Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 487-494 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kasjono H, Yamtana Y, Istiqomah S, Sintawati R, Wardoyo S. Empowerment Model for Batik Home Industry Workers in Eliminating Tuberculosis in Pandak, Bantul, Indonesia. Health Educ Health Promot 2024; 12 (3) :487-494
URL: http://hehp.modares.ac.ir/article-5-76042-en.html
URL: http://hehp.modares.ac.ir/article-5-76042-en.html
1- Department of Environmental Health, Politeknik Kesehatan Kemenkes Yogyakarta, Yogyakarta, Indonesia
2- Departement of Environmental Health, Politeknik Kesehatan Kemenkes Surabaya, Surabaya Special Region, Indonesia
2- Departement of Environmental Health, Politeknik Kesehatan Kemenkes Surabaya, Surabaya Special Region, Indonesia
Full-Text [PDF 617 kb]
(2968 Downloads)
| Abstract (HTML) (877 Views)
Full-Text: (97 Views)
Introduction
Tuberculosis (TB) is a chronic bacterial disease primarily caused by Mycobacterium tuberculosis, which spreads from person to person through the inhalation of respiratory droplets [1, 2]. TB manifests in two forms, including pulmonary (85%) and extra-pulmonary [2]. TB is a deadly bacterial infection [3], ranking as the second leading infectious killer after COVID-19, with an estimated 2 billion people infected and 1.3 million deaths globally in 2020 [4, 5]. Indonesia ranks third in the world for TB-related health problems. The incidence rate of TB in Indonesia in 2021 was 385,295 cases per 100,000 population, while the mortality rate for TB patients was 40 per 100,000 population [6, 7].
According to Garcia et al., informal workers are likely to suffer from infectious diseases, one of which is pulmonary TB. The influence of the environment, particularly a poor work environment, can lead to infectious diseases, including pulmonary TB. Globally, there are approximately 2 billion (61%) workers engaged in the informal economy [3]. The Central Bureau of Statistics (BPS) reported in February 2024 that the Indonesian population working in the informal sector was 84.13 million people (51.17%) [6]. Informal sector workers are often not fully covered by occupational health and safety (OHS) regulations and labor laws, resulting in inadequate hazard control in their work environments and exposing them to higher occupational health risks [7].
The batik home industry is a form of industry that operates within the informal sector. The small and medium industry in the batik handicraft sector in the Bantul region is capable of absorbing a workforce of 2,056 batik makers. According to the latest data on batik small and medium industries (SMIs) in the Bantul region, there are 612 SMIs or batik production houses supported by 2,056 batik makers. Wijirejo Village, located in the Pandak Sub-district of Bantul Regency, is one of the centers of the batik handicraft industry in Yogyakarta. Its products have been widely accepted in the market and have become a source of pride for the community. This industrial center employs a significant number of workers, with around 225 individuals currently involved in batik production. However, it is important to note that the health of the workforce is not yet optimal, despite the presence of a health center that serves as a place for examining workers when they are ill. According to Minister of Manpower Regulation Number 13 of 2022, this regulation addresses the assessment of potential diseases in the workplace, the strengthening of facilities and the competence of TB officers in the workplace, and the implementation of routine TB screenings. Based on this regulation, employers are required to educate their workers on TB prevention and control.
The global End Tuberculosis (TB) Strategy sets an ambitious goal of achieving TB elimination by 2035 [8]. The transition from TB control to TB elimination requires changes in policy, implementation, and capacity, as well as new strategies, new models of empowerment, and increased resources [8]. One of the efforts to achieve TB elimination, particularly in the labor force, involves empowerment initiatives [9]. TB control includes health promotion regarding TB and the factors that increase its risk, with the aim of changing behavior [9, 10].
The application of behavior change to interrupt the transmission of pulmonary TB can utilize a systematic and sustainable method, namely the Iron Fence program, which involves family assistance and applies health coaching to create families that are aware of and alert to TB cases. This method demonstrates promotion as a technique to instill behaviors that can address problems and engage families, thereby fostering adherence to treatment and preventing the transmission of pulmonary TB [11]. Martono et al. indicated that empowering families with the Family Health Promotion Model (FHPM) is a strategy that can enhance family commitment to preventing TB transmission at the family level [12]. The health promotion and health literacy model is an empowerment model designed to increase the independence of TB patients, which positively impacts the recovery rate of TB patients, prevents transmission to family members, and promotes healthy behaviors among patients and their families [13].
Social capital and the health belief model (HBM) are theoretical frameworks used to develop an empowerment model for batik home industry workers in TB elimination. This study aimed to identify the empowerment model of batik home industry workers in tuberculosis elimination that can serve as input regarding the empowerment model for the home industry workforce. The findings of this study are expected to serve as input for the home industry workforce empowerment model, which can subsequently improve employee performance and achieve organizational goals, namely increasing profits for the company [14] and enhancing worker health.
Participants and Methods
This mixed-methods research conducted in Pandak Sub-district, Bantul, Indonesia from July to October 2023, employed a sequential exploratory approach, beginning with a qualitative method that utilized a phenomenological framework to understand the essence of human experiences related to specific phenomena. This method was chosen because the focus of the research was on stakeholders who are directly involved with the TB program in the batik industry area. Data were collected through questionnaires using a total sampling technique from all batik workers (99 people).
Qualitative research was conducted through observations, interviews, and focus group discussions (FGDs) with informants selected using a snowball sampling strategy, involving 11 participants, including batik entrepreneurs, community and religious leaders, and representatives from related agencies. The quantitative method employed a cross-sectional approach, aiming to describe the nature of the situation at the time of the research and to examine the causes of certain symptoms.
Quantitative data analysis was conducted using univariate analysis and path analysis. The results of this qualitative and quantitative analysis were utilized to develop a batik industry labor empowerment model for TB elimination, as recommended by the researcher. The results of this research are presented in the form of descriptions and interview transcripts, with an emphasis on meaning rather than generalization.
Findings
Of the total respondents, 74 (74.75%) were women and 25 (25.25%) were men. The average age of the respondents is 47.63 ± 12.34 years. In terms of education, the majority of respondents had varied educational backgrounds. A total of 24 individuals (24.24%) had completed primary school, while 20 (20.20%) had completed junior secondary school and 19 (19.19%) had completed senior secondary school. The remaining respondents did not complete primary school. Based on marital status, the respondents included 80 married individuals (80.8%), 12 unmarried individuals (12.13%), and seven widows or widowers (7.07%). Regarding home ownership, 68 respondents (68.69%) owned their own houses, while 31 (31.31%) were living in houses owned by their parents. In terms of work experience, respondents’ tenure ranged from 1 year to 43 years, with an average tenure of 14.91 ± 9.98 years.
Perspectives of the batik home industry sector on TB counseling
The results of interviews with four home-based batik entrepreneurs revealed differing perspectives on TB counseling. The first interviewee, a batik entrepreneur, expressed:
"Yes, employers should care about TB for their workers; but there are still those who do not care and are even expelled from the workplace if they are found to have TB, which is unfortunate." (Respondent 1)
The first respondent expressed regret that there are still some employers who do not care about their workers, particularly those who have TB. Employers do not hesitate to threaten these workers with dismissal. This aligns with the data that 96.97% of employees perceive the threat of TB as serious. Conversely, there are employers who support TB counseling programs as a preventive measure. The second and third respondents stated that:
"TB prevention can be done in the workplace so that they can continue to work and be healthy." (Respondent 2)
"In fact, they will continue to produce and be productive if prevention is done in the workplace." (Respondent 3)
The second and third respondents shared similar views, stating that TB prevention efforts can be implemented directly in the workplace for employees, ensuring that productivity continues to run smoothly. However, TB counseling in the batik industry requires more attention in its implementation. Respondent four regarding direction and policy said:
"I think it needs direction and guidance from stakeholders related to TB issues in the workplace. It also needs policy and concern from employers so that after two weeks of being declared TB, they can still work." (Respondent 4)
According to the fourth respondent, TB counseling in batik home industries is not solely the responsibility of employers; it also necessitates the involvement of stakeholders, including community leaders, particularly concerning policies for employees affected by TB. One such policy pertains to the working hours of employees, which should be reinstated after a two-week period.
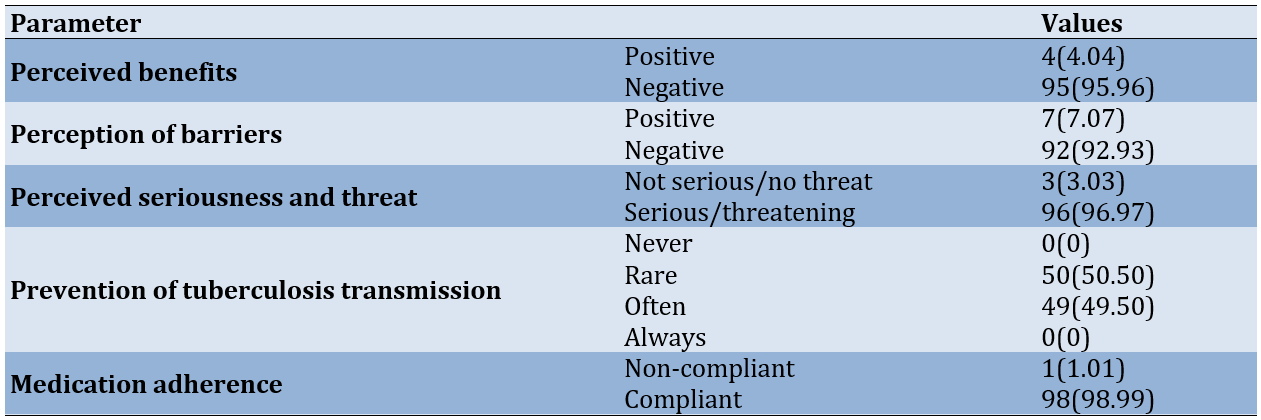
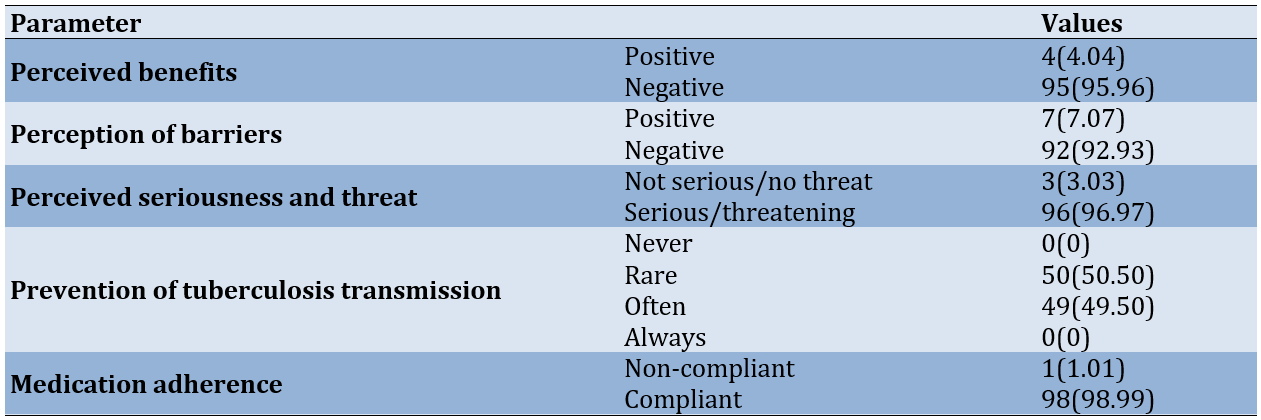
The results of interviews with four batik home industry entrepreneurs are supported by quantitative data, which supports the theory of HBM construction in batik home industry workers at risk of TB (Table 1).
The respondents recognized the seriousness of TB disease as a threat (96.97%). On the other hand, the majority of respondents had a negative perception of the benefits of TB prevention measures (95.96%) and a negative perception of the perceived barriers to TB prevention (92.93%). To overcome these problems, a more effective empowerment model is needed to communicate the benefits of prevention and reduce perceived barriers. One community empowerment intervention is health education, which aims to increase community knowledge and understanding of health behaviors and outcomes [15]. Many health education interventions address the construct of the HBM [16-19]. These face-to-face and video-based interventions are effective in increasing health behaviors (or decreasing risky health behaviors) in people with TB [19-24].
Table 1. Frequency of health belief model (HBM) constructs
The role of government and community institutions in TB counseling
"There is an extension program from the Health Department and especially from the local Puskesmas for TB in the workplace, including batik, but maybe it cannot be routine every week or month." (Bantul Health Department spokesman)
The Bantul Health Department confirmed in its statement that TB counseling had been implemented in various workplaces, but not routinely as expected. The community health center also confirmed its involvement in the implementation of TB counseling, as stated by the spokesperson of the local community health center:
"Yes sir, health two times a year, we do counseling and at the same time evaluation/observation." (Community health center spokesperson)
The community health center also stated that the frequency of implementation of TB counseling is the same as that of the Bantul Health Department, namely twice a year. However, there is a difference in treatment from the local community health center, who conduct observation and evaluation of the batik industry as needed. In addition to the Bantul District Health Department and local health centers, the Bantul Employment Department is also involved in the implementation of TB counseling.
"There is a counseling program from the Manpower Office once a year." (Spokesperson from Bantul Employment Department)
The Bantul Employment Department acknowledged its involvement in TB counseling but in a different timeframe than other parties. That is, once a year for workers in the batik industry. Nevertheless, each party from the government agency is still trying to organize the TB counseling properly. Apart from the government, there are also non-governmental organizations:
"There is a TB health promotion program in the workplace, but in this area only once in early 2024." (Spokesperson of a non-governmental organization)
Non-governmental organizations confirmed that they were also involved in workplace TB counseling, although only once in early 2024. In addition, community leaders are also willing to help implement the TB counseling program, as expressed by the following community leaders:
"I strongly agree with this workplace TB program. But it needs the cooperation of all of us to help each other, including the stakeholders, yes, I am ready to help." (Community leader)
Community leaders agree with the existence of TB counseling and each layer of society must work together in an effort to realize a healthy work environment, including stakeholders, namely government and non-government (Table 2).
Table 2. Frequency of social capital categories
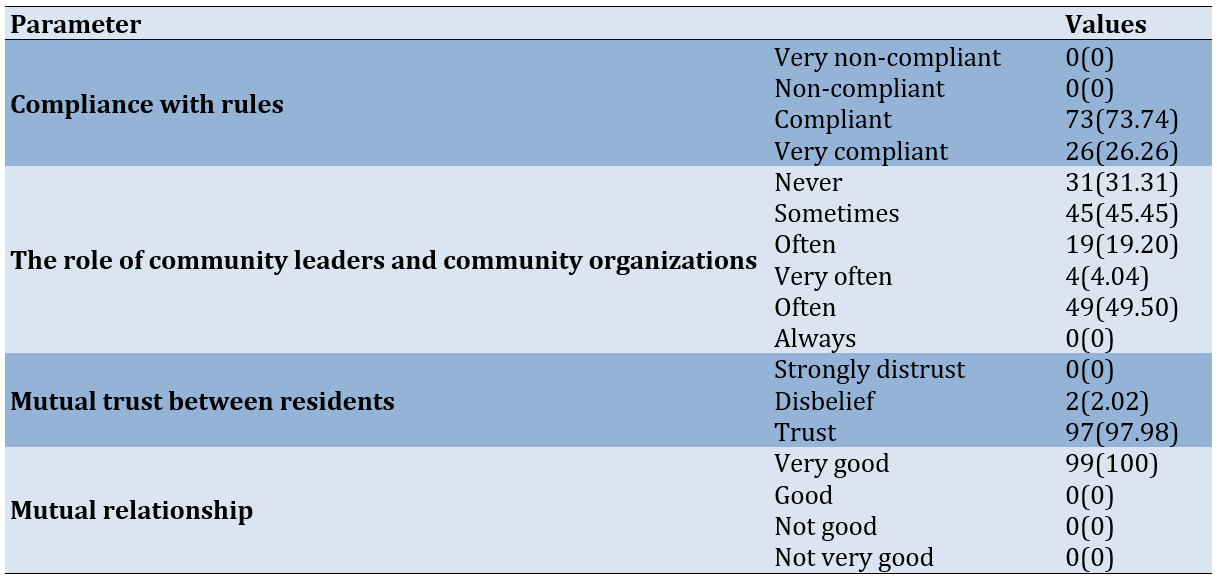
The majority of respondents had a high level of compliance, a strong level of trust among residents, and excellent social relations in the community. This is certainly an important foundation for social capital.
Path analysis results
Path analysis aims to measure the direct and indirect relationships between parameters in the model [25]. The results of the path analysis showed that after the path diagram is made following the research framework, the next step is to identify the model. The model is said to be identified if the degree of freedom value is equal to or greater than zero [26]. The goodness of fit values presented support the alignment between the conceptual model and field data, with a chi-square value of 6.470 and a probability of 0.373, as well as an RMSEA of 0.028, indicating that the model is a good fit and can be used to explain the relationships between parameters. Thus, this appropriate model is used to answer the research hypothesis (observation=600; adjusted R-squared =0.601).
TB education and social capital had a significant impact on community attitudes toward TB transmission prevention in the workplace and treatment adherence. The path analysis model indicated that the most effective path in preventing TB transmission in the workplace starts from the perception of readiness or threat to TB with a path coefficient of 0.85, followed by social capital, which directly influenced the perception of readiness or threat to TB with a value of 0.56. Additionally, social capital also significantly affected the perception of the benefits of TB prevention, which subsequently played a role in shaping preventive actions in the workplace. This finding is consistent with previous research, indicating that 81% of respondents agree on the high category of understanding the benefits of TB prevention actions, and 78% positively recognize the level of TB threat [27]. As a result, respondents are willing to engage in TB prevention efforts. Moreover, a study by Zhi-Juan et al. on health education among middle school students in Shanghai showed that the greatest impact is on the perception of threats related to school injuries following the intervention [28]. On the other hand, threat perception is positively related to preventive behavior, thereby mediating the relationship between perceived seriousness/threat and disease prevention behavior [29]. According to the HBM, the perception of barriers explains that the higher the barriers faced, the more they affect an individual's willingness to prevent disease transmission [27]. Based on the results of the path analysis and qualitative findings, the final model recommended for empowering batik home industry workers in TB elimination efforts, using a social capital-based approach, shows a strong connection between several key parameters. Social capital and TB education directly influenced workers' perceptions of TB prevention and treatment adherence (Figure 1).
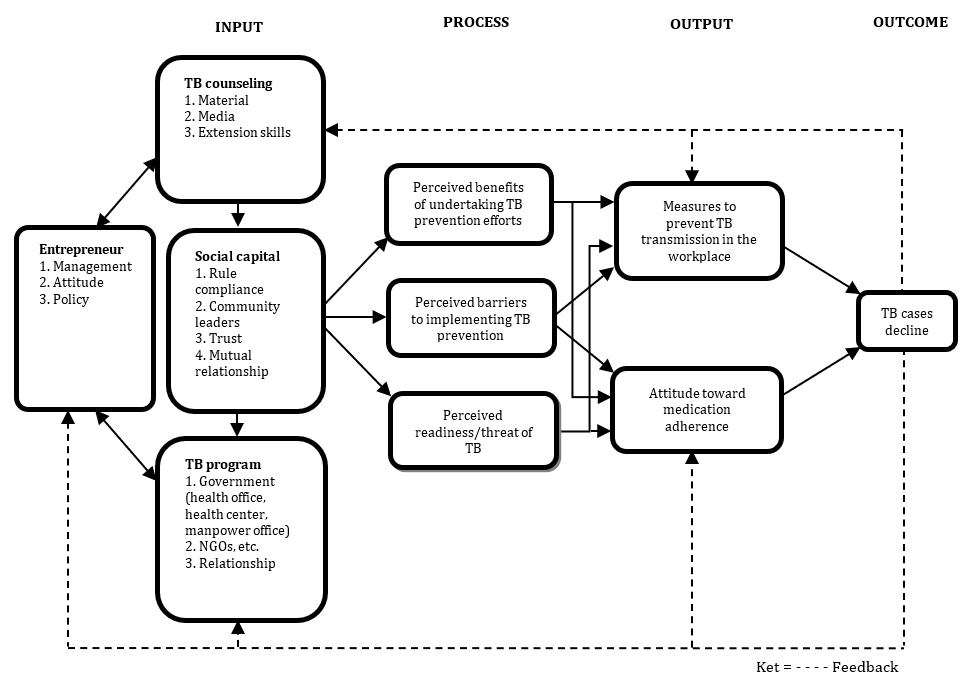
Figure 1. Empowerment model based on social capital, tuberculosis (TB) program, TB counseling, and health belief model
Discussion
This study aimed to identify the empowerment model of batik home industry workers in tuberculosis elimination that can serve as input regarding the empowerment model for the home industry workforce. The findings of this study emphasize the importance of TB prevention efforts in the home-based batik industry, with clear implications for worker health. The high level of seriousness regarding the TB threat among workers indicates the need for greater awareness of this risk. This is especially relevant because workplaces in the manufacturing sector are a key focus in national TB control programs, particularly in countries with a high TB burden, such as Bangladesh, which reported a TB prevalence of 402 cases (all forms, including PTB and non-PTB) and an incidence of 224 per 100,000 annually in 2013 [30, 31]. However, despite this awareness, the low perception of the benefits of TB prevention, and the perception of barriers, reveal a gap between knowledge and action. A study conducted in the garment industry in Bangladesh found that barriers to TB prevention efforts include a lack of time to participate in TB prevention programs [30]. This comparison demonstrates that simply raising awareness is insufficient without addressing structural barriers, such as working conditions, access to healthcare, and employer support.
The role of social capital, particularly compliance with workplace regulations and the involvement of community leaders, was highly significant in this study, as it provided a support system that could enhance TB prevention efforts. This aligns with research conducted in Nigeria, which found that a crucial aspect of the intervention is the strong involvement of community leaders who facilitate the implementation of these interventions. The engagement of local leaders to address community resistance has been noted as a key consideration for interventions and is an important step in creating effective health initiatives in Nigeria [32]. Additionally, social capital in the form of trust and mutual relationships significantly impacts workers’ actions in TB prevention. These findings are consistent with those of Khan et al., who demonstrated that financial incentives are not always the primary motivator for community health workers. Instead, intrinsic motivation, derived from moral or religious factors (such as the desire to help others), can play a significant role [33].
Successful education, utilizing relevant materials and effective methods, can increase workers’ awareness of the importance of TB prevention and strengthen their perception of the benefits of preventive measures. Previous research has identified perceived benefits as a key factor in preventive behavior [34]. Support from social capital, including compliance with regulations and the involvement of community leaders, helps reduce barriers and increases individual motivation. This is consistent with findings that indicate social capital can mediate the relationship between psychological capital (PsyCap) and preventive behavior [34, 35]. This process promotes better actions in the workplace, such as the use of masks and adherence to health protocols, aligning with studies that demonstrate the critical role of perceived benefits and threats in influencing preventive behavior. Conversely, perceived barriers can reduce the effectiveness of prevention in certain situations [36].
The reduction in TB cases reflects the overall effectiveness of the prevention program and reinforces the importance of involving all elements of the work community to achieve optimal prevention outcomes, as outlined in studies that assess the role of threats and benefits in preventive behavior [35]. Overall, this study contributes to the growing body of evidence that TB prevention in the informal sector requires a multifaceted approach. By integrating health promotion, empowerment strategies, and the active involvement of community and business leaders, we can overcome barriers to TB prevention and improve health outcomes for vulnerable populations. The end result is better prevention and improved treatment adherence, which can ultimately reduce the number of TB cases. This holistic approach emphasizes the importance of engaging all elements of the working community to achieve optimal results.
This study has several limitations that need to be considered. Firstly, despite involving 99 batik industry workers, the results may not be fully representative of the entire population of batik workers in the Pandak sub-district, given the specific characteristics of the sample. Secondly, the negative perceptions toward tuberculosis patients identified in this study may reflect a broader social stigma within the community; however, this study did not explore in depth the social and cultural factors that may influence such perceptions. Additionally, although this study found that social capital plays an important role in worker motivation, the influence of other variables, such as economic conditions, accessibility of health services, and government policies in tuberculosis control, was not analyzed in detail. This limitation is important to consider for future research.
Conclusion
A high level of seriousness regarding the TB threat exists among workers; however, they have a low perception of the benefits of TB prevention and a significant perception of barriers.
Acknowledgments: The authors express their deepest gratitude to all parties who contributed to the completion of this research.
Ethical Permissions: Ethical clearance was granted by the Health Research Ethics Committee of the Health Polytechnic of the Ministry of Health Yogyakarta. The researcher obtained informed consent from the respondents, explaining the purpose, objectives, benefits, and potential impacts of the study, and ensured that participation was voluntary.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Kasjono HS (First Author), Methodologist/Main Researcher (35%); Yamtana Y (Second Author), Main Researcher (20%); Istiqomah SH (Third Author), Main Researcher (20%); Sintawati RE (Fourth Author), Assistant Researcher (15%); Wardoyo S (Fifth Author), Assistant Researcher (10%)
Funding/Support: This study received no funding.
Tuberculosis (TB) is a chronic bacterial disease primarily caused by Mycobacterium tuberculosis, which spreads from person to person through the inhalation of respiratory droplets [1, 2]. TB manifests in two forms, including pulmonary (85%) and extra-pulmonary [2]. TB is a deadly bacterial infection [3], ranking as the second leading infectious killer after COVID-19, with an estimated 2 billion people infected and 1.3 million deaths globally in 2020 [4, 5]. Indonesia ranks third in the world for TB-related health problems. The incidence rate of TB in Indonesia in 2021 was 385,295 cases per 100,000 population, while the mortality rate for TB patients was 40 per 100,000 population [6, 7].
According to Garcia et al., informal workers are likely to suffer from infectious diseases, one of which is pulmonary TB. The influence of the environment, particularly a poor work environment, can lead to infectious diseases, including pulmonary TB. Globally, there are approximately 2 billion (61%) workers engaged in the informal economy [3]. The Central Bureau of Statistics (BPS) reported in February 2024 that the Indonesian population working in the informal sector was 84.13 million people (51.17%) [6]. Informal sector workers are often not fully covered by occupational health and safety (OHS) regulations and labor laws, resulting in inadequate hazard control in their work environments and exposing them to higher occupational health risks [7].
The batik home industry is a form of industry that operates within the informal sector. The small and medium industry in the batik handicraft sector in the Bantul region is capable of absorbing a workforce of 2,056 batik makers. According to the latest data on batik small and medium industries (SMIs) in the Bantul region, there are 612 SMIs or batik production houses supported by 2,056 batik makers. Wijirejo Village, located in the Pandak Sub-district of Bantul Regency, is one of the centers of the batik handicraft industry in Yogyakarta. Its products have been widely accepted in the market and have become a source of pride for the community. This industrial center employs a significant number of workers, with around 225 individuals currently involved in batik production. However, it is important to note that the health of the workforce is not yet optimal, despite the presence of a health center that serves as a place for examining workers when they are ill. According to Minister of Manpower Regulation Number 13 of 2022, this regulation addresses the assessment of potential diseases in the workplace, the strengthening of facilities and the competence of TB officers in the workplace, and the implementation of routine TB screenings. Based on this regulation, employers are required to educate their workers on TB prevention and control.
The global End Tuberculosis (TB) Strategy sets an ambitious goal of achieving TB elimination by 2035 [8]. The transition from TB control to TB elimination requires changes in policy, implementation, and capacity, as well as new strategies, new models of empowerment, and increased resources [8]. One of the efforts to achieve TB elimination, particularly in the labor force, involves empowerment initiatives [9]. TB control includes health promotion regarding TB and the factors that increase its risk, with the aim of changing behavior [9, 10].
The application of behavior change to interrupt the transmission of pulmonary TB can utilize a systematic and sustainable method, namely the Iron Fence program, which involves family assistance and applies health coaching to create families that are aware of and alert to TB cases. This method demonstrates promotion as a technique to instill behaviors that can address problems and engage families, thereby fostering adherence to treatment and preventing the transmission of pulmonary TB [11]. Martono et al. indicated that empowering families with the Family Health Promotion Model (FHPM) is a strategy that can enhance family commitment to preventing TB transmission at the family level [12]. The health promotion and health literacy model is an empowerment model designed to increase the independence of TB patients, which positively impacts the recovery rate of TB patients, prevents transmission to family members, and promotes healthy behaviors among patients and their families [13].
Social capital and the health belief model (HBM) are theoretical frameworks used to develop an empowerment model for batik home industry workers in TB elimination. This study aimed to identify the empowerment model of batik home industry workers in tuberculosis elimination that can serve as input regarding the empowerment model for the home industry workforce. The findings of this study are expected to serve as input for the home industry workforce empowerment model, which can subsequently improve employee performance and achieve organizational goals, namely increasing profits for the company [14] and enhancing worker health.
Participants and Methods
This mixed-methods research conducted in Pandak Sub-district, Bantul, Indonesia from July to October 2023, employed a sequential exploratory approach, beginning with a qualitative method that utilized a phenomenological framework to understand the essence of human experiences related to specific phenomena. This method was chosen because the focus of the research was on stakeholders who are directly involved with the TB program in the batik industry area. Data were collected through questionnaires using a total sampling technique from all batik workers (99 people).
Qualitative research was conducted through observations, interviews, and focus group discussions (FGDs) with informants selected using a snowball sampling strategy, involving 11 participants, including batik entrepreneurs, community and religious leaders, and representatives from related agencies. The quantitative method employed a cross-sectional approach, aiming to describe the nature of the situation at the time of the research and to examine the causes of certain symptoms.
Quantitative data analysis was conducted using univariate analysis and path analysis. The results of this qualitative and quantitative analysis were utilized to develop a batik industry labor empowerment model for TB elimination, as recommended by the researcher. The results of this research are presented in the form of descriptions and interview transcripts, with an emphasis on meaning rather than generalization.
Findings
Of the total respondents, 74 (74.75%) were women and 25 (25.25%) were men. The average age of the respondents is 47.63 ± 12.34 years. In terms of education, the majority of respondents had varied educational backgrounds. A total of 24 individuals (24.24%) had completed primary school, while 20 (20.20%) had completed junior secondary school and 19 (19.19%) had completed senior secondary school. The remaining respondents did not complete primary school. Based on marital status, the respondents included 80 married individuals (80.8%), 12 unmarried individuals (12.13%), and seven widows or widowers (7.07%). Regarding home ownership, 68 respondents (68.69%) owned their own houses, while 31 (31.31%) were living in houses owned by their parents. In terms of work experience, respondents’ tenure ranged from 1 year to 43 years, with an average tenure of 14.91 ± 9.98 years.
Perspectives of the batik home industry sector on TB counseling
The results of interviews with four home-based batik entrepreneurs revealed differing perspectives on TB counseling. The first interviewee, a batik entrepreneur, expressed:
"Yes, employers should care about TB for their workers; but there are still those who do not care and are even expelled from the workplace if they are found to have TB, which is unfortunate." (Respondent 1)
The first respondent expressed regret that there are still some employers who do not care about their workers, particularly those who have TB. Employers do not hesitate to threaten these workers with dismissal. This aligns with the data that 96.97% of employees perceive the threat of TB as serious. Conversely, there are employers who support TB counseling programs as a preventive measure. The second and third respondents stated that:
"TB prevention can be done in the workplace so that they can continue to work and be healthy." (Respondent 2)
"In fact, they will continue to produce and be productive if prevention is done in the workplace." (Respondent 3)
The second and third respondents shared similar views, stating that TB prevention efforts can be implemented directly in the workplace for employees, ensuring that productivity continues to run smoothly. However, TB counseling in the batik industry requires more attention in its implementation. Respondent four regarding direction and policy said:
"I think it needs direction and guidance from stakeholders related to TB issues in the workplace. It also needs policy and concern from employers so that after two weeks of being declared TB, they can still work." (Respondent 4)
According to the fourth respondent, TB counseling in batik home industries is not solely the responsibility of employers; it also necessitates the involvement of stakeholders, including community leaders, particularly concerning policies for employees affected by TB. One such policy pertains to the working hours of employees, which should be reinstated after a two-week period.
The results of interviews with four batik home industry entrepreneurs are supported by quantitative data, which supports the theory of HBM construction in batik home industry workers at risk of TB (Table 1).
The respondents recognized the seriousness of TB disease as a threat (96.97%). On the other hand, the majority of respondents had a negative perception of the benefits of TB prevention measures (95.96%) and a negative perception of the perceived barriers to TB prevention (92.93%). To overcome these problems, a more effective empowerment model is needed to communicate the benefits of prevention and reduce perceived barriers. One community empowerment intervention is health education, which aims to increase community knowledge and understanding of health behaviors and outcomes [15]. Many health education interventions address the construct of the HBM [16-19]. These face-to-face and video-based interventions are effective in increasing health behaviors (or decreasing risky health behaviors) in people with TB [19-24].
Table 1. Frequency of health belief model (HBM) constructs
The role of government and community institutions in TB counseling
"There is an extension program from the Health Department and especially from the local Puskesmas for TB in the workplace, including batik, but maybe it cannot be routine every week or month." (Bantul Health Department spokesman)
The Bantul Health Department confirmed in its statement that TB counseling had been implemented in various workplaces, but not routinely as expected. The community health center also confirmed its involvement in the implementation of TB counseling, as stated by the spokesperson of the local community health center:
"Yes sir, health two times a year, we do counseling and at the same time evaluation/observation." (Community health center spokesperson)
The community health center also stated that the frequency of implementation of TB counseling is the same as that of the Bantul Health Department, namely twice a year. However, there is a difference in treatment from the local community health center, who conduct observation and evaluation of the batik industry as needed. In addition to the Bantul District Health Department and local health centers, the Bantul Employment Department is also involved in the implementation of TB counseling.
"There is a counseling program from the Manpower Office once a year." (Spokesperson from Bantul Employment Department)
The Bantul Employment Department acknowledged its involvement in TB counseling but in a different timeframe than other parties. That is, once a year for workers in the batik industry. Nevertheless, each party from the government agency is still trying to organize the TB counseling properly. Apart from the government, there are also non-governmental organizations:
"There is a TB health promotion program in the workplace, but in this area only once in early 2024." (Spokesperson of a non-governmental organization)
Non-governmental organizations confirmed that they were also involved in workplace TB counseling, although only once in early 2024. In addition, community leaders are also willing to help implement the TB counseling program, as expressed by the following community leaders:
"I strongly agree with this workplace TB program. But it needs the cooperation of all of us to help each other, including the stakeholders, yes, I am ready to help." (Community leader)
Community leaders agree with the existence of TB counseling and each layer of society must work together in an effort to realize a healthy work environment, including stakeholders, namely government and non-government (Table 2).
Table 2. Frequency of social capital categories
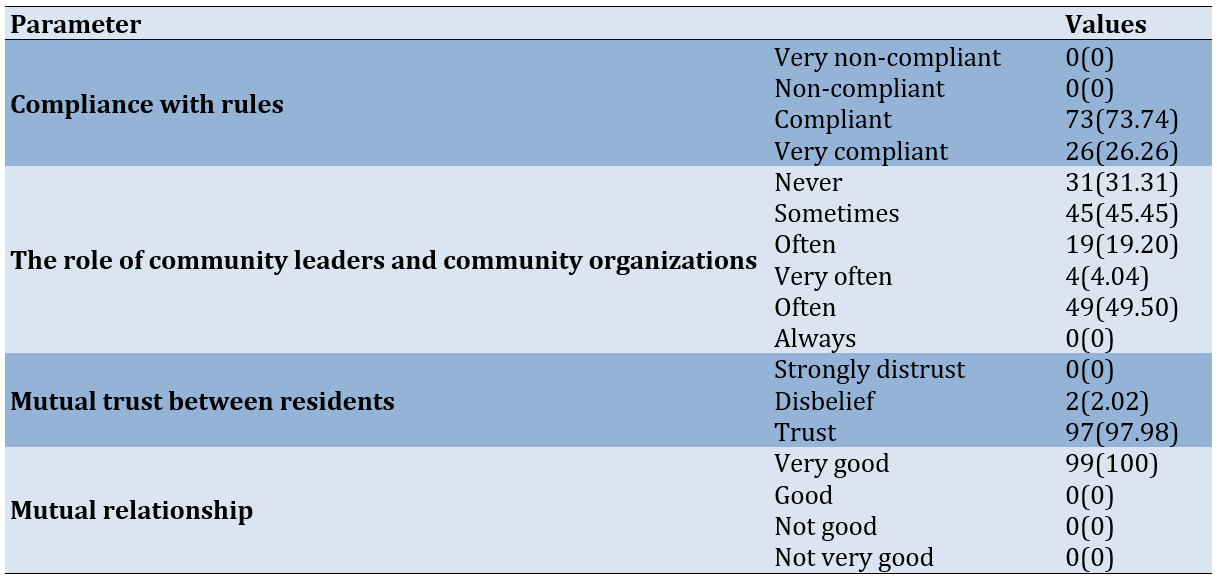
The majority of respondents had a high level of compliance, a strong level of trust among residents, and excellent social relations in the community. This is certainly an important foundation for social capital.
Path analysis results
Path analysis aims to measure the direct and indirect relationships between parameters in the model [25]. The results of the path analysis showed that after the path diagram is made following the research framework, the next step is to identify the model. The model is said to be identified if the degree of freedom value is equal to or greater than zero [26]. The goodness of fit values presented support the alignment between the conceptual model and field data, with a chi-square value of 6.470 and a probability of 0.373, as well as an RMSEA of 0.028, indicating that the model is a good fit and can be used to explain the relationships between parameters. Thus, this appropriate model is used to answer the research hypothesis (observation=600; adjusted R-squared =0.601).
TB education and social capital had a significant impact on community attitudes toward TB transmission prevention in the workplace and treatment adherence. The path analysis model indicated that the most effective path in preventing TB transmission in the workplace starts from the perception of readiness or threat to TB with a path coefficient of 0.85, followed by social capital, which directly influenced the perception of readiness or threat to TB with a value of 0.56. Additionally, social capital also significantly affected the perception of the benefits of TB prevention, which subsequently played a role in shaping preventive actions in the workplace. This finding is consistent with previous research, indicating that 81% of respondents agree on the high category of understanding the benefits of TB prevention actions, and 78% positively recognize the level of TB threat [27]. As a result, respondents are willing to engage in TB prevention efforts. Moreover, a study by Zhi-Juan et al. on health education among middle school students in Shanghai showed that the greatest impact is on the perception of threats related to school injuries following the intervention [28]. On the other hand, threat perception is positively related to preventive behavior, thereby mediating the relationship between perceived seriousness/threat and disease prevention behavior [29]. According to the HBM, the perception of barriers explains that the higher the barriers faced, the more they affect an individual's willingness to prevent disease transmission [27]. Based on the results of the path analysis and qualitative findings, the final model recommended for empowering batik home industry workers in TB elimination efforts, using a social capital-based approach, shows a strong connection between several key parameters. Social capital and TB education directly influenced workers' perceptions of TB prevention and treatment adherence (Figure 1).
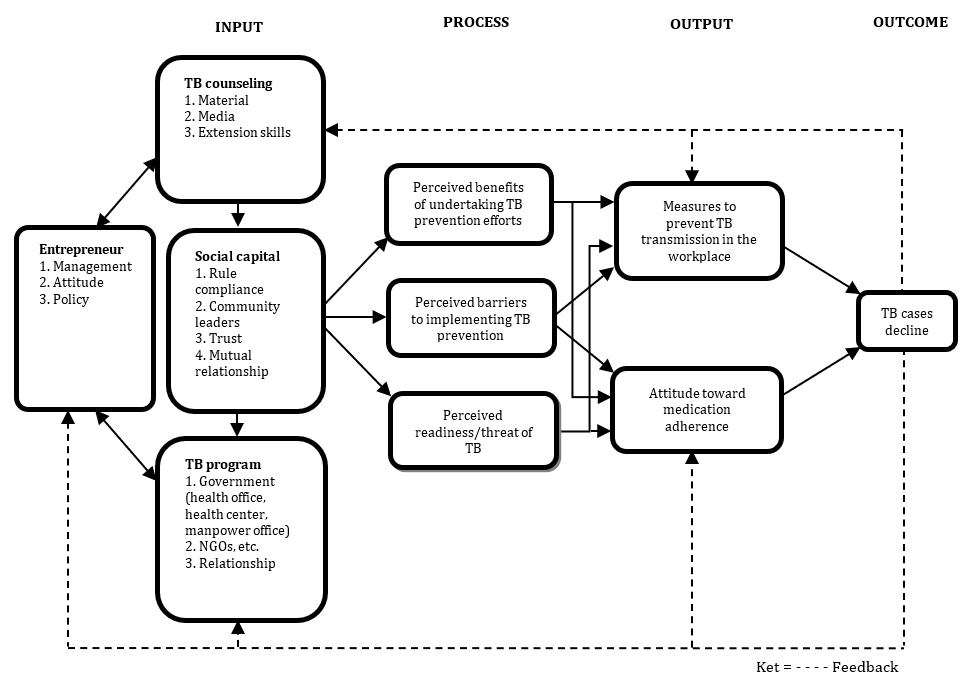
Figure 1. Empowerment model based on social capital, tuberculosis (TB) program, TB counseling, and health belief model
Discussion
This study aimed to identify the empowerment model of batik home industry workers in tuberculosis elimination that can serve as input regarding the empowerment model for the home industry workforce. The findings of this study emphasize the importance of TB prevention efforts in the home-based batik industry, with clear implications for worker health. The high level of seriousness regarding the TB threat among workers indicates the need for greater awareness of this risk. This is especially relevant because workplaces in the manufacturing sector are a key focus in national TB control programs, particularly in countries with a high TB burden, such as Bangladesh, which reported a TB prevalence of 402 cases (all forms, including PTB and non-PTB) and an incidence of 224 per 100,000 annually in 2013 [30, 31]. However, despite this awareness, the low perception of the benefits of TB prevention, and the perception of barriers, reveal a gap between knowledge and action. A study conducted in the garment industry in Bangladesh found that barriers to TB prevention efforts include a lack of time to participate in TB prevention programs [30]. This comparison demonstrates that simply raising awareness is insufficient without addressing structural barriers, such as working conditions, access to healthcare, and employer support.
The role of social capital, particularly compliance with workplace regulations and the involvement of community leaders, was highly significant in this study, as it provided a support system that could enhance TB prevention efforts. This aligns with research conducted in Nigeria, which found that a crucial aspect of the intervention is the strong involvement of community leaders who facilitate the implementation of these interventions. The engagement of local leaders to address community resistance has been noted as a key consideration for interventions and is an important step in creating effective health initiatives in Nigeria [32]. Additionally, social capital in the form of trust and mutual relationships significantly impacts workers’ actions in TB prevention. These findings are consistent with those of Khan et al., who demonstrated that financial incentives are not always the primary motivator for community health workers. Instead, intrinsic motivation, derived from moral or religious factors (such as the desire to help others), can play a significant role [33].
Successful education, utilizing relevant materials and effective methods, can increase workers’ awareness of the importance of TB prevention and strengthen their perception of the benefits of preventive measures. Previous research has identified perceived benefits as a key factor in preventive behavior [34]. Support from social capital, including compliance with regulations and the involvement of community leaders, helps reduce barriers and increases individual motivation. This is consistent with findings that indicate social capital can mediate the relationship between psychological capital (PsyCap) and preventive behavior [34, 35]. This process promotes better actions in the workplace, such as the use of masks and adherence to health protocols, aligning with studies that demonstrate the critical role of perceived benefits and threats in influencing preventive behavior. Conversely, perceived barriers can reduce the effectiveness of prevention in certain situations [36].
The reduction in TB cases reflects the overall effectiveness of the prevention program and reinforces the importance of involving all elements of the work community to achieve optimal prevention outcomes, as outlined in studies that assess the role of threats and benefits in preventive behavior [35]. Overall, this study contributes to the growing body of evidence that TB prevention in the informal sector requires a multifaceted approach. By integrating health promotion, empowerment strategies, and the active involvement of community and business leaders, we can overcome barriers to TB prevention and improve health outcomes for vulnerable populations. The end result is better prevention and improved treatment adherence, which can ultimately reduce the number of TB cases. This holistic approach emphasizes the importance of engaging all elements of the working community to achieve optimal results.
This study has several limitations that need to be considered. Firstly, despite involving 99 batik industry workers, the results may not be fully representative of the entire population of batik workers in the Pandak sub-district, given the specific characteristics of the sample. Secondly, the negative perceptions toward tuberculosis patients identified in this study may reflect a broader social stigma within the community; however, this study did not explore in depth the social and cultural factors that may influence such perceptions. Additionally, although this study found that social capital plays an important role in worker motivation, the influence of other variables, such as economic conditions, accessibility of health services, and government policies in tuberculosis control, was not analyzed in detail. This limitation is important to consider for future research.
Conclusion
A high level of seriousness regarding the TB threat exists among workers; however, they have a low perception of the benefits of TB prevention and a significant perception of barriers.
Acknowledgments: The authors express their deepest gratitude to all parties who contributed to the completion of this research.
Ethical Permissions: Ethical clearance was granted by the Health Research Ethics Committee of the Health Polytechnic of the Ministry of Health Yogyakarta. The researcher obtained informed consent from the respondents, explaining the purpose, objectives, benefits, and potential impacts of the study, and ensured that participation was voluntary.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Kasjono HS (First Author), Methodologist/Main Researcher (35%); Yamtana Y (Second Author), Main Researcher (20%); Istiqomah SH (Third Author), Main Researcher (20%); Sintawati RE (Fourth Author), Assistant Researcher (15%); Wardoyo S (Fifth Author), Assistant Researcher (10%)
Funding/Support: This study received no funding.
Article Type: Qualitative Research |
Subject:
Health Education and Health Behavior
Received: 2024/07/11 | Accepted: 2024/09/29 | Published: 2024/10/20
Received: 2024/07/11 | Accepted: 2024/09/29 | Published: 2024/10/20
References
1. Yulanda NA, Maulana MA, Priyono D. Application of the health promotion model as an effort to combat tuberculosis patients in Punggur Kapuas village, Sungai Kakap district, Kubu Raya regency, West Kalimantan. PENGABDIANMU J Community Serv. 2020;5(3):224-31. [Indonesian] [Link] [DOI:10.33084/pengabdianmu.v5i2.1078]
2. Heydari A, Shadan MR, Miri A, Khoushabi F. The effects of health belief model (HBM) based on health education and food advised on the promotion of self-care behaviors in tuberculosis patients. Sch Res Libr. 2017;9(5):60-72. [Link]
3. Garcia R, Spiegel JM, Yassi A, Ehrlich R, Romão P, Nunes EA, et al. Preventing occupational tuberculosis in health workers: An analysis of state responsibilities and worker rights in Mozambique. Int J Environ Res Public Health. 2020;17(20):7546. [Link] [DOI:10.3390/ijerph17207546]
4. WHO. Global tuberculosis report 2021. Geneva: World Health Organization; 2021. [Link]
5. Cohen A, Mathiasen VD, Schön T, Wejse C. The global prevalence of latent tuberculosis: A systematic review and meta-analysis. Eur Respir J. 2019;54(3):1900655. [Link] [DOI:10.1183/13993003.00655-2019]
6. BPS. Labor force situation in Indonesia February 2024. Jakarta: BPS-Statistics Indonesia; 2024. [Indonesian] [Link]
7. Ko Ko T, Dickson-Gomez J, Yasmeen G, Han WW, Quinn K, Beyer K, et al. Informal workplaces and their comparative effects on the health of street vendors and home-based garment workers in Yangon, Myanmar: A qualitative study. BMC Public Health. 2020;20:524. [Link] [DOI:10.1186/s12889-020-08624-6]
8. Main S, Lestari T, Triasih R, Chan G, Davidson L, Majumdar S, et al. Training for tuberculosis elimination in Indonesia: Achievements, reflections, and potential for impact. Trop Med Infect Dis. 2019;4(3):107. [Link] [DOI:10.3390/tropicalmed4030107]
9. Fukuyama F. Social capital and civil society. Washington, D.C.: International Monetary Fund; 1999. [Link] [DOI:10.2139/ssrn.879582]
10. Hargreaves JR, Boccia D, Evans CA, Adato M, Petticrew M, Porter JDH. The social determinants of tuberculosis: From evidence to action. Am J Public Health. 2011;101(4):654-62. [Link] [DOI:10.2105/AJPH.2010.199505]
11. Has EMM, Ulfiana E, Krisnana I, Arief YS, Mufidah A, Fathoni M. The iron fence program (assistance for tuberculosis-aware and alert families) to achieve zero TB cases by 2020 in the working area of Klampis Ngasem Health Center, Surabaya City. J Community Serv Health. 2020;2(2):36-41. [Indonesian] [Link] [DOI:10.20473/jpmk.v2i2.20798]
12. Martono M, Akhyar M, Pamungkasari EP, Lestari A, Lestari A, Anantanyu S, et al. Implementation of the family health promotion model (FHPM) on family commitment in TB transmission preventive action among the heads of familiesof TB patients: A structural model. Proc Int Conf Nurs Health Sci. 2023;4(1):31-44. [Link] [DOI:10.37287/picnhs.v4i1.1679]
13. Khariroh S, Soedirham O, Hamidah H, Abdullah E. Model of empowerment to improve autonomy directly observed treatment (DOT) tuberculosis patients. Int J Public Health Sci. 2016;5(2):164-9. [Link] [DOI:10.11591/ijphs.v5i2.4781]
14. Hughes M, Perrons RK. Shaping and re-shaping social capital in buyer-supplier relationships. J Bus Res. 2011;64(2):164-71. [Link] [DOI:10.1016/j.jbusres.2009.12.009]
15. Ojukwu JU, Stimatze T. Using the health belief model to assess the impact of latent tuberculosis infection health education video towards screening adoption in foreign-born persons living in California. Durham: Research Square; 2024. [Link] [DOI:10.21203/rs.3.rs-3891838/v1]
16. Al Junidel R, Alaqel M, Al Qahtani SH, Ogaiel A, Jammaz AMA, Alshammari S. Using the health belief model to predict the uptake of mammographic screening among Saudi women. Cureus. 2020;12(10):e11121. [Link] [DOI:10.7759/cureus.11121]
17. Gabriel EH, McCann RS, Hoch MC, Cramer RJ. An intervention based on the health belief model led to improvements in self-efficacy towards ERIPP participation and functional performance in club sport athletes: A pilot study. J Sci Med Sport. 2020;23(10):921-6. [Link] [DOI:10.1016/j.jsams.2020.04.002]
18. McArthur LH, Riggs A, Uribe F, Spaulding TJ. Health belief model offers opportunities for designing weight management interventions for college students. J Nutr Educ Behav. 2018;50(5):485-93. [Link] [DOI:10.1016/j.jneb.2017.09.010]
19. Gao J, Cook VJ, Mayhew M. Preventing tuberculosis in a low incidence setting: Evaluation of a multi-lingual, online, educational video on latent tuberculosis. J Immigr Minor Health. 2018;20(3):687-96. [Link] [DOI:10.1007/s10903-017-0601-9]
20. Hatzenbuehler LA, Starke JR, Smith EO, Turner TL, Balmer DF, Arif Z, et al. Increased adolescent knowledge and behavior following a one-time educational intervention about tuberculosis. Patient Educ Couns. 2017;100(5):950-6. [Link] [DOI:10.1016/j.pec.2016.11.020]
21. Massey PD, Asugeni R, Wakageni J, Kekeubata E, Maena'aadi J, Laete'esafi J, et al. Steps on a journey to TB control in Solomon Islands: A cross-sectional, mixed methods pre-post evaluation of a local language DVD. BMC Int Health Hum Rights. 2015;15(1):1. [Link] [DOI:10.1186/s12914-015-0041-3]
22. Reeves H, Grandjean Lapierre S, Razafindrina K, Andriamiadanarivo A, Rakotosamimanana N, Razafindranaivo T, et al. Evaluating the use of educational videos to support the tuberculosis care cascade in remote Madagascar. Int J Tuberc Lung Dis. 2020;24(1):28-35. [Link] [DOI:10.5588/ijtld.19.0161]
23. Wieland ML, Weis JA, Olney MW, Alemán M, Sullivan S, Millington K, et al. Screening for tuberculosis at an adult education center: Results of a community-based participatory process. Am J Public Health. 2011;101(7):1264-7. [Link] [DOI:10.2105/AJPH.2010.300024]
24. Wieland ML, Nelson J, Palmer T, O'Hara C, Weis JA, Nigon JA, et al. Evaluation of a tuberculosis education video among immigrants and refugees at an adult education center: A community-based participatory approach. J Health Commun. 2013;18(3):343-53. [Link] [DOI:10.1080/10810730.2012.727952]
25. Eriksson U, Hochwälder J, Carlsund A, Sellström E. Health outcomes among Swedish children: The role of social capital in the family, school and neighbourhood. Acta Paediatr. 2012;101(5):513-7. [Link] [DOI:10.1111/j.1651-2227.2011.02579.x]
26. Kasjono HS. Health promotion, community empowerment, and social capital. Yogyakarta: NUHA MEDIKA; 2016. [Indonesian] [Link]
27. Supinganto A, Kusrini I, Setyarini A, Amaliah L, Hadi SPI, Budiana I. Efforts to prevent tuberculosis transmission based on the health belief model theory in West Lombok. STRADA Sci J Health. 2020;9(2):1274-84. [Link] [DOI:10.30994/sjik.v9i2.463]
28. Zhi-Juan C, Yue C, Shu-Mei W. Health belief model based evaluation of school health education programme for injury prevention among high school students in the community context. BMC Public Health. 2014;14:26. [Link] [DOI:10.1186/1471-2458-14-26]
29. Sarwar F, Jameel HT, Panatik SA. Understanding public's adoption of preventive behavior during COVID-19 pandemic using health belief model: Role of psychological capital and health appraisals. SAGE Open. 2023;13(3):1-18. [Link] [DOI:10.1177/21582440231192185]
30. Islam QS, Islam MA, Islam S, Ahmed SM. Prevention and control of tuberculosis in workplaces: How knowledgeable are the workers in Bangladesh?. BMC Public Health. 2015;15:1291. [Link] [DOI:10.1186/s12889-015-2622-4]
31. WHO. Global tuberculosis report 2015. Geneva: World Health Organization; 2015. [Link]
32. Eyo AS, Obot VO, Onyedinachi O, Aguilera Vasquez N, Bigio J, Sanaie A, et al. A multi-faceted approach to tuberculosis active case finding among remote riverine communities in southern Nigeria. Int J Environ Res Public Health. 2021;18(18):9424. [Link] [DOI:10.3390/ijerph18189424]
33. Khan MS, Mehboob N, Rahman-Shepherd A, Naureen F, Rashid A, Buzdar N, et al. What can motivate lady health workers in Pakistan to engage more actively in tuberculosis case-finding?. BMC Public Health. 2019;19:999. [Link] [DOI:10.1186/s12889-019-7326-8]
34. Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25(8):661-9. [Link] [DOI:10.1080/10410236.2010.521906]
35. Scherr CL, Jensen JD, Christy K. Dispositional pandemic worry and the health belief model: Promoting vaccination during pandemic events. J Public Health. 2017;39(4):e242-50. [Link] [DOI:10.1093/pubmed/fdw101]
36. Bottemanne H, Morlaas O, Fossati P, Schmidt L. Does the coronavirus epidemic take advantage of human optimism bias?. Front Psychol. 2020;11:2001. [Link] [DOI:10.3389/fpsyg.2020.02001]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |