Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 255-260 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fadliyah L, Hendarto H, Sudaryanti L, Susilo I, Mardika A, Iswatun I, et al . Increasing Menopausal Women’s Knowledge of Independent Ending of Contraception through Education. Health Educ Health Promot 2024; 12 (2) :255-260
URL: http://hehp.modares.ac.ir/article-5-74592-en.html
URL: http://hehp.modares.ac.ir/article-5-74592-en.html
L. Fadliyah *1, H. Hendarto1, L. Sudaryanti1, I. Susilo2, A. Mardika1, I. Iswatun1, E. Sulfat1, I.I. Hassan3
1- Faculty of Medicine, Airlangga University, Surabaya, Indonesia
2- Faculty of Medicine and Health, Sepuluh Nopember Institute of Technology, Surabaya, Indonesia
3- School of Health Science, University of Malaysia, Kuala Lumpur, Malaysia
2- Faculty of Medicine and Health, Sepuluh Nopember Institute of Technology, Surabaya, Indonesia
3- School of Health Science, University of Malaysia, Kuala Lumpur, Malaysia
Full-Text [PDF 583 kb]
(2609 Downloads)
| Abstract (HTML) (1504 Views)
Full-Text: (338 Views)
Introduction
According to the World Health Organization (WHO), menopause is defined as the permanent cessation of menstruation in women, typically resulting from the loss of ovarian follicle activity or their non-functioning. It is commonly viewed as the conclusion of a woman’s reproductive capability. Menopause usually occurs between the ages of 45 and 55 as a natural aspect of the aging process [1]. Women undergoing menopause undergo significant fluctuations in gonadal hormone levels, including a decline in estradiol levels. Women aged 40-52 who use contraception exhibit strong motivation for various reasons, including concerns about unplanned pregnancy, adjustments in contraceptive methods over time due to health issues, experiencing symptoms of perimenopause without full awareness, and past negative encounters with contraceptive methods and traumatic life events [2].
Hormonal changes in menopausal women may lead to symptoms, such as hot flashes, sleep disturbances, night sweats, irritability, and mild cognitive impairment (MCI) [3]. During menopause, women no longer require contraception as the ovaries cease egg production, preventing fertilization [4]. Some women may not realize they have reached menopause and continue to use contraception to prevent unwanted pregnancies [5]. There are women who actively use contraceptives upon entering menopause, although the proportion of contraceptive users is not substantial [6, 7]. Various factors influencing continued contraceptive use in Indonesia include the woman’s age, number of children, level of education, socioeconomic status, and access to information [8].
In Indonesia, women show significant interest in various contraceptive methods, particularly short-term options, like pills and injections [9], as well as long-term methods, such as the intrauterine device (IUD) [10] and implants [11]. The side effects of contraception use can vary, including menstrual cycle disruptions and the possibility of experiencing amenorrhea (lack of menstruation) [12], a common occurrence with hormonal contraceptive use. Hormonal contraceptives can impact the menstrual cycle in two ways: either by maintaining cyclic bleeding or by suppressing part or all of the regular cycle [13]. Non-hormonal contraception, like the copper IUD, offers an alternative [14]. This type of IUD contraception can aid in menopause detection by not causing amenorrhea, which can complicate the recognition of menopausal symptoms [15].
Insufficient awareness about contraception among postmenopausal women can elevate the chances of unintended pregnancies or heighten health risks, particularly for individuals with specific health issues like heart disease or high blood pressure. Simultaneously, a lack of access to precise information and education on contraception can pose challenges. Various obstacles hinder menopausal women from making well-informed decisions about contraceptive methods that align with their requirements and health circumstances [16]. Hence, it is crucial to offer trustworthy sources of information and comprehensive education to empower menopausal women to make informed choices and grasp the health consequences associated with their contraceptive decisions [17].
According to Minister of Health Regulation Number 28 of 2017 Article 18, midwives are explicitly authorized to offer counseling and services related to reproductive health and family planning (KB) to women [18]. With this mandate, midwives can play a pivotal role in enhancing women’s knowledge and comprehension of various crucial aspects of reproductive health [19]. By delivering high-quality education and counseling, midwives can furnish women with precise, evidence-based information on family planning concepts, available contraceptive methods, the advantages and risks associated with each method, and instructions on safe and effective usage [20]. Additionally, midwives can aid women in understanding the bodily changes during the reproductive cycle and provide emotional and practical support in managing any reproductive health issues they may encounter [21]. Therefore, this regulation establishes a robust framework for midwives to enhance women’s reproductive health through comprehensive and scientifically grounded education and counseling [22].
Support from individuals closest to women undergoing menopause, such as spouses, friends, and family members, holds significant importance [23]. This support serves not only as a source of moral encouragement but also as a cornerstone for women to navigate the physical, emotional, and hormonal changes that accompany this transitional phase [24]. Through this assistance, women in menopause can feel more self-assured in adapting to shifts in their surroundings and daily circumstances [25]. Support from close individuals forms a crucial aspect of social support, fostering comfort, attention, recognition, and aid in embracing the challenges faced [26]. Whether received individually or in group settings, this support fosters a sense of community and empathy that aids women in confronting the hurdles of menopause [27]. Hence, enhancing relationships and communication with those nearest and dearest is vital in bolstering support for women undergoing menopause [28].
