Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 439-441 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Shadani F, Shahali S, Hosseini F, Bahrampour B. Effect of Yoga on Women’s Sexual Function and Sexual Quality of Life after Vaginal Delivery. Health Educ Health Promot 2024; 12 (3) :439-441
URL: http://hehp.modares.ac.ir/article-5-76009-en.html
URL: http://hehp.modares.ac.ir/article-5-76009-en.html
1- Department of Reproductive Health and Midwifery, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Department of Biostatistics and Epidemiology, Faculty of Occupational Health, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Biostatistics and Epidemiology, Faculty of Occupational Health, Tehran University of Medical Sciences, Tehran, Iran
Keywords: Sexual Dysfunction, Physiological [MeSH], Sexual Dysfunction, Psychological [MeSH], Quality of Life [MeSH], Yoga [MeSH]
Full-Text [PDF 616 kb]
(3179 Downloads)
| Abstract (HTML) (1159 Views)
Full-Text: (206 Views)
Introduction
The World Health Organization defines sexual health as a state of complete physical, mental, and social well-being related to sexuality. This definition encompasses a positive and respectful approach to gender and sexual relations, facilitating healthy and pleasurable sexual experiences free from coercion, discrimination, and violence [1]. It also enhances psychological well-being, emotions, and feelings, while strengthening the relationship between partners [2].
Sexual quality of life is a crucial aspect of sexual health, referring to an individual’s perception of their position in relation to their culture, goals, expectations, standards, and priorities. It reflects how one’s understanding of their sexual life influences their mental state. A fulfilling sex life fosters healthy and effective relationships between couples [3], whereas poor sexual quality can lead to separation or extramarital affairs. Sexual function significantly impacts the overall quality of life [4]. Zare et al. examined the quality of sexual life among 104 women after childbirth, indicating a low quality of sexual life for women following childbirth [5].
Sexual function refers to the body’s reactions during the various stages of the sexual response cycle [6]. Sexual dysfunction is a problem that arises during this cycle and prevents a person from experiencing sexual satisfaction [7]. According to the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), female sexual dysfunction (FSD) is classified into four categories: desire disorder, arousal disorder, female orgasmic disorder, and genito-pelvic pain/penetration disorder [8]. McCabe et al. showed that 10% to 31.7% of men and 21.4% to 50% of women experience sexual dysfunction [9]. According to Banaei et al.’s study involving 432 Iranian women, 31.25% report a lack of sexual desire, 33.13% have difficulty achieving orgasm, and 40% experience pain during sexual intercourse [10].
Pregnancy and childbirth induce biological and psychological changes that can impact sexual function, with evidence suggesting a decline during pregnancy that does not fully recover in the postpartum period [11]. Changes in body shape, sleep deprivation, anxiety, stress, and frequent urination contribute to high rates of sexual dysfunction among postpartum women, both in Iran and globally. In a 2018 study, the prevalence of sexual dysfunction among Iranian postpartum women is 85.95% [10]. According to Gutzeit et al., postpartum dysfunction affects all areas of sexual function, including pain during intercourse, decreased lubrication, lack of orgasm, and reduced sexual desire [11]. While medication can be useful for treating sexual dysfunction, its disadvantages include rejection by women, low efficacy, and side effects.
Yoga is a form of complementary therapy used in both developed and developing countries [12]. Several experimental studies on yoga have found its beneficial effects on various aspects of physical and mental function, demonstrating that yoga can be effective in improving and treating FSD [12-15]. Given that the impact of yoga techniques on sexual function in postpartum women has not yet been assessed, it is unclear whether yoga also influences sexual function in postpartum women or if these techniques affect the sexual quality of life of women after vaginal delivery. Consequently, we aimed to measure the effect of yoga on the sexual function and sexual quality of life of these women.
Materials and Methods
Study design
This parallel randomized controlled trial involved 50 primiparous women who were 8-10 weeks post-vaginal delivery and sought postpartum care or infant vaccination at a health center in Isfahan, Iran, from January 2020 to March 2021.
Inclusion and exclusion criteria
The inclusion criteria were primiparous women of reproductive age who were at least 8-10 weeks postpartum and had resumed sexual intercourse. Participants were exclusively breastfeeding, had no known underlying conditions (infections, psychological disorders, chronic diseases, or COVID-19), and had no history of alcohol or drug use or the use of medications affecting sexual activity. They were not practicing yoga, experienced no complications during labor (e.g., vacuum delivery or prolonged labor), had no history of pelvic surgeries (such as colporrhaphy), did not suffer from severe vaginal tears after delivery, had no postpartum vaginal healing issues, and had no history of infertility, bleeding, or threats of miscarriage during pregnancy or after delivery.
Sampling
After evaluating the eligibility criteria, informed written consent was obtained from all participants, who were then randomized using block randomization with a block size of four. Based on Dhikav et al., which was conducted on the quality of sexual life, and the standard deviations obtained before and after the intervention (S1=8.51 and S2=6.73), and considering the first type error (α=0.05) and the second type error (β=0.2), a sample size of 18 individuals for each group was determined. Considering a 15% attrition rate, a sample of 50 participants (25 cases per group) was considered [12]. It should be noted that in the control group, five women were infected with COVID-19, and two women did not respond to the researcher. In the intervention group, four women were infected with COVID-19, and three women were unwilling to continue the intervention for personal reasons; all of these individuals were excluded. Therefore, each group included 18 cases.
Data collection tools
The Sexual Quality of Life-Female (SQOL-F) Questionnaire and the Female Sexual Function Index (FSFI) were used to measure the women’s sexual quality of life and sexual function.
The SQOL-F, designed by Symonds et al. [16] in 2005, consists of 18 items that cover four areas, including sexual, psychological emotion, sexual and marital satisfaction, self-deprecation, and sexual repression. The total score ranges from 18 to 108, with a higher score indicating a better quality of life. Maasoumi et al. demonstrated high internal consistency and good test-retest reliability, with a Cronbach’s alpha coefficient of 0.73 and an intraclass correlation coefficient (ICC) of 0.88. The average scores for the content validity index (CVI) and content validity ratio (CVR) were 0.91 and 0.84, respectively [17].
The FSFI was developed by Rosen et al. [18] in 2000. It contains 19 questions that measure women’s sexual performance in six areas, including desire, arousal, lubrication, orgasm, sexual satisfaction, and pain. The overall FSFI score ranges from 2 to 36, with a cutoff score 28. A higher score is associated with a lower degree of sexual dysfunction. Mohammadi et al. [19] confirmed the validity and reliability of the Persian version of this tool in 2008, reporting overall reliability coefficients of 78% for halving and 75% for retesting. Sub-test reliability using the halving method ranged from 63% to 75%, while the retesting method ranged from 70% to 81%.
Intervention
All participants completed the FSFI and SQOL-F questionnaires and a demographic and reproductive health survey. The intervention group began individual yoga training, adhering to health protocols, with one-hour sessions twice a week for 12 weeks (24 sessions). At the beginning of each session, participants engaged in relaxation exercises. A certified yoga practitioner taught the techniques in a private room at the health center in Isfahan, Iran, while the participants (women 8-10 weeks post-vaginal delivery) practiced them. The following practical guidelines were used to perform the techniques.
1. Exercise for the nipple: The left palm was placed on the left nipple, and the right palm was placed on the right. This technique involved rotating the palms of the hands with gentle pressure on the nipples. After 20 rotational movements, participants rested for 30 seconds before repeating the movement. This technique was repeated 2-3 times.
2. Exercise for the breasts: The individual was relaxed. Then, the breasts were massaged with the palms of the hands using rubbing movements. The massage should not cause pain, and there was no time limit for performing this technique.
3. Exercise for pelvic floor muscles: This technique involves applying gentle pressure to the pelvic floor muscles while the individual lies on their back. Relaxation was achieved through deep breathing. The middle finger touched most of the pelvic floor muscles and applied gentle pressure. After some time, the pressure was increased to a level that did not induce pain.
4. Exercise to strengthen the vaginal walls: When standing, the legs were positioned shoulder-width apart. Relaxation was initiated through the person’s tailbone while the anal muscles and sphincter were contracted. This movement was performed 3-4 times, with 50 contractions each time.
5. Exercise to increase sexual desire (exercise of fantasy): The individual could perform this technique in any comfortable or lying position while focusing on their breathing, which would help promote relaxation. The hand was placed next to the body, and sexual intercourse was imagined. The individual could visualize anything that aroused them. After a few minutes, a diffuse warming sensation in the lower abdomen was felt, and lubrication occurred. At this point, the visualization process was stopped. The duration of this exercise varied for each person [20].
The control group received only routine care and information on postpartum recovery and lactation. At the end of the first, second, and third months, both groups completed the SQOL-F and FSFI questionnaires.
Statistical analysis
Data were analyzed using R software Version 4.1. Descriptive analysis included absolute frequency distribution, mean, and standard deviation. The independent sample t-test and Mann-Whitney U test were used to compare the two groups. ANOVA and Friedman's test were utilized to compare qualitative and quantitative data for the four data sets (before the intervention and one month, two months, and three months after the intervention). The Chi-square test assessed pre- and post-test qualitative data. Statistical significance was set at a p-value of less than 0.05. The corresponding author will provide the datasets used in this study upon reasonable request.
Findings
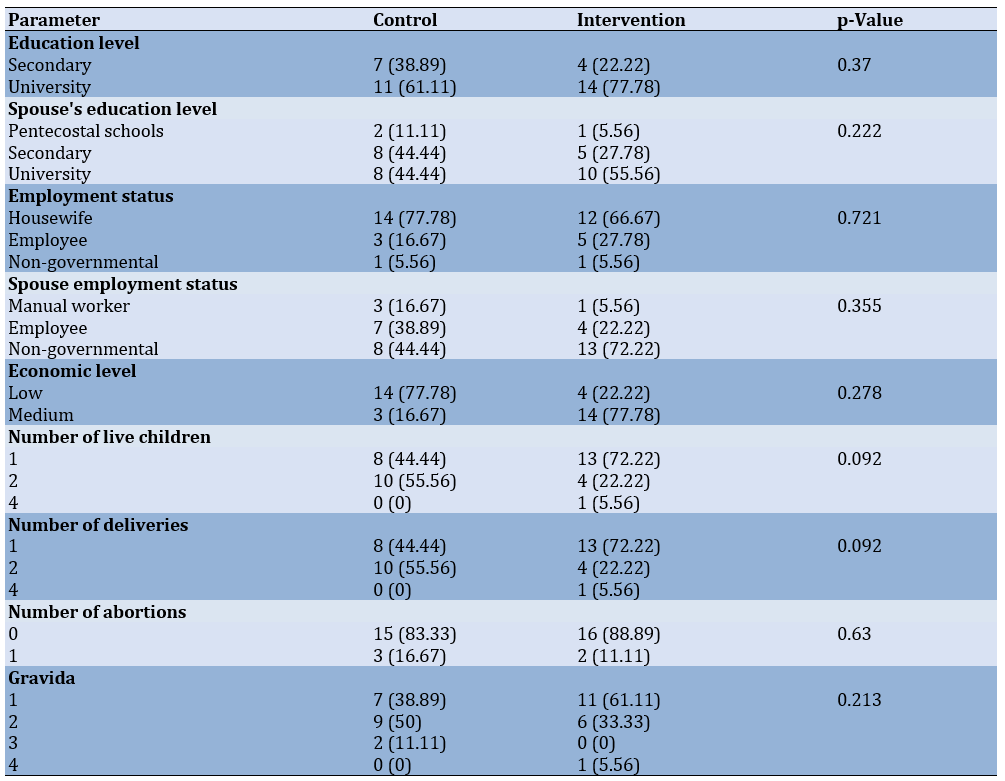
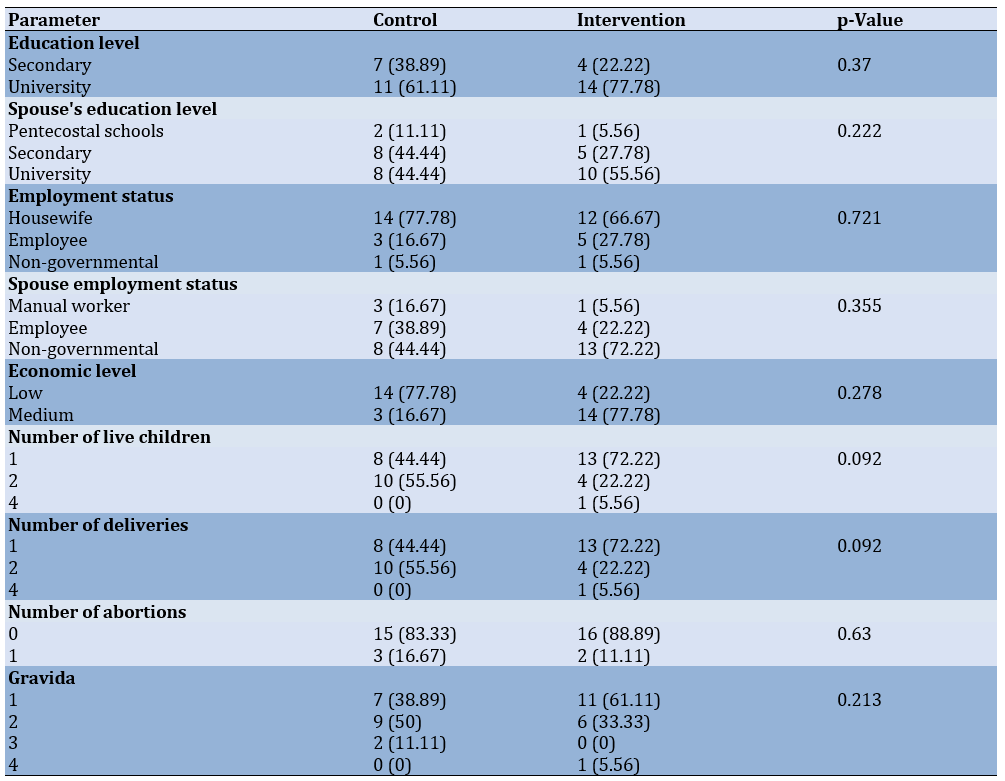
There were no significant differences between the two groups in the demographic parameters. Also, no significant differences were seen in the age of control (3.39±3.43) and intervention (30.89±3.97) groups (p=0.69), spouse’s age of control (33.67±4.04) and intervention (35.11±4.80) groups (p=0.34), and marriage duration of control (7.75±3.10) and intervention (6.42±5.33) groups (p=0.37; Table 1).
Table 1. Baseline characteristics of the participants
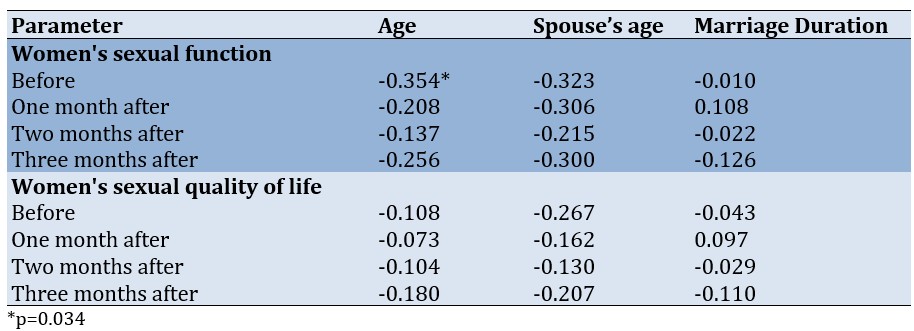
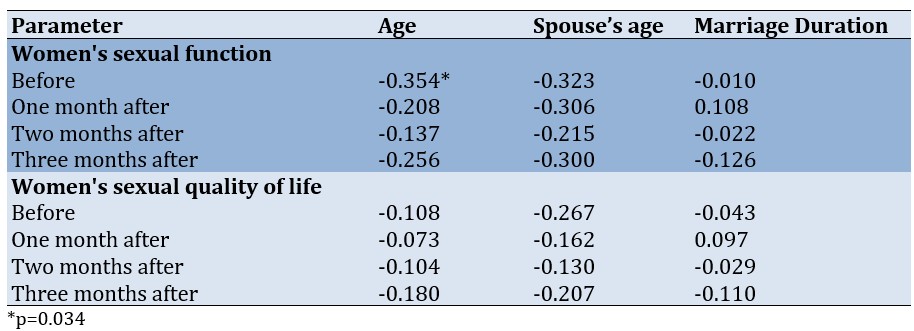
Pearson’s correlation coefficient between sexual quality of life, sexual function indices, and demographic parameters showed no significant linear relationship in the studied parameters (p>0.05; Table 2).
Table 2. Correlation between the studied parameters and demographic characteristics by study stages
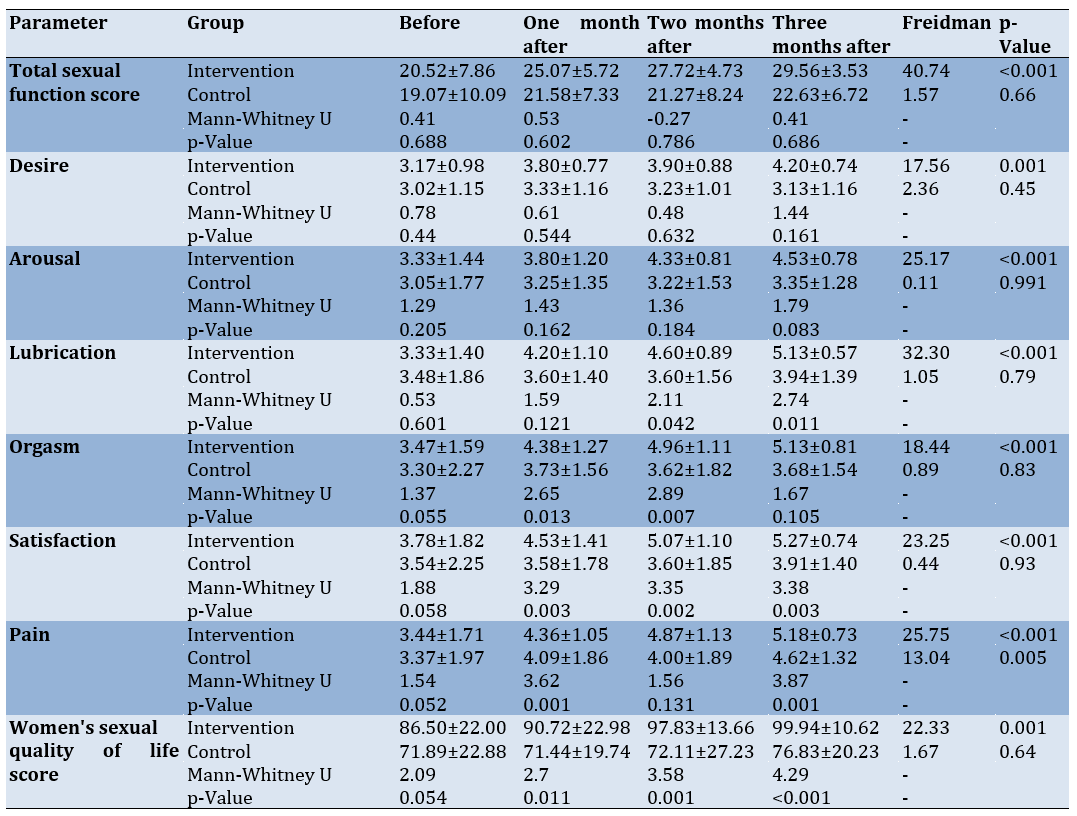
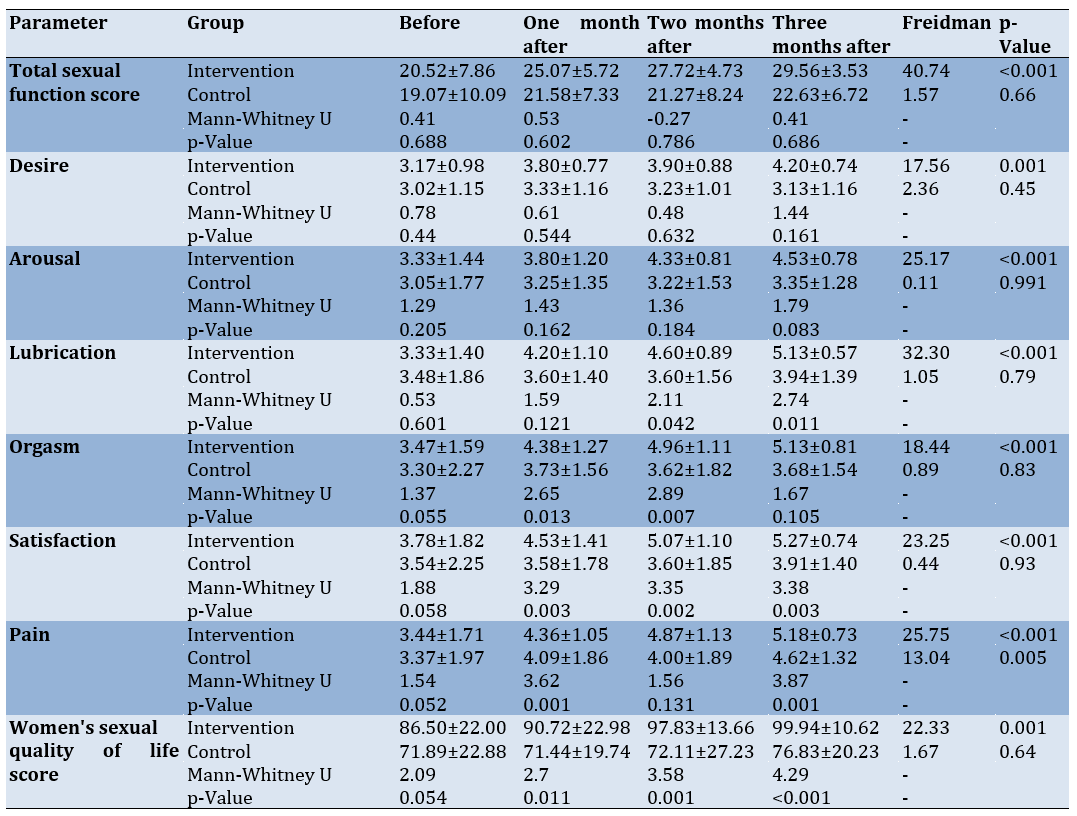
The mean total score of sexual function at three months showed a significant improvement in the intervention group after the intervention compared to before the intervention ((20.52 (7.86) vs. 29.56 (3.53), t(34, 0.975), p<0.001). However, no significant difference was found between the intervention and control groups three months after the intervention. The sexual quality of life in the intervention group significantly improved after three months of intervention compared to before the intervention (86.50 (22.00) vs. 99.94 (10.62), t(34, 0.975), p<0.001) and compared to the control group (99.94 (10.62) vs. 76.83 (20.23), t(34, 0.975), p<0.001; Table 3).
Table 3. Comparison of the mean scores of the studied parameters in the control and intervention groups by study stages
Discussion
This study investigated the effect of yoga on sexual function and sexual quality of life in postpartum women after vaginal delivery and aligns with and contributes to existing theories and models in the field of research on postpartum sexual health. The biopsychosocial model posits that health outcomes are influenced by biological, psychological, and social factors [21]. The findings of our study support this model by demonstrating the multifaceted nature of postpartum sexual health. Yoga interventions address biological aspects, such as pelvic floor strength and blood circulation, psychological factors, including stress and body image concerns, and social dimensions through group dynamics and social support within yoga classes [22]. Stress and coping theory suggests that individuals employ coping mechanisms to manage stressors and adapt to challenging situations [23]. Yoga techniques can serve as coping strategies for postpartum women dealing with stressors related to childbirth, childcare, and changes in relationships. By reducing stress and promoting emotional resilience, yoga contributes to improved sexual function and quality of life [24]. The health belief model proposes that health-related behaviors are influenced by perceived susceptibility, severity, benefits, and barriers [25]. Postpartum women may perceive sexual dysfunction as a significant concern affecting their quality of life. Yoga interventions offer perceived benefits, such as enhanced physical well-being, stress reduction, and improved body image, thereby motivating women to engage in these practices to address postpartum sexual concerns [24, 26].
Previous research on yoga interventions has also reported improvements in sexual function and quality of life. Studies have highlighted the positive effects of yoga on pelvic floor muscle strength, relaxation, and psychological well-being, all of which contribute to enhanced sexual health [12-15, 27-29].
Like the present study, previous research has observed significant increases in the mean scores of sexual function and quality of life post-intervention among women who participated in yoga programs [12-15, 27-29].
While the present study specifically focused on postpartum women after vaginal delivery, previous research has included women from diverse populations. Variations in the duration, intensity, and type of yoga interventions across studies may contribute to differences in outcomes. Some studies have employed longer intervention periods or incorporated additional components, such as meditation and breathwork, which could influence the magnitude of the effects observed.
Overall, while our findings are consistent with previous research demonstrating the beneficial effects of yoga on sexual health, further investigation is warranted to elucidate the mechanisms underlying these effects and to address potential variations in outcomes across different populations and intervention protocols. By building upon existing theories and models and integrating empirical evidence from diverse studies, researchers can advance our understanding of the role of yoga in promoting sexual well-being during the postpartum period. Additionally, considering the prevalence of these issues after childbirth and their impact on quality of life, it is recommended that medical staff become familiar with these techniques and incorporate them into their practice.
As a limitation of this study, because sexual activity is a mutual relationship and men’s sexual function is likely to be influenced by their wives’ sexual function, it is advisable to inquire about male sexual function and sexual quality of life after their wives’ yoga practice in future studies.
Conclusion
Yoga techniques improve women’s sexual function and enhance sexual quality of life.
Acknowledgments: We appreciate and thank all the women who participated in this study for their cooperation and willingness to volunteer.
Ethical Permissions: The study received approval from the Ethics Committee of Tarbiat Modares University, Tehran, Iran (Code of Ethics: IR.MODARES.REC.1398.145). All research was conducted in compliance with the Declaration of Helsinki. Participants provided informed consent after receiving a detailed explanation of the study’s goals. Confidentiality and voluntary participation were guaranteed, and participants had the right to withdraw at any point. The study was registered at the Iranian Registry of Clinical Trials (IRCT20191023045221N1).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Shadani F (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (30%); Shahali Sh (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (40%); Hosseini F (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Bahrampour B (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher (15%)
Funding/Support: This study was funded by the Tarbiat Modares University.
The World Health Organization defines sexual health as a state of complete physical, mental, and social well-being related to sexuality. This definition encompasses a positive and respectful approach to gender and sexual relations, facilitating healthy and pleasurable sexual experiences free from coercion, discrimination, and violence [1]. It also enhances psychological well-being, emotions, and feelings, while strengthening the relationship between partners [2].
Sexual quality of life is a crucial aspect of sexual health, referring to an individual’s perception of their position in relation to their culture, goals, expectations, standards, and priorities. It reflects how one’s understanding of their sexual life influences their mental state. A fulfilling sex life fosters healthy and effective relationships between couples [3], whereas poor sexual quality can lead to separation or extramarital affairs. Sexual function significantly impacts the overall quality of life [4]. Zare et al. examined the quality of sexual life among 104 women after childbirth, indicating a low quality of sexual life for women following childbirth [5].
Sexual function refers to the body’s reactions during the various stages of the sexual response cycle [6]. Sexual dysfunction is a problem that arises during this cycle and prevents a person from experiencing sexual satisfaction [7]. According to the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), female sexual dysfunction (FSD) is classified into four categories: desire disorder, arousal disorder, female orgasmic disorder, and genito-pelvic pain/penetration disorder [8]. McCabe et al. showed that 10% to 31.7% of men and 21.4% to 50% of women experience sexual dysfunction [9]. According to Banaei et al.’s study involving 432 Iranian women, 31.25% report a lack of sexual desire, 33.13% have difficulty achieving orgasm, and 40% experience pain during sexual intercourse [10].
Pregnancy and childbirth induce biological and psychological changes that can impact sexual function, with evidence suggesting a decline during pregnancy that does not fully recover in the postpartum period [11]. Changes in body shape, sleep deprivation, anxiety, stress, and frequent urination contribute to high rates of sexual dysfunction among postpartum women, both in Iran and globally. In a 2018 study, the prevalence of sexual dysfunction among Iranian postpartum women is 85.95% [10]. According to Gutzeit et al., postpartum dysfunction affects all areas of sexual function, including pain during intercourse, decreased lubrication, lack of orgasm, and reduced sexual desire [11]. While medication can be useful for treating sexual dysfunction, its disadvantages include rejection by women, low efficacy, and side effects.
Yoga is a form of complementary therapy used in both developed and developing countries [12]. Several experimental studies on yoga have found its beneficial effects on various aspects of physical and mental function, demonstrating that yoga can be effective in improving and treating FSD [12-15]. Given that the impact of yoga techniques on sexual function in postpartum women has not yet been assessed, it is unclear whether yoga also influences sexual function in postpartum women or if these techniques affect the sexual quality of life of women after vaginal delivery. Consequently, we aimed to measure the effect of yoga on the sexual function and sexual quality of life of these women.
Materials and Methods
Study design
This parallel randomized controlled trial involved 50 primiparous women who were 8-10 weeks post-vaginal delivery and sought postpartum care or infant vaccination at a health center in Isfahan, Iran, from January 2020 to March 2021.
Inclusion and exclusion criteria
The inclusion criteria were primiparous women of reproductive age who were at least 8-10 weeks postpartum and had resumed sexual intercourse. Participants were exclusively breastfeeding, had no known underlying conditions (infections, psychological disorders, chronic diseases, or COVID-19), and had no history of alcohol or drug use or the use of medications affecting sexual activity. They were not practicing yoga, experienced no complications during labor (e.g., vacuum delivery or prolonged labor), had no history of pelvic surgeries (such as colporrhaphy), did not suffer from severe vaginal tears after delivery, had no postpartum vaginal healing issues, and had no history of infertility, bleeding, or threats of miscarriage during pregnancy or after delivery.
Sampling
After evaluating the eligibility criteria, informed written consent was obtained from all participants, who were then randomized using block randomization with a block size of four. Based on Dhikav et al., which was conducted on the quality of sexual life, and the standard deviations obtained before and after the intervention (S1=8.51 and S2=6.73), and considering the first type error (α=0.05) and the second type error (β=0.2), a sample size of 18 individuals for each group was determined. Considering a 15% attrition rate, a sample of 50 participants (25 cases per group) was considered [12]. It should be noted that in the control group, five women were infected with COVID-19, and two women did not respond to the researcher. In the intervention group, four women were infected with COVID-19, and three women were unwilling to continue the intervention for personal reasons; all of these individuals were excluded. Therefore, each group included 18 cases.
Data collection tools
The Sexual Quality of Life-Female (SQOL-F) Questionnaire and the Female Sexual Function Index (FSFI) were used to measure the women’s sexual quality of life and sexual function.
The SQOL-F, designed by Symonds et al. [16] in 2005, consists of 18 items that cover four areas, including sexual, psychological emotion, sexual and marital satisfaction, self-deprecation, and sexual repression. The total score ranges from 18 to 108, with a higher score indicating a better quality of life. Maasoumi et al. demonstrated high internal consistency and good test-retest reliability, with a Cronbach’s alpha coefficient of 0.73 and an intraclass correlation coefficient (ICC) of 0.88. The average scores for the content validity index (CVI) and content validity ratio (CVR) were 0.91 and 0.84, respectively [17].
The FSFI was developed by Rosen et al. [18] in 2000. It contains 19 questions that measure women’s sexual performance in six areas, including desire, arousal, lubrication, orgasm, sexual satisfaction, and pain. The overall FSFI score ranges from 2 to 36, with a cutoff score 28. A higher score is associated with a lower degree of sexual dysfunction. Mohammadi et al. [19] confirmed the validity and reliability of the Persian version of this tool in 2008, reporting overall reliability coefficients of 78% for halving and 75% for retesting. Sub-test reliability using the halving method ranged from 63% to 75%, while the retesting method ranged from 70% to 81%.
Intervention
All participants completed the FSFI and SQOL-F questionnaires and a demographic and reproductive health survey. The intervention group began individual yoga training, adhering to health protocols, with one-hour sessions twice a week for 12 weeks (24 sessions). At the beginning of each session, participants engaged in relaxation exercises. A certified yoga practitioner taught the techniques in a private room at the health center in Isfahan, Iran, while the participants (women 8-10 weeks post-vaginal delivery) practiced them. The following practical guidelines were used to perform the techniques.
1. Exercise for the nipple: The left palm was placed on the left nipple, and the right palm was placed on the right. This technique involved rotating the palms of the hands with gentle pressure on the nipples. After 20 rotational movements, participants rested for 30 seconds before repeating the movement. This technique was repeated 2-3 times.
2. Exercise for the breasts: The individual was relaxed. Then, the breasts were massaged with the palms of the hands using rubbing movements. The massage should not cause pain, and there was no time limit for performing this technique.
3. Exercise for pelvic floor muscles: This technique involves applying gentle pressure to the pelvic floor muscles while the individual lies on their back. Relaxation was achieved through deep breathing. The middle finger touched most of the pelvic floor muscles and applied gentle pressure. After some time, the pressure was increased to a level that did not induce pain.
4. Exercise to strengthen the vaginal walls: When standing, the legs were positioned shoulder-width apart. Relaxation was initiated through the person’s tailbone while the anal muscles and sphincter were contracted. This movement was performed 3-4 times, with 50 contractions each time.
5. Exercise to increase sexual desire (exercise of fantasy): The individual could perform this technique in any comfortable or lying position while focusing on their breathing, which would help promote relaxation. The hand was placed next to the body, and sexual intercourse was imagined. The individual could visualize anything that aroused them. After a few minutes, a diffuse warming sensation in the lower abdomen was felt, and lubrication occurred. At this point, the visualization process was stopped. The duration of this exercise varied for each person [20].
The control group received only routine care and information on postpartum recovery and lactation. At the end of the first, second, and third months, both groups completed the SQOL-F and FSFI questionnaires.
Statistical analysis
Data were analyzed using R software Version 4.1. Descriptive analysis included absolute frequency distribution, mean, and standard deviation. The independent sample t-test and Mann-Whitney U test were used to compare the two groups. ANOVA and Friedman's test were utilized to compare qualitative and quantitative data for the four data sets (before the intervention and one month, two months, and three months after the intervention). The Chi-square test assessed pre- and post-test qualitative data. Statistical significance was set at a p-value of less than 0.05. The corresponding author will provide the datasets used in this study upon reasonable request.
Findings
There were no significant differences between the two groups in the demographic parameters. Also, no significant differences were seen in the age of control (3.39±3.43) and intervention (30.89±3.97) groups (p=0.69), spouse’s age of control (33.67±4.04) and intervention (35.11±4.80) groups (p=0.34), and marriage duration of control (7.75±3.10) and intervention (6.42±5.33) groups (p=0.37; Table 1).
Table 1. Baseline characteristics of the participants
Pearson’s correlation coefficient between sexual quality of life, sexual function indices, and demographic parameters showed no significant linear relationship in the studied parameters (p>0.05; Table 2).
Table 2. Correlation between the studied parameters and demographic characteristics by study stages
The mean total score of sexual function at three months showed a significant improvement in the intervention group after the intervention compared to before the intervention ((20.52 (7.86) vs. 29.56 (3.53), t(34, 0.975), p<0.001). However, no significant difference was found between the intervention and control groups three months after the intervention. The sexual quality of life in the intervention group significantly improved after three months of intervention compared to before the intervention (86.50 (22.00) vs. 99.94 (10.62), t(34, 0.975), p<0.001) and compared to the control group (99.94 (10.62) vs. 76.83 (20.23), t(34, 0.975), p<0.001; Table 3).
Table 3. Comparison of the mean scores of the studied parameters in the control and intervention groups by study stages
Discussion
This study investigated the effect of yoga on sexual function and sexual quality of life in postpartum women after vaginal delivery and aligns with and contributes to existing theories and models in the field of research on postpartum sexual health. The biopsychosocial model posits that health outcomes are influenced by biological, psychological, and social factors [21]. The findings of our study support this model by demonstrating the multifaceted nature of postpartum sexual health. Yoga interventions address biological aspects, such as pelvic floor strength and blood circulation, psychological factors, including stress and body image concerns, and social dimensions through group dynamics and social support within yoga classes [22]. Stress and coping theory suggests that individuals employ coping mechanisms to manage stressors and adapt to challenging situations [23]. Yoga techniques can serve as coping strategies for postpartum women dealing with stressors related to childbirth, childcare, and changes in relationships. By reducing stress and promoting emotional resilience, yoga contributes to improved sexual function and quality of life [24]. The health belief model proposes that health-related behaviors are influenced by perceived susceptibility, severity, benefits, and barriers [25]. Postpartum women may perceive sexual dysfunction as a significant concern affecting their quality of life. Yoga interventions offer perceived benefits, such as enhanced physical well-being, stress reduction, and improved body image, thereby motivating women to engage in these practices to address postpartum sexual concerns [24, 26].
Previous research on yoga interventions has also reported improvements in sexual function and quality of life. Studies have highlighted the positive effects of yoga on pelvic floor muscle strength, relaxation, and psychological well-being, all of which contribute to enhanced sexual health [12-15, 27-29].
Like the present study, previous research has observed significant increases in the mean scores of sexual function and quality of life post-intervention among women who participated in yoga programs [12-15, 27-29].
While the present study specifically focused on postpartum women after vaginal delivery, previous research has included women from diverse populations. Variations in the duration, intensity, and type of yoga interventions across studies may contribute to differences in outcomes. Some studies have employed longer intervention periods or incorporated additional components, such as meditation and breathwork, which could influence the magnitude of the effects observed.
Overall, while our findings are consistent with previous research demonstrating the beneficial effects of yoga on sexual health, further investigation is warranted to elucidate the mechanisms underlying these effects and to address potential variations in outcomes across different populations and intervention protocols. By building upon existing theories and models and integrating empirical evidence from diverse studies, researchers can advance our understanding of the role of yoga in promoting sexual well-being during the postpartum period. Additionally, considering the prevalence of these issues after childbirth and their impact on quality of life, it is recommended that medical staff become familiar with these techniques and incorporate them into their practice.
As a limitation of this study, because sexual activity is a mutual relationship and men’s sexual function is likely to be influenced by their wives’ sexual function, it is advisable to inquire about male sexual function and sexual quality of life after their wives’ yoga practice in future studies.
Conclusion
Yoga techniques improve women’s sexual function and enhance sexual quality of life.
Acknowledgments: We appreciate and thank all the women who participated in this study for their cooperation and willingness to volunteer.
Ethical Permissions: The study received approval from the Ethics Committee of Tarbiat Modares University, Tehran, Iran (Code of Ethics: IR.MODARES.REC.1398.145). All research was conducted in compliance with the Declaration of Helsinki. Participants provided informed consent after receiving a detailed explanation of the study’s goals. Confidentiality and voluntary participation were guaranteed, and participants had the right to withdraw at any point. The study was registered at the Iranian Registry of Clinical Trials (IRCT20191023045221N1).
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Shadani F (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (30%); Shahali Sh (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (40%); Hosseini F (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Bahrampour B (Fourth Author), Introduction Writer/Methodologist/Assistant Researcher (15%)
Funding/Support: This study was funded by the Tarbiat Modares University.
Article Type: Original Research |
Subject:
Sexual Health Education/Promotion
Received: 2024/07/9 | Accepted: 2024/09/10 | Published: 2024/10/5
Received: 2024/07/9 | Accepted: 2024/09/10 | Published: 2024/10/5
References
1. WHO. Sexual and reproductive health and research (SRH) [Internet]. Geneva: World Health Organization [cited 2023 Oct 11]. Available from: https://www.who.int/teams/sexual-and-reproductive-health-and-research/key-areas-of-work/sexual-health/defining-sexual-health [Link]
2. Banaei M, Azizi M, Moridi A, Dashti S, Yabandeh AP, Roozbeh N. Sexual dysfunction and related factors in pregnancy and postpartum: A systematic review and meta-analysis protocol. Syst Rev. 2019;8(1):161. [Link] [DOI:10.1186/s13643-019-1079-4]
3. Karbasi Z, Riazi H, Firoozi A. The effect of narrative therapy on sexual self-efficacy and sexual quality of life in women. Payesh. 2023;22(4):443-53. [Persian] [Link] [DOI:10.61186/payesh.22.4.443]
4. Castelo-Branco C, Naumova I. Quality of life and sexual function in women with polycystic ovary syndrome: A comprehensive review. Gynecol Endocrinol. 2020;36(2):96-103. [Link] [DOI:10.1080/09513590.2019.1670788]
5. Zare Z, Golmakani N, Shareh H, Shakeri MT. Survey of relationship between sexual self-efficacy and sexual life quality with marital satisfaction in primiparous women after childbirth. J Stud Res Cent. 2016;21(2):1-10. [Persian] [Link]
6. Basson R. Human sexual response. Handb Clin Neurol. 2015;130:11-8. [Link] [DOI:10.1016/B978-0-444-63247-0.00002-X]
7. Amiri FN, Omidvar S, Bakhtiari A, Hajiahmadi M. Female sexual outcomes in primiparous women after vaginal delivery and cesarean section. Afr Health Sci. 2017;17(3):623-31. [Link] [DOI:10.4314/ahs.v17i3.4]
8. American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5TM. Washington D.C: American Psychiatric Publishing; 2013. [Link] [DOI:10.1176/appi.books.9780890425596]
9. McCabe MP, Sharlip ID, Lewis R, Atalla E, Balon R, Fisher AD, et al. Incidence and prevalence of sexual dysfunction in women and men: A consensus statement from the fourth international consultation on sexual medicine 2015. J Sex Med. 2016;13(2):144-52. [Link] [DOI:10.1016/j.jsxm.2015.12.034]
10. Banaei M, Moridi A, Dashti S. Sexual dysfunction and its associated factors after delivery: Longitudinal study in Iranian women. Mater Sociomed. 2018;30(3):198-203. [Link] [DOI:10.5455/msm.2018.30.198-203]
11. Gutzeit O, Levy G, Lowenstein L. Postpartum female sexual function: Risk factors for postpartum sexual dysfunction. Sex Med. 2020;8(1):8-13. [Link] [DOI:10.1016/j.esxm.2019.10.005]
12. Dhikav V, Karmarkar G, Gupta R, Verma M, Gupta R, Gupta S, et al. Yoga in female sexual functions. J Sex Med. 2010;7(2 Pt 2):964-70. [Link] [DOI:10.1111/j.1743-6109.2009.01580.x]
13. Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among the Iranian women with multiple sclerosis: A randomized controlled trial. Afr J Tradit Complement Altern Med. 2014;11(5):78-82. [Link] [DOI:10.4314/ajtcam.v11i5.13]
14. Brotto LA, Mehak L, Kit C. Yoga and sexual functioning: A review. J Sex Marital Ther. 2009;35(5):378-90. [Link] [DOI:10.1080/00926230903065955]
15. Kim HN, Ryu J, Kim KS, Song SW. Effects of yoga on sexual function in women with metabolic syndrome: A randomized controlled trial. J Sex Med. 2013;10(11):2741-51. [Link] [DOI:10.1111/jsm.12283]
16. Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. J Sex Marital Ther. 2005;31(5):385-97. [Link] [DOI:10.1080/00926230591006502]
17. Maasoumi R, Lamyian M, Montazeri A, Azin SA, Aguilar-Vafaie ME, Hajizadeh E. The sexual quality of life-female (SQOL-F) questionnaire: Translation and psychometric properties of the Iranian version. Reprod Health. 2013;10:25. [Link] [DOI:10.1186/1742-4755-10-25]
18. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191-208. [Link] [DOI:10.1080/009262300278597]
19. Mohammadi Kh, Heydari M, Faghihzadeh S. The female sexual function index (FSFI): Validation of the Iranian version. Payesh. 2008;7(3). [Persian] [Link]
20. Advait. Yoga for sex: 30 simple exercises for ultimate sexual pleasure. Seattle: Amazon; 2014. [Link]
21. Papadimitriou G. The "Biopsychosocial Model": 40 years of application in Psychiatry. Psychiatriki. 2017;28(2):107-10. [Link] [DOI:10.22365/jpsych.2017.282.107]
22. Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49-54. [Link] [DOI:10.4103/0973-6131.85485]
23. Tan SY, Yip A. Hans Selye (1907-1982): Founder of the stress theory. Singapore Med J. 2018;59(4):170-1. [Link] [DOI:10.11622/smedj.2018043]
24. Munns L, Spark N, Crossland A, Preston C. The effects of yoga-based interventions on postnatal mental health and well-being: A systematic review. Heliyon. 2024;10(3):e25455. [Link] [DOI:10.1016/j.heliyon.2024.e25455]
25. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The health belief model as an explanatory framework in communication research: Exploring parallel, serial, and moderated mediation. Health Commun. 2015;30(6):566-76. [Link] [DOI:10.1080/10410236.2013.873363]
26. Gong H, Ni C, Shen X, Wu T, Jiang C. Yoga for prenatal depression: A systematic review and meta-analysis. BMC Psychiatry. 2015;15:14. [Link] [DOI:10.1186/s12888-015-0393-1]
27. Thakur P, Mohammad A, Rastogi YR, Saini RV, Saini AK. Yoga as an intervention to manage multiple sclerosis symptoms. J Ayurveda Integr Med. 2020;11(2):114-7. [Link] [DOI:10.1016/j.jaim.2019.04.005]
28. Dording CM, Sangermano L. Female sexual dysfunction: Natural and complementary treatments. Focus. 2018;16(1):19-23. [Link] [DOI:10.1176/appi.focus.20170049]
29. Finley N. Lifestyle choices can augment female sexual well-being. Am J Lifestyle Med. 2017;12(1):38-41. [Link] [DOI:10.1177/1559827617740823]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |