Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 761-765 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sridhar S, Srinivasan V, Muthulakshmi K, Bhuvana B, Arithra A, Suganthirababu P et al . Impact of Physical Therapy on Post Traumatic Stress Disorder in Post COVID-19 Geriatric Survivors. Health Educ Health Promot 2023; 11 (5) :761-765
URL: http://hehp.modares.ac.ir/article-5-74309-en.html
URL: http://hehp.modares.ac.ir/article-5-74309-en.html
S. Sridhar1, V. Srinivasan *2, K. Muthulakshmi1, B. Bhuvana1, A. Arithra1, P. Suganthirababu1, J. Alagesan1
1- Saveetha College of Physiotherapy, Saveetha Institute of Medical and Technical Sciences, Chennai, India
2- Saveetha Institute of Medical and Technical Sciences, Chennai, India
2- Saveetha Institute of Medical and Technical Sciences, Chennai, India
Keywords: Post-Traumatic Stress Disorder [MeSH], Transcutaneous Nerve Stimulation [MeSH], Relaxation [MeSH]
Full-Text [PDF 536 kb]
(1835 Downloads)
| Abstract (HTML) (665 Views)
Full-Text: (88 Views)
Introduction
The coronavirus disease outbreak of 2019 (COVID-19) began in Wuhan, China, and spread throughout the world at a quick rate, raising concerns about public health. The new coronavirus was found to have a greater effect on elderly individuals, specifically on those with a higher comorbidity burden. In actuality, older persons are far more vulnerable to COVID-19 problems because of the immune system's aging-related alterations linked to multimorbidity [1]. The COVID-19 problems that we address here merely correspond to the psychiatric illnesses and the stressors elderly people experience in their day-to-day lives. Elderly survivors who were exposed to new trauma reported having more intrusive thoughts and experiencing symptoms of hyperarousal associated with the reactivation of traumatic memories [2, 3]. The traumatic experiences they faced during the COVID-19 outbreak were tremendous which led to the majority of the elderly developing post-traumatic stress disorder (PTSD) [4].
PTSD is an important concern of public health and it is defined by three main symptom clusters. The three main symptom clusters of PTSD are bothersome thoughts, methods of avoidance, and heightened arousal [5]. The DSM third edition published by the American Psychiatric Association (APA), presents PTSD as a diagnosis. According to the APA [6], PTSD is defined by three symptom clusters under the DSM-IV-TR: Intrusion, avoidance, and hyperarousal. Initially, individuals with PTSD frequently relive parts of the horrific incident through intense and bothersome flashbacks and nightmares [7]. Refusing to engage with people, places, things, ideas, and other stimuli connected to the traumatic experience is the second cluster of symptoms [8]. Hyper-arousal symptoms, which encompass symptoms that include poor memory and focus, trouble sleeping, physiological responsiveness, higher startle response, and hypervigilance, constitute an element of the third cluster [9, 10]. There are numerous reasons why this phenomenon might occur, including Reminiscence and life review activities that frequently occur in the elderly [11]. The sentiments of being powerless and vulnerable may also have an adverse effect [12].
Psychological treatment, neurostimulation techniques, medication, and mind-body interventions, relaxation techniques are various treatments given in the management of PTSD. Two classes of antidepressants, such as SSRIs and SNRIs, are examples of pharmaceutical treatments for PTSD [13]. There are non-invasive and invasive approaches used in neurostimulation techniques. The non-invasive techniques include Electroconvulsive Therapy (ECT), Vagal Nerve Stimulation, Electrical Stimulation at the transcranial level, Direct Current Stimulation at the transcranial level (tDCS), Repetitive Magnetic Stimulation at the transcranial level (rTMS). Examples of invasive methods are Stimulation of the brain (DBS) and Transcutaneous Vagus Nerve Stimulation (VNS) [14].
The Impact of Event Scale-Revised (IES-R) is an outcome measure used to assess post-traumatic stress disorder. The IES-R is a frequently utilized self-administered tool that assesses psychological triggered by a traumatic occurrence [15]. Weiss created the IES-R scale, a revised 22-item version in 1997 to fulfill the DSM-IV criteria. They did this by adding questions on hyper-arousal symptoms and flashback experiences to the original variant. Because of the IES-R's high concurrent validity, ease of administration, and internal reliability, it is also one of the most valid tools for evaluating PTSD and its post-trauma experiences [16, 17].
Stress should be affected by alteration to the vagus nerve, according to the neuroanatomy of stress management. The areas involved in controlling stress are the insula and amygdala. During stimulation of the vagal nerve, these areas become more active when VNS is applied [18, 19]. Non-invasive taVNS devices have the same effectiveness as the devices that are implanted, and the former offers the advantages of being affordable, non-invasive, lightweight, and experiencing fewer side effects [20]. Transcutaneous devices fall into two categories: Auricular (taVNS) and cervical (tcVNS). The devices used are called the trans auricular devices. The support that is obtained structurally is from the concha of the ear which encompasses the vagal nerve’s auricular branch [21].
Jacobson’s progressive muscle relaxation technique (JPMRT) is one of the mind-body interventions and may also have a beneficial effect on PTSD [22]. There are numerous physiological and psychological advantages to using the JPMRT [23]. The JPMRT counteracts the negative effects of stress by reducing sympathetic nervous system activity and balancing the anterior and posterior hypothalamus. By using the JPMRT, one can increase bodily and mental calmness by reducing muscle contraction [24]. Accordingly, the study aimed to determine how well taVNS reduces PTSD among post-COVID-19 geriatric survivors.
Materials and Methods
Study design and participant selection
The study was carried out in a tertiary hospital and old age homes in the southern part of India from November 2022 to October 2023. The geriatric population, those who survived the COVID-19 pandemic and had traumatic experiences with it, was chosen. Prior to participant recruiting, the study proposal was submitted, and approval was given by the Institutional Scientific Research Board (ISRB). Ethical approval was given for the study treatment protocol. The selection of participants was done based on the IES-R value of more than 24; participants' drug dosage was tapered for post-traumatic stress disorder one month before the start of the intervention, both male and female participants and participants who committed to taking part in the therapy and follow-up and acknowledged the subject matter of the scale were included. Exclusion criteria included participants with an IES-R value of less than 24, participants having a history of mental illness of any kind, those with cardiovascular conditions, and those who expressed no interest in taking part in the study. Out of the 80 individuals who were invited to take part in the study, 60 expressed interests. The IES-R was used as the assessment tool to assess the 60 participants, out of which 24 participants were diagnosed with PTSD. A total of 24 participants were included in the study. Following a thorough explanation of the study to each of the 24 participants, informed consent was obtained. Informed consent was given by each participant. Participant numbers were randomly assigned to two groups of twelve each using the closed envelope technique.
Impact of Event Scale-Revised (IES-R)
The DSM-III of APA presents clusters of symptoms that are indicative of PTSD, and these clusters of symptoms form the basis of the self-administered, 22-item IES-R questionnaire. Participants are said to have mild PTSD if their score ranges between 24-32, moderate PTSD if scores range between 33-36, and severe PTSD if scores range above 37. Using the IES-R scale, the stress developed due to trauma was measured on day 0 and day 28 (end of the fourth week).
Procedure
Two groups, the taVNS group and the JPMRT group, were randomly assigned to participants. The allocation process used a computer-generated random sequence, and the participant's allocation was kept within a closed envelope. The taVNS group underwent treatment for four weeks (1 month). Each week comprised four sessions. Each session was for thirty minutes. The positioning of the electrodes was on the left ear over the cymbal concha. A waveform of sinusoidal pattern with 250 millisecond pulse width, 20 Hz frequency, 80 µs pulse width, and 1.5 milliampere amplitude was chosen as the stimulation configuration. The JPMRT group underwent treatment for four weeks (1 month). Each week, there were four sessions, each lasting thirty minutes. Participants in the Jacobson relaxation technique were asked to close their eyes and sit in a comfortable position. Participants in this exercise cycle were instructed to contract their muscles tightly, hold them for five slow counts, and then quickly and totally relax them for ten seconds. After each step, they were asked to take three deep breaths, inhaling through their nose and expelling through their mouth to relax.
Data on post-test values were gathered, and the participants' post-treatment IES-R scores were evaluated. The obtained pre- and post-treatment scores were documented and evaluated statistically.
Statistical analysis
Data was obtained on days 0 and 28 using the IES-R. Twenty-four participants in groups taVNS and JPMRT, each with twelve participants, were statistically assessed. For groups taVNS and JPMRT in the IES-R scale, the Wilcoxon signed rank test is utilized to determine within the group pre-test and post-test values. To analyze post-treatment values between groups taVNS and JPMRT, the Mann-Whitney rank sum test was used.
Findings
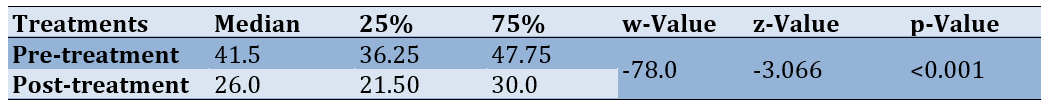
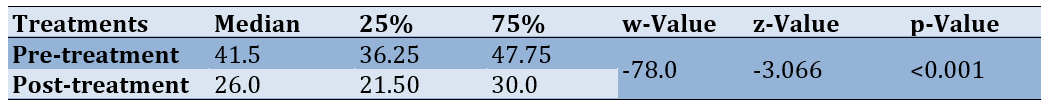
Data obtained using IES-R was examined statistically. The taVNS group and JPMRT group's pre-treatment and post-treatment IES-R scores obtained underwent data analysis using the Wilcoxon signed rank test. The taVNS group and JPMRT group's post-treatment IES-R scores obtained underwent data analysis using the Mann-Whitney rank sum test. The pre-test scores of the taVNS group using IES-R exhibit a median value of 41.5, with 25% of values being 36.25 and 75% of values being 47.75. The post-test scores of the taVNS group using IES-R exhibit a median value of 26.0, with 25% values of 21.5 and 75% values of 30.0. The discrepancy of values that occurred within the group is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 1).
Table 1. IES-R scale pre-treatment and post-treatment values of taVNS group obtained using Wilcoxon-Signed rank test
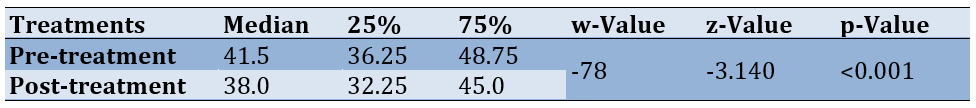
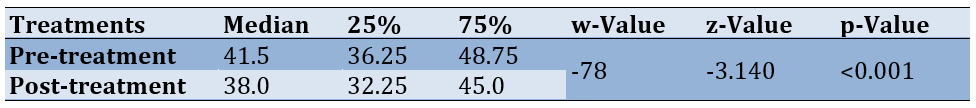
The pre-test value of the JPMRT group using IES-R exhibits a median value of 41.5, with 25% of values being 36.25 and 75% of values being 47.75. The post-test values of the JPMRT group using IES-R exhibit a median value of 38.0, with 25% of values of 32.25, and 75% of values of 45.0. The discrepancy of values that occurred within the group is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 2).
Table 2. IES-R scale pre-treatment and post-treatment values of JPMRT group obtained using Wilcoxon-Signed rank test
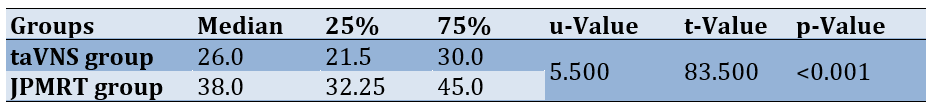
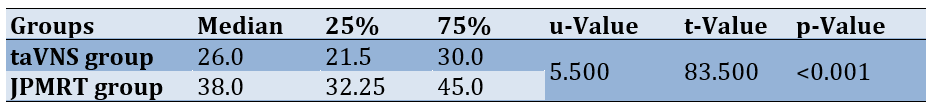
The Mann-Whitney rank sum test was utilized to compare the median values of the taVNS group and the JPMRT group post-tests using the IES-R. The results indicate that for the taVNS group post-test, the median value is 26.0, with 25% at 21.5, and 75% at 30.0. Conversely, for the JPMRT group post-test, the median value of IES-R is 38.000, with 25% at 32.25 and 75% at 45.0. The discrepancy in median values between the two groups is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 3).
Table 3. IES-R scale post-treatment values of the taVNS group and JPMRT group obtained using Mann-Whitney rank sum test
Discussion
The purpose of this study was to investigate the presence of undetected post-traumatic stress disorder among elderly individuals who have survived COVID-19. The primary purpose of the study is to assess the efficacy of taVNS in treating PTSD in older adults who survived the COVID-19 pandemic. According to our findings, transcutaneous auricular vagal nerve stimulation significantly affects the regulation of PTSD and has a great impact on reducing PTSD.
PTSD poses a substantial public health concern. Initially, individuals suffering from PTSD frequently relive parts of the horrific incident through intense and bothersome flashbacks and nightmares [7]. Rutherford et al. conducted a study on the COVID-19 pandemic’s mental response of older adults and concluded that the traumatic experiences the geriatric population faced during the COVID-19 outbreak were tremendous, which led to the majority of the elderly population having PTSD [4]. Kinzie et al. conducted a study on the effects of September 11 on traumatized refugees and found that a stressor that occurs later in life will bring back the distressing memories associated with a past trauma [2]. Hence, there is a need to address this issue and find a solution for COVID-19’s impacts on the elderly population. Many non-invasive neurostimulation methods, including transcutaneous vagal nerve stimulation and stimulation of the brain at a deeper level (DBS), are available as treatment options for PTSD [14]. Bremner et al. conducted a study on the application of non-invasive vagal nerve stimulation to treat psychiatric disorders associated with stress and concluded that taVNS targets the auricular branch of taVNS and has an effect on stress physiology and is effective in the prevention and treatment of stress-related disorders [25]. The effectiveness of taVNS among geriatric survivors to lessen PTSD during the post-COVID-19 pandemic was investigated with the support of the literature that is available. Jacobson’s relaxation technique is one among the mind-body interventions and also has a beneficial effect on PTSD. Akbari et al., conducted a study on relaxation techniques on Stress in Multiple Sclerosis Patients [Jacobsen and Benson] and concluded that the Jacobson relaxation technique is helpful in lessening anxiety, stress, and depression [22].
Horowitz et al. established the IES scale. Weiss et al. designed a revised version of the scale, IES-R, which was utilized in this investigation. The scale included the 22-item version, and higher scores indicate severe PTSD. The IES-R is the most used measure to evaluate PTSD because of its construct’s validity and reliability [16, 17]. Hence, IES-R was included in the current study as an outcome measure.
According to the statistical analysis of the current study, post-COVID-19 geriatric survivors who received transcutaneous auricular vagal nerve stimulation reported a notable improvement in their ability to manage post-traumatic stress disorder. The study's strength lies in the non-invasive, cost-effective nature of taVNS and Jacobson relaxation techniques.
The limitations of this study include the IES-R Scale being a self-reported questionnaire and a subjective scale in which the perception of feeling might differ from individual to individual. So, the use of objective measurement can help the study much better. As a result, more sophisticated interpretation tools and testing can be used for future research.
Conclusion
taVNS is better and more effective than Jacobson’s progressive muscle relaxation technique in reducing post-traumatic stress disorder among post-COVID-19 geriatric survivors.
Acknowledgments: The author thanks all the participants who contributed to and actively participated in the study. Researchers express their sincere gratitude to the Impact of Event scale-Revised (IES-R) author.
Ethical Permissions: This article is approved under the ethical permission code of 01/017/2023/ISRB/PGSR/SCPT.
Conflicts of Interests: The authors disclosed not having any conflicts of interest.
Authors’ Contribution: Sridhar S (First Author), Methodologist/Discussion Writer (25%); Srinivasan V (Second Author), Introduction Writer/Statistical Analyst (25%); Muthulakshmi K (Third Author), Assistant Researcher (10%); Bhuvana (Fourth Author), Assistant Researcher (10%); Arithra A (Fifth Author), Assistant Researcher (10%); Suganthirababu P (Sixth Author), Introduction Writer/Statistical Analyst (10%); Alagesan J (Seventh Author), Discussion Writer (10%)
Funding/Support: This research was carried out without financial support from the funders.
The coronavirus disease outbreak of 2019 (COVID-19) began in Wuhan, China, and spread throughout the world at a quick rate, raising concerns about public health. The new coronavirus was found to have a greater effect on elderly individuals, specifically on those with a higher comorbidity burden. In actuality, older persons are far more vulnerable to COVID-19 problems because of the immune system's aging-related alterations linked to multimorbidity [1]. The COVID-19 problems that we address here merely correspond to the psychiatric illnesses and the stressors elderly people experience in their day-to-day lives. Elderly survivors who were exposed to new trauma reported having more intrusive thoughts and experiencing symptoms of hyperarousal associated with the reactivation of traumatic memories [2, 3]. The traumatic experiences they faced during the COVID-19 outbreak were tremendous which led to the majority of the elderly developing post-traumatic stress disorder (PTSD) [4].
PTSD is an important concern of public health and it is defined by three main symptom clusters. The three main symptom clusters of PTSD are bothersome thoughts, methods of avoidance, and heightened arousal [5]. The DSM third edition published by the American Psychiatric Association (APA), presents PTSD as a diagnosis. According to the APA [6], PTSD is defined by three symptom clusters under the DSM-IV-TR: Intrusion, avoidance, and hyperarousal. Initially, individuals with PTSD frequently relive parts of the horrific incident through intense and bothersome flashbacks and nightmares [7]. Refusing to engage with people, places, things, ideas, and other stimuli connected to the traumatic experience is the second cluster of symptoms [8]. Hyper-arousal symptoms, which encompass symptoms that include poor memory and focus, trouble sleeping, physiological responsiveness, higher startle response, and hypervigilance, constitute an element of the third cluster [9, 10]. There are numerous reasons why this phenomenon might occur, including Reminiscence and life review activities that frequently occur in the elderly [11]. The sentiments of being powerless and vulnerable may also have an adverse effect [12].
Psychological treatment, neurostimulation techniques, medication, and mind-body interventions, relaxation techniques are various treatments given in the management of PTSD. Two classes of antidepressants, such as SSRIs and SNRIs, are examples of pharmaceutical treatments for PTSD [13]. There are non-invasive and invasive approaches used in neurostimulation techniques. The non-invasive techniques include Electroconvulsive Therapy (ECT), Vagal Nerve Stimulation, Electrical Stimulation at the transcranial level, Direct Current Stimulation at the transcranial level (tDCS), Repetitive Magnetic Stimulation at the transcranial level (rTMS). Examples of invasive methods are Stimulation of the brain (DBS) and Transcutaneous Vagus Nerve Stimulation (VNS) [14].
The Impact of Event Scale-Revised (IES-R) is an outcome measure used to assess post-traumatic stress disorder. The IES-R is a frequently utilized self-administered tool that assesses psychological triggered by a traumatic occurrence [15]. Weiss created the IES-R scale, a revised 22-item version in 1997 to fulfill the DSM-IV criteria. They did this by adding questions on hyper-arousal symptoms and flashback experiences to the original variant. Because of the IES-R's high concurrent validity, ease of administration, and internal reliability, it is also one of the most valid tools for evaluating PTSD and its post-trauma experiences [16, 17].
Stress should be affected by alteration to the vagus nerve, according to the neuroanatomy of stress management. The areas involved in controlling stress are the insula and amygdala. During stimulation of the vagal nerve, these areas become more active when VNS is applied [18, 19]. Non-invasive taVNS devices have the same effectiveness as the devices that are implanted, and the former offers the advantages of being affordable, non-invasive, lightweight, and experiencing fewer side effects [20]. Transcutaneous devices fall into two categories: Auricular (taVNS) and cervical (tcVNS). The devices used are called the trans auricular devices. The support that is obtained structurally is from the concha of the ear which encompasses the vagal nerve’s auricular branch [21].
Jacobson’s progressive muscle relaxation technique (JPMRT) is one of the mind-body interventions and may also have a beneficial effect on PTSD [22]. There are numerous physiological and psychological advantages to using the JPMRT [23]. The JPMRT counteracts the negative effects of stress by reducing sympathetic nervous system activity and balancing the anterior and posterior hypothalamus. By using the JPMRT, one can increase bodily and mental calmness by reducing muscle contraction [24]. Accordingly, the study aimed to determine how well taVNS reduces PTSD among post-COVID-19 geriatric survivors.
Materials and Methods
Study design and participant selection
The study was carried out in a tertiary hospital and old age homes in the southern part of India from November 2022 to October 2023. The geriatric population, those who survived the COVID-19 pandemic and had traumatic experiences with it, was chosen. Prior to participant recruiting, the study proposal was submitted, and approval was given by the Institutional Scientific Research Board (ISRB). Ethical approval was given for the study treatment protocol. The selection of participants was done based on the IES-R value of more than 24; participants' drug dosage was tapered for post-traumatic stress disorder one month before the start of the intervention, both male and female participants and participants who committed to taking part in the therapy and follow-up and acknowledged the subject matter of the scale were included. Exclusion criteria included participants with an IES-R value of less than 24, participants having a history of mental illness of any kind, those with cardiovascular conditions, and those who expressed no interest in taking part in the study. Out of the 80 individuals who were invited to take part in the study, 60 expressed interests. The IES-R was used as the assessment tool to assess the 60 participants, out of which 24 participants were diagnosed with PTSD. A total of 24 participants were included in the study. Following a thorough explanation of the study to each of the 24 participants, informed consent was obtained. Informed consent was given by each participant. Participant numbers were randomly assigned to two groups of twelve each using the closed envelope technique.
Impact of Event Scale-Revised (IES-R)
The DSM-III of APA presents clusters of symptoms that are indicative of PTSD, and these clusters of symptoms form the basis of the self-administered, 22-item IES-R questionnaire. Participants are said to have mild PTSD if their score ranges between 24-32, moderate PTSD if scores range between 33-36, and severe PTSD if scores range above 37. Using the IES-R scale, the stress developed due to trauma was measured on day 0 and day 28 (end of the fourth week).
Procedure
Two groups, the taVNS group and the JPMRT group, were randomly assigned to participants. The allocation process used a computer-generated random sequence, and the participant's allocation was kept within a closed envelope. The taVNS group underwent treatment for four weeks (1 month). Each week comprised four sessions. Each session was for thirty minutes. The positioning of the electrodes was on the left ear over the cymbal concha. A waveform of sinusoidal pattern with 250 millisecond pulse width, 20 Hz frequency, 80 µs pulse width, and 1.5 milliampere amplitude was chosen as the stimulation configuration. The JPMRT group underwent treatment for four weeks (1 month). Each week, there were four sessions, each lasting thirty minutes. Participants in the Jacobson relaxation technique were asked to close their eyes and sit in a comfortable position. Participants in this exercise cycle were instructed to contract their muscles tightly, hold them for five slow counts, and then quickly and totally relax them for ten seconds. After each step, they were asked to take three deep breaths, inhaling through their nose and expelling through their mouth to relax.
Data on post-test values were gathered, and the participants' post-treatment IES-R scores were evaluated. The obtained pre- and post-treatment scores were documented and evaluated statistically.
Statistical analysis
Data was obtained on days 0 and 28 using the IES-R. Twenty-four participants in groups taVNS and JPMRT, each with twelve participants, were statistically assessed. For groups taVNS and JPMRT in the IES-R scale, the Wilcoxon signed rank test is utilized to determine within the group pre-test and post-test values. To analyze post-treatment values between groups taVNS and JPMRT, the Mann-Whitney rank sum test was used.
Findings
Data obtained using IES-R was examined statistically. The taVNS group and JPMRT group's pre-treatment and post-treatment IES-R scores obtained underwent data analysis using the Wilcoxon signed rank test. The taVNS group and JPMRT group's post-treatment IES-R scores obtained underwent data analysis using the Mann-Whitney rank sum test. The pre-test scores of the taVNS group using IES-R exhibit a median value of 41.5, with 25% of values being 36.25 and 75% of values being 47.75. The post-test scores of the taVNS group using IES-R exhibit a median value of 26.0, with 25% values of 21.5 and 75% values of 30.0. The discrepancy of values that occurred within the group is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 1).
Table 1. IES-R scale pre-treatment and post-treatment values of taVNS group obtained using Wilcoxon-Signed rank test
The pre-test value of the JPMRT group using IES-R exhibits a median value of 41.5, with 25% of values being 36.25 and 75% of values being 47.75. The post-test values of the JPMRT group using IES-R exhibit a median value of 38.0, with 25% of values of 32.25, and 75% of values of 45.0. The discrepancy of values that occurred within the group is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 2).
Table 2. IES-R scale pre-treatment and post-treatment values of JPMRT group obtained using Wilcoxon-Signed rank test
The Mann-Whitney rank sum test was utilized to compare the median values of the taVNS group and the JPMRT group post-tests using the IES-R. The results indicate that for the taVNS group post-test, the median value is 26.0, with 25% at 21.5, and 75% at 30.0. Conversely, for the JPMRT group post-test, the median value of IES-R is 38.000, with 25% at 32.25 and 75% at 45.0. The discrepancy in median values between the two groups is statistically significant (p<0.001), suggesting a substantial difference beyond what would occur by chance (Table 3).
Table 3. IES-R scale post-treatment values of the taVNS group and JPMRT group obtained using Mann-Whitney rank sum test
Discussion
The purpose of this study was to investigate the presence of undetected post-traumatic stress disorder among elderly individuals who have survived COVID-19. The primary purpose of the study is to assess the efficacy of taVNS in treating PTSD in older adults who survived the COVID-19 pandemic. According to our findings, transcutaneous auricular vagal nerve stimulation significantly affects the regulation of PTSD and has a great impact on reducing PTSD.
PTSD poses a substantial public health concern. Initially, individuals suffering from PTSD frequently relive parts of the horrific incident through intense and bothersome flashbacks and nightmares [7]. Rutherford et al. conducted a study on the COVID-19 pandemic’s mental response of older adults and concluded that the traumatic experiences the geriatric population faced during the COVID-19 outbreak were tremendous, which led to the majority of the elderly population having PTSD [4]. Kinzie et al. conducted a study on the effects of September 11 on traumatized refugees and found that a stressor that occurs later in life will bring back the distressing memories associated with a past trauma [2]. Hence, there is a need to address this issue and find a solution for COVID-19’s impacts on the elderly population. Many non-invasive neurostimulation methods, including transcutaneous vagal nerve stimulation and stimulation of the brain at a deeper level (DBS), are available as treatment options for PTSD [14]. Bremner et al. conducted a study on the application of non-invasive vagal nerve stimulation to treat psychiatric disorders associated with stress and concluded that taVNS targets the auricular branch of taVNS and has an effect on stress physiology and is effective in the prevention and treatment of stress-related disorders [25]. The effectiveness of taVNS among geriatric survivors to lessen PTSD during the post-COVID-19 pandemic was investigated with the support of the literature that is available. Jacobson’s relaxation technique is one among the mind-body interventions and also has a beneficial effect on PTSD. Akbari et al., conducted a study on relaxation techniques on Stress in Multiple Sclerosis Patients [Jacobsen and Benson] and concluded that the Jacobson relaxation technique is helpful in lessening anxiety, stress, and depression [22].
Horowitz et al. established the IES scale. Weiss et al. designed a revised version of the scale, IES-R, which was utilized in this investigation. The scale included the 22-item version, and higher scores indicate severe PTSD. The IES-R is the most used measure to evaluate PTSD because of its construct’s validity and reliability [16, 17]. Hence, IES-R was included in the current study as an outcome measure.
According to the statistical analysis of the current study, post-COVID-19 geriatric survivors who received transcutaneous auricular vagal nerve stimulation reported a notable improvement in their ability to manage post-traumatic stress disorder. The study's strength lies in the non-invasive, cost-effective nature of taVNS and Jacobson relaxation techniques.
The limitations of this study include the IES-R Scale being a self-reported questionnaire and a subjective scale in which the perception of feeling might differ from individual to individual. So, the use of objective measurement can help the study much better. As a result, more sophisticated interpretation tools and testing can be used for future research.
Conclusion
taVNS is better and more effective than Jacobson’s progressive muscle relaxation technique in reducing post-traumatic stress disorder among post-COVID-19 geriatric survivors.
Acknowledgments: The author thanks all the participants who contributed to and actively participated in the study. Researchers express their sincere gratitude to the Impact of Event scale-Revised (IES-R) author.
Ethical Permissions: This article is approved under the ethical permission code of 01/017/2023/ISRB/PGSR/SCPT.
Conflicts of Interests: The authors disclosed not having any conflicts of interest.
Authors’ Contribution: Sridhar S (First Author), Methodologist/Discussion Writer (25%); Srinivasan V (Second Author), Introduction Writer/Statistical Analyst (25%); Muthulakshmi K (Third Author), Assistant Researcher (10%); Bhuvana (Fourth Author), Assistant Researcher (10%); Arithra A (Fifth Author), Assistant Researcher (10%); Suganthirababu P (Sixth Author), Introduction Writer/Statistical Analyst (10%); Alagesan J (Seventh Author), Discussion Writer (10%)
Funding/Support: This research was carried out without financial support from the funders.
Article Type: Original Research |
Subject:
Health Promotion Approaches
Received: 2024/03/15 | Accepted: 2024/04/26 | Published: 2024/05/20
Received: 2024/03/15 | Accepted: 2024/04/26 | Published: 2024/05/20
References
1. Boccardi V, Ruggiero C, Mecocci P. COVID-19: A geriatric emergency. Geriatrics. 2020;5(2):24. [Link] [DOI:10.3390/geriatrics5020024]
2. Kinzie JD, Boehnlein JK, Riley C, Sparr L. The effects of September 11 on traumatized refugees: Reactivation of posttraumatic stress disorder. J Nerv Ment Dis. 2002;190(7):437-41. [Link] [DOI:10.1097/00005053-200207000-00003]
3. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM Int J Med. 2020;113(5):311-2. [Link] [DOI:10.1093/qjmed/hcaa110]
4. Rutherford BR, Choi CJ, Chrisanthopolous M, Salzman C, Zhu C, Montes-Garcia C, et al. The COVID-19 pandemic as a traumatic stressor: Mental health responses of older adults with chronic PTSD. Am J Geriatr Psychiatry. 2021;29(2):105-14. [Link] [DOI:10.1016/j.jagp.2020.10.010]
5. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048-60. [Link] [DOI:10.1001/archpsyc.1995.03950240066012]
6. Fossion P, Leys C, Kempenaers C, Braun S, Verbanck P, Linkowski P. Beware of multiple traumas in PTSD assessment: The role of reactivation mechanism in intrusive and hyper-arousal symptoms. Aging Ment Health. 2015;19(3):258-63. [Link] [DOI:10.1080/13607863.2014.924901]
7. Davison EH, Pless AP, Gugliucci MR, King LA, King DW, Salgado DM, et al. Late-life emergence of early-life trauma: The phenomenon of late-onset stress symptomatology among aging combat veterans. Res Aging. 2006;28(1):84-114. [Link] [DOI:10.1177/0164027505281560]
8. Lindemann E. Symptomatology and management of acute grief. Am J Psychiatry. 1944;101(2):141-8. [Link] [DOI:10.1176/ajp.101.2.141]
9. Jiao Y, Guo X, Luo M, Li S, Liu A, Zhao Y, et al. Effect of transcutaneous vagus nerve stimulation at auricular concha for insomnia: A randomized clinical trial. Evid Based Complement Alternat Med. 2020;2020:6049891. [Link] [DOI:10.1155/2020/6049891]
10. Somer E. Effects of incest in aging survivors: Psychopathology and treatment issues. J Clin Geropsychol. 2000;6(1):53-61. [Link] [DOI:10.1023/A:1009576223866]
11. Gagnon M, Hersen M. Unresolved childhood sexual abuse and older adults: Late-life vulnerabilities. J Clin Geropsychol. 2000;6(3):187-98. [Link] [DOI:10.1023/A:1009589115942]
12. McNally RJ. Posttraumatic stress disorder and dissociative disorders. In: Blaney PH, Krueger RF, Millon T, editors. Oxford textbook of psychopathology. Oxford: Oxford University Press; 2015. p. 191-204. [Link]
13. Farach FJ, Pruitt LD, Jun JJ, Jerud AB, Zoellner LA, Roy-Byrne PP. Pharmacological treatment of anxiety disorders: Current treatments and future directions. J Anxiety Disord. 2012;26(8):833-43. [Link] [DOI:10.1016/j.janxdis.2012.07.009]
14. Kar SK, Sarkar S. Neuro-stimulation techniques for the management of anxiety disorders: An update. Clin Psychopharmacol Neurosci. 2016;14(4):330-7. [Link] [DOI:10.9758/cpn.2016.14.4.330]
15. Bienvenu OJ, Williams JB, Yang A, Hopkins RO, Needham DM. Posttraumatic stress disorder in survivors of acute lung injury: Evaluating the impact of event scale-revised. Chest. 2013;144(1):24-31. [Link] [DOI:10.1378/chest.12-0908]
16. Beck JG, Grant DM, Read JP, Clapp JD, Coffey SF, Miller LM, et al. The impact of event scale-revised: Psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22(2):187-98. [Link] [DOI:10.1016/j.janxdis.2007.02.007]
17. Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale-revised. Behav Res Ther. 2003;41(12):1489-96. [Link] [DOI:10.1016/j.brat.2003.07.010]
18. Rangon CM, Krantic S, Moyse E, Fougère B. The vagal autonomic pathway of COVID-19 at the crossroad of Alzheimer's disease and aging: A review of knowledge. J Alzheimers Dis Rep. 2020;4(1):537-51. [Link] [DOI:10.3233/ADR-200273]
19. George MS, Ward Jr HE, Ninan PT, Pollack M, Nahas Z, Anderson B, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimul. 2008;1(2):112-21. [Link] [DOI:10.1016/j.brs.2008.02.001]
20. Wang L, Zhang J, Guo C, He J, Zhang S, Wang Y, et al. The efficacy and safety of transcutaneous auricular vagus nerve stimulation in patients with mild cognitive impairment: A double blinded randomized clinical trial. Brain Stimul. 2022;15(6):1405-14. [Link] [DOI:10.1016/j.brs.2022.09.003]
21. Wu Y, Song L, Wang X, Li N, Zhan S, Rong P, et al. Transcutaneous vagus nerve stimulation could improve the effective rate on the quality of sleep in the treatment of primary insomnia: A randomized control trial. Brain Sci. 2022;12(10):1296. [Link] [DOI:10.3390/brainsci12101296]
22. Akbari A, Ahmadi F, Jalili E, Khazaei S. The effect of relaxation technique (Jacobsen and Benson) on depression, anxiety, and stress in patients with multiple sclerosis. Curr Psychiatry Res Rev. 2020;16(3):213-9. [Link] [DOI:10.2174/2666082216999200819105928]
23. Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39:101132. [Link] [DOI:10.1016/j.ctcp.2020.101132]
24. Kumaresan A, Sebastian N, Suganthirababu P, Srinivasan V, Vishnuram S, Kumar P, et al. Efficacy of physiotherapy management on burnout syndrome amongst IT professionals during the COVID-19 pandemic. Work. 2022;73(3):769-75. [Link] [DOI:10.3233/WOR-220051]
25. Bremner JD, Gurel NZ, Jiao Y, Wittbrodt MT, Levantsevych OM, Huang M, et al. Transcutaneous vagal nerve stimulation blocks stress-induced activation of interleukin-6 and interferon-γ in posttraumatic stress disorder: A double-blind, randomized, sham-controlled trial. Brain Behav Immun Health. 2020;9:100138. [Link] [DOI:10.1016/j.bbih.2020.100138]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |