Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 755-760 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Trung N, Long N, Huong T, Thuan D, Tam N, Lan N, et al . Effects of a Pandemic on the Professional Quality of Life in Vietnamese Healthcare Workers. Health Educ Health Promot 2023; 11 (5) :755-760
URL: http://hehp.modares.ac.ir/article-5-74790-en.html
URL: http://hehp.modares.ac.ir/article-5-74790-en.html
1- Department of Community Medicine and Preventive Medicine, University of Medicine and Pharmacy, Hanoi, Vietnam
2- Saint Paul Hospital, Hanoi, Vietnam
3- Department of Preventive Medicine, Faculty of Medicine, Dai Nam University, Hanoi, Vietnam
4- Department of Basic Medicine and Pharmacy, University of Medicine and Pharmacy, Hanoi, Vietnam
5- Department of Basic Pharmaceutical Sciences, Faculty of Pharmacy, University of Medicine and Pharmacy, Hanoi, Vietnam
2- Saint Paul Hospital, Hanoi, Vietnam
3- Department of Preventive Medicine, Faculty of Medicine, Dai Nam University, Hanoi, Vietnam
4- Department of Basic Medicine and Pharmacy, University of Medicine and Pharmacy, Hanoi, Vietnam
5- Department of Basic Pharmaceutical Sciences, Faculty of Pharmacy, University of Medicine and Pharmacy, Hanoi, Vietnam
Keywords: Quality of Life [MeSH], Healthcare Workers [MeSH], Pandemics [MeSH], COVID-19 [MeSH], Urban [MeSH]
Full-Text [PDF 557 kb]
(2364 Downloads)
| Abstract (HTML) (980 Views)
Full-Text: (188 Views)
Introduction
The onset of a pandemic has presented healthcare workers (HCWs) with a diverse array of difficulties, including the experience of encountering a high volume of fatalities, grappling with ethical decision-making, facing the constant threat of infection and the potential exposure of their family members, coping with an increased workload, and operating without adequate equipment [1, 2]. These stress-inducing circumstances have also manifested as symptoms of mental disorders and somatization among healthcare workers [3, 4]. Consequently, these immediate and enduring challenges have had a profound impact on the effectiveness of health professionals, their levels of occupational stress, and the quality of care they provide to patients, thereby influencing their professional quality of life (ProQoL).
ProQoL encompasses a multifaceted construct pertaining to the extent to which individuals can satisfy their personal needs within the context of their work environment encounters [5]. The concept involves a sense of renewal and energy as a result of individuals’ engagement in their work, burnout, and secondary traumatic stress stemming from their compassion-driven efforts. Several prior studies have indicated that a higher level of professional quality of life is connected to a lower occurrence of mental disorders [6, 7] as well as reduced perceived stress [8, 9]. Various factors pertaining to healthcare professionals' professional and social roles, such as ambiguity, role conflict, and workload, can lead to work-related stress, consequently diminishing professional effectiveness, particularly during the ongoing COVID-19 pandemic [10, 11]. The COVID-19 outbreak has been recognized as a widespread public health challenge with significant repercussions on nations' healthcare infrastructures and economies [12, 13].
To date, Vietnam has suffered significant health, social, and economic impacts of the COVID-19 pandemic [14]. HCWs were recognized among the most vulnerable populations to physical and mental disorders due to COVID-19 [15, 16]. Several studies have been performed to measure the QoL of HCWs [17, 18], including one study that attempted to measure ProQoL [18]. However, this previous study was conducted with only a small sample size, with the main objective of validating the ProQoL instrument. Given the matter that ProQoL is an individual’s perception about their work aspects, therefore, it is highly dependent on contextual background, socioeconomic and workplace characteristics. Therefore, more evidence should be provided about the ProQoL of HCWs, particularly among frontline HCWs during an epidemic, in order to develop appropriate interventions to improve the ProQoL of HCWs.
This study aimed to measure the ProQoL of HCWs in an urban hospital in Vietnam and identify associated factors after the epidemic.
Instrument and Methods
Study design and setting
A cross-sectional study was conducted on an urban hospital in Hanoi, Vietnam, from July to September 2022. Participants were HCWs who worked in the hospital for at least three months, voluntarily participated in the study, and gave written informed consent. Individuals working in the hospital for less than three months, having acute illnesses, or disagreeing to participate in the study were excluded. We included all people who met the eligibility criteria. A total of 924 participants were recruited in the study.
Data collection
A self-reported structured questionnaire was developed and distributed to the participants. The questionnaire's contents were piloted in 10 participants and revised according to their feedback. Each participant spent 10-15 minutes completing the Socio-demographic questionnaire (job characteristics, age, gender, education, marital status, years of experience, position, time working per day and week, number of days on duty per week, and changing the amount of work or income during the COVID-19 pandemic). The Professional Quality of Life Scale for Health Workers (Pro-Qol Health) was employed [19]. The instrument consists of 30 items, which encompass five domains; Compassion Satisfaction (CS), Perceived Support (PS), Burnout (BO), Secondary Traumatic Stress (STS), and Moral Distress (MD). Each section comprises six inquiries, with the responses allocated a corresponding numerical value on a scale of 1 (Never), 2 (Rarely), 3 (Sometimes), 4 (Often), and 5 (Very often). The upper limit for the cumulative score in each domain is 30 points. The evaluation of each aspect was conducted based on its corresponding score, which was categorized into three levels: 1) Low, indicating a score of 12 or less; 2) Average, representing a score within the range of 13 to 23; And 3) High, indicating a score of 24 or more. The Cronbach alpha test was conducted to assess the alpha value for Pro-Qol Health and its respective domains, including CS, PS, BO, STS, and MD, yielding values of 0.84, 0.87, 0.82, 0.82, 0.74, and 0.70. The Vietnamese version of Pro-Qol Health has been validated elsewhere [18].
Statistical analysis
The data was analyzed using the Stata 14.0 by Chi-square test and the Kruskal-Wallis test to discern disparities in ratios or means among various groups based on variations in working time (whether it increased, remained constant, or decreased) after the COVID-19 pandemic. The associated parameters with each domain of healthcare workers' professional quality of life were investigated using multivariate Tobit regression models. A forward stepwise selection approach was employed to eliminate variables that were not statistically significant, whereby the criterion for selection of variables in the reduced models was set at a p-value of less than 0.2 for the log-likelihood ratio test. A p-value below the threshold of 0.05 was deemed to indicate statistical significance.
Findings
The average age of the participants was 37.2±7.9. There was no significant difference between the age groups of the participants according to their viewpoint on the amount of work (increase/constant/decrease) during the pandemic (p=0.21).
Men comprised 31.4% of the sample, with a significantly smaller proportion experiencing an increased workload during the pandemic compared to women. The percentages of participants possessing undergraduate, graduate, and postgraduate education were 22.0, 35.4, and 40.6%, respectively (Table 1).
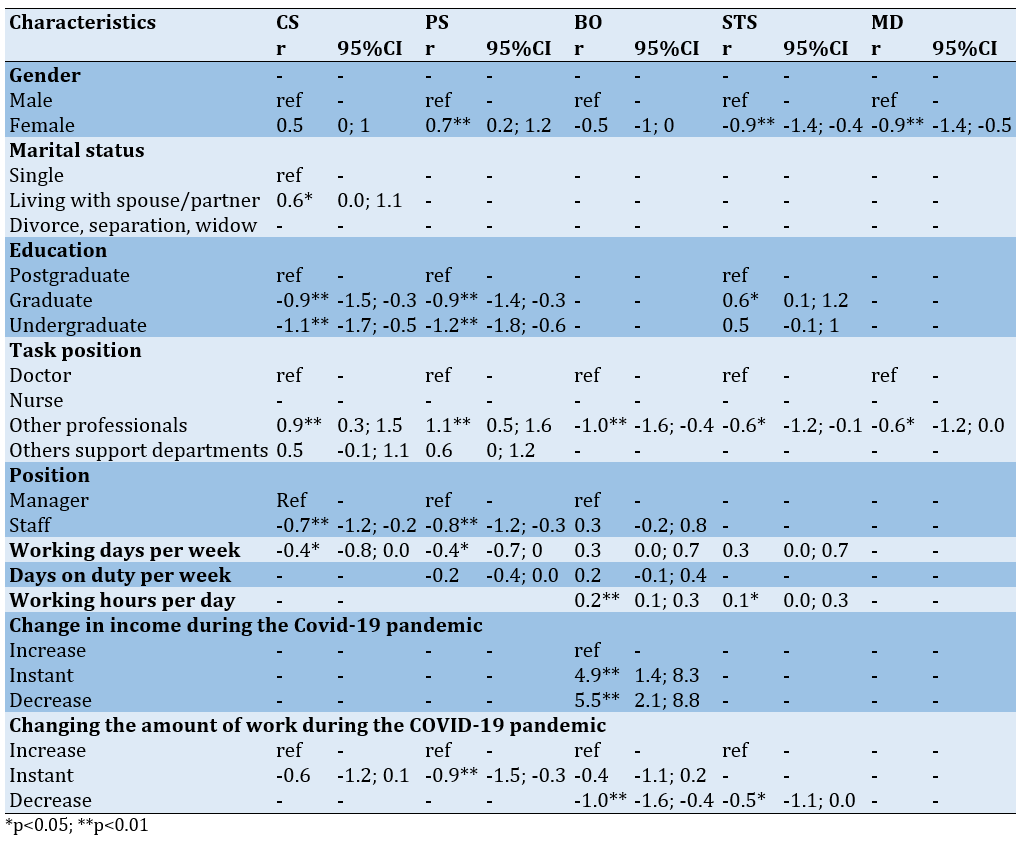
Table 1. Comparing the frequency (the numbers in parentheses are percentages) of participants’ viewpoints on the amount of work during the pandemics according to the sociodemographic characteristics (n=924)
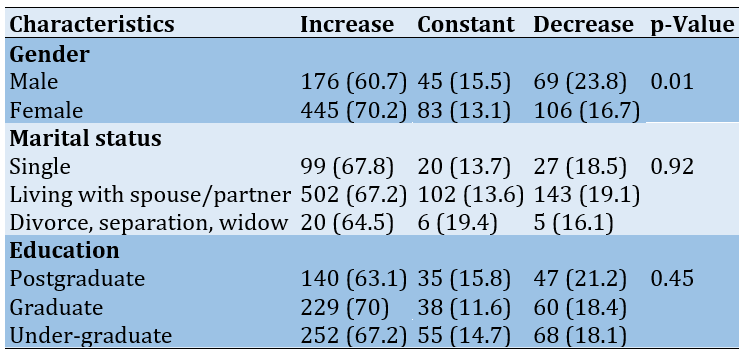
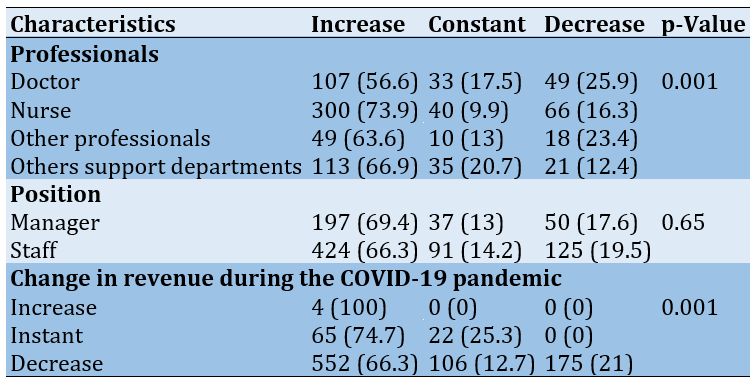
The majority of participants were nurses (43.9%), and their mean experience was 12.9±8.6 years. There was no significant difference between the participants' years of experience groups according to their viewpoint on the amount of work (increase/constant/decrease) during the pandemic (p=0.18).
Nurses experienced the greatest surge in workload during the pandemic, while doctors had the least increase compared to their regular duties (p<0.01). The mean number of working days per week was 5.3±0.6 days per week, the mean number of days on duty per week was 1.3±1.0 days, and the mean number of working hours per day of 8.7±1.8 hours per day. The majority of individuals experienced a decline or no change in their incomes throughout the duration of the pandemic.
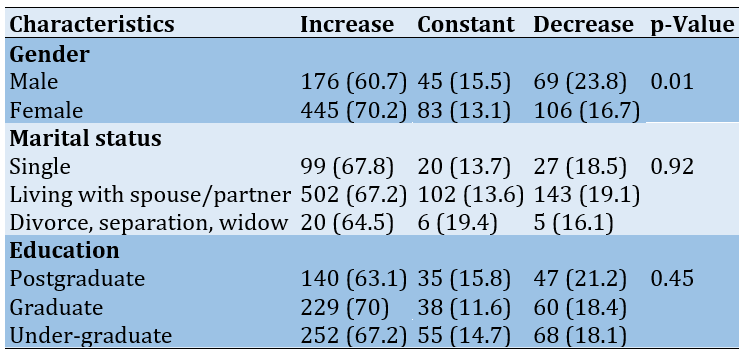
Table 2. Comparing the frequency (the numbers in parentheses are percentages) of participants’ viewpoints on the amount of work during the pandemics according to the job characteristics (n=924)
The mean professional quality of life scores for HCWs in the CS, PS, BO, STS, and MD categories were 20.6±3.5, 20.4±3.4, 17.6±3.5, 16.6±3.2, and 16.3±3.4, respectively. The proportion of HCWs who had the lowest levels of CS (1.9%) and PS (2.1%) was the lowest among all groups (Figure 1).
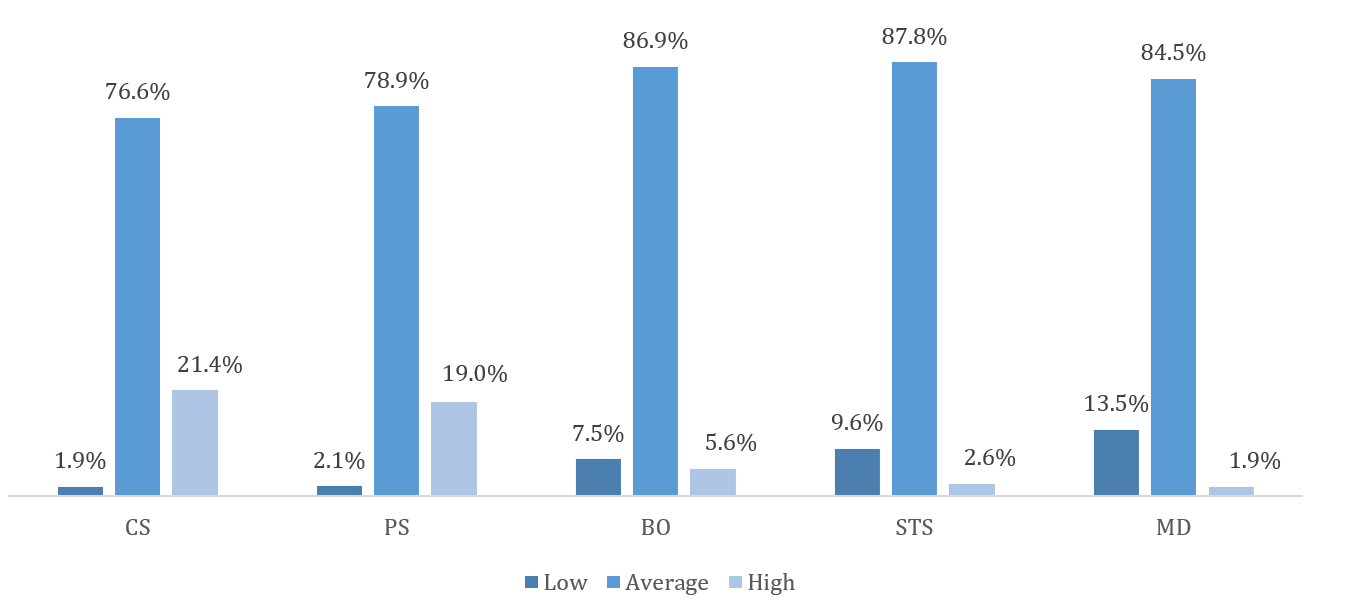
Figure 1. Professional quality of life among healthcare workers
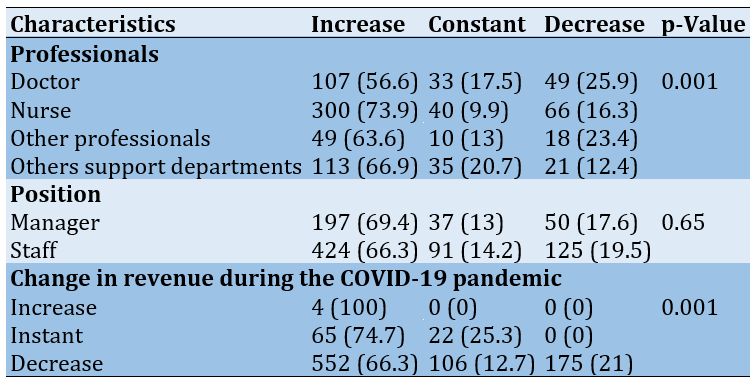
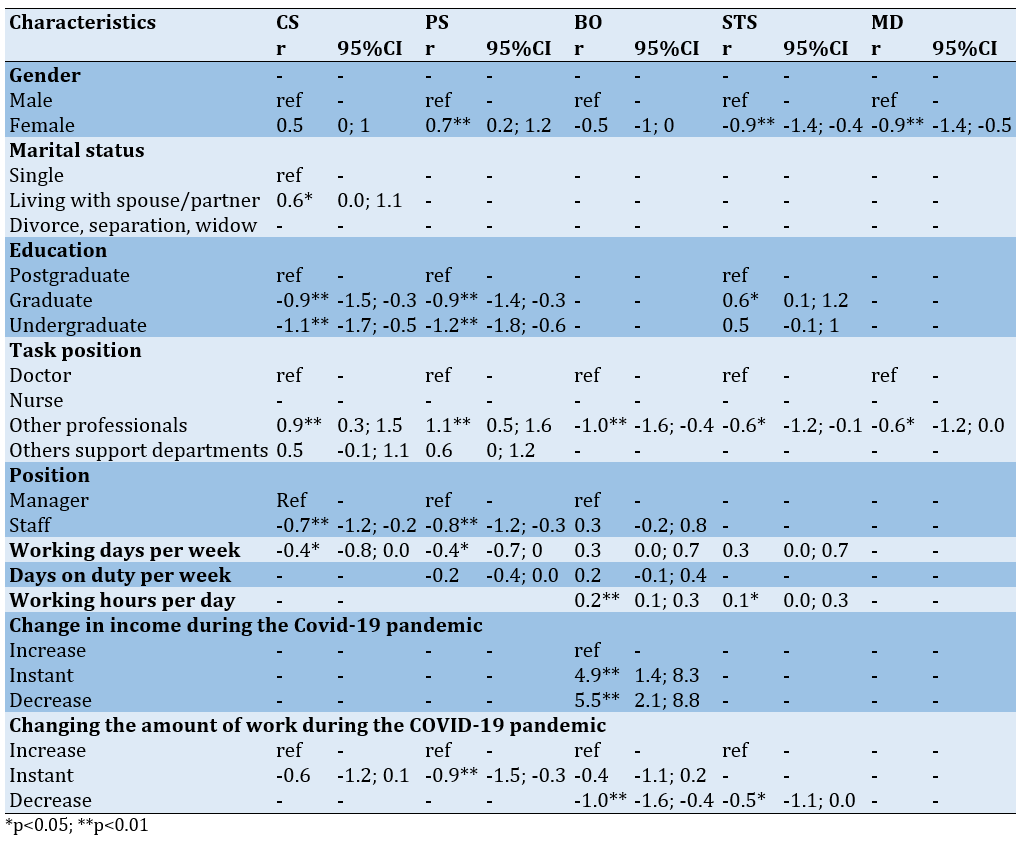
Regarding sociodemographic characteristics, being female was positively associated with the PS domain (r=0.7) but negatively related to STS (r=-0.9) and MD domains (r=-0.9). Living with a spouse/partner was positively associated with the CS domain (r=0.6). Lower education level was negatively correlated with CS and PS scores. Regarding job characteristics, participants having other professionals (e.g., technicians, midwifery, etc.) had higher CS (r=0.9) and PS (r=1.1) scores but lower BO (r=-1.0), STS (r=-0.6) and MD scores (r=-0.6). Being staff was negatively associated with CS and PS scores. Higher working days per week were negatively correlated with CS (r=-0.4) and PS scores (r=-0.4), while a higher number of working hours per day was positively correlated with BO (r=0.2) and STS scores (r=0.1). Participants with stable or decreased incomes had significantly higher BO scores than those with increased income. In addition, participants with a stable amount of work had a lower PS score, while those with a decreased amount of work had lower BO and STS scores (Table 3).
Table 3. Factors associated with Compassion Satisfaction (CS), Perceived Support (PS), Burnout (BO), Secondary Traumatic Stress (STS), and Moral Distress (MD) among participants
Discussion
The results showed a moderate professional quality of life among Vietnamese HCWs after the COVID-19 pandemic. Moreover, we found different demographic and job characteristics that were related to the professional quality of life, which could be potentially used to develop appropriate interventions to improve the ProQoL of HCWs.
The present study employed the Pro-Qol Health instrument to assess the professional quality of life of HCWs. Findings suggested that Vietnamese HCWs had moderate professional quality of life, aligning with a study of Portuguese physicians and nurses during the third wave of the COVID-19 pandemic, which showed a moderate level of CS, BO, and STS among these HCWs [20]. Indeed, this study was performed during the latter half of 2022, when a global subjugation of the COVID-19 pandemic was observed. In the context of Vietnam, the current phase could be denoted as the new normal post-COVID-19 stage. Hence, it is evident that there exists minimal disparity in the overall professional well-being experienced by HCWs in the immediate aftermath of the pandemic when compared to the initial outbreak phase. The professional life of HCWs has been profoundly impacted since the onset of the epidemic, leading to a discernible decline in its overall quality.
Regarding specific domains of ProQoL, CS occurs when empathy motivates healthcare professionals to relieve patient pain. CS is the satisfaction that HCWs find in productivity, aiding them in managing work challenges [21]. Meanwhile, PS is the awareness of HCWs’ access to practical work support when needed, including task performance, advice, or emotional support. A higher PS score corresponds to better support [19]. CS and PS are powerful aspects of professional quality of life. In this study, high-grade CS and PS accounted for approximately 20%, which was higher than a prior report in Spain during the pandemic with 18.2% [20], but lower than a study in China (35.3%) [22]. Cuartero-Castañer et al. suggested that the social recognition of HCWs during the epidemic may cause a high prevalence of CS [23]. CS and PS scores were higher in other HCWs, such as technicians, midwives, and pharmacists, than doctors, which might be explained by the matter in the increasing workload during the outbreak among other HCWs. According to Wu et al., working at the frontline positively affects CS [24]. Increased workloads during an epidemic may promote satisfaction due to a deeper sense of self-employment in the fight against the epidemic. Crediting overworked HCWs during the pandemic can boost support for them and increase PS. Women had higher PS scores than men, which might be due to women having more relationships and social support compared to men [25]. HCWs living with spouses had higher CS scores than those who are single, which could be explained that these HCWs developed coping mechanisms [23], and they sought help from their parents to take care of their families because they were usually on duty [20]. CS and PS scores were also reported to be significantly lower in those with undergraduate/graduate education, and lower in staff versus management groups. Prior research suggested that HCWs with better clinical skills might have higher CS levels [26]. Indeed, HCWs with higher education levels were often appointed to management positions, which might result in better CS than those who were staff. Furthermore, there is evidence that managers tended to have better friendships and more support in the workplace [27].
Burnout refers to feelings of hopelessness that make it challenging to be productive at work. Meanwhile, STS is exposure to traumatic events at work, like witnessing suffering, violence, or death; While MD refers to when frontline HCWs have to act against personal values and ethics [19]. These vulnerabilities can cause medical errors and impact patient care [28] and professional relationships [29]. Our study showed a pervasiveness of moderate levels of BO, STS, and MD, which was different from prior studies [20, 22, 30]. However, the low rate of high levels of BO, STS, and MD in our study could be explained by the commonness of CS. Indeed, CS could play a role as a protective factor, which helped to lower STS and BO [31]. During the epidemic, the role of HCWs was enhanced, which boosted CS and, eventually, positively impacted STS and BO. Nonetheless, at the time of this investigation, HCWs in Vietnam had not only failed to recognize the worthy efforts in fighting the epidemic but also faced public criticism, which might explain the high scores of BO, STS, and MD.
Regression analysis showed that women had lower STS and MD levels than men. This result was different from other reports showing that women were at higher risk of STS than men because they had a more sensitive hypothalamic-pituitary gland [31-33]. We supposed that females had a higher score of PS than their male counterparts, which helps balance the BO, STS, and MD factors. In addition, the analysis showed that the increased number of working hours per day increased the levels of BO and STS among HCWs, which was in line with other studies [34-36]. Healthcare workers with stable or reduced income during the pandemic had higher BO levels. In Vietnam, during the pandemic, HCWs still work despite the colonial expansion, and many HCWs exceeded their expected workload while their income increased significantly. Some authors have shown that income affects the quality of health workers' professional life [37, 38]. Moreover, job satisfaction increases when employees are paid fairly, reducing financial burdens and improving conditions for professional activities [37].
This study is among a few research using the Pro-Qol Health instrument to describe the professional quality of life among HCWs in Vietnam post-pandemic. The study helps improve healthcare services in the new normal. However, this study has limitations. The study was conducted at an urban hospital, which hinder the generalizability of the study’s findings to HCWs in Vietnam. Furthermore, the absence of evidence from the Pro-Qol Health tool hinders comparisons of study results with other studies. Finally, the cross-sectional descriptive study design limits the ability to conclude a causal relationship.
Conclusion
This study showed a moderate professional quality of life among Vietnamese HCWs after the COVID-19 pandemic. Strengthening the healthcare system's capacity should be a top priority, along with supporting healthcare professionals in managing stress and developing psychological resilience, to improve HCWs' ProQoL.
Acknowledgments: We would like to thank Vietnam National University, Hanoi (VNU), and the staff of Saint Paul Hospital for supporting us throughout the research process.
Ethical Permissions: The research has been approved by the Institutional Review Board, University of Public Health. No. 426/2023/YTCC-HD3, November 16, 2023.
Conflict of Interest: Nothing to be reported.
Authors’ Contribution: Trung NT (First Author), Methodologist (12.5%); Long ND (Second Author), Methodologist (12.5%); Huong TL (Third Author), Main Researcher (12.5%); Thuan DT (Fourth Author), Main Researcher (12.5%); Tam NT (Fifth Author), Statistical Analyst (12.5%); Phuong Lan NT (Sixth Author), Assistant Researcher (12.5%); Tuan MD (Seventh Author), Assistant Researcher (12.5%); Bach NX (Eighth Author), Introduction Writer (12.5%)
Funding/Support: This research was funded by the research project QG (QGSP.2022.07) of Vietnam National University, Hanoi.
The onset of a pandemic has presented healthcare workers (HCWs) with a diverse array of difficulties, including the experience of encountering a high volume of fatalities, grappling with ethical decision-making, facing the constant threat of infection and the potential exposure of their family members, coping with an increased workload, and operating without adequate equipment [1, 2]. These stress-inducing circumstances have also manifested as symptoms of mental disorders and somatization among healthcare workers [3, 4]. Consequently, these immediate and enduring challenges have had a profound impact on the effectiveness of health professionals, their levels of occupational stress, and the quality of care they provide to patients, thereby influencing their professional quality of life (ProQoL).
ProQoL encompasses a multifaceted construct pertaining to the extent to which individuals can satisfy their personal needs within the context of their work environment encounters [5]. The concept involves a sense of renewal and energy as a result of individuals’ engagement in their work, burnout, and secondary traumatic stress stemming from their compassion-driven efforts. Several prior studies have indicated that a higher level of professional quality of life is connected to a lower occurrence of mental disorders [6, 7] as well as reduced perceived stress [8, 9]. Various factors pertaining to healthcare professionals' professional and social roles, such as ambiguity, role conflict, and workload, can lead to work-related stress, consequently diminishing professional effectiveness, particularly during the ongoing COVID-19 pandemic [10, 11]. The COVID-19 outbreak has been recognized as a widespread public health challenge with significant repercussions on nations' healthcare infrastructures and economies [12, 13].
To date, Vietnam has suffered significant health, social, and economic impacts of the COVID-19 pandemic [14]. HCWs were recognized among the most vulnerable populations to physical and mental disorders due to COVID-19 [15, 16]. Several studies have been performed to measure the QoL of HCWs [17, 18], including one study that attempted to measure ProQoL [18]. However, this previous study was conducted with only a small sample size, with the main objective of validating the ProQoL instrument. Given the matter that ProQoL is an individual’s perception about their work aspects, therefore, it is highly dependent on contextual background, socioeconomic and workplace characteristics. Therefore, more evidence should be provided about the ProQoL of HCWs, particularly among frontline HCWs during an epidemic, in order to develop appropriate interventions to improve the ProQoL of HCWs.
This study aimed to measure the ProQoL of HCWs in an urban hospital in Vietnam and identify associated factors after the epidemic.
Instrument and Methods
Study design and setting
A cross-sectional study was conducted on an urban hospital in Hanoi, Vietnam, from July to September 2022. Participants were HCWs who worked in the hospital for at least three months, voluntarily participated in the study, and gave written informed consent. Individuals working in the hospital for less than three months, having acute illnesses, or disagreeing to participate in the study were excluded. We included all people who met the eligibility criteria. A total of 924 participants were recruited in the study.
Data collection
A self-reported structured questionnaire was developed and distributed to the participants. The questionnaire's contents were piloted in 10 participants and revised according to their feedback. Each participant spent 10-15 minutes completing the Socio-demographic questionnaire (job characteristics, age, gender, education, marital status, years of experience, position, time working per day and week, number of days on duty per week, and changing the amount of work or income during the COVID-19 pandemic). The Professional Quality of Life Scale for Health Workers (Pro-Qol Health) was employed [19]. The instrument consists of 30 items, which encompass five domains; Compassion Satisfaction (CS), Perceived Support (PS), Burnout (BO), Secondary Traumatic Stress (STS), and Moral Distress (MD). Each section comprises six inquiries, with the responses allocated a corresponding numerical value on a scale of 1 (Never), 2 (Rarely), 3 (Sometimes), 4 (Often), and 5 (Very often). The upper limit for the cumulative score in each domain is 30 points. The evaluation of each aspect was conducted based on its corresponding score, which was categorized into three levels: 1) Low, indicating a score of 12 or less; 2) Average, representing a score within the range of 13 to 23; And 3) High, indicating a score of 24 or more. The Cronbach alpha test was conducted to assess the alpha value for Pro-Qol Health and its respective domains, including CS, PS, BO, STS, and MD, yielding values of 0.84, 0.87, 0.82, 0.82, 0.74, and 0.70. The Vietnamese version of Pro-Qol Health has been validated elsewhere [18].
Statistical analysis
The data was analyzed using the Stata 14.0 by Chi-square test and the Kruskal-Wallis test to discern disparities in ratios or means among various groups based on variations in working time (whether it increased, remained constant, or decreased) after the COVID-19 pandemic. The associated parameters with each domain of healthcare workers' professional quality of life were investigated using multivariate Tobit regression models. A forward stepwise selection approach was employed to eliminate variables that were not statistically significant, whereby the criterion for selection of variables in the reduced models was set at a p-value of less than 0.2 for the log-likelihood ratio test. A p-value below the threshold of 0.05 was deemed to indicate statistical significance.
Findings
The average age of the participants was 37.2±7.9. There was no significant difference between the age groups of the participants according to their viewpoint on the amount of work (increase/constant/decrease) during the pandemic (p=0.21).
Men comprised 31.4% of the sample, with a significantly smaller proportion experiencing an increased workload during the pandemic compared to women. The percentages of participants possessing undergraduate, graduate, and postgraduate education were 22.0, 35.4, and 40.6%, respectively (Table 1).
Table 1. Comparing the frequency (the numbers in parentheses are percentages) of participants’ viewpoints on the amount of work during the pandemics according to the sociodemographic characteristics (n=924)
The majority of participants were nurses (43.9%), and their mean experience was 12.9±8.6 years. There was no significant difference between the participants' years of experience groups according to their viewpoint on the amount of work (increase/constant/decrease) during the pandemic (p=0.18).
Nurses experienced the greatest surge in workload during the pandemic, while doctors had the least increase compared to their regular duties (p<0.01). The mean number of working days per week was 5.3±0.6 days per week, the mean number of days on duty per week was 1.3±1.0 days, and the mean number of working hours per day of 8.7±1.8 hours per day. The majority of individuals experienced a decline or no change in their incomes throughout the duration of the pandemic.
Table 2. Comparing the frequency (the numbers in parentheses are percentages) of participants’ viewpoints on the amount of work during the pandemics according to the job characteristics (n=924)
The mean professional quality of life scores for HCWs in the CS, PS, BO, STS, and MD categories were 20.6±3.5, 20.4±3.4, 17.6±3.5, 16.6±3.2, and 16.3±3.4, respectively. The proportion of HCWs who had the lowest levels of CS (1.9%) and PS (2.1%) was the lowest among all groups (Figure 1).
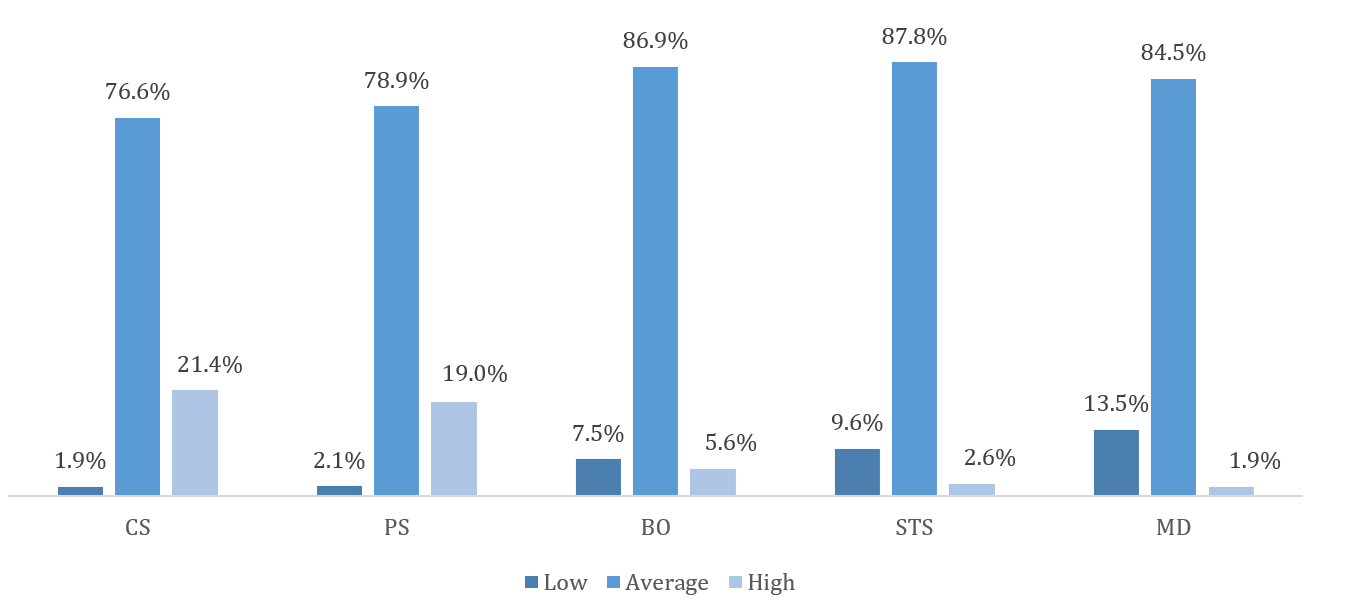
Figure 1. Professional quality of life among healthcare workers
Regarding sociodemographic characteristics, being female was positively associated with the PS domain (r=0.7) but negatively related to STS (r=-0.9) and MD domains (r=-0.9). Living with a spouse/partner was positively associated with the CS domain (r=0.6). Lower education level was negatively correlated with CS and PS scores. Regarding job characteristics, participants having other professionals (e.g., technicians, midwifery, etc.) had higher CS (r=0.9) and PS (r=1.1) scores but lower BO (r=-1.0), STS (r=-0.6) and MD scores (r=-0.6). Being staff was negatively associated with CS and PS scores. Higher working days per week were negatively correlated with CS (r=-0.4) and PS scores (r=-0.4), while a higher number of working hours per day was positively correlated with BO (r=0.2) and STS scores (r=0.1). Participants with stable or decreased incomes had significantly higher BO scores than those with increased income. In addition, participants with a stable amount of work had a lower PS score, while those with a decreased amount of work had lower BO and STS scores (Table 3).
Table 3. Factors associated with Compassion Satisfaction (CS), Perceived Support (PS), Burnout (BO), Secondary Traumatic Stress (STS), and Moral Distress (MD) among participants
Discussion
The results showed a moderate professional quality of life among Vietnamese HCWs after the COVID-19 pandemic. Moreover, we found different demographic and job characteristics that were related to the professional quality of life, which could be potentially used to develop appropriate interventions to improve the ProQoL of HCWs.
The present study employed the Pro-Qol Health instrument to assess the professional quality of life of HCWs. Findings suggested that Vietnamese HCWs had moderate professional quality of life, aligning with a study of Portuguese physicians and nurses during the third wave of the COVID-19 pandemic, which showed a moderate level of CS, BO, and STS among these HCWs [20]. Indeed, this study was performed during the latter half of 2022, when a global subjugation of the COVID-19 pandemic was observed. In the context of Vietnam, the current phase could be denoted as the new normal post-COVID-19 stage. Hence, it is evident that there exists minimal disparity in the overall professional well-being experienced by HCWs in the immediate aftermath of the pandemic when compared to the initial outbreak phase. The professional life of HCWs has been profoundly impacted since the onset of the epidemic, leading to a discernible decline in its overall quality.
Regarding specific domains of ProQoL, CS occurs when empathy motivates healthcare professionals to relieve patient pain. CS is the satisfaction that HCWs find in productivity, aiding them in managing work challenges [21]. Meanwhile, PS is the awareness of HCWs’ access to practical work support when needed, including task performance, advice, or emotional support. A higher PS score corresponds to better support [19]. CS and PS are powerful aspects of professional quality of life. In this study, high-grade CS and PS accounted for approximately 20%, which was higher than a prior report in Spain during the pandemic with 18.2% [20], but lower than a study in China (35.3%) [22]. Cuartero-Castañer et al. suggested that the social recognition of HCWs during the epidemic may cause a high prevalence of CS [23]. CS and PS scores were higher in other HCWs, such as technicians, midwives, and pharmacists, than doctors, which might be explained by the matter in the increasing workload during the outbreak among other HCWs. According to Wu et al., working at the frontline positively affects CS [24]. Increased workloads during an epidemic may promote satisfaction due to a deeper sense of self-employment in the fight against the epidemic. Crediting overworked HCWs during the pandemic can boost support for them and increase PS. Women had higher PS scores than men, which might be due to women having more relationships and social support compared to men [25]. HCWs living with spouses had higher CS scores than those who are single, which could be explained that these HCWs developed coping mechanisms [23], and they sought help from their parents to take care of their families because they were usually on duty [20]. CS and PS scores were also reported to be significantly lower in those with undergraduate/graduate education, and lower in staff versus management groups. Prior research suggested that HCWs with better clinical skills might have higher CS levels [26]. Indeed, HCWs with higher education levels were often appointed to management positions, which might result in better CS than those who were staff. Furthermore, there is evidence that managers tended to have better friendships and more support in the workplace [27].
Burnout refers to feelings of hopelessness that make it challenging to be productive at work. Meanwhile, STS is exposure to traumatic events at work, like witnessing suffering, violence, or death; While MD refers to when frontline HCWs have to act against personal values and ethics [19]. These vulnerabilities can cause medical errors and impact patient care [28] and professional relationships [29]. Our study showed a pervasiveness of moderate levels of BO, STS, and MD, which was different from prior studies [20, 22, 30]. However, the low rate of high levels of BO, STS, and MD in our study could be explained by the commonness of CS. Indeed, CS could play a role as a protective factor, which helped to lower STS and BO [31]. During the epidemic, the role of HCWs was enhanced, which boosted CS and, eventually, positively impacted STS and BO. Nonetheless, at the time of this investigation, HCWs in Vietnam had not only failed to recognize the worthy efforts in fighting the epidemic but also faced public criticism, which might explain the high scores of BO, STS, and MD.
Regression analysis showed that women had lower STS and MD levels than men. This result was different from other reports showing that women were at higher risk of STS than men because they had a more sensitive hypothalamic-pituitary gland [31-33]. We supposed that females had a higher score of PS than their male counterparts, which helps balance the BO, STS, and MD factors. In addition, the analysis showed that the increased number of working hours per day increased the levels of BO and STS among HCWs, which was in line with other studies [34-36]. Healthcare workers with stable or reduced income during the pandemic had higher BO levels. In Vietnam, during the pandemic, HCWs still work despite the colonial expansion, and many HCWs exceeded their expected workload while their income increased significantly. Some authors have shown that income affects the quality of health workers' professional life [37, 38]. Moreover, job satisfaction increases when employees are paid fairly, reducing financial burdens and improving conditions for professional activities [37].
This study is among a few research using the Pro-Qol Health instrument to describe the professional quality of life among HCWs in Vietnam post-pandemic. The study helps improve healthcare services in the new normal. However, this study has limitations. The study was conducted at an urban hospital, which hinder the generalizability of the study’s findings to HCWs in Vietnam. Furthermore, the absence of evidence from the Pro-Qol Health tool hinders comparisons of study results with other studies. Finally, the cross-sectional descriptive study design limits the ability to conclude a causal relationship.
Conclusion
This study showed a moderate professional quality of life among Vietnamese HCWs after the COVID-19 pandemic. Strengthening the healthcare system's capacity should be a top priority, along with supporting healthcare professionals in managing stress and developing psychological resilience, to improve HCWs' ProQoL.
Acknowledgments: We would like to thank Vietnam National University, Hanoi (VNU), and the staff of Saint Paul Hospital for supporting us throughout the research process.
Ethical Permissions: The research has been approved by the Institutional Review Board, University of Public Health. No. 426/2023/YTCC-HD3, November 16, 2023.
Conflict of Interest: Nothing to be reported.
Authors’ Contribution: Trung NT (First Author), Methodologist (12.5%); Long ND (Second Author), Methodologist (12.5%); Huong TL (Third Author), Main Researcher (12.5%); Thuan DT (Fourth Author), Main Researcher (12.5%); Tam NT (Fifth Author), Statistical Analyst (12.5%); Phuong Lan NT (Sixth Author), Assistant Researcher (12.5%); Tuan MD (Seventh Author), Assistant Researcher (12.5%); Bach NX (Eighth Author), Introduction Writer (12.5%)
Funding/Support: This research was funded by the research project QG (QGSP.2022.07) of Vietnam National University, Hanoi.
Article Type: Descriptive & Survey |
Subject:
Family Health Education/Promotion
Received: 2024/03/22 | Accepted: 2024/04/30 | Published: 2024/05/20
Received: 2024/03/22 | Accepted: 2024/04/30 | Published: 2024/05/20
References
1. Halcomb E, McInnes S, Williams A, Ashley C, James S, Fernandez R, et al. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J Nurs Scholarsh. 2020;52(5):553-63. [Link] [DOI:10.1111/jnu.12589]
2. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, Carmona-Rega MI, Sánchez-Ruiz MJ, Ortega-Galán Á M. Professional quality of life, self-compassion, resilience, and empathy in healthcare professionals during COVID-19 crisis in Spain. Res Nurs Health. 2021;44(4):620-32. [Link] [DOI:10.1002/nur.22158]
3. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-7. [Link] [DOI:10.1016/j.bbi.2020.05.026]
4. Mahmud S, Hossain S, Muyeed A, Islam MM, Mohsin M. The global prevalence of depression, anxiety, stress, and, insomnia and its changes among health professionals during COVID-19 pandemic: A rapid systematic review and meta-analysis. Heliyon. 2021;7(7):e07393. [Link] [DOI:10.1016/j.heliyon.2021.e07393]
5. Roney LN, Acri MC. The cost of caring: An exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. J Pediatr Nurs. 2018;40:74-80. [Link] [DOI:10.1016/j.pedn.2018.01.016]
6. Hegney DG, Craigie M, Hemsworth D, Osseiran-Moisson R, Aoun S, Francis K, et al. Compassion satisfaction, compassion fatigue, anxiety, depression and stress in registered nurses in Australia: Study 1 results. J Nurs Manag. 2014;22(4):506-18. [Link] [DOI:10.1111/jonm.12160]
7. Yadollahi M, Razmjooei A, Jamali K, Niakan MH, Ghahramani Z. The relationship between professional quality of life (ProQol) and general health in Rajaee trauma hospital staff of Shiraz, Iran. Shiraz E Med J. 2016;17(9):e39253. [Link] [DOI:10.17795/semj39253]
8. Zhang YY, Han WL, Qin W, Yin HX, Zhang CF, Kong C, et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: A meta-analysis. J Nurs Manag. 2018;26(7):810-9. [Link] [DOI:10.1111/jonm.12589]
9. Amin AA, Vankar JR, Nimbalkar SM, Phatak AG. Perceived stress and professional quality of life in neonatal intensive care unit nurses in Gujarat, India. Indian J Pediatr. 2015;82(11):1001-5. [Link] [DOI:10.1007/s12098-015-1794-3]
10. Alyahya S, AboGazalah F. Work-related stressors among the healthcare professionals in the fever clinic centers for individuals with symptoms of COVID-19. Healthcare. 2021;9(5):548. [Link] [DOI:10.3390/healthcare9050548]
11. Said RM, El-Shafei DA. Occupational stress, job satisfaction, and intent to leave: Nurses working on front lines during COVID-19 pandemic in Zagazig City, Egypt. Environ Sci Pollut Res Int. 2021;28(7):8791-8801. [Link] [DOI:10.1007/s11356-020-11235-8]
12. Blumenthal D, Fowler EJ, Abrams M, Collins SR. Covid-19-implications for the health care system. N Engl J Med. 2020;383(15):1483-8. [Link] [DOI:10.1056/NEJMsb2021088]
13. Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293-306. [Link] [DOI:10.1016/j.bpa.2020.11.009]
14. WHO. Coronavirus (COVID-19) in Vietnam [Internet]. Geneva: World Health Organization; 2023 [cited 2023; Aug; 25]. Available from: https://covid19.who.int/region/wpro/country/vn. [Link]
15. Tran B, Nguyen MT, Auquier P, Boyer L, Fond G, Vu GT, et al. Psychological impacts of COVID-19 on Vietnamese health workers over the prolonged restricted COVID-19 responses: A cross-sectional study. BMJ Open. 2023;13(8):e069239. [Link] [DOI:10.1136/bmjopen-2022-069239]
16. Hoang TD, Colebunders R, Fodjo JNS, Nguyen NPT, Tran TD, Vo TV. Well-being of healthcare workers and the general public during the COVID-19 pandemic in Vietnam: An online survey. Int J Environ Res Public Health. 2021;18(9):4737. [Link] [DOI:10.3390/ijerph18094737]
17. Minh LD, Phan HH, Le Mai DN, Dat NT, Tri NM, Ha NV, et al. Pattern and perceived changes in quality of life of Vietnamese medical and nursing students during the COVID-19 pandemic. PLoS One. 2022;17(12):e0279446. [Link] [DOI:10.1371/journal.pone.0279446]
18. Tran ANP, To QG, Huynh VN, Le KM, To KG. Professional quality of life and its associated factors among Vietnamese doctors and nurses. BMC Health Serv Res. 2023;23(1):924. [Link] [DOI:10.1186/s12913-023-09908-4]
19. The Center for Victims of Torture. Professional Quality of Life scale for health worker (Pro-Qol Health) toolkit. Version 1. 2021 [cited 2023; Aug; 25]. Available from: https://proqol.org/proqol-health-1. [Link]
20. Serrão C, Martins V, Ribeiro C, Maia P, Pinho R, Teixeira A, et al. Professional quality of life among physicians and nurses working in Portuguese hospitals during the third wave of the COVID-19 pandemic. Front Psychol. 2022;13:814109. [Link] [DOI:10.3389/fpsyg.2022.814109]
21. Bahari G, Asiri K, Nouh N, Alqahtani N. Professional quality of life among nurses: Compassion satisfaction, burnout, and secondary traumatic stress: A multisite study. SAGE Open Nurs. 2022;8:23779608221112329. [Link] [DOI:10.1177/23779608221112329]
22. Niu A, Li P, Duan P, Ding L, Xu S, Yang Y, et al. Professional quality of life in nurses on the frontline against COVID-19. J Nurs Manag. 2022;30(5):1115-24. [Link] [DOI:10.1111/jonm.13620]
23. Cuartero-Castañer ME, Hidalgo-Andrade P, Cañas-Lerma AJ. Professional quality of life, engagement, and self-care in healthcare professionals in ecuador during the COVID-19 pandemic. Healthcare. 2021;9(5):515. [Link] [DOI:10.3390/healthcare9050515]
24. Wu Y, Wang J, Luo C, Hu S, Lin X, Anderson AE, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag. 2020;60(1):e60-5. [Link] [DOI:10.1016/j.jpainsymman.2020.04.008]
25. Kneavel M. Relationship between gender, stress, and quality of social support. Psychol Rep. 2021;124(4):1481-501. [Link] [DOI:10.1177/0033294120939844]
26. Kim K, Han Y, Kwak Y, Kim JS. Professional quality of life and clinical competencies among Korean nurses. Asian Nurs Res. 2015;9(3):200-6. [Link] [DOI:10.1016/j.anr.2015.03.002]
27. Lin CT. Relationship between job position, job attributes, and workplace friendship: Taiwan and China. J Technol Manag China. 2010;5(1):55-68. [Link] [DOI:10.1108/17468771011032796]
28. Dewar B. Cultivating compassionate care. Nurs Stand. 2013;27(34):48-55. [Link] [DOI:10.7748/ns2013.04.27.34.48.e7460]
29. Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: A systematic review. Int J Environ Res Public Health. 2016;13(6):618. [Link] [DOI:10.3390/ijerph13060618]
30. Zakeri MA, Ghaedi-Heidari F, Khaloobagheri E, Hossini Rafsanjanipoor SM, Ganjeh H, Pakdaman H, et al. The relationship between nurse's professional quality of life, mindfulness, and hardiness: A cross-sectional study during the COVID-19 outbreak. Front Psychol. 2022;13:866038. [Link] [DOI:10.3389/fpsyg.2022.866038]
31. Magnavita N, Tripepi G, Di Prinzio RR. Symptoms in health care workers during the COVID-19 epidemic. A cross-sectional survey. Int J Environ Res Public Health. 2020;17(14):5218. [Link] [DOI:10.3390/ijerph17145218]
32. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arc Gen Psychiatry. 2005;62(6):617-27. [Link] [DOI:10.1001/archpsyc.62.6.617]
33. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959-92. [Link] [DOI:10.1037/0033-2909.132.6.959]
34. Goehring C, Bouvier Gallacchi M, Künzi B, Bovier P. Psychosocial and professional characteristics of burnout in Swiss primary care practitioners: A cross-sectional survey. Swiss Med Wkly. 2005;135(7-8):101-8. [Link]
35. Benson MA, Peterson T, Salazar L, Morris W, Hall R, Howlett B, et al. Burnout in rural physician assistants: An initial study. J Physician Assist Educ. 2016;27(2):81-3. [Link] [DOI:10.1097/JPA.0000000000000069]
36. Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, et al. High level of burnout in intensivists: Prevalence and associated factors. Am J Respir Crit Care Med. 2007;175(7):686-92. [Link] [DOI:10.1164/rccm.200608-1184OC]
37. Sawatzky JA, Enns CL. Exploring the key predictors of retention in emergency nurses. J Nurs Manag. 2012;20(5):696-707. [Link] [DOI:10.1111/j.1365-2834.2012.01355.x]
38. Samios CJM. Burnout and psychological adjustment in mental health workers in rural Australia: The roles of mindfulness and compassion satisfaction. Mindfulness. 2018;9(4):1088-99. [Link] [DOI:10.1007/s12671-017-0844-5]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |