Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 315-322 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bakhshi F, Safavi S, Sadeghi R. Social Cognitive Theory and Healthy Lifestyle among Elderly. Health Educ Health Promot 2024; 12 (2) :315-322
URL: http://hehp.modares.ac.ir/article-5-74429-en.html
URL: http://hehp.modares.ac.ir/article-5-74429-en.html
1- “Department of Health Education & Promotion, School of Health” and “Research Center of Health and Environment”, Guilan University of Medical Sciences, Rasht, Iran
2- Department of Health Education & Promotion, School of Health, Tehran University of Medical Sciences, Tehran, Iran
2- Department of Health Education & Promotion, School of Health, Tehran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 620 kb]
(4274 Downloads)
| Abstract (HTML) (1728 Views)
Full-Text: (465 Views)
Introduction
Aging is a natural process that affects all individuals [1]. The proportion of elderly people in the world and Iran is steadily increasing, emphasizing the need to prioritize their health and well-being [2, 3]. Adopting a healthy lifestyle is crucial in maintaining the physical and mental health of the elderly [4]. Along with the rise in the elderly population, their health problems have become more prominent. Factors such as physical inactivity, reduced social networks, loss of loved ones, and mental and physical illnesses have made maintaining a healthy lifestyle a significant challenge for many older adults [5, 6].
A healthy lifestyle, characterized by behaviors like healthy eating, regular physical activity, stress management, and positive interpersonal relationships, plays a vital role in preventing or delaying disability and improving the quality of life among the elderly [7, 8]. Research conducted in the UK has shown that engaging in health-promoting behaviors can lead to healthy aging and enhanced quality of life for older adults [9, 10]. A physical activity intervention in Taiwan positively affects the health behaviors of older adults and encourages health-promoting lifestyles. These findings underscore the importance of adopting and promoting healthy behaviors as a key strategy for promoting well-being and maximizing the potential for successful aging in older populations [10].
The effective implementation of theories and models in health education and promotion programs is essential for their success [11]. Social cognitive theory (SCT) is a well-established theoretical framework that explains the dynamic relationship between behavior and individual, as well as environmental, factors [12]. SCT has been widely utilized in the study of physical activity behavior among various populations, including the elderly [13].
Numerous studies have substantiated the effectiveness of SCT in promoting a healthy lifestyle [14]. Guan et al. [15] found that applying SCT principles in an intervention targeting physical activity results in significant improvements in exercise behavior among older adults. Similarly, a systematic review conducted by Bagherniya et al. [16] revealed that SCT-based interventions are effective in promoting healthy eating behaviors and weight management in older populations. These studies highlight the robust evidence supporting the efficacy of SCT in facilitating behavior change and promoting healthy lifestyles among older adults. This theory of human motivation and action elucidates the internal and external processes (cognitive, situational, self-reflective, and self-regulatory) that influence psychosocial functioning [17].
By understanding the factors that influence the lifestyle of the elderly, health professionals can design effective educational programs to support active and happy aging [18]. The current study aimed to leverage the utility of SCT constructs as a theoretical basis for tailoring lifestyle programs to the elderly population.
Instrument and Methods
This cross-sectional study was conducted in Rasht City, the North of Iran, among individuals aged 60 years in 2021. The participants were selected from a total of 38 comprehensive health service centers and bases in Rasht City.
According to a similar study by Alaei et al. [19], the formula N=z2 p (1-p)/d2 was used for sample size calculation considering the first type error of 5%, with d being equal to 3%. Based on the formula, the required number of samples was calculated as 350 people, which increased to 420 people when considering the design effect equal to 1.2. Eventually, the sample size was determined to be 455. The required samples were selected using the relative classification method, where the number of participants selected from each center was proportional to the total number of elderly registered at that center based on the inclusion/exclusion criteria. The selected samples were contacted and invited to the considered center to complete the questionnaire. After explaining the research project’s objectives and obtaining written consent, one of the project partners read the questionnaire to the elderly participants and recorded their opinions.
The initial selection of participants was done randomly using the SIB system and the household file numbers. Subsequent participants were then selected using a random number table to reach the desired sample size of 455. The data collection took place over a period of approximately 55 days, from December to the end of February 2019.
Questionnaires were completed through face-to-face interviews. Before filling out the questionnaires, the study’s purpose was explained to the participants, and they were assured that their data would be kept confidential and used solely for research purposes. Written consent was obtained from all participants. Individuals aged 60 years and older, without movement problems, who expressed satisfaction with their participation, were included in the study, while incomplete questionnaire responses were considered as an exclusion criterion.
Research tools
The data collection tool consisted of three parts. The first part was demographic characteristics (13 questions), including age, height, weight, body mass index (BMI), level of education, sex, marital status, number of children, occupation, second job during retirement, total monthly income, history of chronic illness (respiratory disease, heart disease, blood pressure, blood fat, and diabetes), and living status.
The second part was the constructs of the SCT (48 questions), including the construct of awareness (nine questions) with a three-point Likert scoring system (correct=two points, don’t know=one point, and incorrect=zero), self-efficacy construct (six questions), outcome expectation (eight questions), outcome expectancies (nine questions), social support (seven questions), observational learning (three questions), and self-regulation structure (six questions). These six constructs were scored on a five-point Likert scale (completely agree=five, agree=four, have no opinion=three, disagree=two, and completely disagree=one). The self-efficacy construct was taken from Sherer’s questionnaire [20]. The remaining questions in this section were developed from a researcher-made questionnaire and compiled using similar studies, library research, and the experiences of the research team.
The third part was the Healthy Lifestyle Questionnaire, adapted from the 26-question Ishaghi Scale for measuring the healthy lifestyle of the elderly, including eight prevention questions, nine nutrition questions, one physical activity question, five stress management questions, and three questions about social and interpersonal relationships. Using a five-point Likert scale for frequency evaluation, a score of one indicated never, two indicated rarely, three indicated sometimes, four indicated often, and five indicated always. The maximum score was 130, where a score between 26 and 76 indicated an unhealthy lifestyle, a score of 77-101 indicated an average lifestyle, and a score of 102-130 indicated a healthy lifestyle [18].
The opinions of ten faculty members (including one epidemiologist, one statistician, one nutritionist, and seven health education and health promotion specialists) were utilized to calculate the questionnaire content validity ratio (CVR). In the questionnaire containing the SCT constructs, the CVR values calculated were 0.78 for consciousness, one for self-efficacy, 0.97 for outcome expectation, 0.80 for outcome expectancies, 0.97 for the environment, 0.90 for observational learning, and one for self-regulation. The content validity index (CVI) values obtained were 0.96 for consciousness, one for self-efficacy (with one question omitted), 0.90 for outcome expectation (with one question omitted), 0.98 for outcome expectancies, one for the environment, 0.78 for observational learning, and one for self-regulation. Mean values above 0.8 were also obtained for the reliability coefficient of consciousness (0.77), self-efficacy (0.91), outcome expectation (0.91), outcome expectancies (0.82), environment (0.87), observational learning (0.81), and self-regulation (0.83).
In the Healthy Lifestyle Questionnaire, the CVR values were 0.97 for prevention, 0.95 for nutrition, one for exercise, 0.88 for stress management, and one for social and interpersonal relationships. The CVI values were calculated as one for the prevention domain, 0.90 for the nutrition domain, 0.90 for the exercise domain, one for the stress management domain, and one for social relations and interpersonal relationships. Formal validity was assessed in terms of text, grammar, and editing. A pilot study was completed with 30 elderly living in Rasht to evaluate the questionnaire’s reliability, which was confirmed.
Statistical analysis
Statistical analysis was performed using R software 4.1.2 and SPSS 22.0. Qualitative variables were expressed as numbers (percentages), while quantitative variables were expressed as mean and standard deviation. The Kolmogorov-Smirnov test was used to evaluate the normality of the data. The Spearman correlation coefficient was used to determine the relationship between the quantitative studied variables. All analyses were performed two-sided, and a significance level was considered at 0.05. The Shapiro-Wilk test was used to assess the normal distribution of age and BMI. An independent t-test was used to compare quantitative variables between groups. The Chi-squared and Fisher’s exact tests were used to examine the relative distribution of patients assigned to different categories of qualitative variables.
Findings
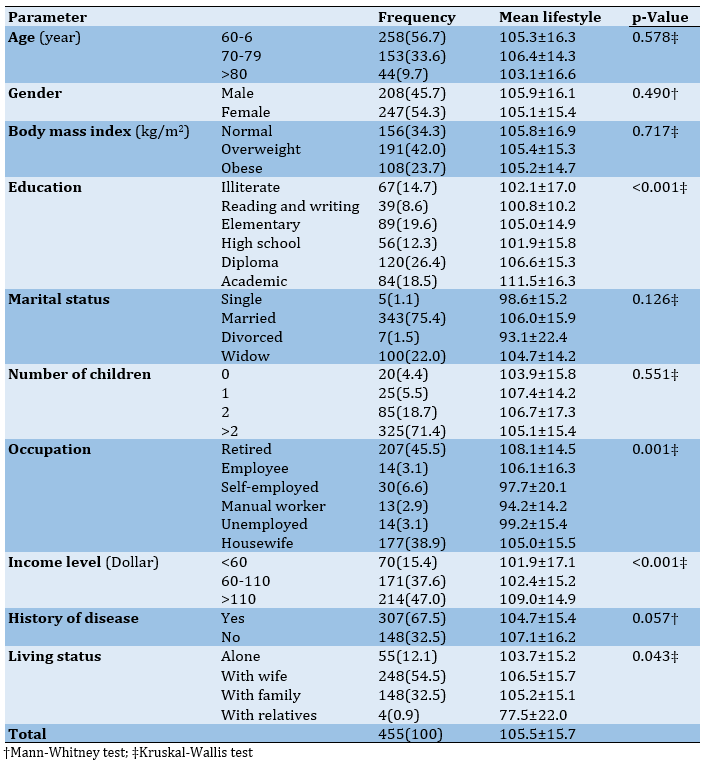
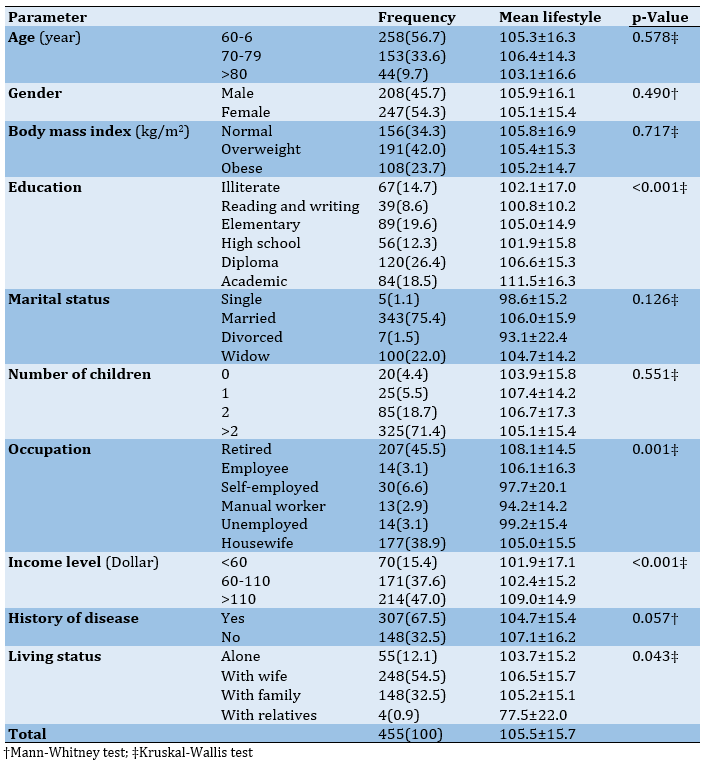
Out of the 455 elderly participants in the study, 247 (54.3%) were female. Regarding age, 56.7% of the elderly were in the age group of 60-69 years (young-old), and 33.6% were in the age group of 70-79 years (middle-old). Also, 26.4% of the participants had a diploma, 75.4% were married, 71.4% had more than two children, 45.5% were retired, 47% had a monthly income of more than $110, and 67.5% had at least one chronic disease. In addition, 54.5% of the elderly were living with their spouse at the time of answering the questionnaire. In terms of BMI, 42.0% were overweight. The results indicated that the healthy lifestyle score was associated with education, occupation, income level, and living status. Elderly participants who had attained a higher level of education demonstrated higher lifestyle scores. As income increased, the lifestyle score increased as well. Additionally, the elderly who resided with their spouse and family exhibited a higher quality of life score (Table 1).
Table 1. Frequency of socio-demographic characteristics and comparison of the lifestyle scores in the elderly
Most participants (60.9%) were found to have a healthy lifestyle. Among the various components, prevention had the highest balanced score (0-100) for a healthy lifestyle in the elderly, while physical activity had the lowest score.
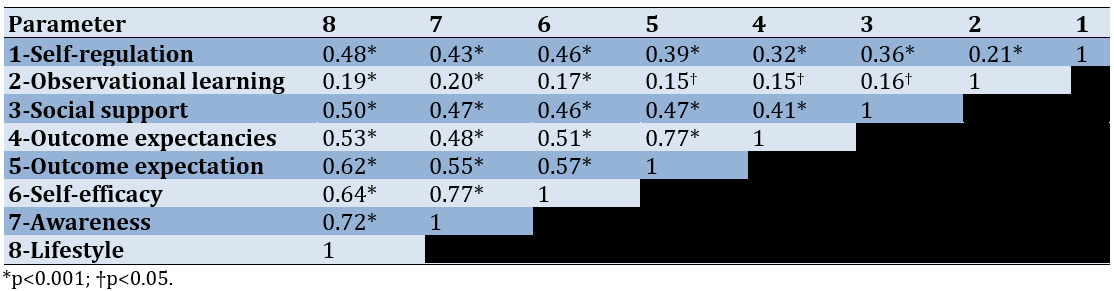
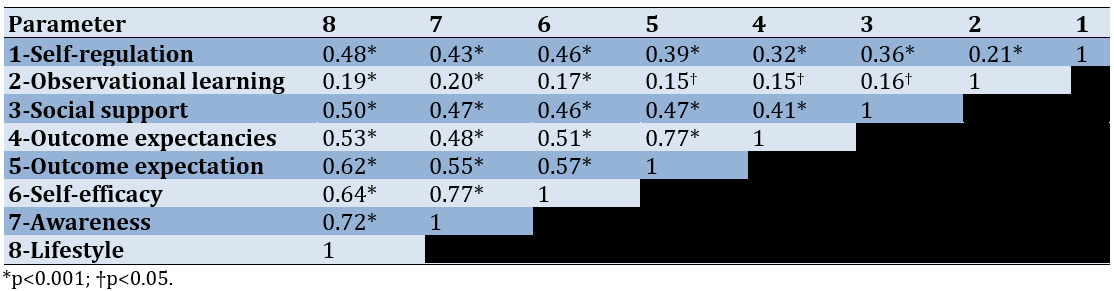
Outcome expectancies had the highest average score at 80.7%, while the self-efficacy structure had the lowest average score at 60.2% in the constructs of SCT. Regarding the correlation between SCT constructs and healthy lifestyle scores in the elderly, all correlations were significant and direct (Table 2). The strongest correlation between healthy lifestyle and SCT constructs was found in the self-regulation construct (r=0.48; p<0.001), while the weakest was found in the awareness construct (r=0.21; p<0.001). Additionally, the highest correlation was observed between SCT constructs, specifically between social support and observational learning (r=0.77; p<0.001), while the lowest correlation was found between awareness and self-efficacy (r=0.16; p=0.001; Table 2).
Table 2. Correlation between the social cognitive theory constructs and healthy lifestyle score
Discussion
The current study aimed to leverage the utility of SCT constructs as a theoretical basis for tailoring lifestyle programs to Sthe elderly population. Based on SCT studies, various constructs have been identified as the strongest predictors of lifestyle-related behaviors in the elderly [20-24]. In our study, the self-efficacy constructs obtained the lowest percentage (68.15%), while the outcome expectation constructs (84.55%) and outcome expectancies (84%) scored the highest. Other researchers have found similar results, reporting outcome expectancies scoring the highest, while self-efficacy scores the lowest [25]. Additionally, the expectation of the outcome is the construct with the highest score among the constructs of SCT [23]. In the study by Ghoreishi et al. [25], anticipation, outcome expectancies, and self-regulation are the strongest predictors. However, the findings of our study are inconsistent with those of Amini Moridani et al. [26], who found that perceived social support constructs obtain the highest score, while environmental structures score the lowest. The reason for this difference may be variations in study timing and cultural differences across the studied cities.
There was no statistically significant difference between the mean scores of SCT constructs by gender and BMI. There was a significant relationship between constructs’ outcome expectancies and outcome expectations with a history of chronic disease. The elderly with no history of chronic disease had higher mean structural value scores and expected outcomes. The importance that the elderly attribute to desired behaviors forms the foundation for health promotion. In contrast, our study’s findings contradict those that reported a significant relationship between the history of chronic disease and both self-efficacy and self-regulatory structure [27]. This difference may be due to differences in the study subjects. Another significant finding of this study was the relationship between the mean score of outcome expectancies and the number of children. Elderly with two children tended to achieve better-expected outcomes on average. Unfortunately, no similar article was found regarding these findings. Children can support their parents when they become old, and it is most likely that the elderly who have more children will receive more support compared to those without children.
A significant relationship was observed between the construct of outcome expectancies and social support with living status. Old people living with families had an average outcome expectancy score, and elderly people living with their spouses had a higher social support score because of the increased need for family support. On the other hand, the results of our study oppose those of Heidari-Soureshjani et al. [27], reporting a statistically considerable association between marital status and self-efficacy. The variation in the findings may be due to discrepancies in the populations examined (only women with diabetes referring to diabetes centers).
There was a significant relationship between the mean value of constructs and outcome expectation, social support, observational learning, and self-regulation according to education. The average score of these constructs was higher in the elderly who have a university education. With the increase in education, people’s awareness increases due to the ability to read different books and magazines or benefit from scientific websites, which is attributed to the literacy of the elderly with the ability to read different books and have life skills. Their worldview is better and more open towards life. These results are consistent with findings from other studies [28-31].
A statistically significant relationship between the mean values of SCT constructs and the outcome and social support based on occupation. Among the elderly, those employed as employees scored higher in these two constructs compared to their counterparts, which is in line with the results of other studies [17, 30]. However, Heidari-Soureshjani et al. [27] reported that there is a statistically significant relationship between employment status and self-efficacy and self-regulation structures, contradicting our findings. This contradiction may be due to factors, such as the gender and diabetes condition of the participants, as well as the variances in time between the two studies.
There was a statistically significant relationship between the constructs of awareness, outcome expectancies and expectations, social support, observational learning, and self-regulation in terms of income. The average scores of these constructs were higher among the elderly with higher incomes (>$110). Income and economic status are among the most important determinants of health in people, especially the elderly [10, 28, 31]. Therefore, government policies should prioritize providing special financial support through organizations like the Ministry of Welfare and Social Affairs. This support would encourage families who are unable to care for the elderly and ensure that all seniors can enjoy the benefits of living with family [32].
The findings also showed a direct and positive relationship between the mean scores of awareness, self-efficacy, outcome expectancies, social support, observational learning, self-regulation, and healthy lifestyle. Khani Jeihooni et al. [33] and Ryan [34] reported that there is a statistically significant relationship between nutritional performance, walking, and self-regulation, indicating consistency with the present study. These results suggest that the constructs of awareness, self-efficacy, outcome expectancies, social support, observational learning, and self-regulation from the SCT play an important role in healthy lifestyle behavior.
According to the results of the present study, of all the variables, including SCT and demographic variables, 26.3% of healthy lifestyle behavior was predicted by these two categories of variables. The constructs of social support, self-regulation, outcome expectancies, and awareness showed significant predictability using a multivariate linear regression model and step-wise method. They accounted for 25.9% of the variance in lifestyle behavior. According to this model, the included demographic variables were not significant and were removed from the model. Similar findings have also been observed in previous studies [35-37]. Therefore, as individuals age and enter old age, the need for environmental support, particularly from family members, increases. In general, social support has a positive impact on the lifestyle of older adults [35].
Regarding awareness, older individuals exhibited a higher level of awareness, knowledge, and information regarding health-promoting behaviors and lifestyles, also known as health literacy. They demonstrated an equal understanding and application of health issues and lifestyle. Moreover, these individuals were perceived more favorably. According to Bandura, self-regulatory strategies are crucial for targeting and planning regular physical activity [38]. Self-regulation plays a pivotal role in social cognitive approaches to modifying health behaviors. In our study, elderly participants who practiced self-control and goal setting in shaping their lifestyle behaviors exhibited a more desirable lifestyle. Furthermore, the likelihood of engaging in desired behavior increases with an individual’s higher value placed on the expected outcome.
Step-wise multiple regression analyses conducted in the study by Sung & Lim [39] revealed that the social support structure, with a 55% predictive power, is the strongest predictor for a health-promoting lifestyle. Peyman et al. [40] reported that self-regulatory and social support are the strongest predictors of physical activity in type 2 diabetic women. The results of Liu’s study [41] demonstrated that social support structures from friends are the strongest predictors according to the SCT in students’ physical activity. Umstattd & Hallam [23] indicated that self-regulation and expectation are the most influential factors in predicting physical activity among adults.
Our results are inconsistent with those of Yari et al. [35], where self-efficacy is one of the strongest predictors of physical activity, and also with the study by Nematollahi & Eslami [42], in which self-regulation has the greatest impact on physical activity, while self-efficacy has the least impact. The existing discrepancy in this field can be justified by the differences between the geographical area, culture, and climate of the present study.
Linear regression analysis in the study by Abdi et al. [43] showed that among the SCT constructs, environment and self-efficacy are the strongest predictors of a healthy lifestyle in overweight and obese employees. However, their results are inconsistent with ours. This discrepancy may be due to differences in the target groups regarding climatic and occupational conditions of the study subjects. According to Mahmoudi et al. [36], the SCT constructs (self-efficacy, outcome expectations, outcome expectancies, family support, and friend support) account for 13% of the variance of physical activity behavior in Borkhar and Shahin Shahr health network employees in Isfahan. The results of the present study are inconsistent with this study.
Furthermore, in the study by Gothe & Kendall [44], self-efficacy and outcome expectation are the most important predictors of physical activity for African-American adults. The findings of the present study were inconsistent with this study. These differences may be attributed to the heterogeneous population in the mentioned studies, which had different age ranges, demographic characteristics, and cultural and climatic differences that were distinct from the present study.
Among the limitations of the present study was the collection of information in a self-reporting manner. This method, which relied on participants being honest and accurate in answering questions, was beyond the control of the researcher. Additionally, the study faced challenges due to the large number of questions included in the questionnaire. It is important to note that the data collection coincided with the COVID-19 pandemic, which posed difficulties in ensuring convenient access to all elderly participants during quarantine. These circumstances may have influenced the quality of the data obtained. The results highlighted the importance of targeting these cognitive and social constructs when designing educational interventions to foster healthy lifestyles in the elderly. Further research is needed to explore other potential variables that may influence healthy lifestyle behaviors in this age group.
Conclusion
SCT is a suitable framework for understanding and promoting healthy lifestyles among the elderly. Factors, such as awareness, self-efficacy, self-regulation, social support, outcome expectations, and observational learning are key predictors of healthy lifestyle behaviors in the elderly, with social support, both from peers and family, being a particularly important factor.
Acknowledgments: The authors express their gratitude to the research deputy of Tehran and Guilan University, and they would like to express their gratitude and appreciation to the elderly for their sincere cooperation.
Ethical Permissions: This article is part of the MSc thesis on health education and health promotion (2020.434) and was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.2020.434).
Conflicts of Interests: The authors declared no potential conflicts of interests.
Authors’ Contribution: Bakhshi F (First Author), Introduction Writer/Assistant Researcher (30%); Safavi SR (Second Author), Main Researcher/Statistical Analyst/Methodologist/Discussion Writer (40%); Sadeghi R (Third Author), Statistical Analyst/Assistant Researcher (30%)
Funding/Support: None declared by the authors.
Aging is a natural process that affects all individuals [1]. The proportion of elderly people in the world and Iran is steadily increasing, emphasizing the need to prioritize their health and well-being [2, 3]. Adopting a healthy lifestyle is crucial in maintaining the physical and mental health of the elderly [4]. Along with the rise in the elderly population, their health problems have become more prominent. Factors such as physical inactivity, reduced social networks, loss of loved ones, and mental and physical illnesses have made maintaining a healthy lifestyle a significant challenge for many older adults [5, 6].
A healthy lifestyle, characterized by behaviors like healthy eating, regular physical activity, stress management, and positive interpersonal relationships, plays a vital role in preventing or delaying disability and improving the quality of life among the elderly [7, 8]. Research conducted in the UK has shown that engaging in health-promoting behaviors can lead to healthy aging and enhanced quality of life for older adults [9, 10]. A physical activity intervention in Taiwan positively affects the health behaviors of older adults and encourages health-promoting lifestyles. These findings underscore the importance of adopting and promoting healthy behaviors as a key strategy for promoting well-being and maximizing the potential for successful aging in older populations [10].
The effective implementation of theories and models in health education and promotion programs is essential for their success [11]. Social cognitive theory (SCT) is a well-established theoretical framework that explains the dynamic relationship between behavior and individual, as well as environmental, factors [12]. SCT has been widely utilized in the study of physical activity behavior among various populations, including the elderly [13].
Numerous studies have substantiated the effectiveness of SCT in promoting a healthy lifestyle [14]. Guan et al. [15] found that applying SCT principles in an intervention targeting physical activity results in significant improvements in exercise behavior among older adults. Similarly, a systematic review conducted by Bagherniya et al. [16] revealed that SCT-based interventions are effective in promoting healthy eating behaviors and weight management in older populations. These studies highlight the robust evidence supporting the efficacy of SCT in facilitating behavior change and promoting healthy lifestyles among older adults. This theory of human motivation and action elucidates the internal and external processes (cognitive, situational, self-reflective, and self-regulatory) that influence psychosocial functioning [17].
By understanding the factors that influence the lifestyle of the elderly, health professionals can design effective educational programs to support active and happy aging [18]. The current study aimed to leverage the utility of SCT constructs as a theoretical basis for tailoring lifestyle programs to the elderly population.
Instrument and Methods
This cross-sectional study was conducted in Rasht City, the North of Iran, among individuals aged 60 years in 2021. The participants were selected from a total of 38 comprehensive health service centers and bases in Rasht City.
According to a similar study by Alaei et al. [19], the formula N=z2 p (1-p)/d2 was used for sample size calculation considering the first type error of 5%, with d being equal to 3%. Based on the formula, the required number of samples was calculated as 350 people, which increased to 420 people when considering the design effect equal to 1.2. Eventually, the sample size was determined to be 455. The required samples were selected using the relative classification method, where the number of participants selected from each center was proportional to the total number of elderly registered at that center based on the inclusion/exclusion criteria. The selected samples were contacted and invited to the considered center to complete the questionnaire. After explaining the research project’s objectives and obtaining written consent, one of the project partners read the questionnaire to the elderly participants and recorded their opinions.
The initial selection of participants was done randomly using the SIB system and the household file numbers. Subsequent participants were then selected using a random number table to reach the desired sample size of 455. The data collection took place over a period of approximately 55 days, from December to the end of February 2019.
Questionnaires were completed through face-to-face interviews. Before filling out the questionnaires, the study’s purpose was explained to the participants, and they were assured that their data would be kept confidential and used solely for research purposes. Written consent was obtained from all participants. Individuals aged 60 years and older, without movement problems, who expressed satisfaction with their participation, were included in the study, while incomplete questionnaire responses were considered as an exclusion criterion.
Research tools
The data collection tool consisted of three parts. The first part was demographic characteristics (13 questions), including age, height, weight, body mass index (BMI), level of education, sex, marital status, number of children, occupation, second job during retirement, total monthly income, history of chronic illness (respiratory disease, heart disease, blood pressure, blood fat, and diabetes), and living status.
The second part was the constructs of the SCT (48 questions), including the construct of awareness (nine questions) with a three-point Likert scoring system (correct=two points, don’t know=one point, and incorrect=zero), self-efficacy construct (six questions), outcome expectation (eight questions), outcome expectancies (nine questions), social support (seven questions), observational learning (three questions), and self-regulation structure (six questions). These six constructs were scored on a five-point Likert scale (completely agree=five, agree=four, have no opinion=three, disagree=two, and completely disagree=one). The self-efficacy construct was taken from Sherer’s questionnaire [20]. The remaining questions in this section were developed from a researcher-made questionnaire and compiled using similar studies, library research, and the experiences of the research team.
The third part was the Healthy Lifestyle Questionnaire, adapted from the 26-question Ishaghi Scale for measuring the healthy lifestyle of the elderly, including eight prevention questions, nine nutrition questions, one physical activity question, five stress management questions, and three questions about social and interpersonal relationships. Using a five-point Likert scale for frequency evaluation, a score of one indicated never, two indicated rarely, three indicated sometimes, four indicated often, and five indicated always. The maximum score was 130, where a score between 26 and 76 indicated an unhealthy lifestyle, a score of 77-101 indicated an average lifestyle, and a score of 102-130 indicated a healthy lifestyle [18].
The opinions of ten faculty members (including one epidemiologist, one statistician, one nutritionist, and seven health education and health promotion specialists) were utilized to calculate the questionnaire content validity ratio (CVR). In the questionnaire containing the SCT constructs, the CVR values calculated were 0.78 for consciousness, one for self-efficacy, 0.97 for outcome expectation, 0.80 for outcome expectancies, 0.97 for the environment, 0.90 for observational learning, and one for self-regulation. The content validity index (CVI) values obtained were 0.96 for consciousness, one for self-efficacy (with one question omitted), 0.90 for outcome expectation (with one question omitted), 0.98 for outcome expectancies, one for the environment, 0.78 for observational learning, and one for self-regulation. Mean values above 0.8 were also obtained for the reliability coefficient of consciousness (0.77), self-efficacy (0.91), outcome expectation (0.91), outcome expectancies (0.82), environment (0.87), observational learning (0.81), and self-regulation (0.83).
In the Healthy Lifestyle Questionnaire, the CVR values were 0.97 for prevention, 0.95 for nutrition, one for exercise, 0.88 for stress management, and one for social and interpersonal relationships. The CVI values were calculated as one for the prevention domain, 0.90 for the nutrition domain, 0.90 for the exercise domain, one for the stress management domain, and one for social relations and interpersonal relationships. Formal validity was assessed in terms of text, grammar, and editing. A pilot study was completed with 30 elderly living in Rasht to evaluate the questionnaire’s reliability, which was confirmed.
Statistical analysis
Statistical analysis was performed using R software 4.1.2 and SPSS 22.0. Qualitative variables were expressed as numbers (percentages), while quantitative variables were expressed as mean and standard deviation. The Kolmogorov-Smirnov test was used to evaluate the normality of the data. The Spearman correlation coefficient was used to determine the relationship between the quantitative studied variables. All analyses were performed two-sided, and a significance level was considered at 0.05. The Shapiro-Wilk test was used to assess the normal distribution of age and BMI. An independent t-test was used to compare quantitative variables between groups. The Chi-squared and Fisher’s exact tests were used to examine the relative distribution of patients assigned to different categories of qualitative variables.
Findings
Out of the 455 elderly participants in the study, 247 (54.3%) were female. Regarding age, 56.7% of the elderly were in the age group of 60-69 years (young-old), and 33.6% were in the age group of 70-79 years (middle-old). Also, 26.4% of the participants had a diploma, 75.4% were married, 71.4% had more than two children, 45.5% were retired, 47% had a monthly income of more than $110, and 67.5% had at least one chronic disease. In addition, 54.5% of the elderly were living with their spouse at the time of answering the questionnaire. In terms of BMI, 42.0% were overweight. The results indicated that the healthy lifestyle score was associated with education, occupation, income level, and living status. Elderly participants who had attained a higher level of education demonstrated higher lifestyle scores. As income increased, the lifestyle score increased as well. Additionally, the elderly who resided with their spouse and family exhibited a higher quality of life score (Table 1).
Table 1. Frequency of socio-demographic characteristics and comparison of the lifestyle scores in the elderly
Most participants (60.9%) were found to have a healthy lifestyle. Among the various components, prevention had the highest balanced score (0-100) for a healthy lifestyle in the elderly, while physical activity had the lowest score.
Outcome expectancies had the highest average score at 80.7%, while the self-efficacy structure had the lowest average score at 60.2% in the constructs of SCT. Regarding the correlation between SCT constructs and healthy lifestyle scores in the elderly, all correlations were significant and direct (Table 2). The strongest correlation between healthy lifestyle and SCT constructs was found in the self-regulation construct (r=0.48; p<0.001), while the weakest was found in the awareness construct (r=0.21; p<0.001). Additionally, the highest correlation was observed between SCT constructs, specifically between social support and observational learning (r=0.77; p<0.001), while the lowest correlation was found between awareness and self-efficacy (r=0.16; p=0.001; Table 2).
Table 2. Correlation between the social cognitive theory constructs and healthy lifestyle score
Discussion
The current study aimed to leverage the utility of SCT constructs as a theoretical basis for tailoring lifestyle programs to Sthe elderly population. Based on SCT studies, various constructs have been identified as the strongest predictors of lifestyle-related behaviors in the elderly [20-24]. In our study, the self-efficacy constructs obtained the lowest percentage (68.15%), while the outcome expectation constructs (84.55%) and outcome expectancies (84%) scored the highest. Other researchers have found similar results, reporting outcome expectancies scoring the highest, while self-efficacy scores the lowest [25]. Additionally, the expectation of the outcome is the construct with the highest score among the constructs of SCT [23]. In the study by Ghoreishi et al. [25], anticipation, outcome expectancies, and self-regulation are the strongest predictors. However, the findings of our study are inconsistent with those of Amini Moridani et al. [26], who found that perceived social support constructs obtain the highest score, while environmental structures score the lowest. The reason for this difference may be variations in study timing and cultural differences across the studied cities.
There was no statistically significant difference between the mean scores of SCT constructs by gender and BMI. There was a significant relationship between constructs’ outcome expectancies and outcome expectations with a history of chronic disease. The elderly with no history of chronic disease had higher mean structural value scores and expected outcomes. The importance that the elderly attribute to desired behaviors forms the foundation for health promotion. In contrast, our study’s findings contradict those that reported a significant relationship between the history of chronic disease and both self-efficacy and self-regulatory structure [27]. This difference may be due to differences in the study subjects. Another significant finding of this study was the relationship between the mean score of outcome expectancies and the number of children. Elderly with two children tended to achieve better-expected outcomes on average. Unfortunately, no similar article was found regarding these findings. Children can support their parents when they become old, and it is most likely that the elderly who have more children will receive more support compared to those without children.
A significant relationship was observed between the construct of outcome expectancies and social support with living status. Old people living with families had an average outcome expectancy score, and elderly people living with their spouses had a higher social support score because of the increased need for family support. On the other hand, the results of our study oppose those of Heidari-Soureshjani et al. [27], reporting a statistically considerable association between marital status and self-efficacy. The variation in the findings may be due to discrepancies in the populations examined (only women with diabetes referring to diabetes centers).
There was a significant relationship between the mean value of constructs and outcome expectation, social support, observational learning, and self-regulation according to education. The average score of these constructs was higher in the elderly who have a university education. With the increase in education, people’s awareness increases due to the ability to read different books and magazines or benefit from scientific websites, which is attributed to the literacy of the elderly with the ability to read different books and have life skills. Their worldview is better and more open towards life. These results are consistent with findings from other studies [28-31].
A statistically significant relationship between the mean values of SCT constructs and the outcome and social support based on occupation. Among the elderly, those employed as employees scored higher in these two constructs compared to their counterparts, which is in line with the results of other studies [17, 30]. However, Heidari-Soureshjani et al. [27] reported that there is a statistically significant relationship between employment status and self-efficacy and self-regulation structures, contradicting our findings. This contradiction may be due to factors, such as the gender and diabetes condition of the participants, as well as the variances in time between the two studies.
There was a statistically significant relationship between the constructs of awareness, outcome expectancies and expectations, social support, observational learning, and self-regulation in terms of income. The average scores of these constructs were higher among the elderly with higher incomes (>$110). Income and economic status are among the most important determinants of health in people, especially the elderly [10, 28, 31]. Therefore, government policies should prioritize providing special financial support through organizations like the Ministry of Welfare and Social Affairs. This support would encourage families who are unable to care for the elderly and ensure that all seniors can enjoy the benefits of living with family [32].
The findings also showed a direct and positive relationship between the mean scores of awareness, self-efficacy, outcome expectancies, social support, observational learning, self-regulation, and healthy lifestyle. Khani Jeihooni et al. [33] and Ryan [34] reported that there is a statistically significant relationship between nutritional performance, walking, and self-regulation, indicating consistency with the present study. These results suggest that the constructs of awareness, self-efficacy, outcome expectancies, social support, observational learning, and self-regulation from the SCT play an important role in healthy lifestyle behavior.
According to the results of the present study, of all the variables, including SCT and demographic variables, 26.3% of healthy lifestyle behavior was predicted by these two categories of variables. The constructs of social support, self-regulation, outcome expectancies, and awareness showed significant predictability using a multivariate linear regression model and step-wise method. They accounted for 25.9% of the variance in lifestyle behavior. According to this model, the included demographic variables were not significant and were removed from the model. Similar findings have also been observed in previous studies [35-37]. Therefore, as individuals age and enter old age, the need for environmental support, particularly from family members, increases. In general, social support has a positive impact on the lifestyle of older adults [35].
Regarding awareness, older individuals exhibited a higher level of awareness, knowledge, and information regarding health-promoting behaviors and lifestyles, also known as health literacy. They demonstrated an equal understanding and application of health issues and lifestyle. Moreover, these individuals were perceived more favorably. According to Bandura, self-regulatory strategies are crucial for targeting and planning regular physical activity [38]. Self-regulation plays a pivotal role in social cognitive approaches to modifying health behaviors. In our study, elderly participants who practiced self-control and goal setting in shaping their lifestyle behaviors exhibited a more desirable lifestyle. Furthermore, the likelihood of engaging in desired behavior increases with an individual’s higher value placed on the expected outcome.
Step-wise multiple regression analyses conducted in the study by Sung & Lim [39] revealed that the social support structure, with a 55% predictive power, is the strongest predictor for a health-promoting lifestyle. Peyman et al. [40] reported that self-regulatory and social support are the strongest predictors of physical activity in type 2 diabetic women. The results of Liu’s study [41] demonstrated that social support structures from friends are the strongest predictors according to the SCT in students’ physical activity. Umstattd & Hallam [23] indicated that self-regulation and expectation are the most influential factors in predicting physical activity among adults.
Our results are inconsistent with those of Yari et al. [35], where self-efficacy is one of the strongest predictors of physical activity, and also with the study by Nematollahi & Eslami [42], in which self-regulation has the greatest impact on physical activity, while self-efficacy has the least impact. The existing discrepancy in this field can be justified by the differences between the geographical area, culture, and climate of the present study.
Linear regression analysis in the study by Abdi et al. [43] showed that among the SCT constructs, environment and self-efficacy are the strongest predictors of a healthy lifestyle in overweight and obese employees. However, their results are inconsistent with ours. This discrepancy may be due to differences in the target groups regarding climatic and occupational conditions of the study subjects. According to Mahmoudi et al. [36], the SCT constructs (self-efficacy, outcome expectations, outcome expectancies, family support, and friend support) account for 13% of the variance of physical activity behavior in Borkhar and Shahin Shahr health network employees in Isfahan. The results of the present study are inconsistent with this study.
Furthermore, in the study by Gothe & Kendall [44], self-efficacy and outcome expectation are the most important predictors of physical activity for African-American adults. The findings of the present study were inconsistent with this study. These differences may be attributed to the heterogeneous population in the mentioned studies, which had different age ranges, demographic characteristics, and cultural and climatic differences that were distinct from the present study.
Among the limitations of the present study was the collection of information in a self-reporting manner. This method, which relied on participants being honest and accurate in answering questions, was beyond the control of the researcher. Additionally, the study faced challenges due to the large number of questions included in the questionnaire. It is important to note that the data collection coincided with the COVID-19 pandemic, which posed difficulties in ensuring convenient access to all elderly participants during quarantine. These circumstances may have influenced the quality of the data obtained. The results highlighted the importance of targeting these cognitive and social constructs when designing educational interventions to foster healthy lifestyles in the elderly. Further research is needed to explore other potential variables that may influence healthy lifestyle behaviors in this age group.
Conclusion
SCT is a suitable framework for understanding and promoting healthy lifestyles among the elderly. Factors, such as awareness, self-efficacy, self-regulation, social support, outcome expectations, and observational learning are key predictors of healthy lifestyle behaviors in the elderly, with social support, both from peers and family, being a particularly important factor.
Acknowledgments: The authors express their gratitude to the research deputy of Tehran and Guilan University, and they would like to express their gratitude and appreciation to the elderly for their sincere cooperation.
Ethical Permissions: This article is part of the MSc thesis on health education and health promotion (2020.434) and was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.2020.434).
Conflicts of Interests: The authors declared no potential conflicts of interests.
Authors’ Contribution: Bakhshi F (First Author), Introduction Writer/Assistant Researcher (30%); Safavi SR (Second Author), Main Researcher/Statistical Analyst/Methodologist/Discussion Writer (40%); Sadeghi R (Third Author), Statistical Analyst/Assistant Researcher (30%)
Funding/Support: None declared by the authors.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2024/03/24 | Accepted: 2024/05/15 | Published: 2024/06/21
Received: 2024/03/24 | Accepted: 2024/05/15 | Published: 2024/06/21
References
1. World Health Organization. World report on ageing and health. Geneva: World Health Organization; 2015. [Link]
2. United Nations. World population ageing 2019. New York: United Nations; 2020. [Link]
3. Statistical Center of Iran. The results of the 2016 national population and housing census. Tehran: Statistical Center of Iran; 2018. [Link]
4. Wang J, Chen CY, Lai LJ, Chen ML, Chen MY. The effectiveness of a community-based health promotion program for rural elders: A quasi-experimental design. Appl Nurs Res. 2014;27(3):181-5. [Link] [DOI:10.1016/j.apnr.2013.11.014]
5. Suraj S, Singh A. Study of sense of coherence health promoting behavior in north Indian students. Indian J Med Res. 2011;134(5):645-52. [Link] [DOI:10.4103/0971-5916.90989]
6. Fernández-Villa JM, Márquez DX, Sánchez-Garrido N, Pérez-Zepeda MU, González-Lara M. Association of healthy habits beliefs and mortality in older adults: A longitudinal analysis of the Mexican health and aging study. J Aging Health. 2017;29(6):973-85. [Link] [DOI:10.1177/0898264317719130]
7. Lee TW, Ko IS, Lee KJ. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: A cross-sectional survey. Int J Nurs Stud. 2006;43(3):293-300. [Link] [DOI:10.1016/j.ijnurstu.2005.06.009]
8. Walker SN, Sechrist KR, Pender NJ. The health-promoting lifestyle profile: Development and psychometric characteristics. Nurs Res. 1987;36(2):76-81. [Link] [DOI:10.1097/00006199-198703000-00002]
9. Davies N. Promoting healthy ageing: The importance of lifestyle. Nurs Stand. 2011;25(19):43-9. [Link] [DOI:10.7748/ns.25.19.43.s51]
10. Chia F, Huang WY, Huang H, Wu CE. Promoting healthy behaviors in older adults to optimize health-promoting lifestyle: An intervention study. Int J Environ Res Public Health. 2023;20(2):1628. [Link] [DOI:10.3390/ijerph20021628]
11. McKenzie JF, Neiger BL, Thackeray R. Planning, implementing and evaluating health promotion programs. Burlington: Jones & Bartlett Learning; 2022. [Link]
12. Nutbeam D, Harris E, Wise W. Theory in a nutshell: A practical guide to health promotion theories. Sydney: McGraw-Hill; 2010. [Link]
13. Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv. 2015;9(2):305-38. [Link] [DOI:10.1007/s11764-014-0413-z]
14. Bandura A. Social cognitive theory: An agentic perspective. Annu Rev Psychol. 2001;52:1-26. [DOI:10.1146/annurev.psych.52.1.1]
15. McHugh J, Lee O, Aspell N, Lawlor BA, Brennan S. A shared mealtime approach to improving social and nutritional functioning among older adults living alone: study protocol for a randomized controlled trial. JMIR Res Protoc. 2015;4(2):e43. [Link] [DOI:10.2196/resprot.4050]
16. Bagherniya M, Sharma M, Mostafavi Darani F, Maracy MR, Safarian M, Allipour Birgani R, et al. School-based nutrition education interventions to promote healthy behaviors among adolescents: A systematic review. Adv Nutr. 2019;10(5):826-39. [Link]
17. Bandura A. Social foundations of thought and action: A social cognitive theory. New Jersey: Prentice-Hall; 1986. [Link]
18. Eshaghi SR, Farajzadegan Z, Babak A. Healty lifestyle assessment questionnaire in elderly: Translation, reliability and validity. Payesh. 2010;9(1):91-9. [Persian] [Link]
19. Alaei A, Rezaei M, Sadeghi K. A cross-sectional study on the prevalence of chronic diseases among individuals aged 60 and above in Rasht City, northern Iran. J Aging Res. 2021, 1234567. [Link]
20. Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The self-efficacy scale: Construction and validation. Psychol Rep. 1982;51(2):663-71. [Link] [DOI:10.2466/pr0.1982.51.2.663]
21. White SM, Wójcicki TR, McAuley E. Social cognitive influences on physical activity behavior in middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2012;67(1):18-26. [Link] [DOI:10.1093/geronb/gbr064]
22. Uszynski MK, Casey B, Hayes S, Gallagher S, Purtill H, Motl RW, et al. Social cognitive theory correlates of physical activity in inactive adults with multiple sclerosis. Int J MS Care. 2018;20(3):129-35. [Link] [DOI:10.7224/1537-2073.2016-111]
23. Umstattd MR, Hallam J. Older adults' exercise behavior: Roles of selected constructs of social-cognitive theory. J Aging Phys Act. 2007;15(2):206-18. [Link] [DOI:10.1123/japa.15.2.206]
24. Stacey F, James E, Chapman K, Lubans D. Social cognitive theory mediators of physical activity in a lifestyle program for cancer survivors and carers: Findings from the ENRICH randomized controlled trial. Int J Behav Nutr Phys Act. 2016;13:49. [Link] [DOI:10.1186/s12966-016-0372-z]
25. Ghoreishi MS, Vahedian-Shahroodi M, Esmaily H, Tehrani H. Predictive factors related to self-care behaviors among type2 diabetic patients by using social cognitive model. Iran J Health Educ Health Promot. 2018;6(3):241-50. [Persian] [Link] [DOI:10.30699/acadpub.ijhehp.6.3.241]
26. Amini Moridani M, Tol A, Sadeghi R, Mohebbi B, Azam K. Assessing the effect of family-based intervention education program on perceived social support among older adults with type 2 diabetes: Application of social cognitive theory. J Nurs Educ. 2015;4(3):30-40. [Persian] [Link]
27. Heidari-Soureshjani S, Yarmohammadi P, Torabi-Farsani Z, Solati K, Ahmadi A. Relationship between adherence to health behaviors and several social cognitive theory structures in diabetic women. J Diabetes Nurs. 2018;6(3):517-29. [Persian] [Link]
28. Tang H, Zhang W, Liu W, Xiao H, Jing H, Song F, et al. The nutritional literacy of breast cancer patients receiving chemotherapy and its association with treatment self-regulation and perceived social support. Support Care Cancer. 2023;31(8):472. [Link] [DOI:10.1007/s00520-023-07941-x]
29. Abusalehi A, Vahedian-Shahroodi M, Esmaily H, Jafari A, Tehrani H. Mental health promotion of the elderly in nursing homes: A social-cognitive intervention. Int J Gerontol. 2021;15(3):221-7. [Link]
30. Kaveh MH, Montazer M, Karimi M, Hassanzadeh J. Effects of a theory-based training program with follow-up home visits on self-management behavior, glycemic index, and quality of life among Iranian patients with type 2 diabetes mellitus. BMC Public Health. 2022;22(1):1559. [Link] [DOI:10.1186/s12889-022-13959-3]
31. Zheng X, Xue Y, Dong F, Shi L, Xiao S, Zhang J, et al. The association between health-promoting-lifestyles, and socioeconomic, family relationships, social support, health-related quality of life among older adults in china: A cross sectional study. Health Qual Life Outcomes. 2022;20(1):64. [Link] [DOI:10.1186/s12955-022-01968-0]
32. Rababa M, Al Ali N, Alshaman A. Health promoting behaviors, health needs and associated factors among older adults in Jordan: A cross-sectional study. Int J Community Based Nurs Midwifery. 2021;9(2):106-16. [Link]
33. Khani Jeihooni A, Hidarnia A, Kaveh MH, Hajizadeh E, Gholami T. Survey of osteoporosis preventive behaviors among women in Fasa: The application of the health belief model and social cognitive theory. Iran South Med J. 2016;19(1):48-62. [Persian] [Link]
34. Ryan P. Integrated theory of health behavior change: Background and intervention development. Clin Nurse Spec. 2009;23(3):161-70. [Link] [DOI:10.1097/NUR.0b013e3181a42373]
35. Yari A, Hassani L, Ziapour A, Toghroli R, Mohammadkhah R, Yazdi F. Prediction of self-care behaviors among diabetic patients based on social cognitive theory. J Public Health Res. 2023;12(1):22799036221150330. [Link] [DOI:10.1177/22799036221150330]
36. Mahmoudi I, Fathian-Dastgerdi Z, Eslami AA. Factors explaining regular physical activity among Borkhar and Shahinshahr health network employees, Isfahan, Iran, based on social cognitive theory. Health Syst Res. 2018;14(2):252-7. [Persian] [Link]
37. Visser M, Wijnhoven HA, Comijs HC, Thomése FG, Twisk JW, Deeg DJ. A healthy lifestyle in old age and prospective change in four domains of functioning. J Aging Health. 2019;31(7):1297-314. [Link] [DOI:10.1177/0898264318774430]
38. Bandura A, Freeman WH, Lightsey R. Self-efficacy: The exercise of control. J Cogn Psychother. 1999;13(2). [Link] [DOI:10.1891/0889-8391.13.2.158]
39. Sung MH, Lim YM. The study on health promoting lifestyle of the elderly women. Taehan Kanho Hakhoe Chi. 2003;33(6):762-71. [Korean] [Link] [DOI:10.4040/jkan.2003.33.6.762]
40. Peyman N, Mahdizadeh M, Taghipour A, Esmaily H. Using of social cognitive theory: Predictors of physical activity among women with diabetestype 2. J Res Health. 2013;3(2):345-54. [Link]
41. Liu J, Zeng M, Wang D, Zhang Y, Shang B, Ma X. Applying social cognitive theory in predicting physical activity among Chinese adolescents: A cross-sectional study with multigroup structural equation model. Front Psychol. 2022;12:695241. [Link] [DOI:10.3389/fpsyg.2021.695241]
42. Nematollahi M, Eslami AA. A survey of social cognitive determinants of physical activity among Iranian women using path analysis method. J Prev Med Hyg. 2019;60(1):E43-9. [Link]
43. Abdi J, Eftekhar H, Mahmoodi M, Shojayzadeh D, Sadeghi R, Saber M. Effect of the intervention based on new communication technologies and the social-cognitive theory on the weight control of the employees with overweight and obesity. J Res Health Sci. 2015;15(4):256-61. [Link]
44. Gothe NP, Kendall BJ. Barriers, motivations, and preferences for physical activity among female African American older adults. Gerontol Geriatr Med. 2016;2:2333721416677399. [Link] [DOI:10.1177/2333721416677399]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |