Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 341-346 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Karbasi Z, Ram M, Hajesmaeel Gohari S, Sabahi A. Investigating the e-Health Literacy of Patients with Type 2 Diabetes in the Use of Self-Care Mobile Health Applications. Health Educ Health Promot 2024; 12 (2) :341-346
URL: http://hehp.modares.ac.ir/article-5-75999-en.html
URL: http://hehp.modares.ac.ir/article-5-75999-en.html
1- Medical Informatics Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
2- Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
3- Department of Health Information Technology, Ferdows Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
2- Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
3- Department of Health Information Technology, Ferdows Faculty of Medical Sciences, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 632 kb]
(2866 Downloads)
| Abstract (HTML) (1075 Views)
Full-Text: (244 Views)
Introduction
One of the most common types of diabetes is T2D [1], with its incidence increasing due to various reasons, including obesity, unhealthy diet, and metabolic syndrome [2-4]. Evidence shows that there is a possibility of more than 500 million individuals suffering from T2D by 2030 [5]. However, many people are not aware of the complications associated with diabetes [6]. Individuals with T2D suffer from complications such as diabetic retinopathy and cardiovascular diseases that affect their quality of life [7]. Self-management can play a significant role in controlling the disease [8]. One of the ways to improve the self-care of patients is acquiring knowledge [9].
The basis of diabetes care is self-management [10]. Today, health literacy is essential [11] and can be highly effective for diseases such as T2D [12]. The ability of individuals to acquire health information and process it to make appropriate decisions is referred to as health literacy [13]. Electronic health literacy is almost defined as similar to health literacy, with the difference that it focuses on electronic information resources [14]. Evidence has shown that high health literacy has an indirect effect on diabetes self-care and blood sugar control [15]. The results of the research by Ernsting et al. revealed that patients with heart diseases or diabetes who used m-Health applications demonstrated a high level of e-Health literacy [16]. According to the literature, mobile applications are widely used by individuals, but not all of them can use these applications for blood sugar control and self-care [17].
Using information technology such as the Internet, mobile phones, and computers, electronic health has provided individuals with the possibility of self-care and disease management [18, 19]. Using electronic health programs, patients can monitor their health status and interact with healthcare providers [20-22]. The positive effects of m-Health applications on self-care and knowledge enhancement among patients with diabetes have been established [23]. Factors such as limited understanding of technology, lack of knowledge about electronic health programs, and lack of tools to access electronic health prevent from using digital interventions for self-management and changing health behaviors [24, 25]. In addition to m-Health applications that have facilitated access to information [26], information available on the Internet is effective in changing health behaviors and disease management [27].
The use of electronic health information and programs among patients with diabetes depends on various factors that need to be examined. Therefore, this study was conducted to investigate the e-health literacy of patients with T2D in using self-care m-Health applications in Kerman City in 2023.
Instrument and Methods
This cross-sectional study was conducted in 2023. Patients referred to a selected clinic in Kerman City were the research population of this study. A total of 198 patients were included in the study using available sampling, and questionnaires were distributed among them. After reviewing the completed questionnaires, 10 participants did not responded to the questionnaire precisely and the remaining 188 questionnaires were analyzed. The inclusion criteria were diagnosis of diabetes and informed consent of the participants, and those who did not cooperate in filling the questionnaire were excluded. The collection tools in this study included a demographic information checklist, an e-health literacy questionnaire, and a researcher-made questionnaire to investigate patients' preferences and tendencies. Demographic information included age, gender, marital status, type of residence, duration of disease, and other diseases. In this study, Norman and Skinner's e-health literacy questionnaire was used, which includes eight components to evaluate e-health literacy [28]. The validity and reliability of the Persian-translated version of the questionnaire were evaluated by Bazm et al., and Cronbach's alpha coefficient was reported as 0.88 [29]. The third part of the researcher-made questionnaire includes 14 questions about m-Health methods for the self-management of the disease, patient preferences and inclinations for using a variety of m-Health methods, patient preferences and inclinations for using m-Health for self-management of T2D, and intervals and sequences preferred to receive training. Experts in health information management and medical informatics were used to determine content validity, and the reliability of the questionnaire was calculated based on Cronbach's alpha coefficient and using SPSS version 26 software. Accordingly, Cronbach's alpha coefficient of this questionnaire is 0.876. Frequency, mean, and standard deviation were used to describe the data. Analytical statistical methods such as Mann-Whitney were also employed. Confidentiality of information was maintained in this study, and the questionnaires were completed voluntarily and anonymously.
Findings
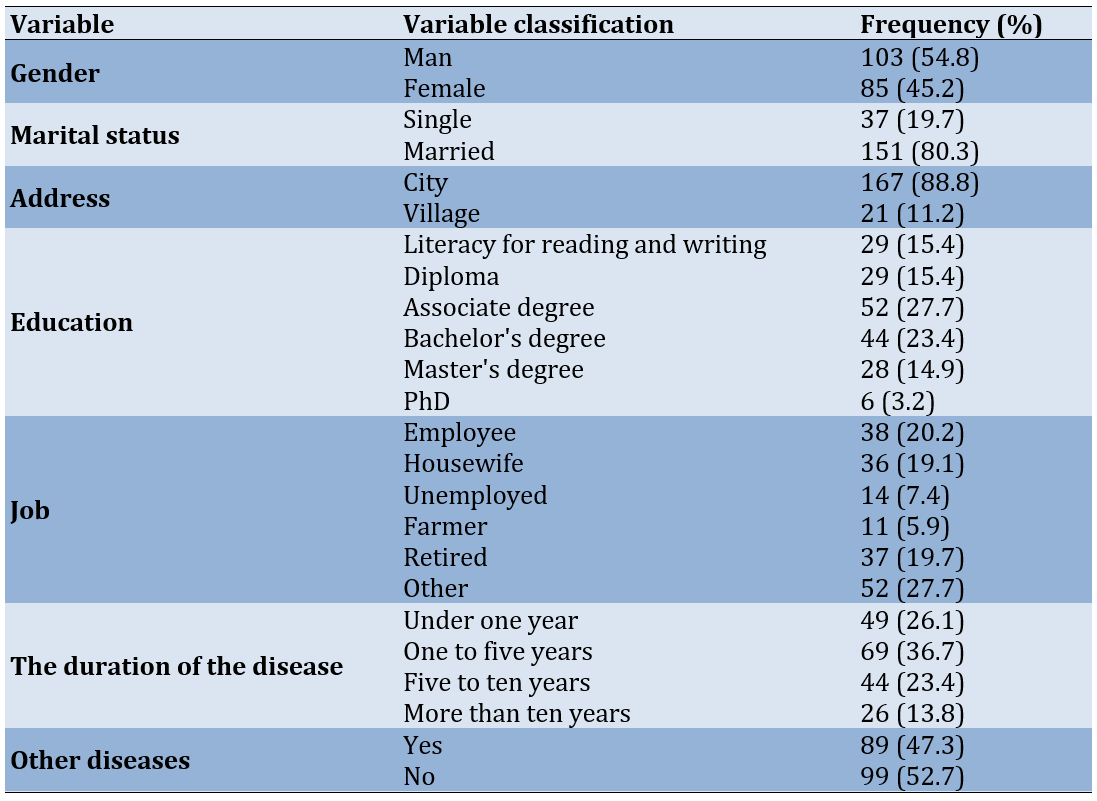
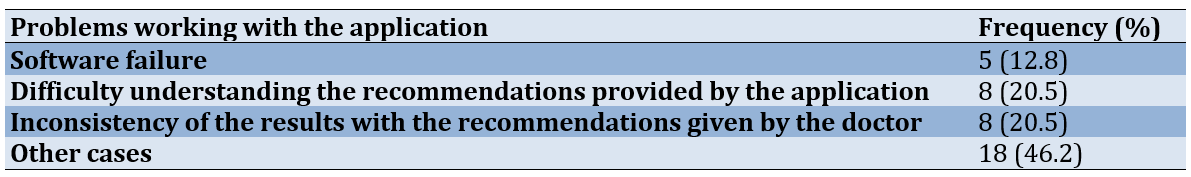
188 individuals participated in this research, 103 (54.8%) participants were men and the rest were women. The average age of the participants in the research was 50.17±12.91 years, with the lowest age being 22 years old and the highest age being 80 years old. A total of 151 participants (80.3%) were married and the rest were single. Most of the participants (88.8%) lived in urban areas. Among the participants, 38 individuals (20.2%) were employed. In terms of disease duration, 69 individuals (36.7%) had been suffering from the disease for one to five years (Table 1).
Table 1. Frequency distribution of demographic variables in study participants
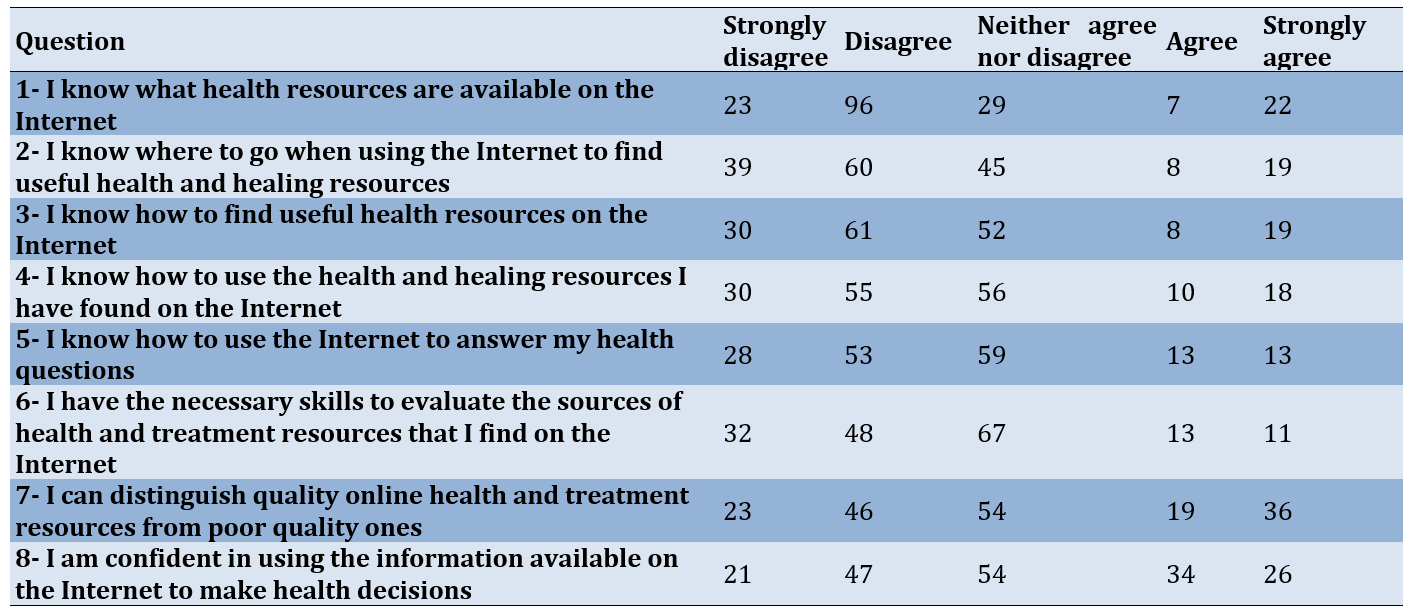
Regarding e-health literacy questions, 51.3% of the participants disagreed and did not know what resources are related to health issues on the Internet. The majority of the participants (35.1%) chose the disagree option for question 2. Regarding question 3, 35.9% of the participants disagreed and did not know how to find healthcare resources on the Internet. In response to questions 4, 5, 6, 7, and 8, the percentages of participants who chose "neither agree nor disagree" were 33.1%, 35.5%, 39.2%, 30.3%, and 29.7%, respectively (Table 2).
Table 2. Frequency of answers to e-health literacy questions
Based on the obtained information, the average health literacy score of the participants in the study was 24.75±9.04. The number of participants who used methods based on m-Health to manage their disease was 100, and telephone calls were the most frequent with 54% among the different methods based on m-Health.
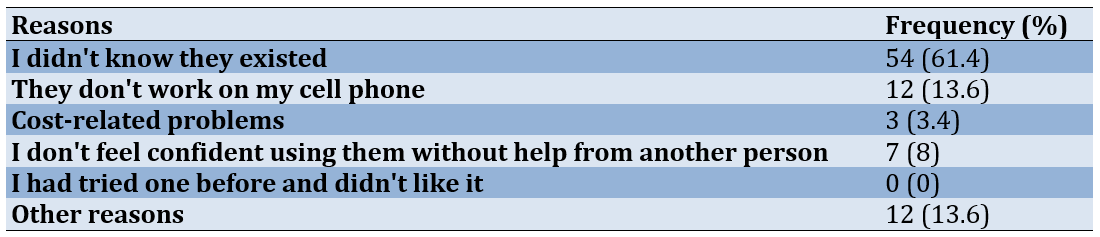
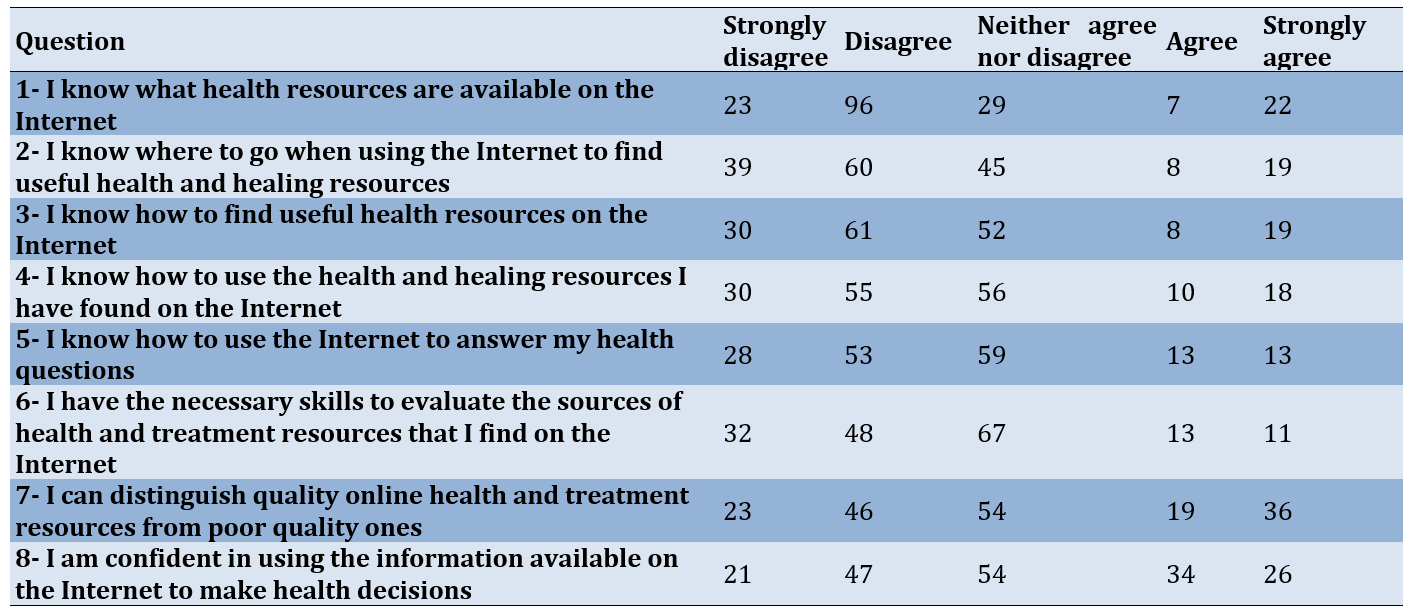
Out of 188 patients participating in the study, 88 had not used any of the m-Health methods in the management of their disease, and the majority of the participants (61.4%) mentioned that they were unaware that these methods were available for managing their disease (Table 3).
Table 3. The frequency of reasons for not using m-Health-based programs in disease management by type 2 diabetes (T2D) patients
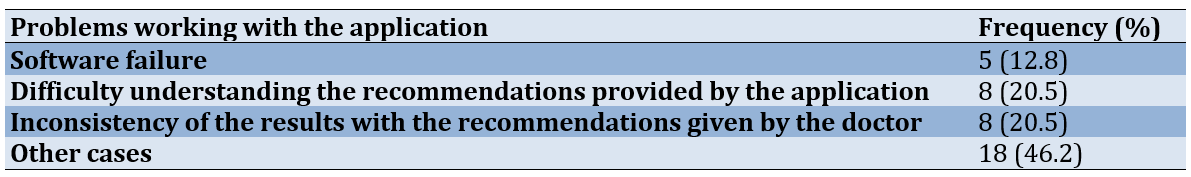
Among the patients, only 39 participants used diabetes applications to manage their disease. According to the data, 33 patients (82.5%) reported the daily blood glucose level monitoring feature as the most useful feature of the application (Table 4).
Table 4. Frequency of issues encountered by patients while working with diabetes applications
There was a statistically significant difference between the health literacy of patients who had used applications for the self-management of their disease and those who had not (p=0.029).
Discussion
This cross-sectional study investigated the e-health literacy of patients with T2D using self-care mobile health applications in Kerman City. The mean score of the e-health literacy in the participants was low. In another study by Guo et al., the mean score of e-health literacy in the participants is 30.16, and only a few participants use eHealth tools [17]. These discrepancies may be due to differences in the number of participants and the mean age of the participants, as well as cultural differences. This study was conducted in Iran with 188 patients with a mean age of 50.1 years old, while another study is performed in Taiwan with 262 patients with a mean age of 44.5 years old. Younger individuals are more likely to use the Internet in their daily lives and have higher e-health literacy than the elderly [30]. On the other hand, 80% of Iranians use the Internet [31], while this number in Taiwan is 91% of the total population [32].
Most of the participants used phone calls among the different m-Health methods for managing their diabetes. The results of a study shows that phone call education about diabetes had a significant impact on the reduction of Hemoglobin A1c (HbA1c) levels and increases patients’ knowledge about diabetes management [33]. According to the participants, the main reason for not using other methods was the lack of knowledge about the existence of these methods. This lack of knowledge is a crucial factor that affects e-health literacy. Awareness of the accessibility of online resources is the predictor associated with a higher e-health literacy level [30].
Only 39 patients used diabetes apps to manage their disease. In contrast. another multinational study reports that 48% of the participants use the apps to manage their diabetes [25]. Smartphone apps can significantly reduce HbA1C levels compared to the Short Message Service (SMS) and websites [34]. There is a relationship between the usability of the apps, e-health literacy, and willingness to use mobile apps. E-health literacy has an impact on patients’ perceptions of usefulness and ease of use. Moreover, perceived usefulness and ease of use influenced patients’ willingness to use mobile apps to manage diabetes [35]. According to the patients, the most useful feature of the apps was the daily blood glucose level report. This result is similar to the result of the previous study [25]. Monitoring blood glucose is a vital task for controlling diabetes; Therefore, measuring and reporting its level daily can be useful for identifying values outside the normal range for proper and timely treatment.
Patients prefer to use m-Health tools for blood glucose control, insulin dose management, and adherence to the diet. Patients prefer features such as nutrient values of foods, blood glucose control, and physical exercise tracker for future apps [25]. In addition to taking insulin, nutrition and physical activity are important in diabetic patients. A healthy meal plan and being active can help to keep the blood glucose level in the normal range.
The main issues with using application were difficulty in understanding the recommendations provided by the application and the inconsistency of the results with the recommendations provided by the doctor. Considering these challenges, researchers believe that mobile health applications should be designed according to guidelines [36]. According to the results of the study by Jezrawi et al., in addition to the desire to use applications, patients heavily rely on doctor's prescriptions [37]. In our study, the majority of the participants stated that they did not know about the existence of applications. Therefore, through increasing e-health literacy and providing necessary training, patients can be directed to use safe applications [37].
Overall, patients who are more knowledgeable about using mobile health applications tend to manage their disease more effectively and achieve better outcomes than other patients. As a result, the complications of the disease will decrease and the quality of life will improve. In this regard, more training from doctors and healthcare providers on the use of trusted applications can improve the e-health literacy of patients.
To the best of our knowledge, this is the first study to investigate the e-health literacy of patients with T2D in using self-care apps in Kerman. However, this study had some limitations. Patient cooperation in filling out the questionnaires was not very good, which may have affected the results. Additionally, this study focused solely on patients with T2D, and better results might have been obtained if all types of diabetes were included.
Conclusion
The e-health literacy level of the participants is low. About one-third of patients use diabetes apps to manage their disease. While, the most useful feature of the studied apps is the daily blood glucose level report.
Acknowledgments: We would like to express our gratitude to the Institute for Future Studies in Health, Kerman University of Medical Sciences, for providing the research environment for this project.
Ethical Permissions: This research was approved by the Ethics Committee of Kerman University of Medical Sciences with Ethical ID IR.KMU.REC.1401.410.
Conflicts of Interests: The authors declare that they have no conflict of interests.
Authors' Contribution: Karbasi Z (First Author), Introduction Writer/Methodologist/Original Researcher (40%); Ram M (Second Author), Assistant Researcher/Statistical Analyst (20%); Hajesmaeel Gohari S (Third Author), Assistant Researcher/Discussion Writer (20%); Sabahi A (Fourth Author Assistant Researcher (20%)
Funding/Support: This study was funded by the Kerman University of Medical Sciences with the research ID 401000698.
One of the most common types of diabetes is T2D [1], with its incidence increasing due to various reasons, including obesity, unhealthy diet, and metabolic syndrome [2-4]. Evidence shows that there is a possibility of more than 500 million individuals suffering from T2D by 2030 [5]. However, many people are not aware of the complications associated with diabetes [6]. Individuals with T2D suffer from complications such as diabetic retinopathy and cardiovascular diseases that affect their quality of life [7]. Self-management can play a significant role in controlling the disease [8]. One of the ways to improve the self-care of patients is acquiring knowledge [9].
The basis of diabetes care is self-management [10]. Today, health literacy is essential [11] and can be highly effective for diseases such as T2D [12]. The ability of individuals to acquire health information and process it to make appropriate decisions is referred to as health literacy [13]. Electronic health literacy is almost defined as similar to health literacy, with the difference that it focuses on electronic information resources [14]. Evidence has shown that high health literacy has an indirect effect on diabetes self-care and blood sugar control [15]. The results of the research by Ernsting et al. revealed that patients with heart diseases or diabetes who used m-Health applications demonstrated a high level of e-Health literacy [16]. According to the literature, mobile applications are widely used by individuals, but not all of them can use these applications for blood sugar control and self-care [17].
Using information technology such as the Internet, mobile phones, and computers, electronic health has provided individuals with the possibility of self-care and disease management [18, 19]. Using electronic health programs, patients can monitor their health status and interact with healthcare providers [20-22]. The positive effects of m-Health applications on self-care and knowledge enhancement among patients with diabetes have been established [23]. Factors such as limited understanding of technology, lack of knowledge about electronic health programs, and lack of tools to access electronic health prevent from using digital interventions for self-management and changing health behaviors [24, 25]. In addition to m-Health applications that have facilitated access to information [26], information available on the Internet is effective in changing health behaviors and disease management [27].
The use of electronic health information and programs among patients with diabetes depends on various factors that need to be examined. Therefore, this study was conducted to investigate the e-health literacy of patients with T2D in using self-care m-Health applications in Kerman City in 2023.
Instrument and Methods
This cross-sectional study was conducted in 2023. Patients referred to a selected clinic in Kerman City were the research population of this study. A total of 198 patients were included in the study using available sampling, and questionnaires were distributed among them. After reviewing the completed questionnaires, 10 participants did not responded to the questionnaire precisely and the remaining 188 questionnaires were analyzed. The inclusion criteria were diagnosis of diabetes and informed consent of the participants, and those who did not cooperate in filling the questionnaire were excluded. The collection tools in this study included a demographic information checklist, an e-health literacy questionnaire, and a researcher-made questionnaire to investigate patients' preferences and tendencies. Demographic information included age, gender, marital status, type of residence, duration of disease, and other diseases. In this study, Norman and Skinner's e-health literacy questionnaire was used, which includes eight components to evaluate e-health literacy [28]. The validity and reliability of the Persian-translated version of the questionnaire were evaluated by Bazm et al., and Cronbach's alpha coefficient was reported as 0.88 [29]. The third part of the researcher-made questionnaire includes 14 questions about m-Health methods for the self-management of the disease, patient preferences and inclinations for using a variety of m-Health methods, patient preferences and inclinations for using m-Health for self-management of T2D, and intervals and sequences preferred to receive training. Experts in health information management and medical informatics were used to determine content validity, and the reliability of the questionnaire was calculated based on Cronbach's alpha coefficient and using SPSS version 26 software. Accordingly, Cronbach's alpha coefficient of this questionnaire is 0.876. Frequency, mean, and standard deviation were used to describe the data. Analytical statistical methods such as Mann-Whitney were also employed. Confidentiality of information was maintained in this study, and the questionnaires were completed voluntarily and anonymously.
Findings
188 individuals participated in this research, 103 (54.8%) participants were men and the rest were women. The average age of the participants in the research was 50.17±12.91 years, with the lowest age being 22 years old and the highest age being 80 years old. A total of 151 participants (80.3%) were married and the rest were single. Most of the participants (88.8%) lived in urban areas. Among the participants, 38 individuals (20.2%) were employed. In terms of disease duration, 69 individuals (36.7%) had been suffering from the disease for one to five years (Table 1).
Table 1. Frequency distribution of demographic variables in study participants
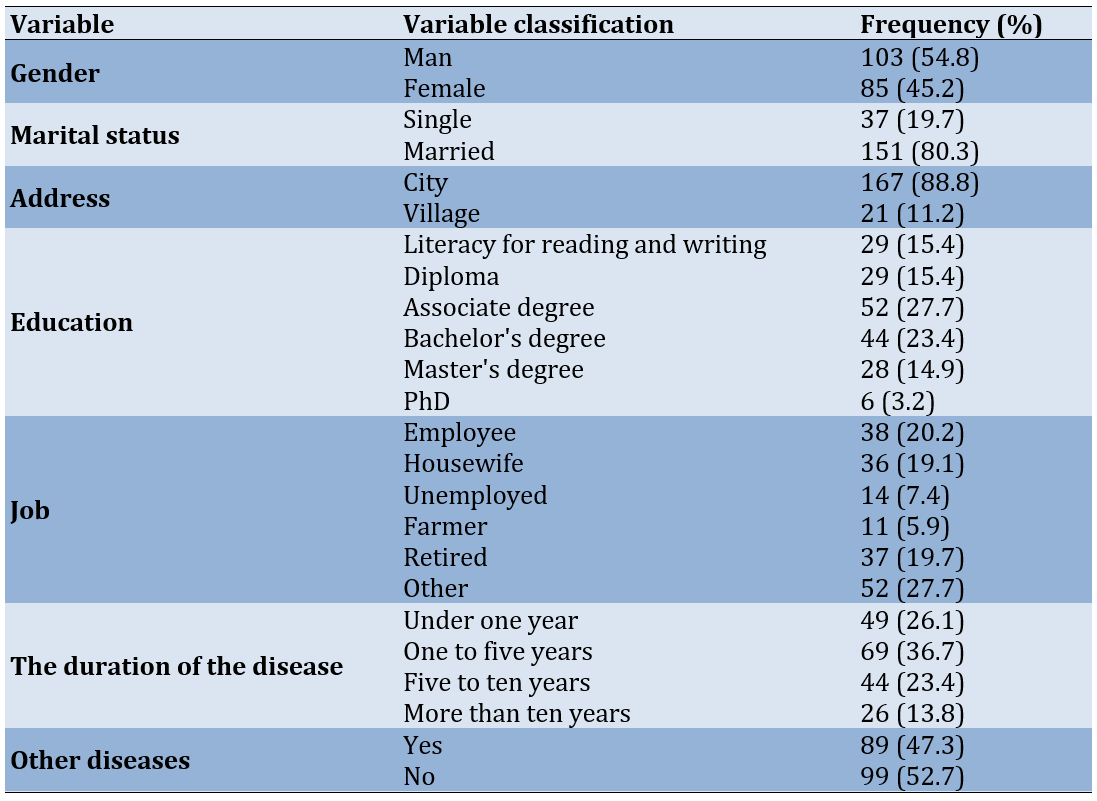
Regarding e-health literacy questions, 51.3% of the participants disagreed and did not know what resources are related to health issues on the Internet. The majority of the participants (35.1%) chose the disagree option for question 2. Regarding question 3, 35.9% of the participants disagreed and did not know how to find healthcare resources on the Internet. In response to questions 4, 5, 6, 7, and 8, the percentages of participants who chose "neither agree nor disagree" were 33.1%, 35.5%, 39.2%, 30.3%, and 29.7%, respectively (Table 2).
Table 2. Frequency of answers to e-health literacy questions
Based on the obtained information, the average health literacy score of the participants in the study was 24.75±9.04. The number of participants who used methods based on m-Health to manage their disease was 100, and telephone calls were the most frequent with 54% among the different methods based on m-Health.
Out of 188 patients participating in the study, 88 had not used any of the m-Health methods in the management of their disease, and the majority of the participants (61.4%) mentioned that they were unaware that these methods were available for managing their disease (Table 3).
Table 3. The frequency of reasons for not using m-Health-based programs in disease management by type 2 diabetes (T2D) patients
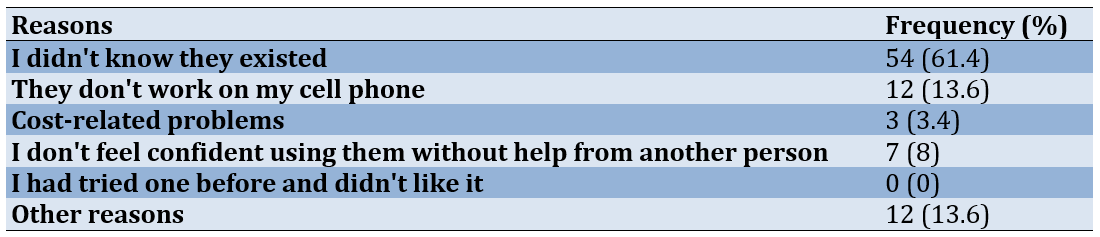
Among the patients, only 39 participants used diabetes applications to manage their disease. According to the data, 33 patients (82.5%) reported the daily blood glucose level monitoring feature as the most useful feature of the application (Table 4).
Table 4. Frequency of issues encountered by patients while working with diabetes applications
There was a statistically significant difference between the health literacy of patients who had used applications for the self-management of their disease and those who had not (p=0.029).
Discussion
This cross-sectional study investigated the e-health literacy of patients with T2D using self-care mobile health applications in Kerman City. The mean score of the e-health literacy in the participants was low. In another study by Guo et al., the mean score of e-health literacy in the participants is 30.16, and only a few participants use eHealth tools [17]. These discrepancies may be due to differences in the number of participants and the mean age of the participants, as well as cultural differences. This study was conducted in Iran with 188 patients with a mean age of 50.1 years old, while another study is performed in Taiwan with 262 patients with a mean age of 44.5 years old. Younger individuals are more likely to use the Internet in their daily lives and have higher e-health literacy than the elderly [30]. On the other hand, 80% of Iranians use the Internet [31], while this number in Taiwan is 91% of the total population [32].
Most of the participants used phone calls among the different m-Health methods for managing their diabetes. The results of a study shows that phone call education about diabetes had a significant impact on the reduction of Hemoglobin A1c (HbA1c) levels and increases patients’ knowledge about diabetes management [33]. According to the participants, the main reason for not using other methods was the lack of knowledge about the existence of these methods. This lack of knowledge is a crucial factor that affects e-health literacy. Awareness of the accessibility of online resources is the predictor associated with a higher e-health literacy level [30].
Only 39 patients used diabetes apps to manage their disease. In contrast. another multinational study reports that 48% of the participants use the apps to manage their diabetes [25]. Smartphone apps can significantly reduce HbA1C levels compared to the Short Message Service (SMS) and websites [34]. There is a relationship between the usability of the apps, e-health literacy, and willingness to use mobile apps. E-health literacy has an impact on patients’ perceptions of usefulness and ease of use. Moreover, perceived usefulness and ease of use influenced patients’ willingness to use mobile apps to manage diabetes [35]. According to the patients, the most useful feature of the apps was the daily blood glucose level report. This result is similar to the result of the previous study [25]. Monitoring blood glucose is a vital task for controlling diabetes; Therefore, measuring and reporting its level daily can be useful for identifying values outside the normal range for proper and timely treatment.
Patients prefer to use m-Health tools for blood glucose control, insulin dose management, and adherence to the diet. Patients prefer features such as nutrient values of foods, blood glucose control, and physical exercise tracker for future apps [25]. In addition to taking insulin, nutrition and physical activity are important in diabetic patients. A healthy meal plan and being active can help to keep the blood glucose level in the normal range.
The main issues with using application were difficulty in understanding the recommendations provided by the application and the inconsistency of the results with the recommendations provided by the doctor. Considering these challenges, researchers believe that mobile health applications should be designed according to guidelines [36]. According to the results of the study by Jezrawi et al., in addition to the desire to use applications, patients heavily rely on doctor's prescriptions [37]. In our study, the majority of the participants stated that they did not know about the existence of applications. Therefore, through increasing e-health literacy and providing necessary training, patients can be directed to use safe applications [37].
Overall, patients who are more knowledgeable about using mobile health applications tend to manage their disease more effectively and achieve better outcomes than other patients. As a result, the complications of the disease will decrease and the quality of life will improve. In this regard, more training from doctors and healthcare providers on the use of trusted applications can improve the e-health literacy of patients.
To the best of our knowledge, this is the first study to investigate the e-health literacy of patients with T2D in using self-care apps in Kerman. However, this study had some limitations. Patient cooperation in filling out the questionnaires was not very good, which may have affected the results. Additionally, this study focused solely on patients with T2D, and better results might have been obtained if all types of diabetes were included.
Conclusion
The e-health literacy level of the participants is low. About one-third of patients use diabetes apps to manage their disease. While, the most useful feature of the studied apps is the daily blood glucose level report.
Acknowledgments: We would like to express our gratitude to the Institute for Future Studies in Health, Kerman University of Medical Sciences, for providing the research environment for this project.
Ethical Permissions: This research was approved by the Ethics Committee of Kerman University of Medical Sciences with Ethical ID IR.KMU.REC.1401.410.
Conflicts of Interests: The authors declare that they have no conflict of interests.
Authors' Contribution: Karbasi Z (First Author), Introduction Writer/Methodologist/Original Researcher (40%); Ram M (Second Author), Assistant Researcher/Statistical Analyst (20%); Hajesmaeel Gohari S (Third Author), Assistant Researcher/Discussion Writer (20%); Sabahi A (Fourth Author Assistant Researcher (20%)
Funding/Support: This study was funded by the Kerman University of Medical Sciences with the research ID 401000698.
Article Type: Descriptive & Survey |
Subject:
Technology of Health Education
Received: 2024/07/8 | Accepted: 2024/08/11 | Published: 2024/08/29
Received: 2024/07/8 | Accepted: 2024/08/11 | Published: 2024/08/29
References
1. Tripathi BK, Srivastava AK. Diabetes mellitus: Complications and therapeutics. Med Sci Monit. 2006;12(7):130-47. [Link]
2. Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care. 2010;33(12):e147-67. [Link] [DOI:10.2337/dc10-9990]
3. Ginter E, Simko V. Global prevalence and future of diabetes mellitus. Adv Exp Med Biol. 2012;771:35-41. [Link] [DOI:10.1007/978-1-4614-5441-0_5]
4. Ginter E, Simko V. Type 2 diabetes mellitus, pandemic in 21st century. Adv Exp Med Biol. 2012;771:42-50. [Link] [DOI:10.1007/978-1-4614-5441-0_6]
5. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311-21. [Link] [DOI:10.1016/j.diabres.2011.10.029]
6. Beagley J, Guariguata L, Weil C, Motala AA. Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin Pract. 2014;103(2):150-60. [Link] [DOI:10.1016/j.diabres.2013.11.001]
7. Zhao Y, Jiang Z, Guo C. New hope for type 2 diabetics: Targeting insulin resistance through the immune modulation of stem cells. Autoimmun Rev. 2011;11(2):137-42. [Link] [DOI:10.1016/j.autrev.2011.09.003]
8. Hildebrand JA, Billimek J, Lee JA, Sorkin DH, Olshansky EF, Clancy SL, et al. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: A systematic review and meta-analysis. Patient Educ Couns. 2020;103(2):266-75. [Link] [DOI:10.1016/j.pec.2019.09.009]
9. Afroz A, Alramadan MJ, Hossain MN, Romero L, Alam K, Magliano DJ, et al. Cost-of-illness of type 2 diabetes mellitus in low and lower-middle income countries: A systematic review. BMC Health Serv Res. 2018;18:972. [Link] [DOI:10.1186/s12913-018-3772-8]
10. Bonger Z, Shiferaw S, Tariku EZ. Adherence to diabetic self-care practices and its associated factors among patients with type 2 diabetes in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2018;12:963-70. [Link] [DOI:10.2147/PPA.S156043]
11. Yarmohammadi S, Momenyan S, Ghaffari M, Ali R, Azizpour M. Impact of functional, communicative and critical health literacy on glycemic control among patients with type 2 diabetes, and the mediating role of self-care. Psychol Res Behav Manag. 2019;12:427-35. [Link] [DOI:10.2147/PRBM.S207466]
12. Guo XM, Zhai X, Hou BR. Adequacy of health literacy and its effect on diabetes self-management: A meta-analysis. Aus J Prim Health. 2020;26(6):458-65. [Link] [DOI:10.1071/PY20079]
13. Selden CR, Zorn M, Ratzan S, Parker RM. National library of medicine current bibliographies in medicine: Health literacy. Bethesda: National Institutes of Health; 2000. [Link]
14. Kim H, Xie B. Health literacy in the eHealth era: A systematic review of the literature. Patient Educ Couns. 2017;100(6):1073-82. [Link] [DOI:10.1016/j.pec.2017.01.015]
15. Osborn CY, Bains SS, Egede LE. Health literacy, diabetes self-care, and glycemic control in adults with type 2 diabetes. Diabetes Technol Ther. 2010;12(11):913-9. [Link] [DOI:10.1089/dia.2010.0058]
16. Ernsting C, Stühmann LM, Dombrowski SU, Voigt-Antons JN, Kuhlmey A, Gellert P. Associations of health app use and perceived effectiveness in people with cardiovascular diseases and diabetes: Population-based survey. JMIR Mhealth Uhealth. 2019;7(3):e12179. [Link] [DOI:10.2196/12179]
17. Guo SHM, Hsing HC, Lin JL, Lee CC. Relationships between mobile eHealth literacy, diabetes self-care, and glycemic outcomes in taiwanese patients with type 2 diabetes: Cross-sectional study. JMIR Mhealth Uhealth. 2021;9(2):e18404. [Link] [DOI:10.2196/18404]
18. Boogerd EA, Arts T, Engelen LJ, Van De Belt TH. "What is eHealth": Time for an update?. JMIR Res Protoc. 2015;4(1):e29. [Link] [DOI:10.2196/resprot.4065]
19. Vandelanotte C, Müller AM, Short CE, Hingle M, Nathan N, Williams SL, et al. Past, present, and future of eHealth and mHealth research to improve physical activity and dietary behaviors. J Nutr Educ Behav. 2016;48(3):219-28. [Link] [DOI:10.1016/j.jneb.2015.12.006]
20. Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: A systematic review and meta-analysis. PLoS Med. 2013;10(1):e1001363. [Link] [DOI:10.1371/journal.pmed.1001363]
21. Fiksdal AS, Kumbamu A, Jadhav AS, Cocos C, Nelsen LA, Pathak J, et al. Evaluating the process of online health information searching: A qualitative approach to exploring consumer perspectives. J Med Internet Res. 2014;16(10):e224. [Link] [DOI:10.2196/jmir.3341]
22. Ross J, Stevenson F, Lau R, Murray E. Factors that influence the implementation of e-health: A systematic review of systematic reviews (an update). Implement Sci. 2016;11(1):146. [Link] [DOI:10.1186/s13012-016-0510-7]
23. El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: Status and potential. J Diabetes Sci Technol. 2013;7(1):247-62. [Link] [DOI:10.1177/193229681300700130]
24. Reiners F, Sturm J, Bouw LJ, Wouters EJ. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health. 2019;16(4):645. [Link] [DOI:10.3390/ijerph16040645]
25. Adu MD, Malabu UH, Malau-Aduli AE, Malau-Aduli BS. Users' preferences and design recommendations to promote engagements with mobile apps for diabetes self-management: Multi-national perspectives. PloS One. 2018;13(12):e0208942. [Link] [DOI:10.1371/journal.pone.0208942]
26. Jo S, Park HA. Development and evaluation of a smartphone application for managing gestational diabetes mellitus. Healthc Inform Res. 2016;22(1):11-21. [Link] [DOI:10.4258/hir.2016.22.1.11]
27. Nettleton S, Burrows R, O'Malley L. The mundane realities of the everyday lay use of the internet for health, and their consequences for media convergence. Sociol Health Illn. 2005;27(7):972-92. [Link] [DOI:10.1111/j.1467-9566.2005.00466.x]
28. Norman CD, Skinner HA. eHEALS: The eHealth literacy scale. J Med Internet Res. 2006;8(4):e27. [Link] [DOI:10.2196/jmir.8.4.e27]
29. Bazm S, Mirzaei M, Fallahzadeh H, Bazm R. Validity and reliability of Iranian version of eHealth literacy scale. J Community Health Res. 2016;5(2):121-30. [Link]
30. Shiferaw KB, Tilahun BC, Endehabtu BF, Gullslett MK, Mengiste SA. E-health literacy and associated factors among chronic patients in a low-income country: A cross-sectional survey. BMC Med Inform Decis Mak. 2020;20(1):181. [Link] [DOI:10.1186/s12911-020-01202-1]
31. Statista. Number of internet users in Iran from 2013 to 2028 [Internet]. New York: Statista [cited 2024 Jan 14]. Available from: https://www.statista.com/forecasts/1146999/internet-users-in-iran. [Link]
32. Statista. Number of internet users in Taiwan from January 2014 to January 2024 [Internet]. New York: Statista [cited 2024 Jan 14]. Available from: https://www.statista.com/statistics/1296415/taiwan-online-population/. [Link]
33. Kundury KK, Bovilla VR, Kumar KSP, Chandrashekarappa SM, Madhunapantula SV, Hathur B. Providing diabetes education through phone calls assisted in the better control of hyperglycemia and improved the knowledge of patients on diabetes management. Healthcare. 2023;11(4):528. [Link] [DOI:10.3390/healthcare11040528]
34. Moschonis G, Siopis G, Jung J, Eweka E, Willems R, Kwasnicka D, et al. Effectiveness, reach, uptake, and feasibility of digital health interventions for adults with type 2 diabetes: A systematic review and meta-analysis of randomised controlled trials. Lancet Digit Health. 2023;5(3):e125-43. [Link]
35. Zhang M, Zhang H, Zhu R, Yang H, Chen M, Wang X, et al. Factors affecting the willingness of patients with type 2 diabetes to use digital disease management applications: A cross-sectional study. Front Public Health. 2023;11:1259158. [Link] [DOI:10.3389/fpubh.2023.1259158]
36. Ye Q, Khan U, Boren SA, Simoes EJ, Kim MS. An analysis of diabetes mobile applications features compared to AADE7™: Addressing self-management behaviors in people with diabetes. J Diabetes Sci Technol. 2018;12(4):808-16. [Link] [DOI:10.1177/1932296818754907]
37. Jezrawi R, Balakumar S, Masud R, Gabizon I, Bhagirath V, Varughese J, et al. Patient and physician perspectives on the use and outcome measures of mHealth apps: Exploratory survey and focus group study. Digit Health. 2022;8:20552076221102773. [Link] [DOI:10.1177/20552076221102773]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |