Volume 12, Issue 3 (2024)
Health Educ Health Promot 2024, 12(3): 383-388 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadati L, Edalattalab F, Nouri Khaneghah Z, Karami S, Khalilnejad M, Abjar R. Comparing Student-Centered Teaching Methods in Virtual Education; Interactive Lectures vs. Jigsaw Puzzles. Health Educ Health Promot 2024; 12 (3) :383-388
URL: http://hehp.modares.ac.ir/article-5-74948-en.html
URL: http://hehp.modares.ac.ir/article-5-74948-en.html
1- Department of Operating Room, School of Paramedical Sciences, Alborz University of Medical Sciences, Karaj, Iran
2- “Center for Educational Research in Medical Sciences (CERMS)” and “Department of Medical Education, School of Medicine”, Iran University of Medical Sciences, Tehran, Iran
3- Department of Medical Education, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
2- “Center for Educational Research in Medical Sciences (CERMS)” and “Department of Medical Education, School of Medicine”, Iran University of Medical Sciences, Tehran, Iran
3- Department of Medical Education, School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 580 kb]
(3199 Downloads)
| Abstract (HTML) (1238 Views)
Full-Text: (101 Views)
Introduction
The emergence of COVID-19 in late 2019 posed unprecedented challenges to educational systems. As countries implemented social distancing measures and health protocols, educational institutions faced the daunting task of transitioning to remote learning environments, particularly in medical education [1, 2]. This abrupt shift led to the temporary suspension of most in-person medical training activities, necessitating innovative solutions to ensure continuity in education [3, 4]. In response to these challenges, various virtual platforms, webinars, social media tools, and simulators were rapidly developed and deployed to facilitate both online and offline learning experiences [5]. However, educators worldwide grappled with the complex task of adapting their teaching methodologies from traditional classroom settings to virtual environments [6]. One of the common teaching methods affected by virtual education was the lecture. Despite growing concerns about the effectiveness of the lecture-based teaching method and considerable criticisms regarding its ability to empower health system learners, it has still been the most commonly used method by professors [7-9].
Recent literature highlights the potential of replacing conventional lectures with participatory learning approaches that emphasize interpersonal interactions between instructors and students, as well as among students themselves [10]. These interactions, along with frequent discussions and questions from students in interactive teaching, transform a lecture into an effective, student-centered teaching method [11]. Such methods have been shown to enhance active learning and improve overall satisfaction [12]. Furthermore, they strengthen deep learning, critical thinking abilities, academic performance, and self-directed learning among medical students [13]. Undoubtedly, educators’ proficiency in utilizing social networks and virtual technologies can significantly enhance their interaction with students, potentially increasing academic enthusiasm and learning motivation [14]. The concept of academic enthusiasm refers to the amount of effort a learner puts into academic affairs and its efficiency, which is influenced by factors, such as the subject of study, educational atmosphere, and the level of learner participation in the learning process [15].
In addition to interactive lectures, other participatory learning approaches, such as the jigsaw puzzle method, have gained attention in student-centered teaching. This technique assigns more responsibilities to students in the learning process, potentially increasing motivation and self-directed learning [16-18]. Studies have demonstrated improvements in learning outcomes, retention, and clinical skills among students exposed to jigsaw puzzle-based learning [19, 20]. While numerous studies have reported positive effects of participatory teaching methods compared to traditional approaches in face-to-face settings [21, 22], there is limited research on the efficacy of these methods in virtual education environments. Given the importance of surgical technology education and the scarcity of studies comparing student-centered teaching methods in virtual settings, this study aimed to compare interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) methods regarding knowledge retention and academic enthusiasm among surgical technology students.
Materials and Methods
Design and setting
This quasi-experimental study employed a one-group pre-post design and was conducted at Alborz University of Medical Sciences from 2020 to 2021 as a pilot study.
Participants and sampling
Forty-five undergraduate surgical technology students were selected through a census method. The inclusion criteria were informed consent, enrollment in the gastrointestinal and endocrine surgical technology course, and access to the virtual system “Skype Room” and the social network “WhatsApp.” Three participants were excluded for missing one test or more than two teaching sessions.
Research tools
Educational outcomes were assessed using pre-post tests and an academic enthusiasm questionnaire. Multiple-choice questions were designed based on the course syllabus and blueprint, with content and face validity confirmed by eight surgeons and operating room faculty experts. Some items were modified, and others were deleted based on expert evaluation to improve validity. Construct validity was established through key checks by experts, as recommended [23]. Finally, based on experts’ opinions, an 80-item exam was obtained and included five specific questions per surgical procedure across eight sessions. Each group’s test consisted of 40 specific questions, with each question worth half a mark. The reliability of the exam was confirmed by calculating the kappa coefficient (0.83) and the correlation coefficient of even and odd scores using Pearson’s correlation coefficient (0.79).
Academic enthusiasm was measured using the 15-item Academic Enthusiasm Questionnaire developed by Fredericks et al., which assessed behavioral, emotional, and cognitive dimensions on a five-point Likert scale. Its reliability has been confirmed in previous studies, with a Cronbach’s alpha of 0.66 [24]. In this study, Cronbach’s alpha was 0.71.
Data collection
Based on the course plan, general surgery topics were divided into two sections. Section one was taught using the IOLB method, while section two utilized the OJPB method. To minimize the effects of content difficulty, topics were homogenized according to the expert panel’s recommendations. In the first section, a pre-test consisting of 40 multiple-choice questions evaluated students’ baseline knowledge concerning the modules in this section.
IOLB teaching occurred over eight sessions, which included presenting slides/images, and videos, and facilitating questioning via Skype. The instructor maintained engagement by numbering questions and encouraging interaction. After presenting images and videos, the instructor asked questions to identify and address misconceptions with student participation. A post-test followed the eighth session.
Pre-testing for the second section, using the OJPB teaching method, was then conducted. An introductory session explained the puzzle teaching method. Students were divided into six groups of five members each (A-F) on WhatsApp. Each of the six main groups (A-F) was considered a household group. Prepared topics were presented as puzzles under five heading titles, which were accessible to each member. For example, student one covered pre- and post-operative care, student two covered instruments, student three covered surgical techniques, and so on. File numbering was consistent across all household groups. To begin teaching, group members with similar headings formed skill groups on WhatsApp. They discussed their similar headings related to different procedures for 20 minutes. To enhance their understanding, students asked questions or utilized online resources. Students then presented the content of their files in ten-minute WhatsApp voice conferences to their household groups (with times adjusted based on content and agreement). Finally, the instructor summarized and completed the content. After eight sessions, a post-test was administered.
Pre-post tests were compared for both sections. Academic enthusiasm was evaluated over the course duration. To assess retention, post-tests were repeated after six weeks and compared between groups.
Data analysis
Data were analyzed using SPSS 25 at p<0.05. Normality was tested via the Kolmogorov-Smirnov test. Independent t-tests were used to compare learning, retention, and enthusiasm between groups. Paired t-tests compared pre-post outcomes within groups. Linear regression examined the relationships between quantitative variables after assessing the significance of the correlation coefficients. All analyses adhered to statistical principles and precision.
Findings
The sample (n=42) consisted of 28 females (66.7%) and 14 males (33.3%), with a mean age of 20.26±0.63 years. The baseline grade point average (GPA) was 16.43±0.94.
The t-test showed no significant difference in learning scores between the two groups before the intervention (p=0.48). However, a significant difference was observed between the IOLB and OJPB groups in terms of post-test scores (p=0.007, d=0.58). The mean score reported in the IOLB group was 1.21 units higher than that of the OJPB group (17.01 versus 15.80).
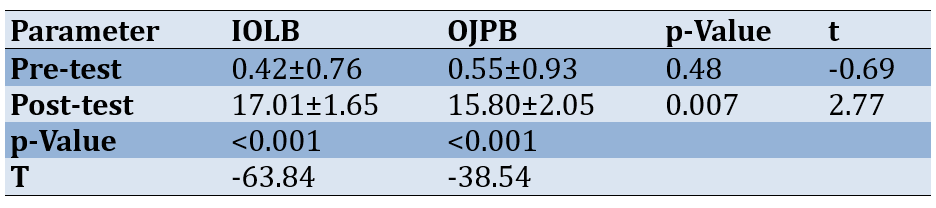
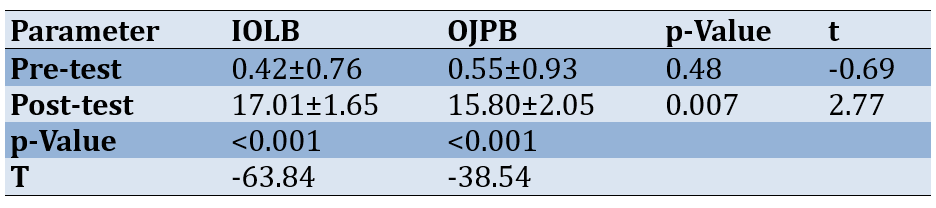
Within groups, paired samples t-tests revealed significantly improved post-intervention learning scores relative to baseline for both the IOLB (p<0.001, d=0.35) and OJPB (p<0.001, d=0.36) groups. However, the between-groups effect size suggests that the extent of improvement was greater for the IOLB group (Table 1).
Table 1. Comparing students' mean learning scores between the interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) groups
An independent samples t-test indicated no significant difference in knowledge retention scores between the IOLB and OJPB groups (p=0.92, t=0.09, d=0.13) when assessed at the six-week follow-up. Both teaching methods demonstrated similar retention over this interval.
Total enthusiasm scores were marginally higher in the IOLB group (M=43.20, SD=4.95) compared to the OJPB group (M=41.25, SD=6.15), although an independent samples t-test found no significant difference between the groups overall (p>0.05; Table 2).
Table 2. Comparing students’ enthusiasm scores across three domains between the two interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) teaching methods
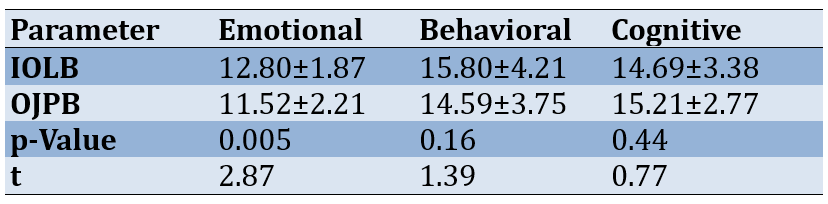
When examining enthusiasm domains, the IOLB group showed significantly greater behavioral enthusiasm than the OJPB group (p=0.005, d=0.67). No significant differences emerged for emotional enthusiasm (p=0.16, d=0.31) or cognitive enthusiasm (p=0.44, d=0.16).
In evaluating academic performance, Pearson correlation revealed a significant moderate positive association between baseline GPA and learning scores in the IOLB group. Linear regression indicated that this relationship was non-linear prior to the intervention (p=0.01, f=6.20) but linear afterward (p<0.001, f=21.87). GPA explained 35% of the variance in IOLB learning scores (adjusted R²=0.35), highlighting its utility in predicting academic performance for this teaching method.
Discussion
The present study compared IOLB and OJPB teaching methods regarding learning, retention, and academic enthusiasm. The central finding was that students in the IOLB group demonstrated significantly higher learning outcomes on the post-intervention assessment compared to their OJPB counterparts. This finding aligns with and builds upon the study by Iwanaga et al., who previously advocated for the value of interactive virtual lectures in online clinical anatomy education. Their study highlighted the ability to successfully facilitate participatory learning in virtual environments, despite the inherent lack of in-person contact [25].
The present results suggest that incorporating interactivity into online lectures, through strategies, such as prompting questions, soliciting feedback, and encouraging student discussions, can enhance engagement and knowledge gains, even in technical content areas like surgical technology. As noted by earlier researchers, active learning techniques appear essential for modern medical educators striving to move beyond static, passive lectures, regardless of whether in physical or virtual classroom settings [26, 27]. The interactive format used here may have facilitated deeper levels of understanding, integration, and retention of key concepts, consistent with theories emphasizing the cognitive benefits of student participation [7, 9].
At the same time, the OJPB approach also led to significant pre-to-post-learning improvements, although not to the same extent as the IOLB method. This contrasts with several studies demonstrating the superiority of in-person jigsaw puzzle teaching techniques over traditional lectures [28-31]. Replicating small group collaborations and peer-to-peer learning online likely poses substantial challenges. Technical difficulties related to concentration, coordination, and sustained participation could reduce the effectiveness of virtual jigsaw methods. Additional research should further explore optimal implementation schemes, group sizes, platform choices, and instructor support to enhance the viability of this approach for remote medical trainees. Creative solutions to simulate the immersive, game-like puzzle experience may help offset the barriers associated with web-based delivery.
An encouraging finding was that both the IOLB and OJPB groups showed comparable long-term knowledge retention when re-assessed six weeks later. This contrasts with the study by Zamani et al., reporting that in-person puzzle teaching and traditional lectures yield different retention rates over a one-month follow-up [32]. Appropriately designed virtual education techniques, grounded in pedagogical theory and evidence, can foster durable learning gains that persist beyond the initial teaching encounter. While the puzzle format may have advantages for motivation and engagement, the IOLB approach appeared equally capable of supporting lasting content assimilation and application.
Analysis of academic enthusiasm scores also provides valuable insights. Overall academic enthusiasm was moderately high for both groups, with no significant between-group differences in composite scores. However, the IOLB group reported higher behavioral engagement, encompassing dimensions such as effort, participation, and rule-following [33, 34]. This suggests that the real-time interactivity of lectures promoted greater involvement than the more complex, asynchronous interactions required for virtual puzzle teamwork. Technical and coordination issues inherent in online group activities may have also been limiting factors.
In contrast, measurements of emotional and cognitive motivation were comparable between the groups. These constructs are more closely tied to intrinsic qualities, such as interest in the material, academic self-efficacy, and the desire for self-directed learning [33]. Some researchers have proposed that well-implemented jigsaw designs enhance perceived autonomy, drive, and self-regulation [35-37]. However, in the current virtual context, the two methods appeared equivalent in these dimensions. The COVID-19 circumstances likely impacted these facets of motivation as well, as chronic stress diminishes efficiency, focus, and determination [38]. Follow-up studies should examine virtual jigsaw teaching under typical conditions to further investigate the effects on student attitudes and engagement.
The findings provide guidance for developing impactful virtual curricula grounded in pedagogical theory when traditional instruction is disrupted. Despite these insights, it is important to acknowledge the limitations of this study. Notably, the research was conducted during the early stages of the COVID-19 pandemic, which introduced unique circumstances that may have influenced the results. Replications in post-pandemic contexts will clarify conclusions about optimal virtual teaching techniques for surgical technology students. The study also relied on a small convenience sample from one institution, limiting generalizability. Follow-up with larger randomized controlled trials is warranted to further compare these novel virtual education methods. Optimizing virtual interactivity, group coordination, self-directed learning, and platform reliability can facilitate engagement and motivation for online students. Educators should leverage evidence-based techniques that creatively adapt in-person active learning strategies to remote settings.
Conclusion
Interactive online lectures lead to superior learning outcomes, supporting the transition of traditional techniques online with interactivity. However, virtual jigsaw puzzles exhibit weaker educational effects, potentially due to coordination challenges.
Acknowledgments: The present article is the result of a research project with the same title and ethics code IR.ABZUMS.REC.1399.183, which was approved and implemented at Alborz University of Medical Sciences. The project team would like to express their appreciation to the research deputy of the Alborz University of Medical Sciences for supporting this research. They also thank the surgical technologist students at Alborz University of Medical Sciences for their participation, which made it possible to conduct the study.
Ethical Permissions: The Ethics Committee of Alborz University of Medical Sciences approved the study (IR.ABZUMS.REC.1399.183), confirming that it adhered to ethical principles. Before starting, students received information about the objectives, methods, and details, and they volunteered to participate. Personal information was kept confidential.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Sadati L (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (25%); Edalattalab F (Second Author), Introduction Writer/Assistant Researcher/Statistical Analyst (15%); Nouri Khaneghah Z (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Karami S (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Khalilnejad M (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Abjar R (sixth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research was funded by the Alborz University of Medical Sciences.
The emergence of COVID-19 in late 2019 posed unprecedented challenges to educational systems. As countries implemented social distancing measures and health protocols, educational institutions faced the daunting task of transitioning to remote learning environments, particularly in medical education [1, 2]. This abrupt shift led to the temporary suspension of most in-person medical training activities, necessitating innovative solutions to ensure continuity in education [3, 4]. In response to these challenges, various virtual platforms, webinars, social media tools, and simulators were rapidly developed and deployed to facilitate both online and offline learning experiences [5]. However, educators worldwide grappled with the complex task of adapting their teaching methodologies from traditional classroom settings to virtual environments [6]. One of the common teaching methods affected by virtual education was the lecture. Despite growing concerns about the effectiveness of the lecture-based teaching method and considerable criticisms regarding its ability to empower health system learners, it has still been the most commonly used method by professors [7-9].
Recent literature highlights the potential of replacing conventional lectures with participatory learning approaches that emphasize interpersonal interactions between instructors and students, as well as among students themselves [10]. These interactions, along with frequent discussions and questions from students in interactive teaching, transform a lecture into an effective, student-centered teaching method [11]. Such methods have been shown to enhance active learning and improve overall satisfaction [12]. Furthermore, they strengthen deep learning, critical thinking abilities, academic performance, and self-directed learning among medical students [13]. Undoubtedly, educators’ proficiency in utilizing social networks and virtual technologies can significantly enhance their interaction with students, potentially increasing academic enthusiasm and learning motivation [14]. The concept of academic enthusiasm refers to the amount of effort a learner puts into academic affairs and its efficiency, which is influenced by factors, such as the subject of study, educational atmosphere, and the level of learner participation in the learning process [15].
In addition to interactive lectures, other participatory learning approaches, such as the jigsaw puzzle method, have gained attention in student-centered teaching. This technique assigns more responsibilities to students in the learning process, potentially increasing motivation and self-directed learning [16-18]. Studies have demonstrated improvements in learning outcomes, retention, and clinical skills among students exposed to jigsaw puzzle-based learning [19, 20]. While numerous studies have reported positive effects of participatory teaching methods compared to traditional approaches in face-to-face settings [21, 22], there is limited research on the efficacy of these methods in virtual education environments. Given the importance of surgical technology education and the scarcity of studies comparing student-centered teaching methods in virtual settings, this study aimed to compare interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) methods regarding knowledge retention and academic enthusiasm among surgical technology students.
Materials and Methods
Design and setting
This quasi-experimental study employed a one-group pre-post design and was conducted at Alborz University of Medical Sciences from 2020 to 2021 as a pilot study.
Participants and sampling
Forty-five undergraduate surgical technology students were selected through a census method. The inclusion criteria were informed consent, enrollment in the gastrointestinal and endocrine surgical technology course, and access to the virtual system “Skype Room” and the social network “WhatsApp.” Three participants were excluded for missing one test or more than two teaching sessions.
Research tools
Educational outcomes were assessed using pre-post tests and an academic enthusiasm questionnaire. Multiple-choice questions were designed based on the course syllabus and blueprint, with content and face validity confirmed by eight surgeons and operating room faculty experts. Some items were modified, and others were deleted based on expert evaluation to improve validity. Construct validity was established through key checks by experts, as recommended [23]. Finally, based on experts’ opinions, an 80-item exam was obtained and included five specific questions per surgical procedure across eight sessions. Each group’s test consisted of 40 specific questions, with each question worth half a mark. The reliability of the exam was confirmed by calculating the kappa coefficient (0.83) and the correlation coefficient of even and odd scores using Pearson’s correlation coefficient (0.79).
Academic enthusiasm was measured using the 15-item Academic Enthusiasm Questionnaire developed by Fredericks et al., which assessed behavioral, emotional, and cognitive dimensions on a five-point Likert scale. Its reliability has been confirmed in previous studies, with a Cronbach’s alpha of 0.66 [24]. In this study, Cronbach’s alpha was 0.71.
Data collection
Based on the course plan, general surgery topics were divided into two sections. Section one was taught using the IOLB method, while section two utilized the OJPB method. To minimize the effects of content difficulty, topics were homogenized according to the expert panel’s recommendations. In the first section, a pre-test consisting of 40 multiple-choice questions evaluated students’ baseline knowledge concerning the modules in this section.
IOLB teaching occurred over eight sessions, which included presenting slides/images, and videos, and facilitating questioning via Skype. The instructor maintained engagement by numbering questions and encouraging interaction. After presenting images and videos, the instructor asked questions to identify and address misconceptions with student participation. A post-test followed the eighth session.
Pre-testing for the second section, using the OJPB teaching method, was then conducted. An introductory session explained the puzzle teaching method. Students were divided into six groups of five members each (A-F) on WhatsApp. Each of the six main groups (A-F) was considered a household group. Prepared topics were presented as puzzles under five heading titles, which were accessible to each member. For example, student one covered pre- and post-operative care, student two covered instruments, student three covered surgical techniques, and so on. File numbering was consistent across all household groups. To begin teaching, group members with similar headings formed skill groups on WhatsApp. They discussed their similar headings related to different procedures for 20 minutes. To enhance their understanding, students asked questions or utilized online resources. Students then presented the content of their files in ten-minute WhatsApp voice conferences to their household groups (with times adjusted based on content and agreement). Finally, the instructor summarized and completed the content. After eight sessions, a post-test was administered.
Pre-post tests were compared for both sections. Academic enthusiasm was evaluated over the course duration. To assess retention, post-tests were repeated after six weeks and compared between groups.
Data analysis
Data were analyzed using SPSS 25 at p<0.05. Normality was tested via the Kolmogorov-Smirnov test. Independent t-tests were used to compare learning, retention, and enthusiasm between groups. Paired t-tests compared pre-post outcomes within groups. Linear regression examined the relationships between quantitative variables after assessing the significance of the correlation coefficients. All analyses adhered to statistical principles and precision.
Findings
The sample (n=42) consisted of 28 females (66.7%) and 14 males (33.3%), with a mean age of 20.26±0.63 years. The baseline grade point average (GPA) was 16.43±0.94.
The t-test showed no significant difference in learning scores between the two groups before the intervention (p=0.48). However, a significant difference was observed between the IOLB and OJPB groups in terms of post-test scores (p=0.007, d=0.58). The mean score reported in the IOLB group was 1.21 units higher than that of the OJPB group (17.01 versus 15.80).
Within groups, paired samples t-tests revealed significantly improved post-intervention learning scores relative to baseline for both the IOLB (p<0.001, d=0.35) and OJPB (p<0.001, d=0.36) groups. However, the between-groups effect size suggests that the extent of improvement was greater for the IOLB group (Table 1).
Table 1. Comparing students' mean learning scores between the interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) groups
An independent samples t-test indicated no significant difference in knowledge retention scores between the IOLB and OJPB groups (p=0.92, t=0.09, d=0.13) when assessed at the six-week follow-up. Both teaching methods demonstrated similar retention over this interval.
Total enthusiasm scores were marginally higher in the IOLB group (M=43.20, SD=4.95) compared to the OJPB group (M=41.25, SD=6.15), although an independent samples t-test found no significant difference between the groups overall (p>0.05; Table 2).
Table 2. Comparing students’ enthusiasm scores across three domains between the two interactive online lecture-based (IOLB) and online jigsaw puzzle-based (OJPB) teaching methods
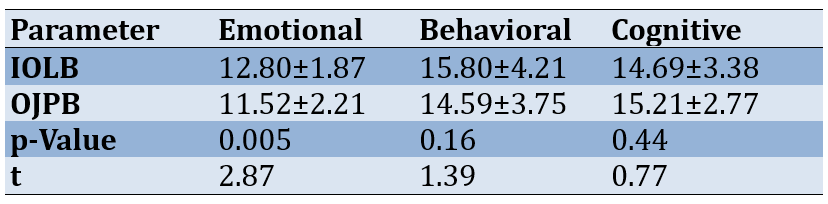
When examining enthusiasm domains, the IOLB group showed significantly greater behavioral enthusiasm than the OJPB group (p=0.005, d=0.67). No significant differences emerged for emotional enthusiasm (p=0.16, d=0.31) or cognitive enthusiasm (p=0.44, d=0.16).
In evaluating academic performance, Pearson correlation revealed a significant moderate positive association between baseline GPA and learning scores in the IOLB group. Linear regression indicated that this relationship was non-linear prior to the intervention (p=0.01, f=6.20) but linear afterward (p<0.001, f=21.87). GPA explained 35% of the variance in IOLB learning scores (adjusted R²=0.35), highlighting its utility in predicting academic performance for this teaching method.
Discussion
The present study compared IOLB and OJPB teaching methods regarding learning, retention, and academic enthusiasm. The central finding was that students in the IOLB group demonstrated significantly higher learning outcomes on the post-intervention assessment compared to their OJPB counterparts. This finding aligns with and builds upon the study by Iwanaga et al., who previously advocated for the value of interactive virtual lectures in online clinical anatomy education. Their study highlighted the ability to successfully facilitate participatory learning in virtual environments, despite the inherent lack of in-person contact [25].
The present results suggest that incorporating interactivity into online lectures, through strategies, such as prompting questions, soliciting feedback, and encouraging student discussions, can enhance engagement and knowledge gains, even in technical content areas like surgical technology. As noted by earlier researchers, active learning techniques appear essential for modern medical educators striving to move beyond static, passive lectures, regardless of whether in physical or virtual classroom settings [26, 27]. The interactive format used here may have facilitated deeper levels of understanding, integration, and retention of key concepts, consistent with theories emphasizing the cognitive benefits of student participation [7, 9].
At the same time, the OJPB approach also led to significant pre-to-post-learning improvements, although not to the same extent as the IOLB method. This contrasts with several studies demonstrating the superiority of in-person jigsaw puzzle teaching techniques over traditional lectures [28-31]. Replicating small group collaborations and peer-to-peer learning online likely poses substantial challenges. Technical difficulties related to concentration, coordination, and sustained participation could reduce the effectiveness of virtual jigsaw methods. Additional research should further explore optimal implementation schemes, group sizes, platform choices, and instructor support to enhance the viability of this approach for remote medical trainees. Creative solutions to simulate the immersive, game-like puzzle experience may help offset the barriers associated with web-based delivery.
An encouraging finding was that both the IOLB and OJPB groups showed comparable long-term knowledge retention when re-assessed six weeks later. This contrasts with the study by Zamani et al., reporting that in-person puzzle teaching and traditional lectures yield different retention rates over a one-month follow-up [32]. Appropriately designed virtual education techniques, grounded in pedagogical theory and evidence, can foster durable learning gains that persist beyond the initial teaching encounter. While the puzzle format may have advantages for motivation and engagement, the IOLB approach appeared equally capable of supporting lasting content assimilation and application.
Analysis of academic enthusiasm scores also provides valuable insights. Overall academic enthusiasm was moderately high for both groups, with no significant between-group differences in composite scores. However, the IOLB group reported higher behavioral engagement, encompassing dimensions such as effort, participation, and rule-following [33, 34]. This suggests that the real-time interactivity of lectures promoted greater involvement than the more complex, asynchronous interactions required for virtual puzzle teamwork. Technical and coordination issues inherent in online group activities may have also been limiting factors.
In contrast, measurements of emotional and cognitive motivation were comparable between the groups. These constructs are more closely tied to intrinsic qualities, such as interest in the material, academic self-efficacy, and the desire for self-directed learning [33]. Some researchers have proposed that well-implemented jigsaw designs enhance perceived autonomy, drive, and self-regulation [35-37]. However, in the current virtual context, the two methods appeared equivalent in these dimensions. The COVID-19 circumstances likely impacted these facets of motivation as well, as chronic stress diminishes efficiency, focus, and determination [38]. Follow-up studies should examine virtual jigsaw teaching under typical conditions to further investigate the effects on student attitudes and engagement.
The findings provide guidance for developing impactful virtual curricula grounded in pedagogical theory when traditional instruction is disrupted. Despite these insights, it is important to acknowledge the limitations of this study. Notably, the research was conducted during the early stages of the COVID-19 pandemic, which introduced unique circumstances that may have influenced the results. Replications in post-pandemic contexts will clarify conclusions about optimal virtual teaching techniques for surgical technology students. The study also relied on a small convenience sample from one institution, limiting generalizability. Follow-up with larger randomized controlled trials is warranted to further compare these novel virtual education methods. Optimizing virtual interactivity, group coordination, self-directed learning, and platform reliability can facilitate engagement and motivation for online students. Educators should leverage evidence-based techniques that creatively adapt in-person active learning strategies to remote settings.
Conclusion
Interactive online lectures lead to superior learning outcomes, supporting the transition of traditional techniques online with interactivity. However, virtual jigsaw puzzles exhibit weaker educational effects, potentially due to coordination challenges.
Acknowledgments: The present article is the result of a research project with the same title and ethics code IR.ABZUMS.REC.1399.183, which was approved and implemented at Alborz University of Medical Sciences. The project team would like to express their appreciation to the research deputy of the Alborz University of Medical Sciences for supporting this research. They also thank the surgical technologist students at Alborz University of Medical Sciences for their participation, which made it possible to conduct the study.
Ethical Permissions: The Ethics Committee of Alborz University of Medical Sciences approved the study (IR.ABZUMS.REC.1399.183), confirming that it adhered to ethical principles. Before starting, students received information about the objectives, methods, and details, and they volunteered to participate. Personal information was kept confidential.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors' Contribution: Sadati L (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (25%); Edalattalab F (Second Author), Introduction Writer/Assistant Researcher/Statistical Analyst (15%); Nouri Khaneghah Z (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Karami S (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Khalilnejad M (Fifth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (10%); Abjar R (sixth Author), Introduction Writer/Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research was funded by the Alborz University of Medical Sciences.
Article Type: Original Research |
Subject:
Technology of Health Education
Received: 2024/05/5 | Accepted: 2024/08/28 | Published: 2024/09/5
Received: 2024/05/5 | Accepted: 2024/08/28 | Published: 2024/09/5
References
1. Pilehroud MN. A review of the challenges and educational opportunities in the period prevalence COVID-19. Paramed Sci Mil Health. 2021;16(1):57-64. [Persian] [Link]
2. Sadeghi Mahali N, Arsalani N, Rad M, Nematifard T, Khaki S, Fallahi-Khoshkenab M. Comparison of virtual education challenges in nursing before and after COVID-19; A systematic review. Iran J Syst Rev Med Sci. 2023;1(3):81-103. [Persian] [Link]
3. Sadati L, Abjar R, Nosrati Abarghoee S, Edalat F, Nouri Z. E-learning challenges and opportunities as experienced by the students Alborz University of Medical Sciences during the Covid-19 pandemic: A qualitative study. Educ Dev Judishapur. 2022;12(4):1011-23. [Persian] [Link]
4. Sadati L, Nouri Z, Hajfiroozabadi M, Abjar R. Faculty members' experiences about virtual education opportunities and challenges during the Covid-19: A qualitative study. J Med Educ Dev. 2021;14(42):1-10. [Persian] [Link] [DOI:10.52547/edcj.14.42.1]
5. Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and surgical education challenges and innovations in the COVID-19 era: A systematic review. In Vivo. 2020;34(3 Suppl):1603-11. [Link] [DOI:10.21873/invivo.11950]
6. Safari M, Yazdanpanah B, Ghafarian H, Yazdanpanah S. Comparing the effect of lecture and discussion methods on students' learning and satisfaction. Iran J Med Educ. 2006;6(1):59-64. [Persian] [Link]
7. Wolff M, Wagner MJ, Poznanski S, Schiller J, Santen S. Not another boring lecture: Engaging learners with active learning techniques. J Emerg Med. 2015;48(1):85-93. [Link] [DOI:10.1016/j.jemermed.2014.09.010]
8. Kumar R, Kandhasamy K, Chauhan R, Bazroy J, Purty A, Singh Z. Tutorials: An effective and interactive method of teaching undergraduate medical students. Int J Community Med Public Health. 2016;3(9):2593-5. [Link] [DOI:10.18203/2394-6040.ijcmph20163079]
9. Begum J, Ali SI, Panda M. Introduction of interactive teaching for undergraduate students in community medicine. Indian J Community Med. 2020;45(1):72-6. [Link] [DOI:10.4103/ijcm.IJCM_232_19]
10. Schwartzstein RM, Roberts DH. Saying goodbye to lectures in medical school-paradigm shift or passing fad?. N Engl J Med. 2017;377(7):605-7. [Link] [DOI:10.1056/NEJMp1706474]
11. Chilwant K. Comparison of two teaching methods, structured interactive lectures and conventional lectures. Biomed Res. 2012;23(3):363-6. [Link]
12. Sadati L, Pazouki AR, Golchin E, Mehdizadehkashi A, Pishgahroudsari M, Tamannaie Z. The effect of cooperative teaching based on students' active participation on learning level in the paramedical faculty of Alborz university of medical sciences. Med Educ J. 2013;1(2):46-52. [Persian] [Link]
13. Khalid K, Ahmad SA. Effectiveness of interactive lectures on knowledge retention and students' motivation in undergraduate medical education-a mixed method study. Pak Armed Forces Med J. 2019;69(1):206-11. [Link]
14. Leon J, Medina-Garrido E, Núñez JL. Teaching quality in math class: The development of a scale and the analysis of its relationship with engagement and achievement. Front Psychol. 2017;8:895. [Link] [DOI:10.3389/fpsyg.2017.00895]
15. Maulana R, Opdenakker MC, Stroet K, Bosker R. Observed lesson structure during the first year of secondary education: Exploration of change and link with academic engagement. Teach Teach Educ. 2012;28(6):835-50. [Link] [DOI:10.1016/j.tate.2012.03.005]
16. Zare H, Arezi S. The effect of teaching methods of puzzle on students learning. Res Sch Virtual Learn. 2014;2(6):7-16. [Persian] [Link]
17. Azimi M, Kiani Gh, Adib Y, Piri M. Effect of different methods performance of cooperative learning on students general self-efficiency. Res Curric Plan. 2016;13(49):99-109. [Persian] [Link]
18. Amani Saribaglo J, Babai Sangleji M, Adib Y, Fathi-Azar E. Students' motivational and social experiences in jig saw cooperative learning method: A qualitative study. J Child Ment Health. 2018;5(1):92-104. [Persian] [Link]
19. Mousavi MS, Mahmoudi M, Hekmat Pou D, Asgari P. Comparison of problem solving and participatory teaching methods on clinical learning, anxiety and satisfaction of nursing students in Arak University of Medical Sciences. J Nurs Educ. 2018;7(1):55-63. [Persian] [Link]
20. Aghapour SA, Vakili MA, Karbasi M, Badeli R. Comparison the effect of student-based group discussion and lecture methods teaching on midwifery student's learning level. Sci J Educ Strateg Med Sci. 2015;8(5):281-6. [Persian] [Link]
21. Zingone MM, Franks AS, Guirguis AB, George CM, Howard-Thompson A, Heidel RE. Comparing team-based and mixed active-learning methods in an ambulatory care elective course. Am J Pharm Educ. 2010;74(9):160. [Link] [DOI:10.5688/aj7409160]
22. Andrews TM, Leonard MJ, Colgrove CA, Kalinowski ST. Active learning not associated with student learning in a random sample of college biology courses. CBE Life Sci Educ. 2011;10(4):394-405. [Link] [DOI:10.1187/cbe.11-07-0061]
23. Haladyna TM. Developing and validating multiple-choice test items. 3rd ed. New York: Routledge; 2004. [Link] [DOI:10.4324/9780203825945]
24. Abbasi M, Dargahi S, Pirani Z, Bonyadi F. Role of procrastination and motivational self-regulation in predicting students' academic engagement. Iran J Med Educ. 2015;15:160-9. [Persian] [Link]
25. Iwanaga J, Loukas M, Dumont AS, Tubbs RS. A review of anatomy education during and after the COVID-19 pandemic: Revisiting traditional and modern methods to achieve future innovation. Clin Anat. 2021;34(1):108-14. [Link] [DOI:10.1002/ca.23655]
26. Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: Medical students' knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15(11):e0242905. [Link] [DOI:10.1371/journal.pone.0242905]
27. Alaagib NA, Musa OA, Saeed AM. Comparison of the effectiveness of lectures based on problems and traditional lectures in physiology teaching in Sudan. BMC Med Educ. 2019;19(1):365. [Link] [DOI:10.1186/s12909-019-1799-0]
28. Abedi N, Taherabadi AA, Kheirollahi F, Jamshidi B. The effect of teaching method STAD, JIGSAW and virtual education on achieving students' cognitive goals of financial statements based on bloom's classification. Account Audit Rev. 2022;29(1):113-45. [Persian] [Link]
29. Hannani S, Samii N, Khacian A. Comparison of traditional and Jigsaw teaching methods on learning and perception of learning environment of operating room students of Iran university of medical sciences. J Nurs Educ. 2019;8(5):39-46. [Persian] [Link]
30. Melinamani S, Francis F, George R, Pushpa LM, Vergheese S. The Jigsaw effect: Impact of Jigsaw learning technique on nursing students to learn the concepts of normal labor. Asian J Nurs Educ Res. 2017;7(2):181-4. [Link] [DOI:10.5958/2349-2996.2017.00037.4]
31. Shakerian S, Khoshgoftar Z, Rezayof E, Amadi M. The use of the Jigsaw cooperative learning technique for the health science students in Iran: A meta-analysis. Educ Res Med Sci. 2020;9(1):e102043. [Link] [DOI:10.5812/erms.102043]
32. Zamani P, Haghighi SB, Ravanbakhsh M. The use of crossword puzzles as an educational tool. J Adv Med Educ Prof. 2021;9(2):102-8. [Link]
33. Alrashidi O, Phan HP, Ngu BH. Academic engagement: An overview of its definitions, dimensions, and major conceptualisations. Int Educ Stud. 2016;9(12):41-52. [Link] [DOI:10.5539/ies.v9n12p41]
34. Fredricks JA, Blumenfeld PC, Paris AH. School engagement: Potential of the concept, state of the evidence. Rev Educ Res. 2004;74(1):59-109. [Link] [DOI:10.3102/00346543074001059]
35. Azizi S, Bagheri M, Karimi Moonaghi H, Mazloum S. Comparison of the effect of two educational methods of Jigsaw and feedback on the level of satisfaction of nursing and anesthesia students of Mashhad school of nursing and midwifery. Res Med Educ. 2021;12(4):16-28. [Persian] [Link] [DOI:10.52547/rme.12.4.16]
36. Hahn S, Ryu YM. A study on the correlations among IRAT, GRAT, problem solving, communication, learning motivation, and learning satisfaction after team-based learning in nursing students. Int J Pure Appl Math. 2018;118(24). [Link]
37. Sanaie N, Vasli P, Sedighi L, Sadeghi B. Comparing the effect of lecture and Jigsaw teaching strategies on the nursing students' self-regulated learning and academic motivation: A quasi-experimental study. Nurse Educ Today. 2019;79:35-40. [Link] [DOI:10.1016/j.nedt.2019.05.022]
38. Alotiby AA. The correlation between stress levels among undergraduate medical students and their motivation for studying medicine. Educ Res Int. 2022;2022(1):1605435. [Link] [DOI:10.1155/2022/1605435]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






