Volume 12, Issue 2 (2024)
Health Educ Health Promot 2024, 12(2): 197-205 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Umrana S, Risnawati R, Susanty S. Loneliness, Social Isolation, and Sleep Pattern in Elderly; A Systematic Review. Health Educ Health Promot 2024; 12 (2) :197-205
URL: http://hehp.modares.ac.ir/article-5-72989-en.html
URL: http://hehp.modares.ac.ir/article-5-72989-en.html
1- Department of Nursing, Karya Kesehatan College of Health Sciences, Kendari, Indonesia
2- Department of Nursing, Faculty of Medicine, University of Halu Oleo, Kendari, Indonesia
2- Department of Nursing, Faculty of Medicine, University of Halu Oleo, Kendari, Indonesia
Full-Text [PDF 648 kb]
(2831 Downloads)
| Abstract (HTML) (1572 Views)
Full-Text: (336 Views)
Introduction
Loneliness encompasses an individual’s subjective perception of emotional distress stemming from inadequate social connections in terms of quality or quantity [1]. In contrast, social isolation denotes an objective absence of social interactions [2]. Both loneliness and social isolation have been linked to declining health and heightened mortality rates in elderly populations [3, 4]. Despite their correlation, these two phenomena are distinct; a person experiencing loneliness may not necessarily be socially isolated, and vice versa [5, 6].
The issue of elderly individuals living alone is a significant societal concern often overlooked, and its prevalence has surged due to growing economic pressures [7]. The circumstance arises from various factors like separation from a spouse, children, or a desire for independence [8]. Loneliness encompasses a complex range of emotions tied to unmet social and personal needs and is closely intertwined with social isolation, particularly prevalent among older adults. A longitudinal study conducted over eight years revealed that 9% of the elderly population in the UK experience severe loneliness, while 30% have mild loneliness, indicating the importance of strong social networks and good health in preventing loneliness. Furthermore, the growth of the elderly population has resulted in a surge in the number of seniors residing in long-term care institutions [9].
Numerous research endeavors spanning various countries, such as Australia, Iran, Malaysia, and the United States have delved into the escalating issue of loneliness among older individuals [10-12]. These studies primarily focused on examining the correlation between community engagement and feelings of loneliness. In Malaysia, particular attention was given to exploring the link between loneliness and the involvement of older adults in religious activities, which often serve as a cornerstone for social interactions in numerous cultures and offer external support. As the global population ages at a swift pace, fostering a sense of community becomes increasingly crucial, especially considering the revelation of the World Health Organization (WHO) regarding the substantial surge in older people living in solitude worldwide, including in rural areas [13].
The literature discusses different forms of social isolation, categorizing them as subjective and objective. Subjective social isolation refers to the personal perception of inadequate social resources, like companionship or support from others [14]. Studies have consistently shown a direct link between both types of social isolation and conditions like sleep disruptions, depression, and fatigue. Emotional loneliness, a form of subjective social isolation rooted in inadequate support from peers, is strongly linked to reduced sleep quality [15]. Wakefield et al. [16] reported that individuals with strong social connections experience better sleep.
Interrupted sleep, and insufficient time for recuperation, have been proposed to interfere with typical hormonal, metabolic, and neurological functions [17], leading to declining health [18], diminished life satisfaction [19], and heightened mortality rates [20]. Additionally, numerous other factors contributing to sleep disorders and disruptions have been identified, such as being female, economic hardship [21], loss of a spouse [22], early signs of cognitive decline [23], feelings of depression [24], respiratory issues, cardiovascular conditions [25], and even cancer [26].
The previous systematic review elucidated the correlation between social relationships, particularly close ones, and individuals’ sleep patterns. However, these studies encompassed a broad spectrum of research across different age groups and health statuses [27]. The present review aimed to thoroughly examine the existing body of literature regarding the connection between loneliness, social isolation, and sleep. A systematic investigation was carried out to analyze the current state of research on the correlation between feelings of isolation and sleep patterns, giving particular attention to how samples were selected and measurements were conducted.
Information and Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 2020 [28].
Inclusion criteria
The inclusion criteria were studies in English assessing the elderly as defined by the WHO aged 65 years or older and also those discussing the relationship between loneliness or social isolation among the elderly and all forms of sleep disturbances. Also, the included studies should be observational or mixed methods studies. For the study location, we limited it to the community or locations outside of geriatric service facilities, such as nursing homes or similar hospitals. Typically, there were well-structured or scheduled programs for the elderly in the neighborhood, even if their next of kin visits infrequently. Additionally, the elderly may feel more engaged when reside in such environments due to the presence of other elderly that creates a more comfortable atmosphere for them. Studies involving sleep disorders, like sleep apnea and other severe disorders were excluded. Dissertations, proceedings, books, commentaries, case studies, and systematic reviews were also eliminated.
Search strategy
We utilized four reputable electronic databases to search for relevant literature, namely PubMed, Cochrane Library, Wiley Online Library, and ScienceDirect. To ensure the collection of all relevant articles in each database, a filter was applied to include the studies conducted from 2000 to October 2022. The exploration involved combining keywords associated with loneliness and its related aspects, along with terms related to social isolation and its impact on sleep patterns. The search was conducted by examining subject headings (MeSH terms) and reviewing both the title and the content within the abstracts of the articles. Search terms were adjusted as necessary for different databases. The search terms used are ((((((((((((("loneliness" [MeSH terms]) OR ("loneliness/psychology" [MeSH terms])) AND ("social isolation" [MeSH terms])) OR ("social isolation/complications" [MeSH terms])) OR ("social isolation/diagnosis" [MeSH terms])) AND ("sleep" [MeSH terms]))) OR ("sleep duration" [MeSH terms])) OR ("sleep latency" [MeSH terms])) OR ("sleep quality" [MeSH terms])))) AND (elderly [Title/Abstract])) OR ("older adult" [Title/Abstract]).
The review involved examining the reference lists of selected studies obtained through electronic searches and review of the articles. We manually explored other potentially relevant studies, including dissertations, conference reports, and unpublished sources, by employing unrestricted text and keyword queries in Zetoc (a platform for conference records) and OpenGrey (a repository for grey literature in Europe). In cases where necessary or feasible, we reached out to authors via email to acquire full text or seek clarification on specific points.
Selection process
Three reviewers individually selected studies for inclusion in the review (STU, RSI, and SRS). They screened all titles of the identified studies. Subsequently, they reviewed the abstracts of relevant studies and retrieved and examined the full texts of those still considered potentially pertinent. Another reviewer cross-checked all studies approved by one assessor to ensure compliance with the inclusion criteria during the selection process. The consensus between reviewers exceeded 99%. Any queries regarding inclusion or exclusion were resolved through discussions involving a third evaluator (STU, RSI, and SRS).
Quality appraisal
The included studies underwent evaluation concerning study design, methodology, and analysis. Subsequently, the studies were categorized as strong, moderate, or weak based on the criteria outlined in the EPHPP tool. This tool assesses studies using specific criteria, such as selection bias, study design, confounding factors, blinding, data collection techniques, withdrawals, drop-outs, intervention integrity (for intervention studies), and analyses. It demonstrated significant consistency among individual components and a notable intra-class correlation coefficient. These methods for assessing quality and the resulting ratings assess the credibility of individual studies. They do not aim to compare the significance of findings across studies but rather indicated the robustness of the study and, consequently, the confidence or reliability of the study’s outcomes.
Findings
Study selection
A systematic electronic search yielded a total of 13,418 publications through a comprehensive examination of related papers. Subsequent screening of full-text articles was conducted on 12,376 papers. During the full-text screening phase, 88 of these papers did not meet the eligibility criteria, resulting in a total of 13 articles deemed suitable for further in-depth investigation (Figure 1).
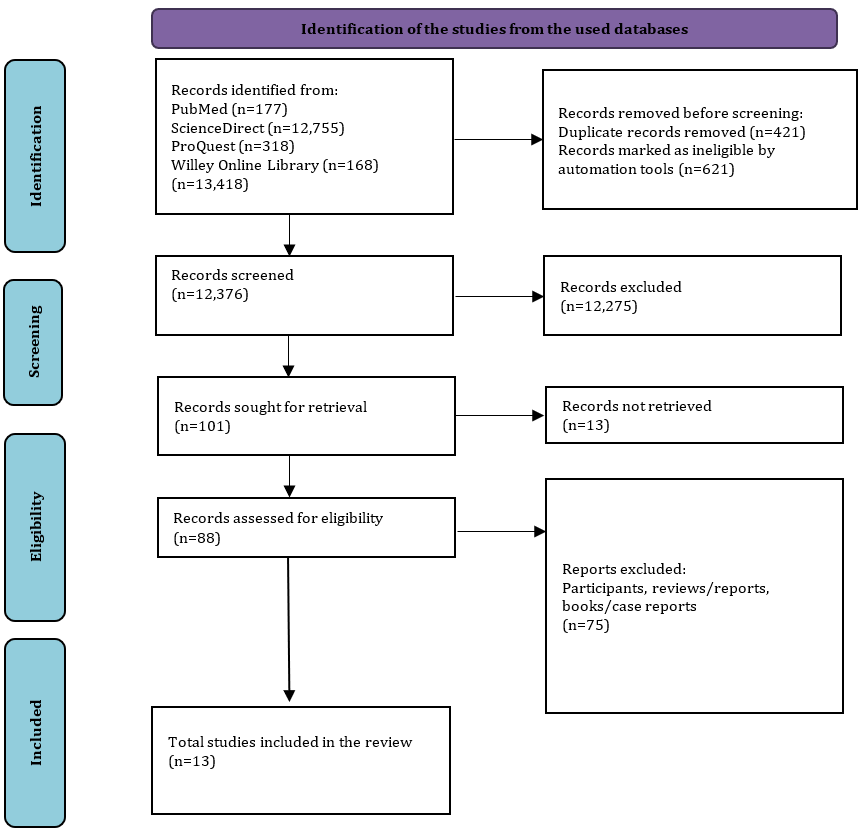
Figure 1. PRISMA flow diagram of the literature search
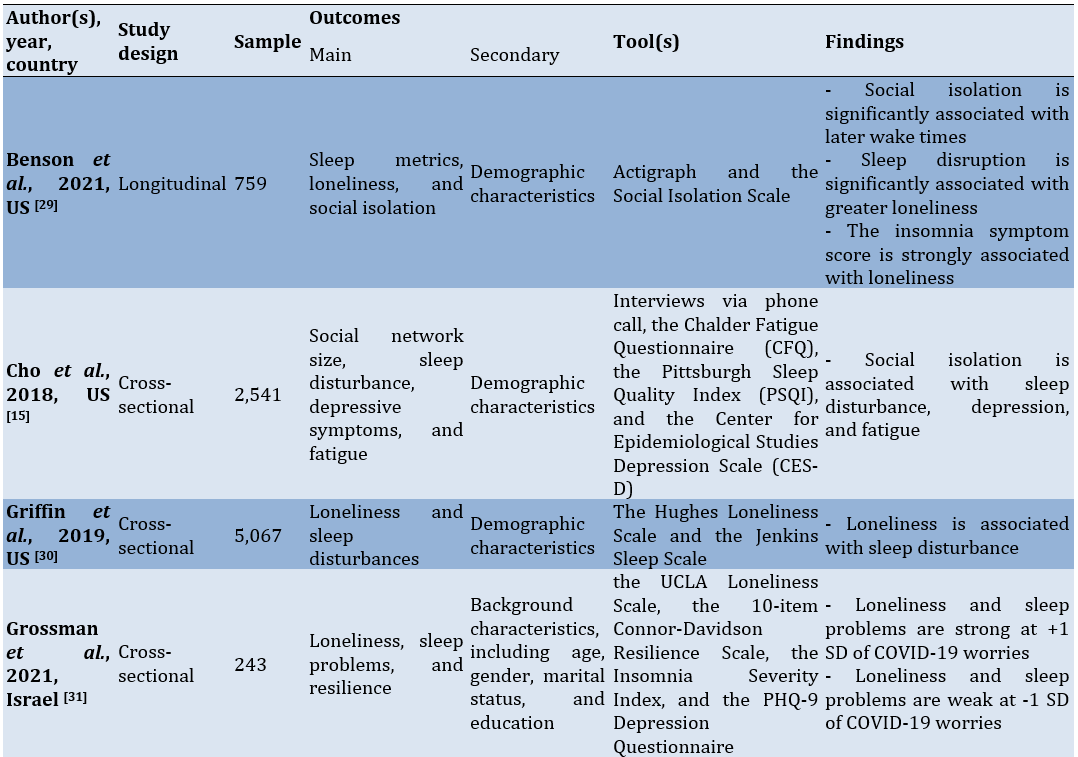
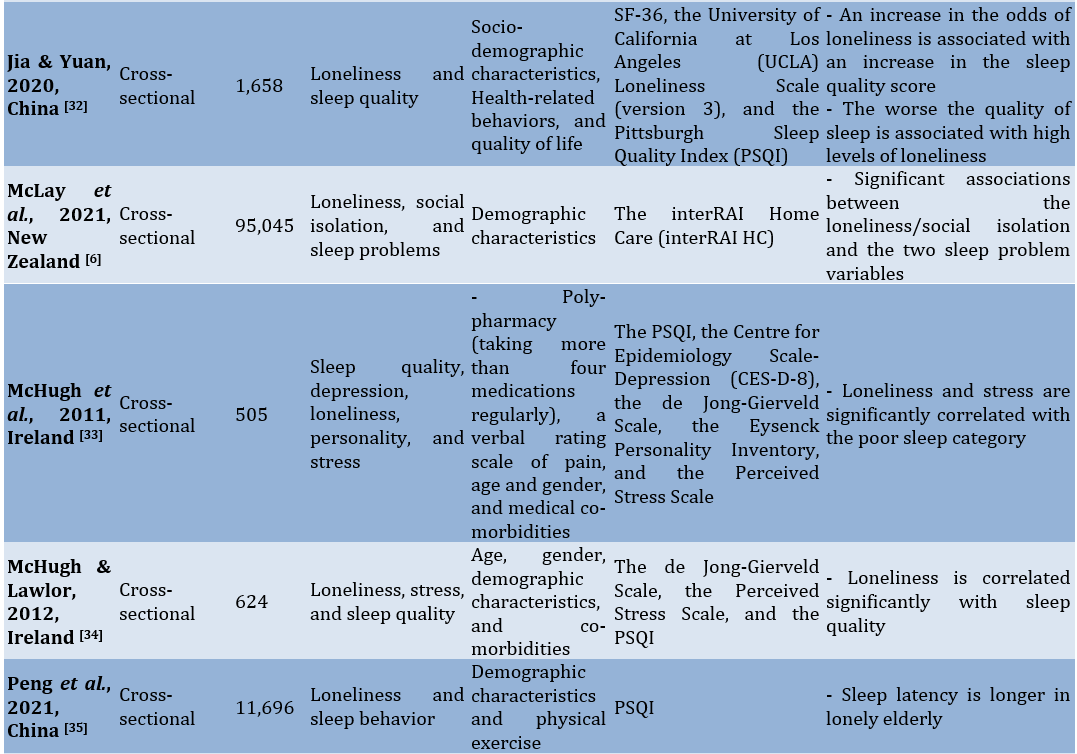
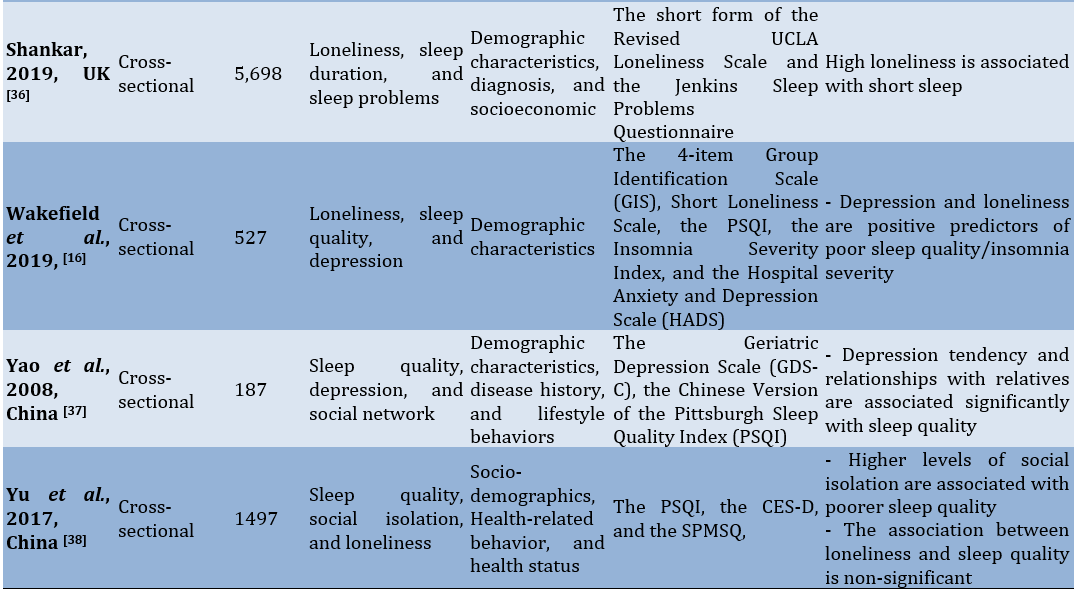
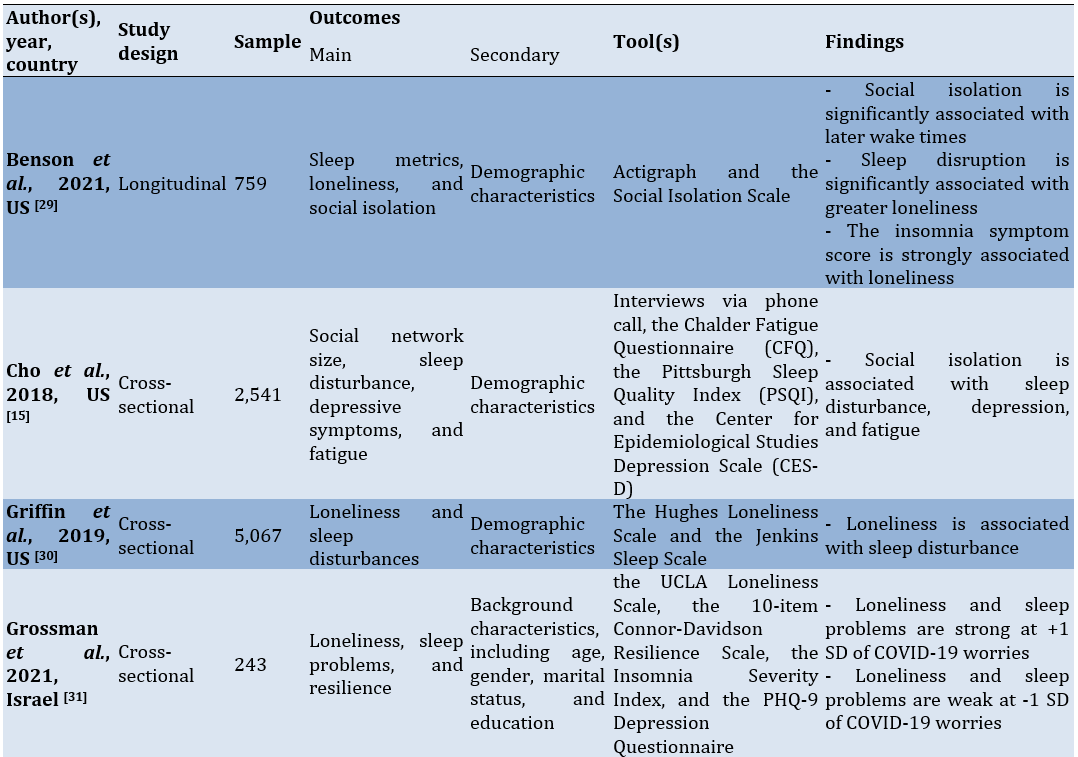
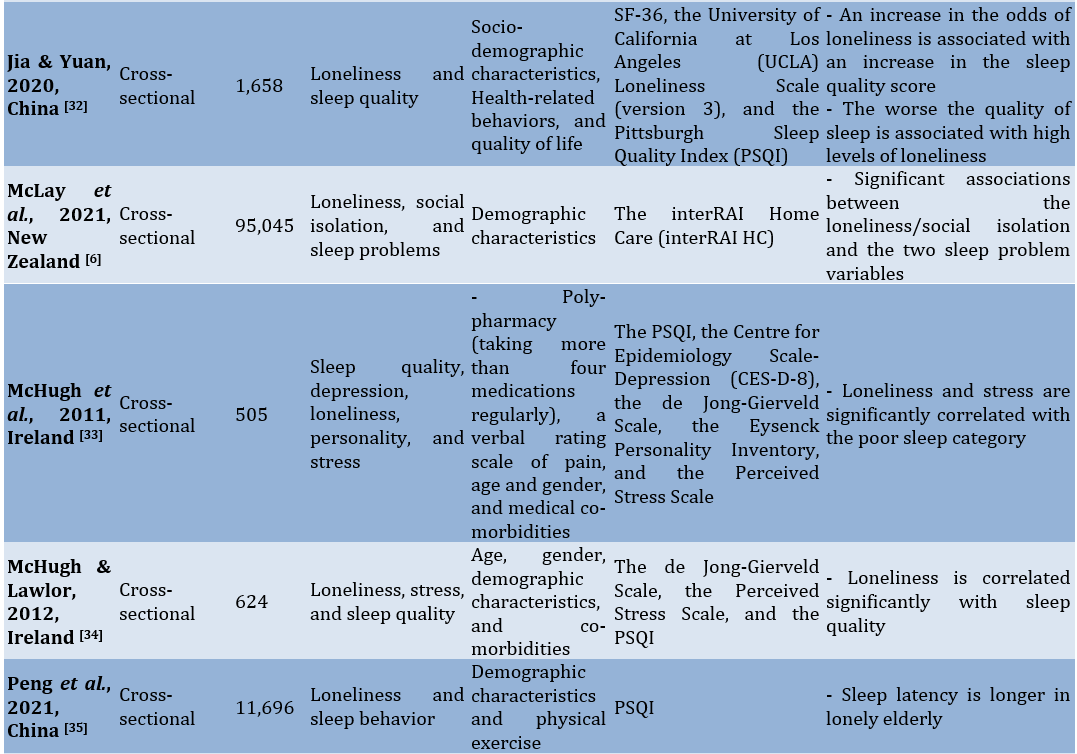
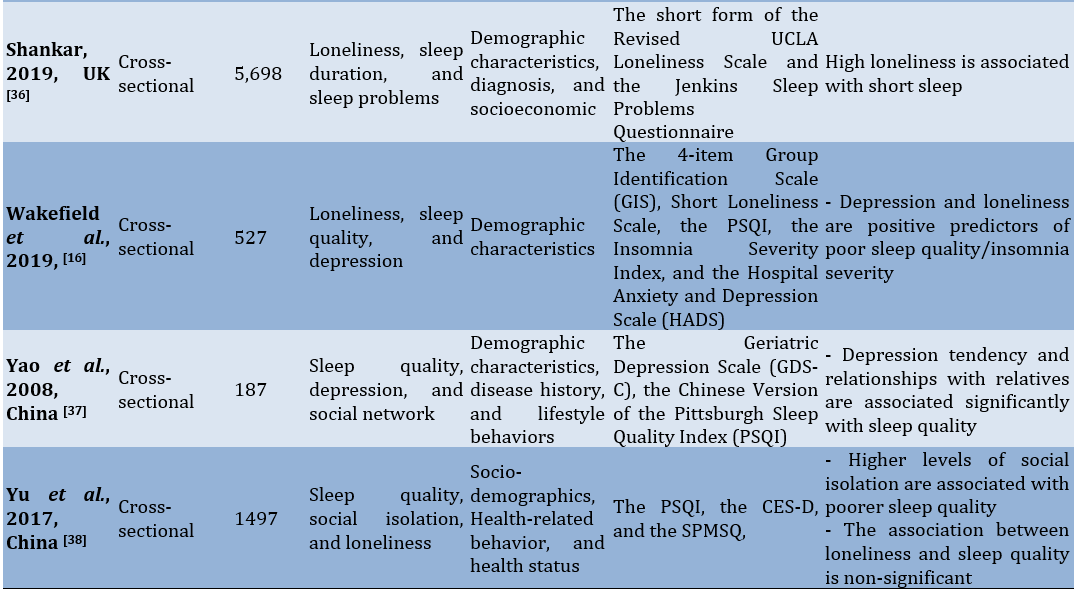
The characteristics of the included studies extracted in terms of their design, sample, outcomes, tools and findings (Table 1).
Table 1. Characteristics of studies included
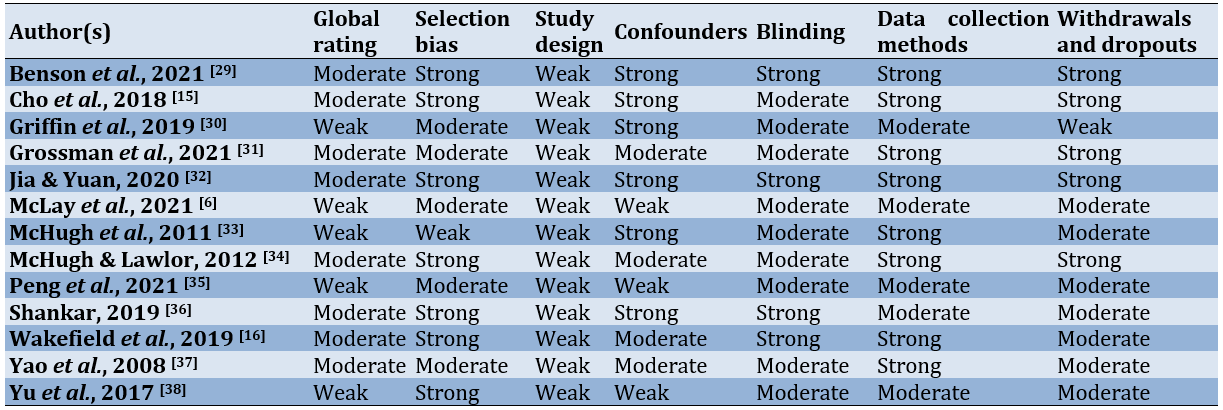
Study quality
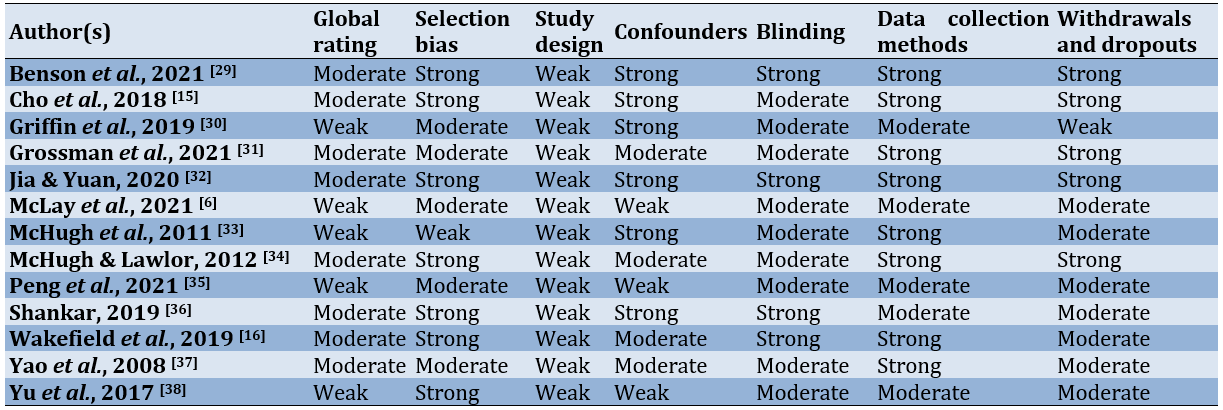
The moderately weighted cross-sectional design of quantitative research prevented them from receiving a high-quality ranking based on the EPHPP criteria. One study exhibited weakness in selection bias, while the other five studies fell into the moderate category. Three studies lacked confounding controls, and four studies were classified as moderate in this aspect. One study displayed weaknesses in withdrawal and dropout. Overall, five studies were categorized as weak in quality (Table 2).
Table 2. Summary of EPHPP quality assessment ratings
Characteristics of the studies included
Geographically, the included studies originated from six different countries classified as developed countries, including China (n=4), the United States (n=3), the United Kingdom, and Ireland, each contributing two studies, and one study each from Israel and New Zealand. The number of participants in the study, drawn from both secondary and direct data sources, ranged from 187 to 95,054 older adults. There were no reports of restrictions on characteristics based on gender or other significant attributes. The ethnic variable of each participant was also documented, indicating a general and random sampling approach. Each study highlighted significant ethnic diversity among participants, particularly in European and American countries.
Loneliness effect on sleep
The reviews included in this study indicated a significant degree of correlation between the research outcomes. However, the research did not find any connection between loneliness and poor sleep, or poor sleep quality in the elderly.
Discussion
The present review aimed to explore the interconnection between loneliness, social isolation, and sleep. Loneliness is prevalent among the elderly [39], particularly in developed countries facing significant economic pressures to meet daily needs [40-44]. Consequently, this situation notably affects non-productive groups such as the elderly. Several studies have highlighted the impact of loneliness on health conditions across all age groups [45-49]. In certain instances, there is a high likelihood of individuals experiencing dangerous psychological disorders like suicidal ideation [50, 51]. Loneliness can be a subjective feeling that one person may encounter while others may not, even in similar circumstances [52]. A theory suggests that an individual’s capacity to adapt to an environment or stressor varies considerably. There is no certainty regarding whether a person can effectively cope with it [53-55].
Loneliness among the elderly served as a triggering factor for sleep disturbances. Reduced sleep quality in the elderly may manifest as insomnia [56], sleep latency [57], alterations in circadian rhythms [58], and snoring [59]. A study indicates that social isolation acts as an intermediary linking the occurrence of sleep disturbances. However, as highlighted by Yu et al. [38], both social isolation and loneliness may have distinct roles in contributing to sleep difficulties. The impact of social isolation on sleep problems could persist for a longer duration compared to self-reported loneliness, or it is plausible that social isolation exacerbates sleep issues in individuals experiencing loneliness.
In addition to social isolation, depression also contributes to changes in sleep patterns among the elderly. McHugh & Lawlor [34] demonstrate that there is a relationship between depression, as measured by HADS and PSQI scores, in the elderly. Numerous studies have established a strong connection between these two factors, with depression identified as a primary psychological element contributing to sleep-related issues in elderly individuals. Negative endorsements provide substantial support for a significant relationship between depression and sleep patterns in the elderly, as evidenced by several items in the PSQI assessment. Yao et al. [37] emphasize that depression significantly impacts sleep quality, underscoring the importance of addressing depression not only for mental well-being but also for enhancing overall sleep quality. Depressed individuals exhibit higher total brain glucose metabolism than healthy individuals in the non-REM stage [60], supporting the over-arousal hypothesis in depressed individuals. The reduction in brain activity from the wakeful state to non-REM sleep may be hindered by hypo-frontality during wakefulness [61]. Typically, there is a noticeable decrease in cortical brain activity during non-REM sleep in healthy individuals. This decline in brain activity from pre-sleep to non-REM phases is believed to aid in the restoration of cognitive function during sleep. Conversely, individuals experiencing depression may struggle to reduce cortical activity, especially in the frontal region, leading to sleep disturbances and non-refreshing sleep [62].
Considering other variables, particularly depression, diminishes the connection between loneliness and sleep disruption, highlighting a close association between loneliness and depression. However, solely focusing on depression does not fully elucidate the interplay among depression, loneliness, and sleep disturbance [39]. Further investigation is necessary to comprehend how loneliness and sleep disruption are intertwined with depression, encompassing their relationships with additional elements such as demographic factors.
We did not find any evidence suggesting that age or gender influences the correlation between loneliness and sleep disruption. Consistent with previous comprehensive studies examining social relationships, isolation, loneliness, and social support, gender did not emerge as a factor influencing this connection [4, 63]. However, the available information on age as a moderating factor is inconclusive: In younger groups, the association between mortality, loneliness, isolation, and living alone appears more pronounced [4]. Conversely, another meta-analysis indicated a stronger relationship between mortality and social support in the elderly [63]. Despite this discrepancy, age was not identified as a moderator in these studies. Age was only viewed as a risk factor and a source of resilience in later life in these analyses. Consequently, protective mechanisms might become apparent later in adulthood, potentially altering the relationship between loneliness and sleep disruption in the opposite direction.
We acknowledge the existence of limitations in the current study that may impact the general applicability of the findings. Therefore, future researchers utilizing the results of this study must exercise caution in their interpretations. The limitations of this study are linked to the non-exhaustive literature search primarily due to the authors’ limited access to high-quality databases, hindering swift access to the databases in question. Additionally, we restricted articles to those published in English. However, we do not discount the possibility that numerous high-quality articles may exist in languages other than English.
The World Health Organization’s report outlines strategies to combat loneliness, emphasizing the identification of high-risk individuals and the implementation of diverse approaches, including group interactions and technology-based initiatives, ideally with interactive and socially beneficial components. These interventions should be customized based on specific population characteristics, taking into account cultural diversity, institutional settings, and physical limitations. Strategies aimed at reducing loneliness should be incorporated into sleep improvement programs designed for older adults facing sleep challenges.
Conclusion
Feelings of loneliness and social isolation are linked to decreased sleep quality among older individuals.
Acknowledgments: We extend our gratitude to all involved parties, especially the dean of the Medical College at Haluoleo University and the director of Karya Kesehatan School of Health Sciences.
Ethical Permissions: Not applicable.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors’ Contribution: Umrana S (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (60%); Risnawati (Second Author), Assistant Researcher/Discussion Writer (15%); Susanty S (Third Author), Introduction Writer/Assistant Researcher/Discussion Writer/Statistical Analyst (15%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Loneliness encompasses an individual’s subjective perception of emotional distress stemming from inadequate social connections in terms of quality or quantity [1]. In contrast, social isolation denotes an objective absence of social interactions [2]. Both loneliness and social isolation have been linked to declining health and heightened mortality rates in elderly populations [3, 4]. Despite their correlation, these two phenomena are distinct; a person experiencing loneliness may not necessarily be socially isolated, and vice versa [5, 6].
The issue of elderly individuals living alone is a significant societal concern often overlooked, and its prevalence has surged due to growing economic pressures [7]. The circumstance arises from various factors like separation from a spouse, children, or a desire for independence [8]. Loneliness encompasses a complex range of emotions tied to unmet social and personal needs and is closely intertwined with social isolation, particularly prevalent among older adults. A longitudinal study conducted over eight years revealed that 9% of the elderly population in the UK experience severe loneliness, while 30% have mild loneliness, indicating the importance of strong social networks and good health in preventing loneliness. Furthermore, the growth of the elderly population has resulted in a surge in the number of seniors residing in long-term care institutions [9].
Numerous research endeavors spanning various countries, such as Australia, Iran, Malaysia, and the United States have delved into the escalating issue of loneliness among older individuals [10-12]. These studies primarily focused on examining the correlation between community engagement and feelings of loneliness. In Malaysia, particular attention was given to exploring the link between loneliness and the involvement of older adults in religious activities, which often serve as a cornerstone for social interactions in numerous cultures and offer external support. As the global population ages at a swift pace, fostering a sense of community becomes increasingly crucial, especially considering the revelation of the World Health Organization (WHO) regarding the substantial surge in older people living in solitude worldwide, including in rural areas [13].
The literature discusses different forms of social isolation, categorizing them as subjective and objective. Subjective social isolation refers to the personal perception of inadequate social resources, like companionship or support from others [14]. Studies have consistently shown a direct link between both types of social isolation and conditions like sleep disruptions, depression, and fatigue. Emotional loneliness, a form of subjective social isolation rooted in inadequate support from peers, is strongly linked to reduced sleep quality [15]. Wakefield et al. [16] reported that individuals with strong social connections experience better sleep.
Interrupted sleep, and insufficient time for recuperation, have been proposed to interfere with typical hormonal, metabolic, and neurological functions [17], leading to declining health [18], diminished life satisfaction [19], and heightened mortality rates [20]. Additionally, numerous other factors contributing to sleep disorders and disruptions have been identified, such as being female, economic hardship [21], loss of a spouse [22], early signs of cognitive decline [23], feelings of depression [24], respiratory issues, cardiovascular conditions [25], and even cancer [26].
The previous systematic review elucidated the correlation between social relationships, particularly close ones, and individuals’ sleep patterns. However, these studies encompassed a broad spectrum of research across different age groups and health statuses [27]. The present review aimed to thoroughly examine the existing body of literature regarding the connection between loneliness, social isolation, and sleep. A systematic investigation was carried out to analyze the current state of research on the correlation between feelings of isolation and sleep patterns, giving particular attention to how samples were selected and measurements were conducted.
Information and Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines 2020 [28].
Inclusion criteria
The inclusion criteria were studies in English assessing the elderly as defined by the WHO aged 65 years or older and also those discussing the relationship between loneliness or social isolation among the elderly and all forms of sleep disturbances. Also, the included studies should be observational or mixed methods studies. For the study location, we limited it to the community or locations outside of geriatric service facilities, such as nursing homes or similar hospitals. Typically, there were well-structured or scheduled programs for the elderly in the neighborhood, even if their next of kin visits infrequently. Additionally, the elderly may feel more engaged when reside in such environments due to the presence of other elderly that creates a more comfortable atmosphere for them. Studies involving sleep disorders, like sleep apnea and other severe disorders were excluded. Dissertations, proceedings, books, commentaries, case studies, and systematic reviews were also eliminated.
Search strategy
We utilized four reputable electronic databases to search for relevant literature, namely PubMed, Cochrane Library, Wiley Online Library, and ScienceDirect. To ensure the collection of all relevant articles in each database, a filter was applied to include the studies conducted from 2000 to October 2022. The exploration involved combining keywords associated with loneliness and its related aspects, along with terms related to social isolation and its impact on sleep patterns. The search was conducted by examining subject headings (MeSH terms) and reviewing both the title and the content within the abstracts of the articles. Search terms were adjusted as necessary for different databases. The search terms used are ((((((((((((("loneliness" [MeSH terms]) OR ("loneliness/psychology" [MeSH terms])) AND ("social isolation" [MeSH terms])) OR ("social isolation/complications" [MeSH terms])) OR ("social isolation/diagnosis" [MeSH terms])) AND ("sleep" [MeSH terms]))) OR ("sleep duration" [MeSH terms])) OR ("sleep latency" [MeSH terms])) OR ("sleep quality" [MeSH terms])))) AND (elderly [Title/Abstract])) OR ("older adult" [Title/Abstract]).
The review involved examining the reference lists of selected studies obtained through electronic searches and review of the articles. We manually explored other potentially relevant studies, including dissertations, conference reports, and unpublished sources, by employing unrestricted text and keyword queries in Zetoc (a platform for conference records) and OpenGrey (a repository for grey literature in Europe). In cases where necessary or feasible, we reached out to authors via email to acquire full text or seek clarification on specific points.
Selection process
Three reviewers individually selected studies for inclusion in the review (STU, RSI, and SRS). They screened all titles of the identified studies. Subsequently, they reviewed the abstracts of relevant studies and retrieved and examined the full texts of those still considered potentially pertinent. Another reviewer cross-checked all studies approved by one assessor to ensure compliance with the inclusion criteria during the selection process. The consensus between reviewers exceeded 99%. Any queries regarding inclusion or exclusion were resolved through discussions involving a third evaluator (STU, RSI, and SRS).
Quality appraisal
The included studies underwent evaluation concerning study design, methodology, and analysis. Subsequently, the studies were categorized as strong, moderate, or weak based on the criteria outlined in the EPHPP tool. This tool assesses studies using specific criteria, such as selection bias, study design, confounding factors, blinding, data collection techniques, withdrawals, drop-outs, intervention integrity (for intervention studies), and analyses. It demonstrated significant consistency among individual components and a notable intra-class correlation coefficient. These methods for assessing quality and the resulting ratings assess the credibility of individual studies. They do not aim to compare the significance of findings across studies but rather indicated the robustness of the study and, consequently, the confidence or reliability of the study’s outcomes.
Findings
Study selection
A systematic electronic search yielded a total of 13,418 publications through a comprehensive examination of related papers. Subsequent screening of full-text articles was conducted on 12,376 papers. During the full-text screening phase, 88 of these papers did not meet the eligibility criteria, resulting in a total of 13 articles deemed suitable for further in-depth investigation (Figure 1).
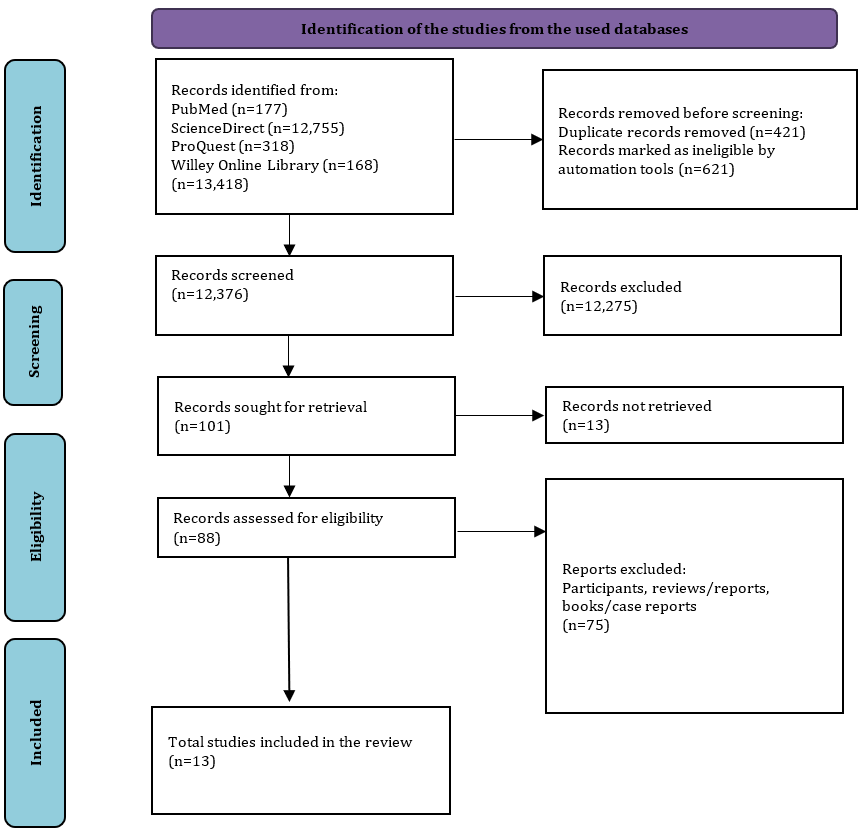
Figure 1. PRISMA flow diagram of the literature search
The characteristics of the included studies extracted in terms of their design, sample, outcomes, tools and findings (Table 1).
Table 1. Characteristics of studies included
Study quality
The moderately weighted cross-sectional design of quantitative research prevented them from receiving a high-quality ranking based on the EPHPP criteria. One study exhibited weakness in selection bias, while the other five studies fell into the moderate category. Three studies lacked confounding controls, and four studies were classified as moderate in this aspect. One study displayed weaknesses in withdrawal and dropout. Overall, five studies were categorized as weak in quality (Table 2).
Table 2. Summary of EPHPP quality assessment ratings
Characteristics of the studies included
Geographically, the included studies originated from six different countries classified as developed countries, including China (n=4), the United States (n=3), the United Kingdom, and Ireland, each contributing two studies, and one study each from Israel and New Zealand. The number of participants in the study, drawn from both secondary and direct data sources, ranged from 187 to 95,054 older adults. There were no reports of restrictions on characteristics based on gender or other significant attributes. The ethnic variable of each participant was also documented, indicating a general and random sampling approach. Each study highlighted significant ethnic diversity among participants, particularly in European and American countries.
Loneliness effect on sleep
The reviews included in this study indicated a significant degree of correlation between the research outcomes. However, the research did not find any connection between loneliness and poor sleep, or poor sleep quality in the elderly.
Discussion
The present review aimed to explore the interconnection between loneliness, social isolation, and sleep. Loneliness is prevalent among the elderly [39], particularly in developed countries facing significant economic pressures to meet daily needs [40-44]. Consequently, this situation notably affects non-productive groups such as the elderly. Several studies have highlighted the impact of loneliness on health conditions across all age groups [45-49]. In certain instances, there is a high likelihood of individuals experiencing dangerous psychological disorders like suicidal ideation [50, 51]. Loneliness can be a subjective feeling that one person may encounter while others may not, even in similar circumstances [52]. A theory suggests that an individual’s capacity to adapt to an environment or stressor varies considerably. There is no certainty regarding whether a person can effectively cope with it [53-55].
Loneliness among the elderly served as a triggering factor for sleep disturbances. Reduced sleep quality in the elderly may manifest as insomnia [56], sleep latency [57], alterations in circadian rhythms [58], and snoring [59]. A study indicates that social isolation acts as an intermediary linking the occurrence of sleep disturbances. However, as highlighted by Yu et al. [38], both social isolation and loneliness may have distinct roles in contributing to sleep difficulties. The impact of social isolation on sleep problems could persist for a longer duration compared to self-reported loneliness, or it is plausible that social isolation exacerbates sleep issues in individuals experiencing loneliness.
In addition to social isolation, depression also contributes to changes in sleep patterns among the elderly. McHugh & Lawlor [34] demonstrate that there is a relationship between depression, as measured by HADS and PSQI scores, in the elderly. Numerous studies have established a strong connection between these two factors, with depression identified as a primary psychological element contributing to sleep-related issues in elderly individuals. Negative endorsements provide substantial support for a significant relationship between depression and sleep patterns in the elderly, as evidenced by several items in the PSQI assessment. Yao et al. [37] emphasize that depression significantly impacts sleep quality, underscoring the importance of addressing depression not only for mental well-being but also for enhancing overall sleep quality. Depressed individuals exhibit higher total brain glucose metabolism than healthy individuals in the non-REM stage [60], supporting the over-arousal hypothesis in depressed individuals. The reduction in brain activity from the wakeful state to non-REM sleep may be hindered by hypo-frontality during wakefulness [61]. Typically, there is a noticeable decrease in cortical brain activity during non-REM sleep in healthy individuals. This decline in brain activity from pre-sleep to non-REM phases is believed to aid in the restoration of cognitive function during sleep. Conversely, individuals experiencing depression may struggle to reduce cortical activity, especially in the frontal region, leading to sleep disturbances and non-refreshing sleep [62].
Considering other variables, particularly depression, diminishes the connection between loneliness and sleep disruption, highlighting a close association between loneliness and depression. However, solely focusing on depression does not fully elucidate the interplay among depression, loneliness, and sleep disturbance [39]. Further investigation is necessary to comprehend how loneliness and sleep disruption are intertwined with depression, encompassing their relationships with additional elements such as demographic factors.
We did not find any evidence suggesting that age or gender influences the correlation between loneliness and sleep disruption. Consistent with previous comprehensive studies examining social relationships, isolation, loneliness, and social support, gender did not emerge as a factor influencing this connection [4, 63]. However, the available information on age as a moderating factor is inconclusive: In younger groups, the association between mortality, loneliness, isolation, and living alone appears more pronounced [4]. Conversely, another meta-analysis indicated a stronger relationship between mortality and social support in the elderly [63]. Despite this discrepancy, age was not identified as a moderator in these studies. Age was only viewed as a risk factor and a source of resilience in later life in these analyses. Consequently, protective mechanisms might become apparent later in adulthood, potentially altering the relationship between loneliness and sleep disruption in the opposite direction.
We acknowledge the existence of limitations in the current study that may impact the general applicability of the findings. Therefore, future researchers utilizing the results of this study must exercise caution in their interpretations. The limitations of this study are linked to the non-exhaustive literature search primarily due to the authors’ limited access to high-quality databases, hindering swift access to the databases in question. Additionally, we restricted articles to those published in English. However, we do not discount the possibility that numerous high-quality articles may exist in languages other than English.
The World Health Organization’s report outlines strategies to combat loneliness, emphasizing the identification of high-risk individuals and the implementation of diverse approaches, including group interactions and technology-based initiatives, ideally with interactive and socially beneficial components. These interventions should be customized based on specific population characteristics, taking into account cultural diversity, institutional settings, and physical limitations. Strategies aimed at reducing loneliness should be incorporated into sleep improvement programs designed for older adults facing sleep challenges.
Conclusion
Feelings of loneliness and social isolation are linked to decreased sleep quality among older individuals.
Acknowledgments: We extend our gratitude to all involved parties, especially the dean of the Medical College at Haluoleo University and the director of Karya Kesehatan School of Health Sciences.
Ethical Permissions: Not applicable.
Conflicts of Interests: The authors reported no conflicts of interests.
Authors’ Contribution: Umrana S (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer (60%); Risnawati (Second Author), Assistant Researcher/Discussion Writer (15%); Susanty S (Third Author), Introduction Writer/Assistant Researcher/Discussion Writer/Statistical Analyst (15%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Article Type: Systematic Review |
Subject:
Quality of Life
Received: 2023/12/18 | Accepted: 2024/04/5 | Published: 2024/06/21
Received: 2023/12/18 | Accepted: 2024/04/5 | Published: 2024/06/21
References
1. Nicolaisen M, Thorsen K. Who are lonely? Loneliness in different age groups (18-81 years old), using two measures of loneliness. Int J Aging Hum Dev. 2014;78(3):229-57. [Link] [DOI:10.2190/AG.78.3.b]
2. Kim J, Park GR. Prolonged social isolation and cognitive function in older adults: Lack of informal social contact versus formal social activity as the source of social isolation. Aging Ment Health. 2023;27(12):2438-45. [Link] [DOI:10.1080/13607863.2023.2202616]
3. Kobayashi LC, Steptoe A. Social isolation, loneliness, and health behaviors at older ages: Longitudinal cohort study. Ann Behav Med. 2018;52(7):582-93. [Link] [DOI:10.1093/abm/kax033]
4. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015;10(2):227-37. [Link] [DOI:10.1177/1745691614568352]
5. Beller J, Wagner A. Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. 2018;37(9):808-13. [Link] [DOI:10.1037/hea0000605]
6. McLay L, Jamieson HA, France KG, Schluter PJ. Loneliness and social isolation is associated with sleep problems among older community dwelling women and men with complex needs. Sci Rep. 2021;11(1):4877. [Link] [DOI:10.1038/s41598-021-83778-w]
7. Reher D, Requena M. Living alone in later life: A global perspective. Popul Dev Rev. 2018;44(3):427-54. [Link] [DOI:10.1111/padr.12149]
8. Kaplan DB. Older adults living alone [Internet]. Rahway, NJ: MSD Manuals. 2023 Apr [cited 2023; April]. Available from: https://www.msdmanuals.com/professional/geriatrics/social-issues-in-older-adults/older-adults-living-alone [Link]
9. De Medeiros MMD, Carletti TM, Magno MB, Maia LC, Cavalcanti YW, Rodrigues-Garcia RCM. Does the institutionalization influence elderly's quality of life? A systematic review and meta-analysis. BMC Geriatr. 2020;20(1):44. [Link] [DOI:10.1186/s12877-020-1452-0]
10. Khosravan S, Alaviani M, Alami A, Tavakolizadeh J. Epidemiology of loneliness in elderly women. J Res Health. 2014;4(4):871-7. [Link]
11. Tani M, Cheng Z, Piracha M, Wang B. Ageing, health, loneliness and wellbeing. Soc Indic Res. 2020;160(2-3):791-807. [Link] [DOI:10.1007/s11205-020-02450-4]
12. Teh JKL, Tey NP, Ng ST. Family support and loneliness among older persons in multiethnic Malaysia. Sci World J. 2014;2014:654382. [Link] [DOI:10.1155/2014/654382]
13. WHO. Abuse of older people [Internet]. Geneva: World Health Organization. 2022 Jun 13 [cited June 15, 2022]. Available from: https://www.who.int/news-room/fact-sheets/detail/abuse-of-older-people [Link]
14. Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health. 2020;20(1):129. [Link] [DOI:10.1186/s12889-020-8251-6]
15. Cho JHJ, Olmstead R, Choi H, Carrillo C, Seeman TE, Irwin MR. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging Ment Health. 2019;23(9):1130-8. [Link] [DOI:10.1080/13607863.2018.1481928]
16. Wakefield JRH, Bowe M, Kellezi B, Butcher A, Groeger JA. Longitudinal associations between family identification, loneliness, depression, and sleep quality. Br J Health Psychol. 2020;25(1):1-16. [Link] [DOI:10.1111/bjhp.12391]
17. Medic G, Wille M, Hemels MEH. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151-61. [Link] [DOI:10.2147/NSS.S134864]
18. Morin CM, Jarrin DC. Epidemiology of insomnia: Prevalence, course, risk factors, and public health burden. Sleep Med Clin. 2022;17(2):173-91. [Link] [DOI:10.1016/j.jsmc.2022.03.003]
19. Choi EPH, Wan EYF, Kwok JYY, Chin WY, Lam CLK. The mediating role of sleep quality in the association between nocturia and health-related quality of life. Health Qual Life Outcomes. 2019;17(1):181. [Link] [DOI:10.1186/s12955-019-1251-5]
20. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-4. [Link] [DOI:10.5665/sleep.4716]
21. Etindele Sosso FA, Kreidlmayer M, Pearson D, Bendaoud I. Towards a socioeconomic model of sleep health among the Canadian population: A systematic review of the relationship between age, income, employment, education, social class, socioeconomic status and sleep disparities. Eur J Investig Health Psychol Educ. 2022;12(8):1143-67. [Link] [DOI:10.3390/ejihpe12080080]
22. De Feijter M, O'Connor MF, Arizmendi BJ, Ikram MA, Luik AI. The longitudinal association of actigraphy-estimated sleep with grief in middle-aged and elderly persons. J Psychiatr Res. 2021;137:66-72. [Link] [DOI:10.1016/j.jpsychires.2021.02.042]
23. You JC, Jones E, Cross DE, Lyon AC, Kang H, Newberg AB, et al. Association of β-amyloid burden with sleep dysfunction and cognitive impairment in elderly individuals with cognitive disorders. JAMA Netw Open. 2019;2(10):e1913383. [Link] [DOI:10.1001/jamanetworkopen.2019.13383]
24. Yang JJ, Cai H, Xia L, Nie W, Zhang Y, Wang S, et al. The prevalence of depressive and insomnia symptoms, and their association with quality of life among older adults in rural areas in China. Front Psychiatry. 2021;12:727939. [Link] [DOI:10.3389/fpsyt.2021.727939]
25. Mc Carthy CE. Sleep disturbance, sleep disorders and co-morbidities in the care of the older person. Med Sci. 2021;9(2):31. [Link] [DOI:10.3390/medsci9020031]
26. Strollo SE, Fallon EA, Gapstur SM, Smith TG. Cancer-related problems, sleep quality, and sleep disturbance among long-term cancer survivors at 9-years post diagnosis. Sleep Med. 2020;65:177-85. [Link] [DOI:10.1016/j.sleep.2019.10.008]
27. Gordon AM, Carrillo B, Barnes CM. Sleep and social relationships in healthy populations: A systematic review. Sleep Med Rev. 2021;57:101428. [Link] [DOI:10.1016/j.smrv.2021.101428]
28. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. [Link] [DOI:10.1136/bmj.n160]
29. Benson JA, McSorley VE, Hawkley LC, Lauderdale DS. Associations of loneliness and social isolation with actigraph and self-reported sleep quality in a national sample of older adults. Sleep. 2021;44(1):zsaa140. [Link] [DOI:10.1093/sleep/zsaa140]
30. Griffin SC, Williams AB, Mladen SN, Perrin PB, Dzierzewski JM, Rybarczyk BD. Reciprocal effects between loneliness and sleep disturbance in older Americans. J Aging Health. 2020;32(9):1156-64. [Link] [DOI:10.1177/0898264319894486]
31. Grossman ES, Hoffman YSG, Palgi Y, Shrira A. COVID-19 related loneliness and sleep problems in older adults: Worries and resilience as potential moderators. Pers Individ Dif. 2021;168:110371. [Link] [DOI:10.1016/j.paid.2020.110371]
32. Jia G, Yuan P. The association between sleep quality and loneliness in rural older individuals: A cross-sectional study in Shandong Province, China. BMC Geriatr. 2020;20(1):180. [Link] [DOI:10.1186/s12877-020-01554-3]
33. McHugh JE, Casey AM, Lawlor BA. Psychosocial correlates of aspects of sleep quality in community-dwelling Irish older adults. Aging Ment Health. 2011;15(6):749-55. [Link] [DOI:10.1080/13607863.2011.562180]
34. McHugh JE, Lawlor BA. Perceived stress mediates the relationship between emotional loneliness and sleep quality over time in older adults. Br J Health Psychol. 2013;18(3):546-55. [Link] [DOI:10.1111/j.2044-8287.2012.02101.x]
35. Peng A, Tang Y, He S, Ji S, Dong B, Chen L. Association between loneliness, sleep behavior and quality: A propensity-score-matched case-control study. Sleep Med. 2021;86:19-24. [Link] [DOI:10.1016/j.sleep.2021.08.008]
36. Shankar A. Loneliness and sleep in older adults. Social psychiatry and psychiatric epidemiology. 2020;55(2):269-72. [Link] [DOI:10.1007/s00127-019-01805-8]
37. Yao KW, Yu S, Cheng SP, Chen IJ. Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. J Nurs Res. 2008;16(2):131-9. [Link] [DOI:10.1097/01.JNR.0000387298.37419.ff]
38. Yu B, Steptoe A, Niu K, Ku PW, Chen LJ. Prospective associations of social isolation and loneliness with poor sleep quality in older adults. Qual Life Res. 2018;27(3):683-91. [Link] [DOI:10.1007/s11136-017-1752-9]
39. Wong A, Chau AKC, Fang Y, Woo J. Illuminating the psychological experience of elderly loneliness from a societal perspective: A qualitative study of alienation between older people and society. Int J Environ Res Public Health. 2017;14(7):824. [Link] [DOI:10.3390/ijerph14070824]
40. Esmaeilzadeh S, Oz F. Effect of psychosocial care model applied in an "elderly day care center" on loneliness, depression, quality of life, and elderly attitude. Niger J Clin Pract. 2020;23(2):189-97. [Link] [DOI:10.4103/njcp.njcp_366_19]
41. Pandya SP. Meditation program mitigates loneliness and promotes wellbeing, life satisfaction and contentment among retired older adults: A two-year follow-up study in four South Asian cities. Aging Ment Health. 2021;25(2):286-98. [Link] [DOI:10.1080/13607863.2019.1691143]
42. Shorey S, Chan V. The experiences and needs of Asian older adults who are socially isolated and lonely: A qualitative systematic review. Arch Gerontol Geriatr. 2021;92:104254. [Link] [DOI:10.1016/j.archger.2020.104254]
43. Ojembe BU, Ebe Kalu M. Describing reasons for loneliness among older people in Nigeria. J Gerontol Soc Work. 2018;61(6):640-58. [Link] [DOI:10.1080/01634372.2018.1487495]
44. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Glob Health Res Policy. 2020;5:27. [Link] [DOI:10.1186/s41256-020-00154-3]
45. Christiansen J, Larsen FB, Lasgaard M. Do stress, health behavior, and sleep mediate the association between loneliness and adverse health conditions among older people?. Soc Sci Med. 2016;152:80-6. [Link] [DOI:10.1016/j.socscimed.2016.01.020]
46. Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. 2015;105(5):1013-9. [Link] [DOI:10.2105/AJPH.2014.302427]
47. Crewdson JA. The effect of loneliness in the elderly population: A review. Healthy Aging Clin Care Elder. 2016;8:1-8. [Link] [DOI:10.4137/HACCE.S35890]
48. Yanguas J, Pinazo-Henandis S, Tarazona-Santabalbina FJ. The complexity of loneliness. Acta Biomedica. 2018;89(2):302-14. [Link]
49. Petitte T, Mallow J, Barnes E, Petrone A, Barr T, Theeke L. A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol J. 2015;8(Suppl 2):113-32. [Link] [DOI:10.2174/1874350101508010113]
50. Antonelli-Salgado T, Monteiro GMC, Marcon G, Roza TH, Zimerman A, Hoffmann MS, et al. Loneliness, but not social distancing, is associated with the incidence of suicidal ideation during the COVID-19 outbreak: A longitudinal study. J Affect Disord. 2021;290:52-60. [Link] [DOI:10.1016/j.jad.2021.04.044]
51. McClelland H, Evans JJ, Nowland R, Ferguson E, O'Connor RC. Loneliness as a predictor of suicidal ideation and behaviour: A systematic review and meta-analysis of prospective studies. J Affect Disord. 2020;274:880-96. [Link] [DOI:10.1016/j.jad.2020.05.004]
52. Tkach E. Psychological features of the relationship of personality resilience and subjective feelings of loneliness. E3S Web Conf. 2021;284(107):08022. [Link] [DOI:10.1051/e3sconf/202128408022]
53. Chen L, Alston M, Guo W. The influence of social support on loneliness and depression among older elderly people in China: Coping styles as mediators. J Community Psychol. 2019;47(5):1235-45. [Link] [DOI:10.1002/jcop.22185]
54. Galiana L, Tomás JM, Fernández I, Oliver A. Predicting well-being among the elderly: The role of coping strategies. Front Psychol. 2020;11:00616. [Link] [DOI:10.3389/fpsyg.2020.00616]
55. Shen S, Wan Y, Xie Y, Chen Z, Li F. Care stress experienced by caregivers of elderly individuals with disabilities and the coping strategies utilized: A survey study in the city of Nanjing, China. J Fam Issues. 2019;40(10):1396-414. [Link] [DOI:10.1177/0192513X19841659]
56. Liu R, Shao W, Lai JK, Zhou L, Ren M, Sun N. Identification of comprehensive geriatric assessment-based risk factors for insomnia in elderly Chinese hospitalized patients. Aging Med. 2021;4(1):26-34. [Link] [DOI:10.1002/agm2.12146]
57. Suh SW, Han JW, Han JH, Bae J Bin, Moon W, Kim HS, et al. Sex differences in subjective age-associated changes in sleep: A prospective elderly cohort study. Aging. 2020;12(21):21942-58. [Link] [DOI:10.18632/aging.104016]
58. Garbarino S, Lanteri P, Sannita WG, Bragazzi NL, Scoditti E. Circadian rhythms, sleep, immunity, and fragility in the elderly: The model of the susceptibility to infections. Front Neurol. 2020;11:558417. [Link] [DOI:10.3389/fneur.2020.558417]
59. Song J, Wang C, Ma A, Zheng H, Zheng W, Hou X, et al. Self-reported snoring is associated with chronic kidney disease independent of metabolic syndrome in middle-aged and elderly Chinese. J Diabetes Investig. 2019;10(1):124-30. [Link] [DOI:10.1111/jdi.12855]
60. Kay DB, Karim HT, Hasler BP, James JA, Germain A, Hall MH, et al. Impact of acute sleep restriction on cerebral glucose metabolism during recovery non-rapid eye movement sleep among individuals with primary insomnia and good sleeper controls. Sleep Med. 2019;55:81-91. [Link] [DOI:10.1016/j.sleep.2018.12.007]
61. Tubbs AS. The mind after midnight: Nocturnal wakefulness and the answers project [dissertation]. Tucson: The University of Arizona; 2021. [Link]
62. Zhang R, Tomasi D, Manza P, Shokri-Kojori E, Demiral SB, Feldman DE, et al. Sleep disturbances are associated with cortical and subcortical atrophy in alcohol use disorder. Transl Psychiatry. 2021;11(1):428. [Link] [DOI:10.1038/s41398-021-01534-0]
63. Shor E, Roelfs DJ, Yogev T. The strength of family ties: A meta-analysis and meta-regression of self-reported social support and mortality. Soc Netw. 2013;35(4):626-38. [Link] [DOI:10.1016/j.socnet.2013.08.004]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







