Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 323-329 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zarean F, Sheykholeslami A, Sadri Damirchi E, Rezaei Sharif A. Effectiveness of Mindfulness-Based Cognitive Therapy on Infertility-Related Stigma and Sexual Self-Esteem in Infertile Women. Health Educ Health Promot 2024; 12 (2) :323-329
URL: http://hehp.modares.ac.ir/article-5-75559-en.html
URL: http://hehp.modares.ac.ir/article-5-75559-en.html
1- Department of Counseling, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran
Keywords: Mindfulness [MeSH], Cognitive Therapy [MeSH], Social Stigma [MeSH], Self-Esteem [MeSH], Infertility [MeSH], Women [MeSH]
Full-Text [PDF 622 kb]
(2704 Downloads)
| Abstract (HTML) (1427 Views)
Full-Text: (182 Views)
Introduction
Marriage has been widely recognized as a beneficial and structuring element in societies, fulfilling the personal needs of individuals [1]. It provides a sense of attachment and security that surpasses any other human relationship. Understanding the quality and value of marriage is crucial for comprehending its impact on all processes within and outside the family [2]. As marital relationships develop, various factors can intertwine and contribute to a multitude of challenges for couples [3]. Infertility is one such factor that affects individuals, families, marriages, and societies across cultures, causing significant stress [4].
Infertility is defined by Vander Borght & Wyns [5] as the failure to achieve a clinical pregnancy after at least 12 months or more of regular sexual intercourse. Researchers have reported feelings of helplessness in these individuals, especially with prolonged and sometimes unsuccessful treatments [6]. Infertility can also lead to disrupted marital quality, intimacy, fear of relationship dissolution, and other psychological disorders [7]. Individuals' responses to the infertility crisis vary depending on their cognitive interpretation of the phenomenon and the emotional regulation styles they employ to cope with the negative emotions experienced as a result of the awareness of their inability to have children [8].
When an individual's traits and actions are deemed non-normative by society, they may experience feelings of stigma and pressure, leading to feelings of inadequacy [9]. Yang et al. [10] emphasized that stigma is not an individual problem or a component of an illness but rather a social issue. Social stigma refers to prejudiced judgments and discrimination against individuals belonging to a particular group [11]. In our society, the issue of infertility takes on a deeper dimension due to our unique cultural structure. The emotional consequences of experiencing infertility stigma for families generally include feelings of disrespect and discrimination in society. To cope with these feelings, families often choose isolation and withdrawal from social interactions, believing it prevents the disclosure of their situation [12].
The most detrimental consequences of stigma arise when families internalize societal stigma and adopt negative societal views towards themselves, leading to internal or emotional stigma [13]. Given the negative impacts of stigma on the mental health of families and the importance of family in the care, follow-up, and continuation of infertility treatment, stigma is considered a fundamental and crucial issue that demands attention in the field of mental health [14]. Studies by Yu et al. [15] have shown that individualistic cultures exhibit lower stigmatizing attitudes compared to collectivistic cultures. In Iran, a collectivistic society, family members are naturally more concerned about the negative impacts of infertility on their family's reputation and others' perceptions rather than the negative impact on themselves [16, 17].
Beyond the physical challenges, infertility can significantly impact a woman's sense of self, particularly her sexual self-esteem [18]. Sexual self-esteem refers to a woman's feelings and beliefs about herself as a sexual being. It encompasses aspects like desirability, attractiveness, and confidence in her sexual abilities [19]. Examining sexual self-esteem in infertile women is crucial for several reasons. Firstly, infertility can lead to a distorted view of femininity and womanhood. Societal pressures often link motherhood to a woman's worth, and the inability to conceive can trigger feelings of inadequacy. Secondly, the stress and emotional strain associated with infertility can negatively impact sexual desire, arousal, and satisfaction. This creates a vicious cycle, where low sexual self-esteem further hinders intimacy [20]. Riazi et al. [21] consider negative perceptions as an important factor in sexual disorders and suggest focusing on psychological/cognitive factors and using cognitive restructuring methods for treating sexual disorders. When a person experiencing infertility develops a stigma of infertility, they may also develop negative thoughts about themselves and their sexual relationships, affecting their sexual self-esteem. Understanding how infertility shapes a woman's sexual self-esteem empowers healthcare professionals to provide holistic care. By addressing these concerns, they can help women navigate this challenging experience and maintain a healthy, fulfilling sex life [18].
Mindfulness-based cognitive therapy (MBCT) is one of the effective interventions for the population of infertile women [22]. This therapy is a type of cognitive therapy that utilizes mindfulness. Mindfulness is defined as paying attention in a specific, purposeful way, in the present moment, without judgment or prejudice [23]. Mindfulness leads to awareness and understanding of emotions, acceptance of emotions, the ability to control impulsive behaviors, and goal-oriented behaviors when experiencing negative emotions, in a way that achieves goals for the individual [24]. Clinical psychology and psychiatry have offered several mindfulness-based therapy programs since the 1970s to help people who experience various psychological conditions [25]. Mindfulness also involves regulating cognitive evaluations and objectively observing experiences [26]. Additionally, mindfulness allows for more adaptive coping strategies and management of unwanted stimuli [27]. This method helps the individual observe their thoughts without judgment, reducing anxiety [28]. Based on the research background, the present study aimed to investigate the effectiveness of MBCT on infertility-related stigma and sexual self-esteem in infertile women.
Materials and Methods
The present study was a three-stage semi-experimental research with two groups (experimental and control). The statistical population of this study included all infertile women referred to infertility treatment centers in Isfahan City, Iran in 2023. In the present study, 40 people who were willing to participate in the research project were selected as a sample and were randomly assigned to two groups of 20, experimental and control. The sample size was determined using a power analysis with a desired power of 0.80, an alpha level of 0.05, an anticipated large effect size of 0.85, and a projected attrition rate of 10%. After obtaining informed consent, the pre-test was administered simultaneously to both intervention and control groups using the infertility stigma and sexual self-esteem questionnaires under the same conditions. The inclusion criteria were an age range of 25-45 years, at least secondary education and infertility after medical intervention and confirmation by a specialist. The exclusion criteria were individuals who were still in the evaluation and infertility testing stage, pregnancy during the study, use of psychiatric medications due to serious mental disorders and absence from more than two therapy sessions. After the last session, the post-test was administered to both groups (experimental and control). After the intervention on the experimental group, a 45-day follow-up was conducted to determine the long-term effectiveness of this approach.
Instrument
Infertility Stigma Scale (ISS)
The Infertility Stigma Scale (ISS) is a psychometric instrument designed to assess perceived stigma among infertile women [29]. The 27-item scale utilizes a 5-point Likert scoring system to capture four distinct dimensions of infertility stigma: Self-devaluation, social withdrawal, public stigma, and family stigma. Scores range from 27 (lowest) to 135 (highest), reflecting the degree of perceived stigma. Fu et al. [29] demonstrated the scale's high internal consistency (Cronbach's alpha>0.94).
Sexual Self-Esteem Inventory (SSEI)
The Sexual Self-Esteem Inventory (SSEI) is a well-established 35-item self-report measure developed by Doyle Zeanah & Schwarz [30] to assess women's sexual self-esteem. Respondents use a 5-point Likert scale (1=strongly disagree, 5=strongly agree) to answer questions across five subscales: Skill and experience, control, attractiveness, moral judgment, and adaptiveness. These subscales capture various aspects of sexual self-esteem, with higher total scores indicating greater positive self-regard in the sexual domain. The SSEI demonstrates acceptable internal consistency, with Cronbach's alpha coefficients reported by Farokhi & Shareh [31] ranging from 0.68 to 0.82 for the subscales and 0.82 for the total scale.
Intervention
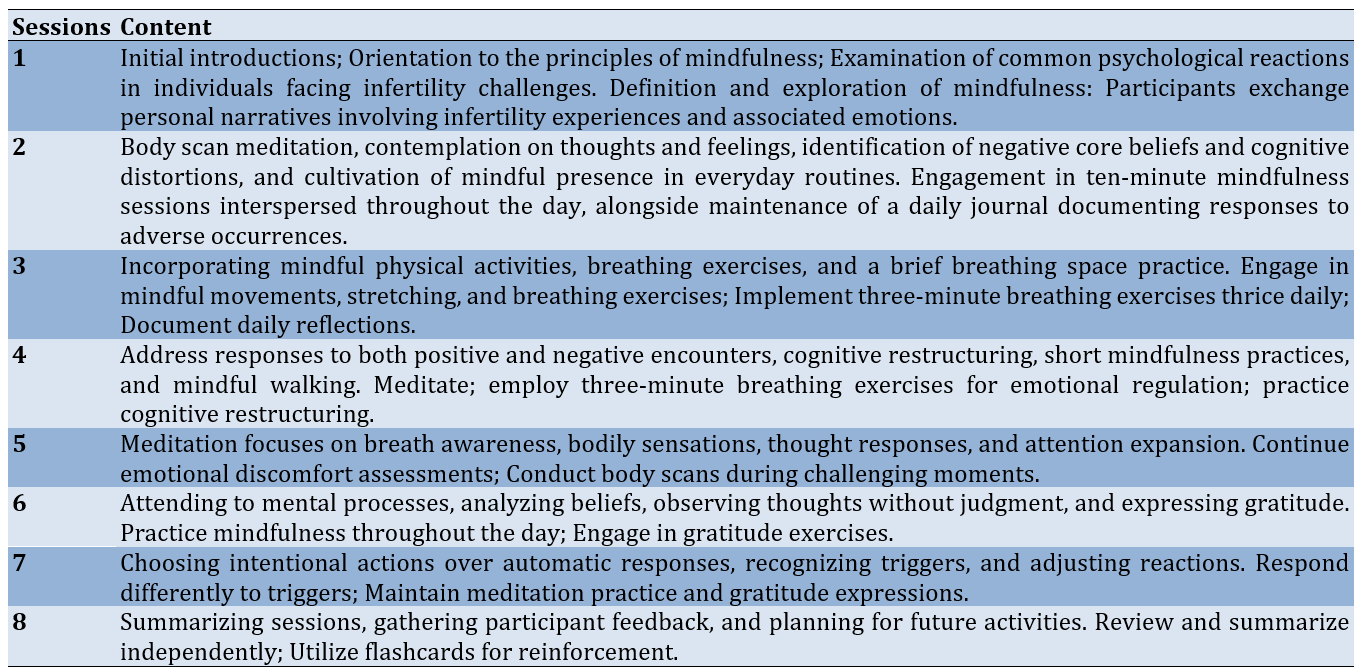
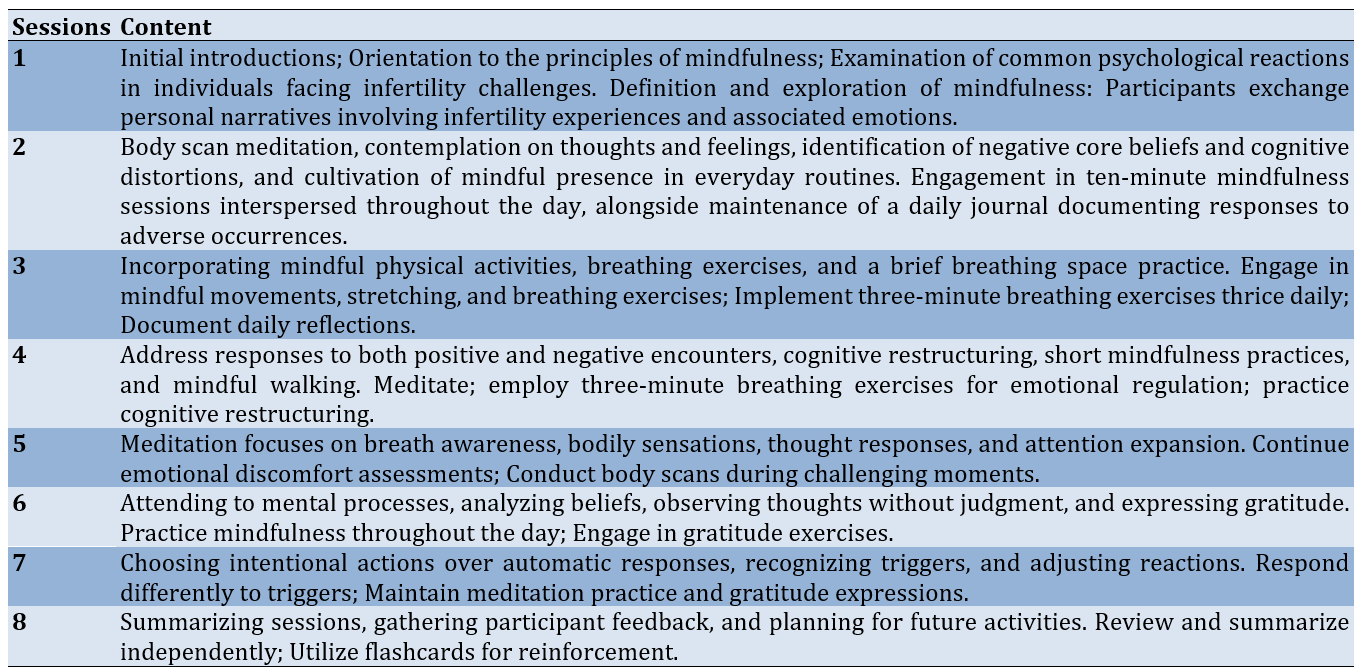
The intervention group received MBCT sessions [32] in the form of eight sessions (one 90-minute session per week) (Table 1). The control group did not receive this intervention and was placed on a waiting list.
Table 1. A summary of the mindfulness-based cognitive therapy sessions
Questionnaires were filled with the participants’ satisfaction and written informed consent was obtained from the participants in this study.
Data analysis
Data were analyzed using repeated-measures ANOVA with SPSS version 24.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Findings
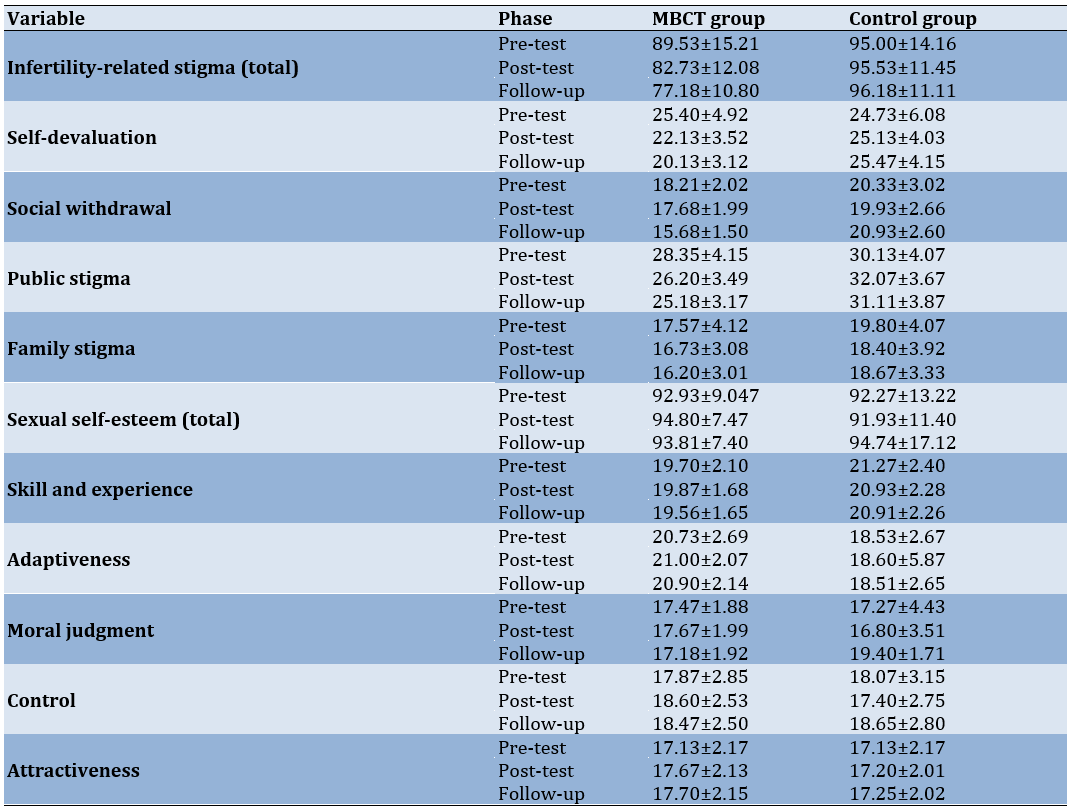
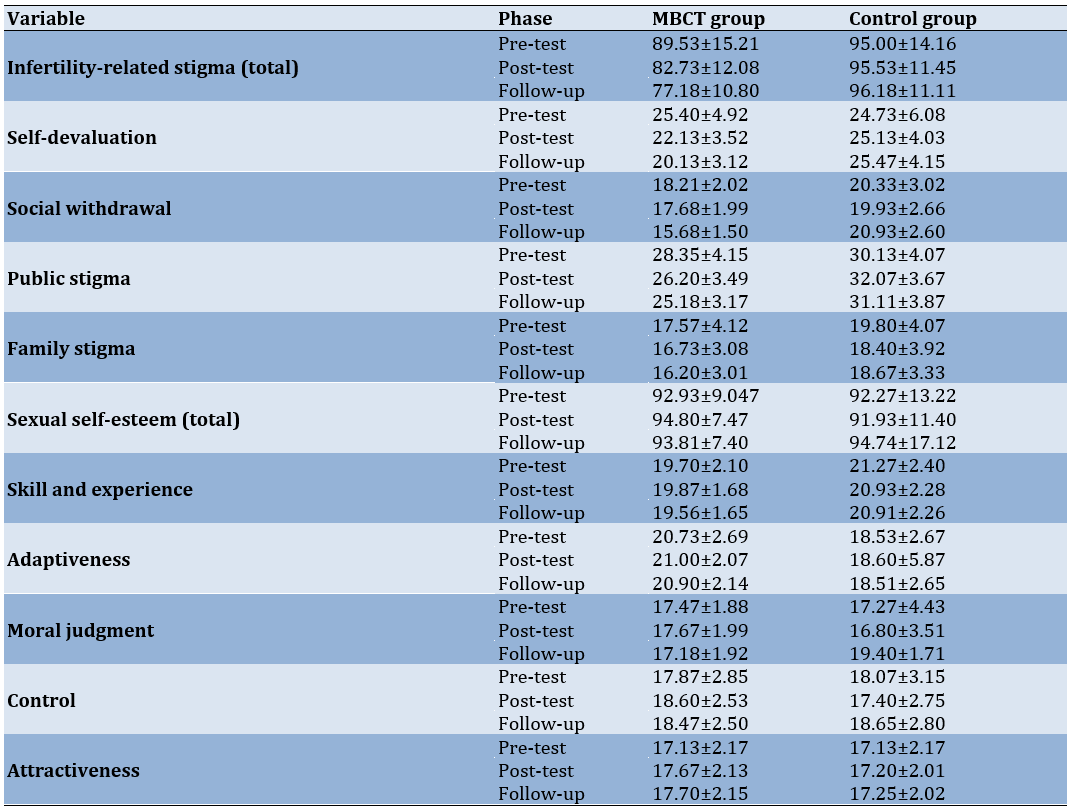
The study involved 40 infertile women. The mean age of the women in the experimental and control groups was 33.70±6.39 and 35.42±5.58 years, respectively. The means and standard deviations of infertility-related stigma and sexual self-esteem scores, disaggregated by experimental and control groups were all calculated (Table 2).
Table 2. Mean and standard deviations (SD) of infertility-related stigma and sexual self-esteem
Prior to conducting the repeated-measures ANOVA, the assumptions of homogeneity of variances and normality of distribution were assessed. Levene's test for equality of variances indicated no significant differences between the groups regarding the variances of the research variables (p>0.05). Furthermore, the Shapiro-Wilk test for normality revealed that the distribution of the scores did not deviate significantly from a normal distribution (p>0.05). As the assumption of sphericity was violated for all the components under investigation, the Greenhouse-Geisser correction was employed.
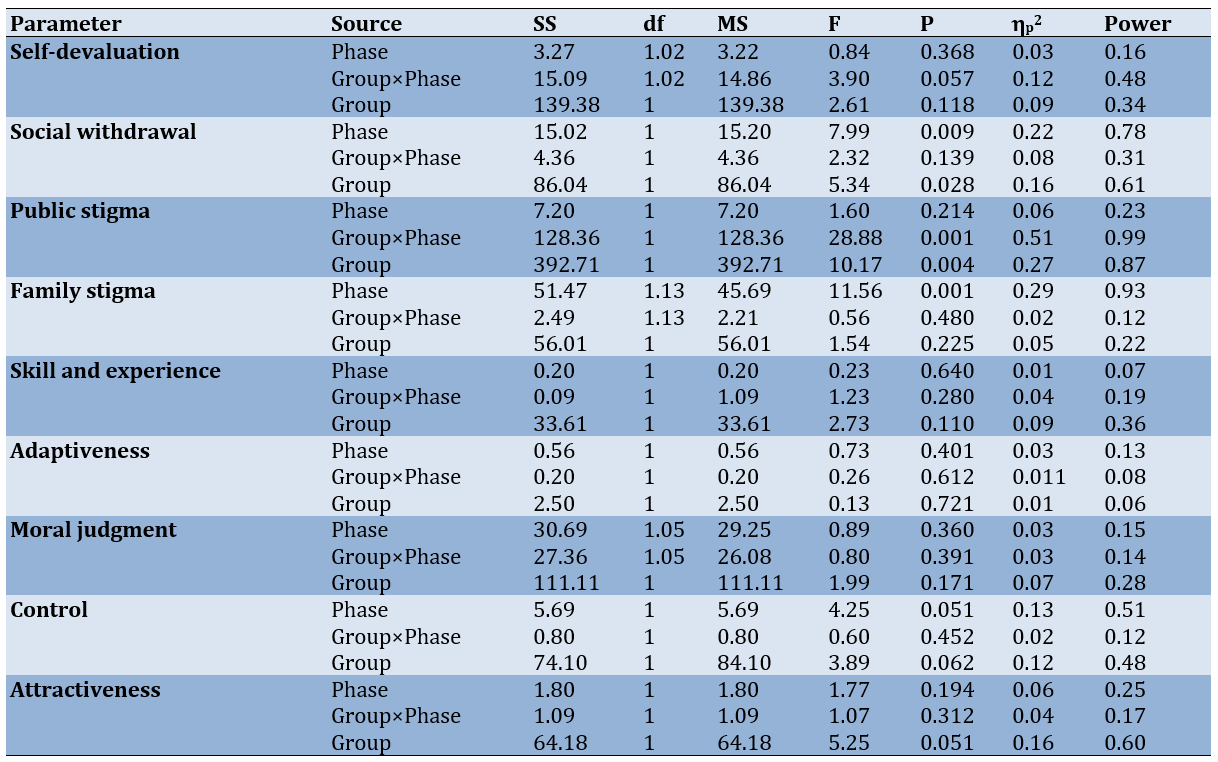
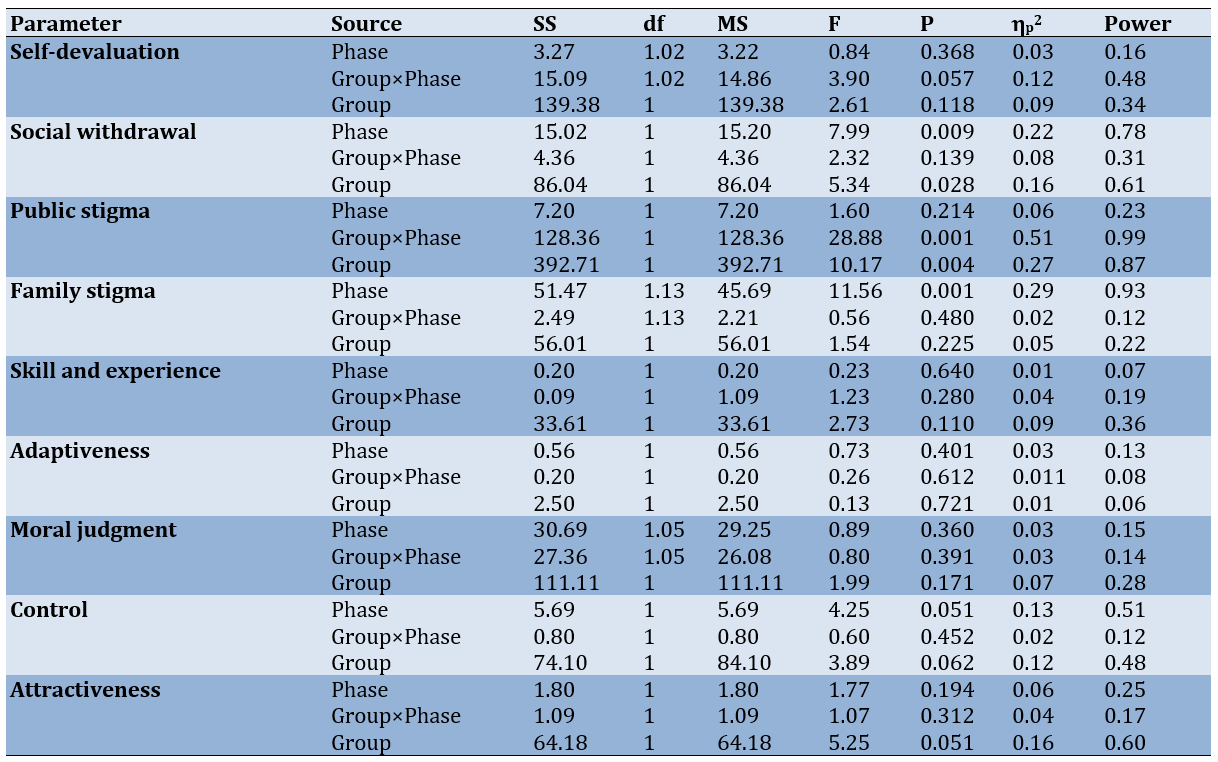
The results of the repeated-measures ANOVA examined the between-subjects and within-subjects effects at the pre-test, post-test, and follow-up stages (Table 3). Significant within-subject effects were observed for the dimensions of social withdrawal (p=0.009) and family stigma (p=0.001) across the pre-test, post-test, and follow-up time points, indicating that these dimensions changed significantly over time. Additionally, a significant between-subjects effect was found for the source group, suggesting that there was a significant difference between the experimental and control groups in terms of the dimensions of social withdrawal (p=0.028) and public stigma (p=0.004). However, the effectiveness of MBCT on the dimensions of personal worthlessness and family stigma was not confirmed. No significant within-subject effects were observed for the dimension of sexual self-esteem across the three-time points of pre-test, post-test, and follow-up. Furthermore, the between-subjects effect for the source group was not significant, indicating that there was no significant difference between the experimental and control groups in terms of sexual self-esteem, and the effectiveness of the intervention was not confirmed.
Table 3. Results of the repeated-measures ANOVA
Discussion
The present study examined the efficacy of MBCT in mitigating the multifaceted dimensions of infertility-related stigma while also evaluating its impact on sexual self-esteem among infertile women. Results indicated that MBCT was efficacious in reducing the psychological burden associated with social withdrawal, familial stigma, and public scrutiny often experienced by individuals struggling with infertility. However, the intervention did not yield significant improvements in sexual self-esteem within the study parameters. These findings align with previous research highlighting the potential benefits of MBCT in addressing the emotional and social challenges inherent to infertility [22, 26].
Mindfulness can be conceptualized as an emotion regulation strategy that fosters present-moment awareness [24]. By encouraging acceptance rather than avoidance of distressing experiences, mindfulness may have facilitated greater emotional flexibility among participants [26]. This increased flexibility can be contributed to reductions in infertility-related stigma. Cultivating curiosity towards thoughts and feelings through mindfulness can mitigate the automatic negative responses often triggered by emotional distress [27]. This process may have enabled participants to approach infertility-related challenges with greater openness, reducing feelings of isolation and shame. Moreover, mindfulness can foster self-compassion, a crucial factor in coping with infertility [29]. By treating oneself with kindness and understanding, individuals may be better equipped to manage the emotional toll of infertility and reduce associated stigma. The structured nature of the MBCT intervention likely equipes participants with the skills to integrate mindfulness into daily life, promoting sustained benefits in emotional regulation and resilience [30]. The potential role of perceived social support in mitigating the impact of stigma should also be considered [28]. By fostering a sense of connection and understanding, mindfulness may have enhanced participants' social support networks, thereby reducing the negative effects of stigma.
Mindfulness, by reflecting acceptance of experiences without judgment and avoiding suppression attempts, can lead to a reduction in individuals’ reactive behaviors when faced with stigma, thereby decreasing their social withdrawal. It allows them to interrupt negative infertility-related cognitions that arise from perceptions of others and establish positive relationships with those around them [25]. By fostering a non-judgmental awareness of their feelings and thoughts, individuals practicing mindfulness can transform their relationship with both internal and external stimuli. Instead of succumbing to the automatic, often negative reactions typically associated with stigma, they become equipped to respond more thoughtfully and constructively. Mindfulness and its training promote emotion regulation without judgment and enhance awareness of psychological and physical sensations, facilitating a clear observation and acceptance of emotions and physical phenomena as they occur. This acceptance is crucial, as it allows individuals to confront the emotional turmoil often associated with infertility rather than avoiding it. Research indicates that avoidance behaviors can exacerbate feelings of sadness, anxiety, and frustration, creating a cycle of emotional distress [26]. Mindfulness interrupts this cycle by encouraging individuals to acknowledge their feelings without the added layer of judgment, thus breaking the patterns that lead to emotional distress and disengagement. Moreover, mindfulness can play a significant role in modifying negative infertility-related beliefs [22]. By recognizing and observing these beliefs as passing thoughts rather than absolutes, individuals can begin to challenge the validity of stigmatizing narratives. Mindfulness facilitates cognitive restructuring, allowing individuals to replace harmful beliefs associated with infertility (such as feelings of inadequacy or shame) with more compassionate and realistic perspectives. This cognitive shift can lead to reduced stigma, as individuals no longer internalize negative societal beliefs but instead foster a self-accepting attitude. Recognizing these challenges and providing interventions such as mindfulness-based therapies is a crucial component of treatment for improving psychological well-being.
Mindfulness-based approaches, including MBCT, specifically cater to individuals dealing with stigma by equipping them with tools to face their emotional experiences head-on rather than retreating into avoidance. In MBCT, infertile women engage in repeated practices of intentionally directing attention to a neutral object (e.g., breath flow) and observing their thoughts, emotions, or bodily sensations [28]. This practice allows them to develop a deeper awareness of their internal experiences and fosters a sense of autonomy over how they respond to stressors. Additionally, participation in such mindfulness practices may promote a sense of community among individuals undergoing similar experiences. Group settings often associated with mindfulness training can provide social support, reducing feelings of isolation that are common among those facing infertility. Sharing experiences in a safe, structured environment can help break down walls of stigma, allowing individuals to connect with others who understand their struggles [29]. This sense of connection is vital, as it not only alleviates feelings of loneliness but encourages communal resilience against shared experiences of stigma. Importantly, the implications of mindfulness extend beyond immediate emotional relief; They may also foster long-term psychological health. Regular mindfulness practice can lead to lasting changes in brain function and structure that enhance emotion regulation capacities. Studies suggest that mindfulness training positively impacts neural pathways associated with emotional reactivity and regulation, potentially leading to sustained improvements in mental health outcomes [30]. This suggests that mindfulness isn’t merely a temporary coping mechanism, but rather a foundational skill that empowers individuals to navigate their emotional landscapes more effectively over time.
Continuous mindfulness practice fosters a heightened awareness of bodily sensations, emotions, and thoughts. By cultivating a non-judgmental stance towards these experiences, individuals can observe them without being overwhelmed or compelled to react impulsively. This metacognitive shift cultivates emotional intelligence, enabling individuals to discern and understand the nuances of their internal states [32]. Moreover, mindfulness enhances interoceptive sensitivity, facilitating a deeper connection between mind and body. This heightened awareness can lead to more adaptive responses to emotional challenges, as individuals can accurately assess their emotional states and engage in appropriate coping strategies. By detaching from automatic thought patterns, mindfulness practitioners develop a greater capacity for emotional regulation. This ability to observe thoughts without judgment reduces the likelihood of rumination and emotional reactivity, fostering a sense of calm and centeredness [24]. Consequently, individuals become more resilient in the face of adversity, including the stressors associated with infertility. Crucially, mindfulness training empowers individuals to respond to their experiences rather than simply reacting to them. This proactive approach can lead to significant improvements in overall well-being and coping mechanisms.
The present study has some limitations that should be considered when interpreting the findings. Firstly, the use of self-report measures may have introduced bias into the results, as participants may have consciously or unconsciously attempted to present themselves in a more favorable light. Secondly, the demographic characteristics of the participants, such as socioeconomic status, were not controlled by the researchers and may have influenced the outcomes of the study. These limitations highlight the need for future research to employ more objective measures and to consider a broader range of participant characteristics.
Conclusions
MBCT effectively reduces social, family, and public stigma associated with infertility, but does not significantly impact sexual self-esteem. MBCT is a beneficial intervention for managing the psychological distress of infertility by targeting negative thought patterns and fostering acceptance.
Acknowledgments: The authors would like to extend their sincere thanks to all those who contributed to this study.
Ethical Permissions: The study was approved by the Ethical Committee of University of Mohaghegh Ardabili, Ardabil, Iran.
Conflicts of Interests: This article was extracted from a part of the PhD dissertation of Mrs. Fahimeh Zarean in the Department of Counseling, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
Authors' Contribution: Zarean F (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Sheykholeslami A (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (35%); Sadri Damirchi E (Third Author), Methodologist/Assistant Researcher/Statistical Analyst (15%); Rezaei Sharif A (Fourth Author), Assistant Researcher/Discussion Writer (15%)
Funding/Support: This article did not receive any government or university funding for the project.
Marriage has been widely recognized as a beneficial and structuring element in societies, fulfilling the personal needs of individuals [1]. It provides a sense of attachment and security that surpasses any other human relationship. Understanding the quality and value of marriage is crucial for comprehending its impact on all processes within and outside the family [2]. As marital relationships develop, various factors can intertwine and contribute to a multitude of challenges for couples [3]. Infertility is one such factor that affects individuals, families, marriages, and societies across cultures, causing significant stress [4].
Infertility is defined by Vander Borght & Wyns [5] as the failure to achieve a clinical pregnancy after at least 12 months or more of regular sexual intercourse. Researchers have reported feelings of helplessness in these individuals, especially with prolonged and sometimes unsuccessful treatments [6]. Infertility can also lead to disrupted marital quality, intimacy, fear of relationship dissolution, and other psychological disorders [7]. Individuals' responses to the infertility crisis vary depending on their cognitive interpretation of the phenomenon and the emotional regulation styles they employ to cope with the negative emotions experienced as a result of the awareness of their inability to have children [8].
When an individual's traits and actions are deemed non-normative by society, they may experience feelings of stigma and pressure, leading to feelings of inadequacy [9]. Yang et al. [10] emphasized that stigma is not an individual problem or a component of an illness but rather a social issue. Social stigma refers to prejudiced judgments and discrimination against individuals belonging to a particular group [11]. In our society, the issue of infertility takes on a deeper dimension due to our unique cultural structure. The emotional consequences of experiencing infertility stigma for families generally include feelings of disrespect and discrimination in society. To cope with these feelings, families often choose isolation and withdrawal from social interactions, believing it prevents the disclosure of their situation [12].
The most detrimental consequences of stigma arise when families internalize societal stigma and adopt negative societal views towards themselves, leading to internal or emotional stigma [13]. Given the negative impacts of stigma on the mental health of families and the importance of family in the care, follow-up, and continuation of infertility treatment, stigma is considered a fundamental and crucial issue that demands attention in the field of mental health [14]. Studies by Yu et al. [15] have shown that individualistic cultures exhibit lower stigmatizing attitudes compared to collectivistic cultures. In Iran, a collectivistic society, family members are naturally more concerned about the negative impacts of infertility on their family's reputation and others' perceptions rather than the negative impact on themselves [16, 17].
Beyond the physical challenges, infertility can significantly impact a woman's sense of self, particularly her sexual self-esteem [18]. Sexual self-esteem refers to a woman's feelings and beliefs about herself as a sexual being. It encompasses aspects like desirability, attractiveness, and confidence in her sexual abilities [19]. Examining sexual self-esteem in infertile women is crucial for several reasons. Firstly, infertility can lead to a distorted view of femininity and womanhood. Societal pressures often link motherhood to a woman's worth, and the inability to conceive can trigger feelings of inadequacy. Secondly, the stress and emotional strain associated with infertility can negatively impact sexual desire, arousal, and satisfaction. This creates a vicious cycle, where low sexual self-esteem further hinders intimacy [20]. Riazi et al. [21] consider negative perceptions as an important factor in sexual disorders and suggest focusing on psychological/cognitive factors and using cognitive restructuring methods for treating sexual disorders. When a person experiencing infertility develops a stigma of infertility, they may also develop negative thoughts about themselves and their sexual relationships, affecting their sexual self-esteem. Understanding how infertility shapes a woman's sexual self-esteem empowers healthcare professionals to provide holistic care. By addressing these concerns, they can help women navigate this challenging experience and maintain a healthy, fulfilling sex life [18].
Mindfulness-based cognitive therapy (MBCT) is one of the effective interventions for the population of infertile women [22]. This therapy is a type of cognitive therapy that utilizes mindfulness. Mindfulness is defined as paying attention in a specific, purposeful way, in the present moment, without judgment or prejudice [23]. Mindfulness leads to awareness and understanding of emotions, acceptance of emotions, the ability to control impulsive behaviors, and goal-oriented behaviors when experiencing negative emotions, in a way that achieves goals for the individual [24]. Clinical psychology and psychiatry have offered several mindfulness-based therapy programs since the 1970s to help people who experience various psychological conditions [25]. Mindfulness also involves regulating cognitive evaluations and objectively observing experiences [26]. Additionally, mindfulness allows for more adaptive coping strategies and management of unwanted stimuli [27]. This method helps the individual observe their thoughts without judgment, reducing anxiety [28]. Based on the research background, the present study aimed to investigate the effectiveness of MBCT on infertility-related stigma and sexual self-esteem in infertile women.
Materials and Methods
The present study was a three-stage semi-experimental research with two groups (experimental and control). The statistical population of this study included all infertile women referred to infertility treatment centers in Isfahan City, Iran in 2023. In the present study, 40 people who were willing to participate in the research project were selected as a sample and were randomly assigned to two groups of 20, experimental and control. The sample size was determined using a power analysis with a desired power of 0.80, an alpha level of 0.05, an anticipated large effect size of 0.85, and a projected attrition rate of 10%. After obtaining informed consent, the pre-test was administered simultaneously to both intervention and control groups using the infertility stigma and sexual self-esteem questionnaires under the same conditions. The inclusion criteria were an age range of 25-45 years, at least secondary education and infertility after medical intervention and confirmation by a specialist. The exclusion criteria were individuals who were still in the evaluation and infertility testing stage, pregnancy during the study, use of psychiatric medications due to serious mental disorders and absence from more than two therapy sessions. After the last session, the post-test was administered to both groups (experimental and control). After the intervention on the experimental group, a 45-day follow-up was conducted to determine the long-term effectiveness of this approach.
Instrument
Infertility Stigma Scale (ISS)
The Infertility Stigma Scale (ISS) is a psychometric instrument designed to assess perceived stigma among infertile women [29]. The 27-item scale utilizes a 5-point Likert scoring system to capture four distinct dimensions of infertility stigma: Self-devaluation, social withdrawal, public stigma, and family stigma. Scores range from 27 (lowest) to 135 (highest), reflecting the degree of perceived stigma. Fu et al. [29] demonstrated the scale's high internal consistency (Cronbach's alpha>0.94).
Sexual Self-Esteem Inventory (SSEI)
The Sexual Self-Esteem Inventory (SSEI) is a well-established 35-item self-report measure developed by Doyle Zeanah & Schwarz [30] to assess women's sexual self-esteem. Respondents use a 5-point Likert scale (1=strongly disagree, 5=strongly agree) to answer questions across five subscales: Skill and experience, control, attractiveness, moral judgment, and adaptiveness. These subscales capture various aspects of sexual self-esteem, with higher total scores indicating greater positive self-regard in the sexual domain. The SSEI demonstrates acceptable internal consistency, with Cronbach's alpha coefficients reported by Farokhi & Shareh [31] ranging from 0.68 to 0.82 for the subscales and 0.82 for the total scale.
Intervention
The intervention group received MBCT sessions [32] in the form of eight sessions (one 90-minute session per week) (Table 1). The control group did not receive this intervention and was placed on a waiting list.
Table 1. A summary of the mindfulness-based cognitive therapy sessions
Questionnaires were filled with the participants’ satisfaction and written informed consent was obtained from the participants in this study.
Data analysis
Data were analyzed using repeated-measures ANOVA with SPSS version 24.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Findings
The study involved 40 infertile women. The mean age of the women in the experimental and control groups was 33.70±6.39 and 35.42±5.58 years, respectively. The means and standard deviations of infertility-related stigma and sexual self-esteem scores, disaggregated by experimental and control groups were all calculated (Table 2).
Table 2. Mean and standard deviations (SD) of infertility-related stigma and sexual self-esteem
Prior to conducting the repeated-measures ANOVA, the assumptions of homogeneity of variances and normality of distribution were assessed. Levene's test for equality of variances indicated no significant differences between the groups regarding the variances of the research variables (p>0.05). Furthermore, the Shapiro-Wilk test for normality revealed that the distribution of the scores did not deviate significantly from a normal distribution (p>0.05). As the assumption of sphericity was violated for all the components under investigation, the Greenhouse-Geisser correction was employed.
The results of the repeated-measures ANOVA examined the between-subjects and within-subjects effects at the pre-test, post-test, and follow-up stages (Table 3). Significant within-subject effects were observed for the dimensions of social withdrawal (p=0.009) and family stigma (p=0.001) across the pre-test, post-test, and follow-up time points, indicating that these dimensions changed significantly over time. Additionally, a significant between-subjects effect was found for the source group, suggesting that there was a significant difference between the experimental and control groups in terms of the dimensions of social withdrawal (p=0.028) and public stigma (p=0.004). However, the effectiveness of MBCT on the dimensions of personal worthlessness and family stigma was not confirmed. No significant within-subject effects were observed for the dimension of sexual self-esteem across the three-time points of pre-test, post-test, and follow-up. Furthermore, the between-subjects effect for the source group was not significant, indicating that there was no significant difference between the experimental and control groups in terms of sexual self-esteem, and the effectiveness of the intervention was not confirmed.
Table 3. Results of the repeated-measures ANOVA
Discussion
The present study examined the efficacy of MBCT in mitigating the multifaceted dimensions of infertility-related stigma while also evaluating its impact on sexual self-esteem among infertile women. Results indicated that MBCT was efficacious in reducing the psychological burden associated with social withdrawal, familial stigma, and public scrutiny often experienced by individuals struggling with infertility. However, the intervention did not yield significant improvements in sexual self-esteem within the study parameters. These findings align with previous research highlighting the potential benefits of MBCT in addressing the emotional and social challenges inherent to infertility [22, 26].
Mindfulness can be conceptualized as an emotion regulation strategy that fosters present-moment awareness [24]. By encouraging acceptance rather than avoidance of distressing experiences, mindfulness may have facilitated greater emotional flexibility among participants [26]. This increased flexibility can be contributed to reductions in infertility-related stigma. Cultivating curiosity towards thoughts and feelings through mindfulness can mitigate the automatic negative responses often triggered by emotional distress [27]. This process may have enabled participants to approach infertility-related challenges with greater openness, reducing feelings of isolation and shame. Moreover, mindfulness can foster self-compassion, a crucial factor in coping with infertility [29]. By treating oneself with kindness and understanding, individuals may be better equipped to manage the emotional toll of infertility and reduce associated stigma. The structured nature of the MBCT intervention likely equipes participants with the skills to integrate mindfulness into daily life, promoting sustained benefits in emotional regulation and resilience [30]. The potential role of perceived social support in mitigating the impact of stigma should also be considered [28]. By fostering a sense of connection and understanding, mindfulness may have enhanced participants' social support networks, thereby reducing the negative effects of stigma.
Mindfulness, by reflecting acceptance of experiences without judgment and avoiding suppression attempts, can lead to a reduction in individuals’ reactive behaviors when faced with stigma, thereby decreasing their social withdrawal. It allows them to interrupt negative infertility-related cognitions that arise from perceptions of others and establish positive relationships with those around them [25]. By fostering a non-judgmental awareness of their feelings and thoughts, individuals practicing mindfulness can transform their relationship with both internal and external stimuli. Instead of succumbing to the automatic, often negative reactions typically associated with stigma, they become equipped to respond more thoughtfully and constructively. Mindfulness and its training promote emotion regulation without judgment and enhance awareness of psychological and physical sensations, facilitating a clear observation and acceptance of emotions and physical phenomena as they occur. This acceptance is crucial, as it allows individuals to confront the emotional turmoil often associated with infertility rather than avoiding it. Research indicates that avoidance behaviors can exacerbate feelings of sadness, anxiety, and frustration, creating a cycle of emotional distress [26]. Mindfulness interrupts this cycle by encouraging individuals to acknowledge their feelings without the added layer of judgment, thus breaking the patterns that lead to emotional distress and disengagement. Moreover, mindfulness can play a significant role in modifying negative infertility-related beliefs [22]. By recognizing and observing these beliefs as passing thoughts rather than absolutes, individuals can begin to challenge the validity of stigmatizing narratives. Mindfulness facilitates cognitive restructuring, allowing individuals to replace harmful beliefs associated with infertility (such as feelings of inadequacy or shame) with more compassionate and realistic perspectives. This cognitive shift can lead to reduced stigma, as individuals no longer internalize negative societal beliefs but instead foster a self-accepting attitude. Recognizing these challenges and providing interventions such as mindfulness-based therapies is a crucial component of treatment for improving psychological well-being.
Mindfulness-based approaches, including MBCT, specifically cater to individuals dealing with stigma by equipping them with tools to face their emotional experiences head-on rather than retreating into avoidance. In MBCT, infertile women engage in repeated practices of intentionally directing attention to a neutral object (e.g., breath flow) and observing their thoughts, emotions, or bodily sensations [28]. This practice allows them to develop a deeper awareness of their internal experiences and fosters a sense of autonomy over how they respond to stressors. Additionally, participation in such mindfulness practices may promote a sense of community among individuals undergoing similar experiences. Group settings often associated with mindfulness training can provide social support, reducing feelings of isolation that are common among those facing infertility. Sharing experiences in a safe, structured environment can help break down walls of stigma, allowing individuals to connect with others who understand their struggles [29]. This sense of connection is vital, as it not only alleviates feelings of loneliness but encourages communal resilience against shared experiences of stigma. Importantly, the implications of mindfulness extend beyond immediate emotional relief; They may also foster long-term psychological health. Regular mindfulness practice can lead to lasting changes in brain function and structure that enhance emotion regulation capacities. Studies suggest that mindfulness training positively impacts neural pathways associated with emotional reactivity and regulation, potentially leading to sustained improvements in mental health outcomes [30]. This suggests that mindfulness isn’t merely a temporary coping mechanism, but rather a foundational skill that empowers individuals to navigate their emotional landscapes more effectively over time.
Continuous mindfulness practice fosters a heightened awareness of bodily sensations, emotions, and thoughts. By cultivating a non-judgmental stance towards these experiences, individuals can observe them without being overwhelmed or compelled to react impulsively. This metacognitive shift cultivates emotional intelligence, enabling individuals to discern and understand the nuances of their internal states [32]. Moreover, mindfulness enhances interoceptive sensitivity, facilitating a deeper connection between mind and body. This heightened awareness can lead to more adaptive responses to emotional challenges, as individuals can accurately assess their emotional states and engage in appropriate coping strategies. By detaching from automatic thought patterns, mindfulness practitioners develop a greater capacity for emotional regulation. This ability to observe thoughts without judgment reduces the likelihood of rumination and emotional reactivity, fostering a sense of calm and centeredness [24]. Consequently, individuals become more resilient in the face of adversity, including the stressors associated with infertility. Crucially, mindfulness training empowers individuals to respond to their experiences rather than simply reacting to them. This proactive approach can lead to significant improvements in overall well-being and coping mechanisms.
The present study has some limitations that should be considered when interpreting the findings. Firstly, the use of self-report measures may have introduced bias into the results, as participants may have consciously or unconsciously attempted to present themselves in a more favorable light. Secondly, the demographic characteristics of the participants, such as socioeconomic status, were not controlled by the researchers and may have influenced the outcomes of the study. These limitations highlight the need for future research to employ more objective measures and to consider a broader range of participant characteristics.
Conclusions
MBCT effectively reduces social, family, and public stigma associated with infertility, but does not significantly impact sexual self-esteem. MBCT is a beneficial intervention for managing the psychological distress of infertility by targeting negative thought patterns and fostering acceptance.
Acknowledgments: The authors would like to extend their sincere thanks to all those who contributed to this study.
Ethical Permissions: The study was approved by the Ethical Committee of University of Mohaghegh Ardabili, Ardabil, Iran.
Conflicts of Interests: This article was extracted from a part of the PhD dissertation of Mrs. Fahimeh Zarean in the Department of Counseling, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
Authors' Contribution: Zarean F (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Sheykholeslami A (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (35%); Sadri Damirchi E (Third Author), Methodologist/Assistant Researcher/Statistical Analyst (15%); Rezaei Sharif A (Fourth Author), Assistant Researcher/Discussion Writer (15%)
Funding/Support: This article did not receive any government or university funding for the project.
Article Type: Original Research |
Subject:
Sexual Health Education/Promotion
Received: 2024/06/9 | Accepted: 2024/08/8 | Published: 2024/08/18
Received: 2024/06/9 | Accepted: 2024/08/8 | Published: 2024/08/18
References
1. Tahir NN. Understanding arranged marriage: An unbiased analysis of a traditional marital institution. Int J Law Policy Fam. 2021;35(1):ebab005. [Link]
2. Mohammadi K, Samavi A, Ghazavi Z. The relationship between attachment styles and lifestyle with marital satisfaction. Iran Red Crescent Med J. 2016;18(4):e23839. [Link] [DOI:10.5812/ircmj.23839]
3. Kiecolt-Glaser JK, Wilson SJ. Lovesick: How couples' relationships influence health. Annu Rev Clin Psychol. 2017;13:421-43. [Link] [DOI:10.1146/annurev-clinpsy-032816-045111]
4. Mousazadeh Y, Najafi E, Salmani R, MoradAbadi A, Salimi Kivi M, Salmani R. Association of marital satisfaction and sexual health literacy with fertility among Iranian couples. Health Educ Health Promot. 2024;12(1):145-52. [Link]
5. Vander Borght M, Wyns C. Fertility and infertility: Definition and epidemiology. Clin Biochem. 2018;62:2-10. [Link] [DOI:10.1016/j.clinbiochem.2018.03.012]
6. Sambasivam I, Jennifer HG. Understanding the experiences of helplessness, fatigue and coping strategies among women seeking treatment for infertility-A qualitative study. J Educ Health Promot. 2023;12:309. [Link] [DOI:10.4103/jehp.jehp_1600_22]
7. Jamali Gandomani S, Taebi M, Mirghiasi AR, Nilforoushan P. Association between infertility factors and perceived relationship quality in infertile couples. J Educ Health Promot. 2022;11:360. [Link] [DOI:10.4103/jehp.jehp_428_21]
8. Zareh Zardini S, Jafari A, Ghamari M. Prediction of marital burnout based on feelings of loneliness and emotional divorce in infertile women. J Res Health. 2021;11(5):323-32. [Link] [DOI:10.32598/JRH.11.5.1854.1]
9. Ahmedani BK. Mental health stigma: Society, individuals, and the profession. J Soc Work Values Ethics. 2011;8(2):1-16. [Link]
10. Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: Adding moral experience to stigma theory. Soc Sci Med. 2007;64(7):1524-35. [Link] [DOI:10.1016/j.socscimed.2006.11.013]
11. Klein P, Fairweather AK, Lawn S. Structural stigma and its impact on healthcare for borderline personality disorder: A scoping review. Int J Ment Health Syst. 2022;16:48. [Link] [DOI:10.1186/s13033-022-00558-3]
12. Taebi M, Kariman N, Montazeri A, Alavi Majd H. Infertility stigma: A qualitative study on feelings and experiences of infertile women. Int J Fertil Steril. 2021;15(3):189-96. [Link]
13. Xie Y, Ren Y, Niu C, Zheng Y, Yu P, Li L. The impact of stigma on mental health and quality of life of infertile women: A systematic review. Front Psychol. 2023;13:1093459. [Link] [DOI:10.3389/fpsyg.2022.1093459]
14. Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Med. 2019;17:25. [Link] [DOI:10.1186/s12916-019-1256-2]
15. Yu BCL, Chio FHN, Mak WWS, Corrigan PW, Chan KKY. Internalization process of stigma of people with mental illness across cultures: A meta-analytic structural equation modeling approach. Clin Psychol Rev. 2021;87:102029. [Link] [DOI:10.1016/j.cpr.2021.102029]
16. Amiri M, Khosravi A, Chaman R, Sadeghi Z, Raei M, Jahanitiji M, et al. Social consequences of infertility on families in Iran. Glob J Health Sci. 2016;8(5):89-95. [Link] [DOI:10.5539/gjhs.v8n5p89]
17. Hasanpoor-Azghdy SB, Simbar M, Vedadhir A. The social consequences of infertility among Iranian women: A qualitative study. Int J Fertil Steril. 2015;8(4):409-20. [Link]
18. Zayed AA, El-Hadidy MA. Sexual satisfaction and self-esteem in women with primary infertility. Middle East Fertil Soc J. 2020;25:13. [Link] [DOI:10.1186/s43043-020-00024-5]
19. Marvi N, Golmakani N, Esmaily H, Shareh H. The relationship between sexual satisfaction and genital self-image in infertile women. J Midwifery Reprod Health. 2018;6(4):1478-85. [Link]
20. Lotfollahi H, Riazi H, Omani-Samani R, Maroufizadeh S, Montazeri A. Sexual self-concept in fertile and infertile women: A comparative study. Int J Fertil Steril. 2021;15(1):60-4. [Link]
21. Riazi H, Lotfollahi H, Omani-Samani R, Maroufizadeh S, Montazeri A. Evaluation of sexual function among infertile women and their sexual self-concept. J Reprod Infertil. 2020;21(4):291-7. [Link] [DOI:10.18502/jri.v21i4.4334]
22. Fard TR, Kalantarkousheh M, Faramarzi M. Effect of mindfulness-based cognitive infertility stress therapy on psychological well-being of women with infertility. Middle East Fertil Soc J. 2018;23(4):476-81. [Link] [DOI:10.1016/j.mefs.2018.06.001]
23. Williams JM, Russell I, Russell D. Mindfulness-based cognitive therapy: Further issues in current evidence and future research. J Consult Clin Psychol. 2008;76(3):524-9. [Link] [DOI:10.1037/0022-006X.76.3.524]
24. Javedani Masroor M, Aerabsheybani H, Ramezani N, Aerabsheybani K. The effectiveness of mindfulness-based cognitive therapy (MBCT) in increasing infertile couples' resilience and reducing anxiety, stress, and depression. NeuroQuantology. 2017;15(3):94-100. [Link] [DOI:10.14704/nq.2017.15.3.1088]
25. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol. 2010;78(2):169-83. [Link] [DOI:10.1037/a0018555]
26. Abedi Shargh N, Bakhshani NM, Mohebbi MD, Mahmudian K, Ahovan M, Mokhtari M, et al. The effectiveness of mindfulness-based cognitive group therapy on marital satisfaction and general health in woman with infertility. Glob J Health Sci. 2015;8(3):230-5. [Link] [DOI:10.5539/gjhs.v8n3p230]
27. Kundarti FI, Titisari I, Rahayu DE, Kiswati, Jamhariyah. Mindfulness improves the mental health of infertile women: A systematic review. J Public Health Res. 2023;12(3):22799036231196693. [Link] [DOI:10.1177/22799036231196693]
28. Hosseini Nejad S, Bokaie M, Yassini Ardekani SM. Effectiveness of sexual health counseling based on mindfulness approach on sexual satisfaction in women suffering from infertility: An RCT. Int J Reprod Biomed. 2023;21(2):147-58. [Link]
29. Fu B, Qin N, Cheng L, Tang G, Cao Y, Yan C, et al. Development and validation of an infertility stigma scale for Chinese women. J Psychosom Res. 2015;79(1):69-75. [Link] [DOI:10.1016/j.jpsychores.2014.11.014]
30. Doyle Zeanah P, Schwarz JC. Reliability and validity of the sexual self-esteem inventory for women. Assessment. 1996;3(1):1-15. [Link] [DOI:10.1177/107319119600300101]
31. Farokhi S, Shareh H. Psychometric properties of the Persian version of the sexual self-esteem index for woman-short form. Iran J Psychiatry Clin Psychol. 2014;20(3):252-63. [Persian] [Link] [DOI:10.1037/t54661-000]
32. Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry. 2010;67(12):1256-64. [Link] [DOI:10.1001/archgenpsychiatry.2010.168]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |