Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 449-458 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Risnawati R, Umrana S, Susanty S. Key Risk Factors of Dementia in Elderly Populations. Health Educ Health Promot 2024; 12 (3) :449-458
URL: http://hehp.modares.ac.ir/article-5-75495-en.html
URL: http://hehp.modares.ac.ir/article-5-75495-en.html
1- Department of Nursing, Karya Kesehatan School of Health Sciences, Kendari, Indonesia
2- Department of Nursing, Faculty of Medicine, University of Halu Oleo, Kendari, Indonesia
2- Department of Nursing, Faculty of Medicine, University of Halu Oleo, Kendari, Indonesia
Keywords: Dementia [MeSH], Elderly [MeSH], Risk Factors [MeSH], Psychiatric Disorders [MeSH], Chronic Disease [MeSH]
Full-Text [PDF 852 kb]
(2543 Downloads)
| Abstract (HTML) (1254 Views)
Full-Text: (177 Views)
Introduction
Dementia is a disorder characterized by a gradual decline in cognitive abilities, severely impacting daily activities [1]. Worldwide data suggests that the incidence of dementia is either rising or remaining constant in the majority of countries [2]. With the aging baby boomer population, the number of seniors affected by dementia is anticipated to increase significantly [3-5]. This trend has profound health, social, and economic implications for both patients and caregivers [6, 7]. Given the lack of treatments that can alter the disease’s progression, it is vital to focus on reducing the risk of dementia in seniors to enhance their quality of life [8].
Dementia arises from a range of conditions that progressively damage nerve cells and affect the brain, leading to a decline in cognitive abilities that exceeds normal aging expectations [9]. Although consciousness remains intact, cognitive decline frequently precedes changes in mood, emotional regulation, behavior, and motivation [10, 11]. Dementia impacts medical, psychological, social, and economic aspects, affecting not only those diagnosed but also their caregivers, families, and the broader community. Unfortunately, there is often insufficient awareness and understanding of dementia, which fosters stigma and hinders appropriate diagnosis and care [12-19].
Across the globe, the provision of dementia care has typically imposed a significant financial strain on government budgets. In 2019, global costs for dementia amounted to approximately $1,313.4 billion, affecting 55.2 million people and costing around $23,796 per person. Of the total, $213.2 billion (16%) was allocated for direct medical expenses. Direct social sector costs, which include long-term care, totaled $448.7 billion, accounting for 34% of the overall expenses. Informal care costs amounted to $651.4 billion, representing 50%. The exorbitant expenses associated with dementia on a global scale place a significant strain on healthcare systems and families, with high-income countries bearing the highest financial burden despite the majority of dementia cases residing in low- and middle-income countries (LMICs). The substantial financial burdens of dementia affect both healthcare systems and families worldwide. While most dementia cases are found in LMICs, the highest total and per capita costs are observed in high-income countries [20]. Seventy-five percent of caregivers experience stress while balancing the care of dementia patients with their other responsibilities [21]. Currently, aducanumab is the only disease-modifying drug approved for the treatment of Alzheimer’s disease (AD) [22], although its approval remains controversial. At present, no treatments exist that can delay the onset or stop the progression of other types of dementia. This is largely due to complex interactions between genes and the environment, as well as unclear pathophysiological mechanisms, which create obstacles for targeted drug development efforts [23, 24]. The conundrum of a high disease burden coupled with the absence of effective treatments underscores the imperative for primary prevention strategies [25].
Numerous studies have observed a promising decrease in dementia prevalence, indicating positive progress in this area [26], likely influenced by factors, such as higher education levels and improved management of vascular risk factors [27-30]. According to the Lancet Commission, modifiable factors contribute to approximately 40% of dementia cases globally [31], suggesting that interventions targeting these factors could help in dementia prevention. Variations in study designs and inconsistencies between studies can introduce biases, making it challenging to establish reliable evidence hierarchies across different factors. The principal aim of this review was to evaluate the potential risk factors linked to the incidence of dementia among older adults across various countries worldwide.
Information and Methods
The current systematic review followed the 2020 edition of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [32], to examine all potential risk factors associated with the development of dementia in older adults.
Search strategy
The literature search was conducted between March and May 2024, utilizing freely accessible databases, such as PubMed, ScienceDirect, Wiley Online Library, and ProQuest. Additionally, we conducted a manual search of the bibliographies of relevant studies using Google Scholar. In each database, searches were performed across all available years during the specified timeframe, using keywords, including “Dementia,” “Alzheimer,” and “Vascular dementia,” followed by other keywords, such as “Elderly,” “Senior age,” and “Aging,” both individually and in combination.
Inclusion and exclusion criteria
Articles were included in this review if they were primary research articles with either a qualitative or quantitative approach, available in English, published in a peer-reviewed reputable journal, focused on older adults, and participants were classified as elderly according to the World Health Organization (WHO) criteria. The exclusion criteria were articles of other types, such as review articles, editorials, and studies, in which participants were not elderly. Additionally, the bibliographies of the examined studies were reviewed for further publication.
Data extraction
All authors independently extracted information from each article into a spreadsheet. The data collected included the name of the author(s), year of study, country, study design, sample size, mean age of participants, types of dementia, risk factors, and main findings. Reviewers examined the articles and provided comments in the table.
Study quality assessment
The authors independently assessed the methodological quality of the eligible studies using the instrument developed by the National Institutes of Health (NIH). It consists of 14 questions that serve as criteria for categorizing the quality of the study, focusing on the core concept of internal validity. The study quality was categorized as good (90-100%), fair (70-89%), and poor (≤69%).
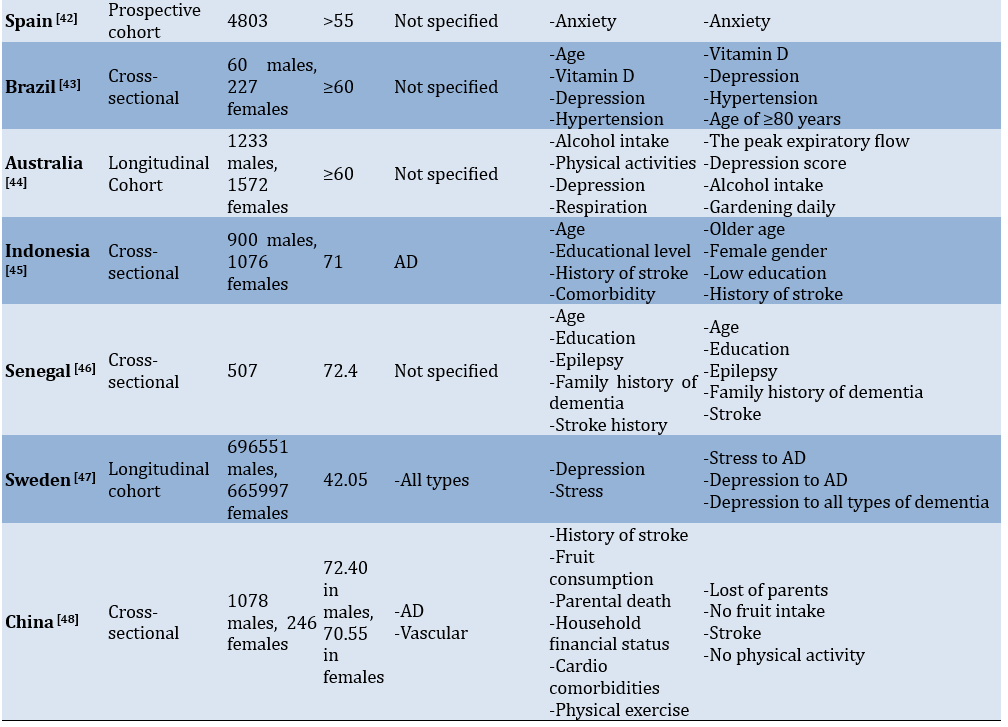
A search of the database resulted in 1,658 articles, including those identified through hand searching. After eliminating duplicate articles and reviewing titles and abstracts, 506 articles were selected for screening. Of these, 69 articles were excluded as they were review studies or case reports and irrelevant age ranges. The remaining 16 studies were included in the systematic review (Figure 1).
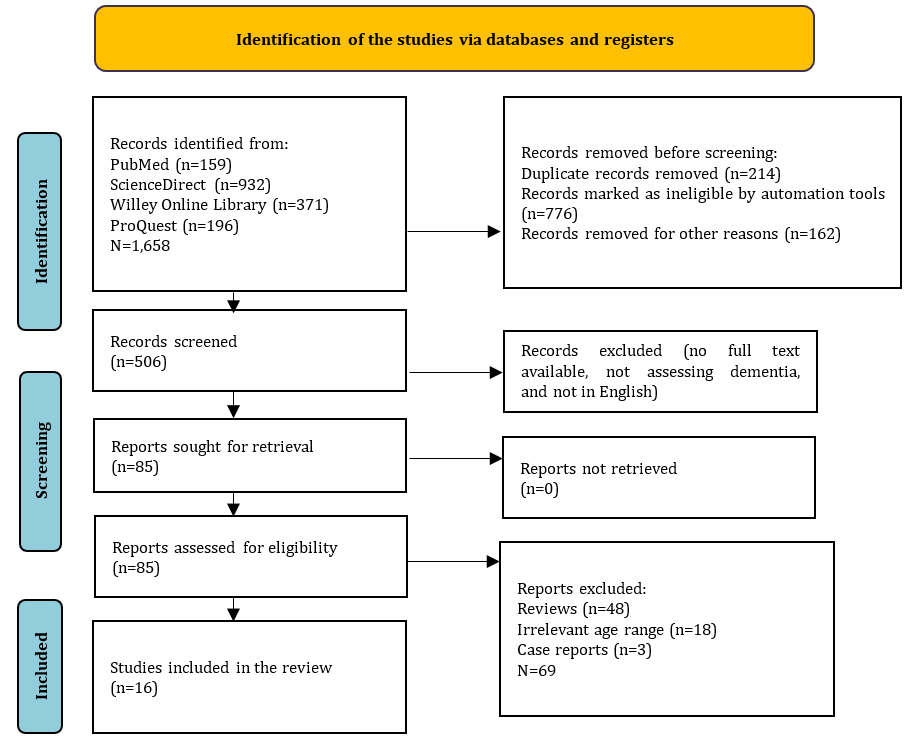
Figure 1. Flow chart of the study selection.
Findings
General characteristics of eligible studies
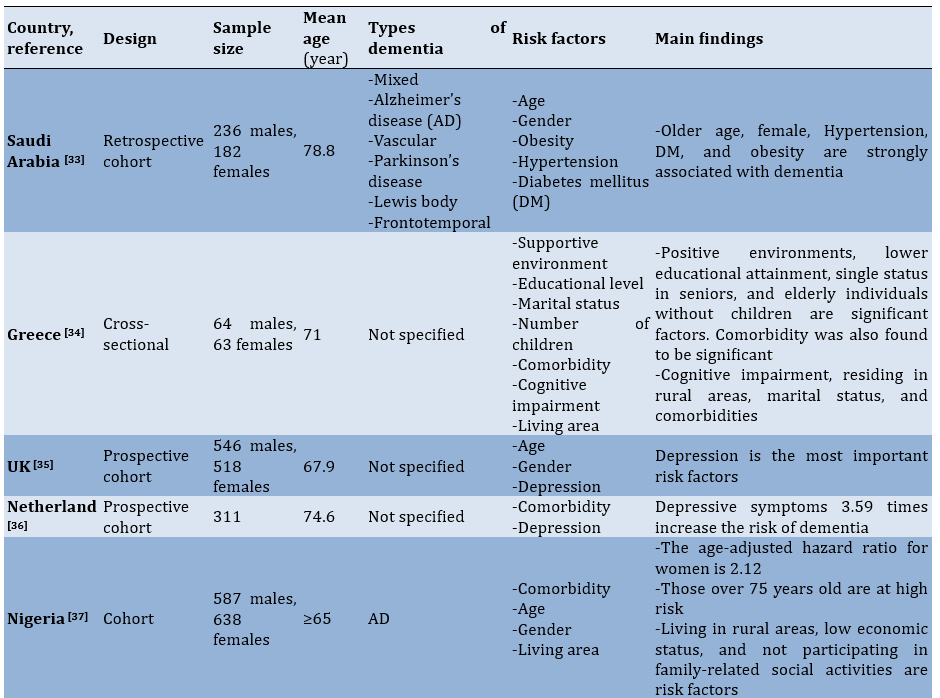
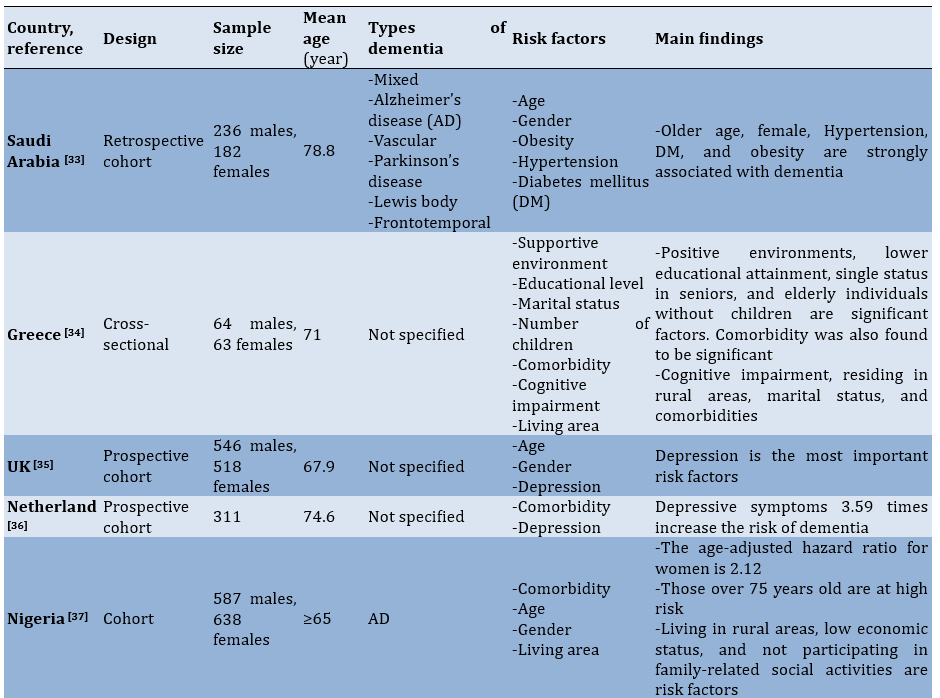
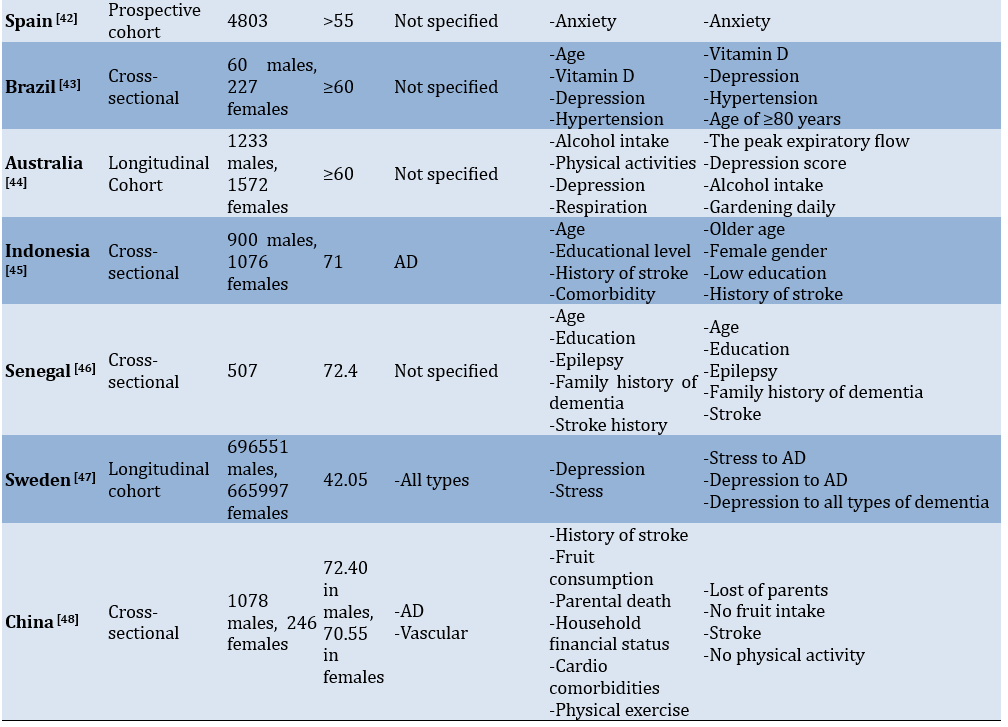
The current review gathered 16 studies from five different continents. Each country represented one study included in this review. The countries that contributed to the studies on dementia risk factors were grouped by continent, including Nigeria [37] and Senegal [46] from Africa, Saudi Arabia [33], Indonesia [45], China [38, 48], India [40], Turkey [39] from Asia, Greece [34], Italy [41], Spain [42], Sweden [47], Netherland [36], United Kingdom [35] from Europe, Australia [44] from Oceania, and Brazil [43] from South America.
The eligible studies included a wide range of participant groups, with sample size ranging from as few as 127 elderly individuals [34] to a several hundreds of thousands from national survey records [47]. The number of participants was related to the used study design, which is generally observational with a cross-sectional approach [34, 38-40, 43, 45, 46, 48], along with retrospective-prospective cohort studies [33, 35-37, 41, 42] and longitudinal studies [44, 47].
Most of the studies indicated that the age of participants was over 60 years, categorizing them as elderly. However, there was one study that included participants with a mean age of 42.05 [47]. Age is an important factor when discussing risk factors for dementia, as it was a non-modifiable risk factor. In terms of gender, the number of female participants appeared to be greater than that of male participants (Table 1).
Table 1. Features of the included studies
Summary of study quality appraisal
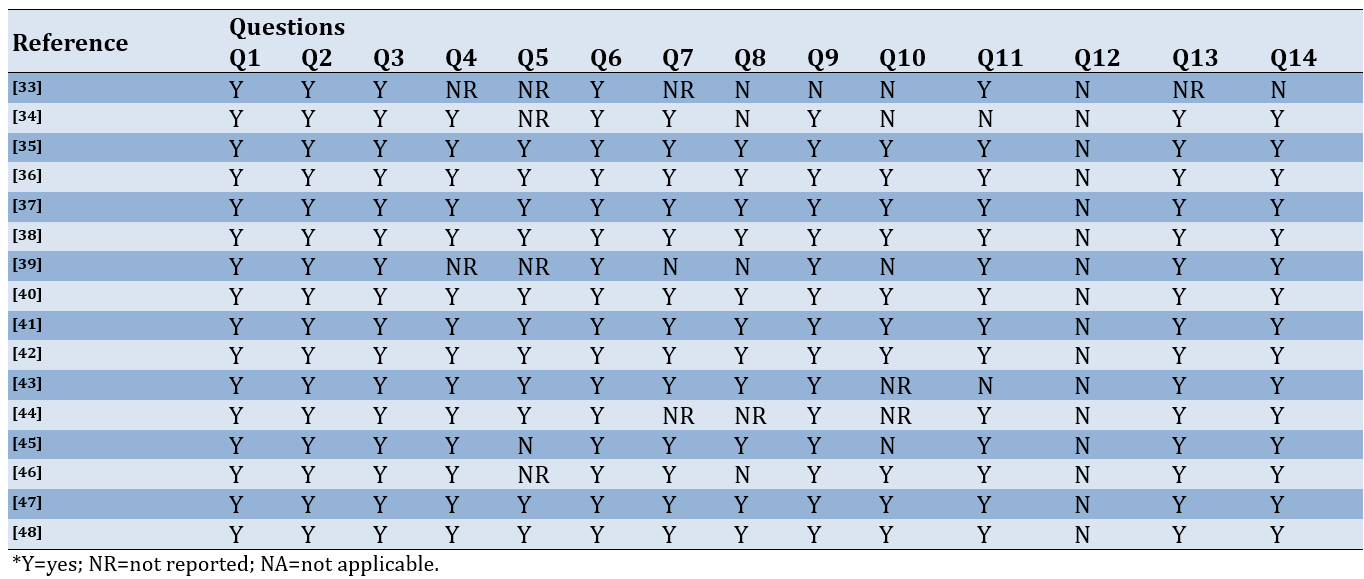
Methodologically, we identified three studies with “poor” quality, as they did not clearly explain the sampling criteria, including the calculation of the number of samples and the power description. Three other studies fell into the “fair” category, while most of the remaining studies were classified as having “good” quality (Table 2).
Table 2. Summary of study quality assessment
Risk of bias assessment
Most of the studies were categorized as having a low risk of bias, while a small proportion raised some concerns, indicating that there are items that remain uncertain. Five studies were classified in the high risk of bias category due to having more than two concerns or insufficient information (Figure 2).
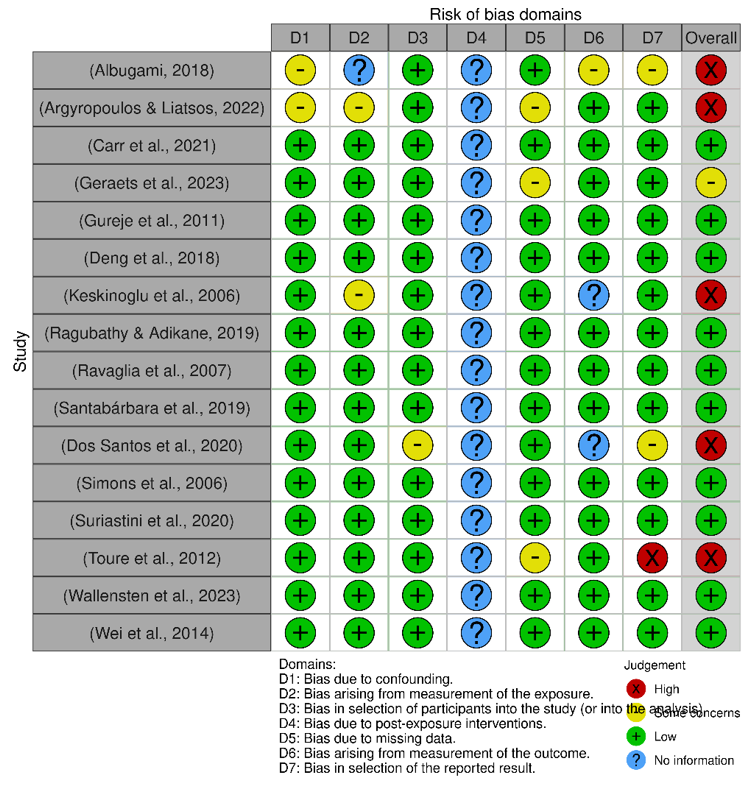
Figure 2. Risk of bias assessment.
Mapping risk factors for dementia
We identified approximately 27 risk factors significantly associated with the prevalence of dementia across countries representative of their respective continents. To summarize the risk factors identified, we attempted to classify them into demographic factors, chronic diseases, lifestyle factors, and psychological disorders.
Demographic factors related to dementia
In the studies reviewed, demographic factors, primarily age and gender, are discussed. Overall, the studies agree that older age increases the prevalence of dementia. The significance values for age among the studies showed a strong association [33, 37-39, 45, 46]. When considering gender, older women are at a higher risk of developing dementia, contributing to an increase in the number of dementia sufferers in this group [37]. The reviewed studies consistently indicate a universal consensus regarding the comparison between males and females, with findings consistently showing that females are more likely to develop dementia than males. This is further supported by the high prevalence rate observed among females [33, 37, 45]. However, we identified one study reporting a higher incidence of dementia among males compared to females [40].
Educational level, occupation, and household income are closely aligned in their contribution to the prevalence of dementia. Among the studies reviewed, it was noted that among all elderly individuals with dementia, those with a low level of education exhibit a strong association [34, 37, 38, 45]. In the Netherlands, elderly individuals with a low economic status have four times the risk of developing dementia [36]. Meanwhile, a study in Turkey indicates that elderly individuals who do not work are 3.22 times more likely to experience dementia than those who are employed [39]. In their study of older individuals residing in well-educated communities in China, Wei et al. discovered a strong correlation between family financial status and the incidence of dementia, with those in poorer financial conditions nearly three times more likely to experience dementia compared to older individuals with sufficient financial resources [48]. Studies in India have linked the number of grandchildren to the incidence of dementia, suggesting that this is more related to the economic conditions of the family. Researchers believe that in Indian society, most people with low economic status tend to have more family members living together in one household [40]. A family history of dementia is a significant contributor to the incidence of dementia in the elderly. In Senegal, there is a strong correlation between a family history of dementia and dementia incidence [46]. This correlation is also observed among the elderly in India, but it occurs only between parents and their children, not between siblings [40].
Lifestyle factors related to dementia
Engaging in both physical and social activities can significantly reduce the risk of dementia among older adults. This suggests that a lack of regular physical and social activity may elevate the risk of developing dementia. Deng et al. illustrate the importance of physical and social activities for the elderly, noting that those who never engage in social activities are at high risk for dementia. Similarly, those who do not participate in physical activity, housework, exercise, and playing Mahjong or chess are also associated with dementia [38]. Regarding activities, daily gardening is identified as a protective factor against the incidence of dementia, with elderly individuals who do not engage in daily gardening having a one-fold increased chance of experiencing dementia compared to those who do [44]. A similar finding was reported by Wei et al., where the elderly who do not engage in physical activity contribute to an approximately three-fold increase in the incidence of dementia [48]. In Nigeria, the elderly who do not participate in social activities are also at high risk for dementia (p=0.04) [37].
Elderly who actively consume alcohol and smoke are at high risk of developing dementia [38, 40, 41, 44]. In addition to these harmful habits, dietary patterns are also an important factor that needs to be considered for the elderly. For example, in China, the elderly who do not consume freshwater fish are at risk of dementia (p=0.004) [38]. Although the significance value is not very strong, the consumption of seafood, liver, and fats is also included in the dietary recommendations of the Chinese study [38]. Another example is that a lack of fruit in the diet of the elderly is associated with a high risk of dementia [48].
History Chronic diseases
Some of the chronic conditions experienced by older adults with dementia include hypertension, stroke, diabetes mellitus (DM), obesity, ventilation disorders, and other cardiovascular-related conditions. A history of stroke has been mentioned repeatedly in the studies reviewed to date, with high significance. Therefore, this factor may need to be a focus in future research, along with hypertension, obesity, and DM, which are closely related to these chronic conditions. Albugami et al. reported a strong association between hypertension and dementia, similar to other studies in Greece and China [33, 34, 38]. Dos Santos et al. provided evidence that older individuals with previous episodes of high blood pressure have roughly a threefold increased likelihood of developing dementia [43]. As stated by Ragubathy & Adikane, midlife and late-life hypertension are major predictors of the onset of arterial dementia in later life [40]. Meanwhile, a history of stroke appears to be a stronger risk factor for dementia compared to hypertension [45, 46]. Meanwhile, a study in China indicates that the elderly with a history of stroke have nearly four times the risk of developing dementia [48]. Another condition associated with cardiovascular disorders is a history of myocardial infarction [34]. Similar to hypertension, DM also has a strong association with dementia in the elderly, as found in studies conducted in Saudi Arabia [33], India [40], and Indonesia [45]. There is only one study that addressed a connection between seizures and dementia, and the findings indicated a robust association [46]. Obesity in the elderly must also be a concern, as some studies have shown it to be associated with dementia in this population [33, 38, 40].
Psychiatric disorders related to dementia
Impairment in this area was the strongest factor among the various factors considered. Depression is the most frequently measured condition in the studies reviewed, and its significance remained stable across these studies. The UK study identified depression as a major factor in the incidence of dementia, associated with a threefold risk [35]. Several countries demonstrate a strong significance in this relationship, including China (p=0.003), Turkey (p=0.0001), Brazil (p<0.001), and Australia, which exhibit the strongest association among the other three factors (p<0.001). Additionally, Sweden and the Netherlands show odds ratios (OR) of 2.39 and 3.59, respectively [38, 39, 43, 44, 47]. According to Ragubathy & Adikane’s research, a previous episode of clinical depression lasting roughly a decade is considered a potential factor. Nonetheless, the histories collected generally cover a period of weeks to years, which is comparatively less significant [40].
Discussion
This study aimed to provide a narrative assessment of the risk factors associated with the incidence of dementia in older adults. In summary, the studies reviewed indicate that the risk factors for dementia are diverse and intricately interconnected. We attempted to classify the identified risk factors into demographic factors, lifestyle choices, chronic illnesses, and psychological conditions. However, we encountered discrepancies among the studies, methodological shortcomings that affected the reliability of their results, and a limited overall number of available studies.
We assessed that within the category of psychological disorders, the level of depression is the strongest factor among several other conditions in this group, including anxiety and stress. Symptoms of depression in older adults manifest in diverse ways, impacting both their sense of well-being and how they are perceived by others. Key characteristics of geriatric depression include a persistent low mood and slowed psychomotor functions. Anxiety and irritability are common, along with numerous physical and psychological complaints. Patients may experience feelings of poverty and hypochondria, as well as sleep disturbances and a heightened risk of suicide attempts. This condition tends to recur and typically has a poor prognosis [49-54]. Depression among older adults can lead not only to work absenteeism but also to complete withdrawal from employment, such as retiring or closing a business. Even among unemployed individuals, a decline in hobbies and domestic activities can lead to a decrease in muscle strength in the lower extremities, which in turn can contribute to a reduction in activities of daily living (ADLs). Preventing the deterioration of ADLs can be achieved through the early detection of depression. According to recent systematic studies, the most significant risk factor for later suicidal behavior in older individuals is depression. Suicidal tendencies in older adults are closely linked to physical illnesses and impairments, stress, living alone, and poor health, all of which are risk factors for suicide attempts [55].
We found evidence that advancing age increases the risk of dementia among seniors. The brain is susceptible to the effects of aging, undergoing various alterations in both its structure and function as individuals grow older [56, 57]. In terms of brain biology, advancing age is a significant risk factor for the onset of cognitive impairments, such as AD, the most common form of dementia, which affects approximately 55 million people globally [58]. While both normal and pathological aging brains experience brain atrophy and cognitive decline, the mechanisms driving these changes are distinct. In normal aging, cognitive decline results from disruptions in circuits and synapses, without significant neuronal loss. This contrasts with dementia and related conditions, which involve extensive neuronal death [59, 60]. In addition to age, gender also appears to be a strong contributor to dementia, as mentioned in the studies reviewed. First, there is a tendency for women to experience depression; several studies indicate that women are twice as likely to encounter depression compared to men during their lifetime [61, 62]. Secondly, the presence of sex hormone factors plays a role, as menopausal women experience an increase in estrogen during this period, which may trigger the onset of dementia [63].
Almost all people with dementia have one or more other chronic conditions [64]. Many of these conditions may cause, or at least contribute to, cognitive decline and dementia. Once a person has dementia, intellectual disability can complicate the management of these other conditions [65]. High blood pressure (hypertension) significantly influences dementia events, as it appears to increase the risk of early cognitive decline, which can progress to dementia or stroke over several years. During this asymptomatic period for most people with hypertension, elevated blood pressure can lead to mild changes, including arteriolar narrowing or microvascular alterations that cause chronic small vessel ischemia (lacunar or white matter lesions), as well as hemosiderin deposits around blood vessels, particularly in deeply penetrating arteries (microbleeds) [66].
This study faced some limitations. Firstly, very few studies were included in this review due to a lack of access to some databases, especially credible ones. Secondly, we included some studies that are of low quality and high bias; therefore, we would like to remind readers and researchers to be cautious in using the results of these studies. However, we are quite confident that the original locations of the studies included are from highly varied countries. For greater detail and accuracy, it is important to conduct a future meta-analysis focusing on one of the most significant variables identified in the current study.
Conclusion
Demographics, lifestyle, chronic diseases, and psychological disorders are risk factors for dementia among older adults.
Acknowledgments: We would like to thank the Chief of STIKES Karya Kesehatan and the Dean of the Faculty of Medicine at Halu Oleo University for granting permission to conduct this study and for the use of laboratory facilities.
Ethical Permissions: There is no ethical clearance for this review.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Risnawati R (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (50%); Umrana S (Second Author), Introduction Writer/Methodologist/Assistant Researcher (15%); Susanty S (Third Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (35%)
Funding/Support: We did not receive any financial support from any party.
Dementia is a disorder characterized by a gradual decline in cognitive abilities, severely impacting daily activities [1]. Worldwide data suggests that the incidence of dementia is either rising or remaining constant in the majority of countries [2]. With the aging baby boomer population, the number of seniors affected by dementia is anticipated to increase significantly [3-5]. This trend has profound health, social, and economic implications for both patients and caregivers [6, 7]. Given the lack of treatments that can alter the disease’s progression, it is vital to focus on reducing the risk of dementia in seniors to enhance their quality of life [8].
Dementia arises from a range of conditions that progressively damage nerve cells and affect the brain, leading to a decline in cognitive abilities that exceeds normal aging expectations [9]. Although consciousness remains intact, cognitive decline frequently precedes changes in mood, emotional regulation, behavior, and motivation [10, 11]. Dementia impacts medical, psychological, social, and economic aspects, affecting not only those diagnosed but also their caregivers, families, and the broader community. Unfortunately, there is often insufficient awareness and understanding of dementia, which fosters stigma and hinders appropriate diagnosis and care [12-19].
Across the globe, the provision of dementia care has typically imposed a significant financial strain on government budgets. In 2019, global costs for dementia amounted to approximately $1,313.4 billion, affecting 55.2 million people and costing around $23,796 per person. Of the total, $213.2 billion (16%) was allocated for direct medical expenses. Direct social sector costs, which include long-term care, totaled $448.7 billion, accounting for 34% of the overall expenses. Informal care costs amounted to $651.4 billion, representing 50%. The exorbitant expenses associated with dementia on a global scale place a significant strain on healthcare systems and families, with high-income countries bearing the highest financial burden despite the majority of dementia cases residing in low- and middle-income countries (LMICs). The substantial financial burdens of dementia affect both healthcare systems and families worldwide. While most dementia cases are found in LMICs, the highest total and per capita costs are observed in high-income countries [20]. Seventy-five percent of caregivers experience stress while balancing the care of dementia patients with their other responsibilities [21]. Currently, aducanumab is the only disease-modifying drug approved for the treatment of Alzheimer’s disease (AD) [22], although its approval remains controversial. At present, no treatments exist that can delay the onset or stop the progression of other types of dementia. This is largely due to complex interactions between genes and the environment, as well as unclear pathophysiological mechanisms, which create obstacles for targeted drug development efforts [23, 24]. The conundrum of a high disease burden coupled with the absence of effective treatments underscores the imperative for primary prevention strategies [25].
Numerous studies have observed a promising decrease in dementia prevalence, indicating positive progress in this area [26], likely influenced by factors, such as higher education levels and improved management of vascular risk factors [27-30]. According to the Lancet Commission, modifiable factors contribute to approximately 40% of dementia cases globally [31], suggesting that interventions targeting these factors could help in dementia prevention. Variations in study designs and inconsistencies between studies can introduce biases, making it challenging to establish reliable evidence hierarchies across different factors. The principal aim of this review was to evaluate the potential risk factors linked to the incidence of dementia among older adults across various countries worldwide.
Information and Methods
The current systematic review followed the 2020 edition of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [32], to examine all potential risk factors associated with the development of dementia in older adults.
Search strategy
The literature search was conducted between March and May 2024, utilizing freely accessible databases, such as PubMed, ScienceDirect, Wiley Online Library, and ProQuest. Additionally, we conducted a manual search of the bibliographies of relevant studies using Google Scholar. In each database, searches were performed across all available years during the specified timeframe, using keywords, including “Dementia,” “Alzheimer,” and “Vascular dementia,” followed by other keywords, such as “Elderly,” “Senior age,” and “Aging,” both individually and in combination.
Inclusion and exclusion criteria
Articles were included in this review if they were primary research articles with either a qualitative or quantitative approach, available in English, published in a peer-reviewed reputable journal, focused on older adults, and participants were classified as elderly according to the World Health Organization (WHO) criteria. The exclusion criteria were articles of other types, such as review articles, editorials, and studies, in which participants were not elderly. Additionally, the bibliographies of the examined studies were reviewed for further publication.
Data extraction
All authors independently extracted information from each article into a spreadsheet. The data collected included the name of the author(s), year of study, country, study design, sample size, mean age of participants, types of dementia, risk factors, and main findings. Reviewers examined the articles and provided comments in the table.
Study quality assessment
The authors independently assessed the methodological quality of the eligible studies using the instrument developed by the National Institutes of Health (NIH). It consists of 14 questions that serve as criteria for categorizing the quality of the study, focusing on the core concept of internal validity. The study quality was categorized as good (90-100%), fair (70-89%), and poor (≤69%).
A search of the database resulted in 1,658 articles, including those identified through hand searching. After eliminating duplicate articles and reviewing titles and abstracts, 506 articles were selected for screening. Of these, 69 articles were excluded as they were review studies or case reports and irrelevant age ranges. The remaining 16 studies were included in the systematic review (Figure 1).
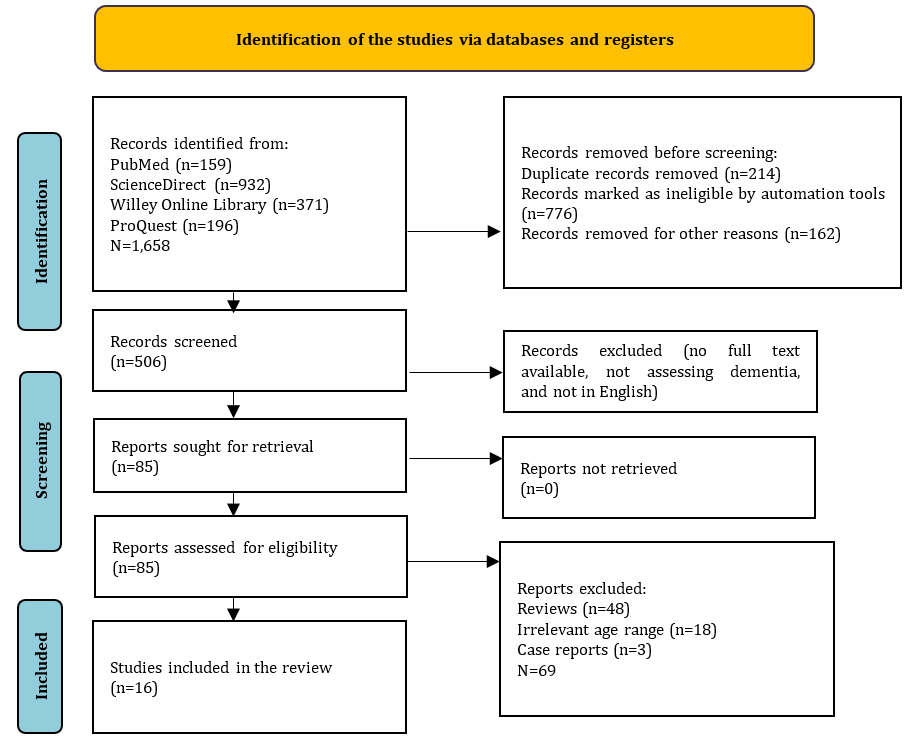
Figure 1. Flow chart of the study selection.
Findings
General characteristics of eligible studies
The current review gathered 16 studies from five different continents. Each country represented one study included in this review. The countries that contributed to the studies on dementia risk factors were grouped by continent, including Nigeria [37] and Senegal [46] from Africa, Saudi Arabia [33], Indonesia [45], China [38, 48], India [40], Turkey [39] from Asia, Greece [34], Italy [41], Spain [42], Sweden [47], Netherland [36], United Kingdom [35] from Europe, Australia [44] from Oceania, and Brazil [43] from South America.
The eligible studies included a wide range of participant groups, with sample size ranging from as few as 127 elderly individuals [34] to a several hundreds of thousands from national survey records [47]. The number of participants was related to the used study design, which is generally observational with a cross-sectional approach [34, 38-40, 43, 45, 46, 48], along with retrospective-prospective cohort studies [33, 35-37, 41, 42] and longitudinal studies [44, 47].
Most of the studies indicated that the age of participants was over 60 years, categorizing them as elderly. However, there was one study that included participants with a mean age of 42.05 [47]. Age is an important factor when discussing risk factors for dementia, as it was a non-modifiable risk factor. In terms of gender, the number of female participants appeared to be greater than that of male participants (Table 1).
Table 1. Features of the included studies
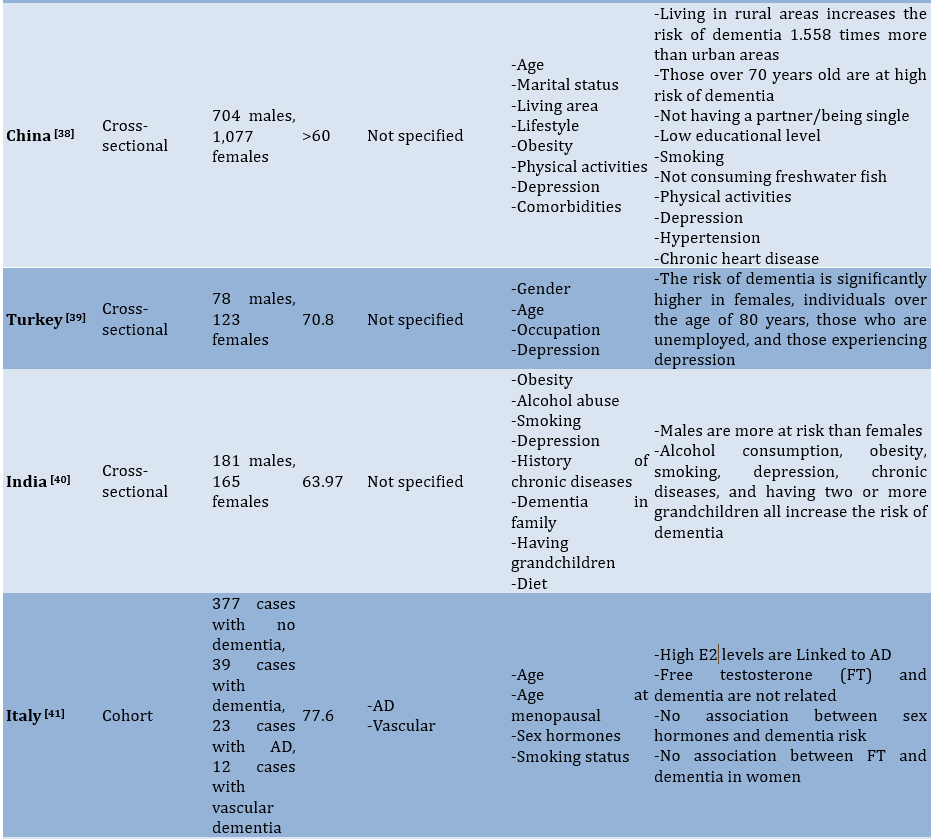
Summary of study quality appraisal
Methodologically, we identified three studies with “poor” quality, as they did not clearly explain the sampling criteria, including the calculation of the number of samples and the power description. Three other studies fell into the “fair” category, while most of the remaining studies were classified as having “good” quality (Table 2).
Table 2. Summary of study quality assessment
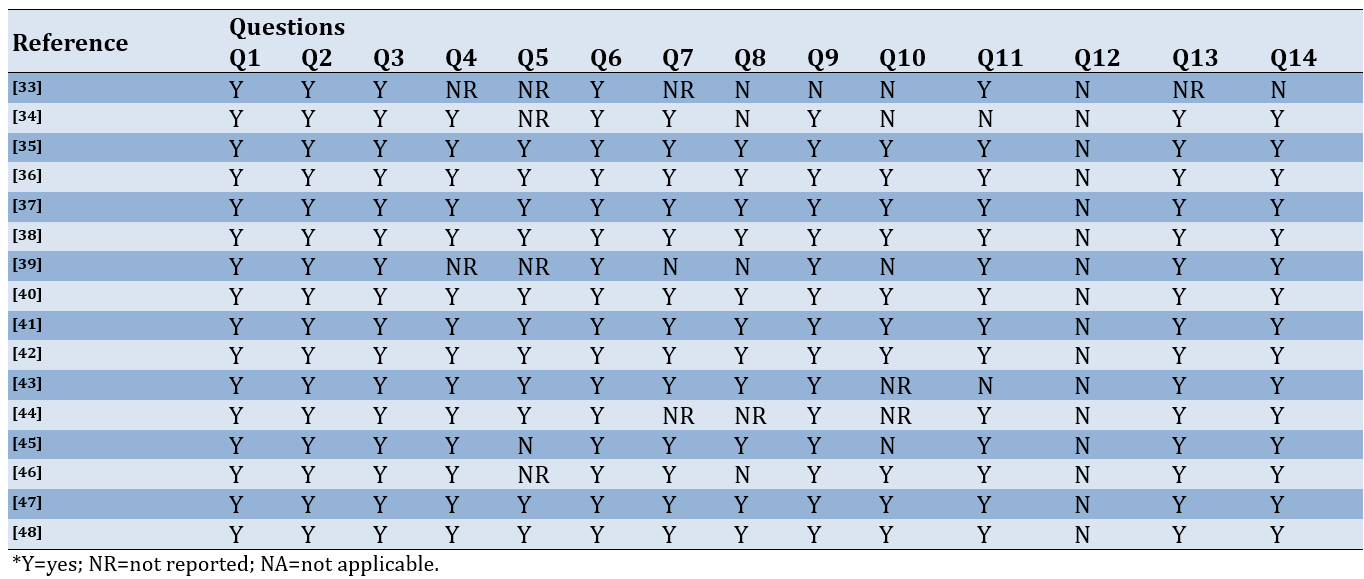
Risk of bias assessment
Most of the studies were categorized as having a low risk of bias, while a small proportion raised some concerns, indicating that there are items that remain uncertain. Five studies were classified in the high risk of bias category due to having more than two concerns or insufficient information (Figure 2).
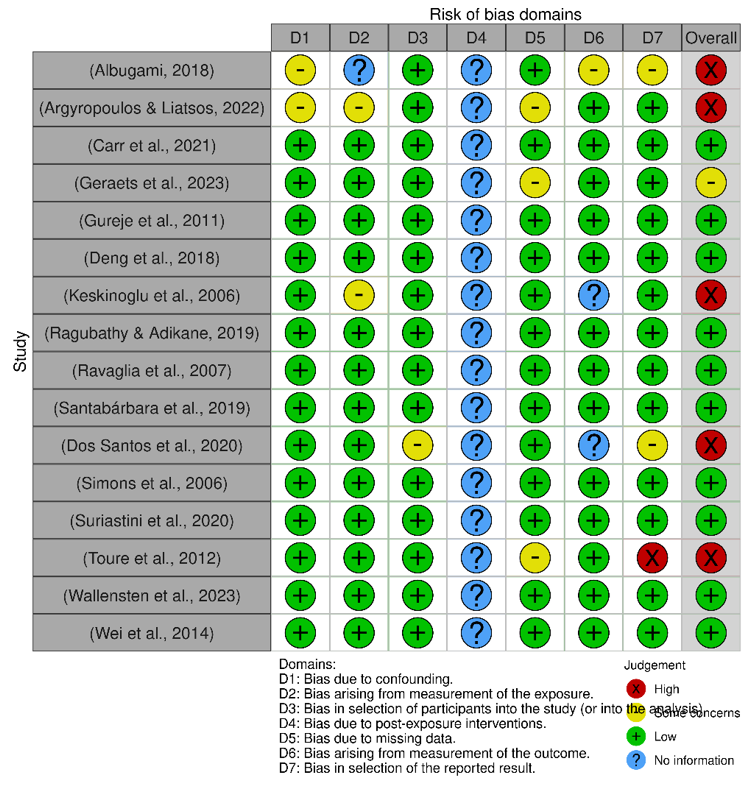
Figure 2. Risk of bias assessment.
Mapping risk factors for dementia
We identified approximately 27 risk factors significantly associated with the prevalence of dementia across countries representative of their respective continents. To summarize the risk factors identified, we attempted to classify them into demographic factors, chronic diseases, lifestyle factors, and psychological disorders.
Demographic factors related to dementia
In the studies reviewed, demographic factors, primarily age and gender, are discussed. Overall, the studies agree that older age increases the prevalence of dementia. The significance values for age among the studies showed a strong association [33, 37-39, 45, 46]. When considering gender, older women are at a higher risk of developing dementia, contributing to an increase in the number of dementia sufferers in this group [37]. The reviewed studies consistently indicate a universal consensus regarding the comparison between males and females, with findings consistently showing that females are more likely to develop dementia than males. This is further supported by the high prevalence rate observed among females [33, 37, 45]. However, we identified one study reporting a higher incidence of dementia among males compared to females [40].
Educational level, occupation, and household income are closely aligned in their contribution to the prevalence of dementia. Among the studies reviewed, it was noted that among all elderly individuals with dementia, those with a low level of education exhibit a strong association [34, 37, 38, 45]. In the Netherlands, elderly individuals with a low economic status have four times the risk of developing dementia [36]. Meanwhile, a study in Turkey indicates that elderly individuals who do not work are 3.22 times more likely to experience dementia than those who are employed [39]. In their study of older individuals residing in well-educated communities in China, Wei et al. discovered a strong correlation between family financial status and the incidence of dementia, with those in poorer financial conditions nearly three times more likely to experience dementia compared to older individuals with sufficient financial resources [48]. Studies in India have linked the number of grandchildren to the incidence of dementia, suggesting that this is more related to the economic conditions of the family. Researchers believe that in Indian society, most people with low economic status tend to have more family members living together in one household [40]. A family history of dementia is a significant contributor to the incidence of dementia in the elderly. In Senegal, there is a strong correlation between a family history of dementia and dementia incidence [46]. This correlation is also observed among the elderly in India, but it occurs only between parents and their children, not between siblings [40].
Lifestyle factors related to dementia
Engaging in both physical and social activities can significantly reduce the risk of dementia among older adults. This suggests that a lack of regular physical and social activity may elevate the risk of developing dementia. Deng et al. illustrate the importance of physical and social activities for the elderly, noting that those who never engage in social activities are at high risk for dementia. Similarly, those who do not participate in physical activity, housework, exercise, and playing Mahjong or chess are also associated with dementia [38]. Regarding activities, daily gardening is identified as a protective factor against the incidence of dementia, with elderly individuals who do not engage in daily gardening having a one-fold increased chance of experiencing dementia compared to those who do [44]. A similar finding was reported by Wei et al., where the elderly who do not engage in physical activity contribute to an approximately three-fold increase in the incidence of dementia [48]. In Nigeria, the elderly who do not participate in social activities are also at high risk for dementia (p=0.04) [37].
Elderly who actively consume alcohol and smoke are at high risk of developing dementia [38, 40, 41, 44]. In addition to these harmful habits, dietary patterns are also an important factor that needs to be considered for the elderly. For example, in China, the elderly who do not consume freshwater fish are at risk of dementia (p=0.004) [38]. Although the significance value is not very strong, the consumption of seafood, liver, and fats is also included in the dietary recommendations of the Chinese study [38]. Another example is that a lack of fruit in the diet of the elderly is associated with a high risk of dementia [48].
History Chronic diseases
Some of the chronic conditions experienced by older adults with dementia include hypertension, stroke, diabetes mellitus (DM), obesity, ventilation disorders, and other cardiovascular-related conditions. A history of stroke has been mentioned repeatedly in the studies reviewed to date, with high significance. Therefore, this factor may need to be a focus in future research, along with hypertension, obesity, and DM, which are closely related to these chronic conditions. Albugami et al. reported a strong association between hypertension and dementia, similar to other studies in Greece and China [33, 34, 38]. Dos Santos et al. provided evidence that older individuals with previous episodes of high blood pressure have roughly a threefold increased likelihood of developing dementia [43]. As stated by Ragubathy & Adikane, midlife and late-life hypertension are major predictors of the onset of arterial dementia in later life [40]. Meanwhile, a history of stroke appears to be a stronger risk factor for dementia compared to hypertension [45, 46]. Meanwhile, a study in China indicates that the elderly with a history of stroke have nearly four times the risk of developing dementia [48]. Another condition associated with cardiovascular disorders is a history of myocardial infarction [34]. Similar to hypertension, DM also has a strong association with dementia in the elderly, as found in studies conducted in Saudi Arabia [33], India [40], and Indonesia [45]. There is only one study that addressed a connection between seizures and dementia, and the findings indicated a robust association [46]. Obesity in the elderly must also be a concern, as some studies have shown it to be associated with dementia in this population [33, 38, 40].
Psychiatric disorders related to dementia
Impairment in this area was the strongest factor among the various factors considered. Depression is the most frequently measured condition in the studies reviewed, and its significance remained stable across these studies. The UK study identified depression as a major factor in the incidence of dementia, associated with a threefold risk [35]. Several countries demonstrate a strong significance in this relationship, including China (p=0.003), Turkey (p=0.0001), Brazil (p<0.001), and Australia, which exhibit the strongest association among the other three factors (p<0.001). Additionally, Sweden and the Netherlands show odds ratios (OR) of 2.39 and 3.59, respectively [38, 39, 43, 44, 47]. According to Ragubathy & Adikane’s research, a previous episode of clinical depression lasting roughly a decade is considered a potential factor. Nonetheless, the histories collected generally cover a period of weeks to years, which is comparatively less significant [40].
Discussion
This study aimed to provide a narrative assessment of the risk factors associated with the incidence of dementia in older adults. In summary, the studies reviewed indicate that the risk factors for dementia are diverse and intricately interconnected. We attempted to classify the identified risk factors into demographic factors, lifestyle choices, chronic illnesses, and psychological conditions. However, we encountered discrepancies among the studies, methodological shortcomings that affected the reliability of their results, and a limited overall number of available studies.
We assessed that within the category of psychological disorders, the level of depression is the strongest factor among several other conditions in this group, including anxiety and stress. Symptoms of depression in older adults manifest in diverse ways, impacting both their sense of well-being and how they are perceived by others. Key characteristics of geriatric depression include a persistent low mood and slowed psychomotor functions. Anxiety and irritability are common, along with numerous physical and psychological complaints. Patients may experience feelings of poverty and hypochondria, as well as sleep disturbances and a heightened risk of suicide attempts. This condition tends to recur and typically has a poor prognosis [49-54]. Depression among older adults can lead not only to work absenteeism but also to complete withdrawal from employment, such as retiring or closing a business. Even among unemployed individuals, a decline in hobbies and domestic activities can lead to a decrease in muscle strength in the lower extremities, which in turn can contribute to a reduction in activities of daily living (ADLs). Preventing the deterioration of ADLs can be achieved through the early detection of depression. According to recent systematic studies, the most significant risk factor for later suicidal behavior in older individuals is depression. Suicidal tendencies in older adults are closely linked to physical illnesses and impairments, stress, living alone, and poor health, all of which are risk factors for suicide attempts [55].
We found evidence that advancing age increases the risk of dementia among seniors. The brain is susceptible to the effects of aging, undergoing various alterations in both its structure and function as individuals grow older [56, 57]. In terms of brain biology, advancing age is a significant risk factor for the onset of cognitive impairments, such as AD, the most common form of dementia, which affects approximately 55 million people globally [58]. While both normal and pathological aging brains experience brain atrophy and cognitive decline, the mechanisms driving these changes are distinct. In normal aging, cognitive decline results from disruptions in circuits and synapses, without significant neuronal loss. This contrasts with dementia and related conditions, which involve extensive neuronal death [59, 60]. In addition to age, gender also appears to be a strong contributor to dementia, as mentioned in the studies reviewed. First, there is a tendency for women to experience depression; several studies indicate that women are twice as likely to encounter depression compared to men during their lifetime [61, 62]. Secondly, the presence of sex hormone factors plays a role, as menopausal women experience an increase in estrogen during this period, which may trigger the onset of dementia [63].
Almost all people with dementia have one or more other chronic conditions [64]. Many of these conditions may cause, or at least contribute to, cognitive decline and dementia. Once a person has dementia, intellectual disability can complicate the management of these other conditions [65]. High blood pressure (hypertension) significantly influences dementia events, as it appears to increase the risk of early cognitive decline, which can progress to dementia or stroke over several years. During this asymptomatic period for most people with hypertension, elevated blood pressure can lead to mild changes, including arteriolar narrowing or microvascular alterations that cause chronic small vessel ischemia (lacunar or white matter lesions), as well as hemosiderin deposits around blood vessels, particularly in deeply penetrating arteries (microbleeds) [66].
This study faced some limitations. Firstly, very few studies were included in this review due to a lack of access to some databases, especially credible ones. Secondly, we included some studies that are of low quality and high bias; therefore, we would like to remind readers and researchers to be cautious in using the results of these studies. However, we are quite confident that the original locations of the studies included are from highly varied countries. For greater detail and accuracy, it is important to conduct a future meta-analysis focusing on one of the most significant variables identified in the current study.
Conclusion
Demographics, lifestyle, chronic diseases, and psychological disorders are risk factors for dementia among older adults.
Acknowledgments: We would like to thank the Chief of STIKES Karya Kesehatan and the Dean of the Faculty of Medicine at Halu Oleo University for granting permission to conduct this study and for the use of laboratory facilities.
Ethical Permissions: There is no ethical clearance for this review.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Risnawati R (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (50%); Umrana S (Second Author), Introduction Writer/Methodologist/Assistant Researcher (15%); Susanty S (Third Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (35%)
Funding/Support: We did not receive any financial support from any party.
Article Type: Systematic Review |
Subject:
Social Determinants of Health
Received: 2024/06/6 | Accepted: 2024/08/8 | Published: 2024/10/10
Received: 2024/06/6 | Accepted: 2024/08/8 | Published: 2024/10/10
References
1. Chertkow H, Feldman HH, Jacova C, Massoud F. Definitions of dementia and predementia states in Alzheimer's disease and vascular cognitive impairment: Consensus from the Canadian conference on diagnosis of dementia. Alzheimers Res Ther. 2013;5(Suppl 1):S2. [Link] [DOI:10.1186/alzrt198]
2. Stephan B, Birdi R, Tang EYH, Cosco TD, Donini LM, Licher S, et al. Secular trends in dementia prevalence and incidence worldwide: A systematic review. J Alzheimers Dis. 2018;66(2):653-80. [Link] [DOI:10.3233/JAD-180375]
3. Cao Q, Tan CC, Xu W, Hu H, Cao XP, Dong Q, et al. The prevalence of dementia: A systematic review and meta-analysis. J Alzheimers Dis. 2020;73(3):1157-66. [Link] [DOI:10.3233/JAD-191092]
4. Jia L, Quan M, Fu Y, Zhao T, Li Y, Wei C, et al. Dementia in China: Epidemiology, clinical management, and research advances. Lancet Neurol. 2020;19(1):81-92. [Link] [DOI:10.1016/S1474-4422(19)30290-X]
5. GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105-25. [Link]
6. Cheng ST. Dementia caregiver burden: A research update and critical analysis. Curr Psychiatry Rep. 2017;19(9):64. [Link] [DOI:10.1007/s11920-017-0818-2]
7. Shon C, Yoon H. Health-economic burden of dementia in South Korea. BMC Geriatr. 2021;21(1):549. [Link] [DOI:10.1186/s12877-021-02526-x]
8. Burks HB, Des Bordes JKA, Chadha R, Holmes HM, Rianon NJ. Quality of life assessment in older adults with dementia: A systematic review. Dement Geriatr Cogn Disord. 2021;50(2):103-10. [Link] [DOI:10.1159/000515317]
9. Hermann P, Zerr I. Rapidly progressive dementias-aetiologies, diagnosis and management. Nat Rev Neurol. 2022;18:363-76. [Link] [DOI:10.1038/s41582-022-00659-0]
10. Jenkins LM, Wang L, Rosen H, Weintraub S. A transdiagnostic review of neuroimaging studies of apathy and disinhibition in dementia. Brain. 2022;145(6):1886-905. [Link] [DOI:10.1093/brain/awac133]
11. Warren J, Collinge J, Fox N, Mead S, Mummery C, Rohrer J, et al. Cognitive impairment and dementia. In: Neurology: A queen square textbook. Hoboken: John Wiley & Sons; 2024. p. 319-67. [Link] [DOI:10.1002/9781119715672.ch11]
12. Lindeza P, Rodrigues M, Costa J, Guerreiro M, Rosa MM. Impact of dementia on informal care: A systematic review of family caregivers' perceptions. BMJ Support Palliat Care. 2020;14:e38-49. [Link] [DOI:10.1136/bmjspcare-2020-002242]
13. Murphy C, De Laine C, Macaulay M, Hislop Lennie K, Fader M. Problems faced by people living at home with dementia and incontinence: causes, consequences and potential solutions. Age Ageing. 2021;50(3):944-54. [Link] [DOI:10.1093/ageing/afaa262]
14. Angeles RC, Berge LI, Gedde MH, Kjerstad E, Vislapuu M, Puaschitz NG, et al. Which factors increase informal care hours and societal costs among caregivers of people with dementia? A systematic review of Resource Utilization in Dementia (RUD). Health Econ Rev. 2021;11(1):37. [Link] [DOI:10.1186/s13561-021-00333-z]
15. Farina N, Hicks B, Baxter K, Birks Y, Brayne C, Dangoor M, et al. DETERMinants of quality of life, care and costs, and consequences of INequalities in people with Dementia and their carers (DETERMIND): A protocol paper. Int J Geriatr Psychiatry. 2020;35(3):290-301. [Link] [DOI:10.1002/gps.5246]
16. Velilla L, Acosta-Baena N, Allen I, Lopera F, Kramer J. Analysis of family stigma and socioeconomic factors impact among caregivers of patients with early-and late-onset Alzheimer's disease and frontotemporal dementia. Sci Rep. 2022;12(1):12663. [Link] [DOI:10.1038/s41598-022-16400-2]
17. Sörensen S, Conwell Y. Issues in dementia caregiving: Effects on mental and physical health, intervention strategies, and research needs. Am J Geriatr Psychiatry. 2011;19(6):491-6. [Link] [DOI:10.1097/JGP.0b013e31821c0e6e]
18. Schulz R, Martire LM. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12(3):240-9. [Link] [DOI:10.1097/00019442-200405000-00002]
19. Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: A systematically conducted narrative review of dementia-specific measurement scales. Aging Ment Health. 2015;19(1):13-31. [Link] [DOI:10.1080/13607863.2014.915923]
20. Wimo A, Seeher K, Cataldi R, Cyhlarova E, Dielemann JL, Frisell O, et al. The worldwide costs of dementia in 2019. Alzheimers Dement. 2023;19(7):2865-73. [Link] [DOI:10.1002/alz.12901]
21. Lynch C. World Alzheimer report 2019: Attitudes to dementia, a global survey: Public health: Engaging people in ADRD research. Alzheimers Dement. 2020;16(S10):e038255. [Link] [DOI:10.1002/alz.038255]
22. Rabinovici GD, La Joie R. Amyloid-targeting monoclonal antibodies for Alzheimer disease. JAMA. 2023;330(6):507-9. [Link] [DOI:10.1001/jama.2023.11703]
23. Mok VCT, Lam BYK, Wong A, Ko H, Markus HS, Wong LKS. Early-onset and delayed-onset poststroke dementia-revisiting the mechanisms. Nat Rev Neurol. 2017;13:148-59. [Link] [DOI:10.1038/nrneurol.2017.16]
24. Gauthier S, Albert M, Fox N, Goedert M, Kivipelto M, Mestre-Ferrandiz J, et al. Why has therapy development for dementia failed in the last two decades?. Alzheimers Dement. 2016;12(1):60-4. [Link] [DOI:10.1016/j.jalz.2015.12.003]
25. Niotis K, Saperia C, Saif N, Carlton C, Isaacson RS. Alzheimer's disease risk reduction in clinical practice: A priority in the emerging field of preventive neurology. Nat Ment Health. 2024;2:25-40. [Link] [DOI:10.1038/s44220-023-00191-0]
26. Wolters FJ, Chibnik LB, Waziry R, Anderson R, Berr C, Beiser A, et al. Twenty-seven-year time trends in dementia incidence in Europe and the United States: The Alzheimer Cohorts Consortium. Neurology. 2020;95(5):e519-31. [Link] [DOI:10.1212/WNL.0000000000010022]
27. Lecordier S, Manrique-Castano D, El Moghrabi Y, ElAli A. Neurovascular alterations in vascular dementia: Emphasis on risk factors. Front Aging Neurosci. 2021;13:727590. [Link] [DOI:10.3389/fnagi.2021.727590]
28. Takeda S, Rakugi H, Morishita R. Roles of vascular risk factors in the pathogenesis of dementia. Hypertens Res. 2020;43(3):162-7. [Link] [DOI:10.1038/s41440-019-0357-9]
29. Parial LL, Lam SC, Ho JYS, Suen LKP, Leung AYM. Public knowledge of the influence of modifiable cardiovascular risk factors on dementia: A systematic literature review and meta-analysis. Aging Ment Health. 2021;25(8):1395-409. [Link] [DOI:10.1080/13607863.2020.1786801]
30. Rolandi E, Zaccaria D, Vaccaro R, Abbondanza S, Pettinato L, Davin A, et al. Estimating the potential for dementia prevention through modifiable risk factors elimination in the real-world setting: A population-based study. Alzheimers Res Ther. 2020;12(1):94. [Link] [DOI:10.1186/s13195-020-00661-y]
31. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413-46. [Link] [DOI:10.1016/S0140-6736(20)30367-6]
32. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [Link] [DOI:10.1136/bmj.n71]
33. Albugami M, Qadi M, Almugbel F, Mohammed A. The demographic characteristics and the risk factors of dementia in Saudi elderly. Am J Psychiatry Neurosci. 2018;6(1):1-8. [Link] [DOI:10.11648/j.ajpn.20180601.11]
34. Argyropoulos K, Liatsos C. Prevalence and risk factors of dementia and depressive symptoms in the elderly: A cross-sectional study in west-Greece. Achaiki Iatriki. 2022;41(3):118-25. [Link]
35. Carr AL, Sluiman AJ, Grecian SM, Forster R, McLachlan S, Strachan MWJ, et al. Depression as a risk factor for dementia in older people with type 2 diabetes and the mediating effect of inflammation. Diabetologia. 2021;64(2):448-57. [Link] [DOI:10.1007/s00125-020-05301-6]
36. Geraets AFJ, Leist AK, Deckers K, Verhey FRJ, Schram MT, Köhler S. Contributions of modifiable risk factors to increased dementia risk in depression. Psychol Med. 2023;53(14):6583-91. [Link] [DOI:10.1017/S0033291722003968]
37. Gureje O, Ogunniyi A, Kola L, Abiona T. Incidence of and risk factors for dementia in the Ibadan study of aging. J Am Geriatr Soc. 2011;59(5):869-74. [Link] [DOI:10.1111/j.1532-5415.2011.03374.x]
38. Deng J, Cao C, Jiang Y, Peng B, Wang T, Yan K, et al. Prevalence and effect factors of dementia among the community elderly in Chongqing, China. Psychogeriatrics. 2018;18(5):412-20. [Link] [DOI:10.1111/psyg.12343]
39. Keskinoglu P, Giray H, Picakciefe M, Bilgic N, Ucku R. The prevalence and risk factors of dementia in the elderly population in a low socio-economic region of Izmir, Turkey. Arch Gerontol Geriatr. 2006;43(1):93-100. [Link] [DOI:10.1016/j.archger.2005.09.006]
40. Ragubathy PK, Adikane H. Prevalence of risk factors for dementia in elderly population in tribal area of Central India-A community-based cross-sectional study. J Med Sci Health. 2019;5(3):19-30. [Link] [DOI:10.46347/JMSH.2019.v05i03.004]
41. Ravaglia G, Forti P, Maioli F, Bastagli L, Montesi F, Pisacane N, et al. Endogenous sex hormones as risk factors for dementia in elderly men and women. J Gerontol A Biol Sci Med Sci. 2007;62(9):1035-41. [Link] [DOI:10.1093/gerona/62.9.1035]
42. Santabárbara J, Lopez-Anton R, De La Cámara C, Lobo E, Gracia-García P, Villagrasa B, et al. Clinically significant anxiety as a risk factor for dementia in the elderly community. Acta Psychiatr Scand. 2019;139(1):6-14. [Link] [DOI:10.1111/acps.12966]
43. Dos Santos CDS, De Bessa TA, Xavier AJ. Factors associated with dementia in elderly. Ciencia e Saude Coletiva. 2020;25(2):603-11. [Link] [DOI:10.1590/1413-81232020252.02042018]
44. Simons LA, Simons J, McCallum J, Friedlander Y. Lifestyle factors and risk of dementia: Dubbo study of the elderly. Med J Aust. 2006;184(2):68-70. [Link] [DOI:10.5694/j.1326-5377.2006.tb00120.x]
45. Suriastini NW, Turana Y, Supraptilah B, Wicaksono TY, Mulyanto ED. Prevalence and risk factors of dementia and caregiver's knowledge of the early symptoms of Alzheimer's disease. Aging Med Healthc. 2020;11(2):60-6. [Link] [DOI:10.33879/AMH.2020.065-1811.032]
46. Toure K, Coume M, Ndiaye M, Zunzunegui MV, Bacher Y, Diop AG, et al. Risk factors for dementia in a Senegalese elderly population aged 65 years and over. Dement Geriatr Cogn Dis Extra. 2012;2(1):160-8. [Link] [DOI:10.1159/000332022]
47. Wallensten J, Ljunggren G, Nager A, Wachtler C, Bogdanovic N, Petrovic P, et al. Stress, depression, and risk of dementia-a cohort study in the total population between 18 and 65 years old in Region Stockholm. Alzheimers Res Ther. 2023;15(1):161. [Link] [DOI:10.1186/s13195-023-01308-4]
48. Wei CJ, Cheng Y, Zhang Y, Sun F, Zhang WS, Zhang MY. Risk factors for dementia in highly educated elderly people in Tianjin, China. Clin Neurol Neurosurg. 2014;122:4-8. [Link] [DOI:10.1016/j.clineuro.2014.04.004]
49. Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363-89. [Link] [DOI:10.1146/annurev.clinpsy.032408.153621]
50. Sözeri-Varma G. Depression in the elderly: Clinical features and risk factors. Aging Dis. 2012;3(6):465-71. [Link]
51. Becker NB, Jesus SN, Joao KADR, Viseu JN, Martins RIS. Depression and sleep quality in older adults: A meta-analysis. Psychol Health Med. 2017;22(8):889-95. [Link] [DOI:10.1080/13548506.2016.1274042]
52. Haigh EAP, Bogucki OE, Sigmon ST, Blazer DG. Depression among older adults: A 20-year update on five common myths and misconceptions. Am J Geriatr Psychiatry. 2018;26(1):107-22. [Link] [DOI:10.1016/j.jagp.2017.06.011]
53. Mitchell AJ, Subramaniam H. Prognosis of depression in old age compared to middle age: A systematic review of comparative studies. Am J Psychiatry. 2005;162(9):1588-601. [Link] [DOI:10.1176/appi.ajp.162.9.1588]
54. Comijs HC, Nieuwesteeg J, Kok R, Van Marwijk HW, Van Der Mast RC, Naarding P, et al. The two-year course of late-life depression; Results from the Netherlands study of depression in older persons. BMC Psychiatry. 2015;15:20. [Link] [DOI:10.1186/s12888-015-0401-5]
55. Beghi M, Butera E, Cerri CG, Cornaggia CM, Febbo F, Mollica A, et al. Suicidal behaviour in older age: A systematic review of risk factors associated to suicide attempts and completed suicides. Neurosci Biobehav Rev. 2021;127:193-211. [Link] [DOI:10.1016/j.neubiorev.2021.04.011]
56. Nouchi R, Taki Y, Takeuchi H, Sekiguchi A, Hashizume H, Nozawa T, et al. Four weeks of combination exercise training improved executive functions, episodic memory, and processing speed in healthy elderly people: Evidence from a randomized controlled trial. Age. 2014;36(2):787-99. [Link] [DOI:10.1007/s11357-013-9588-x]
57. Eikelboom WS, Bertens D, Kessels RPC. Cognitive rehabilitation in normal aging and individuals with subjective cognitive decline. In: Cognitive rehabilitation and neuroimaging. Cham: Springer; 2020. p. 37-67. [Link] [DOI:10.1007/978-3-030-48382-1_3]
58. Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: A cross-sectional study. Lancet Public Health. 2020;5(12):e661-71. [Link] [DOI:10.1016/S2468-2667(20)30185-7]
59. Dumitriu D, Hao J, Hara Y, Kaufmann J, Janssen WGM, Lou W, et al. Selective changes in thin spine density and morphology in monkey prefrontal cortex correlate with aging-related cognitive impairment. J Neurosci. 2010;30(22):7507-15. [Link] [DOI:10.1523/JNEUROSCI.6410-09.2010]
60. Burke SN, Barnes CA. Neural plasticity in the ageing brain. Nat Rev Neurosci. 2006;7:30-40. [Link] [DOI:10.1038/nrn1809]
61. Kuehner C. Why is depression more common among women than among men?. Lancet Psychiatry. 2017;4(2):146-58. [Link] [DOI:10.1016/S2215-0366(16)30263-2]
62. Albert PR. Why is depression more prevalent in women?. J Psychiatry Neurosci. 2015;40(4):219-21. [Link] [DOI:10.1503/jpn.150205]
63. Kundakovic M, Rocks D. Sex hormone fluctuation and increased female risk for depression and anxiety disorders: From clinical evidence to molecular mechanisms. Front Neuroendocrinol. 2022;66:101010. [Link] [DOI:10.1016/j.yfrne.2022.101010]
64. Snowden MB, Steinman LE, Bryant LL, Cherrier MM, Greenlund KJ, Leith KH, et al. Dementia and co‐occurring chronic conditions: a systematic literature review to identify what is known and where are the gaps in the evidence?. Int J Geriatr Psychiatry. 2017;32(4):357-71. [Link] [DOI:10.1002/gps.4652]
65. Rost NS, Brodtmann A, Pase MP, Van Veluw SJ, Biffi A, Duering M, et al. Post-stroke cognitive impairment and dementia. Circ Res. 2022;130(8):1252-71. [Link] [DOI:10.1161/CIRCRESAHA.122.319951]
66. Sierra C. Hypertension and the risk of dementia. Front Cardiovasc Med. 2020;7:5. [Link] [DOI:10.3389/fcvm.2020.00005]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |