Volume 12, Issue 1 (2024)
Health Educ Health Promot 2024, 12(1): 91-104 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rojas J, Fuster-Guillén D, Flores J, Hernandez R. Successful Practices in the Teaching-Learning of Physical Therapy. Health Educ Health Promot 2024; 12 (1) :91-104
URL: http://hehp.modares.ac.ir/article-5-73382-en.html
URL: http://hehp.modares.ac.ir/article-5-73382-en.html
1- Postgraduate School, Cesar Vallejo University, Lima, Perú
2- Faculty of Health Sciences, San Juan Bautista Private University, Lima, Perú
3- Postgraduate School, Continental University, Lima, Perú
4- Research Department, Norbert Wiener Private University, Lima, Perú
2- Faculty of Health Sciences, San Juan Bautista Private University, Lima, Perú
3- Postgraduate School, Continental University, Lima, Perú
4- Research Department, Norbert Wiener Private University, Lima, Perú
Keywords: Simulation [Mesh], Inverted Classroom [MeSH], earning Strategies [MeSH], roblem-Based Learning [MeSH], Active Methodology [MeSH]
Full-Text [PDF 805 kb]
(4683 Downloads)
| Abstract (HTML) (1825 Views)
Full-Text: (326 Views)
Introduction
This study is focused on identifying successful practices in the teaching-learning of physiotherapy. The practices integral to professional training transcend mere theoretical knowledge and content delivery. They serve as conduits for bridging theory with practice, enabling students to concretely apply competencies, skills, and abilities in real-world scenarios. Students gain firsthand experience in the complexities of patient care, honing their conceptual, methodological, and ethical acumen by engaging in these practices [1, 2]. Active methodologies focused on the learner take precedence over traditional content-centric approaches, challenging long-standing orthodox teaching paradigms in physiotherapy education. This shift redefines the role of the teacher as a mediator, facilitator, and guide, fostering active engagement, collaborative interactions, creativity, critical thinking, and reflective practice. The didactic strategies are tailored to address real-world challenges, encouraging problem-solving and application-oriented learning [3-5]. This approach aligns with a constructivist point of view wherein the learning and evaluation process is viewed as dynamic and contextually situated [6, 7]. Multiple studies have left evidence of implementing such practices.
The advancement of science is in permanent transformation every day, demanding methods that empower students to develop abilities that allow autonomous learning and critical and reflective thinking. However, higher education systems in health disciplines, especially physiotherapy, are still dominated by traditional teacher-centric approaches. These methods typically entail one-way content delivery and rote memorization, relegating students to passive receivers. Therefore, such methodologies fail to equip learners with the necessary tools to navigate the complexities of real-world professional scenarios [7, 8]. Teaching in physiotherapy requires practical engagement with patients to develop professional competencies. While online instruction and simulation can facilitate certain practical skills, they cannot fully substitute direct patient interaction [1, 9]. Therefore, it is essential to resort to active and dynamic methodologies so that the student is the architect of their knowledge and skills development.
This study addresses the different didactic and methodological strategies of a practical and dynamic nature developed in physiotherapy and distributed in 7 thematic blocks. Based on socioconstructivist principles [5], the students' active and collaborative participation takes precedence. They reject rote memorization in favor of developing creativity, critical reflection, and problem-solving skills. Among these methodologies is clinical case resolution, which facilitates skill development, critical thinking, synthesis, and inference-making, preparing students to tackle academic and clinical challenges [3].
In the second order, we consider simulation-based learning, which reproduces real clinical experiences through simulated scenarios, creating a safe environment conducive to enhancing the learners' technical skills and cognitive processes, including information analysis, clinical decision-making, self-efficacy, communication skills, and multidisciplinary development [10, 11]. Moreover, this approach improves professional behavioral competencies, communication, patient assessment, therapeutic analysis and design, intervention, evidence-based practice, and risk management compared to traditional methods [12].
Third, problem-based learning promotes active learning through problem-solving. It is initiated by presenting problems for the students to solve. By investigating potential solution alternatives, students acquire new knowledge that is gradually integrated into their cognitive frameworks, preparing them to address real-life professional challenges [13]. For this reason, PBL contributes to autonomous learning, teamwork, interpersonal skills, and the promotion of values and attitudes [7]. Case-based learning or case studies analysis facilitates learning through dissecting real or simulated cases. It involves interpreting the case, formulating hypotheses, investigating information and data, their comparison to test hypotheses, and proposing possible alternative solutions [7, 14, 15]. Project-based learning empowers students, overcoming their positions as passive recipients of content the teacher develops in the classroom. Through project execution, the learner engages in inquiry processes to resolve identified problems, necessitating acquiring knowledge and skills for planning, designing, organizing, and implementing activities and tasks while gaining new insights [7, 15].
In the fourth order, team-based learning seeks to achieve significant learning for students through collaborative work. Students are organized into teams committed to achieving predefined objectives, where each member holds responsibility for their learning and that of their peers [16-17]. This requires implementing case analysis, group discussion, scientific article review, group and individual assignments, audiovisual materials, participation in forums, and role-playing activities [18].
Fifth, the Inverted Classroom is a model that disrupts the sequence of a traditional class. It requires prior preparation of students through the study and investigation of data autonomously of the contents to be developed, which must be socialized before the class session using printed materials, audiovisual media, and ICT supportive activities. Subsequently, the activities are centered around applying the previously obtained knowledge [19-20].
Sixth, interprofessional education (IPE) positively impacts communication skills and cooperative work, as it facilitates the clinical application of theoretical knowledge [21]. IPE facilitates the development of professional values [22] and favors communication, leadership, patient-centered care, role clarification, teamwork, and conflict resolution [23].
Finally, we have service-learning (A+S), which is rooted in community action and involves applying knowledge and skills (such as communication, leadership, patient-centered care, role clarification, teamwork, and resolution of disagreements) to address [24]. It generates motivation to obtain new knowledge and skills while also contributing to developing civic values among students, such as a sense of community, solidarity, and civic responsibility [7].
This study aimed to explain how successful practices contribute to the teaching and learning of physiotherapy.
Information and Methods
This study used a literature review methodology involving a systematic process to minimize biases and random errors. Its objectives were to synthesize the most relevant recent scientific knowledge on a topic, seek high methodological standards in its development, incorporate primary or original studies on the same topic, and seek to consolidate current knowledge [25-26]. As an essential point, this study corresponds to a qualitative approach characterized by its capacity to comprehend unique realities that are difficult to understand through a singular perspective. It serves as an interdisciplinary and transdisciplinary field, employing methods that involve the interrelation between the researcher and the research subjects for data collection, analysis, and validation [27]. In this research, 80 articles were analyzed in the literature concerning successful practices contributing to the teaching and learning of physical therapy between 2014-2022. Following the conclusion of the information search, a validation and reliability assessment was conducted to ensure the suitability and relevance of the selected material to the research problem (Figure 1).
The references encompassed both national and international literature. To comprehensively explore the subject matter, multiple databases were utilized, including Scopus (n=10), SciELO (n=9), ResearchGate (n=2), Latindex (n=4), Google Scholar (n=4), Dialnet (n=4), ClinicalKey (n=2), Springer (n=2), DOAJ (n=2), Redalyc (n=2), ERIC (n=2), OJS (n=2), Elsevier (n=1), PubMed (n=1), IDUNN (n=1), and TORROSA (n=1). The search strategies used to compile the information were by author, subject, keywords, bibliographic references, search tricks, and Boolean operators such as AND and OR. Regarding the geographic scope of the selected research, they originate from different countries.

Figure 1. Prisma diagram
Findings
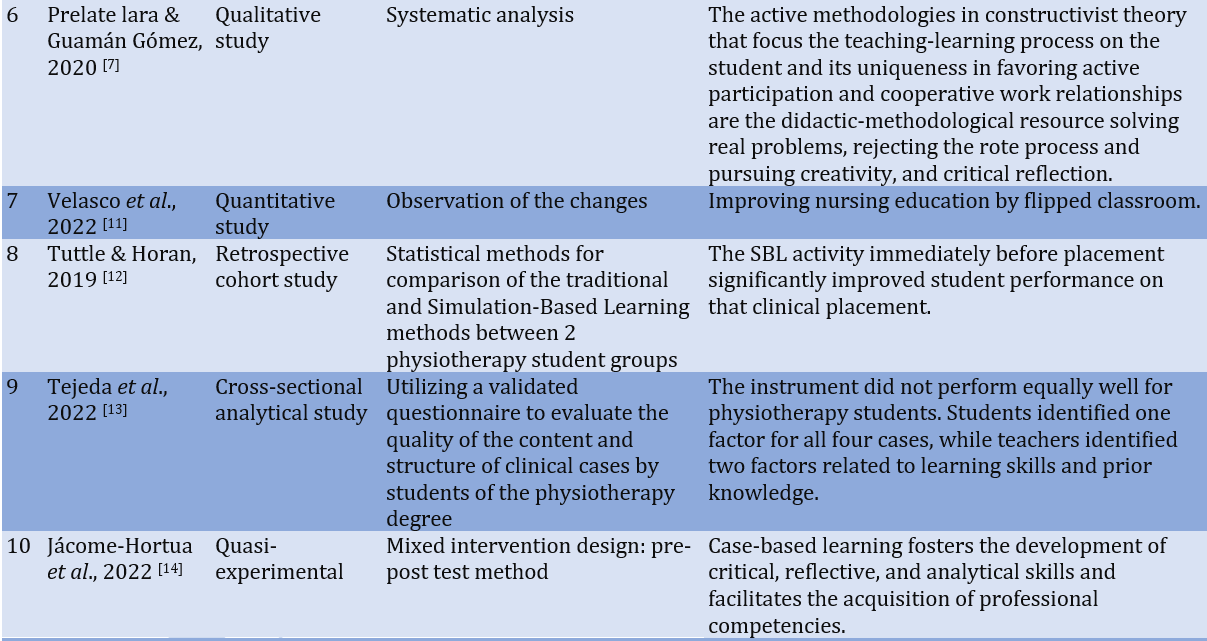
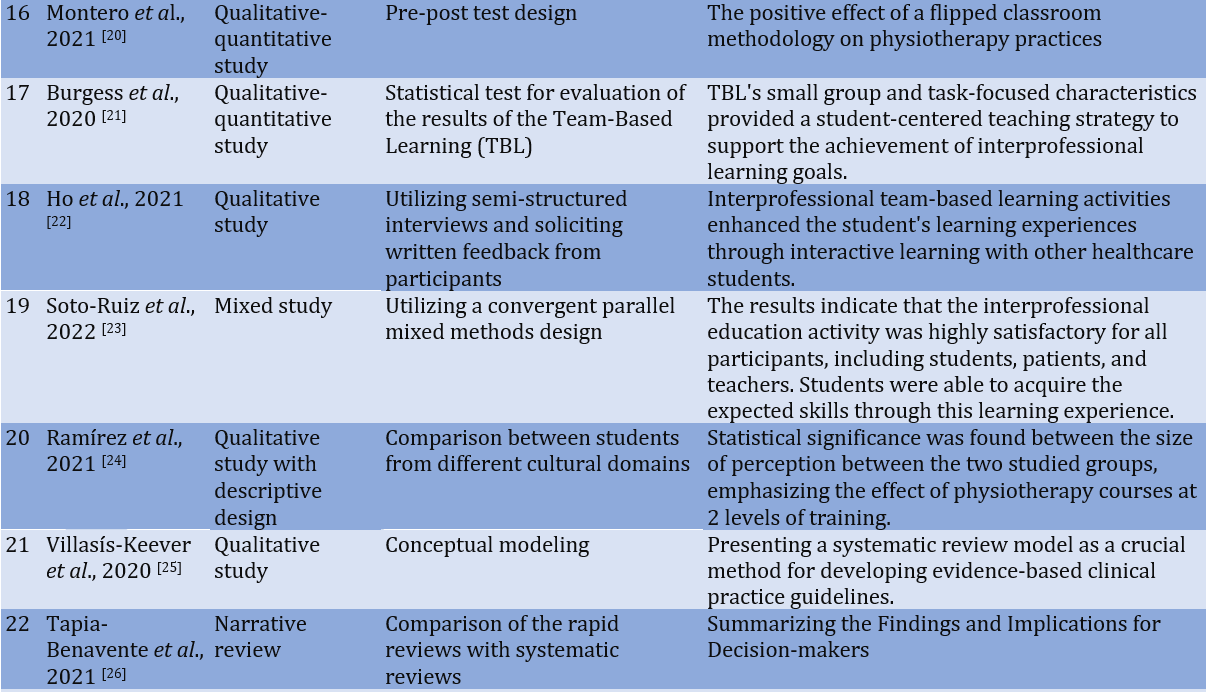
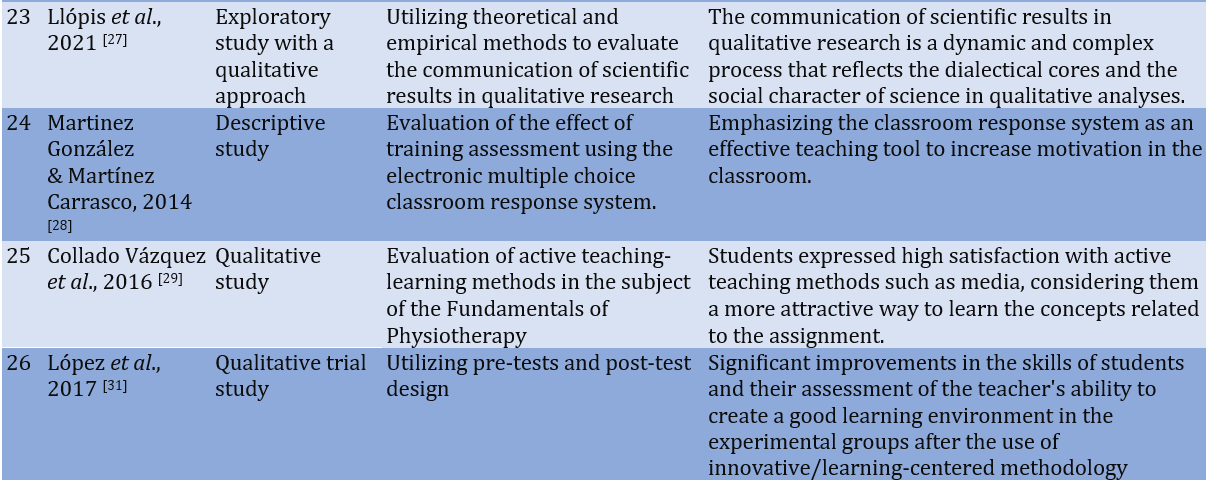
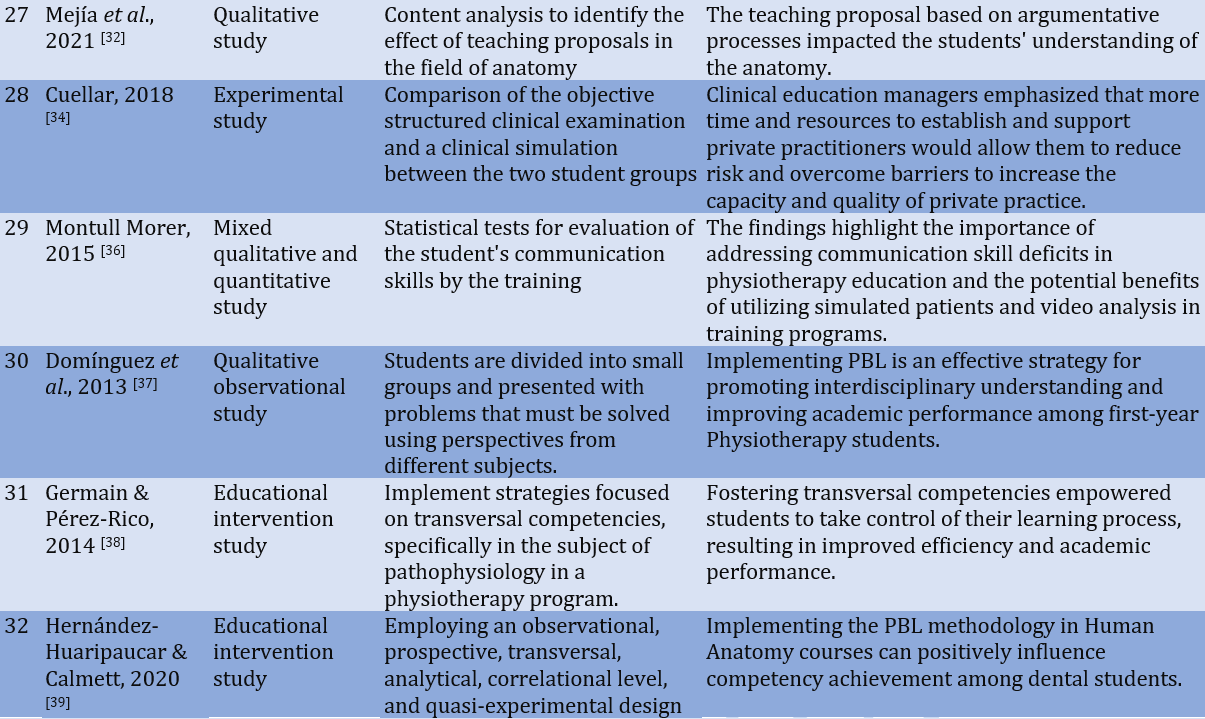
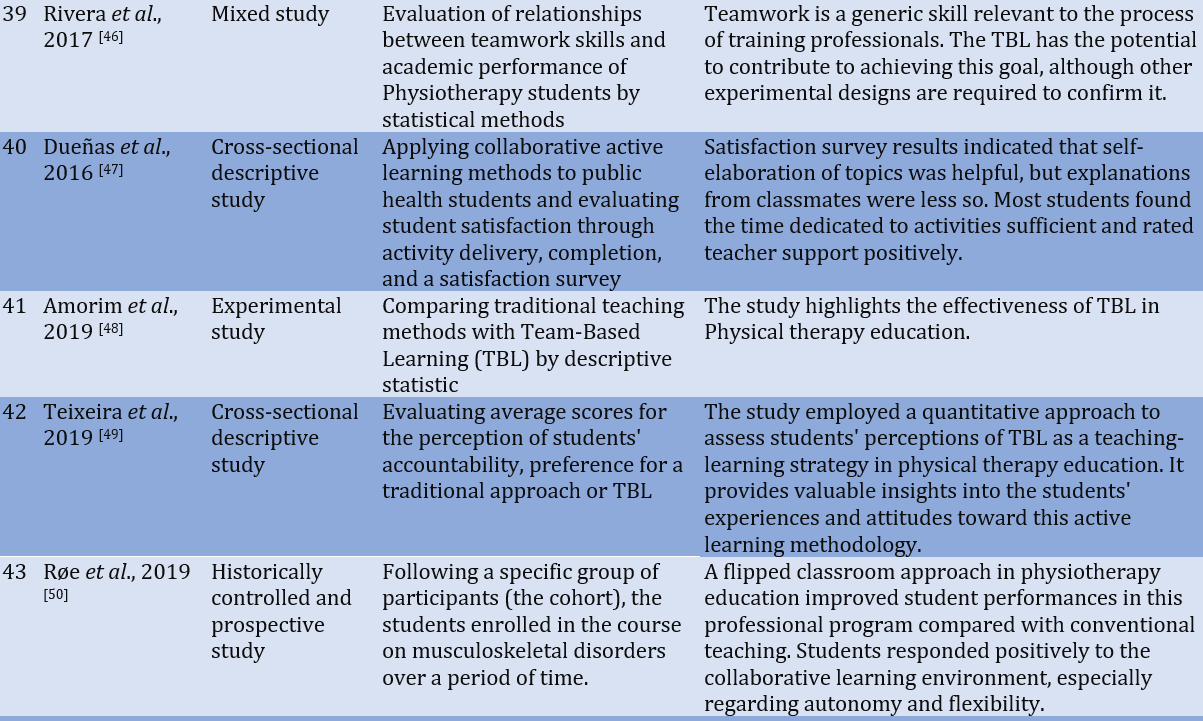
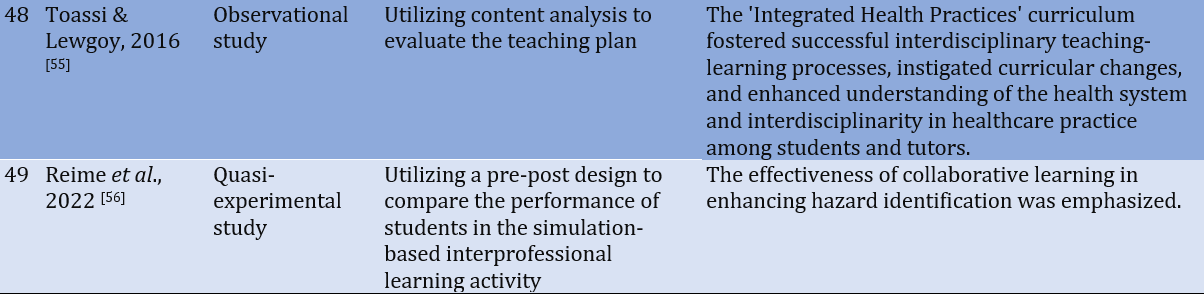
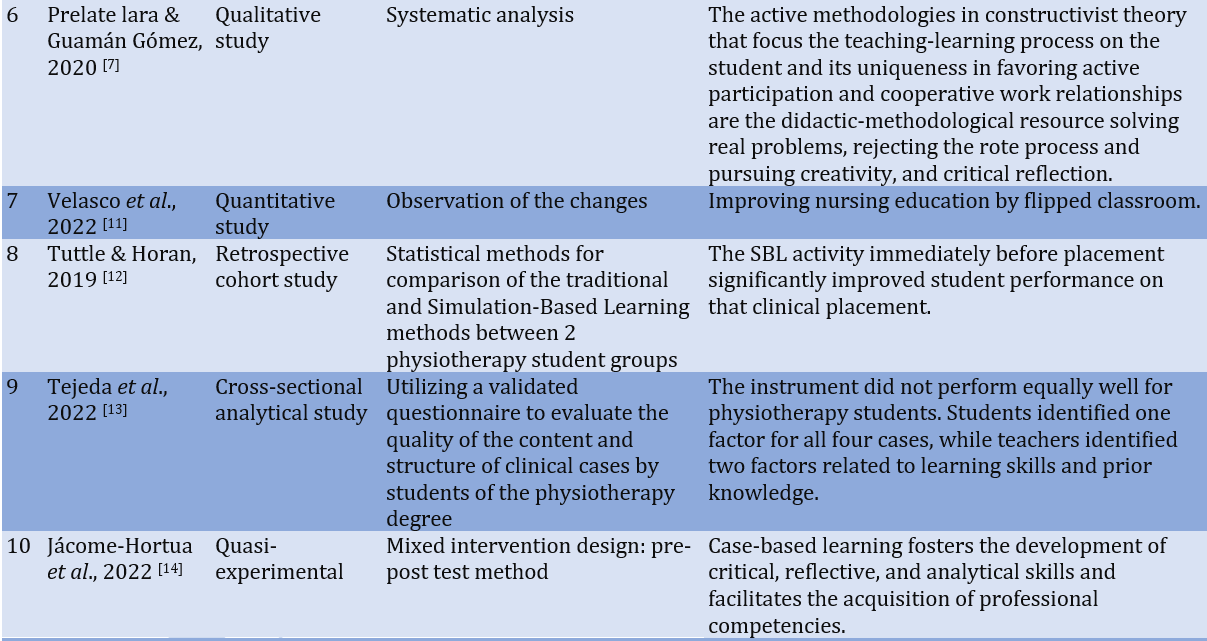
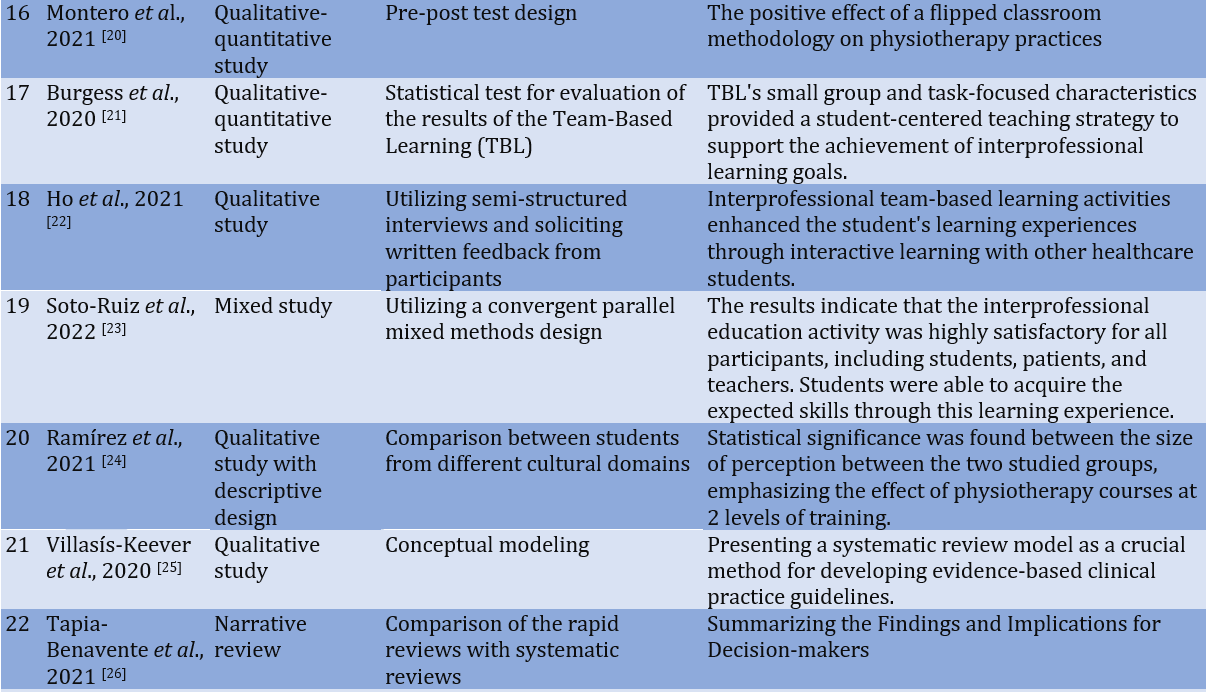
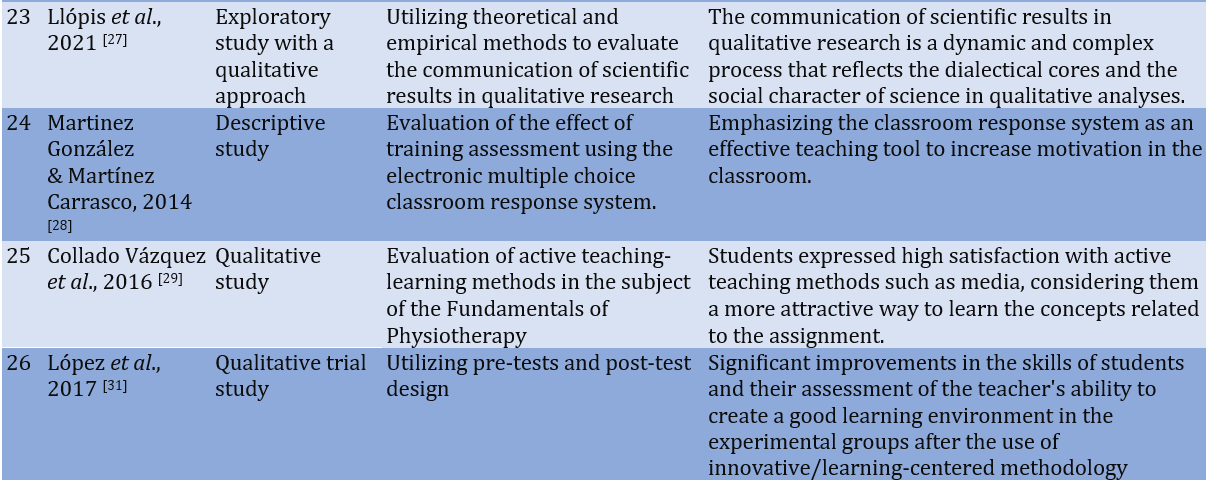
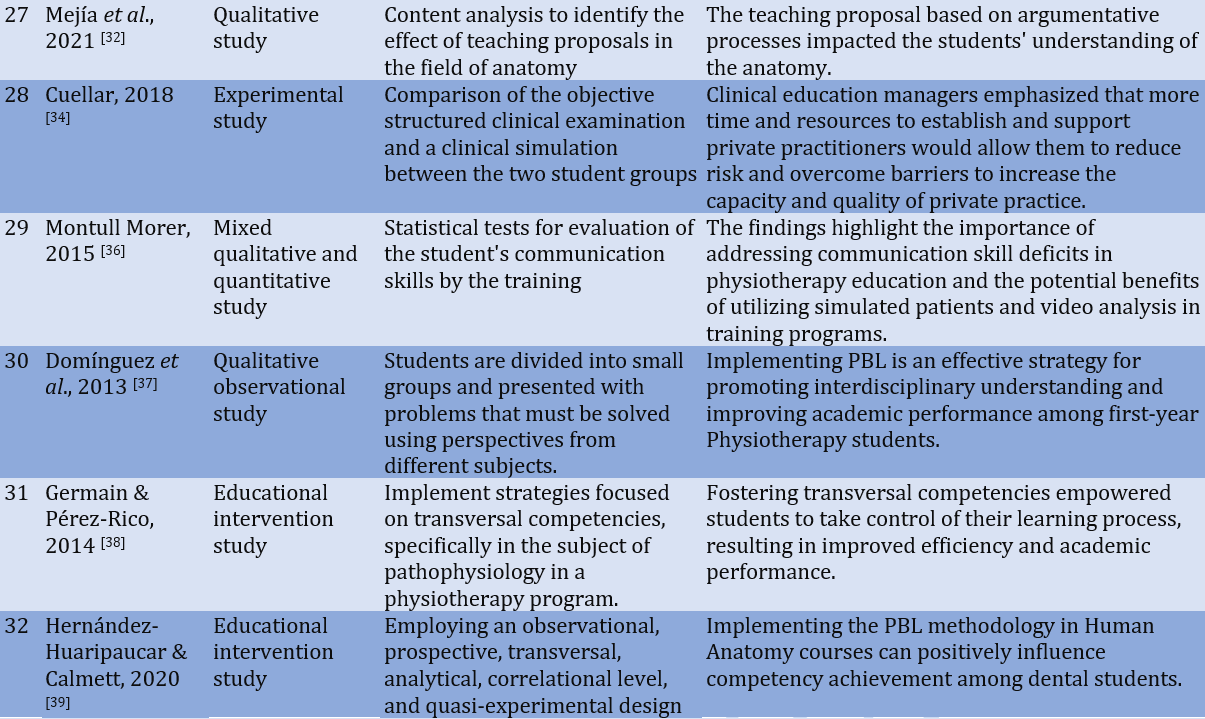
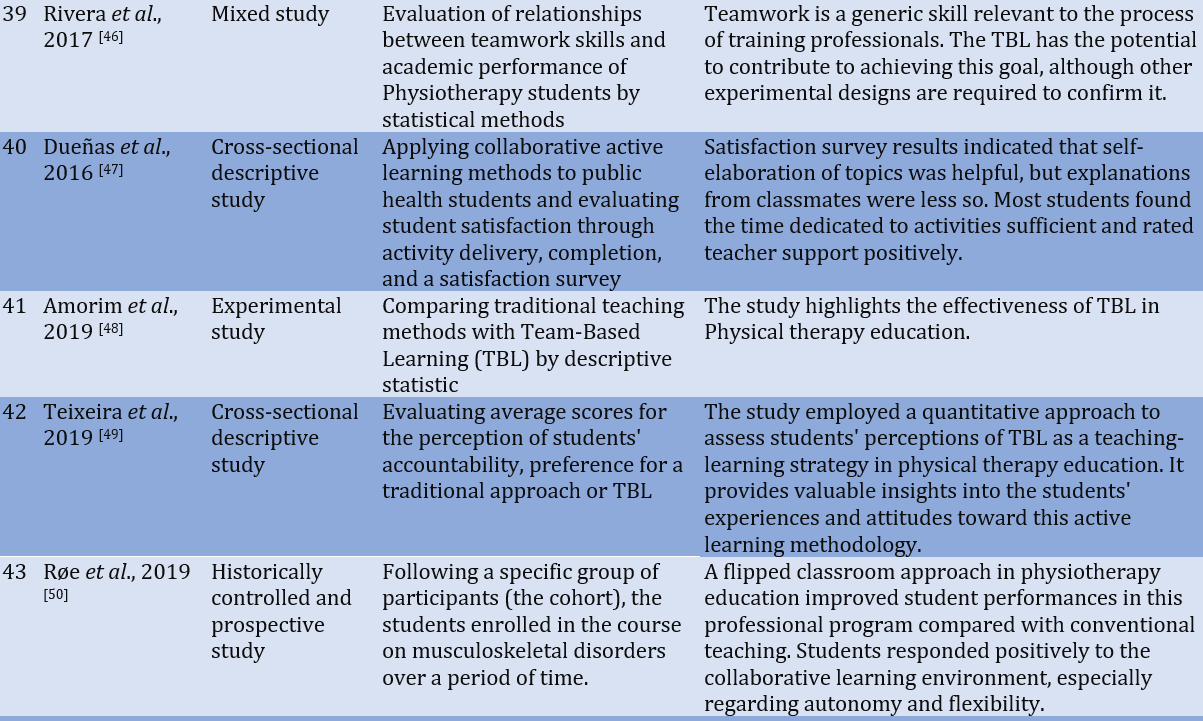
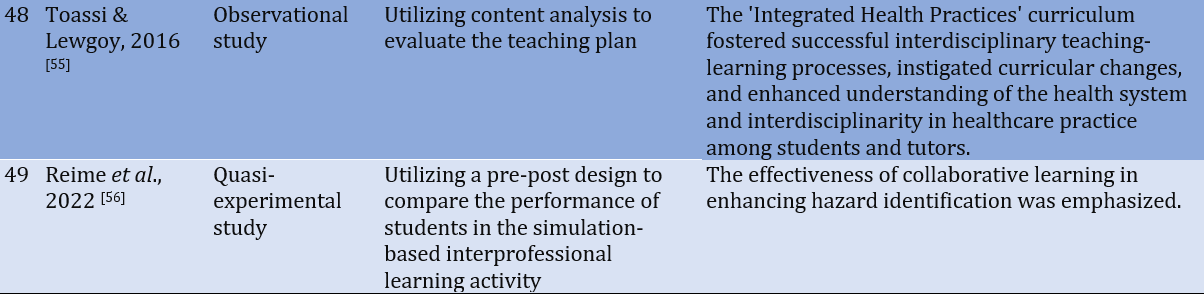
The analysis result of 49 documents were presented in Table 1.
Active methodologies
Learning is gaining knowledge through active engagement, participation, and collaborative interaction between learners and teachers. The subject matter to be learned, the context, teaching methodologies, educational environment, and assessment strategies collectively control the learning approach adopted by the learner [3]. Active methodologies prioritize the learner as an active participant in the teaching-learning process. This pedagogical conception is constructivist, as it involves constructing knowledge based on the student's experience [5]. Among them are resolving clinical cases, inverted classrooms, role-playing, service-learning, and peer tutoring [5]. Throughout the training process, several elements were identified as facilitators of learning, including encouraging dialogue in the classroom, incorporating active pauses for students, providing various tools (in addition to clinical cases), telling stories and different clinical experiences, utilizing imagery to generate emotions and facilitating the enjoyment for both students and teachers [5]. Physical therapy education requires implementing learning and teaching methods to foster skills, critical thinking processes, synthesis, and making inferences. Examining learning approaches is critical to preparing physical therapy educators to meet academic and clinical challenges [3]. There is a marked improvement in motivation, metacognition, context mastery, inquiry and choice, and learning strategies and approaches [28]. Learners who perceive classroom sessions as more interactive and dynamic and incorporate diverse strategies tend to have a more positive perception of their learning experience [16]. During the clinical years, teaching methods often involve clinical and community-based learning. This includes clinical-based learning with practice on patients in real situations to learn new skills. The basic knowledge acquired in the preclinical years is applied to medical conditions during the clinical years. In the clinical phase, more emphasis is placed on the problem-based learning method, which plays a pivotal role in developing deep learning. The deep learning process enhances critical thinking and promotes personal development among students.
Deep processing of knowledge and skills is essential in the clinical phase to formulate rational hypotheses and patient management plans [2-3]. Receiving timely feedback regarding learners' understanding of a particular topic equips them with tools. It fosters incremental learning of concepts, clarifying fundamental aspects essential for grasping corresponding practices and contributing to acquiring professional competencies in physical therapy [28]. During the clinical phase, teaching methods primarily encompass clinical and community-based learning. It includes case-based learning with practice on patients in real situations to learn new skills. There is a significant emphasis on the Problem-Based Learning Method, which primarily fosters deep learning. The deep learning process enhances critical thinking and personal development among learners through analytical observation, novel problem-solving, or teamwork. This deep processing of knowledge and skills is essential in the clinical phase, enabling students to formulate rational hypotheses and develop patient management plans [29-32, 3].
Simulation in physiotherapy
The simulation-based learning model aims to reproduce real clinical experiences through simulated scenarios by creating a safe environment that facilitates learners to increase technical skills and cognitive processes, also known as non-technical skills, including information analysis, clinical decision-making, self-efficacy, communication skills, and multidisciplinary development [10-11]. Studies have demonstrated that simulation improves professional behavioral competencies, communication, patient assessment, therapeutic analysis and design, intervention, evidence-based practice, and risk management compared to traditional methods [12]. Therefore, simulated practice in physiotherapy involves two phases: a planning phase and an execution phase. During these phases, physiotherapeutic care is provided, incorporating factors such as anamnesis, application of the test and measurements, explanation of the evaluation, physiotherapeutic diagnosis, prognosis, and treatment planning [33]. This approach enhances knowledge retention and skill acquisition compared to traditional methods.
Simulation practice has demonstrated its effectiveness in enhancing high-level skills across several areas, such as clinical skills, self-confidence, performance, safety, and decision-making during the professional reasoning process in clinical practice [11, 34-35].
Table 1. The research attributes of the studied articles




Problem-Based Learning
Problem-based learning (PBL) is a learner-centric method emphasizing autonomous learning and teamwork. It involves small groups of five to eight learners, facilitating effective conflict management. PBL enables the integration of different academic disciplines, requiring students to conduct research, combine theory and practice, devise practical solutions to a defined problem, and apply their knowledge and skills. It enables students to synthesize their learning into a cohesive whole [36, 38-40]. PBL helps students to acquire basic knowledge and essential competencies for their professional practice. It fosters the development of analytical and synthetic skills, encourages self-critique and critical evaluation of peers, and enhances oral and written communication abilities [37]. The transversal competencies are identical to different disciplines, including teamwork, communication, leadership, interdisciplinary environment, self-directed learning, lifelong learning, professional growth, and social responsibility [38]. PBL facilitates reflection, research, and group discussion around a problematic situation the teacher-tutor presents. Rather than simply transmitting knowledge, the teacher-tutor encourages learning. The teacher does not seek to solve problems but, on the contrary, uses them to determine learning goals [39]. Applied to physiotherapy, PBL facilitates the acquisition of skills necessary for conducting a comprehensive functional diagnosis, selecting appropriate treatment, engaging in effective peer discussion, promoting metacognition, and taking ownership of learning. Clinical cases utilized in PBL should be open-ended, with difficulty tailored to the student's proficiency, fostering active participation in their learning process [13]. Organizing debates and discussions as part of the learning process strengthens communication skills, promotes knowledge exchange, and facilitates the use of professional vocabulary. A shared language is a powerful tool that facilitates the assimilation of the disciplines addressed and develops the objectives of essential professional knowledge [38, 13]. This innovative methodology enhances skills and strengths, aiding in the reconstruction of the scientific method. Since the students are responsible for their learning process, they demonstrate greater involvement and commitment [41]. For its effective application, it is essential to analyze the context of the problem, brainstorm solutions, make a list of known information and what is needed, solve and define the problem, and finally obtain information [39]. The objectives of PBL in health sciences are to foster reasoning, problem-solving skills, self-directed learning, communication skills, and an in-depth understanding of the concepts. Principles in the curriculum create a more positive attitude among students and improve metacognitive awareness and critical thinking skills compared to lecture-based methods [40-41]. Creating conditions allowing trial and error is essential since reflecting on mistakes often leads to the most profound learning experiences. By empowering learners to take ownership of their learning and structure their knowledge, PBL fosters depth, impact, and lasting understanding [38]. PBL generates positive values, appreciation, and affective moods. It positively influences the achievement of attitudinal competencies [39]. PBL is a pedagogical practice conducive to fostering a more human and critical formation, particularly when implemented as an active teaching method per established guidelines outlined in the literature [43]. The teacher-student relationship within PBL should balance the necessary closeness to build trust and provide mentorship while maintaining appropriate distance to prevent psychological dynamics [38]. Including clinical cases as an educational tool in physical therapy has yielded numerous benefits such as improvements in patient assessment, greater capacity for comprehensive functional diagnosis, goal setting, and choice of appropriate treatment. In addition, utilizing clinical cases improves communication skills and fosters critical thinking, which encompasses self-regulated reflection on emotions, knowledge, behaviors, and the environment in which the individual develops. This reflective process involves skills such as analysis, inference, evaluation, and evidence-based practice. Additionally, clinical cases promote clinical judgment through students' critical reflection; all focused on problem-solving. These various aspects converge to promoting clinical reasoning, improving behavior and teamwork, acquiring clinical skills, and achieving better patient results [13, 42]. It allows students to interpret data and design strategies to be applied in their professional practice [13].
Collaborative or Team-Based Learning
Team-based learning (TBL) is a versatile teaching method based on the socio-constructivist and learner-centered paradigms. Originating in the United States, Larry Michaelsen introduced TBL as an innovative departure from conventional teaching methodologies [21]. It cultivates a collaborative atmosphere aimed at realizing objectives designed by team members alongside educational objectives promoted by the teacher. Despite the integration of technological tools, ABE focuses more on learning contents and concepts, often manifesting in problem-solving scenarios mirroring real-world or daily life challenges [17]. It has been shown to promote significant student learning outcomes, engendering a highlighted active attitude [44]. This is favored in correspondence to the execution of case analysis, group discussion, review of scientific articles, group, and individual papers, use of audiovisual material, participation in forums, and role-playing [18]. Critical thinking plays a pivotal role in structuring reasoned experiences and critically analyzing the cases situated within authentic contexts based on scientific principles [45]. Rivera et al. [46] revealed that groups outperformed individuals, enhanced the integration of skills, and had a high level of group cohesion. Collaborative endeavors foster the sharing of information, knowledge, and solutions. Thereby promoting collaborative relationships among students. This collaborative dynamic fosters a strong peer commitment, favoring mutual learning [47]. The TBL approach catalyzes increased student engagement, encouraging active participation in pre-class reading during lessons. The preparation phase enables teachers to address and focus on learning gaps, while teamwork promotes peer interaction and active participation [48]. Teachers must possess skills such as learning team activities, inspiring discussions within and outside the team, and specializing in the role of the facilitator. They should also provide continuous and timely feedback, focusing on designing team application exercises, modeling collaborative teaching, and facilitating the clinical application of theoretical knowledge [21, 44]. The cultivation of autonomy, critical thinking, and solidarity are encouraged in constructing knowledge and fostering ongoing dialogue among group members.
Inverted classroom
The inverted classroom model represents a pedagogical strategy that redefines the learning processes by shifting a portion of the learning activities outside the classroom. During class sessions, the focus is on leveraging teaching expertise to facilitate and enhance various knowledge acquisition and practical application processes. The transformation of the classroom environment aims to create an interactive and dynamic learning space in which the teacher guides students through practical exercises using questioning techniques and case studies to encourage the inquiry and application of ideas through pre-class video materials. This approach promotes creative participation in the course content [19, 20]. The application of the inverted classroom pedagogical model has been shown to enhance academic performance by providing students with contextualized learning experiences aligned with the demands of their future professions [50]. Therefore, it is essential to integrate healthcare practices based on user-centered clinical reasoning within the context of the prevailing health model. Likewise, these teaching-learning strategies facilitate the development of student autonomy, communication skills, and ethical and humanistic responsibility [51]. In this regard, the flipped classroom approach aims to contextualize the students for the challenges they will face in their future careers. Its influence on learning patterns and techniques of the Proprioceptive Neuromuscular Facilitation-PNF concept supported by short video clips is similar to the traditional methods [51]. It also improves the quality of students' work [50]. Utilizing concise video lectures watched outside the classroom liberates more in-class time for active learning, offering the advantage of easy availability and repeated viewings, considering that students' learning speed may vary [51, 52].
Interprofessional Learning
Interprofessional education (IPE) and collaborative practice can play a pivotal role in moderating various challenges facing healthcare systems worldwide. These initiatives generate greater coordination and continuity of patient care, increase patient satisfaction, and promote collaborative decision-making processes. IPE positively impacts communication skills and cooperative work, facilitating the translation of theoretical knowledge into clinical practice. It provides an important platform for undergraduate students to explore and develop their professional values [22], gaining knowledge and competencies (communication, leadership, patient-centered care, role clarification, teamwork, and disagreement resolution) for teamwork with active patient participation [23]. Team efforts consistently outperform individual efforts. Both current and past attendance is important to team performance, consistent with an IPE program where subsequent sessions build on and extend content presented in previous ones [53]. Students valued their interactions with other students from different professional backgrounds, citing the opportunity to problem solve, receive peer support, and gain insights from various perspectives on patient cases [21-22]. Ideally, IPE should begin early in the trainee's professional career [23]. Most new physical therapy graduates demonstrate confidence in communicating with professionals from diverse backgrounds and understanding their roles, but they often exhibit low self-efficacy levels when faced with interprofessional conflict resolution and when providing feedback to peers [54]. It is recommended that future curricula incorporate IPE to familiarize students with communication, role recognition, and conflict resolution before professional practice [54]. Learning is not a natural or spontaneous process; it requires intentionality, planning, and methodological rigor [55]. The interdisciplinary dialogue within healthcare professions fosters innovative pedagogical practices among teachers. Students appreciate the diversity of professional backgrounds and knowledge among their peers. Their awareness drives students to actively seek out and acquire specific knowledge from disciplines they have not yet encountered [22]. In this perspective, students and faculty collaborate to develop integrated products each semester, which materialize from the partnership established with the unit's Health Team [55].
Service Learning Training Practice
Formative Practice (FP) is where the students link the knowledge, abilities, and skills obtained in the elementary level of training with the experiences acquired in practice through the different areas of professional training [24]. It is focused on facilitating learning and enhancing professional competencies, where practical aspects are prepared using techniques that effectively connect theory with practice, thereby becoming a crucial component of professional development. The evaluation of the Practicum emphasizes the assessment of the practical phase, integrating considerations of both human and ethical competencies [39]. Among the essential qualities assuming responsibility, demonstrating a commitment to actions and patients, and possessing requisite prior knowledge they must possess to begin the practicum. As well as the learning that they gradually develop with the accompaniment of their tutors [24]. These attributes are parts of the transversal competencies stipulated for physical therapists by the professional community. Rooted in professionalism and ethics, these competencies aim to cultivate autonomy and self-regulation in the exercise of practice and professional knowledge. They are aligned with globally recognized ethical, political, and techno-scientific principles, which are socially legitimized and respected by the professional collective [7]. The most prominent feelings experienced by the students are happiness at the beginning of a new stage and the satisfaction of accomplishing their goals; however, they also grapple with anxiety stemming from facing the unknown, such as interacting with patients [24]. The active involvement of practical professionals in facilitating learning is a significant motivator for students and increases the consolidation of their knowledge, fostering greater transferability of learning outcomes [39]. Increasing practical training opportunities for students in the early stages of their education is crucial. This enables a more concrete approach to the situations they will encounter during their training, thereby helping them develop the skills necessary to navigate the challenges of practice. By providing concrete early on, students can better manage the anxiety and insecurity often associated with practical training. Focusing on early practical experiences ensures that students' aspirations are directed toward the learning process, fostering a more positive and productive educational journey [24]. Service-learning allows students to practice the skills and techniques they've learned in the classroom within a real or practical environment. The results were obtained professionally and personally, and the participating patients were rewarded for the work done [57]. The efficiency of the teaching-learning process has been underscored, with online training emerging as a valuable tool for addressing training gaps and acquiring new knowledge within the context of training practice or service learning. The proposal in the e-learning modality allows updating the content, modernizing the presentation of the materials, proximity and permanent interaction of the teacher in the student's learning, and the freedom and active contribution to the final result of the training on the part of the learners. The transversal formative aspects make e-learning systems viable instructional tools across diverse clinical or professional areas of physical therapy [58]. The learning contract has been found to facilitate the development of high-quality learning since it promotes autonomy and enables students to take control of their learning, which is fundamental in their future professional practice. This approach aims to enhance students' motivation to learn and facilitates the integration of theory into practice. It supports the development of skills such as thinking and communicating or solving problems, leading to more meaningful learning for the student. The effort involved in implementing the learning contract in terms of time consumption promotes the active participation of students in their learning. It is important to encourage future physical therapists to increase their skills by developing autonomous learning throughout their professional lives [35].
Practices within public services must adopt a comprehensive care approach, which includes health promotion and injury prevention strategies [59]. By integrating undergraduate students into primary healthcare settings, they become agents capable of effecting real-world change. Their presence and collaboration in care interventions enhance the quality of healthcare delivery, contributing to the training of professionals who are cognisant of social realities and equipped with the skills necessary for health promotion, health education, and injury prevention. This collaborative approach improves the service delivery process and enhances student training, ultimately leading to better health outcomes for the population being served. It helps to mitigate the inherent characteristics of the biomedical model of care, fostering a more holistic and patient-centered approach to healthcare [7].
Integrating students into healthcare services has been recognized as a transformative element in professional practices, particularly due to the opportunity for collaborative discussion among teachers, students, and professionals regarding shared actions and interventions. The insertion of formative processes that articulate learning with practice in the different disciplinary fields will change the training of physical therapists, guiding them to expand their understanding of the demands and complexity of work in the single health system (SUS) [59].
Discussion
Based on the findings, the implementation of active methodologies in education has shown significant improvements in various abilities, including autonomous, self-managed, and self-regulated learning, as well as problem-solving and communicative skills. The semiological model favors the integration of knowledge interrelated with clinical evaluation and allows stimulating the student's thinking to models that relate structure and function. This approach stimulates critical thinking and deepens understanding of the topics under study, enabling students to grasp complex concepts more thoroughly. The teacher's ability to establish an enriched and constructive learning environment, providing guidance for understanding, offering feedback to support learning, evaluation, teacher-discussant relationship, relationship between learners, ensuring curriculum coherence, and employing methods focused on student learning and empowerment of their autonomy and self-regulation are highly appreciated [31, 2]. Six explanatory models are recognized for the didactics of anatomy to elucidate the anatomical concept, including structural, functional, semiological, integrative, pseudo-integrative, and heterogeneous. Personal constructions can be based on the interrelationships between the students and their academic, social, and cultural environment. The anatomical segment studied is a concept that must link structure and function, integrated into teaching to reduce the risk of seeing a body structure isolated from its impact on the organism's function. The semiological model indicates knowledge integration is closely related to clinical evaluation. It allows educators and students to discuss the broader implications and functional interpretations of symptoms manifested in medical situations.
The significance of the intervention lies in its ability to encourage students to transition from fragmented models of thinking to ones that aim to establish meaningful relationships between structure and function. This transition is crucial for comprehensively understanding the phenomenon under study [32].
Simulation in physical therapy has proven to improve professional behavioral competencies, such as communication, patient assessment, therapeutic analysis and design, intervention techniques, evidence-based practice, and risk management. Through simulation practice, students demonstrate increased clinical skills, self-confidence, and proficiency in performance and safety protocols. Moreover, it has been observed to enhance decision-making abilities during the professional reasoning process in clinical practice, improving learning outcomes and efficiency in multidisciplinary work. Simulation-based education provides a controlled and safe modulated learning environment for learners to learn and generate these skills before encountering real patients, where the consequences of their performance are crucial in medical practice [11]. Utilizing video and simulated patients offers diverse applications, including employing simulated patient instructors who can assume both patient and instructor roles while providing student feedback within a controlled environment. Video observation or analysis is a practical and current tool for assessing tasks in health simulation environments, facilitating the evaluation of clinical interviews [35]. This approach enables the analysis of clinical skill management and capitalizes on feedback while reviewing video recordings of interviews provided by both students and instructors, thereby enhancing session effectiveness [36]. Another way is technique demonstration and role reversal. However, this method overlooks a way of teaching a profession without considering the experience lived by the participants immersed in the training process [33]. Simulation-based models improve learning and clinical practice outcomes, clinical decision-making, and efficiency in multidisciplinary work [10].
Problem-based learning helps students acquire basic knowledge and skills that are essential for their professional practice. It guides them in developing their capacity for analysis and synthesis, fostering critical thinking in self-assessment and evaluating their peers. Additionally, PBL enhances oral and written communication skills. When applied to physical therapy, PBL facilitates the development of skills necessary for establishing a comprehensive functional diagnosis, selecting appropriate treatment strategies, and engaging in effective peer discussions. Furthermore, it promotes metacognition and facilitates knowledge acquisition. Project-based Learning (ABPro), which is applied in physical therapy education, offers numerous benefits for students. It enhances creativity, teamwork, autonomy, assertive communication, and recognition of population needs. Moreover, it encourages students to inquire about strategies and plan approaches often utilizing ICT, favors the development of clinical reasoning competence on spinal pain, and is a positive experience that favors the development of academic content and obtaining learning skills [15]. Students find this method to be a positive experience for creating digital material focused on preventing musculoskeletal complications, promoting healthy habits, and providing guidance on proper postural hygiene [7, 15]. PBL, applied in the classroom, leads students to effectively address real problems and formulate proposals to overcome what has been observed, leading to the construction of solutions to problems based on the student's real life to activate prior knowledge and simultaneously motivate a dialogue that considers critically assessing the options in the students through research and analysis processes [42]. PBL and ABPro are closely linked to each other and other methods [39]. Case-Based Learning (ABC) is a pedagogical method that encourages the discovery of new knowledge by facilitating interconnection between current and previous knowledge and develops autonomy, critical thinking, and argumentative skills in real situations. Students find this experiential approach highly motivating, and educators consider it enriching. It promotes critical, reflective, and analytical skills and attaining professional competencies. It positively influences the attainment of communicative, procedural, and attitudinal competencies and reinforces previously learned knowledge [7, 14].
Team-based learning fosters significant learning among students by cultivating a more active learning attitude. It facilitates the development of critical thinking skills, enabling students to structure reasoned experiences and critically analyze cases within real-world contexts based on scientific principles. This method also demonstrates a better-improved group performance compared to individual efforts. Moreover, it encourages collaborative relationships by promoting the sharing of information, knowledge, and solutions among team members. This approach stimulates reasoned, cooperative, and conclusive reflection on the proposed common therapeutic process [45]. The learners perceive this method as more enjoyable [49]. ABE has three phases: preparation, Assurance Testing (IRAT) followed by Team Readiness Assurance Testing (TRAT), and group review aimed at knowledge sharing. Instructors provide feedback geared towards leveraging collaborative learning to bolster students' problem-solving abilities. Finally, the teams apply the acquired knowledge to solve real-world problems or case studies [17]. Flipped classroom teaching has been shown to have the potential to refine higher-order thinking skills and promote self-regulated learning among students [51]. A critical success factor for these learning approaches is the preparation of students before class attendance and collaborative learning within the classroom, both of which are integral components of the flipped classroom model [51]. Although the flipped classroom model does not provide instructions regarding learning activities, it represents an opportunity to implement higher-order learning skills in teaching and improve clinical competencies among healthcare students [51]. This approach gives students a well-planned, flexible, and consistent learning process.
Applying the inverted classroom pedagogical model has enhanced academic performance by enabling students to contextualize their future professional roles. It is essential to include it in healthcare practice based on user-centered clinical practice within the context of the healthcare model. It also facilitates the development of student autonomy, communication skills, and the humanistic acceptance of technological advances. By transforming students into active learners, it fosters the cultivation of analytical, synthesis, and evaluative capacities. Applying this method in gait analysis outperforms the effectiveness of the traditional teaching method [52]. The inverted classroom model cultivates active learners by developing their capacity for analysis, synthesis, and evaluation [52]. The passive learning of the flipped classroom occurs during video lectures outside of class, optimizing in-class time for active learning [52]. Students' limited attention spans are effectively counteracted through interactive learning and group exercise [52].
Sixthly, interprofessional learning positively impacts communication skills and cooperative work by facilitating the clinical application of theoretical knowledge and teamwork skills. Through active patient involvement, IPL enhances competencies such as communication, leadership, patient-centered care, clarification of roles, teamwork, and conflict resolution. Through IPL, students acquire a comprehensive understanding of interdisciplinary collaboration, preparing them to engage in interprofessional healthcare environments effectively. The opportunity for students to interact with peers from diverse academic backgrounds promotes a deeper understanding of each team member's role and their unique contributions to patient care. This interaction also plays a pivotal role in shaping students' professional identities, which serve as the central and overarching axis in various educational models and programs [23]. Students develop confidence in their knowledge and communication skills through interprofessional team-based learning in trusting and complementary relationships. They explore their specific roles, understand their professional limitations, and equip themselves to be more competent in working collaboratively in patient care and improving patient outcomes [22]. Working in interprofessional teams enhances the identification of hospital risks, as this expands participants' observational, critical thinking, and situational awareness skills [56].
Through the application of formative practice or service learning, students articulate the knowledge, skills, and abilities acquired during the basic level of training, using the experiences developed in clinical settings. This approach enables students to practice the skills and techniques in a real-world environment, fostering autonomy and control over their learning. It enhances their motivation to learn and develops critical thinking, communication, problem-solving, and more meaningful learning skills. During the search process, relevant sources were found related to methodologies that stimulate the development of clinical reasoning; however, only three sources were found, which were insufficient to structure a thematic block. We hope that future research will address this important skill with greater emphasis, which is fundamental for students to understand complex clinical cases in their future professional practice. Professional training in physiotherapy needs to enhance interdisciplinary and multi-professional practices during graduation. This entails providing students with opportunities to engage in interventions across different teaching-learning scenarios involving students from different academic backgrounds. Through these experiences, students gain insights into the roles and contributions of different disciplines within the professional team. By experimenting with and reflecting on interdisciplinary collaboration during their undergraduate education, students develop a deeper understanding of healthcare practices that extend beyond biotechnological and physiotherapeutic knowledge. This critical analysis of their training journey fosters a broader perspective on the role of physiotherapy professionals within the healthcare system [7, 59].
Conclusion
Using multiple active learner-centered strategies in physical therapy education significantly contributes to developing autonomous learning, clinical reasoning, collaborative work, and critical thinking among students. These strategies also foster the development of communication and problem-solving skills, equipping students to tackle challenges in their professional futures.
Acknowledgments: None declared by the authors.
Ethical Permissions: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Authors’ Contribution: Rojas JG (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Fuster-Guillén D (Second Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Flores JRC (Third Author), Methodologist/Statistical Analyst/Assistant Researcher (20%); Hernández RM (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (20%)
Funding/Support: None declared by the authors.
This study is focused on identifying successful practices in the teaching-learning of physiotherapy. The practices integral to professional training transcend mere theoretical knowledge and content delivery. They serve as conduits for bridging theory with practice, enabling students to concretely apply competencies, skills, and abilities in real-world scenarios. Students gain firsthand experience in the complexities of patient care, honing their conceptual, methodological, and ethical acumen by engaging in these practices [1, 2]. Active methodologies focused on the learner take precedence over traditional content-centric approaches, challenging long-standing orthodox teaching paradigms in physiotherapy education. This shift redefines the role of the teacher as a mediator, facilitator, and guide, fostering active engagement, collaborative interactions, creativity, critical thinking, and reflective practice. The didactic strategies are tailored to address real-world challenges, encouraging problem-solving and application-oriented learning [3-5]. This approach aligns with a constructivist point of view wherein the learning and evaluation process is viewed as dynamic and contextually situated [6, 7]. Multiple studies have left evidence of implementing such practices.
The advancement of science is in permanent transformation every day, demanding methods that empower students to develop abilities that allow autonomous learning and critical and reflective thinking. However, higher education systems in health disciplines, especially physiotherapy, are still dominated by traditional teacher-centric approaches. These methods typically entail one-way content delivery and rote memorization, relegating students to passive receivers. Therefore, such methodologies fail to equip learners with the necessary tools to navigate the complexities of real-world professional scenarios [7, 8]. Teaching in physiotherapy requires practical engagement with patients to develop professional competencies. While online instruction and simulation can facilitate certain practical skills, they cannot fully substitute direct patient interaction [1, 9]. Therefore, it is essential to resort to active and dynamic methodologies so that the student is the architect of their knowledge and skills development.
This study addresses the different didactic and methodological strategies of a practical and dynamic nature developed in physiotherapy and distributed in 7 thematic blocks. Based on socioconstructivist principles [5], the students' active and collaborative participation takes precedence. They reject rote memorization in favor of developing creativity, critical reflection, and problem-solving skills. Among these methodologies is clinical case resolution, which facilitates skill development, critical thinking, synthesis, and inference-making, preparing students to tackle academic and clinical challenges [3].
In the second order, we consider simulation-based learning, which reproduces real clinical experiences through simulated scenarios, creating a safe environment conducive to enhancing the learners' technical skills and cognitive processes, including information analysis, clinical decision-making, self-efficacy, communication skills, and multidisciplinary development [10, 11]. Moreover, this approach improves professional behavioral competencies, communication, patient assessment, therapeutic analysis and design, intervention, evidence-based practice, and risk management compared to traditional methods [12].
Third, problem-based learning promotes active learning through problem-solving. It is initiated by presenting problems for the students to solve. By investigating potential solution alternatives, students acquire new knowledge that is gradually integrated into their cognitive frameworks, preparing them to address real-life professional challenges [13]. For this reason, PBL contributes to autonomous learning, teamwork, interpersonal skills, and the promotion of values and attitudes [7]. Case-based learning or case studies analysis facilitates learning through dissecting real or simulated cases. It involves interpreting the case, formulating hypotheses, investigating information and data, their comparison to test hypotheses, and proposing possible alternative solutions [7, 14, 15]. Project-based learning empowers students, overcoming their positions as passive recipients of content the teacher develops in the classroom. Through project execution, the learner engages in inquiry processes to resolve identified problems, necessitating acquiring knowledge and skills for planning, designing, organizing, and implementing activities and tasks while gaining new insights [7, 15].
In the fourth order, team-based learning seeks to achieve significant learning for students through collaborative work. Students are organized into teams committed to achieving predefined objectives, where each member holds responsibility for their learning and that of their peers [16-17]. This requires implementing case analysis, group discussion, scientific article review, group and individual assignments, audiovisual materials, participation in forums, and role-playing activities [18].
Fifth, the Inverted Classroom is a model that disrupts the sequence of a traditional class. It requires prior preparation of students through the study and investigation of data autonomously of the contents to be developed, which must be socialized before the class session using printed materials, audiovisual media, and ICT supportive activities. Subsequently, the activities are centered around applying the previously obtained knowledge [19-20].
Sixth, interprofessional education (IPE) positively impacts communication skills and cooperative work, as it facilitates the clinical application of theoretical knowledge [21]. IPE facilitates the development of professional values [22] and favors communication, leadership, patient-centered care, role clarification, teamwork, and conflict resolution [23].
Finally, we have service-learning (A+S), which is rooted in community action and involves applying knowledge and skills (such as communication, leadership, patient-centered care, role clarification, teamwork, and resolution of disagreements) to address [24]. It generates motivation to obtain new knowledge and skills while also contributing to developing civic values among students, such as a sense of community, solidarity, and civic responsibility [7].
This study aimed to explain how successful practices contribute to the teaching and learning of physiotherapy.
Information and Methods
This study used a literature review methodology involving a systematic process to minimize biases and random errors. Its objectives were to synthesize the most relevant recent scientific knowledge on a topic, seek high methodological standards in its development, incorporate primary or original studies on the same topic, and seek to consolidate current knowledge [25-26]. As an essential point, this study corresponds to a qualitative approach characterized by its capacity to comprehend unique realities that are difficult to understand through a singular perspective. It serves as an interdisciplinary and transdisciplinary field, employing methods that involve the interrelation between the researcher and the research subjects for data collection, analysis, and validation [27]. In this research, 80 articles were analyzed in the literature concerning successful practices contributing to the teaching and learning of physical therapy between 2014-2022. Following the conclusion of the information search, a validation and reliability assessment was conducted to ensure the suitability and relevance of the selected material to the research problem (Figure 1).
The references encompassed both national and international literature. To comprehensively explore the subject matter, multiple databases were utilized, including Scopus (n=10), SciELO (n=9), ResearchGate (n=2), Latindex (n=4), Google Scholar (n=4), Dialnet (n=4), ClinicalKey (n=2), Springer (n=2), DOAJ (n=2), Redalyc (n=2), ERIC (n=2), OJS (n=2), Elsevier (n=1), PubMed (n=1), IDUNN (n=1), and TORROSA (n=1). The search strategies used to compile the information were by author, subject, keywords, bibliographic references, search tricks, and Boolean operators such as AND and OR. Regarding the geographic scope of the selected research, they originate from different countries.

Figure 1. Prisma diagram
Findings
The analysis result of 49 documents were presented in Table 1.
Active methodologies
Learning is gaining knowledge through active engagement, participation, and collaborative interaction between learners and teachers. The subject matter to be learned, the context, teaching methodologies, educational environment, and assessment strategies collectively control the learning approach adopted by the learner [3]. Active methodologies prioritize the learner as an active participant in the teaching-learning process. This pedagogical conception is constructivist, as it involves constructing knowledge based on the student's experience [5]. Among them are resolving clinical cases, inverted classrooms, role-playing, service-learning, and peer tutoring [5]. Throughout the training process, several elements were identified as facilitators of learning, including encouraging dialogue in the classroom, incorporating active pauses for students, providing various tools (in addition to clinical cases), telling stories and different clinical experiences, utilizing imagery to generate emotions and facilitating the enjoyment for both students and teachers [5]. Physical therapy education requires implementing learning and teaching methods to foster skills, critical thinking processes, synthesis, and making inferences. Examining learning approaches is critical to preparing physical therapy educators to meet academic and clinical challenges [3]. There is a marked improvement in motivation, metacognition, context mastery, inquiry and choice, and learning strategies and approaches [28]. Learners who perceive classroom sessions as more interactive and dynamic and incorporate diverse strategies tend to have a more positive perception of their learning experience [16]. During the clinical years, teaching methods often involve clinical and community-based learning. This includes clinical-based learning with practice on patients in real situations to learn new skills. The basic knowledge acquired in the preclinical years is applied to medical conditions during the clinical years. In the clinical phase, more emphasis is placed on the problem-based learning method, which plays a pivotal role in developing deep learning. The deep learning process enhances critical thinking and promotes personal development among students.
Deep processing of knowledge and skills is essential in the clinical phase to formulate rational hypotheses and patient management plans [2-3]. Receiving timely feedback regarding learners' understanding of a particular topic equips them with tools. It fosters incremental learning of concepts, clarifying fundamental aspects essential for grasping corresponding practices and contributing to acquiring professional competencies in physical therapy [28]. During the clinical phase, teaching methods primarily encompass clinical and community-based learning. It includes case-based learning with practice on patients in real situations to learn new skills. There is a significant emphasis on the Problem-Based Learning Method, which primarily fosters deep learning. The deep learning process enhances critical thinking and personal development among learners through analytical observation, novel problem-solving, or teamwork. This deep processing of knowledge and skills is essential in the clinical phase, enabling students to formulate rational hypotheses and develop patient management plans [29-32, 3].
Simulation in physiotherapy
The simulation-based learning model aims to reproduce real clinical experiences through simulated scenarios by creating a safe environment that facilitates learners to increase technical skills and cognitive processes, also known as non-technical skills, including information analysis, clinical decision-making, self-efficacy, communication skills, and multidisciplinary development [10-11]. Studies have demonstrated that simulation improves professional behavioral competencies, communication, patient assessment, therapeutic analysis and design, intervention, evidence-based practice, and risk management compared to traditional methods [12]. Therefore, simulated practice in physiotherapy involves two phases: a planning phase and an execution phase. During these phases, physiotherapeutic care is provided, incorporating factors such as anamnesis, application of the test and measurements, explanation of the evaluation, physiotherapeutic diagnosis, prognosis, and treatment planning [33]. This approach enhances knowledge retention and skill acquisition compared to traditional methods.
Simulation practice has demonstrated its effectiveness in enhancing high-level skills across several areas, such as clinical skills, self-confidence, performance, safety, and decision-making during the professional reasoning process in clinical practice [11, 34-35].
Table 1. The research attributes of the studied articles




Problem-Based Learning
Problem-based learning (PBL) is a learner-centric method emphasizing autonomous learning and teamwork. It involves small groups of five to eight learners, facilitating effective conflict management. PBL enables the integration of different academic disciplines, requiring students to conduct research, combine theory and practice, devise practical solutions to a defined problem, and apply their knowledge and skills. It enables students to synthesize their learning into a cohesive whole [36, 38-40]. PBL helps students to acquire basic knowledge and essential competencies for their professional practice. It fosters the development of analytical and synthetic skills, encourages self-critique and critical evaluation of peers, and enhances oral and written communication abilities [37]. The transversal competencies are identical to different disciplines, including teamwork, communication, leadership, interdisciplinary environment, self-directed learning, lifelong learning, professional growth, and social responsibility [38]. PBL facilitates reflection, research, and group discussion around a problematic situation the teacher-tutor presents. Rather than simply transmitting knowledge, the teacher-tutor encourages learning. The teacher does not seek to solve problems but, on the contrary, uses them to determine learning goals [39]. Applied to physiotherapy, PBL facilitates the acquisition of skills necessary for conducting a comprehensive functional diagnosis, selecting appropriate treatment, engaging in effective peer discussion, promoting metacognition, and taking ownership of learning. Clinical cases utilized in PBL should be open-ended, with difficulty tailored to the student's proficiency, fostering active participation in their learning process [13]. Organizing debates and discussions as part of the learning process strengthens communication skills, promotes knowledge exchange, and facilitates the use of professional vocabulary. A shared language is a powerful tool that facilitates the assimilation of the disciplines addressed and develops the objectives of essential professional knowledge [38, 13]. This innovative methodology enhances skills and strengths, aiding in the reconstruction of the scientific method. Since the students are responsible for their learning process, they demonstrate greater involvement and commitment [41]. For its effective application, it is essential to analyze the context of the problem, brainstorm solutions, make a list of known information and what is needed, solve and define the problem, and finally obtain information [39]. The objectives of PBL in health sciences are to foster reasoning, problem-solving skills, self-directed learning, communication skills, and an in-depth understanding of the concepts. Principles in the curriculum create a more positive attitude among students and improve metacognitive awareness and critical thinking skills compared to lecture-based methods [40-41]. Creating conditions allowing trial and error is essential since reflecting on mistakes often leads to the most profound learning experiences. By empowering learners to take ownership of their learning and structure their knowledge, PBL fosters depth, impact, and lasting understanding [38]. PBL generates positive values, appreciation, and affective moods. It positively influences the achievement of attitudinal competencies [39]. PBL is a pedagogical practice conducive to fostering a more human and critical formation, particularly when implemented as an active teaching method per established guidelines outlined in the literature [43]. The teacher-student relationship within PBL should balance the necessary closeness to build trust and provide mentorship while maintaining appropriate distance to prevent psychological dynamics [38]. Including clinical cases as an educational tool in physical therapy has yielded numerous benefits such as improvements in patient assessment, greater capacity for comprehensive functional diagnosis, goal setting, and choice of appropriate treatment. In addition, utilizing clinical cases improves communication skills and fosters critical thinking, which encompasses self-regulated reflection on emotions, knowledge, behaviors, and the environment in which the individual develops. This reflective process involves skills such as analysis, inference, evaluation, and evidence-based practice. Additionally, clinical cases promote clinical judgment through students' critical reflection; all focused on problem-solving. These various aspects converge to promoting clinical reasoning, improving behavior and teamwork, acquiring clinical skills, and achieving better patient results [13, 42]. It allows students to interpret data and design strategies to be applied in their professional practice [13].
Collaborative or Team-Based Learning
Team-based learning (TBL) is a versatile teaching method based on the socio-constructivist and learner-centered paradigms. Originating in the United States, Larry Michaelsen introduced TBL as an innovative departure from conventional teaching methodologies [21]. It cultivates a collaborative atmosphere aimed at realizing objectives designed by team members alongside educational objectives promoted by the teacher. Despite the integration of technological tools, ABE focuses more on learning contents and concepts, often manifesting in problem-solving scenarios mirroring real-world or daily life challenges [17]. It has been shown to promote significant student learning outcomes, engendering a highlighted active attitude [44]. This is favored in correspondence to the execution of case analysis, group discussion, review of scientific articles, group, and individual papers, use of audiovisual material, participation in forums, and role-playing [18]. Critical thinking plays a pivotal role in structuring reasoned experiences and critically analyzing the cases situated within authentic contexts based on scientific principles [45]. Rivera et al. [46] revealed that groups outperformed individuals, enhanced the integration of skills, and had a high level of group cohesion. Collaborative endeavors foster the sharing of information, knowledge, and solutions. Thereby promoting collaborative relationships among students. This collaborative dynamic fosters a strong peer commitment, favoring mutual learning [47]. The TBL approach catalyzes increased student engagement, encouraging active participation in pre-class reading during lessons. The preparation phase enables teachers to address and focus on learning gaps, while teamwork promotes peer interaction and active participation [48]. Teachers must possess skills such as learning team activities, inspiring discussions within and outside the team, and specializing in the role of the facilitator. They should also provide continuous and timely feedback, focusing on designing team application exercises, modeling collaborative teaching, and facilitating the clinical application of theoretical knowledge [21, 44]. The cultivation of autonomy, critical thinking, and solidarity are encouraged in constructing knowledge and fostering ongoing dialogue among group members.
Inverted classroom
The inverted classroom model represents a pedagogical strategy that redefines the learning processes by shifting a portion of the learning activities outside the classroom. During class sessions, the focus is on leveraging teaching expertise to facilitate and enhance various knowledge acquisition and practical application processes. The transformation of the classroom environment aims to create an interactive and dynamic learning space in which the teacher guides students through practical exercises using questioning techniques and case studies to encourage the inquiry and application of ideas through pre-class video materials. This approach promotes creative participation in the course content [19, 20]. The application of the inverted classroom pedagogical model has been shown to enhance academic performance by providing students with contextualized learning experiences aligned with the demands of their future professions [50]. Therefore, it is essential to integrate healthcare practices based on user-centered clinical reasoning within the context of the prevailing health model. Likewise, these teaching-learning strategies facilitate the development of student autonomy, communication skills, and ethical and humanistic responsibility [51]. In this regard, the flipped classroom approach aims to contextualize the students for the challenges they will face in their future careers. Its influence on learning patterns and techniques of the Proprioceptive Neuromuscular Facilitation-PNF concept supported by short video clips is similar to the traditional methods [51]. It also improves the quality of students' work [50]. Utilizing concise video lectures watched outside the classroom liberates more in-class time for active learning, offering the advantage of easy availability and repeated viewings, considering that students' learning speed may vary [51, 52].
Interprofessional Learning
Interprofessional education (IPE) and collaborative practice can play a pivotal role in moderating various challenges facing healthcare systems worldwide. These initiatives generate greater coordination and continuity of patient care, increase patient satisfaction, and promote collaborative decision-making processes. IPE positively impacts communication skills and cooperative work, facilitating the translation of theoretical knowledge into clinical practice. It provides an important platform for undergraduate students to explore and develop their professional values [22], gaining knowledge and competencies (communication, leadership, patient-centered care, role clarification, teamwork, and disagreement resolution) for teamwork with active patient participation [23]. Team efforts consistently outperform individual efforts. Both current and past attendance is important to team performance, consistent with an IPE program where subsequent sessions build on and extend content presented in previous ones [53]. Students valued their interactions with other students from different professional backgrounds, citing the opportunity to problem solve, receive peer support, and gain insights from various perspectives on patient cases [21-22]. Ideally, IPE should begin early in the trainee's professional career [23]. Most new physical therapy graduates demonstrate confidence in communicating with professionals from diverse backgrounds and understanding their roles, but they often exhibit low self-efficacy levels when faced with interprofessional conflict resolution and when providing feedback to peers [54]. It is recommended that future curricula incorporate IPE to familiarize students with communication, role recognition, and conflict resolution before professional practice [54]. Learning is not a natural or spontaneous process; it requires intentionality, planning, and methodological rigor [55]. The interdisciplinary dialogue within healthcare professions fosters innovative pedagogical practices among teachers. Students appreciate the diversity of professional backgrounds and knowledge among their peers. Their awareness drives students to actively seek out and acquire specific knowledge from disciplines they have not yet encountered [22]. In this perspective, students and faculty collaborate to develop integrated products each semester, which materialize from the partnership established with the unit's Health Team [55].
Service Learning Training Practice
Formative Practice (FP) is where the students link the knowledge, abilities, and skills obtained in the elementary level of training with the experiences acquired in practice through the different areas of professional training [24]. It is focused on facilitating learning and enhancing professional competencies, where practical aspects are prepared using techniques that effectively connect theory with practice, thereby becoming a crucial component of professional development. The evaluation of the Practicum emphasizes the assessment of the practical phase, integrating considerations of both human and ethical competencies [39]. Among the essential qualities assuming responsibility, demonstrating a commitment to actions and patients, and possessing requisite prior knowledge they must possess to begin the practicum. As well as the learning that they gradually develop with the accompaniment of their tutors [24]. These attributes are parts of the transversal competencies stipulated for physical therapists by the professional community. Rooted in professionalism and ethics, these competencies aim to cultivate autonomy and self-regulation in the exercise of practice and professional knowledge. They are aligned with globally recognized ethical, political, and techno-scientific principles, which are socially legitimized and respected by the professional collective [7]. The most prominent feelings experienced by the students are happiness at the beginning of a new stage and the satisfaction of accomplishing their goals; however, they also grapple with anxiety stemming from facing the unknown, such as interacting with patients [24]. The active involvement of practical professionals in facilitating learning is a significant motivator for students and increases the consolidation of their knowledge, fostering greater transferability of learning outcomes [39]. Increasing practical training opportunities for students in the early stages of their education is crucial. This enables a more concrete approach to the situations they will encounter during their training, thereby helping them develop the skills necessary to navigate the challenges of practice. By providing concrete early on, students can better manage the anxiety and insecurity often associated with practical training. Focusing on early practical experiences ensures that students' aspirations are directed toward the learning process, fostering a more positive and productive educational journey [24]. Service-learning allows students to practice the skills and techniques they've learned in the classroom within a real or practical environment. The results were obtained professionally and personally, and the participating patients were rewarded for the work done [57]. The efficiency of the teaching-learning process has been underscored, with online training emerging as a valuable tool for addressing training gaps and acquiring new knowledge within the context of training practice or service learning. The proposal in the e-learning modality allows updating the content, modernizing the presentation of the materials, proximity and permanent interaction of the teacher in the student's learning, and the freedom and active contribution to the final result of the training on the part of the learners. The transversal formative aspects make e-learning systems viable instructional tools across diverse clinical or professional areas of physical therapy [58]. The learning contract has been found to facilitate the development of high-quality learning since it promotes autonomy and enables students to take control of their learning, which is fundamental in their future professional practice. This approach aims to enhance students' motivation to learn and facilitates the integration of theory into practice. It supports the development of skills such as thinking and communicating or solving problems, leading to more meaningful learning for the student. The effort involved in implementing the learning contract in terms of time consumption promotes the active participation of students in their learning. It is important to encourage future physical therapists to increase their skills by developing autonomous learning throughout their professional lives [35].
Practices within public services must adopt a comprehensive care approach, which includes health promotion and injury prevention strategies [59]. By integrating undergraduate students into primary healthcare settings, they become agents capable of effecting real-world change. Their presence and collaboration in care interventions enhance the quality of healthcare delivery, contributing to the training of professionals who are cognisant of social realities and equipped with the skills necessary for health promotion, health education, and injury prevention. This collaborative approach improves the service delivery process and enhances student training, ultimately leading to better health outcomes for the population being served. It helps to mitigate the inherent characteristics of the biomedical model of care, fostering a more holistic and patient-centered approach to healthcare [7].
Integrating students into healthcare services has been recognized as a transformative element in professional practices, particularly due to the opportunity for collaborative discussion among teachers, students, and professionals regarding shared actions and interventions. The insertion of formative processes that articulate learning with practice in the different disciplinary fields will change the training of physical therapists, guiding them to expand their understanding of the demands and complexity of work in the single health system (SUS) [59].
Discussion
Based on the findings, the implementation of active methodologies in education has shown significant improvements in various abilities, including autonomous, self-managed, and self-regulated learning, as well as problem-solving and communicative skills. The semiological model favors the integration of knowledge interrelated with clinical evaluation and allows stimulating the student's thinking to models that relate structure and function. This approach stimulates critical thinking and deepens understanding of the topics under study, enabling students to grasp complex concepts more thoroughly. The teacher's ability to establish an enriched and constructive learning environment, providing guidance for understanding, offering feedback to support learning, evaluation, teacher-discussant relationship, relationship between learners, ensuring curriculum coherence, and employing methods focused on student learning and empowerment of their autonomy and self-regulation are highly appreciated [31, 2]. Six explanatory models are recognized for the didactics of anatomy to elucidate the anatomical concept, including structural, functional, semiological, integrative, pseudo-integrative, and heterogeneous. Personal constructions can be based on the interrelationships between the students and their academic, social, and cultural environment. The anatomical segment studied is a concept that must link structure and function, integrated into teaching to reduce the risk of seeing a body structure isolated from its impact on the organism's function. The semiological model indicates knowledge integration is closely related to clinical evaluation. It allows educators and students to discuss the broader implications and functional interpretations of symptoms manifested in medical situations.
The significance of the intervention lies in its ability to encourage students to transition from fragmented models of thinking to ones that aim to establish meaningful relationships between structure and function. This transition is crucial for comprehensively understanding the phenomenon under study [32].
Simulation in physical therapy has proven to improve professional behavioral competencies, such as communication, patient assessment, therapeutic analysis and design, intervention techniques, evidence-based practice, and risk management. Through simulation practice, students demonstrate increased clinical skills, self-confidence, and proficiency in performance and safety protocols. Moreover, it has been observed to enhance decision-making abilities during the professional reasoning process in clinical practice, improving learning outcomes and efficiency in multidisciplinary work. Simulation-based education provides a controlled and safe modulated learning environment for learners to learn and generate these skills before encountering real patients, where the consequences of their performance are crucial in medical practice [11]. Utilizing video and simulated patients offers diverse applications, including employing simulated patient instructors who can assume both patient and instructor roles while providing student feedback within a controlled environment. Video observation or analysis is a practical and current tool for assessing tasks in health simulation environments, facilitating the evaluation of clinical interviews [35]. This approach enables the analysis of clinical skill management and capitalizes on feedback while reviewing video recordings of interviews provided by both students and instructors, thereby enhancing session effectiveness [36]. Another way is technique demonstration and role reversal. However, this method overlooks a way of teaching a profession without considering the experience lived by the participants immersed in the training process [33]. Simulation-based models improve learning and clinical practice outcomes, clinical decision-making, and efficiency in multidisciplinary work [10].
Problem-based learning helps students acquire basic knowledge and skills that are essential for their professional practice. It guides them in developing their capacity for analysis and synthesis, fostering critical thinking in self-assessment and evaluating their peers. Additionally, PBL enhances oral and written communication skills. When applied to physical therapy, PBL facilitates the development of skills necessary for establishing a comprehensive functional diagnosis, selecting appropriate treatment strategies, and engaging in effective peer discussions. Furthermore, it promotes metacognition and facilitates knowledge acquisition. Project-based Learning (ABPro), which is applied in physical therapy education, offers numerous benefits for students. It enhances creativity, teamwork, autonomy, assertive communication, and recognition of population needs. Moreover, it encourages students to inquire about strategies and plan approaches often utilizing ICT, favors the development of clinical reasoning competence on spinal pain, and is a positive experience that favors the development of academic content and obtaining learning skills [15]. Students find this method to be a positive experience for creating digital material focused on preventing musculoskeletal complications, promoting healthy habits, and providing guidance on proper postural hygiene [7, 15]. PBL, applied in the classroom, leads students to effectively address real problems and formulate proposals to overcome what has been observed, leading to the construction of solutions to problems based on the student's real life to activate prior knowledge and simultaneously motivate a dialogue that considers critically assessing the options in the students through research and analysis processes [42]. PBL and ABPro are closely linked to each other and other methods [39]. Case-Based Learning (ABC) is a pedagogical method that encourages the discovery of new knowledge by facilitating interconnection between current and previous knowledge and develops autonomy, critical thinking, and argumentative skills in real situations. Students find this experiential approach highly motivating, and educators consider it enriching. It promotes critical, reflective, and analytical skills and attaining professional competencies. It positively influences the attainment of communicative, procedural, and attitudinal competencies and reinforces previously learned knowledge [7, 14].
Team-based learning fosters significant learning among students by cultivating a more active learning attitude. It facilitates the development of critical thinking skills, enabling students to structure reasoned experiences and critically analyze cases within real-world contexts based on scientific principles. This method also demonstrates a better-improved group performance compared to individual efforts. Moreover, it encourages collaborative relationships by promoting the sharing of information, knowledge, and solutions among team members. This approach stimulates reasoned, cooperative, and conclusive reflection on the proposed common therapeutic process [45]. The learners perceive this method as more enjoyable [49]. ABE has three phases: preparation, Assurance Testing (IRAT) followed by Team Readiness Assurance Testing (TRAT), and group review aimed at knowledge sharing. Instructors provide feedback geared towards leveraging collaborative learning to bolster students' problem-solving abilities. Finally, the teams apply the acquired knowledge to solve real-world problems or case studies [17]. Flipped classroom teaching has been shown to have the potential to refine higher-order thinking skills and promote self-regulated learning among students [51]. A critical success factor for these learning approaches is the preparation of students before class attendance and collaborative learning within the classroom, both of which are integral components of the flipped classroom model [51]. Although the flipped classroom model does not provide instructions regarding learning activities, it represents an opportunity to implement higher-order learning skills in teaching and improve clinical competencies among healthcare students [51]. This approach gives students a well-planned, flexible, and consistent learning process.
Applying the inverted classroom pedagogical model has enhanced academic performance by enabling students to contextualize their future professional roles. It is essential to include it in healthcare practice based on user-centered clinical practice within the context of the healthcare model. It also facilitates the development of student autonomy, communication skills, and the humanistic acceptance of technological advances. By transforming students into active learners, it fosters the cultivation of analytical, synthesis, and evaluative capacities. Applying this method in gait analysis outperforms the effectiveness of the traditional teaching method [52]. The inverted classroom model cultivates active learners by developing their capacity for analysis, synthesis, and evaluation [52]. The passive learning of the flipped classroom occurs during video lectures outside of class, optimizing in-class time for active learning [52]. Students' limited attention spans are effectively counteracted through interactive learning and group exercise [52].
Sixthly, interprofessional learning positively impacts communication skills and cooperative work by facilitating the clinical application of theoretical knowledge and teamwork skills. Through active patient involvement, IPL enhances competencies such as communication, leadership, patient-centered care, clarification of roles, teamwork, and conflict resolution. Through IPL, students acquire a comprehensive understanding of interdisciplinary collaboration, preparing them to engage in interprofessional healthcare environments effectively. The opportunity for students to interact with peers from diverse academic backgrounds promotes a deeper understanding of each team member's role and their unique contributions to patient care. This interaction also plays a pivotal role in shaping students' professional identities, which serve as the central and overarching axis in various educational models and programs [23]. Students develop confidence in their knowledge and communication skills through interprofessional team-based learning in trusting and complementary relationships. They explore their specific roles, understand their professional limitations, and equip themselves to be more competent in working collaboratively in patient care and improving patient outcomes [22]. Working in interprofessional teams enhances the identification of hospital risks, as this expands participants' observational, critical thinking, and situational awareness skills [56].
Through the application of formative practice or service learning, students articulate the knowledge, skills, and abilities acquired during the basic level of training, using the experiences developed in clinical settings. This approach enables students to practice the skills and techniques in a real-world environment, fostering autonomy and control over their learning. It enhances their motivation to learn and develops critical thinking, communication, problem-solving, and more meaningful learning skills. During the search process, relevant sources were found related to methodologies that stimulate the development of clinical reasoning; however, only three sources were found, which were insufficient to structure a thematic block. We hope that future research will address this important skill with greater emphasis, which is fundamental for students to understand complex clinical cases in their future professional practice. Professional training in physiotherapy needs to enhance interdisciplinary and multi-professional practices during graduation. This entails providing students with opportunities to engage in interventions across different teaching-learning scenarios involving students from different academic backgrounds. Through these experiences, students gain insights into the roles and contributions of different disciplines within the professional team. By experimenting with and reflecting on interdisciplinary collaboration during their undergraduate education, students develop a deeper understanding of healthcare practices that extend beyond biotechnological and physiotherapeutic knowledge. This critical analysis of their training journey fosters a broader perspective on the role of physiotherapy professionals within the healthcare system [7, 59].
Conclusion
Using multiple active learner-centered strategies in physical therapy education significantly contributes to developing autonomous learning, clinical reasoning, collaborative work, and critical thinking among students. These strategies also foster the development of communication and problem-solving skills, equipping students to tackle challenges in their professional futures.
Acknowledgments: None declared by the authors.
Ethical Permissions: None declared by the authors.
Conflicts of Interests: None declared by the authors.
Authors’ Contribution: Rojas JG (First Author), Introduction Writer/Main Researcher/Discussion Writer (35%); Fuster-Guillén D (Second Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Flores JRC (Third Author), Methodologist/Statistical Analyst/Assistant Researcher (20%); Hernández RM (Fourth Author), Methodologist/Assistant Researcher/Discussion Writer (20%)
Funding/Support: None declared by the authors.
Article Type: Systematic Review |
Subject:
Health Literacy
Received: 2024/01/12 | Accepted: 2024/03/5 | Published: 2024/03/22
Received: 2024/01/12 | Accepted: 2024/03/5 | Published: 2024/03/22
References
1. Giraldo Ríos V, Ortíz Restrepo Y. Formative practices in the physical therapy program. CES University: Antioquia; 2014. [Link]
2. Negro-Dellacqua M, Junior PM, de Sá-Junior AR, Bortolotto T, Costa FV, de Sousa IF. Potencialidades e desafios na aplicação de metodologias ativas no ensino de Fisioterapia: visão discente. Research, Society and Development. 2019;8(5):01-17. [Link] [DOI:10.33448/rsd-v8i5.1022]
3. Walankar PP, Panhale VP, Situt SA. Evaluation of learning approaches in physiotherapy students: A valuable insight. Journal of Education and Health Promotion. 2019;8. [Link] [DOI:10.4103/jehp.jehp_254_18]
4. Simon E, Jezine E, Vasconcelos EM, Ribeiro KSQS. Metodologias ativas de ensino-aprendizagem e educação popular: encontros e desencontros no contexto da formação dos profissionais de saúde. Interface-Comunicação, Saúde, Educação. 2014;18:1355-1364. [Link] [DOI:10.1590/1807-57622013.0477]
5. Ruescas Nicolau MA, Sánchez Sánchez ML, Cezón Serrano N, Sempere Rubio N. Ruescas Nicolau MA, Sánchez Sánchez ML, Cezón Serrano N, Sempere Rubio N. Investigación e innovación responsable en Fisioterapia. Libro de resúmenes. 2022 [Link]
6. Silva Quiroz J, Maturana Castillo D. A proposed model for introducing active methodologies in higher education. Innovación Educativa (Mexico DF). 2017;17(73). [Link]
7. Peralta Lara DC, Guamán Gómez VJ. Active methodologies for teaching and learning social studies. Society & Technology. 2020;3(2):2-10. [Link] [DOI:10.51247/st.v3i2.62]
8. Villalobos Delgado V, Avila Palet J, Olivares SL. Problem-based learning in chemistry and critical thinking in high school. Revista Mexicana de Investigación Educativa. 2016;21(69):557-581. [Link]
9. Tello NC, Ordoñez AS, Mora LTO, Arana JED. Usefulness of virtuality in physiotherapy professional practices in the context of the COVID-19 pandemic. Challenges. 2022;43:185-91. [Link] [DOI:10.47197/retos.v43i0.87875]
10. Alfonso-Mora ML, Castellanos-Garrido AL, Nieto ADDPV, Acosta-Otálora ML, Sandoval-Cuellar C, del Pilar Castellanos-Vega R, et al. Simulation-based learning: pedagogical strategy in physical therapy. Integrative review. Medical Education. 2020;21(6):357-363. [Link] [DOI:10.1016/j.edumed.2018.11.001]
11. Velasco GG, Hernandez GLS, Daniel GAB. Interprofessional clinical simulation scenario on mixed delirium in undergraduate medicine and physiotherapy. Investigación en Educación Médica. 2021;10(40):29-36. [Link] [DOI:10.22201/fm.20075057e.2021.40.21353]
12. Tuttle N, Horan SA. The effect of replacing 1 week of content teaching with an intensive simulation-based learning activity on physiotherapy student clinical placement performance. Advances in Simulation. 2019;4(1):1-8. [Link] [DOI:10.1186/s41077-019-0095-8]
13. Tejeda CX, Alpuche HA, Aburto-Arciniega MB, Gutiérrez CC. Research in Medical Education. 2022;11(44):67-75. [Link] [DOI:10.22201/fm.20075057e.2022.44.22439]
14. Jácome-Hortua AM, Muñoz-Robles SC, Gonzáles HL. Impact of the implementation of the Case-Based Learning (ABC) strategy on clinical practicum students in physical therapy. Iatreia. 2022;35(1):48-56. [Link]
15. Rodríguez Cáceres AAR, Lever Méndez J, Alfonxo Mora ML, Vanegas Riaño MA, Sanchez Gutiérrez LA, Bermúdez Jiménez VN, Sarmiento Vargas CA. Project-based learning for physiotherapeutic reasoning about spinal pain during quarantine by COVID-19. Medical Education. 2021;22(5):267-272. [Link] [DOI:10.1016/j.edumed.2021.06.003]
16. Olmedo EO, Sánchez IM. Meaningful learning as the basis of innovative methodologies. Hekademos: digital educational journal. 2019;(26):18-30. [Link]
17. Ferrada Quezada N, Contreras Álvarez J. Team-Based Learning: The perspective of prospective teachers. Journal of Studies and Experiences in Education. 2021;20(42):117-135. [Link] [DOI:10.21703/rexe.20212042ferrada7]
18. Vela GPS, Chacón LJ R, Masache GAD, Carrión SAA. Educational intervention from physical therapy in times of COVID-19 in Ecuador; a contribution from the scientific and human area. Contemporary Dilemmas: Education, Politics and Values. 2022. [Link]
19. Bravo PM, López GS, Andreu MRG. Effectiveness of a flipped classroom methodology combined with clinical simulation in the learning of pediatric basic life support in nursing. In: Proceedings of the III International Conference on Teaching Innovation and Research in Higher Education: changes in the teaching-learning process of the Knowledge Areas. November 15-20, 2021. University Association of Education and Psychology (ASUNIVEP); 2021. p. 45. [Link]
20. Montero S, Botella JM, Del Rio S, Isabel M, Rocha VMP, Molina FJ, et al. Flipped learning: the use of the flipped classroom model in physiotherapy practices. In: I Congreso CEU de Innovación Educativa y Docente 2020. San Pablo University Foundation; September 2021. p. 37. [Link]
21. Burgess A, Kalman E, Haq I, Leaver A, Roberts C, Bleasel J. Interprofessional team-based learning (TBL): how do students engage?. BMC medical education. 2020;20(1):118 [Link] [DOI:10.1186/s12909-020-02024-5]
22. Ho JMC, Wong AYL, Schoeb V, Chan ASW, Tang PMK, Wong FKY. Interprofessional team-based learning: A qualitative study on the experiences of nursing and physiotherapy students. Frontiers in Public Health. 2021;31(9):706346. [Link] [DOI:10.3389/fpubh.2021.706346]
23. Soto-Ruiz N, Escalada-Hernández P, Ortega-Moneo M, San Martín-Rodríguez L, Viscarret-Garro JJ. Interprofessional health sciences education with patient collaboration. Medical Education. 2022;23(1):100718. [Link] [DOI:10.1016/j.edumed.2022.100718]
24. Ramírez EG, Hernández CO, Soto AC. Social representations of formative practice in physical therapy students in Colombia. Fisioterapia. 2021;43(1):12-18. [Link] [DOI:10.1016/j.ft.2020.06.005]
25. Villasís-Keever MA, Rendón-Macías ME, García H, Miranda-Novales MG, Escamilla-Núñez A. Systematic review and meta-analysis as support tools for clinical and research. Revista alergia México. 2020;67(1):62-72. [Link] [DOI:10.29262/ram.v67i1.733]
26. Tapia-Benavente L, Vergara-Merino L, Garegnani LI, Ortiz-Muñoz L, Loézar Hernández C, Vargas-Peirano M. Rapid reviews: definitions and uses. Medwave. 2021;21(01). [Link] [DOI:10.5867/medwave.2021.01.8090]
27. Llópis PEA, Morales YG, Estevez ALG, Mesa CR. Scientific communication in research that assumes the qualitative approach: an evaluative look. EduMeCentro. 2021;13(2):172-191. [Link]
28. Martínez González M, Martínez-Carrasco A. Interactive technologies for learning in physiotherapy: electronic response commands. Fisioterapia. 2014;36(1). [Link] [DOI:10.1016/j.ft.2013.03.002]
29. Collado Vázquez S, de la LLave Rincón A, Palacios Ceña D, Miangolarra Page J. Active teaching-learning methodologies in the subject Fundamentals of Physical Therapy. In: In-Red 2016. II National Congress of educational innovation and networked teaching. Editorial Universitat Politècnica de València; July 2016. [Link]
30. González-Contreras A, Pérez-Villalobos C, Hechenleitner M, Vaccarezza-Garrido G, Toirkens-Niklitschek J. Academic satisfaction and pedagogical practices perceived by health students in Chile. FEM: Journal of the Medical Education Foundation. 2019;22(3):103-107. [Link] [DOI:10.33588/fem.223.992]
31. López BG, Iranzo MÀC, Chust BS, Garcés MA B, Blasco AQ. Learning-centered methods in Physical Therapy: student capabilities and learning context. REDU: Revista de Docencia Universitaria. 2017;15(2):329-348. [Link] [DOI:10.4995/redu.2017.7868]
32. Mejía OAA, Ruiz-Ortega FJ, Arias SL, Trujillo L. Explanatory models in anatomy. Tecné, Episteme y Didaxis: TED. 2021;(49). [Link]
33. Otálora MLA, Mora MLA, Garrido ALC, Vega RDP C, Mejía EAC, Ortegón RLG, et al. Clinical simulation: an experience in physical therapy. Universidad de La Sabana. 2020. [Link]
34. Sandoval-Cuellar C, Alfonso-Mora ML, Castellanos-Garrido AL, del Pilar Villarraga-Nieto A, Goyeneche-Ortegón RL, Acosta-Otalora ML, del Pilar Castellanos-Vega R, Cobo-Mejía EA. Simulation in physiotherapy students for clinical decisions during interaction with people with low back pain: randomised controlled trial. BMC medical education. 2021;21(1):1-8. [Link] [DOI:10.1186/s12909-021-02812-7]
35. Rodríguez IG, Bitata MD, Escudero MG, Arce DÁ, Quintana MG, Ramirez RI. Vídeo-análisis en ciencias de la salud: una experiencia de simulación en entrevista clínica en fisioterapia. Revista Española de Educación Médica. 2022;3(2). [Link] [DOI:10.6018/edumed.523411]
36. Montull Morer S. Learning basic communication skills in physiotherapy: a training proposal using video and simulated patient instructor. Revista de Ciències de l'Educació. 2015;1:97-99. [Link] [DOI:10.17345/ute.2015.1.665]
37. Domínguez EG, Fisac IH, Hernández MAN. Problem-Based Learning (PBL): a tool for knowledge integration in Physiotherapy. Hekademos: digital educational journal. 2013;(13):27-34. [Link]
38. Germain F, Pérez-Rico C. Competency-based education as a means to facilitate student takeover of learning. FEM: Journal of the Medical Education Foundation. 2014;17(1). [Link] [DOI:10.4321/S2014-98322014000100004]
39. Hernández-Huaripaucar EM, Calmett RMY. Problem-Based Learning (PBL) as an innovative didactic strategy in the teaching of human anatomy. Horizon of Science. 2020;10(19):165-177. [Link] [DOI:10.26490/uncp.horizonteciencia.2020.19.595]
40. Edwards DJ, Kupczynski L, Groff SL. Learning styles in problem-based learning environments: impacts on student achievement and professional preparation in university level physical therapy courses. International Journal of Higher Education. 2019;8(3):206-213. [Link] [DOI:10.5430/ijhe.v8n3p206]
41. Pulido Gómez DA. Evaluation of problem-based learning as a method for understanding the subject of kinematics [Doctoral dissertation]. Bogotá: Universidad Externado de Colombia; 2019. [Link]
42. Pernalete Lugo J, Odor Rossel Y, Rosales Veitía J. Critical thinking in the university context: an aspect of problem-based learning. Warisata - Revista De Educación. 2022;4(10):34-54. [Link] [DOI:10.61287/warisata.v4i10.3]
43. Chesani FH, Maestrelli SRP, Cutolo LRA, Nunes R. Aprendizagem baseada em problemas e a formação do fisioterapeuta: estudo de caso. Trabalho, Educação e Saúde. 2017;15:931-950. [Link] [DOI:10.1590/1981-7746-sol00074]
44. Fernández-Huerta L, Córdova-León K, Pérez-Galdavini V. Team-based learning in a professionalizing subject of a kinesiology school. FEM: Journal of the Medical Education Foundation. 2020;23(5). [Link] [DOI:10.33588/fem.235.1081]
45. Mesa LMM, Bolívar NR. An experience from the university classroom in physiotherapy based on collaborative learning and use of technological platforms. Lúdica Pedagógica. 2020;1(32):1-16. [Link] [DOI:10.17227/ludica.num32-12186]
46. Rivera MD, Henry EF, Villalobos CP, Fuentes NR, Saéz PS, Vallejos CR, et al. Teamwork and academic performance in a kinesiology course employing team-based learning. Research in Medical Education. 2017;6(22):80-87. [Link] [DOI:10.1016/j.riem.2016.05.006]
47. Dueñas M, Salazar A, Ojeda B, de Sola H, Failde I. Application and evaluation of collaborative active learning methods in public health teaching in physical therapy. Medical Education. 2016;17(4):164-169. [Link] [DOI:10.1016/j.edumed.2016.05.001]
48. Amorim JSCD, Poltronieri BC, Ribeiro AM, Ferla AA. Team-based learning in Physical therapy undergraduate course: experiment report. Fisioterapia em Movimento. 2019;32. [Link] [DOI:10.1590/1980-5918.032.ao46]
49. Teixeira RDC, Magalhaes AB, Palacios VR, Teixeira MDM. Physiotherapy students' perceptions of team-based learning using the team-based learning student assessment. Journal of Education and Learning. 2019;8(4):43-51. [Link] [DOI:10.5539/jel.v8n4p43]
50. Røe Y, Rowe M, Ødegaard NB, Sylliaas H, Dahl-Michelsen T. Learning with technology in physiotherapy education: design, implementation and evaluation of a flipped classroom teaching approach. BMC medical education. 2019;19(1):1-8. [Link] [DOI:10.1186/s12909-019-1728-2]
51. Guerrero-Isaza Y, Mariño-Neira CM. Reverse class with video in learning the concept of Proprioceptive Neuromuscular Facilitation. Cultura Educación Y Sociedad. 2022;13(2):219-32. [Link] [DOI:10.17981/cultedusoc.13.2.2022.12]
52. Grover P, Phadke S. Efficacy of flipped classroom teaching on the cognitive domain in second-year physiotherapy students. Medical Journal of Dr. DY Patil Vidyapeeth. 2021;14(6):642-645. [Link] [DOI:10.4103/mjdrdypu.mjdrdypu_290_20]
53. Bhattacharya SB, Jernigan S, Hyatt M, Sabata D, Johnston S, Burkhardt C. Preparing a healthcare workforce for geriatrics care: an Interprofessional team-based learning program. BMC geriatrics. 2021;21(1):1-10. [Link] [DOI:10.1186/s12877-021-02456-8]
54. Jones A, Ingram ME, Forbes R. Physiotherapy new graduate self-efficacy and readiness for interprofessional collaboration: a mixed methods study. Journal of Interprofessional Care. 2021;35(1):64-73. [Link] [DOI:10.1080/13561820.2020.1723508]
55. Toassi RFC, Lewgoy AMB. Integrated Health Practices I: an innovative experience through inter-curricular integration and interdisciplinarity. Interface-Comunicação, Saúde, Educação. 2016;20:449-61. [Link] [DOI:10.1590/1807-57622015.0123]
56. Reime MH, Molloy MA, Blodgett TJ, Telnes KI. Why an IPE Team Matters... Improvement in identification of hospital hazards: a room of horrors pilot study. Journal of Multidisciplinary Healthcare. 2022:1349-1360. [Link] [DOI:10.2147/JMDH.S368363]
57. Lafuente R, Calvo S, Buesa A, Pérez S, López M, Fortún R, et al. Service-learning in Final Degree Work in Physical Therapy during times of pandemic. RIDAS. Iberoamerican Journal of Service-Learning. 2020;(10):62-76. [Link] [DOI:10.1344/RIDAS2020.10.6]
58. Donat-Roca R, Sánchez-Socarrás V, Camacho-Martí M. Online training in physiotherapy: experience of an instructional design of learning using the moodle virtual platform. FEM: Journal of the Medical Education Foundation. 2015;18(1):27-34. [Link] [DOI:10.4321/S2014-98322015000100005]
59. Gauer APM, Ferretti F, Teo CRPA. Professional training in physiotherapy: barriers to the diversification of practical learning scenarios and for teaching-service integration. Fisioterapia em Movimento. 2018;31. [Link] [DOI:10.1590/1980-5918.031.ao28]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






