Volume 12, Issue 4 (2024)
Health Educ Health Promot 2024, 12(4): 661-674 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dahmardeh Kemmak F, Sarbaz M, Mousavi Baigi S, Marouzi P, Sheykhotayefeh M, Kimiafar K. Physicians’ and Nurses’ Attitudes, Awareness, Knowledge, and Skill in Telemedicine. Health Educ Health Promot 2024; 12 (4) :661-674
URL: http://hehp.modares.ac.ir/article-5-77768-en.html
URL: http://hehp.modares.ac.ir/article-5-77768-en.html
F. Dahmardeh Kemmak1, M. Sarbaz2, S.F. Mousavi Baigi1, P. Marouzi2, M. Sheykhotayefeh2, Kh. Kimiafar *2
1- “Department of Health Information Technology, School of Paramedical and Rehabilitation Sciences” and “Student of Research Committee”, Mashhad University of Medical Sciences, Mashhad, Iran
2- Department of Health Information Technology, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran
2- Department of Health Information Technology, School of Paramedical and Rehabilitation Sciences, Mashhad University of Medical Sciences, Mashhad, Iran
Full-Text [PDF 737 kb]
(2237 Downloads)
| Abstract (HTML) (773 Views)
Full-Text: (63 Views)
Introduction
Telemedicine is defined as using web-based sources and electronic information together with advanced digital network technology to promote remote professional health services, publish medical safety reports, present health-related training to people, and monitor public health [1]. Indeed, telemedicine is a branch of medicine that uses electronic media to build relationships among healthcare employees, including physicians, nurses, healthcare providers, and patients. As a vital factor for health specialists, telemedicine facilitates the exchange of information for the diagnosis, treatment, and prevention of diseases and traumas, as well as assessment, research, and healthcare providers’ training, improving individual and social health [2]. Today, telemedicine, employed by numerous medical specialists, such as cardiologists, neurologists, surgeons, optometrists, radiologists, and pediatricians is recognized as an approach to improving care access, quality, and efficiency [3]. In addition, telemedicine shortens patients’ hospitalization time, reduces the number of visits and care-associated costs, improves healthcare access, decreases care traveling time and cost, and enhances patient satisfaction [4, 5]. Many care professionals prefer to work in metropolises, and this issue results in the shortage of healthcare services in rural and underprivileged regions. In the meantime, telemedicine can be a promising solution for many of these drawbacks by eliminating the barriers of physical distance [6]. On the other hand, the World Health Organization (WHO) recommends introducing telemedicine in locales with high patient demands [7]. Despite numerous likely barriers, such as the inability to examine physically, and limited access to sensitive communities with low literacy, like villagers, ethnic minorities, elderly patients, and poor socioeconomic communities, telemedicine is counted as a helpful tool for physicians and patient care [6]. Telemedicine is historically used to provide healthcare to rural populations to manage chronic diseases, psychological and medical conditions, and real-time visits in acute care settings and facilitates video counseling and the use of mobile apps to provide medical consultation, diagnosis, and treatment and reduce the risk of infection. On the whole, many physicians believe that telemedicine is extensively promising for the management of patient care [8, 9].
Although the present advantages of telemedicine have been proved, the health domain has been slow to adopt Information and Communication Technology (ICT) compared to other sectors [10]. There are many reasons why the implementation of e-health systems is still challenging despite the existing studies on its clinical benefits, efficient cost, and high healthcare accessibility at macro levels [11-13]. Regardless of the merits and potential technical superiority of telemedicine, its acceptance is often considered a failed project [14], and user non-acceptance is one of the pivotal causes of failure in this respect [15]. In other words, to ensure telemedicine acceptance and use, it is necessary to possess gross resource capital and human forces and attempt to recognize its utility [4]. On the other hand, since the success of every novel technology depends on many factors, such as the respective professionals’ knowledge and perceptions of the concept, acquired skills, and working environments [16], health specialists’ attitudes, awareness, knowledge, and skill in telemedicine are among the imperatives of the successful implementation of telemedicine [17].
Despite the increasing contribution of telemedicine to healthcare and studies on physicians’ and nurses’ attitudes toward telemedicine, a few systematic reviews have synthesized the best evidence and provided a general view in this domain, and neither has so far examined physicians’ and nurses’ attitudes, awareness, knowledge, and skill as health professionals. Hence, the present systematic review investigated physicians’ and nurses’ attitudes, knowledge, awareness, and skills in telemedicine.
Information and Methods
Design
This systematic review followed PRISMA guidelines to report evidence from included studies [18, 19]. In this respect, the researchers searched some keywords in titles, abstracts, and the PubMed, Embase, Scopus, and Web of Sciences databases on March, 2023, and employed the MeSH and Emtree keywords and terms in the three below categories to search the databases.
1. Physicians OR Physician OR Doctors OR Doctor OR Nurses OR Nurse OR "Personnel, nursing" OR "Nursing personnel" OR "Registered nurses" OR "Nurse, registered" OR "Nurses, registered" OR "Registered nurse".
2. Attitude OR Attitudes OR Knowledge OR Awareness OR Awarenesses OR Skill OR Skills.
3. "Telemedicine" OR "Telerehabilitation" OR "telehealth" OR "Mobile Health" OR "Health, Mobile" OR "Virtual Medicine" OR "Medicine, Virtual" OR "eHealth" OR "mHealth" (Table 1).
Table 1. Search strategy for each database

Eligibility criteria
Studies that possessed the following inclusion criteria were entered into the examination process:
1) Cross-sectional studies investigating physicians’ and nurses’ attitudes, awareness, knowledge, and skill in telemedicine;
2) Studies examining physician and nurse populations.
On the other hand, the exclusion criteria were:
1) Publication types other than papers of high-prestigious journals, such as books, review papers, and letters to editors-in-chief;
2) Not accessing the full text of the paper in English;
3) Irrelevance of the title, abstract, or full text to the purpose of the study.
Data extraction and synthesis
After the extraction of studies from the databases, repeated studies were removed. First, titles and abstracts were screened independently based on the eligibility criteria. Papers lacking the inclusion criteria were omitted from the investigation. Then, the full texts were retrieved and screened independently by two researchers based on the eligibility criteria. The inter-researcher conflicts were solved through discussions. A similar checklist was used for data extraction. The data items in this checklist included the reference, examined country, publishing year, applied instruments, study purposes, telemedicine attitudes, telemedicine knowledge, telemedicine awareness, telemedicine skills, and main findings.
Quality assessment
Joanna Briggs Institute’s (JBI) critical appraisal checklist specific to cross-sectional studies was used for the quality assessment of the included studies [20]. In particular, with eight questions for assessing the quality of studies, this checklist involves the following issues: The inclusion criteria of samples, examined population, examined setting, and valid and reliable measurement instruments (mentioning the validity and reliability of the questionnaires). The included studies used standard measurement criteria, identified confounding factors, pursued strategies to cope with confounding factors, reported valid results, and followed appropriate statistical analyses. The responses to the questions included four yes, no, unclear, and not applicable categories. Positively and negatively answered questions received scores of 1 and 0, respectively, and the maximum quality score of every study was 8. If the quality score of a study was <5, it was omitted from the review.
Findings
Selection of studies
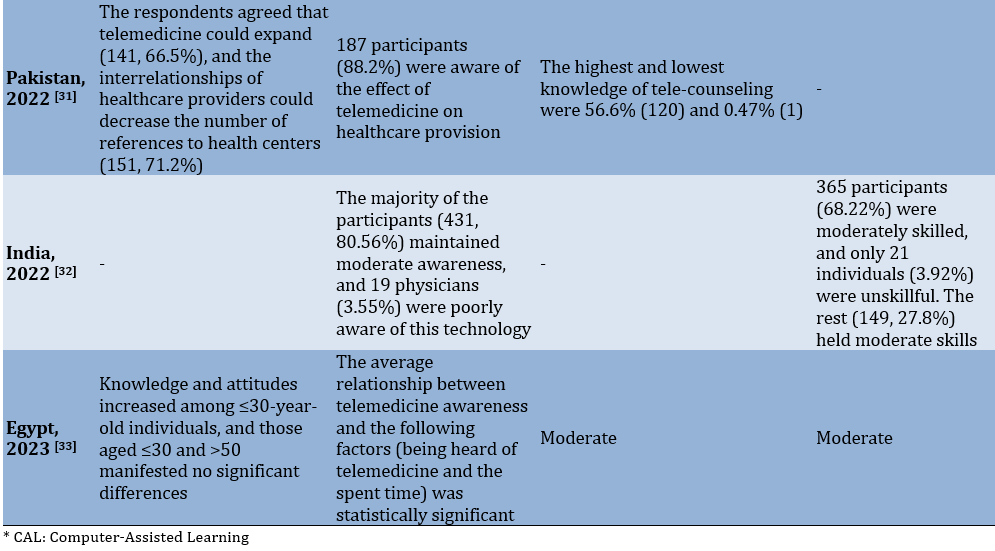
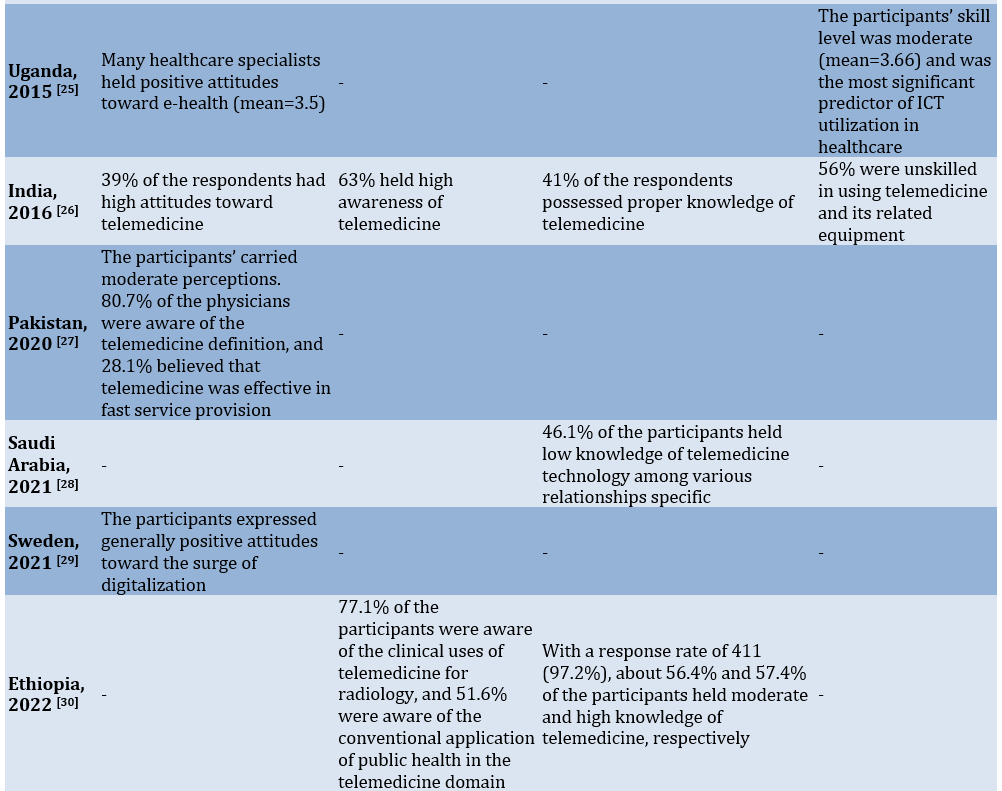
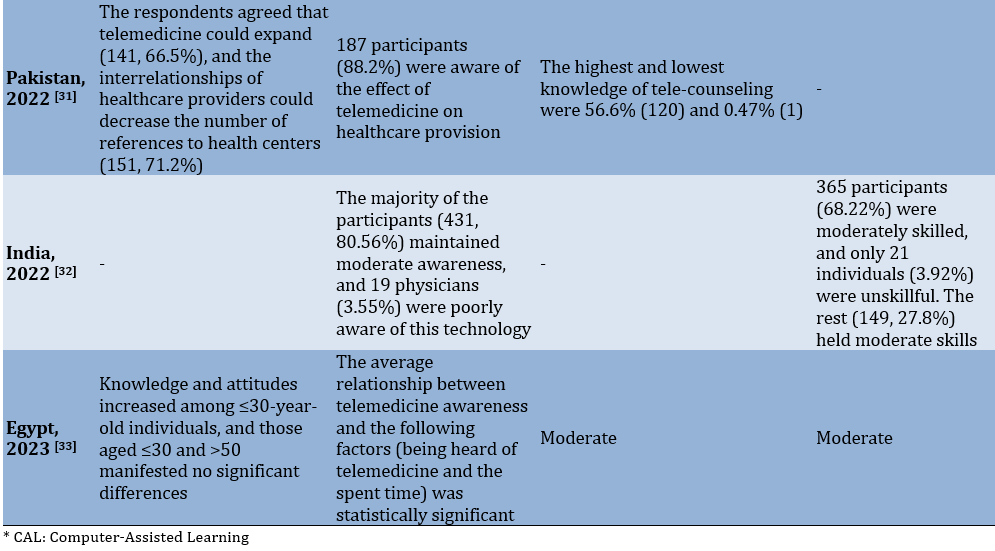
The search into scientific databases led to the retrieval of a total of 9398 studies initially. After the omission of repetitive cases (2873), 6525 studies remained for the title and abstract examination. 6494 studies not aligning with the purpose of the study were removed. Then, 31 remaining papers were examined with their full texts, and finally, 13 eligible papers were entered into the study (Table 2; Figure 1).
Table2. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist
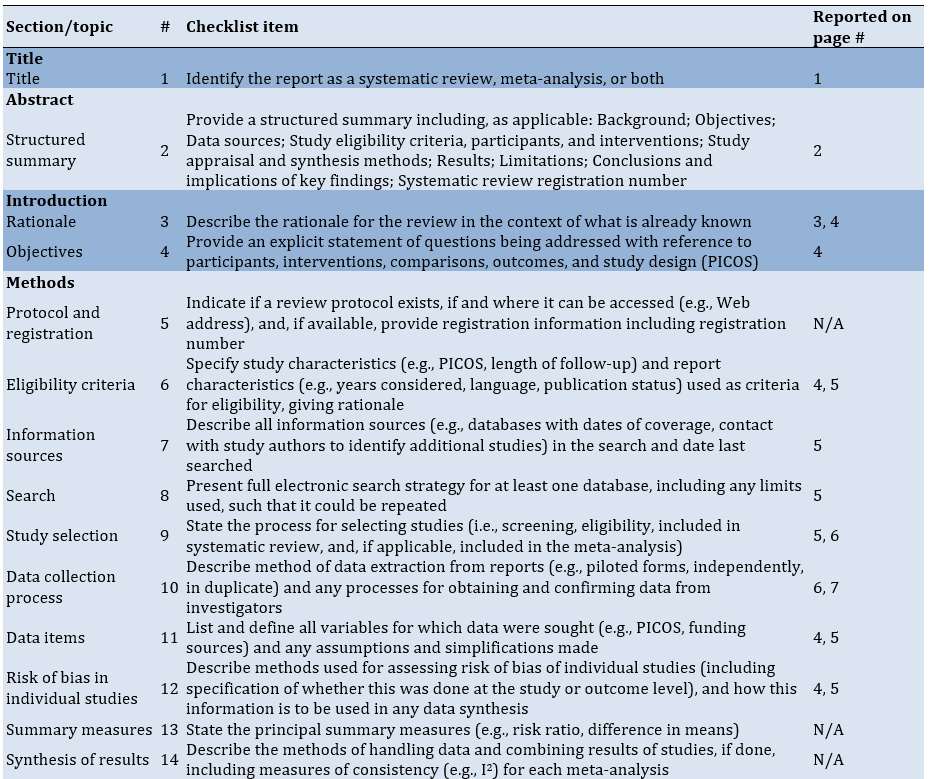
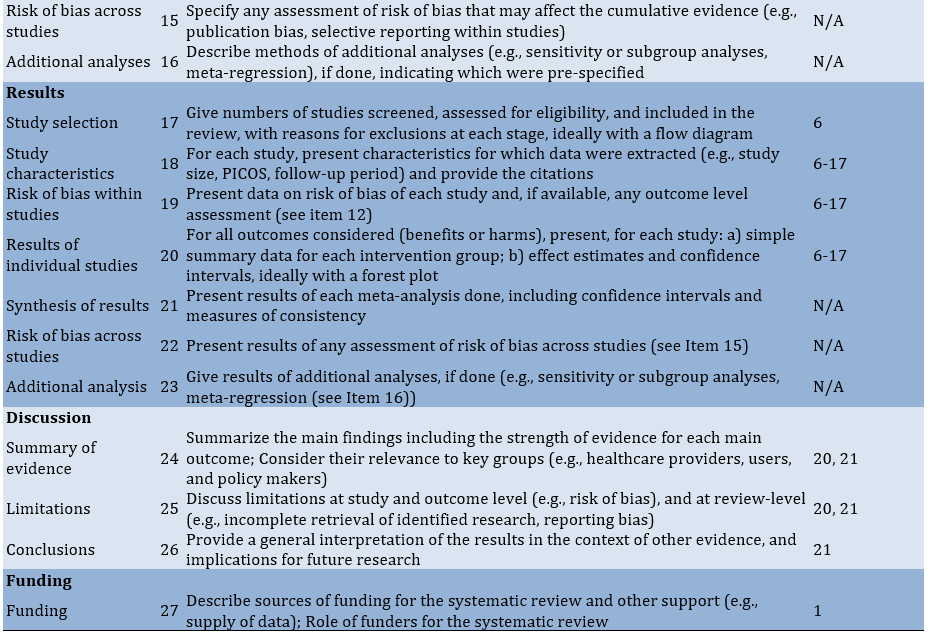
Figure 1. Study selection PRISMA
Quality assessment
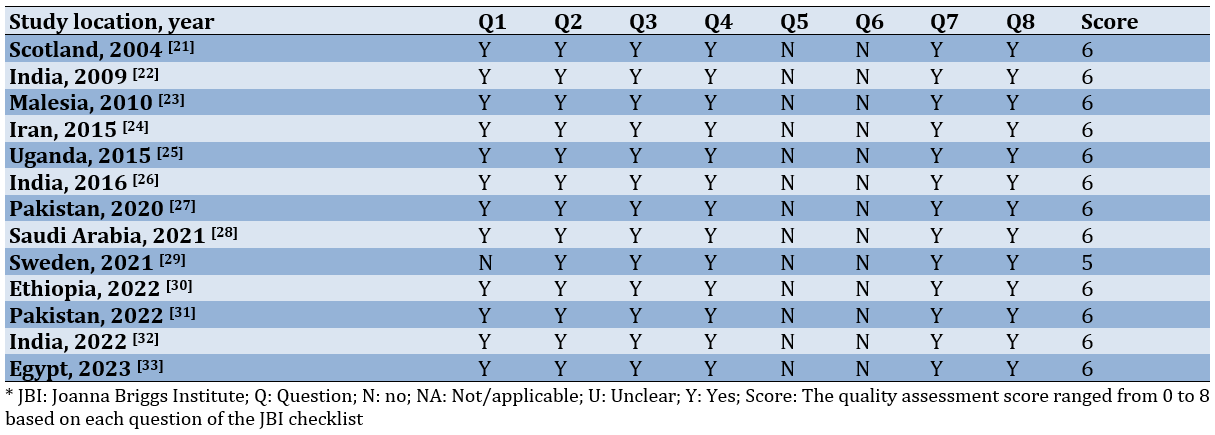
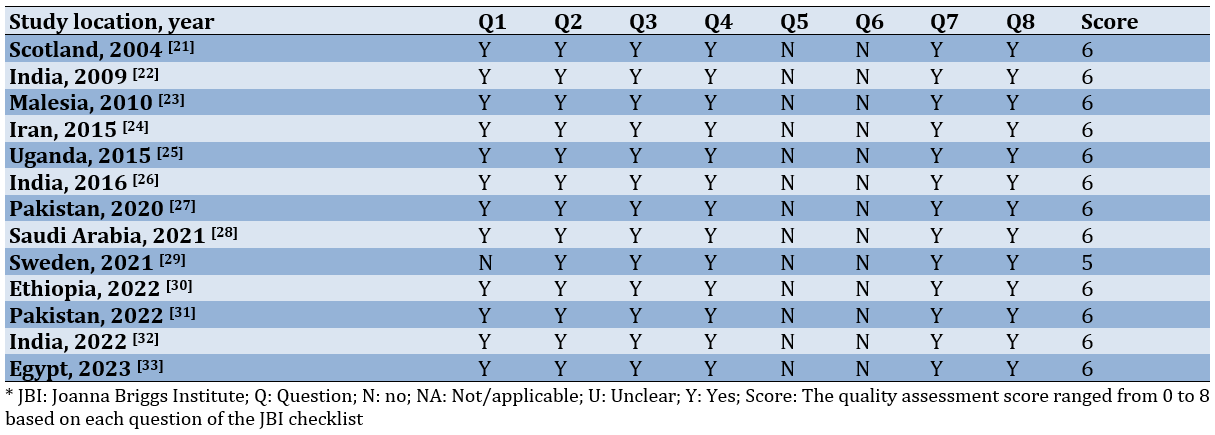
No considerable bias was observed in the studies, and all studies were entered into the systematic review (Table 3).
Table 3. Summary of the quality assessment of articles using the JBI critical appraisal checklist
Characteristics of studies
Out of 13 studies, three (23%) were conducted in India [22, 26, 32], two (15%) in Pakistan [27, 31], and the rest in Scotland, Malesia, Iran, Uganda, Saudi Arabia, Sweden, Ethiopia, and Egypt [21, 23-25, 28-30, 33]. In addition, only one study [29] belonged to a developed country, and 12 were performed in developing nations [21-28, 30-33]. The data were collected by questionnaires in all studies; Two studies had posted their questionnaires [21, 26], three had administered in-person questionnaires [28, 30, 31], one had used online questionnaires [29], and seven had provided no relevant details (Table4 & 5) [22, 25, 27, 32, 33].
Table 4. Summary of characteristics of studies
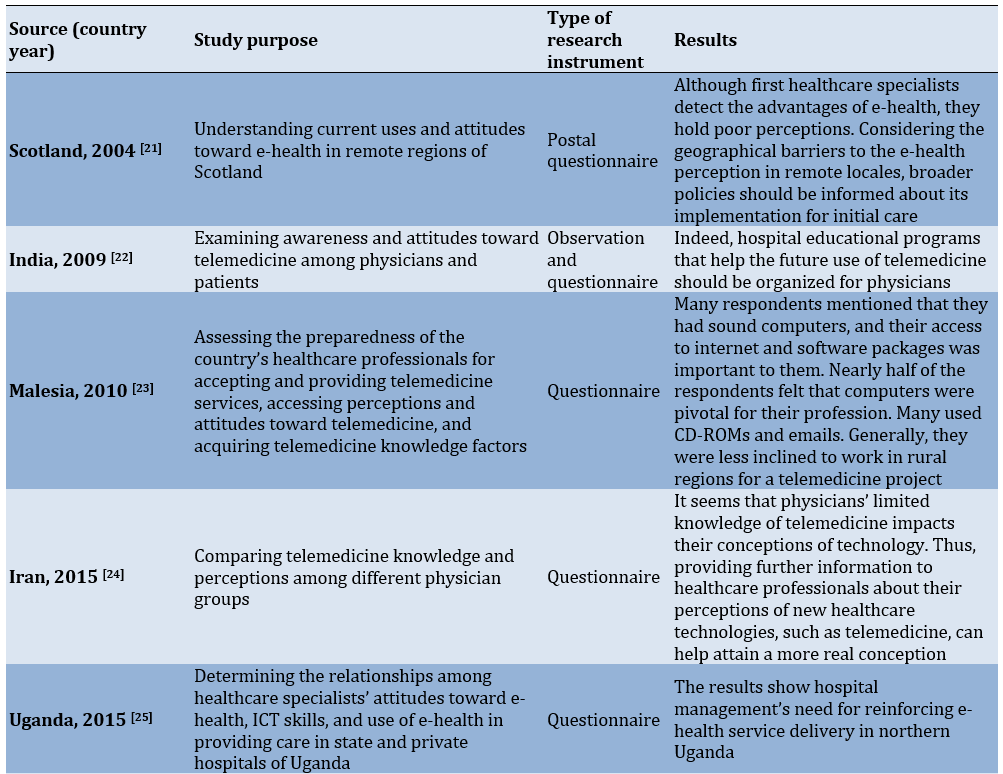

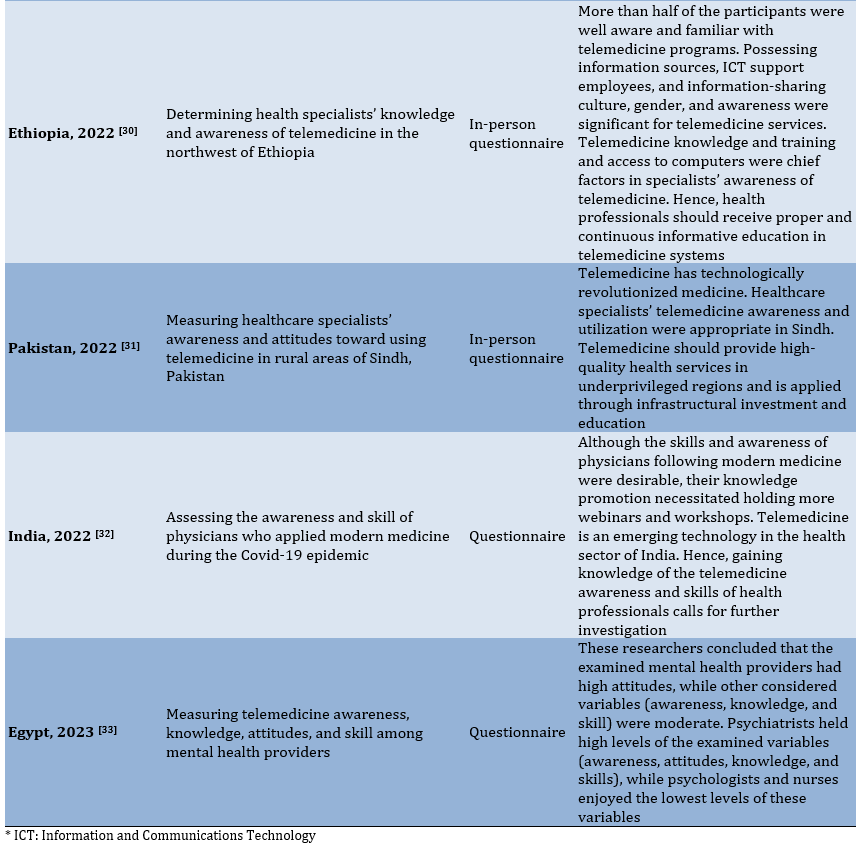
Table 5. Summary of included studies
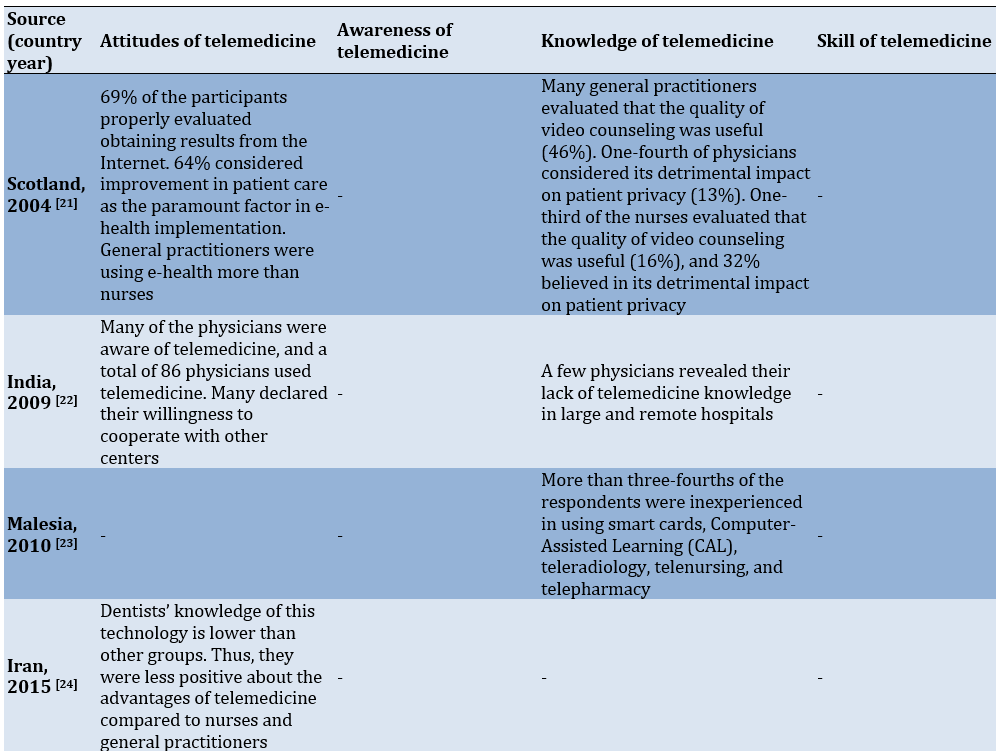
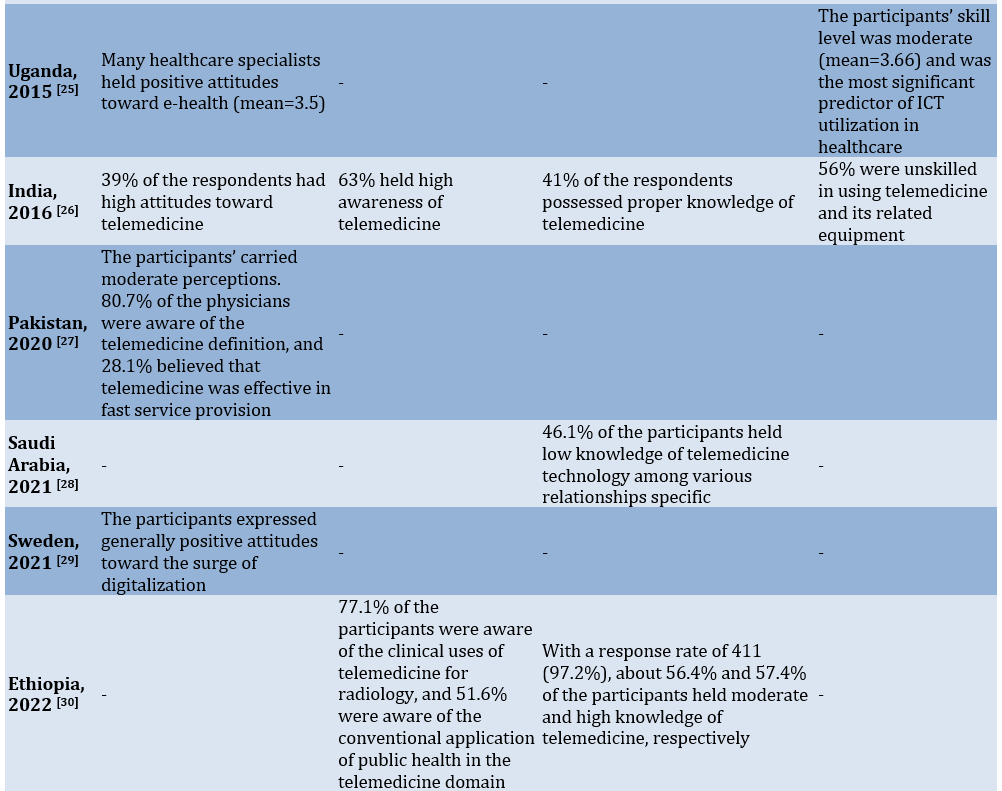
Physicians’ and nurses’ attitudes toward telemedicine
Seven of the studies included in this review evaluated health specialists’ attitudes toward telemedicine, and all revealed the positive and promising attitudes of the examined physicians and health specialists toward telemedicine (Tables 2 & 3) [21, 22, 25, 26, 29, 31, 33].
Richards et al. [21] report that when their participants have been asked to explain their e-health programs, 112 respondents (54%) were familiar with the internet-based informing of laboratory results, 20% were acquainted with video conferences held for education or clinical purposes, and 27% were informed of other applied programs. 68% declare that they have good or excellent experiences and positively evaluate the experiences of easy equipment utilization (74%), equipment performance (75%), clinical utility (76%), technical support (44%), and education (39%). Also, Meher et al. [22] document that many physicians are aware of telemedicine technology, and a total of 86 physicians are using telemedicine. The majority of these 86 physicians express their willingness to cooperate with other centers. In Olok et al.’s [25] study, many healthcare specialists maintain positive attitudes toward e-health properties (Mean=3.5), and the average comparative advantage of ICT, adaptability, testability, and observability is 4.3, 3.8, 3.2, and 3.5, respectively. Zayapragassarazan & Kumar [26] report that many physicians hold high and positive attitudes toward telemedicine. 29% of the respondents possess high altitudes, 31% moderate attitudes, and 30% low attitudes. The maximum and minimum averages associated with attitudes toward telemedicine are obtained for 51-60-year-old (35.61±3.12) and paraclinical respondents (33.21±3.76). Likewise, Glock et al. [29] report that first-care doctors express generally positive attitudes toward digitalization and are almost impatient for it. They assert that enormous sources should be accessed in healthcare and particularly perceived that, along with simplifying physicians’ responsibilities, telemedicine enhances patient empowerment and improves medical care, though some physicians held skeptical attitudes. Furthermore, Kumar et al. [31] show their respondents have agreed that telemedicine can help enhance the interrelationships of healthcare providers (141 individuals), decrease the number of references to health centers (151 individuals), accelerate the accomplishment of tasks (118 individuals), improve clinical decisions (67 individuals), and present more inclusive health services. In addition, Fouad et al. [33] have found high attitudes of mental health providers toward telemedicine and a statistically significant relationship between attitudes toward telemedicine and every one of the following cases: Being heard of telemedicine, willingness to participate in every telemedicine educational program, time spent on individual or collective treatments with telemedicine, time spent on tele-assessment, advantages of telemedicine, reasons for using telemedicine, and telemedicine in specific psychotherapies.
Physicians’ and nurses’ awareness of telemedicine
Among the included studies, all in developing countries, five have evaluated health specialists’ awareness of telemedicine [26, 30, 31, 33]. Only one study addresses nurses and reports their moderate awareness [33]. Three studies document high telemedicine awareness of healthcare specialists [26, 30, 31], and two uncover healthcare specialists’ moderate awareness of telemedicine [32, 33].
In their research, Zayapragassarazan & Kumar [26] show that telemedicine awareness is low for 12%, moderate for 25%, and high for 63% of the respondents. The maximum telemedicine awareness belongs to the 30-40-year age group. Moreover, Kumar et al. [31] Considering the perspectives of 183 participants, express that telemedicine can save time for healthcare specialists and physicians. In contrast, Sukumaran et al. [32] discover moderate telemedicine awareness among the majority of their participants (431 individuals), and 19 physicians maintain poor awareness. In the current COVID-19 scenario, many medical webinars and seminars are held remotely worldwide. A total of 249 participants believe in the training of specific software for telemedicine practices. Almost 262 individuals are concerned with the complaints about arising problems for patients during telemedicine operations. The researchers also have found a weak positive and significant correlation between awareness and skill scores (Pearson correlation=0.20; P<0.0001). Furthermore, Fouad et al. [33] report moderate telemedicine awareness of their participants and show telemedicine awareness maintained statistically significant relationships with being heard of the telemedicine terminology and the spent time. On the other hand, they have found out telemedicine awareness had statistically significant relationships with the benefits of providing mental health services remotely, reasons for using remote mental health services, reasons for not employing telemedicine, and using telemedicine for specific cases. Assaye et al. [30] have discovered that telemedicine awareness is strongly related to knowledge, such that healthcare professionals are aware of telemedicine services. In this respect, 77.1% of the participants are aware of the clinical telemedicine uses for radiology, and 51.6% are aware of the conventional uses of public health in the telemedicine domain. Teaching about telemedicine is strongly associated with awareness of telemedicine services in this study. Those receiving telemedicine training are likely 2.33 times more aware of telemedicine services than untrained ones. Another factor influencing telemedicine awareness was access to computers in hospitals where health specialists worked. Those accessing computers in their hospitals were apparently 1.42 times more aware of telemedicine than those not accessing this technology.
Physicians’ and nurses’ knowledge of telemedicine
Ten examined studies, all in developing countries, evaluated health specialists’ knowledge of telemedicine [21-24, 26-28, 30, 32, 33]. Seven studies reported high and excellent telemedicine knowledge and its application [21-23, 26, 27, 30, 32]. Only one studies investigated nurses and reported their moderate knowledge and sufficient experience in employing telemedicine equipment [25]. Among these studies, one documented moderate knowledge [33], and two found poor telemedicine knowledge of healthcare specialists. In conclusion, they argued that constant education and meetings and conferences held on telemedicine were among the helpful approaches to knowledge enhancement [24, 28].
Richards et al. [21] have reported that many general practitioners consider the effect of counseling on patient privacy useful (44%), and only one-fourth claimed its detrimental impact (13%). 44% hve positively evaluated access to general practitioners, and just one-third hold positive attitudes toward the effect of counseling on patient privacy (16%). 32% consider it harmful, and 21% agree that e-health increases enjoyment. Meher et al. [22] report that the majority of their participants possess high knowledge, while a few lack any knowledge of telemedicine in large and remote hospitals. Ibrahim et al. [23] have found out that many of their respondents employ CD-ROMs (82%), emails (84%), and modems (76%), while more than three-fourths of the respondents are inexperienced in using smart cards, Computer-Assisted Learning (CAL), tele-radiology, tele-surgery, telenursing, and tele-pharmacy. On the other hand, their general awareness of the components are 82% for CAL, 66% for telenursing, 57% for tele-surgery, 55% for tele-radiology, 55% for tele-pharmacy, and 46% for smart cards. Likewise, Zayapragassarazan & Kumar [26] have reported that 41% of the respondents lack proper knowledge, 35% are devoid of fair knowledge, and 24% maintain inadequate knowledge of telemedicine. Assaye et al. [30] discover that 57% of health specialists maintain high knowledge, and 56.4% hold moderate knowledge of telemedicine. Also, 36.7% (151 participants) of the respondents are informed of telephone communications, 28.47% (117 respondents) of online communications, and 15.33% (63) of live communications. Males maintain 1.73 times more knowledge of telemedicine services than females. Hence, health specialists in hospitals with IT support employees are 1.87 times more knowledgeable than their peers in hospitals lacking IT support staff. Another factor affecting health professionals' knowledge of telemedicine services is the culture of information sharing. Health professionals with an information sharing culture were three times more likely than those without an information sharing culture to have a good knowledge of telemedicine services. Information source was another factor associated with telemedicine knowledge. Health specialists using the internet as their source possessed 1.80 times more information than their peers. Besides, telemedicine awareness was strongly related to knowledge, i.e., those specialists who were aware of telemedicine services probably maintained 1.35 times extra knowledge than their unaware counterparts. Kumar et al. [31] assert that a total of 112 participants (52.8%) have worked with telemedicine equipment. The Internet (90, 42.4%) and public media (9, 55.25) were the main sources of telemedicine information. Concerning the tools of the telemedicine era, tele-counseling (120, 56.6%) and teleportation (1, 0.47%) were the most and least known tools. In addition, Ashfaq et al. [27] have found out that many physicians maintained high awareness (80.7) and moderate knowledge of telemedicine. For this reason, a large number (98.2%) have complained about the lack of conferences and meetings on telemedicine in their workplaces, leading to inadequate awareness of telemedicine guidelines. They believe that constant training is necessary for physicians, who should be equipped with the latest telemedicine advancements. On the other hand, physicians’ perceptions of telemedicine support, development, and research are high. A considerable number of specialists had employed telemedicine for telephone counseling with physicians. Doctors found that telemedicine helped reduce transportation and hospitalization costs for patients who could be treated with a monitor while sitting in their homes. However, 42.9% of the physicians averagely believed that telemedicine distorted the doctor-patient relationship, violated patient privacy, or raised costs.
In contrast, Ayatollahi et al. [24] reveal that many physicians’ knowledge of telemedicine technology is considerably low (1.75±0.51). They believe that continuous training in telemedicine utilization would be the most efficient approach to raising their knowledge of telemedicine. Among physicians, pharmacists maintained higher knowledge of telemedicine applications than other doctors and dentists (1.14±0.37). Physicians’ perceptions of the benefits of telemedicine were moderate. The maximum average belonged to the reduction in unnecessary transport costs, and the minimum average was associated with the general familiarity of physicians with telemedicine benefits. Concerning the reduction in unnecessary transport costs, nurses and pharmacists had the highest and lowest means, respectively. Likewise, Albarrak et al. [28] report that 46.1% of the participants hold low knowledge of telemedicine technology among various special relationships. Also, this study shows that 53.1% of the specialists are unfamiliar with telemedicine tools and their medical uses and technology. Interestingly, 69.5% reported that a few conferences, lectures, or meetings were held on telemedicine technology in their workplaces. On the whole, 77.4% of the specialists asserted that constant education was indispensable for telemedicine application (p=0.01).
Physicians’ and nurses’ skill in telemedicine
Among examined studies, three evaluated healthcare specialists’ skills in telemedicine technology in developing countries [25, 26, 32]. Two of these studies reported moderate skills of specialists in telemedicine [25, 32], and one found that healthcare specialists were unskillful in applying telemedicine and its related equipment [26].
Olok et al.’s [25] study reveals that the ICT skill of the respondents is moderate (mean=3.66) and differs in all applied ICT programs and facilities in hospitals. It is also the most significant predictor of ICT application in healthcare. However, the results showed that the skill level for the real use of the ICT tool was slightly better than other cases. Just as this tool was highly used for accessing mobile phones, the mean score of the respondents was also high in using computers and their axillary equipment. Yet, whether these observed differences in the use and real utilization of ICT tools reflect the degree of access to this equipment in physicians’ workplaces in northern Uganda or not is unclear. Sukumaran et al. [32] report that the telemedicine skill of specialists is moderate (68.22%), good (27.85%), and poor (3.92%), and females’ moderate skillfulness (72.39%) is higher than males’ (61.72%). Likewise, the telemedicine skills were significantly different among physicians with various years of experience (0.025), and a larger number of doctors with 5-10 years of experience were poorly skilled compared to others. On the whole, 374 participants knew that the first consultation of patients with registered doctors was called the first counseling, and all knew that medical records should not be sent to the medical council every counseling session. Only 198 respondents knew that the first counseling session was considered for patients consulting with doctors earlier but over six months ago. Only 246 knew that patients had consulted with doctors earlier, but the first counseling was considered for their different health conditions. Generally, 401 participants knew that the next counseling might be in the case of a chronic disease or a treatment, such as re-prescribing or changing drugs when in-person counseling was unnecessary. On the contrary, Zayapragassarazan & Kumar’s [26] study on the telemedicine skills of respondents shows that 19% have been highly skilled or expert, 25% maintained moderate skills, e.g., learners or beginners, and 56% are unskilled in using telemedicine and its associated equipment. The maximum and minimum mean scores for telemedicine skills belonged to paraclinical (25.14±3.58) respondents and the 41-50-years aged group (22.10±4.56), respectively.
Discussion
The present systematic review aimed to synthesize the best research evidence on the telemedicine attitudes, awareness, knowledge, and skills of physicians. In this respect, it identified 13 studies meeting the inclusion criteria. All these studies were cross-sectional and evaluated health specialists’ attitudes, knowledge, awareness, and skills in telemedicine. The results of this investigation revealed that health specialists held positive and promising attitudes toward telemedicine for education, treatment, and care. Furthermore, many studies reported above-moderate and desirable telemedicine awareness, knowledge, and skill among specialists. In this regard, a systematic review of the telemedicine attitudes, awareness, and knowledge of medical students showed that the subjects maintained positive and promising attitudes toward telemedicine technology for education, treatment, and care. However, their knowledge level was low, and many had passed no educational courses. Such results can pave the way for the commitments of policymakers in the health, education, digital health empowerment, and telemedicine literacy domains to medical students as the main players of social health [34].
According to our outcomes, seven cases of the examined studies evaluated specialists’ attitudes toward telemedicine and reported their participants’ positive and promising attitudes [21, 22, 25, 26, 29, 31, 33].
In their recent study in Saudi Arabia, Bashir et al. [35] report the positive attitudes of the participants toward telemedicine and have found out that education and nationality minimally contribute to health specialists’ attitudes toward this technology. They also assert that the proper attitudes of medical specialists toward this technology shape a compulsion enabling telemedicine implementation broadly. In America, Barton et al. [36] argue that urban regions use telehealth more than rural areas (p<0.001), and rural/border patients considerably maintaine lower attitudes than urban patients. Extra video calls by urban providers and telephone calls by rural/border providers highlight the difference between urban and rural areas in telemedicine access and attitudes. Thus, several factors, such as the perceived application facility, perceived utility, and facilitative conditions can enhance the acceptance of the mobile health system. Therefore, it is recommended that these factors be considered in planning to implement these systems [37]. Willingness to apply telemedicine may also be influenced by attitudes toward this technology, attitudes toward the doctor-patient relationship, and the anxiety level of the technology [26].
Hence, it seems that regional differences and the passing of time with diverse problems and limitations did not drastically influence specialists’ attitudes. On the other hand, according to the findings of the present review, there were no observable differences in the results of studies on attitudes in developed and developing countries since both revealed high and positive attitudes. However, since only one examined study was carried out in a developed country, this claim needs further investigation to be proven. Yet, the outnumbering of studies in developing countries (16 cases), compared to developed nations, indicates further attention to telemedicine technology in developing and low-income countries. In this regard, Owolabi et al. [38] examine telemedicine applications and expansion for surgery in low- and moderate-income countries and discover that telemedicine is expanding in less-developed and low-income countries and platforms, such as WhatsApp, WeChat, phone calls, and bilateral messages were used for post-surgery follow-up and education.
On the other hand, according to the physicians employed in high-care hospitals and clinics in Karachi, the current problem in first-world countries in telemedicine operation is physician accreditation, which may cause resistance to telesurgery, while many doctors agreed that the problems in third-world countries were related to the lack of adequate profit, internet connections, and education [27].
Five examined studies evaluated health specialists’ awareness of telemedicine. Three of these studies reported high telemedicine awareness among respondents [26, 30, 31]. A study in Ethiopia documents that specialists’ awareness is significantly associated with computer-related training, technical skills, experiences in supporting patients with ICT tools, and work experiences (p<0.05) [39]. In contrast, two studies reported moderate awareness of telemedicine among their participants. Telemedicine unawareness is one of the causes of physicians’ unwillingness to provide telemedicine services [32, 33]. In their recent research, Purba et al. [40] report moderate telemedicine awareness of nurses in Indonesia (76%). Moderate awareness, self-confidence, and perceived attitudes indicate the need for improving educational programs through training and work experiences. Likewise, telemedicine raises nurses’ knowledge and trust in developing positive attitudes toward the telemedicine concept. An Iranian study reports low awareness of care providers, especially among ICU nurses. The participants cast doubts about the positive or negative impacts of telemedicine but agree on its negative effect on the privacy of patients and caregivers [41]. In another Iranian study, Sheikhtaheri et al. [42] examine clinical employees’ readiness, awareness, and attitudes toward telemedicine and show that awareness is higher in nurses and doctors than in other examined groups. Also, another study reports that health specialists’ awareness of telemedicine is strongly associated with their knowledge, and the use of the internet as an information source increases knowledge 1.8 times more than other sources [30]. The results of this study were in line with the findings of a quest in Bangladesh, where many students used the Internet for health decisions [43].
Ten examined studies evaluated health specialists’ knowledge of telemedicine. Seven of these inquiries reported that healthcare professionals held appropriate and high knowledge of telemedicine applications [21-23, 26, 30, 32], two studies documented moderate knowledge of its participants [27, 33], and one study reported low knowledge [24]. Therefore, the most significant organizational barrier to attracting e-health is the lack of proper perceptions among specialists and, in particular, nurses [21]. This issue can be solved by implementing Continuing Dental Education (CDE) and informing programs that help at different levels [44].
Three examined studies assessed health specialists’ skills in telemedicine and mostly reported moderate telemedicine skills, perhaps due to the participants’ low self-confidence and perceptions. They also revealed that physicians with varying working experiences were significantly different in their telemedicine skills (0.025) [25, 32]. Another study in Lebanon reports that respondents with professional computer skills considerably maintain high awareness (p<0.001). Thus, it is imperative to train and support healthcare employees and initiate programs that provide sufficient and supportive health services to patients in developing countries [1]. Only one study found that the participants’ unskillfulness in applying telemedicine and its related equipment and emphasized the necessity for informing programs, specialist training, and the organization of educational hospital programs facilitating telemedicine use in the future for all physicians [26]. Therefore, the lack of ICT knowledge, unreliable ICT equipment, high ICT cost, the low skill of potential users, limited access to ICT, and unwillingness to employ e-health in healthcare services were reported as the challenges of ICT utilization [25]. Thus, constant informing programs may be significant in improving applied telemedicine programs in healthcare [23].
In addition, many of the included studies suggested holding educational workshops and webinars on telemedicine and informing about its associated equipment and infrastructures to enhance health specialists’ awareness, knowledge, and skills [21, 22, 25, 27, 28, 30-32]. In this regard, Mousavi Baigi et al. [16] and Ftouni et al. [45] examine the challenges of telemedicine during the Covid-19 epidemic and find out that education is one of the challenges of telemedicine application. Therefore, the correct utilization of telemedicine highlights the provision of training to health providers and patients [46].
Conforming to our results, Naqvi et al. [47] have investigated care providers’ knowledge and attitudes toward telemedicine during the Covid-19 epidemic through global surveys from WHO-listed countries and have reported that the respondents possessed positive attitudes toward telemedicine. 80% thought that telemedicine reduced the work volume of employees, and 40.5% believed that telemedicine threatened information confidentiality and patient privacy. Hence, they concluded that an optimistic scope existed for introducing remote working systems worldwide after providing suitable healthcare training [47]. Likewise, Emami Zeydi et al. [48] systematically have reviewed nurses’ awareness and attitudes toward telemedicine and report the positive attitudes of nurses, 56% of whom are desirably aware of this technology. Also, nurses’ awareness and attitudes were significantly and directly associated. Hence, they concluded that one of the paramount components of telemedicine in nurse education was to raise their awareness.
Also, Mousavi Baigi et al. recently have conducted a systematic review with the aim of investigating the attitude, knowledge, and skills of health students in the field of artificial intelligence. The results of their study show that healthcare students have a positive and promising attitude toward artificial intelligence in medicine. However, most students have little knowledge of and limited skills in working with artificial intelligence [49]. Recently, many studies have been conducted in order to investigate the impact of telemedicine, telerehabilitation, and various methods of providing health and medical services based on technology, which proves their effectiveness, safety, and efficiency [50-53]. However, the lack of knowledge and skills of specialists and nurses as the main users of these services hinders significant progress in the health of society in the first place, and from a broader perspective, it hinders progress in the economies of countries. Spending the right amount on health services, especially telemedicine services, which empower patients to self-manage and prevent various diseases, prevents additional expenses later. Therefore, investing in the knowledge, awareness, and skills of students and healthcare professionals can be a powerful approach for further development [34, 49, 54-58].
In sum, the findings of this study indicated that health specialists maintained positive and promising attitudes and above-moderate awareness, knowledge, and skills, while many of the included studies asked for passing related courses on telemedicine. Thus, we suggest providing educational fundamentals, workshops, and classes about telemedicine, informing through media campaigns, and encouraging the treatment cadre to raise awareness.
Strengths and limitations
Among the limitations of this study, we can refer to the studies published in languages other than English and thus ignored in this review. Also, the differences in the specialty of the participants, the publication year of the studies, and the examined context, culture, and gender, as well as the degree of access to IT specialists in various places, may lead to bias in the results. Furthermore, the included studies employed various questionnaires with different items. Thus, one study might have questioned primary telemedicine knowledge and skills, e.g., working with emails and WhatsApp, and another interrogated the knowledge and skill in working with intricate telemedicine tools, such as artificial intelligence, working with robot surgeons, etc., and reported low knowledge of the participants. Thus, future studies are suggested to examine and assess an international survey with a standard and identical questionnaire to confirm the evidence of this systematic review. However, this research was the first systematic review evaluating the telemedicine attitudes, awareness, knowledge, and skills of health specialists that were the key players in the health system of countries and provided valuable perspectives to policymakers and planners.
Conclusion
Health specialists held positive and promising attitudes toward telemedicine. Telemedicine awareness, knowledge, and skill among health professionals is above-moderate and desirable.
Acknowledgments: We would like to thank all of the participants in this research as well as the Mashhad University of Medical Sciences Student Research Committee for their assistance.
Ethical Permissions: This study was approved by the Ethical Committee of Mashhad University of Medical Sciences (approval number: IR.MUMS.REC.1401.196).
Conflicts of Interests: The authors have declared that they have no conflicts of interest.
Authors' Contribution: Dahmardeh Kemmak F (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (30%); Sarbaz M (Second Author), Introduction Writer/Methodologist/Main Researcher (10%); Mousavi Baigi SF (Third Author), Methodologist/Statistical Analyst (10%); Marouzi P (Fourth Author), Introduction Writer/Statistical Analyst (10%); Sheykhotayefeh M (Fifth Author), Methodologist/Main or Assistant Researcher (10%); Kimiafar Kh (Sixth Author), Methodologist/Discussion Writer/Statistical Analyst (30%)
Funding/Support: The authors did not receive support from any organization for this research.
Telemedicine is defined as using web-based sources and electronic information together with advanced digital network technology to promote remote professional health services, publish medical safety reports, present health-related training to people, and monitor public health [1]. Indeed, telemedicine is a branch of medicine that uses electronic media to build relationships among healthcare employees, including physicians, nurses, healthcare providers, and patients. As a vital factor for health specialists, telemedicine facilitates the exchange of information for the diagnosis, treatment, and prevention of diseases and traumas, as well as assessment, research, and healthcare providers’ training, improving individual and social health [2]. Today, telemedicine, employed by numerous medical specialists, such as cardiologists, neurologists, surgeons, optometrists, radiologists, and pediatricians is recognized as an approach to improving care access, quality, and efficiency [3]. In addition, telemedicine shortens patients’ hospitalization time, reduces the number of visits and care-associated costs, improves healthcare access, decreases care traveling time and cost, and enhances patient satisfaction [4, 5]. Many care professionals prefer to work in metropolises, and this issue results in the shortage of healthcare services in rural and underprivileged regions. In the meantime, telemedicine can be a promising solution for many of these drawbacks by eliminating the barriers of physical distance [6]. On the other hand, the World Health Organization (WHO) recommends introducing telemedicine in locales with high patient demands [7]. Despite numerous likely barriers, such as the inability to examine physically, and limited access to sensitive communities with low literacy, like villagers, ethnic minorities, elderly patients, and poor socioeconomic communities, telemedicine is counted as a helpful tool for physicians and patient care [6]. Telemedicine is historically used to provide healthcare to rural populations to manage chronic diseases, psychological and medical conditions, and real-time visits in acute care settings and facilitates video counseling and the use of mobile apps to provide medical consultation, diagnosis, and treatment and reduce the risk of infection. On the whole, many physicians believe that telemedicine is extensively promising for the management of patient care [8, 9].
Although the present advantages of telemedicine have been proved, the health domain has been slow to adopt Information and Communication Technology (ICT) compared to other sectors [10]. There are many reasons why the implementation of e-health systems is still challenging despite the existing studies on its clinical benefits, efficient cost, and high healthcare accessibility at macro levels [11-13]. Regardless of the merits and potential technical superiority of telemedicine, its acceptance is often considered a failed project [14], and user non-acceptance is one of the pivotal causes of failure in this respect [15]. In other words, to ensure telemedicine acceptance and use, it is necessary to possess gross resource capital and human forces and attempt to recognize its utility [4]. On the other hand, since the success of every novel technology depends on many factors, such as the respective professionals’ knowledge and perceptions of the concept, acquired skills, and working environments [16], health specialists’ attitudes, awareness, knowledge, and skill in telemedicine are among the imperatives of the successful implementation of telemedicine [17].
Despite the increasing contribution of telemedicine to healthcare and studies on physicians’ and nurses’ attitudes toward telemedicine, a few systematic reviews have synthesized the best evidence and provided a general view in this domain, and neither has so far examined physicians’ and nurses’ attitudes, awareness, knowledge, and skill as health professionals. Hence, the present systematic review investigated physicians’ and nurses’ attitudes, knowledge, awareness, and skills in telemedicine.
Information and Methods
Design
This systematic review followed PRISMA guidelines to report evidence from included studies [18, 19]. In this respect, the researchers searched some keywords in titles, abstracts, and the PubMed, Embase, Scopus, and Web of Sciences databases on March, 2023, and employed the MeSH and Emtree keywords and terms in the three below categories to search the databases.
1. Physicians OR Physician OR Doctors OR Doctor OR Nurses OR Nurse OR "Personnel, nursing" OR "Nursing personnel" OR "Registered nurses" OR "Nurse, registered" OR "Nurses, registered" OR "Registered nurse".
2. Attitude OR Attitudes OR Knowledge OR Awareness OR Awarenesses OR Skill OR Skills.
3. "Telemedicine" OR "Telerehabilitation" OR "telehealth" OR "Mobile Health" OR "Health, Mobile" OR "Virtual Medicine" OR "Medicine, Virtual" OR "eHealth" OR "mHealth" (Table 1).
Table 1. Search strategy for each database

Eligibility criteria
Studies that possessed the following inclusion criteria were entered into the examination process:
1) Cross-sectional studies investigating physicians’ and nurses’ attitudes, awareness, knowledge, and skill in telemedicine;
2) Studies examining physician and nurse populations.
On the other hand, the exclusion criteria were:
1) Publication types other than papers of high-prestigious journals, such as books, review papers, and letters to editors-in-chief;
2) Not accessing the full text of the paper in English;
3) Irrelevance of the title, abstract, or full text to the purpose of the study.
Data extraction and synthesis
After the extraction of studies from the databases, repeated studies were removed. First, titles and abstracts were screened independently based on the eligibility criteria. Papers lacking the inclusion criteria were omitted from the investigation. Then, the full texts were retrieved and screened independently by two researchers based on the eligibility criteria. The inter-researcher conflicts were solved through discussions. A similar checklist was used for data extraction. The data items in this checklist included the reference, examined country, publishing year, applied instruments, study purposes, telemedicine attitudes, telemedicine knowledge, telemedicine awareness, telemedicine skills, and main findings.
Quality assessment
Joanna Briggs Institute’s (JBI) critical appraisal checklist specific to cross-sectional studies was used for the quality assessment of the included studies [20]. In particular, with eight questions for assessing the quality of studies, this checklist involves the following issues: The inclusion criteria of samples, examined population, examined setting, and valid and reliable measurement instruments (mentioning the validity and reliability of the questionnaires). The included studies used standard measurement criteria, identified confounding factors, pursued strategies to cope with confounding factors, reported valid results, and followed appropriate statistical analyses. The responses to the questions included four yes, no, unclear, and not applicable categories. Positively and negatively answered questions received scores of 1 and 0, respectively, and the maximum quality score of every study was 8. If the quality score of a study was <5, it was omitted from the review.
Findings
Selection of studies
The search into scientific databases led to the retrieval of a total of 9398 studies initially. After the omission of repetitive cases (2873), 6525 studies remained for the title and abstract examination. 6494 studies not aligning with the purpose of the study were removed. Then, 31 remaining papers were examined with their full texts, and finally, 13 eligible papers were entered into the study (Table 2; Figure 1).
Table2. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist
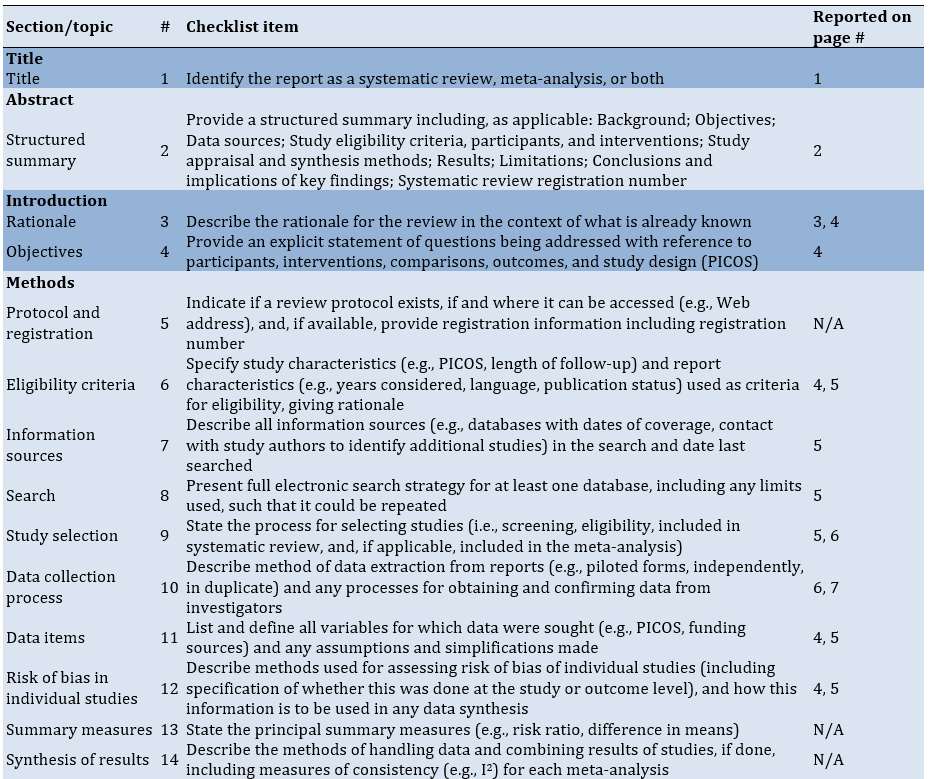
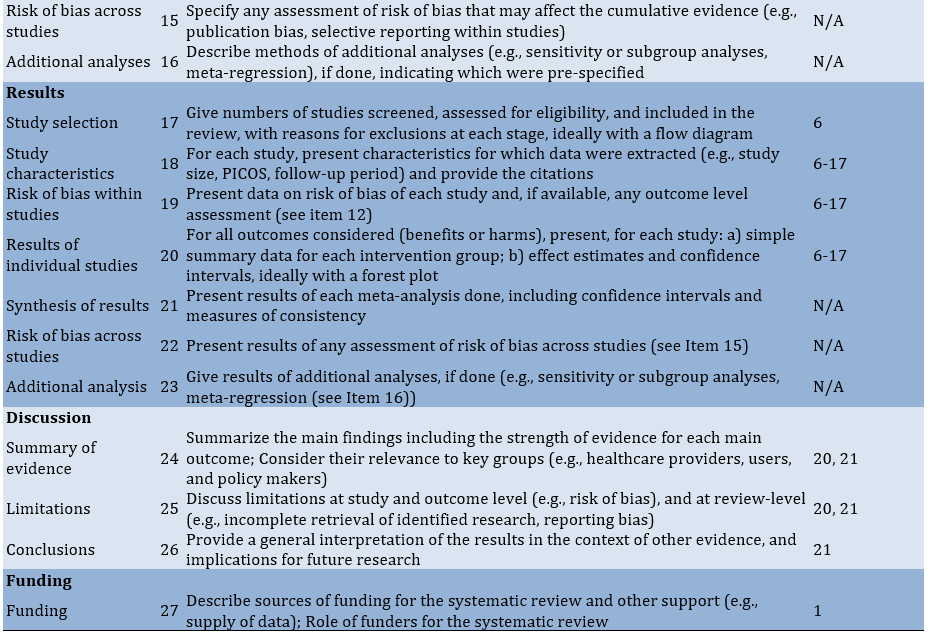
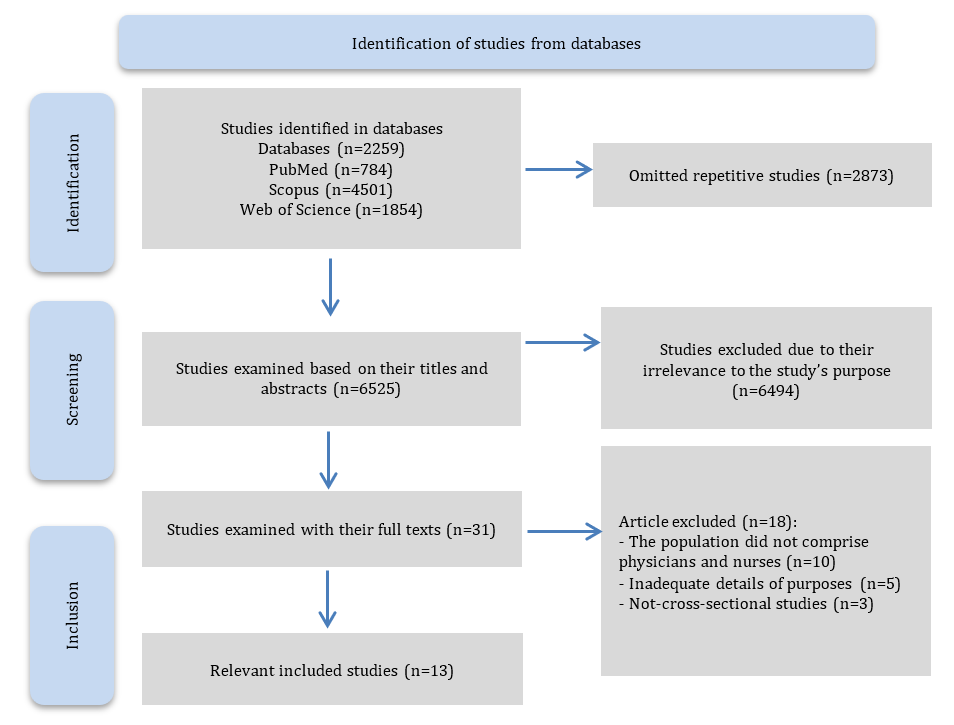
Figure 1. Study selection PRISMA
Quality assessment
No considerable bias was observed in the studies, and all studies were entered into the systematic review (Table 3).
Table 3. Summary of the quality assessment of articles using the JBI critical appraisal checklist
Characteristics of studies
Out of 13 studies, three (23%) were conducted in India [22, 26, 32], two (15%) in Pakistan [27, 31], and the rest in Scotland, Malesia, Iran, Uganda, Saudi Arabia, Sweden, Ethiopia, and Egypt [21, 23-25, 28-30, 33]. In addition, only one study [29] belonged to a developed country, and 12 were performed in developing nations [21-28, 30-33]. The data were collected by questionnaires in all studies; Two studies had posted their questionnaires [21, 26], three had administered in-person questionnaires [28, 30, 31], one had used online questionnaires [29], and seven had provided no relevant details (Table4 & 5) [22, 25, 27, 32, 33].
Table 4. Summary of characteristics of studies
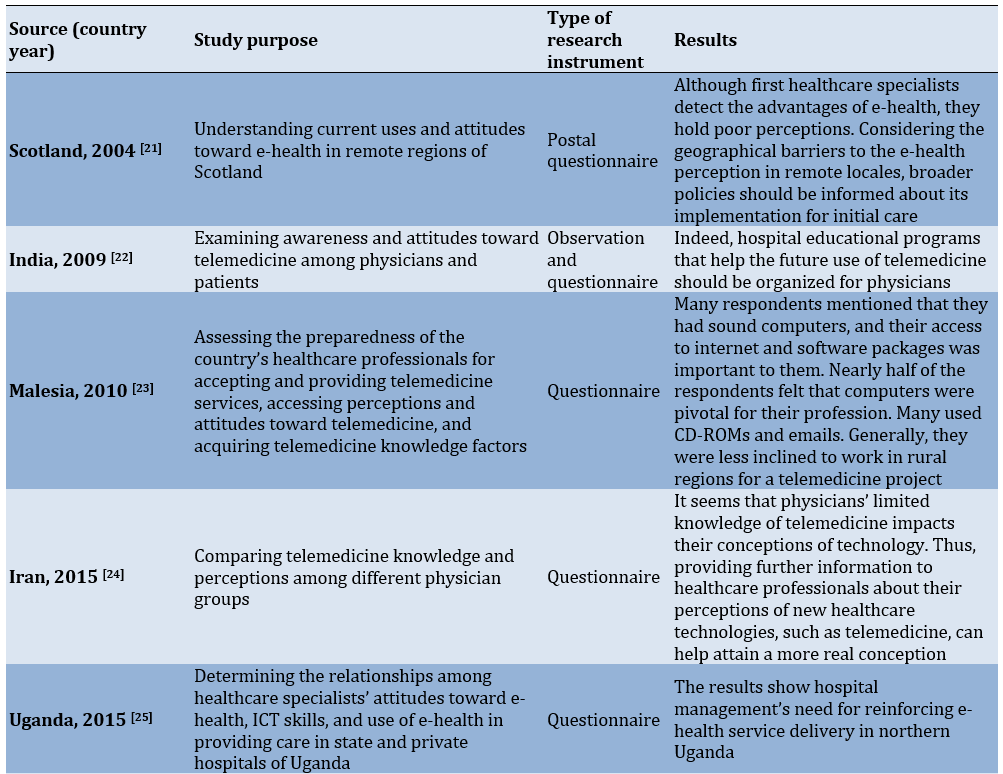

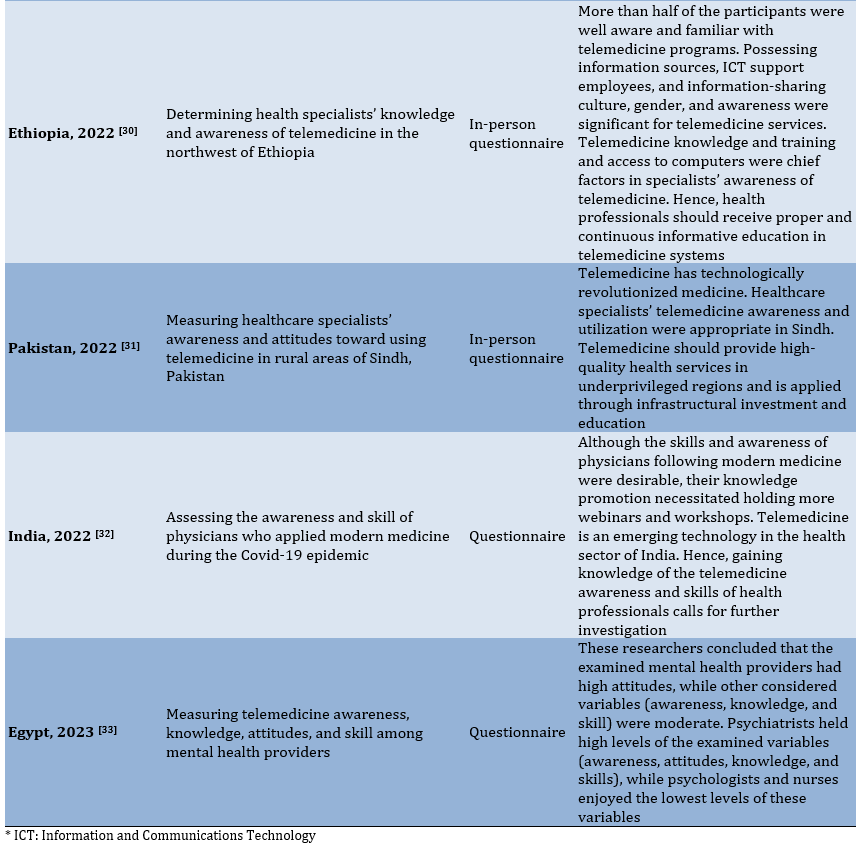
Table 5. Summary of included studies
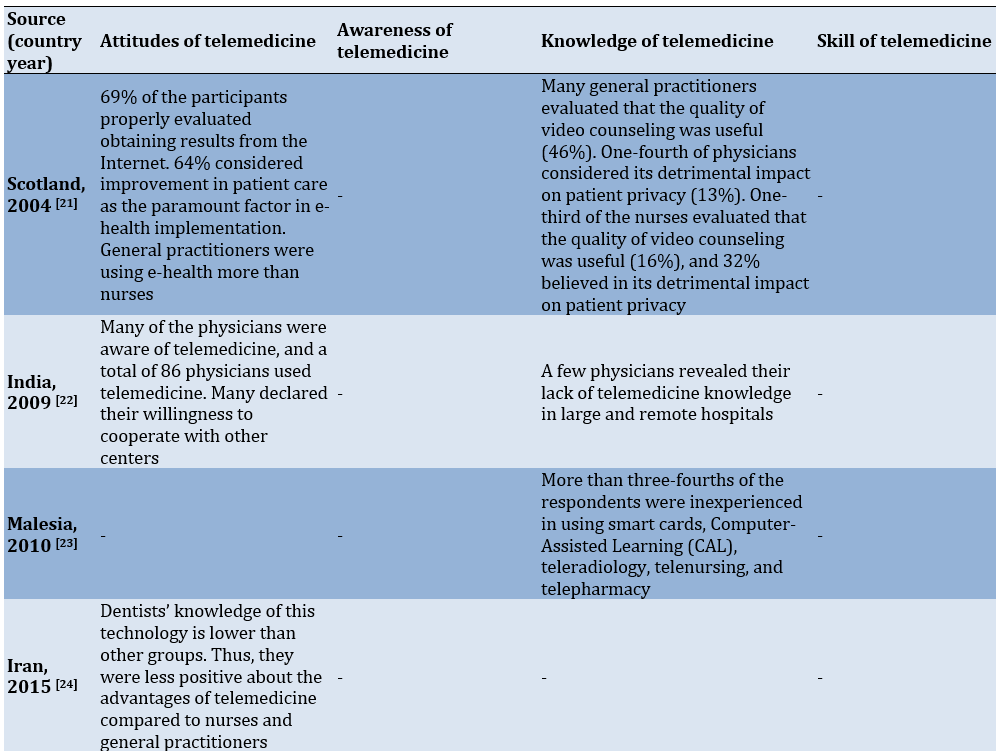
Physicians’ and nurses’ attitudes toward telemedicine
Seven of the studies included in this review evaluated health specialists’ attitudes toward telemedicine, and all revealed the positive and promising attitudes of the examined physicians and health specialists toward telemedicine (Tables 2 & 3) [21, 22, 25, 26, 29, 31, 33].
Richards et al. [21] report that when their participants have been asked to explain their e-health programs, 112 respondents (54%) were familiar with the internet-based informing of laboratory results, 20% were acquainted with video conferences held for education or clinical purposes, and 27% were informed of other applied programs. 68% declare that they have good or excellent experiences and positively evaluate the experiences of easy equipment utilization (74%), equipment performance (75%), clinical utility (76%), technical support (44%), and education (39%). Also, Meher et al. [22] document that many physicians are aware of telemedicine technology, and a total of 86 physicians are using telemedicine. The majority of these 86 physicians express their willingness to cooperate with other centers. In Olok et al.’s [25] study, many healthcare specialists maintain positive attitudes toward e-health properties (Mean=3.5), and the average comparative advantage of ICT, adaptability, testability, and observability is 4.3, 3.8, 3.2, and 3.5, respectively. Zayapragassarazan & Kumar [26] report that many physicians hold high and positive attitudes toward telemedicine. 29% of the respondents possess high altitudes, 31% moderate attitudes, and 30% low attitudes. The maximum and minimum averages associated with attitudes toward telemedicine are obtained for 51-60-year-old (35.61±3.12) and paraclinical respondents (33.21±3.76). Likewise, Glock et al. [29] report that first-care doctors express generally positive attitudes toward digitalization and are almost impatient for it. They assert that enormous sources should be accessed in healthcare and particularly perceived that, along with simplifying physicians’ responsibilities, telemedicine enhances patient empowerment and improves medical care, though some physicians held skeptical attitudes. Furthermore, Kumar et al. [31] show their respondents have agreed that telemedicine can help enhance the interrelationships of healthcare providers (141 individuals), decrease the number of references to health centers (151 individuals), accelerate the accomplishment of tasks (118 individuals), improve clinical decisions (67 individuals), and present more inclusive health services. In addition, Fouad et al. [33] have found high attitudes of mental health providers toward telemedicine and a statistically significant relationship between attitudes toward telemedicine and every one of the following cases: Being heard of telemedicine, willingness to participate in every telemedicine educational program, time spent on individual or collective treatments with telemedicine, time spent on tele-assessment, advantages of telemedicine, reasons for using telemedicine, and telemedicine in specific psychotherapies.
Physicians’ and nurses’ awareness of telemedicine
Among the included studies, all in developing countries, five have evaluated health specialists’ awareness of telemedicine [26, 30, 31, 33]. Only one study addresses nurses and reports their moderate awareness [33]. Three studies document high telemedicine awareness of healthcare specialists [26, 30, 31], and two uncover healthcare specialists’ moderate awareness of telemedicine [32, 33].
In their research, Zayapragassarazan & Kumar [26] show that telemedicine awareness is low for 12%, moderate for 25%, and high for 63% of the respondents. The maximum telemedicine awareness belongs to the 30-40-year age group. Moreover, Kumar et al. [31] Considering the perspectives of 183 participants, express that telemedicine can save time for healthcare specialists and physicians. In contrast, Sukumaran et al. [32] discover moderate telemedicine awareness among the majority of their participants (431 individuals), and 19 physicians maintain poor awareness. In the current COVID-19 scenario, many medical webinars and seminars are held remotely worldwide. A total of 249 participants believe in the training of specific software for telemedicine practices. Almost 262 individuals are concerned with the complaints about arising problems for patients during telemedicine operations. The researchers also have found a weak positive and significant correlation between awareness and skill scores (Pearson correlation=0.20; P<0.0001). Furthermore, Fouad et al. [33] report moderate telemedicine awareness of their participants and show telemedicine awareness maintained statistically significant relationships with being heard of the telemedicine terminology and the spent time. On the other hand, they have found out telemedicine awareness had statistically significant relationships with the benefits of providing mental health services remotely, reasons for using remote mental health services, reasons for not employing telemedicine, and using telemedicine for specific cases. Assaye et al. [30] have discovered that telemedicine awareness is strongly related to knowledge, such that healthcare professionals are aware of telemedicine services. In this respect, 77.1% of the participants are aware of the clinical telemedicine uses for radiology, and 51.6% are aware of the conventional uses of public health in the telemedicine domain. Teaching about telemedicine is strongly associated with awareness of telemedicine services in this study. Those receiving telemedicine training are likely 2.33 times more aware of telemedicine services than untrained ones. Another factor influencing telemedicine awareness was access to computers in hospitals where health specialists worked. Those accessing computers in their hospitals were apparently 1.42 times more aware of telemedicine than those not accessing this technology.
Physicians’ and nurses’ knowledge of telemedicine
Ten examined studies, all in developing countries, evaluated health specialists’ knowledge of telemedicine [21-24, 26-28, 30, 32, 33]. Seven studies reported high and excellent telemedicine knowledge and its application [21-23, 26, 27, 30, 32]. Only one studies investigated nurses and reported their moderate knowledge and sufficient experience in employing telemedicine equipment [25]. Among these studies, one documented moderate knowledge [33], and two found poor telemedicine knowledge of healthcare specialists. In conclusion, they argued that constant education and meetings and conferences held on telemedicine were among the helpful approaches to knowledge enhancement [24, 28].
Richards et al. [21] have reported that many general practitioners consider the effect of counseling on patient privacy useful (44%), and only one-fourth claimed its detrimental impact (13%). 44% hve positively evaluated access to general practitioners, and just one-third hold positive attitudes toward the effect of counseling on patient privacy (16%). 32% consider it harmful, and 21% agree that e-health increases enjoyment. Meher et al. [22] report that the majority of their participants possess high knowledge, while a few lack any knowledge of telemedicine in large and remote hospitals. Ibrahim et al. [23] have found out that many of their respondents employ CD-ROMs (82%), emails (84%), and modems (76%), while more than three-fourths of the respondents are inexperienced in using smart cards, Computer-Assisted Learning (CAL), tele-radiology, tele-surgery, telenursing, and tele-pharmacy. On the other hand, their general awareness of the components are 82% for CAL, 66% for telenursing, 57% for tele-surgery, 55% for tele-radiology, 55% for tele-pharmacy, and 46% for smart cards. Likewise, Zayapragassarazan & Kumar [26] have reported that 41% of the respondents lack proper knowledge, 35% are devoid of fair knowledge, and 24% maintain inadequate knowledge of telemedicine. Assaye et al. [30] discover that 57% of health specialists maintain high knowledge, and 56.4% hold moderate knowledge of telemedicine. Also, 36.7% (151 participants) of the respondents are informed of telephone communications, 28.47% (117 respondents) of online communications, and 15.33% (63) of live communications. Males maintain 1.73 times more knowledge of telemedicine services than females. Hence, health specialists in hospitals with IT support employees are 1.87 times more knowledgeable than their peers in hospitals lacking IT support staff. Another factor affecting health professionals' knowledge of telemedicine services is the culture of information sharing. Health professionals with an information sharing culture were three times more likely than those without an information sharing culture to have a good knowledge of telemedicine services. Information source was another factor associated with telemedicine knowledge. Health specialists using the internet as their source possessed 1.80 times more information than their peers. Besides, telemedicine awareness was strongly related to knowledge, i.e., those specialists who were aware of telemedicine services probably maintained 1.35 times extra knowledge than their unaware counterparts. Kumar et al. [31] assert that a total of 112 participants (52.8%) have worked with telemedicine equipment. The Internet (90, 42.4%) and public media (9, 55.25) were the main sources of telemedicine information. Concerning the tools of the telemedicine era, tele-counseling (120, 56.6%) and teleportation (1, 0.47%) were the most and least known tools. In addition, Ashfaq et al. [27] have found out that many physicians maintained high awareness (80.7) and moderate knowledge of telemedicine. For this reason, a large number (98.2%) have complained about the lack of conferences and meetings on telemedicine in their workplaces, leading to inadequate awareness of telemedicine guidelines. They believe that constant training is necessary for physicians, who should be equipped with the latest telemedicine advancements. On the other hand, physicians’ perceptions of telemedicine support, development, and research are high. A considerable number of specialists had employed telemedicine for telephone counseling with physicians. Doctors found that telemedicine helped reduce transportation and hospitalization costs for patients who could be treated with a monitor while sitting in their homes. However, 42.9% of the physicians averagely believed that telemedicine distorted the doctor-patient relationship, violated patient privacy, or raised costs.
In contrast, Ayatollahi et al. [24] reveal that many physicians’ knowledge of telemedicine technology is considerably low (1.75±0.51). They believe that continuous training in telemedicine utilization would be the most efficient approach to raising their knowledge of telemedicine. Among physicians, pharmacists maintained higher knowledge of telemedicine applications than other doctors and dentists (1.14±0.37). Physicians’ perceptions of the benefits of telemedicine were moderate. The maximum average belonged to the reduction in unnecessary transport costs, and the minimum average was associated with the general familiarity of physicians with telemedicine benefits. Concerning the reduction in unnecessary transport costs, nurses and pharmacists had the highest and lowest means, respectively. Likewise, Albarrak et al. [28] report that 46.1% of the participants hold low knowledge of telemedicine technology among various special relationships. Also, this study shows that 53.1% of the specialists are unfamiliar with telemedicine tools and their medical uses and technology. Interestingly, 69.5% reported that a few conferences, lectures, or meetings were held on telemedicine technology in their workplaces. On the whole, 77.4% of the specialists asserted that constant education was indispensable for telemedicine application (p=0.01).
Physicians’ and nurses’ skill in telemedicine
Among examined studies, three evaluated healthcare specialists’ skills in telemedicine technology in developing countries [25, 26, 32]. Two of these studies reported moderate skills of specialists in telemedicine [25, 32], and one found that healthcare specialists were unskillful in applying telemedicine and its related equipment [26].
Olok et al.’s [25] study reveals that the ICT skill of the respondents is moderate (mean=3.66) and differs in all applied ICT programs and facilities in hospitals. It is also the most significant predictor of ICT application in healthcare. However, the results showed that the skill level for the real use of the ICT tool was slightly better than other cases. Just as this tool was highly used for accessing mobile phones, the mean score of the respondents was also high in using computers and their axillary equipment. Yet, whether these observed differences in the use and real utilization of ICT tools reflect the degree of access to this equipment in physicians’ workplaces in northern Uganda or not is unclear. Sukumaran et al. [32] report that the telemedicine skill of specialists is moderate (68.22%), good (27.85%), and poor (3.92%), and females’ moderate skillfulness (72.39%) is higher than males’ (61.72%). Likewise, the telemedicine skills were significantly different among physicians with various years of experience (0.025), and a larger number of doctors with 5-10 years of experience were poorly skilled compared to others. On the whole, 374 participants knew that the first consultation of patients with registered doctors was called the first counseling, and all knew that medical records should not be sent to the medical council every counseling session. Only 198 respondents knew that the first counseling session was considered for patients consulting with doctors earlier but over six months ago. Only 246 knew that patients had consulted with doctors earlier, but the first counseling was considered for their different health conditions. Generally, 401 participants knew that the next counseling might be in the case of a chronic disease or a treatment, such as re-prescribing or changing drugs when in-person counseling was unnecessary. On the contrary, Zayapragassarazan & Kumar’s [26] study on the telemedicine skills of respondents shows that 19% have been highly skilled or expert, 25% maintained moderate skills, e.g., learners or beginners, and 56% are unskilled in using telemedicine and its associated equipment. The maximum and minimum mean scores for telemedicine skills belonged to paraclinical (25.14±3.58) respondents and the 41-50-years aged group (22.10±4.56), respectively.
Discussion
The present systematic review aimed to synthesize the best research evidence on the telemedicine attitudes, awareness, knowledge, and skills of physicians. In this respect, it identified 13 studies meeting the inclusion criteria. All these studies were cross-sectional and evaluated health specialists’ attitudes, knowledge, awareness, and skills in telemedicine. The results of this investigation revealed that health specialists held positive and promising attitudes toward telemedicine for education, treatment, and care. Furthermore, many studies reported above-moderate and desirable telemedicine awareness, knowledge, and skill among specialists. In this regard, a systematic review of the telemedicine attitudes, awareness, and knowledge of medical students showed that the subjects maintained positive and promising attitudes toward telemedicine technology for education, treatment, and care. However, their knowledge level was low, and many had passed no educational courses. Such results can pave the way for the commitments of policymakers in the health, education, digital health empowerment, and telemedicine literacy domains to medical students as the main players of social health [34].
According to our outcomes, seven cases of the examined studies evaluated specialists’ attitudes toward telemedicine and reported their participants’ positive and promising attitudes [21, 22, 25, 26, 29, 31, 33].
In their recent study in Saudi Arabia, Bashir et al. [35] report the positive attitudes of the participants toward telemedicine and have found out that education and nationality minimally contribute to health specialists’ attitudes toward this technology. They also assert that the proper attitudes of medical specialists toward this technology shape a compulsion enabling telemedicine implementation broadly. In America, Barton et al. [36] argue that urban regions use telehealth more than rural areas (p<0.001), and rural/border patients considerably maintaine lower attitudes than urban patients. Extra video calls by urban providers and telephone calls by rural/border providers highlight the difference between urban and rural areas in telemedicine access and attitudes. Thus, several factors, such as the perceived application facility, perceived utility, and facilitative conditions can enhance the acceptance of the mobile health system. Therefore, it is recommended that these factors be considered in planning to implement these systems [37]. Willingness to apply telemedicine may also be influenced by attitudes toward this technology, attitudes toward the doctor-patient relationship, and the anxiety level of the technology [26].
Hence, it seems that regional differences and the passing of time with diverse problems and limitations did not drastically influence specialists’ attitudes. On the other hand, according to the findings of the present review, there were no observable differences in the results of studies on attitudes in developed and developing countries since both revealed high and positive attitudes. However, since only one examined study was carried out in a developed country, this claim needs further investigation to be proven. Yet, the outnumbering of studies in developing countries (16 cases), compared to developed nations, indicates further attention to telemedicine technology in developing and low-income countries. In this regard, Owolabi et al. [38] examine telemedicine applications and expansion for surgery in low- and moderate-income countries and discover that telemedicine is expanding in less-developed and low-income countries and platforms, such as WhatsApp, WeChat, phone calls, and bilateral messages were used for post-surgery follow-up and education.
On the other hand, according to the physicians employed in high-care hospitals and clinics in Karachi, the current problem in first-world countries in telemedicine operation is physician accreditation, which may cause resistance to telesurgery, while many doctors agreed that the problems in third-world countries were related to the lack of adequate profit, internet connections, and education [27].
Five examined studies evaluated health specialists’ awareness of telemedicine. Three of these studies reported high telemedicine awareness among respondents [26, 30, 31]. A study in Ethiopia documents that specialists’ awareness is significantly associated with computer-related training, technical skills, experiences in supporting patients with ICT tools, and work experiences (p<0.05) [39]. In contrast, two studies reported moderate awareness of telemedicine among their participants. Telemedicine unawareness is one of the causes of physicians’ unwillingness to provide telemedicine services [32, 33]. In their recent research, Purba et al. [40] report moderate telemedicine awareness of nurses in Indonesia (76%). Moderate awareness, self-confidence, and perceived attitudes indicate the need for improving educational programs through training and work experiences. Likewise, telemedicine raises nurses’ knowledge and trust in developing positive attitudes toward the telemedicine concept. An Iranian study reports low awareness of care providers, especially among ICU nurses. The participants cast doubts about the positive or negative impacts of telemedicine but agree on its negative effect on the privacy of patients and caregivers [41]. In another Iranian study, Sheikhtaheri et al. [42] examine clinical employees’ readiness, awareness, and attitudes toward telemedicine and show that awareness is higher in nurses and doctors than in other examined groups. Also, another study reports that health specialists’ awareness of telemedicine is strongly associated with their knowledge, and the use of the internet as an information source increases knowledge 1.8 times more than other sources [30]. The results of this study were in line with the findings of a quest in Bangladesh, where many students used the Internet for health decisions [43].
Ten examined studies evaluated health specialists’ knowledge of telemedicine. Seven of these inquiries reported that healthcare professionals held appropriate and high knowledge of telemedicine applications [21-23, 26, 30, 32], two studies documented moderate knowledge of its participants [27, 33], and one study reported low knowledge [24]. Therefore, the most significant organizational barrier to attracting e-health is the lack of proper perceptions among specialists and, in particular, nurses [21]. This issue can be solved by implementing Continuing Dental Education (CDE) and informing programs that help at different levels [44].
Three examined studies assessed health specialists’ skills in telemedicine and mostly reported moderate telemedicine skills, perhaps due to the participants’ low self-confidence and perceptions. They also revealed that physicians with varying working experiences were significantly different in their telemedicine skills (0.025) [25, 32]. Another study in Lebanon reports that respondents with professional computer skills considerably maintain high awareness (p<0.001). Thus, it is imperative to train and support healthcare employees and initiate programs that provide sufficient and supportive health services to patients in developing countries [1]. Only one study found that the participants’ unskillfulness in applying telemedicine and its related equipment and emphasized the necessity for informing programs, specialist training, and the organization of educational hospital programs facilitating telemedicine use in the future for all physicians [26]. Therefore, the lack of ICT knowledge, unreliable ICT equipment, high ICT cost, the low skill of potential users, limited access to ICT, and unwillingness to employ e-health in healthcare services were reported as the challenges of ICT utilization [25]. Thus, constant informing programs may be significant in improving applied telemedicine programs in healthcare [23].
In addition, many of the included studies suggested holding educational workshops and webinars on telemedicine and informing about its associated equipment and infrastructures to enhance health specialists’ awareness, knowledge, and skills [21, 22, 25, 27, 28, 30-32]. In this regard, Mousavi Baigi et al. [16] and Ftouni et al. [45] examine the challenges of telemedicine during the Covid-19 epidemic and find out that education is one of the challenges of telemedicine application. Therefore, the correct utilization of telemedicine highlights the provision of training to health providers and patients [46].
Conforming to our results, Naqvi et al. [47] have investigated care providers’ knowledge and attitudes toward telemedicine during the Covid-19 epidemic through global surveys from WHO-listed countries and have reported that the respondents possessed positive attitudes toward telemedicine. 80% thought that telemedicine reduced the work volume of employees, and 40.5% believed that telemedicine threatened information confidentiality and patient privacy. Hence, they concluded that an optimistic scope existed for introducing remote working systems worldwide after providing suitable healthcare training [47]. Likewise, Emami Zeydi et al. [48] systematically have reviewed nurses’ awareness and attitudes toward telemedicine and report the positive attitudes of nurses, 56% of whom are desirably aware of this technology. Also, nurses’ awareness and attitudes were significantly and directly associated. Hence, they concluded that one of the paramount components of telemedicine in nurse education was to raise their awareness.
Also, Mousavi Baigi et al. recently have conducted a systematic review with the aim of investigating the attitude, knowledge, and skills of health students in the field of artificial intelligence. The results of their study show that healthcare students have a positive and promising attitude toward artificial intelligence in medicine. However, most students have little knowledge of and limited skills in working with artificial intelligence [49]. Recently, many studies have been conducted in order to investigate the impact of telemedicine, telerehabilitation, and various methods of providing health and medical services based on technology, which proves their effectiveness, safety, and efficiency [50-53]. However, the lack of knowledge and skills of specialists and nurses as the main users of these services hinders significant progress in the health of society in the first place, and from a broader perspective, it hinders progress in the economies of countries. Spending the right amount on health services, especially telemedicine services, which empower patients to self-manage and prevent various diseases, prevents additional expenses later. Therefore, investing in the knowledge, awareness, and skills of students and healthcare professionals can be a powerful approach for further development [34, 49, 54-58].
In sum, the findings of this study indicated that health specialists maintained positive and promising attitudes and above-moderate awareness, knowledge, and skills, while many of the included studies asked for passing related courses on telemedicine. Thus, we suggest providing educational fundamentals, workshops, and classes about telemedicine, informing through media campaigns, and encouraging the treatment cadre to raise awareness.
Strengths and limitations
Among the limitations of this study, we can refer to the studies published in languages other than English and thus ignored in this review. Also, the differences in the specialty of the participants, the publication year of the studies, and the examined context, culture, and gender, as well as the degree of access to IT specialists in various places, may lead to bias in the results. Furthermore, the included studies employed various questionnaires with different items. Thus, one study might have questioned primary telemedicine knowledge and skills, e.g., working with emails and WhatsApp, and another interrogated the knowledge and skill in working with intricate telemedicine tools, such as artificial intelligence, working with robot surgeons, etc., and reported low knowledge of the participants. Thus, future studies are suggested to examine and assess an international survey with a standard and identical questionnaire to confirm the evidence of this systematic review. However, this research was the first systematic review evaluating the telemedicine attitudes, awareness, knowledge, and skills of health specialists that were the key players in the health system of countries and provided valuable perspectives to policymakers and planners.
Conclusion
Health specialists held positive and promising attitudes toward telemedicine. Telemedicine awareness, knowledge, and skill among health professionals is above-moderate and desirable.
Acknowledgments: We would like to thank all of the participants in this research as well as the Mashhad University of Medical Sciences Student Research Committee for their assistance.
Ethical Permissions: This study was approved by the Ethical Committee of Mashhad University of Medical Sciences (approval number: IR.MUMS.REC.1401.196).
Conflicts of Interests: The authors have declared that they have no conflicts of interest.
Authors' Contribution: Dahmardeh Kemmak F (First Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (30%); Sarbaz M (Second Author), Introduction Writer/Methodologist/Main Researcher (10%); Mousavi Baigi SF (Third Author), Methodologist/Statistical Analyst (10%); Marouzi P (Fourth Author), Introduction Writer/Statistical Analyst (10%); Sheykhotayefeh M (Fifth Author), Methodologist/Main or Assistant Researcher (10%); Kimiafar Kh (Sixth Author), Methodologist/Discussion Writer/Statistical Analyst (30%)
Funding/Support: The authors did not receive support from any organization for this research.
Article Type: Systematic Review |
Subject:
Health Communication
Received: 2024/10/31 | Accepted: 2024/12/2 | Published: 2024/12/12
Received: 2024/10/31 | Accepted: 2024/12/2 | Published: 2024/12/12
References
1. Elhadi M, Elhadi A, Bouhuwaish A, Bin Alshiteewi F, Elmabrouk A, Alsuyihili A, et al. Telemedicine awareness, knowledge, attitude, and skills of health care workers in a low-resource country during the COVID-19 pandemic: Cross-sectional study. J Med Internet Res. 2021;23(2):e20812. [Link] [DOI:10.2196/20812]
2. Ahmed T, Baig M, Bashir M, Gazzaz Z, Butt N, Khan S. Knowledge, attitudes, and perceptions related to telemedicine among young doctors and nursing staff at the King Abdul-Aziz University Hospital Jeddah, KSA. Niger J Clin Pract. 2021;24(4):464-9. [Link] [DOI:10.4103/njcp.njcp_34_20]
3. Russo L, Campagna I, Ferretti B, Agricola E, Pandolfi E, Carloni E, et al. What drives attitude towards telemedicine among families of pediatric patients? A survey. BMC Pediatr. 2017;17:21. [Link] [DOI:10.1186/s12887-016-0756-x]
4. Abdool S, Abdallah S, Akhlaq S, Razzak HA. User acceptance level of and attitudes towards telemedicine in the United Arab Emirates: A quantitative study. Sultan Qaboos Univ Med J. 2021;21(2):e203-9. [Link] [DOI:10.18295/squmj.2021.21.02.008]
5. Barsom EZ, Jansen M, Tanis PJ, Van De Ven AWH, Blussé Van Oud-Alblas M, Buskens CJ, et al. Video consultation during follow up care: Effect on quality of care and patient-and provider attitude in patients with colorectal cancer. Surg Endosc. 2020;35(3):1278-87. [Link] [DOI:10.1007/s00464-020-07499-3]
6. Hasson SP, Waissengrin B, Shachar E, Hodruj M, Fayngor R, Brezis M, et al. Rapid implementation of telemedicine during the COVID‐19 pandemic: Perspectives and preferences of patients with cancer. Oncologist. 2021;26(4):e679-85. [Link] [DOI:10.1002/onco.13676]
7. Ming WK, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, Levy JC, et al. Telemedicine technologies for diabetes in pregnancy: A systematic review and meta-analysis. J Med Internet Res. 2016;18(11):e290. [Link] [DOI:10.2196/jmir.6556]
8. Yoon EJ, Tong D, Anton GM, Jasinski JM, Claus CF, Soo TM, et al. Patient satisfaction with neurosurgery telemedicine visits during the coronavirus disease 2019 pandemic: A prospective cohort study. World Neurosurg. 2021;145:e184-91. [Link] [DOI:10.1016/j.wneu.2020.09.170]
9. Hertling S, Hertling D, Martin D, Graul I. Acceptance, use, and barriers of telemedicine in transgender health care in times of SARS-CoV-2: Nationwide cross-sectional survey. JMIR Public Health Surveill. 2021;7(12):e30278. [Link] [DOI:10.2196/30278]
10. Hu XJ, Barber LK, Park Y, Day A. Defrag and reboot? Consolidating information and communication technology research in IO psychology. Ind Organ Psychol. 2021;14(3):371-96. [Link] [DOI:10.1017/iop.2021.3]
11. Mousavi Baigi SF, Sarbaz M, Ghaddaripouri K, Noori N, Kimiafar K. The effect of tele-rehabilitation on improving physical activity in patients with chronic obstructive pulmonary disease: A systematic review of randomized controlled clinical trials. Front Health Inform. 2022;11(1):113. [Link] [DOI:10.30699/fhi.v11i1.359]
12. Ghaddaripouri K, Baigi SFM, Noori N, Habibi MRM. Investigating the effect of virtual reality on reducing the anxiety in children: A systematic review. Front Health Inform. 2022;11(1):114. [Link] [DOI:10.30699/fhi.v11i1.373]
13. Mousavi Baigi SF, Mousavi AS, Kimiafar K, Sarbaz M. Evaluating the cost effectiveness of tele-rehabilitation: A systematic review of randomized clinical trials. Front Health Inform. 2022;11(1):118. [Link] [DOI:10.30699/fhi.v11i1.368]
14. Müller SD, Wehner DL, Konzag H, Vesterby M, Høybye MT. The paradox of project success despite lack of the "My Pathway" telehealth platform usage. Health Inform J. 2021;27(1):1460458220976734. [Link] [DOI:10.1177/1460458220976734]
15. Reinhardt G, Schwarz PE, Harst L. Non-use of telemedicine: A scoping review. Health Inform J. 2021;27(4):14604582211043147. [Link] [DOI:10.1177/14604582211043147]
16. Mousavi Baigi SF, Baigi SMM, Habibi MRM. Challenges and opportunities of using telemedicine during Covid-19 epidemic: A systematic review. Front Health Inform. 2022;11(1):109. [Link] [DOI:10.30699/fhi.v11i1.346]
17. Ly BA, Labonté R, Bourgeault IL, Niang MN. The individual and contextual determinants of the use of telemedicine: A descriptive study of the perceptions of Senegal's physicians and telemedicine projects managers. PLoS One. 2017;12(7):e0181070. [Link] [DOI:10.1371/journal.pone.0181070]
18. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151(4):264-9. [Link] [DOI:10.7326/0003-4819-151-4-200908180-00135]
19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann Intern Med. 2009;151(4):W65-94. [Link] [DOI:10.7326/0003-4819-151-4-200908180-00136]
20. Joanna Briggs Institute. Checklist for analytical cross sectional studies: Critical appraisal tools for use in JBI systematic reviews. Adelaide: JBI; 2017. [Link]
21. Richards H, King G, Reid M, Selvaraj S, McNicol I, Brebner E, et al. Remote working: Survey of attitudes to eHealth of doctors and nurses in rural general practices in the United Kingdom. Fam Pract. 2005;22(1):2-7. [Link] [DOI:10.1093/fampra/cmh716]
22. Meher SK, Tyagi RS, Chaudhry T. Awareness and attitudes to telemedicine among doctors and patients in India. J Telemed Telecare. 2009;15(3):139-41. [Link] [DOI:10.1258/jtt.2009.003011]
23. Ibrahim MIM, Phing C, Palaian S. Evaluation of knowledge and perception of Malaysian health professionals about telemedicine. J Clin Diagn Res. 2010;4(1):2052-6. [Link]
24. Ayatollahi H, Sarabi FZP, Langarizadeh M. Clinicians' knowledge and perception of telemedicine technology. Perspect Health Inf Manag. 2015;12(Fall):1c. [Link]
25. Olok GT, Yagos WO, Ovuga E. Knowledge and attitudes of doctors towards e-health use in healthcare delivery in government and private hospitals in Northern Uganda: A cross-sectional study. BMC Med Inform Decis Mak. 2015;15:87. [Link] [DOI:10.1186/s12911-015-0209-8]
26. Zayapragassarazan Z, Kumar S. Awareness, knowledge, attitude and skills of telemedicine among health professional faculty working in teaching hospitals. J Clin Diagn Res. 2016;10(3):JC01-4. [Link] [DOI:10.7860/JCDR/2016/19080.7431]
27. Ashfaq A, Memon SF, Zehra A, Barry S, Jawed H, Akhtar M, et al. Knowledge and attitude regarding telemedicine among doctors in Karachi. Cureus. 2020;12(2):e6927. [Link] [DOI:10.7759/cureus.6927]
28. Albarrak AI, Mohammed R, Almarshoud N, Almujalli L, Aljaeed R, Altuwaijiri S, et al. Assessment of physician's knowledge, perception and willingness of telemedicine in Riyadh region, Saudi Arabia. J Infect Public Health. 2021;14(1):97-102. [Link] [DOI:10.1016/j.jiph.2019.04.006]
29. Glock H, Milos Nymberg V, Borgström Bolmsjö B, Holm J, Calling S, Wolff M, et al. Attitudes, barriers, and concerns regarding telemedicine among Swedish primary care physicians: A qualitative study. Int J Gen Med. 2021;14:9237-46. [Link] [DOI:10.2147/IJGM.S334782]
30. Assaye BT, Jemere AT, Nigatu AM. Knowledge and awareness of health professionals towards telemedicine services in Northwest, Ethiopia. Digit Health. 2022;8:20552076221143250. [Link] [DOI:10.1177/20552076221143250]
31. Kumar G, Shardha HK, Tariq W, Qazi MA, Kumar K, Maheshwari C, et al. Assessment of knowledge and attitude of healthcare professionals regarding the use of telemedicine: A cross-sectional study from rural areas of Sindh, Pakistan. Front Public Health. 2022;10:967440. [Link] [DOI:10.3389/fpubh.2022.967440]
32. Sukumaran AB, Leela M, Suresh K, Selvin H, Jose R, Prakash S, et al. Awareness and skills of modern telemedicine practice among doctors in Kerala-A cross-sectional study. J Clin Diagn Res. 2022;16(4):LC21-6. [Link] [DOI:10.7860/JCDR/2022/51754.16209]
33. Fouad AA, Osman MA, Abdelmonaem YMM, Karim NAHA. Awareness, knowledge, attitude, and skills of telemedicine among mental healthcare providers. Middle East Curr Psychiatry. 2023;30(1):5. [Link] [DOI:10.1186/s43045-022-00272-3]
34. Ghaddaripouri K, Mousavi Baigi SF, Abbaszadeh A, Mazaheri Habibi MR. Attitude, awareness, and knowledge of telemedicine among medical students: A systematic review of cross-sectional studies. Health Sci Rep. 2023;6(3):e1156. [Link] [DOI:10.1002/hsr2.1156]
35. Bashir MS, Lalithabai DS, AlOtaiby S, Abu-Shaheen A. Health care professionals' knowledge and attitudes toward telemedicine. Front Public Health. 2023;11:957681. [Link] [DOI:10.3389/fpubh.2023.957681]
36. Barton AJ, Amura CR, Willems EL, Medina R, Centi S, Hernandez T, et al. Patient and provider perceptions of COVID-19-Driven telehealth use from nurse-led care models in rural, frontier, and urban Colorado communities. J Patient Exp. 2023;10:23743735231151546. [Link] [DOI:10.1177/23743735231151546]
37. Garavand A, Samadbeik M, Kafashi M, Abhari S. Acceptance of health information technologies, acceptance of mobile health: A review article. J Biomed Phys Eng. 2017;7(4):403-8. [Link]
38. Owolabi EO, Mac Quene T, Louw J, Davies JI, Chu KM. Telemedicine in surgical care in low- and middle-income countries: A scoping review. World J Surg. 2022;46(8):1855-69. [Link] [DOI:10.1007/s00268-022-06549-2]
39. Seboka BT, Yilma TM, Birhanu AY. Awareness and readiness to use telemonitoring to support diabetes care among care providers at teaching hospitals in Ethiopia: An institution-based cross-sectional study. BMJ Open. 2021;11(10):e050812. [Link] [DOI:10.1136/bmjopen-2021-050812]
40. Purba C, Sinaga I, Rawung S, Manik MJ, Sibuea R. Nurses' perceived knowledge, self-confidence, and attitudes in using telemedicine: A case study from West Indonesia. Enferm Clin. 2023;33:S12-6. [Link] [DOI:10.1016/j.enfcli.2023.01.006]
41. Mohammadi M, Bahaadinbeigy K, Ahmadinejad M, Chaboki B, Tabesh H, Etminani K. Clinical dashboard in the intensive care unit: Need-assessment and survey about attitudes and acceptance of Tele-ICU from the viewpoint of nurses and clinicians in the intensive care unit. Tanaffos. 2019;18(2):142-51. [Link]
42. Sheikhtaheri A, Sarbaz M, Kimiafar K, Ghayour M, Rahmani S. Awareness, attitude and readiness of clinical staff towards telemedicine: A study in Mashhad, Iran. Stud Health Technol Inform. 2016:228:142-6. [Link] [DOI:10.3233/978-1-61499-678-1-142]
43. Islam MM, Touray M, Yang HC, Poly TN, Nguyen PA, Li YJ, et al. E-health literacy and health information seeking behavior among university students in Bangladesh. Stud Health Technol Inform. 2017;245:122-5. [Link]
44. Boringi M, Waghray S, Lavanya R, Babu DB, Badam RK, Harsha N, et al. Knowledge and awareness of teledentistry among dental professionals-A cross sectional study. J Clin Diagn Res. 2015;9(8):ZC41-4. [Link] [DOI:10.7860/JCDR/2015/13303.6320]
45. Ftouni R, AlJardali B, Hamdanieh M, Ftouni L, Salem N. Challenges of telemedicine during the COVID-19 pandemic: A systematic review. BMC Med Inform Decis Mak. 2022;22(1):207. [Link] [DOI:10.1186/s12911-022-01952-0]
46. Richard E, Moll Van Charante EP, Hoevenaar-Blom MP, Coley N, Barbera M, Van Der Groep A, et al. Healthy ageing through internet counselling in the elderly (HATICE): A multinational, randomised controlled trial. Lancet Digit Health. 2019;1(8):e424-34. [Link] [DOI:10.1016/S2589-7500(19)30153-0]
47. Naqvi SZ, Ahmad S, Rocha IC, Ramos KG, Javed H, Yasin F, et al. Healthcare workers' knowledge and attitude toward telemedicine during the COVID-19 pandemic: A global survey. Cureus. 2022;14(10):e30079. [Link] [DOI:10.7759/cureus.30079]
48. Emami Zeydi A, Ghazanfari MJ, Ghanbari R, Karkhah S. Knowledge and attitude of nurses towards using telehealth: A systematic review. Proceedings of the 4th Shiraz International Congress on Mobile Health. Shiraz; 2021. [Link]
49. Mousavi Baigi SF, Sarbaz M, Ghaddaripouri K, Ghaddaripouri M, Mousavi AS, Kimiafar K. Attitudes, knowledge, and skills towards artificial intelligence among healthcare students: A systematic review. Health Sci Rep. 2023;6(3):e1138. [Link] [DOI:10.1002/hsr2.1138]
50. Sarbaz M, Manouchehri Monazah F, Eslami S, Kimiafar K, Mousavi Baigi SF. Effect of mobile health interventions for side effects management in patients undergoing chemotherapy: A systematic review. Health Policy Technol. 2022;11(4):100680. [Link] [DOI:10.1016/j.hlpt.2022.100680]
51. Mousavi Baigi SF, Moradi F, Vasseifard F, Mohammad Abadi F, Mazaheri Habibi MR. The effect of nutrition training on knowledge of students at university of medical sciences. Top Clin Nutr. 2022;37(3):236‐41. [Link] [DOI:10.1097/TIN.0000000000000290]
52. Mousavi AS, Baigi SF, Dahmardeh F, Mehneh MR, Darrudi R. Teleophthalmology: A systematic review of randomized controlled trials. Front Health Inform. 2023;12:141. [Link] [DOI:10.30699/fhi.v12i0.414]
53. Mousavi Baigi SF, Raei Mehneh M, Sarbaz M, Norouzi Aval R, Kimiafar K. Telerehabilitation in response to critical coronavirus: A systematic review based on current evidence. J Isfahan Med School. 2022;40(678):498-508. [Persian] [Link]
54. Mousavi Baigi SF, Sarbaz M, Marouzi P, Kimiafar K. Evaluating the impact of digital game on learning medical terminology of paramedical students: Protocol for a randomized controlled trial. Stud Health Technol Inform. 2022;295:51-4. [Link] [DOI:10.3233/SHTI220658]
55. Galpin K, Sikka N, King SL, Horvath KA, Shipman SA, AAMC Telehealth Advisory Committee. Expert consensus: Telehealth skills for health care professionals. Telemed J E Health. 2021;27(7):820-4. [Link] [DOI:10.1089/tmj.2020.0420]
56. Mousavi Baigi SF, Sarbaz M, Sobhani-Rad D, Mousavi AS, Kimiafar K. Rehabilitation registration systems: Current recommendations and challenges. Front Health Inform. 2022;11(1):124. [Link] [DOI:10.30699/fhi.v11i1.388]
57. Mousavi Baigi SF, Sarbaz M, Sobhani-Rad D, Kimiafar K. A comparative study of rehabilitation information systems in 8 countries: A literature review. Iran Rehabil J. 2023;21(1):1-16. [Link] [DOI:10.32598/irj.21.1.1766.1]
58. Mousavi Baigi S, Dahmardeh Kemmak F, Sarbaz M, Norouzi Aval R, Kimiafar K. Application of artificial intelligence in occupational therapy. Health Educ Health Promot. 2024;12(3):513-20. [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |