Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 477-485 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
La Rangki R, Fithria F. Factors Affecting the Quality of Life of Adults with Stomas. Health Educ Health Promot 2024; 12 (3) :477-485
URL: http://hehp.modares.ac.ir/article-5-76518-en.html
URL: http://hehp.modares.ac.ir/article-5-76518-en.html
R. La Rangki *1, F. Fithria2
1- Department of Nursing, Medical Faculty, University of Halu Oleo, Kendari, Indonesia
2- Department of Public Health, Public Health of Faculty, University of Halu Oleo, Kendari, Indonesia
2- Department of Public Health, Public Health of Faculty, University of Halu Oleo, Kendari, Indonesia
Keywords: Quality of Life [MeSH], Psychological Well-Being [MeSH], Colostomy [MeSH], Ileostomy [MeSH]
Full-Text [PDF 965 kb]
(347 Downloads)
| Abstract (HTML) (405 Views)
Full-Text: (7 Views)
Introduction
Quality of life (QoL) encompasses a person’s overall contentment with life and is influenced by a range of factors, including health, cultural norms, social circumstances, and psychological well-being. The introduction of a stoma appears to impact QoL, as it may disrupt bodily functions and self-image, leading to potential physical, emotional, and social challenges [1, 2].
An intestinal stoma is surgically created to connect the intestine with the outside environment, compensating for the function of a compromised organ, and is performed for various reasons. Research involving 216 individuals with intestinal stomas revealed that the predominant reason for creating a stoma is colorectal cancer, accounting for 40.7% of cases [3, 4].
Individuals with stomas encounter a range of difficulties, including recognizing the significance of their surgery and adapting to the physical changes it brings, which affect their psychological well-being and social interactions. Additionally, concerns about potential leakage can provoke anxiety, particularly in social settings [1]. Individuals with stomas, especially those struggling to adapt, often experience biopsychosocial challenges that can negatively impact their QoL. Research conducted on Chinese individuals with stomas reported the majority (87.0%) have lived with their stoma for up to three months with a low average QoL score, indicating significant adverse effects on their well-being due to the stoma. Individuals with stomas experience changes that impact their body image and self-esteem, which in turn affect their QoL. These individuals need to develop personal coping strategies influenced by various factors, including health education and attitudes toward personal care. Therefore, it is crucial for support networks, especially healthcare providers, to gain a comprehensive understanding of each person, taking into account their individual, social, economic, and cultural contexts to deliver holistic care [5, 6].
QoL focuses on the general well-being of individuals or groups, prioritizing health and happiness over financial status [7]. It encompasses how patients perceive their own health across physical, mental, social, and spiritual dimensions. Research into the well-being of ostomy patients should consider these various aspects: physical health, psychological condition, social engagement, and spiritual life. Typically, patients experience a shift in their QoL after ostomy surgery, moving from initial negative impacts to improved outcomes as they adapt over time [8]. Various factors affect the QoL of ostomy patients, including challenges in managing the ostomy, access to healthcare coverage, and the financial burden associated with procuring necessary supplies [5, 9]. Complications related to ostomy care, exacerbated by the absence of specialized nursing support, are linked to lower QoL scores [9]. Such complications often impose significant physical and psychosocial limitations on individuals and their families [10]. Emotional stress, physical discomfort, and doubts are identified as key contributors to these negative consequences following ostomy surgery. Additionally, inadequate family and social support can diminish patients’ self-identity and self-esteem, compounding these negative effects [6]. While the precise prevalence of stomal and peristomal complications remains unclear, it is estimated that a substantial majority of ostomy patients (up to 70%) experience emotional, psychological, and financial hardships that impact their QoL [11].
The present review aimed to evaluate factors related to the QoL of adults with an intestinal stoma and how those factors influence their perceived QoL.
Information and Methods
Protocol
The present review complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, 2020 version [12].
Search strategy
We explored various databases, including PubMed, Scopus, Web of Science, and ProQuest. Searches were conducted using individual and combined terms, such as “stoma,” “colostomy,” “ileostomy,” and “quality of life,” along with Boolean operators, like “AND” and “OR” to link these keywords. The search was limited to English-language articles, and we adjusted the filters to enhance the relevance and accuracy of the results.
Inclusion criteria
This review encompassed all research examining risk factors for diabetes mellitus in children and adolescents. There was no restriction on the search timeframe to ensure a comprehensive compilation of relevant studies. However, studies published in conference proceedings, reviews, meta-analyses, commentaries, book chapters, reports, case studies, and letters to the editor were excluded from consideration.
Selection process
Two authors independently and separately screened the titles and abstracts of the identified studies. In cases of conflicting opinions between the two screening authors, the first author made the final decision. This rapid screening involved assessing the titles, objectives, and conclusions of the relevant studies. We conducted a deeper review of specific studies by examining their main texts to extract any additional necessary information.
Study quality
We assessed each quantitative study based on five criteria, including study details, sample characteristics, measurement methods, data analysis, and result interpretation. This evaluation checklist uses critical appraisal tools [2], specifically designed for systematic reviews. The quality of studies was assessed based on five key criteria, including clear explanations of the research objectives, data collection methods, and participant details, well-defined sampling methods and sufficient sample size (N≥200), the use of valid and reliable measurement tools, appropriate data analysis techniques, and consistency between the discussion, conclusions, and results. Studies meeting all five criteria are considered high quality. Those meeting at least three of the criteria are deemed moderate in quality, while studies fulfilling only one or two criteria are classified as low quality.
Risk of bias assessment
We utilized the Risk of Bias in Non-randomized Studies-Exposure Studies (ROBINS-E) tool to identify potential biases in each study [13]. This tool evaluates seven domains to gauge both internal and external validity. The outcomes are categorized as low, some concerns, high, or very high based on the assessment. The final risk of bias evaluations was reviewed and endorsed by all authors, incorporating feedback from external reviewers.
Data extraction and synthesis
Two authors collaborated in the crucial information extraction process. In cases where there were differing opinions regarding the extracted data, they were reconciled through consensus. The extraction criteria included the first author and publication year, sample size, age, mean time since surgery, instruments, factors analyzed, and main findings.
Findings
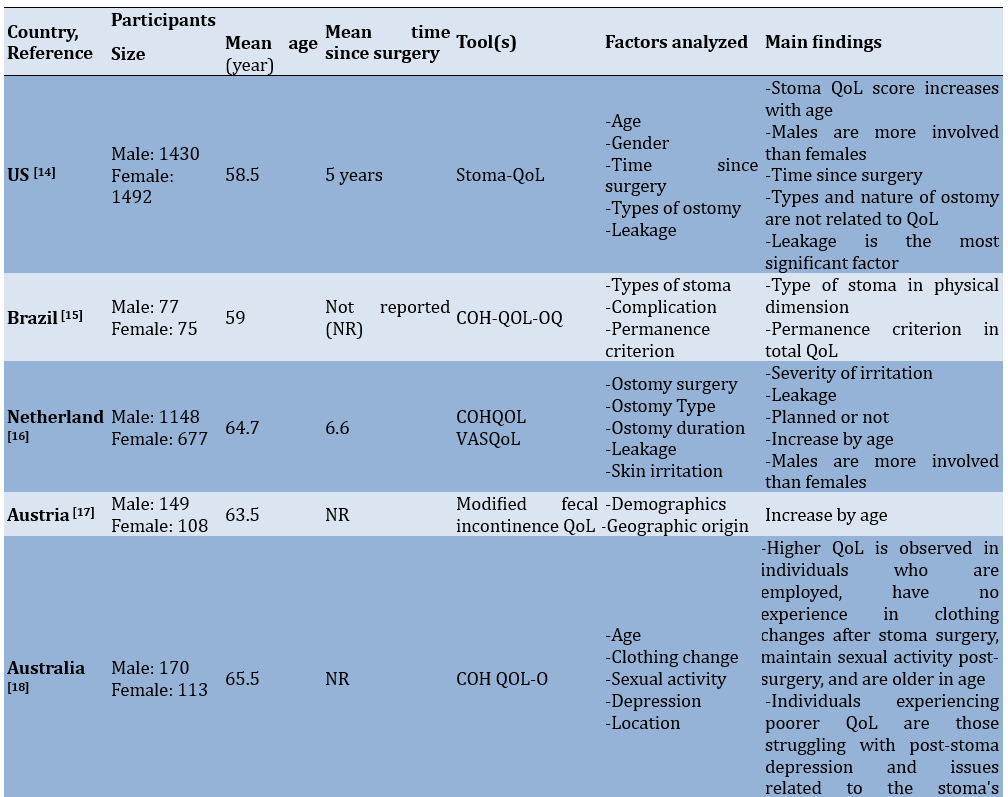
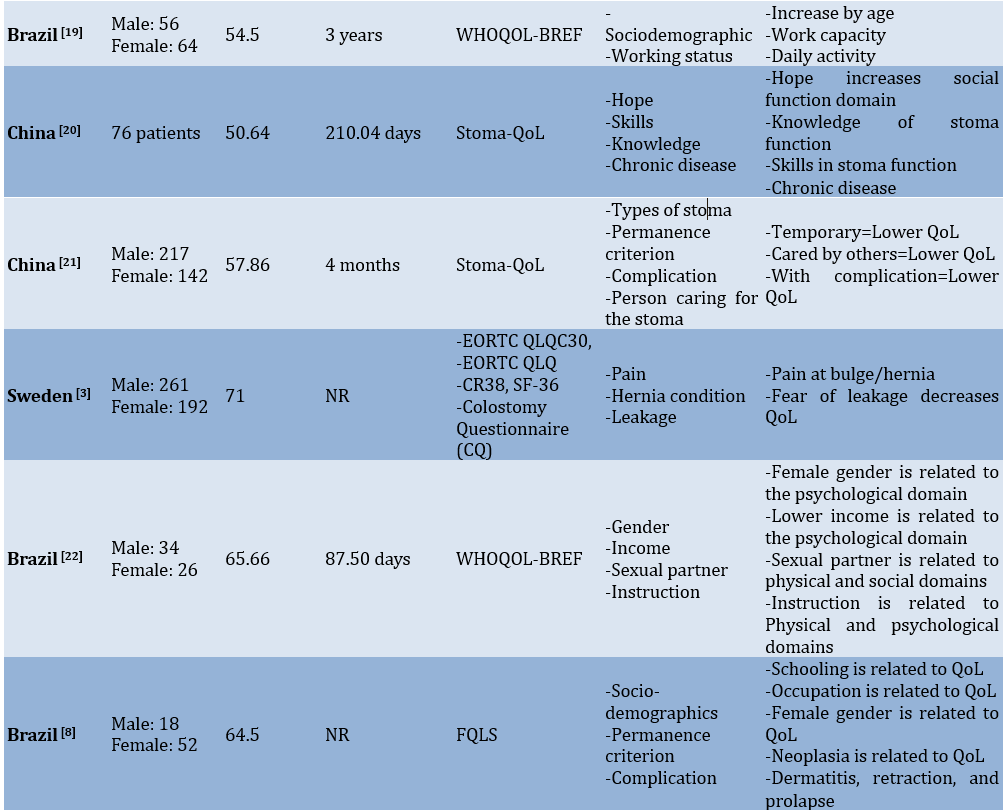
The initial database search retrieved 899 articles. After removing 707 duplicates and ineligible articles not relevant to the review’s theme, 192 articles remained for screening. During the eligibility assessment, 28 studies were evaluated, and nine articles were excluded for various reasons. Ultimately, only 19 studies met the criteria and will proceed to the next stage for extraction and analysis (Figure 1 and Table 1).
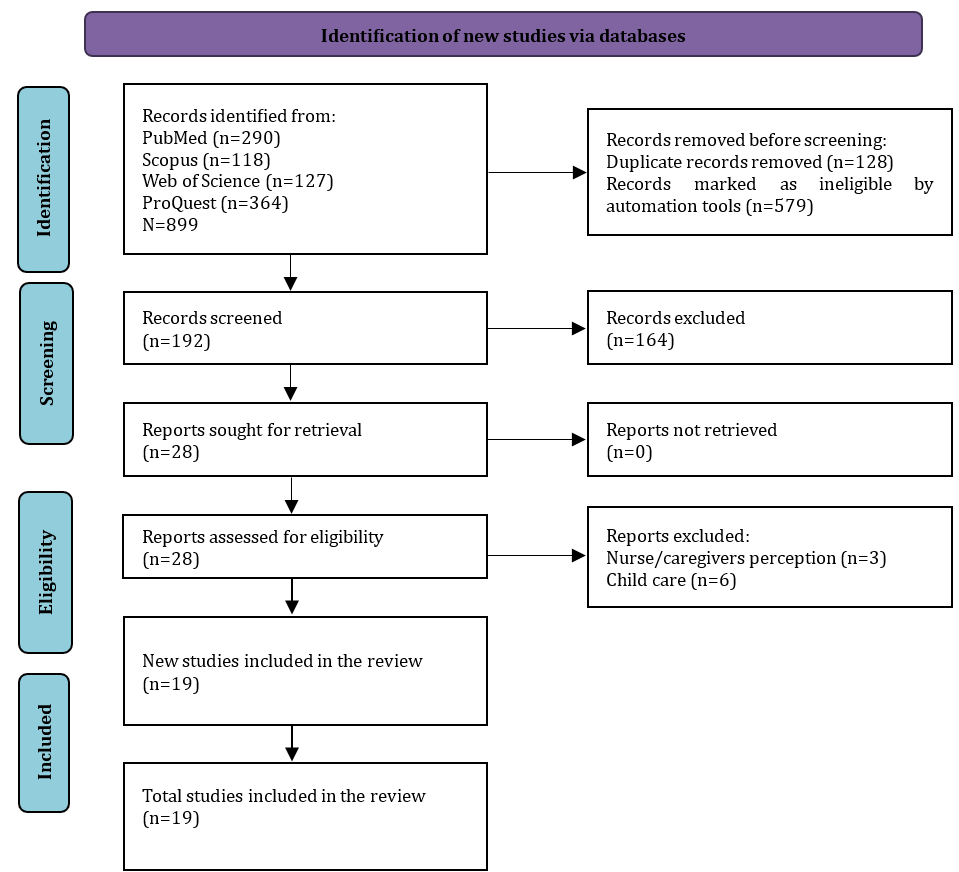
Figure 1. PRISMA flow diagram for literature search
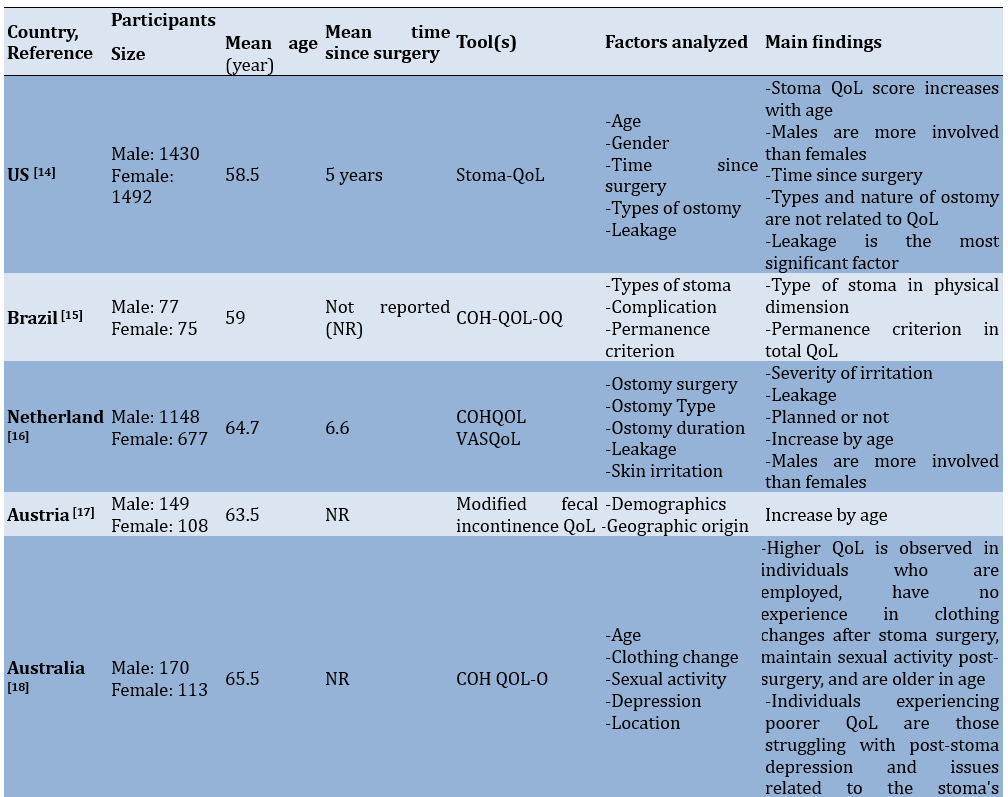
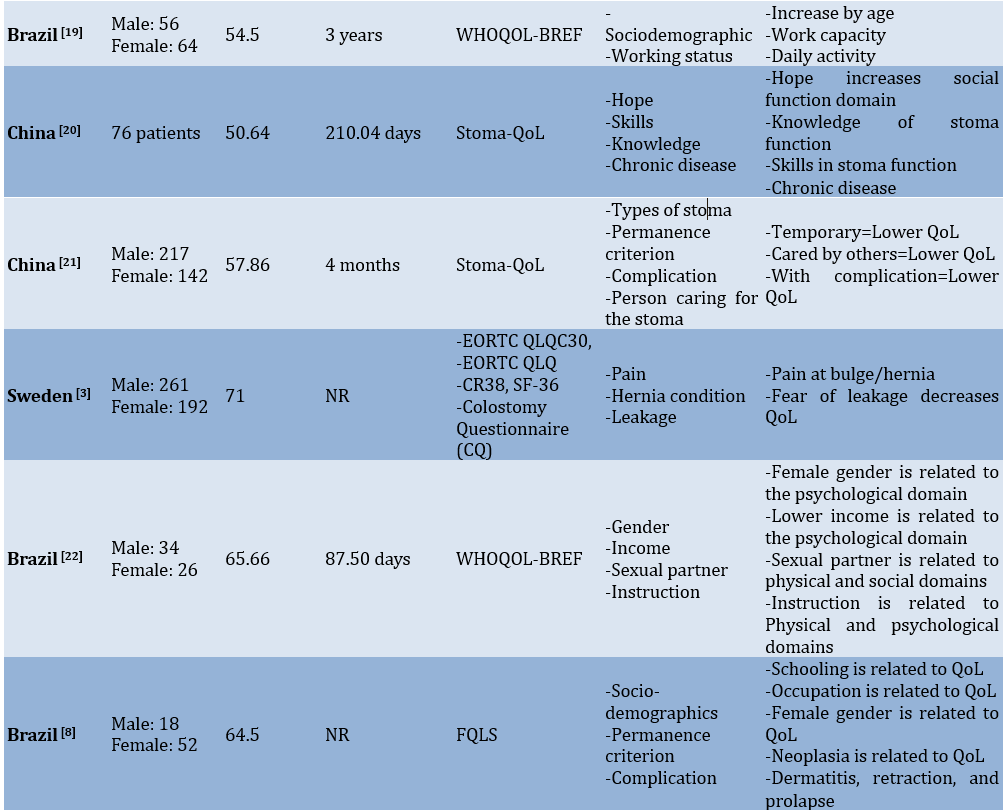
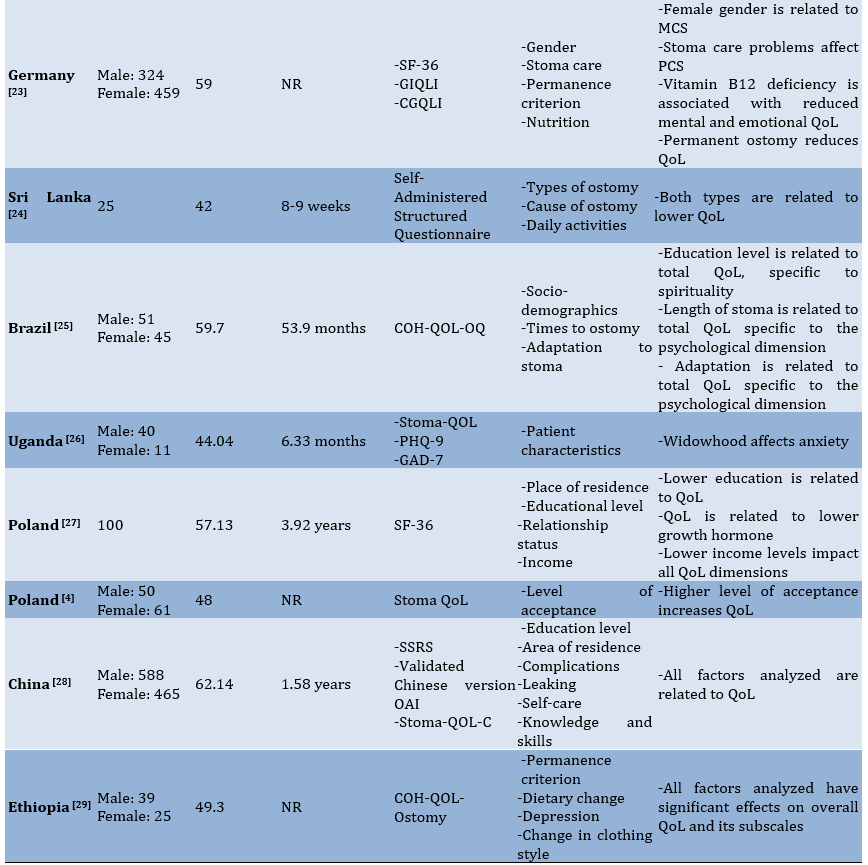
Table 1. Data extraction of the included studieSs
Overview of the eligible studies
We identified 19 studies that addressed factors related to the QoL of individuals with intestinal stomas, with most studies conducted in European populations across five different countries, including Poland (n=2) [4, 29], and one study each from Austria [17], the Netherlands [16], Sweden [3], and Germany [25]. Other studies came from the Americas, including Brazil (n=5) [8, 15, 23, 27, 30] and the US [14]. In Asia, we found the most studies from China, with three studies [20, 21-31], followed by one study each from Australia [18] and Sri Lanka [26]. On the African continent, there are two studies from two different countries, including Uganda [28] and Ethiopia [32].
The total number of patients participating in the study was 8,860 individuals living with an intestinal stoma, with a mean age of 56.5 years. The mean time since ostomy also showed high variation, ranging from two months to sixty months. The tools used included Stoma-QoL, COH-QOL-OQ, Modified FI-QoL, QoL-O, WHO-QOL-bref, EORTC QLQ-C30, EORTC QLQ-CR38, SF-36, CQ, FQLS, GIQLI, CGQLI, PHQ-9, GAD-7, and SSRS.
Results of the study quality assessment
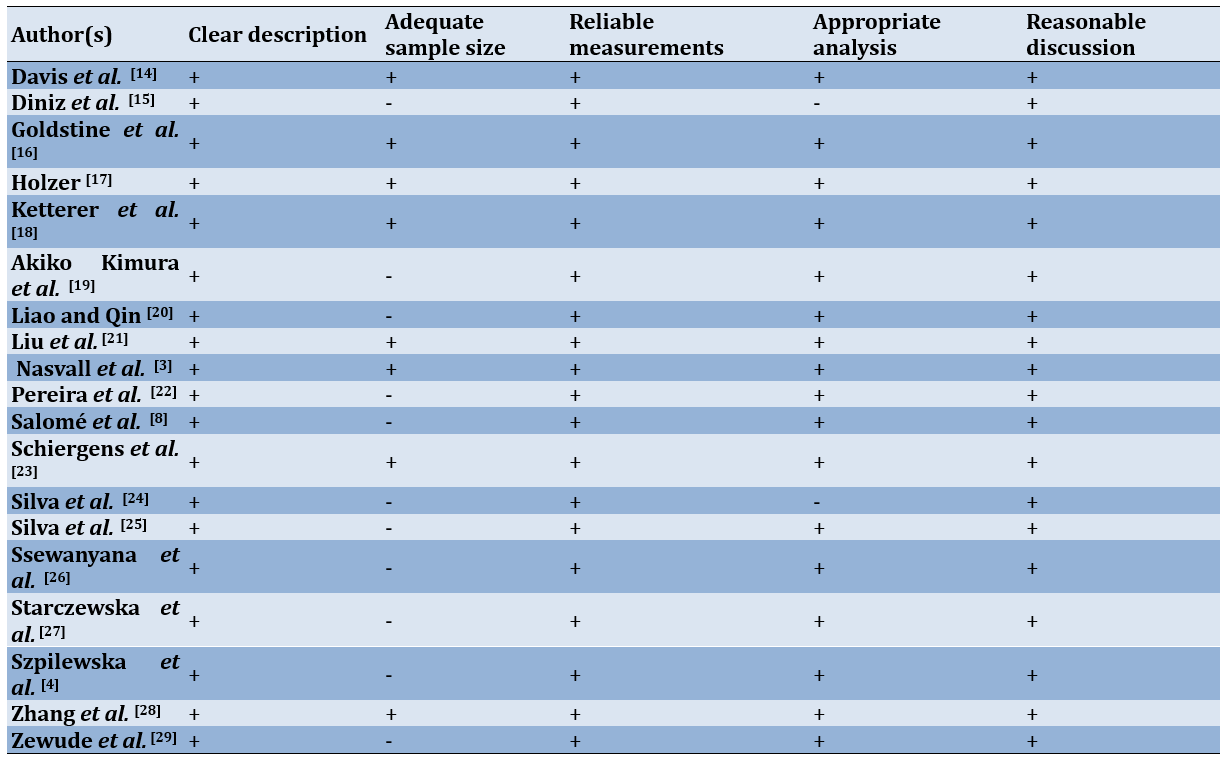
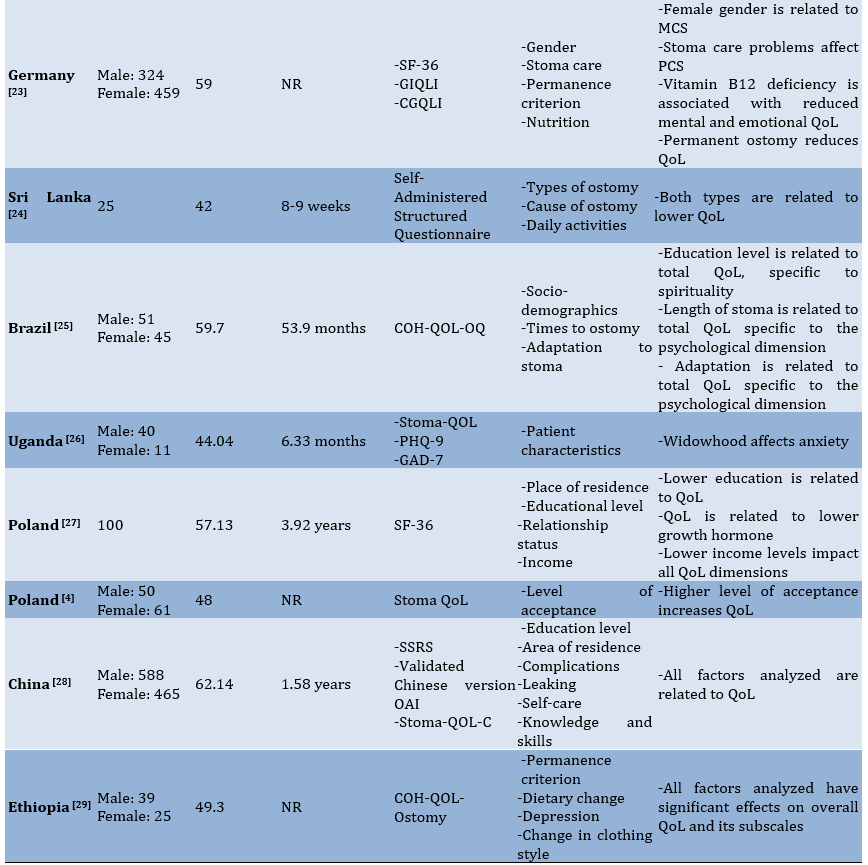
The quality assessment results indicated that, overall, the studies included fell into the moderate to good quality range (Table 2).
Table 2. Summary of quality appraisal
Results of risk of bias assessment
We assessed risk of bias in the studies, and found its seven domains (Figure 2).
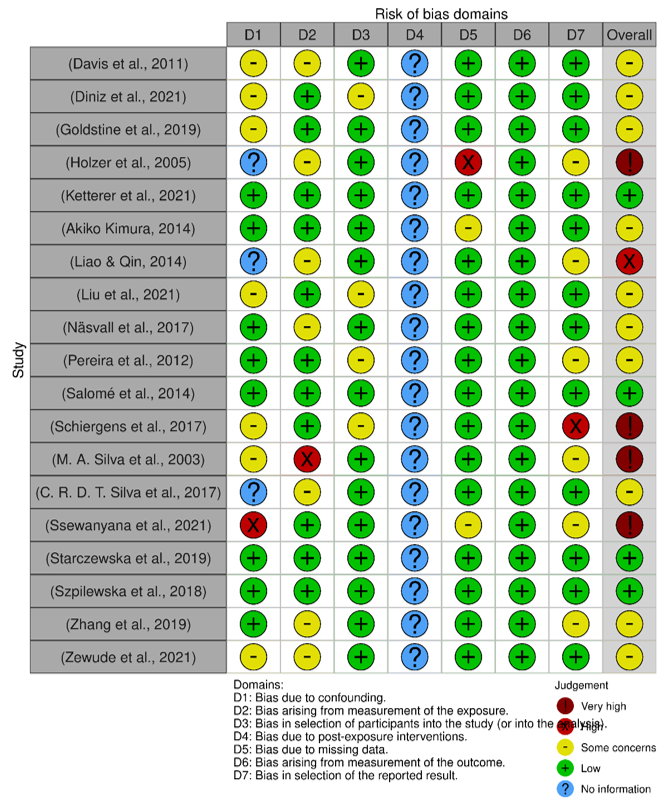
Figure 2. Result of risk of bias assessment.
Factors related to QoL
Of the 19 studies descriptively analyzed, in general, two categories of factors (personal and ostomy factors) were strongly associated with one or more of the QoL domains. Among the studies we collected, two studies [4, 31] did not specifically mention the correlation between the identified factors and the domains of QoL. Generally, the QoL domains mentioned in the tools used in the studies included physical, psychological, social, and spiritual aspects. The quality of the studies can vary depending on the specific instrument used for assessment. For instance, different tools cover a range of domains. Stoma-QoL addresses family and social relationships and the impact of the ostomy bag, FIQL focuses on lifestyle, coping, depression/self-perception, and embarrassment, WHOQOL-BREF includes the environment, EORTC QLQ-C30 assesses global health, functioning scales (physical, emotional, cognitive, and social), and specific items (dyspnea, insomnia, appetite loss, bowel function, and financial impact), SF-36 evaluates physical function, role limitations, body pain, general health, vitality, social functioning, emotional role, and mental health, CQ considers daily life, physical activity, profession, sexuality, pain, stoma protrusion, urinary continence, and daily life limitations, FQLS reviews material and physical well-being, relationships, social activities, community involvement, personal development, and recreation, GIQLI examines gastrointestinal symptoms, emotional status, physical and social functioning, and distress, CGQLI looks at current QoL, health quality, and energy levels, OAI-23 (Chinese version) assesses persistent worry, life attitude, and acceptance, and SSRS measures subjective support, objective support, and support utilization.
In a study conducted in China, researchers explored how psychosocial adaptation relates to QoL and identified several factors strongly linked to all QoL dimensions, including education level, method of medical payment, residence area, peristomal complications, regularity of defecation, occurrence of leaks, self-care capability, patient-provider communication, and stoma care knowledge and skills [31]. In contrast, a study in the US found that QoL is influenced by factors, such as leakage from the ostomy appliance, peristomal skin condition, age, gender, and time elapsed since surgery [14]. Additionally, factors, like peristomal skin irritation, leaks affecting the peristomal skin, surgical planning [16], geographic location, education [17], employment status, clothing changes, sexual activity, age, depression, and stoma location [8, 18] also impact QoL. In the following sections, we described the link between each factor and the domains of the QoL instruments analyzed in the included studies.
Personal factors
Personal factors analyzed in eligible studies included socio-demographics (age, gender, marital status, geographic origin, employment status, income, and education level), sexual activity, expectations, depression, knowledge, nutrition, and daily activities.
Several studies have mentioned that age is strongly associated with QoL. With increasing age, QoL scores are better compared to those of younger individuals [16, 23, 29]. Specifically, Pereira et al. noted that age correlates with higher scores in each domain of the WHOQOL-BREF, including physical, psychological, social, and environmental domains [22]. In another study, it was mentioned that SF-36 scores increase with age, particularly in relation to the domains of physical functioning, role limitations, pain perception, general health, social functioning, and mental health [29]. Gender also contributes to the QoL of patients. Liao and Qin [20] indicated that gender is significantly associated with Stoma-QoL scores, although it is not strong enough to be considered a predictor. This relationship appears to be especially prominent regarding self-care agency, where there is generally a marked difference between males and females in concerns about appearance. Additionally, gender factors have a strong influence on scores in the psychological domain [23, 28]. Similarly, in a study conducted in Germany, females showed lower scores in the physical and mental domains [25].
In addition to age, marital status was also found to have a strong correlation with several dimensions of QoL measurement. As mentioned in a Brazilian study, marital status is related to the social psychological domain. Marriage positively affects the emotional state limitations aspect of QoL. In contrast, single individuals demonstrate better overall health and physical well-being in their QoL assessments [15]. Another study in Brazil indicates that married patients have good QoL, especially in the physical and psychological domains [28, 19]. Similar to having a sexual partner, Pereira et al. [22] found that this factor is associated with the physical and social domains. In Poland, individuals in relationships reported lower scores in general health and physical well-being compared to those who are single or not in a relationship. Conversely, those in relationships have higher scores in the domain related to limitations caused by emotional states [29].
Regarding work status, it appears that patients with stomas who are still actively working have higher QoL scores compared to those who are not working, especially in the physical domain [19]. In China, having employment positively influences QoL scores related to concerns about the stoma, sleep, sexuality, and body image [21]. It is quite interesting that after discussing the work status factor, we continue with the patient or family income factor. In Brazil, patients living in families with low income experience a negative impact on QoL, particularly in the psychological domain [23]. In Poland, income levels affect various aspects of QoL, including overall health, vitality, social interaction, mental well-being, and both physical and mental health, as measured by the SF-36 assessment [29].
Another factor mentioned in some of the included studies is educational level. Silva et al. [25] report a strong relationship between education level and the psychological and physical domains. Meanwhile, a study in Poland reported that a patient’s education level affects physical functioning, pain perception, vitality, social functioning, and mental health [29]. This is likely related to the patient’s knowledge or ability to understand the situation at hand. One study reported that knowledge level is strongly associated with QoL, especially in the sexuality and body image domain of the Stoma-QoL [20].
Another factor that falls under this personal category is nutrition. Vitamin B12 impacts the mental and emotional dimensions of the SF-36. In addition, iron deficiency contributes to QoL, especially in the physical domain [25].
Ostomy factors
Some of the factors included in this section are the type of stoma, the nature of the stoma, the time since surgery, the indication for ostomy, leakage, clothing changes, complications, comorbidities, adaptation to the stoma, stoma care, pain and discomfort, and hernia conditions. We will elaborate in detail on how each of these potential factors relates to the QoL domains.
Comparing ileostomy and colostomy, Diniz et al. [15] reported that ileostomy is the type of stoma that shows higher scores in the physical domain. Meanwhile, a study in Sri Lanka reported that ileostomy is better for personal hygiene than colostomy, but for sexual activity, ileostomy shows lower scores [26]. In another study conducted in Ethiopia with most participants being patients with colostomy, colostomy is strongly associated with the physical and psychosocial domains [32]. In addition to the type of ostomy, other differences also arise in the nature of the stoma (permanent or temporary). A permanent stoma is strongly associated with the psychosocial and social domains, where scores in these domains show a high mean [15, 27]. Meanwhile, another study states that temporary stomas exhibit low QoL scores across all domains [21]. Time since surgery, or the difference between shorter and longer periods after ostomy, was also analyzed in several studies, which we included as one of the factors contributing to QoL. Overall satisfaction is related to stoma duration, where a longer stoma duration correlates with higher satisfaction scores on the Stoma-QoL assessment [20]. A similar finding is also observed in a study that assessed QoL using the SF-36 [29].
Regarding the indication for ostomy, metastasis from colorectal cancer is associated with the social domain in QoL measurements using WHOQOL-BREF [23]. A different study revealed that individuals with colorectal cancer reported poorer scores in the physical domain compared to those with ulcerative colitis and Crohn’s disease. Meanwhile, those with Crohn’s disease have lower scores for general and mental health [25]. In Ethiopia, the most common indication for ostomy is malignancy, which also shows a correlation with the COH-QOL-Ostomy assessment, particularly in the social domain [32].
Other factors analyzed include the condition of the peristomal skin. Patients who do not experience irritation in the stoma area show better COH-QOL scores compared to those who do [16]. A study in Brazil examined the complications that occurred in patients with stomas, identifying issues, such as peristomal dermatitis, retraction, and prolapse. These complications significantly impact QoL, particularly in the domains of spiritual well-being, psychological well-being, and physical well-being [15].
Discussion
The present review aimed to evaluate factors related to the QoL of individuals with an intestinal stoma and how those factors influence their perceived QoL. By thoroughly reviewing the literature on the factors affecting the QoL for individuals with a stoma, we gain deeper insights into this issue. This study identified all potential influences on QoL for stoma patients, demonstrating that their QoL is shaped by a range of factors rather than a single aspect of their personal lives. Systematically summarizing these factors allows us to build a detailed understanding based on previous research. This approach not only highlights the current level of awareness regarding QoL factors in stoma research but also serves as a comprehensive resource for developing interventions aimed at enhancing the QoL for stoma patients.
The study’s findings indicated that the physical and psychological dimensions are consistently and strongly related to the factors analyzed. In contrast, most personal factors were strongly associated with all dimensions of QoL. These results provide clear guidance for improving QoL in individuals with stomas. For instance, while some studies suggest that QoL improves with age, there are inconsistencies regarding this parameter, and overall, socio-demographic factors did not significantly correlate with QoL in several studies reviewed [17, 21, 23, 25]. Another study found that age and gender, when adjusted for family income and body image, significantly relate to QoL. Specifically, older age positively impacts QoL for individuals with a stoma, and males tend to have a more positive QoL than females. Women exhibit notably higher levels of anxiety, whereas men report lower scores in social functioning and on various symptom scales, including fatigue, shortness of breath, and financial difficulties [31]. In summary, our research indicated that the QoL for individuals with a stoma is influenced by more than just socio-demographic factors, like age and gender. This finding prompts a reconsideration of the tools required to fully understand how these parameters interact with QoL.
Additionally, this review explored numerous significant factors that impact the QoL for individuals with stomas. Caregivers often overlook some of these factors when creating care plans [32]. Self-care is crucial for individuals with an ostomy, but it can be challenging to implement. In such situations, caregivers play a vital role in encouraging and supporting self-care practices [33]. Thus, the insights from this review can be valuable for effective care planning. However, the influence of these factors on the QoL for older adults with dementia varies. Therefore, focusing on specific contexts, such as personal or ostomy-related factors, can help pinpoint the most affected areas and enable targeted interventions. By doing so, the QoL for people from different backgrounds can be maintained or enhanced efficiently with the right resources.
This study identified that the main factors influencing the QoL of individuals with a stoma fell into two personal and ostomy-related categories. Ostomy factors, in particular, exhibited the strongest relationship with QoL across all dimensions. Personal factors, on the other hand, played a supportive role in either positively or negatively affecting QoL. For example, irritation and poor maintenance of the skin around the stoma can significantly lower scores in the physical domain, while individuals who are married or have a partner tend not to experience these issues [16]. Leakage is linked to both the occurrence and severity of complications involving the skin around the stoma, such as peristomal skin irritation [11]. Consequently, a previous study recommends the urgent implementation of a partnership-based program for stoma care to enhance caregivers’ knowledge and practices, thereby improving patient health status [34]. Furthermore, the length of time an individual has had a stoma plays a crucial role; those who have lived with a stoma for over a year generally report higher QoL scores. This implies that QoL tends to improve as patients adapt to their condition over time.
Having a stoma can increase the likelihood of various complications, and the location of the stoma is a significant factor influencing the risk of these complications [35]. Peristomal complications are common, affecting nearly 80% of patients who experience issues after surgery. Those who develop these complications face significantly higher costs for postoperative care and endure considerable discomfort, distress, and negative impacts on their health-related quality of life (HRQOL) [36]. The majority of peristomal complications emerge within the first month following surgery [37]. The most common stoma-related issues are parastomal hernia, stoma prolapse, and mucocutaneous separation. With the exception of mucocutaneous separation, stoma complications generally develop later than peristomal complications [38].
Patients who undergo colostomy surgery often face a range of intense and distressing emotions [39]. The significant changes brought about by the colostomy can severely impact personal and social lives [40]. Stoma patients often experience a sense of uncertainty and no longer feel the same trust in their bodies as they did before. They work to regain control of their lives based on their own abilities and circumstances, with assistance from healthcare professionals. Engaging with others who face similar challenges and sharing experiences in areas, such as body image, sexuality, and social activities can help these patients adjust to their new life with a stoma [41]. Gaining independence is crucial for enhancing their QoL [42]. Effective adaptation to life following a colostomy depends on various factors, including the acceptance of a partner, the opportunity to return to a supportive job, and support from family, friends, and healthcare providers [43, 44]. The patient’s overall health, existing comorbidities, and recovery progress also play key roles in their adaptation. The role of healthcare services, especially the educational efforts of nurses, is crucial for facilitating a seamless transition through all stages of the condition, ultimately fostering self-management and independence [45].
There are several limitations to consider. Firstly, this review was exclusively based on four PubMed, Scopus, Web of Science, and ProQuest databases, and does not include gray literature. Additionally, some authors may have provided extra details or clarifications regarding their findings or methodologies, including sample selection, characteristics, and study settings. However, we did not reach out to these authors for such information, which may have resulted in gaps in our data.
Another limitation is the diversity of assessment tools used across the studies reviewed. QoL is a complex and somewhat ambiguous concept, and the research utilized eleven different instruments to measure it. Each of these tools has unique indicators and may capture different aspects of QoL for individuals with stomas. Consequently, some contradictory findings among the reviewed papers have emerged, warranting careful consideration. The lack of a standardized measurement instrument also complicates the comparison of results across studies, diminishing the significance of such comparisons. Nonetheless, the majority of the studies reviewed utilized reliable and valid measurement tools, which enhances the credibility of the findings to some extent.
This review offers valuable insights for nurses and caregivers in digestive health settings seeking to enhance the QoL for individuals with stomas. It highlights the importance of addressing symptoms of depression and anxiety as a priority. Implementing psychosocial interventions could be one approach; however, further exploration into the relationship between QoL and these symptoms is recommended. Specifically, longitudinal studies are necessary to identify factors linked to changes in QoL over time. Such data are essential for creating effective community-based interventions to improve the QoL for stoma patients.
Conclusion
Demographic, physical, psychological, social, and spiritual factors affect the quality of life for individuals with a stoma.
Acknowledgments: We extend our sincere gratitude to the Dean of the Faculty of Medicine at Halu Oleo University for his invaluable support in providing access to the databases essential for this study. We also wish to acknowledge the librarians of the Faculty of Medicine for their assistance in facilitating access to these resources.
Ethical Permissions: Not applicable.
Conflicts of Interests: The authors reported no conflicts of intersts.
Authors' Contribution: La Rangki R (First Author), Introduction Writer/Main Researcher/Discussion Writer/Statistical Analyst (50%); Fithria F (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (50%)
Funding/Support: None declared.
Quality of life (QoL) encompasses a person’s overall contentment with life and is influenced by a range of factors, including health, cultural norms, social circumstances, and psychological well-being. The introduction of a stoma appears to impact QoL, as it may disrupt bodily functions and self-image, leading to potential physical, emotional, and social challenges [1, 2].
An intestinal stoma is surgically created to connect the intestine with the outside environment, compensating for the function of a compromised organ, and is performed for various reasons. Research involving 216 individuals with intestinal stomas revealed that the predominant reason for creating a stoma is colorectal cancer, accounting for 40.7% of cases [3, 4].
Individuals with stomas encounter a range of difficulties, including recognizing the significance of their surgery and adapting to the physical changes it brings, which affect their psychological well-being and social interactions. Additionally, concerns about potential leakage can provoke anxiety, particularly in social settings [1]. Individuals with stomas, especially those struggling to adapt, often experience biopsychosocial challenges that can negatively impact their QoL. Research conducted on Chinese individuals with stomas reported the majority (87.0%) have lived with their stoma for up to three months with a low average QoL score, indicating significant adverse effects on their well-being due to the stoma. Individuals with stomas experience changes that impact their body image and self-esteem, which in turn affect their QoL. These individuals need to develop personal coping strategies influenced by various factors, including health education and attitudes toward personal care. Therefore, it is crucial for support networks, especially healthcare providers, to gain a comprehensive understanding of each person, taking into account their individual, social, economic, and cultural contexts to deliver holistic care [5, 6].
QoL focuses on the general well-being of individuals or groups, prioritizing health and happiness over financial status [7]. It encompasses how patients perceive their own health across physical, mental, social, and spiritual dimensions. Research into the well-being of ostomy patients should consider these various aspects: physical health, psychological condition, social engagement, and spiritual life. Typically, patients experience a shift in their QoL after ostomy surgery, moving from initial negative impacts to improved outcomes as they adapt over time [8]. Various factors affect the QoL of ostomy patients, including challenges in managing the ostomy, access to healthcare coverage, and the financial burden associated with procuring necessary supplies [5, 9]. Complications related to ostomy care, exacerbated by the absence of specialized nursing support, are linked to lower QoL scores [9]. Such complications often impose significant physical and psychosocial limitations on individuals and their families [10]. Emotional stress, physical discomfort, and doubts are identified as key contributors to these negative consequences following ostomy surgery. Additionally, inadequate family and social support can diminish patients’ self-identity and self-esteem, compounding these negative effects [6]. While the precise prevalence of stomal and peristomal complications remains unclear, it is estimated that a substantial majority of ostomy patients (up to 70%) experience emotional, psychological, and financial hardships that impact their QoL [11].
The present review aimed to evaluate factors related to the QoL of adults with an intestinal stoma and how those factors influence their perceived QoL.
Information and Methods
Protocol
The present review complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, 2020 version [12].
Search strategy
We explored various databases, including PubMed, Scopus, Web of Science, and ProQuest. Searches were conducted using individual and combined terms, such as “stoma,” “colostomy,” “ileostomy,” and “quality of life,” along with Boolean operators, like “AND” and “OR” to link these keywords. The search was limited to English-language articles, and we adjusted the filters to enhance the relevance and accuracy of the results.
Inclusion criteria
This review encompassed all research examining risk factors for diabetes mellitus in children and adolescents. There was no restriction on the search timeframe to ensure a comprehensive compilation of relevant studies. However, studies published in conference proceedings, reviews, meta-analyses, commentaries, book chapters, reports, case studies, and letters to the editor were excluded from consideration.
Selection process
Two authors independently and separately screened the titles and abstracts of the identified studies. In cases of conflicting opinions between the two screening authors, the first author made the final decision. This rapid screening involved assessing the titles, objectives, and conclusions of the relevant studies. We conducted a deeper review of specific studies by examining their main texts to extract any additional necessary information.
Study quality
We assessed each quantitative study based on five criteria, including study details, sample characteristics, measurement methods, data analysis, and result interpretation. This evaluation checklist uses critical appraisal tools [2], specifically designed for systematic reviews. The quality of studies was assessed based on five key criteria, including clear explanations of the research objectives, data collection methods, and participant details, well-defined sampling methods and sufficient sample size (N≥200), the use of valid and reliable measurement tools, appropriate data analysis techniques, and consistency between the discussion, conclusions, and results. Studies meeting all five criteria are considered high quality. Those meeting at least three of the criteria are deemed moderate in quality, while studies fulfilling only one or two criteria are classified as low quality.
Risk of bias assessment
We utilized the Risk of Bias in Non-randomized Studies-Exposure Studies (ROBINS-E) tool to identify potential biases in each study [13]. This tool evaluates seven domains to gauge both internal and external validity. The outcomes are categorized as low, some concerns, high, or very high based on the assessment. The final risk of bias evaluations was reviewed and endorsed by all authors, incorporating feedback from external reviewers.
Data extraction and synthesis
Two authors collaborated in the crucial information extraction process. In cases where there were differing opinions regarding the extracted data, they were reconciled through consensus. The extraction criteria included the first author and publication year, sample size, age, mean time since surgery, instruments, factors analyzed, and main findings.
Findings
The initial database search retrieved 899 articles. After removing 707 duplicates and ineligible articles not relevant to the review’s theme, 192 articles remained for screening. During the eligibility assessment, 28 studies were evaluated, and nine articles were excluded for various reasons. Ultimately, only 19 studies met the criteria and will proceed to the next stage for extraction and analysis (Figure 1 and Table 1).
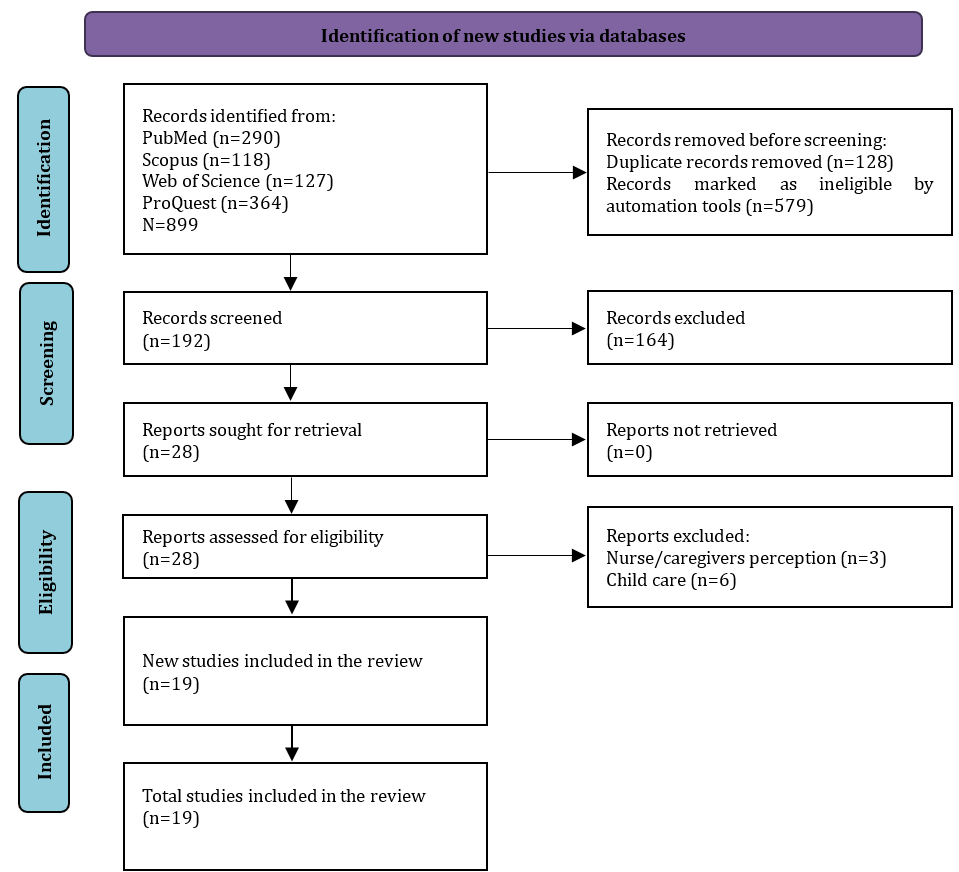
Figure 1. PRISMA flow diagram for literature search
Table 1. Data extraction of the included studieSs
Overview of the eligible studies
We identified 19 studies that addressed factors related to the QoL of individuals with intestinal stomas, with most studies conducted in European populations across five different countries, including Poland (n=2) [4, 29], and one study each from Austria [17], the Netherlands [16], Sweden [3], and Germany [25]. Other studies came from the Americas, including Brazil (n=5) [8, 15, 23, 27, 30] and the US [14]. In Asia, we found the most studies from China, with three studies [20, 21-31], followed by one study each from Australia [18] and Sri Lanka [26]. On the African continent, there are two studies from two different countries, including Uganda [28] and Ethiopia [32].
The total number of patients participating in the study was 8,860 individuals living with an intestinal stoma, with a mean age of 56.5 years. The mean time since ostomy also showed high variation, ranging from two months to sixty months. The tools used included Stoma-QoL, COH-QOL-OQ, Modified FI-QoL, QoL-O, WHO-QOL-bref, EORTC QLQ-C30, EORTC QLQ-CR38, SF-36, CQ, FQLS, GIQLI, CGQLI, PHQ-9, GAD-7, and SSRS.
Results of the study quality assessment
The quality assessment results indicated that, overall, the studies included fell into the moderate to good quality range (Table 2).
Table 2. Summary of quality appraisal
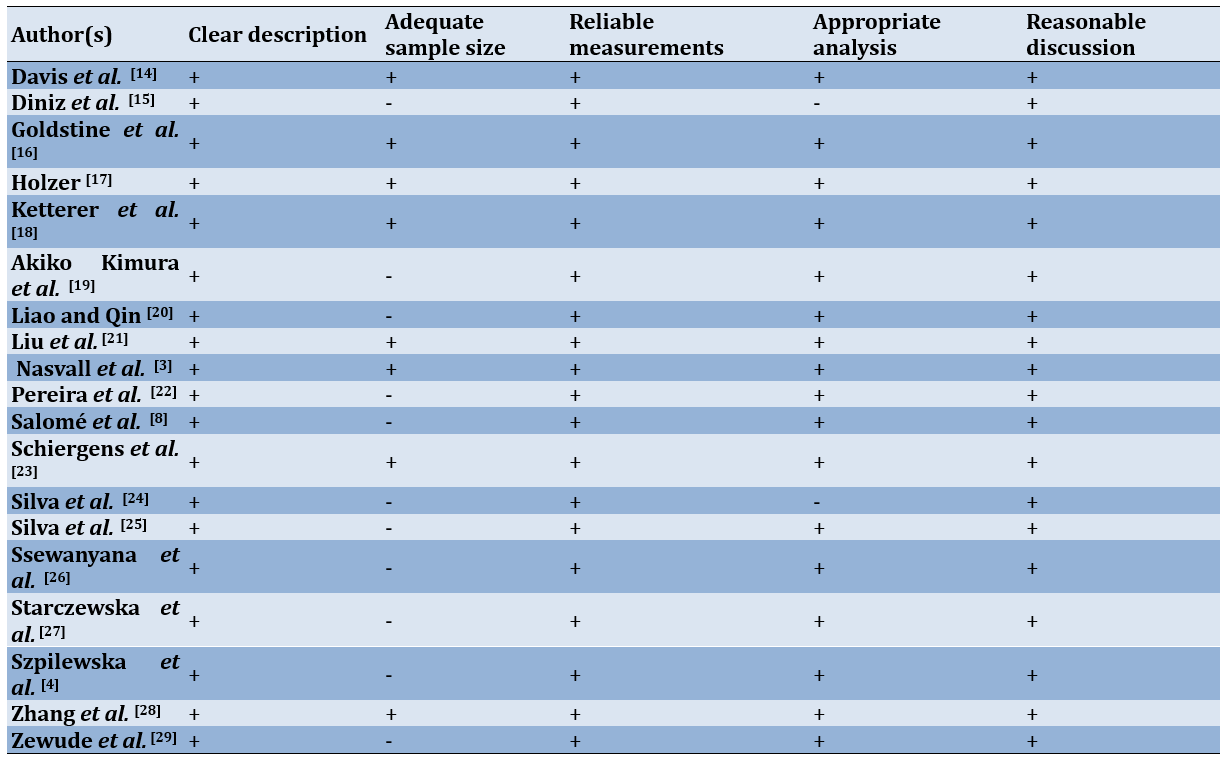
Results of risk of bias assessment
We assessed risk of bias in the studies, and found its seven domains (Figure 2).
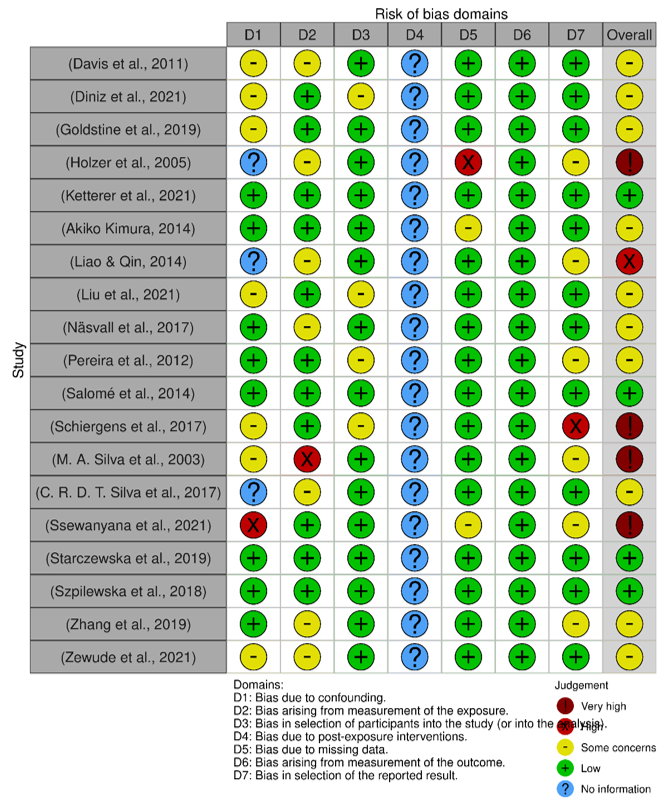
Figure 2. Result of risk of bias assessment.
Factors related to QoL
Of the 19 studies descriptively analyzed, in general, two categories of factors (personal and ostomy factors) were strongly associated with one or more of the QoL domains. Among the studies we collected, two studies [4, 31] did not specifically mention the correlation between the identified factors and the domains of QoL. Generally, the QoL domains mentioned in the tools used in the studies included physical, psychological, social, and spiritual aspects. The quality of the studies can vary depending on the specific instrument used for assessment. For instance, different tools cover a range of domains. Stoma-QoL addresses family and social relationships and the impact of the ostomy bag, FIQL focuses on lifestyle, coping, depression/self-perception, and embarrassment, WHOQOL-BREF includes the environment, EORTC QLQ-C30 assesses global health, functioning scales (physical, emotional, cognitive, and social), and specific items (dyspnea, insomnia, appetite loss, bowel function, and financial impact), SF-36 evaluates physical function, role limitations, body pain, general health, vitality, social functioning, emotional role, and mental health, CQ considers daily life, physical activity, profession, sexuality, pain, stoma protrusion, urinary continence, and daily life limitations, FQLS reviews material and physical well-being, relationships, social activities, community involvement, personal development, and recreation, GIQLI examines gastrointestinal symptoms, emotional status, physical and social functioning, and distress, CGQLI looks at current QoL, health quality, and energy levels, OAI-23 (Chinese version) assesses persistent worry, life attitude, and acceptance, and SSRS measures subjective support, objective support, and support utilization.
In a study conducted in China, researchers explored how psychosocial adaptation relates to QoL and identified several factors strongly linked to all QoL dimensions, including education level, method of medical payment, residence area, peristomal complications, regularity of defecation, occurrence of leaks, self-care capability, patient-provider communication, and stoma care knowledge and skills [31]. In contrast, a study in the US found that QoL is influenced by factors, such as leakage from the ostomy appliance, peristomal skin condition, age, gender, and time elapsed since surgery [14]. Additionally, factors, like peristomal skin irritation, leaks affecting the peristomal skin, surgical planning [16], geographic location, education [17], employment status, clothing changes, sexual activity, age, depression, and stoma location [8, 18] also impact QoL. In the following sections, we described the link between each factor and the domains of the QoL instruments analyzed in the included studies.
Personal factors
Personal factors analyzed in eligible studies included socio-demographics (age, gender, marital status, geographic origin, employment status, income, and education level), sexual activity, expectations, depression, knowledge, nutrition, and daily activities.
Several studies have mentioned that age is strongly associated with QoL. With increasing age, QoL scores are better compared to those of younger individuals [16, 23, 29]. Specifically, Pereira et al. noted that age correlates with higher scores in each domain of the WHOQOL-BREF, including physical, psychological, social, and environmental domains [22]. In another study, it was mentioned that SF-36 scores increase with age, particularly in relation to the domains of physical functioning, role limitations, pain perception, general health, social functioning, and mental health [29]. Gender also contributes to the QoL of patients. Liao and Qin [20] indicated that gender is significantly associated with Stoma-QoL scores, although it is not strong enough to be considered a predictor. This relationship appears to be especially prominent regarding self-care agency, where there is generally a marked difference between males and females in concerns about appearance. Additionally, gender factors have a strong influence on scores in the psychological domain [23, 28]. Similarly, in a study conducted in Germany, females showed lower scores in the physical and mental domains [25].
In addition to age, marital status was also found to have a strong correlation with several dimensions of QoL measurement. As mentioned in a Brazilian study, marital status is related to the social psychological domain. Marriage positively affects the emotional state limitations aspect of QoL. In contrast, single individuals demonstrate better overall health and physical well-being in their QoL assessments [15]. Another study in Brazil indicates that married patients have good QoL, especially in the physical and psychological domains [28, 19]. Similar to having a sexual partner, Pereira et al. [22] found that this factor is associated with the physical and social domains. In Poland, individuals in relationships reported lower scores in general health and physical well-being compared to those who are single or not in a relationship. Conversely, those in relationships have higher scores in the domain related to limitations caused by emotional states [29].
Regarding work status, it appears that patients with stomas who are still actively working have higher QoL scores compared to those who are not working, especially in the physical domain [19]. In China, having employment positively influences QoL scores related to concerns about the stoma, sleep, sexuality, and body image [21]. It is quite interesting that after discussing the work status factor, we continue with the patient or family income factor. In Brazil, patients living in families with low income experience a negative impact on QoL, particularly in the psychological domain [23]. In Poland, income levels affect various aspects of QoL, including overall health, vitality, social interaction, mental well-being, and both physical and mental health, as measured by the SF-36 assessment [29].
Another factor mentioned in some of the included studies is educational level. Silva et al. [25] report a strong relationship between education level and the psychological and physical domains. Meanwhile, a study in Poland reported that a patient’s education level affects physical functioning, pain perception, vitality, social functioning, and mental health [29]. This is likely related to the patient’s knowledge or ability to understand the situation at hand. One study reported that knowledge level is strongly associated with QoL, especially in the sexuality and body image domain of the Stoma-QoL [20].
Another factor that falls under this personal category is nutrition. Vitamin B12 impacts the mental and emotional dimensions of the SF-36. In addition, iron deficiency contributes to QoL, especially in the physical domain [25].
Ostomy factors
Some of the factors included in this section are the type of stoma, the nature of the stoma, the time since surgery, the indication for ostomy, leakage, clothing changes, complications, comorbidities, adaptation to the stoma, stoma care, pain and discomfort, and hernia conditions. We will elaborate in detail on how each of these potential factors relates to the QoL domains.
Comparing ileostomy and colostomy, Diniz et al. [15] reported that ileostomy is the type of stoma that shows higher scores in the physical domain. Meanwhile, a study in Sri Lanka reported that ileostomy is better for personal hygiene than colostomy, but for sexual activity, ileostomy shows lower scores [26]. In another study conducted in Ethiopia with most participants being patients with colostomy, colostomy is strongly associated with the physical and psychosocial domains [32]. In addition to the type of ostomy, other differences also arise in the nature of the stoma (permanent or temporary). A permanent stoma is strongly associated with the psychosocial and social domains, where scores in these domains show a high mean [15, 27]. Meanwhile, another study states that temporary stomas exhibit low QoL scores across all domains [21]. Time since surgery, or the difference between shorter and longer periods after ostomy, was also analyzed in several studies, which we included as one of the factors contributing to QoL. Overall satisfaction is related to stoma duration, where a longer stoma duration correlates with higher satisfaction scores on the Stoma-QoL assessment [20]. A similar finding is also observed in a study that assessed QoL using the SF-36 [29].
Regarding the indication for ostomy, metastasis from colorectal cancer is associated with the social domain in QoL measurements using WHOQOL-BREF [23]. A different study revealed that individuals with colorectal cancer reported poorer scores in the physical domain compared to those with ulcerative colitis and Crohn’s disease. Meanwhile, those with Crohn’s disease have lower scores for general and mental health [25]. In Ethiopia, the most common indication for ostomy is malignancy, which also shows a correlation with the COH-QOL-Ostomy assessment, particularly in the social domain [32].
Other factors analyzed include the condition of the peristomal skin. Patients who do not experience irritation in the stoma area show better COH-QOL scores compared to those who do [16]. A study in Brazil examined the complications that occurred in patients with stomas, identifying issues, such as peristomal dermatitis, retraction, and prolapse. These complications significantly impact QoL, particularly in the domains of spiritual well-being, psychological well-being, and physical well-being [15].
Discussion
The present review aimed to evaluate factors related to the QoL of individuals with an intestinal stoma and how those factors influence their perceived QoL. By thoroughly reviewing the literature on the factors affecting the QoL for individuals with a stoma, we gain deeper insights into this issue. This study identified all potential influences on QoL for stoma patients, demonstrating that their QoL is shaped by a range of factors rather than a single aspect of their personal lives. Systematically summarizing these factors allows us to build a detailed understanding based on previous research. This approach not only highlights the current level of awareness regarding QoL factors in stoma research but also serves as a comprehensive resource for developing interventions aimed at enhancing the QoL for stoma patients.
The study’s findings indicated that the physical and psychological dimensions are consistently and strongly related to the factors analyzed. In contrast, most personal factors were strongly associated with all dimensions of QoL. These results provide clear guidance for improving QoL in individuals with stomas. For instance, while some studies suggest that QoL improves with age, there are inconsistencies regarding this parameter, and overall, socio-demographic factors did not significantly correlate with QoL in several studies reviewed [17, 21, 23, 25]. Another study found that age and gender, when adjusted for family income and body image, significantly relate to QoL. Specifically, older age positively impacts QoL for individuals with a stoma, and males tend to have a more positive QoL than females. Women exhibit notably higher levels of anxiety, whereas men report lower scores in social functioning and on various symptom scales, including fatigue, shortness of breath, and financial difficulties [31]. In summary, our research indicated that the QoL for individuals with a stoma is influenced by more than just socio-demographic factors, like age and gender. This finding prompts a reconsideration of the tools required to fully understand how these parameters interact with QoL.
Additionally, this review explored numerous significant factors that impact the QoL for individuals with stomas. Caregivers often overlook some of these factors when creating care plans [32]. Self-care is crucial for individuals with an ostomy, but it can be challenging to implement. In such situations, caregivers play a vital role in encouraging and supporting self-care practices [33]. Thus, the insights from this review can be valuable for effective care planning. However, the influence of these factors on the QoL for older adults with dementia varies. Therefore, focusing on specific contexts, such as personal or ostomy-related factors, can help pinpoint the most affected areas and enable targeted interventions. By doing so, the QoL for people from different backgrounds can be maintained or enhanced efficiently with the right resources.
This study identified that the main factors influencing the QoL of individuals with a stoma fell into two personal and ostomy-related categories. Ostomy factors, in particular, exhibited the strongest relationship with QoL across all dimensions. Personal factors, on the other hand, played a supportive role in either positively or negatively affecting QoL. For example, irritation and poor maintenance of the skin around the stoma can significantly lower scores in the physical domain, while individuals who are married or have a partner tend not to experience these issues [16]. Leakage is linked to both the occurrence and severity of complications involving the skin around the stoma, such as peristomal skin irritation [11]. Consequently, a previous study recommends the urgent implementation of a partnership-based program for stoma care to enhance caregivers’ knowledge and practices, thereby improving patient health status [34]. Furthermore, the length of time an individual has had a stoma plays a crucial role; those who have lived with a stoma for over a year generally report higher QoL scores. This implies that QoL tends to improve as patients adapt to their condition over time.
Having a stoma can increase the likelihood of various complications, and the location of the stoma is a significant factor influencing the risk of these complications [35]. Peristomal complications are common, affecting nearly 80% of patients who experience issues after surgery. Those who develop these complications face significantly higher costs for postoperative care and endure considerable discomfort, distress, and negative impacts on their health-related quality of life (HRQOL) [36]. The majority of peristomal complications emerge within the first month following surgery [37]. The most common stoma-related issues are parastomal hernia, stoma prolapse, and mucocutaneous separation. With the exception of mucocutaneous separation, stoma complications generally develop later than peristomal complications [38].
Patients who undergo colostomy surgery often face a range of intense and distressing emotions [39]. The significant changes brought about by the colostomy can severely impact personal and social lives [40]. Stoma patients often experience a sense of uncertainty and no longer feel the same trust in their bodies as they did before. They work to regain control of their lives based on their own abilities and circumstances, with assistance from healthcare professionals. Engaging with others who face similar challenges and sharing experiences in areas, such as body image, sexuality, and social activities can help these patients adjust to their new life with a stoma [41]. Gaining independence is crucial for enhancing their QoL [42]. Effective adaptation to life following a colostomy depends on various factors, including the acceptance of a partner, the opportunity to return to a supportive job, and support from family, friends, and healthcare providers [43, 44]. The patient’s overall health, existing comorbidities, and recovery progress also play key roles in their adaptation. The role of healthcare services, especially the educational efforts of nurses, is crucial for facilitating a seamless transition through all stages of the condition, ultimately fostering self-management and independence [45].
There are several limitations to consider. Firstly, this review was exclusively based on four PubMed, Scopus, Web of Science, and ProQuest databases, and does not include gray literature. Additionally, some authors may have provided extra details or clarifications regarding their findings or methodologies, including sample selection, characteristics, and study settings. However, we did not reach out to these authors for such information, which may have resulted in gaps in our data.
Another limitation is the diversity of assessment tools used across the studies reviewed. QoL is a complex and somewhat ambiguous concept, and the research utilized eleven different instruments to measure it. Each of these tools has unique indicators and may capture different aspects of QoL for individuals with stomas. Consequently, some contradictory findings among the reviewed papers have emerged, warranting careful consideration. The lack of a standardized measurement instrument also complicates the comparison of results across studies, diminishing the significance of such comparisons. Nonetheless, the majority of the studies reviewed utilized reliable and valid measurement tools, which enhances the credibility of the findings to some extent.
This review offers valuable insights for nurses and caregivers in digestive health settings seeking to enhance the QoL for individuals with stomas. It highlights the importance of addressing symptoms of depression and anxiety as a priority. Implementing psychosocial interventions could be one approach; however, further exploration into the relationship between QoL and these symptoms is recommended. Specifically, longitudinal studies are necessary to identify factors linked to changes in QoL over time. Such data are essential for creating effective community-based interventions to improve the QoL for stoma patients.
Conclusion
Demographic, physical, psychological, social, and spiritual factors affect the quality of life for individuals with a stoma.
Acknowledgments: We extend our sincere gratitude to the Dean of the Faculty of Medicine at Halu Oleo University for his invaluable support in providing access to the databases essential for this study. We also wish to acknowledge the librarians of the Faculty of Medicine for their assistance in facilitating access to these resources.
Ethical Permissions: Not applicable.
Conflicts of Interests: The authors reported no conflicts of intersts.
Authors' Contribution: La Rangki R (First Author), Introduction Writer/Main Researcher/Discussion Writer/Statistical Analyst (50%); Fithria F (Second Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer (50%)
Funding/Support: None declared.
Article Type: Systematic Review |
Subject:
Quality of Life
Received: 2024/07/26 | Accepted: 2024/09/2 | Published: 2024/09/28
Received: 2024/07/26 | Accepted: 2024/09/2 | Published: 2024/09/28
References
1. Baxter NN, Novotny PJ, Jacobson T, Maidl LJ, Sloan J, Young-Fadok TM. A stoma quality of life scale. Dis Colon Rectum. 2006;49(2):205-12. [Link] [DOI:10.1007/s10350-005-0275-6]
2. Jing W, Willis R, Feng Z. Factors influencing quality of life of elderly people with dementia and care implications: A systematic review. Arch Gerontol Geriatr. 2016;66:23-41. [Link] [DOI:10.1016/j.archger.2016.04.009]
3. Nasvall P, Dahlstrand U, Lowenmark T, Rutegard J, Gunnarsson U, Strigard K. Quality of life in patients with a permanent stoma after rectal cancer surgery. Qual Life Res. 2017;26(1):55-64. [Link] [DOI:10.1007/s11136-016-1367-6]
4. Szpilewska K, Juzwiszyn J, Bolanowska Z, Bolanowska Z, Milan M, Chabowski M, et al. Acceptance of disease and the quality of life in patients with enteric stoma. Pol J Surg. 2018;90(1):13-7. [Link] [DOI:10.5604/01.3001.0011.5954]
5. Coons SJ, Chongpison Y, Wendel CS, Grant M, Krouse RS. Overall quality of life and difficulty paying for ostomy supplies in the Veterans Affairs ostomy health-related quality of life study: An exploratory analysis. Med Care. 2007;45(9):891-5. [Link] [DOI:10.1097/MLR.0b013e318074ce9b]
6. Cetolin SF, Beltrame V, Cetolin SK, Presta AA. Social and family dynamic with patients with definitive intestinal ostomy. Arquivos Brasileiros de Cirurgia Digestiva. 2013;26(3):170-2. [Link] [DOI:10.1590/S0102-67202013000300003]
7. Post M. Definitions of quality of life: What has happened and how to move on. Top Spinal Cord Inj Rehabil. 2014;20(3):167-80. [Link] [DOI:10.1310/sci2003-167]
8. Salomé GM, De Almeida SA, Silveira MM. Quality of life and self-esteem of patients with intestinal stoma. J Coloproctol. 2014;34(4):231-9. [Link] [DOI:10.1016/j.jcol.2014.05.009]
9. Pittman J, Rawl SM, Schmidt CM, Grant M, Ko CY, Wendel C, et al. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. J Wound Ostomy Continence Nurs. 2008;35(5):493-503. [Link] [DOI:10.1097/01.WON.0000335961.68113.cb]
10. Davidson F. Quality of life, wellbeing and care needs of Irish ostomates. Br J Nurs. 2016;25(17):S4-12. [Link] [DOI:10.12968/bjon.2016.25.17.S4]
11. Maydick-Youngberg D. A descriptive study to explore the effect of peristomal skin complications on quality of life of adults with a permanent ostomy. Ostomy Wound Manag. 2017;63(5):10-23. [Link]
12. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [Link] [DOI:10.1136/bmj.n71]
13. Higgins J, Morgan R, Rooney A, Taylor K, Thayer K, Silva R, et al. Risk of bias in non-randomized studies-of exposure (ROBINS-E): Launch version. Risk of Bias. 2022. [Link]
14. Davis JS, Svavarsdóttir MH, Pudło M, Arena R, Lee Y, Jensen MK. Factors impairing quality of life for people with an ostomy. Gastrointest Nurs. 2011;9(Suppl 2). [Link] [DOI:10.12968/gasn.2011.9.Sup2.14]
15. Diniz IV, Costa IKF, Nascimento JA, Da Silva IP, De Mendonça AEO, Soares MJGO. Factors associated to quality of life in people with intestinal stomas. Revista da Escola de Enfermagem. 2021;55:e20200377. [Link] [DOI:10.1590/1980-220x-reeusp-2020-0377]
16. Goldstine J, Van Hees R, Van De Vorst D, Skountrianos G, Nichols T. Factors influencing health-related quality of life of those in the Netherlands living with an ostomy. Br J Nurs. 2019;28(22):S10-7. [Link] [DOI:10.12968/bjon.2019.28.22.S10]
17. Holzer B, Matzel K, Schiedeck T, Christiansen J, Christensen P, Rius J, et al. Do geographic and educational factors influence the quality of life in rectal cancer patients with a permanent colostomy?. Dis Colon Rectum. 2005;48(12):2209-16. [Link] [DOI:10.1007/s10350-005-0194-6]
18. Ketterer SN, Leach MJ, Fraser C. Factors associated with quality of life among people living with a stoma in nonmetropolitan areas. Nurs Res. 2021;70(4):281-8. [Link] [DOI:10.1097/NNR.0000000000000511]
19. Akiko Kimura C, Kamada I, Costa De Jesus CA, Guilhem D. Quality of life of colorectal cancer patients with intestinal stomas. J Carcinog Mutagen. 2014;S10:007. [Link] [DOI:10.4172/2157-2518.S10-007]
20. Liao C, Qin Y. Factors associated with stoma quality of life among stoma patients. Int J Nurs Sci. 2014;1(2):196-201. [Link] [DOI:10.1016/j.ijnss.2014.05.007]
21. Liu H, Zhu X, Yu J, He P, Shen B, Tang X, et al. The quality of life of patients with colorectal cancer and a stoma in China: A quantitative cross-sectional study. Adv Skin Wound Care. 2021;34(6):302-7. [Link] [DOI:10.1097/01.ASW.0000744348.32773.b9]
22. Pereira APDS, Cesarino CB, Ismael Martins MR, Pinto MH, Netinho JG. Associations among socio-demographic and clinical factors and the quality of life of ostomized patients. Revista Latino-Americana de Enfermagem. 2012;20(1):93-100. [Link] [DOI:10.1590/S0104-11692012000100013]
23. Schiergens TS, Hoffmann V, Schobel TN, Englert GH, Kreis ME, Thasler WE, et al. Long-term quality of life of patients with permanent end ileostomy: Results of a nationwide cross-sectional survey. Dis Colon Rectum. 2017;60(1):51-60. [Link] [DOI:10.1097/DCR.0000000000000732]
24. Silva MA, Ratnayake G, Deen KI. Quality of life of stoma patients: Temporary ileostomy versus colostomy. World J Surg. 2003;27(4):421-4. [Link] [DOI:10.1007/s00268-002-6699-4]
25. Silva CRDT, Andrade EMLR, Luz MHBA, Andrade JX, Da Silva GRF. Quality of life of people with intestinal stomas. Acta Paulista de Enfermagem. 2017;30(2):144-51. [Link] [DOI:10.1590/1982-0194201700023]
26. Ssewanyana Y, Ssekitooleko B, Suuna B, Bua E, Wadeya J, Makumbi TK, et al. Quality of life of adult individuals with intestinal stomas in Uganda: A cross sectional study. Afr Health Sci. 2021;21(1):427-36. [Link] [DOI:10.4314/ahs.v21i1.53]
27. Starczewska ME, Kaczmarek J, Rybicka A, Knyszyńska A, Pankiewicz M, Błażejewska J, et al. Quality of life of intestinal stoma patients. Problemy Pielęgniarstwa. 2019;27(1):38-44. [Link]
28. Zhang Y, Xian H, Yang Y, Zhang X, Wang X. Relationship between psychosocial adaptation and health-related quality of life of patients with stoma: A descriptive, cross-sectional study. J Clin Nurs. 2019;28(15-16):2880-8. [Link] [DOI:10.1111/jocn.14876]
29. Zewude WC, Derese T, Suga Y, Teklewold B. Quality of life in patients living with stoma. Ethiop J Health Sci. 2021;31(5):993-1000. [Link] [DOI:10.4314/ejhs.v31i5.11]
30. Anaraki F, Vafaie M, Behboo R, Maghsoodi N, Esmaeilpour S, Safaee A. Quality of life outcomes in patients living with stoma. Indian J Palliat Care. 2012;18(3):176-80. [Link] [DOI:10.4103/0973-1075.105687]
31. Aluzaite K, Nuttall JW, O'Connor M, Harvie R, Schultz M. Quality of life in postostomy surgery patients: A cross‐sectional survey. JGH Open. 2020;4(5):987-94. [Link] [DOI:10.1002/jgh3.12383]
32. Lin H, Lin R, Yan M, Lin L, Sun X, Wu M, et al. Associations between preparedness, perceived stress, depression, and quality of life in family caregivers of patients with a temporary enterostomy. Eur J Oncol Nurs. 2024;70:102557. [Link] [DOI:10.1016/j.ejon.2024.102557]
33. Giordano V, Iovino P, Corvese F, Vellone E, Alvaro R, Villa G. Caregiver contribution to self‐care and its associated variables among caregivers of ostomy patients: Results of a cross‐sectional study. J Clin Nurs. 2022;31(1-2):99-110. [Link] [DOI:10.1111/jocn.15851]
34. Rashed NI, Khalifa MI, Zein El Dein NA, Omar TK. Effect of partnership based program with primary caregivers of children on stoma care. Menoufia Nurs J. 2020;5(1):39-54. [Link] [DOI:10.21608/menj.2020.123663]
35. Ambe PC, Kugler CM, Breuing J, Grohmann E, Friedel J, Hess S, et al. The effect of preoperative stoma site marking on risk of stoma‐related complications in patients with intestinal ostomy-a systematic review and meta‐analysis. Colorectal Dis. 2022;24(8):904-17. [Link] [DOI:10.1111/codi.16118]
36. Zelga P, Kluska P, Zelga M, Piasecka-Zelga J, Dziki A. Patient-related factors associated with stoma and peristomal complications following fecal ostomy surgery: A scoping review. J Wound Ostomy Continence Nurs. 2021;48(5):415-30. [Link] [DOI:10.1097/WON.0000000000000796]
37. Voegeli D, Karlsmark T, Eddes EH, Hansen HD, Zeeberg R, Hakan-Bloch J, et al. Factors influencing the incidence of peristomal skin complications: Evidence from a multinational survey on living with a stoma. Gastrointest Nurs. 2020;18(Suppl 4):S31-8. [Link] [DOI:10.12968/gasn.2020.18.Sup4.S31]
38. Maglio A, Malvone AP, Scaduto V, Brambilla D, Denti FC. The frequency of early stomal, peristomal and skin complications. Br J Nurs. 2021;30(22):1272-6. [Link] [DOI:10.12968/bjon.2021.30.22.1272]
39. Polidano K, Chew-Graham CA, Farmer AD, Saunders B. Access to psychological support for young people following stoma surgery: Exploring patients' and clinicians' perspectives. Qual Health Res. 2021;31(3):535-49. [Link] [DOI:10.1177/1049732320972338]
40. Black P, Notter J. Psychological issues affecting patients living with a stoma. Br J Nurs. 2021;30(6):S20-32. [Link] [DOI:10.12968/bjon.2021.30.6.S20]
41. Kittscha J, Wilson V, Fairbrother G, Bliokas V. The role of peer support groups in adjustment to stoma: A qualitative study. Collegian. 2024;31(3):173-9. [Link] [DOI:10.1016/j.colegn.2024.03.002]
42. Keng CJ, Lee J, Valencia M, McKechnie T, Forbes S, Eskicioglu C. Transition home following new fecal ostomy creation: A qualitative study. J Wound Ostomy Continence Nurs. 2021;48(6):537-43. [Link] [DOI:10.1097/WON.0000000000000814]
43. Ren Y, Zhou Y, Zhang L, Yang Y, Xia R, Yang Y, et al. Readiness for return-to-work model-based analysis of return-to-work perception of young and middle-aged colorectal cancer patients with stoma in the early postoperative period: A descriptive qualitative study. Support Care Cancer. 2023;31(7):411. [Link] [DOI:10.1007/s00520-023-07828-x]
44. Yang F, Cui S, Cai M, Feng F, Zhao M, Sun M, et al. The experiences of family resilience in patients with permanent colostomy and their spouses: A dyadic qualitative study. Eur J Oncol Nurs. 2024;70:102590. [Link] [DOI:10.1016/j.ejon.2024.102590]
45. Stavropoulou A, Vlamakis D, Kaba E, Kalemikerakis I, Polikandrioti M, Fasoi G, et al. "Living with a stoma": Exploring the lived experience of patients with permanent colostomy. Int J Environ Res Public Health. 2021;18(16):8512. [Link] [DOI:10.3390/ijerph18168512]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |