Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 147-153 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Damayantie N, Ernawati E, Dewi M. Impact of the Health Belief Model on Hypoglycemia Prevention Skills in Diabetes Mellitus Patients. Health Educ Health Promot 2025; 13 (1) :147-153
URL: http://hehp.modares.ac.ir/article-5-78751-en.html
URL: http://hehp.modares.ac.ir/article-5-78751-en.html
1- Department of Nursing, Health Polytechnic, Ministry of Health Jambi, Jambi, Indonesia
Keywords: Diabetes Mellitus [MeSH], Hypoglycemia [MeSH], Health Belief Model [MeSH], Health Education [MeSH], Mobile Health [MeSH]
Full-Text [PDF 591 kb]
(258 Downloads)
| Abstract (HTML) (591 Views)
Full-Text: (56 Views)
Introduction
Diabetes mellitus (DM) refers to a collection of metabolic conditions marked by persistent hyperglycemia caused by impaired insulin secretion, action, or both [1, 2]. As of 2021, diabetes affects over 537 million people globally, with this number expected to climb to 643 million by 2030 and 783 million by 2045. The prevalence of DM, diagnosed by medical professionals in individuals aged 15 and above, has consistently risen over the years, increasing from 1.5% in 2013 [1] to 2.0% in 2018 [2], and reaching 2.2% in 2023 [3].
Insulin therapy often leads to hypoglycemia, a condition resulting from an insulin dose that exceeds the patient’s physiological needs, causing a significant drop in blood sugar levels. Additionally, hypoglycemia may arise from the failure of counterregulatory mechanisms, which can occur as a consequence of long-term DM [4]. It is the most common complication among DM patients, with approximately 90% of those receiving insulin therapy reported to have experienced hypoglycemic episodes [5].
Preventing hypoglycemia requires improved blood glucose control and early detection of the condition. This includes educating patients about the signs and symptoms of hypoglycemia, as well as the immediate steps for temporary management [6, 7]. Knowledge and understanding of hypoglycemia are crucial for identifying its onset, interpreting early symptoms, and making informed decisions—whether through self-directed actions or by seeking assistance [8]. Awareness of type 2 diabetes mellitus (T2DM) management and hypoglycemia symptoms has been shown to positively influence patients’ ability to detect hypoglycemia [9]. Independent blood glucose monitoring can be successfully implemented after appropriate training [10]. Enhanced knowledge of T2DM management and hypoglycemia symptoms contributes significantly to improving patients’ self-awareness and response to hypoglycemic events [11].
Knowledge, as a product of the learning process, is a dynamic element capable of shaping an individual’s actions [12]. The health belief model (HBM) serves as a theoretical framework for analyzing health-related behaviors and the factors influencing a person’s compliance with health management guidelines [13, 14]. According to the HBM, people are more inclined to adopt health-enhancing practices when they acknowledge their susceptibility to potential health risks (perceived susceptibility), comprehend the gravity of those risks (perceived severity), believe in the positive outcomes of adopting healthier behaviors (perceived benefits), and can effectively overcome challenges to implementing those behaviors (perceived barriers) [15, 16].
Moreover, self-efficacy (the confidence in one’s capacity to carry out particular tasks) serves as a pivotal factor in fostering positive health behaviors and eliminating harmful ones. Cues to action represent the stimuli or signals that encourage individuals to initiate behavior change [17, 18]. A study conducted by Shabibi et al. on the effectiveness of HBM-based educational interventions in promoting self-care practices among patients with T2DM reveals notable enhancements in perceived susceptibility, severity, benefits, barriers, self-efficacy, and self-care behaviors [19].
Advancements in science and technology continue to drive efforts to integrate technology into the learning process. The adoption of new technologies enhances the role of specialized nurses by enabling the efficient and sustainable implementation of technology-based nursing practices [20]. This involves identifying and utilizing technology and application systems that align with the care plans and specific needs of patients with DM [21].
According to Mayer, multimedia refers to the presentation of material using a combination of text and images, which facilitates better comprehension among learners compared to text-only formats [22]. The cognitive theory of multimedia posits that humans process information through two channels (visual and auditory), each with limited capacity. An active learning process engages these cognitive channels, promoting coordination and improving the understanding of educational material [23, 24].
The integration of mobile health technology into DM education represents an innovative approach to engaging patients and promoting positive health behaviors. Various mobile technology-based strategies have been employed to assess their effectiveness, including videophones, mobile phones tailored for diabetes management [25-27], mHealth management applications aimed at improving adherence and preventing hypoglycemia [28, 29], and smartphone applications such as Hypomap, which is designed to reduce hypoglycemia in type 1 DM. Additionally, the IMB-DSC model has been used to evaluate self-care behaviors [30].
Despite these advancements, there is a notable lack of research on the development of diabetes education models utilizing smartphone applications specifically designed to prevent and detect hypoglycemia in patients with T2DM. A systematic review conducted by Mufidah et al. [31] highlights the potential benefits of smartphone applications as educational tools for individuals with DM, emphasizing their value as a medium for patient education.
In 2023, we designed a health education framework rooted in the principles of the HBM to aid in the prevention of hypoglycemia among individuals with DM. The model was designed and developed using the ADDIE framework, which comprises five stages, including analysis, design, development, implementation, and evaluation. This educational model represents a scientifically grounded learning design, detailed in an academic paper. To assess its practicality and effectiveness, researchers created a website-based prototype as part of the model’s development—a smartphone application named NEDTA (nursing education diabetic therapeutic application). Field trials are essential to validate the application’s capability to accurately detect early signs of hypoglycemia. Building on this foundation, this study aimed to assess the impact of this HBM-based education on patients’ ability to prevent hypoglycemia in DM.
Materials and Methods
Study design
This quasi-experimental research employed a design and development methodology, utilizing the ADDIE framework as the guiding model. The research process followed a structured sequence of phases, including analysis, design & development, formative evaluation, and evaluation [32].
Subjects
The study was done between February and August 2024 in the service areas of Puskesmas Simpang Kawat and Puskesmas Pakuan Baru. Primary data were gathered via interviews, utilizing questionnaires administered to 36 participants in the intervention group and 36 in the control group. The sample size was determined using the methodology proposed by Sastroasmoro & Ismael [33]:
The sample size was calculated using a formula that incorporated a 5% type I error rate (Zα=1.96) and a 10% type II error rate (Zβ=1.28). Mean values for the pre- and post-intervention groups were referenced from prior work by Song et al. [34], with a pre-intervention average of 9.52, a post-intervention average of 12.11, and a standard deviation of 4.46. Based on these inputs, the calculated sample size (n) was 31.128, which was rounded up to 32 participants. To mitigate the impact of potential dropouts, an additional 10% (four participants) was included, leading to a final count of 36 respondents per group for both the intervention and control groups. Eligibility criteria required participants to own and be proficient in using a smartphone, demonstrate a willingness to cooperate, and provide informed consent for participation.
Instrument
The primary outcome was the capacity to prevent hypoglycemia. Data were gathered through a questionnaire aimed at evaluating the cognitive skills of individuals with DM in managing hypoglycemia prevention. The instrument was adapted from a validated and reliable tool developed by Supadi [35] and underwent thorough validity and reliability testing. Validity assessments demonstrated that all items had correlation coefficients exceeding the threshold value (r table), confirming their validity. Reliability analysis produced a Cronbach’s Alpha score of 0.85, signifying that the questionnaire is highly reliable.
The questionnaire included 20 items, with a score of one given for correct responses and zero for incorrect ones. The scores reflecting the ability to prevent hypoglycemic episodes were treated as ratio data, with a possible range from 0 to 20. These assessments were carried out through both pre-test and post-test evaluations.
The HBM is a design product based on the analysis, design & development, formative evaluation, and evaluation phases. This smartphone-based HBM health education model was implemented to prevent hypoglycemia in patients with DM.
Data collection
The data collection process began with discussions with the development team to revise the existing application by adding images and explanations to the media. The application was then validated by IT experts to ensure that the website-based educational tool was suitable for use in the research [36].
Next, respondents were identified according to the inclusion criteria; 36 DM patients from the Simpang Kawat Puskesmas work area (intervention group) and 36 DM patients from the Pakuan Baru work area (control group).
In the intervention group, a socialization session was conducted to explain the application and its usage on smartphones. Participants were provided with an application manual and video tutorials to ensure they could use the application independently, without the need for researcher assistance. The hypoglycemia prevention application was then installed on the respondents’ smartphones.
Participants were instructed to complete the pre-test items via the application. The intervention, which was grounded in the HBM Health Education Framework, took place over two months, providing participants with sufficient time to explore, engage with, and internalize the information offered in the hypoglycemia prevention application. After two months, a post-test evaluation was conducted. In the control group, a socialization session was held to provide an explanation of DM and hypoglycemia, along with the distribution of a pocketbook on hypoglycemia and its management. A pre-test was then conducted, during which respondents were asked to review and familiarize themselves with the material in the pocketbook. After two months, a post-test evaluation was conducted. Throughout the research activities, the researchers were supported by six enumerators who had been trained for the study.
Data analysis
Descriptive statistics, including mean, standard deviation, minimum, and maximum values, were used to analyze the univariate data for age and duration of DM. For categorical data, such as gender, education level, occupation, history of hypoglycemia, glucometer ownership, and type of DM medication, frequency distributions were calculated. The distribution of the data was first evaluated using the Kolmogorov-Smirnov test, which confirmed that the data followed a normal distribution. Then, inferential statistical analyses, including dependent and independent t-tests, were conducted to compare mean values and assess the mean differences between the two groups. All tests were performed with a significance level set at p<0.05, and data analysis was carried out using SPSS version 23.0.
Findings
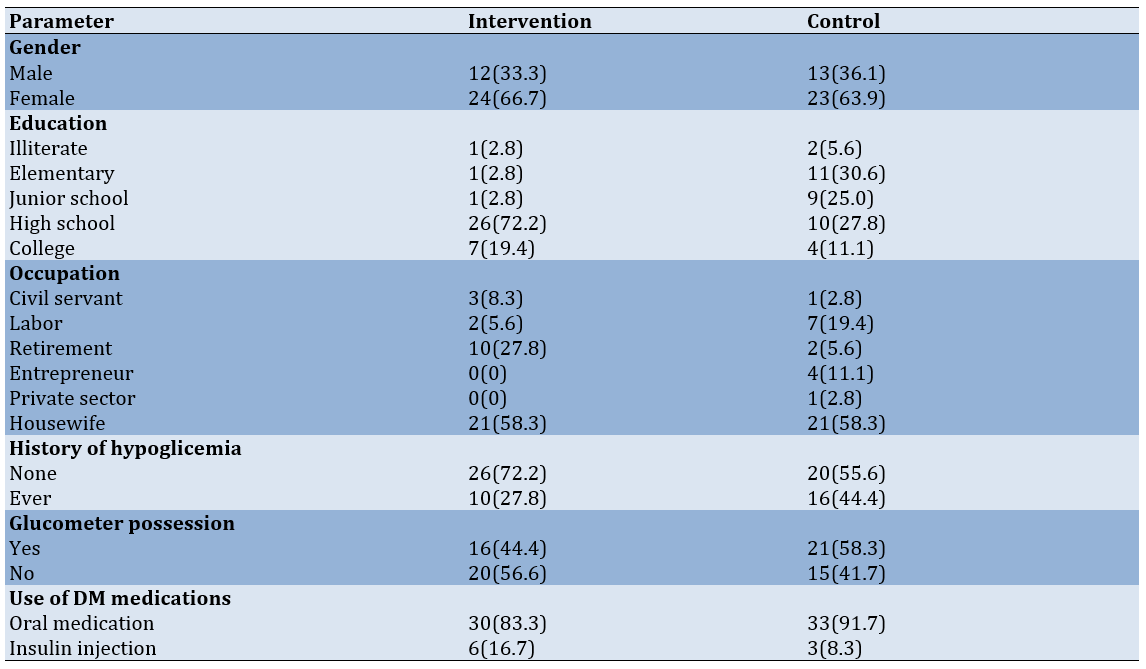
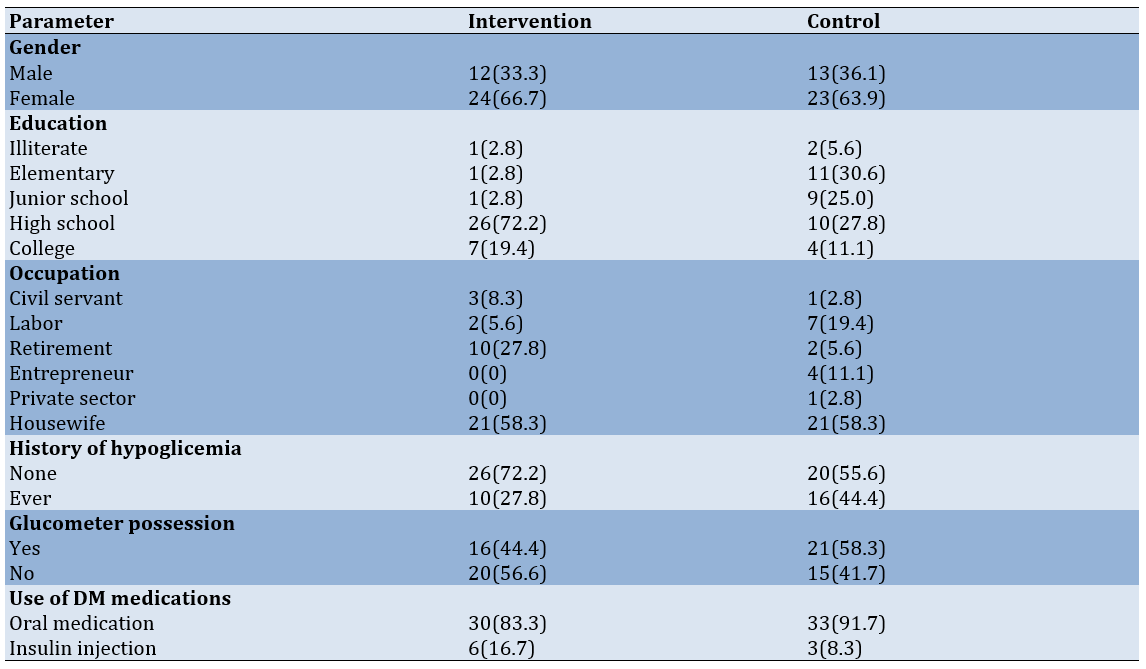
The intervention group was younger (59.92±8.80 years) compared to the control group (62.89±7.62 years), with the majority being female. Most participants in the intervention group had a high school education, while the control group was dominated by elementary school graduates. The most common occupation in both groups was housewife. Most individuals in the intervention group had no history of hypoglycemia, whereas glucometers were more commonly owned by the control group. The primary treatment in both groups was oral medication, with the average duration of diabetes being slightly longer in the intervention group compared to the controls (5.22±5.20 vs. 4.00±2.04 years, respectively) (Table 1).
Table 1. Frequency of demographic and clinical characteristics of diabetes mellitus patients
There was an improvement in hypoglycemia prevention scores in both the intervention and control groups. In the intervention group, the average pre-test score was 48.11±6.17, with a median of 47, which significantly rose to 55.89±6.92, with a median of 58, in the post-test (p-value=0.0001). For the control group, the mean pre-test score was 43.170±4.74, with a median of 44, which increased to 45.39±5.92, with a median of 45, in the post-test (p-value=0.0001).
There was a noteworthy difference in hypoglycemia prevention abilities between the intervention and control groups in the post-test. The intervention group had a mean score of 50.64±6.42 for hypoglycemia prevention (p-value=0.0001).
Discussion
This study aimed to assess the impact of this HBM-based education on patients’ ability to prevent hypoglycemia in DM. More than two-thirds of the participants were women. Global studies generally indicate that women are at a higher risk of hypoglycemia than men. According to Yang et al. [37], there is a significant correlation between gender and hypoglycemia, with women experiencing more frequent hypoglycemic episodes. This could be linked to hormonal changes during menopause, such as reduced estrogen and progesterone levels, which may lead to increased fat storage and alterations in lipid profiles, ultimately decreasing insulin sensitivity in the liver and muscles [38, 39]. While some research suggests no significant difference between men and women in detecting hypoglycemic events [40], overall, women tend to be more vulnerable to hypoglycemia.
The majority of participants in the intervention group had a high school education, which likely made it easier for them to understand the information provided by the researchers. Education level is an important factor in knowledge improvement, as individuals with higher education are generally assumed to absorb information more easily. However, education level should not be seen as an indicator of mastery in specific fields but rather as a sign that an individual has completed formal education in a particular area. The ability to prevent hypoglycemia results from the interaction of knowledge, attitudes, and actions regarding hypoglycemia management, which can be gained through personal experiences, others’ experiences, media, or formal education. According to Chrisanto & Agustama [40], education level influences an individual’s ability to understand their health condition. Those with lower education levels may struggle to recognize health issues and understand disease management guidelines, whereas individuals with higher education levels are better equipped to recognize health-related factors and understand the long-term implications for their health.
The participants in the intervention group were, on average, in the elderly age range. This suggests that these individuals had considerable life experience and well-developed decision-making and judgment abilities. However, older adults are more vulnerable to hypoglycemia due to factors such as diminished kidney function, which impairs drug clearance, the use of multiple medications and potential drug interactions, and a decline in cognitive abilities [41]. Cognitive decline in older adults can increase their risk of hypoglycemia, while hypoglycemic episodes can also worsen or contribute to further cognitive impairments [42].
The duration of DM is often directly related to the improvement in experience, particularly for family members living with individuals who have DM. Based on the study results, the average duration of diabetes in the intervention group was just over five years. For the patients themselves, a longer duration of DM increases the likelihood of experiencing hypoglycemia. Over time, individuals with DM tend to have more frequent hypoglycemic episodes, making these experiences a key stimulus for preventing hypoglycemia. The theory of pain behavior suggests that individuals who frequently experience pain or its symptoms are more likely to be attentive to their condition and seek appropriate help [28].
The HBM aims to strengthen the ability of individuals with DM to prevent hypoglycemia. This model is based on the theory of the HBM, which provides a framework for understanding the factors that drive health behaviors and influence whether people follow or ignore health management guidelines. According to the HBM, individuals are more inclined to adopt health-promoting actions if they believe they are at risk (perceived susceptibility), acknowledge the seriousness of the risk (perceived severity), trust that making changes will yield positive outcomes (perceived benefit), and feel confident in overcoming obstacles to adopting healthier behaviors (perceived barriers). Additionally, self-efficacy refers to an individual’s confidence in their ability to take action, improve health, and eliminate harmful habits. Cues to action are the signals or motivations that prompt individuals to initiate change [16]. Research by Shabibi et al. [19] found that using HBM-based educational interventions significantly improves self-care behaviors in individuals with T2DM, demonstrating improvements in perceptions of risk, severity, benefits, barriers, self-efficacy, and overall attitudes toward health management [19, 43, 44].
The NEDTA application was designed to provide individuals with DM the opportunity to learn at their convenience, anytime and anywhere. At the start of the study, not all participants were able to access the application link provided by the researchers. However, the initial socialization meeting facilitated the process by allowing the researchers and their team to assist participants in installing the application on their smartphones. The researchers recognized that effectively utilizing mobile applications for health promotion requires clear communication and commitment-building, ensuring that participants engage fully with each activity. Simply sharing the application link does not guarantee active participation in efforts to maintain health. Therefore, a comprehensive strategy is essential to ensure the effectiveness of smartphone-based education for adults. This includes identifying the participants’ informational needs, defining performance objectives, developing appropriate steps for transferring information through the smartphone, and ultimately evaluating the impact of the intervention on improving the ability of DM patients to detect hypoglycemia.
The intervention aimed at improving the competence of DM patients focuses on providing education about the disease process, treatment, and prevention of hypoglycemic complications. Education is delivered through health promotion, which empowers individuals and communities to maintain and enhance their health. This empowerment goes beyond simply sharing information (such as health education) and includes efforts to change behaviors and attitudes. The involvement of community cadres and Puskesmas in this educational program is crucial, as it enables the community to play an active role in managing DM and improving self-care behaviors among patients. This approach aligns with Indonesian government policy, particularly in the context of the infectious disease prevention and control program. The implementation of a health education model based on the HBM was effective in enhancing the ability of DM patients to prevent hypoglycemia. The intervention demonstrated a significant impact compared to the non-intervention group, indicating that a structured educational approach can help patients better understand and manage the risks associated with hypoglycemia.
This study has several limitations that should be acknowledged. First, the relatively small sample size and the use of purposive sampling may limit the generalizability of the findings to the broader population of diabetes mellitus patients. Second, the intervention was implemented over a relatively short period of two months, which may not fully capture long-term behavioral changes or sustained improvements in hypoglycemia prevention skills. Third, although the use of a smartphone application provides flexibility and accessibility, not all participants may have had equal digital literacy, which could influence their ability to engage optimally with the intervention. Future studies should consider employing larger and more diverse samples, extending the duration of follow-up, incorporating objective measures of behavioral change, and exploring additional factors such as cultural beliefs and family support that may influence the effectiveness of digital health interventions.
Conclusion
The HBM-based education model effectively improves the ability of diabetes mellitus patients to prevent hypoglycemia.
Acknowledgments: The authors would like to thank all participants for their participation and cooperation throughout the study. They also thank the Head of the Health Polytechnic of the Ministry of Health in Jambi for their support and assistance, as well as the researchers, data collection team, enumerator team, and all parties involved in this project.
Ethical Permissions: Participants’ privacy was protected, there was no incentive to engage in the study, and registered prospective respondents signed an informed consent form. The researcher obtained ethical permission before beginning data collection. According to the authors, this study was authorized by the Health Polytechnic of the Ministry of Health in Jambi, under approval number: LB.02.06/2/300.1/2024.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Damayantie N (First Author), Introduction Writer/Original Researcher/Methodologist/Discussion Writer/Statistical Analyst (40%); Ernawati E (Second Author), Original Researcher/Discussion Writer (30%); Dewi M (Third Author), Introduction Writer/Original Researcher/Discussion Writer (30%)
Funding/Support: We did not receive any financial support from any party.
Diabetes mellitus (DM) refers to a collection of metabolic conditions marked by persistent hyperglycemia caused by impaired insulin secretion, action, or both [1, 2]. As of 2021, diabetes affects over 537 million people globally, with this number expected to climb to 643 million by 2030 and 783 million by 2045. The prevalence of DM, diagnosed by medical professionals in individuals aged 15 and above, has consistently risen over the years, increasing from 1.5% in 2013 [1] to 2.0% in 2018 [2], and reaching 2.2% in 2023 [3].
Insulin therapy often leads to hypoglycemia, a condition resulting from an insulin dose that exceeds the patient’s physiological needs, causing a significant drop in blood sugar levels. Additionally, hypoglycemia may arise from the failure of counterregulatory mechanisms, which can occur as a consequence of long-term DM [4]. It is the most common complication among DM patients, with approximately 90% of those receiving insulin therapy reported to have experienced hypoglycemic episodes [5].
Preventing hypoglycemia requires improved blood glucose control and early detection of the condition. This includes educating patients about the signs and symptoms of hypoglycemia, as well as the immediate steps for temporary management [6, 7]. Knowledge and understanding of hypoglycemia are crucial for identifying its onset, interpreting early symptoms, and making informed decisions—whether through self-directed actions or by seeking assistance [8]. Awareness of type 2 diabetes mellitus (T2DM) management and hypoglycemia symptoms has been shown to positively influence patients’ ability to detect hypoglycemia [9]. Independent blood glucose monitoring can be successfully implemented after appropriate training [10]. Enhanced knowledge of T2DM management and hypoglycemia symptoms contributes significantly to improving patients’ self-awareness and response to hypoglycemic events [11].
Knowledge, as a product of the learning process, is a dynamic element capable of shaping an individual’s actions [12]. The health belief model (HBM) serves as a theoretical framework for analyzing health-related behaviors and the factors influencing a person’s compliance with health management guidelines [13, 14]. According to the HBM, people are more inclined to adopt health-enhancing practices when they acknowledge their susceptibility to potential health risks (perceived susceptibility), comprehend the gravity of those risks (perceived severity), believe in the positive outcomes of adopting healthier behaviors (perceived benefits), and can effectively overcome challenges to implementing those behaviors (perceived barriers) [15, 16].
Moreover, self-efficacy (the confidence in one’s capacity to carry out particular tasks) serves as a pivotal factor in fostering positive health behaviors and eliminating harmful ones. Cues to action represent the stimuli or signals that encourage individuals to initiate behavior change [17, 18]. A study conducted by Shabibi et al. on the effectiveness of HBM-based educational interventions in promoting self-care practices among patients with T2DM reveals notable enhancements in perceived susceptibility, severity, benefits, barriers, self-efficacy, and self-care behaviors [19].
Advancements in science and technology continue to drive efforts to integrate technology into the learning process. The adoption of new technologies enhances the role of specialized nurses by enabling the efficient and sustainable implementation of technology-based nursing practices [20]. This involves identifying and utilizing technology and application systems that align with the care plans and specific needs of patients with DM [21].
According to Mayer, multimedia refers to the presentation of material using a combination of text and images, which facilitates better comprehension among learners compared to text-only formats [22]. The cognitive theory of multimedia posits that humans process information through two channels (visual and auditory), each with limited capacity. An active learning process engages these cognitive channels, promoting coordination and improving the understanding of educational material [23, 24].
The integration of mobile health technology into DM education represents an innovative approach to engaging patients and promoting positive health behaviors. Various mobile technology-based strategies have been employed to assess their effectiveness, including videophones, mobile phones tailored for diabetes management [25-27], mHealth management applications aimed at improving adherence and preventing hypoglycemia [28, 29], and smartphone applications such as Hypomap, which is designed to reduce hypoglycemia in type 1 DM. Additionally, the IMB-DSC model has been used to evaluate self-care behaviors [30].
Despite these advancements, there is a notable lack of research on the development of diabetes education models utilizing smartphone applications specifically designed to prevent and detect hypoglycemia in patients with T2DM. A systematic review conducted by Mufidah et al. [31] highlights the potential benefits of smartphone applications as educational tools for individuals with DM, emphasizing their value as a medium for patient education.
In 2023, we designed a health education framework rooted in the principles of the HBM to aid in the prevention of hypoglycemia among individuals with DM. The model was designed and developed using the ADDIE framework, which comprises five stages, including analysis, design, development, implementation, and evaluation. This educational model represents a scientifically grounded learning design, detailed in an academic paper. To assess its practicality and effectiveness, researchers created a website-based prototype as part of the model’s development—a smartphone application named NEDTA (nursing education diabetic therapeutic application). Field trials are essential to validate the application’s capability to accurately detect early signs of hypoglycemia. Building on this foundation, this study aimed to assess the impact of this HBM-based education on patients’ ability to prevent hypoglycemia in DM.
Materials and Methods
Study design
This quasi-experimental research employed a design and development methodology, utilizing the ADDIE framework as the guiding model. The research process followed a structured sequence of phases, including analysis, design & development, formative evaluation, and evaluation [32].
Subjects
The study was done between February and August 2024 in the service areas of Puskesmas Simpang Kawat and Puskesmas Pakuan Baru. Primary data were gathered via interviews, utilizing questionnaires administered to 36 participants in the intervention group and 36 in the control group. The sample size was determined using the methodology proposed by Sastroasmoro & Ismael [33]:
The sample size was calculated using a formula that incorporated a 5% type I error rate (Zα=1.96) and a 10% type II error rate (Zβ=1.28). Mean values for the pre- and post-intervention groups were referenced from prior work by Song et al. [34], with a pre-intervention average of 9.52, a post-intervention average of 12.11, and a standard deviation of 4.46. Based on these inputs, the calculated sample size (n) was 31.128, which was rounded up to 32 participants. To mitigate the impact of potential dropouts, an additional 10% (four participants) was included, leading to a final count of 36 respondents per group for both the intervention and control groups. Eligibility criteria required participants to own and be proficient in using a smartphone, demonstrate a willingness to cooperate, and provide informed consent for participation.
Instrument
The primary outcome was the capacity to prevent hypoglycemia. Data were gathered through a questionnaire aimed at evaluating the cognitive skills of individuals with DM in managing hypoglycemia prevention. The instrument was adapted from a validated and reliable tool developed by Supadi [35] and underwent thorough validity and reliability testing. Validity assessments demonstrated that all items had correlation coefficients exceeding the threshold value (r table), confirming their validity. Reliability analysis produced a Cronbach’s Alpha score of 0.85, signifying that the questionnaire is highly reliable.
The questionnaire included 20 items, with a score of one given for correct responses and zero for incorrect ones. The scores reflecting the ability to prevent hypoglycemic episodes were treated as ratio data, with a possible range from 0 to 20. These assessments were carried out through both pre-test and post-test evaluations.
The HBM is a design product based on the analysis, design & development, formative evaluation, and evaluation phases. This smartphone-based HBM health education model was implemented to prevent hypoglycemia in patients with DM.
Data collection
The data collection process began with discussions with the development team to revise the existing application by adding images and explanations to the media. The application was then validated by IT experts to ensure that the website-based educational tool was suitable for use in the research [36].
Next, respondents were identified according to the inclusion criteria; 36 DM patients from the Simpang Kawat Puskesmas work area (intervention group) and 36 DM patients from the Pakuan Baru work area (control group).
In the intervention group, a socialization session was conducted to explain the application and its usage on smartphones. Participants were provided with an application manual and video tutorials to ensure they could use the application independently, without the need for researcher assistance. The hypoglycemia prevention application was then installed on the respondents’ smartphones.
Participants were instructed to complete the pre-test items via the application. The intervention, which was grounded in the HBM Health Education Framework, took place over two months, providing participants with sufficient time to explore, engage with, and internalize the information offered in the hypoglycemia prevention application. After two months, a post-test evaluation was conducted. In the control group, a socialization session was held to provide an explanation of DM and hypoglycemia, along with the distribution of a pocketbook on hypoglycemia and its management. A pre-test was then conducted, during which respondents were asked to review and familiarize themselves with the material in the pocketbook. After two months, a post-test evaluation was conducted. Throughout the research activities, the researchers were supported by six enumerators who had been trained for the study.
Data analysis
Descriptive statistics, including mean, standard deviation, minimum, and maximum values, were used to analyze the univariate data for age and duration of DM. For categorical data, such as gender, education level, occupation, history of hypoglycemia, glucometer ownership, and type of DM medication, frequency distributions were calculated. The distribution of the data was first evaluated using the Kolmogorov-Smirnov test, which confirmed that the data followed a normal distribution. Then, inferential statistical analyses, including dependent and independent t-tests, were conducted to compare mean values and assess the mean differences between the two groups. All tests were performed with a significance level set at p<0.05, and data analysis was carried out using SPSS version 23.0.
Findings
The intervention group was younger (59.92±8.80 years) compared to the control group (62.89±7.62 years), with the majority being female. Most participants in the intervention group had a high school education, while the control group was dominated by elementary school graduates. The most common occupation in both groups was housewife. Most individuals in the intervention group had no history of hypoglycemia, whereas glucometers were more commonly owned by the control group. The primary treatment in both groups was oral medication, with the average duration of diabetes being slightly longer in the intervention group compared to the controls (5.22±5.20 vs. 4.00±2.04 years, respectively) (Table 1).
Table 1. Frequency of demographic and clinical characteristics of diabetes mellitus patients
There was an improvement in hypoglycemia prevention scores in both the intervention and control groups. In the intervention group, the average pre-test score was 48.11±6.17, with a median of 47, which significantly rose to 55.89±6.92, with a median of 58, in the post-test (p-value=0.0001). For the control group, the mean pre-test score was 43.170±4.74, with a median of 44, which increased to 45.39±5.92, with a median of 45, in the post-test (p-value=0.0001).
There was a noteworthy difference in hypoglycemia prevention abilities between the intervention and control groups in the post-test. The intervention group had a mean score of 50.64±6.42 for hypoglycemia prevention (p-value=0.0001).
Discussion
This study aimed to assess the impact of this HBM-based education on patients’ ability to prevent hypoglycemia in DM. More than two-thirds of the participants were women. Global studies generally indicate that women are at a higher risk of hypoglycemia than men. According to Yang et al. [37], there is a significant correlation between gender and hypoglycemia, with women experiencing more frequent hypoglycemic episodes. This could be linked to hormonal changes during menopause, such as reduced estrogen and progesterone levels, which may lead to increased fat storage and alterations in lipid profiles, ultimately decreasing insulin sensitivity in the liver and muscles [38, 39]. While some research suggests no significant difference between men and women in detecting hypoglycemic events [40], overall, women tend to be more vulnerable to hypoglycemia.
The majority of participants in the intervention group had a high school education, which likely made it easier for them to understand the information provided by the researchers. Education level is an important factor in knowledge improvement, as individuals with higher education are generally assumed to absorb information more easily. However, education level should not be seen as an indicator of mastery in specific fields but rather as a sign that an individual has completed formal education in a particular area. The ability to prevent hypoglycemia results from the interaction of knowledge, attitudes, and actions regarding hypoglycemia management, which can be gained through personal experiences, others’ experiences, media, or formal education. According to Chrisanto & Agustama [40], education level influences an individual’s ability to understand their health condition. Those with lower education levels may struggle to recognize health issues and understand disease management guidelines, whereas individuals with higher education levels are better equipped to recognize health-related factors and understand the long-term implications for their health.
The participants in the intervention group were, on average, in the elderly age range. This suggests that these individuals had considerable life experience and well-developed decision-making and judgment abilities. However, older adults are more vulnerable to hypoglycemia due to factors such as diminished kidney function, which impairs drug clearance, the use of multiple medications and potential drug interactions, and a decline in cognitive abilities [41]. Cognitive decline in older adults can increase their risk of hypoglycemia, while hypoglycemic episodes can also worsen or contribute to further cognitive impairments [42].
The duration of DM is often directly related to the improvement in experience, particularly for family members living with individuals who have DM. Based on the study results, the average duration of diabetes in the intervention group was just over five years. For the patients themselves, a longer duration of DM increases the likelihood of experiencing hypoglycemia. Over time, individuals with DM tend to have more frequent hypoglycemic episodes, making these experiences a key stimulus for preventing hypoglycemia. The theory of pain behavior suggests that individuals who frequently experience pain or its symptoms are more likely to be attentive to their condition and seek appropriate help [28].
The HBM aims to strengthen the ability of individuals with DM to prevent hypoglycemia. This model is based on the theory of the HBM, which provides a framework for understanding the factors that drive health behaviors and influence whether people follow or ignore health management guidelines. According to the HBM, individuals are more inclined to adopt health-promoting actions if they believe they are at risk (perceived susceptibility), acknowledge the seriousness of the risk (perceived severity), trust that making changes will yield positive outcomes (perceived benefit), and feel confident in overcoming obstacles to adopting healthier behaviors (perceived barriers). Additionally, self-efficacy refers to an individual’s confidence in their ability to take action, improve health, and eliminate harmful habits. Cues to action are the signals or motivations that prompt individuals to initiate change [16]. Research by Shabibi et al. [19] found that using HBM-based educational interventions significantly improves self-care behaviors in individuals with T2DM, demonstrating improvements in perceptions of risk, severity, benefits, barriers, self-efficacy, and overall attitudes toward health management [19, 43, 44].
The NEDTA application was designed to provide individuals with DM the opportunity to learn at their convenience, anytime and anywhere. At the start of the study, not all participants were able to access the application link provided by the researchers. However, the initial socialization meeting facilitated the process by allowing the researchers and their team to assist participants in installing the application on their smartphones. The researchers recognized that effectively utilizing mobile applications for health promotion requires clear communication and commitment-building, ensuring that participants engage fully with each activity. Simply sharing the application link does not guarantee active participation in efforts to maintain health. Therefore, a comprehensive strategy is essential to ensure the effectiveness of smartphone-based education for adults. This includes identifying the participants’ informational needs, defining performance objectives, developing appropriate steps for transferring information through the smartphone, and ultimately evaluating the impact of the intervention on improving the ability of DM patients to detect hypoglycemia.
The intervention aimed at improving the competence of DM patients focuses on providing education about the disease process, treatment, and prevention of hypoglycemic complications. Education is delivered through health promotion, which empowers individuals and communities to maintain and enhance their health. This empowerment goes beyond simply sharing information (such as health education) and includes efforts to change behaviors and attitudes. The involvement of community cadres and Puskesmas in this educational program is crucial, as it enables the community to play an active role in managing DM and improving self-care behaviors among patients. This approach aligns with Indonesian government policy, particularly in the context of the infectious disease prevention and control program. The implementation of a health education model based on the HBM was effective in enhancing the ability of DM patients to prevent hypoglycemia. The intervention demonstrated a significant impact compared to the non-intervention group, indicating that a structured educational approach can help patients better understand and manage the risks associated with hypoglycemia.
This study has several limitations that should be acknowledged. First, the relatively small sample size and the use of purposive sampling may limit the generalizability of the findings to the broader population of diabetes mellitus patients. Second, the intervention was implemented over a relatively short period of two months, which may not fully capture long-term behavioral changes or sustained improvements in hypoglycemia prevention skills. Third, although the use of a smartphone application provides flexibility and accessibility, not all participants may have had equal digital literacy, which could influence their ability to engage optimally with the intervention. Future studies should consider employing larger and more diverse samples, extending the duration of follow-up, incorporating objective measures of behavioral change, and exploring additional factors such as cultural beliefs and family support that may influence the effectiveness of digital health interventions.
Conclusion
The HBM-based education model effectively improves the ability of diabetes mellitus patients to prevent hypoglycemia.
Acknowledgments: The authors would like to thank all participants for their participation and cooperation throughout the study. They also thank the Head of the Health Polytechnic of the Ministry of Health in Jambi for their support and assistance, as well as the researchers, data collection team, enumerator team, and all parties involved in this project.
Ethical Permissions: Participants’ privacy was protected, there was no incentive to engage in the study, and registered prospective respondents signed an informed consent form. The researcher obtained ethical permission before beginning data collection. According to the authors, this study was authorized by the Health Polytechnic of the Ministry of Health in Jambi, under approval number: LB.02.06/2/300.1/2024.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Damayantie N (First Author), Introduction Writer/Original Researcher/Methodologist/Discussion Writer/Statistical Analyst (40%); Ernawati E (Second Author), Original Researcher/Discussion Writer (30%); Dewi M (Third Author), Introduction Writer/Original Researcher/Discussion Writer (30%)
Funding/Support: We did not receive any financial support from any party.
Article Type: Original Research |
Subject:
Technology of Health Education
Received: 2025/01/1 | Accepted: 2025/02/5 | Published: 2025/02/15
Received: 2025/01/1 | Accepted: 2025/02/5 | Published: 2025/02/15
References
1. Kementrian Kesehatan RI. National report of Riskesdas 2013. Jakarta: Badan Penelitian dan Pengembangan Kesehatan; 2013. [Indonesian] [Link]
2. Kementerian Kesehatan RI. Jambi Province Riskesdas 2018 Report. Jakarta: Kementrian Kesehatan RI; 2018. [Indonesian] [Link]
3. Kementrian Kesehatan RI. Indonesian Health Survey (SKI). Jakarta: Badan Kebijakan Pembangunan Kesehatan; 2023. [Indonesian] [Link]
4. American Diabetes Assosiation. Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S256-8. [Link] [DOI:10.2337/dc22-Sdis]
5. Shafiee G, Mohajeri-Tehrani M, Pajouhi M, Larijani B. The importance of hypoglycemia in diabetic patients. J Diabetes Metab Disord. 2012;11:17. [Link] [DOI:10.1186/2251-6581-11-17]
6. Ashfaq Z, Rafay A, Mumtaz R, Zaidi SMH, Saleem H, Zaidi SAR, et al. A review of enabling technologies for Internet of Medical Things (IoMT) ecosystem. AIN SHAMS Eng J. 2022;13(4):101660. [Link] [DOI:10.1016/j.asej.2021.101660]
7. Maranta F, Cianfanelli L, Cianflone D. Glycaemic control and vascular complications in diabetes mellitus type 2. Adv Exp Med Biol. 2021;1307:129-52. [Link] [DOI:10.1007/5584_2020_514]
8. Bellfield EJ, Sharp LK, Xia Y, Gerber BS. Use of a mobile app to facilitate blood glucose monitoring in adolescents with type 1 diabetes: Single-subject nonrandomized clinical trial. JMIR Diabetes. 2018;3(1):e3. [Link] [DOI:10.2196/diabetes.8357]
9. Algahtani FD, Hassan SUN, Alsaif B, Zrieq R. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2021;18(3):847. [Link] [DOI:10.3390/ijerph18030847]
10. Vashist SK. Point-of-care diabetes management softwares and smart applications. In: Point-of-care technologies enabling next-generation healthcare monitoring and management. Cham: Springer; 2019. p. 117-32. [Link] [DOI:10.1007/978-3-030-11416-9_4]
11. Martín-Timón I, Del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes. 2015;6(7):912-26. [Link] [DOI:10.4239/wjd.v6.i7.912]
12. Alifariki LO, Rahmawati R, Sukurni S, Siagian HJ. Comparative study of learning media: Video animation and e-book in education on drugs abuse in students. Health Educ Health Promot. 2023;11(1):141-5. [Link]
13. Fitriani Y, Pristianty L, Hermansyah A. Adopting health belief model theory to analyze the compliance of type 2 diabetes mellitus patient when using insulin injection. Pharm J Indones. 2019;16(2):167-77. [Indonesian] [Link] [DOI:10.30595/pharmacy.v16i2.5427]
14. Muhlisa M, Amira BSA. Kepatuhan medikasi penderita diabetes mellitus berdasarkan teori health belief model (HBM) di diabetes center kota ternate tahun 2017. INTEREST: JURNAL ILMU KESEHATAN. 2018;7(2):144-9. [Indonesian] [Link] [DOI:10.37341/interest.v7i2.23]
15. Anuar H, Shah SA, Gafor H, Mahmood MI, Ghazi HF. Usage of Health Belief Model (HBM) in health behavior: A systematic review. Malays J Med Health Sci. 2020;16(11):201-9. [Link]
16. Champion VL, Skinner CS. The health belief model. In: Health behavior and health education: Theory, research, and practice. Hoboken: Jossey-Bass; 2008. p. 45-65. [Link]
17. Jalilian F, Motlagh FZ, Solhi M, Gharibnavaz H. Effectiveness of self-management promotion educational program among diabetic patients based on health belief model. J Educ Health Promot. 2014;3(1):14. [Link] [DOI:10.4103/2277-9531.127580]
18. Sharifirad G, Entezari MH, Kamran A, Azadbakht L. The effectiveness of nutritional education on the knowledge of diabetic patients using the health belief model. J Res Med Sci. 2009;14(1):1-6. [Link]
19. Shabibi P, Zavareh MSA, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B, et al. Effect of educational intervention based on the Health Belief Model on promoting self-care behaviors of type-2 diabetes patients. Electron Physician. 2017;9(12):5960-8. [Link] [DOI:10.19082/5960]
20. Salber P, Niksch A. Digital health tools for diabetes. J Ambul Care Manag. 2015;38(2):196-9. [Link] [DOI:10.1097/JAC.0000000000000080]
21. Isaacs D, Cox C, Schwab K, Oser TK, Rinker J, Mason MJ, et al. Technology integration: The role of the diabetes care and education specialist in practice. Diabetes Educ. 2020;46(4):323-34. [Link] [DOI:10.1177/0145721720935123]
22. Mayer RE. Multimedia learning. 3rd ed. Cambridge: Cambridge University Press; 2020. [Link] [DOI:10.1017/9781108894333.003]
23. Stanger C, Kowatsch T, Xie H, Nahum-Shani I, Lim-Liberty F, Anderson M, et al. A digital health intervention (SweetGoals) for young adults with type 1 diabetes: Protocol for a factorial randomized trial. JMIR Res Protoc. 2021;10(2):e27109. [Link] [DOI:10.2196/27109]
24. Sukma FJ, Hidayati IR, Pristianty L. Behavioral factor analysis of the accuracy in using gastritis drugs at the Puskesmas Arjuno in Malang City with the Health Belief Model (HBM) approach. FARMASAINS. 2021;6(1):15-9. [Link]
25. Tavsanli NG, Karadacovan A, Saygili F. The use of videophone technology (telenursing) in the glycaemic control of diabetic patients: A randomized controlled trial. J Diabetes Res Clin Metab. 2013;2(1):1. [Link] [DOI:10.7243/2050-0866-2-1]
26. Mehraeen E, Mehrtak M, Janfaza N, Karimi A, Heydari M, Mirzapour P, et al. Design and development of a mobile-based self-care application for patients with type 2 diabetes. J Diabetes Sci Technol. 2022;16(4):1008-15. [Link] [DOI:10.1177/19322968211007124]
27. Jahanbakhsh M, Ehteshami A, Afkhami S. Developing "Aryan": Diabetes self-care mobile application. Int J Prev Med. 2019;10(1):59. [Link] [DOI:10.4103/ijpvm.IJPVM_344_17]
28. Bonoto BC, De Araújo VE, Godói IP, De Lemos LLP, Godman B, Bennie M, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth. 2017;5(3):e4. [Link] [DOI:10.2196/mhealth.6309]
29. Baron JS, Hirani S, Newman SP. A randomised, controlled trial of the effects of a mobile telehealth intervention on clinical and patient-reported outcomes in people with poorly controlled diabetes. J Telemed Telecare. 2017;23(2):207-16. [Link] [DOI:10.1177/1357633X16631628]
30. Jeon E, Park HA. Experiences of patients with a diabetes self-care app developed based on the information-motivation-behavioral skills model: Before-and-after study. JMIR Diabetes. 2019;4(2):e11590. [Link] [DOI:10.2196/11590]
31. Mufidah A, Kurniawati ND, Widyawati IY. Smartphones as educational media for diabetes mellitus patients: A systematic review. J Health Res FORIKES VOICE. 2021;12(1):89-92. [Indonesian] [Link]
32. Rusdi M. Educational treatment-based research. Depok: Rajawali; 2020. [Indonesian] [Link]
33. Sastroasmoro S, Ismael S. Basics of clinical research methodology. Selection of research subjects and research design. Jakarta: Sagung Seto; 2010. [Indonesian] [Link]
34. Song Y, Nam S, Park S, Shin IS, Ku BJ. The impact of social support on self-care of patients with diabetes: What is the effect of diabetes type? Systematic review and meta-analysis. Diabetes Educ. 2017;43(4):396-412. [Link] [DOI:10.1177/0145721717712457]
35. Supadi S. The study of some factors relating to clients abilities to detect hypoglycaemia episodic with diabetes mellitus at the margono soekarjo purwokerto. JURNAL KESMASINDO. 2011;4(2):119-36. [Indonesian] [Link]
36. Damayantie N, Ernawati E, Dewi M, Fahmi I. Nursing education on diabetes through smartphone therapeutic applications. Health Educ Health Promot. 2024;12(1):9-15. [Link]
37. Yang A, Wu H, Lau ESH, Zhang X, Shi M, Fan B, et al. Glucose-lowering drug use, glycemic outcomes, and severe hypoglycemia: 18-Year trends in 0.9 million adults with Diabetes in Hong Kong (2002-2019). Lancet Reg Health West Pac. 2022;26:100509. [Link] [DOI:10.1016/j.lanwpc.2022.100509]
38. Al-Azzawi F, Palacios S. Hormonal changes during menopause. Maturitas. 2009;63(2):135-7. [Link] [DOI:10.1016/j.maturitas.2009.03.009]
39. Burger HG, Dudley EC, Robertson DM, Dennerstein L. Hormonal changes in the menopause transition. Recent Prog Horm Res. 2002;57:257-75. [Link] [DOI:10.1210/rp.57.1.257]
40. Chrisanto EY, Agustama A. Self-management behaviour of diabetic foot ulcer occurrence among patient with type 2 diabetes mellitus. Holistik J Kesehat. 2020;14(3):391-400. [Indonesian] [Link] [DOI:10.33024/hjk.v14i3.1888]
41. Böhm AK, Jensen ML, Sørensen MR, Stargardt T. Real-world evidence of user engagement with mobile health for diabetes management: Longitudinal observational study. JMIR mHealth uHealth. 2020;8(11):e22212. [Link] [DOI:10.2196/22212]
42. Abdelhafiz AH, Rodríguez-Mañas L, Morley JE, Sinclair AJ. Hypoglycemia in older people-a less well recognized risk factor for frailty. Aging Dis. 2015;6(2):156-67. [Link] [DOI:10.14336/AD.2014.0330]
43. Vazini H, Barati M. The health belief model and self-care behaviors among type 2 diabetic patients. Iran J Diabetes Obes. 2014;6(3):107-13. [Link]
44. Dehghani-Tafti A, Mahmoodabad SSM, Morowatisharifabad MA, Ardakani MA, Rezaeipandari H, Lotfi MH. Determinants of self-care in diabetic patients based on health belief model. Glob J Health Sci. 2015;7(5):33-42. [Link] [DOI:10.5539/gjhs.v7n5p33]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |