Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 695-700 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rabiei H, Rabiei R, Arayeshgari M, Ghasemi T, Sadeghian E. Depression’s Associated Factors in Cancer Patients in Post-COVID-19 Pandemic. Health Educ Health Promot 2023; 11 (5) :695-700
URL: http://hehp.modares.ac.ir/article-5-72903-en.html
URL: http://hehp.modares.ac.ir/article-5-72903-en.html
1- “Neurosurgery Research Group (NRG)” and ”Student Research Committee”, Hamadan University of Medical Sciences, Hamadan, Iran
2- “Department of Nursing, School of Nursing and Midwifery” and “Student Research Committee”, Hamadan University of Medical Sciences, Hamadan, Iran
3- Department of Biostatistics, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4- Clinical Research Development Unit of Shahid Beheshti Hospital, Hamadan University of Medical Sciences, Hamadan, Iran
5- “Department of Nursing, School of Nursing and Midwifery” and “Chronic Diseases (Home care) Research Center”, Hamadan University of Medical Sciences, Hamadan, Iran
2- “Department of Nursing, School of Nursing and Midwifery” and “Student Research Committee”, Hamadan University of Medical Sciences, Hamadan, Iran
3- Department of Biostatistics, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
4- Clinical Research Development Unit of Shahid Beheshti Hospital, Hamadan University of Medical Sciences, Hamadan, Iran
5- “Department of Nursing, School of Nursing and Midwifery” and “Chronic Diseases (Home care) Research Center”, Hamadan University of Medical Sciences, Hamadan, Iran
Full-Text [PDF 595 kb]
(2281 Downloads)
| Abstract (HTML) (905 Views)
Full-Text: (90 Views)
Introduction
The estimated number of new cancer cases worldwide in 2020 was 19.3 million, resulting in 10 million deaths. It is predicted that by 2040, the global burden of cancer will rise to 28.4 million cases, indicating a 47% increase compared to 2020 [1]. In Iran, cancer is ranked as the second most prevalent chronic non-communicable disease and the third leading cause of death, following heart disease, accidents, and other natural phenomena [2]. A cancer diagnosis has a profound psychological impact on patients, as it remains one of the most feared illnesses. Consequently, many individuals diagnosed with cancer often experience psychological issues, such as depression [3].
Depression is a psychological impact experienced by cancer patients, leading to a lack of adherence to treatment procedures due to feelings of despair. This non-compliance can potentially contribute to higher mortality rates among individuals with cancer [4-6]. Research has consistently revealed a higher prevalence of depression among patients with chronic and fatal diseases, including cancer, than among healthy populations [7].
During chemotherapy, depression tends to worsen and can persist for a long time, even after the end of treatment. Moreover, it can contribute to the recurrence of the disease [8]. These feelings of depression often stem from perceived threats, such as the loss of bodily functions, changes in appearance, disruptions to family and life plans, thoughts of death, reduced quality of life, and unpleasant symptoms like pain, nausea, and fatigue [9]. Depression can hinder a patient's ability to cope with their illness, resulting in decreased acceptance of treatment and longer hospital stays. It also has a negative impact on the overall quality of life and increases the risk of suicide for patients. Furthermore, depression has been shown to have detrimental effects on patient outcomes, leading to higher mortality rates [10-12]. Research indicates that individuals experiencing depressive symptoms have a mortality rate that is 26% higher compared to those without such symptoms. Moreover, individuals diagnosed with major depression face a significantly higher mortality rate of 39% [13].
The release of neurobiological factors following depression can contribute to the spread of cancer and the progression of diseases [14]. Several factors may cause depression in these individuals, such as their reaction to a severe diagnosis and the anticipated decline in their health status, treatment with immune response modifiers, chemotherapy regimens, metabolic and endocrine changes, alterations in body image, chronic pain, and extensive surgical interventions [15, 16]. The isolation and quarantine of cancer patients during the COVID-19 pandemic may contribute to their depression. It is crucial for medical professionals to diagnose and address symptoms of depression, cognitive disorders, sleep problems, and fatigue in these patients as a top health priority [4]. As depression is associated with significant distress and disability, poor quality of life, increased physical symptoms such as pain and nausea, poor adherence to treatment, increased risk of suicide, poorer prognosis, and higher mortality, assessment, diagnosis, and timely treatment of depression would be preventive for many of these consequences [17-19]. It is crucial to assess the psychological distress of cancer patients to identify those needing support and additional evaluation, ultimately leading to appropriate healthcare intervention. This emphasizes the growing recognition of depression as a significant issue among cancer patients. The majority of research on depression in this population has originated from developed nations, with limited studies examining populations from low- and middle-income countries.
We planned to conduct a study in 2022, at the end of the COVID-19 pandemic, to examine the prevalence of depression among patients in the oncology department of Shahid Beheshti Hospital.
Instrument and Methods
In the present cross-sectional study, the research population included all patients admitted to the oncology department of Shahid Beheshti Hospital and Imam Khomeini Clinic, selected by the convenience sampling method in 2022. Among the advantages of sampling this way are easy access to participants, reduced research costs, and quick data collection. Still, because the sample was not chosen randomly, the sample will never be fully representative of the population being studied. Considering 5% alpha, "d" equal to 0.05, 80% power of the test, and 10% of biased questionnaires, the sample size was estimated to be 299 subjects using the Cochran formula. The inclusion criteria were selected based on previous similar studies. Patients who had the physical and mental capacity to respond to questions, a minimum of 6 months since their disease had been diagnosed, were aware of their diagnosis, absence of any adverse events history during the month to the time of the study, and lacked specific chronic physical or mental illnesses were the inclusion criteria. Otherwise, the obtained results may be related to recent events or physical and mental illness.
Afterward, the necessary permits were obtained to collect data from all participating patients who met the study's inclusion criteria. To begin, the researcher explained the objectives, study procedure, and confidentiality of the information to the patients. Afterward, the patients were asked to sign informed consent. Following that, the questionnaires were given to the patients for completion. On average, it took patients 15 minutes to complete the questionnaire. To ensure the patients' convenience, a specific time for questionnaire completion would not interfere with treatment or rest time. During the completion of the questionnaire, the researcher was available in the research setting to address any queries from the participants. Once the questionnaire was finished, the researcher collected them and expressed gratitude to the participants. The data for this study were gathered using two specific tools. The sampling process lasted nine months, from November 2021 to July 2022.
The demographic information questionnaire included factors such as age, gender, marital status, education level, underlying diseases, length of disease, length of chemotherapy, family size, and age at the onset of cancer. Ten faculty members of Hamadan University of Medical Sciences confirmed the validity of this questionnaire's face and content.
We utilized the BDI-II-Persian, a translated version of the Beck depression questionnaire, to assess depression in cancer patients. Numerous research studies have utilized the BDI-II-Persian questionnaire as a tool to evaluate the degree of depression among individuals [20-22]. The Beck depression scale comprises 21 questions that individuals must respond to using a four-point scale ranging from zero to three. The questionnaire covers various aspects such as sadness, pessimism, past failures, loss of pleasure, guilty feelings, punishment feelings, self-dislike, self-criticalness, crying, agitation, loss of interest, indecisiveness, worthlessness, loss of energy, changes in sleeping patterns, irritability, changes in appetite, difficulty concentrating, tiredness or fatigue, and loss of interest in sex. The test score ranges from zero to 63, with zero being the minimum and 63 being the maximum. The individual's overall score is determined by summing up the scores for each subject. The following scores can indicate the general level of depression: 0 to 13: No or minimal; 14 to 19: Mild; 20 to 28: Moderate; And 29 to 63: Severe depression. The BDI-II-Persian had high internal consistency (Cronbach's alpha=0.87) and acceptable test-retest reliability (r=0.74) [23].
Neglecting the adequate handling of the missing data can lead to biased estimates of parameters such as means or regression coefficients, culminating in inaccuracies in standard errors, confidence intervals, and the outcomes of significance tests. Multiple Imputation (MI) has emerged as a favored method for effectively addressing this issue. MI provides plausible estimations of missing values by harnessing the distribution of observed data. Multiple Imputation by Chained Equations (MICE) is a practical technique that employs diverse imputation models to manage missing data across variable types, ensuring a holistic approach to data imputation [24].
In the present study, initially, the "MICE" package of R software (version 4.1.1) was utilized to estimate the missing values (ranging from 0.3 to 32%) employing the MICE procedure. Then, descriptive statistics were performed to summarize and present the main characteristics of the dataset, one-way analysis of variance (ANOVA) was chosen to compare the mean of outcome variable between multiple groups, the Pearson correlation test to explore linear relationships between quantitative variables and the outcome variable, and the multiple linear regression model to examine the impact of the explanatory variables on the outcome variable. All these statistical analyses were performed using SPSS 25 software.
Findings
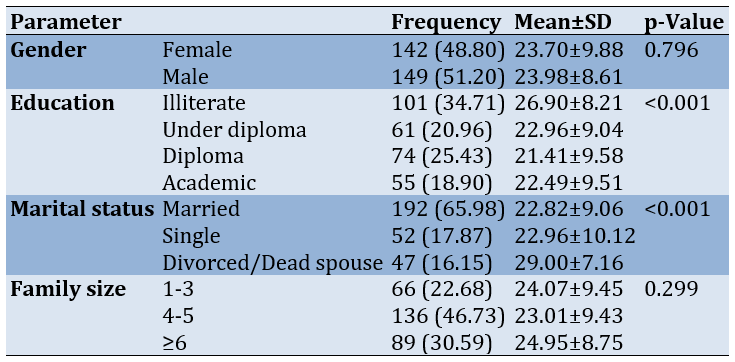
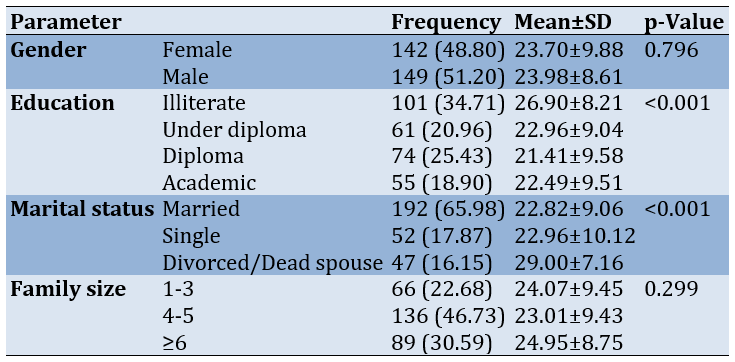
The mean age of the patients was 49.34±16.58 years, with the disease typically starting at a mean age of 47.56±16.45. The average duration of the disease was 21.29±16.92 months, and the average length of chemotherapy was 6.53±6.22 months. Depression was significantly associated with education (p<0.001) and marital status (p<0.001; Table 1).
Table 1. Frequency (numbers in parentheses are percentages) of the demographic characteristics of the participants (n=291) and comparing the mean of depression according to the demographic characteristics (one-way analysis of variance)
The Mean depression score was 23.84±9.24. Based on the cutoff points of 13 (mild), 19 (moderate), and 28 (severe) for a total score of depression, 48 patients (16.49%) suffered from mild depression (95%CI: 12.22-20.75), 114 patienAts (39.17%) suffered from moderate depression (95%CI: 33.56-44.77), and 89 (30.89%) suffered from severe depression (95%CI: 25.29-35.88).
The Pearson correlation coefficient also showed significant positive linear correlations between depression and age (r=0.21; p<0.001), age at onset of disease (r=0.20; p=0.001), length of disease (r=0.24; p<0.001) and length of chemotherapy (r=0.14; p=0.016).
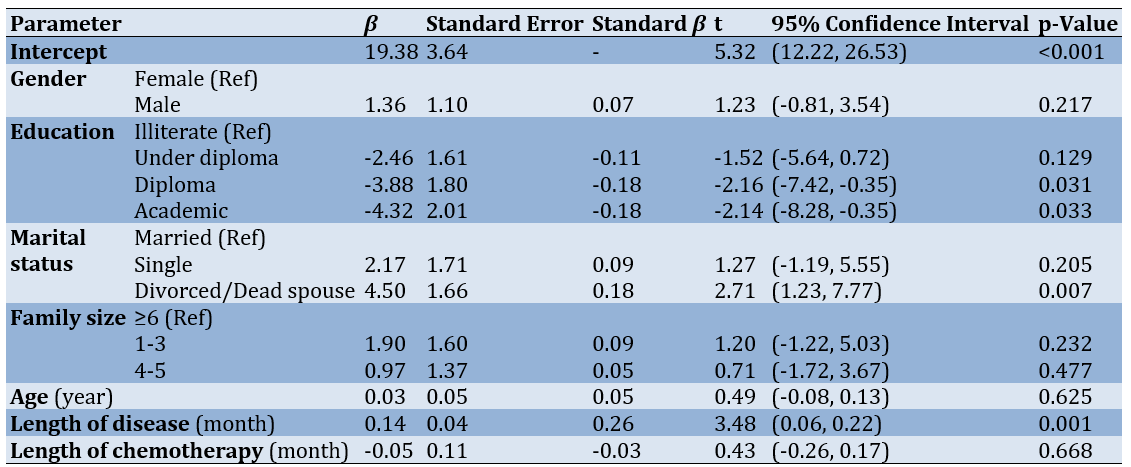
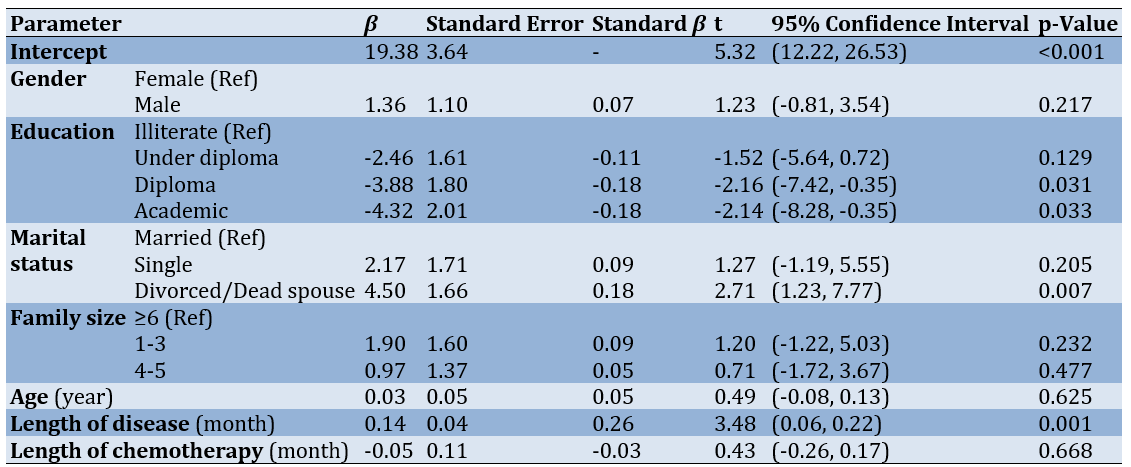
According to the multiple linear regression model, education, marital status, and length of disease were correlated with depression significantly. A diploma and an academic degree were associated with a decrease of 3.88 (p=0.031) and a decrease of 4.32 (p=0.033) in the depression score, respectively. The marital status of the "divorced/dead spouse" was associated with an increase of 4.50 in the depression score (p=0.007). An increase of one month in the length of the disease was associated with an increase of 0.14 in the depression score (p=0.001; Table 2).
Table 2. Identifying factors associated with depression score through a multiplSe linear regression model
Discussion
This study aims to investigate the occurrence of depression symptoms among Iranian cancer patients. The findings revealed a relatively high prevalence of depression among these patients, with approximately 39% (95%CI: 33.56%-44.77%) experiencing moderate depression and 30% (95%CI: 25.29%-35.88%) experiencing severe depression.
Aryankhesal et al. reported a depression prevalence of 35% (95%CI: 16%-70%) among Iranian cancer patients [25]. According to a study conducted by Darvishi et al., the prevalence of depression in cancer patients in Iran was reported to be 50.1% (95%CI: 40.6%-59.6%) [26]. The findings of this study were in line with Derakhshanfar's [27] research conducted in Iran on cancer patients. It was discovered that 38.2% of patients experienced moderate depression, while 28% experienced severe or very severe depression. Similar to Derakhshanfar's study, a significant correlation was observed between depression in these patients and factors such as age, education level, marital status, chemotherapy duration, or disease duration [27]. In another study, Adzrago et al. [28] assessed the prevalence of depression in cancer patients before and after the COVID-19 pandemic using the Patient Health Questionnaire. The prevalence of anxiety/depression symptoms among cancer patients was 32.7% before the COVID‐19 pandemic and 31.1% during the pandemic. However, they found that individuals aged 50-64 and over 65 had a lower likelihood of experiencing depression compared to those aged 35-49, which contradicts our study findings. One potential explanation for this discrepancy could be the disparity in geriatric care and support systems between these two cultures. There is coordination between Adzrago's study and ours as Adzrago reported a lower likelihood of depression in individuals with higher education levels, such as a college degree, than those with less than a high school education. This finding could be attributed to depression prevention courses in high schools or universities [28].
In other countries, several studies have been conducted to examine the prevalence of depression in cancer patients. For instance, Bakhiet et al. found that the prevalence of depression was 41.2% [29]. Ayalew et al. reported a higher rate of depression, with a prevalence of 58.8. Moreover, its result identified several independent factors significantly associated with depressive factors, including older age, unemployment, advanced stages of cancer such as stage III and stage IV, comorbid psychotic, and eating problems in the past two weeks [30]. Another study conducted by Naser et al. observed a lower prevalence of depressive symptoms, with 23.4% of all patients experiencing depression [31].
In line with the present study, the findings of a study conducted by Muche Belete et al. in 2021 showed that the prevalence of depression was 33.1% (95% CI=0.2858, 0.3761) [3].
The current study found a significant correlation between depression scores in cancer patients and various factors, including age, age at disease onset, duration of chemotherapy, duration of the disease, marital status, and education level. Specifically, illiterate cancer patients, those with a longer period of illness, and individuals who were widowed or divorced exhibited higher depression scores compared to the other groups. Taghavi et al. showed a significant relationship between a higher depression score and being widowed or divorced, consistent with our study [32]. Furthermore, the study conducted by Heidarirad et al. revealed a significant correlation between the depression score in women diagnosed with breast cancer and various factors, including age, marital status, presence of children, educational attainment, place of residence, type of treatment, number of interventions, disease severity, and history of previous cancer [33]. In justifying the correlation between the depression score and the level of education in this study as well as previous studies, having a higher education can be said to be associated with information sources and studies on cancer and its treatment methods can provide patients with a sense of hope and potentially reduce the likelihood of depression [33].
A cross-sectional study was conducted by Rajabizadeh et al. in Kerman, examining 120 breast cancer patients referred to the chemotherapy centers of this city. The study utilized the Beck questionnaire and found that 40.8% of the patients experienced moderate to severe depression. Additionally, the study identified a significant correlation between the patients' occupational status and level of education. As the level of education increased, the depression score exhibited a consistent decreasing trend, aligning with our own findings. Furthermore, our study found no substantial correlation between gender and depression, aligning with previous research. On the other hand, age, place of residence, marital status, and duration of chemotherapy showed no significant association in this study [34]. This disparity could be attributed to variations in the study populations, such as diverse cancer types, cultural disparities, other sociodemographic factors, and the consideration of depression severity.
One limitation of this study was that it did not consider the variations in cancer types and severity among different patients. As a result, it was not feasible to examine depression specifically in patients with a particular type of cancer due to insufficient sample size. A significant limitation was the high percentage of missing data for the chemotherapy duration, accounting for 32% of the total data. Considering the correlation between marital status and depression scores and its alignment with previous research, it is recommended that social and public institutions offer increased emotional support to widowed or divorced individuals with cancer. Regarding the relationship between depression scores and the duration of chemotherapy and the number of family members with depression scores, more studies should be done.
Conclusion
Most cancerous patients suffer moderate to severe depression. Cancer patients should undergo regular psychological evaluations to address depression when identified.
Acknowledgments: The authors would like to thank the staff of the oncology department of Shahid Beheshti Hospital and Imam Khomeini Clinic and the cancer patients who participated in this study.
Ethical Permission: The current study incorporated all ethical considerations, including adherence to the ethics code approved by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1399.1062).
Conflicts of Interests: All authors declare no conflict of interest.
Authors’ Contribution: Rabiei H (First Author), Methodologist/Main Researcher/Statistical Analyst (35%); Rabiei R (Second Author), Methodologist/Main Researcher (10%); Arayeshgari M (Third Author), Statistical Analyst (10%); Ghasemi T (Fourth Author), Assistant Researcher (10%); Sadeghian E (Fifth Author), Discussion Writer (35%)
Funding/Support: The Vice‐Chancellor of Research and Technology of Hamadan University of Medical Sciences supported this study (NO: 1400011051).
The estimated number of new cancer cases worldwide in 2020 was 19.3 million, resulting in 10 million deaths. It is predicted that by 2040, the global burden of cancer will rise to 28.4 million cases, indicating a 47% increase compared to 2020 [1]. In Iran, cancer is ranked as the second most prevalent chronic non-communicable disease and the third leading cause of death, following heart disease, accidents, and other natural phenomena [2]. A cancer diagnosis has a profound psychological impact on patients, as it remains one of the most feared illnesses. Consequently, many individuals diagnosed with cancer often experience psychological issues, such as depression [3].
Depression is a psychological impact experienced by cancer patients, leading to a lack of adherence to treatment procedures due to feelings of despair. This non-compliance can potentially contribute to higher mortality rates among individuals with cancer [4-6]. Research has consistently revealed a higher prevalence of depression among patients with chronic and fatal diseases, including cancer, than among healthy populations [7].
During chemotherapy, depression tends to worsen and can persist for a long time, even after the end of treatment. Moreover, it can contribute to the recurrence of the disease [8]. These feelings of depression often stem from perceived threats, such as the loss of bodily functions, changes in appearance, disruptions to family and life plans, thoughts of death, reduced quality of life, and unpleasant symptoms like pain, nausea, and fatigue [9]. Depression can hinder a patient's ability to cope with their illness, resulting in decreased acceptance of treatment and longer hospital stays. It also has a negative impact on the overall quality of life and increases the risk of suicide for patients. Furthermore, depression has been shown to have detrimental effects on patient outcomes, leading to higher mortality rates [10-12]. Research indicates that individuals experiencing depressive symptoms have a mortality rate that is 26% higher compared to those without such symptoms. Moreover, individuals diagnosed with major depression face a significantly higher mortality rate of 39% [13].
The release of neurobiological factors following depression can contribute to the spread of cancer and the progression of diseases [14]. Several factors may cause depression in these individuals, such as their reaction to a severe diagnosis and the anticipated decline in their health status, treatment with immune response modifiers, chemotherapy regimens, metabolic and endocrine changes, alterations in body image, chronic pain, and extensive surgical interventions [15, 16]. The isolation and quarantine of cancer patients during the COVID-19 pandemic may contribute to their depression. It is crucial for medical professionals to diagnose and address symptoms of depression, cognitive disorders, sleep problems, and fatigue in these patients as a top health priority [4]. As depression is associated with significant distress and disability, poor quality of life, increased physical symptoms such as pain and nausea, poor adherence to treatment, increased risk of suicide, poorer prognosis, and higher mortality, assessment, diagnosis, and timely treatment of depression would be preventive for many of these consequences [17-19]. It is crucial to assess the psychological distress of cancer patients to identify those needing support and additional evaluation, ultimately leading to appropriate healthcare intervention. This emphasizes the growing recognition of depression as a significant issue among cancer patients. The majority of research on depression in this population has originated from developed nations, with limited studies examining populations from low- and middle-income countries.
We planned to conduct a study in 2022, at the end of the COVID-19 pandemic, to examine the prevalence of depression among patients in the oncology department of Shahid Beheshti Hospital.
Instrument and Methods
In the present cross-sectional study, the research population included all patients admitted to the oncology department of Shahid Beheshti Hospital and Imam Khomeini Clinic, selected by the convenience sampling method in 2022. Among the advantages of sampling this way are easy access to participants, reduced research costs, and quick data collection. Still, because the sample was not chosen randomly, the sample will never be fully representative of the population being studied. Considering 5% alpha, "d" equal to 0.05, 80% power of the test, and 10% of biased questionnaires, the sample size was estimated to be 299 subjects using the Cochran formula. The inclusion criteria were selected based on previous similar studies. Patients who had the physical and mental capacity to respond to questions, a minimum of 6 months since their disease had been diagnosed, were aware of their diagnosis, absence of any adverse events history during the month to the time of the study, and lacked specific chronic physical or mental illnesses were the inclusion criteria. Otherwise, the obtained results may be related to recent events or physical and mental illness.
Afterward, the necessary permits were obtained to collect data from all participating patients who met the study's inclusion criteria. To begin, the researcher explained the objectives, study procedure, and confidentiality of the information to the patients. Afterward, the patients were asked to sign informed consent. Following that, the questionnaires were given to the patients for completion. On average, it took patients 15 minutes to complete the questionnaire. To ensure the patients' convenience, a specific time for questionnaire completion would not interfere with treatment or rest time. During the completion of the questionnaire, the researcher was available in the research setting to address any queries from the participants. Once the questionnaire was finished, the researcher collected them and expressed gratitude to the participants. The data for this study were gathered using two specific tools. The sampling process lasted nine months, from November 2021 to July 2022.
The demographic information questionnaire included factors such as age, gender, marital status, education level, underlying diseases, length of disease, length of chemotherapy, family size, and age at the onset of cancer. Ten faculty members of Hamadan University of Medical Sciences confirmed the validity of this questionnaire's face and content.
We utilized the BDI-II-Persian, a translated version of the Beck depression questionnaire, to assess depression in cancer patients. Numerous research studies have utilized the BDI-II-Persian questionnaire as a tool to evaluate the degree of depression among individuals [20-22]. The Beck depression scale comprises 21 questions that individuals must respond to using a four-point scale ranging from zero to three. The questionnaire covers various aspects such as sadness, pessimism, past failures, loss of pleasure, guilty feelings, punishment feelings, self-dislike, self-criticalness, crying, agitation, loss of interest, indecisiveness, worthlessness, loss of energy, changes in sleeping patterns, irritability, changes in appetite, difficulty concentrating, tiredness or fatigue, and loss of interest in sex. The test score ranges from zero to 63, with zero being the minimum and 63 being the maximum. The individual's overall score is determined by summing up the scores for each subject. The following scores can indicate the general level of depression: 0 to 13: No or minimal; 14 to 19: Mild; 20 to 28: Moderate; And 29 to 63: Severe depression. The BDI-II-Persian had high internal consistency (Cronbach's alpha=0.87) and acceptable test-retest reliability (r=0.74) [23].
Neglecting the adequate handling of the missing data can lead to biased estimates of parameters such as means or regression coefficients, culminating in inaccuracies in standard errors, confidence intervals, and the outcomes of significance tests. Multiple Imputation (MI) has emerged as a favored method for effectively addressing this issue. MI provides plausible estimations of missing values by harnessing the distribution of observed data. Multiple Imputation by Chained Equations (MICE) is a practical technique that employs diverse imputation models to manage missing data across variable types, ensuring a holistic approach to data imputation [24].
In the present study, initially, the "MICE" package of R software (version 4.1.1) was utilized to estimate the missing values (ranging from 0.3 to 32%) employing the MICE procedure. Then, descriptive statistics were performed to summarize and present the main characteristics of the dataset, one-way analysis of variance (ANOVA) was chosen to compare the mean of outcome variable between multiple groups, the Pearson correlation test to explore linear relationships between quantitative variables and the outcome variable, and the multiple linear regression model to examine the impact of the explanatory variables on the outcome variable. All these statistical analyses were performed using SPSS 25 software.
Findings
The mean age of the patients was 49.34±16.58 years, with the disease typically starting at a mean age of 47.56±16.45. The average duration of the disease was 21.29±16.92 months, and the average length of chemotherapy was 6.53±6.22 months. Depression was significantly associated with education (p<0.001) and marital status (p<0.001; Table 1).
Table 1. Frequency (numbers in parentheses are percentages) of the demographic characteristics of the participants (n=291) and comparing the mean of depression according to the demographic characteristics (one-way analysis of variance)
The Mean depression score was 23.84±9.24. Based on the cutoff points of 13 (mild), 19 (moderate), and 28 (severe) for a total score of depression, 48 patients (16.49%) suffered from mild depression (95%CI: 12.22-20.75), 114 patienAts (39.17%) suffered from moderate depression (95%CI: 33.56-44.77), and 89 (30.89%) suffered from severe depression (95%CI: 25.29-35.88).
The Pearson correlation coefficient also showed significant positive linear correlations between depression and age (r=0.21; p<0.001), age at onset of disease (r=0.20; p=0.001), length of disease (r=0.24; p<0.001) and length of chemotherapy (r=0.14; p=0.016).
According to the multiple linear regression model, education, marital status, and length of disease were correlated with depression significantly. A diploma and an academic degree were associated with a decrease of 3.88 (p=0.031) and a decrease of 4.32 (p=0.033) in the depression score, respectively. The marital status of the "divorced/dead spouse" was associated with an increase of 4.50 in the depression score (p=0.007). An increase of one month in the length of the disease was associated with an increase of 0.14 in the depression score (p=0.001; Table 2).
Table 2. Identifying factors associated with depression score through a multiplSe linear regression model
Discussion
This study aims to investigate the occurrence of depression symptoms among Iranian cancer patients. The findings revealed a relatively high prevalence of depression among these patients, with approximately 39% (95%CI: 33.56%-44.77%) experiencing moderate depression and 30% (95%CI: 25.29%-35.88%) experiencing severe depression.
Aryankhesal et al. reported a depression prevalence of 35% (95%CI: 16%-70%) among Iranian cancer patients [25]. According to a study conducted by Darvishi et al., the prevalence of depression in cancer patients in Iran was reported to be 50.1% (95%CI: 40.6%-59.6%) [26]. The findings of this study were in line with Derakhshanfar's [27] research conducted in Iran on cancer patients. It was discovered that 38.2% of patients experienced moderate depression, while 28% experienced severe or very severe depression. Similar to Derakhshanfar's study, a significant correlation was observed between depression in these patients and factors such as age, education level, marital status, chemotherapy duration, or disease duration [27]. In another study, Adzrago et al. [28] assessed the prevalence of depression in cancer patients before and after the COVID-19 pandemic using the Patient Health Questionnaire. The prevalence of anxiety/depression symptoms among cancer patients was 32.7% before the COVID‐19 pandemic and 31.1% during the pandemic. However, they found that individuals aged 50-64 and over 65 had a lower likelihood of experiencing depression compared to those aged 35-49, which contradicts our study findings. One potential explanation for this discrepancy could be the disparity in geriatric care and support systems between these two cultures. There is coordination between Adzrago's study and ours as Adzrago reported a lower likelihood of depression in individuals with higher education levels, such as a college degree, than those with less than a high school education. This finding could be attributed to depression prevention courses in high schools or universities [28].
In other countries, several studies have been conducted to examine the prevalence of depression in cancer patients. For instance, Bakhiet et al. found that the prevalence of depression was 41.2% [29]. Ayalew et al. reported a higher rate of depression, with a prevalence of 58.8. Moreover, its result identified several independent factors significantly associated with depressive factors, including older age, unemployment, advanced stages of cancer such as stage III and stage IV, comorbid psychotic, and eating problems in the past two weeks [30]. Another study conducted by Naser et al. observed a lower prevalence of depressive symptoms, with 23.4% of all patients experiencing depression [31].
In line with the present study, the findings of a study conducted by Muche Belete et al. in 2021 showed that the prevalence of depression was 33.1% (95% CI=0.2858, 0.3761) [3].
The current study found a significant correlation between depression scores in cancer patients and various factors, including age, age at disease onset, duration of chemotherapy, duration of the disease, marital status, and education level. Specifically, illiterate cancer patients, those with a longer period of illness, and individuals who were widowed or divorced exhibited higher depression scores compared to the other groups. Taghavi et al. showed a significant relationship between a higher depression score and being widowed or divorced, consistent with our study [32]. Furthermore, the study conducted by Heidarirad et al. revealed a significant correlation between the depression score in women diagnosed with breast cancer and various factors, including age, marital status, presence of children, educational attainment, place of residence, type of treatment, number of interventions, disease severity, and history of previous cancer [33]. In justifying the correlation between the depression score and the level of education in this study as well as previous studies, having a higher education can be said to be associated with information sources and studies on cancer and its treatment methods can provide patients with a sense of hope and potentially reduce the likelihood of depression [33].
A cross-sectional study was conducted by Rajabizadeh et al. in Kerman, examining 120 breast cancer patients referred to the chemotherapy centers of this city. The study utilized the Beck questionnaire and found that 40.8% of the patients experienced moderate to severe depression. Additionally, the study identified a significant correlation between the patients' occupational status and level of education. As the level of education increased, the depression score exhibited a consistent decreasing trend, aligning with our own findings. Furthermore, our study found no substantial correlation between gender and depression, aligning with previous research. On the other hand, age, place of residence, marital status, and duration of chemotherapy showed no significant association in this study [34]. This disparity could be attributed to variations in the study populations, such as diverse cancer types, cultural disparities, other sociodemographic factors, and the consideration of depression severity.
One limitation of this study was that it did not consider the variations in cancer types and severity among different patients. As a result, it was not feasible to examine depression specifically in patients with a particular type of cancer due to insufficient sample size. A significant limitation was the high percentage of missing data for the chemotherapy duration, accounting for 32% of the total data. Considering the correlation between marital status and depression scores and its alignment with previous research, it is recommended that social and public institutions offer increased emotional support to widowed or divorced individuals with cancer. Regarding the relationship between depression scores and the duration of chemotherapy and the number of family members with depression scores, more studies should be done.
Conclusion
Most cancerous patients suffer moderate to severe depression. Cancer patients should undergo regular psychological evaluations to address depression when identified.
Acknowledgments: The authors would like to thank the staff of the oncology department of Shahid Beheshti Hospital and Imam Khomeini Clinic and the cancer patients who participated in this study.
Ethical Permission: The current study incorporated all ethical considerations, including adherence to the ethics code approved by the Ethics Committee of Hamadan University of Medical Sciences (IR.UMSHA.REC.1399.1062).
Conflicts of Interests: All authors declare no conflict of interest.
Authors’ Contribution: Rabiei H (First Author), Methodologist/Main Researcher/Statistical Analyst (35%); Rabiei R (Second Author), Methodologist/Main Researcher (10%); Arayeshgari M (Third Author), Statistical Analyst (10%); Ghasemi T (Fourth Author), Assistant Researcher (10%); Sadeghian E (Fifth Author), Discussion Writer (35%)
Funding/Support: The Vice‐Chancellor of Research and Technology of Hamadan University of Medical Sciences supported this study (NO: 1400011051).
Article Type: Descriptive & Survey |
Subject:
Health Care
Received: 2023/12/12 | Accepted: 2024/04/8 | Published: 2023/05/28
Received: 2023/12/12 | Accepted: 2024/04/8 | Published: 2023/05/28
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-49. [Link] [DOI:10.3322/caac.21660]
2. Farhood B, Geraily G, Alizadeh A. Incidence and mortality of various cancers in Iran and compare to other countries: A review article. Iran J Public Health. 2018;47(3):309-16. [Link]
3. Belete AM, Alemagegn A, Mulu AT, Yazie TS, Bewket B, Asefa A, et al. Prevalence of depression and associated factors among adult cancer patients receiving chemotherapy during the era of COVID-19 in Ethiopia. Hospital-based cross-sectional study. PLoS One. 2022;17(6):e0270293. [Link] [DOI:10.1371/journal.pone.0270293]
4. Bortolato B, Hyphantis TN, Valpione S, Perini G, Maes M, Morris G, et al. Depression in cancer: The many biobehavioral pathways driving tumor progression. Cancer Treat Rev. 2017;52:58-70. [Link] [DOI:10.1016/j.ctrv.2016.11.004]
5. Chang HA, Barreto N, Davtyan A, Beier E, Cangin MA, Salman J, et al. Depression predicts longitudinal declines in social support among women with newly diagnosed breast cancer. Psycho‐oncology. 2019;28(3):635-42. [Link] [DOI:10.1002/pon.5003]
6. Sudarisan SSP, Abraham B, George C. Prevalence, correlates of depression, and its impact on quality of life of cancer patients attending a palliative care setting in South India. Psycho-oncology. 2019;28(6):1308-13. [Link] [DOI:10.1002/pon.5083]
7. Gan GG, Ng DLC, Leong YC, Bee PC, Chin EF, Abdul Halim H. Anxiety and depression in patients with haematological neoplasms in Malaysia. Med J Malaysia. 2019;74(3):191-7. [Link]
8. Polikandrioti M, Evaggelou E, Zerva S, Zerdila M, Koukoularis D, Kyritsi E. Evaluation of depression in patients undergoing chemotherapy. Health Sci J. 2008;2(3):162-72. [Link]
9. Prieto JM, Blanch J, Atala J, Carreras E, Rovira M, Cirera E, et al. Psychiatric morbidity and impact on hospital length of stay among hematologic cancer patients receiving stem-cell transplantation. J Clin Oncol. 2002;20(7):1907-17. [Link] [DOI:10.1200/JCO.2002.07.101]
10. Krebber AMH, Buffart LM, Kleijn G, Riepma IC, De Bree R, Leemans CR, et al. Prevalence of depression in cancer patients: A meta‐analysis of diagnostic interviews and self‐report instruments. Psycho‐oncology. 2014;23(2):121-30. [Link] [DOI:10.1002/pon.3409]
11. Pinquart M, Duberstein PR. Depression and cancer mortality: A meta-analysis. Psychol Med. 2010;40(11):1797-810. [Link] [DOI:10.1017/S0033291709992285]
12. So WKW, Marsh G, Ling WM, Leung FY, Lo JCK, Yeung M, et al. Anxiety, depression and quality of life among Chinese breast cancer patients during adjuvant therapy. Eur J Oncol Nurs. 2010;14(1):17-22. [Link] [DOI:10.1016/j.ejon.2009.07.005]
13. Satin JR, Linden W, Phillips MJ. Depression as a predictor of disease progression and mortality in cancer patients: A meta‐analysis. Cancer. 2009;115(22):5349-61. [Link] [DOI:10.1002/cncr.24561]
14. Ostuzzi G, Matcham F, Dauchy S, Barbui C, Hotopf M. Antidepressants for the treatment of depression in people with cancer. Cochrane Database Syst Rev. 2018;(4):CD011006. [Link] [DOI:10.1002/14651858.CD011006.pub3]
15. Irwin MR. Depression and insomnia in cancer: Prevalence, risk factors, and effects on cancer outcomes. Curr Psychiatry Rep. 2013;15(11):404. [Link] [DOI:10.1007/s11920-013-0404-1]
16. Sotelo JL, Musselman D, Nemeroff C. The biology of depression in cancer and the relationship between depression and cancer progression. Int Rev Psychiatry. 2014;26(1):16-30. [Link] [DOI:10.3109/09540261.2013.875891]
17. Caruso R, Nanni MG, Riba MB, Sabato S, Grassi L. The burden of psychosocial morbidity related to cancer: Patient and family issues. Int Rev Psychiatry. 2017;29(5):389-402. [Link] [DOI:10.1080/09540261.2017.1288090]
18. Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, et al. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: A systematic review and meta-analysis of 282,203 patients. Mol Psychiatry. 2020;25(12):3186-97. [Link] [DOI:10.1038/s41380-020-00865-6]
19. Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25(7):1487-99. [Link] [DOI:10.1038/s41380-019-0595-x]
20. Farpour HR, Hoveidaei AH, Habibi L, Moosavi M, Farpour S. The impact of social media use on depression in multiple sclerosis patients. Acta Neurol Belg. 2020;120(6):1405-9. [Link] [DOI:10.1007/s13760-020-01407-1]
21. Mohsenpour MA, Mohammadi F, Razmjooei N, Eftekhari MH, Hejazi N. Milk kefir drink may not reduce depression in patients with non-alcoholic fatty liver disease: Secondary outcome analysis of a randomized, single-blinded, controlled clinical trial. BMC Nutr. 2023;9:80. [Link] [DOI:10.1186/s40795-023-00732-x]
22. Omidian M, Mahmoudi M, Abshirini M, Eshraghian MR, Javanbakht MH, Zarei M, et al. Effects of vitamin D supplementation on depressive symptoms in type 2 diabetes mellitus patients: Randomized placebo-controlled double-blind clinical trial. Diabetes Metab Syndr. 2019;13(4):2375-80. [Link] [DOI:10.1016/j.dsx.2019.06.011]
23. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21(4):185-92. [Link] [DOI:10.1002/da.20070]
24. White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377-99. [Link] [DOI:10.1002/sim.4067]
25. Aryankhesal A, Ghashghaee A, Sardari E, Mahmoudi S, Alihosseini S, Dehnad A, et al. Prevalence of depression in patients with cancer in Iran: A systematic review and meta-analysis. BMJ Support Palliat Care. 2022;12(e4):e518-25. [Link] [DOI:10.1136/bmjspcare-2018-001724]
26. Darvishi N, Ghasemi H, Rahbaralam Z, Shahrjerdi P, Akbari H, Mohammadi M. The prevalence of depression and anxiety in patients with cancer in Iran: A systematic review and meta-analysis. Support Care Cancer. 2022;30(12):10273-84. [Link] [DOI:10.1007/s00520-022-07371-1]
27. Derakhshanfar A, Niayesh A, Abbasi M, Ghalaeeha A, Shojaee M. Frequency of depression in breast cancer patients: A study in Farshchianand Besat Hospitals of Hamedan during 2007-8. Iran J Surg. 2013;21(2):68-74. [Persian] [Link]
28. Adzrago D, Sulley S, Tagoe I, Ormiston CK, Odame EA, Mamudu L, et al. Assessment of anxiety/depression among cancer patients before and during the COVID-19 pandemic. Psycho-oncology. 2022;31(10):1681-91. [Link] [DOI:10.1002/pon.6026]
29. Bakhiet TE, Ali SM, Bakhiet AM. Prevalence of depression and anxiety among adult patients undergoing chemotherapy in Khartoum, Sudan: A cross-sectional study. J Affect Disord Rep. 2021;6:100218. [Link] [DOI:10.1016/j.jadr.2021.100218]
30. Ayalew M, Deribe B, Duko B, Geleta D, Bogale N, Gemechu L, et al. Prevalence of depression and anxiety symptoms and their determinant factors among patients with cancer in southern Ethiopia: A cross-sectional study. BMJ Open. 2022;12(1):e051317. [Link] [DOI:10.1136/bmjopen-2021-051317]
31. Naser AY, Hameed AN, Mustafa N, Alwafi H, Dahmash EZ, Alyami HS, et al. Depression and anxiety in patients with cancer: A cross-sectional study. Front Psychol. 2021;12:585534. [Link] [DOI:10.3389/fpsyg.2021.585534]
32. Taghavi M, Kalafi E, Talei AR, Dehbozorgi G, Taghavi SM. Investigating the relation of depression and religious coping and social support in women with breast cancer. J Isfahan Med Sch. 2011;28(115):901-8. [Persian] [Link]
33. Heidarirad F, Yarahmadi M, Heidarirad H, Shafiei M. Evaluation of prevalence of depression and its related factors among women with breast cancer referred to the radiotherapy center of Tawhid Hospital of Sanandaj, Iran in 2017. Sci J Nurs Midwifery Paramed Fac. 2018;4(2):39-49. [Persian] [Link]
34. Rajabizadeh G, Mansoori SM, Shakibi MR, Ramezani MR. Determination of factors related to depression in cancer patients of the oncology ward in Kerman. J Kerman Univ Med Sci. 2005;12(4):142-7. [Persian] [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







