Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 299-307 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mulyana B, Trisyani Y, Nuraeni A, Astrada A, Pamungkas R, Ekawaty D et al . Effect of the Affective Stimulation-Based Family-Centered Integrated Spiritual Support on Psychological Aspects of Acute Coronary Syndrome Patients. Health Educ Health Promot 2024; 12 (2) :299-307
URL: http://hehp.modares.ac.ir/article-5-74151-en.html
URL: http://hehp.modares.ac.ir/article-5-74151-en.html
1- Department of Nursing, Faculty of Health Sciences, Esa Unggul University, Jakarta, Indonesia
2- Department of Critical Care Nursing, Faculty of Nursing, Padjadjaran University, Bandung, Indonesia
3- Department of Education and Training, Tarakan Hospital, Jakarta, Indonesia
4- Department of Education and Training, Wishan Medika Clinic, Jakarta, Indonesia
2- Department of Critical Care Nursing, Faculty of Nursing, Padjadjaran University, Bandung, Indonesia
3- Department of Education and Training, Tarakan Hospital, Jakarta, Indonesia
4- Department of Education and Training, Wishan Medika Clinic, Jakarta, Indonesia
Keywords: Acute Coronary Syndrome [MeSH], Anxiety [MeSH], Chest Pain [MeSH], Coronary Care Unit [MeSH], Psychological Well-Being [MeSH]
Full-Text [PDF 790 kb]
(1557 Downloads)
| Abstract (HTML) (855 Views)
Full-Text: (98 Views)
Introduction
Approximately 422.7 million cases of acute coronary syndrome (ACS) are reported globally, and 17.92 million deaths from ACS are projected to increase to 23.3 million by 2030 [1].
The effects of critical patients with ACS can be categorized into two types, including immediate effects, such as chest pain [2], and indirect effects, which include physical issues (weakness, immobility, muscle stiffness, and pain) as well as psychological issues (pain, hopelessness, fear, grief, feelings of isolation, disturbed sleep, discomfort, and anxiety) resulting from the critical care services required for ACS patients. Furthermore, pain and anxiety are intensified by invasive procedures, separation from family, and the introduction of a new critical care team [3-5].
Anxiety and pain are psychological issues that are among the most common and detrimental to heart health [6]. Persistent pain and anxiety experienced by patients can impede the healing process and survival in conditions such as infarction, endothelial dysfunction, myocardial ischemia, plaque rupture, thrombosis, and malignant arrhythmias. Additionally, a decrease in bodily resistance can occur in patients, increasing the risk of death due to hormonal imbalances caused by stress, including elevated levels of cortisol, thyroid hormones, and sympathetic nerve activity, which in turn raises the body’s metabolism. Uncontrolled metabolism due to pain and anxiety can further hinder the healing process. Moreover, in patients with ACS, oxygen consumption must be carefully regulated, as the oxygen supply to the heart is limited, which inhibits the heart’s ability to pump blood effectively without adequate oxygen [7].
Pharmacological therapies can alleviate or eliminate pain and anxiety in individuals with ACS. However, these therapies may not always provide optimal pain relief, and it is impossible to separate the development of side effects from ongoing pharmacological use. Therefore, non-pharmacological therapy (as an additional treatment) is necessary to reduce or eliminate pain [8]. Non-pharmacological treatments for pain and anxiety can include relaxation techniques, hypnotherapy, music therapy, massage, dhikr, and family-based interventions [9-11].
Since pain and anxiety are subjective responses of patients, the interventions should focus on changing the patient’s emotional response to these feelings. Family-centered affective stimulation is an intervention carried out by family members on patients, based on two main aspects: sensory and affective. This intervention is conducted repeatedly to provide encouragement, motivation, and enthusiasm to patients, helping them change their perception of the pain and anxiety they experience. The repetition of certain words or phrases that incorporate elements of faith and belief can elicit a stronger relaxation response than relaxation techniques that lack these elements. The patient’s spiritual beliefs hold a calming significance, as they serve as a source of individual coping that aids the patient in adapting to the stressors they encounter [12].
The difference in the effects of stimulation provided by familiar versus unfamiliar individuals is significant. Patients may receive and respond to sensory and affective stimuli differently depending on whether the stimulation comes from someone they know or not. Sensory and affective stimulation provided by family members is considered more effective than that provided by strangers due to the continuity and familiarity of the relationship. Conversely, constant stimulation from unknown individuals can hinder the stimulation process [12].
According to research by Goldfarb et al., Zuo et al., and Mulyana et al., there are five elements of family and patient involvement. The findings indicate that family and patient involvement increases awareness and cognition in comatose patients with traumatic brain injury, improves the quality of life, enhances psychological well-being, boosts patient and family satisfaction, decreases pain intensity and anxiety, and shortens ICU length of stay [13-16].
Abbasi et al. [12], Salmani et al. [17], and Zuo et al. [14] utilizing a family-centered affective stimulation intervention in unconscious patients due to brain injury, have assessed outcome values, such as GCS and delirium. However, they have not addressed its effects on conscious patients, particularly regarding the pain and anxiety scales. Therefore, in the current study, we aimed to examine the impact of affective stimulation-based, family-centered, integrated spiritual support on chest pain and anxiety among ACS patients in the coronary intensive care unit (CICU).
Materials and Methods
Research design
This pilot study employed a quasi-experimental pre- and post-test design with a non-equivalent control group.
Sample size and setting
This research involved 30 patients diagnosed with ACS in the CICU and was conducted from June 15, 2021, to July 21, 2021. Patients were assigned to either the experimental group (n=15) or the control group (n=15) based on the inclusion criteria using a consecutive sampling technique. The inclusion criteria included patients aged over 21 years with a primary diagnosis of ACS and mild to moderate chest pain, who were alert, undergoing pharmacological therapy with or without percutaneous coronary intervention (PCI), and able to communicate. Additionally, the family inclusion criteria specified that nuclear family members should be aged between 18 and 55.
The sample size was calculated based on a comparative study of two means by Salmani et al. [17]. The researchers hypothesized that the experimental group would differ from the control group, with a minimal difference in pain scores considered significant at five. According to the literature, the combined standard deviation of the pain scale was 2.85. Considering the type I error of 5% and the type II error of 20%, the number of samples required was 11 per group. An additional 30% was added to account for potential dropout events. Thus, the total sample size for this study was 15 respondents in each group [12, 17]. Calculating using G*Power 3.1.9.7, the power was found to be 0.4. All patients who met the inclusion criteria entered the study, resulting in a dropout rate of 0%.
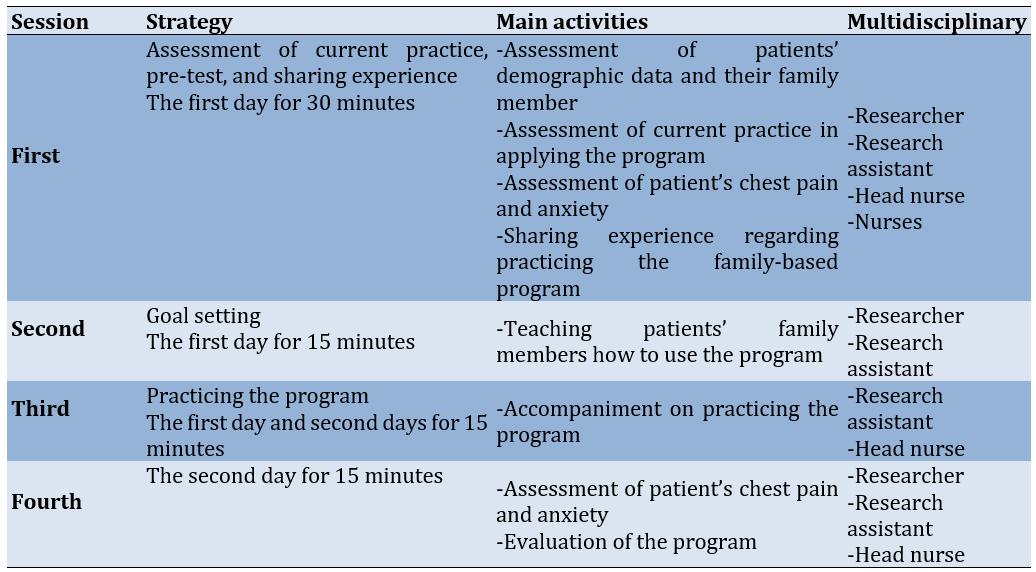
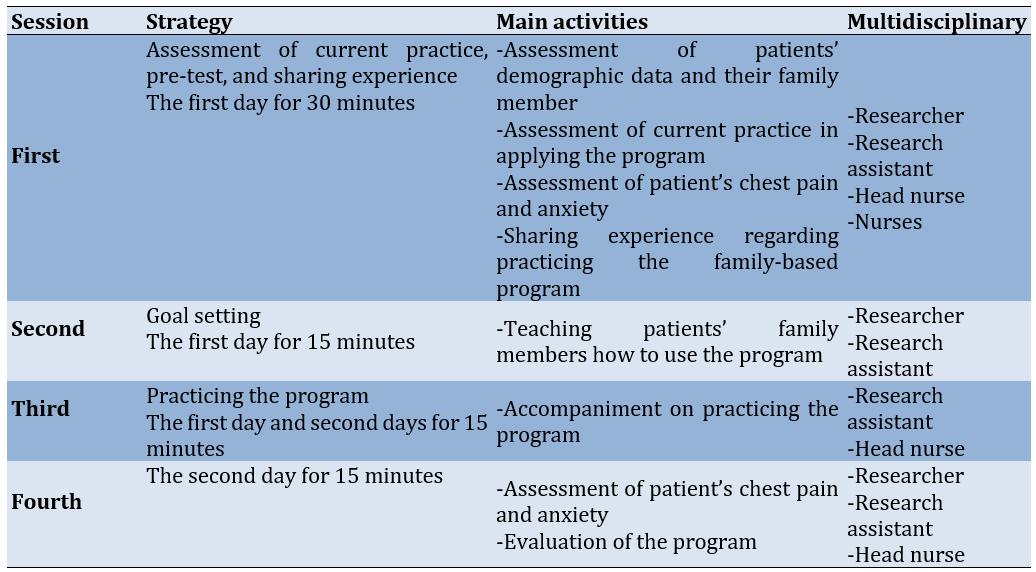
Affective Stimulation-Based Family-Centered Integrated Spiritual Support
The program was developed based on patient- and family-centered care and spiritual support models [18-20]. Patients in the experimental group received routine care in the CICU, accompanied by a four-session participatory program over two days. The program comprised an assessment of current practices, measuring the patients’ chest pain and anxiety, sharing experiences and challenges related to the family-based program, goal setting for teaching patients’ family members how to perform the program, accompaniment during the practice of the program, and measuring the patients’ chest pain and anxiety and evaluating the program. The intervention was administered by family members and was blinded to the patients and healthcare providers, including nurses in the CICU. The outcomes were measured by CICU nurses who were blinded to the intervention (Table 1).
Participants in the control group received only routine treatment according to CICU guidelines. The routine care provided by healthcare providers in the CICU included standard CICU care and standard medication for ACS patients.
Table 1. The intervention provided for the experimental group
Research tools
The information from respondents was gathered using three questionnaires, including the Socio-Demographic and Health Information (SDHI), the Numeric Pain Rating Scale (NPRS), and the Visual Analog Scale for Anxiety.
Socio-Demographic and Health Information (SDHI) Scale
This Scale was used to measure socio-demographic and health-related information. An interview questionnaire was employed to evaluate the SDHI.
Numeric Pain Rating Scale (NPRS)
The NPRS was used to assess the patient’s chest pain. It is commonly used in hospitals and has become a standard tool in clinical settings. The scale consists of a horizontal line with a starting point marked zero, indicating “no pain,” and an endpoint marked ten, indicating “worst possible pain.” Respondents were asked to rate their pain from zero to ten, selecting the number that best represented their pain intensity. Pain is typically classified as mild when it falls between one and three, moderate between four and six, and severe when it reaches even ten [21, 22].
Visual Analog Scale for Anxiety (VAS-A)
The VAS-A was used to assess a patient’s anxiety, which is frequently utilized in both clinical settings and research. This instrument was also employed to study ACS patients pre- and post-surgery. Furthermore, it did not interfere with the patient during the assessment, as the use of oxygen must be limited in ACS patients. This scale consists of a horizontal line with a starting point marked 0mm, indicating “not at all anxious,” and an endpoint marked 100mm, indicating “very anxious.” Respondents were asked to rate their anxiety from 0 to 100, selecting the point that best represented their feelings [23, 24].
Statistical analysis
We used the normality test based on the Shapiro-Wilk method, while the homogeneity test employed the chi-square and Levene tests. Data for categorical descriptions were presented using frequency and percentage, while numerical data were reported using the mean and standard deviation. Since the data were normally distributed (p>0.05) and homogeneous (p>0.5), the subsequent analyses for this research included a paired t-test, an independent t-test, and Cohen’s d. The analysis then proceeded using an analysis of covariance. The data were analyzed using the intention to treat (ITT) method with SPSS 23.
Findings
Socio-demographic and health-related information
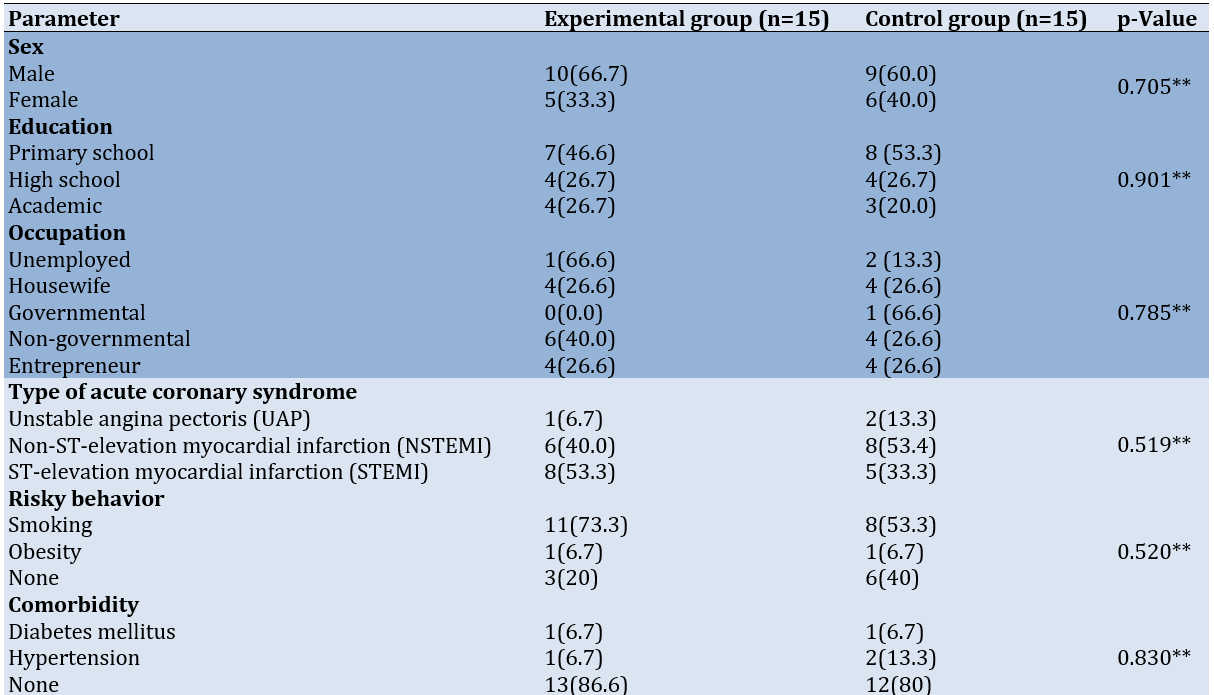
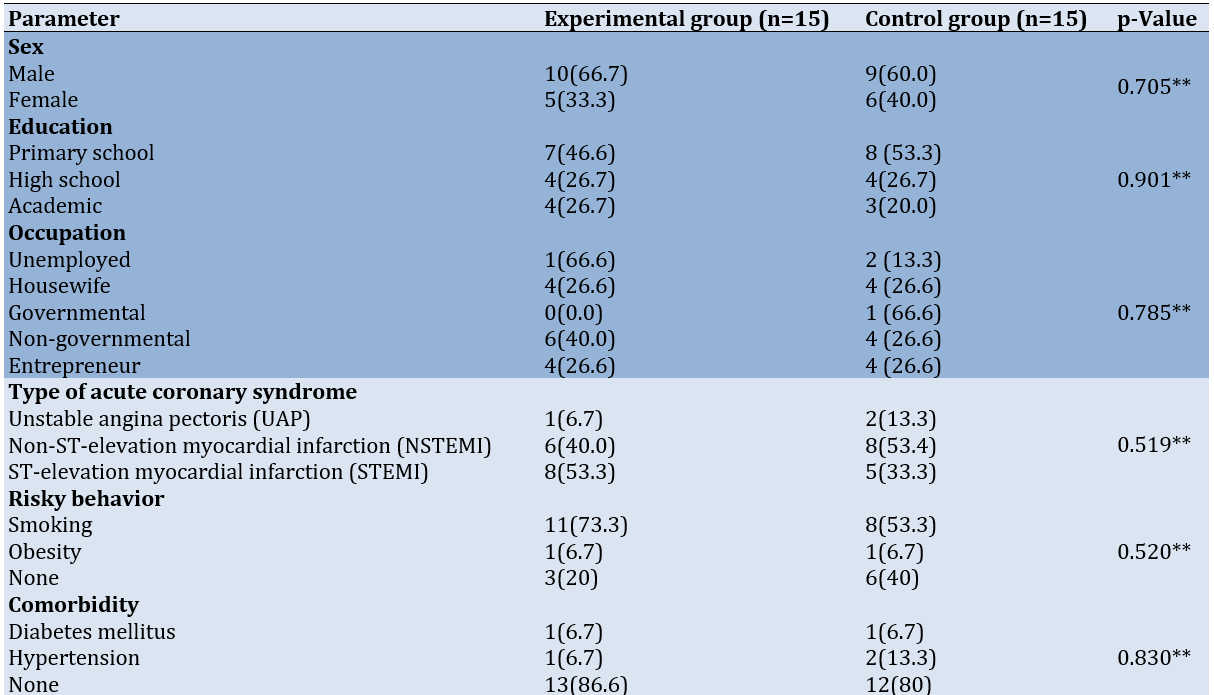
With an average age of 53.74±6.07 years in the experimental group and 56.73±9.49 years in the control group, male participants comprised the largest percentage of the experimental group (66.7%) and the control group (60.0%). In the control group, 53.3% of participants had completed primary school, while 46.6% in the experimental group had the same educational level. Some participants in the experimental group (40.0%) and the control group (26.6%) were employed as private employees. These results also indicate that the data variation between the experimental and control groups is homogeneous (p<0.05).
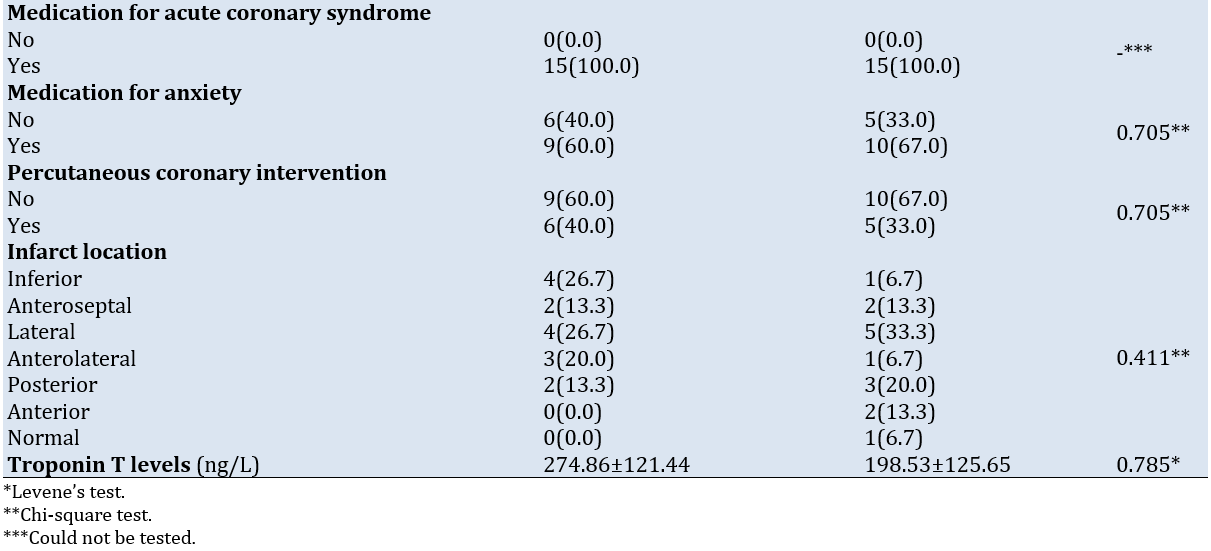
Health-related information indicated that more than half of the participants were diagnosed with STEMI (53.3%) in the experimental group and non-ST-elevation myocardial infarction (NSTEMI) (53.4%) in the control group. Most participants in the experimental group (73.3%) and the control group (53.3%) had a smoking history, with no comorbid diseases (experimental and control groups=86.6% vs. 80.0%, respectively). All participants received standard ACS medications (100%), while only 60.0% in the experimental group and 67.0% in the control group received usual anxiety medications. The average troponin T levels were 274.86±121.44ng/L in the experimental group and 198.53±125.65ng/L in the control group, with infarct locations most commonly occurring in the inferior, lateral, and superior regions of the heart (Table 2).
Table 2. Sociodemographic characteristics and health-related information (n=30)
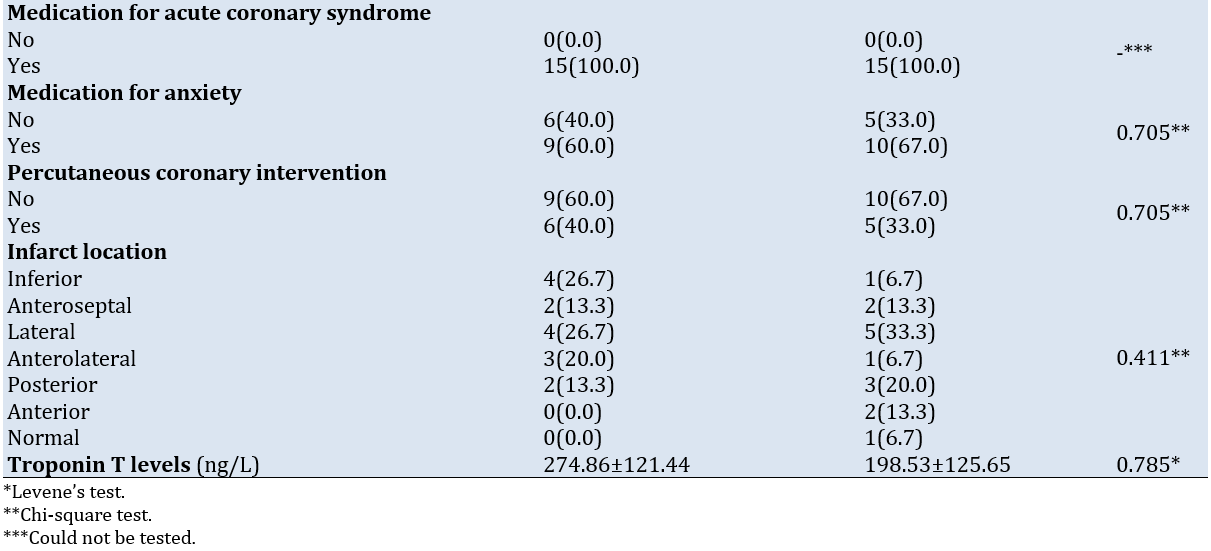
Comparison of the mean scores of pain and anxiety within the groups
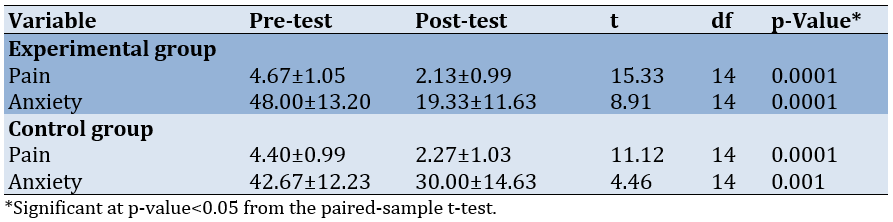
The mean score of pain (p<0.05) and anxiety (p<0.05) decreased significantly in both the experimental and control groups. The most significant reductions in pain and anxiety scores were observed in the experimental group (Table 3).
Table 3. Mean scores of pain and anxiety within the groups
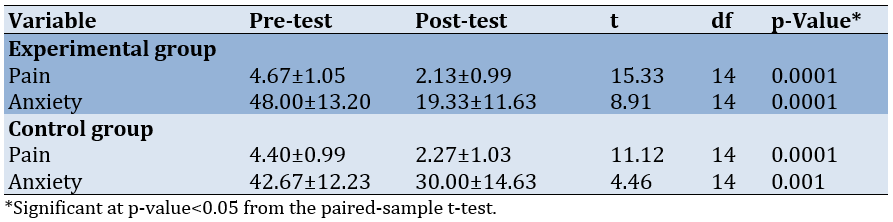
Comparison of Mean Scores on Pain and Anxiety Between the Groups
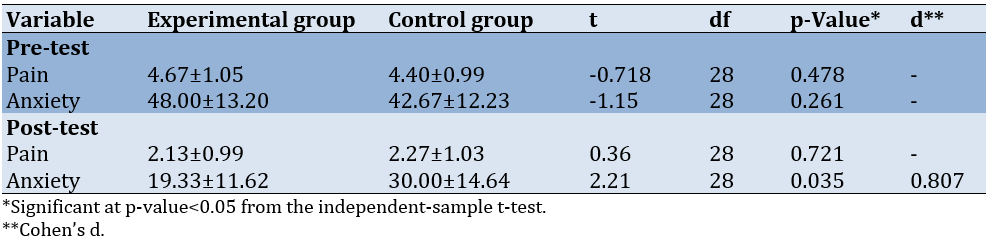
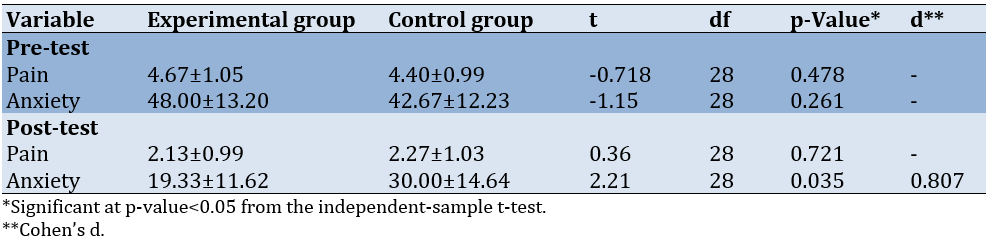
There was no discernible difference in pain scores between the experimental and control groups (p-value=0.721). In contrast, a significant difference was observed in anxiety scores between the experimental and control groups (p-value=0.035; effect size=0.807; Table 4).
Table 4. Means scores of pain and anxiety between the groups
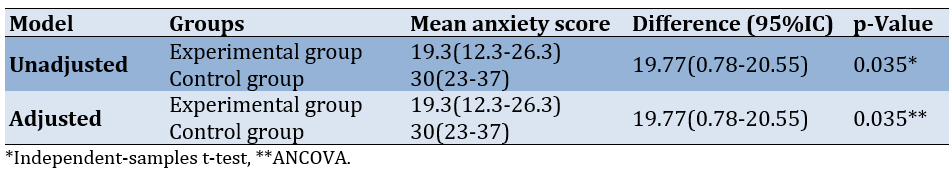
Effect of the intervention on mean anxiety scores of patients
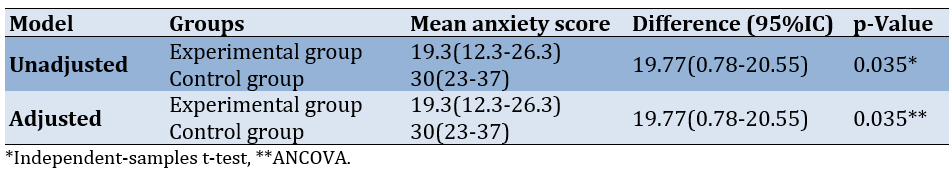
After controlling for pharmacological therapy for anxiety as a confounding variable, the average unadjusted and adjusted anxiety score in the experimental group was 19.3±11.62, while in the control group, it was 30±14.64. There was no difference in anxiety scores before and after controlling for pharmacological therapy for anxiety (Table 5).
Table 5. Effect of the intervention on the mean patients’ anxiety score
Discussion
This study examined the impact of affective stimulation-based, family-centered, integrated spiritual support on chest pain and anxiety among ACS patients in the CICU. The findings showed that men were more likely to have ACS. A previous study also indicated that males are at an increased risk of ACS due to having lower levels of the hormone estrogen compared to females. Estrogen helps maintain the elasticity of blood vessels; smoking habits and stress, which are more prevalent in males, further increase the risk of ACS [25-28].
Most of our ACS patients were elderly. ACS tends to be more common among older individuals [25, 29-31]. Age is a significant risk factor for ACS; as a person ages, the elasticity of blood vessels changes, ultimately affecting heart function. Additionally, the formation of atherosclerosis increases fivefold between the ages of 40 and 60 [32]. Furthermore, Overbaugh stated that as a person ages, the risk of experiencing disorders of vital organs, such as the cardiovascular, respiratory, and neurological systems, also rises [33].
Most patients were diagnosed with NSTEMI and STEMI, presenting with high troponin T levels and a history of smoking. Previous studies also have reported the majority of respondents being diagnosed with STEMI with a history of hypertension and smoking, both in the past and prior to hospital admission [29, 30, 34]. This finding is supported by research from Trisnaamijaya et al., indicating a relationship between smoking behavior and the incidence of ACS [35]. Sagala et al. also noted that patients with NSTEMI and STEMI can exhibit troponin T levels ranging from 100 to 2000ng/L, with the most common locations of infarction being anterolateral [36].
Patients with unstable angina pectoris (UAP) tend to ignore the pain they experience, as the blockage in the arteries has not yet occurred, leading to a decrease in pain when the condition stabilizes. This factor may cause patients not to seek care at health facilities. In contrast, patients with NSTEMI and STEMI experience ischemia and necrosis due to plaque erosion and rupture, resulting in persistent pain even at rest. This factor prompts patients to visit health facilities. Additionally, patients with a history of smoking have a greater risk of developing ACS. Exposure to toxic substances (free radicals) in cigarettes adheres to blood vessels, ultimately damaging the endothelium and reducing the elasticity of blood vessels [7, 25].
Troponin T is one of the protein components in the heart muscle that plays an essential role in muscle contraction. In patients with ACS, damage to heart muscle cells occurs due to a lack of blood flow and oxygen to the heart. This condition results in the lysis or rupture of heart muscle cells, which causes the release of troponin T into the bloodstream. Elevated levels of troponin T in the blood are often used as sensitive and specific biomarkers to detect heart muscle damage [37].
This study found a significantly lower pain and anxiety score in the experimental group. However, the difference appears to have little to no clinical implications for the patient’s pain but does have clinical implications for the patient’s anxiety.
Intensive care presents high stressors, particularly for those with ACS [38]. In addition to chest pain, patients experience other issues, such as weakness, immobilization, muscle stiffness, hopelessness, fear, sadness, feelings of isolation, sleep disturbances, discomfort, and anxiety [39]. Pain and anxiety are exacerbated by invasive procedures, separation from family, dependence on mechanical ventilation, and a new critical care team [3-5]. Furthermore, anxiety can be intensified by national regulations that prohibited family visits during the COVID-19 pandemic, contributing to patients’ feelings of loneliness and isolation.
In addition to the physical and psychological impact on critically ill patients with ACS, family members often find themselves in confusing environments and experience emotional distress, including anxiety, depression, and feelings of helplessness. This emotional distress arises because family members are anxious about seeing the patient in bed and desire to be close to the patient to provide support [40, 41].
Pain and anxiety are subjective responses experienced by the patient, emphasizing that only the patient can truly feel these sensations. According to Gaol, stress results from an imbalance between physical and psychological demands and the ability to respond. There is a simple model, in which the stress process consists of four interrelated stages: environmental need, perception, response, and behavioral consequences. According to Gaol, interventions should focus on the second stage of the stress process to prevent stress, specifically addressing individual perceptions of environmental demands. Positive perceptions of environmental needs should be fostered to prevent the occurrence of stress [11, 42].
Affective stimulation-based, family-centered, integrated spiritual support is an intervention that family members provide to patients. It is based on two main aspects of sensory and affective, which are repeated to encourage, motivate, and instill enthusiasm, ultimately changing the patient’s perception of pain and anxiety. The use of specific words or sentences that are read repeatedly, incorporating elements of faith and belief, elicits a stronger relaxation response than relaxation techniques that focus solely on belief [11, 12, 14, 17].
The patient’s beliefs hold calming significance, as spirituality is one of the individual coping resources that patients can utilize to adapt to the stressors they face [43]. Therefore, to achieve optimal results, the affective aspect must include spiritual support [44]. Willemse et al. clarify that spirituality encompasses relationships with others, including family members. It is defined as social support, which refers to an individual’s perception of being loved, cared for, valued, and recognized as part of a social network. Furthermore, their research explains that social support positively influences a person’s physical and mental health. Love and attention from family members and others around participants make them feel more meaningful and valued. Feeling valued serves as a significant source of internal strength for ACS patients. Social support is one of the most effective forms of coping [45].
The crucial aspect is the potential variations in responses to stimuli from known and unknown individuals. In other words, patients may react to sensory and affective stimulation from people they know differently than from those they do not know. The patient’s family—those they are most familiar with—should provide sensory and affective stimulation for more meaningful outcomes. Kydonaki et al. state that the patient’s family is the closest relative with whom they share an emotional connection and maintain constant contact regarding their normal status [46]. However, prolonged exposure to sensory and affective stimulation from unfamiliar individuals can eventually lead to stimulation inhibition [17].
The theoretical and physiological distinction between family-centered and sensory-centered affective stimulation is based on psychological, cognitive, and motivational factors. These aspects can accelerate the healing process by stimulating the parasympathetic nervous system and inhibiting sympathetic nerves, which in turn suppresses the hypothalamic-pituitary axis (HPA) process and the renin-aldosterone-angiotensinogen system (RAAS) process, ultimately reducing pain and anxiety. Simultaneously, the body secretes endorphins that enhance interest, motivation, and pleasure, thereby reducing pain and stress while decreasing metabolism and oxygen consumption [7, 17, 47].
The family plays a vital role in the healing of patients. There are five family duties in the health sector, including recognizing health development disorders, making decisions to take appropriate action, providing care to sick family members, maintaining a favorable atmosphere for health, and sustaining social relations between the family and existing health institutions. According to Kiwanuka et al., patients positively perceive that they are cared for, not left behind in their critical state, and feel calm and comfortable. The influence of family members is that they feel like individuals who benefit their loved ones. Most importantly, the inner and social bonds between patients and family members are maintained even in the worst conditions [48].
Information is one of the primary needs assessed by family members. Doctors and nurses should inform patients about their illnesses, the treatments received, tests performed, required medical care, and the actions of family members to aid in the patient’s recovery. This is done to alleviate psychological pressure, facilitate decision-making regarding the patient, and support their needs [49, 50].
The foremost need of critically ill ACS patients is the emotional need to be close to their family members [17]. The American College of Critical Care Medicine strongly advises using a shared decision-making paradigm when communicating with families to achieve patient and family goals [51]. Over the past decade, academies and hospitals have increasingly gravitated toward family-centered interventions and programs in the nursing process to support interaction and bonding between patients and family members, ultimately improving care outcomes [12, 52, 53]. This approach is supported by Florence Nightingale’s nursing theory, which emphasizes the significant influence of visitors, family, and friends on the critically ill. To view critical nursing practice holistically, nurses must consider the patient’s family [5].
Many non-pharmacological interventions are used to reduce patient pain and anxiety, such as cognitive behavioral therapy (CBT), mindfulness and relaxation techniques, and standard family support programs. CBT is a well-established non-pharmacological approach for managing anxiety, focusing on changing thought patterns to influence behavior and emotional states [54]. Our intervention differs by incorporating spiritual support and family involvement, which can enhance emotional support and provide comfort through familiar and culturally relevant practices.
Mindfulness and relaxation techniques, such as meditation, guided imagery, and progressive muscle relaxation, are commonly used to reduce pain and anxiety. These approaches are effective in promoting relaxation but may require significant patient engagement and adherence [55]. Our family-centered approach leverages the existing support system, which may enhance compliance and effectiveness, especially in a hospital setting.
Traditional family support programs typically involve emotional and practical support from family members without a structured framework [48, 52]. Our intervention formalizes this support with specific strategies and integrates spiritual elements, which can be particularly meaningful for patients from specific cultural or religious backgrounds.
This study had limitations. Sensory stimulation was not provided in the same form to all patients. Depending on family culture, families were allowed to hold hands, gaze, hug, kiss the forehead, rub the back, or rub the head. Also, only one family member was permitted to wait for the patient in the family waiting room, which meant that the patient could not choose which family members might visit them based on their comfort. This limitation could affect the stimulation provided by family members to the patient. In addition, the frequency of patients admitted to the ICCU was not assessed, whether the patient was admitted to the ICCU for the first time or had been repeatedly admitted. This could influence the patient’s response to the pain experienced. Lastly, the presence of any accompanying diseases with ACS was not evaluated, which could impact the patient’s coping mechanisms in dealing with pain.
Conclusion
Routine care combined with affective stimulation-based family-centered integrated spiritual support results in a better average pain and anxiety score.
Acknowledgments: The authors thank the Institute for Research and Community Services at Esa Unggul University, Padjadjaran University, Wishan Global Medika, and Tarakan Hospital.
Ethical Permissions: The ethical considerations in this study focused on the safety of patients, families, and researchers. This research was conducted during the COVID-19 pandemic in DKI Jakarta. Procedures were implemented to prevent transmission during the research process, including conducting rapid antigen tests each time a family visited the patient and when the researcher interacted with the patient and family. This research was approved by the Ethics Committees of Padjadjaran University (577/UN6.KEP/EC/2021) and Tarakan Hospital (020/KEPK/RSUDT/2021). Informed consent was obtained from each participant willing to take part in the study.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors’ Contribution: Mulyana B (First Author), Introduction Writer/Methodologist/Main Researcher (20%); Trisyani Y (Second Author), Methodologist/Main Researcher (15%); Nuraeni A (Third Author), Assistant Researcher/Statistical Analyst (15%); Astrada A (Fourth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Pamungkas RA (Fifth Author), Assistant Researcher/Discussion Writer (15%); Ekawaty D (Sixth Author), Assistant Researcher (10%); Wariani W (Seventh Author), Assistant Researcher (10%)
Funding/Support: This research received a specific grant from the Institute for Research and Community Services at Esa Unggul University.
Approximately 422.7 million cases of acute coronary syndrome (ACS) are reported globally, and 17.92 million deaths from ACS are projected to increase to 23.3 million by 2030 [1].
The effects of critical patients with ACS can be categorized into two types, including immediate effects, such as chest pain [2], and indirect effects, which include physical issues (weakness, immobility, muscle stiffness, and pain) as well as psychological issues (pain, hopelessness, fear, grief, feelings of isolation, disturbed sleep, discomfort, and anxiety) resulting from the critical care services required for ACS patients. Furthermore, pain and anxiety are intensified by invasive procedures, separation from family, and the introduction of a new critical care team [3-5].
Anxiety and pain are psychological issues that are among the most common and detrimental to heart health [6]. Persistent pain and anxiety experienced by patients can impede the healing process and survival in conditions such as infarction, endothelial dysfunction, myocardial ischemia, plaque rupture, thrombosis, and malignant arrhythmias. Additionally, a decrease in bodily resistance can occur in patients, increasing the risk of death due to hormonal imbalances caused by stress, including elevated levels of cortisol, thyroid hormones, and sympathetic nerve activity, which in turn raises the body’s metabolism. Uncontrolled metabolism due to pain and anxiety can further hinder the healing process. Moreover, in patients with ACS, oxygen consumption must be carefully regulated, as the oxygen supply to the heart is limited, which inhibits the heart’s ability to pump blood effectively without adequate oxygen [7].
Pharmacological therapies can alleviate or eliminate pain and anxiety in individuals with ACS. However, these therapies may not always provide optimal pain relief, and it is impossible to separate the development of side effects from ongoing pharmacological use. Therefore, non-pharmacological therapy (as an additional treatment) is necessary to reduce or eliminate pain [8]. Non-pharmacological treatments for pain and anxiety can include relaxation techniques, hypnotherapy, music therapy, massage, dhikr, and family-based interventions [9-11].
Since pain and anxiety are subjective responses of patients, the interventions should focus on changing the patient’s emotional response to these feelings. Family-centered affective stimulation is an intervention carried out by family members on patients, based on two main aspects: sensory and affective. This intervention is conducted repeatedly to provide encouragement, motivation, and enthusiasm to patients, helping them change their perception of the pain and anxiety they experience. The repetition of certain words or phrases that incorporate elements of faith and belief can elicit a stronger relaxation response than relaxation techniques that lack these elements. The patient’s spiritual beliefs hold a calming significance, as they serve as a source of individual coping that aids the patient in adapting to the stressors they encounter [12].
The difference in the effects of stimulation provided by familiar versus unfamiliar individuals is significant. Patients may receive and respond to sensory and affective stimuli differently depending on whether the stimulation comes from someone they know or not. Sensory and affective stimulation provided by family members is considered more effective than that provided by strangers due to the continuity and familiarity of the relationship. Conversely, constant stimulation from unknown individuals can hinder the stimulation process [12].
According to research by Goldfarb et al., Zuo et al., and Mulyana et al., there are five elements of family and patient involvement. The findings indicate that family and patient involvement increases awareness and cognition in comatose patients with traumatic brain injury, improves the quality of life, enhances psychological well-being, boosts patient and family satisfaction, decreases pain intensity and anxiety, and shortens ICU length of stay [13-16].
Abbasi et al. [12], Salmani et al. [17], and Zuo et al. [14] utilizing a family-centered affective stimulation intervention in unconscious patients due to brain injury, have assessed outcome values, such as GCS and delirium. However, they have not addressed its effects on conscious patients, particularly regarding the pain and anxiety scales. Therefore, in the current study, we aimed to examine the impact of affective stimulation-based, family-centered, integrated spiritual support on chest pain and anxiety among ACS patients in the coronary intensive care unit (CICU).
Materials and Methods
Research design
This pilot study employed a quasi-experimental pre- and post-test design with a non-equivalent control group.
Sample size and setting
This research involved 30 patients diagnosed with ACS in the CICU and was conducted from June 15, 2021, to July 21, 2021. Patients were assigned to either the experimental group (n=15) or the control group (n=15) based on the inclusion criteria using a consecutive sampling technique. The inclusion criteria included patients aged over 21 years with a primary diagnosis of ACS and mild to moderate chest pain, who were alert, undergoing pharmacological therapy with or without percutaneous coronary intervention (PCI), and able to communicate. Additionally, the family inclusion criteria specified that nuclear family members should be aged between 18 and 55.
The sample size was calculated based on a comparative study of two means by Salmani et al. [17]. The researchers hypothesized that the experimental group would differ from the control group, with a minimal difference in pain scores considered significant at five. According to the literature, the combined standard deviation of the pain scale was 2.85. Considering the type I error of 5% and the type II error of 20%, the number of samples required was 11 per group. An additional 30% was added to account for potential dropout events. Thus, the total sample size for this study was 15 respondents in each group [12, 17]. Calculating using G*Power 3.1.9.7, the power was found to be 0.4. All patients who met the inclusion criteria entered the study, resulting in a dropout rate of 0%.
Affective Stimulation-Based Family-Centered Integrated Spiritual Support
The program was developed based on patient- and family-centered care and spiritual support models [18-20]. Patients in the experimental group received routine care in the CICU, accompanied by a four-session participatory program over two days. The program comprised an assessment of current practices, measuring the patients’ chest pain and anxiety, sharing experiences and challenges related to the family-based program, goal setting for teaching patients’ family members how to perform the program, accompaniment during the practice of the program, and measuring the patients’ chest pain and anxiety and evaluating the program. The intervention was administered by family members and was blinded to the patients and healthcare providers, including nurses in the CICU. The outcomes were measured by CICU nurses who were blinded to the intervention (Table 1).
Participants in the control group received only routine treatment according to CICU guidelines. The routine care provided by healthcare providers in the CICU included standard CICU care and standard medication for ACS patients.
Table 1. The intervention provided for the experimental group
Research tools
The information from respondents was gathered using three questionnaires, including the Socio-Demographic and Health Information (SDHI), the Numeric Pain Rating Scale (NPRS), and the Visual Analog Scale for Anxiety.
Socio-Demographic and Health Information (SDHI) Scale
This Scale was used to measure socio-demographic and health-related information. An interview questionnaire was employed to evaluate the SDHI.
Numeric Pain Rating Scale (NPRS)
The NPRS was used to assess the patient’s chest pain. It is commonly used in hospitals and has become a standard tool in clinical settings. The scale consists of a horizontal line with a starting point marked zero, indicating “no pain,” and an endpoint marked ten, indicating “worst possible pain.” Respondents were asked to rate their pain from zero to ten, selecting the number that best represented their pain intensity. Pain is typically classified as mild when it falls between one and three, moderate between four and six, and severe when it reaches even ten [21, 22].
Visual Analog Scale for Anxiety (VAS-A)
The VAS-A was used to assess a patient’s anxiety, which is frequently utilized in both clinical settings and research. This instrument was also employed to study ACS patients pre- and post-surgery. Furthermore, it did not interfere with the patient during the assessment, as the use of oxygen must be limited in ACS patients. This scale consists of a horizontal line with a starting point marked 0mm, indicating “not at all anxious,” and an endpoint marked 100mm, indicating “very anxious.” Respondents were asked to rate their anxiety from 0 to 100, selecting the point that best represented their feelings [23, 24].
Statistical analysis
We used the normality test based on the Shapiro-Wilk method, while the homogeneity test employed the chi-square and Levene tests. Data for categorical descriptions were presented using frequency and percentage, while numerical data were reported using the mean and standard deviation. Since the data were normally distributed (p>0.05) and homogeneous (p>0.5), the subsequent analyses for this research included a paired t-test, an independent t-test, and Cohen’s d. The analysis then proceeded using an analysis of covariance. The data were analyzed using the intention to treat (ITT) method with SPSS 23.
Findings
Socio-demographic and health-related information
With an average age of 53.74±6.07 years in the experimental group and 56.73±9.49 years in the control group, male participants comprised the largest percentage of the experimental group (66.7%) and the control group (60.0%). In the control group, 53.3% of participants had completed primary school, while 46.6% in the experimental group had the same educational level. Some participants in the experimental group (40.0%) and the control group (26.6%) were employed as private employees. These results also indicate that the data variation between the experimental and control groups is homogeneous (p<0.05).
Health-related information indicated that more than half of the participants were diagnosed with STEMI (53.3%) in the experimental group and non-ST-elevation myocardial infarction (NSTEMI) (53.4%) in the control group. Most participants in the experimental group (73.3%) and the control group (53.3%) had a smoking history, with no comorbid diseases (experimental and control groups=86.6% vs. 80.0%, respectively). All participants received standard ACS medications (100%), while only 60.0% in the experimental group and 67.0% in the control group received usual anxiety medications. The average troponin T levels were 274.86±121.44ng/L in the experimental group and 198.53±125.65ng/L in the control group, with infarct locations most commonly occurring in the inferior, lateral, and superior regions of the heart (Table 2).
Table 2. Sociodemographic characteristics and health-related information (n=30)
Comparison of the mean scores of pain and anxiety within the groups
The mean score of pain (p<0.05) and anxiety (p<0.05) decreased significantly in both the experimental and control groups. The most significant reductions in pain and anxiety scores were observed in the experimental group (Table 3).
Table 3. Mean scores of pain and anxiety within the groups
Comparison of Mean Scores on Pain and Anxiety Between the Groups
There was no discernible difference in pain scores between the experimental and control groups (p-value=0.721). In contrast, a significant difference was observed in anxiety scores between the experimental and control groups (p-value=0.035; effect size=0.807; Table 4).
Table 4. Means scores of pain and anxiety between the groups
Effect of the intervention on mean anxiety scores of patients
After controlling for pharmacological therapy for anxiety as a confounding variable, the average unadjusted and adjusted anxiety score in the experimental group was 19.3±11.62, while in the control group, it was 30±14.64. There was no difference in anxiety scores before and after controlling for pharmacological therapy for anxiety (Table 5).
Table 5. Effect of the intervention on the mean patients’ anxiety score
Discussion
This study examined the impact of affective stimulation-based, family-centered, integrated spiritual support on chest pain and anxiety among ACS patients in the CICU. The findings showed that men were more likely to have ACS. A previous study also indicated that males are at an increased risk of ACS due to having lower levels of the hormone estrogen compared to females. Estrogen helps maintain the elasticity of blood vessels; smoking habits and stress, which are more prevalent in males, further increase the risk of ACS [25-28].
Most of our ACS patients were elderly. ACS tends to be more common among older individuals [25, 29-31]. Age is a significant risk factor for ACS; as a person ages, the elasticity of blood vessels changes, ultimately affecting heart function. Additionally, the formation of atherosclerosis increases fivefold between the ages of 40 and 60 [32]. Furthermore, Overbaugh stated that as a person ages, the risk of experiencing disorders of vital organs, such as the cardiovascular, respiratory, and neurological systems, also rises [33].
Most patients were diagnosed with NSTEMI and STEMI, presenting with high troponin T levels and a history of smoking. Previous studies also have reported the majority of respondents being diagnosed with STEMI with a history of hypertension and smoking, both in the past and prior to hospital admission [29, 30, 34]. This finding is supported by research from Trisnaamijaya et al., indicating a relationship between smoking behavior and the incidence of ACS [35]. Sagala et al. also noted that patients with NSTEMI and STEMI can exhibit troponin T levels ranging from 100 to 2000ng/L, with the most common locations of infarction being anterolateral [36].
Patients with unstable angina pectoris (UAP) tend to ignore the pain they experience, as the blockage in the arteries has not yet occurred, leading to a decrease in pain when the condition stabilizes. This factor may cause patients not to seek care at health facilities. In contrast, patients with NSTEMI and STEMI experience ischemia and necrosis due to plaque erosion and rupture, resulting in persistent pain even at rest. This factor prompts patients to visit health facilities. Additionally, patients with a history of smoking have a greater risk of developing ACS. Exposure to toxic substances (free radicals) in cigarettes adheres to blood vessels, ultimately damaging the endothelium and reducing the elasticity of blood vessels [7, 25].
Troponin T is one of the protein components in the heart muscle that plays an essential role in muscle contraction. In patients with ACS, damage to heart muscle cells occurs due to a lack of blood flow and oxygen to the heart. This condition results in the lysis or rupture of heart muscle cells, which causes the release of troponin T into the bloodstream. Elevated levels of troponin T in the blood are often used as sensitive and specific biomarkers to detect heart muscle damage [37].
This study found a significantly lower pain and anxiety score in the experimental group. However, the difference appears to have little to no clinical implications for the patient’s pain but does have clinical implications for the patient’s anxiety.
Intensive care presents high stressors, particularly for those with ACS [38]. In addition to chest pain, patients experience other issues, such as weakness, immobilization, muscle stiffness, hopelessness, fear, sadness, feelings of isolation, sleep disturbances, discomfort, and anxiety [39]. Pain and anxiety are exacerbated by invasive procedures, separation from family, dependence on mechanical ventilation, and a new critical care team [3-5]. Furthermore, anxiety can be intensified by national regulations that prohibited family visits during the COVID-19 pandemic, contributing to patients’ feelings of loneliness and isolation.
In addition to the physical and psychological impact on critically ill patients with ACS, family members often find themselves in confusing environments and experience emotional distress, including anxiety, depression, and feelings of helplessness. This emotional distress arises because family members are anxious about seeing the patient in bed and desire to be close to the patient to provide support [40, 41].
Pain and anxiety are subjective responses experienced by the patient, emphasizing that only the patient can truly feel these sensations. According to Gaol, stress results from an imbalance between physical and psychological demands and the ability to respond. There is a simple model, in which the stress process consists of four interrelated stages: environmental need, perception, response, and behavioral consequences. According to Gaol, interventions should focus on the second stage of the stress process to prevent stress, specifically addressing individual perceptions of environmental demands. Positive perceptions of environmental needs should be fostered to prevent the occurrence of stress [11, 42].
Affective stimulation-based, family-centered, integrated spiritual support is an intervention that family members provide to patients. It is based on two main aspects of sensory and affective, which are repeated to encourage, motivate, and instill enthusiasm, ultimately changing the patient’s perception of pain and anxiety. The use of specific words or sentences that are read repeatedly, incorporating elements of faith and belief, elicits a stronger relaxation response than relaxation techniques that focus solely on belief [11, 12, 14, 17].
The patient’s beliefs hold calming significance, as spirituality is one of the individual coping resources that patients can utilize to adapt to the stressors they face [43]. Therefore, to achieve optimal results, the affective aspect must include spiritual support [44]. Willemse et al. clarify that spirituality encompasses relationships with others, including family members. It is defined as social support, which refers to an individual’s perception of being loved, cared for, valued, and recognized as part of a social network. Furthermore, their research explains that social support positively influences a person’s physical and mental health. Love and attention from family members and others around participants make them feel more meaningful and valued. Feeling valued serves as a significant source of internal strength for ACS patients. Social support is one of the most effective forms of coping [45].
The crucial aspect is the potential variations in responses to stimuli from known and unknown individuals. In other words, patients may react to sensory and affective stimulation from people they know differently than from those they do not know. The patient’s family—those they are most familiar with—should provide sensory and affective stimulation for more meaningful outcomes. Kydonaki et al. state that the patient’s family is the closest relative with whom they share an emotional connection and maintain constant contact regarding their normal status [46]. However, prolonged exposure to sensory and affective stimulation from unfamiliar individuals can eventually lead to stimulation inhibition [17].
The theoretical and physiological distinction between family-centered and sensory-centered affective stimulation is based on psychological, cognitive, and motivational factors. These aspects can accelerate the healing process by stimulating the parasympathetic nervous system and inhibiting sympathetic nerves, which in turn suppresses the hypothalamic-pituitary axis (HPA) process and the renin-aldosterone-angiotensinogen system (RAAS) process, ultimately reducing pain and anxiety. Simultaneously, the body secretes endorphins that enhance interest, motivation, and pleasure, thereby reducing pain and stress while decreasing metabolism and oxygen consumption [7, 17, 47].
The family plays a vital role in the healing of patients. There are five family duties in the health sector, including recognizing health development disorders, making decisions to take appropriate action, providing care to sick family members, maintaining a favorable atmosphere for health, and sustaining social relations between the family and existing health institutions. According to Kiwanuka et al., patients positively perceive that they are cared for, not left behind in their critical state, and feel calm and comfortable. The influence of family members is that they feel like individuals who benefit their loved ones. Most importantly, the inner and social bonds between patients and family members are maintained even in the worst conditions [48].
Information is one of the primary needs assessed by family members. Doctors and nurses should inform patients about their illnesses, the treatments received, tests performed, required medical care, and the actions of family members to aid in the patient’s recovery. This is done to alleviate psychological pressure, facilitate decision-making regarding the patient, and support their needs [49, 50].
The foremost need of critically ill ACS patients is the emotional need to be close to their family members [17]. The American College of Critical Care Medicine strongly advises using a shared decision-making paradigm when communicating with families to achieve patient and family goals [51]. Over the past decade, academies and hospitals have increasingly gravitated toward family-centered interventions and programs in the nursing process to support interaction and bonding between patients and family members, ultimately improving care outcomes [12, 52, 53]. This approach is supported by Florence Nightingale’s nursing theory, which emphasizes the significant influence of visitors, family, and friends on the critically ill. To view critical nursing practice holistically, nurses must consider the patient’s family [5].
Many non-pharmacological interventions are used to reduce patient pain and anxiety, such as cognitive behavioral therapy (CBT), mindfulness and relaxation techniques, and standard family support programs. CBT is a well-established non-pharmacological approach for managing anxiety, focusing on changing thought patterns to influence behavior and emotional states [54]. Our intervention differs by incorporating spiritual support and family involvement, which can enhance emotional support and provide comfort through familiar and culturally relevant practices.
Mindfulness and relaxation techniques, such as meditation, guided imagery, and progressive muscle relaxation, are commonly used to reduce pain and anxiety. These approaches are effective in promoting relaxation but may require significant patient engagement and adherence [55]. Our family-centered approach leverages the existing support system, which may enhance compliance and effectiveness, especially in a hospital setting.
Traditional family support programs typically involve emotional and practical support from family members without a structured framework [48, 52]. Our intervention formalizes this support with specific strategies and integrates spiritual elements, which can be particularly meaningful for patients from specific cultural or religious backgrounds.
This study had limitations. Sensory stimulation was not provided in the same form to all patients. Depending on family culture, families were allowed to hold hands, gaze, hug, kiss the forehead, rub the back, or rub the head. Also, only one family member was permitted to wait for the patient in the family waiting room, which meant that the patient could not choose which family members might visit them based on their comfort. This limitation could affect the stimulation provided by family members to the patient. In addition, the frequency of patients admitted to the ICCU was not assessed, whether the patient was admitted to the ICCU for the first time or had been repeatedly admitted. This could influence the patient’s response to the pain experienced. Lastly, the presence of any accompanying diseases with ACS was not evaluated, which could impact the patient’s coping mechanisms in dealing with pain.
Conclusion
Routine care combined with affective stimulation-based family-centered integrated spiritual support results in a better average pain and anxiety score.
Acknowledgments: The authors thank the Institute for Research and Community Services at Esa Unggul University, Padjadjaran University, Wishan Global Medika, and Tarakan Hospital.
Ethical Permissions: The ethical considerations in this study focused on the safety of patients, families, and researchers. This research was conducted during the COVID-19 pandemic in DKI Jakarta. Procedures were implemented to prevent transmission during the research process, including conducting rapid antigen tests each time a family visited the patient and when the researcher interacted with the patient and family. This research was approved by the Ethics Committees of Padjadjaran University (577/UN6.KEP/EC/2021) and Tarakan Hospital (020/KEPK/RSUDT/2021). Informed consent was obtained from each participant willing to take part in the study.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors’ Contribution: Mulyana B (First Author), Introduction Writer/Methodologist/Main Researcher (20%); Trisyani Y (Second Author), Methodologist/Main Researcher (15%); Nuraeni A (Third Author), Assistant Researcher/Statistical Analyst (15%); Astrada A (Fourth Author), Assistant Researcher/Discussion Writer/Statistical Analyst (15%); Pamungkas RA (Fifth Author), Assistant Researcher/Discussion Writer (15%); Ekawaty D (Sixth Author), Assistant Researcher (10%); Wariani W (Seventh Author), Assistant Researcher (10%)
Funding/Support: This research received a specific grant from the Institute for Research and Community Services at Esa Unggul University.
Article Type: Original Research |
Subject:
Health Care
Received: 2024/03/5 | Accepted: 2024/05/29 | Published: 2024/06/30
Received: 2024/03/5 | Accepted: 2024/05/29 | Published: 2024/06/30
References
1. Pangestika DD, Trisyani Y, Nur'aeni A. The effect of dhikr therapy on the cardiac chest pain of acute coronary syndrome (ACS) patients. Nurse Media J Nurs. 2020;10(2):200-10. [Link] [DOI:10.14710/nmjn.v10i2.25638]
2. Bjørnnes AK, Rustøen T, Lie I, Watt-Watson J, Leegaard M. Pain characteristics and analgesic intake before and following cardiac surgery. Eur J Cardiovasc Nurs. 2016;15(1):47-54. [Link] [DOI:10.1177/1474515114550441]
3. Gonzalez-Martin S, Becerro-de-Bengoa-Vallejo R, Angulo-Carrere MT, Iglesias ME, Martinez-Jimenez EM, Casado-Hernandez I, et al. Effects of a visit prior to hospital admission on anxiety, depression and satisfaction of patients in an intensive care unit. Intensive Crit Care Nurs. 2019;54:46-53. [Link] [DOI:10.1016/j.iccn.2019.07.001]
4. Xiao Y, Li W, Zhou J, Zheng J, Cai X, Guo M, et al. Impact of depression and/or anxiety on patients with percutaneous coronary interventions after acute coronary syndrome: A protocol for a real-world prospective cohort study. BMJ Open. 2019;9(9):e027964. [Link] [DOI:10.1136/bmjopen-2018-027964]
5. Morton PG, Fontaine D, Hudak CM, Gallo BM. Critical care nursing: A holistic approach. 8th ed. Jakarta: EGC; 2013. [Link]
6. Iles-Smith H, McGowan L, Campbell M, Mercer C, Deaton C. A prospective cohort study investigating readmission, symptom attribution and psychological health within six months of primary percutaneous coronary intervention. Eur J Cardiovasc Nurs. 2015;14(6):506-15. [Link] [DOI:10.1177/1474515114543227]
7. Black JM, Hawks JH. Medical surgical nursing: Clinical management for positive outcomes. Singapure: Elsevier; 2009. [Link]
8. Sağlık DS, Çağlar S. The effect of parental presence on pain and anxiety levels during invasive procedures in the pediatric emergency department. J Emerg Nurs. 2019;45(3):278-85. [Link] [DOI:10.1016/j.jen.2018.07.003]
9. Farquhar JM, Stonerock GL, Blumenthal JA. Treatment of anxiety in patients with coronary heart disease: A systematic review. Psychosomatics. 2018;59(4):318-32. [Link] [DOI:10.1016/j.psym.2018.03.008]
10. Agrawal H, Aggarwal K, Littrell R, Velagapudi P, Turagam MK, Mittal M, et al. Pharmacological and non pharmacological strategies in the management of coronary artery disease and chronic kidney disease. Curr Cardiol Rev. 2015;11(3):261-9. [Link] [DOI:10.2174/1573403X1103150514155757]
11. Sahrayi Zarghi S, Najafi Ghezeljeh T, Rasouli M. The effect of aromatherapy and the benson relaxation technique on the anxiety of patients with acute coronary syndrome: Randomized controlled trial. J Client Cent Nurs Care. 2020;6(2):109-16. [Link] [DOI:10.32598/JCCNC.6.2.34.2]
12. Abbasi M, Mohammadi E, Sheaykh Rezayi A. Effect of a regular family visiting program as an affective, auditory, and tactile stimulation on the consciousness level of comatose patients with a head injury. Jpn J Nurs Sci. 2009;6(1):21-6. [Link] [DOI:10.1111/j.1742-7924.2009.00117.x]
13. Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: A systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-61. [Link] [DOI:10.1097/CCM.0000000000002624]
14. Zuo J, Tao Y, Liu M, Feng L, Yang Y, Liao L. The effect of family-centered sensory and affective stimulation on comatose patients with traumatic brain injury: A systematic review and meta-analysis. Int J Nurs Stud. 2021;115:103846. [Link] [DOI:10.1016/j.ijnurstu.2020.103846]
15. Ding X, Zhu L, Zhang R, Wang L, Wang TT, Latour JM. Effects of family-centred care interventions on preterm infants and parents in neonatal intensive care units: A systematic review and meta-analysis of randomised controlled trials. Aust Crit Care. 2019;32(1):63-75. [Link] [DOI:10.1016/j.aucc.2018.10.007]
16. Mulyana B, Yanny Trisyani W, Nur'aeni A, Pamungkas RA. A systematic review of family-centered intervention among critical ill patients. Indones J Nurs Health Sci. 2021;6(2):133-57. [Link]
17. Salmani F, Mohammadi E, Rezvani M, Kazemnezhad A. The effects of family-centered affective stimulation on brain-injured comatose patients' level of consciousness: A randomized controlled trial. Int J Nurs Stud. 2017;74:44-52. [Link] [DOI:10.1016/j.ijnurstu.2017.05.014]
18. ipfcc.org [Internet]. Virginia: Institute for Patient- and Family-Centered Care: Transforming Health Care Through Partnerships; 2024 [cited 2024, January, 04]. Available from: https://ipfcc.org/. [Link]
19. aacn.org [Internet]. Aliso Viejo: American Association of Critical-Care Nurses; c1996-2024 [cited 2024, January, 04]. Available from: https://www.aacn.org/. [Link]
20. sdicompanions.org [Internet]. Seattle: Spiritual Directors International; c2024 [cited 2024, January, 04]. Available from: https://www.sdicompanions.org/. [Link]
21. Baarslag MA, Jhingoer S, Ista E, Allegaert K, Tibboel D, Van Dijk M. How often do we perform painful and stressful procedures in the paediatric intensive care unit? A prospective observational study. Aust Crit Care. 2019;32(1):4-10. [Link] [DOI:10.1016/j.aucc.2018.04.003]
22. Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, et al. Results of a double-blind, randomized, placebo-controlled study of nabiximols oromucosal spray as an adjunctive therapy in advanced cancer patients with chronic uncontrolled pain. J Pain Symptom Manag. 2018;55(2):179-88. [Link] [DOI:10.1016/j.jpainsymman.2017.09.001]
23. Wu SI, Wu CC, Tsai PJ, Cheng LH, Hsu CC, Shan IK, et al. Psychobiotic supplementation of PS128TM improves stress, anxiety, and insomnia in highly stressed information technology specialists: A pilot study. Front Nutr. 2021;8:614105. [Link] [DOI:10.3389/fnut.2021.614105]
24. Utli H, Vural Doğru B. The effect of the COVID-19 pandemic on self-management in patients with type 2 diabetics. Prim Care Diabetes. 2021;15(5):799-805. [Link] [DOI:10.1016/j.pcd.2021.07.009]
25. Indonesian Heart Association. Guidelines for the management of acute coronary syndrome. Jakarta: Indonesian Heart Association; 2015. [Indonesian] [Link]
26. Juzar DA, Muzakkir AF, Ilhami YR, Taufiq N, Astiawati T, Junior RA IM, et al. Management of acute coronary syndrome Indonesia: Insight from one ACS multicenter registry. Indones J Cardiol. 2022;43(2):45-55. [Link] [DOI:10.30701/ijc.1406]
27. Khesroh AA, Al-Roumi F, Al-Zakwani I, Attur S, Rashed W, Zubaid M. Gender differences among patients with acute coronary syndrome in the middle east. Heart Views. 2017;18(3):77-82. [Link] [DOI:10.4103/HEARTVIEWS.HEARTVIEWS_10_17]
28. Sapriyanti, Natasha D, Gayatri D. Spiritual well-being and quality of life of coronary heart disease patients in hospitals. Jurnal Penelitian Kesehatan Suara Forikes. 2021;12(3):78-82. [Indonesian] [Link]
29. Diputra MDR, Wita IW, Aryadana W. Characteristics of acute coronary syndrome patients at sanglah hospital denpasar, 2016. E-Jurnal Medika. 2018;7(10). [Indonesian] [Link]
30. Muhibbah M, Wahid A, Agustina R, Iilliandri O. Characteristics of acute coronary syndrome patients in tulip room inpatients at ulin regional hospital, Banjarmasin. Indones J Health Sci. 2019;3(1):6-12. [Indonesian] [Link] [DOI:10.24269/ijhs.v3i1.1567]
31. Suling FRW, Patricia MI, Suling TE. Prevalence and risk factors of acute coronary syndrome at the Indonesian Christian university general hospital. Med J Christ Univ Indones. 2018;34(3):110-4. [Indonesian] [Link]
32. Al-Saif SM, Alhabib KF, Ullah A, Hersi A, Alfaleh H, Alnemer K, et al. Age and its relationship to acute coronary syndromes in the Saudi Project for Assessment of Coronary Events (SPACE) registry: The SPACE age study. J Saudi Heart Assoc. 2012;24(1):9-16. [Link] [DOI:10.1016/j.jsha.2011.08.001]
33. Overbaugh KJ. Acute coronary syndrome. Am J Nurs. 2009;109(5):42-52. [Link] [DOI:10.1097/01.NAJ.0000351508.39509.e2]
34. Jatiman T, Wibisono S, Lefi A. Clinical description of acute coronary syndrome based on blood sugar status at RSUD Dr. Soetomoe Surabaya. Surabaya: Faculty of Medicine Airlangga University; 2013. [Indonesian] [Link]
35. Trisnaamijaya D, Pangemanan J, Mandang V. Relationship between smoking behavior and unstable angina pectoris. E-CliniC. 2014;2(1):1-6. [Indonesian] [Link] [DOI:10.35790/ecl.2.1.2014.3597]
36. Sagala SGL, Pangemanan JA, Djafar DU. Description of troponin T levels based on examination time and location of infarction in patients with acute myocardial infarction at RSUP Prof. Dr. R. D Kandou for the period January-December 2015. E-CliniC. 2016;4(2). [Indonesian] [Link] [DOI:10.35790/ecl.4.2.2016.14465]
37. Haider A, Bengs S, Luu J, Osto E, Siller-Matula JM, Muka T, et al. Sex and gender in cardiovascular medicine: Presentation and outcomes of acute coronary syndrome. Eur Heart J. 2020;41(13):1328-36. [Link] [DOI:10.1093/eurheartj/ehz898]
38. Mourad G, Strömberg A, Johansson P, Jaarsma T. Depressive symptoms, cardiac anxiety, and fear of body sensations in patients with non-cardiac chest pain, and their relation to healthcare-seeking behavior: A cross-sectional study. Patient. 2016;9(1):69-77. [Link] [DOI:10.1007/s40271-015-0125-0]
39. Toronto CE, LaRocco SA. Family perception of and experience with family presence during cardiopulmonary resuscitation: An integrative review. J Clin Nurs. 2019;28(1-2):32-46. [Link] [DOI:10.1111/jocn.14649]
40. Torke AM, Wocial LD, Johns SA, Sachs GA, Callahan CM, Bosslet GT, et al. The family navigator: A pilot intervention to support intensive care unit family surrogates. Am J Crit Care. 2016;25(6):498-507. [Link] [DOI:10.4037/ajcc2016730]
41. Carson SS, Cox CE, Wallenstein S, Hanson LC, Danis M, Tulsky JA, et al. Effect of palliative care-led meetings for families of patients with chronic critical illness: A randomized clinical trial. JAMA. 2016;316(1):51-62. [Link] [DOI:10.1001/jama.2016.8474]
42. Gaol NTL. Stress theories: Stimulus, response, and transactional. Buletin Psikologi. 2016;24(1):1-11. [Indonesian] [Link] [DOI:10.22146/bpsi.11224]
43. Palmeira AFA, Lopes CT, Neves VR. Nursing professionals' education on the spiritual dimension of critical patients. Revista Gaúcha de Enfermagem. 2023;44:. [Portuguese] [Link] [DOI:10.1590/1983-1447.2023.20220069.en]
44. Badanta B, Rivilla-García E, Lucchetti G, De Diego-Cordero R. The influence of spirituality and religion on critical care nursing: An integrative review. Nurs Crit Care. 2022;27(3):348-66. [Link] [DOI:10.1111/nicc.12645]
45. Willemse S, Smeets W, Van Leeuwen E, Janssen L, Foudraine N. Spiritual care in the ICU: Perspectives of Dutch intensivists, ICU nurses, and spiritual caregivers. J Relig Health. 2018;57(2):583-95. [Link] [DOI:10.1007/s10943-017-0457-2]
46. Kydonaki K, Kean S, Tocher J. Family involvement in intensive care: A qualitative exploration of critically ill patients, their families and critical care nurses (input study). J Clin Nurs. 2020;29(7-8):1115-28. [Link] [DOI:10.1111/jocn.15175]
47. LeMone P, Burke KM, Bauldoff G. Text book of medical surgical nursing. Jakarta: EGC; 2012. [Indonesian] [Link]
48. Kiwanuka F, Shayan SJ, Tolulope AA. Barriers to patient and family-centred care in adult intensive care units: A systematic review. Nurs Open. 2019;6(3):676-84. [Link] [DOI:10.1002/nop2.253]
49. Chiang VCL, Lee RLP, Ho FM, Leung CK, Tang YP, Wong WS, et al. Fulfilling the psychological and information need of the family members of critically ill patients using interactive mobile technology: A randomised controlled trial. Intensive Crit Care Nurs. 2017;41:77-83. [Link] [DOI:10.1016/j.iccn.2017.03.006]
50. Azoulay E, Pochard F, Chevret S, Jourdain M, Bornstain C, Wernet A, et al. Impact of a family information leaflet on effectiveness of information provided to family members of intensive care unit patients: A multicenter, prospective, randomized, controlled trial. Am J Respir Crit Care Med. 2002;165(4):438-42. [Link] [DOI:10.1164/ajrccm.165.4.200108-006oc]
51. Garrouste-Orgeas M, Max A, Lerin T, Gregoire C, Ruckly S, Kloeckner M, et al. Impact of proactive nurse participation in ICU family conferences: A mixed-method study. Crit Care Med. 2016;44(6):1116-28. [Link] [DOI:10.1097/CCM.0000000000001632]
52. Ciufo D, Hader R, Holly C. A comprehensive systematic review of visitation models in adult critical care units within the context of patient- and family-centred care. Int J Evid Based Healthc. 2011;9(4):362-87. [Link] [DOI:10.1111/j.1744-1609.2011.00229.x]
53. Tawil I, Brown LH, Comfort D, Crandall CS, West SD, Rollstin AD, et al. Family presence during brain death evaluation: A randomized controlled trial*. Crit Care Med. 2014;42(4):934-42. [Link] [DOI:10.1097/CCM.0000000000000102]
54. Sanabria-Mazo JP, Colomer-Carbonell A, Fernández-Vázquez Ó, Noboa-Rocamora G, Cardona-Ros G, McCracken LM, et al. A systematic review of cognitive behavioral therapy-based interventions for comorbid chronic pain and clinically relevant psychological distress. Front Psychol. 2023;14:1200685. [Link] [DOI:10.3389/fpsyg.2023.1200685]
55. Vambheim SM, Kyllo TM, Hegland S, Bystad M. Relaxation techniques as an intervention for chronic pain: A systematic review of randomized controlled trials. Heliyon. 2021;7(8):e07837. [Link] [DOI:10.1016/j.heliyon.2021.e07837]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






