Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 459-469 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nurmila W, Erika K, Erfina E. Nurses' Experience Evaluation in Traditional and Complementary Medicine; A Systematic Review. Health Educ Health Promot 2024; 12 (3) :459-469
URL: http://hehp.modares.ac.ir/article-5-75453-en.html
URL: http://hehp.modares.ac.ir/article-5-75453-en.html
1- Department of Nursing, Faculty of Nursing, Hasanuddin University, Makassar, Indonesia
Full-Text [PDF 787 kb]
(1944 Downloads)
| Abstract (HTML) (905 Views)
Full-Text: (86 Views)
Introduction
The concept of traditional, complementary, alternative, and integrative medicines is often used in healthcare delivery. The term "traditional medicine" (TM) is used in healthcare practices that have evolved over generations within a country, while "complementary medicine" (CM) or alternative is interchangeably used by some countries that do not include these practices in their national tradition [1]. Further, WHO defines traditional and complementary medicine (T&CM) as a combination of TM and CM, including products, practices, and practitioners [1].
Various countries have started to pay attention to the use of T&CM. According to the global report on T&CM in 2019, 98% of WHO member countries have policies related to T&CM [2]. The prevalence of T&CM use varies from 24-71.3% in the general population [3] and shows increased usage among children [4], adults [5], and the elderly [6]. These practices are used for various physical and psychological health issues [7, 8]. T&CM is considered holistic, and expectations of benefits are the main reasons for its use, although the scientific evidence remains debated [9].
The ongoing conflict between modern medicine and T&CM often shows that both can coexist, although modern medicine does not always support T&CM [10]. Doctors and nurses believe that combining complementary and conventional cancer treatments is risky [11]. Nurses, who have a fundamental responsibility to provide holistic care to a diverse patient population, need to be aware of T&CM [12]. A study showed that nurses are more familiar with and have more positive attitudes and beliefs toward T&CM, believing it has a more significant impact on patient care compared to other healthcare workers [13]. Nurses must be able to consider and provide information about T&CM in delivering patient care [14]. Nurses use a cultural perspective in their practice, since transcultural nursing contributes to the establishment and adaptation of healthy family units [15]. Specifically, nurses should be encouraged to learn more about the cultural needs of a diverse patient population and provide consistent care, thus evaluating nurses' experiences with T&CM is necessary.
Previous studies have reviewed how the practice of T&CM among nurses has been conducted in various countries [16, 17]. Furthermore, information about the instruments used is needed. Quality instruments play a crucial role in assessing nurses' experiences with multi-professional care that involves a holistic approach [18]. The assessment of T&CM use among nurses in many parts of the world has been addressed in earlier studies, but an important aspect of these studies remains unexplored. Quality instruments remain necessary in measuring how nurses deal with T&CM if any, while providing multi-professional, holistic, primary health care. However, as of now, there have been no comprehensive reviews of these instruments documented in the literature. It is important to bring greater attention to this omission since the use of Traditional and Complementary Medicine (T&CM) is growing globally, leading to an increased need for transcultural nursing care.
Medical policies and nursing management need excellent instruments in the collection of trustable data concerning nurses’ experiences of working with T&CM. This is necessary in assessing the current practices, developmental needs, and improving techniques that would strengthen transcultural nursing skills. In the absence of such understanding, it is always very difficult, if not impossible, to make appropriate clinical decisions regarding T&CM incorporation in clinicians’ education and practice and about the education of nursing such policies. Therefore, this scope review aims to provide an overview of the instruments used in recent research. These tools will be filtered and examined to inform researchers, educators, and health authorities as part of their considerations for the development of nursing in the field of T&CM.
Information and Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-SCR) guidelines to enhance reporting quality and ensure fidelity in the review process [19]. The review used the Scoping Review Framework, which includes five stages; 1) identifying the research question, 2) identifying relevant studies, 3) study selection, 4) charting the data, and 5) collating, summarizing, and reporting the results [20].
Review question (stage 1)
The goals and questions of the scoping review were based on the Population, Concept, and Context (PCC) framework [21]. Furthermore, PCC is used in search keywords. The search keywords were: Population: Nurses OR nursing professionals OR clinical nurses; Concept: Assessment tool OR instrument OR scale OR questionnaire OR survey; And Context: Complementary therapy OR alternative medicine OR integrative healthcare or CAM OR complementary alternative medicine OR TCM OR traditional complementary medicine. The review question based on the PCC framework was: What is known from the literature about the assessment instruments used in evaluating the experience in T&CM among nurses? What domains are assessed by these instruments? Have the instruments been validated?
Identifying relevant studies (stage 2)
A comprehensive literature search was conducted in March 2024 on six databases: PubMed, ScienceDirect, DOAJ, Taylor & Francis, Wiley, and GARUDA (provides integrated access to institutional repositories, scholarly journals, theses, and diverse academic literature resources from Indonesia). In addition, we checked the citations of the studies and reviews that were included and conducted a manual search. All articles that conducted research using questionnaires on nurse populations to measure their views on T&CM were considered. Inclusion criteria were articles published within the last ten years (2014-2024), original papers, and full-text available. Exclusion criteria included non-English articles, theses, review articles, commentaries, conceptual, qualitative, and case studies. The article selection process followed the PRISMA checklist guidelines to enhance accuracy in article search [22].
Study selection (stage 3)
The PRISMA flowchart depicts the process, screening outcomes, and criteria for articles extraction following the initial search, which adhered to the study's inclusion and exclusion criteria (Figure 1). The abstracts found during the article search were retrieved using the reference manager software Mendeley and then transferred to the Rayyan software program to facilitate and record the article screening process [23]. In total, 400 pertinent abstracts were gathered from the 7 databases, and an additional 15 manuscripts identified by reference. After eliminating duplicates and articles published more than 10 years ago, 192 articles were retained. Articles were then screened, eliminating 382 articles, and 18 articles were included and deemed suitable for review.
Charting the data (stage 4)
This review utilized recommendations from The Joanna Briggs Institute for the extraction, analysis, and presentation of results in scoping reviews [24]. The data were extracted to incorporate crucial details such as the study site, research design, sample size, and the instruments used in the study.
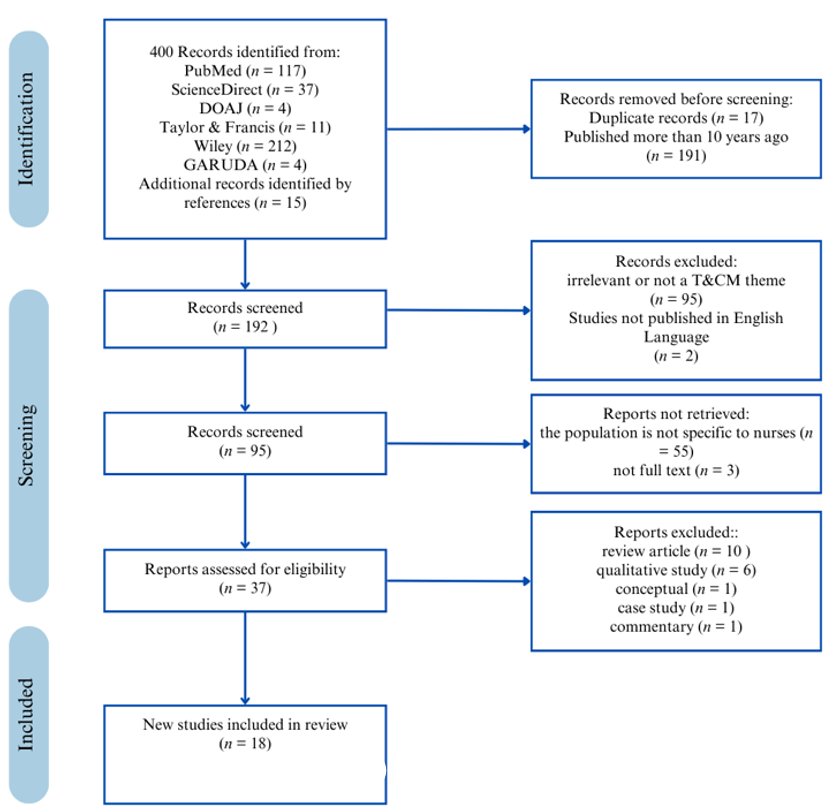
Figure 1. PRISMA flowcharts for study selection and inclusion
Findings
Characteristics of the studies
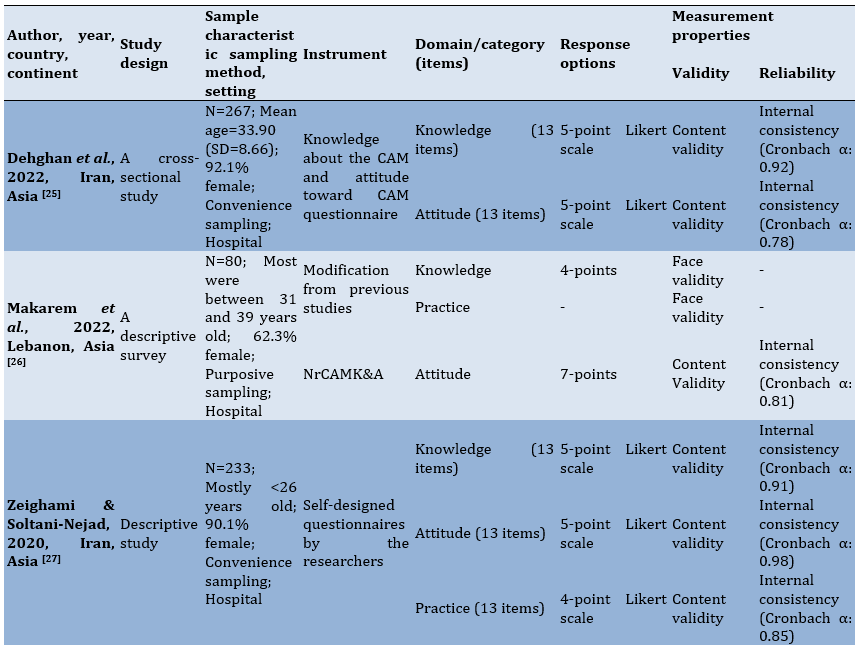
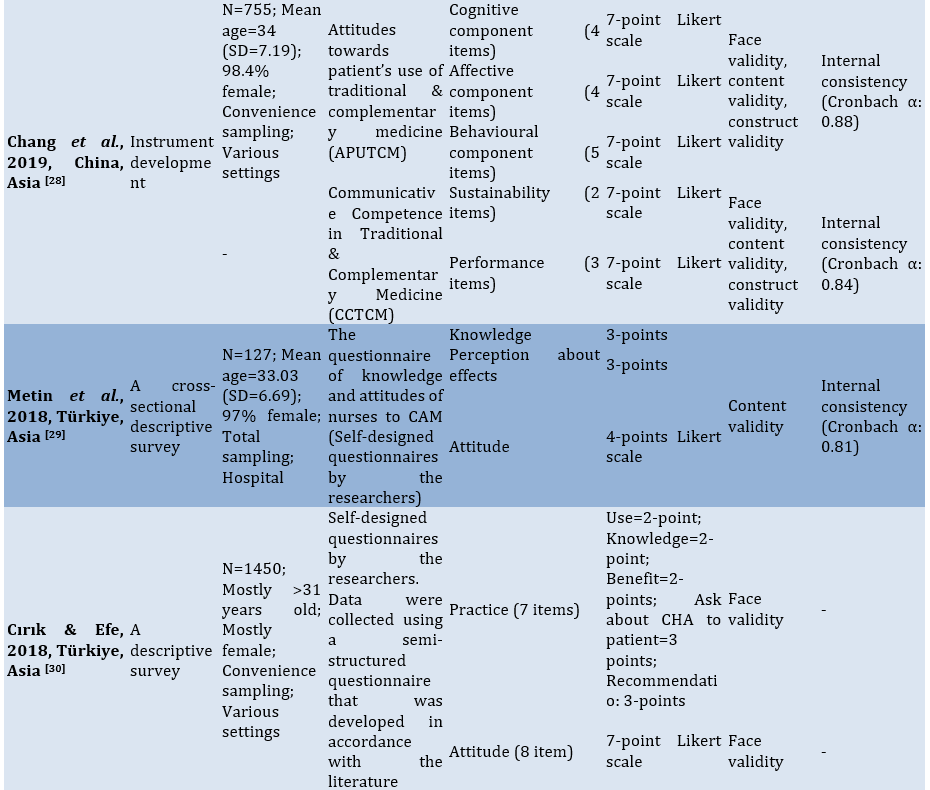
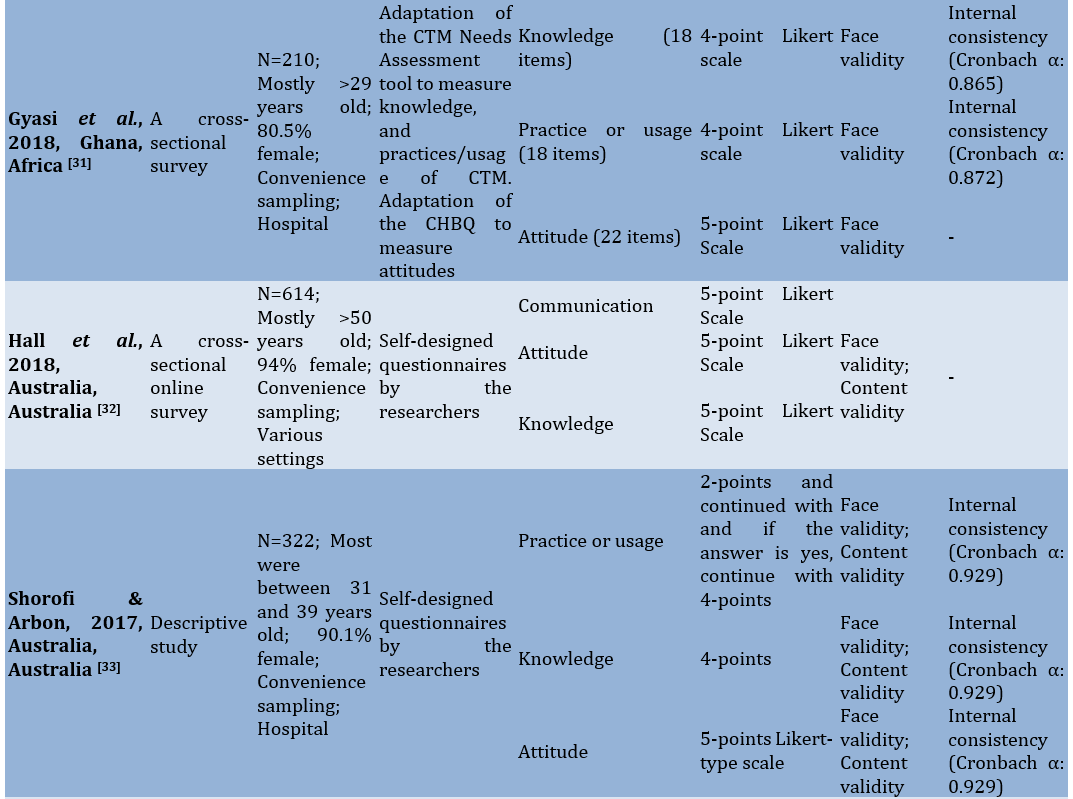
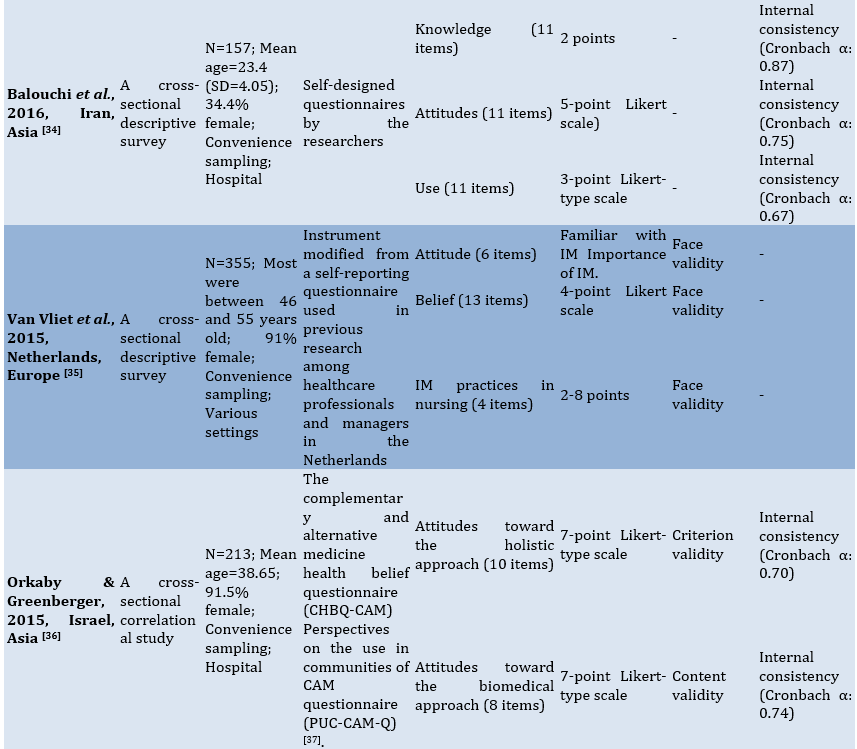
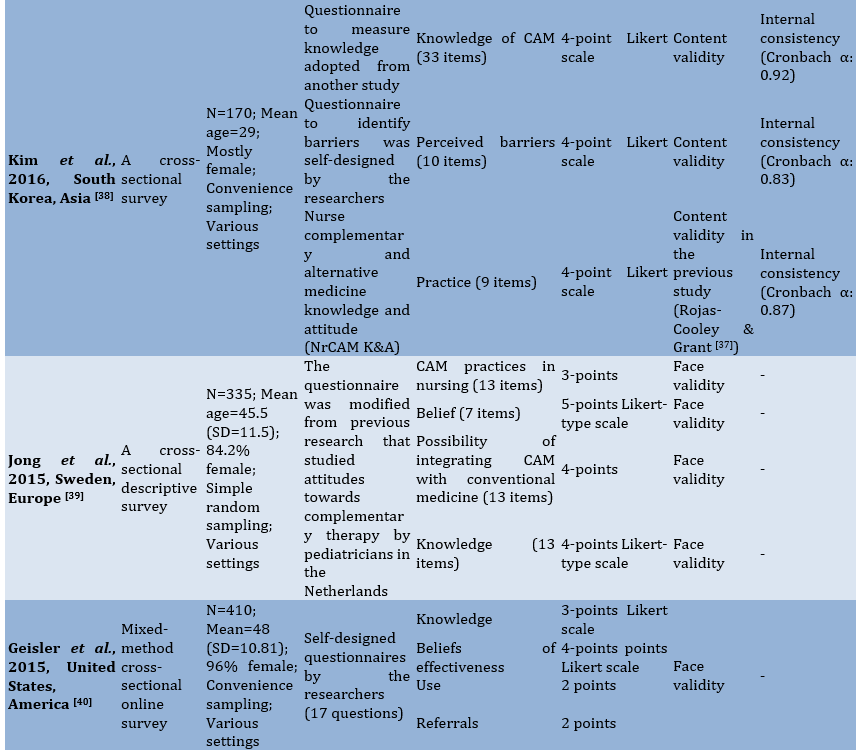
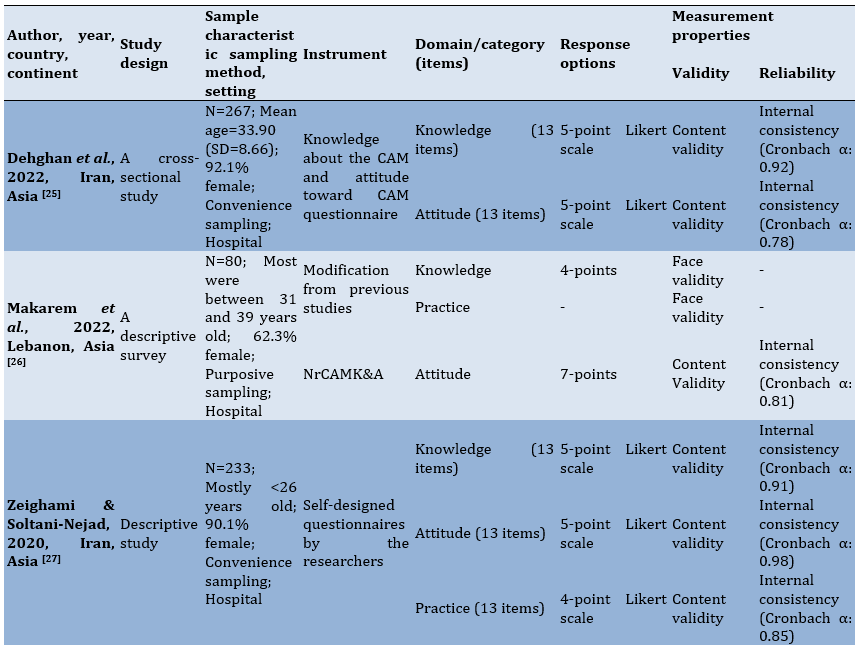
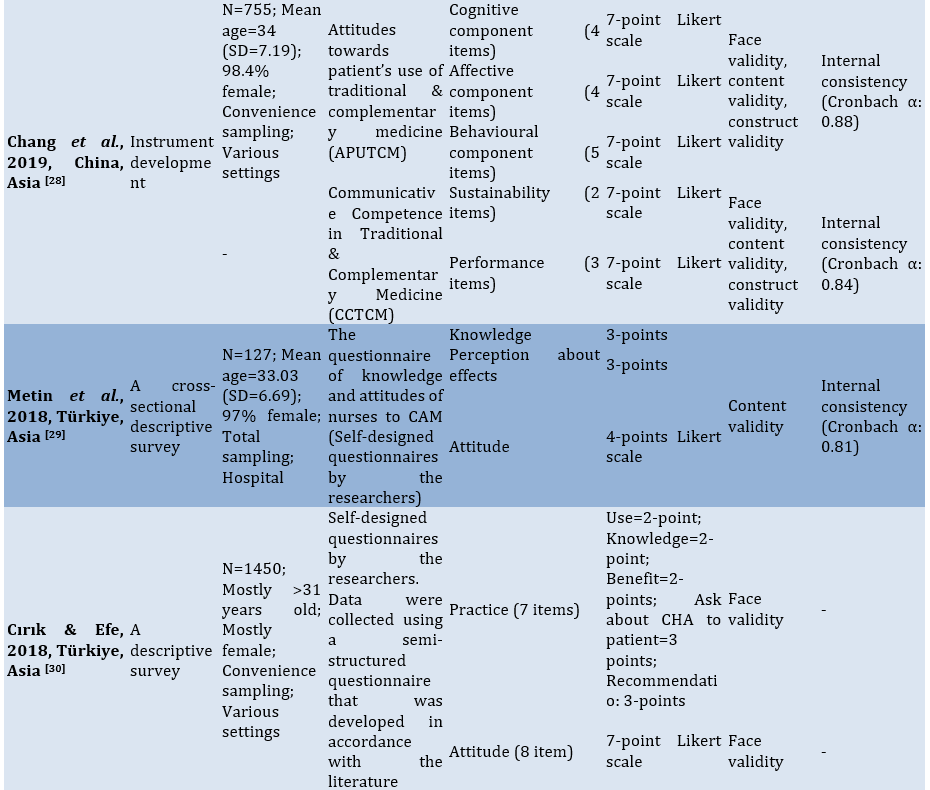
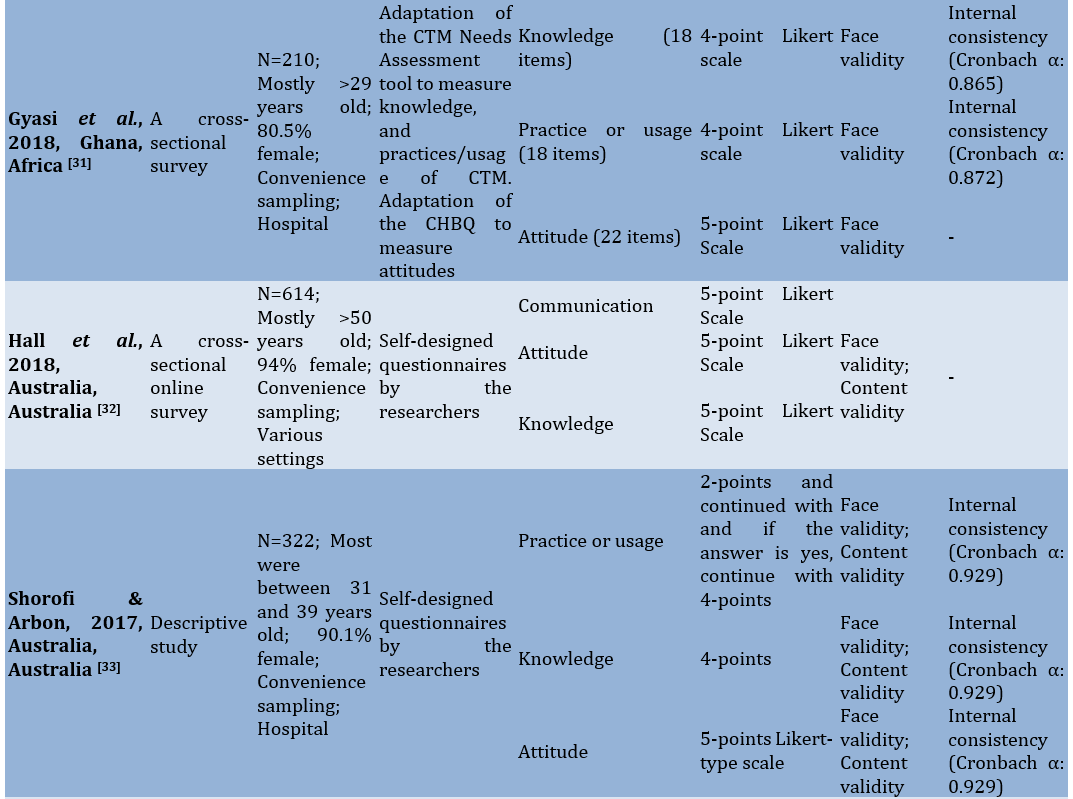
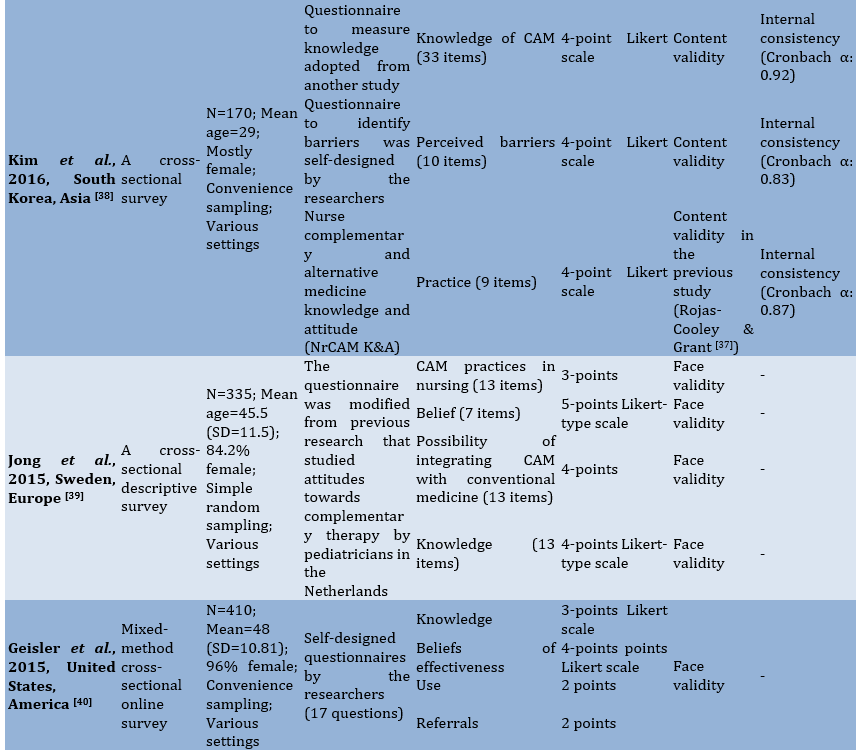
This review found that the majority of articles were conducted in Asia (55.6%), followed by the Americas (16.7%), then Europe (11.11%), Australia (11.11%), and Africa (5.5%). Most (15 studies) used a survey design, only one study employed instrument development, and two studies used a descriptive design. Most studies were implemented in hospitals (n=11) and 7 others in various settings. The average sample size was 354 nurses. The used sampling methods included convenience sampling (n=13), purposive sampling (n=2), simple random sampling (n=2), and total sampling (n=1; Table 1).
Table 1. Extracted data from the final documents
Description of the instruments
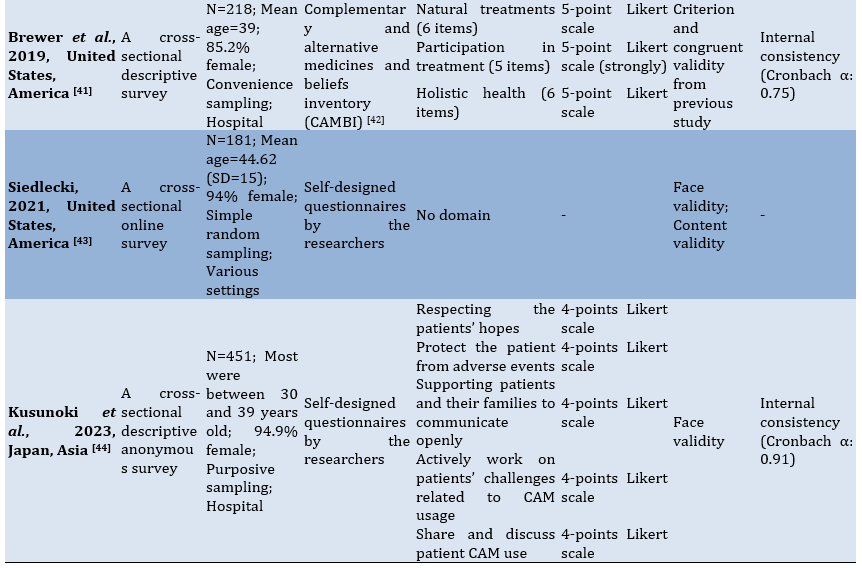
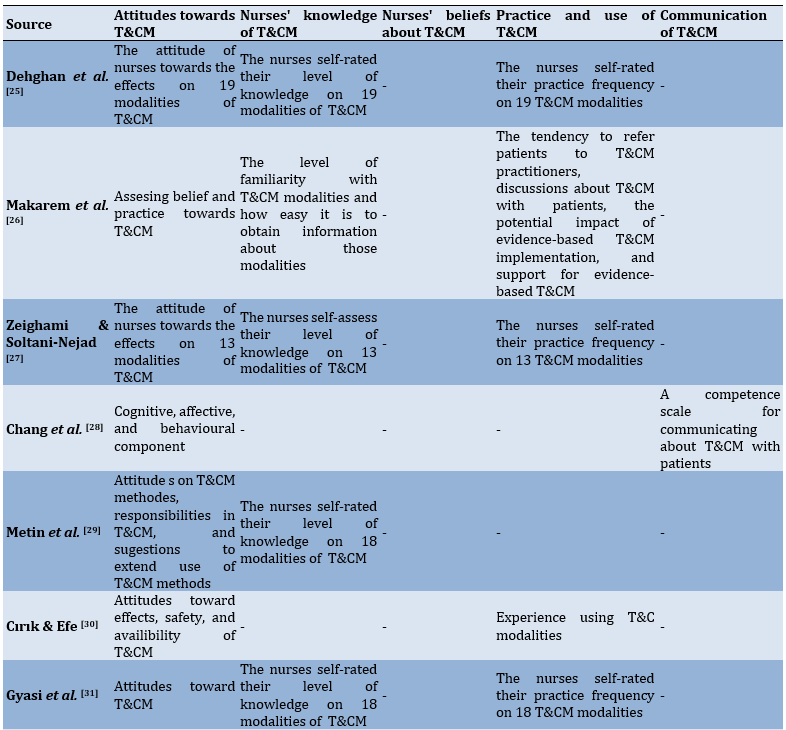
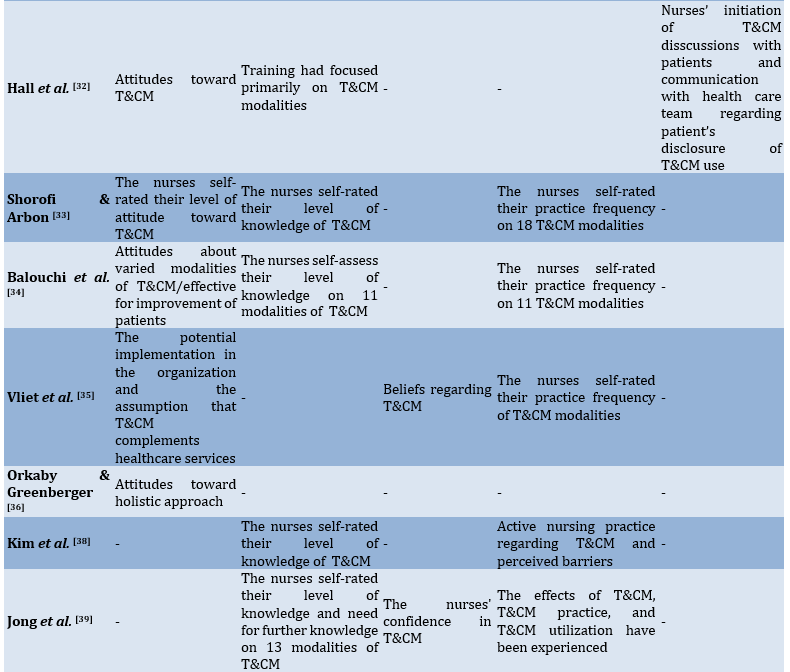
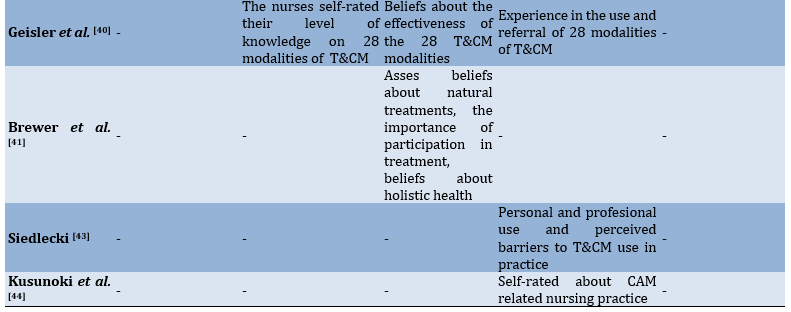
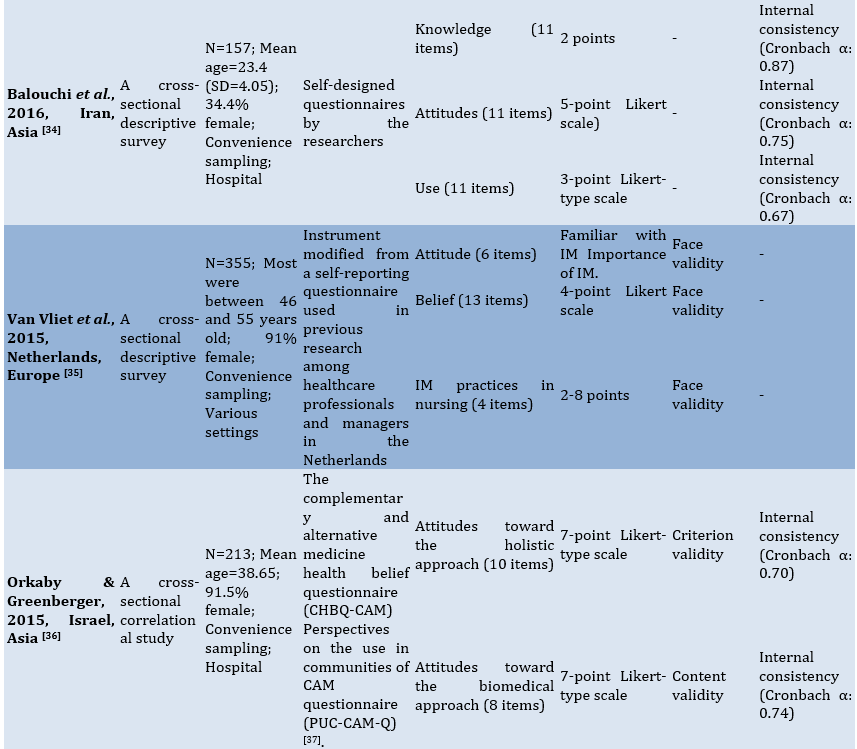
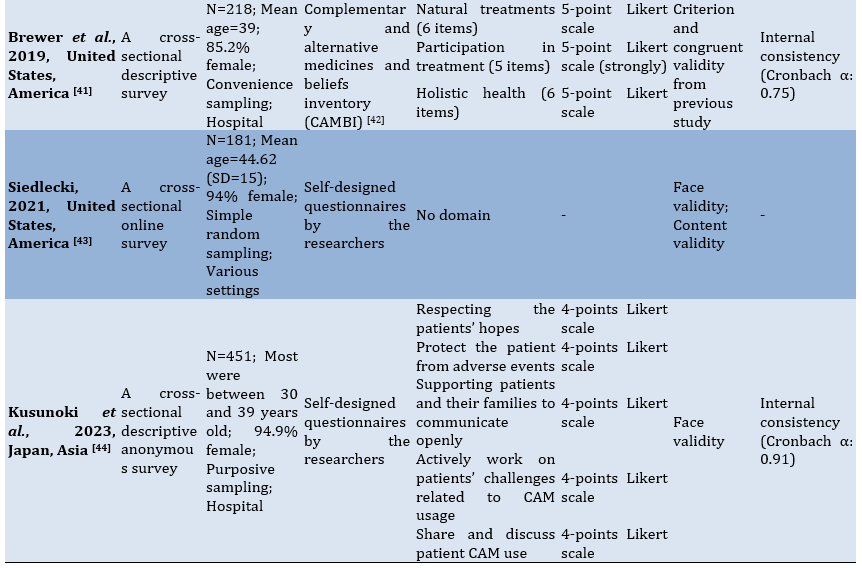
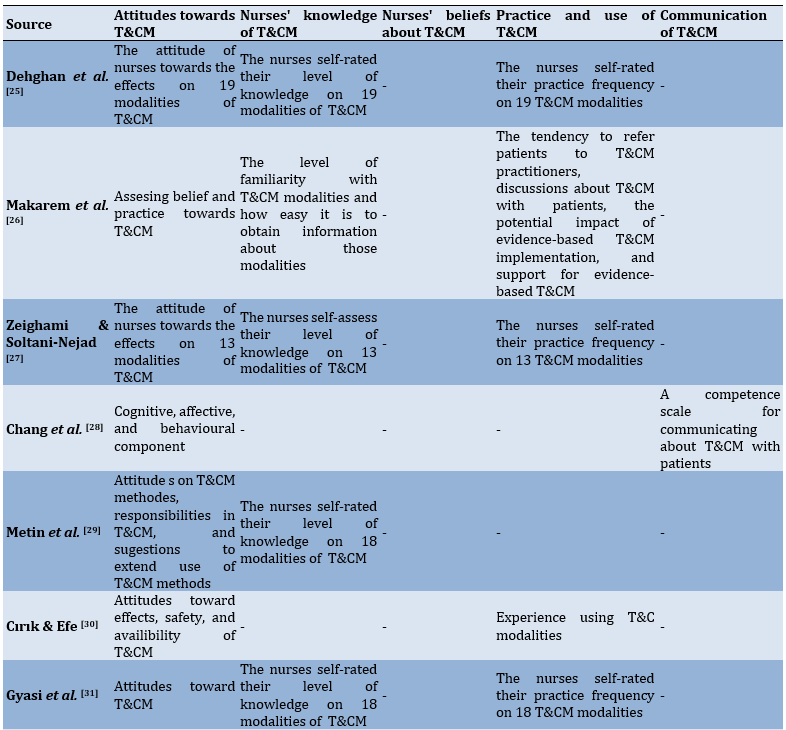
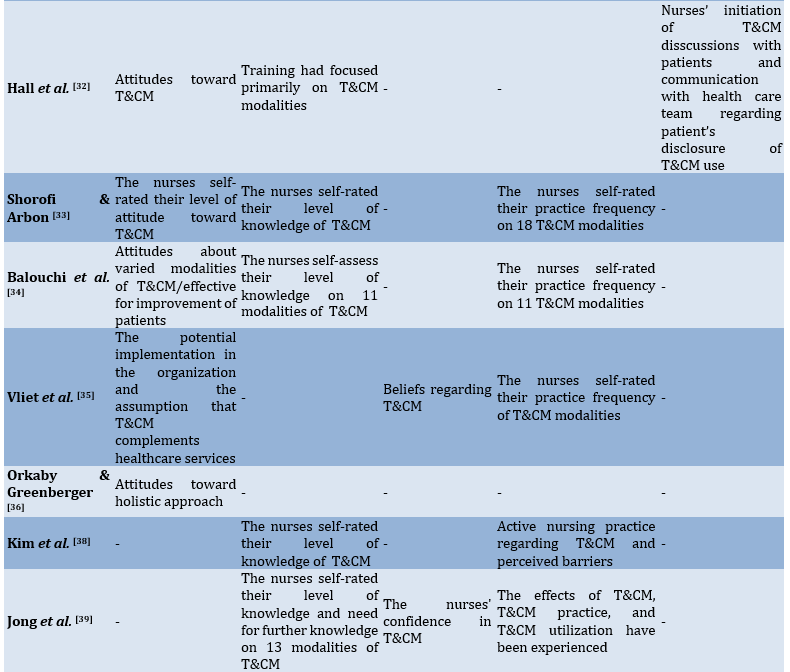
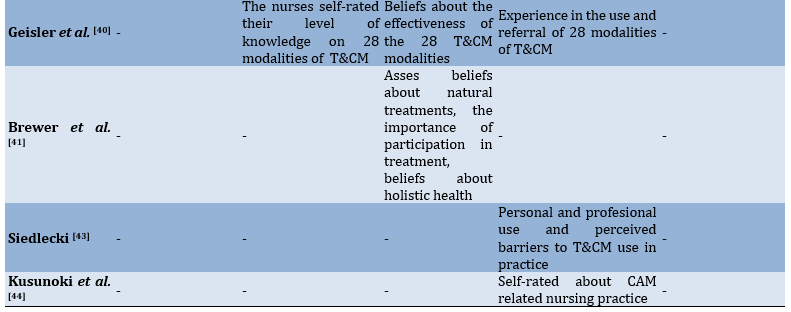
Most of the studies (n=11) used instruments self-developed by researchers, five parts of the study instruments adopted from previous research, while the rest were adapted from earlier studies. Each instrument along with the attributes being measured. Most instruments evaluated nurses' attitudes towards T&CM (n=12), knowledge (n=11), and practices (n=11), while relatively few assessed beliefs (n=4) and communication (n=3; Table 2).
Table 2. Instruments from included studies classified by TCM attribute among nurses
Nurses' attitudes towards T&CM
12 out of 18 studies measured nurses' attitudes toward T&CM [25-36]. These studies used self-designed instruments (n=8), adaptations of the same instrument, namely The Complementary and Alternative Medicine Health Belief Questionnaire (CHBQ-CAM; n=2), adoption from previous research (n=2), and the Nurse Complementary and Alternative Medicine Knowledge and Attitude (NrCAM K&A) developed by Rojas-Cooley & Grant [37] (n=1). Most studies (n=11) used Likert scales, predominantly a 5-point scale. Eight studies reported question items on attitude measurement, with question items ranging from 6 to 22 items. One study did not report a validity test, while others used face validity (n=3), content validity (n=4), face validity and content validity (n=3), face, content and construct validity (n=1), and criterion validity (n=1). Additionally, five studies did not report reliability tests. A total of eight studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.70 to 0.92. Most of the instruments inquired about the effects of T&CM modalities (n=4), followed by items questioning attitudes towards T&CM (n=3), the potential implementation of T&CM within their organizations (n=1), beliefs and practices (n=1), and aspects of cognitive, affective, and behavioral components (n=1).
Nurses' knowledge of T&CM
Out of 18 studies, 11 measured nurses' knowledge of T&CM [25-27, 29, 31-34, 38-40]. Instruments used in these studies were self-designed (n=6), adopted from previous research (n=2), and modified from previous research (n=3). Five studies used Likert scales, most commonly a 5-point scale. Only six studies reported question items in the knowledge measurement, with question items ranging from 11 to 13 items. One study did not report a validity test, and others used face validity (n=4), content validity (n=4), face and content validity (n=2). Additionally, four studies did not report reliability tests. A total of eight studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.81 to 0.92. In order to assess knowledge, most instruments asked the nurses to self-rate their level of knowledge on T&CM modalities (n=9), followed by their level of familiarity with T&CM modalities and how easy it is to obtain information about those modalities (n=1), with training primarily focusing on T&CM modalities (n=1).
Nurses' beliefs about T&CM
A total of four studies measured nurses' beliefs about T&CM [35, 39-41]. These studies used instruments modified from previous research (n=3) and self-designed (n=1). Two studies reported question items on belief measurement, with 7 and 13 items. Only one study reported a validity test from previous research using Criterion and congruent validity (Complementary and Alternative Medicines and Beliefs Inventory (CAMBI) by Bishop et al. [42]). Only one study reported a reliability test using Internal Consistency with Cronbach's α: 0.75. To assess beliefs, the questions in the instrument are nurses' beliefs regarding T&CM (n=2), the nurses' confidence in T&CM (n=1), and about the effectiveness of the T&CM modalities (n=1).
Practice and use of T&CM
A total of 13 studies measured the practice and use of T&CM among nurses [26, 27, 30, 31, 33-35, 38-40, 43]. Most studies (n=6) used self-designed instruments, followed by modified instruments (n=3), and then adapted NrCAM K&A (n=2). Most studies used frequency response options for T&CM use among nurses. Seven studies reported question items on practice measurement, with question items ranging from 4 to 18 items. One study did not report a validity test, while others used face validity (n=6), content validity (n=2), face validity and content validity (n=2). Additionally, six studies did not report reliability tests. A total of five studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.67 to 0.92. To measure the practices and use of T&CM, the instrument asked about the nurses' self-rated frequency of practice on T&CM modalities (n=7), self-rating regarding CAM-related nursing practice (n=1), personal and professional use and perceived barriers to T&CM use in practice (n=1), experience using T&C modalities (n=1), active nursing practice regarding T&CM and perceived barriers (n=1), the effects of T&CM, T&CM practice, and T&CM utilization that have been experienced (n=1), and experience in the use and referral of modalities of T&CM (n=1).
Communication of T&CM
A total of three studies measured communication and the use of T&CM among nurses [28, 32, 44]. All studies used self-designed instruments and Likert scales (4, 5, and 7-point scales). Two studies reported question items on communication measurement, with 5 question items. All studies reported validity tests with face validity (n=1), face and content validity (n=1), and face, content and construct validity (n=1). Additionally, one study did not report a reliability test. A total of two studies reported reliability tests, both using Internal Consistency with Cronbach's α values of 0.88 and 0.91. The instrument includes questions about nurses initiating T&CM discussions with patients and communicating with the healthcare team about the patient's disclosure of T&CM use (n=1), along with a competency scale for discussing T&CM with patients (n=1). To measure communication, the instruments used inquire about nurses' initiation of T&CM discussions with patients and communication with the healthcare team regarding patients' disclosure of T&CM use (n=1), as well as a competence scale for communicating about T&CM with patients (n=1).
Discussion
From the 18 studies identified, the measuring tools used to evaluate nurses in T&CM consisted of domains such as knowledge, attitude, beliefs, practice, and communication. The diversity of domains assessed indicated that T&CM is a broad and continually evolving theme across various countries. The study came from all the continents from 12 countries; Japan, Iran, United States, Australia, Turkey, China, Israel, South Korea, Lebanon, Netherlands, Sweden, and Ghana. Studies on this topic is conducted in several nations, considering the implementation of Traditional and Complementary Medicine (T&CM) based on country-specific WHO data, which may vary between regions [2]. This underscored the relevance and importance of this theme.
Most studies were conducted in Asia (55.6%). This is based on the fact that T&CM was initially used empirically and developed in every culture or tribe [2]. This is related to the fact that continents with strong traditions, biodiversity, local knowledge, as well as regulatory support and research publications are mainly found in Asia [45, 46]. Recent research has demonstrated the increasing integration of T&CM into healthcare systems throughout Asia, which supports this trend [47]. Nevertheless, the limited representation of Africa (5.5%) indicated a necessity for additional research in this region, particularly considering the pervasive use of traditional medicine in numerous African countries [48].
The prevalence of self-developed instruments (61.1%) in the reviewed studies raised questions about the comparability and standardization of measurements across different contexts. Recent literature on healthcare measurement tools has highlighted this issue [49]. The absence of standardized, validated instruments tailored to nurses' experiences with T&CM represented a significant gap in the field. We identified only two questionnaires specifically applied to nurses: NrCAM K&A by Rojas-Cooley & Grant [37], assess Attitudes towards Patient's Use of TCM (APUTCM) and to measure a Communicative Competence in TCM (CCTCM) [28].
These instruments were developed considering that evaluating nurses' knowledge, attitude, and communication in T&CM will assist nurses in their self-development to meet the diverse cultural needs of patient populations. Instrument content, particularly those measuring attitudes and knowledge, tends to focus on self-rated familiarity with T&CM modalities. While this approach provided insight into nurses' perceived competence, it may not accurately reflect their actual knowledge or skills. The objective measurement of T&CM knowledge among healthcare providers often differs from the self-reported measures [17].
This review identified that most instruments have been validated, although face validity was commonly used. Face validity is not considered strong evidence of validity, but it can be useful when combined with other types of validity [50]. There were studies that only conducted a validity test on the instruments used, while others combined it with content, construct, criterion, congruent validity. When choosing an instrument, content validity is regarded as the most crucial measuring quality to take into account [51]. If the content of an instrument accurately represents a construct, then the instrument is more likely to successfully achieve its measuring goals [50]. However, it is important or better to perform validity from various types, such as content, construct, and criterion validity [52].
Valid, reliable, and acceptable tools are necessary for registered nurses working in healthcare services [53]. In this review, compared to validity tests (n=1), more studies did not report reliability tests (n=7). For reliability, most studies calculated the internal consistency through Cronbach’s alpha, with values ranging from 0.67 to 0.92. The most important form of reliability for multi-item instruments is the internal consistency of the instrument, and the internal consistency of scales is measured with Cronbach's alpha, which ranges from 0 to 1, with optimal values ranging from 0.7 to 0.9 [52]. Most of the studies used a design that appears to combine several instruments to examine various variables in nurses in T&CM. When modifying an instrument or combining instruments in a study, the original validity and reliability may not apply to the new instrument, making it important to establish validity and reliability during the upcoming analysis [50, 52].
To our knowledge, there has not yet been a scoping review focused on instruments with the theme of T&CM specifically among nurses. This review has identified studies globally involving nurse samples. Regarding constraints, T&CM covers a very broad scope, and the use of the term T&CM varies from one language to another and even from one region to another. Utilizing other databases, adjusting the time window, or selecting different languages may result in the discovery of more tools.
Conclusion
The instruments used to measure nurses' attitudes, knowledge, beliefs, practices, and communication regarding T&CM are primarily self-developed or adapted from previous research, with varied reliability and validity testing. Most studies focused on assessing attitudes and knowledge, while fewer addressed beliefs or communication.
Acknowledgments: The authors much appreciated the facilities and resources provided by the Faculty of Nursing, Hasanuddin University.
Ethical Permissions: There is nothing to be declared.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Nurmila W (First Author), Introduction Writer/Original Researcher (60%); Erika KA (Second Author), Methodologist/Assistant Researcher/Discussion Writer (20%); Erina E (Third Author), Assistant Researcher/Discussion Writer (20%)
Funding/Support: This research did not receive any financial support.
The concept of traditional, complementary, alternative, and integrative medicines is often used in healthcare delivery. The term "traditional medicine" (TM) is used in healthcare practices that have evolved over generations within a country, while "complementary medicine" (CM) or alternative is interchangeably used by some countries that do not include these practices in their national tradition [1]. Further, WHO defines traditional and complementary medicine (T&CM) as a combination of TM and CM, including products, practices, and practitioners [1].
Various countries have started to pay attention to the use of T&CM. According to the global report on T&CM in 2019, 98% of WHO member countries have policies related to T&CM [2]. The prevalence of T&CM use varies from 24-71.3% in the general population [3] and shows increased usage among children [4], adults [5], and the elderly [6]. These practices are used for various physical and psychological health issues [7, 8]. T&CM is considered holistic, and expectations of benefits are the main reasons for its use, although the scientific evidence remains debated [9].
The ongoing conflict between modern medicine and T&CM often shows that both can coexist, although modern medicine does not always support T&CM [10]. Doctors and nurses believe that combining complementary and conventional cancer treatments is risky [11]. Nurses, who have a fundamental responsibility to provide holistic care to a diverse patient population, need to be aware of T&CM [12]. A study showed that nurses are more familiar with and have more positive attitudes and beliefs toward T&CM, believing it has a more significant impact on patient care compared to other healthcare workers [13]. Nurses must be able to consider and provide information about T&CM in delivering patient care [14]. Nurses use a cultural perspective in their practice, since transcultural nursing contributes to the establishment and adaptation of healthy family units [15]. Specifically, nurses should be encouraged to learn more about the cultural needs of a diverse patient population and provide consistent care, thus evaluating nurses' experiences with T&CM is necessary.
Previous studies have reviewed how the practice of T&CM among nurses has been conducted in various countries [16, 17]. Furthermore, information about the instruments used is needed. Quality instruments play a crucial role in assessing nurses' experiences with multi-professional care that involves a holistic approach [18]. The assessment of T&CM use among nurses in many parts of the world has been addressed in earlier studies, but an important aspect of these studies remains unexplored. Quality instruments remain necessary in measuring how nurses deal with T&CM if any, while providing multi-professional, holistic, primary health care. However, as of now, there have been no comprehensive reviews of these instruments documented in the literature. It is important to bring greater attention to this omission since the use of Traditional and Complementary Medicine (T&CM) is growing globally, leading to an increased need for transcultural nursing care.
Medical policies and nursing management need excellent instruments in the collection of trustable data concerning nurses’ experiences of working with T&CM. This is necessary in assessing the current practices, developmental needs, and improving techniques that would strengthen transcultural nursing skills. In the absence of such understanding, it is always very difficult, if not impossible, to make appropriate clinical decisions regarding T&CM incorporation in clinicians’ education and practice and about the education of nursing such policies. Therefore, this scope review aims to provide an overview of the instruments used in recent research. These tools will be filtered and examined to inform researchers, educators, and health authorities as part of their considerations for the development of nursing in the field of T&CM.
Information and Methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-SCR) guidelines to enhance reporting quality and ensure fidelity in the review process [19]. The review used the Scoping Review Framework, which includes five stages; 1) identifying the research question, 2) identifying relevant studies, 3) study selection, 4) charting the data, and 5) collating, summarizing, and reporting the results [20].
Review question (stage 1)
The goals and questions of the scoping review were based on the Population, Concept, and Context (PCC) framework [21]. Furthermore, PCC is used in search keywords. The search keywords were: Population: Nurses OR nursing professionals OR clinical nurses; Concept: Assessment tool OR instrument OR scale OR questionnaire OR survey; And Context: Complementary therapy OR alternative medicine OR integrative healthcare or CAM OR complementary alternative medicine OR TCM OR traditional complementary medicine. The review question based on the PCC framework was: What is known from the literature about the assessment instruments used in evaluating the experience in T&CM among nurses? What domains are assessed by these instruments? Have the instruments been validated?
Identifying relevant studies (stage 2)
A comprehensive literature search was conducted in March 2024 on six databases: PubMed, ScienceDirect, DOAJ, Taylor & Francis, Wiley, and GARUDA (provides integrated access to institutional repositories, scholarly journals, theses, and diverse academic literature resources from Indonesia). In addition, we checked the citations of the studies and reviews that were included and conducted a manual search. All articles that conducted research using questionnaires on nurse populations to measure their views on T&CM were considered. Inclusion criteria were articles published within the last ten years (2014-2024), original papers, and full-text available. Exclusion criteria included non-English articles, theses, review articles, commentaries, conceptual, qualitative, and case studies. The article selection process followed the PRISMA checklist guidelines to enhance accuracy in article search [22].
Study selection (stage 3)
The PRISMA flowchart depicts the process, screening outcomes, and criteria for articles extraction following the initial search, which adhered to the study's inclusion and exclusion criteria (Figure 1). The abstracts found during the article search were retrieved using the reference manager software Mendeley and then transferred to the Rayyan software program to facilitate and record the article screening process [23]. In total, 400 pertinent abstracts were gathered from the 7 databases, and an additional 15 manuscripts identified by reference. After eliminating duplicates and articles published more than 10 years ago, 192 articles were retained. Articles were then screened, eliminating 382 articles, and 18 articles were included and deemed suitable for review.
Charting the data (stage 4)
This review utilized recommendations from The Joanna Briggs Institute for the extraction, analysis, and presentation of results in scoping reviews [24]. The data were extracted to incorporate crucial details such as the study site, research design, sample size, and the instruments used in the study.
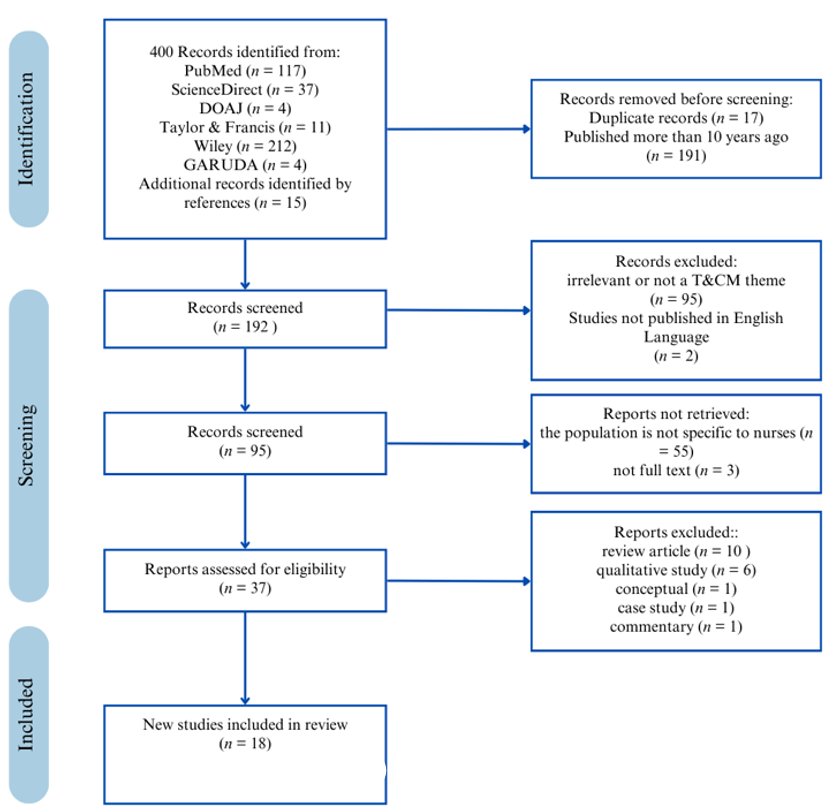
Figure 1. PRISMA flowcharts for study selection and inclusion
Findings
Characteristics of the studies
This review found that the majority of articles were conducted in Asia (55.6%), followed by the Americas (16.7%), then Europe (11.11%), Australia (11.11%), and Africa (5.5%). Most (15 studies) used a survey design, only one study employed instrument development, and two studies used a descriptive design. Most studies were implemented in hospitals (n=11) and 7 others in various settings. The average sample size was 354 nurses. The used sampling methods included convenience sampling (n=13), purposive sampling (n=2), simple random sampling (n=2), and total sampling (n=1; Table 1).
Table 1. Extracted data from the final documents
Description of the instruments
Most of the studies (n=11) used instruments self-developed by researchers, five parts of the study instruments adopted from previous research, while the rest were adapted from earlier studies. Each instrument along with the attributes being measured. Most instruments evaluated nurses' attitudes towards T&CM (n=12), knowledge (n=11), and practices (n=11), while relatively few assessed beliefs (n=4) and communication (n=3; Table 2).
Table 2. Instruments from included studies classified by TCM attribute among nurses
Nurses' attitudes towards T&CM
12 out of 18 studies measured nurses' attitudes toward T&CM [25-36]. These studies used self-designed instruments (n=8), adaptations of the same instrument, namely The Complementary and Alternative Medicine Health Belief Questionnaire (CHBQ-CAM; n=2), adoption from previous research (n=2), and the Nurse Complementary and Alternative Medicine Knowledge and Attitude (NrCAM K&A) developed by Rojas-Cooley & Grant [37] (n=1). Most studies (n=11) used Likert scales, predominantly a 5-point scale. Eight studies reported question items on attitude measurement, with question items ranging from 6 to 22 items. One study did not report a validity test, while others used face validity (n=3), content validity (n=4), face validity and content validity (n=3), face, content and construct validity (n=1), and criterion validity (n=1). Additionally, five studies did not report reliability tests. A total of eight studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.70 to 0.92. Most of the instruments inquired about the effects of T&CM modalities (n=4), followed by items questioning attitudes towards T&CM (n=3), the potential implementation of T&CM within their organizations (n=1), beliefs and practices (n=1), and aspects of cognitive, affective, and behavioral components (n=1).
Nurses' knowledge of T&CM
Out of 18 studies, 11 measured nurses' knowledge of T&CM [25-27, 29, 31-34, 38-40]. Instruments used in these studies were self-designed (n=6), adopted from previous research (n=2), and modified from previous research (n=3). Five studies used Likert scales, most commonly a 5-point scale. Only six studies reported question items in the knowledge measurement, with question items ranging from 11 to 13 items. One study did not report a validity test, and others used face validity (n=4), content validity (n=4), face and content validity (n=2). Additionally, four studies did not report reliability tests. A total of eight studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.81 to 0.92. In order to assess knowledge, most instruments asked the nurses to self-rate their level of knowledge on T&CM modalities (n=9), followed by their level of familiarity with T&CM modalities and how easy it is to obtain information about those modalities (n=1), with training primarily focusing on T&CM modalities (n=1).
Nurses' beliefs about T&CM
A total of four studies measured nurses' beliefs about T&CM [35, 39-41]. These studies used instruments modified from previous research (n=3) and self-designed (n=1). Two studies reported question items on belief measurement, with 7 and 13 items. Only one study reported a validity test from previous research using Criterion and congruent validity (Complementary and Alternative Medicines and Beliefs Inventory (CAMBI) by Bishop et al. [42]). Only one study reported a reliability test using Internal Consistency with Cronbach's α: 0.75. To assess beliefs, the questions in the instrument are nurses' beliefs regarding T&CM (n=2), the nurses' confidence in T&CM (n=1), and about the effectiveness of the T&CM modalities (n=1).
Practice and use of T&CM
A total of 13 studies measured the practice and use of T&CM among nurses [26, 27, 30, 31, 33-35, 38-40, 43]. Most studies (n=6) used self-designed instruments, followed by modified instruments (n=3), and then adapted NrCAM K&A (n=2). Most studies used frequency response options for T&CM use among nurses. Seven studies reported question items on practice measurement, with question items ranging from 4 to 18 items. One study did not report a validity test, while others used face validity (n=6), content validity (n=2), face validity and content validity (n=2). Additionally, six studies did not report reliability tests. A total of five studies reported reliability tests, all using Internal Consistency with Cronbach's α values ranging from 0.67 to 0.92. To measure the practices and use of T&CM, the instrument asked about the nurses' self-rated frequency of practice on T&CM modalities (n=7), self-rating regarding CAM-related nursing practice (n=1), personal and professional use and perceived barriers to T&CM use in practice (n=1), experience using T&C modalities (n=1), active nursing practice regarding T&CM and perceived barriers (n=1), the effects of T&CM, T&CM practice, and T&CM utilization that have been experienced (n=1), and experience in the use and referral of modalities of T&CM (n=1).
Communication of T&CM
A total of three studies measured communication and the use of T&CM among nurses [28, 32, 44]. All studies used self-designed instruments and Likert scales (4, 5, and 7-point scales). Two studies reported question items on communication measurement, with 5 question items. All studies reported validity tests with face validity (n=1), face and content validity (n=1), and face, content and construct validity (n=1). Additionally, one study did not report a reliability test. A total of two studies reported reliability tests, both using Internal Consistency with Cronbach's α values of 0.88 and 0.91. The instrument includes questions about nurses initiating T&CM discussions with patients and communicating with the healthcare team about the patient's disclosure of T&CM use (n=1), along with a competency scale for discussing T&CM with patients (n=1). To measure communication, the instruments used inquire about nurses' initiation of T&CM discussions with patients and communication with the healthcare team regarding patients' disclosure of T&CM use (n=1), as well as a competence scale for communicating about T&CM with patients (n=1).
Discussion
From the 18 studies identified, the measuring tools used to evaluate nurses in T&CM consisted of domains such as knowledge, attitude, beliefs, practice, and communication. The diversity of domains assessed indicated that T&CM is a broad and continually evolving theme across various countries. The study came from all the continents from 12 countries; Japan, Iran, United States, Australia, Turkey, China, Israel, South Korea, Lebanon, Netherlands, Sweden, and Ghana. Studies on this topic is conducted in several nations, considering the implementation of Traditional and Complementary Medicine (T&CM) based on country-specific WHO data, which may vary between regions [2]. This underscored the relevance and importance of this theme.
Most studies were conducted in Asia (55.6%). This is based on the fact that T&CM was initially used empirically and developed in every culture or tribe [2]. This is related to the fact that continents with strong traditions, biodiversity, local knowledge, as well as regulatory support and research publications are mainly found in Asia [45, 46]. Recent research has demonstrated the increasing integration of T&CM into healthcare systems throughout Asia, which supports this trend [47]. Nevertheless, the limited representation of Africa (5.5%) indicated a necessity for additional research in this region, particularly considering the pervasive use of traditional medicine in numerous African countries [48].
The prevalence of self-developed instruments (61.1%) in the reviewed studies raised questions about the comparability and standardization of measurements across different contexts. Recent literature on healthcare measurement tools has highlighted this issue [49]. The absence of standardized, validated instruments tailored to nurses' experiences with T&CM represented a significant gap in the field. We identified only two questionnaires specifically applied to nurses: NrCAM K&A by Rojas-Cooley & Grant [37], assess Attitudes towards Patient's Use of TCM (APUTCM) and to measure a Communicative Competence in TCM (CCTCM) [28].
These instruments were developed considering that evaluating nurses' knowledge, attitude, and communication in T&CM will assist nurses in their self-development to meet the diverse cultural needs of patient populations. Instrument content, particularly those measuring attitudes and knowledge, tends to focus on self-rated familiarity with T&CM modalities. While this approach provided insight into nurses' perceived competence, it may not accurately reflect their actual knowledge or skills. The objective measurement of T&CM knowledge among healthcare providers often differs from the self-reported measures [17].
This review identified that most instruments have been validated, although face validity was commonly used. Face validity is not considered strong evidence of validity, but it can be useful when combined with other types of validity [50]. There were studies that only conducted a validity test on the instruments used, while others combined it with content, construct, criterion, congruent validity. When choosing an instrument, content validity is regarded as the most crucial measuring quality to take into account [51]. If the content of an instrument accurately represents a construct, then the instrument is more likely to successfully achieve its measuring goals [50]. However, it is important or better to perform validity from various types, such as content, construct, and criterion validity [52].
Valid, reliable, and acceptable tools are necessary for registered nurses working in healthcare services [53]. In this review, compared to validity tests (n=1), more studies did not report reliability tests (n=7). For reliability, most studies calculated the internal consistency through Cronbach’s alpha, with values ranging from 0.67 to 0.92. The most important form of reliability for multi-item instruments is the internal consistency of the instrument, and the internal consistency of scales is measured with Cronbach's alpha, which ranges from 0 to 1, with optimal values ranging from 0.7 to 0.9 [52]. Most of the studies used a design that appears to combine several instruments to examine various variables in nurses in T&CM. When modifying an instrument or combining instruments in a study, the original validity and reliability may not apply to the new instrument, making it important to establish validity and reliability during the upcoming analysis [50, 52].
To our knowledge, there has not yet been a scoping review focused on instruments with the theme of T&CM specifically among nurses. This review has identified studies globally involving nurse samples. Regarding constraints, T&CM covers a very broad scope, and the use of the term T&CM varies from one language to another and even from one region to another. Utilizing other databases, adjusting the time window, or selecting different languages may result in the discovery of more tools.
Conclusion
The instruments used to measure nurses' attitudes, knowledge, beliefs, practices, and communication regarding T&CM are primarily self-developed or adapted from previous research, with varied reliability and validity testing. Most studies focused on assessing attitudes and knowledge, while fewer addressed beliefs or communication.
Acknowledgments: The authors much appreciated the facilities and resources provided by the Faculty of Nursing, Hasanuddin University.
Ethical Permissions: There is nothing to be declared.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Nurmila W (First Author), Introduction Writer/Original Researcher (60%); Erika KA (Second Author), Methodologist/Assistant Researcher/Discussion Writer (20%); Erina E (Third Author), Assistant Researcher/Discussion Writer (20%)
Funding/Support: This research did not receive any financial support.
Article Type: Systematic Review |
Subject:
Health Care
Received: 2024/06/4 | Accepted: 2024/09/7 | Published: 2024/10/12
Received: 2024/06/4 | Accepted: 2024/09/7 | Published: 2024/10/12
References
1. WHO. WHO traditional medicine strategy: 2014-2023. Geneva: World Health Organization; 2013. [Link]
2. WHO. WHO global report on traditional and complementary medicine 2019. Geneva: World Health Organization; 2019. [Link]
3. Lee EL, Richards N, Harrison J, Barnes J. Prevalence of use of traditional, complementary and alternative medicine by the general population: A systematic review of national studies published from 2010 to 2019. Drug Saf. 2022;45(7):713-35. [Link] [DOI:10.1007/s40264-022-01189-w]
4. Alsabri M, Carfagnini C, Amin M, Castilo F, Lewis J, Ashkar M, et al. Complementary and alternative medicine for children with sickle cell disease: A systematic review. Blood Rev. 2023;59:101052. [Link] [DOI:10.1016/j.blre.2023.101052]
5. Mwaka AD, Abbo C, Kinengyere AA. Traditional and complementary medicine use among adult cancer patients undergoing conventional treatment in Sub-Saharan Africa: A scoping review on the use, safety and risks. Cancer Manag Res. 2020;12:3699-712. [Link] [DOI:10.2147/CMAR.S251975]
6. Zhao S, Otieno F, Akpan A, Moots RJ. Complementary and alternative medicine use in rheumatoid arthritis: Considerations for the pharmacological management of elderly patients. Drugs Aging. 2017;34(4):255-64. [Link] [DOI:10.1007/s40266-017-0443-0]
7. Thomson P, Jones J, Evans JM, Leslie SL. Factors influencing the use of complementary and alternative medicine and whether patients inform their primary care physician. Complement Ther Med. 2012;20(1-2):45-53. [Link] [DOI:10.1016/j.ctim.2011.10.001]
8. Wemrell M, Olsson A, Landgren K. The use of complementary and alternative medicine (CAM) in psychiatric units in Sweden. Issues Ment Health Nurs. 2020;41(10):946-57. [Link] [DOI:10.1080/01612840.2020.1744203]
9. Tangkiatkumjai M, Boardman H, Walker DM. Potential factors that influence usage of complementary and alternative medicine worldwide: A systematic review. BMC Complement Med Ther. 2020;20(1):363. [Link] [DOI:10.1186/s12906-020-03157-2]
10. Gunaydin N, Ozpulat F. The role of nurses in traditional-modern medicine conflict. New Trends Issues Proc Adv Pure Appl Sci. 2018;(10):110-3. [Link] [DOI:10.18844/gjpaas.v0i10.3751]
11. Stub T, Quandt SA, Arcury TA, Sandberg JC, Kristoffersen AE. Attitudes and knowledge about direct and indirect risks among conventional and complementary health care providers in cancer care. BMC Complement Altern Med. 2018;18(1):44. [Link] [DOI:10.1186/s12906-018-2106-z]
12. Bengre A. Transcultural nursing: Cultural competence in nurses. Int J Nurs Educ. 2012;4(1). [Link]
13. Casbarro N, Ezomo O, Woolley K, Smith R, Hardin C, Feinn R, et al. Complementary and integrative medicine: An observational study on pediatric clinicians' knowledge, beliefs and practices. Complement Ther Med. 2021;58:102693. [Link] [DOI:10.1016/j.ctim.2021.102693]
14. Schulenburg J. Considerations for complementary and alternative interventions for pain. AORN J. 2015;101(3):319-26. [Link] [DOI:10.1016/j.aorn.2015.01.013]
15. Erika KA. The effect of transcultural nursing, child healthcare model and transtheoretical model approaches to knowledge and culture of family. Jurnal Ners. 2016;9(2):262-9. [Link] [DOI:10.20473/jn.v9i2.2572]
16. Chang HY, Chang HL. A review of nurses' knowledge, attitudes, and ability to communicate the risks and benefits of complementary and alternative medicine. J Clin Nurs. 2015;24(11-12):1466-78. [Link] [DOI:10.1111/jocn.12790]
17. Hall H, Leach M, Brosnan C, Collins M. Nurses' attitudes towards complementary therapies: A systematic review and meta-synthesis. Int J Nurs Stud. 2017;69:47-56. [Link] [DOI:10.1016/j.ijnurstu.2017.01.008]
18. Glarcher M, Schumacher P, Fritz E. Care quality instruments. Int J Health Care Qual Assur. 2015;28(5):532-59. [Link] [DOI:10.1108/IJHCQA-01-2015-0010]
19. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467-73. [Link] [DOI:10.7326/M18-0850]
20. Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19-32. [Link] [DOI:10.1080/1364557032000119616]
21. Peters MDJ, Godfrey C, McInerney P, Khalil H, Larsen P, Marnie C, et al. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid Synth. 2022;20(4):953-68. [Link] [DOI:10.11124/JBIES-21-00242]
22. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [Link] [DOI:10.1136/bmj.n71]
23. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. [Link] [DOI:10.1186/s13643-016-0384-4]
24. Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC, et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. 2023;21(3):520-32. [Link] [DOI:10.11124/JBIES-22-00123]
25. Dehghan M, Namjoo Z, Jafari M, Kordestani G, Tabebordbar N, Payam F, et al. Iranian nurses' knowledge and attitude toward complementary and alternative medicines: Is there any relation with quality of nursing care?. Front Public Health. 2022;10:942354. [Link] [DOI:10.3389/fpubh.2022.942354]
26. Makarem NN, Brome D, Romani M. Knowledge, attitude, and practices of complementary and alternative medicine: A survey of physicians and nurses at an academic medical center in Beirut. Libyan J Med. 2022;17(1):2071813. [Link] [DOI:10.1080/19932820.2022.2071813]
27. Zeighami M, Soltani-Nejad S. Knowledge, attitude, and practice of complementary and alternative medicine: A survey of Iranian nurses. J Res Nurs. 2020;25(4):380-8. [Link] [DOI:10.1177/1744987120925852]
28. Chang HY, Lo CL, Hung YY. Development and validation of traditional & complementary medicine (TCM) scales for nurses: Using structural equation modelling (SEM). BMC Complement Altern Med. 2019;19(1):321. [Link] [DOI:10.1186/s12906-019-2733-z]
29. Metin ZG, Izgu N, Karadas C, Donmez AA. Perspectives of oncology nurses on complementary and alternative medicine in Turkey: A cross-sectional survey. Holist Nurs Pract. 2018;32(2):107-13. [Link] [DOI:10.1097/HNP.0000000000000256]
30. Cırık V, Efe E. Pediatric nurses' usage and experience toward complementary health approaches. J Altern Complement Med. 2018;24(11):1120-7. [Link] [DOI:10.1089/acm.2018.0075]
31. Gyasi RM, Abass K, Adu-Gyamfi S, Accam BT, Nyamadi VM. The capabilities of nurses for complementary and traditional medicine integration in Africa. J Altern Complement Med. 2018;24(3):282-90. [Link] [DOI:10.1089/acm.2017.0133]
32. Hall H, Leach MJ, Brosnan C, Cant R, Collins M. Registered nurses' communication about patients' use of complementary therapies: A national survey. Patient Educ Couns. 2018;101(8):1403-9. [Link] [DOI:10.1016/j.pec.2018.03.010]
33. Shorofi SA, Arbon P. Complementary and alternative medicine (CAM) among Australian hospital-based nurses: Knowledge, attitude, personal and professional use, reasons for use, CAM referrals, and socio-demographic predictors of CAM users. Complement Ther Clin Pract. 2017;27:37-45. [Link] [DOI:10.1016/j.ctcp.2017.03.001]
34. Balouchi A, Rahnama M, Hastings-Tolsma M, Shoja MM, Bolaydehyi E. Knowledge, attitude and use of complementary and integrative health strategies: A preliminary survey of Iranian nurses. J Integr Med. 2016;14(2):121-7. [Link] [DOI:10.1016/S2095-4964(16)60245-5]
35. Van Vliet M, Jong M, Busch M, Meijer JEM, Von Rosenstiel IA, Jong MC. Attitudes, beliefs, and practices of integrative medicine among nurses in the Netherlands. J Holist Nurs. 2015;33(2):110-21. [Link] [DOI:10.1177/0898010114555339]
36. Orkaby B, Greenberger C. Israeli nurses' attitudes to the holistic approach to health and their use of complementary and alternative therapies. J Holist Nurs. 2015;33(1):19-26. [Link] [DOI:10.1177/0898010114542876]
37. Rojas-Cooley MT, Grant M. Complementary and alternative medicine: Oncology nurses' knowledge and attitudes. Oncol Nurs Forum. 2009;36(2):217-24. [Link] [DOI:10.1188/09.ONF.217-224]
38. Kim S, Lee MN, Lee S. Nurses' knowledge, perceived barriers, and practices regarding complementary and alternative medicine in South Korea. Holist Nurs Pract. 2016;30(6):338-44. [Link] [DOI:10.1097/HNP.0000000000000176]
39. Jong M, Lundqvist V, Jong MC. A cross-sectional study on Swedish licensed nurses' use, practice, perception and knowledge about complementary and alternative medicine. Scand J Caring Sci. 2015;29(4):642-50. [Link] [DOI:10.1111/scs.12192]
40. Geisler C, Cheung C, Johnson Steinhagen S, Neubeck P, Brueggeman AD. Nurse practitioner knowledge, use, and referral of complementary/alternative therapies. J Am Assoc Nurse Pract. 2015;27(7):380-8. [Link] [DOI:10.1002/2327-6924.12190]
41. Brewer NJ, Turrise SL, Kim-Godwin YS, Pond RS. Nurses' knowledge and treatment beliefs: Use of complementary and alternative medicine for pain management. J Holist Nurs. 2019;37(3):248-59. [Link] [DOI:10.1177/0898010118822212]
42. Bishop FL, Yardley L, Lewith G. Developing a measure of treatment beliefs: The complementary and alternative medicine beliefs inventory. Complement Ther Med. 2005;13(2):144-9. [Link] [DOI:10.1016/j.ctim.2005.01.005]
43. Siedlecki SL. Complementary and alternative therapies (CAT) in academic programs and nursing practice: Is more education is needed?. Complement Ther Clin Pract. 2021;43:101327. [Link] [DOI:10.1016/j.ctcp.2021.101327]
44. Kusunoki J, Ikezaki S, Majima T. Factors associated with nursing practice for cancer patients using complementary and alternative medicine. Collegian. 2023;30(5):668-75. [Link] [DOI:10.1016/j.colegn.2023.08.001]
45. WHO. Traditional medicine in the WHO South-East Asia region: Review of progress 2014-2019. Geneva: World Health Organization; 2020. [Link]
46. Guo DA. Surging cooperation with ASEAN countries on traditional medicine. Chin Herb Med. 2021;13(4):439-40. [Link] [DOI:10.1016/j.chmed.2021.09.007]
47. Park YL, Canaway R. Integrating traditional and complementary medicine with national healthcare systems for universal health coverage in Asia and the western pacific. Health Syst Reform. 2019;5(1):24-31. [Link] [DOI:10.1080/23288604.2018.1539058]
48. James PB, Wardle J, Steel A, Adams J. Traditional, complementary and alternative medicine use in Sub-Saharan Africa: A systematic review. BMJ Glob Health. 2018;3(5):e000895. [Link] [DOI:10.1136/bmjgh-2018-000895]
49. Alqudimat MR, Toupin April K, Hundert A, Jibb L, Victor C, Nathan PC, et al. Questionnaires assessing the use of complementary health approaches in pediatrics and their measurement properties: A systematic review. Complement Ther Med. 2020;53:102520. [Link] [DOI:10.1016/j.ctim.2020.102520]
50. Polit DF, Beck CT. Nursing research: Generating and assessing evidence for nursing practice. 11th ed. Philadelphia: Wolters Kluwer; 2021. [Link]
51. Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: A Delphi study. Qual Life Res. 2018;27(5):1159-70. [Link] [DOI:10.1007/s11136-018-1829-0]
52. Creswell JW, Creswell JD. Research design: Qualitative, quantitative, and mixed methods approaches. 5th ed. Washington DC: SAGE Publications; 2018. [Link]
53. Belita E, Fisher K, Yost J, Squires JE, Ganann R, Dobbins M. Validity, reliability, and acceptability of the evidence-informed decision-making (EIDM) competence measure. PLoS One. 2022;17(8):e0272699. [Link] [DOI:10.1371/journal.pone.0272699]
54. Osmancevic S, Schoberer D, Lohrmann C, Großschädl F. Psychometric properties of instruments used to measure the cultural competence of nurses: A systematic review. Int J Nurs Stud. 2021;113:103789. [Link] [DOI:10.1016/j.ijnurstu.2020.103789]
55. Kurniati D, Adi Nugroho T, Yeni Wulandari R, Kurniawan M. The relationship of knowledge and role of nurse in management with hypertension patients. Idea Nurs J. 2024;3(1). [Link] [DOI:10.53690/inj.v3i01.212]
56. Amir H, Permatananda PANK, Cahyani DD, Langelo W, Rosita R, Sajodin S, et al. Enhancing skill conceptualization, critical thinking, and nursing knowledge through reflective case discussions: A systematic review. J Med Life. 2023;16(6):851-5. [Link] [DOI:10.25122/jml-2023-0042]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |