Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 407-413 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ezalina E, Alfianur A. Correlation between Social Capital and Loneliness in Older Adults in Pekanbaru, Indonesia. Health Educ Health Promot 2024; 12 (3) :407-413
URL: http://hehp.modares.ac.ir/article-5-75346-en.html
URL: http://hehp.modares.ac.ir/article-5-75346-en.html
E. Ezalina *1, A. Alfianur1
1- Department of Nursing, Institute of Health Science Payung Negeri, Pekanbaru, Indonesia
Full-Text [PDF 599 kb]
(2668 Downloads)
| Abstract (HTML) (1098 Views)
Full-Text: (217 Views)
Introduction
Loneliness, a significant concern for mental well-being, is especially prevalent among older individuals and arises from exposure to numerous aging-related factors [1]. This emotional condition entails sensations such as unease, sadness, emptiness, distress, isolation, a sense of purposelessness, disconnection, and a lack of social ties [2-4]. Previous studies suggest that unmet social needs, whether in terms of the quantity or quality of relationships, may contribute to the experience of loneliness [5]. Loneliness can manifest differently among older adults, with experiences ranging from deliberate social isolation due to trauma to feelings of abandonment and emotional suffering caused by being confined to a care home [6].
When loneliness becomes severe and prolonged, it poses risks to both physical and mental well-being. A thorough examination revealed that loneliness is significantly related to conditions such as heart disease, hypertension, stroke, and lung disease [7]. In addition to these illnesses, loneliness affects various other aspects of health, including reduced physical abilities, disruptions in sleep patterns, and decreased sleep quality [8, 9]. Loneliness is also associated with negative mental health consequences, such as increased psychological distress, anxiety, depression, a decline in cognitive function, and dementia [10-12]. Furthermore, loneliness significantly increases the chances of suicide and is correlated with a higher risk of mortality [13-15].
Being a fundamental aspect of quality of life, social engagement has traditionally been linked to favorable physical and psychological effects among older adults in the broader population [16]. Sustained engagement in various activities enhances the overall well-being of older individuals in the later stages of life, contributing to their attainment of successful aging [17]. Studies indicate a correlation between social involvement and reduced levels of depression, even after accounting for parameters, such as demographics, health status, and participation in physical activities among older adults living in the community [18, 19].
Research indicates that practicing leisure activities and maintaining social engagement can help older adults preserve cognitive function, physical function, and mental health, thereby contributing to successful aging [20]. Older adults who sustain engagement in socially productive activities report greater personal satisfaction and well-being [21]. Furthermore, sustained engagement in activities, such as enhanced activities of daily living (EADLs) is critical for quality of life and health outcomes in older individuals [22].
Lack of social engagement can indeed contribute to loneliness and social isolation [23]. Social isolation refers to the objective absence of social contact, while loneliness is the subjective feeling of being alone [24]. Although social isolation is strongly associated with loneliness, the relationship between the two is not straightforward [25]. Factors, such as social relationships, community engagement, and leisure activities play a crucial role in social integration, affecting the multidimensional individual, societal, and environmental aspects [26].
Life transitions, retirement, loss of significant others, and reduced mobility can collectively place older adults at a higher risk of experiencing loneliness and social isolation, impacting their health service use and associated costs [27]. Loneliness and social isolation have been identified as risk factors for adverse outcomes, including all-cause mortality among older adults [27].
Effectively tackling loneliness among older adults living in the community necessitates a comprehensive strategy that encompasses the promotion of social involvement, the nurturing of social connections, and the facilitation of opportunities for meaningful interactions. By understanding the intricate relationship between social engagement and loneliness, targeted interventions can be devised to bolster the mental well-being of community-dwelling older individuals. Currently, there is limited research in Indonesia exploring the determinants of loneliness among older adults in community settings. Thus, this study aimed to explore the correlation between social capital and loneliness among older adults residing in the community.
Instrument and Methods
Design
This cross-sectional research employed an analytical survey among community-dwelling older adults in Pekanbaru, Indonesia, and was conducted in February 2022.
Sample and setting
The sample consisted of all individuals aged 60 years or older residing in the Payung Sekaki sub-district, selected through multistage cluster sampling. The inclusion criteria comprised older adult individuals with adequate reading and hearing abilities, those who were not bedridden, and those willing to participate. The sample size was estimated using the Raosoft sample size calculator (http://www.raosoft.com/samplesize.html), considering a total population of 5,079 older adults in the Payung Sekaki sub-district, a margin of error of 5%, and a confidence level of 90%, resulting in a minimum sample size of 257. The sampling procedure involved multiple stages. First, one out of 12 sub-districts was randomly selected, and subsequently, one village was randomly chosen from the selected sub-district. From this village, nine neighborhood sites were proportionally selected based on the inclusion criteria. Ultimately, 252 participants met the inclusion criteria and participated in the study.
Data collection
The researchers visited older adults in the Payung Sekaki sub-district, employing a door-to-door approach to engage with individuals until the desired sample size was achieved. Upon identifying eligible participants, informed consent was obtained through the completion of a consent form. Subsequently, participants were asked to complete a questionnaire, a process that typically took approximately 15-20 minutes.
Research tools
Data collection involved the administration of three questionnaires. The socio-demographic questionnaire covered information, such as age, gender, education level, and marital status. Then, the UCLA Loneliness Scale was used to gauge feelings of loneliness among participants. Lastly, the Social Engagement Questionnaire assessed aspects, like social activities and social networks.
The Indonesian adaptation of the UCLA Loneliness Scale (version 3) was employed to assess loneliness levels among older adults [28]. This questionnaire comprised 20 items, encompassing two dimensions, including emotional isolation, which refers to individuals lacking deep emotional connections, and social engagement, consisting of six items, and social isolation, reflecting a lack of engagement in community activities and a sense of intentional exclusion from networks, consisting of ten and five items, respectively. Respondents provided answers on a Likert scale ranging from one (never) to four (always). The total loneliness score was categorized as 20-<40 (low loneliness), 40-<60 (moderate loneliness), and 60-≤80 (high loneliness) [4] demonstrating robust internal consistency (Cronbach’s alpha ranging from 0.89 to 0.94) and reliability (r = 0.73). Convergent validity was evidenced by significant correlations with other loneliness measures, with validity scores ranging from r = 0.38 to 0.83, where r > 0.36.
The Social Engagement Questionnaire was developed based on a literature review. It encompassed two main components, including social activities and social networks [29]. Social activities were evaluated by assessing the frequency of visits to places of worship at least once a week, membership in community groups, and engagement in environmental activities such as shopping and traveling. Questions included inquiries about membership in various organizations or clubs, attendance at religious gatherings, social clubs, leisure or sports clubs, and participation in voluntary or charity work, or none of the above. Social networks were evaluated based on the frequency of contact, including both direct (face-to-face) and indirect (via video calls, telephone, and SMS) interactions. Participants were asked about the presence of close friends, relatives, or neighbors, and the frequency of socializing with them. If respondents reported socializing nearly every day, once a week, two or three times a week, or once a month during the past month, they were considered to have social networks (yes=one). Other responses indicating less frequent socialization (e.g., once every two months, once or twice a year) were interpreted as lacking social engagement. A combined overall index score of three to four was categorized as good social engagement, while a score of one to two was considered poor [30]. The validity testing of the social engagement scale demonstrated a total item correlation coefficient ranging from 0.28 to 0.65, with a reliability coefficient of 0.80.
Statistical analysis
The data underwent analysis using SPSS 22 (IBM Corp., Armonk, N.Y., USA). Descriptive statistics, including frequencies, percentages, means, and standard deviations (SDs), were employed to summarize characteristics, such as age, gender, educational level, and marital status. The Chi-square test was utilized to explore the relationships between research parameters. Additionally, binary logistic regression analysis was performed to ascertain factors influencing loneliness among older adults. Statistical significance was established at a two-sided p-value of <0.05.
Findings
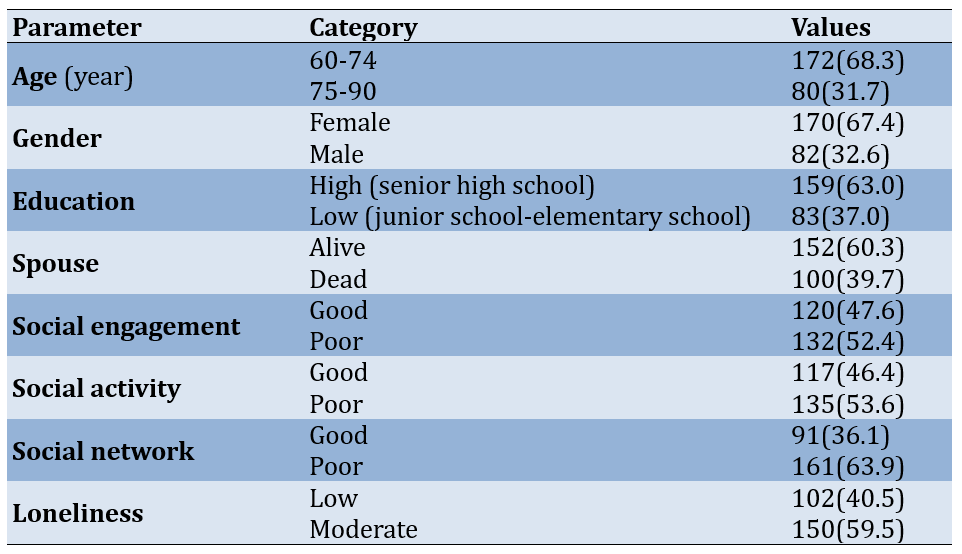
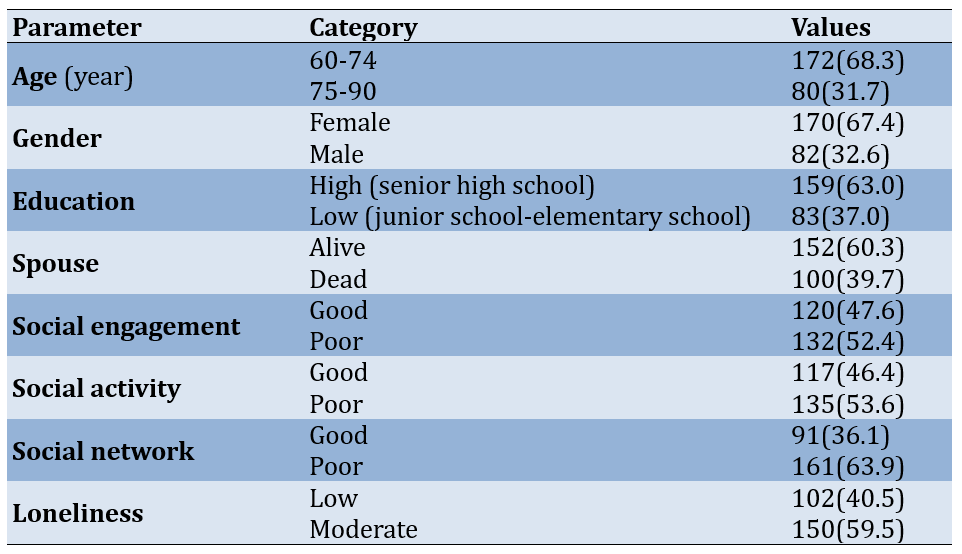
The majority of participants were between 60 and 74 years old, with a mean age of 68.85±5.00 years, while the remaining 31.7% were aged 75 to 90 years. Females made up a larger proportion of the sample, accounting for 67.4%, while males represented 32.6%. In terms of education, 63.0% had attained a high level of education (senior high school or above), whereas 37.0% had a low level of education (junior school to elementary school). Regarding marital status, 60.3% of the older adults had a living spouse, while 39.7% were widowed (Table 1).
Social engagement was classified as good in 47.6% of participants, with a mean score of 11.19±2.27, and poor in 52.4%. Similarly, social activity was considered good in 46.4%, with a mean score of 5.23±1.15, and poor in 53.6% of the sample. Regarding social networks, 36.1% had a good social network, with a mean score of 5.55±1.49, while 63.9% had a poor social network. Lastly, the levels of loneliness among the participants were categorized as low for 40.5%%, with a mean score of 24.51±8.64, and moderate for 59.5%.
Table 1. Frequency of the participants’ socio-demographic characteristics, social capital, and loneliness (n=252)
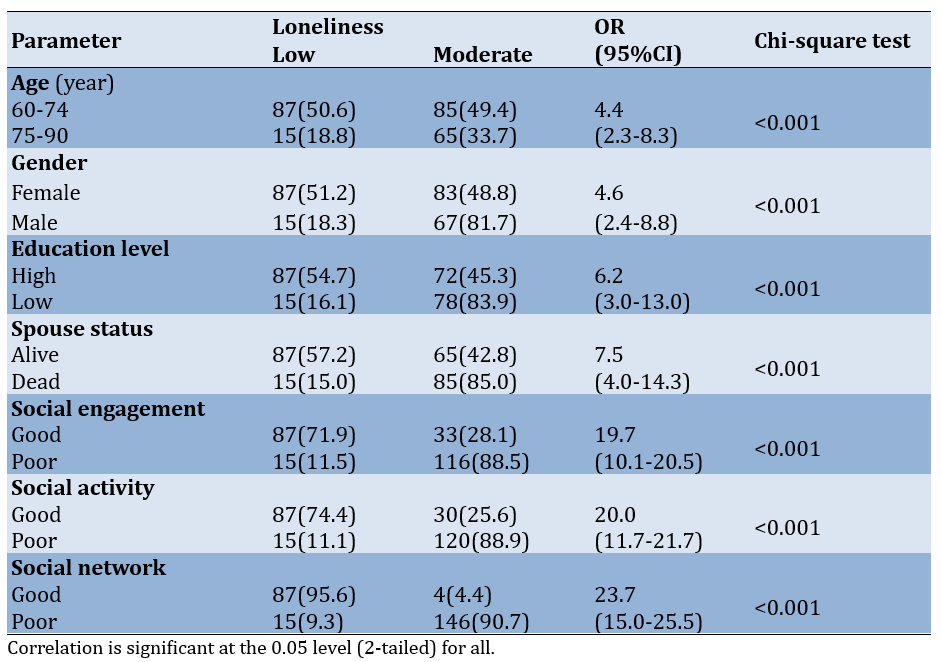
Correlation between socio-demographic characteristics and social capital and loneliness among older adults
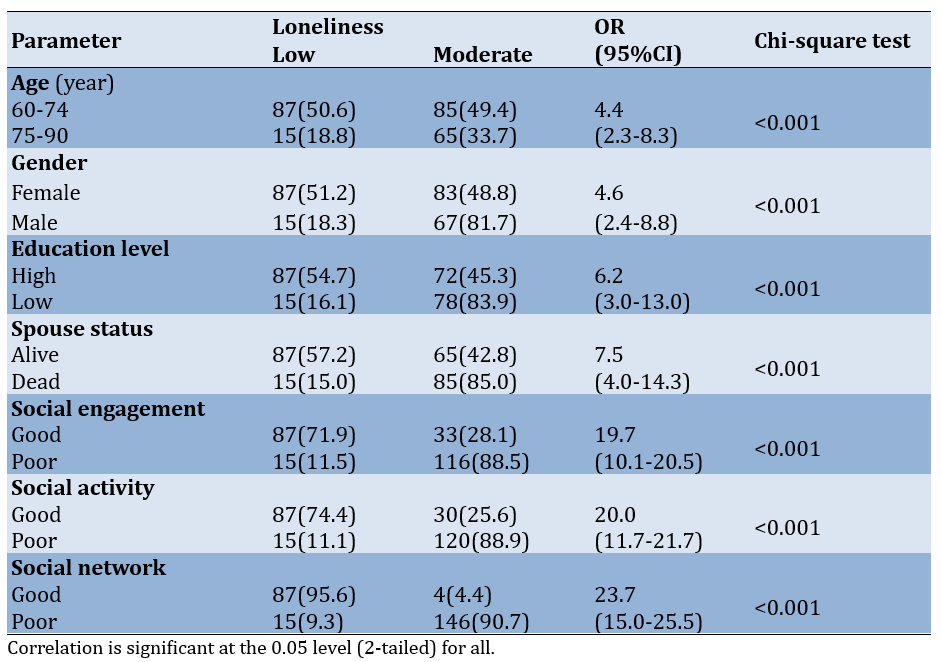
Socio-demographic characteristics and social capital showed a significant correlation with loneliness among older adults (p<0.05; Table 2). The largest odds ratio (OR=23.7) was associated with social networks, indicating that older adults with strong social networks were 23 times less likely to experience loneliness compared to those with poor social connections. Similarly, the bivariate analysis results for social activities revealed an OR of 20, suggesting that older adults engaging in favorable social activities were 20 times less likely to experience loneliness compared to those with poor participation in social activities.
Table 2. Correlation between socio-demographic characteristics and social capital and loneliness (n=252)
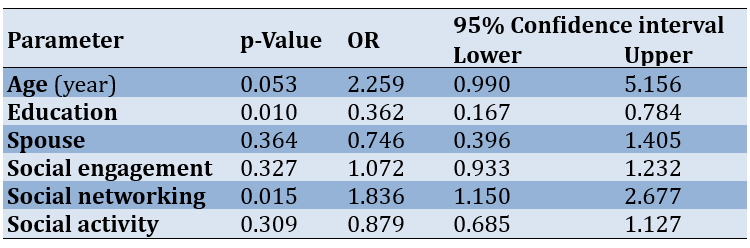
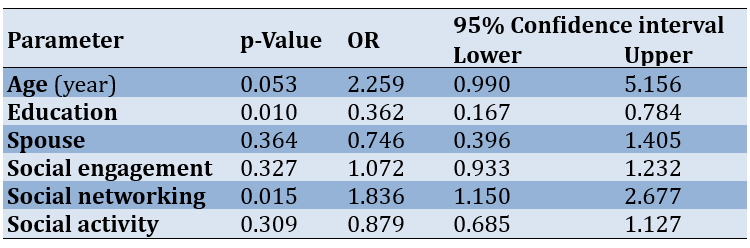
Furthermore, the results of the multivariate analysis using binary logistic regression revealed that education (p=0.010; OR=0.362; 95% CI=0.167-0.784) and social network (p=0.015; OR=1.836; 95% CI=1.150-2.677) were significant predictors of loneliness. Although social activity (p=0.309; OR = 0.879; 95% CI = 0.685-1.127), social engagement (p=0.327; OR=1.072; 95% CI = 0.933-1.232), spouse status (p=0.364; OR=0.746; 95% CI=0.396-1.405), and age (p=0.053; OR=2.259; 95% CI=0.990-5.156) were included in the model, they did not reach statistical significance. Thus, lower education and weaker social networks were independently associated with higher levels of loneliness in older adults (Table 3).
Table 3. Result of the multivariate analysis using binary logistic regression
Discussion
The objective of this research was to investigate the relationship between social capital and loneliness among older adults living in the community. The findings revealed that almost half of the older adults experienced moderate levels of loneliness. Additionally, the elderly living alone often seek comfort in social activities and relationships with peers to alleviate their loneliness. Moreover, the analysis demonstrated significant correlations between loneliness and factors, such as age, gender, education, marital status, and social capital among older adults.
In line with previous research, which suggests that loneliness is influenced by multiple factors, such as solitary living arrangements, social isolation, and limited involvement in communal activities, there is a notable paradox in European societies. Despite a rising trend in solitary living, which can exacerbate feelings of loneliness, fewer individuals report experiencing loneliness. This could be attributed to widespread internet access and active participation in social groups, both of which are prevalent in these societies [31-34].
Moreover, older adults with feelings of loneliness but maintaining social connections demonstrate associations with stress-related biomarkers. Conversely, those who experience both loneliness and social isolation are more likely to exhibit depressive symptoms [35]. These findings emphasize the multifaceted nature of loneliness and the importance of social connections in mitigating its effects.
Additionally, older adults with robust social networks were significantly less susceptible to loneliness, showing a staggering 23-fold decrease compared to those with limited social connections. Similarly, active participation in social activities reduced the likelihood of experiencing loneliness by 20 times in older adults compared to those with minimal engagement.
Previous research consistently underscores the protective role of strong social networks against loneliness among older adults. One study highlighted the association between a supportive social network and enhanced mental and physical well-being in this demographic [36]. Similarly, previous findings suggest that social networks play a crucial role in mediating the relationship between loneliness and depression among the elderly [37].
Furthermore, participating in beneficial social activities has been connected to a decreased likelihood of older adults experiencing loneliness. A prior study showcased that specific types of social engagements correlate with fewer symptoms of insomnia, with loneliness playing a mediating role in this association [38]. Moreover, another study underscored the significance of social engagement during the COVID-19 pandemic, suggesting that measures, like social distancing might heighten feelings of loneliness among older adults [39].
Additionally, our findings underscored the significant role of social networks among older adults, surpassing factors, such as age, education, marital status, social activities, and social relationships. In essence, maintaining robust social networks emerges as the most influential factor in alleviating loneliness among older individuals [40]. Preserving strong social networks proves pivotal in combating loneliness among older adults. Research emphasizes that these networks, encompassing family, friends, and neighbors, offer diverse forms of support, including informational, functional, psychological, and social assistance, thereby fostering feelings of connection and care among older individuals [41].
Variations in social support, involvement in social activities, financial contentment, stress levels, and depressive symptoms significantly influence the extent of loneliness experienced by older individuals. Moreover, the feeling of belonging to a community and overall connectedness within the community emerge as potent factors in alleviating loneliness among older adults [42]. Furthermore, older individuals may opt for emotionally intimate social bonds to cope with loneliness, with support from spouses playing a crucial role in mitigating feelings of loneliness, particularly among those grappling with cognitive impairment or dementia [43].
Additionally, bolstering or maintaining the size and quality of social networks has been associated with positive outcomes in social support and a decrease in loneliness among older adults [44]. Research has consistently emphasized the pivotal role of social support in mitigating loneliness among older individuals, with satisfaction with social support serving as a notable predictor of loneliness [45]. Furthermore, various factors, including socio-demographic characteristics, health conditions, and psychosocial aspects, have been identified as correlates of loneliness in older adults [46]. Therefore, this study underscored the importance of robust social networks in combating loneliness among older adults. Initiatives aimed at fostering social interactions, promoting social support, and addressing loneliness can profoundly impact the overall well-being and quality of life of older individuals.
The findings highlight the crucial role of social networks and social support in mitigating loneliness within this demographic. Strategies aimed at enhancing the size and quality of social networks, fostering social interactions, and promoting satisfaction with social support can effectively alleviate loneliness among older individuals. Additionally, interventions targeting factors, such as socio-demographic characteristics, health conditions, and psychosocial aspects can further contribute to reducing loneliness in this population. Implementing these strategies not only improves the mental and emotional well-being of older adults but also enhances their overall quality of life.
Several limitations in this study should be considered to contextualize the findings. The social dynamics, cultural norms, and community structures in this specific region may differ significantly from those in other parts of Indonesia or globally. Therefore, caution should be exercised when generalizing these findings to older adults in other communities, especially in areas where social interaction is influenced by different cultural, religious, or economic factors. We also did not fully explore the role of modern technology and digital communication in addressing loneliness. With the increasing use of social media, video calls, and other digital tools among older adults, virtual social engagement could be an important factor in reducing loneliness. This aspect was not investigated in the study, leaving a gap in understanding how digital connectivity might influence loneliness, particularly in a post-pandemic world where physical distancing and isolation are more common. Lastly, the influence of economic factors was not examined in depth. Financial stability can play a significant role in shaping social opportunities for older adults, such as their ability to participate in community events or maintain relationships with family and friends. The absence of this analysis limits our understanding of how economic disparities within this population may contribute to varying experiences of loneliness and social engagement.
Conclusion
Socio-demographic characteristics and social capital are associated with loneliness.
Acknowledgments: The authors would like to thank all participants.
Ethical Permissions: This research was approved by the ethics committee of Institut Kesehatan Payung Negeri (Ref. Number: 088/STIKES-PN/KEPK/VIII/2022). The research was conducted after obtaining ethical clearance and approval from the respondents. Respondents had the right to refuse to participate or withdraw at any time, and the confidentiality and privacy of the respondents were maintained.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Ezalina E (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (50%); Alfianur A (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: This study received funding from the Institute of Health Science Payung Negeri Pekanbaru.
Loneliness, a significant concern for mental well-being, is especially prevalent among older individuals and arises from exposure to numerous aging-related factors [1]. This emotional condition entails sensations such as unease, sadness, emptiness, distress, isolation, a sense of purposelessness, disconnection, and a lack of social ties [2-4]. Previous studies suggest that unmet social needs, whether in terms of the quantity or quality of relationships, may contribute to the experience of loneliness [5]. Loneliness can manifest differently among older adults, with experiences ranging from deliberate social isolation due to trauma to feelings of abandonment and emotional suffering caused by being confined to a care home [6].
When loneliness becomes severe and prolonged, it poses risks to both physical and mental well-being. A thorough examination revealed that loneliness is significantly related to conditions such as heart disease, hypertension, stroke, and lung disease [7]. In addition to these illnesses, loneliness affects various other aspects of health, including reduced physical abilities, disruptions in sleep patterns, and decreased sleep quality [8, 9]. Loneliness is also associated with negative mental health consequences, such as increased psychological distress, anxiety, depression, a decline in cognitive function, and dementia [10-12]. Furthermore, loneliness significantly increases the chances of suicide and is correlated with a higher risk of mortality [13-15].
Being a fundamental aspect of quality of life, social engagement has traditionally been linked to favorable physical and psychological effects among older adults in the broader population [16]. Sustained engagement in various activities enhances the overall well-being of older individuals in the later stages of life, contributing to their attainment of successful aging [17]. Studies indicate a correlation between social involvement and reduced levels of depression, even after accounting for parameters, such as demographics, health status, and participation in physical activities among older adults living in the community [18, 19].
Research indicates that practicing leisure activities and maintaining social engagement can help older adults preserve cognitive function, physical function, and mental health, thereby contributing to successful aging [20]. Older adults who sustain engagement in socially productive activities report greater personal satisfaction and well-being [21]. Furthermore, sustained engagement in activities, such as enhanced activities of daily living (EADLs) is critical for quality of life and health outcomes in older individuals [22].
Lack of social engagement can indeed contribute to loneliness and social isolation [23]. Social isolation refers to the objective absence of social contact, while loneliness is the subjective feeling of being alone [24]. Although social isolation is strongly associated with loneliness, the relationship between the two is not straightforward [25]. Factors, such as social relationships, community engagement, and leisure activities play a crucial role in social integration, affecting the multidimensional individual, societal, and environmental aspects [26].
Life transitions, retirement, loss of significant others, and reduced mobility can collectively place older adults at a higher risk of experiencing loneliness and social isolation, impacting their health service use and associated costs [27]. Loneliness and social isolation have been identified as risk factors for adverse outcomes, including all-cause mortality among older adults [27].
Effectively tackling loneliness among older adults living in the community necessitates a comprehensive strategy that encompasses the promotion of social involvement, the nurturing of social connections, and the facilitation of opportunities for meaningful interactions. By understanding the intricate relationship between social engagement and loneliness, targeted interventions can be devised to bolster the mental well-being of community-dwelling older individuals. Currently, there is limited research in Indonesia exploring the determinants of loneliness among older adults in community settings. Thus, this study aimed to explore the correlation between social capital and loneliness among older adults residing in the community.
Instrument and Methods
Design
This cross-sectional research employed an analytical survey among community-dwelling older adults in Pekanbaru, Indonesia, and was conducted in February 2022.
Sample and setting
The sample consisted of all individuals aged 60 years or older residing in the Payung Sekaki sub-district, selected through multistage cluster sampling. The inclusion criteria comprised older adult individuals with adequate reading and hearing abilities, those who were not bedridden, and those willing to participate. The sample size was estimated using the Raosoft sample size calculator (http://www.raosoft.com/samplesize.html), considering a total population of 5,079 older adults in the Payung Sekaki sub-district, a margin of error of 5%, and a confidence level of 90%, resulting in a minimum sample size of 257. The sampling procedure involved multiple stages. First, one out of 12 sub-districts was randomly selected, and subsequently, one village was randomly chosen from the selected sub-district. From this village, nine neighborhood sites were proportionally selected based on the inclusion criteria. Ultimately, 252 participants met the inclusion criteria and participated in the study.
Data collection
The researchers visited older adults in the Payung Sekaki sub-district, employing a door-to-door approach to engage with individuals until the desired sample size was achieved. Upon identifying eligible participants, informed consent was obtained through the completion of a consent form. Subsequently, participants were asked to complete a questionnaire, a process that typically took approximately 15-20 minutes.
Research tools
Data collection involved the administration of three questionnaires. The socio-demographic questionnaire covered information, such as age, gender, education level, and marital status. Then, the UCLA Loneliness Scale was used to gauge feelings of loneliness among participants. Lastly, the Social Engagement Questionnaire assessed aspects, like social activities and social networks.
The Indonesian adaptation of the UCLA Loneliness Scale (version 3) was employed to assess loneliness levels among older adults [28]. This questionnaire comprised 20 items, encompassing two dimensions, including emotional isolation, which refers to individuals lacking deep emotional connections, and social engagement, consisting of six items, and social isolation, reflecting a lack of engagement in community activities and a sense of intentional exclusion from networks, consisting of ten and five items, respectively. Respondents provided answers on a Likert scale ranging from one (never) to four (always). The total loneliness score was categorized as 20-<40 (low loneliness), 40-<60 (moderate loneliness), and 60-≤80 (high loneliness) [4] demonstrating robust internal consistency (Cronbach’s alpha ranging from 0.89 to 0.94) and reliability (r = 0.73). Convergent validity was evidenced by significant correlations with other loneliness measures, with validity scores ranging from r = 0.38 to 0.83, where r > 0.36.
The Social Engagement Questionnaire was developed based on a literature review. It encompassed two main components, including social activities and social networks [29]. Social activities were evaluated by assessing the frequency of visits to places of worship at least once a week, membership in community groups, and engagement in environmental activities such as shopping and traveling. Questions included inquiries about membership in various organizations or clubs, attendance at religious gatherings, social clubs, leisure or sports clubs, and participation in voluntary or charity work, or none of the above. Social networks were evaluated based on the frequency of contact, including both direct (face-to-face) and indirect (via video calls, telephone, and SMS) interactions. Participants were asked about the presence of close friends, relatives, or neighbors, and the frequency of socializing with them. If respondents reported socializing nearly every day, once a week, two or three times a week, or once a month during the past month, they were considered to have social networks (yes=one). Other responses indicating less frequent socialization (e.g., once every two months, once or twice a year) were interpreted as lacking social engagement. A combined overall index score of three to four was categorized as good social engagement, while a score of one to two was considered poor [30]. The validity testing of the social engagement scale demonstrated a total item correlation coefficient ranging from 0.28 to 0.65, with a reliability coefficient of 0.80.
Statistical analysis
The data underwent analysis using SPSS 22 (IBM Corp., Armonk, N.Y., USA). Descriptive statistics, including frequencies, percentages, means, and standard deviations (SDs), were employed to summarize characteristics, such as age, gender, educational level, and marital status. The Chi-square test was utilized to explore the relationships between research parameters. Additionally, binary logistic regression analysis was performed to ascertain factors influencing loneliness among older adults. Statistical significance was established at a two-sided p-value of <0.05.
Findings
The majority of participants were between 60 and 74 years old, with a mean age of 68.85±5.00 years, while the remaining 31.7% were aged 75 to 90 years. Females made up a larger proportion of the sample, accounting for 67.4%, while males represented 32.6%. In terms of education, 63.0% had attained a high level of education (senior high school or above), whereas 37.0% had a low level of education (junior school to elementary school). Regarding marital status, 60.3% of the older adults had a living spouse, while 39.7% were widowed (Table 1).
Social engagement was classified as good in 47.6% of participants, with a mean score of 11.19±2.27, and poor in 52.4%. Similarly, social activity was considered good in 46.4%, with a mean score of 5.23±1.15, and poor in 53.6% of the sample. Regarding social networks, 36.1% had a good social network, with a mean score of 5.55±1.49, while 63.9% had a poor social network. Lastly, the levels of loneliness among the participants were categorized as low for 40.5%%, with a mean score of 24.51±8.64, and moderate for 59.5%.
Table 1. Frequency of the participants’ socio-demographic characteristics, social capital, and loneliness (n=252)
Correlation between socio-demographic characteristics and social capital and loneliness among older adults
Socio-demographic characteristics and social capital showed a significant correlation with loneliness among older adults (p<0.05; Table 2). The largest odds ratio (OR=23.7) was associated with social networks, indicating that older adults with strong social networks were 23 times less likely to experience loneliness compared to those with poor social connections. Similarly, the bivariate analysis results for social activities revealed an OR of 20, suggesting that older adults engaging in favorable social activities were 20 times less likely to experience loneliness compared to those with poor participation in social activities.
Table 2. Correlation between socio-demographic characteristics and social capital and loneliness (n=252)
Furthermore, the results of the multivariate analysis using binary logistic regression revealed that education (p=0.010; OR=0.362; 95% CI=0.167-0.784) and social network (p=0.015; OR=1.836; 95% CI=1.150-2.677) were significant predictors of loneliness. Although social activity (p=0.309; OR = 0.879; 95% CI = 0.685-1.127), social engagement (p=0.327; OR=1.072; 95% CI = 0.933-1.232), spouse status (p=0.364; OR=0.746; 95% CI=0.396-1.405), and age (p=0.053; OR=2.259; 95% CI=0.990-5.156) were included in the model, they did not reach statistical significance. Thus, lower education and weaker social networks were independently associated with higher levels of loneliness in older adults (Table 3).
Table 3. Result of the multivariate analysis using binary logistic regression
Discussion
The objective of this research was to investigate the relationship between social capital and loneliness among older adults living in the community. The findings revealed that almost half of the older adults experienced moderate levels of loneliness. Additionally, the elderly living alone often seek comfort in social activities and relationships with peers to alleviate their loneliness. Moreover, the analysis demonstrated significant correlations between loneliness and factors, such as age, gender, education, marital status, and social capital among older adults.
In line with previous research, which suggests that loneliness is influenced by multiple factors, such as solitary living arrangements, social isolation, and limited involvement in communal activities, there is a notable paradox in European societies. Despite a rising trend in solitary living, which can exacerbate feelings of loneliness, fewer individuals report experiencing loneliness. This could be attributed to widespread internet access and active participation in social groups, both of which are prevalent in these societies [31-34].
Moreover, older adults with feelings of loneliness but maintaining social connections demonstrate associations with stress-related biomarkers. Conversely, those who experience both loneliness and social isolation are more likely to exhibit depressive symptoms [35]. These findings emphasize the multifaceted nature of loneliness and the importance of social connections in mitigating its effects.
Additionally, older adults with robust social networks were significantly less susceptible to loneliness, showing a staggering 23-fold decrease compared to those with limited social connections. Similarly, active participation in social activities reduced the likelihood of experiencing loneliness by 20 times in older adults compared to those with minimal engagement.
Previous research consistently underscores the protective role of strong social networks against loneliness among older adults. One study highlighted the association between a supportive social network and enhanced mental and physical well-being in this demographic [36]. Similarly, previous findings suggest that social networks play a crucial role in mediating the relationship between loneliness and depression among the elderly [37].
Furthermore, participating in beneficial social activities has been connected to a decreased likelihood of older adults experiencing loneliness. A prior study showcased that specific types of social engagements correlate with fewer symptoms of insomnia, with loneliness playing a mediating role in this association [38]. Moreover, another study underscored the significance of social engagement during the COVID-19 pandemic, suggesting that measures, like social distancing might heighten feelings of loneliness among older adults [39].
Additionally, our findings underscored the significant role of social networks among older adults, surpassing factors, such as age, education, marital status, social activities, and social relationships. In essence, maintaining robust social networks emerges as the most influential factor in alleviating loneliness among older individuals [40]. Preserving strong social networks proves pivotal in combating loneliness among older adults. Research emphasizes that these networks, encompassing family, friends, and neighbors, offer diverse forms of support, including informational, functional, psychological, and social assistance, thereby fostering feelings of connection and care among older individuals [41].
Variations in social support, involvement in social activities, financial contentment, stress levels, and depressive symptoms significantly influence the extent of loneliness experienced by older individuals. Moreover, the feeling of belonging to a community and overall connectedness within the community emerge as potent factors in alleviating loneliness among older adults [42]. Furthermore, older individuals may opt for emotionally intimate social bonds to cope with loneliness, with support from spouses playing a crucial role in mitigating feelings of loneliness, particularly among those grappling with cognitive impairment or dementia [43].
Additionally, bolstering or maintaining the size and quality of social networks has been associated with positive outcomes in social support and a decrease in loneliness among older adults [44]. Research has consistently emphasized the pivotal role of social support in mitigating loneliness among older individuals, with satisfaction with social support serving as a notable predictor of loneliness [45]. Furthermore, various factors, including socio-demographic characteristics, health conditions, and psychosocial aspects, have been identified as correlates of loneliness in older adults [46]. Therefore, this study underscored the importance of robust social networks in combating loneliness among older adults. Initiatives aimed at fostering social interactions, promoting social support, and addressing loneliness can profoundly impact the overall well-being and quality of life of older individuals.
The findings highlight the crucial role of social networks and social support in mitigating loneliness within this demographic. Strategies aimed at enhancing the size and quality of social networks, fostering social interactions, and promoting satisfaction with social support can effectively alleviate loneliness among older individuals. Additionally, interventions targeting factors, such as socio-demographic characteristics, health conditions, and psychosocial aspects can further contribute to reducing loneliness in this population. Implementing these strategies not only improves the mental and emotional well-being of older adults but also enhances their overall quality of life.
Several limitations in this study should be considered to contextualize the findings. The social dynamics, cultural norms, and community structures in this specific region may differ significantly from those in other parts of Indonesia or globally. Therefore, caution should be exercised when generalizing these findings to older adults in other communities, especially in areas where social interaction is influenced by different cultural, religious, or economic factors. We also did not fully explore the role of modern technology and digital communication in addressing loneliness. With the increasing use of social media, video calls, and other digital tools among older adults, virtual social engagement could be an important factor in reducing loneliness. This aspect was not investigated in the study, leaving a gap in understanding how digital connectivity might influence loneliness, particularly in a post-pandemic world where physical distancing and isolation are more common. Lastly, the influence of economic factors was not examined in depth. Financial stability can play a significant role in shaping social opportunities for older adults, such as their ability to participate in community events or maintain relationships with family and friends. The absence of this analysis limits our understanding of how economic disparities within this population may contribute to varying experiences of loneliness and social engagement.
Conclusion
Socio-demographic characteristics and social capital are associated with loneliness.
Acknowledgments: The authors would like to thank all participants.
Ethical Permissions: This research was approved by the ethics committee of Institut Kesehatan Payung Negeri (Ref. Number: 088/STIKES-PN/KEPK/VIII/2022). The research was conducted after obtaining ethical clearance and approval from the respondents. Respondents had the right to refuse to participate or withdraw at any time, and the confidentiality and privacy of the respondents were maintained.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors' Contribution: Ezalina E (First Author), Introduction Writer/Methodologist/Main Researcher/Statistical Analyst (50%); Alfianur A (Second Author), Assistant Researcher/Discussion Writer/Statistical Analyst (50%)
Funding/Support: This study received funding from the Institute of Health Science Payung Negeri Pekanbaru.
Article Type: Descriptive & Survey |
Subject:
Social Determinants of Health
Received: 2024/05/28 | Accepted: 2024/08/11 | Published: 2024/09/25
Received: 2024/05/28 | Accepted: 2024/08/11 | Published: 2024/09/25
References
1. Donovan NJ, Blazer D. Social isolation and loneliness in older adults: Review and commentary of a national academies report. Am J Geriatr Psychiatry. 2020;28(12):1233-44. [Link] [DOI:10.1016/j.jagp.2020.08.005]
2. Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons. Arch Intern Med. 2012;172(14):1078-83. [Link] [DOI:10.1001/archinternmed.2012.1993]
3. Morlett Paredes A, Lee EE, Chik L, Gupta S, Palmer BW, Palinkas LA, et al. Qualitative study of loneliness in a senior housing community: The importance of wisdom and other coping strategies. Aging Ment Health. 2021;25(3):559-66. [Link] [DOI:10.1080/13607863.2019.1699022]
4. Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Pers Assess. 1978;42(3):290-4. [Link] [DOI:10.1207/s15327752jpa4203_11]
5. Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010;40(2):218-27. [Link] [DOI:10.1007/s12160-010-9210-8]
6. Wijesiri HSMSK, Samarasinghe K, Edberg AK. Loneliness among older people living in care homes in Sri Lanka. Int J Older People Nurs. 2019;14(4):e12253. [Link] [DOI:10.1111/opn.12253]
7. Petitte T, Mallow J, Barnes E, Petrone A, Barr T, Theeke L. A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol J. 2015;8(Suppl 2):113-32. [Link] [DOI:10.2174/1874350101508010113]
8. Kurina LM, Knutson KL, Hawkley LC, Cacioppo JT, Lauderdale DS, Ober C. Loneliness is associated with sleep fragmentation in a communal society. Sleep. 2011;34(11):1519-26. [Link] [DOI:10.5665/sleep.1390]
9. Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people?. Soc Sci Med. 2016;152:80-6. [Link] [DOI:10.1016/j.socscimed.2016.01.020]
10. Stickley A, Koyanagi A, Roberts B, Richardson E, Abbott P, Tumanov S, et al. Loneliness: Its correlates and association with health behaviours and outcomes in nine countries of the former Soviet :union:. PLoS One. 2013;8(7):e67978. [Link] [DOI:10.1371/journal.pone.0067978]
11. Muyan M, Chang EC, Jilani Z, Yu T, Lin J, Hirsch JK. Loneliness and negative affective conditions in adults: Is there any room for hope in predicting anxiety and depressive symptoms?. J Psychol. 2016;150(3):333-41. [Link] [DOI:10.1080/00223980.2015.1039474]
12. Igbokwe CC, Ejeh VJ, Agbaje OS, Umoke PIC, Iweama CN, Ozoemena EL. Prevalence of loneliness and association with depressive and anxiety symptoms among retirees in Northcentral Nigeria: A cross-sectional study. BMC Geriatr. 2020;20(1):153. [Link] [DOI:10.1186/s12877-020-01561-4]
13. Lara E, Martín-María N, De La Torre-Luque A, Koyanagi A, Vancampfort D, Izquierdo A, et al. Does loneliness contribute to mild cognitive impairment and dementia? A systematic review and meta-analysis of longitudinal studies. Ageing Res Rev. 2019;52:7-16. [Link] [DOI:10.1016/j.arr.2019.03.002]
14. Stickley A, Koyanagi A. Loneliness, common mental disorders and suicidal behavior: Findings from a general population survey. J Affect Disord. 2016;197:81-7. [Link] [DOI:10.1016/j.jad.2016.02.054]
15. Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: A national longitudinal study. Soc Sci Med. 2012;74(6):907-14. [Link] [DOI:10.1016/j.socscimed.2011.11.028]
16. Newman-Norlund RD, Newman-Norlund SE, Sayers S, McLain AC, Riccardi N, Fridriksson J. Effects of social isolation on quality of life in elderly adults. PLoS One. 2022;17(11):e0276590. [Link] [DOI:10.1371/journal.pone.0276590]
17. Ho M, Pullenayegum E, Fuller-Thomson E. Is social participation associated with successful aging among older Canadians? Findings from the Canadian Longitudinal Study on Aging (CLSA). Int J Environ Res Public Health. 2023;20(12):6058. [Link] [DOI:10.3390/ijerph20126058]
18. Enamela P, Prybutok GL, Prybutok VR. The role of physical activity and community engagement in understanding mental health among community-dwelling seniors. Comput Inform Nurs. 2023;41(8):563-8. [Link] [DOI:10.1097/CIN.0000000000000974]
19. Liu R, He WB, Cao LJ, Wang L, Wei Q. Association between chronic disease and depression among older adults in China: The moderating role of social participation. Public Health. 2023;221:73-8. [Link] [DOI:10.1016/j.puhe.2023.06.003]
20. Sala G, Jopp D, Gobet F, Ogawa M, Ishioka Y, Masui Y, et al. The impact of leisure activities on older adults' cognitive function, physical function, and mental health. PLoS One. 2019;14(11):e0225006. [Link] [DOI:10.1371/journal.pone.0225006]
21. Law VT, Yee HH, Ng TK, Fong BY. Evaluating the impact of lifelong education on older adults: A case study from Hong Kong. J Adult Contin Educ. 2023;29(2):643-58. [Link] [DOI:10.1177/14779714231156747]
22. Rogers WA, Mitzner TL, Bixter MT. Understanding the potential of technology to support enhanced activities of daily living (EADLs). Gerontechnology. 2020;19(2):125-37. [Link] [DOI:10.4017/gt.2020.19.2.005.00]
23. Ji X, Li X, Yuh A, Watson A, Kendell C, Weimer J, et al. Short: Integrated sensing platform for detecting social isolation and loneliness in the elderly community. Proceedings of the 8th IEEE/ACM Conference on Connected Health: Applications, Systems and Engineering Technologies. Orlando: IEEE; 2023. p. 148-52. [Link] [DOI:10.1145/3580252.3586983]
24. De Jong Gierveld J, Van Tilburg TG. Understanding social isolation and loneliness. In: Reference module in neuroscience and biobehavioral psychology. Amsterdam: Elsevier; 2023. p. 554-60. [Link] [DOI:10.1016/B978-0-323-91497-0.00143-0]
25. McMahon G, Griffin SM, Borinca I, Bradshaw D, Ryan M, Muldoon OT. Social integration: Implications for the association between childhood trauma and stress responsivity. Psychol Trauma. 2024;16(Suppl 1):S133-42. [Link] [DOI:10.1037/tra0001372]
26. Jung W, Thompson HJ, Byun E. Social integration: A concept analysis. Nurs Forum. 2022;57(6):1551-8. [Link] [DOI:10.1111/nuf.12843]
27. Kammar-García A, Ramírez-Aldana R, Roa-Rojas P, Lozano-Juárez LR, Sánchez-García S, Tella-Vega P, et al. Association of loneliness and social isolation with all-cause mortality among older Mexican adults in the Mexican health and aging study: A retrospective observational study. BMC Geriatr. 2023;23(1):45. [Link] [DOI:10.1186/s12877-023-03750-3]
28. Nurdiani AF. Testing the construct validity of the Ucla Loneliness Scale version 3. J Pengukuran Psikologi Pendidikan Indones. 2013;2(8):499-503. [Indonesian] [Link]
29. Rolandi E, Vaccaro R, Abbondanza S, Casanova G, Pettinato L, Colombo M, et al. Loneliness and social engagement in older adults based in Lombardy during the Covid-19 lockdown: The long-term effects of a course on social networking sites use. Int J Environ Res Public Health. 2020;17(21):7912. [Link] [DOI:10.3390/ijerph17217912]
30. Bailey M, Cao R, Kuchler T, Stroebel J, Wong A. Social connectedness: Measurement, determinants, and effects. J Econ Perspect. 2018;32(3):259-80. [Link] [DOI:10.1257/jep.32.3.259]
31. Swader CS, Moraru AV. Social infrastructure and the alleviation of loneliness in Europe. Kölner Zeitschrift für Soziologie und Sozialpsychologie. 2023;75(Suppl 1):387-414. [Link] [DOI:10.1007/s11577-023-00883-6]
32. Arnoso Martínez A, Sancho J, Elgorriaga E, Arnoso Martínez M, Asla N. Loneliness as an unresolved issue in social inclusion programmes. J Soc Incl. 2022;13(2). [Link] [DOI:10.36251/josi247]
33. Langenkamp A. The influence of loneliness on perceived connectedness and trust beliefs-longitudinal evidence from the Netherlands. J Soc Pers Relatsh. 2022;40(7):2298-322. [Link] [DOI:10.1177/02654075221144716]
34. Jiang L, Cheskin LJ, Frankenfeld CL, Rana ZH, De Jonge L. Loneliness is associated with unhealthful dietary behaviors and physical inactivity among US college students. J Am Coll Health. 2022;1-6. [Link] [DOI:10.1080/07448481.2022.2141060]
35. Tsai TY, Chiu CJ, Wang TY, Tseng HH, Chen KC, Chen PS, et al. Loneliness and isolated living status in middle-aged and older adults in Taiwan: Exploration on stress-related biomarkers, depressive symptoms, and disability. BMC Psychiatry. 2022;22(1):177. [Link] [DOI:10.1186/s12888-022-03824-3]
36. Kim YB, Lee SH. Gender differences in correlates of loneliness among community-dwelling older Koreans. Int J Environ Res Public Health. 2022;19(12):7334. [Link] [DOI:10.3390/ijerph19127334]
37. Domènech-Abella J, Lara E, Rubio-Valera M, Olaya B, Moneta MV, Rico-Uribe LA, et al. Loneliness and depression in the elderly: The role of social network. Soc Psychiatry Psychiatr Epidemiol. 2017;52(4):381-90. [Link] [DOI:10.1007/s00127-017-1339-3]
38. Kim DE, Kim E. Types of social activities associated with fewer insomnia symptoms and the mediating role of loneliness in older adults. Psychogeriatrics. 2022;22(3):299-307. [Link] [DOI:10.1111/psyg.12813]
39. Emerson KG. Coping with being cooped up: Social distancing during COVID-19 among 60+ in the United States. Rev Panam Salud Publica. 2020;44:e81. [Link] [DOI:10.26633/RPSP.2020.81]
40. Hussain B, Mirza M, Baines R, Burns L, Stevens S, Asthana S, et al. Loneliness and social networks of older adults in rural communities: A narrative synthesis systematic review. Front Public Health. 2023;11:1113864. [Link] [DOI:10.3389/fpubh.2023.1113864]
41. Su YP, Hsu HC, Chao SF. Changes in health and social relationships on loneliness among older adults. Educ Gerontol. 2024;50(2):114-28. [Link] [DOI:10.1080/03601277.2023.2226504]
42. Smale B, Wilson J, Akubueze N. Exploring the determinants and mitigating factors of loneliness among older adults. Wellbeing Space Soc. 2022;3:100089. [Link] [DOI:10.1016/j.wss.2022.100089]
43. Park S, Park S, Kim B, Baek J, Amano T. Cognitive function and loneliness among older adults: Dynamics of social network and perceived social support. Innov Aging. 2022;6(Suppl 1):825. [Link] [DOI:10.1093/geroni/igac059.2965]
44. Tomaz SA, Coffee P, Ryde GC, Swales B, Neely KC, Connelly J, et al. Loneliness, wellbeing, and social activity in scottish older adults resulting from social distancing during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(9):4517. [Link] [DOI:10.3390/ijerph18094517]
45. Dong X, Chang ES, Wong E, Simon M. Perception and negative effect of loneliness in a Chicago Chinese population of older adults. Arch Gerontol Geriatr. 2012;54(1):151-9. [Link] [DOI:10.1016/j.archger.2011.04.022]
46. Yang F, Zhang J, Wang J. Correlates of loneliness in older adults in Shanghai, China: Does age matter?. BMC Geriatr. 2018;18(1):300. [Link] [DOI:10.1186/s12877-018-0994-x]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |