Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 225-230 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ryosuke O, Kazuma S. Association between Lifestyle Habits and Mortality Rates; A Prefectural Analysis in Japan. Health Educ Health Promot 2024; 12 (2) :225-230
URL: http://hehp.modares.ac.ir/article-5-73243-en.html
URL: http://hehp.modares.ac.ir/article-5-73243-en.html
1- Department of Nursing, School of Nursing, Osaka Metropolitan University, Osaka, Japan
2- Department of Consulting & Sales, Insight Edge, Inc., Chiyoda, Japan
2- Department of Consulting & Sales, Insight Edge, Inc., Chiyoda, Japan
Full-Text [PDF 615 kb]
(2387 Downloads)
| Abstract (HTML) (1139 Views)
Full-Text: (183 Views)
Introduction
Malignant tumors, heart disease, and cerebrovascular disease stand as the top three causes of death in Japan, with these diseases maintaining their leading positions for over 50 years [1]. Mortality rates for these conditions exhibit variations among prefectures within Japan. For instance, Aomori Prefecture records the highest mortality rate for malignant tumors (707 deaths per 100,000 persons), while Nagano Prefecture reports the lowest (486 deaths per 100,000 persons) [1]. Aomori Prefecture also demonstrates the highest death rate from heart disease (190 deaths), contrasting with Shiga Prefecture, which has the lowest rate (103 deaths). Similarly, Ehime Prefecture exhibits the highest rate of mortality from cerebrovascular disease (288 deaths), while Fukuoka Prefecture displays the lowest (154 deaths) [1]. Consequently, there exists an almost twofold difference in mortality rates per 100,000 persons for the same disease across prefectures. To diminish deaths from these three diseases in each prefecture, it is crucial to pinpoint the factors contributing to the mortality rate disparities among prefectures.
Previous studies have indicated that the disparities in mortality rates among prefectures are linked to factors, such as salt intake, weather conditions, and living environments [2-4]. Conversely, deaths attributed to malignant tumors, heart disease, and cerebrovascular disease have been correlated with lifestyle elements like dietary choices and exercise habits [5, 6]. Hence, variations in lifestyle practices across regions may also contribute to the differences in mortality rates among prefectures. Therefore, it is essential to consider the impact of lifestyle when examining the variations in mortality rates among prefectures. Nevertheless, a detailed analysis concerning the differences in mortality rates among prefectures and lifestyle has not been conducted due to the limited availability of nationwide data on individual-level lifestyle habits.
In Japan, specific health checkups are conducted for individuals aged 40 to 74 years to identify those in need of health education aimed at reducing the prevalence of metabolic syndrome and its precursor. These specific health checkups have facilitated the collection of nationwide data on individual lifestyle habits. These data have been publicly available as open data since the fiscal year 2016 under the name of the Japanese National Database of Health Insurance Claims and Specific Health Checkups (NDB). The NDB Open Data is categorized by prefecture, enabling comparisons of lifestyle habits among health checkup participants aged 40 to 74 based on the specific health checkup data. The NDB Open Data is organized by prefecture, allowing for inter-prefecture comparisons. Therefore, this study aimed to elucidate the lifestyle habits associated with the three primary causes of mortality by prefecture, utilizing the 2nd NDB Open Data and the 2015 Vital Statistics.
Instrument and Methods
Data source
This descriptive study utilized the Specified Medical Checkups Questionnaire (items 1-22) from the 2nd NDB Open Data and the age-adjusted mortality rates by prefecture from the 2015 Vital Statistics and was conducted in April 2023 [7, 8]. Both of these datasets represent the most recent available data that can be compared for the same fiscal year.
The questionnaire content used in this analysis aligned with the questions presented to examinees during the specific health check-up.
The data used were collected and published by a government organization; thus, they were already processed. Therefore, no inclusion or exclusion criteria were set for the data used. Regarding sample size, we used a regional correlation design, and examined whether lifestyle habits influenced the mortality rate in each region. Therefore, we did not consider the sample size.
Data extraction and processing
The response data by prefecture for the Specified Medical Checkups Questionnaire in the 2nd NDB Open Data represent individuals who underwent the specified medical checkups, thus displaying values solely for the age group ranging from 40 to 74 years old. Consequently, the response rate (per 100,000 population) for each questionnaire was computed following age adjustment through the direct method, with data confined to the age bracket of 40 to 74 years old, utilizing the 1985 model as the reference population.
When determining the response rate, most questionnaires documented the number of respondents using binary values of ‘yes’ and ‘no’. For these questionnaire items, the percentage of respondents who answered ‘yes’ was calculated. Conversely, certain items recorded the number of respondents with multiple options instead of a binary value (e.g., question 14). For such multiple-choice questions, the proportion of respondents for each option was computed. However, for question 21, the responses were categorized as “I do not intend to improve” (I), “I intend to improve (generally within 6 months)” (II), and “I intend to improve in the near future and have started gradually” (III).
Subsequently, age-adjusted mortality rates by prefecture were obtained for malignant tumors, heart disease, and cerebrovascular disease. These data encompass age-adjusted and age-group-specific mortality rates for 2015 categorized by prefecture, sex, and age group. The age-adjusted mortality data are standardized across all age groups, rendering them incomparable with the NDB Open Data due to differing adjustment conditions. Therefore, age adjustment was confined to the age group between 40 and 74 years to align the adjustment conditions with the NDB open data. Given that age-adjusted mortality rates by age group (per 100,000 population) are outlined in the age-adjusted mortality rates by prefecture, age adjustment was conducted utilizing the 1985 model as the reference population and the direct method to derive age-adjusted mortality rates for the age group between 40 and 74 years
Analysis methods
Multiple regression analysis was performed to elucidate the relationship between the mortality rates of the three primary causes of death by prefecture and the response status to the Specified Medical Checkups Questionnaire. Age-adjusted mortality rates for malignant tumors, heart disease, and cerebrovascular disease were utilized as the dependent variables in the multiple regression analysis. The age-adjusted response rate (per 100,000 population) to the Specified Medical Checkups Questionnaire served as the independent variable. However, as certain questionnaire items, such as medical history and medication history, were deemed to have minimal relevance to lifestyle habits, items 1-7 in Table 1 were excluded from the independent variables in the current analysis.
In the multiple regression analysis, redundant independent variables were eliminated using the stepwise variable selection method. To assess multicollinearity among independent variables, the variance inflation factor (VIF) for each independent variable was calculated, and independent variables with a VIF exceeding ten were excluded before applying the stepwise variable selection method. All analyses were carried out using R version 4.0.3 with a significance level of 5%.
Findings
The results presented in Table 1 were obtained through multiple regression analysis utilizing the stepwise method, with the mortality rates of malignant tumors, heart disease, and cerebrovascular disease as the dependent variables, and the number of respondents to items 8-22 of the Specified Medical Checkups Questionnaire as the independent variable.
Table 1. Results of multiple regression analysis for three major causes of death
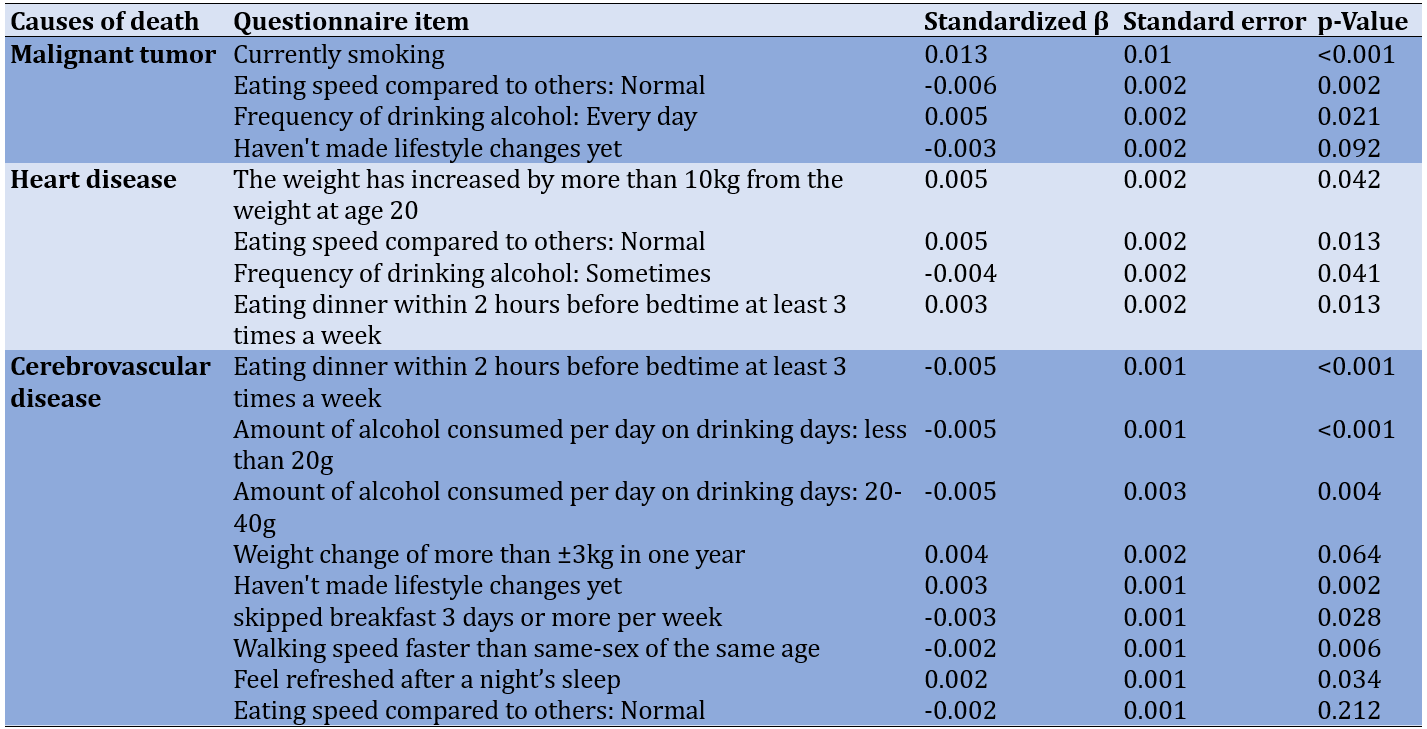
For mortality from malignant tumors by prefecture, significant positive associations were observed with smoking (β=0.013) and frequent daily drinking (β=0.005), while significant negative associations were noted for normal eating speed (β=-0.006) compared to others.
Regarding mortality from heart disease by prefecture, significant positive associations were identified for an increase of more than 10kg from body weight at age 20 (β=0.004), normal eating speed compared to controls (β=0.005), and having dinner at least two hours before bedtime three or more times a week (β=0.003). A significant negative association was found for occasional weekly drinking (β=0.004).
In relation to mortality from cerebrovascular disease by prefecture, significant positive associations were observed for items, such as not yet improving lifestyle (β=0.003) and getting enough rest from sleep (β=0.002). Conversely, significant negative associations were found for consuming less than one drink a day (β=-0.005) or 1-2 drinks a day (β=-0.005), skipping breakfast three or more times a week (β=-0.003), walking faster than their age-mates (β=-0.002), and eating at a normal speed compared to others (β=-0.002).
Discussion
To investigate the factors influencing the regional variations in the top three causes of death in Japan, the findings from the specific health check-ups by the prefecture as published in the NDB open data were utilized and analyzed. The outcomes indicated that certain lifestyle habits were associated with the mortality rates of these diseases across prefectures. These findings imply that lifestyle habits play a role in the divergence of mortality rates among prefectures, alongside factors highlighted in prior research, such as climatic conditions. The lifestyle habits pinpointed in this study will be deliberated upon in relation to the effectiveness of measures aimed at enhancing lifestyle habits.
Initially, smoking and drinking habits were linked to increased mortality from malignant tumors in each prefecture. Concerning smoking habits, several previous studies have indicated that smoking elevates the risk of malignant tumors [9, 10], aligning with the findings of this study. Moreover, there is an association between smoking rates and cancer mortality rates in the prefectures [11], implying that smoking habits contribute to mortality disparities in malignant tumors across prefectures. To decrease the smoking prevalence in the region, implementing non-smoking regulations in public spaces and workplaces has proven effective [12], and similar measures are anticipated to lower smoking rates in each prefecture.
Regarding daily drinking habits, moderate to heavy alcohol consumption poses a risk for cancer at various sites [13], with even small amounts of alcohol posing a risk for pharyngeal and esophageal cancer [14]. These prior studies also indicate that drinking habits are linked to mortality variations among prefectures for malignant tumors. The frequency and volume of alcohol intake are influenced by the density and operating hours of alcohol establishments in the vicinity [15], suggesting that imposing restrictions can reduce alcohol consumption in the area [16]. In prefectures with a high prevalence of habitual drinkers, measures aimed at limiting alcohol availability are likely to reduce the proportion of habitual drinkers.
Subsequently, lifestyle habits linked to increased mortality from heart disease included factors associated with weight gain since the age of 20, speed of food consumption, and meal duration. Specifically, concerning weight gain since the age of 20, research has demonstrated that individuals who have gained 10kg or more since the age of 20, face a risk of coronary heart disease, such as myocardial infarction, approximately two times higher than those who have not [17, 18], with the risk of developing cardiovascular disease being around 1.2 times higher. Irregular eating patterns also pose a risk for heart disease [19], and previous studies indicate an association between a higher proportion of individuals with increased body weight and elevated mortality from heart disease in prefectures where irregular meal times are prevalent. While there is limited research on strategies to combat obesity in adults at the community level, reports suggest that initiatives like nutrition education programs and the dissemination of materials outlining the benefits of exercise have led to a decrease in the prevalence of metabolic syndrome in local communities [20]. Therefore, it is reasonable to anticipate that anti-obesity measures can be effective in addressing these concerns. Conversely, concerning the correlation between food intake speed and heart disease, as per the responses to the Specified Medical Checkups Questionnaire utilized in this study, the highest percentage of individuals reported having a normal eating speed compared to others across all prefectures. It is improbable that a higher percentage of individuals reporting a normal eating speed compared to others would increase the mortality rate of heart disease. It is plausible that unmeasured confounding variables not accounted for in the current study’s analysis may have influenced the outcomes, highlighting a limitation of the study’s design. Future research investigating the link between individual eating speed and the risk of heart disease development is essential to elucidate how eating speed impacts the onset of heart disease.
Lastly, lifestyle habits associated with increased mortality from cerebrovascular disease included not yet improving lifestyle and insufficient rest during sleep. Firstly, concerning the link between lifestyle enhancement and cerebrovascular disease, lifestyle improvements are effective in stroke prevention [21]. Therefore, it is presumed that in prefectures with a significant number of individuals not improving their lifestyle, there is a higher incidence of strokes leading to elevated mortality rates. In this analysis, we categorized the respondents based on whether they had improved their lifestyle at the time of questionnaire completion, regardless of their willingness to make lifestyle changes. Consequently, some respondents who had not improved their lifestyle habits were also grouped among those who ‘intended to improve’. To promote lifestyle enhancements, social support facilitating goal-setting and providing appropriate feedback is effective [22], and continuous health guidance is imperative. Next, regarding the correlation between sleep and stroke, previous studies have indicated that adequate sleep duration is a factor that reduces the risk of stroke [23], a finding that contrasts with earlier research. The questionnaire employed in our study inquired about individuals feeling rested after sleep, rather than directly addressing sleep duration. Hence, the results cannot be universally compared with those of prior studies. Future analyses utilizing data on sleep duration by prefecture will elucidate the relationship between sleep-related lifestyles and disease mortality in each prefecture, enabling the consideration of measures to mitigate mortality differences among prefectures.
As demonstrated, numerous questions in the Specified Health Check-Up Questionnaire pertain to preventing the onset of the three major diseases, indicating the potential effectiveness of local health initiatives and health guidance based on questionnaire responses. However, certain questions yielded results differing from previous studies, and some questions did not align with previous findings regarding associations with the three major causes of death. This underscores the necessity for further research on the link between lifestyle habits and the three major causes of death at the individual level.
A limitation of this study is its reliance on prefecture-based regional correlation analysis using NDB Open Data. Since it does not establish associations at the individual level, causal relationships cannot be inferred from the study results. Furthermore, the NDB data utilized in this study represents a basic tabulation of results from individuals who underwent specific health check-ups. The analysis assumes that individuals who passed away had lifestyles similar to those who underwent health check-ups in the same year when calculating the age-adjusted mortality rate. Moving forward, ongoing comparisons between questionnaire response rates and age-adjusted mortality rates will be conducted using accumulated data. Detailed analyses will be carried out to generate valuable insights for enhancing lifestyle practices in community health initiatives. Ongoing analysis using accumulated data is recommended for future endeavors. Also, the Specified Health Check-Up Questionnaire is deemed suitable for pinpointing lifestyle habits associated with these mortality rates, thereby enabling the consideration of essential measures.
Conclusion
Variations in lifestyle across each prefecture are linked to differences in mortality rates for malignant tumors, heart disease, and cerebrovascular disease by prefecture.
Acknowledgments: We express our gratitude to the Ministry of Health, Labour, and Welfare (MHLW) for making the data utilized in this study publicly accessible.
Ethical Permissions: Since this study solely analyzed published materials, no application was submitted to a research ethics committee.
Conflicts of Interest: No conflicts of interest to disclose.
Authors’ Contribution: Ryosuke O (First Author), Introduction Writer/Main Researcher/Discussion Writer (65%); Kazuma Sh (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (35%)
Funding/Support: Nothing declared by the authors.
Malignant tumors, heart disease, and cerebrovascular disease stand as the top three causes of death in Japan, with these diseases maintaining their leading positions for over 50 years [1]. Mortality rates for these conditions exhibit variations among prefectures within Japan. For instance, Aomori Prefecture records the highest mortality rate for malignant tumors (707 deaths per 100,000 persons), while Nagano Prefecture reports the lowest (486 deaths per 100,000 persons) [1]. Aomori Prefecture also demonstrates the highest death rate from heart disease (190 deaths), contrasting with Shiga Prefecture, which has the lowest rate (103 deaths). Similarly, Ehime Prefecture exhibits the highest rate of mortality from cerebrovascular disease (288 deaths), while Fukuoka Prefecture displays the lowest (154 deaths) [1]. Consequently, there exists an almost twofold difference in mortality rates per 100,000 persons for the same disease across prefectures. To diminish deaths from these three diseases in each prefecture, it is crucial to pinpoint the factors contributing to the mortality rate disparities among prefectures.
Previous studies have indicated that the disparities in mortality rates among prefectures are linked to factors, such as salt intake, weather conditions, and living environments [2-4]. Conversely, deaths attributed to malignant tumors, heart disease, and cerebrovascular disease have been correlated with lifestyle elements like dietary choices and exercise habits [5, 6]. Hence, variations in lifestyle practices across regions may also contribute to the differences in mortality rates among prefectures. Therefore, it is essential to consider the impact of lifestyle when examining the variations in mortality rates among prefectures. Nevertheless, a detailed analysis concerning the differences in mortality rates among prefectures and lifestyle has not been conducted due to the limited availability of nationwide data on individual-level lifestyle habits.
In Japan, specific health checkups are conducted for individuals aged 40 to 74 years to identify those in need of health education aimed at reducing the prevalence of metabolic syndrome and its precursor. These specific health checkups have facilitated the collection of nationwide data on individual lifestyle habits. These data have been publicly available as open data since the fiscal year 2016 under the name of the Japanese National Database of Health Insurance Claims and Specific Health Checkups (NDB). The NDB Open Data is categorized by prefecture, enabling comparisons of lifestyle habits among health checkup participants aged 40 to 74 based on the specific health checkup data. The NDB Open Data is organized by prefecture, allowing for inter-prefecture comparisons. Therefore, this study aimed to elucidate the lifestyle habits associated with the three primary causes of mortality by prefecture, utilizing the 2nd NDB Open Data and the 2015 Vital Statistics.
Instrument and Methods
Data source
This descriptive study utilized the Specified Medical Checkups Questionnaire (items 1-22) from the 2nd NDB Open Data and the age-adjusted mortality rates by prefecture from the 2015 Vital Statistics and was conducted in April 2023 [7, 8]. Both of these datasets represent the most recent available data that can be compared for the same fiscal year.
The questionnaire content used in this analysis aligned with the questions presented to examinees during the specific health check-up.
The data used were collected and published by a government organization; thus, they were already processed. Therefore, no inclusion or exclusion criteria were set for the data used. Regarding sample size, we used a regional correlation design, and examined whether lifestyle habits influenced the mortality rate in each region. Therefore, we did not consider the sample size.
Data extraction and processing
The response data by prefecture for the Specified Medical Checkups Questionnaire in the 2nd NDB Open Data represent individuals who underwent the specified medical checkups, thus displaying values solely for the age group ranging from 40 to 74 years old. Consequently, the response rate (per 100,000 population) for each questionnaire was computed following age adjustment through the direct method, with data confined to the age bracket of 40 to 74 years old, utilizing the 1985 model as the reference population.
When determining the response rate, most questionnaires documented the number of respondents using binary values of ‘yes’ and ‘no’. For these questionnaire items, the percentage of respondents who answered ‘yes’ was calculated. Conversely, certain items recorded the number of respondents with multiple options instead of a binary value (e.g., question 14). For such multiple-choice questions, the proportion of respondents for each option was computed. However, for question 21, the responses were categorized as “I do not intend to improve” (I), “I intend to improve (generally within 6 months)” (II), and “I intend to improve in the near future and have started gradually” (III).
Subsequently, age-adjusted mortality rates by prefecture were obtained for malignant tumors, heart disease, and cerebrovascular disease. These data encompass age-adjusted and age-group-specific mortality rates for 2015 categorized by prefecture, sex, and age group. The age-adjusted mortality data are standardized across all age groups, rendering them incomparable with the NDB Open Data due to differing adjustment conditions. Therefore, age adjustment was confined to the age group between 40 and 74 years to align the adjustment conditions with the NDB open data. Given that age-adjusted mortality rates by age group (per 100,000 population) are outlined in the age-adjusted mortality rates by prefecture, age adjustment was conducted utilizing the 1985 model as the reference population and the direct method to derive age-adjusted mortality rates for the age group between 40 and 74 years
Analysis methods
Multiple regression analysis was performed to elucidate the relationship between the mortality rates of the three primary causes of death by prefecture and the response status to the Specified Medical Checkups Questionnaire. Age-adjusted mortality rates for malignant tumors, heart disease, and cerebrovascular disease were utilized as the dependent variables in the multiple regression analysis. The age-adjusted response rate (per 100,000 population) to the Specified Medical Checkups Questionnaire served as the independent variable. However, as certain questionnaire items, such as medical history and medication history, were deemed to have minimal relevance to lifestyle habits, items 1-7 in Table 1 were excluded from the independent variables in the current analysis.
In the multiple regression analysis, redundant independent variables were eliminated using the stepwise variable selection method. To assess multicollinearity among independent variables, the variance inflation factor (VIF) for each independent variable was calculated, and independent variables with a VIF exceeding ten were excluded before applying the stepwise variable selection method. All analyses were carried out using R version 4.0.3 with a significance level of 5%.
