Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 521-527 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jalilian M, Darabi N, Bazgir N, Chenary R, Saeed Firoozabadi M, Mirzaei A. Prediction of Nutritional Behaviors that Prevent Osteoporosis in Adolescent Girls Using the Health Belief Model. Health Educ Health Promot 2024; 12 (3) :521-527
URL: http://hehp.modares.ac.ir/article-5-76350-en.html
URL: http://hehp.modares.ac.ir/article-5-76350-en.html
1- Department of Public Health, Faculty of Health, Ilam University of Medical Sciences, Ilam, Iran
2- Department of Rheumatology, Faculty of Medicine, Ilam University of Medical Sciences, Ilam, Iran
3- The Persian Gulf Tropical Medicine Research Center, the Persian Gulf Biomedical Sciences Research Institute, Bushehr University of Medical Sciences, Bushehr, Iran
2- Department of Rheumatology, Faculty of Medicine, Ilam University of Medical Sciences, Ilam, Iran
3- The Persian Gulf Tropical Medicine Research Center, the Persian Gulf Biomedical Sciences Research Institute, Bushehr University of Medical Sciences, Bushehr, Iran
Full-Text [PDF 637 kb]
(1954 Downloads)
| Abstract (HTML) (563 Views)
Full-Text: (80 Views)
Introduction
Osteoporosis (OP) is a silent disease of the present age characterized by the loss of bone mass, leading to bones that break easily [1]. It is defined by a decrease in bone density and a decline in the quality of bone structure, which results in an increased risk of fractures. The reduction in bone mass and density occurs slowly and gradually, often with symptoms not becoming apparent until the first fracture occurs. OP is one of the significant causes of disability and death among elderly individuals [1, 2].
Today, OP is considered a major global threat, with approximately one-third of women over 50 years old and one-fifth of men at risk of developing the condition [3, 4]. OP is also prevalent in Iran; the overall prevalence of OP in the country is reported to be 17%, with estimates suggesting that about 60% of Iranian women and 50% of Iranian men suffer from mild OP [5]. Bone mass in women across all age groups is significantly lower than that of men of the same age and race [4, 6]. If preventive measures against OP are not implemented in countries, substantial medical costs will be incurred by affected individuals and the health systems of these nations [5, 7]. According to a study conducted in 2010, the medical costs associated with OP in Iran are estimated to be 28, 51, and 250 million US dollars for the years 2010, 2020, and 2050, respectively [1, 8].
Nutritional behaviors during childhood and adolescence are very important in preventing OP in adulthood. The formation of nutritional habits, including the consumption of foods rich in calcium and vitamin D, such as dairy products, during adolescence can provide the basis for the continuation of these behaviors and eating habits in adulthood [9]. Studies show that health beliefs play an important role in the formation of people's nutritional behaviors. Identifying the beliefs on nutritional behaviors of adolescents is an initial and important step for health education to increase their motivation to act in the direction of OP [10, 11].
There are numerous psychological theories, such as the health belief model (HBM) [11, 12], the social cognitive theory [13], and the stages of change model [14], that can be used to predict people’s health behaviors. The HBM is one of the practical models in health education that examines the association between health beliefs and health behavior. It is based on the hypothesis that preventive behavior is shaped by individuals’ personal beliefs [11, 12]. The HBM emphasizes how a person’s perceptions create motivation and drive behavior. According to the HBM, in order to adopt preventive behaviors, individuals must first recognize their risk of suffering from OP (perceived susceptibility). They must then understand the depth and seriousness of the risk, along with its various complications in physical, psychological, social, and economic dimensions (perceived severity), so that they believe in the usefulness and applicability of the OP prevention program (perceived benefits). Conversely, it is essential for individuals to perceive that the factors preventing action are less significant than the benefits of taking action (perceived barriers) in order to ultimately take steps to prevent OP [15, 16].
Planning any educational intervention aimed at improving the nutritional behavior of adolescent girls to prevent OP requires a clear understanding of the determinants of their nutritional behavior, including health beliefs. The present study examined the determinants of osteoporosis in female students at the 1st secondary school level in Ilam City based on the HBM.
Instrument and Methods
This cross-sectional study was done on 819 female students in the 1st secondary school level selected using a multi-stage random sampling method from October 15 to March 15, 2022. The sample size was determined using Cochran’s formula and considering the population size of 3940 students, a confidence interval of 95%, a measurement error of 0.035, and p=q=0.5. Sampling was conducted as a two-stage cluster process. In the first stage, five schools were randomly selected from among 22 public schools at the first secondary level across different areas of Ilam City. In the second stage, one or two classes (depending on the number of classes in each grade) were included in the study by visiting the selected schools.
The inclusion criteria consisted of being enrolled in one of the 7th, 8th, or 9th grades (1st secondary level), being female, and providing informed consent to participate in the study. Students who were not in suitable physical or mental condition to participate in the study for any reason were excluded. Additionally, distorted and incomplete questionnaires were also excluded from the study.
Research tools
Data were collected using a researcher-developed questionnaire divided into three parts. The first part included demographic and background information with eight items, such as age, educational level, parents’ education level, parents’ employment status, history of OP in the family, and the economic status of the family.
The second part consisted of a questionnaire based on the HBM with 32 items, covering perceived susceptibility (four items, for example, “If I don’t control my diet, I might get OP”), perceived severity (six items, for example, “OP causes disability”), perceived benefits (six items, for example, “By preventing OP, the chance of bone fracture is very low”), perceived barriers (eight items, for example, “It is difficult for me to change my diet”), and perceived self-efficacy (eight items, for example, “I am sure that I can prioritize the consumption of calcium-rich foods”). The responses for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and perceived self-efficacy were scored using a five-point Likert scale, ranging from “completely agree” with a score of five to “completely disagree” with a score of one.
The third part of the questionnaire focused on the preventive behaviors related to OP, measured with ten questions. Eight questions in this section assessed participants’ behaviors over the past seven days (for example, “How much dairy products, such as yogurt and buttermilk, have you consumed in the past seven days?”). Responses were scored on a five-point Likert scale, ranging from “never” with a score of one to “always” with a score of five. The remaining two questions in the behavior section measured the history of taking calcium and vitamin D supplements in the last month, with responses recorded as either “yes” or “no”.
A qualitative method was employed to validate the content of the questionnaire. For this purpose, the questionnaire was provided to eight experts (four in health education and health promotion, two in rheumatology, and two in nutrition sciences), and they were asked to share their opinions regarding the simplicity and clarity of the items, the appropriateness of the questions, the presence of any ambiguities, and the scoring of the questions in relation to the research objectives. After gathering the experts’ feedback, necessary amendments were made.
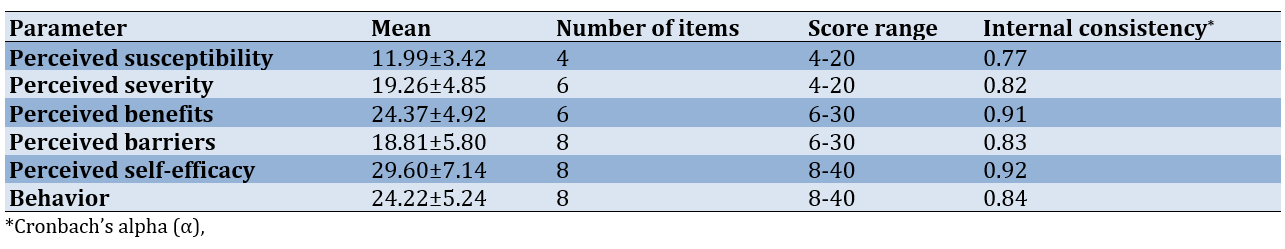
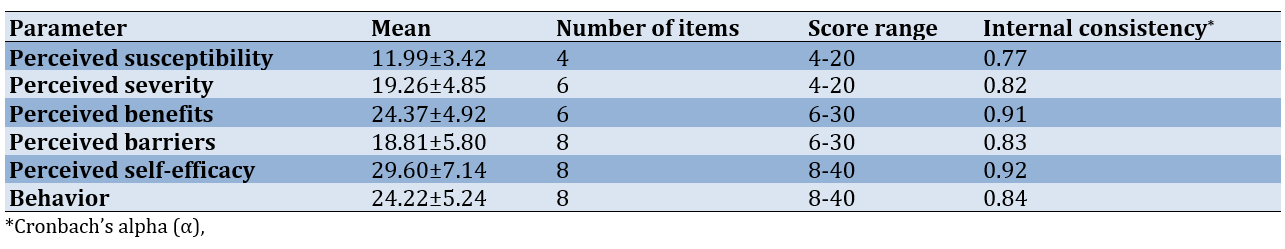
To determine the reliability of the questionnaire, the internal consistency of the items was assessed by calculating Cronbach’s alpha. For this purpose, the questionnaire was completed by 30 randomly selected students from a school (Table 1). The questionnaires were filled out using a self-report method, and the average time taken to complete each questionnaire was approximately 20 minutes.
Statistical analysis
Data analysis was conducted using SPSS version 22 software, employing descriptive and analytical tests, including Pearson’s correlation, multiple linear regression, chi-square, and one-way analysis of variance at a significance level of p<0.05.
Table 1. Mean scores and internal consistency of the health belief model (HBM) constructs and behavior (n=819)
Findings
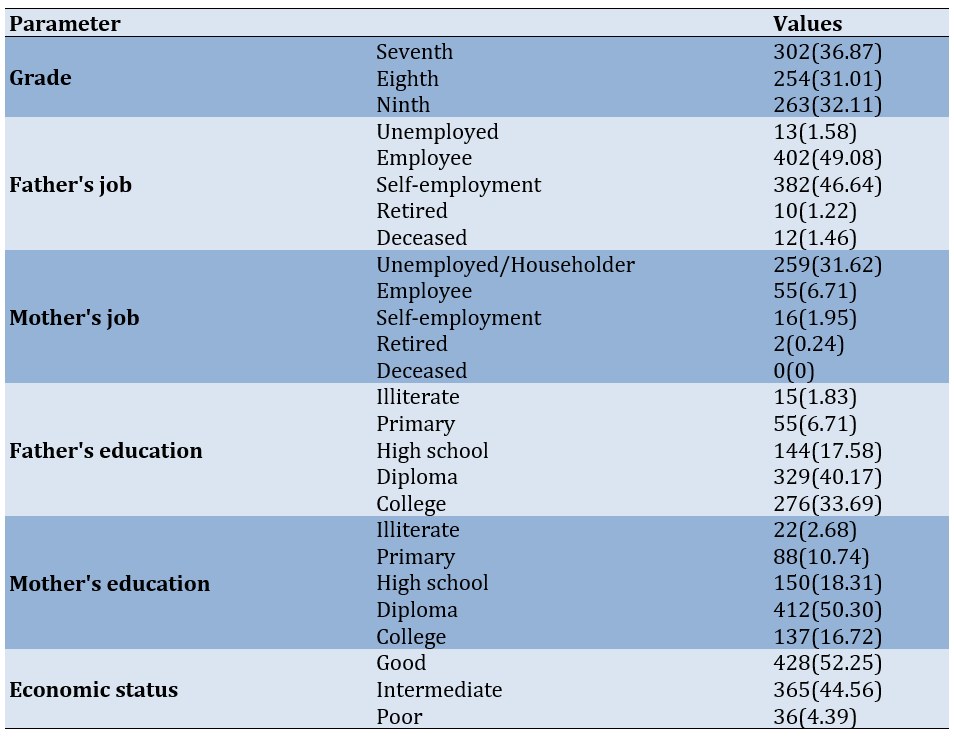
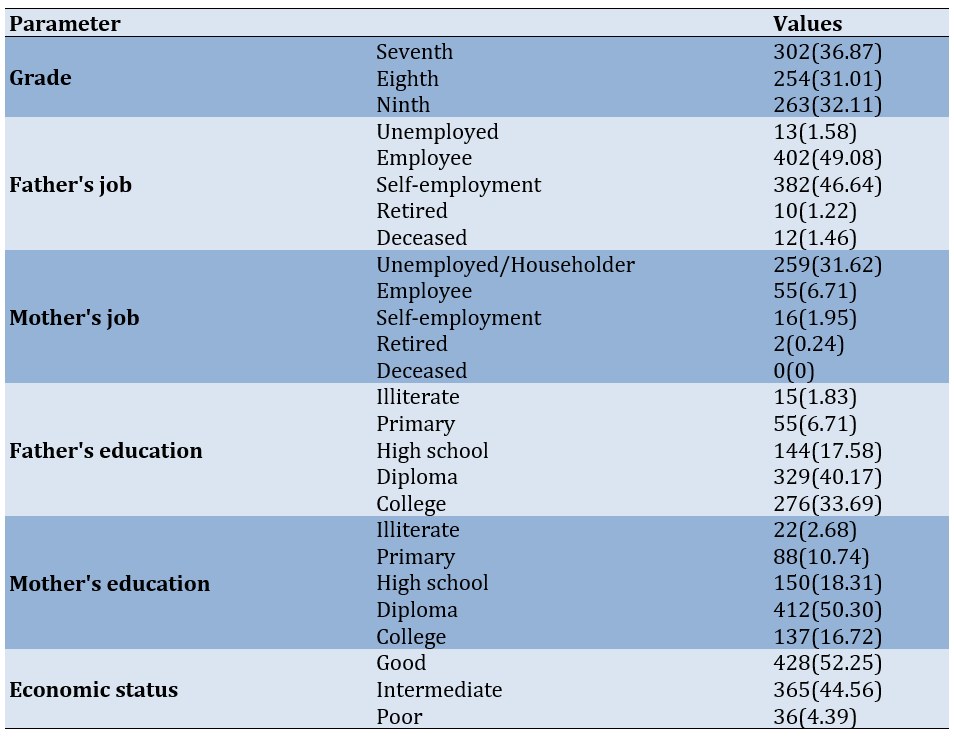
In the present study, 819 female students from the seventh, eighth, and ninth grades in Ilam City participated, with a mean age of 13.72±0.97 years and an age range of 12 to 16 years (Table 2).
Table 2. Frequency of sociodemographic characteristics of the participants
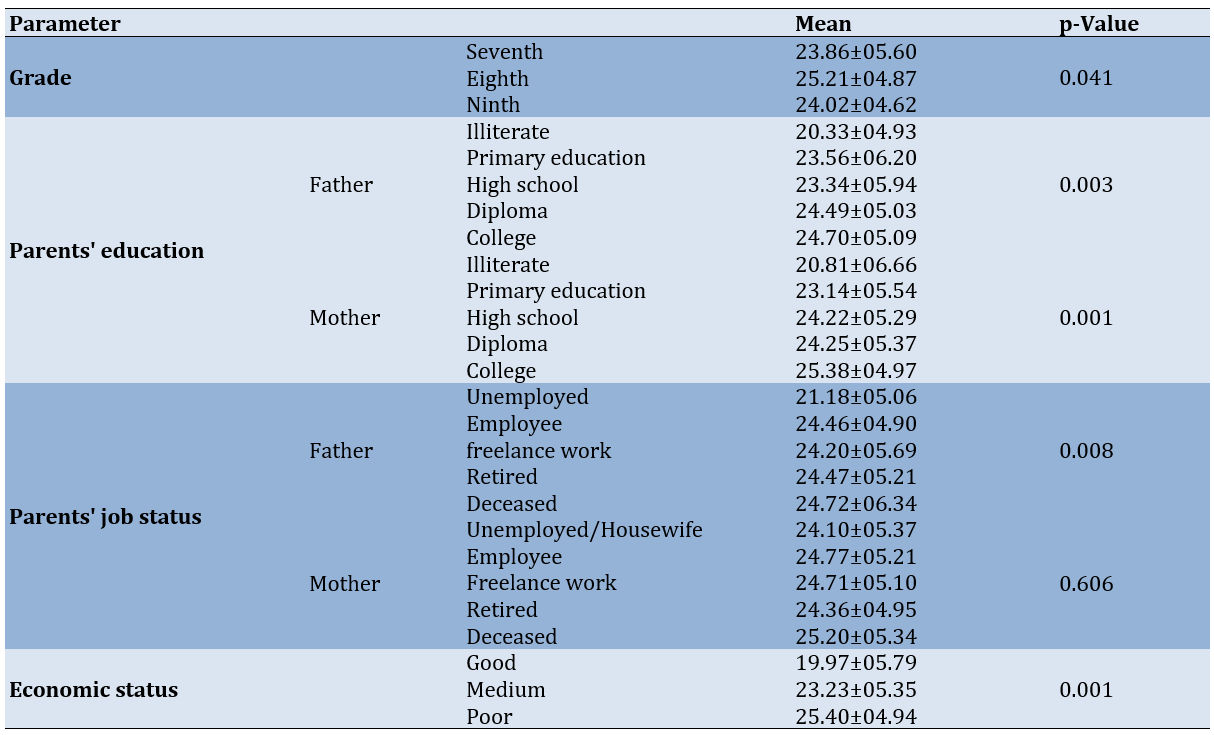
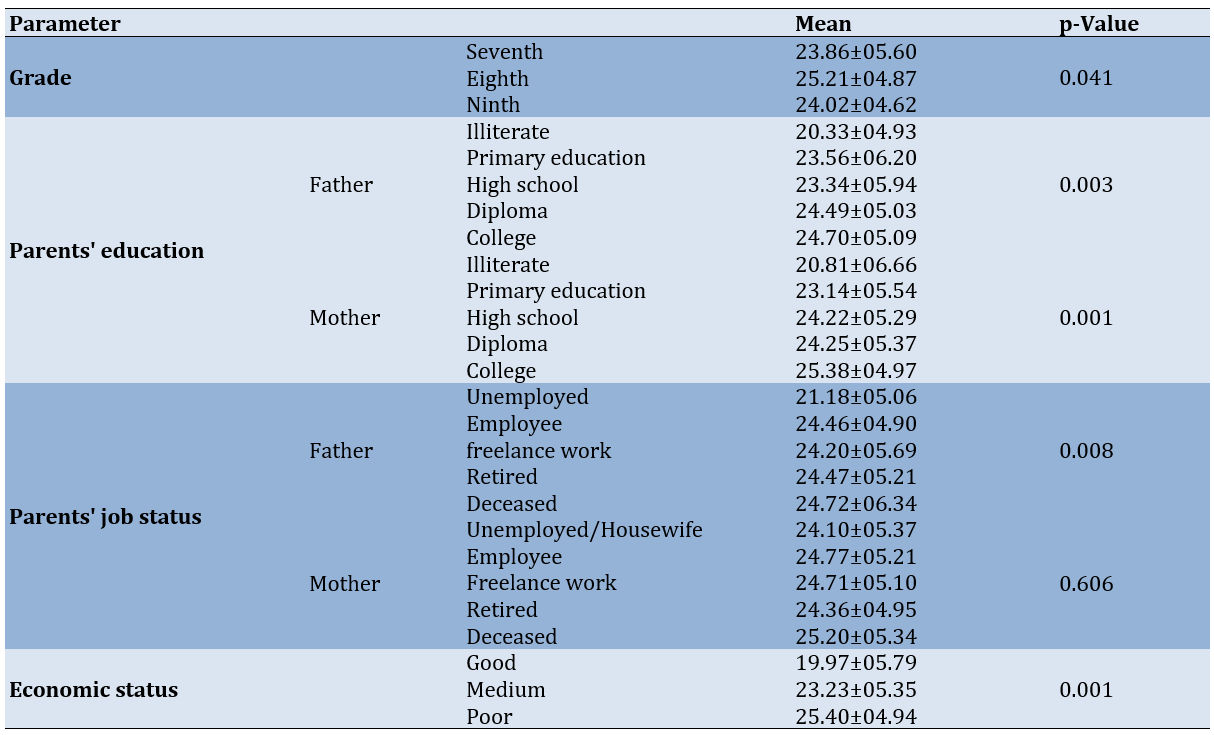
The mean scores of students’ behaviors differed significantly based on educational level (p=0.041), father’s education level (p=0.003), mother’s education level (p=0.001), father’s occupation (p=0.008), and the economic status of the family (p=0.001; Table 3).
Table 3. Comparison of the participants’ mean score of preventive behaviors for osteoporosis according to demographic parameters
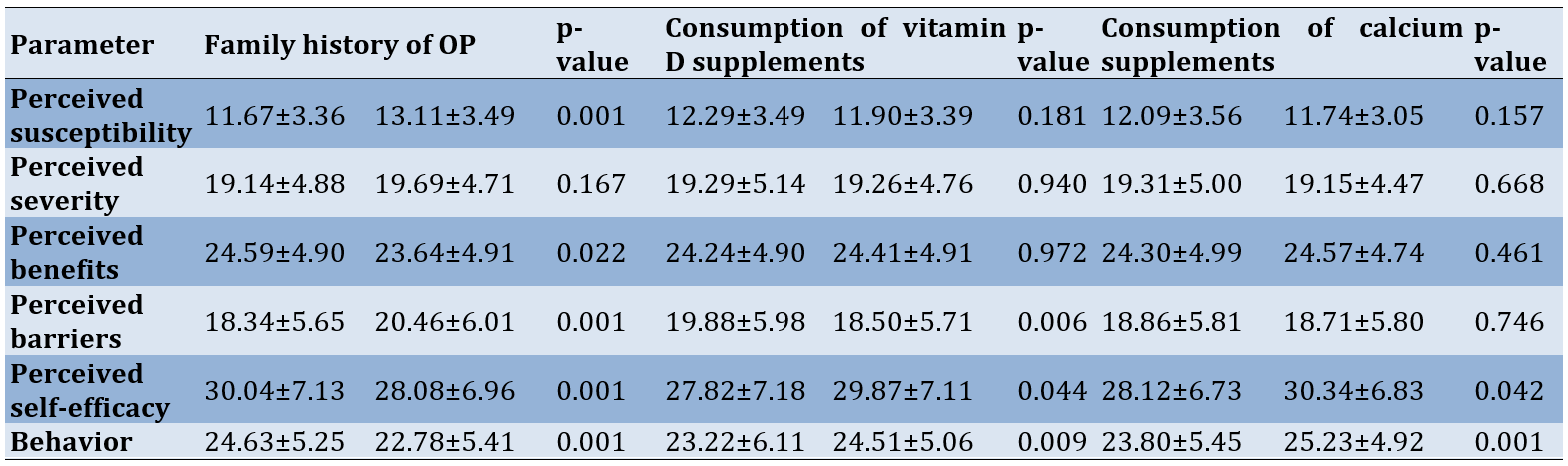
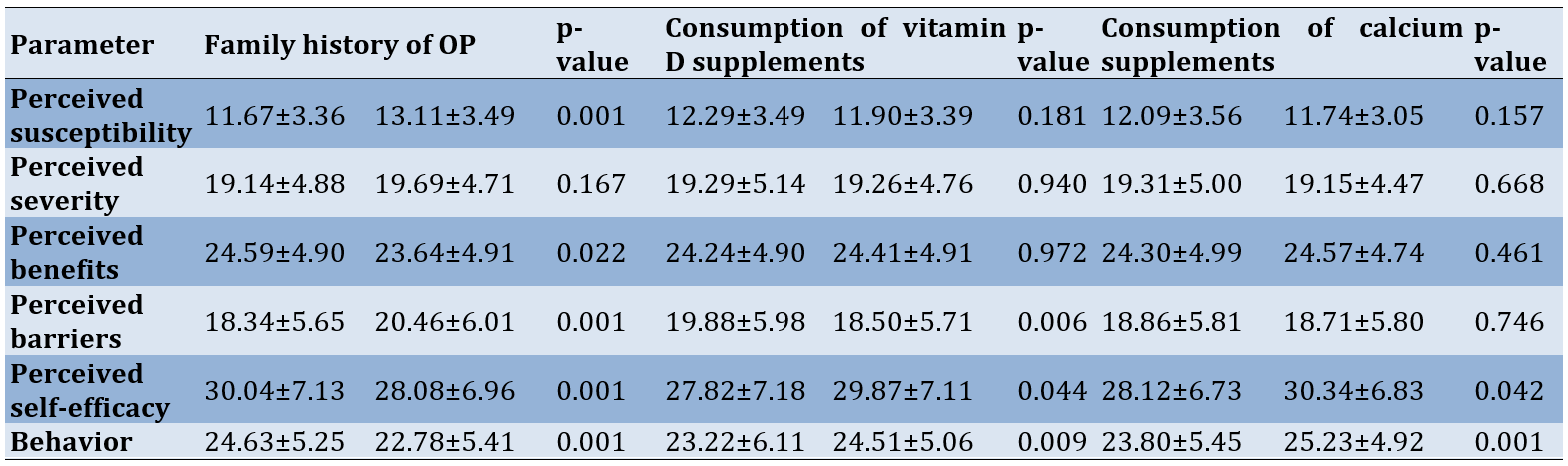
According to the results, 22.2% of participants reported a family history of OP. Additionally, the history of taking calcium and vitamin D supplements in the last month was reported by 29.2% and 22.6% of students, respectively. The mean behavior score of students with a family history of OP was significantly lower than that of other students (p=0.001). Furthermore, the mean behavior score of students who had taken calcium supplements (p=0.009) and vitamin D (p=0.001) in the last month was significantly higher than that of other students (Table 4).
Table 4. Comparison of the participants’ mean score of preventive behaviors for osteoporosis (OP) according to family history of OP and history of taking vitamin D and calcium supplements
The results of Pearson’s correlation test indicated a significant correlation between all constructs of the HBM and behavior. The behavior exhibited the highest correlation with perceived barriers (r=-0.295). The correlation of all constructs with behavior was positive, except for the construct of perceived barriers, which had a negative correlation with behavior. The highest internal correlation among the constructs of the HBM was between perceived benefits and perceived self-efficacy (r=0.496).
Regression model 1 demonstrated a significant effect of the overall HBM constructs on behavior. However, only the constructs of perceived barriers and perceived self-efficacy significantly predicted the preventive behaviors of students against OP. The constructs of the HBM were able to explain 18.9% of the variance in preventive behavior.
To investigate how other constructs affect behavior, two separate regression models (model 2 and model 3) analyzed the impact of the HBM constructs on perceived barriers and perceived self-efficacy. Model 2 showed that the HBM constructs explained a total of 29.1% of the variance in self-efficacy. Among these constructs, the effect of the perceived susceptibility construct was not significant. The results of model 3 also indicated that the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived self-efficacy explained a total of 25.9% of the variance in perceived barriers, with the effect of all constructs being significant (Table 5; Figure 1).
Table 5. Multiple linear regression analysis of the health belief model (HBM) constructs predicting behaviors, self-efficacy, and perceived barriers
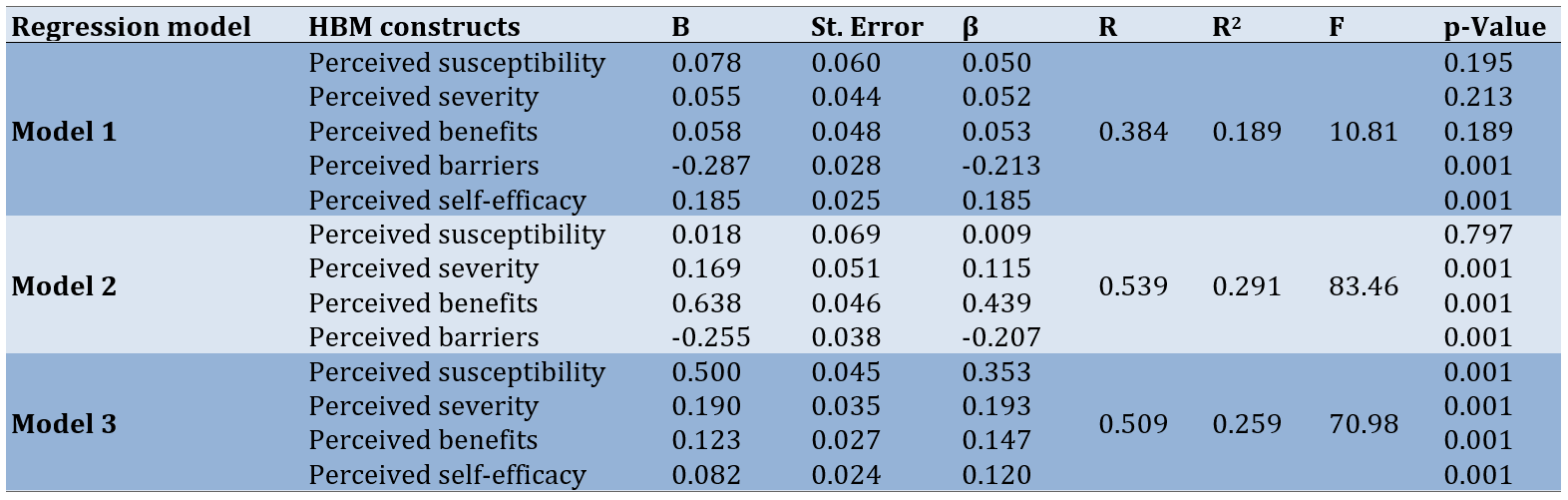
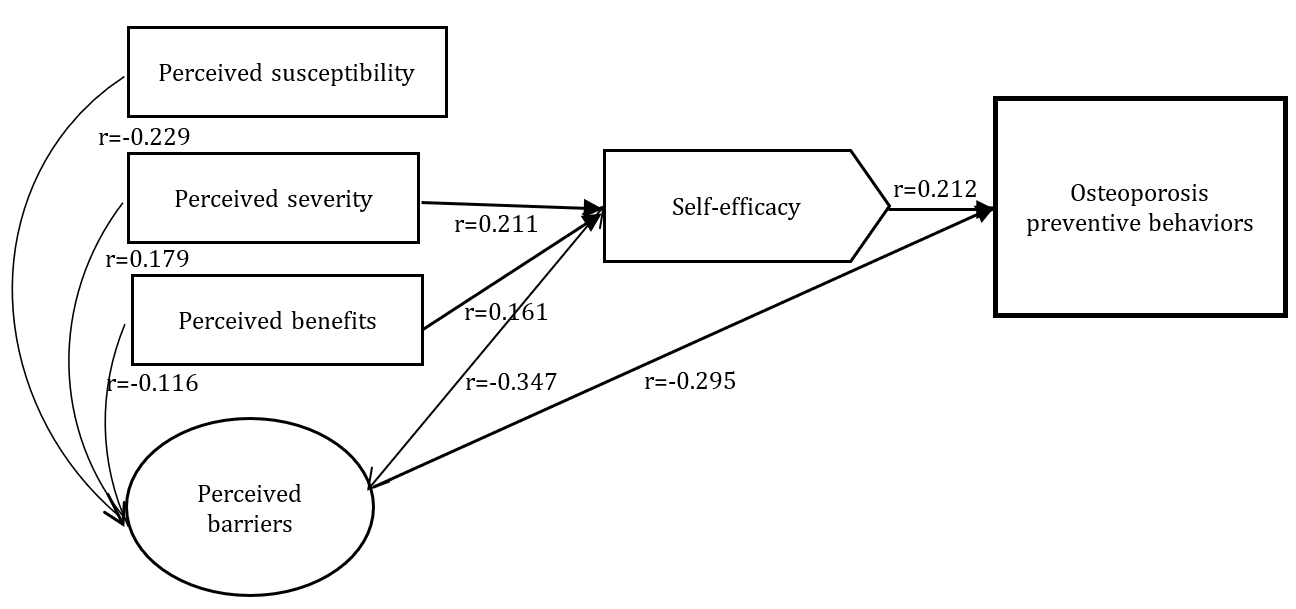
Figure 1. The proposed conceptual framework for an educational intervention aimed at improving nutritional behaviors that prevent osteoporosis in adolescent students
Discussion
This study was conducted to determine effective health beliefs related to nutritional behaviors that prevent OP in female students of the 1st secondary school in Ilam City. The HBM framework was utilized to establish the objectives of the study. The constructs of the HBM were able to predict a total of 18.9% of the variance in nutritional behaviors that prevent OP among the adolescent girls studied. However, although the overall regression model was significant, only the constructs of self-efficacy and perceived barriers significantly predicted behavior, while the other constructs of the model were not significant. The HBM has been able to explain between 6% and 23.5% of the variance in nutritional behaviors that prevent OP, including calcium intake [17-21]. According to Gammage & Klentrou, the HBM constructs together explain 16% of the variance in nutritional behaviors related to calcium intake in adolescent girls. They reported that only the constructs of self-efficacy and perceived barriers significantly predict behavior, while the other constructs of the model do not have a significant role in predicting behavior [17].
Edmonds declared that the constructs of the HBM explain 12% of the nutritional behaviors of female students aimed at preventing OP [18]. In another study, Tsai reported incorporating health knowledge and motivation in addition to the HBM constructs to predict OP prevention behavior. Among the constructs of the HBM, only perceived barriers are significant, and together with health motivation, they explain 23.5% of the variance in behavior [19].
Examining the results of the present study alongside other similar studies, it is evident that self-efficacy and perceived barriers are often the primary determinants of nutritional behaviors related to OP prevention. For instance, in the study by Gammage & Klentrou, similar to our findings, self-efficacy and perceived barriers are identified as two key determinants of calcium intake in adolescent girls [17]. Swaim et al. reported the perceived self-efficacy construct as significant [20], while Vahedian-Shahroodi et al. [21] declared the perceived barrier construct as a significant determinant. Additionally, in Tsai’s study [19], perceived barriers are identified, and in Wallace’s study [22], both self-efficacy and perceived barriers are recognized as determinants of nutritional behaviors that prevent OP [18-22].
Although the roles of the constructs of perceived self-efficacy and perceived barriers in explaining the preventive behaviors of adolescent girls against OP in the present study were decisive and direct, two separate regression models (models 2 and 3) were used to analyze how other constructs affect behavior. The findings of model 2 showed that the remaining HBM constructs—namely, perceived susceptibility, perceived severity, perceived benefits, and perceived barriers—explained a total of 29.1% of the variance in self-efficacy. Among these constructs, the effect of perceived susceptibility was not significant. The results of model 3 indicated that the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived self-efficacy explained a total of 25.9% of the variance in perceived barriers, with the effect of all constructs being significant. The analysis of these findings reveals that, except for the two constructs of perceived self-efficacy and perceived barriers, which had both direct and indirect effects on behavior, the other HBM constructs had an indirect effect on behavior through the mediation of perceived self-efficacy and perceived barriers. Specifically, perceived susceptibility influenced behavior through its effect on perceived barriers, while the constructs of perceived severity and perceived benefits had an indirect effect on behavior by impacting the constructs of perceived self-efficacy and perceived barriers.
Despite the confirmation and emphasis of most similar studies on the high importance of the two constructs of self-efficacy and perceived barriers in predicting behaviors related to the prevention of OP, there are a few studies with different findings that report the impact of other constructs of the HBM. For example, the studies by Kim et al., Sedlak et al., and Kang & Kim report significant correlations between the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers with preventive behaviors against OP [23-25]. Additionally, by Jeihooni et al. and Hazavehei et al., perceived susceptibility to OP is considered a motivational factor for changing the behavior of teenage girls [26, 27]. Abood et al. reported that perceived benefits play an important role in determining preventive behaviors against OP [28]. In the present study, although the constructs of perceived susceptibility, perceived severity, and perceived benefits were not direct predictors of behavior, they exhibited a positive and significant correlation with behavior. Furthermore, by influencing the two mediating constructs—self-efficacy and perceived barriers—they had an indirect effect on behavior.
The results of this study showed that only 29.2% and 22.6% of the studied sample had taken calcium and vitamin D supplements in the last month. On the other hand, nutritional behaviors—such as the consumption of milk and dairy products, fruits and vegetables, and legumes—were also reported to be weak. The perceived barriers to nutritional behaviors that prevent OP included low awareness of ways to prevent OP, insufficient family support, lack of interest, a preference for the taste of dairy products, the high cost of purchasing dairy products, and the existence of some misconceptions about dairy products. The results of many other studies also indicate that the nutritional behaviors of teenage girls, including calcium intake, are poor. For example, according to Hazavehei et al., 76% of teenage girls have insufficient calcium intake [27]. Similar findings to those of the present study are reported in the studies by Gammage & Klentrou, Vahedian-Shahroodi et al., Al Seraty & Ali, and Anderson et al. [17, 21, 29, 30]. In these studies, several perceived barriers, including individual, social, and environmental factors, are identified as contributing to the insufficient intake of calcium by adolescent girls. Among the individual obstacles perceived are a lack of preference for the taste of calcium-rich foods, viewing OP as a disease related to old age and not taking the disease seriously during adolescence, the existence of specific diseases or nutritional incompatibilities (such as lactose intolerance), and low self-efficacy. Additionally, insufficient social and family support (from parents and peers), lack of access to calcium-containing foods at home, the higher cost of calcium-containing foods compared to other foods, and poor social and economic status have been identified as social and environmental barriers to the insufficient intake of calcium by adolescent girls [17, 30-34].
Considering the individual and environmental barriers identified in the present study, as well as the results of other studies, health education planners need to focus on removing these barriers. Additionally, given the strong association between self-efficacy and perceived barriers among participants in this study, promoting adolescents’ self-efficacy can be utilized by health educators as a strategy to overcome the perceived barriers to nutritional behaviors. Previous studies have reported the effectiveness of educational interventions based on the HBM in promoting nutritional behaviors that prevent OP. Notable examples include the studies by Khani Jeihooni et al. [35], Hazavehei et al. [27], and Al Seraty & Ali [29]. To enhance the effectiveness of HBM-based educational interventions in the field of OP prevention, efforts should focus on improving self-efficacy and addressing perceived barriers. The supportive role of the family, particularly parents, is crucial in increasing the motivation of teenage girls to consume foods containing calcium and vitamin D. Parents can play several important roles, such as providing dairy foods at home, reducing the purchase and consumption of carbonated soft drinks, and serving as role models in terms of consuming calcium-rich foods [17, 34, 36]. Designing educational interventions based on the HBM, with a focus on promoting perceived self-efficacy and addressing perceived barriers, can be effective in improving preventive nutritional behaviors related to OP in adolescent girls.
The present study had a few limitations. First, the study was conducted solely on female students and boys were not included in the study. Second, private schools were not included in the study, and the study was conducted with the participation of public schools. Third, we did not measure the cues action construct of the HBM.
Conclusion
The constructs of self-efficacy and perceived barriers directly affected nutritional behavior preventing OP among teenage girls in Ilam City, while another construct had an indirect effect.
Acknowledgments: The authors appreciate the students who participated in the study.
Ethical Permissions: The present study was approved by the Ethics Committee of Ilam University of Medical Sciences (IR.MEDILAM.REC.1400.180). The study participants provided informed consent and completed a written consent form to participate in the study.
Conflicts of Interests: There are no conflicts of interests.
Authors' Contribution: Jalilian M (First Author), Methodologist/Discussion Writer (25%); Darabi N (Second Author), Methodologist/Assistant Researcher (15%); Bazgir N (Third Author), Assistant Researcher/Discussion Writer (10%); Chenary R (Fourth Author), Assistant Researcher/Methodologist (10%); Saeed Firoozabadi M (Fifth Author), Assistant Researcher/Introduction Writer (10%); Mirzaei A (Sixth Author), Original Researcher/Methodologist/Statistical Analyst (30%)
Funding/Support: The present research was financially supported by the Research and Technology Deputy of Ilam University of Medical Sciences, Iran.
Osteoporosis (OP) is a silent disease of the present age characterized by the loss of bone mass, leading to bones that break easily [1]. It is defined by a decrease in bone density and a decline in the quality of bone structure, which results in an increased risk of fractures. The reduction in bone mass and density occurs slowly and gradually, often with symptoms not becoming apparent until the first fracture occurs. OP is one of the significant causes of disability and death among elderly individuals [1, 2].
Today, OP is considered a major global threat, with approximately one-third of women over 50 years old and one-fifth of men at risk of developing the condition [3, 4]. OP is also prevalent in Iran; the overall prevalence of OP in the country is reported to be 17%, with estimates suggesting that about 60% of Iranian women and 50% of Iranian men suffer from mild OP [5]. Bone mass in women across all age groups is significantly lower than that of men of the same age and race [4, 6]. If preventive measures against OP are not implemented in countries, substantial medical costs will be incurred by affected individuals and the health systems of these nations [5, 7]. According to a study conducted in 2010, the medical costs associated with OP in Iran are estimated to be 28, 51, and 250 million US dollars for the years 2010, 2020, and 2050, respectively [1, 8].
Nutritional behaviors during childhood and adolescence are very important in preventing OP in adulthood. The formation of nutritional habits, including the consumption of foods rich in calcium and vitamin D, such as dairy products, during adolescence can provide the basis for the continuation of these behaviors and eating habits in adulthood [9]. Studies show that health beliefs play an important role in the formation of people's nutritional behaviors. Identifying the beliefs on nutritional behaviors of adolescents is an initial and important step for health education to increase their motivation to act in the direction of OP [10, 11].
There are numerous psychological theories, such as the health belief model (HBM) [11, 12], the social cognitive theory [13], and the stages of change model [14], that can be used to predict people’s health behaviors. The HBM is one of the practical models in health education that examines the association between health beliefs and health behavior. It is based on the hypothesis that preventive behavior is shaped by individuals’ personal beliefs [11, 12]. The HBM emphasizes how a person’s perceptions create motivation and drive behavior. According to the HBM, in order to adopt preventive behaviors, individuals must first recognize their risk of suffering from OP (perceived susceptibility). They must then understand the depth and seriousness of the risk, along with its various complications in physical, psychological, social, and economic dimensions (perceived severity), so that they believe in the usefulness and applicability of the OP prevention program (perceived benefits). Conversely, it is essential for individuals to perceive that the factors preventing action are less significant than the benefits of taking action (perceived barriers) in order to ultimately take steps to prevent OP [15, 16].
Planning any educational intervention aimed at improving the nutritional behavior of adolescent girls to prevent OP requires a clear understanding of the determinants of their nutritional behavior, including health beliefs. The present study examined the determinants of osteoporosis in female students at the 1st secondary school level in Ilam City based on the HBM.
Instrument and Methods
This cross-sectional study was done on 819 female students in the 1st secondary school level selected using a multi-stage random sampling method from October 15 to March 15, 2022. The sample size was determined using Cochran’s formula and considering the population size of 3940 students, a confidence interval of 95%, a measurement error of 0.035, and p=q=0.5. Sampling was conducted as a two-stage cluster process. In the first stage, five schools were randomly selected from among 22 public schools at the first secondary level across different areas of Ilam City. In the second stage, one or two classes (depending on the number of classes in each grade) were included in the study by visiting the selected schools.
The inclusion criteria consisted of being enrolled in one of the 7th, 8th, or 9th grades (1st secondary level), being female, and providing informed consent to participate in the study. Students who were not in suitable physical or mental condition to participate in the study for any reason were excluded. Additionally, distorted and incomplete questionnaires were also excluded from the study.
Research tools
Data were collected using a researcher-developed questionnaire divided into three parts. The first part included demographic and background information with eight items, such as age, educational level, parents’ education level, parents’ employment status, history of OP in the family, and the economic status of the family.
The second part consisted of a questionnaire based on the HBM with 32 items, covering perceived susceptibility (four items, for example, “If I don’t control my diet, I might get OP”), perceived severity (six items, for example, “OP causes disability”), perceived benefits (six items, for example, “By preventing OP, the chance of bone fracture is very low”), perceived barriers (eight items, for example, “It is difficult for me to change my diet”), and perceived self-efficacy (eight items, for example, “I am sure that I can prioritize the consumption of calcium-rich foods”). The responses for perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and perceived self-efficacy were scored using a five-point Likert scale, ranging from “completely agree” with a score of five to “completely disagree” with a score of one.
The third part of the questionnaire focused on the preventive behaviors related to OP, measured with ten questions. Eight questions in this section assessed participants’ behaviors over the past seven days (for example, “How much dairy products, such as yogurt and buttermilk, have you consumed in the past seven days?”). Responses were scored on a five-point Likert scale, ranging from “never” with a score of one to “always” with a score of five. The remaining two questions in the behavior section measured the history of taking calcium and vitamin D supplements in the last month, with responses recorded as either “yes” or “no”.
A qualitative method was employed to validate the content of the questionnaire. For this purpose, the questionnaire was provided to eight experts (four in health education and health promotion, two in rheumatology, and two in nutrition sciences), and they were asked to share their opinions regarding the simplicity and clarity of the items, the appropriateness of the questions, the presence of any ambiguities, and the scoring of the questions in relation to the research objectives. After gathering the experts’ feedback, necessary amendments were made.
To determine the reliability of the questionnaire, the internal consistency of the items was assessed by calculating Cronbach’s alpha. For this purpose, the questionnaire was completed by 30 randomly selected students from a school (Table 1). The questionnaires were filled out using a self-report method, and the average time taken to complete each questionnaire was approximately 20 minutes.
Statistical analysis
Data analysis was conducted using SPSS version 22 software, employing descriptive and analytical tests, including Pearson’s correlation, multiple linear regression, chi-square, and one-way analysis of variance at a significance level of p<0.05.
Table 1. Mean scores and internal consistency of the health belief model (HBM) constructs and behavior (n=819)
Findings
In the present study, 819 female students from the seventh, eighth, and ninth grades in Ilam City participated, with a mean age of 13.72±0.97 years and an age range of 12 to 16 years (Table 2).
Table 2. Frequency of sociodemographic characteristics of the participants
The mean scores of students’ behaviors differed significantly based on educational level (p=0.041), father’s education level (p=0.003), mother’s education level (p=0.001), father’s occupation (p=0.008), and the economic status of the family (p=0.001; Table 3).
Table 3. Comparison of the participants’ mean score of preventive behaviors for osteoporosis according to demographic parameters
According to the results, 22.2% of participants reported a family history of OP. Additionally, the history of taking calcium and vitamin D supplements in the last month was reported by 29.2% and 22.6% of students, respectively. The mean behavior score of students with a family history of OP was significantly lower than that of other students (p=0.001). Furthermore, the mean behavior score of students who had taken calcium supplements (p=0.009) and vitamin D (p=0.001) in the last month was significantly higher than that of other students (Table 4).
Table 4. Comparison of the participants’ mean score of preventive behaviors for osteoporosis (OP) according to family history of OP and history of taking vitamin D and calcium supplements
The results of Pearson’s correlation test indicated a significant correlation between all constructs of the HBM and behavior. The behavior exhibited the highest correlation with perceived barriers (r=-0.295). The correlation of all constructs with behavior was positive, except for the construct of perceived barriers, which had a negative correlation with behavior. The highest internal correlation among the constructs of the HBM was between perceived benefits and perceived self-efficacy (r=0.496).
Regression model 1 demonstrated a significant effect of the overall HBM constructs on behavior. However, only the constructs of perceived barriers and perceived self-efficacy significantly predicted the preventive behaviors of students against OP. The constructs of the HBM were able to explain 18.9% of the variance in preventive behavior.
To investigate how other constructs affect behavior, two separate regression models (model 2 and model 3) analyzed the impact of the HBM constructs on perceived barriers and perceived self-efficacy. Model 2 showed that the HBM constructs explained a total of 29.1% of the variance in self-efficacy. Among these constructs, the effect of the perceived susceptibility construct was not significant. The results of model 3 also indicated that the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived self-efficacy explained a total of 25.9% of the variance in perceived barriers, with the effect of all constructs being significant (Table 5; Figure 1).
Table 5. Multiple linear regression analysis of the health belief model (HBM) constructs predicting behaviors, self-efficacy, and perceived barriers
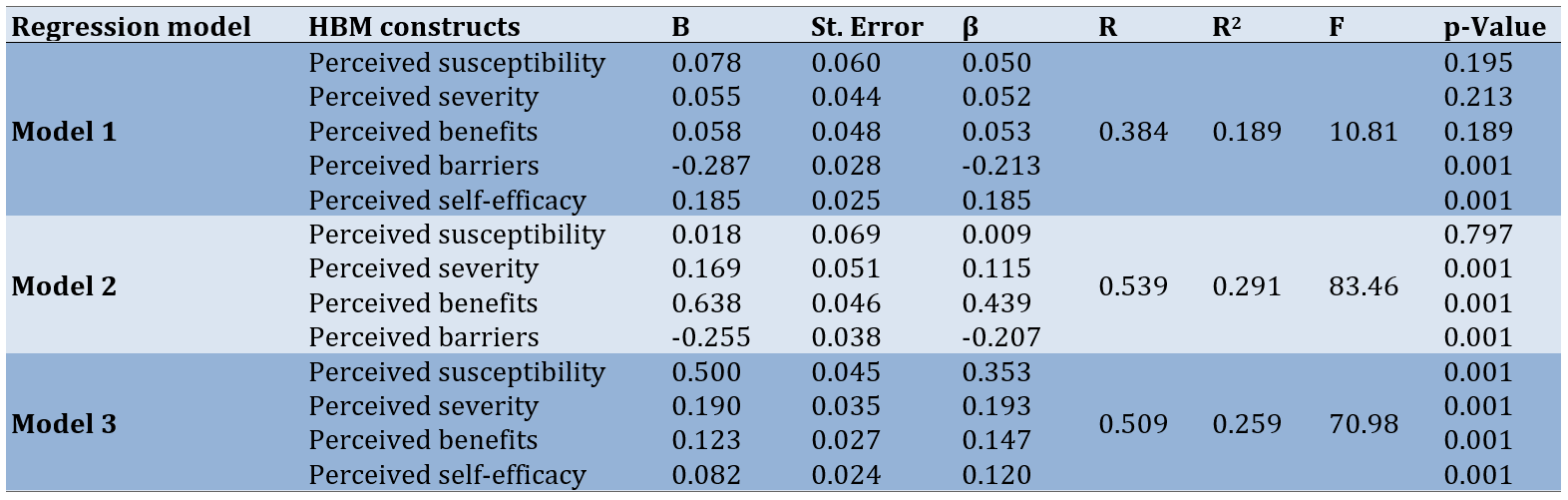
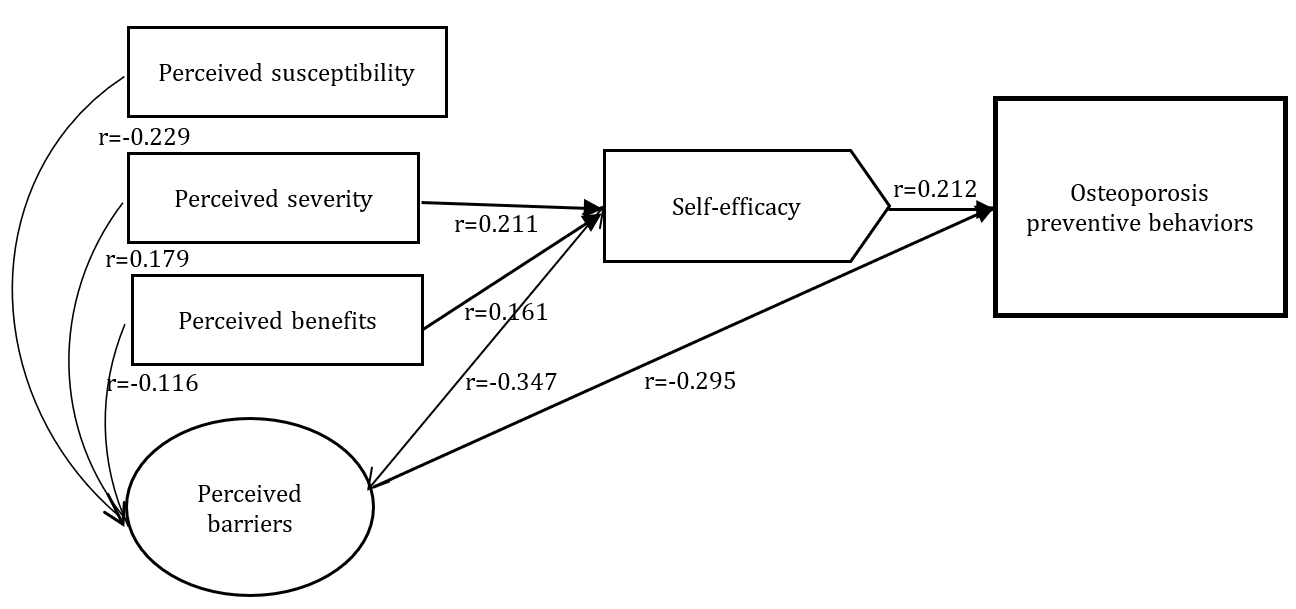
Figure 1. The proposed conceptual framework for an educational intervention aimed at improving nutritional behaviors that prevent osteoporosis in adolescent students
Discussion
This study was conducted to determine effective health beliefs related to nutritional behaviors that prevent OP in female students of the 1st secondary school in Ilam City. The HBM framework was utilized to establish the objectives of the study. The constructs of the HBM were able to predict a total of 18.9% of the variance in nutritional behaviors that prevent OP among the adolescent girls studied. However, although the overall regression model was significant, only the constructs of self-efficacy and perceived barriers significantly predicted behavior, while the other constructs of the model were not significant. The HBM has been able to explain between 6% and 23.5% of the variance in nutritional behaviors that prevent OP, including calcium intake [17-21]. According to Gammage & Klentrou, the HBM constructs together explain 16% of the variance in nutritional behaviors related to calcium intake in adolescent girls. They reported that only the constructs of self-efficacy and perceived barriers significantly predict behavior, while the other constructs of the model do not have a significant role in predicting behavior [17].
Edmonds declared that the constructs of the HBM explain 12% of the nutritional behaviors of female students aimed at preventing OP [18]. In another study, Tsai reported incorporating health knowledge and motivation in addition to the HBM constructs to predict OP prevention behavior. Among the constructs of the HBM, only perceived barriers are significant, and together with health motivation, they explain 23.5% of the variance in behavior [19].
Examining the results of the present study alongside other similar studies, it is evident that self-efficacy and perceived barriers are often the primary determinants of nutritional behaviors related to OP prevention. For instance, in the study by Gammage & Klentrou, similar to our findings, self-efficacy and perceived barriers are identified as two key determinants of calcium intake in adolescent girls [17]. Swaim et al. reported the perceived self-efficacy construct as significant [20], while Vahedian-Shahroodi et al. [21] declared the perceived barrier construct as a significant determinant. Additionally, in Tsai’s study [19], perceived barriers are identified, and in Wallace’s study [22], both self-efficacy and perceived barriers are recognized as determinants of nutritional behaviors that prevent OP [18-22].
Although the roles of the constructs of perceived self-efficacy and perceived barriers in explaining the preventive behaviors of adolescent girls against OP in the present study were decisive and direct, two separate regression models (models 2 and 3) were used to analyze how other constructs affect behavior. The findings of model 2 showed that the remaining HBM constructs—namely, perceived susceptibility, perceived severity, perceived benefits, and perceived barriers—explained a total of 29.1% of the variance in self-efficacy. Among these constructs, the effect of perceived susceptibility was not significant. The results of model 3 indicated that the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived self-efficacy explained a total of 25.9% of the variance in perceived barriers, with the effect of all constructs being significant. The analysis of these findings reveals that, except for the two constructs of perceived self-efficacy and perceived barriers, which had both direct and indirect effects on behavior, the other HBM constructs had an indirect effect on behavior through the mediation of perceived self-efficacy and perceived barriers. Specifically, perceived susceptibility influenced behavior through its effect on perceived barriers, while the constructs of perceived severity and perceived benefits had an indirect effect on behavior by impacting the constructs of perceived self-efficacy and perceived barriers.
Despite the confirmation and emphasis of most similar studies on the high importance of the two constructs of self-efficacy and perceived barriers in predicting behaviors related to the prevention of OP, there are a few studies with different findings that report the impact of other constructs of the HBM. For example, the studies by Kim et al., Sedlak et al., and Kang & Kim report significant correlations between the constructs of perceived susceptibility, perceived severity, perceived benefits, and perceived barriers with preventive behaviors against OP [23-25]. Additionally, by Jeihooni et al. and Hazavehei et al., perceived susceptibility to OP is considered a motivational factor for changing the behavior of teenage girls [26, 27]. Abood et al. reported that perceived benefits play an important role in determining preventive behaviors against OP [28]. In the present study, although the constructs of perceived susceptibility, perceived severity, and perceived benefits were not direct predictors of behavior, they exhibited a positive and significant correlation with behavior. Furthermore, by influencing the two mediating constructs—self-efficacy and perceived barriers—they had an indirect effect on behavior.
The results of this study showed that only 29.2% and 22.6% of the studied sample had taken calcium and vitamin D supplements in the last month. On the other hand, nutritional behaviors—such as the consumption of milk and dairy products, fruits and vegetables, and legumes—were also reported to be weak. The perceived barriers to nutritional behaviors that prevent OP included low awareness of ways to prevent OP, insufficient family support, lack of interest, a preference for the taste of dairy products, the high cost of purchasing dairy products, and the existence of some misconceptions about dairy products. The results of many other studies also indicate that the nutritional behaviors of teenage girls, including calcium intake, are poor. For example, according to Hazavehei et al., 76% of teenage girls have insufficient calcium intake [27]. Similar findings to those of the present study are reported in the studies by Gammage & Klentrou, Vahedian-Shahroodi et al., Al Seraty & Ali, and Anderson et al. [17, 21, 29, 30]. In these studies, several perceived barriers, including individual, social, and environmental factors, are identified as contributing to the insufficient intake of calcium by adolescent girls. Among the individual obstacles perceived are a lack of preference for the taste of calcium-rich foods, viewing OP as a disease related to old age and not taking the disease seriously during adolescence, the existence of specific diseases or nutritional incompatibilities (such as lactose intolerance), and low self-efficacy. Additionally, insufficient social and family support (from parents and peers), lack of access to calcium-containing foods at home, the higher cost of calcium-containing foods compared to other foods, and poor social and economic status have been identified as social and environmental barriers to the insufficient intake of calcium by adolescent girls [17, 30-34].
Considering the individual and environmental barriers identified in the present study, as well as the results of other studies, health education planners need to focus on removing these barriers. Additionally, given the strong association between self-efficacy and perceived barriers among participants in this study, promoting adolescents’ self-efficacy can be utilized by health educators as a strategy to overcome the perceived barriers to nutritional behaviors. Previous studies have reported the effectiveness of educational interventions based on the HBM in promoting nutritional behaviors that prevent OP. Notable examples include the studies by Khani Jeihooni et al. [35], Hazavehei et al. [27], and Al Seraty & Ali [29]. To enhance the effectiveness of HBM-based educational interventions in the field of OP prevention, efforts should focus on improving self-efficacy and addressing perceived barriers. The supportive role of the family, particularly parents, is crucial in increasing the motivation of teenage girls to consume foods containing calcium and vitamin D. Parents can play several important roles, such as providing dairy foods at home, reducing the purchase and consumption of carbonated soft drinks, and serving as role models in terms of consuming calcium-rich foods [17, 34, 36]. Designing educational interventions based on the HBM, with a focus on promoting perceived self-efficacy and addressing perceived barriers, can be effective in improving preventive nutritional behaviors related to OP in adolescent girls.
The present study had a few limitations. First, the study was conducted solely on female students and boys were not included in the study. Second, private schools were not included in the study, and the study was conducted with the participation of public schools. Third, we did not measure the cues action construct of the HBM.
Conclusion
The constructs of self-efficacy and perceived barriers directly affected nutritional behavior preventing OP among teenage girls in Ilam City, while another construct had an indirect effect.
Acknowledgments: The authors appreciate the students who participated in the study.
Ethical Permissions: The present study was approved by the Ethics Committee of Ilam University of Medical Sciences (IR.MEDILAM.REC.1400.180). The study participants provided informed consent and completed a written consent form to participate in the study.
Conflicts of Interests: There are no conflicts of interests.
Authors' Contribution: Jalilian M (First Author), Methodologist/Discussion Writer (25%); Darabi N (Second Author), Methodologist/Assistant Researcher (15%); Bazgir N (Third Author), Assistant Researcher/Discussion Writer (10%); Chenary R (Fourth Author), Assistant Researcher/Methodologist (10%); Saeed Firoozabadi M (Fifth Author), Assistant Researcher/Introduction Writer (10%); Mirzaei A (Sixth Author), Original Researcher/Methodologist/Statistical Analyst (30%)
Funding/Support: The present research was financially supported by the Research and Technology Deputy of Ilam University of Medical Sciences, Iran.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2024/07/31 | Accepted: 2024/10/21 | Published: 2024/10/30
Received: 2024/07/31 | Accepted: 2024/10/21 | Published: 2024/10/30
References
1. Fahimfar N, Noorali S, Yousefi S, Gharibzadeh S, Shafiee G, Panahi N, et al. Prevalence of osteoporosis among the elderly population of Iran. Arch Osteoporos. 2021;16(1):16. [Link] [DOI:10.1007/s11657-020-00872-8]
2. Abdolalipour S, Mirghafourvand M. Effect of education on preventive behaviors of osteoporosis in adolescents: A systematic review and meta-analysis. Int Q Community Health Educ. 2021;41(3):325-47. [Link] [DOI:10.1177/0272684X20936833]
3. Xiao PL, Cui AY, Hsu CJ, Peng R, Jiang N, Xu XH, et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: A systematic review and meta-analysis. Osteoporos Int. 2022;33(10):2137-53. [Link] [DOI:10.1007/s00198-022-06454-3]
4. Kemmak AR, Rezapour A, Jahangiri R, Nikjoo S, Farabi H, Soleimanpour S. Economic burden of osteoporosis in the world: A systematic review. Med J Islam Repub Iran. 2020;34:154. [Link] [DOI:10.21203/rs.2.22372/v1]
5. Cheraghi P, Cheraghi Z, Bozorgmehr S. The prevalence and risk factors of osteoporosis among the elderly in Hamadan province: A cross sectional study. Med J Islam Repub Iran. 2018;32:111. [Link] [DOI:10.14196/mjiri.32.111]
6. Salari N, Ghasemi H, Mohammadi L, Behzadi MH, Rabieenia E, Shohaimi S, et al. The global prevalence of osteoporosis in the world: A comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):609. [Link] [DOI:10.1186/s13018-021-02772-0]
7. Nourmohammadi H, Abdan Z, Hashemipour SM, Sarokhani D, Abdan M, Fakhri M, et al. Prevalence of osteoporosis and osteopenia in people over 60 years in Iran: A systematic review and meta-analysis. Int J Prev Med. 2022;13(1):11. [Link] [DOI:10.4103/ijpvm.IJPVM_657_20]
8. Alipour V, Meshkani Z, Rezapour A, Aboutorabi A, Bagherzadeh R, Saber N. Medical costs of osteoporosis in the Iranian elderly patients. Med J Islam Repub Iran. 2020;34:37. [Link] [DOI:10.47176/mjiri.34.37]
9. Zeinivanmoghadam L, Jalilian M, Mirzaei A. Predictors of fruits and vegetable consumption in adolescent girls based on social cognitive theory. J Educ Community Health. 2020;7(4):285-91. [Persian] [Link] [DOI:10.29252/jech.7.4.285]
10. Khani Jeihooni A, Hidarnia A, Kaveh MH, Hajizadeh E. Survey of predictors osteoporosis preventive behaviors among women in Fasa: Integrated of the health belief model and social cognitive theory. J Health Syst Res. 2015;11(1):53-67. [Persian] [Link]
11. Khani Jihoni A, Haidarnia A, Kave M, Hajizadeh E, Askari A, Haghizadeh M. Designing the validity and reliability of osteoporosis prevention instrument based on health belief model in women. J Ilam Univ Med Sci. 2014;22(3):127-36. [Persian] [Link]
12. Allahverdipoor H. Passing through traditional health education towards theory oriented health education. Health Promot Educ Mag. 2005;1(3):75-9. [Persian] [Link]
13. Mirzaei A, Ghofranipour F, Ghazanfari Z. Social cognitive predictors of breakfast consumption in primary school's male students. Glob J Health Sci. 2015;8(1):124-32. [Link] [DOI:10.5539/gjhs.v8n1p124]
14. Saeidi A, Mirzaei A, Mahaki B, Jalali A, Jalilian M. Physical activity stage of change and its related factors in secondary school students of Sarableh City: A perspective from Iran. Open Access Maced J Med Sci. 2018;6(8):1517-21. [Link] [DOI:10.3889/oamjms.2018.298]
15. Shamsi M, Bayati A, Mohamadbeygi A, Tajik R. The effect of educational program based on health belief model (HBM) on preventive behavior of self-medication in woman with pregnancy in Arak, Iran. PAJOOHANDE. 2010;14(6):324-31. [Persian] [Link]
16. Hidarnia AR. Topics in the health education process. Tehran: Zamani Naser; 2003. [Persian] [Link]
17. Gammage KL, Klentrou P. Predicting osteoporosis prevention behaviors: Health beliefs and knowledge. Am J Health Behav. 2011;35(3):371-82. [Link] [DOI:10.5993/AJHB.35.3.10]
18. Edmonds ET. Osteoporosis knowledge, beliefs, and behaviors of college students: Utilization of the health belief model [dissertation]. Tuscaloosa: The University of Alabama; 2009. [Link]
19. Tsai M. The relationship between osteoporosis knowledge, beliefs and dietary calcium intake among South Asian women in Auckland [dissertation]. Auckland: Massey University; 2008. [Link]
20. Swaim RA, Barner JC, Brown CM. The relationship of calcium intake and exercise to osteoporosis health beliefs in postmenopausal women. Res Soc Administr Pharm. 2008;4(2):153-63. [Link] [DOI:10.1016/j.sapharm.2007.03.004]
21. Vahedian-Shahroodi M, Lael-Monfared E, Esmaily H, Tehrani H, Mohaddes-Hakkak H. Prediction of osteoporosis preventive behaviors using the health belief model. Iran J Health Educ Health Promot. 2014;2(3):199-207. [Persian] [Link]
22. Wallace LS. Osteoporosis prevention in college women: Application of the expanded health belief model. Am J Health Behav. 2002;26(3):163-72. [Link] [DOI:10.5993/AJHB.26.3.1]
23. Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the osteoporosis health belief scale. Res Nurs Health. 1991;14(2):155-63. [Link] [DOI:10.1002/nur.4770140210]
24. Sedlak CA, Doheny MO, Estok PJ, Zeller RA, Winchell J. DXA, health beliefs, and osteoporosis prevention behaviors. J Aging Health. 2007;19(5):742-56. [Link] [DOI:10.1177/0898264307304303]
25. Kang S, Kim YA. Predictors of osteoporosis prevention behaviors in women in their 20s and 30s. Medicine. 2022;101(27):e29260. [Link] [DOI:10.1097/MD.0000000000029260]
26. Jeihooni AK, Hidarnia A, Kaveh MH, Hajizadeh E, Askari A. The effect of an educational program based on health belief model on preventing osteoporosis in women. Int J Prev Med. 2015;6:115. [Link] [DOI:10.4103/2008-7802.170429]
27. Hazavehei SM, Taghdisi MH, Saidi M. Application of the health belief model for osteoporosis prevention among middle school girl students, Garmsar, Iran. Educ Health. 2007;20(1):23. [Link] [DOI:10.4103/1357-6283.101628]
28. Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: Application of the health belief model. J Nutr Educ Behav. 2003;35(5):260-7. [Link] [DOI:10.1016/S1499-4046(06)60057-2]
29. Al Seraty WH, Ali WG. The impacts of health belief model based intervention for osteoporosis prevention among female students in Al Dawadmi Applied Medical Science, Shaqraa University, Saudi Arabia. J Biol Agric Healthc. 2014;4(7):125-31. [Link]
30. Anderson KD, Chad KE, Spink KS. Osteoporosis knowledge, beliefs, and practices among adolescent females. J Adolesc Health. 2005;36(4):305-12. [Link] [DOI:10.1016/j.jadohealth.2004.03.007]
31. Ievers-Landis CE, Burant C, Drotar D, Morgan L, Trapl ES, Kwoh CK. Social support, knowledge, and self-efficacy as correlates of osteoporosis preventive behaviors among preadolescent females. J Pediatr Psychol. 2003;28(5):335-45. [Link] [DOI:10.1093/jpepsy/jsg023]
32. Sharma SV, Hoelscher DM, Kelder SH, Day RS, Hergenroeder A. Psychosocial, environmental and behavioral factors associated with bone health in middle-school girls. Health Educ Res. 2009;24(2):173-84. [Link] [DOI:10.1093/her/cyn009]
33. Larson NI, Story M, Wall M, Neumark-Sztainer D. Calcium and dairy intakes of adolescents are associated with their home environment, taste preferences, personal health beliefs, and meal patterns. J Am Diet Assoc. 2006;106(11):1816-24. [Link] [DOI:10.1016/j.jada.2006.08.018]
34. Vue H, Reicks M. Individual and environmental influences on intake of calcium-rich food and beverages by young Hmong adolescent girls. J Nutr Educ Behav. 2007;39(5):264-72. [Link] [DOI:10.1016/j.jneb.2007.03.092]
35. Khani Jeihooni A, Askari A, Kashfi SM, Khiyali Z, Kashfi SH, Safari O, et al. Application of health belief model in prevention of osteoporosis among primary school girl students. J Pediatr Perspect. 2017;5(11):6017-29. [Link]
36. Auld G, Boushey CJ, Bock MA, Bruhn C, Gabel K, Gustafson D, et al. Perspectives on intake of calcium-rich foods among Asian, Hispanic, and white preadolescent and adolescent females. J Nutr Educ Behav. 2002;34(5):242-51. [Link] [DOI:10.1016/S1499-4046(06)60102-4]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |