Volume 11, Issue 4 (2023)
Health Educ Health Promot 2023, 11(4): 681-686 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rusli Bintang M, Bachtiar A, Candi C. Designing a Tuberculosis E-Screening Tool for Diabetes Mellitus Patients. Health Educ Health Promot 2023; 11 (4) :681-686
URL: http://hehp.modares.ac.ir/article-5-72600-en.html
URL: http://hehp.modares.ac.ir/article-5-72600-en.html
1- Faculty of Public Health, University of Indonesia, Depok, Indonesia
Keywords: Tuberculosis [Mesh], Disease Notification [MeSH], Mass Screening [MeSH], Diabetes Mellitus [MeSH]
Full-Text [PDF 1115 kb]
(2665 Downloads)
| Abstract (HTML) (1220 Views)
Introduction
Full-Text: (250 Views)
Introduction
Tuberculosis (TB) is the leading cause of death worldwide. In 2016, there were 10.4 million cases of TB, equivalent to 120 cases per 100,000 world population, with the majority of cases found in Southeast Asia (45%) and Africa (25%) [1]. Active case finding is intended, especially in groups that have TB risk factors, namely people with HIV/AIDS (ODHA), malnutrition, and diabetes mellitus (DM). Currently, DM is increasing in populations at high risk for contracting TB. DM increases the risk of developing pulmonary TB with a relative risk of 3.00 [2]. This is caused by patients with DM experiencing a decrease in body immunity; thus, the risk of infection in the lung cavities becomes higher, especially in men with excess weight and the elderly. The global prevalence of DM is estimated to increase in every region by 2035. Globally, its prevalence in 2035 will increase by 21% compared to the 2013 estimate, corresponding to the overall prevalence of DM in adults [3].
Active case finding among residents with TB risk factors and enhancing the quality of record-keeping and reporting in all healthcare facilities are crucial measures to improve TB case reporting across all healthcare settings. Nevertheless, the involvement of private healthcare facilities in identifying and treating TB cases in Indonesia remains significantly limited. According to the National TB Report Database (SITB), out of the 428,867 confirmed TB cases in Indonesia, private hospitals accounted for only 20% of case identifications. In comparison, private clinics contributed a mere 0.6% to the overall case identifications [4].
The main challenge encountered in establishing partnerships with the private sector for TB control management is the fragmentation within the private sector. This fragmentation makes it difficult to achieve unified commitment within the sector. Furthermore, expanding the TB Public Private Mix (PPM) program necessitates sufficient and sustainable funding. Currently, public funds are unevenly distributed and are insufficient to maintain collaboration with the private sector [5].
The Tuberculosis Information System (SITB), the primary software for recording and reporting TB cases created by the Ministry of Health in Indonesia, is intended for use across various healthcare facilities, from primary to secondary levels (such as Puskesmas, hospitals, private general practitioners (GPs), clinics, laboratories, and pharmacies). However, access to SITB remains limited, as it is primarily available in larger health facilities with more sophisticated and well-integrated information systems. The recording and reporting of TB cases through SITB face challenges due to a shortage of human resources, insufficient funding, the lack of integrated information systems, and issues with internal network functionality [6].
To address the complexities of healthcare for TB and DM patients, developing a TB e-screening tool is crucial. We developed an efficient information system integrating TB e-screening into the existing diabetes screening process.
Instrument and Methods
This descriptive research with four phases (Figure 1) was performed in 2022. This paper emphasized the final phase, which was a trial of the TB e-screening tool prototype for DM patients.
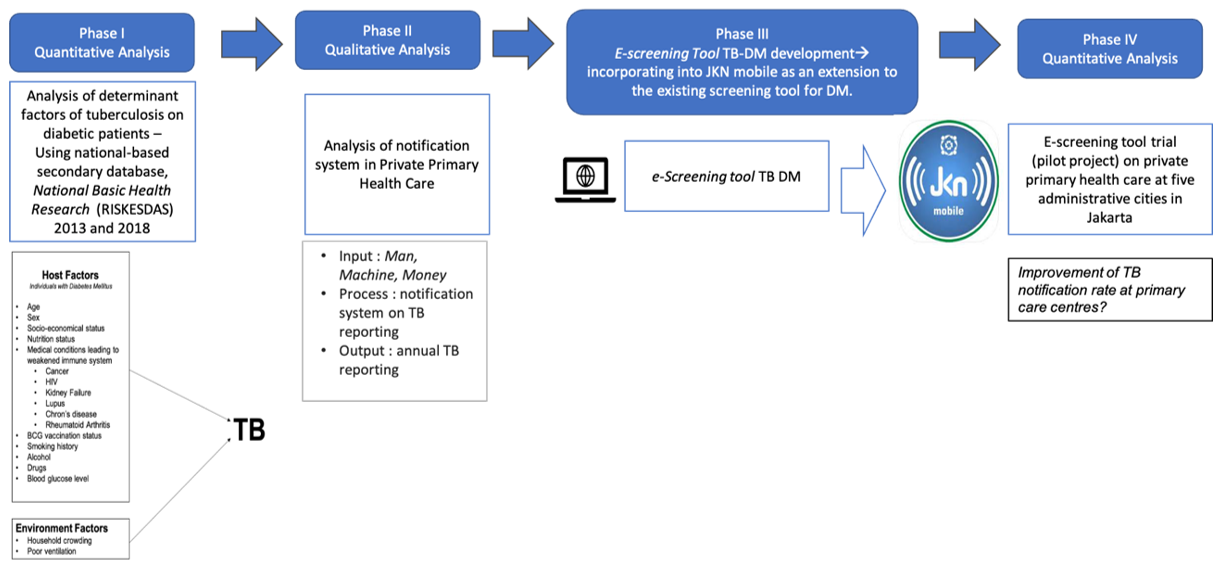
Figure 1. Conceptual framework on developing an e-screening tool for tuberculosis on diabetic patients to increase tuberculosis notification rate in private primary care centers
The pilot test of this tool was conducted at two selected private primary care centers in DKI Jakarta, chosen for their population characteristics, which were deemed representative of the population characteristics of DKI Jakarta residents.
Sample Calculation
The sample size was calculated using the following equation:

n=sample size
z1-α/2=The degree of confidence (confidence interval in this study is 95%; thus, α=5% with a value of 1,96.
P1= TB incidence among DM respondents was 0,42 [7]
P2= TB incidence among non-DM respondents was 0,56 [7]
P= The average P1 and P2 
DEFF=Design effect with a value of 2.
According to the formula, the minimum number of participants required for phase 4 of the research was 266 respondents. Inclusion criteria were all visiting patients aged 18 years and above.
The screening procedure was carried out as shown in Figure 2. Respondents were instructed to complete e-screening through a link. The process finished once the patients were neither diabetic nor indicated with TB; if the results showed that the respondent was diabetic and indicated for TB, they would be directed to register for TB testing at the clinic.
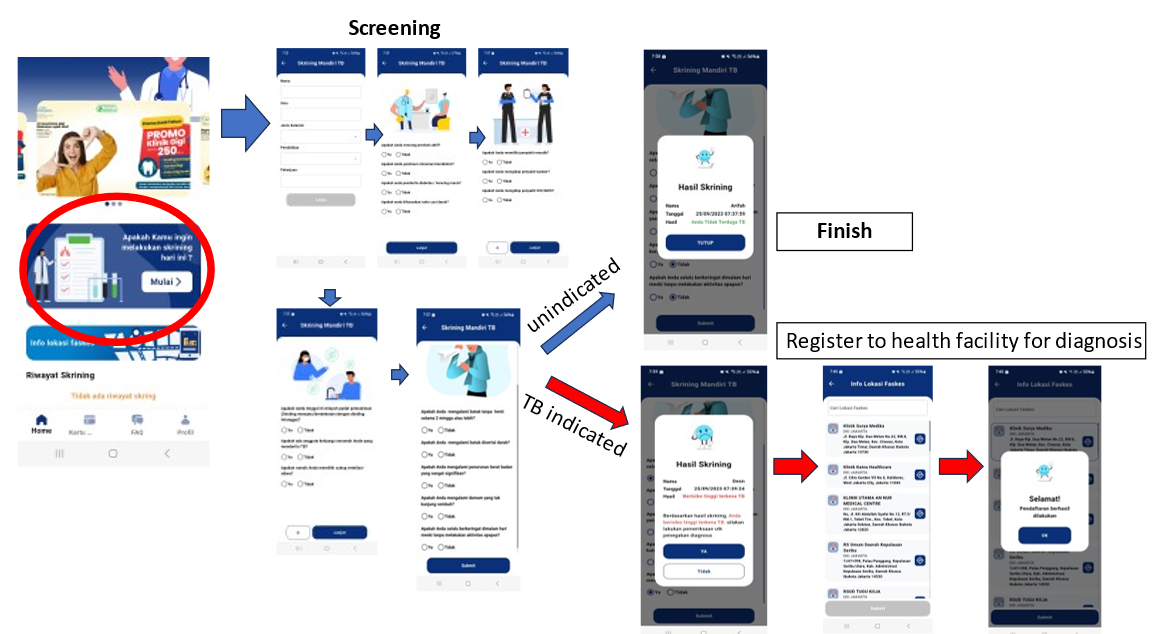
Figure 2. The flow of tuberculosis e-screening.
Once the TB diagnosis was negative, the process was complete; if the diagnosis result were positive, the center would report the patient as TB-positive in the system.
Findings
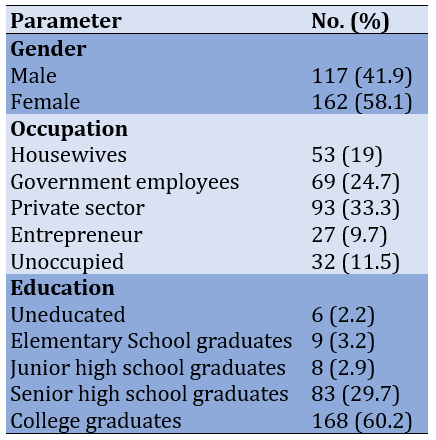
The trial lasted four weeks, with a total of 274 participants. Also, 33 patients (12%) had TB. There were two patients diagnosed with TB (Figure 3) after further tests. Table 1 displays the characteristics of respondents.
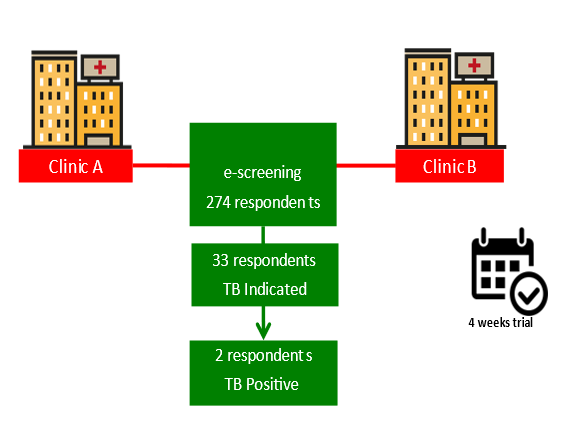
Figure 3. The flow of tuberculosis e-screening tool trial
Table 1. Respondent’s characteristics
The TB-DM e-screening tool included questions about TB risk factors, such as DM and cancer (compiled based on phase 1 result), and symptoms, such as coughing for more than two weeks, coughing up phlegm, coughing up phlegm mixed with blood, chest pain, or shortness of breath.
Thirty-three high-risk patients were identified with TB. Indicated patients in clinic A were asked to produce sputum samples in a sampling bottle provided by the clinic, then sent to the nearest primary health center (Puskesmas) for laboratory testing. Meanwhile, identified patients in clinic B only received a referral letter for sputum sampling and laboratory tests to the nearest Puskesmas. The rapid molecular test results on indicated patients revealed that two people were diagnosed with TB. Within only four weeks, two new cases were found.
Discussion
DM has been recognized as a significant risk factor for pulmonary TB by the World Health Organization (WHO). Previous systematic reviews and meta-analyses have indicated a relatively high global incidence and prevalence of TB cases among patients with diabetes [8]. Previous research has shown that individuals with DM have a 2-4 times higher risk of contracting TB compared to those without diabetes [9]. Diabetes patients are particularly susceptible to pulmonary TB due to weakened immunity, which increases their vulnerability to lung infections [2]. Other studies have also suggested that TB is more likely to occur in diabetic patients due to their compromised immune systems [10].
Cancer is a major health concern and a significant contributor to global mortality and morbidity. Cancer patients often experience decreased immunity due to the depletion of immune cells, malnutrition, and the effects of chemotherapy, which elevate their risk of TB infection [11]. Furthermore, a study conducted in Saudi Arabia revealed a higher prevalence of pulmonary TB among cancer patients undergoing chemotherapy compared to the general population in Saudi Arabia [12].
Early detection is crucial in preventing TB infection in individuals with diabetes. However, early detection of DM-TB remains infrequent, especially in underdeveloped nations [7]. In contrast, TB screening for people with HIV/AIDS (PLWHA) has been mandated in Minister of Health Regulation No. 43 of 2016, which outlines Minimum Service Standards for the Health Sector. The goal of the Health Sector SPM for HIV testing is to identify TB patients. Surprisingly, in Indonesia, there is currently no policy in place for TB-DM screening, despite the fact that individuals with diabetes are three times more likely to contract TB than those with HIV/AIDS. There are no specific protocols for TB screening in cancer patients [13]. This is particularly challenging because pulmonary TB and lung cancer share similar symptoms, making early diagnosis and detection complicated [11].
The e-screening program targets patients with diabetes, cancer, and/or three of the five primary tuberculosis symptoms. The WHO recommends that individuals with diabetes should be screened for TB. Screening methods for suspected TB symptoms include thoracic X-ray, computer-aided detection, and the WHO-recommended rapid molecular diagnostic test. These screening modalities are suitable for use in non-HIV high-risk groups.
According to a study conducted at two private primary care facilities, clinic A and clinic B, the recording and reporting of TB (notification) was low at both clinics. This is supported by the fact that neither Clinic A nor Clinic B has an integrated system for registering TB suspects. Hence, neither Clinic A nor Clinic B has a TB case-finding report. In other words, the SITB was not implemented at either clinic. The results of this study align with previous research conducted by Widada, stating that private health facilities' contribution to the discovery and treatment of TB in Indonesia is still very low [14]. Based on SITB data, among 428,867 confirmed TB cases in Indonesia, private hospitals only contributed 20% of case findings, and private clinics only contributed 0.6% of case findings. Next, one of the factors for low TB notification in private primary care centers was human resources, namely officers who report TB cases. According to research by Wadudah et al., 50% of officers who report TB notifications have not received training or workshops on the Mandatory TB Notification (Wifi) application where the training is facilitated by the Ministry of Health in collaboration with the KNCV TB Foundation (KNCV) [15].
Kurniawati et al. found no data on private general practitioners' contribution to TB case finding [16]. The data had been searched among the TB recording and reporting data at several health centers in Yogyakarta. The reason is due to various factors; for example, private general practitioners and private clinics do not have diagnostic facilities, or there are complications, so they refer to hospitals or health centers. According to Kurniawati et al., the small contribution of private general practitioners to the notification of TB cases, while the large potential number of private practitioners and the pattern of seeking treatment for TB patients that is quite large targeting the private sector makes a large number of TB cases missing. The low acceptability of private general practitioners to this policy may likely contribute to many missing TB cases. Recording and reporting through SITB are not running optimally due to human resources, lack of funding sources for recording and reporting programs in health facilities, and lack of integrated information systems and poor internal networks [17].
Integrating health information systems can be one of the efforts to improve a better service system. Problems that require more effective and efficient utilization of resources, such as limited staff, high costs, and increasing demand for improved service quality, can be overcome by integrating existing health information systems [18]. One of the current information systems in Indonesia is the BPJS Health Management Information System (SIM), which was created to facilitate the flow of health services for the community. Primary care is one of the products of BPJS SIM, a system that contains electronic-based patient information services provided by BPJS Kesehatan. Primary care plays a role in recording all health services performed at primary care centers (FKTP), and the data goes to BPJS Health. Primary care is intended for FKTPs who have obtained a license. Therefore, primary care cannot be used by the general public. For the public to access health services more easily, BPJS Kesehatan built a health information system called Mobile JKN. All people in Indonesia can access this application through their respective devices. Some of the uses of Mobile JKN include registering for health services at the nearest health facility and detecting diseases early through health history screening [19, 20]. In addition to BPJS, the Ministry of Health also has a health information system that is used to monitor, register, and report cases of susceptible TB, drug-resistant TB, laboratories, and logistics in an integrated platform called SITB. However, primary care, mobile JKN, and SITB are still independent and have not become an integrated system.
Recording and reporting cases are crucial components in addressing the TB problem. These processes play significant roles in monitoring the epidemiological trends of TB, tracking treatment progress, and ensuring the continuity of care when patients are referred to other medical facilities. Under-reporting of TB cases is one of the major factors hindering progress toward achieving the WHO End TB Strategy [21]. In Indonesia, all healthcare services are obligated to report both new and re-treated TB cases, along with treatment outcomes, to the local Public Health Office. This mandatory reporting system can be executed manually or through an electronic system called SITB [22]. The SITB system is designed to optimize the TB reporting system, allowing health facilities to contribute to the national TB report without needing physical paperwork [23]. This study revealed that TB cases recording and reporting (notification) at private primary healthcare facilities remain low. The diminished TB notification rate can be attributed to the fact that primary care centers still rely on Puskesmas, as the implementation of SITB demands a sophisticated system and dedicated human resources, which most private primary care centers are ill-prepared to accommodate [6].
Improving TB notification contributions from private primary care centers is essential to enhance the national TB notification rate. Better notification from these centers can be realized by integrating health information systems like E-MR, primary care, Mobile JKN, and SITB. If SITB were implemented in all private primary healthcare centers and integrated into their existing systems, the recording of TB cases could be carried out more systematically, leading to increased TB reporting (notification) from these centers. A recent study in Purwakarta District highlighted a major issue in TB control management: the lack of communication between the public and private health sectors [24]. The e-screening tool prototype aims to bridge this communication gap and improve TB reporting between the two sectors. Indeed, strengthening the public-private mix is crucial for overcoming health system barriers in TB-DM control management [25].
It is worth noting that this study employed a prototype version; therefore, the results may differ when implemented in an integrated version. In the study, users could access the questionnaire directly. In contrast, an integrated version might require users to navigate several steps before reaching the screening questionnaires, potentially affecting the usability feedback component.
Conclusion
TB E-screening tool boosts TB notification in private primary care centers, especially in DM and cancer patients. Integrated and upgrading recording and reporting systems are required to implement this e-screening integrated design countrywide.
Acknowledgments: We would like to express our appreciation to the Agency for Health Policies Development, Ministry of Health, Indonesia, and the Faculty of Public Health University, Indonesia, for their support.
Ethical Permissions: We obtained permission to access the RISKESDAS 2018 database from the Agency for Health Policies Development (BKPK), Ministry of Health, Indonesia. Verbal consent was recorded for in-depth interviews. This research passed the ethical test by the Ethics Committee of the Faculty of Public Health, University of Indonesia (no. Ket- 46/UN2.F10.D11/PPM.00.02/2023).
Conflicts of Interests: The authors have no conflict of interest in this research project.
Authors’ Contribution: Rusli Bintang M (First Author), Introduction Writer/Main Researcher/Discussion Writer (40%); Bachtiar A (Second Author), Methodologist (30%); Candi C (Third Author), Statistical Analyst (30%)
Funding/Support: The research was funded privately by the authors.
Article Type: Original Research |
Subject:
Health Promotion Approaches
Received: 2023/10/24 | Accepted: 2023/12/6 | Published: 2023/12/22
Received: 2023/10/24 | Accepted: 2023/12/6 | Published: 2023/12/22
References
1. World Health Organization. Tuberculosis (TB) [Internet]. Geneva: WHO. 2023- [cited 2023 Oct 1]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/tuberculosis [Link]
2. Narasimhan P, Wood J, MacIntyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:828939. [Link] [DOI:10.1155/2013/828939]
3. Odone A, Houben RM, White RG, Lönnroth K. The effect of diabetes and undernutrition trends on reaching 2035 global tuberculosis targets. Lancet Diabetes Endocrinol. 2014;2(9):754-64. [Link] [DOI:10.1016/S2213-8587(14)70164-0]
4. Nazriati E, Zulharman Z, Chandra F, Putri UA. Public-Private Mix Implementation and Achievements of Tuberculosis Control Program at Puskesmas in Pekanbaru. Mutiara Medika Journal of Medicine and Health. 21(2):86-94. [Indonesian] [Link] [DOI:10.18196/mmjkk.v21i2.11731]
5. Anggraini RD, Rahayu EP, Orianti WO. Evaluation of tuberculosis recording and reporting case system at syarif hidayatullah hospital in 2020. Berita Kedokteran Masyarakat.;34(11). [Indonesian] [Link]
6. Ratnasari Y, Sjaaf AC. Evaluation of tuberculosis recording and reporting case system at syarif hidayatullah hospital in 2020. J Admin Rumah Sakit Indonesia. 2023;9(1):21-4. [Link] [DOI:10.7454/arsi.v9i1.4742]
7. Tenaye L, Mengiste B, Baraki N, Mulu E. Diabetes mellitus among adult tuberculosis patients attending tuberculosis clinics in Eastern Ethiopia. Biomed Res Int. 2019;2019. [Link] [DOI:10.1155/2019/7640836]
8. Wu Q, Liu Y, Ma YB, Liu K, Chen SH. Incidence and prevalence of pulmonary tuberculosis among patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Ann Med. 2022;54(1):1657-66. [Link] [DOI:10.1080/07853890.2022.2085318]
9. Al-Rifai RH, Pearson F, Critchley JA, Abu-Raddad LJ. Association between diabetes mellitus and active tuberculosis: A systematic review and meta-analysis. PloS One. 2017;12(11):e0187967. [Link] [DOI:10.1371/journal.pone.0187967]
10. Hidayah H, Amal S, Rosmalinda AN. Incidence of Pulmonary TB in Type 2 DM Patients at Karya Husada Cikampek Hospital. Pharma Xplore: J Sains dan Ilmu Farmasi. 2021;6(1):23-31. [Indonesian] [Link] [DOI:10.36805/farmasi.v6i1.1446]
11. Aldabbagh MA, Abughasham A, Alansari G, Bougis S, Melibari E, Alhatmi N, et al. The prevalence of mycobacterium tuberculosis infection among cancer patients receiving chemotherapy in a tertiary care center. Cureus. 2022;14(11):e32068. [Link] [DOI:10.7759/cureus.32068]
12. Nugroho NP, Wati FF. Coexistence of Lung Cancer and Tuberculosis. Syifa'Med J Kedokt dan Kesehat. 2020;11(1):49. [Indonesian] [Link] [DOI:10.32502/sm.v11i1.2583]
13. Bae S, Kim YJ, Kim MJ, Kim JH, Yun SC, Jung J, et al. Risk of tuberculosis in patients with cancer treated with immune checkpoint inhibitors: A nationwide observational study. J Immunother Cancer. 2021;9(9);e002960. [Link] [DOI:10.1136/jitc-2021-002960]
14. Widada S. Achievements of the TB and Public Private Mix Control Program in Indonesia. Jakarta: Directorate General of P2P Ministry of Health of the Republic of Indonesia; 2022. [Indonesian] [Link]
15. Wadudah F, Prasetyowati I, Bumi C. Implementation of Mandatory TB Notification (WiFi) at the Jember District Health Service. Pustaka Kesehatan. 2020;8(2):131-8. [Indonesian] [Link] [DOI:10.19184/pk.v8i2.20360]
16. Kurniawati A, Padmawati RS, Mahendradhata Y. Acceptability of mandatory tuberculosis notification among private practitioners in Yogyakarta, Indonesia. BMC Res Notes. 2019;12:543. [Link] [DOI:10.1186/s13104-019-4581-9]
17. Ratnasari Y, Sjaaf AC, Djunawan A. Evaluation of the Tuberculosis Case Recording and Reporting System at Syarif Hidayatullah Hospital. J Manajemen Kesehatan Yayasan RS Dr. Soetomo. 2021;7(1):115-24. [Indonesian] [Link] [DOI:10.29241/jmk.v7i1.608]
18. Tandama'dika R, Qashlim AA, Khairat U. Integration of Hospital Information Systems for Health Facilities and Referral Services. Proceeding KONIK (Konferensi Nasional Ilmu Komputer). 2021;5:406-12. [Indonesian] [Link]
19. Suhadi S, Jumakil J, Irma I. Aplikasi Mobile JKN untuk Memudahkan Akses Pelayanan BPJS. J Health Res Forikes Voice. 2022;13:262-7. [Link]
20. Wardiah R, Izhar MD, Lanita U. Study of the effectiveness of the JKN mobile application on Jambi City National Health Insurance (JKN) participants. J Endurance. 2022;7(3):607-14. [Indonesian] [Link] [DOI:10.22216/jen.v7i3.1664]
21. Zhou D, Pender M, Jiang W, Mao W, Tang S. Under-reporting of TB cases and associated factors: A case study in China. BMC Public Health. 2019;19:1664. [Link] [DOI:10.1186/s12889-019-8009-1]
22. Iskandar D, Suwantika AA, Pradipta IS, Postma MJ, van Boven JF. Clinical and economic burden of drug-susceptible tuberculosis in Indonesia: National trends 2017-19. Lancet Glob Health. 2023;11(1):e117-25. [Link] [DOI:10.1016/S2214-109X(22)00455-7]
23. Nuryani S, Nursilmi DL, Sonia D. Analysis of the system for recording and reporting tuberculosis cases at the X general hospital in Bandung City. Cerdika: J Ilmiah Indonesia. 2021;1(11):1601-7. [Indonesian] [Link] [DOI:10.36418/cerdika.v1i11.232]
24. Paskaria C, Sunjaya DK, Parwati I, Bestari MB. Digital health to strengthen district-based public-private mix tuberculosis control in Purwakarta district, Indonesia: A qualitative research. Int J Environ Res Public Health. 2022;19(19):12097. [Link] [DOI:10.3390/ijerph191912097]
25. Arini M, Sugiyo D, Permana I. Challenges, opportunities, and potential roles of the private primary care providers in tuberculosis and diabetes mellitus collaborative care and control: A qualitative study. BMC Health Serv Res. 2022;22(1):215. [Link] [DOI:10.1186/s12913-022-07612-3]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







