Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 13-19 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
AlHasni N, Ayaad O, Al-Awaisi H, Ibrahim R, Al Faliti B, AlMadhoun E et al . Correlation between Innovation Practices and Occupational Fatigue in Healthcare Professionals. Health Educ Health Promot 2025; 13 (1) :13-19
URL: http://hehp.modares.ac.ir/article-5-78761-en.html
URL: http://hehp.modares.ac.ir/article-5-78761-en.html
N.S. AlHasni1, O. Ayaad *2, H.S. Al-Awaisi1, R.A. Ibrahim2, B.H.S. Al Faliti2, E.T. AlMadhoun3, K. Al-Baimani4
1- “Department of Nursing” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
2- “Department of Quality and Accreditation” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
3- “Department of Pharmacy,” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
4- “Department of Medical Oncology” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
2- “Department of Quality and Accreditation” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
3- “Department of Pharmacy,” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
4- “Department of Medical Oncology” and “Sultan Qaboos Comprehensive Cancer Care and Research Centre (SQCCCRC)”, University Medical City, Muscat, Oman
Keywords: Organizational Innovation [MeSH], Occupational Health [MeSH], Fatigue [MeSH], Leadership [MeSH]
Full-Text [PDF 602 kb]
(483 Downloads)
| Abstract (HTML) (582 Views)
Full-Text: (4 Views)
Introduction
Innovation practices in healthcare refer to the structured implementation of new ideas, processes, and technologies to improve service delivery, patient care, and organizational efficiency [1]. These practices are increasingly critical in addressing complex challenges within healthcare systems, such as rising patient demands and resource constraints. The healthcare ecosystem relies on innovation to foster adaptive responses, ensuring long-term sustainability and effectiveness [2].
Innovation in healthcare operates across various domains that collectively enable its adoption and effectiveness. Key domains include organizational values and culture, which form the foundational mindset for embracing innovation, leadership behaviors, which drive and inspire innovative actions, resource allocation, which ensures the availability of tools and funding for innovation, process innovation, which focuses on improving workflows and clinical procedures, and stakeholder engagement, which integrates perspectives from patients, providers, and external partners [3]. Together, these domains form an integrated framework that supports and sustains innovation in healthcare systems.
The outcomes of innovative practices in healthcare are substantial, ranging from enhanced patient outcomes to improved operational effectiveness and efficiency, as well as increased staff experience and satisfaction. Innovation also fosters a competitive advantage, enabling organizations to stay ahead in a rapidly evolving environment [4]. However, various factors influence the success of innovation, including organizational structure, leadership support, resource availability, and workforce well-being. Among these, occupational fatigue is a significant yet underexplored factor that can hinder the ability to engage in and sustain innovative practices [5].
Fatigue is a multidimensional condition defined as a state of physical, psychosocial, emotional, and mental exhaustion resulting from exposure to any work-related stressors [5]. It is particularly prevalent in healthcare due to the high demands of patient care, long hours, and the emotional strain associated with critical decision-making and outcomes. If left unaddressed, fatigue can significantly impair healthcare professionals’ performance and well-being [6].
The domains of fatigue include physical fatigue, characterized by bodily exhaustion and reduced physical capacity; mental fatigue, which involves diminished cognitive and decision-making abilities; sleep-related fatigue, resulting from inadequate or poor-quality sleep; and shift-related fatigue, associated with irregular or prolonged work schedules [7]. Each of these domains has specific implications for healthcare delivery, particularly in high-intensity settings such as oncology.
The impacts of occupational fatigue are far-reaching and detrimental. Fatigue compromises individual performance, leading to increased medical errors, reduced productivity, and diminished job satisfaction [8]. It also affects organizational outcomes, including decreased innovation adoption, poor teamwork, and lower overall quality of care. Fatigue inhibits creativity, impairs problem-solving abilities, and reduces engagement in innovation processes, all of which are critical in healthcare environments that demand adaptability and efficiency [6].
Despite the recognized impacts of fatigue and the importance of innovation, limited research has examined the correlation between innovation practices and occupational fatigue in healthcare settings. While existing studies have explored individual aspects of innovation or fatigue, there remains a gap in understanding how fatigue directly influences innovation adoption, particularly in oncology settings where the intensity of work and the need for innovation are exceptionally high [5].
The lack of research on this topic underscores the need for studies that investigate the interplay between occupational fatigue and innovation. By addressing this gap, healthcare organizations can better understand how to mitigate fatigue and support innovation, ultimately improving patient outcomes and workforce satisfaction.
The significance of this study lies in its potential to provide actionable insights into the barriers and facilitators of innovation in high-intensity healthcare settings. Understanding the correlation between fatigue and innovation will help identify strategies to promote resilience, reduce burnout, and foster a culture of creativity and collaboration among healthcare professionals [9, 10]. The purpose of this study was to examine the relationship between innovation practices and occupational fatigue among healthcare professionals in oncology settings.
Instrument and Methods
Setting
This cross-sectional study was conducted at the Sultan Qaboos Comprehensive Cancer Center (SQCCC), University Medical City, in Muscat, Oman in 2024. SQCCC, known for its advanced oncology treatments and technologies, is a new center that provides an ideal environment for exploring innovation practices and occupational fatigue among healthcare professionals. The center’s reputation for cutting-edge cancer care, its diverse multidisciplinary team, its cultural context, and its supportive research environment make it a fitting location for this research.
A cross-sectional design was utilized to collect information as a snapshot of the current state of innovation practices and occupational fatigue among healthcare professionals at SQCCC. This design allowed for data collection at a single point in time, facilitating the inclusion of diverse participant perspectives from different roles within the center. The feasibility, efficiency, and analytical versatility of a cross-sectional study made it a suitable approach for this busy healthcare setting.
Sample
The study involved a sample of 163 clinical staff recruited using convenience sampling. Participants were required to have at least six months of experience at the Sultan Qaboos Comprehensive Cancer and Research Center to ensure familiarity with the work environment and exposure to its practices. With a 90% confidence level and a margin of error of 0.05, the minimum sample size required was 161 participants.
Instrument
We used a self-reported questionnaire consisting of three sections. The demographics section gathered basic participant information. The occupational fatigue section utilized the “Fatigue Risk Assessment and Management in High-Risk Environments (FRAME)” instrument, which measured physical, mental, sleep, and shift-related fatigue using 26 items on a five-point Likert scale [8, 11]. The innovation survey section was developed from the “Culture of Innovation Survey,” which was validated for the healthcare context to measure perceptions of innovation practices [12, 13].
The questionnaire used demonstrated strong reliability and validity metrics. The Cronbach’s alpha test ranged from 0.82 to 0.88 for the different sections of the questionnaire, indicating good reliability across all domains. The construct validity was tested through factor analysis. The Kaiser-Meyer-Olkin (KMO) value was calculated and showed a result of 0.85. Bartlett’s test of sphericity yielded a significant result (p<0.05), confirming that the questionnaire items effectively represented the underlying constructs of occupational fatigue and innovation practices.
Data collection
Upon receiving ethical approval from SQCCC’s Institutional Review Board (IRB), participants were recruited via invitation letters distributed through the center’s internal email system. Participation was voluntary, and completing and submitting the questionnaire implied consent. Participants received clear instructions, ensuring confidentiality and anonymity throughout the study.
Data analysis
Descriptive statistics, such as means, frequencies, and standard deviations were used to provide a summary overview of the data collected. Correlation analyses were conducted using Pearson’s correlation coefficient to identify significant associations. To identify differences in study innovation practices and occupational fatigue according to demographics, independent samples t-tests were used, with a p-value significance level set at <0.05. All statistical analyses were performed using SPSS version 23.
Data availability: The data supporting the findings of this study are available upon reasonable request from the corresponding author. Restrictions apply to the availability of these data due to ethical and confidentiality considerations.
Findings
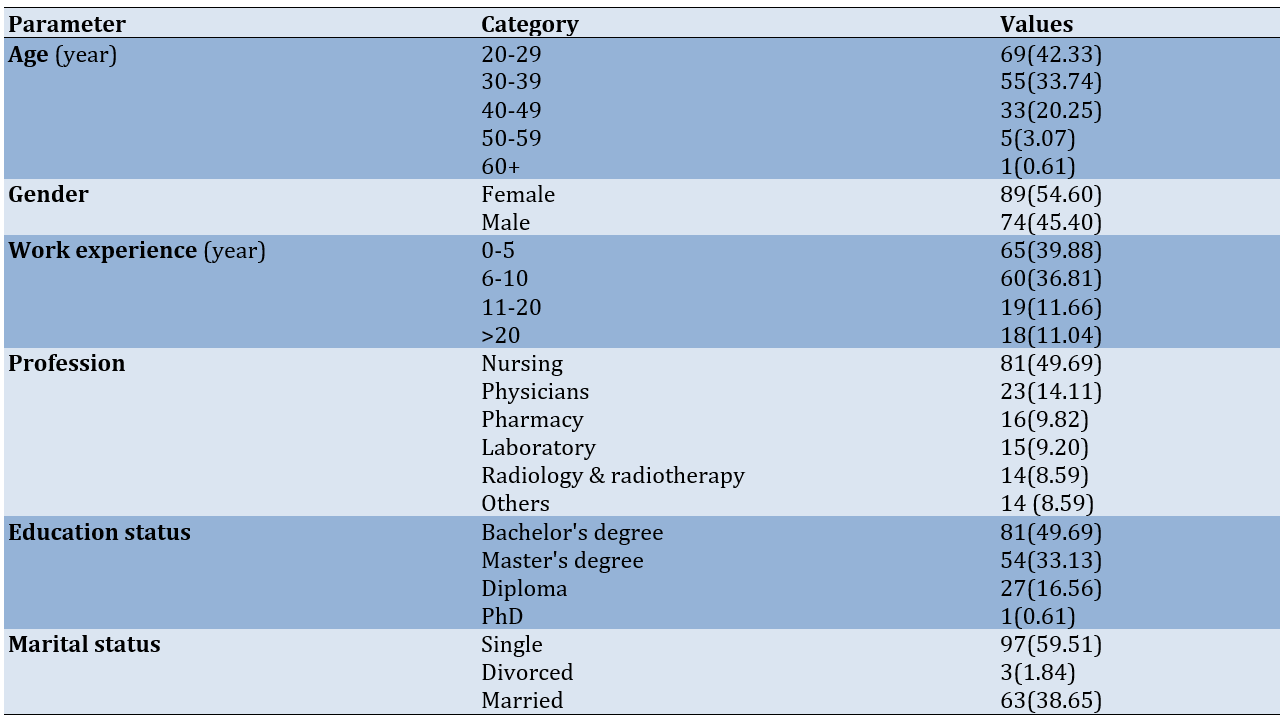
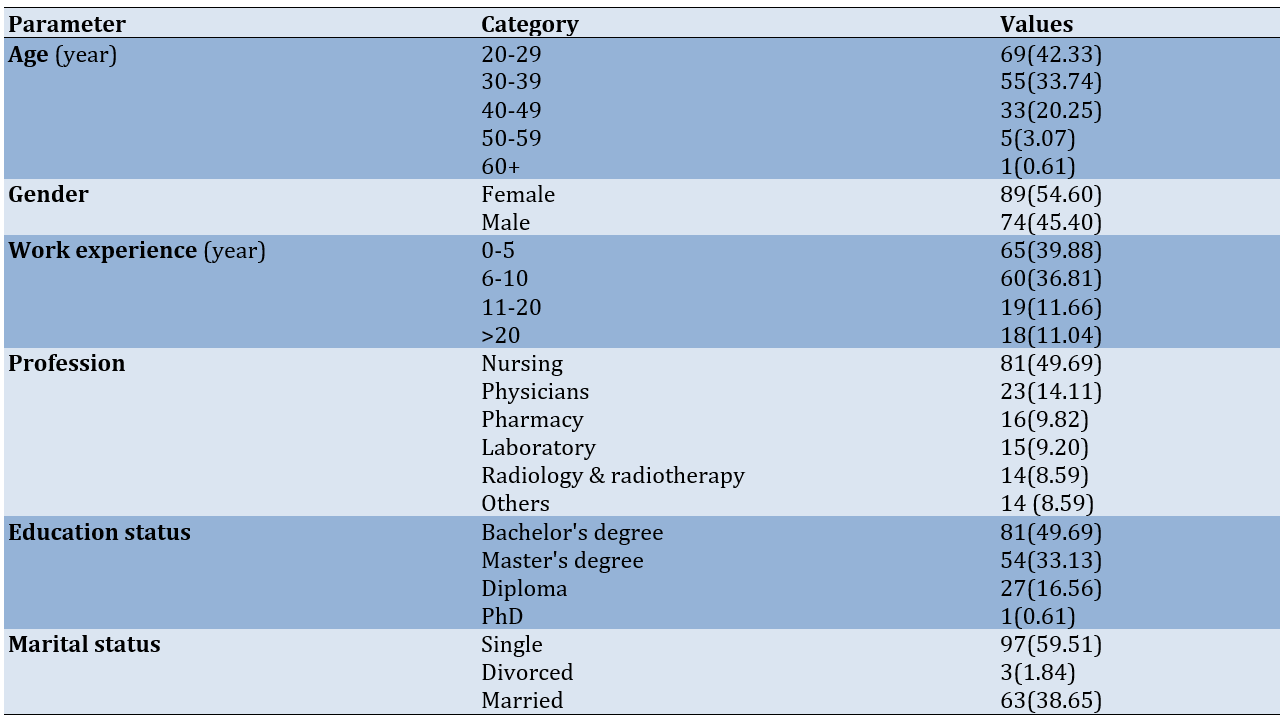
The sample consisted of 163 clinical staff, primarily younger individuals, with the largest age group being 20-29 years. Females made up a slightly larger proportion of the sample compared to males. Most participants had between 0-5 years of total experience (n=65, 39.88%). Professionally, nearly half were nurses (n=81, 49.69%). Educationally, most held a bachelor’s degree (n=81, 49.69%). In terms of marital status, the majority were single (n=97, 59.51%; Table 1).
Table 1. Frequency of samples’ demographics
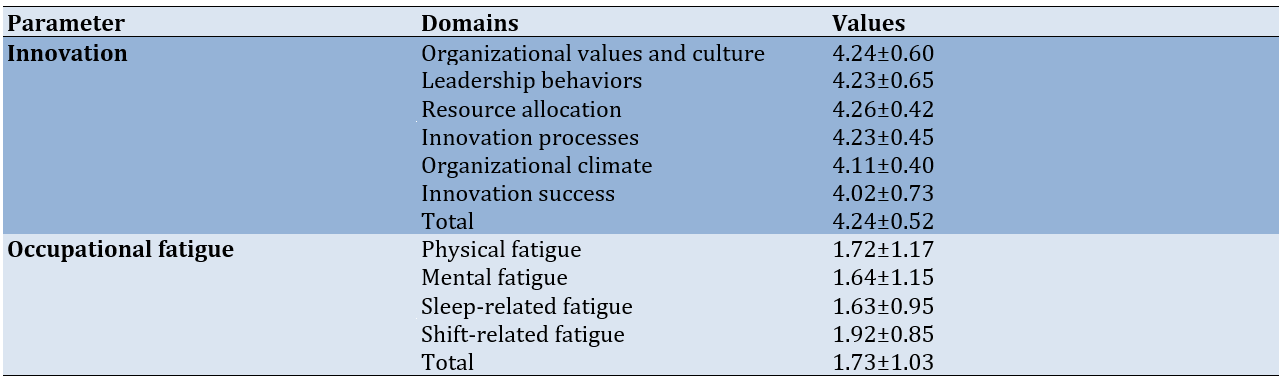
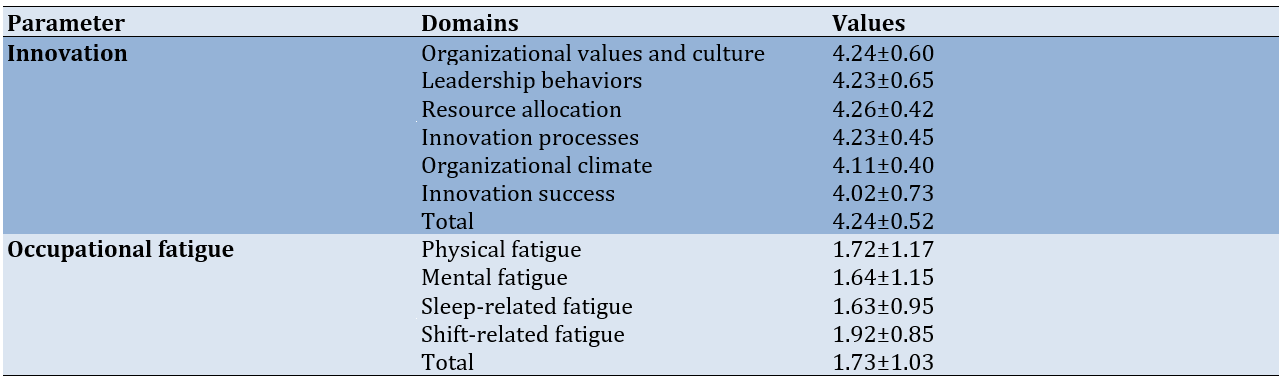
For innovation, the mean scores ranged from 4.02 to 4.26, with an overall mean of 4.24±0.52. In contrast, the domains of occupational fatigue had lower mean scores, ranging from 1.63 to 1.92, with an overall mean of 1.73±1.03 (Table 2).
Table 2. Mean scores of innovation practices and occupational fatigue
The correlation results showed the relationships between the total mean scores of innovation and occupational fatigue. A significant negative correlation was found between innovation and occupational fatigue (r=-0.68, p=0.045), indicating that higher levels of innovation are associated with lower levels of occupational fatigue.
There was a negative correlation between various domains of occupational fatigue and innovation. Specifically, physical fatigue (r=-0.55, p=0.045), mental fatigue (r=-0.60, p=0.041), sleep-related fatigue (r=-0.58, p=0.050), and shift-related fatigue (r=-0.62, p=0.048) all exhibit significant negative correlations with innovation.
All innovation domains had a negative relationship with occupational fatigue. Specifically, leadership behaviors exhibited the strongest negative correlation with occupational fatigue (r=-0.62, p=0.035).
Similarly, innovation processes (r=-0.60, p=0.040) and organizational climate (r=-0.59, p=0.039) also showed strong negative correlations, implying that occupational fatigue hampers the effectiveness of these domains. Other domains, including organizational values and culture (r=-0.58, p=0.042), innovation success (r=-0.57, p=0.041), and resource allocation (r=-0.55, p=0.045), demonstrated a similar pattern, where higher fatigue levels correlated with a decline in innovative capacity.
In terms of innovation, individuals over 40 years old scored significantly lower compared to those aged 20-40 (p=0.038). Experience also played a role, with those having over ten years of experience reporting significantly higher levels of innovation compared to less experienced individuals (p=0.032). Notably, physicians (p=0.029) and those with a master’s degree (p=0.029) or PhD (p=0.022) also scored higher in innovation compared to their counterparts.
For occupational fatigue, those aged over 40 reported significantly higher fatigue levels compared to younger participants (p=0.045). Participants with over ten years of experience reported significantly lower levels of occupational fatigue (p=0.027), while physicians experienced significantly less fatigue compared to nurses (p=0.031). Additionally, individuals with a master’s degree (p=0.035) or PhD (p=0.029) reported lower occupational fatigue compared to those with a bachelor’s degree (Table 3).
Table 3. Differences in innovation practices and occupational fatigue according to demographics

Discussion
The purpose of the study was to examine the relationship between innovation practices and occupational fatigue among healthcare professionals in oncology settings. The demographic composition of the study sample, predominantly younger professionals aged 20-39, suggests that the workforce in this oncology setting comprises a relatively inexperienced yet dynamic group. This demographic pattern is consistent with the global trend of younger professionals entering healthcare due to increased educational opportunities and the sector’s demand for a fresh workforce [4]. Their limited professional experience (0-10 years for most) may influence their perceptions of innovation and occupational fatigue. Early-career professionals are often more adaptable and open to innovation but may also lack the coping strategies required to manage workplace fatigue effectively [14, 15].
The predominance of female participants reflects the gender distribution commonly observed in healthcare professions, especially nursing, which constituted nearly half of the sample. Female healthcare workers often face unique challenges, including balancing professional responsibilities with personal and family obligations, which may contribute to higher fatigue levels [5]. The slightly larger proportion of female participants aligns with studies showing that women are more represented in nursing and other supportive healthcare roles [15, 16].
The educational profile of participants, with the majority holding bachelor’s or master’s degrees, indicates a highly qualified workforce. Advanced education levels correlate with better knowledge of and engagement in innovation practices [1, 17]. However, the underrepresentation of professionals with doctoral degrees suggests potential limitations in research capacity and leadership for driving significant innovation within this setting [16].
We found a high level of perceived innovation across domains, with resource allocation scoring the highest. This result highlights the importance of sufficient resources in fostering innovation, as access to funding, technology, and time enables healthcare professionals to experiment with and implement new ideas [4, 6]. Leadership behaviors and organizational values also score highly, emphasizing the role of supportive leadership and a culture conducive to innovation [3, 7].
Occupational fatigue was relatively low overall, with shift-related fatigue being the most prominent domain. This finding aligns with previous research indicating that shift work disrupts circadian rhythms and sleep patterns, leading to increased fatigue [6, 16]. Sleep-related fatigue was the lowest, possibly due to institutional policies supporting adequate rest or flexible schedules. However, the cumulative effects of other fatigue domains may still impact professionals’ overall capacity to innovate [5, 17]. We revealed a significant negative correlation between occupational fatigue and innovation. This relationship suggests that fatigue diminishes professionals’ ability to engage in innovative practices, likely due to reduced cognitive capacity, creativity, and motivation. The strongest negative correlations were observed in leadership behaviors and organizational climate, emphasizing how fatigue impacts roles that require decision-making and fostering collaborative environments [16, 18].
The demographic findings further elucidated this relationship. Participants over 40 years old reported higher fatigue levels and lower innovation scores, reflecting the cumulative physical and mental strain experienced by older professionals [13, 19]. In contrast, younger participants displayed higher innovation scores, possibly due to greater familiarity with new technologies and openness to change [4, 15].
Interestingly, professionals with over ten years of experience reported lower fatigue levels and higher innovation scores, suggesting that experience equips individuals with better coping mechanisms and a deeper understanding of institutional processes [17]. In contrast, less experienced staff may face challenges adapting to demanding healthcare environments, which affects their capacity for innovation [15, 20].
The significant differences among professions highlight the unique challenges and opportunities within each role. Nurses reported the highest levels of fatigue, consistent with their physically and emotionally demanding duties [14]. Physicians, on the other hand, exhibit higher innovation scores and lower fatigue levels, possibly due to greater autonomy and decision-making power in their roles [16].
Education level also influenced the results, with master’s and doctorate holders displaying higher innovation scores and lower fatigue levels. Advanced education may provide these professionals with better tools to manage stress and engage in innovative practices effectively [21]. Bachelor’s degree holders, who form the majority, showed moderate levels of innovation and fatigue, reflecting their critical role in daily operations without the strategic insights afforded by higher qualifications [22, 23].
Marital status played a minor role, with single participants exhibiting slightly higher innovation scores, possibly due to fewer personal commitments. However, the differences were not substantial, indicating that marital status alone does not significantly influence innovation or fatigue [6, 7].
The correlation matrix underscores the detrimental impact of fatigue on innovation across all domains. Resource allocation and organizational climate, which are key enablers of innovation, were particularly affected, demonstrating that fatigue compromises both the operational and cultural foundations necessary for fostering innovation [3, 7]. The findings emphasize the need for targeted interventions to mitigate occupational fatigue and promote innovation. Strategies such as workload optimization, shift scheduling reforms, and leadership training can significantly enhance both workforce well-being and organizational performance [17, 24].
This study has several limitations. First, the relatively small sample size of 163 participants may limit the generalizability of the results to other oncology settings or healthcare institutions. Larger, more diverse samples would provide a broader perspective and enhance the reliability of the findings. Additionally, the study was conducted in a new specialized cancer center, which may not reflect the practices and challenges present in other healthcare settings, such as primary care or general hospitals.
Second, the use of convenience sampling might have introduced selection bias. Staff who voluntarily chose to participate may differ in their experiences or perceptions of innovation and fatigue compared to those who did not participate. Furthermore, the cross-sectional design captures only a snapshot of the relationship between occupational fatigue and innovation, limiting the ability to infer causality.
Future studies should expand the sample size and include participants from diverse healthcare settings. Comparative studies across different institutions or geographic regions could offer insights into how contextual factors influence the relationship between occupational fatigue and innovation. Moreover, incorporating qualitative methods alongside quantitative findings would provide a more nuanced understanding of individual and organizational experiences.
There is also a need for longitudinal studies to examine how interventions aimed at reducing occupational fatigue impact innovation practices over time. Interventions such as leadership training, resource optimization, and work-life balance programs could be implemented and evaluated for their effectiveness in mitigating fatigue and fostering a culture of innovation. Future studies should also explore the role of technology in alleviating fatigue and enhancing innovation, as technological solutions, such as e-health tools and artificial intelligence are increasingly integral to healthcare settings. This study provides important insights into the correlation between innovation practices and occupational fatigue in a high-intensity oncology setting. By identifying key barriers and enablers of innovation, this research contributes to a deeper understanding of how healthcare organizations can optimize both workforce well-being and organizational outcomes. Addressing occupational fatigue through strategic interventions will not only enhance innovation capacity but also improve overall healthcare quality, making these findings highly relevant for administrators, policymakers, and practitioners alike. The findings demonstrate the negative impact of fatigue on innovation, emphasizing the need for targeted actions to reduce fatigue and support creative, efficient practices among healthcare professionals.
Conclusion
Demographic factors, such as age, experience, and education, play significant roles in shaping perceptions of fatigue and innovation.
Acknowledgments: The authors would like to express their gratitude to the Sultan Qaboos Comprehensive Cancer Center for providing the resources and support necessary for conducting this study. Special thanks go to the clinical staff who participated and shared their experiences, making this research possible.
Ethical Permissions: The study proceeded after obtaining approval from SQCCC’s IRB (CCCRC-79-2024), ensuring that all ethical guidelines were adhered to, including participant confidentiality, informed consent, and voluntary participation.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: AlHasni NS (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Ayaad O (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); AlAwaisi HS (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Ibrahim RA (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (10%); Al Faliti BHS (Fifth Author), Assistant Researcher/Statistical Analyst (10%); AlMadhoun ET (Sixth Author), Assistant Researcher/Discussion Writer (10%); AlBaimani K (Seventh Author), Methodologist/Assistant Researcher/Discussion Writer (15%)
Funding/Support: No funding was received.
Innovation practices in healthcare refer to the structured implementation of new ideas, processes, and technologies to improve service delivery, patient care, and organizational efficiency [1]. These practices are increasingly critical in addressing complex challenges within healthcare systems, such as rising patient demands and resource constraints. The healthcare ecosystem relies on innovation to foster adaptive responses, ensuring long-term sustainability and effectiveness [2].
Innovation in healthcare operates across various domains that collectively enable its adoption and effectiveness. Key domains include organizational values and culture, which form the foundational mindset for embracing innovation, leadership behaviors, which drive and inspire innovative actions, resource allocation, which ensures the availability of tools and funding for innovation, process innovation, which focuses on improving workflows and clinical procedures, and stakeholder engagement, which integrates perspectives from patients, providers, and external partners [3]. Together, these domains form an integrated framework that supports and sustains innovation in healthcare systems.
The outcomes of innovative practices in healthcare are substantial, ranging from enhanced patient outcomes to improved operational effectiveness and efficiency, as well as increased staff experience and satisfaction. Innovation also fosters a competitive advantage, enabling organizations to stay ahead in a rapidly evolving environment [4]. However, various factors influence the success of innovation, including organizational structure, leadership support, resource availability, and workforce well-being. Among these, occupational fatigue is a significant yet underexplored factor that can hinder the ability to engage in and sustain innovative practices [5].
Fatigue is a multidimensional condition defined as a state of physical, psychosocial, emotional, and mental exhaustion resulting from exposure to any work-related stressors [5]. It is particularly prevalent in healthcare due to the high demands of patient care, long hours, and the emotional strain associated with critical decision-making and outcomes. If left unaddressed, fatigue can significantly impair healthcare professionals’ performance and well-being [6].
The domains of fatigue include physical fatigue, characterized by bodily exhaustion and reduced physical capacity; mental fatigue, which involves diminished cognitive and decision-making abilities; sleep-related fatigue, resulting from inadequate or poor-quality sleep; and shift-related fatigue, associated with irregular or prolonged work schedules [7]. Each of these domains has specific implications for healthcare delivery, particularly in high-intensity settings such as oncology.
The impacts of occupational fatigue are far-reaching and detrimental. Fatigue compromises individual performance, leading to increased medical errors, reduced productivity, and diminished job satisfaction [8]. It also affects organizational outcomes, including decreased innovation adoption, poor teamwork, and lower overall quality of care. Fatigue inhibits creativity, impairs problem-solving abilities, and reduces engagement in innovation processes, all of which are critical in healthcare environments that demand adaptability and efficiency [6].
Despite the recognized impacts of fatigue and the importance of innovation, limited research has examined the correlation between innovation practices and occupational fatigue in healthcare settings. While existing studies have explored individual aspects of innovation or fatigue, there remains a gap in understanding how fatigue directly influences innovation adoption, particularly in oncology settings where the intensity of work and the need for innovation are exceptionally high [5].
The lack of research on this topic underscores the need for studies that investigate the interplay between occupational fatigue and innovation. By addressing this gap, healthcare organizations can better understand how to mitigate fatigue and support innovation, ultimately improving patient outcomes and workforce satisfaction.
The significance of this study lies in its potential to provide actionable insights into the barriers and facilitators of innovation in high-intensity healthcare settings. Understanding the correlation between fatigue and innovation will help identify strategies to promote resilience, reduce burnout, and foster a culture of creativity and collaboration among healthcare professionals [9, 10]. The purpose of this study was to examine the relationship between innovation practices and occupational fatigue among healthcare professionals in oncology settings.
Instrument and Methods
Setting
This cross-sectional study was conducted at the Sultan Qaboos Comprehensive Cancer Center (SQCCC), University Medical City, in Muscat, Oman in 2024. SQCCC, known for its advanced oncology treatments and technologies, is a new center that provides an ideal environment for exploring innovation practices and occupational fatigue among healthcare professionals. The center’s reputation for cutting-edge cancer care, its diverse multidisciplinary team, its cultural context, and its supportive research environment make it a fitting location for this research.
A cross-sectional design was utilized to collect information as a snapshot of the current state of innovation practices and occupational fatigue among healthcare professionals at SQCCC. This design allowed for data collection at a single point in time, facilitating the inclusion of diverse participant perspectives from different roles within the center. The feasibility, efficiency, and analytical versatility of a cross-sectional study made it a suitable approach for this busy healthcare setting.
Sample
The study involved a sample of 163 clinical staff recruited using convenience sampling. Participants were required to have at least six months of experience at the Sultan Qaboos Comprehensive Cancer and Research Center to ensure familiarity with the work environment and exposure to its practices. With a 90% confidence level and a margin of error of 0.05, the minimum sample size required was 161 participants.
Instrument
We used a self-reported questionnaire consisting of three sections. The demographics section gathered basic participant information. The occupational fatigue section utilized the “Fatigue Risk Assessment and Management in High-Risk Environments (FRAME)” instrument, which measured physical, mental, sleep, and shift-related fatigue using 26 items on a five-point Likert scale [8, 11]. The innovation survey section was developed from the “Culture of Innovation Survey,” which was validated for the healthcare context to measure perceptions of innovation practices [12, 13].
The questionnaire used demonstrated strong reliability and validity metrics. The Cronbach’s alpha test ranged from 0.82 to 0.88 for the different sections of the questionnaire, indicating good reliability across all domains. The construct validity was tested through factor analysis. The Kaiser-Meyer-Olkin (KMO) value was calculated and showed a result of 0.85. Bartlett’s test of sphericity yielded a significant result (p<0.05), confirming that the questionnaire items effectively represented the underlying constructs of occupational fatigue and innovation practices.
Data collection
Upon receiving ethical approval from SQCCC’s Institutional Review Board (IRB), participants were recruited via invitation letters distributed through the center’s internal email system. Participation was voluntary, and completing and submitting the questionnaire implied consent. Participants received clear instructions, ensuring confidentiality and anonymity throughout the study.
Data analysis
Descriptive statistics, such as means, frequencies, and standard deviations were used to provide a summary overview of the data collected. Correlation analyses were conducted using Pearson’s correlation coefficient to identify significant associations. To identify differences in study innovation practices and occupational fatigue according to demographics, independent samples t-tests were used, with a p-value significance level set at <0.05. All statistical analyses were performed using SPSS version 23.
Data availability: The data supporting the findings of this study are available upon reasonable request from the corresponding author. Restrictions apply to the availability of these data due to ethical and confidentiality considerations.
Findings
The sample consisted of 163 clinical staff, primarily younger individuals, with the largest age group being 20-29 years. Females made up a slightly larger proportion of the sample compared to males. Most participants had between 0-5 years of total experience (n=65, 39.88%). Professionally, nearly half were nurses (n=81, 49.69%). Educationally, most held a bachelor’s degree (n=81, 49.69%). In terms of marital status, the majority were single (n=97, 59.51%; Table 1).
Table 1. Frequency of samples’ demographics
For innovation, the mean scores ranged from 4.02 to 4.26, with an overall mean of 4.24±0.52. In contrast, the domains of occupational fatigue had lower mean scores, ranging from 1.63 to 1.92, with an overall mean of 1.73±1.03 (Table 2).
Table 2. Mean scores of innovation practices and occupational fatigue
The correlation results showed the relationships between the total mean scores of innovation and occupational fatigue. A significant negative correlation was found between innovation and occupational fatigue (r=-0.68, p=0.045), indicating that higher levels of innovation are associated with lower levels of occupational fatigue.
There was a negative correlation between various domains of occupational fatigue and innovation. Specifically, physical fatigue (r=-0.55, p=0.045), mental fatigue (r=-0.60, p=0.041), sleep-related fatigue (r=-0.58, p=0.050), and shift-related fatigue (r=-0.62, p=0.048) all exhibit significant negative correlations with innovation.
All innovation domains had a negative relationship with occupational fatigue. Specifically, leadership behaviors exhibited the strongest negative correlation with occupational fatigue (r=-0.62, p=0.035).
Similarly, innovation processes (r=-0.60, p=0.040) and organizational climate (r=-0.59, p=0.039) also showed strong negative correlations, implying that occupational fatigue hampers the effectiveness of these domains. Other domains, including organizational values and culture (r=-0.58, p=0.042), innovation success (r=-0.57, p=0.041), and resource allocation (r=-0.55, p=0.045), demonstrated a similar pattern, where higher fatigue levels correlated with a decline in innovative capacity.
In terms of innovation, individuals over 40 years old scored significantly lower compared to those aged 20-40 (p=0.038). Experience also played a role, with those having over ten years of experience reporting significantly higher levels of innovation compared to less experienced individuals (p=0.032). Notably, physicians (p=0.029) and those with a master’s degree (p=0.029) or PhD (p=0.022) also scored higher in innovation compared to their counterparts.
For occupational fatigue, those aged over 40 reported significantly higher fatigue levels compared to younger participants (p=0.045). Participants with over ten years of experience reported significantly lower levels of occupational fatigue (p=0.027), while physicians experienced significantly less fatigue compared to nurses (p=0.031). Additionally, individuals with a master’s degree (p=0.035) or PhD (p=0.029) reported lower occupational fatigue compared to those with a bachelor’s degree (Table 3).
Table 3. Differences in innovation practices and occupational fatigue according to demographics

Discussion
The purpose of the study was to examine the relationship between innovation practices and occupational fatigue among healthcare professionals in oncology settings. The demographic composition of the study sample, predominantly younger professionals aged 20-39, suggests that the workforce in this oncology setting comprises a relatively inexperienced yet dynamic group. This demographic pattern is consistent with the global trend of younger professionals entering healthcare due to increased educational opportunities and the sector’s demand for a fresh workforce [4]. Their limited professional experience (0-10 years for most) may influence their perceptions of innovation and occupational fatigue. Early-career professionals are often more adaptable and open to innovation but may also lack the coping strategies required to manage workplace fatigue effectively [14, 15].
The predominance of female participants reflects the gender distribution commonly observed in healthcare professions, especially nursing, which constituted nearly half of the sample. Female healthcare workers often face unique challenges, including balancing professional responsibilities with personal and family obligations, which may contribute to higher fatigue levels [5]. The slightly larger proportion of female participants aligns with studies showing that women are more represented in nursing and other supportive healthcare roles [15, 16].
The educational profile of participants, with the majority holding bachelor’s or master’s degrees, indicates a highly qualified workforce. Advanced education levels correlate with better knowledge of and engagement in innovation practices [1, 17]. However, the underrepresentation of professionals with doctoral degrees suggests potential limitations in research capacity and leadership for driving significant innovation within this setting [16].
We found a high level of perceived innovation across domains, with resource allocation scoring the highest. This result highlights the importance of sufficient resources in fostering innovation, as access to funding, technology, and time enables healthcare professionals to experiment with and implement new ideas [4, 6]. Leadership behaviors and organizational values also score highly, emphasizing the role of supportive leadership and a culture conducive to innovation [3, 7].
Occupational fatigue was relatively low overall, with shift-related fatigue being the most prominent domain. This finding aligns with previous research indicating that shift work disrupts circadian rhythms and sleep patterns, leading to increased fatigue [6, 16]. Sleep-related fatigue was the lowest, possibly due to institutional policies supporting adequate rest or flexible schedules. However, the cumulative effects of other fatigue domains may still impact professionals’ overall capacity to innovate [5, 17]. We revealed a significant negative correlation between occupational fatigue and innovation. This relationship suggests that fatigue diminishes professionals’ ability to engage in innovative practices, likely due to reduced cognitive capacity, creativity, and motivation. The strongest negative correlations were observed in leadership behaviors and organizational climate, emphasizing how fatigue impacts roles that require decision-making and fostering collaborative environments [16, 18].
The demographic findings further elucidated this relationship. Participants over 40 years old reported higher fatigue levels and lower innovation scores, reflecting the cumulative physical and mental strain experienced by older professionals [13, 19]. In contrast, younger participants displayed higher innovation scores, possibly due to greater familiarity with new technologies and openness to change [4, 15].
Interestingly, professionals with over ten years of experience reported lower fatigue levels and higher innovation scores, suggesting that experience equips individuals with better coping mechanisms and a deeper understanding of institutional processes [17]. In contrast, less experienced staff may face challenges adapting to demanding healthcare environments, which affects their capacity for innovation [15, 20].
The significant differences among professions highlight the unique challenges and opportunities within each role. Nurses reported the highest levels of fatigue, consistent with their physically and emotionally demanding duties [14]. Physicians, on the other hand, exhibit higher innovation scores and lower fatigue levels, possibly due to greater autonomy and decision-making power in their roles [16].
Education level also influenced the results, with master’s and doctorate holders displaying higher innovation scores and lower fatigue levels. Advanced education may provide these professionals with better tools to manage stress and engage in innovative practices effectively [21]. Bachelor’s degree holders, who form the majority, showed moderate levels of innovation and fatigue, reflecting their critical role in daily operations without the strategic insights afforded by higher qualifications [22, 23].
Marital status played a minor role, with single participants exhibiting slightly higher innovation scores, possibly due to fewer personal commitments. However, the differences were not substantial, indicating that marital status alone does not significantly influence innovation or fatigue [6, 7].
The correlation matrix underscores the detrimental impact of fatigue on innovation across all domains. Resource allocation and organizational climate, which are key enablers of innovation, were particularly affected, demonstrating that fatigue compromises both the operational and cultural foundations necessary for fostering innovation [3, 7]. The findings emphasize the need for targeted interventions to mitigate occupational fatigue and promote innovation. Strategies such as workload optimization, shift scheduling reforms, and leadership training can significantly enhance both workforce well-being and organizational performance [17, 24].
This study has several limitations. First, the relatively small sample size of 163 participants may limit the generalizability of the results to other oncology settings or healthcare institutions. Larger, more diverse samples would provide a broader perspective and enhance the reliability of the findings. Additionally, the study was conducted in a new specialized cancer center, which may not reflect the practices and challenges present in other healthcare settings, such as primary care or general hospitals.
Second, the use of convenience sampling might have introduced selection bias. Staff who voluntarily chose to participate may differ in their experiences or perceptions of innovation and fatigue compared to those who did not participate. Furthermore, the cross-sectional design captures only a snapshot of the relationship between occupational fatigue and innovation, limiting the ability to infer causality.
Future studies should expand the sample size and include participants from diverse healthcare settings. Comparative studies across different institutions or geographic regions could offer insights into how contextual factors influence the relationship between occupational fatigue and innovation. Moreover, incorporating qualitative methods alongside quantitative findings would provide a more nuanced understanding of individual and organizational experiences.
There is also a need for longitudinal studies to examine how interventions aimed at reducing occupational fatigue impact innovation practices over time. Interventions such as leadership training, resource optimization, and work-life balance programs could be implemented and evaluated for their effectiveness in mitigating fatigue and fostering a culture of innovation. Future studies should also explore the role of technology in alleviating fatigue and enhancing innovation, as technological solutions, such as e-health tools and artificial intelligence are increasingly integral to healthcare settings. This study provides important insights into the correlation between innovation practices and occupational fatigue in a high-intensity oncology setting. By identifying key barriers and enablers of innovation, this research contributes to a deeper understanding of how healthcare organizations can optimize both workforce well-being and organizational outcomes. Addressing occupational fatigue through strategic interventions will not only enhance innovation capacity but also improve overall healthcare quality, making these findings highly relevant for administrators, policymakers, and practitioners alike. The findings demonstrate the negative impact of fatigue on innovation, emphasizing the need for targeted actions to reduce fatigue and support creative, efficient practices among healthcare professionals.
Conclusion
Demographic factors, such as age, experience, and education, play significant roles in shaping perceptions of fatigue and innovation.
Acknowledgments: The authors would like to express their gratitude to the Sultan Qaboos Comprehensive Cancer Center for providing the resources and support necessary for conducting this study. Special thanks go to the clinical staff who participated and shared their experiences, making this research possible.
Ethical Permissions: The study proceeded after obtaining approval from SQCCC’s IRB (CCCRC-79-2024), ensuring that all ethical guidelines were adhered to, including participant confidentiality, informed consent, and voluntary participation.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: AlHasni NS (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (20%); Ayaad O (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); AlAwaisi HS (Third Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (15%); Ibrahim RA (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (10%); Al Faliti BHS (Fifth Author), Assistant Researcher/Statistical Analyst (10%); AlMadhoun ET (Sixth Author), Assistant Researcher/Discussion Writer (10%); AlBaimani K (Seventh Author), Methodologist/Assistant Researcher/Discussion Writer (15%)
Funding/Support: No funding was received.
Article Type: Descriptive & Survey |
Subject:
Health Promotion Setting
Received: 2024/11/5 | Accepted: 2024/12/25 | Published: 2025/01/27
Received: 2024/11/5 | Accepted: 2024/12/25 | Published: 2025/01/27
References
1. Cannavale C, Tammaro AE, Leone D, Schiavone F. Innovation adoption in inter-organizational healthcare networks-The role of artificial intelligence. Eur J Innov Manag. 2022;25(6):758-74. [Link] [DOI:10.1108/EJIM-08-2021-0378]
2. Russo Spena T, Cristina M. Practising innovation in the healthcare ecosystem: The agency of third-party actors. J Bus Ind Mark. 2020;35(3):390-403. [Link] [DOI:10.1108/JBIM-01-2019-0048]
3. Segarra-Oña M, Peiró-Signes Á, Verma R. Fostering innovation through stakeholders' engagement at the healthcare industry: Tapping the right key. Health Policy. 2020;124(8):895-901. [Link] [DOI:10.1016/j.healthpol.2020.05.013]
4. Marques CS, Lopes C, Braga V, Ratten V, Santos G. Intuition and rationality in intrapreneurship and innovation outputs: The case of health professionals in primary health care. Int Entrep Manag J. 2022;18(2):579-602. [Link] [DOI:10.1007/s11365-021-00761-7]
5. Cho H, Sagherian K, Scott LD, Steege LM. Occupational fatigue, workload, and nursing teamwork in hospital nurses. J Adv Nurs. 2022;78(8):2313-26. [Link] [DOI:10.1111/jan.15246]
6. Min A, Kim YM, Yoon YS, Hong HC, Kang M, Scott LD. Effects of work environments and occupational fatigue on care left undone in rotating shift nurses. J Nurs Scholarsh. 2021;53(1):126-36. [Link] [DOI:10.1111/jnu.12604]
7. Al-Ruzzieh MA, Ayaad O. Work stress, coping strategies, and health-related quality of life among nurses at an international specialized cancer center. Asian Pac J Cancer Prev. 2021;22(9):2995-3001. [Link] [DOI:10.31557/APJCP.2021.22.9.2995]
8. Al-Ruzzieh MA, Ayaad O. Measuring occupational fatigue among higher and middle management at a specialized cancer center during the COVID-19 pandemic. Asian Pac J Cancer Prev. 2022;23(10):3265-71. [Link] [DOI:10.31557/APJCP.2022.23.10.3265]
9. Ahmadi M, Choobineh A, Mousavizadeh A, Daneshmandi H. Physical and psychological workloads and their association with occupational fatigue among hospital service personnel. BMC Health Serv Res. 2022;22(1):1150. [Link] [DOI:10.1186/s12913-022-08530-0]
10. Ekiz Kavukoğlu T, İşci E. The mediating role of strategic planning awareness in the impact of organizational innovation on business excellence in hospitals. TQM J. 2023;36(8):2527-50. [Link] [DOI:10.1108/TQM-05-2023-0155]
11. Shortz AE, Mehta RK, Peres SC, Benden ME, Zheng Q. Development of the fatigue risk assessment and management in high-risk environments (FRAME) survey: A participatory approach. Int J Environ Res Public Health. 2019;16(4):522. [Link] [DOI:10.3390/ijerph16040522]
12. Dobni CB. Measuring innovation culture in organizations: The development of a generalized innovation culture construct using exploratory factor analysis. Eur J Innov Manag. 2008;11(4):539-59. [Link] [DOI:10.1108/14601060810911156]
13. Tian M, Deng P, Zhang Y, Salmador MP. How does culture influence innovation? A systematic literature review. Manag Decis. 2018;56(5):1088-107. [Link] [DOI:10.1108/MD-05-2017-0462]
14. Saeed H, Som HM, Mahmood R. Leadership styles, organizational culture, and innovation in healthcare: A conceptual framework. Int J Acad Res Bus Soc Sci. 2022;12(8):1390-408. [Link] [DOI:10.6007/IJARBSS/v12-i8/14551]
15. West MA, Richter AW. Climates and cultures for innovation and creativity at work. In: Handbook of organizational creativity. New York: Psychology Press; 2024. p. 211-36. [Link] [DOI:10.4324/9781003573326-11]
16. Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue, and psychosocial well-being during the COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. 2023;32(15-16):5382-95. [Link] [DOI:10.1111/jocn.15566]
17. Galiano MA, Fergusson MEM, Guerrero WJ, Muñoz MF, Basto GAO, Ramírez JSC, et al. Technological innovation for workload allocation in nursing care management: An integrative review. F1000Res. 2024;12:104. [Link] [DOI:10.12688/f1000research.125421.3]
18. Ding H, Quan G. How and when does follower's strengths-based leadership relate to follower innovative behavior: The roles of self-efficacy and emotional exhaustion. J Creat Behav. 2021;55(3):591-603. [Link] [DOI:10.1002/jocb.473]
19. Büschgens T, Bausch A, Balkin DB. Organizational culture and innovation: A meta-analytic review. J Prod Innov Manag. 2013;30(4):763-81. [Link] [DOI:10.1111/jpim.12021]
20. Najmabadi L, Agénor M, Tendulkar S. "Pouring from an empty cup": Manifestations, drivers, and protective factors of occupational stress among healthcare providers of trauma-informed care. J Interpers Violence. 2024;39(9-10):2041-75. [Link] [DOI:10.1177/08862605231215028]
21. Patole S, Pawale D, Rath C. Interventions for compassion fatigue in healthcare providers-A systematic review of randomised controlled trials. Healthcare. 2024;12(2):171. [Link] [DOI:10.3390/healthcare12020171]
22. Al-Ruzzieh MA, Ayaad O. Impact of nurses' emotional intelligence on the implementation of a professional practice model in cancer care. Br J Nurs. 2021;30(19):1110-6. [Link] [DOI:10.12968/bjon.2021.30.19.1110]
23. Al-Ruzzieh MA, Ayaad O. Nursing professional practice model: Development, implementation, and evaluation at an international specialized cancer center. J Nurs Adm. 2020;50(11):562-4. [Link] [DOI:10.1097/NNA.0000000000000937]
24. Abuseif S, Ayaad O, Abu-Al-Haijaa E. Measuring factors affecting the autonomy of nurses work. Int J Acad Res Bus Soc Sci. 2018;8(12):1785-96. [Link] [DOI:10.6007/IJARBSS/v8-i12/5323]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