Findings
The results presented in Table 1 were obtained through multiple regression analysis utilizing the stepwise method, with the mortality rates of malignant tumors, heart disease, and cerebrovascular disease as the dependent variables, and the number of respondents to items 8-22 of the Specified Medical Checkups Questionnaire as the independent variable.
Table 1. Results of multiple regression analysis for three major causes of death
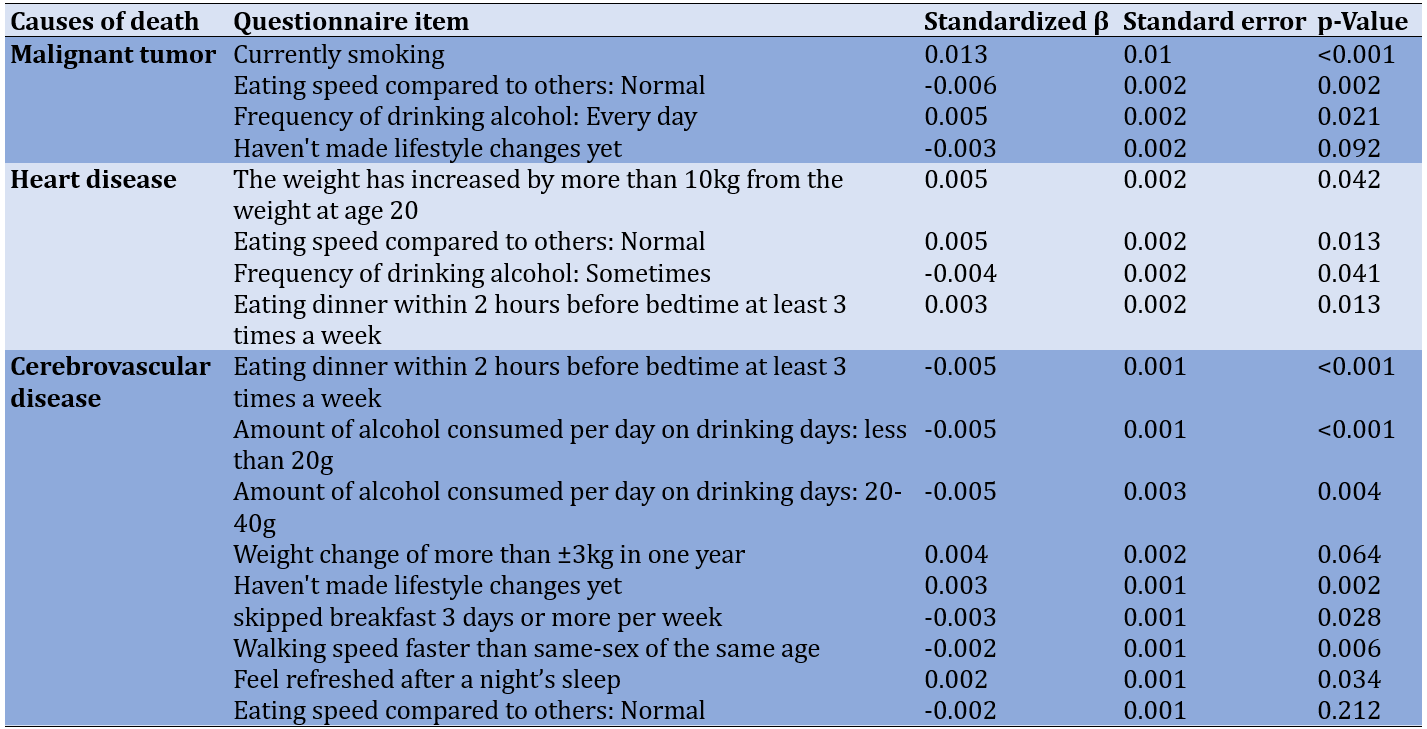
For mortality from malignant tumors by prefecture, significant positive associations were observed with smoking (β=0.013) and frequent daily drinking (β=0.005), while significant negative associations were noted for normal eating speed (β=-0.006) compared to others.
Regarding mortality from heart disease by prefecture, significant positive associations were identified for an increase of more than 10kg from body weight at age 20 (β=0.004), normal eating speed compared to controls (β=0.005), and having dinner at least two hours before bedtime three or more times a week (β=0.003). A significant negative association was found for occasional weekly drinking (β=0.004).
In relation to mortality from cerebrovascular disease by prefecture, significant positive associations were observed for items, such as not yet improving lifestyle (β=0.003) and getting enough rest from sleep (β=0.002). Conversely, significant negative associations were found for consuming less than one drink a day (β=-0.005) or 1-2 drinks a day (β=-0.005), skipping breakfast three or more times a week (β=-0.003), walking faster than their age-mates (β=-0.002), and eating at a normal speed compared to others (β=-0.002).
Discussion
To investigate the factors influencing the regional variations in the top three causes of death in Japan, the findings from the specific health check-ups by the prefecture as published in the NDB open data were utilized and analyzed. The outcomes indicated that certain lifestyle habits were associated with the mortality rates of these diseases across prefectures. These findings imply that lifestyle habits play a role in the divergence of mortality rates among prefectures, alongside factors highlighted in prior research, such as climatic conditions. The lifestyle habits pinpointed in this study will be deliberated upon in relation to the effectiveness of measures aimed at enhancing lifestyle habits.
Initially, smoking and drinking habits were linked to increased mortality from malignant tumors in each prefecture. Concerning smoking habits, several previous studies have indicated that smoking elevates the risk of malignant tumors [9, 10], aligning with the findings of this study. Moreover, there is an association between smoking rates and cancer mortality rates in the prefectures [11], implying that smoking habits contribute to mortality disparities in malignant tumors across prefectures. To decrease the smoking prevalence in the region, implementing non-smoking regulations in public spaces and workplaces has proven effective [12], and similar measures are anticipated to lower smoking rates in each prefecture.
Regarding daily drinking habits, moderate to heavy alcohol consumption poses a risk for cancer at various sites [13], with even small amounts of alcohol posing a risk for pharyngeal and esophageal cancer [14]. These prior studies also indicate that drinking habits are linked to mortality variations among prefectures for malignant tumors. The frequency and volume of alcohol intake are influenced by the density and operating hours of alcohol establishments in the vicinity [15], suggesting that imposing restrictions can reduce alcohol consumption in the area [16]. In prefectures with a high prevalence of habitual drinkers, measures aimed at limiting alcohol availability are likely to reduce the proportion of habitual drinkers.
Subsequently, lifestyle habits linked to increased mortality from heart disease included factors associated with weight gain since the age of 20, speed of food consumption, and meal duration. Specifically, concerning weight gain since the age of 20, research has demonstrated that individuals who have gained 10kg or more since the age of 20, face a risk of coronary heart disease, such as myocardial infarction, approximately two times higher than those who have not [17, 18], with the risk of developing cardiovascular disease being around 1.2 times higher. Irregular eating patterns also pose a risk for heart disease [19], and previous studies indicate an association between a higher proportion of individuals with increased body weight and elevated mortality from heart disease in prefectures where irregular meal times are prevalent. While there is limited research on strategies to combat obesity in adults at the community level, reports suggest that initiatives like nutrition education programs and the dissemination of materials outlining the benefits of exercise have led to a decrease in the prevalence of metabolic syndrome in local communities [20]. Therefore, it is reasonable to anticipate that anti-obesity measures can be effective in addressing these concerns. Conversely, concerning the correlation between food intake speed and heart disease, as per the responses to the Specified Medical Checkups Questionnaire utilized in this study, the highest percentage of individuals reported having a normal eating speed compared to others across all prefectures. It is improbable that a higher percentage of individuals reporting a normal eating speed compared to others would increase the mortality rate of heart disease. It is plausible that unmeasured confounding variables not accounted for in the current study’s analysis may have influenced the outcomes, highlighting a limitation of the study’s design. Future research investigating the link between individual eating speed and the risk of heart disease development is essential to elucidate how eating speed impacts the onset of heart disease.
Lastly, lifestyle habits associated with increased mortality from cerebrovascular disease included not yet improving lifestyle and insufficient rest during sleep. Firstly, concerning the link between lifestyle enhancement and cerebrovascular disease, lifestyle improvements are effective in stroke prevention [21]. Therefore, it is presumed that in prefectures with a significant number of individuals not improving their lifestyle, there is a higher incidence of strokes leading to elevated mortality rates. In this analysis, we categorized the respondents based on whether they had improved their lifestyle at the time of questionnaire completion, regardless of their willingness to make lifestyle changes. Consequently, some respondents who had not improved their lifestyle habits were also grouped among those who ‘intended to improve’. To promote lifestyle enhancements, social support facilitating goal-setting and providing appropriate feedback is effective [22], and continuous health guidance is imperative. Next, regarding the correlation between sleep and stroke, previous studies have indicated that adequate sleep duration is a factor that reduces the risk of stroke [23], a finding that contrasts with earlier research. The questionnaire employed in our study inquired about individuals feeling rested after sleep, rather than directly addressing sleep duration. Hence, the results cannot be universally compared with those of prior studies. Future analyses utilizing data on sleep duration by prefecture will elucidate the relationship between sleep-related lifestyles and disease mortality in each prefecture, enabling the consideration of measures to mitigate mortality differences among prefectures.
As demonstrated, numerous questions in the Specified Health Check-Up Questionnaire pertain to preventing the onset of the three major diseases, indicating the potential effectiveness of local health initiatives and health guidance based on questionnaire responses. However, certain questions yielded results differing from previous studies, and some questions did not align with previous findings regarding associations with the three major causes of death. This underscores the necessity for further research on the link between lifestyle habits and the three major causes of death at the individual level.
A limitation of this study is its reliance on prefecture-based regional correlation analysis using NDB Open Data. Since it does not establish associations at the individual level, causal relationships cannot be inferred from the study results. Furthermore, the NDB data utilized in this study represents a basic tabulation of results from individuals who underwent specific health check-ups. The analysis assumes that individuals who passed away had lifestyles similar to those who underwent health check-ups in the same year when calculating the age-adjusted mortality rate. Moving forward, ongoing comparisons between questionnaire response rates and age-adjusted mortality rates will be conducted using accumulated data. Detailed analyses will be carried out to generate valuable insights for enhancing lifestyle practices in community health initiatives. Ongoing analysis using accumulated data is recommended for future endeavors. Also, the Specified Health Check-Up Questionnaire is deemed suitable for pinpointing lifestyle habits associated with these mortality rates, thereby enabling the consideration of essential measures.
Conclusion
Variations in lifestyle across each prefecture are linked to differences in mortality rates for malignant tumors, heart disease, and cerebrovascular disease by prefecture.
Acknowledgments: We express our gratitude to the Ministry of Health, Labour, and Welfare (MHLW) for making the data utilized in this study publicly accessible.
Ethical Permissions: Since this study solely analyzed published materials, no application was submitted to a research ethics committee.
Conflicts of Interest: No conflicts of interest to disclose.
Authors’ Contribution: Ryosuke O (First Author), Introduction Writer/Main Researcher/Discussion Writer (65%); Kazuma Sh (Second Author), Methodologist/Assistant Researcher/Discussion Writer/Statistical Analyst (35%)
Funding/Support: Nothing declared by the authors.
Article Type: Descriptive & Survey |
Subject:
Healthy Life Style
Received: 2024/01/4 | Accepted: 2024/04/22 | Published: 2024/06/21
Received: 2024/01/4 | Accepted: 2024/04/22 | Published: 2024/06/21
References
1. Ministry of Health, Labour and Welfare. Summary of the 2021 vital statistics monthly report (approximate figures). Tokyo: Ministry of Health, Labour and Welfare; 2022. [Japanese] [Link]
2. Ikeda K, Ueki T. The relationship between mortality and nutrition in Japan. Tokyo Metrop Res Lab Public Health. 2001;52:293-8. [Japanese] [Link]
3. Hayama, Hirofumi, Kamazawa, Yuki, Matsumura, Ryosuke, et al. Effects of climatic conditions and place of death on causes of death. Indic Health. 2011;58(13):1-6. [Japanese] [Link]
4. Ohashi Y. Relationships between acute cardiovascular or cerebrovascular diseases and monthly meteorological or annual climatic changes. J Environ Inform Sci. 2019;33:301-6. [Japanese] [Link]
5. Inoue M, Yamamoto S, Kurahashi N, Iwasaki M, Sasazuki S, Tsugane S, et al. Daily total physical activity level and total cancer risk in men and women: Results from a large-scale population-based cohort study in Japan. Am J Epidemiol. 2008;168(4):391-403. [Link] [DOI:10.1093/aje/kwn146]
6. WCRF. Wholegrains, vegetables and fruit and the risk of cancer. London: World Cancer Research Fund International; 2020. [Link]
7. Ministry of Health, Labour and Welfare. 2nd NDB Open Data; 2012 [cited 2023/10/5]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177221.html. [Japanese] [Link]
8. General Contact Point for Government Statistics. 2015 Age-adjusted mortality rates by prefecture. Tokyo: e-Stat [cited 2023/10/10]. Available from: https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450013&tstat=000001102115&cycle=7&year=20150&month=0&tclass1val=0 [Japanese] [Link]
9. Gandini S, Botteri E, Iodice S, Boniol M, Lowenfels AB, Maisonneuve P, et al. Tobacco smoking and cancer: A meta-analysis. Int J Cancer. 2008;122(1):155-64. [Link] [DOI:10.1002/ijc.23033]
10. Macacu A, Autier P, Boniol M, Boyle P. Active and passive smoking and risk of breast cancer: A meta-analysis. Breast Cancer Res Treat. 2015;154(2):213-24. [Link] [DOI:10.1007/s10549-015-3628-4]
11. Ikegami T. Cancer mortality by prefecture correlates with smoking prevalence. Indic Health. 2019;66(4):43-7. [Japanese] [Link]
12. Wilson LM, Avila Tang E, Chander G, Hutton HE, Odelola OA, Elf JL, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: A systematic review. J Environ Public Health. 2012;2012:961724. [Link] [DOI:10.1155/2012/961724]
13. Papadimitriou N, Markozannes G, Kanellopoulou A, Critselis E, Alhardan S, Karafousia V, et al. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat Commun. 2021;12(1):4579. [Link] [DOI:10.1038/s41467-021-24861-8]
14. Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. Light alcohol drinking and cancer: A meta-analysis. Ann Oncol. 2013;24(2):301-8. [Link] [DOI:10.1093/annonc/mds337]
15. Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: Impacts on alcohol consumption and damage: A systematic review. Alcohol Alcohol. 2009;44(5):500-16. [Link] [DOI:10.1093/alcalc/agp054]
16. Sherk A, Stockwell T, Chikritzhs T, Andréasson S, Angus C, Gripenberg J, et al. Alcohol consumption and the physical availability of take-away alcohol: Systematic reviews and meta-analyses of the days and hours of sale and outlet density. J Stud Alcohol Drugs. 2018;79(1):58-67. [Link] [DOI:10.15288/jsad.2018.79.58]
17. Chei CL, Iso H, Yamagishi K, Inoue M, Tsugane S. Body mass index and weight change since 20 years of age and risk of coronary heart disease among Japanese: The Japan public health center-based study. Int J Obes. 2008;32(1):144-51. [Link] [DOI:10.1038/sj.ijo.0803686]
18. Okada C, Kubota Y, Eshak ES, Cui R, Tamakoshi A, Iso H, et al. Weight change and mortality from cardiovascular diseases: The Japan collaborative cohort study. J Atheroscler Thromb. 2021;28(1):25-33. [Link] [DOI:10.5551/jat.54114]
19. Cahill LE, Chiuve SE, Mekary RA, Jensen MK, Flint AJ, Hu FB, et al. Prospective study of breakfast eating and incident coronary heart disease in a cohort of male US health professionals. Circulation. 2013;128(4):337-43. [Link] [DOI:10.1161/CIRCULATIONAHA.113.001474]
20. Azizi F, Mirmiran P, Momenan AA, Hadaegh F, Habibi Moeini A, Hosseini F, et al. The effect of community-based education for lifestyle intervention on the prevalence of metabolic syndrome and its components: Tehran lipid and glucose study. Int J Endocrinol Metab. 2013;11(3):145-53. [Link] [DOI:10.5812/ijem.5443]
21. Sarikaya H, Ferro J, Arnold M. Stroke prevention--medical and lifestyle measures. Eur Neurol. 2015;73(3-4):150-7. [Link] [DOI:10.1159/000367652]
22. Lachman ME, Lipsitz L, Lubben J, Castaneda-Sceppa C, Jette AM. When adults don't exercise: Behavioral strategies to increase physical activity in sedentary middle-aged and older adults. Innov Aging. 2018;2(1):igy007. [Link] [DOI:10.1093/geroni/igy007]
23. Fan M, Sun D, Zhou T, Heianza Y, Lv J, Li L, et al. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385292 UK biobank participants. Eur Heart J. 2020;41(11):1182-9. [Link] [DOI:10.1093/eurheartj/ehz849]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







