Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 181-187 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nomiko D, Bar A, Monalisa M. Development of an Android-Based Breast Cancer Risk Detector. Health Educ Health Promot 2024; 12 (2) :181-187
URL: http://hehp.modares.ac.ir/article-5-73433-en.html
URL: http://hehp.modares.ac.ir/article-5-73433-en.html
1- Department of Nursing, Health Polytechnic of Ministry of Health Jambi, Jambi, Indonesia
Keywords: Knowledge [MeSH], Breast Self-Examination [MeSH], Mobile Applications [MeSH], Risk Assessment [MeSH]
Full-Text [PDF 654 kb]
(2348 Downloads)
| Abstract (HTML) (1200 Views)
Full-Text: (107 Views)
Introduction
Breast cancer is among the most common cancer types, characterized by the malignant growth of breast tissue due to the uncontrolled development of breast cells, subsequently spreading to adjacent breast tissue and other parts of the body [1, 2].
As per Globocan in 2020, breast cancer represented 30.8% of all cancer cases in women, ranking as the second most prevalent cancer globally, with a mortality rate of 6.9%. Indonesia reported the highest prevalence at 16.6%, accompanied by a mortality rate of 9.6 deaths per 100,000 population [3]. In Jambi Province, data from early breast cancer detection screenings identified 29 cases among women of childbearing age, with 751 individuals suspected of having breast tumors (lumps) out of 91,561 people examined in 2019-2020 [4].
In Indonesia, a striking 80% of breast cancer cases are diagnosed at an advanced stage (III-IV). At this stage, 40% of patients require hospitalization, and the mortality rate soars to 72%, earning it the classification of a late-stage diagnosis with a poorer prognosis [5]. A separate study highlighted that 65.45% of patients deferred examination due to uncertainty about the nature of their breast lump [6]. According to Waks et al. [7], delayed treatment in breast cancer patients is often attributed to a lack of awareness regarding the severity of their condition and infrequent engagement in early breast detection practices.
Breast cancer presents a significant health challenge for women in developing nations such as Indonesia, mainly due to the lack of comprehensive screening programs for detecting pre-cancerous conditions and early-stage cancers [8]. The delay in starting treatment among breast cancer patients often results from a lack of awareness about the disease, combined with infrequent participation in breast screening and early detection practices [1]. Therefore, emphasizing early detection strategies is vital for increasing awareness among women in their 20s about the risks linked to breast cancer [9].
Achieving a 50% reduction in breast cancer incidence is feasible through early detection methods, including clinical breast examination [8]. The initial stage of early detection involves breast self-examination to identify potential signs of breast cancer [10]. A comprehensive breast cancer early detection program encompasses three key pillars: Breast self-examination (SADARI), clinical breast examination (SADANIS), and mammography [11]. Remarkably, 86% of breast lumps are discovered through self-examination by individuals themselves [12].
Early detection, facilitated by the awareness of women of childbearing age, is a straightforward, practical, and cost-free approach. This method is particularly encouraged for women in their 20s [13]. Consequently, educational programs on breast cancer for women of childbearing age are of utmost importance today. These programs play a pivotal role in enhancing promotive and preventive endeavors aimed at reducing breast cancer mortality [6].
A mobile application offering easily accessible information on breast health emerges as an alternative medium for health promotion among women of childbearing age [14, 15]. The improved access to information on ongoing breast cancer care is a significant benefit of using mobile health applications, contributing meaningfully to early detection and prevention programs for breast cancer. Moreover, its user-friendly design ensures easy understanding and availability at any time [6, 16].
This study is significant as the prevalence of breast cancer continues to increase, making it the second leading cause of cancer-related deaths in women globally. Therefore, an early assessment of breast cancer risk in women becomes crucial. The findings from this study on the utilization of breast cancer risk assessment tools provide valuable insights for clinical management, especially for individuals seeking services related to screening and prevention. These tools help predict the likelihood of being at risk for developing breast cancer and contribute to the formulation of screening policies based on risk factors. The development of web-based applications proves instrumental in detecting potential breast cancer risks, preventing delayed awareness, and facilitating prompt follow-up actions before cancer cells spread throughout the body [17, 18].
Detecting breast cancer risk at an early stage and staying informed about the latest advancements in cancer treatment are crucial aspects of the strategy to prevent breast cancer-related deaths [19]. Early detection of breast cancer leads to smaller tumor sizes and limited spread, enhancing the chances of successful treatment. Regular screening examinations are considered the most reliable method for early detection of breast cancer [20].
This research aligns with the government’s commitment to controlling non-communicable diseases through innovative approaches in the health sector, particularly utilizing information technology such as e-health and m-health in Indonesia. To contribute to breast cancer control initiatives, there is a need for a health information system that can be accessed at any time. The objective of this research was to develop an Android-based application for detecting and assessing breast cancer risk.
Materials and Methods
Study design
This quasi-experimental utilized a mixed methods approach [21]. The intervention model will undergo field testing using a quasi-experimental design, specifically a pre- and post-test design with one group. The primary objective was to create media application products, specifically risk assessment detection applications and breast cancer education materials. The development process follows the ADDIE model, which includes analysis, design, development, implementation, and evaluation stages [22].
Participants
This study was conducted from July to August 2023, involving 59 women of childbearing age within the operational area of Puskesmas Simpang IV Sipin, Jambi City, Indonesia. The sampling method employed was purposive, selecting participants who met the inclusion criteria, such as the ability to cooperate during the study, ownership of an Android cellphone, proficiency in reading, and willingness to participate as respondents. Individuals who were unwell among women of childbearing age were excluded from the study. Before the research, the researcher provided detailed explanations and obtained informed consent from prospective respondents regarding the research procedures. Upon agreement, participants signed a consent form to become research respondents.
Sample size
According to Imas Masturoh and Nauri Anggita [23], a total of 59 students were calculated using Slovin's formula considering α=0.05, and the total population was considered to be 70 people.
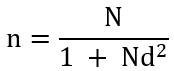
n=Number of samples
N=Number of populations
d=Precision
Research tools
The tools used include a set of question sheets created by the researcher and validated as appropriate. Additionally, the questions were assessed using a validated questionnaire completed by ten women of childbearing age, resulting in a Cronbach’s Alpha value of 0.807, which was greater than the critical value of 0.444, confirming the reliability of the data.
Data collection
A series of research activities were carried out, including the licensing process, feasibility testing for research ethics, the execution of the application development process with IT developers, the sampling procedure, provision of instructional material on application usage, limited application trials, and subsequent evaluation.
Product development involved comprehensive testing by media and material validators, followed by a limited comprehension test conducted with three respondents in a one-on-one setting, ten individuals in a small group, and fifty-nine participants in a large group.
The data collection process, from needs analysis to the evaluation of knowledge levels in large groups, was meticulously conducted by the research team without the involvement of enumerators.
Experimental evaluation
A web-based self-administered questionnaire was directly administered to each student by the development team to analyze their requirements for detecting and assessing breast cancer.
Focus groups
The researcher qualitatively engaged in discussions with the students in small groups to explore their needs regarding breast cancer detection. During these focus group sessions, their responses to the use of applications in detecting breast cancer were also observed.
Statistical analysis
In stage 1, which involves analysis, qualitative data were initially gathered during the initial observation activities, specifically at the needs analysis stage. The analysis phase was built from the ground up, often referred to as an inductive approach. Quantitative data analysis was conducted univariately with the aim of assessing percentages or the extent of issues or indicators under investigation. Quantitative data were collected from individuals who have close contact with tuberculosis patients, specifically the data generated during the needs analysis stage. These data were then subjected to descriptive statistical analysis, enabling a narrative interpretation of the urgency of addressing the identified problems for practical problem-solving purposes. In the prototype development phase, expert validation was qualitatively elucidated. Following this, during the one-on-one trial phase, qualitative analysis techniques, like the spiral method were utilized to uncover product weaknesses and shortcomings. In small group tests, qualitative data were scrutinized to steer enhancements in product quality. Moreover, quantitative data gathered from questionnaires and observations underwent statistical analysis. During the field test, data were presented descriptively, including frequencies. The Wilcoxon test was utilized to determine a causal relationship between the product’s usage and the observed impact, and statistical analyses were performed by SPSS 16.
Findings
The breast cancer risk assessment application was developed through the following stages.
Stage 1. Identification (problem, context, and literature analysis)
This stage was instigated by the global rise in breast cancer incidence rates, notably in Indonesia, where breast cancer ranks as the most prevalent malignancy and the leading cause of cancer-related deaths. Early detection and addressing contributing risk factors through early diagnosis efforts can significantly reduce mortality rates.
During this phase, the researcher identified and evaluated existing issues linked to breast cancer development, as well as potential strategies to mitigate disease incidence and mortality rates. Subsequently, a comprehensive literature review was conducted, examining government health promotion programs, particularly those targeting non-communicable diseases like breast cancer, and gathering numerical data on relevant events and information related to the concept of breast cancer.
Stage 2. Application model design
This stage began with the research team crafting the design concept for the application model. Presenting the storyboard to the IT developer lays the groundwork for developing the module for the breast cancer risk assessment detection application. The agreed-upon design concept revolves around an educational model embedded within the application, covering content on breast cancer concepts and management. This educational tool features text, animated graphics, videos, and other media, presented in an interactive manner through the integration of multimedia elements. Additionally, the application provides unrestricted access to information, overcoming spatial and temporal limitations, and enabling the target audience to engage with the media more flexibly.
Named the Deriskara (breast cancer risk detection) application, this acronym was crafted for easy recall by the target audience. The aim was for users to share the application content with other women of childbearing age, promoting individual follow-ups and benefiting the community.
The Deriskara application incorporated screening features to evaluate the risk of developing breast cancer as a proactive step in managing breast cancer incidence among women. The menu structure in this application was an advancement from the previous Edukara (breast cancer education) application, encompassing the sections, including demographic characteristics of respondents, breast cancer material, early detection through awareness (video), four breast cancer knowledge pre-post-test menus to assess respondents’ comprehension of the provided breast cancer material, introduction of five new menus focusing on breast cancer risk detection screening, which include risk factors, such as the respondent’s age, family history of breast cancer, history of individual tumors/cancers, age at first birth, age at first menstruation (menarche), and body mass index.
Stage 3: Material and media validation
The aim of this phase was to test the application unit to ensure that the upcoming development aligns with the specified requirements. This process involved evaluations from both media and material validators. Media validation was carried out in two rounds. In the initial media validation, the total score was 58 with an average of 2.9 (meeting valid criteria). The suggestions from validators were taken into account, focusing on aspects, such as appearance and communication. Recommendations included removing voice narration from the instructions, adjusting the text size on the option/dropdown to be proportional, and considering the removal of the welcome banner (pending further testing based on the suggestion). Subsequently, the application was refined according to the developer’s suggestions, followed by a second round of media validation, resulting in a score of 67 with an average of 3.35 (meeting valid criteria). This time, the tool was deemed suitable for testing on respondents.
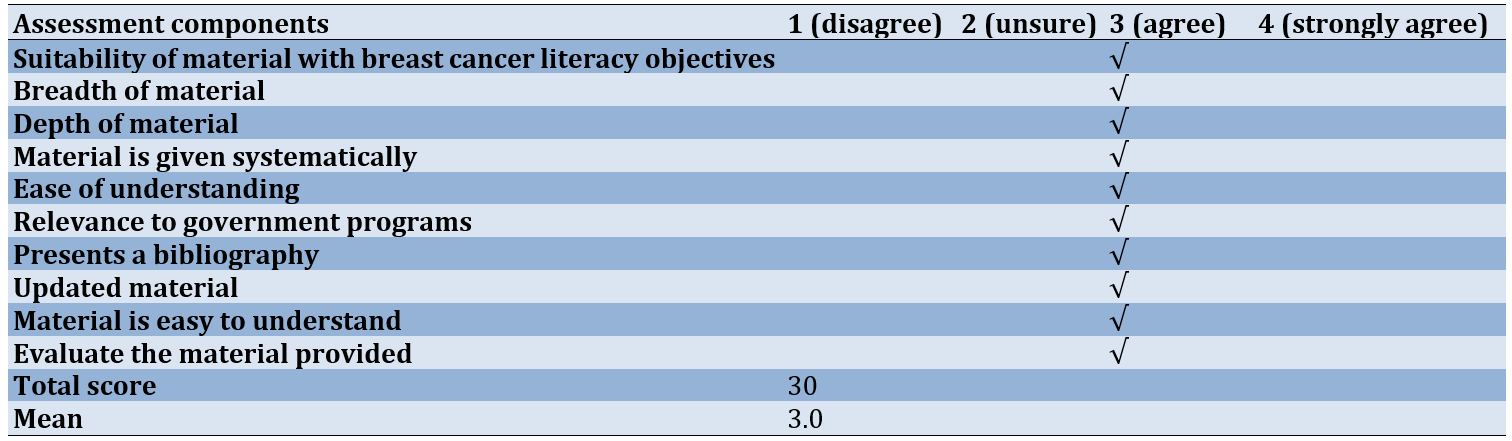
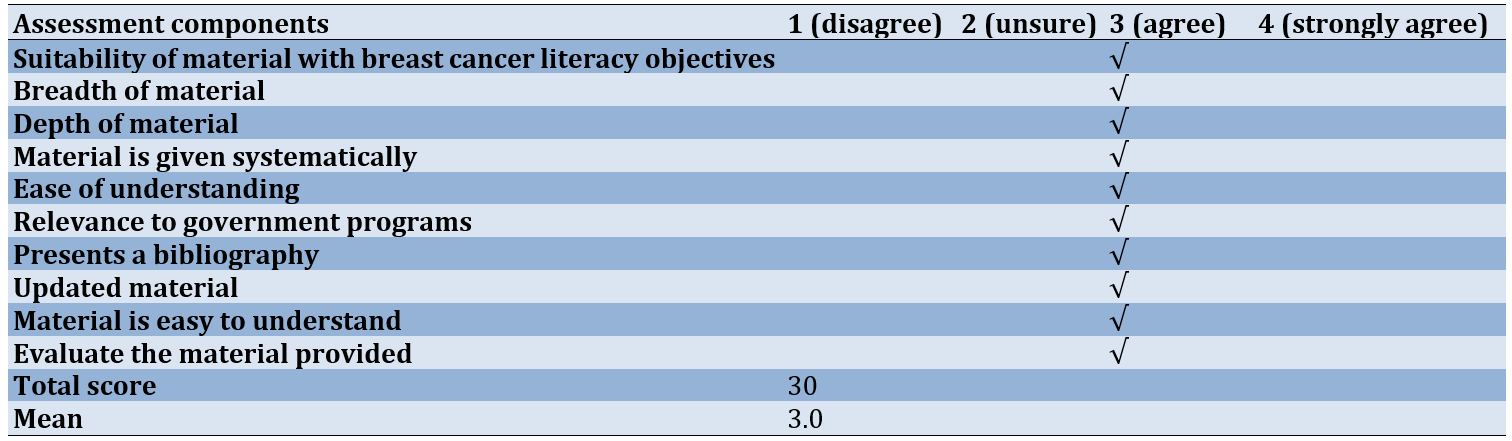
Regarding material validation, the recommendations highlighted that the provided material was in line with government programs, systematically presented, and included a bibliography within the application, enhancing its clarity. The material evaluation, conducted via the pre-post-test menu, underscored the importance of considering the depth and breadth of the material. It was suggested that the material should encompass the concept of breast cancer (including comprehension, symptoms, signs, and management), the concept of breast self-examination, and the assessment of breast cancer risk. These recommendations were considered valuable and worthy of further testing. The results of assessment by media experts were presented using two components of efficiency and media (Table 1), while results of material expert assessment encompassed 10 components (Table 2).
Table 1. Results of assessment by media experts
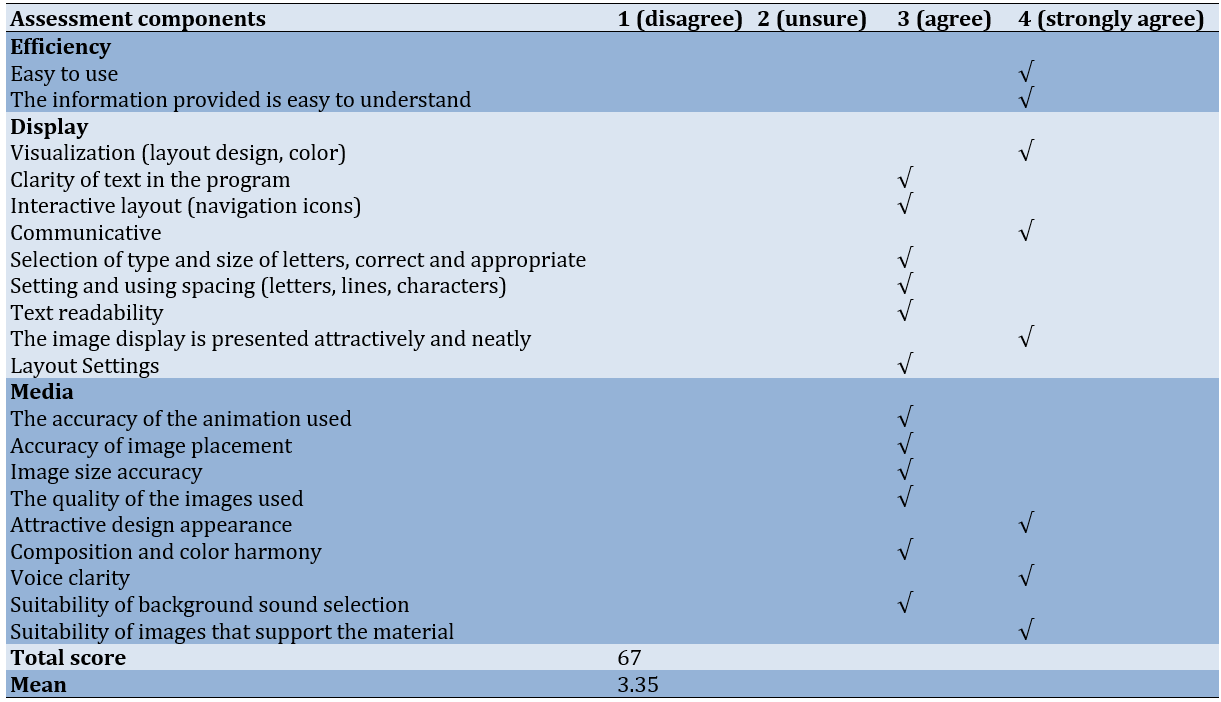
Table 2. Material expert assessment results
Stage 4. Deriskara application acceptance and understanding test
The acceptance testing of the breast cancer risk detection application involved one-on-one trials and small group tests to evaluate the effectiveness of respondents in utilizing the designed applications. The initial acceptance test was carried out through one-on-one trials with three participants. The results indicated that the participants easily understood the material, found the color composition of the media appealing, appreciated the use of simple language, and found the presentation of material in the application engaging. However, suggestions were made, highlighting the necessity for step-by-step instructions in using the application to address some confusion.
Transitioning to the second phase, the acceptance test of the application was expanded to a small group of ten individuals. The results of the acceptance test in small groups averaged 3.39 (meeting good criteria), with positive evaluations across various assessment criteria (Table 3).
Table 3. Results of acceptance test analysis of breast cancer risk detection application based on statement items
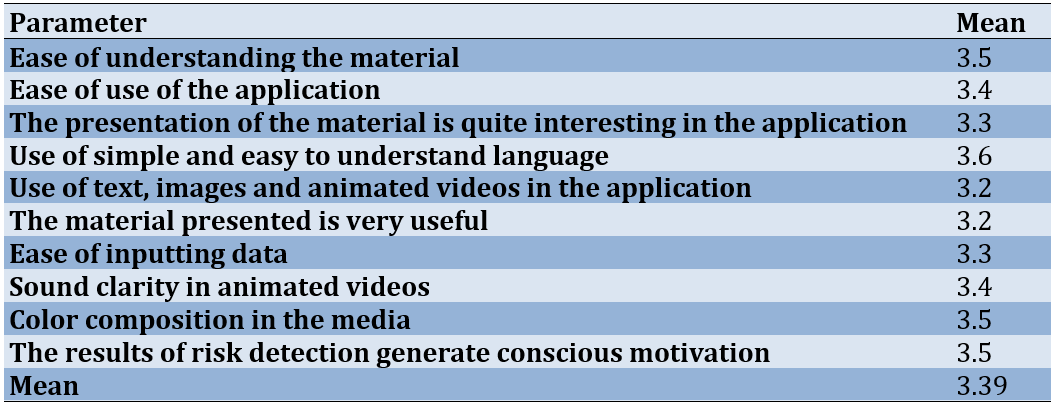
Table 3 demonstrates that the application was engaging and straightforward to comprehend. The videos and tests embedded within the application are highly beneficial for grasping the material, and the content was seen as particularly advantageous for women’s health. The findings from this small group test recommend enhancing the clarity of sound in the videos.
The mean value recorded prior to the intervention, using the Deriskara application, was 8.44. Subsequently, after the intervention with the Deriskara application, the knowledge level of women of childbearing age increased to 12.29, with the Wilcoxon test showing statistical significance.
Discussion
This study was conducted to develop an Android-based application for detecting and assessing breast cancer risk. Breast cancer is characterized by uncontrolled cell changes in the breast tissue, primarily originating from the milk lobules in the ducts [20]. Risk factors for breast cancer can be divided into unchangeable and modifiable factors. Unchangeable factors include age, gender, race, and family history, while modifiable factors consist of pregnancy and breastfeeding, hormone therapy, weight (obesity), physical activity, use of oral contraceptives, radiation during breast growth, history of benign tumors, alcohol consumption, smoking, and intake of fat and red meat [24].
Having risk factors for breast cancer does not guarantee the development of the disease. These factors help identify women who may benefit from increased screening or other preventive measures. Importantly, many women with risk factors never develop breast cancer [25].
Numerous studies have investigated risk factors linked to breast cancer, including giving birth after the age of 35, a family history of breast cancer, early onset of menstruation before the age of 12, menopausal status, gender, age, estrogen hormone levels, and unhealthy lifestyles, all of which increase the risk of developing breast cancer. Early diagnosis significantly contributes to a positive prognosis, with an 80% increase in individual life expectancy over the next five years for those who undergo early screening [25].
Breast cancer prevention and control programs begin by addressing these risk factors and implementing measures to reduce them, utilizing three levels of prevention: Primary, secondary, and tertiary prevention. Screening and early detection, which fall under secondary prevention, aim to detect conditions before cancer develops or is in its early stages. Breast cancer early detection efforts concentrate on identifying the disease early, enabling treatment with reduced physical impact and a greater chance of recovery. When treated effectively, breast cancer has a high cure rate (80%-90%), made possible through both screening and early detection [24].
Screening tests are evaluations used to detect diseases in individuals without any noticeable symptoms. The main goal of breast cancer screening tests is to identify risks at an early stage before symptoms appear. Early detection involves finding and diagnosing the disease before any symptoms arise. The size and spread of the disease are vital factors in predicting the prognosis for women diagnosed with breast cancer [24]. Early detection of risk factors through systematic breast cancer screening substantially decreases mortality rates, followed by subsequent screening for individuals identified as high-risk [26, 27].
The principles guiding screening include, firstly, that the targeted disease must be serious, relatively common, and acknowledged as a public health issue by the community. Secondly, the screening procedure must be safe and acceptable to the community, necessitating the involvement of individuals considered appropriate for screening. Thirdly, screening should be precise and dependable, with accuracy indicating the extent to which test results correspond to the actual health condition being assessed [28-30].
The incorporation of technology in breast cancer prevention is apparent in several studies, showing that the use of technology, especially through m-Health applications for breast cancer, seeks to boost awareness, offer information, and support early cancer detection [6, 11, 31, 32]. Another significant research discovery is that mobile health apps focused on breast cancer aid in prevention programs, improve access to information, and offer continuous education on cancer care. Mobile apps act as a valuable resource to promote education in cancer prevention and treatment [33].
The results of this study indicate that utilizing Android applications for breast cancer risk assessment can improve the awareness of women of childbearing age. This is demonstrated in the Wilcoxon test outcomes, where participants initially exhibited a low knowledge score before the intervention, which then increased following the introduction of the Android applications.
Looking ahead, it is crucial for the government to launch public awareness campaigns concerning the use of mobile phones for breast cancer risk detection applications. Furthermore, women of childbearing age should have easy access to these applications.
The study was limited to a single location, leading to a very restricted number of participants. In future research, it is crucial to broaden the participant pool across different locations to achieve a more diverse range of participant characteristics.
Conclusion
The development of an Android-based breast cancer risk assessment detection application is well-received among women of childbearing age and has a positive impact on enhancing their knowledge.
Acknowledgments: We sincerely thank the President of Jambi Health Polytechnic for valuable support in providing necessary research facilities.
Ethical Permissions: This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi (LB.02.06/2/571/2023).
Conflicts of Interests: Nothing to be declared.
Authors’ Contribution: Nomiko D (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Bar A (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Monalisa (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research did not receive financial support from any party.
Breast cancer is among the most common cancer types, characterized by the malignant growth of breast tissue due to the uncontrolled development of breast cells, subsequently spreading to adjacent breast tissue and other parts of the body [1, 2].
As per Globocan in 2020, breast cancer represented 30.8% of all cancer cases in women, ranking as the second most prevalent cancer globally, with a mortality rate of 6.9%. Indonesia reported the highest prevalence at 16.6%, accompanied by a mortality rate of 9.6 deaths per 100,000 population [3]. In Jambi Province, data from early breast cancer detection screenings identified 29 cases among women of childbearing age, with 751 individuals suspected of having breast tumors (lumps) out of 91,561 people examined in 2019-2020 [4].
In Indonesia, a striking 80% of breast cancer cases are diagnosed at an advanced stage (III-IV). At this stage, 40% of patients require hospitalization, and the mortality rate soars to 72%, earning it the classification of a late-stage diagnosis with a poorer prognosis [5]. A separate study highlighted that 65.45% of patients deferred examination due to uncertainty about the nature of their breast lump [6]. According to Waks et al. [7], delayed treatment in breast cancer patients is often attributed to a lack of awareness regarding the severity of their condition and infrequent engagement in early breast detection practices.
Breast cancer presents a significant health challenge for women in developing nations such as Indonesia, mainly due to the lack of comprehensive screening programs for detecting pre-cancerous conditions and early-stage cancers [8]. The delay in starting treatment among breast cancer patients often results from a lack of awareness about the disease, combined with infrequent participation in breast screening and early detection practices [1]. Therefore, emphasizing early detection strategies is vital for increasing awareness among women in their 20s about the risks linked to breast cancer [9].
Achieving a 50% reduction in breast cancer incidence is feasible through early detection methods, including clinical breast examination [8]. The initial stage of early detection involves breast self-examination to identify potential signs of breast cancer [10]. A comprehensive breast cancer early detection program encompasses three key pillars: Breast self-examination (SADARI), clinical breast examination (SADANIS), and mammography [11]. Remarkably, 86% of breast lumps are discovered through self-examination by individuals themselves [12].
Early detection, facilitated by the awareness of women of childbearing age, is a straightforward, practical, and cost-free approach. This method is particularly encouraged for women in their 20s [13]. Consequently, educational programs on breast cancer for women of childbearing age are of utmost importance today. These programs play a pivotal role in enhancing promotive and preventive endeavors aimed at reducing breast cancer mortality [6].
A mobile application offering easily accessible information on breast health emerges as an alternative medium for health promotion among women of childbearing age [14, 15]. The improved access to information on ongoing breast cancer care is a significant benefit of using mobile health applications, contributing meaningfully to early detection and prevention programs for breast cancer. Moreover, its user-friendly design ensures easy understanding and availability at any time [6, 16].
This study is significant as the prevalence of breast cancer continues to increase, making it the second leading cause of cancer-related deaths in women globally. Therefore, an early assessment of breast cancer risk in women becomes crucial. The findings from this study on the utilization of breast cancer risk assessment tools provide valuable insights for clinical management, especially for individuals seeking services related to screening and prevention. These tools help predict the likelihood of being at risk for developing breast cancer and contribute to the formulation of screening policies based on risk factors. The development of web-based applications proves instrumental in detecting potential breast cancer risks, preventing delayed awareness, and facilitating prompt follow-up actions before cancer cells spread throughout the body [17, 18].
Detecting breast cancer risk at an early stage and staying informed about the latest advancements in cancer treatment are crucial aspects of the strategy to prevent breast cancer-related deaths [19]. Early detection of breast cancer leads to smaller tumor sizes and limited spread, enhancing the chances of successful treatment. Regular screening examinations are considered the most reliable method for early detection of breast cancer [20].
This research aligns with the government’s commitment to controlling non-communicable diseases through innovative approaches in the health sector, particularly utilizing information technology such as e-health and m-health in Indonesia. To contribute to breast cancer control initiatives, there is a need for a health information system that can be accessed at any time. The objective of this research was to develop an Android-based application for detecting and assessing breast cancer risk.
Materials and Methods
Study design
This quasi-experimental utilized a mixed methods approach [21]. The intervention model will undergo field testing using a quasi-experimental design, specifically a pre- and post-test design with one group. The primary objective was to create media application products, specifically risk assessment detection applications and breast cancer education materials. The development process follows the ADDIE model, which includes analysis, design, development, implementation, and evaluation stages [22].
Participants
This study was conducted from July to August 2023, involving 59 women of childbearing age within the operational area of Puskesmas Simpang IV Sipin, Jambi City, Indonesia. The sampling method employed was purposive, selecting participants who met the inclusion criteria, such as the ability to cooperate during the study, ownership of an Android cellphone, proficiency in reading, and willingness to participate as respondents. Individuals who were unwell among women of childbearing age were excluded from the study. Before the research, the researcher provided detailed explanations and obtained informed consent from prospective respondents regarding the research procedures. Upon agreement, participants signed a consent form to become research respondents.
Sample size
According to Imas Masturoh and Nauri Anggita [23], a total of 59 students were calculated using Slovin's formula considering α=0.05, and the total population was considered to be 70 people.
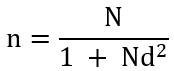
n=Number of samples
N=Number of populations
d=Precision
Research tools
The tools used include a set of question sheets created by the researcher and validated as appropriate. Additionally, the questions were assessed using a validated questionnaire completed by ten women of childbearing age, resulting in a Cronbach’s Alpha value of 0.807, which was greater than the critical value of 0.444, confirming the reliability of the data.
Data collection
A series of research activities were carried out, including the licensing process, feasibility testing for research ethics, the execution of the application development process with IT developers, the sampling procedure, provision of instructional material on application usage, limited application trials, and subsequent evaluation.
Product development involved comprehensive testing by media and material validators, followed by a limited comprehension test conducted with three respondents in a one-on-one setting, ten individuals in a small group, and fifty-nine participants in a large group.
The data collection process, from needs analysis to the evaluation of knowledge levels in large groups, was meticulously conducted by the research team without the involvement of enumerators.
Experimental evaluation
A web-based self-administered questionnaire was directly administered to each student by the development team to analyze their requirements for detecting and assessing breast cancer.
Focus groups
The researcher qualitatively engaged in discussions with the students in small groups to explore their needs regarding breast cancer detection. During these focus group sessions, their responses to the use of applications in detecting breast cancer were also observed.
Statistical analysis
In stage 1, which involves analysis, qualitative data were initially gathered during the initial observation activities, specifically at the needs analysis stage. The analysis phase was built from the ground up, often referred to as an inductive approach. Quantitative data analysis was conducted univariately with the aim of assessing percentages or the extent of issues or indicators under investigation. Quantitative data were collected from individuals who have close contact with tuberculosis patients, specifically the data generated during the needs analysis stage. These data were then subjected to descriptive statistical analysis, enabling a narrative interpretation of the urgency of addressing the identified problems for practical problem-solving purposes. In the prototype development phase, expert validation was qualitatively elucidated. Following this, during the one-on-one trial phase, qualitative analysis techniques, like the spiral method were utilized to uncover product weaknesses and shortcomings. In small group tests, qualitative data were scrutinized to steer enhancements in product quality. Moreover, quantitative data gathered from questionnaires and observations underwent statistical analysis. During the field test, data were presented descriptively, including frequencies. The Wilcoxon test was utilized to determine a causal relationship between the product’s usage and the observed impact, and statistical analyses were performed by SPSS 16.
Findings
The breast cancer risk assessment application was developed through the following stages.
Stage 1. Identification (problem, context, and literature analysis)
This stage was instigated by the global rise in breast cancer incidence rates, notably in Indonesia, where breast cancer ranks as the most prevalent malignancy and the leading cause of cancer-related deaths. Early detection and addressing contributing risk factors through early diagnosis efforts can significantly reduce mortality rates.
During this phase, the researcher identified and evaluated existing issues linked to breast cancer development, as well as potential strategies to mitigate disease incidence and mortality rates. Subsequently, a comprehensive literature review was conducted, examining government health promotion programs, particularly those targeting non-communicable diseases like breast cancer, and gathering numerical data on relevant events and information related to the concept of breast cancer.
Stage 2. Application model design
This stage began with the research team crafting the design concept for the application model. Presenting the storyboard to the IT developer lays the groundwork for developing the module for the breast cancer risk assessment detection application. The agreed-upon design concept revolves around an educational model embedded within the application, covering content on breast cancer concepts and management. This educational tool features text, animated graphics, videos, and other media, presented in an interactive manner through the integration of multimedia elements. Additionally, the application provides unrestricted access to information, overcoming spatial and temporal limitations, and enabling the target audience to engage with the media more flexibly.
Named the Deriskara (breast cancer risk detection) application, this acronym was crafted for easy recall by the target audience. The aim was for users to share the application content with other women of childbearing age, promoting individual follow-ups and benefiting the community.
The Deriskara application incorporated screening features to evaluate the risk of developing breast cancer as a proactive step in managing breast cancer incidence among women. The menu structure in this application was an advancement from the previous Edukara (breast cancer education) application, encompassing the sections, including demographic characteristics of respondents, breast cancer material, early detection through awareness (video), four breast cancer knowledge pre-post-test menus to assess respondents’ comprehension of the provided breast cancer material, introduction of five new menus focusing on breast cancer risk detection screening, which include risk factors, such as the respondent’s age, family history of breast cancer, history of individual tumors/cancers, age at first birth, age at first menstruation (menarche), and body mass index.
Stage 3: Material and media validation
The aim of this phase was to test the application unit to ensure that the upcoming development aligns with the specified requirements. This process involved evaluations from both media and material validators. Media validation was carried out in two rounds. In the initial media validation, the total score was 58 with an average of 2.9 (meeting valid criteria). The suggestions from validators were taken into account, focusing on aspects, such as appearance and communication. Recommendations included removing voice narration from the instructions, adjusting the text size on the option/dropdown to be proportional, and considering the removal of the welcome banner (pending further testing based on the suggestion). Subsequently, the application was refined according to the developer’s suggestions, followed by a second round of media validation, resulting in a score of 67 with an average of 3.35 (meeting valid criteria). This time, the tool was deemed suitable for testing on respondents.
Regarding material validation, the recommendations highlighted that the provided material was in line with government programs, systematically presented, and included a bibliography within the application, enhancing its clarity. The material evaluation, conducted via the pre-post-test menu, underscored the importance of considering the depth and breadth of the material. It was suggested that the material should encompass the concept of breast cancer (including comprehension, symptoms, signs, and management), the concept of breast self-examination, and the assessment of breast cancer risk. These recommendations were considered valuable and worthy of further testing. The results of assessment by media experts were presented using two components of efficiency and media (Table 1), while results of material expert assessment encompassed 10 components (Table 2).
Table 1. Results of assessment by media experts
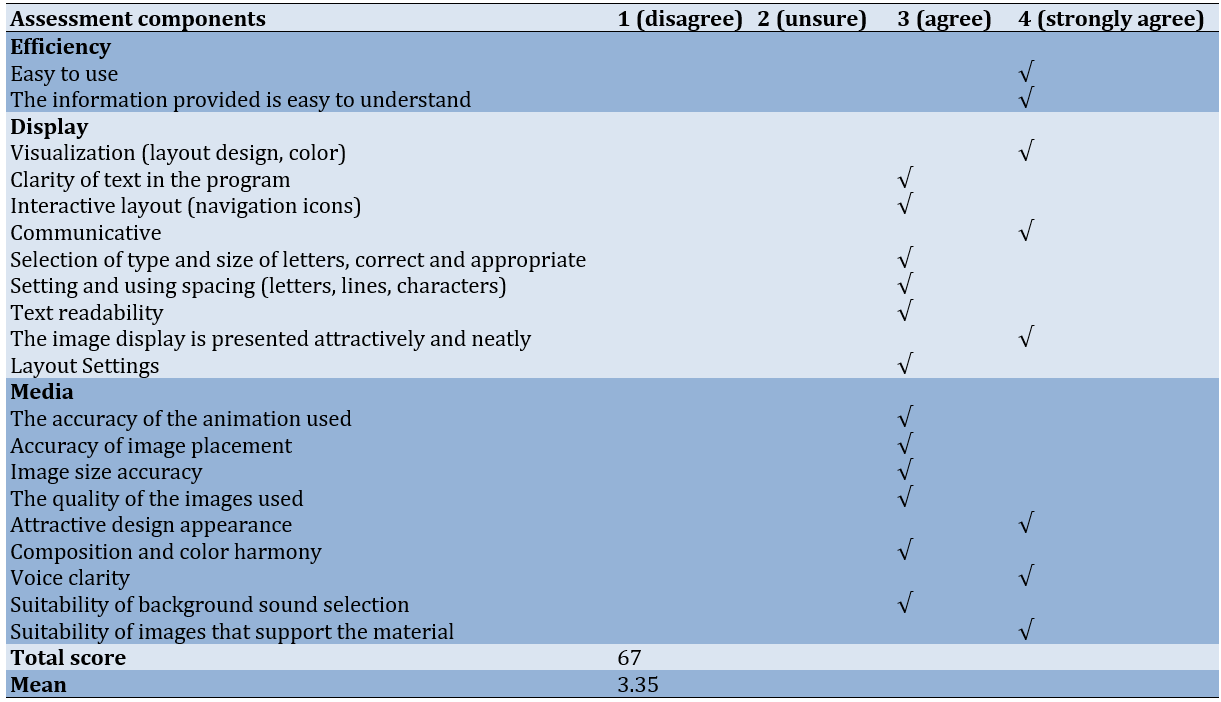
Table 2. Material expert assessment results
Stage 4. Deriskara application acceptance and understanding test
The acceptance testing of the breast cancer risk detection application involved one-on-one trials and small group tests to evaluate the effectiveness of respondents in utilizing the designed applications. The initial acceptance test was carried out through one-on-one trials with three participants. The results indicated that the participants easily understood the material, found the color composition of the media appealing, appreciated the use of simple language, and found the presentation of material in the application engaging. However, suggestions were made, highlighting the necessity for step-by-step instructions in using the application to address some confusion.
Transitioning to the second phase, the acceptance test of the application was expanded to a small group of ten individuals. The results of the acceptance test in small groups averaged 3.39 (meeting good criteria), with positive evaluations across various assessment criteria (Table 3).
Table 3. Results of acceptance test analysis of breast cancer risk detection application based on statement items
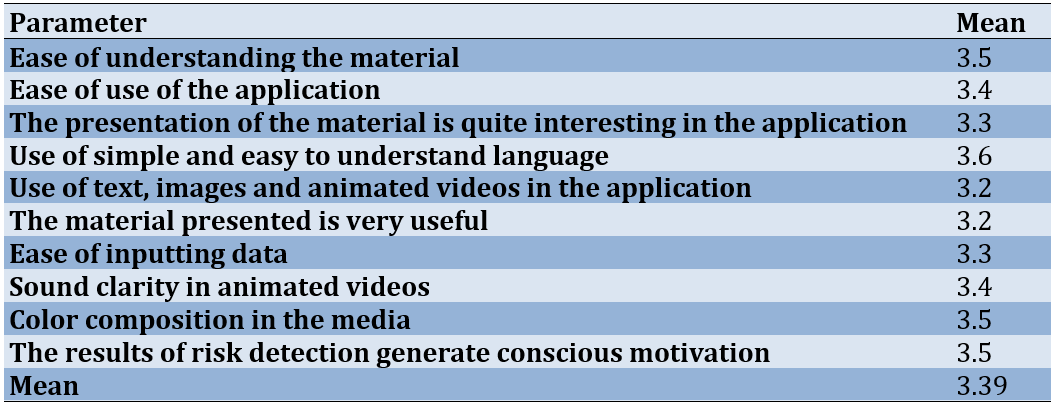
Table 3 demonstrates that the application was engaging and straightforward to comprehend. The videos and tests embedded within the application are highly beneficial for grasping the material, and the content was seen as particularly advantageous for women’s health. The findings from this small group test recommend enhancing the clarity of sound in the videos.
The mean value recorded prior to the intervention, using the Deriskara application, was 8.44. Subsequently, after the intervention with the Deriskara application, the knowledge level of women of childbearing age increased to 12.29, with the Wilcoxon test showing statistical significance.
Discussion
This study was conducted to develop an Android-based application for detecting and assessing breast cancer risk. Breast cancer is characterized by uncontrolled cell changes in the breast tissue, primarily originating from the milk lobules in the ducts [20]. Risk factors for breast cancer can be divided into unchangeable and modifiable factors. Unchangeable factors include age, gender, race, and family history, while modifiable factors consist of pregnancy and breastfeeding, hormone therapy, weight (obesity), physical activity, use of oral contraceptives, radiation during breast growth, history of benign tumors, alcohol consumption, smoking, and intake of fat and red meat [24].
Having risk factors for breast cancer does not guarantee the development of the disease. These factors help identify women who may benefit from increased screening or other preventive measures. Importantly, many women with risk factors never develop breast cancer [25].
Numerous studies have investigated risk factors linked to breast cancer, including giving birth after the age of 35, a family history of breast cancer, early onset of menstruation before the age of 12, menopausal status, gender, age, estrogen hormone levels, and unhealthy lifestyles, all of which increase the risk of developing breast cancer. Early diagnosis significantly contributes to a positive prognosis, with an 80% increase in individual life expectancy over the next five years for those who undergo early screening [25].
Breast cancer prevention and control programs begin by addressing these risk factors and implementing measures to reduce them, utilizing three levels of prevention: Primary, secondary, and tertiary prevention. Screening and early detection, which fall under secondary prevention, aim to detect conditions before cancer develops or is in its early stages. Breast cancer early detection efforts concentrate on identifying the disease early, enabling treatment with reduced physical impact and a greater chance of recovery. When treated effectively, breast cancer has a high cure rate (80%-90%), made possible through both screening and early detection [24].
Screening tests are evaluations used to detect diseases in individuals without any noticeable symptoms. The main goal of breast cancer screening tests is to identify risks at an early stage before symptoms appear. Early detection involves finding and diagnosing the disease before any symptoms arise. The size and spread of the disease are vital factors in predicting the prognosis for women diagnosed with breast cancer [24]. Early detection of risk factors through systematic breast cancer screening substantially decreases mortality rates, followed by subsequent screening for individuals identified as high-risk [26, 27].
The principles guiding screening include, firstly, that the targeted disease must be serious, relatively common, and acknowledged as a public health issue by the community. Secondly, the screening procedure must be safe and acceptable to the community, necessitating the involvement of individuals considered appropriate for screening. Thirdly, screening should be precise and dependable, with accuracy indicating the extent to which test results correspond to the actual health condition being assessed [28-30].
The incorporation of technology in breast cancer prevention is apparent in several studies, showing that the use of technology, especially through m-Health applications for breast cancer, seeks to boost awareness, offer information, and support early cancer detection [6, 11, 31, 32]. Another significant research discovery is that mobile health apps focused on breast cancer aid in prevention programs, improve access to information, and offer continuous education on cancer care. Mobile apps act as a valuable resource to promote education in cancer prevention and treatment [33].
The results of this study indicate that utilizing Android applications for breast cancer risk assessment can improve the awareness of women of childbearing age. This is demonstrated in the Wilcoxon test outcomes, where participants initially exhibited a low knowledge score before the intervention, which then increased following the introduction of the Android applications.
Looking ahead, it is crucial for the government to launch public awareness campaigns concerning the use of mobile phones for breast cancer risk detection applications. Furthermore, women of childbearing age should have easy access to these applications.
The study was limited to a single location, leading to a very restricted number of participants. In future research, it is crucial to broaden the participant pool across different locations to achieve a more diverse range of participant characteristics.
Conclusion
The development of an Android-based breast cancer risk assessment detection application is well-received among women of childbearing age and has a positive impact on enhancing their knowledge.
Acknowledgments: We sincerely thank the President of Jambi Health Polytechnic for valuable support in providing necessary research facilities.
Ethical Permissions: This study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi (LB.02.06/2/571/2023).
Conflicts of Interests: Nothing to be declared.
Authors’ Contribution: Nomiko D (First Author), Introduction Writer/Methodologist/Main Researcher (50%); Bar A (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Monalisa (Third Author), Assistant Researcher/Discussion Writer/Statistical Analyst (25%)
Funding/Support: This research did not receive financial support from any party.
Article Type: Original Research |
Subject:
Health Media
Received: 2024/01/16 | Accepted: 2024/04/5 | Published: 2024/04/27
Received: 2024/01/16 | Accepted: 2024/04/5 | Published: 2024/04/27
References
1. Memon ZA, Kanwal N, Sami M, Larik PA, Farooq MZ. Risk of breast cancer among young women and importance of early screening. Asian Pac J Cancer Prev. 2015;16(17):7485-9. [Link] [DOI:10.7314/APJCP.2015.16.17.7485]
2. Al Husaini MAS, Hadi Habaebi M, Gunawan TS, Islam MR. Self-detection of early breast cancer application with infrared camera and deep learning. Electronics. 2021;10(20):2538. [Link] [DOI:10.3390/electronics10202538]
3. UICC. GLOBOCAN 2020: New global cancer data [Internet]. Geneva: :union: for International Cancer Control. 2020 Dec 17 [2023-12-12]. Available from: https://www.uicc.org/news/globocan-2020-new-global-cancer-data [Link]
4. Kemenkes RI. Main results of RISKESDAS 2018. Jakarta: Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan; 2018. [Indonesian] [Link]
5. Kemenkes RI. Indonesia's health profile in 2021. Jakarta:Kementrian Kesehatan Republik Indonesia; 2023. [Indonesian] [Link]
6. Chowdhury D, Das A, Dey A, Sarkar S, Dwivedi AD, Rao Mukkamala R, et al. ABCanDroid: A cloud integrated android app for noninvasive early breast cancer detection using transfer learning. Sensors. 2022;22(3):832. [Link] [DOI:10.3390/s22030832]
7. Waks AG, Winer EP. Breast cancer treatment: A review. JAMA. 2019;321(3):288-300. [Link] [DOI:10.1001/jama.2018.19323]
8. Milosevic M, Jankovic D, Milenkovic A, Stojanov D. Early diagnosis and detection of breast cancer. Technol Health Care. 2018;26(4):729-59. [Link] [DOI:10.3233/THC-181277]
9. Gupta R, Gupta S, Mehrotra R, Sodhani P. Risk factors of breast cancer and breast self-examination in early detection: Systematic review of awareness among Indian women in community and health care professionals. J Public Health. 2020;42(1):118-31. [Link] [DOI:10.1093/pubmed/fdy228]
10. Moo TA, Sanford R, Dang C, Morrow M. Overview of breast cancer therapy. PET Clin. 2018;13(3):339-54. [Link] [DOI:10.1016/j.cpet.2018.02.006]
11. Suprapto, Anita KW. Breast cancer screening application based on android with the certainty factor method. IAIC Int Conf Ser. 2023;4(1):88-96. [Link] [DOI:10.34306/conferenceseries.v4i1.633]
12. Abo Al-Shiekh SS, Ibrahim MA, Alajerami YS. Breast cancer knowledge and practice of breast self-examination among female university students, Gaza. Sci World J. 2021;2021:6640324. [Link] [DOI:10.1155/2021/6640324]
13. Abd-Elaziz NM, Kamal HH, Abd-Elhady H. Effect of breast self examination programme on women's awareness for early detection of breast cancer. Minia Sci Nur J. 2021;10(1):132-40. [Link] [DOI:10.21608/msnj.2021.107542.1014]
14. Bener A, Barışık CC, Acar A, Özdenkaya Y. Assessment of the gail model in estimating the risk of breast cancer: Effect of cancer worry and risk in healthy women. Asian Pac J Cancer Prev. 2019;20(6):1765-71. [Link] [DOI:10.31557/APJCP.2019.20.6.1765]
15. Basegio DL, Corrêa MPA, Kuiava VA, De Quadros C, De Mattos MPB, Pavan NR, et al. The importance of breast self-examination as a diagnostic method of breast cancer. Mastology. 2019;29(1):14-9. [Link] [DOI:10.29289/2594539420190000424]
16. Ginsburg O, Yip C, Brooks A, Cabanes A, Caleffi M, Dunstan Yataco JA, et al. Breast cancer early detection: A phased approach to implementation. Cancer. 2020;126(Suppl 10):2379-93. [Link] [DOI:10.1002/cncr.32887]
17. Kapoor A, Nambisan P, Baker E. Mobile applications for breast cancer survivorship and self-management: A systematic review. Health Informatics J. 2020;26(4):2892-905. [Link] [DOI:10.1177/1460458220950853]
18. Öztürk ES, Kutlutürkan S. The effect of the mobile application-based symptom monitoring process on the symptom control and quality of life in breast cancer patients. Semin Oncol Nurs. 2021;37(3):151161. [Link] [DOI:10.1016/j.soncn.2021.151161]
19. Louro J, Posso M, Hilton Boon M, Román M, Domingo L, Castells X, et al. A systematic review and quality assessment of individualised breast cancer risk prediction models. Br J Cancer. 2019;121(1):76-85. [Link] [DOI:10.1038/s41416-019-0476-8]
20. American Cancer Society. Cancer facts and figures 2021. Atlanta: American Cancer Society; 2021. [Link]
21. Creswell JW. Steps in conducting a scholarly mixed methods study. DBER Speaker Series; 2013. 48. [Link]
22. Rusdi M. Indonesia's health profile in 2021. Depok: Raja Grafindo Persada PT; 2018. [Indonesian] [Link]
23. Imas Masturoh SKM, Nauri Anggita T. Health research methodology. Jakarta: Kementerian Kesehatan Republik Indonesia; 2018. [Indonesian] [Link]
24. Kementerian Kesehatan RI. Technical guidelines for controlling breast cancer and cervical cancer. Jakarta: Kementrian Kesehatan Republik Indonesia; 2013. [Indonesian] [Link]
25. Kamińska M, Ciszewski T, Łopacka-Szatan K, Miotła P, Starosławska E. Breast cancer risk factors. Prz Menopauzalny. 2015;14(3):196-202. [Link] [DOI:10.5114/pm.2015.54346]
26. Erbil N, Dundar N, Inan C, Bolukbas N. Breast cancer risk assessment using the Gail model: A Turkish study. Asian Pac J Cancer Prev. 2015;16(1):303-6. [Link] [DOI:10.7314/APJCP.2015.16.1.303]
27. Panigroro S, Hernowo BS, Purwanto H. Breast cancer treatment guideline. Jurnal Kesehatan Masyarakat. 2019;4(4):1-50. [Indonesian] [Link]
28. Almurshidi SH, Abu-Naser SS. Breast cancer knowledge based system. Int J Acad Health Med Res. 2018;2(12):7-22. [Link]
29. Cruz FOAM, Vilela RA, Ferreira EB, Melo NS, Reis PEDD. Evidence on the use of mobile apps during the treatment of breast cancer: Systematic review. JMIR Mhealth Uhealth. 2019;7(8):e13245. [Link] [DOI:10.2196/13245]
30. Wright A. Evaluation of two mobile health apps for patients with breast cancer using the Mobile Application Rating Scale. Mhealth. 2021;7:60. [Link] [DOI:10.21037/mhealth-20-161]
31. Bhan AD, Jayaram J. Screening, self-examination and awareness in breast cancer. In: Breast cancer: Comprehensive management. Singapore: Springer; 2022. p. 587-600. [Link] [DOI:10.1007/978-981-16-4546-4_29]
32. Yang S, Bui CN, Park K. Mobile health apps for breast cancer: Content analysis and quality assessment. JMIR Mhealth Uhealth. 2023;11:e43522. [Link] [DOI:10.2196/43522]
33. Panayi ND, Mars MM, Burd R. The promise of digital (mobile) health in cancer prevention and treatment. Future Oncol. 2013;9(5):613-7. [Link] [DOI:10.2217/fon.13.42]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






