Volume 12, Issue 1 (2024)
Health Educ Health Promot 2024, 12(1): 145-152 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mousazadeh Y, Najafi E, Salmani R, MoradAbadi A, Salimi Kivi M, Salmani R. Association of Marital Satisfaction and Sexual Health Literacy with Fertility among Iranian Couples. Health Educ Health Promot 2024; 12 (1) :145-152
URL: http://hehp.modares.ac.ir/article-5-73109-en.html
URL: http://hehp.modares.ac.ir/article-5-73109-en.html
1- Department of Public Health, Khalkhal University of Medical Sciences, Khalkhal, Iran
2- Department of Midwifery, Faculty of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran
3- Department of Medical Laboratory, Khomein University of Medical Sciences, Khomein, Iran
4- Department of Midwifery, Khalkhal University of Medical Sciences, Khalkhal, Iran
2- Department of Midwifery, Faculty of Nursing and Midwifery, Zanjan University of Medical Sciences, Zanjan, Iran
3- Department of Medical Laboratory, Khomein University of Medical Sciences, Khomein, Iran
4- Department of Midwifery, Khalkhal University of Medical Sciences, Khalkhal, Iran
Full-Text [PDF 635 kb]
(3000 Downloads)
| Abstract (HTML) (1511 Views)
Full-Text: (189 Views)
Introduction
Happiness and a desirable quality of life are relative concepts, as each person experiences happiness uniquely. Indeed, happiness and activity are fundamental psychological needs that constantly occupy the human mind due to their significant impact on people's lives [1, 2]. Many people sometimes experience thoughts and worries related to their health, leading to a decreased quality of life and, consequently, reduced marital satisfaction. Marital satisfaction is a significant and complex aspect of a marital relationship [3]. It expresses how the expectations of sexual partners are met by each other, and also it can play an important role in family health [4]. Sexual satisfaction is one of the individual needs and interpersonal interactions that may have a close relationship with health society [5]. Satisfying sexual relations protects a person against many disorders and diseases [5]. Also, it can affect life satisfaction, job satisfaction, income satisfaction, success, and mental health [6]. Couples with high perceived marital satisfaction have a lot of agreement with each other. They are also satisfied with the type and level of their relationship, the type and quality of spending their leisure time, and effectively their time and financial issues [7]. Studies show that psychological factors can play a role in the creation of infertility and can be considered as its result. In this regard, many pieces of evidence show that psychological problems caused by infertility can be a contributing factor in the aggravation of infertility [3].
Many sexual problems are caused by ignorance and false beliefs about sexual relationships [8]. One of the concepts raised in this field is sexual health literacy (SHL), which refers to a set of knowledge, attitudes and beliefs, motivations, and personal abilities in accessing, understanding, appraising, and applying information related to sexual health [9]. An adequate level of sexual health literacy (SHL) enhances a person's ability to analyze, judge, discuss, decide, and change sexual behavior. It also empowers individuals to ensure, maintain, and improve their sexual health [10]. Insufficient health literacy can lead to dissatisfaction in the couple's relationship and problems in their married life. Therefore, improving SHL level is an effective step towards improving marital satisfaction and quality of life [11]. Various studies have highlighted many benefits of sexual and reproductive health literacy. These benefits include improving the ability to understand and evaluate risks related to sexual health, delaying the first sexual experience, selecting low-risk sexual partners, practicing safe sex, reducing unwanted pregnancies and sexually transmitted diseases, fostering a correct understanding of responsibilities and duties in sexual relationships, providing the opportunity to properly express gender roles, enhancing couples' sexual interactions, promoting individual sexual health, and ultimately improving family and social health [12].
Advances in assisted reproductive equipment and techniques help infertile couples manage and reduce their fertility problems [13]. The prevalence rate of infertility is 12 to 15 percent worldwide according to the report of the World Health Organization (WHO) [14]. Infertility rate is reported to be 2% to 20% in Iran [14]. Previous studies on marital satisfaction in infertile people yielded two different views in this regard. On one hand, infertility is regarded as an experience that fosters couple growth [15]. It serves as a challenge that enhances cooperation between partners, as they navigate the infertility crisis together, engage in long-term treatments, make joint decisions, and share their feelings. This collaborative process can result in equal or even greater marital satisfaction compared to fertile couples [16]. On the other hand, medical interventions for infertility can impact the quality of life of infertile couples and their needs [17], potentially leading to reduced marital satisfaction [18]. However, it's crucial to recognize that infertile couples constitute a limited but significant group of patients who require understanding and support. Three key points can be raised regarding marital satisfaction. First, a lack of marital satisfaction may lead to dissatisfaction with married life and a loss of emotional connection between couples. Second, studies suggest that sexual health literacy (SHL) can promote and improve marital satisfaction. Third, fertility and infertility have varying effects on marital satisfaction. Given these factors, conducting a study on this topic can provide valuable data on the elements influencing marital satisfaction, as it examines the impacts of fertility, infertility, and sexual health literacy simultaneously. This data can be used to design relevant interventions.
Therefore, the aims of this study were to compare the SHL level and marital satisfaction in fertile and infertile couples and to investigate the relationship between these parameters.
Instrument & Methods
Study design
This was a descriptive-analytical cross-sectional study conducted in Guilan and Ardabil provinces in the north, and northwest of Iran during 2020-2021.
Study population and sample
The study population included eligible infertile couples who were referred to Mehr Infertility Institute in Rasht, Guilan province, Iran, for the treatment of their fertility problems, and fertile couples referring to healthcare centers in the north and northwest of Iran.
The samples were selected by convenience sampling method. The sample size was determined by the average difference in two independent populations Formula [18] (n=500, 250 people per group). However, 5% was added to this number to increase reliability and compensate for the possible dropout due to reasons like incomplete questionnaires. The variance of the first and second groups was 12.4 and 12.3, respectively.
The study inclusion criteria for the infertile group included primary infertility, having female or male (or both) infertility, and not having chronic diseases. The study inclusion criteria for the fertile group also included the absence of chronic diseases and secondary infertility and having at least one child. Physical or mental disorders, death of close relatives during the last six months, and adoption were among the study exclusion criteria.
The samples were selected after obtaining the necessary permissions from the administrators of Khalkhal University of Medical Sciences and presenting a letter of introduction and obtaining the approval form the infertility institute and health care centers. Written informed consent was obtained from all participants, and this method of consent was also approved by the relevant Institutional Review Board (Ethics Committee of Khalkhal University of Medical Sciences).
Study instruments
Three questionnaires were used in the present study. The demographic questionnaire included questions on age, education level, employment status, duration of marriage, duration of infertility, income level, type of delivery, and contraceptive method (in fertile people). The second questionnaire was the sexual health literacy for adults (SHELA) questionnaire. This 40-item questionnaire is designed by Masoumi et al. [19]. It consists of four dimensions, including access (items 1 to 7), reading and writing (items 8 to 25), analysis and appraisal (items 26 to 30), and application skills (items 31 to 40). Each item is scored based on a five-point Likert scale, ranging from completely agree to completely disagree. The raw score of each subscale is obtained from the algebraic sum of the scores.
To calculate the total score, the scores of subscales are added based on the 0-100 range and divided by the number of subscales (4). The content validity based on the Content Validity Index (CVI) and Content Validity Ratio (CVR) for all items was 0.84 and 0.81, respectively. Exploratory factor analysis explained 68.1% of the variance. Convergent validity of the questionnaire showed the range of 0.31 to 0.70. The reliability of the scale was assessed by Cronbach’s alpha. It ranged from 0.84 to 0.94. Also, this questionnaire showed a high Intraclass Correlation Coefficient (ICC), ranging from 0.90 to 0.97 [19].
The third questionnaire was the enrich marital satisfaction scale-short form. It has been used as a valid research instrument in many research and clinical studies. Olson et al. used this scale to assess marital satisfaction and believed that this scale is sensitive to the changes occurring in the family [20]. This scale consists of 10 satisfaction questions, which are scored based on a five-point Likert scale, ranging from completely agree (5) to completely disagree (1), and thus, higher scores indicate more marital satisfaction. Also, questions 1, 3, 5, 8, and 9 are scored reversely. Arab Alidousti et al. confirmed the reliability and validity of the Persian version of this questionnaire [21]. Face validity is also assessed by qualitative method, receiving the opinions of five married women and five men over 18 years of age. Cronbach's alpha value is also 0.74 in this study [21].
Statistical analysis
After assessing the normality of the data distribution by the Kolmogorov-Smirnov test, independent T-test, and Chi-square test were employed to compare demographic parameters in fertile and infertile couples. Pearson's correlation test was also used to investigate the relationship between SHL, and marital satisfaction. A multivariate regression test was also applied to determine the determinants of marital satisfaction. Data analysis was carried out using descriptive statistics and average estimation in different groups. All statistical analysis was conducted using SPSS 26 Software. A p-value of 0.05 was considered statistically significant.
Findings
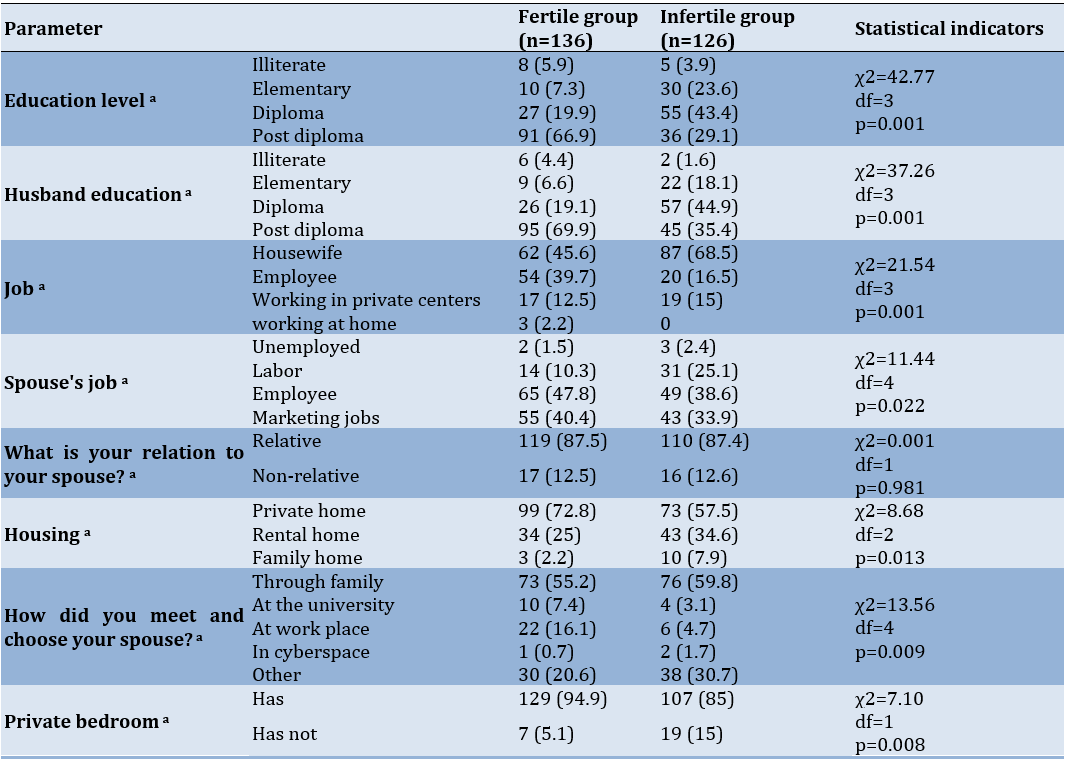
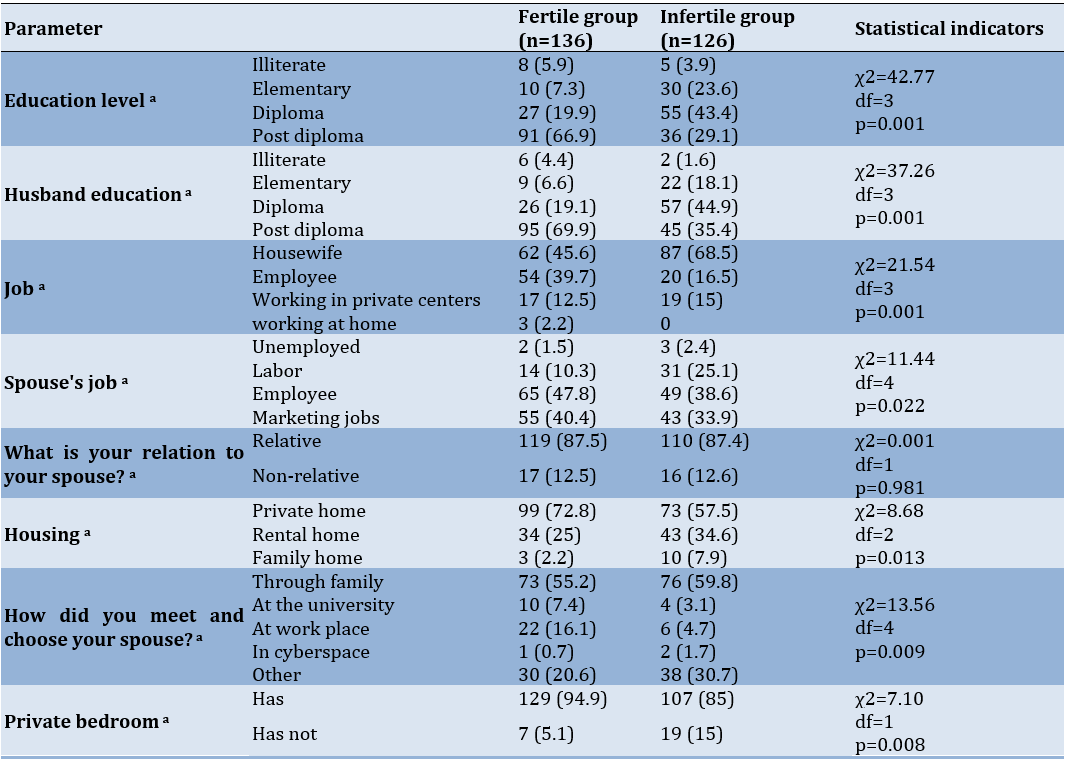
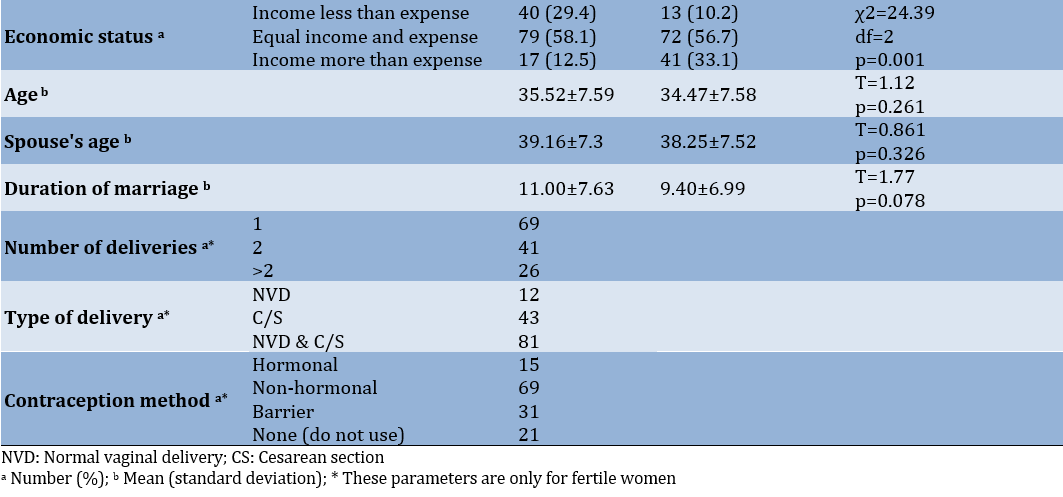
The study population included 126 infertile couples (n=252) and 136 fertile ones (n=272) and their characteristics were collected (Table 1). The mean±standard deviation (SD) of the age of the fertile and infertile women was 35.52±7.59 and 34.47±7.58 years, respectively, which indicated no statistically significant difference (t=1.12; p=0.261). Also, the mean±SD of the age of the fertile and infertile women's spouses was 39.16±7.3 and 38.25±7.52 years, respectively, which also showed no statistically significant difference (t=0.86; p=0.326). Almost two-thirds (66.9%) of fertile women had a higher education level, but there was a different situation in infertile women, so that only 29.1% of the respondents had a higher education level. Most of the husbands of fertile women had higher education levels, whereas 35.4% of the husbands of infertile women had higher education levels, and also approximately 45% earned high school diplomas (Table 1).
Table 1. Individual-social characteristics of the study participants.
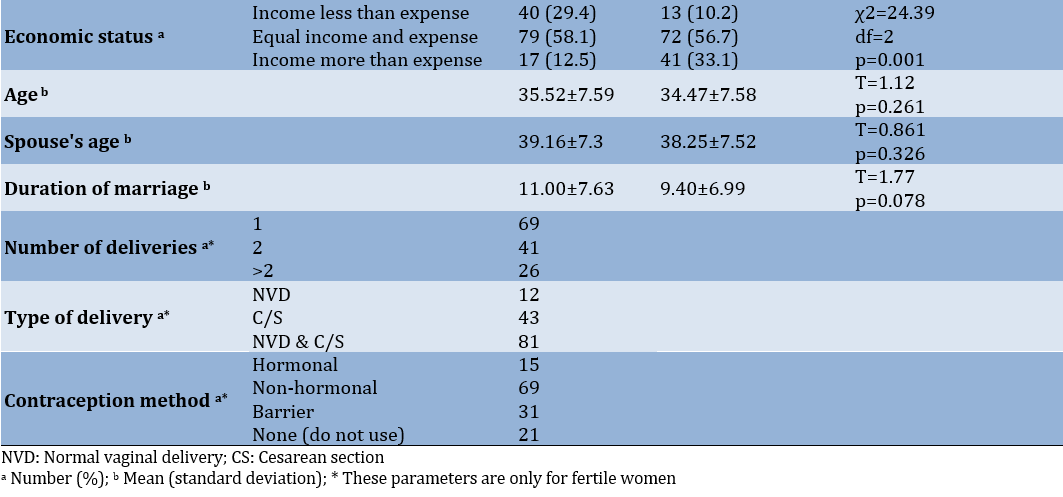
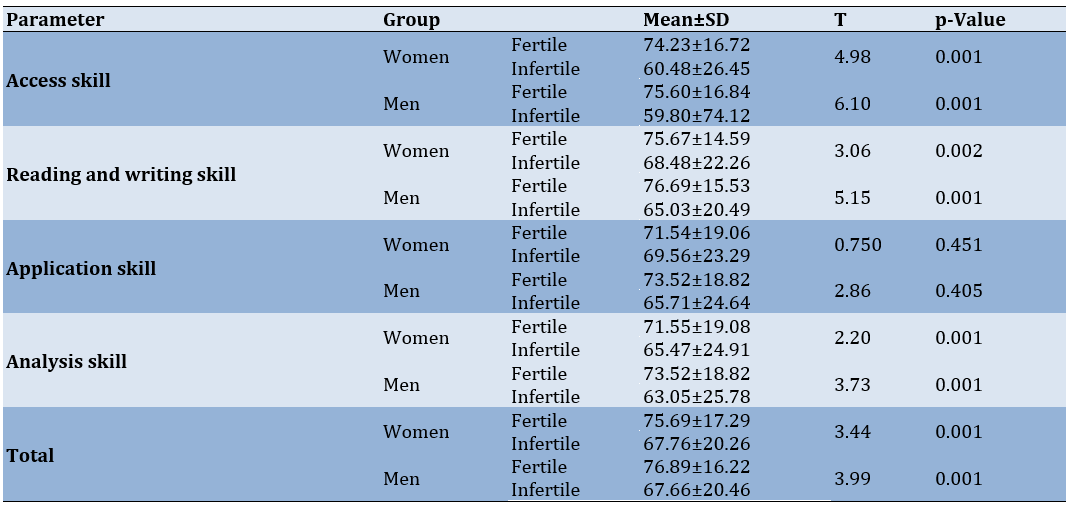
This study indicated a higher SHL level in fertile women than infertile ones. The mean±SD of SHL score in fertile and infertile men was statistically significant (p=0.001) and indicated a higher SHL level in fertile men than infertile ones. The mean scores of all SHL dimensions in both fertile women and fertile men were higher than those in infertile ones, which was statistically significant in all dimensions, except for the application skill dimension (Table 2). The highest mean score was related to the reading and writing skill dimension in both fertile women and men, and the application skill had the lowest score in both fertile women and men. Both infertile women and men have the highest scores in application skills. The lowest score in these two groups was related to access skills (Table 2).
Table 2. Comparison of mean and standard deviation of SHL dimensions in fertile and infertile couples
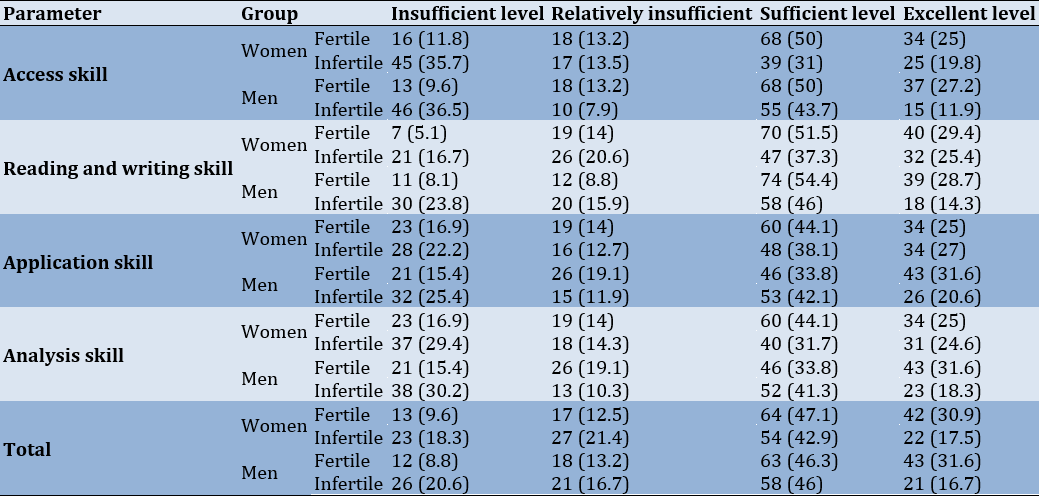
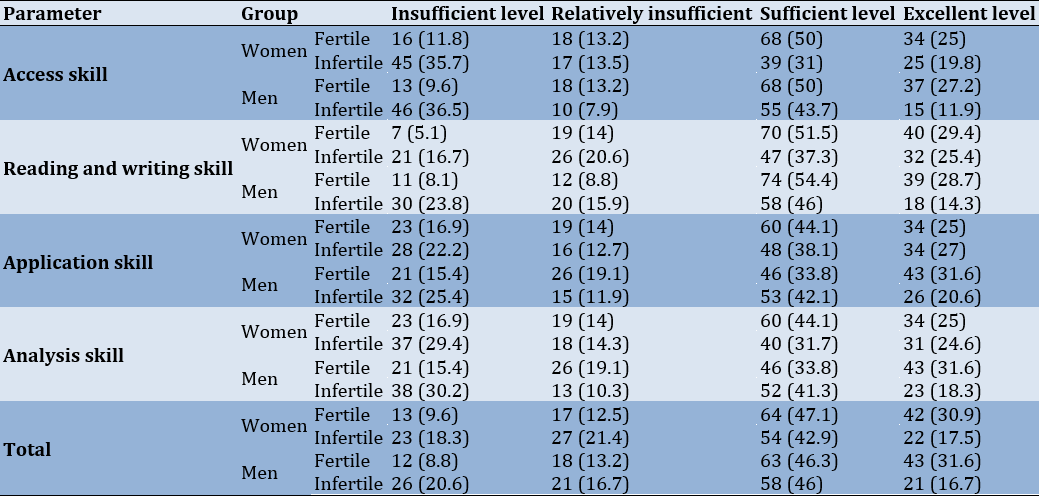
The assessment of the sufficiency of SHL in its different dimensions in fertile and infertile couples showed that 78% of fertile women and 77.9% of fertile men had sufficient and excellent sexual health literacy. This rate was 60.4% and 62.7% for infertile women and men, respectively. The most sufficient information in both groups of fertile women and fertile men was related to reading and writing skills (80.9 and 83.1%, respectively). In infertile women and men, this amount was related to the dimension of application skill (65.1% and 62.1%, respectively). The lowest adequacy of information in fertile women and men was related to application and analysis skills (69.1% and 65.4%, respectively). Furthermore, access skill had the lowest score in infertile women and men (50.8% and 55. 6%, respectively) (Table 3).
Table 3. Sufficiency of SHL in its different dimensions in fertile and infertile couples
The mean±SD of marital satisfaction in fertile and infertile couples was 36.93±6.58 and 36.05±6.25, respectively. The results showed no statistically significant difference in the average marital satisfaction between the fertile and infertile couples (p-value=0.121).
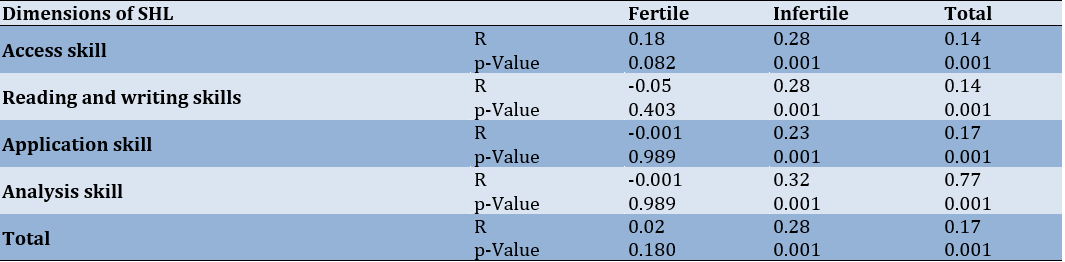
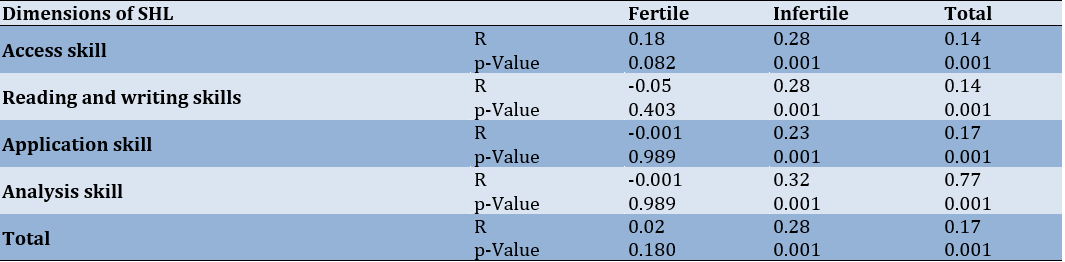
The results showed a significant correlation between SHL and the marital satisfaction in infertile couples (p=0.001; Table 4). Also, a significant correlation was observed between fertile and infertile couples in terms of all four SHL dimensions and the level of marital satisfaction, and the highest correlation in fertile (r=0.77) and infertile couples (r=0.32) was related to the dimension of analysis skills. However, there was no significant correlation between any of the SHL dimensions and marital satisfaction in fertile couples.
Table 4. Correlation of marital satisfaction with different dimensions of SHL
Based on multivariable regression, none of SHL dimensions had a significant relationship with marital satisfaction. The results of the multivariable linear regression model showed that among the independent variables related to marital satisfaction, after entering the multivariable model, husband’s education level and duration of marriage remained significant, the rest of the variables did not show any relationship.
Discussion
This study aimed to compare the SHL level and marital satisfaction in fertile and infertile couples and to investigate the relationship between these parameters.
We found that marital satisfaction in fertile couples was higher than that in infertile ones. Faal Kalkhoran et al. reported that the prevalence rates of anxiety and depression in infertile women are higher than those in fertile ones, but consistent with our study, there is no significant difference between the two groups in terms of marital satisfaction [22]. Amiri et al. showed no significant difference between fertile and infertile women in terms of marital satisfaction [23]. Unlike this study, Monga et al. demonstrated that marital adjustment in infertile couples is significantly less than that in fertile ones [24]. The results of Bakhtiar et al.’s study showed that the depression severity and sexual dissatisfaction in the infertile group are higher than those in the fertile ones [25]. Sahraeian et al. confirmed that the levels of satisfaction in the infertile group are significantly lower than those in the fertile group [26]. The results of a comprehensive review indicate that infertility is one of the factors influencing sexual satisfaction [27].
Kim et al. rejected couples' fertility or infertility as an effective factor in marital satisfaction and reported that both psychological and demographic factors could affect marital satisfaction [28]. A meta-analysis shows that infertility is associated with increased sexual dysfunction [29]. The results of the present study showed that the parameters of the husband’s education level and duration of marriage were the determinants of marital satisfaction, while no significant statistical relationship was found between fertility and infertility, and marital satisfaction. Some studies demonstrate that the duration of infertility (from 3 to 6 years with the most destructive effect), the type, and the number of treatment failures could affect marital satisfaction [30-32]. According to the above-mentioned studies and the results of our study, despite the negative psychological effects of infertility, it is not possible to definitively judge the effect of infertility on marital satisfaction, and also there is a need to investigate other determinants. The difference in marital satisfaction may be due to racial, ethnic, and cultural differences that can affect the level of the expectations of the people.
The results showed that the mean of SHL score in fertile couples was higher than that in infertile ones, which was statistically significant. Also, the sufficiency of SHL in this study was about 80% and 60%, respectively, among fertile and infertile couples. The effect and importance of having SHL have been discussed in a number of studies. Sahebalzamani et al. reported borderline SHL in most infertile couples (49.7% among men and 44.1% among women) [33]. Ghanbari et al. also reported sufficient SHL levels in 45.4% of pregnant women [34]. McMichael and Gifford demonstrate that low SHL led to a decrease in the frequency of condom use and an increase in the possibility of high-risk sexual relationships [35]. Hepburn expressed that more than 65% of African-American women have low and insufficient health literacy [36]. Conversely, the results of Patras et al.'s study indicated that health literacy among infertile women is in a good condition, also they calculate the average of the total health literacy as 79.58 out of 100 [37]. Considering the effects of cultural, social and economic factors on health literacy, the difference between the results of this study and some studies is not far from expected. Also, the use of different health measurement tools may cause this difference.
There was a significant correlation between all couples and infertile couples with respect to all four SHL dimensions and the level of marital satisfaction. Patras et al. also found a significant positive relationship between health literacy and sexual satisfaction [37]. Ziaee et al. conducted a study on 290 infertile women and proved the relationship between health literacy and sexual satisfaction [38]. Sahebalzamani et al. concluded that health literacy was associated with higher levels of sexual performance and sexual satisfaction in men and women, but the strength of these associations is moderate to weak [33]. Also, the results of multi parameters regression performed in this study reveals that none of the SHL dimensions have a significant relationship with marital satisfaction. Samadaee-Gelehkolaee et al. demonstrated that demographic factors, such as age, occupation, education level, duration of marriage, duration of infertility, type of family (nuclear, extended), and income level could be important factors affecting marital satisfaction [27]. Also, the results of the study indicate that occupation due to social status could have a positive effect on marital satisfaction, and there was a positive relationship between the husband's occupation and the wife's life satisfaction [27]. Amiri et al. demonstrated significant differences between fertile and infertile groups concerning marital satisfaction, spouse's occupation, and income level [23]. This suggests that health literacy may influence the mental states and attitudes of couples toward sexual and marital relations, thereby impacting their sexual satisfaction. Moreover, an increase in health literacy is likely to expand individuals' knowledge about sexual physiology and performance, consequently affecting sexual satisfaction. Notably, the highest correlation observed in both fertile and infertile couples pertained to the dimension of analytical skills.
Strengths and limitations
The examination of sexual health literacy in two different sexual and fertility groups (fertile and infertile couples) and the relationship between sexual health literacy and marital satisfaction in these couples were the strengths of this study compared to other similar studies. Also, the importance of preliminary surveys that can be used to design suitable interventions and show the status of the study parameters in a certain geographical area were other characteristics of this study.
For future studies, it is suggested to examine more variables that may be related to marital satisfaction
One of the limitations of the study is the generalizability of its results to people in different regions with different cultures because both study parameters can be influenced by the culture of societies. Due to the randomly selected samples, there was no choice to select all samples properly. Therefore, it is recommended that further studies should be conducted on a larger sample size in order to show the marital satisfaction of couples as the basis of family and society. On the other hand, the limitations of self-reporting and the influence of participants' mental states in completing the questionnaires should be considered.
Conclusion
There is no significant difference between fertile and infertile couples in terms of marital satisfaction in this study. However, there is a correlation between sexual health literacy and marital satisfaction in infertile people and the low level of sexual health literacy in them compared to fertile people.
Acknowledgments: The authors would like to thank Dr. Marzieh Mehrafza and the staff of the of Mehr Infertility Institute in Rasht city and healthcare centers, and the participants who contributed to this study.
Ethical Permissions: The study was approved by the Ethics Committee of Khalkhal University of Medical Sciences (IR.KHALUMS.REC.1398.011).
Conflicts of Interests: There is no conflict of interest.
Authors’ Contribution: Mousazadeh Y (First Author), Main Researcher/Discussion Writer (20%); Najafi E (Second Author), Assistant Researcher/Statistical Analyst (20%); Salmani R (Third Author), Introduction Writer/Assistant Researcher (10%); MoradAbadi A (Fourth Author), Assistant Researcher (10%); Salimi Kivi M (Fifth Author), Assistant Researcher (10%); Salmani R (Sixth Author), Corresponding Author/Methodologist/Main Researcher/Discussion Writer (30%)
Funding/Support: This work was funded and supported by Khalkhal University of Medical Sciences.
Happiness and a desirable quality of life are relative concepts, as each person experiences happiness uniquely. Indeed, happiness and activity are fundamental psychological needs that constantly occupy the human mind due to their significant impact on people's lives [1, 2]. Many people sometimes experience thoughts and worries related to their health, leading to a decreased quality of life and, consequently, reduced marital satisfaction. Marital satisfaction is a significant and complex aspect of a marital relationship [3]. It expresses how the expectations of sexual partners are met by each other, and also it can play an important role in family health [4]. Sexual satisfaction is one of the individual needs and interpersonal interactions that may have a close relationship with health society [5]. Satisfying sexual relations protects a person against many disorders and diseases [5]. Also, it can affect life satisfaction, job satisfaction, income satisfaction, success, and mental health [6]. Couples with high perceived marital satisfaction have a lot of agreement with each other. They are also satisfied with the type and level of their relationship, the type and quality of spending their leisure time, and effectively their time and financial issues [7]. Studies show that psychological factors can play a role in the creation of infertility and can be considered as its result. In this regard, many pieces of evidence show that psychological problems caused by infertility can be a contributing factor in the aggravation of infertility [3].
Many sexual problems are caused by ignorance and false beliefs about sexual relationships [8]. One of the concepts raised in this field is sexual health literacy (SHL), which refers to a set of knowledge, attitudes and beliefs, motivations, and personal abilities in accessing, understanding, appraising, and applying information related to sexual health [9]. An adequate level of sexual health literacy (SHL) enhances a person's ability to analyze, judge, discuss, decide, and change sexual behavior. It also empowers individuals to ensure, maintain, and improve their sexual health [10]. Insufficient health literacy can lead to dissatisfaction in the couple's relationship and problems in their married life. Therefore, improving SHL level is an effective step towards improving marital satisfaction and quality of life [11]. Various studies have highlighted many benefits of sexual and reproductive health literacy. These benefits include improving the ability to understand and evaluate risks related to sexual health, delaying the first sexual experience, selecting low-risk sexual partners, practicing safe sex, reducing unwanted pregnancies and sexually transmitted diseases, fostering a correct understanding of responsibilities and duties in sexual relationships, providing the opportunity to properly express gender roles, enhancing couples' sexual interactions, promoting individual sexual health, and ultimately improving family and social health [12].
Advances in assisted reproductive equipment and techniques help infertile couples manage and reduce their fertility problems [13]. The prevalence rate of infertility is 12 to 15 percent worldwide according to the report of the World Health Organization (WHO) [14]. Infertility rate is reported to be 2% to 20% in Iran [14]. Previous studies on marital satisfaction in infertile people yielded two different views in this regard. On one hand, infertility is regarded as an experience that fosters couple growth [15]. It serves as a challenge that enhances cooperation between partners, as they navigate the infertility crisis together, engage in long-term treatments, make joint decisions, and share their feelings. This collaborative process can result in equal or even greater marital satisfaction compared to fertile couples [16]. On the other hand, medical interventions for infertility can impact the quality of life of infertile couples and their needs [17], potentially leading to reduced marital satisfaction [18]. However, it's crucial to recognize that infertile couples constitute a limited but significant group of patients who require understanding and support. Three key points can be raised regarding marital satisfaction. First, a lack of marital satisfaction may lead to dissatisfaction with married life and a loss of emotional connection between couples. Second, studies suggest that sexual health literacy (SHL) can promote and improve marital satisfaction. Third, fertility and infertility have varying effects on marital satisfaction. Given these factors, conducting a study on this topic can provide valuable data on the elements influencing marital satisfaction, as it examines the impacts of fertility, infertility, and sexual health literacy simultaneously. This data can be used to design relevant interventions.
Therefore, the aims of this study were to compare the SHL level and marital satisfaction in fertile and infertile couples and to investigate the relationship between these parameters.
Instrument & Methods
Study design
This was a descriptive-analytical cross-sectional study conducted in Guilan and Ardabil provinces in the north, and northwest of Iran during 2020-2021.
Study population and sample
The study population included eligible infertile couples who were referred to Mehr Infertility Institute in Rasht, Guilan province, Iran, for the treatment of their fertility problems, and fertile couples referring to healthcare centers in the north and northwest of Iran.
The samples were selected by convenience sampling method. The sample size was determined by the average difference in two independent populations Formula [18] (n=500, 250 people per group). However, 5% was added to this number to increase reliability and compensate for the possible dropout due to reasons like incomplete questionnaires. The variance of the first and second groups was 12.4 and 12.3, respectively.
The study inclusion criteria for the infertile group included primary infertility, having female or male (or both) infertility, and not having chronic diseases. The study inclusion criteria for the fertile group also included the absence of chronic diseases and secondary infertility and having at least one child. Physical or mental disorders, death of close relatives during the last six months, and adoption were among the study exclusion criteria.
The samples were selected after obtaining the necessary permissions from the administrators of Khalkhal University of Medical Sciences and presenting a letter of introduction and obtaining the approval form the infertility institute and health care centers. Written informed consent was obtained from all participants, and this method of consent was also approved by the relevant Institutional Review Board (Ethics Committee of Khalkhal University of Medical Sciences).
Study instruments
Three questionnaires were used in the present study. The demographic questionnaire included questions on age, education level, employment status, duration of marriage, duration of infertility, income level, type of delivery, and contraceptive method (in fertile people). The second questionnaire was the sexual health literacy for adults (SHELA) questionnaire. This 40-item questionnaire is designed by Masoumi et al. [19]. It consists of four dimensions, including access (items 1 to 7), reading and writing (items 8 to 25), analysis and appraisal (items 26 to 30), and application skills (items 31 to 40). Each item is scored based on a five-point Likert scale, ranging from completely agree to completely disagree. The raw score of each subscale is obtained from the algebraic sum of the scores.
To calculate the total score, the scores of subscales are added based on the 0-100 range and divided by the number of subscales (4). The content validity based on the Content Validity Index (CVI) and Content Validity Ratio (CVR) for all items was 0.84 and 0.81, respectively. Exploratory factor analysis explained 68.1% of the variance. Convergent validity of the questionnaire showed the range of 0.31 to 0.70. The reliability of the scale was assessed by Cronbach’s alpha. It ranged from 0.84 to 0.94. Also, this questionnaire showed a high Intraclass Correlation Coefficient (ICC), ranging from 0.90 to 0.97 [19].
The third questionnaire was the enrich marital satisfaction scale-short form. It has been used as a valid research instrument in many research and clinical studies. Olson et al. used this scale to assess marital satisfaction and believed that this scale is sensitive to the changes occurring in the family [20]. This scale consists of 10 satisfaction questions, which are scored based on a five-point Likert scale, ranging from completely agree (5) to completely disagree (1), and thus, higher scores indicate more marital satisfaction. Also, questions 1, 3, 5, 8, and 9 are scored reversely. Arab Alidousti et al. confirmed the reliability and validity of the Persian version of this questionnaire [21]. Face validity is also assessed by qualitative method, receiving the opinions of five married women and five men over 18 years of age. Cronbach's alpha value is also 0.74 in this study [21].
Statistical analysis
After assessing the normality of the data distribution by the Kolmogorov-Smirnov test, independent T-test, and Chi-square test were employed to compare demographic parameters in fertile and infertile couples. Pearson's correlation test was also used to investigate the relationship between SHL, and marital satisfaction. A multivariate regression test was also applied to determine the determinants of marital satisfaction. Data analysis was carried out using descriptive statistics and average estimation in different groups. All statistical analysis was conducted using SPSS 26 Software. A p-value of 0.05 was considered statistically significant.
Findings
The study population included 126 infertile couples (n=252) and 136 fertile ones (n=272) and their characteristics were collected (Table 1). The mean±standard deviation (SD) of the age of the fertile and infertile women was 35.52±7.59 and 34.47±7.58 years, respectively, which indicated no statistically significant difference (t=1.12; p=0.261). Also, the mean±SD of the age of the fertile and infertile women's spouses was 39.16±7.3 and 38.25±7.52 years, respectively, which also showed no statistically significant difference (t=0.86; p=0.326). Almost two-thirds (66.9%) of fertile women had a higher education level, but there was a different situation in infertile women, so that only 29.1% of the respondents had a higher education level. Most of the husbands of fertile women had higher education levels, whereas 35.4% of the husbands of infertile women had higher education levels, and also approximately 45% earned high school diplomas (Table 1).
Table 1. Individual-social characteristics of the study participants.
This study indicated a higher SHL level in fertile women than infertile ones. The mean±SD of SHL score in fertile and infertile men was statistically significant (p=0.001) and indicated a higher SHL level in fertile men than infertile ones. The mean scores of all SHL dimensions in both fertile women and fertile men were higher than those in infertile ones, which was statistically significant in all dimensions, except for the application skill dimension (Table 2). The highest mean score was related to the reading and writing skill dimension in both fertile women and men, and the application skill had the lowest score in both fertile women and men. Both infertile women and men have the highest scores in application skills. The lowest score in these two groups was related to access skills (Table 2).
Table 2. Comparison of mean and standard deviation of SHL dimensions in fertile and infertile couples
The assessment of the sufficiency of SHL in its different dimensions in fertile and infertile couples showed that 78% of fertile women and 77.9% of fertile men had sufficient and excellent sexual health literacy. This rate was 60.4% and 62.7% for infertile women and men, respectively. The most sufficient information in both groups of fertile women and fertile men was related to reading and writing skills (80.9 and 83.1%, respectively). In infertile women and men, this amount was related to the dimension of application skill (65.1% and 62.1%, respectively). The lowest adequacy of information in fertile women and men was related to application and analysis skills (69.1% and 65.4%, respectively). Furthermore, access skill had the lowest score in infertile women and men (50.8% and 55. 6%, respectively) (Table 3).
Table 3. Sufficiency of SHL in its different dimensions in fertile and infertile couples
The mean±SD of marital satisfaction in fertile and infertile couples was 36.93±6.58 and 36.05±6.25, respectively. The results showed no statistically significant difference in the average marital satisfaction between the fertile and infertile couples (p-value=0.121).
The results showed a significant correlation between SHL and the marital satisfaction in infertile couples (p=0.001; Table 4). Also, a significant correlation was observed between fertile and infertile couples in terms of all four SHL dimensions and the level of marital satisfaction, and the highest correlation in fertile (r=0.77) and infertile couples (r=0.32) was related to the dimension of analysis skills. However, there was no significant correlation between any of the SHL dimensions and marital satisfaction in fertile couples.
Table 4. Correlation of marital satisfaction with different dimensions of SHL
Based on multivariable regression, none of SHL dimensions had a significant relationship with marital satisfaction. The results of the multivariable linear regression model showed that among the independent variables related to marital satisfaction, after entering the multivariable model, husband’s education level and duration of marriage remained significant, the rest of the variables did not show any relationship.
Discussion
This study aimed to compare the SHL level and marital satisfaction in fertile and infertile couples and to investigate the relationship between these parameters.
We found that marital satisfaction in fertile couples was higher than that in infertile ones. Faal Kalkhoran et al. reported that the prevalence rates of anxiety and depression in infertile women are higher than those in fertile ones, but consistent with our study, there is no significant difference between the two groups in terms of marital satisfaction [22]. Amiri et al. showed no significant difference between fertile and infertile women in terms of marital satisfaction [23]. Unlike this study, Monga et al. demonstrated that marital adjustment in infertile couples is significantly less than that in fertile ones [24]. The results of Bakhtiar et al.’s study showed that the depression severity and sexual dissatisfaction in the infertile group are higher than those in the fertile ones [25]. Sahraeian et al. confirmed that the levels of satisfaction in the infertile group are significantly lower than those in the fertile group [26]. The results of a comprehensive review indicate that infertility is one of the factors influencing sexual satisfaction [27].
Kim et al. rejected couples' fertility or infertility as an effective factor in marital satisfaction and reported that both psychological and demographic factors could affect marital satisfaction [28]. A meta-analysis shows that infertility is associated with increased sexual dysfunction [29]. The results of the present study showed that the parameters of the husband’s education level and duration of marriage were the determinants of marital satisfaction, while no significant statistical relationship was found between fertility and infertility, and marital satisfaction. Some studies demonstrate that the duration of infertility (from 3 to 6 years with the most destructive effect), the type, and the number of treatment failures could affect marital satisfaction [30-32]. According to the above-mentioned studies and the results of our study, despite the negative psychological effects of infertility, it is not possible to definitively judge the effect of infertility on marital satisfaction, and also there is a need to investigate other determinants. The difference in marital satisfaction may be due to racial, ethnic, and cultural differences that can affect the level of the expectations of the people.
The results showed that the mean of SHL score in fertile couples was higher than that in infertile ones, which was statistically significant. Also, the sufficiency of SHL in this study was about 80% and 60%, respectively, among fertile and infertile couples. The effect and importance of having SHL have been discussed in a number of studies. Sahebalzamani et al. reported borderline SHL in most infertile couples (49.7% among men and 44.1% among women) [33]. Ghanbari et al. also reported sufficient SHL levels in 45.4% of pregnant women [34]. McMichael and Gifford demonstrate that low SHL led to a decrease in the frequency of condom use and an increase in the possibility of high-risk sexual relationships [35]. Hepburn expressed that more than 65% of African-American women have low and insufficient health literacy [36]. Conversely, the results of Patras et al.'s study indicated that health literacy among infertile women is in a good condition, also they calculate the average of the total health literacy as 79.58 out of 100 [37]. Considering the effects of cultural, social and economic factors on health literacy, the difference between the results of this study and some studies is not far from expected. Also, the use of different health measurement tools may cause this difference.
There was a significant correlation between all couples and infertile couples with respect to all four SHL dimensions and the level of marital satisfaction. Patras et al. also found a significant positive relationship between health literacy and sexual satisfaction [37]. Ziaee et al. conducted a study on 290 infertile women and proved the relationship between health literacy and sexual satisfaction [38]. Sahebalzamani et al. concluded that health literacy was associated with higher levels of sexual performance and sexual satisfaction in men and women, but the strength of these associations is moderate to weak [33]. Also, the results of multi parameters regression performed in this study reveals that none of the SHL dimensions have a significant relationship with marital satisfaction. Samadaee-Gelehkolaee et al. demonstrated that demographic factors, such as age, occupation, education level, duration of marriage, duration of infertility, type of family (nuclear, extended), and income level could be important factors affecting marital satisfaction [27]. Also, the results of the study indicate that occupation due to social status could have a positive effect on marital satisfaction, and there was a positive relationship between the husband's occupation and the wife's life satisfaction [27]. Amiri et al. demonstrated significant differences between fertile and infertile groups concerning marital satisfaction, spouse's occupation, and income level [23]. This suggests that health literacy may influence the mental states and attitudes of couples toward sexual and marital relations, thereby impacting their sexual satisfaction. Moreover, an increase in health literacy is likely to expand individuals' knowledge about sexual physiology and performance, consequently affecting sexual satisfaction. Notably, the highest correlation observed in both fertile and infertile couples pertained to the dimension of analytical skills.
Strengths and limitations
The examination of sexual health literacy in two different sexual and fertility groups (fertile and infertile couples) and the relationship between sexual health literacy and marital satisfaction in these couples were the strengths of this study compared to other similar studies. Also, the importance of preliminary surveys that can be used to design suitable interventions and show the status of the study parameters in a certain geographical area were other characteristics of this study.
For future studies, it is suggested to examine more variables that may be related to marital satisfaction
One of the limitations of the study is the generalizability of its results to people in different regions with different cultures because both study parameters can be influenced by the culture of societies. Due to the randomly selected samples, there was no choice to select all samples properly. Therefore, it is recommended that further studies should be conducted on a larger sample size in order to show the marital satisfaction of couples as the basis of family and society. On the other hand, the limitations of self-reporting and the influence of participants' mental states in completing the questionnaires should be considered.
Conclusion
There is no significant difference between fertile and infertile couples in terms of marital satisfaction in this study. However, there is a correlation between sexual health literacy and marital satisfaction in infertile people and the low level of sexual health literacy in them compared to fertile people.
Acknowledgments: The authors would like to thank Dr. Marzieh Mehrafza and the staff of the of Mehr Infertility Institute in Rasht city and healthcare centers, and the participants who contributed to this study.
Ethical Permissions: The study was approved by the Ethics Committee of Khalkhal University of Medical Sciences (IR.KHALUMS.REC.1398.011).
Conflicts of Interests: There is no conflict of interest.
Authors’ Contribution: Mousazadeh Y (First Author), Main Researcher/Discussion Writer (20%); Najafi E (Second Author), Assistant Researcher/Statistical Analyst (20%); Salmani R (Third Author), Introduction Writer/Assistant Researcher (10%); MoradAbadi A (Fourth Author), Assistant Researcher (10%); Salimi Kivi M (Fifth Author), Assistant Researcher (10%); Salmani R (Sixth Author), Corresponding Author/Methodologist/Main Researcher/Discussion Writer (30%)
Funding/Support: This work was funded and supported by Khalkhal University of Medical Sciences.
Article Type: Descriptive & Survey |
Subject:
Sexual Health Education/Promotion
Received: 2023/12/25 | Accepted: 2024/05/2 | Published: 2024/05/20
Received: 2023/12/25 | Accepted: 2024/05/2 | Published: 2024/05/20
References
1. Elahifar H, Ghamari M, Zahrakar K. The effectiveness of group education "quality of life therapy" on the on female teachers' happiness. J Health Promot Manag. 2019;8(5):56-62. [Persian] [Link]
2. Namdar A, Naghizadeh MM, Zamani M, Yaghmaei F, Sameni MH. Quality of life and general health of infertile women. Health Qual Life Outcomes. 2017;15(1):139. [Link] [DOI:10.1186/s12955-017-0712-y]
3. Shokhmgar Z, Rajaei A, Beyazi M, Teimour S. The effect of "cognitive-behavioral group therapy" on marital satisfaction in infertil women applying for IVF. J Health Promot Manag. 2020;9(4):1-11. [Persian] [Link]
4. Edalati A, Redzuan M. Perception of women towards family values and their marital satisfaction. J Am Sci. 2010;6(4):132-7. [Link]
5. Ramos MM, Gameiro S, Canavarro MC, Soares I. Assessing infertility stress: re-examining the factor structure of the Fertility Problem Inventory. Human Reprod. 2012;27(2):496-505. [Link] [DOI:10.1093/humrep/der388]
6. Jonaidy E, Noorani Sadodin S, Mokhber N, Shakeri MT. Comparing the marital satisfaction in infertile and fertile women referred to the public clinics in Mashhad in 2006-07. Iran J Obstet Gynecol Infertilit. 2009;12(1):7-16. [Persian] [Link]
7. Greeff AP. Characteristics of families that function well. J Family Issues. 2000;21(8):948-62. [Link] [DOI:10.1177/019251300021008001]
8. Bahrainian SA, Nazemi F, Dadkhah A. The comparison of marital satisfaction between fertile and infertile women. Iran Rehabil J. 2009;7(1):11-6. [Link]
9. Gilbert M, Ferlatte O, Michelow W, Martin S, Young I, Donelle L, et al. P02.05 sexual health literacy-an emerging framework for research and intervention to improve sexual health for gay men. Sex Transm Infect. 2015;91(2):A85. [Link] [DOI:10.1136/sextrans-2015-052270.226]
10. Tavasoli Z, Nava F. The relationship between health literacy and marital satisfaction and quality of life of married women aged 30 to 40 in Mashhad. J Health Lit. 2017;2(1):31-8. [Persian] [Link] [DOI:10.18869/acadpub.jhl.2.1.31]
11. Akhoundy MM, Korminouri R, Behjati Ardakani Z. Psychosocial aspects of infertility from viewpoint of infertility treating physicians. J Prod Fertil. 2001;3(7):13-26. [Link]
12. Graf AS, Patrick JH. Foundations of life-long sexual health literacy. Health Educ. 2015;115(1):56-70. [Link] [DOI:10.1108/HE-12-2013-0073]
13. Dadkhah N, Askari Khanghah A, Baseri A, Mireskandari F. Surrogacy culture in Tehran, Iran. J Women Stud Sociol Psychol. 2020;18(2):111-52. [Persian] [Link]
14. Gomes ABFdS. A satisfação conjugal em casais candidatos à adopção: Caracterização em função do género e do motivo para adoptar (infertilidade/não-infertilidade) [dissertation]. Lisbon: University of Lisbon; 2009. [Portuguese] [Link]
15. Khanabadi M, Yassini-Ardekani SM, Farahbakhsh K, Esmaeli M. Dimensions of sex-related excellent marital quality among infertile couples: A qualitative study. J Kermanshah Univ Med Sci. 2018;22(3):e81611. [Link] [DOI:10.5812/jkums.81611]
16. Drosdzol A, Skrzypulec V. Evaluation of marital and sexual interactions of Polish infertile couples. J Sex Med. 2009;6(12):3335-46. [Link] [DOI:10.1111/j.1743-6109.2009.01355.x]
17. Da Silva SMG. Perceções de qualidade relacional e de stresse na vivência da infertilidade [dissertation]. Porto: University of Porto; 2011. [Portuguese] [Link]
18. Masoumi SZ, Garousian M, Khani S, Oliaei SR, Shayan A. Comparison of quality of life, sexual satisfaction and marital satisfaction between fertile and infertile couples. Int J Fertil Steril. 2016;10(3):290-6. [Link]
19. Masoumi R, Tavousi M, Zarei F. Development and psychometric properties of sexual health literacy for adults (SHELA) questionnaire. Hayat. 2019;25(1):56-69. [Persian] [Link]
20. Olson DH, McCubbin HI, Barnes H, Larsen A, Muxen M, Wilson M. Families: What makes them work. Beverly Hills: SAGE Publications; 1989. [Link]
21. Arab Alidousti A, Nakhaee N, Khanjani N. Reliability and validity of the Persian versions of the ENRICH marital satisfaction (brief version) and Kansas Marital Satisfaction Scales. Health Dev J. 2015;4(2):158-67. [Persian] [Link]
22. Faal Kalkhoran L, Bahrami H, Farrokhi NA, Zeraati H, Tarahhomi M. Comparing anxiety, depression and marital satisfaction in two selected groups of fertile and infertile women in Tehran. J Reprod Infertil. 2011;12(2):157-63. [Persian] [Link]
23. Amiri M, Sadeqi Z, Hoseinpoor MH, Khosravi A. Marital satisfaction and its influencing factors in fertile and infertile women. J Family Reprod Health. 2016;10(3):139-45. [Link] [DOI:10.1007/s11195-016-9443-y]
24. Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004;63(1):126-30. [Link] [DOI:10.1016/j.urology.2003.09.015]
25. Bakhtiar K, Ardalan A, Ebrahimzadeh F, Almasian M, Bastami F. Depression severity and sexual satisfaction in fertile and infertile women in Iran: A population-based case-control study. Jundishapur J Health Sci. 2022;14(1):e120974. [Link] [DOI:10.5812/jjhs.120974]
26. Sahraeian M, Lotfi R, Qorbani M, Faramarzi M, Dinpajooh F, Ramezani Tehrani F. The effect of cognitive behavioral therapy on sexual function in infertile women: A randomized controlled clinical trial. J Sex Marital Ther. 2019;45(7):574-84. [Link] [DOI:10.1080/0092623X.2019.1594476]
27. Samadaee-Gelehkolaee K, McCarthy BW, Khalilian A, Hamzehgardeshi Z, Peyvandi S, Elyasi F, et al. Factors associated with marital satisfaction in infertile couple: A comprehensive literature review. Glob J Health Sci. 2016;8(5):96-109. [Link] [DOI:10.5539/gjhs.v8n5p96]
28. Kim KY, Park TY, Won HJ, Kim YT, Kim HW, Yoon TK. A study on predictors relating to marital satisfaction of infertile couples. Fertil Steril. 2007;88(Suppl 1):S10. [Link] [DOI:10.1016/j.fertnstert.2007.07.054]
29. Mendonca CR, Arruda JT, Noll M, Campoli PMO, Amaral WN. Sexual dysfunction in infertile women: A systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2017;215:153-63. [Link] [DOI:10.1016/j.ejogrb.2017.06.013]
30. Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility among women. Eur J Obstet Gynecol Reprod Biol. 2004;117(2):126-31. [Link] [DOI:10.1016/j.ejogrb.2004.05.004]
31. Ramezanzadeh F, Aghssa MM, Abedinia N, Zayeri F, Khanafshar N, Shariat M, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(9). [Link] [DOI:10.1186/1472-6874-4-9]
32. Verhaak CM, Smeenk JMJ, Evers AWM, Kremer JAM, Kraaimaat FW, Braat DDM. Women's emotional adjustment to IVF: A systematic review of 25 years of research. Hum Reprod Update. 2007;13(1):27-36. [Link] [DOI:10.1093/humupd/dml040]
33. Sahebalzamani M, Mostaedi Z, Farahani H, Sokhanvar M. Relationship between health literacy and sexual function and sexual satisfaction in infertile couples referred to the Royan Institute. Int J Fertil Steril. 2018;12(2):136-41. [Link]
34. Ghanbari S, Majlessi F, Ghaffari M, Mahmoodi Majdabadi M. Evaluation of health literacy of pregnant women in urban health centers of Shahid Beheshti Medical University. Daneshvar Med. 2012;19(6):1-12. [Persian] [Link]
35. McMichael C, Gifford S. Narratives of sexual health risk and protection amongst young people from refugee backgrounds in Melbourne, Australia. Cult Health Sex. 2010;12(3):263-77. [Link] [DOI:10.1080/13691050903359265]
36. Hepburn M. The relationships between health literacy, self-efficacy and readiness for change to health promotion behaviors in urban black women. Seton Hall University Dissertations and Theses. 2016;2197. [Link] [DOI:10.1161/str.47.suppl_1.ns2]
37. Patras G, Safdari F, Jafari H, Rafiei S, Fathnezhad Kazemi A. Correlation of health literacy and sexual satisfaction in infertile women referred to infertility center of Al-Zahra Hospital in Tabriz. J Health Promot Manag. 2020;9(4):58-67. [Persian] [Link]
38. Ziaee T, Jannati Y, Mobasheri E, Taghavi T, Abdollahi H, Modanloo M, et al. The relationship between marital and sexual satisfaction among married women employees at Golestan University of Medical Sciences, Iran. Iran J Psychiatry Behav Sci. 2014;8(2):44-51. [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |