Volume 13, Issue 1 (2025)
Health Educ Health Promot 2025, 13(1): 61-69 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Oktaviza Y, Yunus M, Ibrahim M, Chan S. Integrating Advanced Technology and Lean Six Sigma for Enhanced Hospital Management and Operations. Health Educ Health Promot 2025; 13 (1) :61-69
URL: http://hehp.modares.ac.ir/article-5-78433-en.html
URL: http://hehp.modares.ac.ir/article-5-78433-en.html
1- Management Department, Economic and Business Faculty, Syiah Kuala University, Aceh, Indonesia
Full-Text [PDF 1081 kb]
(459 Downloads)
| Abstract (HTML) (532 Views)
Full-Text: (34 Views)
Introduction
Hospitals are essential to public health, delivering vital services and contributing significantly to national health development goals, including the achievement of the Sustainable Development Goals. In Indonesia, hospitals play a crucial role in strengthening health service systems, particularly in reducing maternal and child mortality [1]. However, these institutions face increasing operational challenges stemming from rapid technological advancements, evolving patient expectations, and resource constraints [2]. Therefore, efficient management is critical for ensuring the continued delivery of high-quality, accessible healthcare services.
Lean six sigma (LSS), a methodology that emphasizes waste reduction and process optimization, has demonstrated efficacy in improving efficiency and patient satisfaction across various industries, including healthcare [3, 4]. Existing studies on LSS in healthcare primarily focus on its application in developed countries, where healthcare systems and operational contexts differ significantly from those in Indonesia. Research addressing the implementation of LSS in Indonesian hospitals is scarce, with limited attention given to the unique challenges faced by these institutions, such as resource constraints, high patient loads, and cultural resistance to change [5, 6]. Furthermore, while previous studies highlight the general benefits of LSS in improving efficiency and patient satisfaction, there is a lack of specific investigations into its practical application in general polyclinic settings, where operational inefficiencies, such as excessive patient waiting times and staff shortages, are most pronounced. This gap in the literature underscores the need for context-specific research to explore how LSS methodologies can be effectively tailored to address the operational realities of Indonesian hospitals.
This research addressed this gap by investigating the application of LSS at Ibnu Sina Hospital in Banda Aceh, Indonesia, focusing on the specific operational challenges faced by the general polyclinic, such as excessive patient waiting times exceeding 90 minutes, staff shortages, and inadequate resources [1, 7]. LSS provides a structured approach to identifying and eliminating inefficiencies in hospital operations. For instance, by employing tools, such as value stream mapping, LSS can help pinpoint bottlenecks in patient workflows, thereby reducing excessive waiting times. Additionally, techniques, like workload balancing and process standardization enable hospitals to optimize staffing levels, ensuring that available resources are utilized efficiently without overburdening employees. LSS also supports better inventory management through data-driven decision-making, which can address issues such as inadequate medicine stocks. By streamlining processes and minimizing waste, LSS helps healthcare institutions deliver high-quality, timely services despite resource constraints.
According to data from Ibnu Sina Hospital, there are significant discrepancies between ideal service standards and actual performance. The ideal waiting time is less than 60 minutes, whereas the actual waiting time is 90 minutes. Physicians are expected to adhere to an on-time schedule; however, this is often delayed. The ideal staffing level is three administrative staff members, but only one is available. The examination tools are supposed to number five, but only three are functional. Ideally, patient satisfaction should be 90%, but it is currently 70%. The medicine stock is intended to cover 200 units, yet it only covers 150 patients. Finally, the emergency response time should be ≤5 minutes, but it is currently 15 minutes. These discrepancies indicate the significant challenges in maintaining service quality and efficiency in hospitals.
Ibnu Sina Hospital was chosen for this study due to its unique combination of operational challenges and its representativeness of mid-sized hospitals in Indonesia. The hospital faces critical inefficiencies, such as prolonged patient waiting times, insufficient staffing, and resource limitations, which are common issues in many Indonesian healthcare facilities. As a general polyclinic, it serves a diverse patient population, making it an ideal case study to explore the broader applicability of LSS in similar settings across the country. Additionally, its willingness to engage in process improvement initiatives provides a valuable opportunity to assess LSS methodologies in a real-world Indonesian healthcare context.
This research examined the implementation of LSS methodologies to boost operational efficiency and enhance service quality at Ibnu Sina Hospital. The study focused on the practical application of LSS within Indonesia’s healthcare system, exploring the use of techniques like value stream mapping to identify and reduce non-value-adding activities in patient care workflows [8]. Acknowledging the specific challenges associated with adopting LSS in healthcare environments, this investigation addressed issues, such as resistance to change rooted in organizational culture and the importance of employee involvement [9, 10]. The research specifically explored how deeply embedded customs and procedures within hospitals can impede process improvement initiatives and examined how leadership behavior can facilitate cultural transformation and nurture an environment of ongoing improvement [10, 11].
Additionally, this study sought to assess LSS’s capacity to improve operational performance, decrease patient wait times, and elevate overall service quality at Ibnu Sina Hospital [12]. By offering a comparative analysis of LSS applications across various hospital settings, both domestically and internationally [13], this research contributed to the existing knowledge base and provided valuable insights for hospital administrators and policymakers [14, 15]. The purpose of this study was to examine how LSS methodologies can enhance operational efficiency and service quality in healthcare settings. By focusing on the case of Ibnu Sina Hospital, the research aimed to provide evidence-based insights into the practical application of LSS principles. These findings are expected to inform healthcare policy at both national and regional levels, offering a framework for integrating LSS strategies into broader healthcare improvement initiatives. Furthermore, the study aimed to contribute to the development of standardized guidelines for process optimization in public and private hospitals, ultimately improving resource utilization, patient outcomes, and advancing Indonesia’s progress toward achieving the Sustainable Development Goals related to health and well-being.
Materials and Methods
This mixed-method case study investigated the application of LSS, a process enhancement methodology, in hospitals across Aceh, Indonesia in 2024, with a focus on its impact on managerial and operational efficiency. Using a case study approach, the research provided an in-depth analysis of the implementation process, its effects on various stakeholders, and the outcomes achieved. This comprehensive approach captures the context-specific factors influencing the adoption and efficacy of LSS in a practical healthcare setting.
Data collection methods included semi-structured interviews with hospital personnel and patients, direct observations of hospital functions, and an examination of relevant documents. Observations targeted patient wait times at critical entry points, particularly the general polyclinic for internal medicine services and the pharmacy unit, to identify operational inefficiencies and bottlenecks.
Time of study and sample size
The research was conducted over three months, from August to October 2024, allowing sufficient time for observing outpatient processes, conducting interviews, and capturing variations in hospital operations. Observations involved 50 patients selected to effectively represent the outpatient processes at Ibnu Sina Hospital. While no formal statistical method was used for sample size calculation, a pragmatic approach was adopted, considering daily patient volumes and the feasibility of detailed observations within the study period. In qualitative research, sample sizes are guided by data saturation, where data collection ceases once no new information or themes emerge [16].
The study employed a purposive and pragmatic sampling approach [17]. Patients were selected during routine outpatient operations to ensure that diverse interactions and process flow variations were captured. Seven key stakeholders, including the hospital director, an internal medicine specialist, the head of care, the administration and finance manager, the service manager, a general polyclinic patient, and an ER Patient, were interviewed. Their selection was based on their capacity to provide critical insights into LSS implementation, operational challenges, and hospital practices. This strategy ensured a balanced collection of qualitative and observational data, with observational studies focusing on inefficiencies and interviews providing deeper context. Document analysis supplemented these findings, offering robust evidence for examining hospital operations and the impacts of LSS.
Data collection and analysis
Value stream mapping, a LSS tool, was the primary analytical method, enabling the visualization of patient flow, identification of inefficiencies, and determination of areas for improvement. The study maintained methodological rigor through data triangulation, member checking, and a documented audit trail. Findings were presented narratively, offering detailed insights into lean six sigma’s effects on hospital operations, specifically in reducing wait times and enhancing efficiency. The research contributes to the broader knowledge of LSS in healthcare, providing actionable recommendations for improving hospital performance and patient outcomes.
Observational data served as a basis for interviews, fostering a comprehensive understanding of waiting times and bottlenecks, particularly in the pharmacy unit. All methodological stages were framed within LSS principles, ensuring the optimization of hospital operations and the enhancement of patient care quality.
Findings
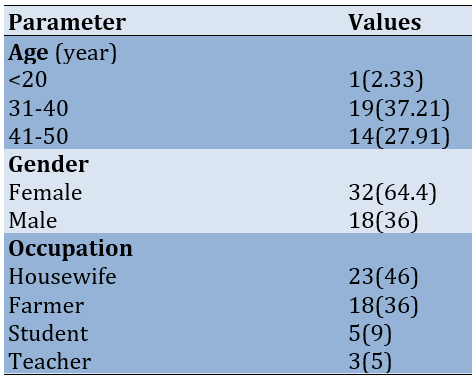
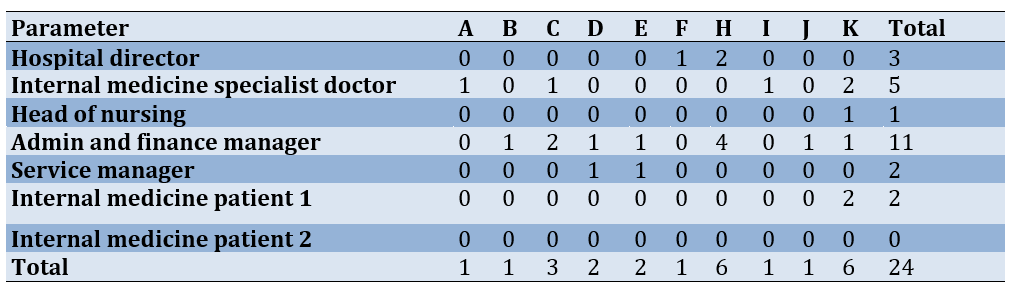
The age distribution indicated that the majority of respondents were within the productive age group, suggesting active participation in healthcare-related decisions. Females formed a significant proportion of the sample, reflecting their prominent role in managing family health and well-being. In terms of occupation, housewives and farmers dominated the respondent pool, while students and teachers represented smaller groups. These demographic insights underscore the diversity of the sample and provide context for understanding their perspectives in the study (Table 1).
Table 1. Frequency of respondents’ demographics
A significant portion of time was spent waiting, which constituted the majority of the overall duration, especially during critical points, such as waiting for the doctor’s examination and picking up medicine at the pharmacy. Value-added activities, which directly contribute to patient care, accounted for only a small fraction of the total time. Non-value-added activities were also evident but were overshadowed by wasted time, particularly in stages involving registration, the doctor’s examination, and pharmacy services. This breakdown underscores the need for process improvements to minimize wasted time and enhance the efficiency of patient flow, focusing on reducing delays in key bottleneck areas while increasing the proportion of value-added activities (Table 2).
Table 2. Patient flow analysis: Time consumption and value assessment
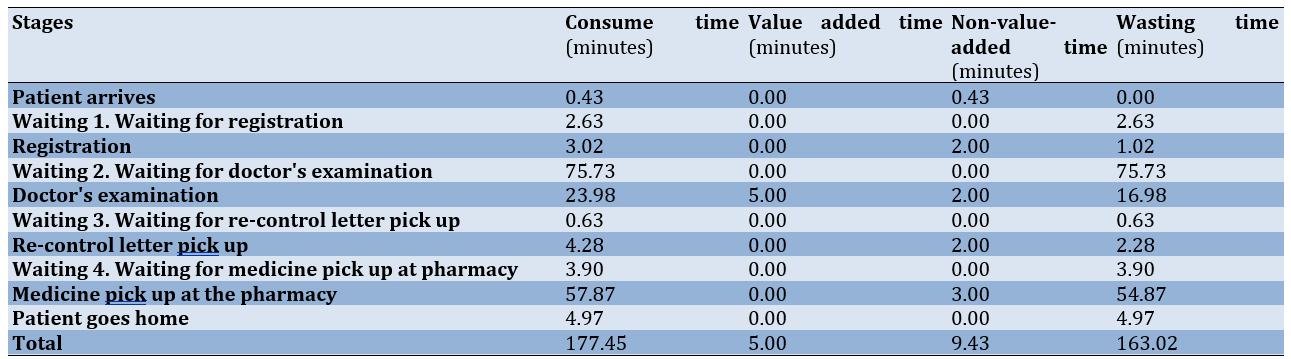
The value stream mapping before the intervention, focusing on the registration process, took 3.02 minutes. Of this time, 1.02 minutes were classified as non-value-added due to the manual printing of medical records. Administrative procedures contributed an additional 2 minutes of non-value-added time, with the physical printing process emerging as a critical bottleneck. Implementing technological solutions, such as automated documentation systems, could significantly streamline this stage by reducing manual handling and minimizing delays. Waiting for physician examination constituted the most substantial delay, averaging 75.73 minutes, all classified as non-value-added time. This delay is primarily attributed to physician scheduling limitations and personnel availability, which are often constrained by multi-facility commitments. Addressing this issue necessitates systemic solutions, including optimized scheduling and increased specialist staffing, to mitigate patient waiting times and enhance the overall experience (Figure 1).
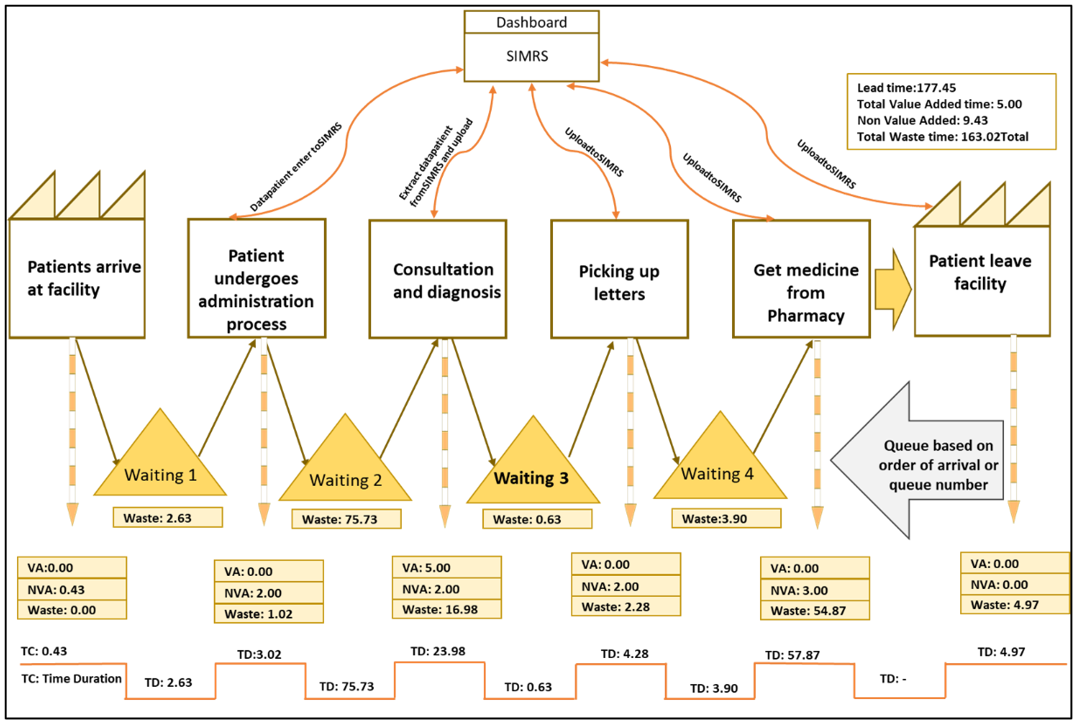
Figure 1. Value stream mapping before the intervention
Medication dispensing at the pharmacy averaged 57.87 minutes, with 54.87 minutes identified as non-value-added time due to manual drug compounding and queuing. The implementation of an e-prescription system and a drug delivery service for compounded medications is recommended. E-prescriptions can expedite dispensing, while drug delivery can reduce on-site waiting times. Overall, of the total 177.45 minutes, only 5 minutes were value-added, with the remainder consumed by non-value-added and wasted time. Value stream mapping underscores the imperative for process streamlining, automation, workforce augmentation, and process optimization to minimize non-value-added activities and enhance outpatient unit productivity, ultimately improving the patient experience.
Reduced hospital wait times through strategic technological integration were observed (Figure 2). The linking of the hospital management information system (SIMRS) with the BPJS JKN app enabled seamless queue management by automatically recording patient registrations, streamlining processes, and providing real-time updates on queue numbers and wait times. Additional systems, such as WhatsApp-based registration and integration with laboratory information management systems (LIMS) and radiology platforms, further enhanced efficiency by improving data handling and coordination. These advancements, though part of an ongoing digital transition, were already improving service delivery, transparency, and patient satisfaction while reducing delays across departments.
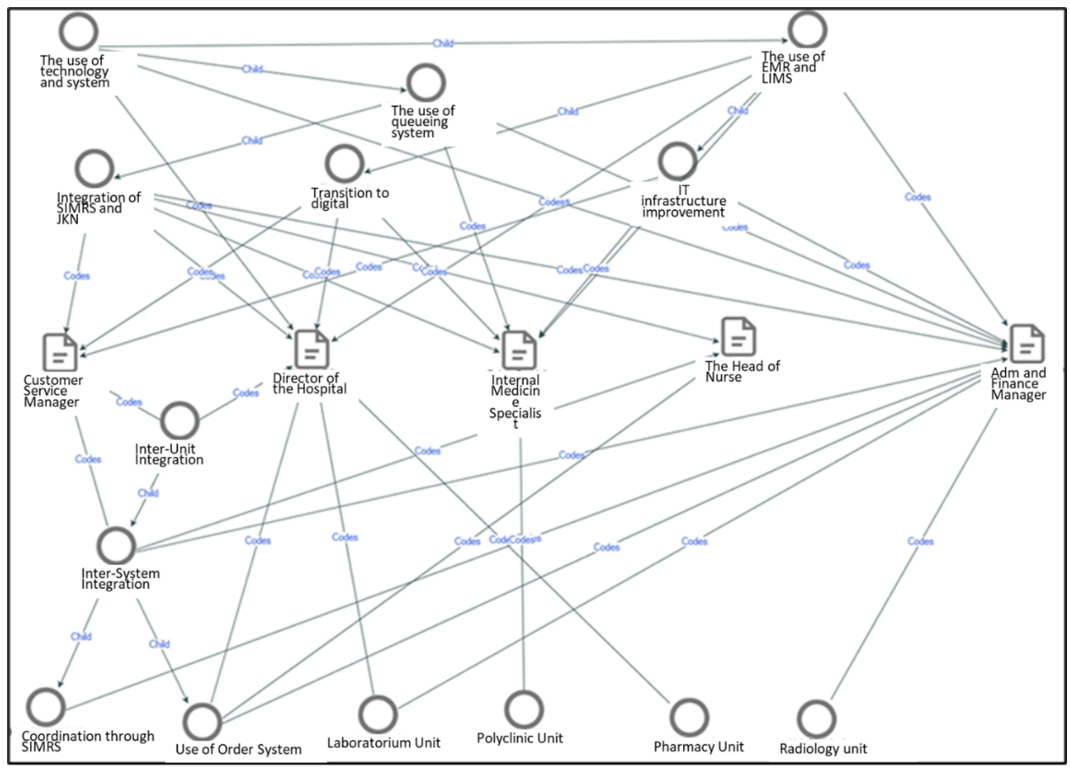
Figure 2. Intervention in technology to reduce wasting time
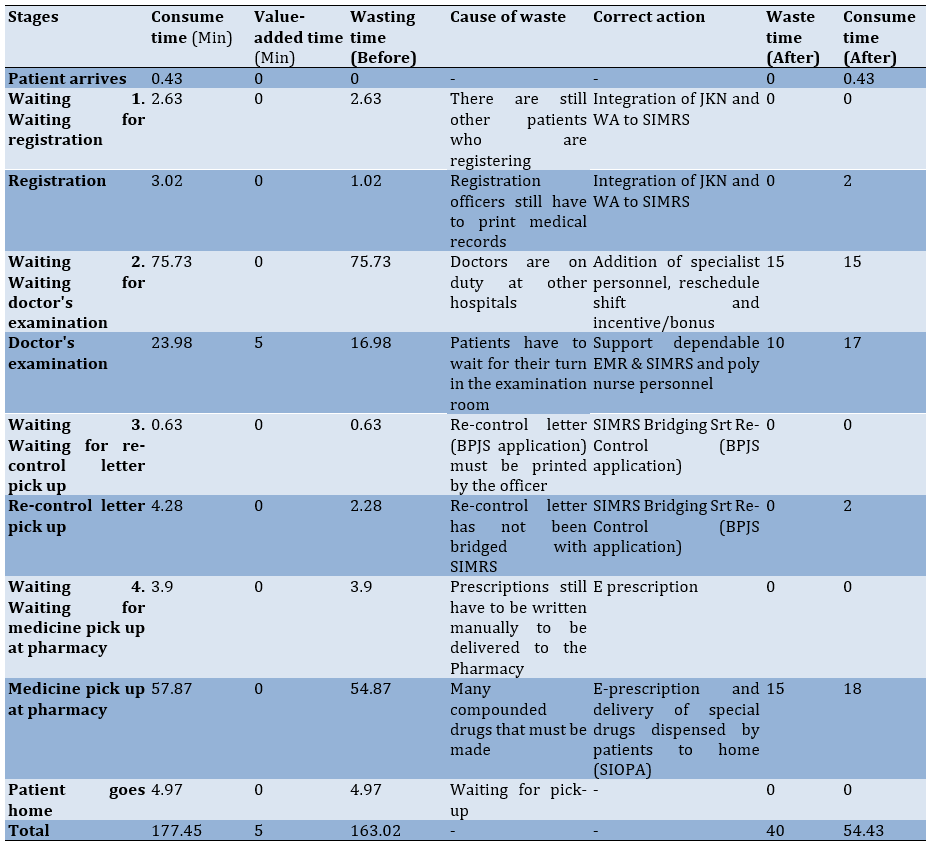
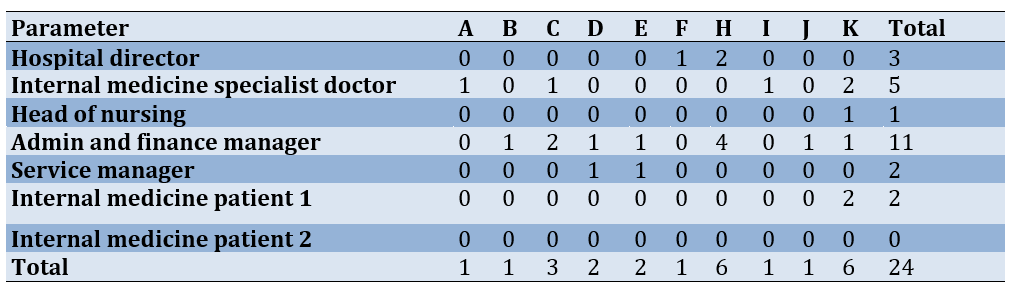
Key suggestions included increasing the number of specialists during peak hours to address the daily patient influx, empowering nurses to handle administrative tasks to allow doctors to focus on medical evaluations, and offering incentives and adjusted working hours for doctors to extend their availability. Additionally, initiatives, like the SIOPA program for home medication delivery, increasing radiology and laboratory staff, adding beds for advanced exams, and optimizing consultation durations were proposed. These strategies aimed to streamline processes, reduce backlogs, and improve overall service efficiency (Table 3).
Table 3. Suggestions to reduce wasting time from a Huma resource development (HRD) perspective
A comprehensive process analysis of the outpatient unit at Ibnu Sina Hospital is imperative for a thorough understanding of patient service efficiency. This analysis quantifies patient wait times across various service stages, from arrival to prescription collection, and identifies areas of temporal inefficiency. Through a systematic evaluation of these stages, the study aimed to elucidate inefficiencies and propose evidence-based solutions for optimizing patient flow. We showed the synergistic benefits of integrating technological advancements with targeted human resource strategies to address scheduling challenges, ultimately enhancing patient care and reducing waiting times.
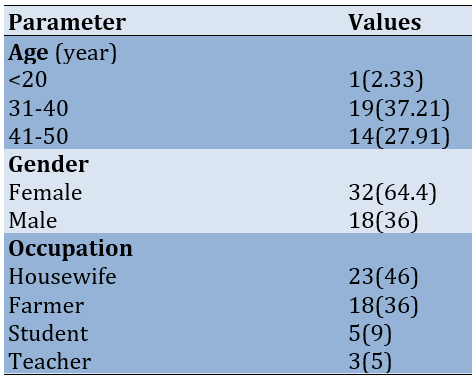
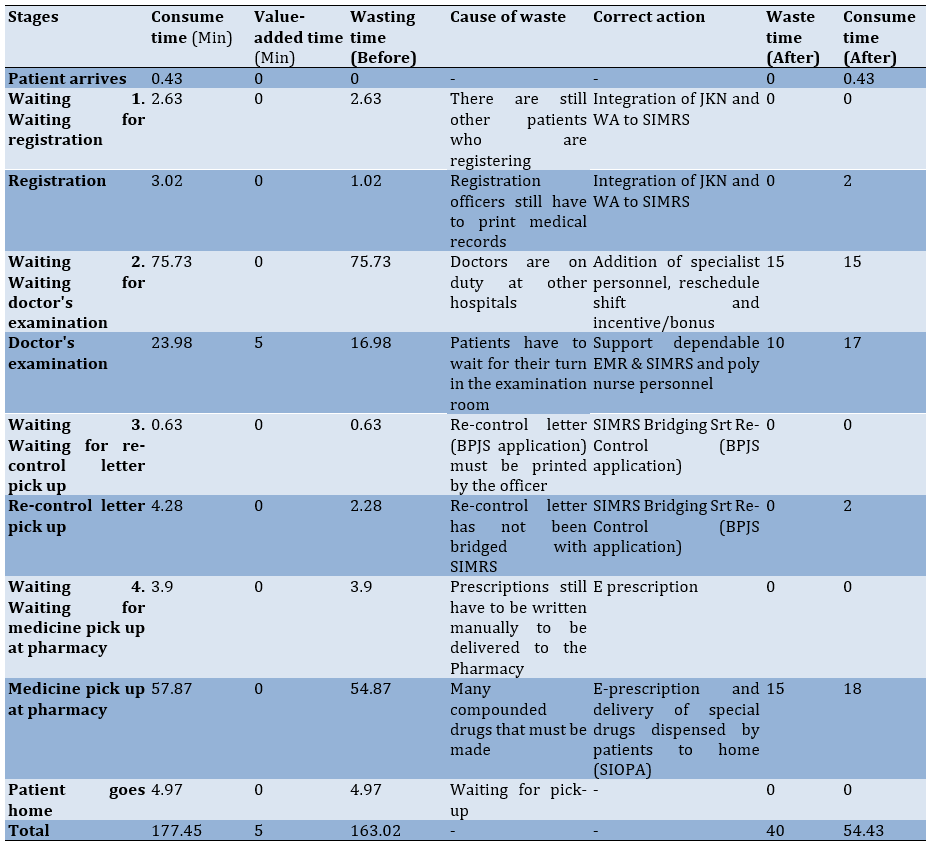
Patient arrival was highly efficient (0.43 minutes) with no non-value-added time. The pre-improvement registration wait time (2.63 minutes) was entirely non-value-added; however, integrating JKN and WhatsApp within SIMRS eliminated this wait, consistent with technology’s role in streamlining registration. While registration time decreased from 3.02 to 2 minutes post-improvement, some administrative processing time persists. The pre-improvement doctor examination wait time (75.73 minutes) was significantly reduced to 15 minutes by adding specialists, rescheduling shifts, and providing incentives, demonstrating the effectiveness of labor-based solutions for scheduling challenges. While EMR, SIMRS, and additional nursing staff reduced non-value-added time during examinations from 16.98 to 10 minutes, total examination time remained relatively consistent at approximately 17 minutes (Figure 3).
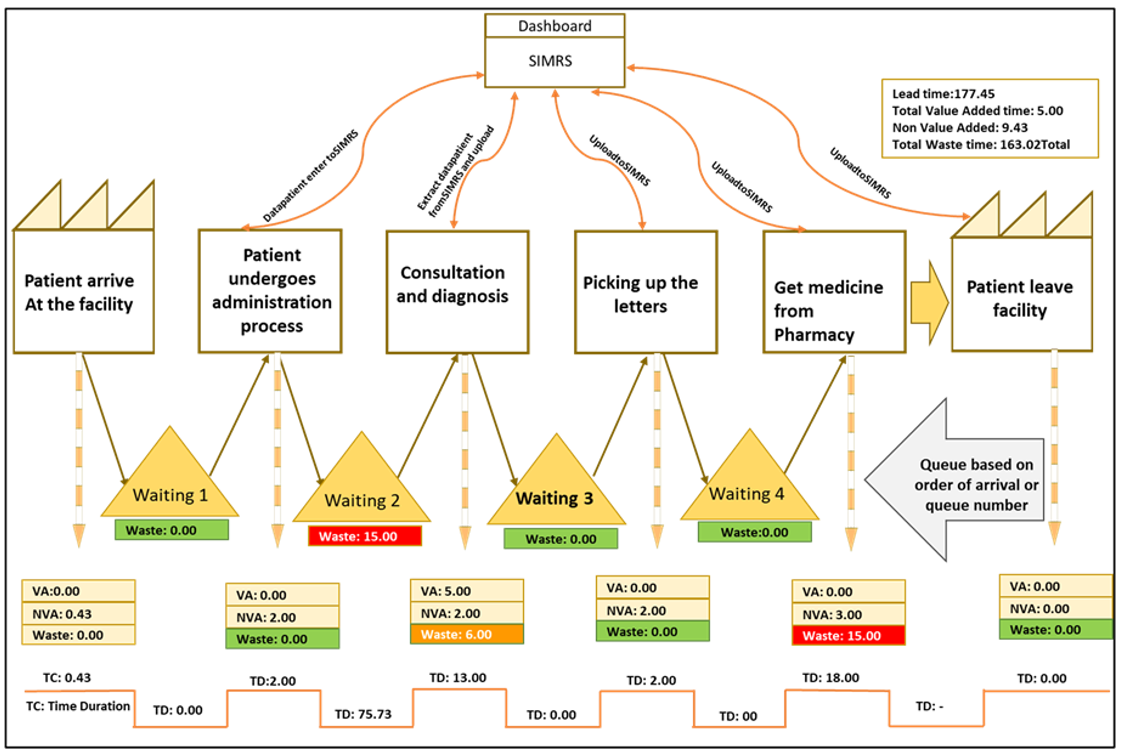
Figure 3. Value stream mapping after the intervention.
Pre-improvement pharmacy wait times (57.87 minutes, with 54.87 minutes classified as non-value-added) significantly reduced to 18 minutes following the implementation of e-prescriptions and the SIOPA drug delivery service, highlighting the effectiveness of technology and logistics-based improvements. The residual wait time was attributed to the complexities of drug compounding. Overall, total time spent decreased from 177.45 minutes (163.02 minutes non-value-added) to 54.43 minutes (40 minutes non-value-added) post-improvement, demonstrating a significant reduction in non-value-added time.
The analysis highlighted various stages of the patient journey, identifying time consumption and waste before interventions, as well as the corrective actions taken to reduce inefficiencies. Key improvements included integrating systems for patient registration, enhancing specialist availability, supporting electronic medical records (EMR) and scheduling, and introducing e-prescriptions for the pharmacy. These changes significantly reduced waiting times, particularly in areas such as registration, doctor’s examination, and medicine pickup. Overall, the interventions resulted in a reduction of wasted time and a more efficient process, improving both patient flow and service delivery (Table 4).
Table 4. Patient flow analysis: Time consumption and value assessment before and after improvements
Discussion
This study investigated the application of lean six sigma principles, specifically value stream mapping, to enhance efficiency and service quality at Ibnu Sina Hospital in Indonesia. Despite these improvements, some stages of the outpatient process, such as doctor consultations and pharmacy services, continue to experience residual delays due to the high demand for specialized personnel and the complexity of manual prescription processes. The addition of specialist doctors and support staff, along with optimized shift scheduling, has alleviated some delays but highlights the need for further structural changes to achieve lasting operational efficiency. The persistence of certain inefficiencies, even after improvements, suggests that while technology can address many surface-level issues, more in-depth workforce and process management strategies are needed to tackle these core challenges fully [15]. While EMR technology has reduced administrative time, examination times remain relatively long due to the inherent complexity and precision required for medical evaluations.
This research contributes valuable insights into the potential of LSS in healthcare and underscores the importance of combining digital integration with strategic workforce management to create a more streamlined patient journey. By systematically examining each stage and implementing targeted improvements, healthcare institutions, like Ibnu Sina General Hospital can not only enhance their service quality but also foster a more patient-centered environment that aligns with broader public health goals. This approach offers a scalable model for other hospitals seeking to improve efficiency and patient satisfaction through a combination of technological and operational advancements [16].
Efficient patient wait time management is crucial for optimizing healthcare service delivery [17]. Leveraging technological advancements offers several strategies to achieve this. Integrating existing systems, such as the SIMRS with the BPJS JKN application, can significantly enhance registration and queue management capabilities. This integration, coupled with alternative registration methods like WhatsApp, contributes to a more streamlined patient experience and reduced wait times.
A key strategy for wait time reduction involves integrating online platforms like SIMRS and the BPJS JKN app [18, 19]. This integration facilitates seamless queue management by automatically registering JKN patients within SIMRS, thereby enhancing efficiency [20]. Additionally, WhatsApp-based registration, whether via text or voice call, allows operators to input patient details into SIMRS, providing real-time queue updates and estimated wait times. This transparency effectively manages patient expectations and contributes to wait time reduction [21, 22].
This research investigated the integration of advanced technology and LSS principles to enhance hospital management and operations [23, 24]. The study reviewed relevant literature, established a defined methodology, and presented the resulting impact on key hospital performance indicators. A detailed discussion analyzed these improvements, explored underlying mechanisms, and acknowledged study limitations while suggesting future research directions [25]. The conclusion summarized key findings and emphasizes practical implications for improved hospital management and operational efficiency [26, 27].
To address protracted patient wait times at the polyclinic, several strategic recommendations have been proposed. These suggestions, derived from input by specialist physicians, nurse managers, and administrative personnel, focused on enhancing service efficiency through resource optimization [19]. A key recommendation is to increase specialist availability during peak hours to minimize patient backlog, particularly given the daily influx of approximately 90 patients. Furthermore, empowering nurses to assume administrative responsibilities can streamline processes, enabling physicians to dedicate more time to medical evaluations. This dual approach of augmenting specialist availability and expanding nursing roles aimed to expedite patient services and improve overall care delivery.
Enhanced resource allocation within the polyclinic, specifically increasing the number of available specialists during peak hours, was recommended by a cohort of stakeholders, including two specialist physicians, the head of nursing, the administrative and financial manager, and a patient representative [28, 29]. This strategic increase aims to minimize patient backlog, particularly given the average daily patient volume of approximately 90. Furthermore, empowering nursing staff to manage administrative tasks, such as pre- and post-examination data entry within the Electronic Medical Record system, was proposed. This delegation of administrative duties allows physicians to focus primarily on medical evaluations, thereby expediting the service process [30, 31]. Incentivizing extended physician availability through adjusted work schedules, as suggested by the administrative, financial, and service managers, offers an additional avenue for mitigating patient backlog. For instance, extending the shifts of morning emergency department physicians into the afternoon could provide support during peak hours and subsequently reduce wait times [32, 33]. Ancillary initiatives include the SIOPA medication home delivery program, which aims to minimize pharmacy wait times, increasing radiology and laboratory staffing, providing additional on-site examination resources (e.g., EKG beds), and optimizing consultation durations. While acknowledging the complexities of reducing consultation times, expanding the number of operational polyclinic outlets has been suggested to improve patient flow and further reduce wait times [34, 35].
The integration of digital solutions such as JKN, WhatsApp, and SIMRS has proven effective in reducing waiting times for registration and prescription pickup, demonstrating the value of technology in healthcare process optimization.
This study offers valuable insights into the integration of Lean Six Sigma principles and digital tools at Ibnu Sina Hospital; however, it is constrained by several limitations. Despite improvements, residual delays in doctor consultations and pharmacy services persist due to high demand for specialized personnel and the complexities of manual prescription processes, indicating that technological enhancements alone cannot resolve deep-rooted operational issues. Moreover, as the research was confined to a single hospital, the generalizability of its findings is limited, and different institutions may experience varying outcomes based on their unique operational structures and patient demographics. Finally, external factors such as policy shifts and demographic variations were not fully considered, underscoring the need for future research to adopt multi-center approaches and comprehensive workforce management strategies for sustainable efficiency gains
Conclusion
There are significant inefficiencies in the outpatient process flow at Ibnu Sina General Hospital, particularly in patient waiting times and manual administrative tasks.
Acknowledgments: The authors thank the Ibnu Sina Hospital management and staff for their support and cooperation during this research.
Ethical Permissions: This study was approved by the Ethical Committee of Ibnu Sina Hospital (2023-04-IRB).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Yenni Oktaviza Y (First Author), Introduction Writer/Methodologist/Main Researcher /Discussion Writer (50%); Yunus M (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Ibrahim M (Third Author), Assistant Researcher/Discussion Writer (15%); Chan S (Fourth Author), Introduction Writer/Discussion Writer (10%)
Funding/Support: No Funding was received.
Hospitals are essential to public health, delivering vital services and contributing significantly to national health development goals, including the achievement of the Sustainable Development Goals. In Indonesia, hospitals play a crucial role in strengthening health service systems, particularly in reducing maternal and child mortality [1]. However, these institutions face increasing operational challenges stemming from rapid technological advancements, evolving patient expectations, and resource constraints [2]. Therefore, efficient management is critical for ensuring the continued delivery of high-quality, accessible healthcare services.
Lean six sigma (LSS), a methodology that emphasizes waste reduction and process optimization, has demonstrated efficacy in improving efficiency and patient satisfaction across various industries, including healthcare [3, 4]. Existing studies on LSS in healthcare primarily focus on its application in developed countries, where healthcare systems and operational contexts differ significantly from those in Indonesia. Research addressing the implementation of LSS in Indonesian hospitals is scarce, with limited attention given to the unique challenges faced by these institutions, such as resource constraints, high patient loads, and cultural resistance to change [5, 6]. Furthermore, while previous studies highlight the general benefits of LSS in improving efficiency and patient satisfaction, there is a lack of specific investigations into its practical application in general polyclinic settings, where operational inefficiencies, such as excessive patient waiting times and staff shortages, are most pronounced. This gap in the literature underscores the need for context-specific research to explore how LSS methodologies can be effectively tailored to address the operational realities of Indonesian hospitals.
This research addressed this gap by investigating the application of LSS at Ibnu Sina Hospital in Banda Aceh, Indonesia, focusing on the specific operational challenges faced by the general polyclinic, such as excessive patient waiting times exceeding 90 minutes, staff shortages, and inadequate resources [1, 7]. LSS provides a structured approach to identifying and eliminating inefficiencies in hospital operations. For instance, by employing tools, such as value stream mapping, LSS can help pinpoint bottlenecks in patient workflows, thereby reducing excessive waiting times. Additionally, techniques, like workload balancing and process standardization enable hospitals to optimize staffing levels, ensuring that available resources are utilized efficiently without overburdening employees. LSS also supports better inventory management through data-driven decision-making, which can address issues such as inadequate medicine stocks. By streamlining processes and minimizing waste, LSS helps healthcare institutions deliver high-quality, timely services despite resource constraints.
According to data from Ibnu Sina Hospital, there are significant discrepancies between ideal service standards and actual performance. The ideal waiting time is less than 60 minutes, whereas the actual waiting time is 90 minutes. Physicians are expected to adhere to an on-time schedule; however, this is often delayed. The ideal staffing level is three administrative staff members, but only one is available. The examination tools are supposed to number five, but only three are functional. Ideally, patient satisfaction should be 90%, but it is currently 70%. The medicine stock is intended to cover 200 units, yet it only covers 150 patients. Finally, the emergency response time should be ≤5 minutes, but it is currently 15 minutes. These discrepancies indicate the significant challenges in maintaining service quality and efficiency in hospitals.
Ibnu Sina Hospital was chosen for this study due to its unique combination of operational challenges and its representativeness of mid-sized hospitals in Indonesia. The hospital faces critical inefficiencies, such as prolonged patient waiting times, insufficient staffing, and resource limitations, which are common issues in many Indonesian healthcare facilities. As a general polyclinic, it serves a diverse patient population, making it an ideal case study to explore the broader applicability of LSS in similar settings across the country. Additionally, its willingness to engage in process improvement initiatives provides a valuable opportunity to assess LSS methodologies in a real-world Indonesian healthcare context.
This research examined the implementation of LSS methodologies to boost operational efficiency and enhance service quality at Ibnu Sina Hospital. The study focused on the practical application of LSS within Indonesia’s healthcare system, exploring the use of techniques like value stream mapping to identify and reduce non-value-adding activities in patient care workflows [8]. Acknowledging the specific challenges associated with adopting LSS in healthcare environments, this investigation addressed issues, such as resistance to change rooted in organizational culture and the importance of employee involvement [9, 10]. The research specifically explored how deeply embedded customs and procedures within hospitals can impede process improvement initiatives and examined how leadership behavior can facilitate cultural transformation and nurture an environment of ongoing improvement [10, 11].
Additionally, this study sought to assess LSS’s capacity to improve operational performance, decrease patient wait times, and elevate overall service quality at Ibnu Sina Hospital [12]. By offering a comparative analysis of LSS applications across various hospital settings, both domestically and internationally [13], this research contributed to the existing knowledge base and provided valuable insights for hospital administrators and policymakers [14, 15]. The purpose of this study was to examine how LSS methodologies can enhance operational efficiency and service quality in healthcare settings. By focusing on the case of Ibnu Sina Hospital, the research aimed to provide evidence-based insights into the practical application of LSS principles. These findings are expected to inform healthcare policy at both national and regional levels, offering a framework for integrating LSS strategies into broader healthcare improvement initiatives. Furthermore, the study aimed to contribute to the development of standardized guidelines for process optimization in public and private hospitals, ultimately improving resource utilization, patient outcomes, and advancing Indonesia’s progress toward achieving the Sustainable Development Goals related to health and well-being.
Materials and Methods
This mixed-method case study investigated the application of LSS, a process enhancement methodology, in hospitals across Aceh, Indonesia in 2024, with a focus on its impact on managerial and operational efficiency. Using a case study approach, the research provided an in-depth analysis of the implementation process, its effects on various stakeholders, and the outcomes achieved. This comprehensive approach captures the context-specific factors influencing the adoption and efficacy of LSS in a practical healthcare setting.
Data collection methods included semi-structured interviews with hospital personnel and patients, direct observations of hospital functions, and an examination of relevant documents. Observations targeted patient wait times at critical entry points, particularly the general polyclinic for internal medicine services and the pharmacy unit, to identify operational inefficiencies and bottlenecks.
Time of study and sample size
The research was conducted over three months, from August to October 2024, allowing sufficient time for observing outpatient processes, conducting interviews, and capturing variations in hospital operations. Observations involved 50 patients selected to effectively represent the outpatient processes at Ibnu Sina Hospital. While no formal statistical method was used for sample size calculation, a pragmatic approach was adopted, considering daily patient volumes and the feasibility of detailed observations within the study period. In qualitative research, sample sizes are guided by data saturation, where data collection ceases once no new information or themes emerge [16].
The study employed a purposive and pragmatic sampling approach [17]. Patients were selected during routine outpatient operations to ensure that diverse interactions and process flow variations were captured. Seven key stakeholders, including the hospital director, an internal medicine specialist, the head of care, the administration and finance manager, the service manager, a general polyclinic patient, and an ER Patient, were interviewed. Their selection was based on their capacity to provide critical insights into LSS implementation, operational challenges, and hospital practices. This strategy ensured a balanced collection of qualitative and observational data, with observational studies focusing on inefficiencies and interviews providing deeper context. Document analysis supplemented these findings, offering robust evidence for examining hospital operations and the impacts of LSS.
Data collection and analysis
Value stream mapping, a LSS tool, was the primary analytical method, enabling the visualization of patient flow, identification of inefficiencies, and determination of areas for improvement. The study maintained methodological rigor through data triangulation, member checking, and a documented audit trail. Findings were presented narratively, offering detailed insights into lean six sigma’s effects on hospital operations, specifically in reducing wait times and enhancing efficiency. The research contributes to the broader knowledge of LSS in healthcare, providing actionable recommendations for improving hospital performance and patient outcomes.
Observational data served as a basis for interviews, fostering a comprehensive understanding of waiting times and bottlenecks, particularly in the pharmacy unit. All methodological stages were framed within LSS principles, ensuring the optimization of hospital operations and the enhancement of patient care quality.
Findings
The age distribution indicated that the majority of respondents were within the productive age group, suggesting active participation in healthcare-related decisions. Females formed a significant proportion of the sample, reflecting their prominent role in managing family health and well-being. In terms of occupation, housewives and farmers dominated the respondent pool, while students and teachers represented smaller groups. These demographic insights underscore the diversity of the sample and provide context for understanding their perspectives in the study (Table 1).
Table 1. Frequency of respondents’ demographics
A significant portion of time was spent waiting, which constituted the majority of the overall duration, especially during critical points, such as waiting for the doctor’s examination and picking up medicine at the pharmacy. Value-added activities, which directly contribute to patient care, accounted for only a small fraction of the total time. Non-value-added activities were also evident but were overshadowed by wasted time, particularly in stages involving registration, the doctor’s examination, and pharmacy services. This breakdown underscores the need for process improvements to minimize wasted time and enhance the efficiency of patient flow, focusing on reducing delays in key bottleneck areas while increasing the proportion of value-added activities (Table 2).
Table 2. Patient flow analysis: Time consumption and value assessment
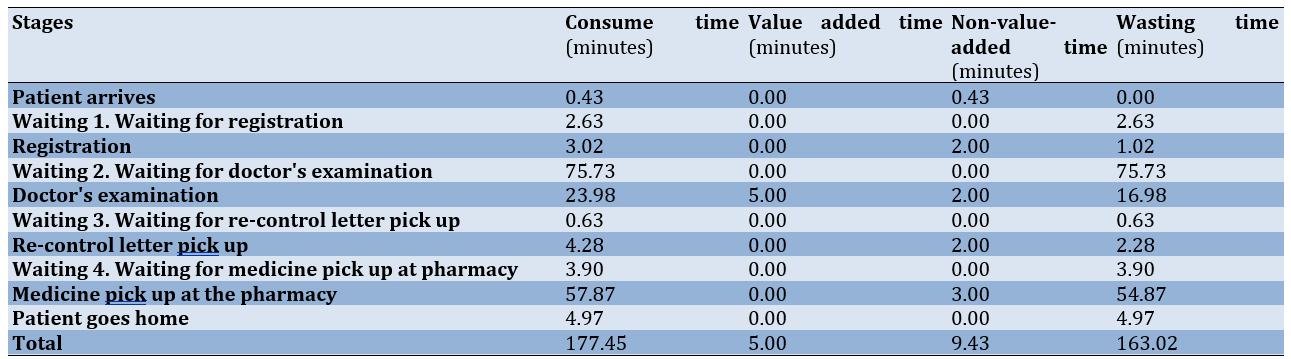
The value stream mapping before the intervention, focusing on the registration process, took 3.02 minutes. Of this time, 1.02 minutes were classified as non-value-added due to the manual printing of medical records. Administrative procedures contributed an additional 2 minutes of non-value-added time, with the physical printing process emerging as a critical bottleneck. Implementing technological solutions, such as automated documentation systems, could significantly streamline this stage by reducing manual handling and minimizing delays. Waiting for physician examination constituted the most substantial delay, averaging 75.73 minutes, all classified as non-value-added time. This delay is primarily attributed to physician scheduling limitations and personnel availability, which are often constrained by multi-facility commitments. Addressing this issue necessitates systemic solutions, including optimized scheduling and increased specialist staffing, to mitigate patient waiting times and enhance the overall experience (Figure 1).
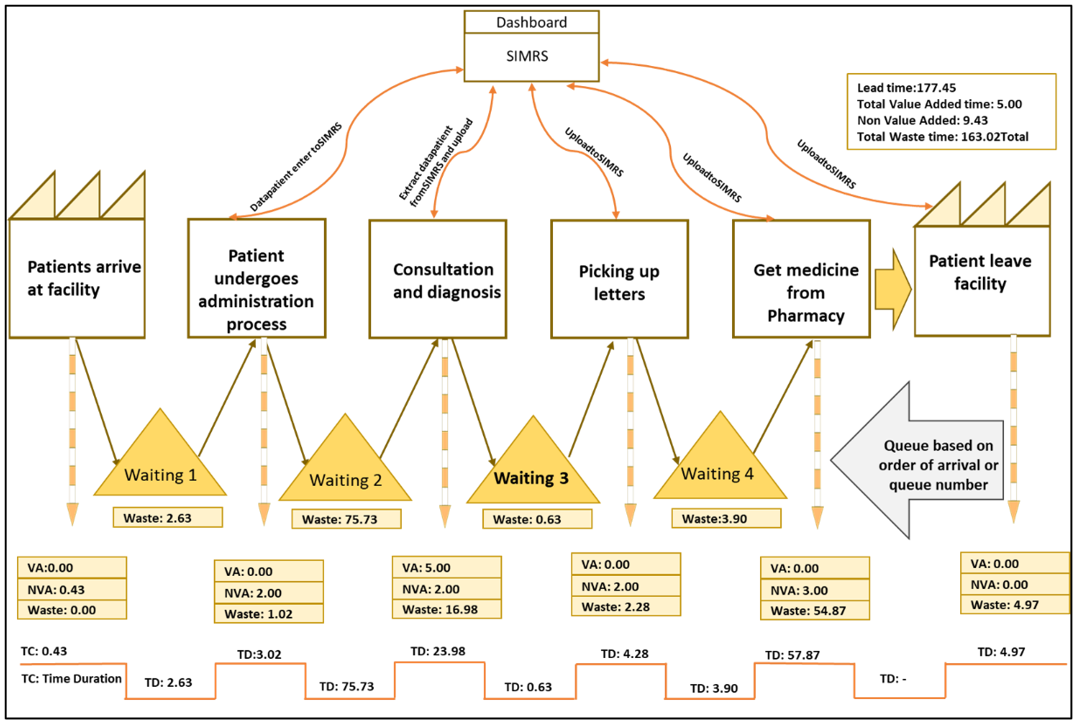
Figure 1. Value stream mapping before the intervention
Medication dispensing at the pharmacy averaged 57.87 minutes, with 54.87 minutes identified as non-value-added time due to manual drug compounding and queuing. The implementation of an e-prescription system and a drug delivery service for compounded medications is recommended. E-prescriptions can expedite dispensing, while drug delivery can reduce on-site waiting times. Overall, of the total 177.45 minutes, only 5 minutes were value-added, with the remainder consumed by non-value-added and wasted time. Value stream mapping underscores the imperative for process streamlining, automation, workforce augmentation, and process optimization to minimize non-value-added activities and enhance outpatient unit productivity, ultimately improving the patient experience.
Reduced hospital wait times through strategic technological integration were observed (Figure 2). The linking of the hospital management information system (SIMRS) with the BPJS JKN app enabled seamless queue management by automatically recording patient registrations, streamlining processes, and providing real-time updates on queue numbers and wait times. Additional systems, such as WhatsApp-based registration and integration with laboratory information management systems (LIMS) and radiology platforms, further enhanced efficiency by improving data handling and coordination. These advancements, though part of an ongoing digital transition, were already improving service delivery, transparency, and patient satisfaction while reducing delays across departments.
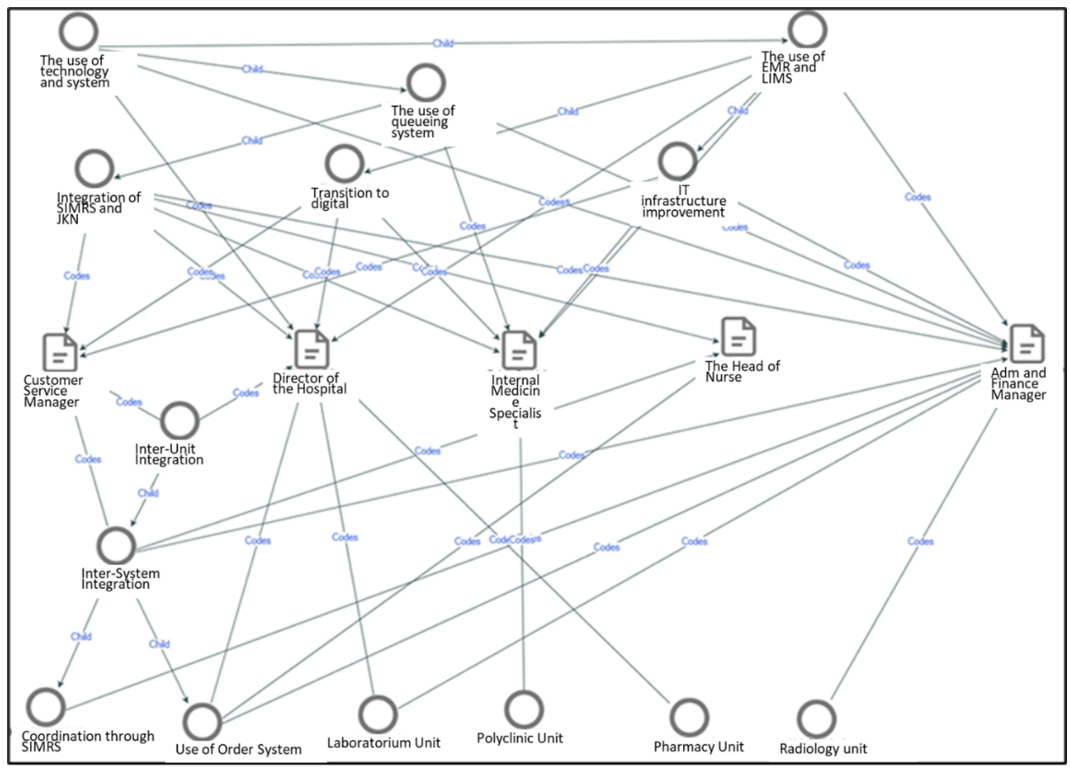
Figure 2. Intervention in technology to reduce wasting time
Key suggestions included increasing the number of specialists during peak hours to address the daily patient influx, empowering nurses to handle administrative tasks to allow doctors to focus on medical evaluations, and offering incentives and adjusted working hours for doctors to extend their availability. Additionally, initiatives, like the SIOPA program for home medication delivery, increasing radiology and laboratory staff, adding beds for advanced exams, and optimizing consultation durations were proposed. These strategies aimed to streamline processes, reduce backlogs, and improve overall service efficiency (Table 3).
Table 3. Suggestions to reduce wasting time from a Huma resource development (HRD) perspective
A comprehensive process analysis of the outpatient unit at Ibnu Sina Hospital is imperative for a thorough understanding of patient service efficiency. This analysis quantifies patient wait times across various service stages, from arrival to prescription collection, and identifies areas of temporal inefficiency. Through a systematic evaluation of these stages, the study aimed to elucidate inefficiencies and propose evidence-based solutions for optimizing patient flow. We showed the synergistic benefits of integrating technological advancements with targeted human resource strategies to address scheduling challenges, ultimately enhancing patient care and reducing waiting times.
Patient arrival was highly efficient (0.43 minutes) with no non-value-added time. The pre-improvement registration wait time (2.63 minutes) was entirely non-value-added; however, integrating JKN and WhatsApp within SIMRS eliminated this wait, consistent with technology’s role in streamlining registration. While registration time decreased from 3.02 to 2 minutes post-improvement, some administrative processing time persists. The pre-improvement doctor examination wait time (75.73 minutes) was significantly reduced to 15 minutes by adding specialists, rescheduling shifts, and providing incentives, demonstrating the effectiveness of labor-based solutions for scheduling challenges. While EMR, SIMRS, and additional nursing staff reduced non-value-added time during examinations from 16.98 to 10 minutes, total examination time remained relatively consistent at approximately 17 minutes (Figure 3).
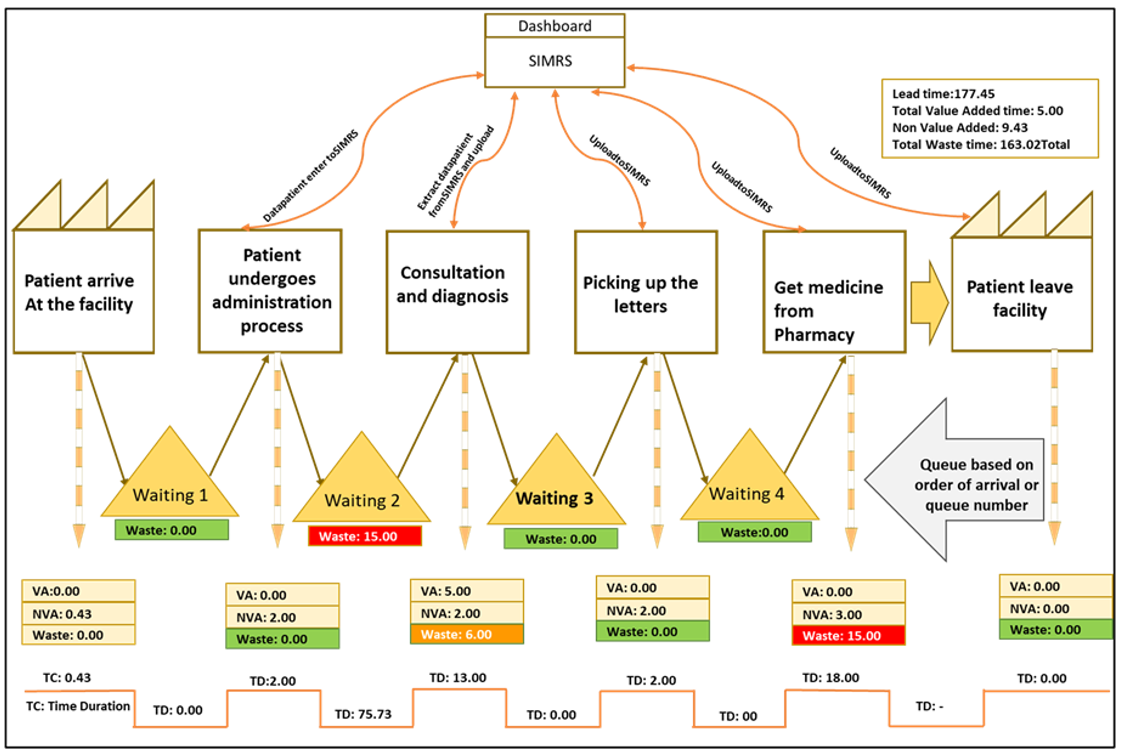
Figure 3. Value stream mapping after the intervention.
Pre-improvement pharmacy wait times (57.87 minutes, with 54.87 minutes classified as non-value-added) significantly reduced to 18 minutes following the implementation of e-prescriptions and the SIOPA drug delivery service, highlighting the effectiveness of technology and logistics-based improvements. The residual wait time was attributed to the complexities of drug compounding. Overall, total time spent decreased from 177.45 minutes (163.02 minutes non-value-added) to 54.43 minutes (40 minutes non-value-added) post-improvement, demonstrating a significant reduction in non-value-added time.
The analysis highlighted various stages of the patient journey, identifying time consumption and waste before interventions, as well as the corrective actions taken to reduce inefficiencies. Key improvements included integrating systems for patient registration, enhancing specialist availability, supporting electronic medical records (EMR) and scheduling, and introducing e-prescriptions for the pharmacy. These changes significantly reduced waiting times, particularly in areas such as registration, doctor’s examination, and medicine pickup. Overall, the interventions resulted in a reduction of wasted time and a more efficient process, improving both patient flow and service delivery (Table 4).
Table 4. Patient flow analysis: Time consumption and value assessment before and after improvements
Discussion
This study investigated the application of lean six sigma principles, specifically value stream mapping, to enhance efficiency and service quality at Ibnu Sina Hospital in Indonesia. Despite these improvements, some stages of the outpatient process, such as doctor consultations and pharmacy services, continue to experience residual delays due to the high demand for specialized personnel and the complexity of manual prescription processes. The addition of specialist doctors and support staff, along with optimized shift scheduling, has alleviated some delays but highlights the need for further structural changes to achieve lasting operational efficiency. The persistence of certain inefficiencies, even after improvements, suggests that while technology can address many surface-level issues, more in-depth workforce and process management strategies are needed to tackle these core challenges fully [15]. While EMR technology has reduced administrative time, examination times remain relatively long due to the inherent complexity and precision required for medical evaluations.
This research contributes valuable insights into the potential of LSS in healthcare and underscores the importance of combining digital integration with strategic workforce management to create a more streamlined patient journey. By systematically examining each stage and implementing targeted improvements, healthcare institutions, like Ibnu Sina General Hospital can not only enhance their service quality but also foster a more patient-centered environment that aligns with broader public health goals. This approach offers a scalable model for other hospitals seeking to improve efficiency and patient satisfaction through a combination of technological and operational advancements [16].
Efficient patient wait time management is crucial for optimizing healthcare service delivery [17]. Leveraging technological advancements offers several strategies to achieve this. Integrating existing systems, such as the SIMRS with the BPJS JKN application, can significantly enhance registration and queue management capabilities. This integration, coupled with alternative registration methods like WhatsApp, contributes to a more streamlined patient experience and reduced wait times.
A key strategy for wait time reduction involves integrating online platforms like SIMRS and the BPJS JKN app [18, 19]. This integration facilitates seamless queue management by automatically registering JKN patients within SIMRS, thereby enhancing efficiency [20]. Additionally, WhatsApp-based registration, whether via text or voice call, allows operators to input patient details into SIMRS, providing real-time queue updates and estimated wait times. This transparency effectively manages patient expectations and contributes to wait time reduction [21, 22].
This research investigated the integration of advanced technology and LSS principles to enhance hospital management and operations [23, 24]. The study reviewed relevant literature, established a defined methodology, and presented the resulting impact on key hospital performance indicators. A detailed discussion analyzed these improvements, explored underlying mechanisms, and acknowledged study limitations while suggesting future research directions [25]. The conclusion summarized key findings and emphasizes practical implications for improved hospital management and operational efficiency [26, 27].
To address protracted patient wait times at the polyclinic, several strategic recommendations have been proposed. These suggestions, derived from input by specialist physicians, nurse managers, and administrative personnel, focused on enhancing service efficiency through resource optimization [19]. A key recommendation is to increase specialist availability during peak hours to minimize patient backlog, particularly given the daily influx of approximately 90 patients. Furthermore, empowering nurses to assume administrative responsibilities can streamline processes, enabling physicians to dedicate more time to medical evaluations. This dual approach of augmenting specialist availability and expanding nursing roles aimed to expedite patient services and improve overall care delivery.
Enhanced resource allocation within the polyclinic, specifically increasing the number of available specialists during peak hours, was recommended by a cohort of stakeholders, including two specialist physicians, the head of nursing, the administrative and financial manager, and a patient representative [28, 29]. This strategic increase aims to minimize patient backlog, particularly given the average daily patient volume of approximately 90. Furthermore, empowering nursing staff to manage administrative tasks, such as pre- and post-examination data entry within the Electronic Medical Record system, was proposed. This delegation of administrative duties allows physicians to focus primarily on medical evaluations, thereby expediting the service process [30, 31]. Incentivizing extended physician availability through adjusted work schedules, as suggested by the administrative, financial, and service managers, offers an additional avenue for mitigating patient backlog. For instance, extending the shifts of morning emergency department physicians into the afternoon could provide support during peak hours and subsequently reduce wait times [32, 33]. Ancillary initiatives include the SIOPA medication home delivery program, which aims to minimize pharmacy wait times, increasing radiology and laboratory staffing, providing additional on-site examination resources (e.g., EKG beds), and optimizing consultation durations. While acknowledging the complexities of reducing consultation times, expanding the number of operational polyclinic outlets has been suggested to improve patient flow and further reduce wait times [34, 35].
The integration of digital solutions such as JKN, WhatsApp, and SIMRS has proven effective in reducing waiting times for registration and prescription pickup, demonstrating the value of technology in healthcare process optimization.
This study offers valuable insights into the integration of Lean Six Sigma principles and digital tools at Ibnu Sina Hospital; however, it is constrained by several limitations. Despite improvements, residual delays in doctor consultations and pharmacy services persist due to high demand for specialized personnel and the complexities of manual prescription processes, indicating that technological enhancements alone cannot resolve deep-rooted operational issues. Moreover, as the research was confined to a single hospital, the generalizability of its findings is limited, and different institutions may experience varying outcomes based on their unique operational structures and patient demographics. Finally, external factors such as policy shifts and demographic variations were not fully considered, underscoring the need for future research to adopt multi-center approaches and comprehensive workforce management strategies for sustainable efficiency gains
Conclusion
There are significant inefficiencies in the outpatient process flow at Ibnu Sina General Hospital, particularly in patient waiting times and manual administrative tasks.
Acknowledgments: The authors thank the Ibnu Sina Hospital management and staff for their support and cooperation during this research.
Ethical Permissions: This study was approved by the Ethical Committee of Ibnu Sina Hospital (2023-04-IRB).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Yenni Oktaviza Y (First Author), Introduction Writer/Methodologist/Main Researcher /Discussion Writer (50%); Yunus M (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Ibrahim M (Third Author), Assistant Researcher/Discussion Writer (15%); Chan S (Fourth Author), Introduction Writer/Discussion Writer (10%)
Funding/Support: No Funding was received.
Article Type: Original Research |
Subject:
Health Communication
Received: 2024/12/12 | Accepted: 2025/01/22 | Published: 2025/01/30
Received: 2024/12/12 | Accepted: 2025/01/22 | Published: 2025/01/30
References
1. Afriana W, Zulyani F, Kurniawan T. Application of Lean Six Sigma method in hospital management process: Performance optimization and waste reduction. Int J Future Stud. 2023;6(3):172-84. [Link] [DOI:10.54783/endlessjournal.v6i3.212]
2. Antony J, Palsuk P, Gupta S, Mishra DP, Barach P. Six Sigma in healthcare: A systematic review of the literature. Int J Qual Reliab Manag. 2018;35(5):1075-92. [Link] [DOI:10.1108/IJQRM-02-2017-0027]
3. Francescatto MB, Júnior AN, Kubota FI, Guimarães GE, Oliveira Bd. Lean Six Sigma case studies literature overview: Critical success factors and difficulties. Int J Product Perform Manag. 2022;72(1):1-23. [Link] [DOI:10.1108/IJPPM-12-2021-0681]
4. Zimmermann GdS, Siqueira LD, Bohomol E. Lean Six Sigma methodology application in health care settings: An integrative review. Rev Bras Enferm. 2020;73(suppl 5):e20190861. [Link] [DOI:10.1590/0034-7167-2019-0861]
5. Peimbert-García RE. Analysis and evaluation of reviews on Lean and Six Sigma in health care. Qual Manag Health Care. 2019;28(4):229-36. [Link] [DOI:10.1097/QMH.0000000000000226]
6. Shamsi MA, Alam A. Exploring Lean Six Sigma implementation barriers in information technology industry. Int J Lean Six Sigma. 2018;9(4):523-42. [Link] [DOI:10.1108/IJLSS-06-2017-0054]
7. Arcidiacono G, Costantino N, Yang K. The AMSE Lean Six Sigma governance model. Int J Lean Six Sigma. 2016;7(3):233-66. [Link] [DOI:10.1108/IJLSS-06-2015-0026]
8. Nadeau S. Lean, Six Sigma and Lean Six Sigma in higher education: A review of experiences around the world. Am J Ind Bus Manag. 2017;7(5):591-603. [Link] [DOI:10.4236/ajibm.2017.75044]
9. Pavão DN, Buttignol M, Pereira AJ, Tanjoni R, Almeida E, Leisnock P, et al. Efficiency in the operational process: Reduction of incorrect entries and guarantee of compliance in the rendering of accounts. Einstein. 2018;16(4). [Link] [DOI:10.31744/einstein_journal/2018GS4200]
10. Tortorella GL, Dun DHv, Almeida AGd. Leadership behaviors during lean healthcare implementation: A review and longitudinal study. J Manuf Technol Manag. 2020;31(1):193-215. [Link] [DOI:10.1108/JMTM-02-2019-0070]
11. Poksińska B, Fialkowska-Filipek M, Engström J. Does Lean healthcare improve patient satisfaction? A mixed-method investigation into primary care. BMJ Qual Saf. 2017;26(2):95-103. [Link] [DOI:10.1136/bmjqs-2015-004290]
12. Montella E, Cicco MVD, Ferraro A, Centobelli P, Raiola E, Triassi M, et al. The application of Lean Six Sigma methodology to reduce the risk of healthcare-associated infections in surgery departments. J Eval Clin Pract. 2017;23(3):530-9. [Link] [DOI:10.1111/jep.12662]
13. Fadhilah AN, Ayubi D. Lean Six Sigma approach for wait time analysis in radiology services at Krakatau Medika Hospital. Devot J Community Serv. 2023;4(12):2371-5. [Link] [DOI:10.59188/devotion.v4i12.631]
14. Al-Zain Y, Al-Fandi L, Arafeh M, Salim S, Al-Quraini S, Al-Yaseen A, et al. Implementing Lean Six Sigma in a Kuwaiti private hospital. Int J Health Care Qual Assur. 2019;32(2):431-46. [Link] [DOI:10.1108/IJHCQA-04-2018-0099]
15. Ahmed F, Manaf NHA, Islam R. Effect of Lean Six Sigma on quality performance in Malaysian hospitals. Int J Health Care Qual Assur. 2018;31(8):973-87. [Link] [DOI:10.1108/IJHCQA-07-2017-0138]
16. Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc Sci Med. 2022;292:114523. [Link] [DOI:10.1016/j.socscimed.2021.114523]
17. Campbell S, Greenwood M, Prior S, Shearer T, Walkem K, Young S, et al. Purposive sampling: Complex or simple? Research case examples. J Res Nurs. 2020;25(8):652-61. [Link] [DOI:10.1177/1744987120927206]
18. Safi M, Clay-Williams R, Thude BR, Vaisman J, Brandt F. Today's referral is tomorrow's repeat patient: Referrals between medical outpatient clinics in a hospital. BMC Health Serv Res. 2022;22(1):254. [Link] [DOI:10.1186/s12913-022-07633-y]
19. Hemmati F, Mahmoudi G, Dabbaghi F, Fatehi F, Rezazadeh E. The factors affecting the waiting time of outpatients in the emergency unit of selected teaching hospitals of Tehran. Electron J Gen Med. 2018;15(4). [Link] [DOI:10.29333/ejgm/93135]
20. Brahmbhatt V. Emergency department average wait time before admission, average time till sent home, and average number of violations for different hospitals types in Tennessee: Date analysis of Medicare data. MedRxiv. 2022. [Link] [DOI:10.1101/2022.12.12.22283361]
21. Nwose Paschal C, Nwose Uchenna C. Quality improvement project to reduce waiting time and improve patient's satisfaction in a private hospital in Lagos, Nigeria. Ibom Med J. 2019;12(1):15-22. [Link] [DOI:10.61386/imj.v12i1.213]
22. Calder-Sprackman S, Kwok E, Bradley R, Landreville JM, Perry JJ, Calder LA. Availability of emergency department wait times information: A patient-centered needs assessment. Emerg Med Int. 2021;2021:8883933. [Link] [DOI:10.1155/2021/8883933]
23. Al-Qatawneh L, Abdallah AA, Zalloum S. Six Sigma application in healthcare logistics: A framework and a case study. J Healthc Eng. 2019;2019:9691568. [Link] [DOI:10.1155/2019/9691568]
24. Arcidiacono G, Pieroni A. The revolution Lean Six Sigma 4.0. Int J Adv Sci Eng Inform Technol. 2018;8(1):141. [Link] [DOI:10.18517/ijaseit.8.1.4593]
25. Gijo EV, Antony J. Reducing patient waiting time in outpatient department using Lean Six Sigma methodology. Qual Reliab Eng Int. 2014;30(8):1481-91. [Link] [DOI:10.1002/qre.1552]
26. Kuiper A, Lee RH, Ham VJ, Does RJMM. A reconsideration of Lean Six Sigma in healthcare after the COVID-19 crisis. Int J Lean Six Sigma. 2021;13(1):101-17. [Link] [DOI:10.1108/IJLSS-01-2021-0013]
27. Samaranayake P, Dadich A, Hayes KJ, Sloan TR. Patient-journey modelling and simulation in computed tomography: An integrated framework. Bus Process Manag J. 2015;21(5):988-1014. [Link] [DOI:10.1108/BPMJ-10-2014-0097]
28. Suman G, Prajapati DR. Utilization of Lean & Six Sigma quality initiatives in Indian healthcare sector. PLoS One. 2021;16(12):e0261747. [Link] [DOI:10.1371/journal.pone.0261747]
29. Régis TKO, Santos LC, Gohr CF. A case-based methodology for Lean implementation in hospital operations. J Health Organ Manag. 2019;33(6):656-76. [Link] [DOI:10.1108/JHOM-09-2018-0267]
30. Improta G, Balato G, Ricciardi C, Russo MA, Santalucia I, Triassi M, et al. Lean Six Sigma in healthcare: Fast track surgery for patients undergoing prosthetic hip replacement surgery. TQM J. 2019;31(4):526-40. [Link] [DOI:10.1108/TQM-10-2018-0142]
31. Lukač A, Sulović N, Ilić A, Mijović M, Tasić D, Smiljić S. Optimal outcome factors in maternity and newborn care for inpatient (hospital maternity ward-HMW) and outpatient deliveries (outhospital maternity clinics-OMC). BMC Pregnancy Childbirth. 2021;21(1):836. [Link] [DOI:10.1186/s12884-021-04319-x]
32. Knapp S. Lean Six Sigma implementation and organizational culture. Int J Health Care Qual Assur. 2015;28(8):855-63. [Link] [DOI:10.1108/IJHCQA-06-2015-0079]
33. Amelia P, Lathifah A, Haq MD, Reimann CL, Setiawan Y. Optimising outpatient pharmacy staffing to minimise patients queue time using discrete event simulation. J Inf Syst Eng Bus Intell. 2021;7(2):102. [Link] [DOI:10.20473/jisebi.7.2.102-111]
34. Improta G, Romano MV, Cicco MVD, Ferraro A, Borrelli A, Verdoliva C, et al. Lean thinking to improve emergency department throughput at AORN Cardarelli Hospital. BMC Health Serv Res. 2018;18(1):914. [Link] [DOI:10.1186/s12913-018-3654-0]
35. Lifvergren S, Gremyr I, Hellström A, Chakhunashvili A, Bergman B. Lessons from Sweden's first large-scale implementation of Six Sigma in healthcare. Oper Manag Res. 2010;3(3):117-28. [Link] [DOI:10.1007/s12063-010-0038-y]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