The objective of this study was to assess the impact of educational interventions on contraceptive discontinuation among menopausal women. In a practical sense, this research aimed to offer valuable insights to healthcare providers regarding the efficacy of educational interventions in influencing changes in contraceptive usage among women transitioning into menopause. Furthermore, from a theoretical perspective, this study sought to make a substantial scientific contribution by enhancing theoretical knowledge, particularly in comprehending the framework and dynamics of enhancing well-being for women undergoing menopause. Therefore, this research holds practical significance within the realm of reproductive health services and is anticipated to make a noteworthy contribution to theoretical advancements and our comprehension of well-being and the menopausal experience at an academic level.
Instrument and Methods
Research design
The quantitative research employed a pre-experimental design utilizing a one-group pre-test and post-test design approach and was conducted on women visiting the Lontar Community Health Center in Surabaya, East Java, between January and March 2022. This methodology enables researchers to directly assess changes before and after intervention within the same group of participants.
Participants
The study’s population comprised all women aged 40-55 years actively using contraception, of whom 112 women who met the inclusion criteria were selected using non-probability sampling, specifically an accidental sampling method. In this method, the subjects are chosen based on their availability and accessibility, without adhering to the random representativeness typically associated with probability sampling techniques. This method enables researchers to secure a representative sample from the target population by capitalizing on field situations and adhering to predetermined inclusion criteria. While this method does not yield a random sample, selecting subjects attending healthcare facilities allows for substantial coverage of the relevant population and facilitates a more comprehensive analysis of the impact of educational interventions on contraceptive discontinuation among postmenopausal women.
Variables and data collection
The independent variable was educational modeling, while the dependent variables were knowledge and self-termination of contraception among women entering menopause. The research instrument comprised a questionnaire with 30 questions derived from a literature review, which included 25 questions related to knowledge and five questions concerning self-termination of contraception. Knowledge responses were assessed using a two-point scale (right and wrong), whereas responses regarding the independent termination of contraception were evaluated using a three-point scale (ending contraceptive use, doubtful, and not ending). The validity of the instrument was tested using the product-moment correlation, where all attitude question items in the questionnaire exhibited a significance value of <0.05. The reliability of the instrument was assessed using Cronbach’s alpha, yielding a value of 0.80.
The researcher thoroughly explained the research’s scope and objectives to the women and provided a questionnaire sheet and detailed instructions on how to complete it. Participants were then requested to fill out a pre-test questionnaire before the educational intervention. Following the pre-test, educational materials were presented to the participants for approximately 30 minutes. A discussion session ensued to reinforce understanding about menopause. The questionnaire content focused on comprehending physical and psychological signs related to menopause and managing associated symptoms. Following the educational intervention, participants completed a post-test by re-filling the questionnaire three months later through a Google form sent via WhatsApp.
Statistical analysis
The normality of data was assessed by the Kolmogorov-Smirnov test with a significance value of 0.01, revealing that the data did not follow a normal distribution. The data utilized an ordinal scale, categorizing levels of knowledge and termination of contraception into three groups, including high (scores 76-100%), medium (scores 56-75%), and low (scores below 56%). Data analysis was conducted using the Wilcoxon Signed Rank test with a significance level of p<0.05, utilizing SPSS 22.0. This analytical approach was selected for its ability to effectively handle ordinal and non-normally distributed data, enabling researchers to assess differences before and after the intervention at a predetermined significance level. Consequently, the data analysis was meticulously performed to yield valid and reliable insights into the impact of educational interventions on contraceptive discontinuation among menopausal women.
Findings
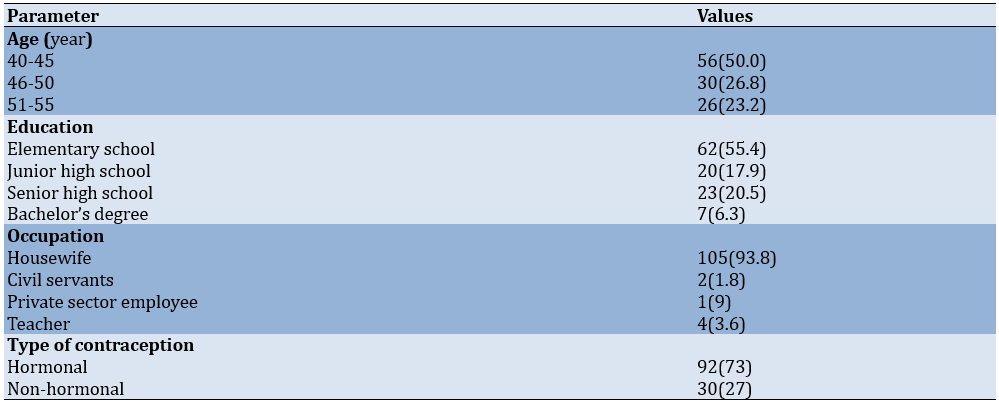
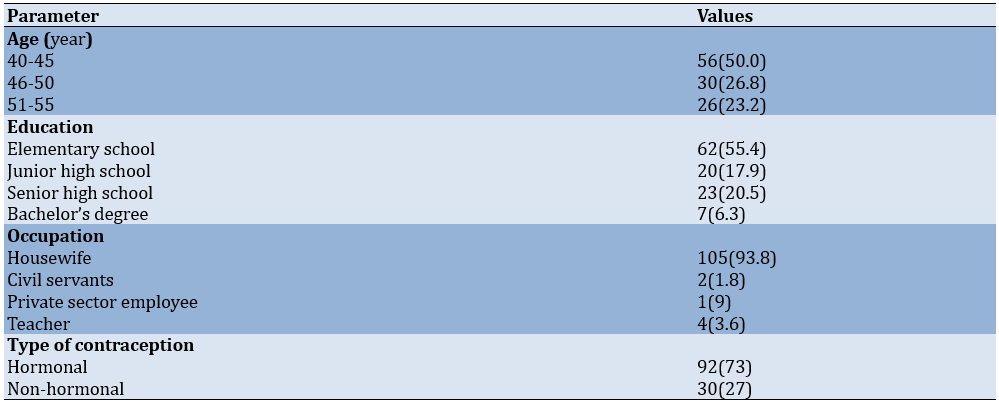
This study assessed 112 women aged 40-55 years actively using contraception (Table 1).
Table 1. Frequency of respondents’ demographic characteristics and type of contraception
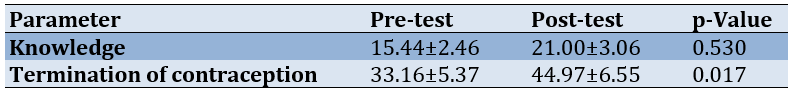
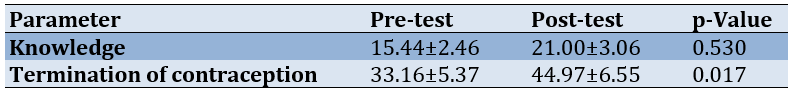
The pre- and post-test analysis revealed significant changes in knowledge (p<0.001) and contraceptive discontinuation among respondents. The comparison between pre- and post-education on menopause, demonstrated a notable increase in knowledge and actions related to contraceptive cessation across all groups (p<0.05; Table 2). Therefore, the educational intervention effectively impacted the enhancement of respondents’ knowledge and understanding regarding menopause, influencing their decisions concerning contraceptive discontinuation positively.
Table 2. Mean values of pre- and post-test analysis
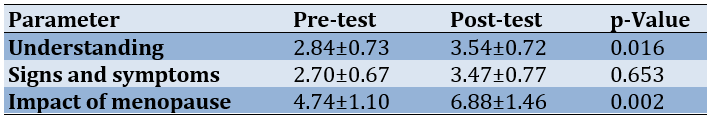
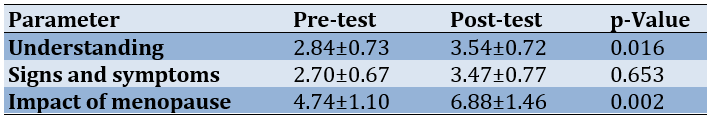
The results of the pre- and post-test analyses revealed a substantial improvement in respondents’ characteristics concerning knowledge about menopause. Particularly, according to the Wilcoxon Signed Rank test, there was a significant rise in the average score from the pre-test to the post-test across all aspects examined, including understanding, signs and symptoms, and the impact of menopause (p<0.05; Table 3).
Table 3. Differences in mean pre- and post-test knowledge about menopause
Discussion
We assessed the impact of educational interventions on contraceptive discontinuation among menopausal women. The results indicated a positive influence of health education interventions on knowledge about menopause and decisions regarding independent termination of contraception among menopausal women. Enhancing knowledge about menopause through health education interventions serves as an initial step in fostering positive behaviors among women transitioning into menopause, enabling them to recognize signs, and symptoms, and make informed choices about discontinuing contraception independently. Offering health education stands as an effective strategy to boost knowledge, shape attitudes, and prompt actions [29].
Women approaching menopause often misunderstand signs and symptoms, mistaking them for age-related complaints. They may not recognize these symptoms as being linked to menopause. Common menopausal symptoms include changes in the menstrual cycle, hot flashes, hair loss, dry skin, breast sagging, weight gain, sexual changes, sleep disturbances, and mental-emotional issues [30]. The average age range for menopause falls between 45 to 55 years, with an estimated age typically ranging from 50 to 52 years, where 45 signifies early menopause [19]. In India, women experience menopause at around 46.2 years, notably younger than women in Western countries (averaging 51 years). The average age for natural menopause is approximately 48.94 years [31]. Factors, such as a woman’s age, use of exogenous hormones, number of childbirths, duration of breastfeeding, lifestyle choices, and health conditions influence the age at which women undergo menopause across different regions [30]. Women who undergo early menopause (before 40 years) face a higher risk of cardiovascular disease [32].
The continuous use of hormonal contraceptives has the potential to disrupt the menstrual cycle, leading to challenges in identifying the onset of menopause. Side effects associated with hormonal contraceptive use may include prolonged menstruation, amenorrhea (lack of menstruation), as well as symptoms, like headaches, dizziness, lower abdominal or back pain, and weight gain. While hormonal contraception is an effective means of preventing pregnancy, it is crucial to acknowledge that its usage can influence the natural hormonal equilibrium within a woman’s body. Therefore, individuals utilizing hormonal contraceptives should be aware of potential side effects and carefully evaluate contraceptive options that align with their specific needs and health conditions [33, 34].
Women with a comprehensive understanding of menopause can make informed decisions about discontinuing contraception independently. Adequate knowledge is crucial for women to recognize their infertility status. Once menopause sets in, pregnancy becomes unlikely. Uncertainty or failure to identify menopausal symptoms may lead women to continue contraceptive use unnecessarily. Enhanced knowledge correlates with improved health behaviors [35]. The level of health knowledge and behavior can be affected by various factors, including age, economic status, educational attainment, proximity to healthcare facilities, and disposable personal income (DPI). Health education plays a significant role in shaping the knowledge and attitudes of adolescent health cadres (KKR) concerning the consumption of iron tablets [36].
This situation is concerning because while menopausal symptoms can significantly impact quality of life, having a better understanding of menopause is crucial as it is linked to an improved quality of life. Interestingly, postmenopausal women reported feeling more knowledgeable than other groups, possibly due to their experiences during perimenopause and their ongoing learning process. When asked about their initial thoughts on menopause, the most common age range for considering this topic was between 40 and 49 years. This suggests that many women only begin contemplating menopause as they approach the age of experiencing it. Moreover, many women mention that they only started thinking about menopause when symptoms started to manifest, or in some instances, due to early menopause. This highlights a lack of readiness for menopause, potentially exacerbating the emotional and psychological toll of the transition. The lack of awareness about menopausal symptoms often leads to delays in diagnosing perimenopause and receiving appropriate advice and treatment.
The knowledge acquired through educational interventions enables women to gain a deeper understanding of menopausal signs, symptoms, and impacts, empowering them to make well-informed choices regarding discontinuing contraception. The results also indicated that a comprehensive understanding of menopause and contraception can alleviate confusion and uncertainty during this phase of a woman’s life cycle. Furthermore, the study highlighted that the continuous use of hormonal contraceptives may disrupt the menstrual cycle, potentially hindering the identification of menopausal onset. This underscores the significance of comprehending the side effects and consequences of hormonal contraceptive use, emphasizing the importance of carefully selecting a contraceptive method that aligns with individual health requirements and preferences.
The limitation of this research is that we only examined increasing menopausal women's knowledge about stopping contraceptives independently through education.
Conclusion
Health education interventions play a crucial role in enhancing knowledge and actions about menopause and the independent cessation of contraception among menopausal women.
Acknowledgments: We wish to extend our deepest gratitude to the dean, department head, and study program head at the Faculty of Vocational Studies, Airlangga University, for their unwavering support throughout the research process. Additionally, we would like to convey our utmost appreciation to the head of the Community Health Center for permitting us to conduct our research at the Lontar Community Health Center in Surabaya, East Java. Lastly, we are grateful to the respondents who generously dedicated their time to participate in our study. Special thanks are also due to the research ethical clearance team at the Muhammadiyah University of Gresik for facilitating the ethical approval process.
Ethical Permissions: The research received ethical approval from the Research Ethics Committee of the Faculty of Health, Muhammadiyah University of Gresik (081/KET/IL3-UMG/KEP/A/2022). Also, the respondents signed the informed consent form.
Conflicts of Interests: All authors declared no conflicts of interests.
Authors’ Contribution: Fadliyah L (First Author), Introduction Writer/Main Researcher (20%); Hendarto H (Second Author), Introduction Writer/Assistant Researcher (20%); Sudaryanti L (Third Author), Methodologist (10%); Susilo I (Fourth Author), Methodologist (10%); Mardika A (Fifth Author), Assistant Researcher (10%); Iswatun I (Sixth Author), Discussion Writer (10%); Sulfat E (Seventh Author), Discussion Writer (10%); Hassan II (Eighth Author), Discussion Writer/Statistical Analyst (10%)
Funding/Support: This study received no funding.
According to the World Health Organization (WHO), menopause is defined as the permanent cessation of menstruation in women, typically resulting from the loss of ovarian follicle activity or their non-functioning. It is commonly viewed as the conclusion of a woman’s reproductive capability. Menopause usually occurs between the ages of 45 and 55 as a natural aspect of the aging process [1]. Women undergoing menopause undergo significant fluctuations in gonadal hormone levels, including a decline in estradiol levels. Women aged 40-52 who use contraception exhibit strong motivation for various reasons, including concerns about unplanned pregnancy, adjustments in contraceptive methods over time due to health issues, experiencing symptoms of perimenopause without full awareness, and past negative encounters with contraceptive methods and traumatic life events [2].
Hormonal changes in menopausal women may lead to symptoms, such as hot flashes, sleep disturbances, night sweats, irritability, and mild cognitive impairment (MCI) [3]. During menopause, women no longer require contraception as the ovaries cease egg production, preventing fertilization [4]. Some women may not realize they have reached menopause and continue to use contraception to prevent unwanted pregnancies [5]. There are women who actively use contraceptives upon entering menopause, although the proportion of contraceptive users is not substantial [6, 7]. Various factors influencing continued contraceptive use in Indonesia include the woman’s age, number of children, level of education, socioeconomic status, and access to information [8].
In Indonesia, women show significant interest in various contraceptive methods, particularly short-term options, like pills and injections [9], as well as long-term methods, such as the intrauterine device (IUD) [10] and implants [11]. The side effects of contraception use can vary, including menstrual cycle disruptions and the possibility of experiencing amenorrhea (lack of menstruation) [12], a common occurrence with hormonal contraceptive use. Hormonal contraceptives can impact the menstrual cycle in two ways: either by maintaining cyclic bleeding or by suppressing part or all of the regular cycle [13]. Non-hormonal contraception, like the copper IUD, offers an alternative [14]. This type of IUD contraception can aid in menopause detection by not causing amenorrhea, which can complicate the recognition of menopausal symptoms [15].
Insufficient awareness about contraception among postmenopausal women can elevate the chances of unintended pregnancies or heighten health risks, particularly for individuals with specific health issues like heart disease or high blood pressure. Simultaneously, a lack of access to precise information and education on contraception can pose challenges. Various obstacles hinder menopausal women from making well-informed decisions about contraceptive methods that align with their requirements and health circumstances [16]. Hence, it is crucial to offer trustworthy sources of information and comprehensive education to empower menopausal women to make informed choices and grasp the health consequences associated with their contraceptive decisions [17].
According to Minister of Health Regulation Number 28 of 2017 Article 18, midwives are explicitly authorized to offer counseling and services related to reproductive health and family planning (KB) to women [18]. With this mandate, midwives can play a pivotal role in enhancing women’s knowledge and comprehension of various crucial aspects of reproductive health [19]. By delivering high-quality education and counseling, midwives can furnish women with precise, evidence-based information on family planning concepts, available contraceptive methods, the advantages and risks associated with each method, and instructions on safe and effective usage [20]. Additionally, midwives can aid women in understanding the bodily changes during the reproductive cycle and provide emotional and practical support in managing any reproductive health issues they may encounter [21]. Therefore, this regulation establishes a robust framework for midwives to enhance women’s reproductive health through comprehensive and scientifically grounded education and counseling [22].
Support from individuals closest to women undergoing menopause, such as spouses, friends, and family members, holds significant importance [23]. This support serves not only as a source of moral encouragement but also as a cornerstone for women to navigate the physical, emotional, and hormonal changes that accompany this transitional phase [24]. Through this assistance, women in menopause can feel more self-assured in adapting to shifts in their surroundings and daily circumstances [25]. Support from close individuals forms a crucial aspect of social support, fostering comfort, attention, recognition, and aid in embracing the challenges faced [26]. Whether received individually or in group settings, this support fosters a sense of community and empathy that aids women in confronting the hurdles of menopause [27]. Hence, enhancing relationships and communication with those nearest and dearest is vital in bolstering support for women undergoing menopause [28].
The objective of this study was to assess the impact of educational interventions on contraceptive discontinuation among menopausal women. In a practical sense, this research aimed to offer valuable insights to healthcare providers regarding the efficacy of educational interventions in influencing changes in contraceptive usage among women transitioning into menopause. Furthermore, from a theoretical perspective, this study sought to make a substantial scientific contribution by enhancing theoretical knowledge, particularly in comprehending the framework and dynamics of enhancing well-being for women undergoing menopause. Therefore, this research holds practical significance within the realm of reproductive health services and is anticipated to make a noteworthy contribution to theoretical advancements and our comprehension of well-being and the menopausal experience at an academic level.
Instrument and Methods
Research design
The quantitative research employed a pre-experimental design utilizing a one-group pre-test and post-test design approach and was conducted on women visiting the Lontar Community Health Center in Surabaya, East Java, between January and March 2022. This methodology enables researchers to directly assess changes before and after intervention within the same group of participants.
Participants
The study’s population comprised all women aged 40-55 years actively using contraception, of whom 112 women who met the inclusion criteria were selected using non-probability sampling, specifically an accidental sampling method. In this method, the subjects are chosen based on their availability and accessibility, without adhering to the random representativeness typically associated with probability sampling techniques. This method enables researchers to secure a representative sample from the target population by capitalizing on field situations and adhering to predetermined inclusion criteria. While this method does not yield a random sample, selecting subjects attending healthcare facilities allows for substantial coverage of the relevant population and facilitates a more comprehensive analysis of the impact of educational interventions on contraceptive discontinuation among postmenopausal women.
Variables and data collection
The independent variable was educational modeling, while the dependent variables were knowledge and self-termination of contraception among women entering menopause. The research instrument comprised a questionnaire with 30 questions derived from a literature review, which included 25 questions related to knowledge and five questions concerning self-termination of contraception. Knowledge responses were assessed using a two-point scale (right and wrong), whereas responses regarding the independent termination of contraception were evaluated using a three-point scale (ending contraceptive use, doubtful, and not ending). The validity of the instrument was tested using the product-moment correlation, where all attitude question items in the questionnaire exhibited a significance value of <0.05. The reliability of the instrument was assessed using Cronbach’s alpha, yielding a value of 0.80.
The researcher thoroughly explained the research’s scope and objectives to the women and provided a questionnaire sheet and detailed instructions on how to complete it. Participants were then requested to fill out a pre-test questionnaire before the educational intervention. Following the pre-test, educational materials were presented to the participants for approximately 30 minutes. A discussion session ensued to reinforce understanding about menopause. The questionnaire content focused on comprehending physical and psychological signs related to menopause and managing associated symptoms. Following the educational intervention, participants completed a post-test by re-filling the questionnaire three months later through a Google form sent via WhatsApp.
Statistical analysis
The normality of data was assessed by the Kolmogorov-Smirnov test with a significance value of 0.01, revealing that the data did not follow a normal distribution. The data utilized an ordinal scale, categorizing levels of knowledge and termination of contraception into three groups, including high (scores 76-100%), medium (scores 56-75%), and low (scores below 56%). Data analysis was conducted using the Wilcoxon Signed Rank test with a significance level of p<0.05, utilizing SPSS 22.0. This analytical approach was selected for its ability to effectively handle ordinal and non-normally distributed data, enabling researchers to assess differences before and after the intervention at a predetermined significance level. Consequently, the data analysis was meticulously performed to yield valid and reliable insights into the impact of educational interventions on contraceptive discontinuation among menopausal women.
Findings
This study assessed 112 women aged 40-55 years actively using contraception (Table 1).
Table 1. Frequency of respondents’ demographic characteristics and type of contraception
The pre- and post-test analysis revealed significant changes in knowledge (p<0.001) and contraceptive discontinuation among respondents. The comparison between pre- and post-education on menopause, demonstrated a notable increase in knowledge and actions related to contraceptive cessation across all groups (p<0.05; Table 2). Therefore, the educational intervention effectively impacted the enhancement of respondents’ knowledge and understanding regarding menopause, influencing their decisions concerning contraceptive discontinuation positively.
Table 2. Mean values of pre- and post-test analysis
The results of the pre- and post-test analyses revealed a substantial improvement in respondents’ characteristics concerning knowledge about menopause. Particularly, according to the Wilcoxon Signed Rank test, there was a significant rise in the average score from the pre-test to the post-test across all aspects examined, including understanding, signs and symptoms, and the impact of menopause (p<0.05; Table 3).
Table 3. Differences in mean pre- and post-test knowledge about menopause
Discussion
We assessed the impact of educational interventions on contraceptive discontinuation among menopausal women. The results indicated a positive influence of health education interventions on knowledge about menopause and decisions regarding independent termination of contraception among menopausal women. Enhancing knowledge about menopause through health education interventions serves as an initial step in fostering positive behaviors among women transitioning into menopause, enabling them to recognize signs, and symptoms, and make informed choices about discontinuing contraception independently. Offering health education stands as an effective strategy to boost knowledge, shape attitudes, and prompt actions [29].
Women approaching menopause often misunderstand signs and symptoms, mistaking them for age-related complaints. They may not recognize these symptoms as being linked to menopause. Common menopausal symptoms include changes in the menstrual cycle, hot flashes, hair loss, dry skin, breast sagging, weight gain, sexual changes, sleep disturbances, and mental-emotional issues [30]. The average age range for menopause falls between 45 to 55 years, with an estimated age typically ranging from 50 to 52 years, where 45 signifies early menopause [19]. In India, women experience menopause at around 46.2 years, notably younger than women in Western countries (averaging 51 years). The average age for natural menopause is approximately 48.94 years [31]. Factors, such as a woman’s age, use of exogenous hormones, number of childbirths, duration of breastfeeding, lifestyle choices, and health conditions influence the age at which women undergo menopause across different regions [30]. Women who undergo early menopause (before 40 years) face a higher risk of cardiovascular disease [32].
The continuous use of hormonal contraceptives has the potential to disrupt the menstrual cycle, leading to challenges in identifying the onset of menopause. Side effects associated with hormonal contraceptive use may include prolonged menstruation, amenorrhea (lack of menstruation), as well as symptoms, like headaches, dizziness, lower abdominal or back pain, and weight gain. While hormonal contraception is an effective means of preventing pregnancy, it is crucial to acknowledge that its usage can influence the natural hormonal equilibrium within a woman’s body. Therefore, individuals utilizing hormonal contraceptives should be aware of potential side effects and carefully evaluate contraceptive options that align with their specific needs and health conditions [33, 34].
Women with a comprehensive understanding of menopause can make informed decisions about discontinuing contraception independently. Adequate knowledge is crucial for women to recognize their infertility status. Once menopause sets in, pregnancy becomes unlikely. Uncertainty or failure to identify menopausal symptoms may lead women to continue contraceptive use unnecessarily. Enhanced knowledge correlates with improved health behaviors [35]. The level of health knowledge and behavior can be affected by various factors, including age, economic status, educational attainment, proximity to healthcare facilities, and disposable personal income (DPI). Health education plays a significant role in shaping the knowledge and attitudes of adolescent health cadres (KKR) concerning the consumption of iron tablets [36].
This situation is concerning because while menopausal symptoms can significantly impact quality of life, having a better understanding of menopause is crucial as it is linked to an improved quality of life. Interestingly, postmenopausal women reported feeling more knowledgeable than other groups, possibly due to their experiences during perimenopause and their ongoing learning process. When asked about their initial thoughts on menopause, the most common age range for considering this topic was between 40 and 49 years. This suggests that many women only begin contemplating menopause as they approach the age of experiencing it. Moreover, many women mention that they only started thinking about menopause when symptoms started to manifest, or in some instances, due to early menopause. This highlights a lack of readiness for menopause, potentially exacerbating the emotional and psychological toll of the transition. The lack of awareness about menopausal symptoms often leads to delays in diagnosing perimenopause and receiving appropriate advice and treatment.
The knowledge acquired through educational interventions enables women to gain a deeper understanding of menopausal signs, symptoms, and impacts, empowering them to make well-informed choices regarding discontinuing contraception. The results also indicated that a comprehensive understanding of menopause and contraception can alleviate confusion and uncertainty during this phase of a woman’s life cycle. Furthermore, the study highlighted that the continuous use of hormonal contraceptives may disrupt the menstrual cycle, potentially hindering the identification of menopausal onset. This underscores the significance of comprehending the side effects and consequences of hormonal contraceptive use, emphasizing the importance of carefully selecting a contraceptive method that aligns with individual health requirements and preferences.
The limitation of this research is that we only examined increasing menopausal women's knowledge about stopping contraceptives independently through education.
Conclusion
Health education interventions play a crucial role in enhancing knowledge and actions about menopause and the independent cessation of contraception among menopausal women.
Acknowledgments: We wish to extend our deepest gratitude to the dean, department head, and study program head at the Faculty of Vocational Studies, Airlangga University, for their unwavering support throughout the research process. Additionally, we would like to convey our utmost appreciation to the head of the Community Health Center for permitting us to conduct our research at the Lontar Community Health Center in Surabaya, East Java. Lastly, we are grateful to the respondents who generously dedicated their time to participate in our study. Special thanks are also due to the research ethical clearance team at the Muhammadiyah University of Gresik for facilitating the ethical approval process.
Ethical Permissions: The research received ethical approval from the Research Ethics Committee of the Faculty of Health, Muhammadiyah University of Gresik (081/KET/IL3-UMG/KEP/A/2022). Also, the respondents signed the informed consent form.
Conflicts of Interests: All authors declared no conflicts of interests.
Authors’ Contribution: Fadliyah L (First Author), Introduction Writer/Main Researcher (20%); Hendarto H (Second Author), Introduction Writer/Assistant Researcher (20%); Sudaryanti L (Third Author), Methodologist (10%); Susilo I (Fourth Author), Methodologist (10%); Mardika A (Fifth Author), Assistant Researcher (10%); Iswatun I (Sixth Author), Discussion Writer (10%); Sulfat E (Seventh Author), Discussion Writer (10%); Hassan II (Eighth Author), Discussion Writer/Statistical Analyst (10%)
Funding/Support: This study received no funding.
Article Type: Descriptive & Survey |
Subject:
Healthy Life Style
Received: 2024/04/7 | Accepted: 2024/05/25 | Published: 2024/06/28
Received: 2024/04/7 | Accepted: 2024/05/25 | Published: 2024/06/28
References
1. WHO. Menopause. Geneva: World Health Organization; 2022. [Link]
2. Burgin J, Bailey JV. Factors affecting contraceptive choice in women over 40: A qualitative study. BMJ Open. 2022;12(11):e064987. [Link] [DOI:10.1136/bmjopen-2022-064987]
3. Yeganeh L, Boyle J, Teede H, Vincent A. Knowledge and attitudes of health professionals regarding menopausal hormone therapies. Climacteric. 2017;20(4):348-55. [Link] [DOI:10.1080/13697137.2017.1304906]
4. Rodiah SST. Proper contraception improves reproductive health. Jakarta: Kemenkes; 2022. [Indonesian] [Link]
5. Kim TY, Haider M, Hancock GR, Boudreaux MH. The role of health literacy in family planning use among Senegalese women. J Health Commun. 2019;24(3):244-61. [Link] [DOI:10.1080/10810730.2019.1601299]
6. Indahwati L, Ratna Wati L, Trias Wulandari D. Age and family planning experience are related to the choice of contraceptive method. J Issues Midwifery. 2017;1(2):9-18. [Indonesian] [Link] [DOI:10.21776/ub.JOIM.2017.001.02.2]
7. Rosidah LK. The influence of education level and age on the use of long-term contraceptive methods in 2018. Jurnal Kebidanan. 2020;9(2):108-14. [Indonesian] [Link]
8. Gafar A, Suza DE, Efendi F, Has EMM, Pramono AP, Susanti IA. Determinants of contraceptive use among married women in Indonesia. Version 1. F1000Res. 2020;9:193. [Link] [DOI:10.12688/f1000research.22482.1]
9. Suwarni L, Selviana S. Premarital sex initiation among adolescents and influencing factors. Jurnal Kesehatan Masyarakat. 2015;10(2):169-77. [Indonesian] [Link] [DOI:10.15294/kemas.v10i2.3378]
10. Machado RB, Monteiro IMU, Magalhães J, Guazzelli CAF, Brito MB, Finotti MF, et al. Long-acting reversible contraception. Revista Brasileira de Ginecologia e Obstetricia. 2017;39(6):294-308. [Portuguese] [Link] [DOI:10.1055/s-0037-1603647]
11. Rocca ML, Palumbo AR, Visconti F, Di Carlo C. Safety and benefits of contraceptive implants: A systematic review. Pharmaceuticals. 2021;14(6):548. [Link] [DOI:10.3390/ph14060548]
12. Rouhbakhsh M, Kermansaravi F, Shakiba M, Navidian A. The effect of couples education on marital satisfaction in menopausal women. J Women Aging. 2019;31(5):432-45. [Link] [DOI:10.1080/08952841.2018.1510244]
13. Stubblefield PG. Menstrual impact of contraception. Am J Obstet Gynecol. 1994;170(5 Pt 2):1513-22. [Link] [DOI:10.1016/S0002-9378(94)05013-1]
14. Howard SA, Benhabbour SR. Non-hormonal contraception. J Clin Med. 2023;12(14):4791. [Link] [DOI:10.3390/jcm12144791]
15. Bitzer J. Overview of perimenopausal contraception. Climacteric. 2019;22(1):44-50. [Link] [DOI:10.1080/13697137.2018.1540566]
16. Moradinazar M, Marzbani B, Shahebrahimi K, Shahabadi S, Marzbani B, Moradinazar Z. Hormone therapy and factors affecting fertility of women under 50-year-old with breast cancer. Breast Cancer. 2019;11:309-19. [Link] [DOI:10.2147/BCTT.S218394]
17. Svallfors S, Billingsley S. Conflict and contraception in Colombia. Stud Fam Plann. 2019;50(2):87-112. [Link] [DOI:10.1111/sifp.12087]
18. Thurman A, Chandra N, Schwartz JL, Brache V, Chen BA, Asin S, et al. The effect of hormonal contraception on cervicovaginal mucosal endpoints associated with HIV acquisition. AIDS Res Hum Retroviruses. 2019;35(9):853-64. [Link] [DOI:10.1089/aid.2018.0298]
19. Ali KY, Erkok U, Mohamed NA, Hilowle NM, Elmi HAH, Mohamud RYH. Age at natural menopause and influencing factors in women attending the gynecological outpatient clinic at a tertiary care hospital. Int J Womens Health. 2023;15:1627-36. [Link] [DOI:10.2147/IJWH.S434123]
20. Munn C, Vaughan L, Talaulikar V, Davies MC, Harper JC. Menopause knowledge and education in women under 40: Results from an online survey. Womens Health. 2022;18:17455057221139660. [Link] [DOI:10.1177/17455057221139660]
21. Tariq B, Phillips S, Biswakarma R, Talaulikar V, Harper JC. Women's knowledge and attitudes to the menopause: a comparison of women over 40 who were in the perimenopause, post menopause and those not in the peri or post menopause. BMC Womens Health. 2023;23(1):460. [Link] [DOI:10.1186/s12905-023-02424-x]
22. Shi D, Liu C, Huang L, Chen XQ. Post-abortion needs-based education via the WeChat platform to lessen fear and encourage effective contraception: A post-abortion care service intervention-controlled trial. BMC Womens Health. 2024;24(1):159. [Link] [DOI:10.1186/s12905-024-03004-3]
23. Wilson LC, Rademacher KH, Rosenbaum J, Callahan RL, Nanda G, Fry S, et al. Seeking synergies: Understanding the evidence that links menstrual health and sexual and reproductive health and rights. Sex Reprod Health Matters. 2021;29(1):1882791. [Link] [DOI:10.1080/26410397.2021.1882791]
24. Oumer M, Manaye A, Mengistu Z. Modern contraceptive method utilization and associated factors among women of reproductive age in Gondar City, Northwest Ethiopia. Open Access J Contracept. 2020;11:53-67. [Link] [DOI:10.2147/OAJC.S252970]
25. El Khoudary SR, Aggarwal B, Beckie TM, Hodis HN, Johnson AE, Langer RD, et al. Menopause transition and cardiovascular disease risk: Implications for the timing of early prevention: A scientific statement from the American heart association. Circulation. 2020;142(25):e506-32. [Link] [DOI:10.1161/CIR.0000000000000912]
26. Stuenkel CA. Reproductive milestones across the lifespan and cardiovascular disease risk in women. Climacteric. 2024;27(1):5-15. [Link] [DOI:10.1080/13697137.2023.2259793]
27. Chapman N, Ching SM, Konradi AO, Nuyt AM, Khan T, Twumasi-Ankrah B, et al. Arterial hypertension in women: State of the art and knowledge gaps. Hypertension. 2023;80(6):1140-9. [Link] [DOI:10.1161/HYPERTENSIONAHA.122.20448]
28. Da Silva Filho AL, Caetano C, Lahav A, Grandi G, Lamaita RM. The difficult journey to treatment for women suffering from heavy menstrual bleeding: A multi-national survey. Eur J Contracept Reprod Health Care. 2021;26(5):390-8. [Link] [DOI:10.1080/13625187.2021.1925881]
29. Iswatun I, Kusnanto K, Nasir A, Fadliyah L, Wijayanti ES, Susanto J, et al. The effect of health education on knowledge, attitudes, and actions in preventing leukorrhea in adolescent girls. J Int Dent Med Res. 2021;14(3):1240-5. [Link]
30. Susilawati S, Rudi Karmi M, Hairunnisa S, Fitria Prihatini M, Made Garnis Dolesgit S, Ratna Juwita M, et al. Maternity nursing textbook. 1st ed. Jambi: Sonpedia Publishing Indonesia; 2023. [Indonesian] [Link]
31. Wang M, Hu RY, Wang H, Gong WW, Wang CM, Xie KX, et al. Age at natural menopause and risk of diabetes in adult women: Findings from the China Kadoorie Biobank study in the Zhejiang area. J Diabetes Investig. 2018;9(4):762-8. [Link] [DOI:10.1111/jdi.12775]
32. Zhu D, Chung HF, Dobson AJ, Pandeya N, Giles GG, Bruinsma F, et al. Age at natural menopause and risk of incident cardiovascular disease: A pooled analysis of individual patient data. Lancet Public Health. 2019;4(11):e553-64. [Link] [DOI:10.1016/S2468-2667(19)30155-0]
33. Mukanga B, Mwila N, Nyirenda HT, Daka V. Perspectives on the side effects of hormonal contraceptives among women of reproductive age in Kitwe district of Zambia: A qualitative explorative study. BMC Womens Health. 2023;23(1):436. [Link] [DOI:10.1186/s12905-023-02561-3]
34. Mackenzie ACL, Curtis SL, Callahan RL, Tolley EE, Speizer IS, Martin SL, et al. Women's perspectives on contraceptive-induced amenorrhea in Burkina Faso and Uganda. Int Perspect Sex Reprod Health. 2020;46:247-62. [Link] [DOI:10.1363/46e1520]
35. Pratiwi IM, Paskarini I, Dwiyanti E, Arini SY, Suswojo H. The relationship of knowledge and attitudes with behavior of implementing health protocols in garment workers. Indones J Occup Saf Health. 2022;11(2):168-77. [Link] [DOI:10.20473/ijosh.v11i2.2022.168-177]
36. Rahmawati E, Wardhani RK, Tamsuri A, Wiseno B. The effect of health education on the knowledge and attitudes of adolescent health cadres about table Fe consumption in Sma N 1 Kediri regency. Healthc Nurs J. 2023;5(1):462-9. [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






