Volume 12, Issue 4 (2024)
Health Educ Health Promot 2024, 12(4): 623-635 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Roza E, Rusdi M, Guspianto G, Hasibuan M. An Educational Intervention Model to Improve Hypertension Self-Management in the Elderly. Health Educ Health Promot 2024; 12 (4) :623-635
URL: http://hehp.modares.ac.ir/article-5-77913-en.html
URL: http://hehp.modares.ac.ir/article-5-77913-en.html
1- Department of Public Health Sciences, Faculty of Mathematics and Natural Sciences Education, Jambi of University, Jambi, Indonesia
2- Department of Chemistry Education, Faculty of Teacher Training and Education, Jambi of University, Jambi, Indonesia
3- Department of Public Health Sciences, Faculty of Medicine and Health Sciences, Jambi of University, Jambi, Indonesia
2- Department of Chemistry Education, Faculty of Teacher Training and Education, Jambi of University, Jambi, Indonesia
3- Department of Public Health Sciences, Faculty of Medicine and Health Sciences, Jambi of University, Jambi, Indonesia
Keywords: Education [MeSH], Self-Management [MeSH], Hypertension [MeSH], Elderly [MeSH], Systematic Review [MeSH]
Full-Text [PDF 832 kb]
(1626 Downloads)
| Abstract (HTML) (919 Views)
Full-Text: (78 Views)
Introduction
High blood pressure (BP), often referred to as hypertension, is a common chronic illness that primarily affects the elderly. It is a significant risk factor for kidney failure, stroke, and cardiovascular diseases, contributing substantially to global morbidity and mortality rates [1-4]. Among older adults, the prevalence of hypertension is particularly high, largely due to age-related vascular changes and the increased occurrence of comorbid conditions, making it a critical health issue for this population [5, 6]. According to the World Health Organization, hypertension control remains suboptimal worldwide, especially among older individuals, who face challenges such as medication non-adherence, poor self-management behaviors, and limited access to tailored health education [7].
Self-management is widely regarded as an essential component of effective hypertension control. This practice includes activities such as monitoring BP, maintaining a balanced diet, adhering to prescribed medications, and engaging in regular physical exercise [8, 9]. Research has shown that consistent self-management behaviors can substantially reduce the risk of hypertension-related complications [10, 11]. However, elderly patients often encounter unique barriers to effective self-management, such as cognitive decline, physical limitations, and limited technological literacy, which can hinder their ability to actively manage their health [12-16].
Educational interventions tailored specifically to the elderly population are essential for addressing these barriers and empowering patients to take control of their hypertension management. Studies indicate that structured educational programs can improve self-efficacy, enhance knowledge about hypertension, and encourage sustainable lifestyle changes, all of which are vital for effective disease management [17]. Furthermore, educational models grounded in theories, such as the health belief model (HBM) and social cognitive theory (SCT) provide a structured approach to instilling motivation and promoting behavioral changes that are critical for managing chronic conditions in elderly populations [18].
With the rise of digital technology, innovative educational models have emerged, including mobile applications and telehealth programs. By making health information more convenient and accessible, telehealth-based educational programs have been shown to increase self-efficacy and encourage healthier lifestyle choices [19]. Digital health tools, such as mobile apps, have been effectively utilized to deliver information on medication adherence, dietary modifications, and lifestyle management for hypertensive patients, demonstrating that technology-assisted interventions can significantly improve health outcomes in elderly patients [20, 21]. Additionally, community-based programs and group education models, which provide social support alongside practical education, have proven effective in helping older adults adopt and maintain self-management behaviors [22, 23].
Despite these advancements, there is still a need for comprehensive educational models that specifically address the unique needs and limitations of elderly populations. Recent research highlights that multidimensional approaches combining digital tools with in-person support yield the most promising outcomes in terms of adherence, self-efficacy, and sustainable lifestyle changes [24]. However, further studies are needed to develop and refine these models to maximize their effectiveness in managing hypertension among the elderly [25, 26].
This systematic review aimed to consolidate evidence on educational interventions designed to improve the self-management of hypertension in elderly populations. By reviewing studies published from 2000 to 2024, this analysis evaluated the effectiveness of various educational models, identified key factors influencing self-management behaviors, and provided evidence-based recommendations for enhancing hypertension care in older adults. These insights are intended to guide healthcare practitioners in implementing effective, tailored educational strategies that improve hypertension outcomes in this vulnerable population.
Information and Methods
Study design
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 standards were followed in the design and execution of this systematic review conducted in 2024 [27]. The goal was to synthesize existing evidence on educational interventions that improve hypertension self-management among elderly populations.
Eligibility criteria
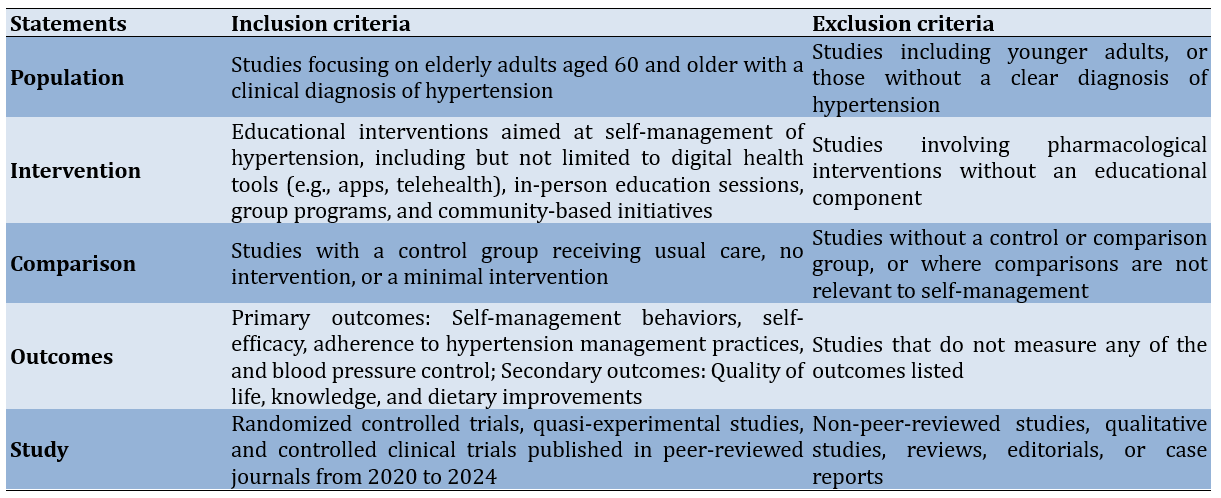
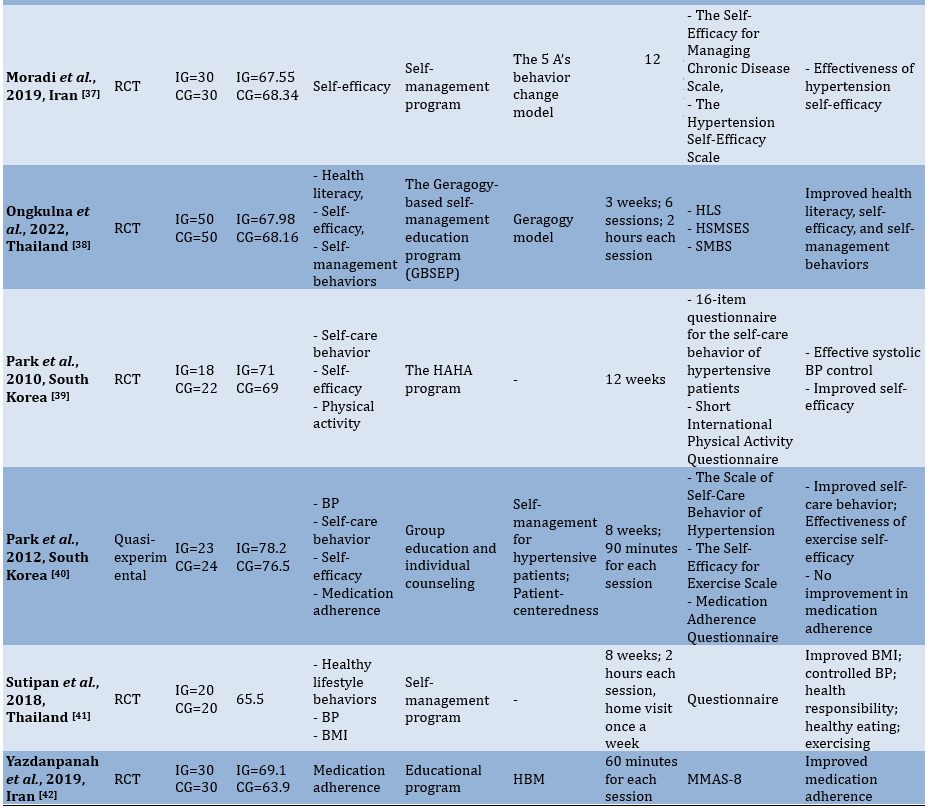
The inclusion and exclusion criteria were developed based on the population, intervention, comparison, outcomes, and study (PICOS) framework to ensure alignment with the research question (Table 1).
Table 1. Statements of the population, intervention, comparison, outcomes, and study (PICOS) framework
Information sources
To identify relevant studies, we systematically searched six electronic databases, including PubMed, Scopus, Web of Science, ScienceDirect, JSTOR, and Cochrane Library. These databases were chosen for their comprehensive coverage of health, clinical, and psychological research. The search encompassed publications from 2000 to 2024 to focus on the most recent 20 years of evidence. Additionally, we conducted hand searches of reference lists in eligible studies and performed citation tracking to identify potentially relevant studies. Experts in hypertension self-management were consulted for insights into unpublished or ongoing studies.
Search strategy
To ensure sensitivity and specificity, a medical librarian assisted in developing the search strategy. The search terms were formulated using both Medical Subject Headings (MeSH) and free-text keywords. The strategy combined terms related to population (“elderly,” “older adults,” “geriatric patients”), intervention (“hypertension education,” “self-management,” “educational models,” “telehealth,” “digital health,” “community-based programs”), and Outcomes (“self-efficacy,” “medication adherence,” “dietary adherence,” “blood pressure control”) (Table 2).
Table 2. Search string in databases

Study quality
The reviewers independently evaluated the literature to determine the quality for inclusion. Although this step is not mandatory in systematic review protocols, the reviewers considered it beneficial for identifying the strengths and limitations of the selected studies. Due to the diverse nature of the articles, the critical appraisal skills program (CASP) for randomized studies was chosen for its ability to systematically evaluate study quality. CASP offers a structured set of questions specifically designed for different study designs, particularly randomized studies. Each CASP checklist includes 11 questions with response options of “yes,” “no,” or “can’t tell,” facilitating a standardized appraisal process. Study quality is classified into three categories, including strong, moderate, and weak. A study is classified as weak if there are three non-affirmative responses, moderate if there are two non-affirmative responses (“can’t tell” or “no”), and strong if all of the responses are affirmative.
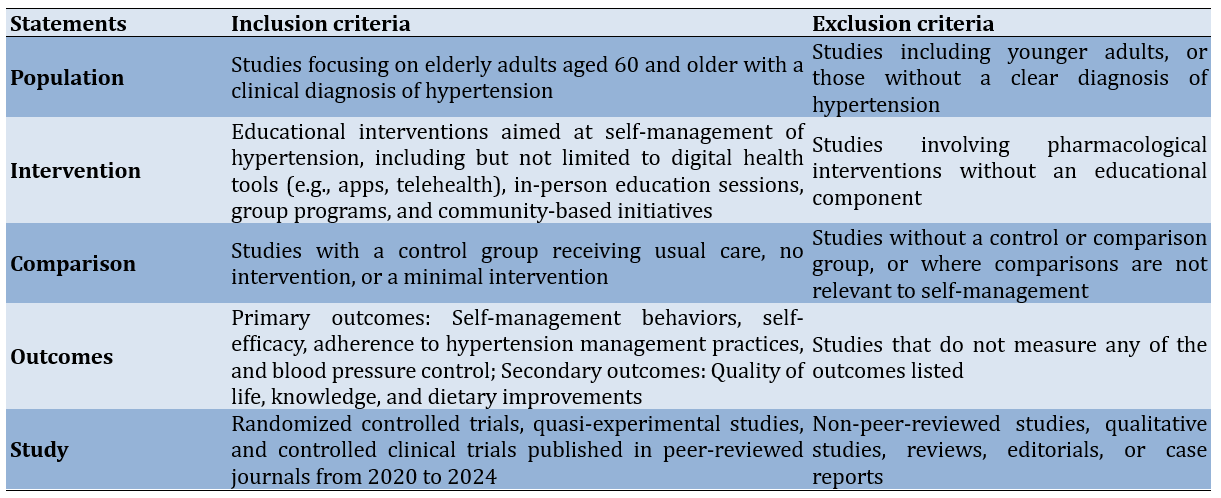
Risk of bias
The assessment of bias in each study was performed using the risk of bias in randomized studies (RoB 2) tool. This tool was chosen for its structured, validated framework tailored to detecting bias specifically within randomized controlled trials (RCTs), addressing essential areas, such as randomization, deviations from the planned interventions, missing outcome data, outcome measurement, and selective reporting. The RoB 2 tool provides a comprehensive and consistent approach to quality assessment, which strengthens the reliability of the review’s conclusions. It includes five domains that assess both internal and external validity, with results classified into four levels, including Low, some concerns, high, and very high. All authors reviewed and approved the RoB assessment results, incorporating feedback from external reviewers.
Data extraction and synthesis
To enhance understanding of the content within the eligible studies, key information was condensed into a table format. Two authors collaborated during this data-gathering process. Any discrepancies in the extracted data were resolved through mutual agreement. The extraction criteria included details, such as the primary author, year of publication, country, study design, sample size, mean age, outcome, intervention, model, duration, evaluation technique, and key findings.
Findings
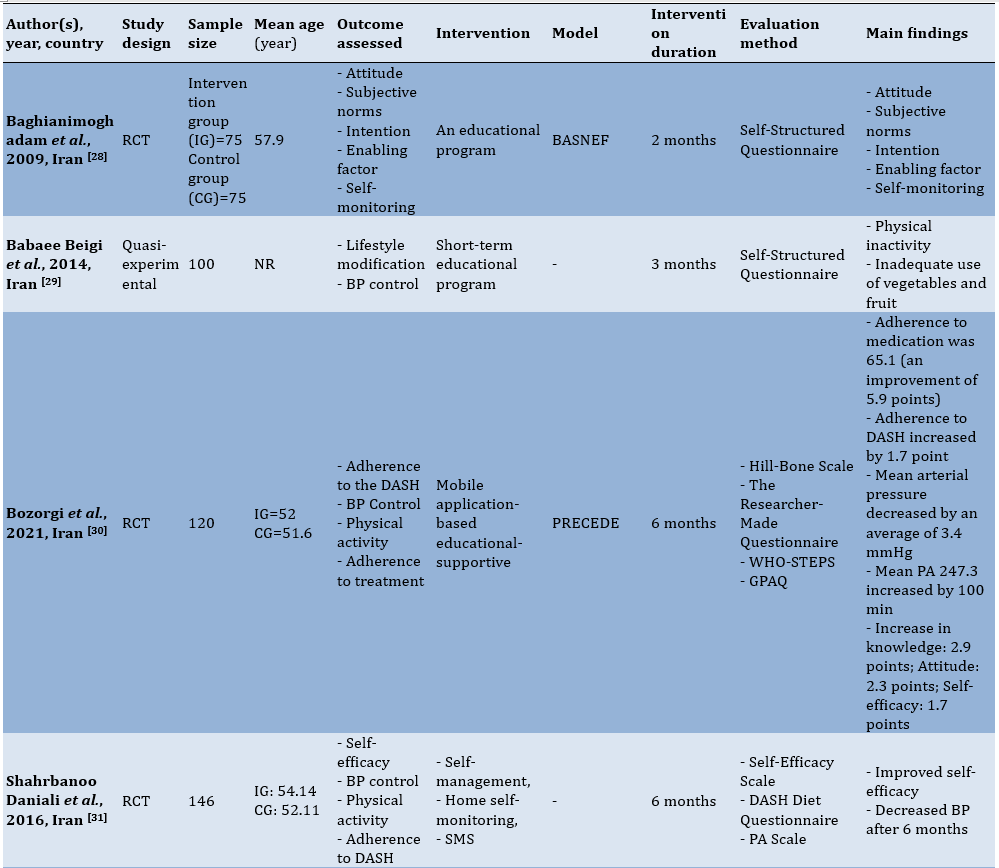
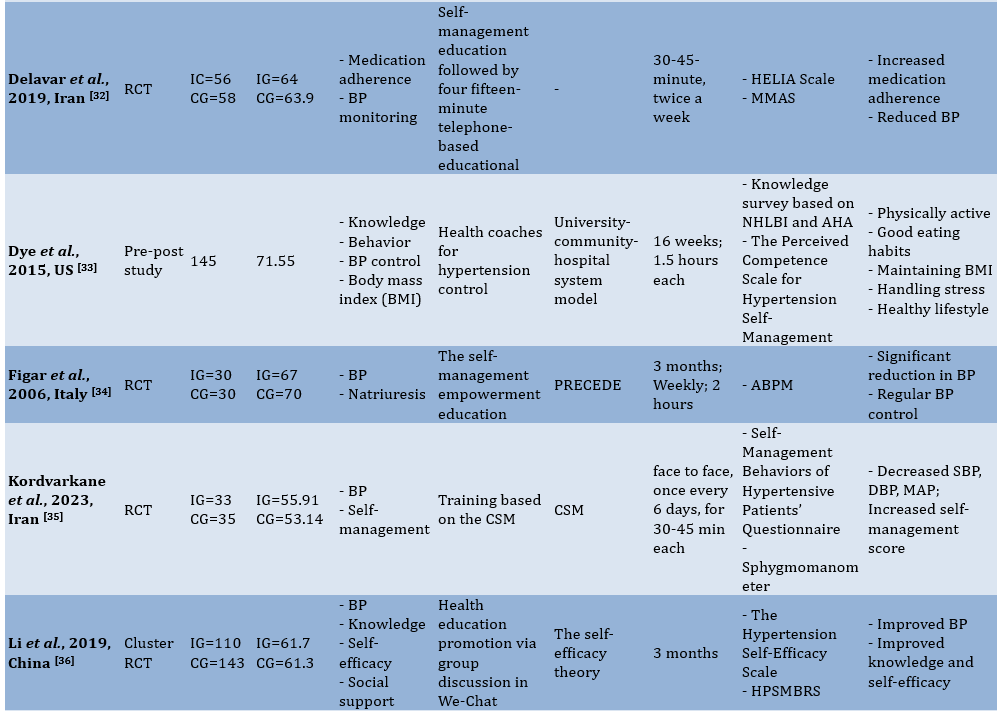
The initial database query yielded 598 articles. Following the removal of 405 duplicates and irrelevant articles unrelated to the review’s focus, 193 articles were available for screening. In the eligibility evaluation, 159 articles were excluded for various reasons. Ultimately, only 15 studies fulfilled the criteria and advanced to the subsequent stage of data extraction and analysis (Figure 1; Table 3).

Figure 1. PRISMA flowchart for study selection.
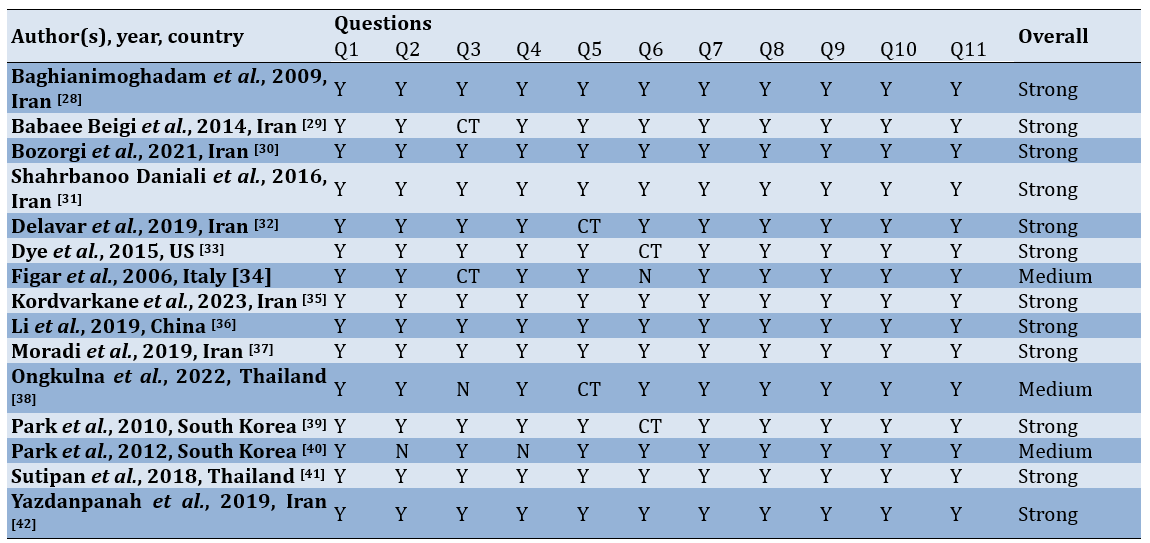
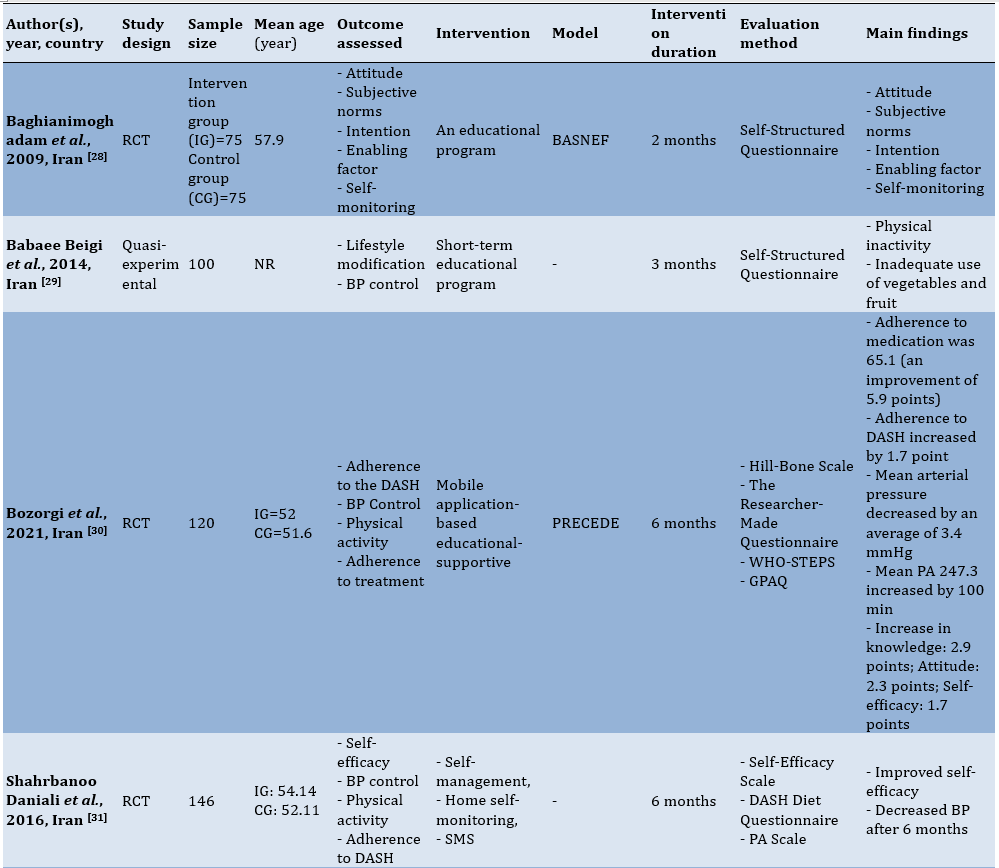
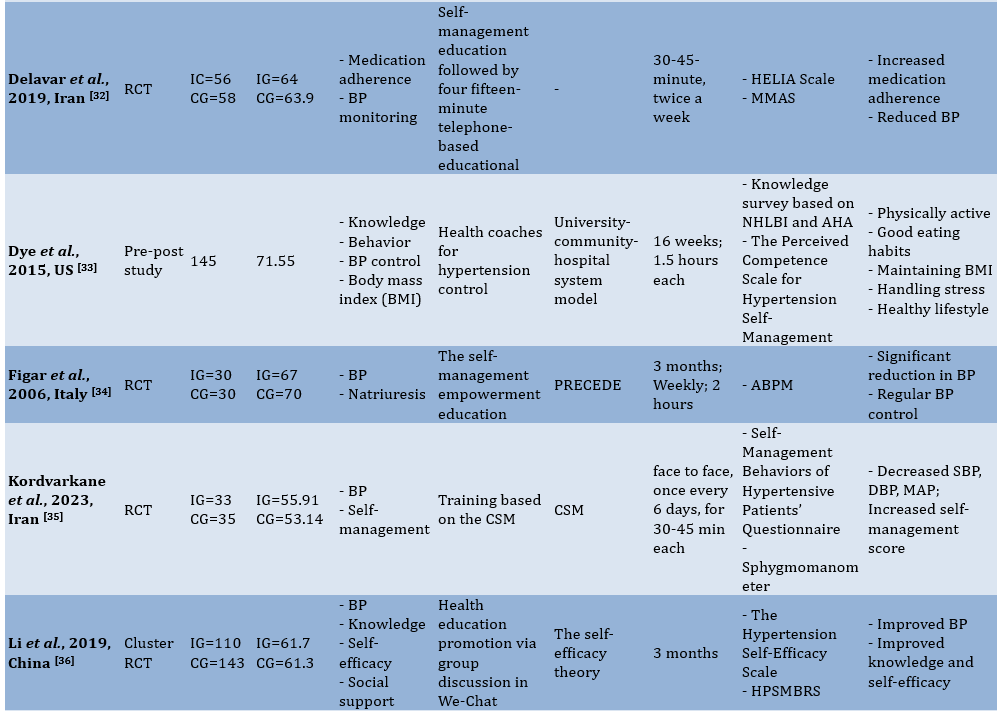
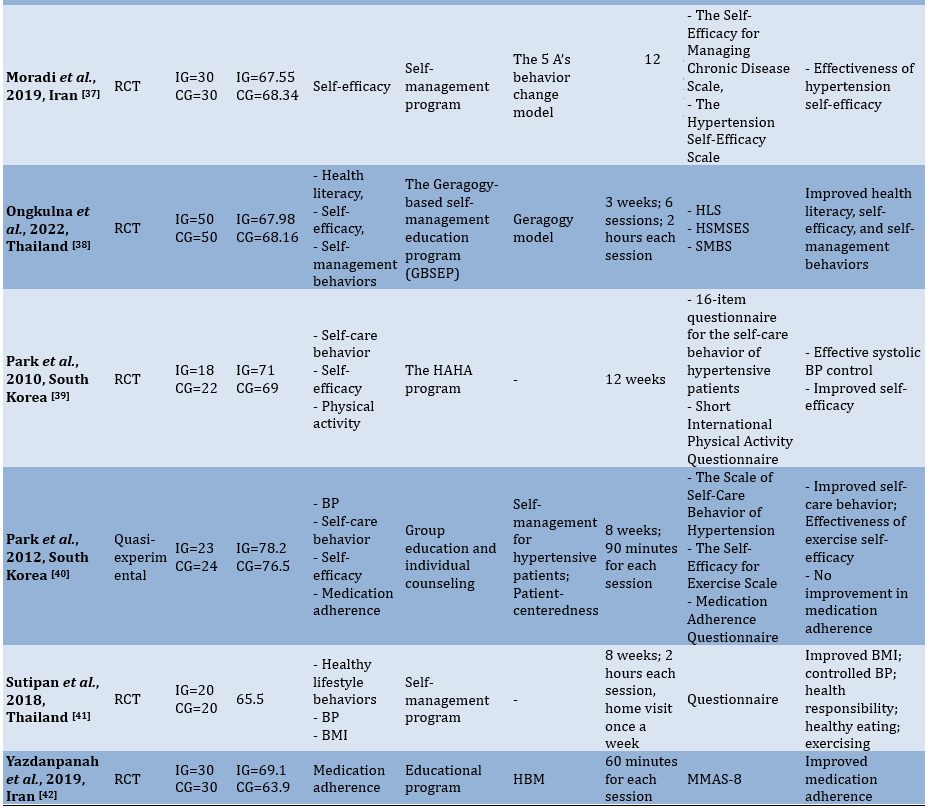
Tabel 3. Characteristics of the eligible studies
General characteristics of the eligible studies
The studies reviewed in this analysis used a variety of interventions aimed at improving health outcomes through educational and self-management strategies. The studies were conducted in diverse countries, including Iran, the United States, China, Italy, Thailand, and South Korea, highlighting both cultural and regional approaches to non-pharmacological health interventions.
The majority of the studies employed RCTs, with a few utilizing quasi-experimental and pre-post study designs. RCTs were the predominant design, indicating a strong focus on controlled interventions for evaluating the effectiveness of educational and behavioral strategies.
Sample sizes varied significantly across studies, ranging from as few as 20 participants in some RCTs (e.g., Sutipan et al. [41]) to larger groups, such as the 253 participants in Li et al.’s [36] cluster RCT in China. Participants were primarily adults, with mean ages typically ranging from the 50s to 70s, reflecting a focus on older adults and individuals managing chronic conditions, particularly hypertension.
Intervention durations ranged from as short as three weeks [38] to as long as six months [30, 31]. Formats included face-to-face sessions, mobile application-based interventions, telephone-based guidance, and online group discussions, indicating a mix of in-person and technology-assisted education.
Outcomes were assessed using a variety of self-reported and validated scales. For example, dietary adherence was evaluated using the DASH diet questionnaire, while self-efficacy was commonly measured using the Self-Efficacy for Managing Chronic Disease Scale and other similar scales. BP control and physical activity were also frequently monitored, often using standard clinical instruments or validated questionnaires (e.g., ABPM for BP in the study by Figar et al. [34]). The primary outcomes varied but were generally centered on improving self-efficacy, adherence to dietary and health recommendations, and managing hypertension. Several studies targeted lifestyle modifications, including improvements in physical activity, dietary diversity, and stress management. Many of the studies reported significant improvements in key outcomes, such as increased knowledge, improved dietary adherence, and better self-management behaviors. Notable findings included reductions in BP (e.g., Kordvarkane et al. [35]), increased adherence to the DASH diet [30], and enhanced self-efficacy for managing chronic conditions [37].
Study quality assessment
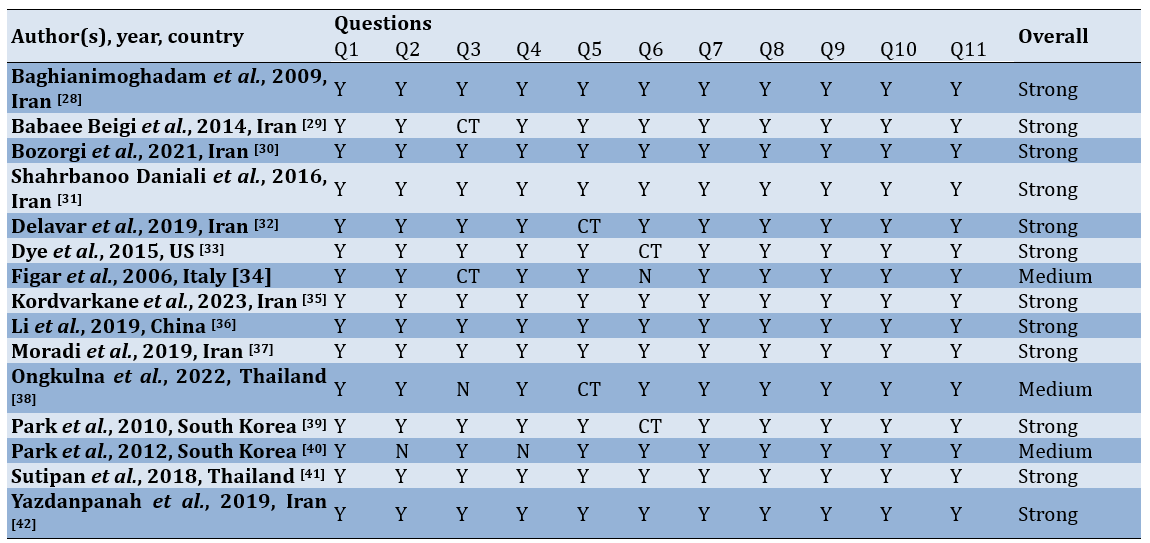
Based on the assessment results, the eligible studies are generally classified in the strong category, while only three studies fall into the medium category (Table 4).
Table 4. Summary of quality assessment
Risk of bias assessment
According to the assessment across the five dimensions of the RoB 2 tool, most of the studies were found to be in the low risk of bias category (Figure 2).
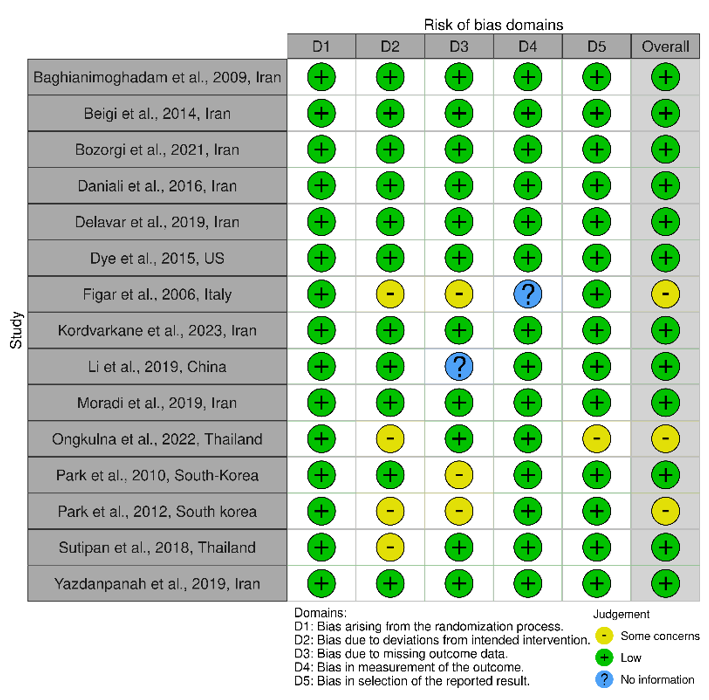
Figure 2. Traffic light plot for risk of bias assessment.
Intervention types and models
A wide range of intervention models was used across the studies, including educational programs, mobile application-based interventions, face-to-face group education, and self-management programs. Several theoretical models supported these interventions, including BASNEF, PRECEDE, Geragogy, and the HBM. These interventions aimed to improve knowledge, self-efficacy, and adherence to dietary and health practices, targeting sustainable health behaviors.
Outcomes
Several studies reported significant improvements in participants’ knowledge and self-efficacy following the interventions. For example, the intervention by Li et al. [36] in China, which used WeChat for health education, improved both BP control (p=0.002) and knowledge/self-efficacy.
Studies focusing on dietary interventions, such as adherence to the DASH diet [30], demonstrated positive effects on dietary adherence, BP control, and physical activity levels.
Improvements in health-related behaviors were observed, including healthy lifestyle practices [41] and self-care behaviors related to BP control [39]. Many studies noted significant reductions in BP, such as that by Figar et al. [34] in Italy, which demonstrated a BP reduction (p=0.02) with regular BP monitoring and empowerment education.
Discussion
This systematic review aimed to consolidate evidence on educational interventions designed to improve the self-management of hypertension in elderly populations. The studies reviewed in this analysis exhibited a wide range of characteristics and approaches, emphasizing non-pharmacological interventions aimed at improving health outcomes through educational and self-management strategies. Conducted across several countries, including Iran, the United States, China, Italy, Thailand, and South Korea, the studies highlighted cultural and regional variations in health interventions, particularly for managing chronic conditions, such as hypertension. This geographic diversity in study settings underscores the universal challenge of chronic disease management and the varying methodologies researchers have adopted in different sociocultural contexts. For instance, while studies from countries, such as Iran and Thailand tended to incorporate traditional face-to-face group educational sessions, other regions, like China, leveraged popular local digital platforms, such as WeChat to deliver health education in more accessible formats [36]. This adaptation to digital platforms is indicative of a global shift toward technology-driven healthcare solutions, especially in environments where face-to-face interaction may be limited by logistical constraints or during times of increased public health concerns.
Another notable characteristic among these studies is the variation in sample sizes, which ranged from as few as 20 participants to as many as 253. Smaller studies, such as Sutipan et al. [41] with 20 participants, often provide a more detailed examination of individual-level responses to interventions but may lack the power to reliably detect smaller effects. In contrast, larger studies, such as Li et al. [36], with a sample size of 253, enhance statistical power, offering more robust insights into intervention effectiveness at the population level. The wide age range, typically focusing on adults in their 50s to 70s, is another distinguishing factor. This age demographic reflects a focus on older adults who are generally more susceptible to chronic conditions and may particularly benefit from lifestyle interventions aimed at promoting self-management and improving overall quality of life [43]. The attention to this age group also reflects a public health priority, given the rising prevalence of hypertension and other chronic diseases in aging populations worldwide [44].
Intervention duration varied significantly, from a brief three-week program [38] to extended interventions lasting up to six months [30, 31]. Shorter interventions can provide immediate insights into the feasibility and short-term effects of an intervention but may not capture long-term adherence or sustainability. On the other hand, longer interventions are advantageous for observing sustained behavior change and determining whether health improvements persist over time. Such extended interventions might offer a better model for real-world applications, where long-term adherence is critical for effectively managing chronic conditions.
In terms of delivery format, the studies employed a mix of traditional and modern methods, ranging from face-to-face sessions to mobile app-based interventions, telephone guidance, and online group discussions. This variety reflects the growing recognition of the need for flexible and accessible healthcare delivery, especially in a post-pandemic world where remote options are increasingly valuable. Mobile health applications and other technology-assisted education methods allow participants to engage with intervention materials at their convenience, which can be particularly beneficial for individuals with limited mobility or those in rural areas with reduced access to healthcare facilities [45, 46]. At the same time, face-to-face interactions remain valuable for personalized guidance, offering opportunities for real-time feedback, social support, and engagement that digital platforms may lack [47-49].
Improvements in knowledge and self-efficacy are crucial components of chronic disease management, particularly in conditions requiring significant lifestyle changes, such as hypertension. Across the reviewed studies, multiple interventions demonstrated statistically significant increases in knowledge and self-efficacy, suggesting that structured educational programs can positively influence individuals’ ability to manage their health. For instance, Li et al. [36] utilized a WeChat-based group discussion for health education in China, which resulted in notable improvements in both BP control and self-efficacy scores among participants. The use of this popular social media platform allows for frequent interaction and support, which likely contributes to the effectiveness of the intervention. This finding aligns with Bozorgi et al. [30], who found that a mobile application-based intervention in Iran improves adherence to the DASH diet, physical activity, and self-efficacy levels. Such digital platforms may enhance accessibility and engagement, providing participants with convenient and continuous support that fosters knowledge retention and self-confidence in managing health behaviors [50, 51].
Previous research has also demonstrated the effectiveness of educational interventions in enhancing knowledge and self-efficacy. For example, a study by Bandura and Wessels [52] shows that interventions aimed at increasing self-efficacy can lead to sustained behavior change, as higher self-efficacy is directly associated with greater resilience in overcoming obstacles. Similarly, Clark and Dodge [53] emphasize the role of self-efficacy in promoting adherence to dietary and exercise regimens, particularly in hypertensive populations. By empowering patients with the knowledge and confidence needed to make informed health choices, these interventions can yield substantial long-term benefits.
In addition to mobile-based interventions, face-to-face educational sessions have also demonstrated substantial efficacy in improving knowledge and self-efficacy. For example, Park et al. [39] implemented the HAHA program in South Korea, which included face-to-face counseling and physical activity sessions. The program led to significant improvements in both self-efficacy and systolic BP control. This result aligns with findings from Yazdanpanah et al. [42] in Iran, where an educational intervention based on the HBM resulted in significant increases in medication adherence and self-efficacy. These findings suggest that in-person interactions allow for personalized feedback, real-time social support, and direct reinforcement of health knowledge, all of which can enhance participants’ self-efficacy and commitment to behavioral change.
The variation in delivery formats (ranging from digital platforms to face-to-face programs) suggests that the effectiveness of these interventions may depend on factors, such as accessibility, frequency of interaction, and participants’ preferences. Ongkulna et al. [38] demonstrated the success of the Geragogy-based self-management education program (GBSEP), which combines in-person sessions with Geragogy principles tailored to older adults. This program improves participants’ health literacy, self-efficacy, and self-management behaviors. These findings are comparable to a similar intervention by Dye et al. [33] in the United States, which used health coaches to foster self-management skills in older adults with hypertension. By adapting interventions to participants’ age-related learning needs, such programs enhance understanding and self-efficacy, facilitating better health behaviors over time.
These findings are consistent with the study using SCT by Bandura and Wessels [52], which posits that knowledge and self-efficacy are critical in driving behavior change. The reviewed studies align with this theory, indicating that well-designed educational interventions can significantly impact self-efficacy and, consequently, adherence to health-promoting behaviors. Taken together, this body of research demonstrates that improvements in both knowledge and self-efficacy are achievable across diverse formats and settings, underscoring the versatility and potential of educational interventions to support chronic disease management across different populations and health systems.
Theoretical models play a critical role in designing health interventions, particularly those aimed at improving self-management behaviors and health outcomes in chronic conditions, such as hypertension. These models provide a structured framework for understanding how individuals adopt and sustain health-promoting behaviors, which is essential for the effectiveness of interventions. In the studies reviewed, several theoretical models were employed to guide intervention development and ensure their success. These include the HBM, SCT, the PRECEDE-PROCEED model, the BASNEF Model, and Geragogy.
Each model contributes unique perspectives and mechanisms for understanding and influencing behavior, thereby supporting tailored and effective interventions. For example, interventions based on the HBM focus on modifying individuals’ perceptions about the severity of their condition, their susceptibility to complications, and the benefits of adopting preventive behaviors. Yazdanpanah et al. [42] used the HBM in their intervention with elderly patients in Iran, demonstrating that when patients perceived their hypertension as serious and recognized the benefits of medication adherence, their adherence significantly improved. This finding aligns with earlier studies showing that the HBM can effectively predict and enhance adherence to health recommendations by emphasizing individual belief systems [54, 55].
The BASNEF model, which combines elements of both the HBM and social influences, was also employed in several interventions to increase adherence to lifestyle modifications. This model considers the impact of social norms and enabling factors, such as family support and access to resources, which are crucial in environments where family dynamics and social support play a significant role in health management. Shahrbanoo Daniali et al. [31] in Iran used the BASNEF model to improve dietary adherence among hypertensive patients, with participants showing substantial improvement in both BP and dietary adherence scores. This success reflects the model’s strength in emphasizing social and environmental influences, suggesting that interventions in family-oriented cultures may benefit from leveraging social support and norms to drive behavior change [56, 57].
Predisposing, reinforcing, and enabling constructs in educational diagnosis and evaluation (PRECEDE) is another theoretical framework that serves as the foundation for several educational interventions. PRECEDE focuses on diagnosing specific factors that predispose, reinforce, or enable behavior change. In the intervention by Baghianimoghadam et al. in Iran, the model was instrumental in structuring an educational program that addressed specific barriers and reinforcing factors for hypertension management. This framework enabled the design of targeted educational content and provided reinforcement through follow-ups and community support, resulting in measurable improvements in participants’ knowledge and BP control [28]. By ensuring that programs are customized to the particular requirements and obstacles faced by specific groups, prior research has also confirmed the efficacy of the PRECEDE approach, particularly in community-based interventions [58, 59].
Geragogy, a model specifically focused on educating older adults, was another theoretical foundation applied in interventions targeting elderly populations with chronic illnesses, like hypertension. Geragogy emphasizes age-specific learning techniques that accommodate cognitive and sensory changes associated with aging. Ongkulna et al. [38] employed this model in a self-management education program for older adults in Thailand, finding that tailoring the intervention to meet age-related needs, such as providing simplified instructions and visual aids, leads to significant improvements in health literacy and self-efficacy. Geragogy’s approach acknowledges that older adults may require different educational strategies than younger populations, as shown in previous studies, which found that Geragogical methods improve health knowledge and self-care practices in older adults more effectively than standard educational approaches [60, 61].
In examining the correlation between educational programs and self-management among hypertensive patients, the data from your systematic review underscore the vital role that structured educational interventions play in enhancing self-management behaviors. Educational programs, particularly those tailored to hypertension management, significantly boost patients’ knowledge, self-efficacy, and adherence to health recommendations. For example, studies in your dataset, such as Li et al. [36] and Moradi et al. [37], demonstrate that education-driven initiatives lead to improved BP control and increased self-management capabilities, including medication adherence and lifestyle adjustments.
Programs integrating personalized coaching, mobile app-based guidance, and self-monitoring tools were particularly effective. These tools encourage patients to take a more active role in their treatment, resulting in better management of hypertension-related risks. Studies that utilized self-management frameworks, such as the HBM [42], further confirmed that interventions with a strong theoretical foundation resulted in measurable improvements in self-care behaviors and BP outcomes.
Comparing these findings with prior studies reinforces the positive relationship between education and self-management. Previous literature has consistently shown that hypertension patients benefit from education on lifestyle changes, medication adherence, and stress reduction [62, 63]. The synergy between education and self-management not only helps reduce hypertension risks but also fosters a sense of personal responsibility in patients, which is pivotal for the long-term management of chronic conditions [64, 65].
This systematic review provides valuable insights into the effectiveness of educational programs in improving self-management and health outcomes for hypertensive patients. However, several limitations should be considered when interpreting the findings. First, the studies included in the review are from diverse geographic regions, such as Iran, the United States, China, Italy, Thailand, and South Korea, which may introduce regional and cultural biases in the interventions. Cultural differences in health behaviors, attitudes toward self-management, and adherence to medical advice may limit the generalizability of the results across different populations.
Second, while RCTs were the predominant study design, a few studies used quasi-experimental or pre-post designs, which are subject to inherent biases and lack the rigorous control found in RCTs. This variation in study design could affect the reliability of the findings. Additionally, the sample sizes in some studies were relatively small (e.g., Sutipan et al. [41] with 20 participants), which could limit the statistical power of these studies and make it difficult to draw firm conclusions about the effects of the interventions on larger populations.
Another limitation is the heterogeneity in the interventions used across studies. The intervention formats ranged from face-to-face sessions to mobile applications, telephone-based guidance, and online discussions, making it challenging to determine which specific elements of the interventions were most effective. Additionally, variations in the duration of the interventions, which ranged from three weeks to six months, make it difficult to compare the long-term effectiveness of different programs. Moreover, outcomes were assessed using various scales, which might introduce inconsistencies in measuring the success of the interventions.
Finally, the quality assessment of the included studies using the CASP tool showed that most studies were categorized as “Strong” in quality, but there were a few studies in the “Medium” category. The presence of studies with moderate quality raises concerns about potential bias or incomplete reporting of intervention details, further limiting the strength of the conclusions drawn from this review.
The evidence highlights the positive impact of both face-to-face and technology-assisted interventions, including mobile applications and online platforms. Notably, the improvements in BP control, adherence to dietary recommendations (such as the DASH diet), and overall health behaviors indicate the potential of educational programs to support hypertensive patients in managing their condition more effectively.
The use of various theoretical models, including the HBM, BASNEF, and PRECEDE, provided a robust framework for many of the interventions, suggesting that a well-structured educational program with a strong theoretical foundation is likely to be more effective. However, the variability in intervention formats, study designs, and assessment methods highlights the need for further research to standardize the approaches used in such programs. Future studies should aim to address the limitations of sample size and study quality to strengthen the evidence base for these interventions.
Despite the promising results, the effectiveness of educational programs may depend on the context in which they are implemented. Cultural differences, the accessibility of technology, and the level of support available for patients are important factors that could influence the success of these interventions. More research is needed to explore the optimal combination of intervention strategies, durations, and theoretical models that could lead to sustainable improvements in the self-management of hypertension on a global scale.
In summary, this review supports the growing body of evidence indicating that educational programs play a crucial role in improving the management of hypertension. The findings underscore the importance of integrating educational strategies with self-management tools to empower patients to make informed decisions about their health and lifestyle.
Conclusion
Educational interventions significantly improve the self-management behaviors, knowledge, and self-efficacy of hypertensive patients.
Acknowledgments: The authors would like to thank all participants for their participation and cooperation throughout the study. They also thank the Head of the Health Polytechnic of the Jambi Ministry of Health for their support and assistance, as well as the researchers, data collection team, enumerator team, and all parties involved in this project.
Ethical Permissions: For this systematic literature review, ethical permissions are not required, as the research only examines and analyzes data that has been previously published in scientific publications. All sources used in this study are works that have been openly published and do not involve direct interaction with human or animal subjects. As part of the procedure, all analyzed data is ensured to meet the ethical standards of publication and the proper use of sources, in accordance with the applicable academic guidelines.
Conflicts of Interests: None declared.
Authors' Contribution: Roza E (First Author), Introduction Writer/Methodologist/Main Researcher (40%); Rusdi M (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Guspianto G (Third Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Hasibuan MHE (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: No funding was received.
High blood pressure (BP), often referred to as hypertension, is a common chronic illness that primarily affects the elderly. It is a significant risk factor for kidney failure, stroke, and cardiovascular diseases, contributing substantially to global morbidity and mortality rates [1-4]. Among older adults, the prevalence of hypertension is particularly high, largely due to age-related vascular changes and the increased occurrence of comorbid conditions, making it a critical health issue for this population [5, 6]. According to the World Health Organization, hypertension control remains suboptimal worldwide, especially among older individuals, who face challenges such as medication non-adherence, poor self-management behaviors, and limited access to tailored health education [7].
Self-management is widely regarded as an essential component of effective hypertension control. This practice includes activities such as monitoring BP, maintaining a balanced diet, adhering to prescribed medications, and engaging in regular physical exercise [8, 9]. Research has shown that consistent self-management behaviors can substantially reduce the risk of hypertension-related complications [10, 11]. However, elderly patients often encounter unique barriers to effective self-management, such as cognitive decline, physical limitations, and limited technological literacy, which can hinder their ability to actively manage their health [12-16].
Educational interventions tailored specifically to the elderly population are essential for addressing these barriers and empowering patients to take control of their hypertension management. Studies indicate that structured educational programs can improve self-efficacy, enhance knowledge about hypertension, and encourage sustainable lifestyle changes, all of which are vital for effective disease management [17]. Furthermore, educational models grounded in theories, such as the health belief model (HBM) and social cognitive theory (SCT) provide a structured approach to instilling motivation and promoting behavioral changes that are critical for managing chronic conditions in elderly populations [18].
With the rise of digital technology, innovative educational models have emerged, including mobile applications and telehealth programs. By making health information more convenient and accessible, telehealth-based educational programs have been shown to increase self-efficacy and encourage healthier lifestyle choices [19]. Digital health tools, such as mobile apps, have been effectively utilized to deliver information on medication adherence, dietary modifications, and lifestyle management for hypertensive patients, demonstrating that technology-assisted interventions can significantly improve health outcomes in elderly patients [20, 21]. Additionally, community-based programs and group education models, which provide social support alongside practical education, have proven effective in helping older adults adopt and maintain self-management behaviors [22, 23].
Despite these advancements, there is still a need for comprehensive educational models that specifically address the unique needs and limitations of elderly populations. Recent research highlights that multidimensional approaches combining digital tools with in-person support yield the most promising outcomes in terms of adherence, self-efficacy, and sustainable lifestyle changes [24]. However, further studies are needed to develop and refine these models to maximize their effectiveness in managing hypertension among the elderly [25, 26].
This systematic review aimed to consolidate evidence on educational interventions designed to improve the self-management of hypertension in elderly populations. By reviewing studies published from 2000 to 2024, this analysis evaluated the effectiveness of various educational models, identified key factors influencing self-management behaviors, and provided evidence-based recommendations for enhancing hypertension care in older adults. These insights are intended to guide healthcare practitioners in implementing effective, tailored educational strategies that improve hypertension outcomes in this vulnerable population.
Information and Methods
Study design
The preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2020 standards were followed in the design and execution of this systematic review conducted in 2024 [27]. The goal was to synthesize existing evidence on educational interventions that improve hypertension self-management among elderly populations.
Eligibility criteria
The inclusion and exclusion criteria were developed based on the population, intervention, comparison, outcomes, and study (PICOS) framework to ensure alignment with the research question (Table 1).
Table 1. Statements of the population, intervention, comparison, outcomes, and study (PICOS) framework
Information sources
To identify relevant studies, we systematically searched six electronic databases, including PubMed, Scopus, Web of Science, ScienceDirect, JSTOR, and Cochrane Library. These databases were chosen for their comprehensive coverage of health, clinical, and psychological research. The search encompassed publications from 2000 to 2024 to focus on the most recent 20 years of evidence. Additionally, we conducted hand searches of reference lists in eligible studies and performed citation tracking to identify potentially relevant studies. Experts in hypertension self-management were consulted for insights into unpublished or ongoing studies.
Search strategy
To ensure sensitivity and specificity, a medical librarian assisted in developing the search strategy. The search terms were formulated using both Medical Subject Headings (MeSH) and free-text keywords. The strategy combined terms related to population (“elderly,” “older adults,” “geriatric patients”), intervention (“hypertension education,” “self-management,” “educational models,” “telehealth,” “digital health,” “community-based programs”), and Outcomes (“self-efficacy,” “medication adherence,” “dietary adherence,” “blood pressure control”) (Table 2).
Table 2. Search string in databases

Study quality
The reviewers independently evaluated the literature to determine the quality for inclusion. Although this step is not mandatory in systematic review protocols, the reviewers considered it beneficial for identifying the strengths and limitations of the selected studies. Due to the diverse nature of the articles, the critical appraisal skills program (CASP) for randomized studies was chosen for its ability to systematically evaluate study quality. CASP offers a structured set of questions specifically designed for different study designs, particularly randomized studies. Each CASP checklist includes 11 questions with response options of “yes,” “no,” or “can’t tell,” facilitating a standardized appraisal process. Study quality is classified into three categories, including strong, moderate, and weak. A study is classified as weak if there are three non-affirmative responses, moderate if there are two non-affirmative responses (“can’t tell” or “no”), and strong if all of the responses are affirmative.
Risk of bias
The assessment of bias in each study was performed using the risk of bias in randomized studies (RoB 2) tool. This tool was chosen for its structured, validated framework tailored to detecting bias specifically within randomized controlled trials (RCTs), addressing essential areas, such as randomization, deviations from the planned interventions, missing outcome data, outcome measurement, and selective reporting. The RoB 2 tool provides a comprehensive and consistent approach to quality assessment, which strengthens the reliability of the review’s conclusions. It includes five domains that assess both internal and external validity, with results classified into four levels, including Low, some concerns, high, and very high. All authors reviewed and approved the RoB assessment results, incorporating feedback from external reviewers.
Data extraction and synthesis
To enhance understanding of the content within the eligible studies, key information was condensed into a table format. Two authors collaborated during this data-gathering process. Any discrepancies in the extracted data were resolved through mutual agreement. The extraction criteria included details, such as the primary author, year of publication, country, study design, sample size, mean age, outcome, intervention, model, duration, evaluation technique, and key findings.
Findings
The initial database query yielded 598 articles. Following the removal of 405 duplicates and irrelevant articles unrelated to the review’s focus, 193 articles were available for screening. In the eligibility evaluation, 159 articles were excluded for various reasons. Ultimately, only 15 studies fulfilled the criteria and advanced to the subsequent stage of data extraction and analysis (Figure 1; Table 3).

Figure 1. PRISMA flowchart for study selection.
Tabel 3. Characteristics of the eligible studies
General characteristics of the eligible studies
The studies reviewed in this analysis used a variety of interventions aimed at improving health outcomes through educational and self-management strategies. The studies were conducted in diverse countries, including Iran, the United States, China, Italy, Thailand, and South Korea, highlighting both cultural and regional approaches to non-pharmacological health interventions.
The majority of the studies employed RCTs, with a few utilizing quasi-experimental and pre-post study designs. RCTs were the predominant design, indicating a strong focus on controlled interventions for evaluating the effectiveness of educational and behavioral strategies.
Sample sizes varied significantly across studies, ranging from as few as 20 participants in some RCTs (e.g., Sutipan et al. [41]) to larger groups, such as the 253 participants in Li et al.’s [36] cluster RCT in China. Participants were primarily adults, with mean ages typically ranging from the 50s to 70s, reflecting a focus on older adults and individuals managing chronic conditions, particularly hypertension.
Intervention durations ranged from as short as three weeks [38] to as long as six months [30, 31]. Formats included face-to-face sessions, mobile application-based interventions, telephone-based guidance, and online group discussions, indicating a mix of in-person and technology-assisted education.
Outcomes were assessed using a variety of self-reported and validated scales. For example, dietary adherence was evaluated using the DASH diet questionnaire, while self-efficacy was commonly measured using the Self-Efficacy for Managing Chronic Disease Scale and other similar scales. BP control and physical activity were also frequently monitored, often using standard clinical instruments or validated questionnaires (e.g., ABPM for BP in the study by Figar et al. [34]). The primary outcomes varied but were generally centered on improving self-efficacy, adherence to dietary and health recommendations, and managing hypertension. Several studies targeted lifestyle modifications, including improvements in physical activity, dietary diversity, and stress management. Many of the studies reported significant improvements in key outcomes, such as increased knowledge, improved dietary adherence, and better self-management behaviors. Notable findings included reductions in BP (e.g., Kordvarkane et al. [35]), increased adherence to the DASH diet [30], and enhanced self-efficacy for managing chronic conditions [37].
Study quality assessment
Based on the assessment results, the eligible studies are generally classified in the strong category, while only three studies fall into the medium category (Table 4).
Table 4. Summary of quality assessment
Risk of bias assessment
According to the assessment across the five dimensions of the RoB 2 tool, most of the studies were found to be in the low risk of bias category (Figure 2).
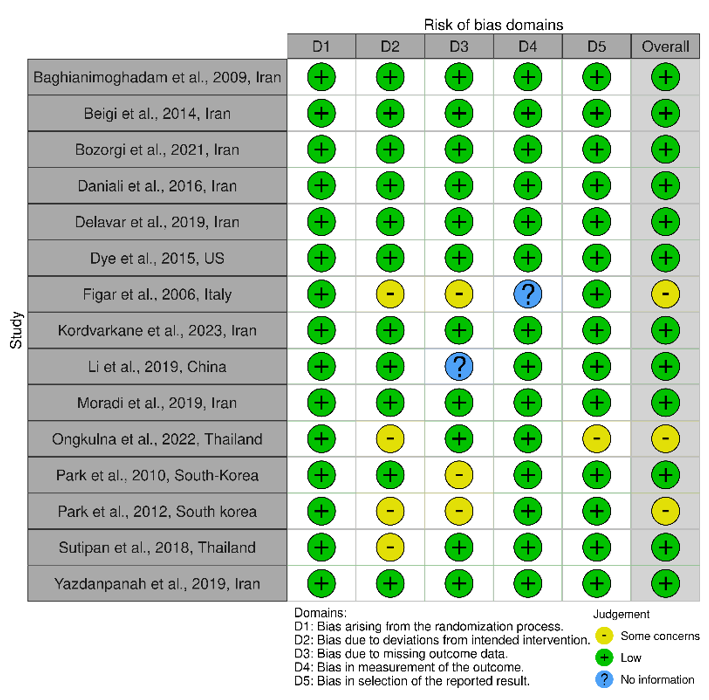
Figure 2. Traffic light plot for risk of bias assessment.
Intervention types and models
A wide range of intervention models was used across the studies, including educational programs, mobile application-based interventions, face-to-face group education, and self-management programs. Several theoretical models supported these interventions, including BASNEF, PRECEDE, Geragogy, and the HBM. These interventions aimed to improve knowledge, self-efficacy, and adherence to dietary and health practices, targeting sustainable health behaviors.
Outcomes
Several studies reported significant improvements in participants’ knowledge and self-efficacy following the interventions. For example, the intervention by Li et al. [36] in China, which used WeChat for health education, improved both BP control (p=0.002) and knowledge/self-efficacy.
Studies focusing on dietary interventions, such as adherence to the DASH diet [30], demonstrated positive effects on dietary adherence, BP control, and physical activity levels.
Improvements in health-related behaviors were observed, including healthy lifestyle practices [41] and self-care behaviors related to BP control [39]. Many studies noted significant reductions in BP, such as that by Figar et al. [34] in Italy, which demonstrated a BP reduction (p=0.02) with regular BP monitoring and empowerment education.
Discussion
This systematic review aimed to consolidate evidence on educational interventions designed to improve the self-management of hypertension in elderly populations. The studies reviewed in this analysis exhibited a wide range of characteristics and approaches, emphasizing non-pharmacological interventions aimed at improving health outcomes through educational and self-management strategies. Conducted across several countries, including Iran, the United States, China, Italy, Thailand, and South Korea, the studies highlighted cultural and regional variations in health interventions, particularly for managing chronic conditions, such as hypertension. This geographic diversity in study settings underscores the universal challenge of chronic disease management and the varying methodologies researchers have adopted in different sociocultural contexts. For instance, while studies from countries, such as Iran and Thailand tended to incorporate traditional face-to-face group educational sessions, other regions, like China, leveraged popular local digital platforms, such as WeChat to deliver health education in more accessible formats [36]. This adaptation to digital platforms is indicative of a global shift toward technology-driven healthcare solutions, especially in environments where face-to-face interaction may be limited by logistical constraints or during times of increased public health concerns.
Another notable characteristic among these studies is the variation in sample sizes, which ranged from as few as 20 participants to as many as 253. Smaller studies, such as Sutipan et al. [41] with 20 participants, often provide a more detailed examination of individual-level responses to interventions but may lack the power to reliably detect smaller effects. In contrast, larger studies, such as Li et al. [36], with a sample size of 253, enhance statistical power, offering more robust insights into intervention effectiveness at the population level. The wide age range, typically focusing on adults in their 50s to 70s, is another distinguishing factor. This age demographic reflects a focus on older adults who are generally more susceptible to chronic conditions and may particularly benefit from lifestyle interventions aimed at promoting self-management and improving overall quality of life [43]. The attention to this age group also reflects a public health priority, given the rising prevalence of hypertension and other chronic diseases in aging populations worldwide [44].
Intervention duration varied significantly, from a brief three-week program [38] to extended interventions lasting up to six months [30, 31]. Shorter interventions can provide immediate insights into the feasibility and short-term effects of an intervention but may not capture long-term adherence or sustainability. On the other hand, longer interventions are advantageous for observing sustained behavior change and determining whether health improvements persist over time. Such extended interventions might offer a better model for real-world applications, where long-term adherence is critical for effectively managing chronic conditions.
In terms of delivery format, the studies employed a mix of traditional and modern methods, ranging from face-to-face sessions to mobile app-based interventions, telephone guidance, and online group discussions. This variety reflects the growing recognition of the need for flexible and accessible healthcare delivery, especially in a post-pandemic world where remote options are increasingly valuable. Mobile health applications and other technology-assisted education methods allow participants to engage with intervention materials at their convenience, which can be particularly beneficial for individuals with limited mobility or those in rural areas with reduced access to healthcare facilities [45, 46]. At the same time, face-to-face interactions remain valuable for personalized guidance, offering opportunities for real-time feedback, social support, and engagement that digital platforms may lack [47-49].
Improvements in knowledge and self-efficacy are crucial components of chronic disease management, particularly in conditions requiring significant lifestyle changes, such as hypertension. Across the reviewed studies, multiple interventions demonstrated statistically significant increases in knowledge and self-efficacy, suggesting that structured educational programs can positively influence individuals’ ability to manage their health. For instance, Li et al. [36] utilized a WeChat-based group discussion for health education in China, which resulted in notable improvements in both BP control and self-efficacy scores among participants. The use of this popular social media platform allows for frequent interaction and support, which likely contributes to the effectiveness of the intervention. This finding aligns with Bozorgi et al. [30], who found that a mobile application-based intervention in Iran improves adherence to the DASH diet, physical activity, and self-efficacy levels. Such digital platforms may enhance accessibility and engagement, providing participants with convenient and continuous support that fosters knowledge retention and self-confidence in managing health behaviors [50, 51].
Previous research has also demonstrated the effectiveness of educational interventions in enhancing knowledge and self-efficacy. For example, a study by Bandura and Wessels [52] shows that interventions aimed at increasing self-efficacy can lead to sustained behavior change, as higher self-efficacy is directly associated with greater resilience in overcoming obstacles. Similarly, Clark and Dodge [53] emphasize the role of self-efficacy in promoting adherence to dietary and exercise regimens, particularly in hypertensive populations. By empowering patients with the knowledge and confidence needed to make informed health choices, these interventions can yield substantial long-term benefits.
In addition to mobile-based interventions, face-to-face educational sessions have also demonstrated substantial efficacy in improving knowledge and self-efficacy. For example, Park et al. [39] implemented the HAHA program in South Korea, which included face-to-face counseling and physical activity sessions. The program led to significant improvements in both self-efficacy and systolic BP control. This result aligns with findings from Yazdanpanah et al. [42] in Iran, where an educational intervention based on the HBM resulted in significant increases in medication adherence and self-efficacy. These findings suggest that in-person interactions allow for personalized feedback, real-time social support, and direct reinforcement of health knowledge, all of which can enhance participants’ self-efficacy and commitment to behavioral change.
The variation in delivery formats (ranging from digital platforms to face-to-face programs) suggests that the effectiveness of these interventions may depend on factors, such as accessibility, frequency of interaction, and participants’ preferences. Ongkulna et al. [38] demonstrated the success of the Geragogy-based self-management education program (GBSEP), which combines in-person sessions with Geragogy principles tailored to older adults. This program improves participants’ health literacy, self-efficacy, and self-management behaviors. These findings are comparable to a similar intervention by Dye et al. [33] in the United States, which used health coaches to foster self-management skills in older adults with hypertension. By adapting interventions to participants’ age-related learning needs, such programs enhance understanding and self-efficacy, facilitating better health behaviors over time.
These findings are consistent with the study using SCT by Bandura and Wessels [52], which posits that knowledge and self-efficacy are critical in driving behavior change. The reviewed studies align with this theory, indicating that well-designed educational interventions can significantly impact self-efficacy and, consequently, adherence to health-promoting behaviors. Taken together, this body of research demonstrates that improvements in both knowledge and self-efficacy are achievable across diverse formats and settings, underscoring the versatility and potential of educational interventions to support chronic disease management across different populations and health systems.
Theoretical models play a critical role in designing health interventions, particularly those aimed at improving self-management behaviors and health outcomes in chronic conditions, such as hypertension. These models provide a structured framework for understanding how individuals adopt and sustain health-promoting behaviors, which is essential for the effectiveness of interventions. In the studies reviewed, several theoretical models were employed to guide intervention development and ensure their success. These include the HBM, SCT, the PRECEDE-PROCEED model, the BASNEF Model, and Geragogy.
Each model contributes unique perspectives and mechanisms for understanding and influencing behavior, thereby supporting tailored and effective interventions. For example, interventions based on the HBM focus on modifying individuals’ perceptions about the severity of their condition, their susceptibility to complications, and the benefits of adopting preventive behaviors. Yazdanpanah et al. [42] used the HBM in their intervention with elderly patients in Iran, demonstrating that when patients perceived their hypertension as serious and recognized the benefits of medication adherence, their adherence significantly improved. This finding aligns with earlier studies showing that the HBM can effectively predict and enhance adherence to health recommendations by emphasizing individual belief systems [54, 55].
The BASNEF model, which combines elements of both the HBM and social influences, was also employed in several interventions to increase adherence to lifestyle modifications. This model considers the impact of social norms and enabling factors, such as family support and access to resources, which are crucial in environments where family dynamics and social support play a significant role in health management. Shahrbanoo Daniali et al. [31] in Iran used the BASNEF model to improve dietary adherence among hypertensive patients, with participants showing substantial improvement in both BP and dietary adherence scores. This success reflects the model’s strength in emphasizing social and environmental influences, suggesting that interventions in family-oriented cultures may benefit from leveraging social support and norms to drive behavior change [56, 57].
Predisposing, reinforcing, and enabling constructs in educational diagnosis and evaluation (PRECEDE) is another theoretical framework that serves as the foundation for several educational interventions. PRECEDE focuses on diagnosing specific factors that predispose, reinforce, or enable behavior change. In the intervention by Baghianimoghadam et al. in Iran, the model was instrumental in structuring an educational program that addressed specific barriers and reinforcing factors for hypertension management. This framework enabled the design of targeted educational content and provided reinforcement through follow-ups and community support, resulting in measurable improvements in participants’ knowledge and BP control [28]. By ensuring that programs are customized to the particular requirements and obstacles faced by specific groups, prior research has also confirmed the efficacy of the PRECEDE approach, particularly in community-based interventions [58, 59].
Geragogy, a model specifically focused on educating older adults, was another theoretical foundation applied in interventions targeting elderly populations with chronic illnesses, like hypertension. Geragogy emphasizes age-specific learning techniques that accommodate cognitive and sensory changes associated with aging. Ongkulna et al. [38] employed this model in a self-management education program for older adults in Thailand, finding that tailoring the intervention to meet age-related needs, such as providing simplified instructions and visual aids, leads to significant improvements in health literacy and self-efficacy. Geragogy’s approach acknowledges that older adults may require different educational strategies than younger populations, as shown in previous studies, which found that Geragogical methods improve health knowledge and self-care practices in older adults more effectively than standard educational approaches [60, 61].
In examining the correlation between educational programs and self-management among hypertensive patients, the data from your systematic review underscore the vital role that structured educational interventions play in enhancing self-management behaviors. Educational programs, particularly those tailored to hypertension management, significantly boost patients’ knowledge, self-efficacy, and adherence to health recommendations. For example, studies in your dataset, such as Li et al. [36] and Moradi et al. [37], demonstrate that education-driven initiatives lead to improved BP control and increased self-management capabilities, including medication adherence and lifestyle adjustments.
Programs integrating personalized coaching, mobile app-based guidance, and self-monitoring tools were particularly effective. These tools encourage patients to take a more active role in their treatment, resulting in better management of hypertension-related risks. Studies that utilized self-management frameworks, such as the HBM [42], further confirmed that interventions with a strong theoretical foundation resulted in measurable improvements in self-care behaviors and BP outcomes.
Comparing these findings with prior studies reinforces the positive relationship between education and self-management. Previous literature has consistently shown that hypertension patients benefit from education on lifestyle changes, medication adherence, and stress reduction [62, 63]. The synergy between education and self-management not only helps reduce hypertension risks but also fosters a sense of personal responsibility in patients, which is pivotal for the long-term management of chronic conditions [64, 65].
This systematic review provides valuable insights into the effectiveness of educational programs in improving self-management and health outcomes for hypertensive patients. However, several limitations should be considered when interpreting the findings. First, the studies included in the review are from diverse geographic regions, such as Iran, the United States, China, Italy, Thailand, and South Korea, which may introduce regional and cultural biases in the interventions. Cultural differences in health behaviors, attitudes toward self-management, and adherence to medical advice may limit the generalizability of the results across different populations.
Second, while RCTs were the predominant study design, a few studies used quasi-experimental or pre-post designs, which are subject to inherent biases and lack the rigorous control found in RCTs. This variation in study design could affect the reliability of the findings. Additionally, the sample sizes in some studies were relatively small (e.g., Sutipan et al. [41] with 20 participants), which could limit the statistical power of these studies and make it difficult to draw firm conclusions about the effects of the interventions on larger populations.
Another limitation is the heterogeneity in the interventions used across studies. The intervention formats ranged from face-to-face sessions to mobile applications, telephone-based guidance, and online discussions, making it challenging to determine which specific elements of the interventions were most effective. Additionally, variations in the duration of the interventions, which ranged from three weeks to six months, make it difficult to compare the long-term effectiveness of different programs. Moreover, outcomes were assessed using various scales, which might introduce inconsistencies in measuring the success of the interventions.
Finally, the quality assessment of the included studies using the CASP tool showed that most studies were categorized as “Strong” in quality, but there were a few studies in the “Medium” category. The presence of studies with moderate quality raises concerns about potential bias or incomplete reporting of intervention details, further limiting the strength of the conclusions drawn from this review.
The evidence highlights the positive impact of both face-to-face and technology-assisted interventions, including mobile applications and online platforms. Notably, the improvements in BP control, adherence to dietary recommendations (such as the DASH diet), and overall health behaviors indicate the potential of educational programs to support hypertensive patients in managing their condition more effectively.
The use of various theoretical models, including the HBM, BASNEF, and PRECEDE, provided a robust framework for many of the interventions, suggesting that a well-structured educational program with a strong theoretical foundation is likely to be more effective. However, the variability in intervention formats, study designs, and assessment methods highlights the need for further research to standardize the approaches used in such programs. Future studies should aim to address the limitations of sample size and study quality to strengthen the evidence base for these interventions.
Despite the promising results, the effectiveness of educational programs may depend on the context in which they are implemented. Cultural differences, the accessibility of technology, and the level of support available for patients are important factors that could influence the success of these interventions. More research is needed to explore the optimal combination of intervention strategies, durations, and theoretical models that could lead to sustainable improvements in the self-management of hypertension on a global scale.
In summary, this review supports the growing body of evidence indicating that educational programs play a crucial role in improving the management of hypertension. The findings underscore the importance of integrating educational strategies with self-management tools to empower patients to make informed decisions about their health and lifestyle.
Conclusion
Educational interventions significantly improve the self-management behaviors, knowledge, and self-efficacy of hypertensive patients.
Acknowledgments: The authors would like to thank all participants for their participation and cooperation throughout the study. They also thank the Head of the Health Polytechnic of the Jambi Ministry of Health for their support and assistance, as well as the researchers, data collection team, enumerator team, and all parties involved in this project.
Ethical Permissions: For this systematic literature review, ethical permissions are not required, as the research only examines and analyzes data that has been previously published in scientific publications. All sources used in this study are works that have been openly published and do not involve direct interaction with human or animal subjects. As part of the procedure, all analyzed data is ensured to meet the ethical standards of publication and the proper use of sources, in accordance with the applicable academic guidelines.
Conflicts of Interests: None declared.
Authors' Contribution: Roza E (First Author), Introduction Writer/Methodologist/Main Researcher (40%); Rusdi M (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Guspianto G (Third Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%); Hasibuan MHE (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (20%)
Funding/Support: No funding was received.
Article Type: Systematic Review |
Subject:
Health Promotion Approaches
Received: 2024/11/10 | Accepted: 2024/12/6 | Published: 2024/12/10
Received: 2024/11/10 | Accepted: 2024/12/6 | Published: 2024/12/10
References
1. Zhang M, Liu Y, Zhang W, Yang J, Yang W, Zhou J, et al. Exploring perceived challenges of self‐management in low‐income older people with hypertension: A qualitative study. Int J Nurs Pract. 2022;28(3):e13059. [Link] [DOI:10.1111/ijn.13059]
2. Putri SE, Rekawati E, Wati DNK. Effectiveness of self-management on adherence to self-care and on health status among elderly people with hypertension. J Public Health Res. 2021;10(s1):jphr.2021.2406. [Link] [DOI:10.4081/jphr.2021.2406]
3. Hansell MW, Mann EM, Kirk JK. Hypertension treatment strategies for older adults. J Fam Pract. 2017;66(9):546-54. [Link]
4. Moss KO, Still CH, Jones LM, Blackshire G, Wright KD. Hypertension self-management perspectives from African American older adults. West J Nurs Res. 2019;41(5):667-84. [Link] [DOI:10.1177/0193945918780331]
5. Pandit AU, Tang JW, Bailey SC, Davis TC, Bocchini M V, Persell SD, et al. Education, literacy, and health: Mediating effects on hypertension knowledge and control. Patient Educ Couns. 2009;75(3):381-5. [Link] [DOI:10.1016/j.pec.2009.04.006]
6. Goudarzi H, Barati M, Bashirian S, Moeini B. Determinants of medication adherence among hypertensive patients using the Pender's health promotion model. J Educ Health Promot. 2020;9(1):89. [Link] [DOI:10.4103/jehp.jehp_687_19]
7. Kurt D, Gurdogan EP. The effect of self-management support on knowledge level, treatment compliance and selfcare management in patients with hypertension. Aust J Adv Nurs. 2022;39(3):14-23. [Link] [DOI:10.37464/2020.393.543]
8. Parati G, Lombardi C, Pengo M, Bilo G, Ochoa JE. Current challenges for hypertension management: From better hypertension diagnosis to improved patients' adherence and blood pressure control. Int J Cardiol. 2021;331:262-9. [Link] [DOI:10.1016/j.ijcard.2021.01.070]
9. Ampofo AG, Khan E, Ibitoye MB. Understanding the role of educational interventions on medication adherence in hypertension: A systematic review and meta-analysis. Heart Lung. 2020;49(5):537-47. [Link] [DOI:10.1016/j.hrtlng.2020.02.039]
10. McManus RJ, Little P, Stuart B, Morton K, Raftery J, Kelly J, et al. Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: Randomised controlled trial. BMJ. 2021;372:m4858. [Link] [DOI:10.1136/bmj.m4858]
11. Khoong EC, Olazo K, Rivadeneira NA, Thatipelli S, Barr-Walker J, Fontil V, et al. Mobile health strategies for blood pressure self-management in urban populations with digital barriers: Systematic review and meta-analyses. NPJ Digit Med. 2021;4(1):114. [Link] [DOI:10.1038/s41746-021-00486-5]
12. Khanal MK, Bhandari P, Dhungana RR, Bhandari P, Rawal LB, Gurung Y, et al. Effectiveness of community-based health education and home support program to reduce blood pressure among patients with uncontrolled hypertension in Nepal: A cluster-randomized trial. PLoS One. 2021;16(10):e0258406. [Link] [DOI:10.1371/journal.pone.0258406]
13. Khoe LC, Wangge G, Soewondo P, Tahapary DL, Widyahening IS. The implementation of community-based diabetes and hypertension management care program in Indonesia. PLoS One. 2020;15(1):e0227806. [Link] [DOI:10.1371/journal.pone.0227806]
14. Valdes Gonzalez Y, Campbell NRC, Pons Barrera E, Calderón Martínez M, Pérez Carrera A, Morales Rigau JM, et al. Implementation of a community‐based hypertension control program in Matanzas, Cuba. J Clin Hypertens. 2020;22(2):142-9. [Link] [DOI:10.1111/jch.13814]
15. Kurnia AD, Melizza N, Ruhyanudin F, Masruroh NL, Prasetyo YB, Setyowati CI, et al. The effect of educational program on hypertension management toward knowledge and attitude among uncontrolled hypertension patients in rural area of Indonesia. Community Health Equity Res Policy. 2022;42(2):181-8. [Link] [DOI:10.1177/0272684X20972846]
16. Sujarwoto S, Maharani A. Participation in community-based health care interventions (CBHIs) and its association with hypertension awareness, control and treatment in Indonesia. PLoS One. 2020;15(12):e0244333. [Link] [DOI:10.1371/journal.pone.0244333]
17. Suriyawong W, Pipatpiboon N. Social cognitive theory-based interventions on healthy lifestyles for hypertensive patients: A systematic review. CMU J Nat Sci. 2022;21(3):e2022040. [Link] [DOI:10.12982/CMUJNS.2022.040]
18. Kolcu M, Ergun A. Effect of a nurse‐led hypertension management program on quality of life, medication adherence and hypertension management in older adults: A randomized controlled trial. Geriatr Gerontol Int. 2020;20(12):1182-9. [Link] [DOI:10.1111/ggi.14068]
19. Chalfont G, Mateus C, Varey S, Milligan C. Self-efficacy of older people using technology to self-manage COPD, hypertension, heart failure, or dementia at home: An overview of systematic reviews. Gerontologist. 2021;61(6):e318-34. [Link] [DOI:10.1093/geront/gnaa045]
20. Saragih ID, Wei C, Batubara SO, Saragih IS, Lee B. Effects of technology‐assisted interventions for people with dementia: A systematic review and meta‐analysis. J Nurs Scholarsh. 2023;55(1):291-303. [Link] [DOI:10.1111/jnu.12808]
21. Albarqi MN. Exploring the effectiveness of technology-assisted interventions for promoting independence in elderly patients: A systematic review. Healthcare. 2024;12(21):2105. [Link] [DOI:10.3390/healthcare12212105]
22. Higa C, Davidson EJ, Loos JR. Integrating family and friend support, information technology, and diabetes education in community-centric diabetes self-management. J Am Med Inform Assoc. 2021;28(2):261-75. [Link] [DOI:10.1093/jamia/ocaa223]
23. Wong AKC, Wong FKY, Chow KKS, Kwan DKS, Lau DYS, Lau ACK. A health-social service partnership programme for improving the health self-management of community-dwelling older adults: A hybrid effectiveness-implementation pilot study protocol. Pilot Feasibility Stud. 2023;9(1):184. [Link] [DOI:10.1186/s40814-023-01412-0]
24. Muhihi AJ, Anaeli A, Mpembeni RNM, Sunguya BF, Leyna G, Kakoko D, et al. Prevalence, awareness, treatment, and control of hypertension among young and middle‐aged adults: Results from a community‐based survey in rural Tanzania. Int J Hypertens. 2020;2020(1):9032476. [Link] [DOI:10.1155/2020/9032476]
25. Omboni S, McManus RJ, Bosworth HB, Chappell LC, Green BB, Kario K, et al. Evidence and recommendations on the use of telemedicine for the management of arterial hypertension: An international expert position paper. Hypertension. 2020;76(5):1368-83. [Link] [DOI:10.1161/HYPERTENSIONAHA.120.15873]
26. Sapna FNU, Raveena FNU, Chandio M, Bai K, Sayyar M, Varrassi G, et al. Advancements in heart failure management: A comprehensive narrative review of emerging therapies. Cureus. 2023;15(10):e46486. [Link] [DOI:10.7759/cureus.46486]
27. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [Link] [DOI:10.1136/bmj.n71]
28. Baghianimoghadam MH, Rahaee Z, Morowatisharifabad MA, Sharifirad G, Andishmand A, Azadbakht L. Effects of education on self-monitoring of blood pressure based on BASNEF model in hypertensive patients. J Res Med Sci. 2009;15(2):70-7. [Link]
29. Babaee Beigi MA, Zibaeenezhad MJ, Aghasadeghi K, Jokar A, Shekarforoush S, Khazraei H. The effect of educational programs on hypertension management. Int Cardiovasc Res J. 2014;8(3):94-8. [Link]
30. Bozorgi A, Hosseini H, Eftekhar H, Majdzadeh R, Yoonessi A, Ramezankhani A, et al. The effect of the mobile "blood pressure management application" on hypertension self-management enhancement: A randomized controlled trial. Trials. 2021;22(1):413. [Link] [DOI:10.1186/s13063-021-05270-0]
31. Shahrbanoo Daniali S, Ali Eslami A, Reza Maracy M, Shahabi J, Mostafavi-Darani F. The impact of educational intervention on self-care behaviors in overweight hypertensive women: A randomized control trial. ARYA Atheroscler. 2017;13(1):20-8. [Link]
32. Delavar F, Pashaeypoor S, Negarandeh R. The effects of self-management education tailored to health literacy on medication adherence and blood pressure control among elderly people with primary hypertension: A randomized controlled trial. Patient Educ Couns. 2020;103(2):336-42. [Link] [DOI:10.1016/j.pec.2019.08.028]
33. Dye CJ, Williams JE, Evatt JH. Improving hypertension self-management with community health coaches. Health Promot Pract. 2015;16(2):271-81. [Link] [DOI:10.1177/1524839914533797]
34. Figar S, Galarza C, Petrlik E, Hornstein L, Rodríguez Loria G, Waisman G, et al. Effect of education on blood pressure control in elderly persons: A randomized controlled trial. Am J Hypertens. 2006;19(7):737-43. [Link] [DOI:10.1016/j.amjhyper.2005.10.005]
35. Kordvarkane Z, Oshvandi K, Mohammadi Y, Azizi A. Effect of education based on the common-sense model of self-regulation on blood pressure and self-management of hypertensive patients: A clinical trial study. Int J Nurs Sci. 2023;10(3):294-301. [Link] [DOI:10.1016/j.ijnss.2023.06.009]
36. Li X, Li T, Chen J, Xie Y, An X, Lv Y, et al. A Wechat-based self-management intervention for community middle-aged and elderly adults with hypertension in Guangzhou, China: A cluster-randomized controlled trial. Int J Environ Res Public Health. 2019;16(21):4058. [Link] [DOI:10.3390/ijerph16214058]
37. Moradi M, Nasiri M, Jahanshahi M, Hajiahmadi M. The effects of a self-management program based on the 5 A's model on self-efficacy among older men with hypertension. Nurs Midwifery Stud. 2019;8(1):21-7. [Link] [DOI:10.4103/nms.nms_97_17]
38. Ongkulna K, Panuthai S, Pothiban L, Chintanawat R. Enhancing self-management through Geragogy-based education in older adults with uncontrolled hypertension: A randomized controlled trial. Pac Rim Int J Nurs Res. 2022;26(4):690-705. [Link]
39. Park YH, Song M, Cho BL, Lim JY, Song W, Kim SH. The effects of an integrated health education and exercise program in community-dwelling older adults with hypertension: A randomized controlled trial. Patient Educ Couns. 2011;82(1):133-7. [Link] [DOI:10.1016/j.pec.2010.04.002]
40. Park YH, Chang H, Kim J, Kwak JS. Patient-tailored self-management intervention for older adults with hypertension in a nursing home. J Clin Nurs. 2013;22(5-6):710-22. [Link] [DOI:10.1111/j.1365-2702.2012.04236.x]
41. Sutipan P, Intarakamhang U, Kittipichai W, Macaskill A. Effects of self-management program on healthy lifestyle behaviors among elderly with hypertension. Int J Behav Sci. 2018;13(2):38-50. [Link]
42. Yazdanpanah Y, Moghadam ARS, Mazlom SR, Beigloo RHA, Mohajer S. Effect of an educational program based on health belief model on medication adherence in elderly patients with hypertension. Evid Based Care J. 2019;9(1):52-62. [Link]
43. Nagano H, Sparrow WA, Mizukami K, Sarashina E, Begg R. A cross-sectional study of foot-ground clearance in healthy community dwelling Japanese cohorts aged 50, 60 and 70 years. BMC Geriatr. 2021;21(1):166. [Link] [DOI:10.1186/s12877-021-02117-w]
44. Lee J, Yu H, Cho HH, Kim M, Yang S. Ageism between medical and preliminary medical persons in Korea. Ann Geriatr Med Res. 2020;24(1):41-9. [Link] [DOI:10.4235/agmr.19.0043]
45. Du Y, Dennis B, Rhodes SL, Sia M, Ko J, Jiwani R, et al. Technology-assisted self-monitoring of lifestyle behaviors and health indicators in diabetes: Qualitative study. JMIR Diabetes. 2020;5(3):e21183. [Link] [DOI:10.2196/21183]
46. Jain SR, Sui Y, Ng CH, Chen ZX, Goh LH, Shorey S. Patients' and healthcare professionals' perspectives towards technology-assisted diabetes self-management education. A qualitative systematic review. PLoS One. 2020;15(8):e0237647. [Link] [DOI:10.1371/journal.pone.0237647]
47. White C, Vanc A, Stafford G. Internal communication, information satisfaction, and sense of community: The effect of personal influence. J Public Relat Res. 2010;22(1):65-84. [Link] [DOI:10.1080/10627260903170985]
48. McDonald J. Is "as good as face-to-face" as good as it gets. J Asynchronous Learn Netw. 2002;6(2):10-23. [Link] [DOI:10.24059/olj.v6i2.1866]
49. Soltani D, Azizi B, Behnoush AH, Meysamie A, Aein A, Nayebirad S, et al. Is lifestyle modification with individual face-to-face education and counseling more effective than usual care for controlling hypertension? A systematic review and meta-analysis of randomized controlled trials. Health Educ Res. 2023;38(5):490-512. [Link] [DOI:10.1093/her/cyad028]
50. De Luca V, Lazic V, Birov S, Piesche K, Beyhan O, Pengo MF, et al. Digitally enabled health service for the integrated management of hypertension: a participatory user-centred design process. Int J Environ Res Public Health. 2021;18(23):12442. [Link] [DOI:10.3390/ijerph182312442]
51. Khanijahani A, Akinci N, Quitiquit E. A systematic review of the role of telemedicine in blood pressure control: Focus on patient engagement. Curr Hypertens Rep. 2022;24(7):247-58. [Link] [DOI:10.1007/s11906-022-01186-5]
52. Bandura A, Wessels S. Self-efficacy. Cambridge: Cambridge University Press; 1997. [Link]
53. Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Educ Behav. 1999;26(1):72-89. [Link] [DOI:10.1177/109019819902600107]
54. Nouri K, Nazari M, Kaveh MH, Hosseini FS. Effectiveness of a health belief model-based educational intervention on treatment adherence among type 2 diabetic patients: Insights from a randomized controlled trial in Iran. J Educ Community Health. 2024;11(2):98-106. [Link] [DOI:10.34172/jech.2585]
55. Dos Santos Ximenes H. Health belief model through enhancing home self-care in hypertensive patients. Public Health Med Sci. 2024;1(1):1-6. [Link]
56. Yang TJ, Cooper LA, Boulware LE, Thornton RLJ. Leveraging delivery of blood pressure control interventions among low-income African American adults: Opportunities to increase social support and produce family-level behavior change. Ethn Dis. 2019;29(4):549-58. [Link] [DOI:10.18865/ed.29.4.549]
57. Zeid W, Makledy FA, Ismail MA, El Gammal HA. Effect of family-oriented health education program on awareness, adherence to treatment and control among hypertensive patients. Suez Canal Univ Med J. 2014;17(1):29-38. [Link] [DOI:10.21608/scumj.2014.45589]
58. Turkson-Ocran RAN, Ogungbe O, Botchway M, Baptiste DL, Owusu B, Ajibewa T, et al. Hypertension management to reduce racial/ethnic disparities: Clinical and community-based interventions. Curr Cardiovasc Risk Rep. 2024;18(12):239-58. [Link] [DOI:10.1007/s12170-024-00750-9]
59. Calano BJD, Cacal MJB, Cal CB, Calletor KP, Guce FICC, Bongar MV V, et al. Effectiveness of a community‐based health programme on the blood pressure control, adherence and knowledge of adults with hypertension: A PRECEDE‐PROCEED model approach. J Clin Nurs. 2019;28(9-10):1879-88. [Link] [DOI:10.1111/jocn.14787]
60. Mansyur S, Irwan AM, Arafat R, Hardianto Y. Effective health education methods to improve self-care in older people with chronic heart failure: A systematic review. Health Sci Rev. 2022;5:100060. [Link] [DOI:10.1016/j.hsr.2022.100060]
61. Usman S, Irwan AM, Arafat R. Family involvement in low-salt diet for hypertensive older adults. Work Older People. 2023;27(1):1-14. [Link] [DOI:10.1108/WWOP-05-2021-0022]
62. Lee YM, Kim RB, Lee HJ, Kim K, Shin MH, Park HK, et al. Relationships among medication adherence, lifestyle modification, and health-related quality of life in patients with acute myocardial infarction: A cross-sectional study. Health Qual Life Outcomes. 2018;16(1):100. [Link] [DOI:10.1186/s12955-018-0921-z]
63. Ojangba T, Boamah S, Miao Y, Guo X, Fen Y, Agboyibor C, et al. Comprehensive effects of lifestyle reform, adherence, and related factors on hypertension control: A review. J Clin Hypertens. 2023;25(6):509-20. [Link] [DOI:10.1111/jch.14653]
64. Balduino AF, Mantovani MF, Lacerda MR, Marin MJ, Wal ML. Experience of hypertensive patients with self‐management of health care. J Adv Nurs. 2016;72(11):2684-94. [Link] [DOI:10.1111/jan.13022]
65. Fix GM, Cohn ES, Solomon JL, Cortés DE, Mueller N, Kressin NR, et al. The role of comorbidities in patients' hypertension self-management. Chronic Illn. 2013;10(2):81-92. [Link] [DOI:10.1177/1742395313496591]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |