.net/JERA.21.197]
31. Aprianti S, Erika, Kurniawan D. Effect of breast cancer detection application on improving knowledge of early detection of breast cancer (BSE) among adolescents. Int J Nurs Health Serv. 2022;5(5):437-45. [Link]
32. Wu TY, Lee J. Promoting breast cancer awareness and screening practices for early detection in low-resource settings. Eur J Breast Health. 2018;15(1):18-25. [Link] [DOI:10.5152/ejbh.2018.4305]
33. Prabarini LP, Abi Muhlisin SKM. The influence of peer group method breast cancer health education on the level of knowledge, attitudes and conscious behavior of pkk mothers in Karangasem subdistrict [dissertation]. Surakarta: Muhammadiyah University of Surakarta; 2017. [Indonesian] [Link]
34. Yusuf A, Yulita YH, Ab Hadi IS, Nasution A, Lean Keng S. Breast awareness mobile apps for health education and promotion for breast cancer. Front Public Health. 2022;10:951641. [Link] [DOI:10.3389/fpubh.2022.951641]
35. Erbil N, Dundar N, Inan C, Bolukbas N. Breast cancer risk assessment using the Gail model: A Turkish study. Asian Pac J Cancer Prev. 2015;16(1):303-6. [Link] [DOI:10.7314/APJCP.2015.16.1.303]
36. Timothy W, Collins Danielle X, Morales SEG. Neonatal rat myocardial extraction. Physiol Behav. 2016;176(1):139-48. [Chinese] [Link]
37. Alam N, Wirakusumah FF, Soepardan S. Knowledge and application-based awareness behavior for early detection of breast tumors in women of childbearing age. JURNAL ILMIAH KESEHATAN. 2021;13(1):95-103. [Indonesian] [Link] [DOI:10.37012/jik.v13i1.441]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






