Volume 12, Issue 1 (2024)
Health Educ Health Promot 2024, 12(1): 159-164 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khodadadi B, Sharafi M, Modarres Moghaddam M, Fazli B. Assessment of Staff Knowledge and Practices for Nosocomial Infection Control and Prevention. Health Educ Health Promot 2024; 12 (1) :159-164
URL: http://hehp.modares.ac.ir/article-5-72582-en.html
URL: http://hehp.modares.ac.ir/article-5-72582-en.html
1- Department of Nursing, Mashhad Branch, Islamic Azad University, Mashhad, Iran
2- Department of Anesthesiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
2- Department of Anesthesiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Keywords: Infectious Disease Transmission, Patient-to-Professional [Mesh], Health Personnel [MeSH], Hand Hygiene [MeSH], Infection Control [MeSH]
Full-Text [PDF 602 kb]
(3779 Downloads)
| Abstract (HTML) (1318 Views)
Full-Text: (1012 Views)
Introduction
Hospital infections are on the rise and significantly contribute to mortality rates among hospitalized patients. Research indicates that about 25% of hospital-acquired infections occur in intensive care units. Medical staff, particularly nurses and other personnel in direct contact with patients, play a crucial role in preventing and controlling these infections, underscoring the need for their continual education in this area [1, 2]. Additionally, a 24-hour point prevalence study conducted across 1,150 sites in 88 countries found that 54% of patients had suspected or confirmed infections, with 70% receiving at least one antibiotic for prophylactic or therapeutic purposes. The hospital mortality rate for these patients was 30% [3].
It is vital for relevant authorities to implement decisive educational initiatives in this field. While invasive medical procedures and equipment have been linked to a decrease in healthcare-associated infections over the past decade, many infections still penetrate intensive care units. This complicates treatment and jeopardizes patient outcomes, especially in the context of emerging infections. The COVID-19 pandemic is a prime example, highlighting the challenges of adapting prevention strategies to new pathogens and balancing the risk of exposure to caregivers with the provision of high-quality care [4].
Questionnaires are invaluable tools for assessing individuals' knowledge, attitudes, and behaviors. They are particularly significant due to their simplicity, cost-effectiveness, and flexibility, offering a time-efficient method for data collection.
Several studies in Iran have explored the knowledge, beliefs, and practices of medical staff regarding infection control, showing that these professionals generally demonstrate satisfactory knowledge and performance [5, 6]. However, other studies present conflicting results, particularly highlighting inadequate hand hygiene among nurses [7, 8]. Hand hygiene is critical in reducing hospital infections by 50%. Healthcare workers' hands are the primary vectors for transmitting microorganisms between patients, different areas of the same patient's body, and from contaminated environments to patients. Therefore, maintaining rigorous hand hygiene is crucial [9].
This study aimed to assess the knowledge, attitudes, and practices of nurses and patient-related staff within the special care units of Ghaem Hospital, Mashhad, focusing on the control and prevention of hospital-acquired infections.
Instrument and Methods
This descriptive-analytical study was conducted from 2022 to 2023 in the special care units of Ghaem Hospital, Mashhad. Using a census and convenience sampling method, all nurses, doctors, and paramedics working in the department were involved in the study. According to the study by Allah-Bakhshian et al. [11], with an alpha of 0.05, a beta of 0.2, and an error margin of 0.1 p, a population proportion (p) of 0.8 was calculated using the formula for estimating a ratio, resulting in a required sample size of 96 individuals.
Data collection tools included a researcher-designed questionnaire with 44 questions for gathering demographic information and separate questionnaires for assessing the knowledge, attitudes, and practices of nurses and patient-related staff regarding infection control methods. After preparing the checklist, the information was recorded in the respective file.
The validity of the questionnaire of “Measuring the knowledge attitude and performance of nurses and medical staff of ICU about infection control methods” was assessed through content validity, while reliability was determined by retesting for the knowledge and attitude sections and by bisecting for the performance section [10]. The content validity index (CVI) and content validity coefficient (CVC) for the entire questionnaire ranged from 0.8 to 1. The face validity of the questions was assessed at 3.35. Richardson’s coefficient for the knowledge section was 0.81, while Cronbach’s alpha coefficients for the attitude and performance sections were 0.71 and 0.83, respectively. The correlation coefficients were 0.9 for awareness, 0.85 for attitude, and 0.9 for performance, indicating favorable conditions. The responses on the Likert scale ranged from “I agree” to “I have no opinion” and “I disagree.”
Five questionnaires were developed based on standards from nursing reference books to assess general knowledge, precautions for intravenous injections and serum therapy, wound dressing precautions, procedures for inserting an angiocath, and suction techniques. Responses were categorized as “always,” “often,” “sometimes,” “rarely,” and “never.”
The study included nurses and patient care personnel in the intensive care unit, excluding those with less than a year’s experience in the unit and those working in other departments. Confidentiality principles were maintained, including omitting names from the database and publishing results in a generalized format. Eligible participants who were willing to participate were provided with informed consent forms. All questionnaires were administered anonymously, ensuring strict confidentiality of the results.
Upon collection, data were entered into SPSS 26. P-values less than 0.05 were considered statistically significant. Data were described using central and dispersion indices and frequency tables. The independent t-test or its non-parametric equivalent was utilized to compare the means of quantitative variables between two groups, while the Chi-squared test was applied to examine qualitative variables.
Findings
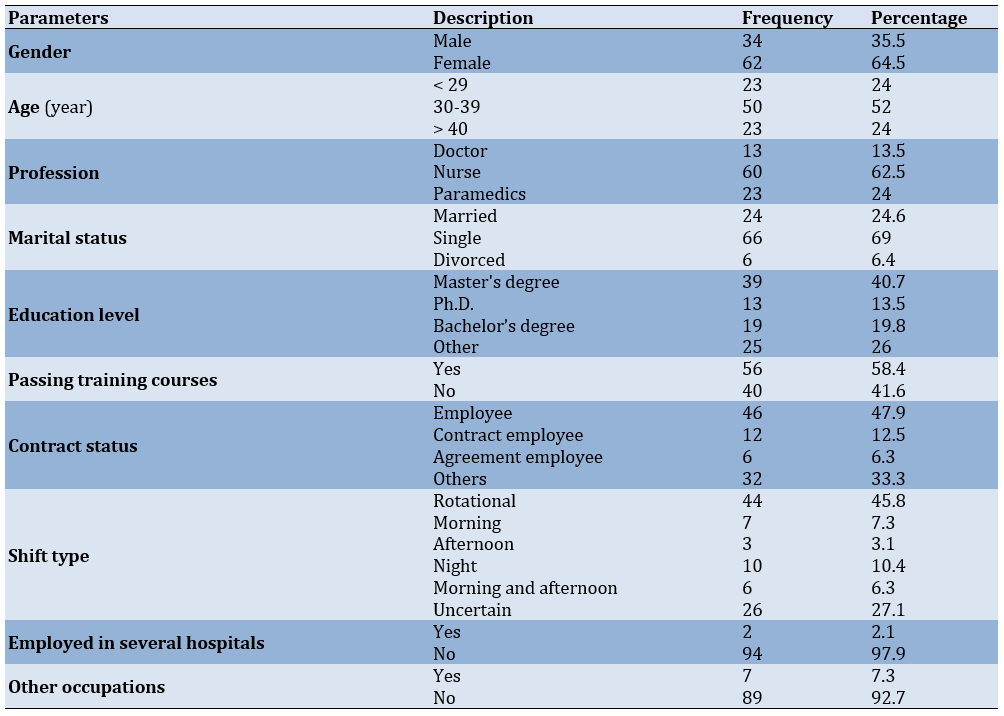
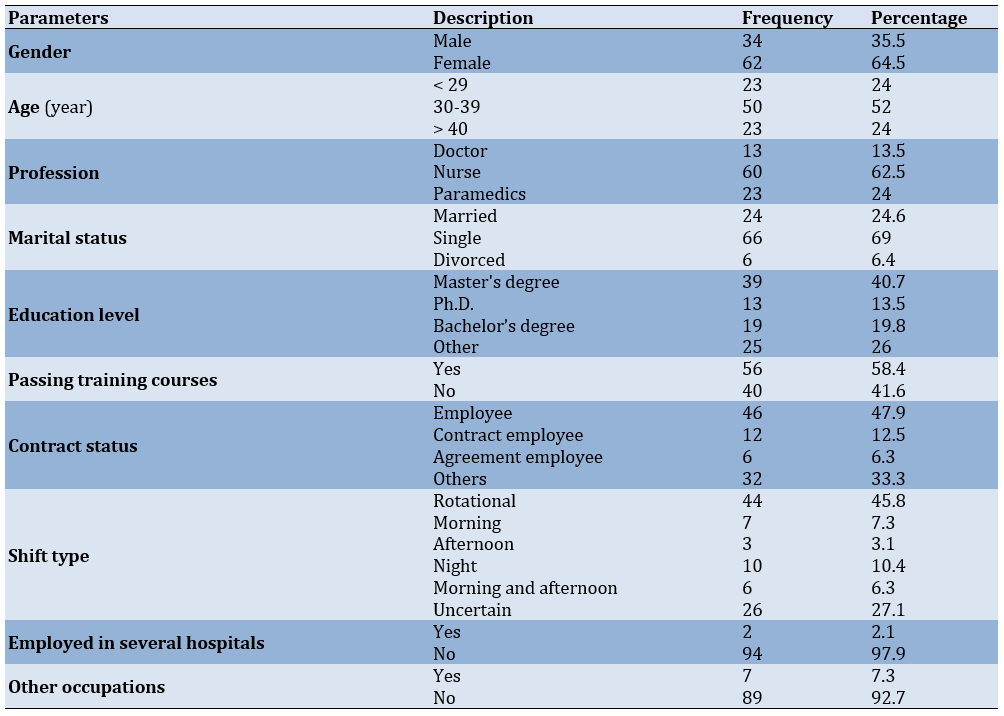
A total of 96 individuals (34 males and 62 females) participated in this study (Table 1).
Table 1. Frequency and percentage of participants' demographic information
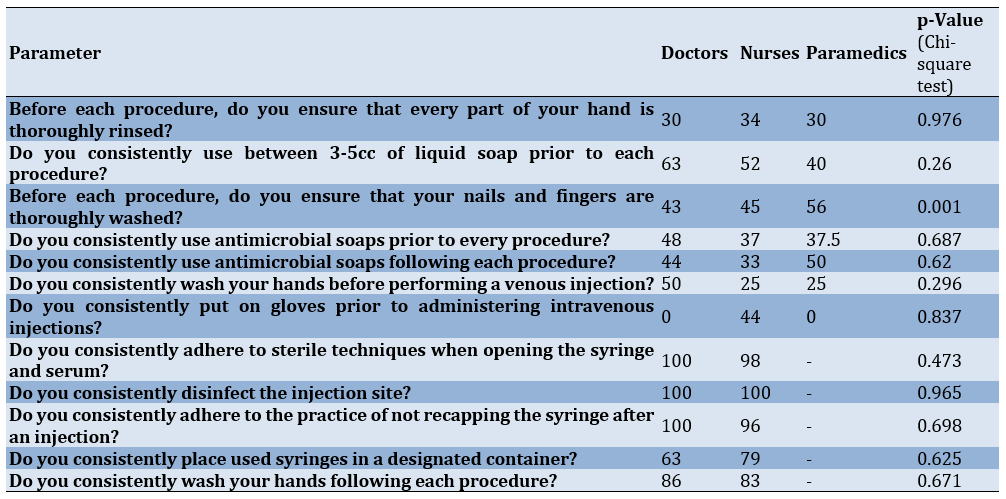
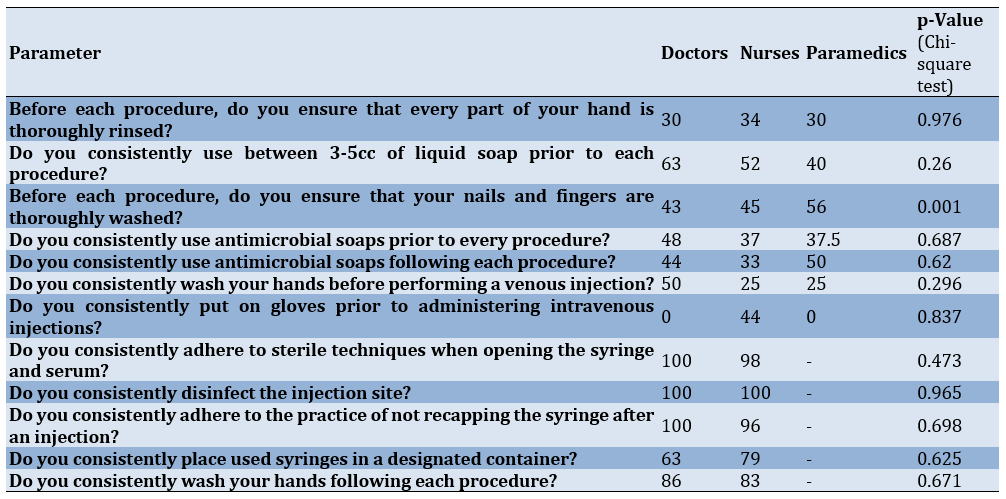
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to health guidelines and profession regarding awareness by Chi-square test showed a statistically significant correlation between thorough hand washing, including fingernails, before procedures (p<0.001). However, no significant relationship was found in other categories (Table 2).
Table 2. Relationship between adherence to health guidelines and occupation regarding awareness
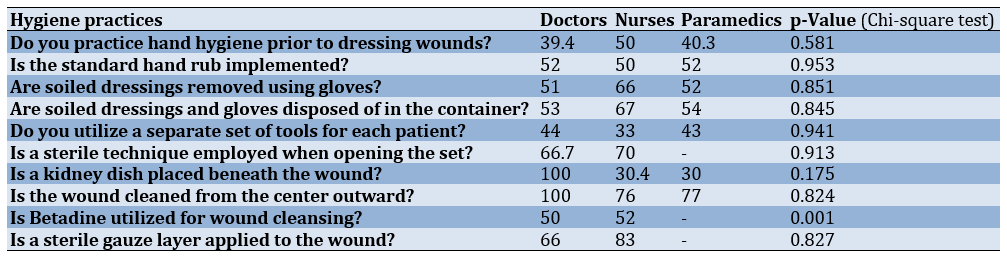
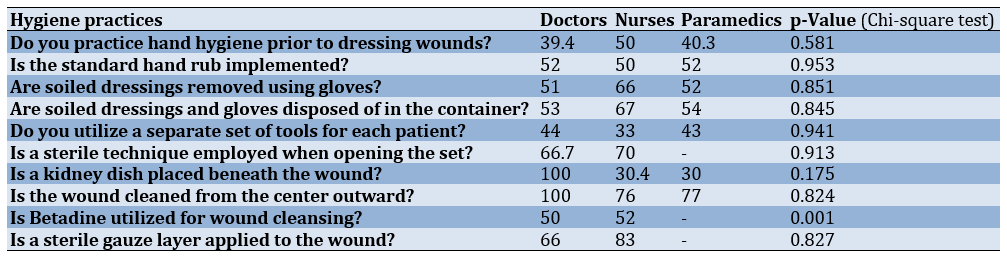
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to health guidelines and professional roles in pre-bandage procedures by Chi-square test showed a significant difference in the use of Betadine for wound cleansing, with 50% of doctors and 52% of nurses using it (p<0.001). No significant differences were found in other aspects (Table 3).
Table 3. Relationship between occupational roles and hygiene practices in pre-bandage procedures
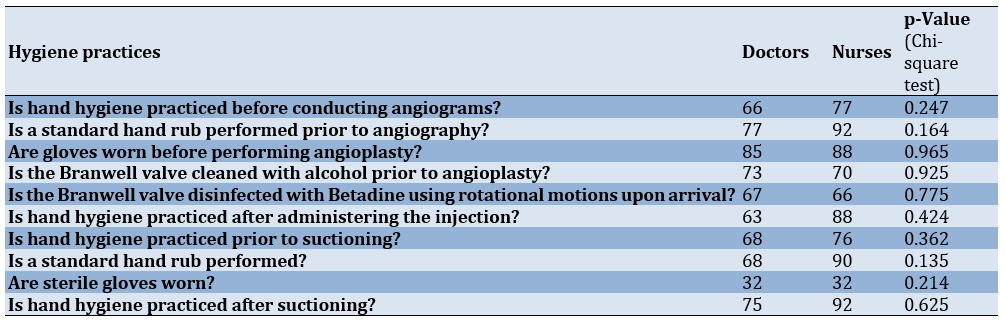
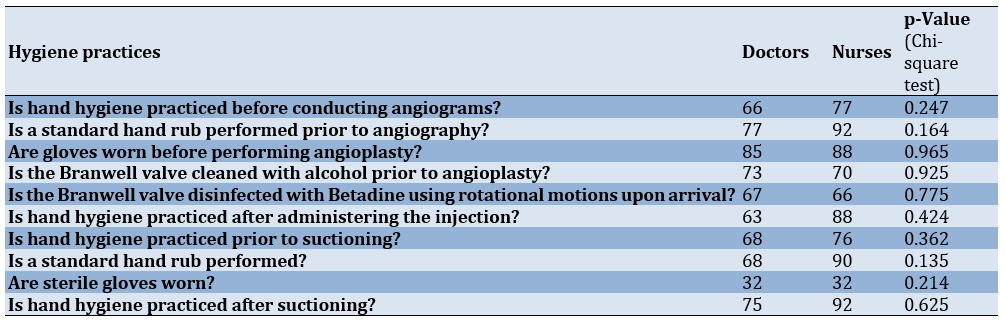
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to hygiene practices during angiocatheter insertion and pre-suction procedures by Chi-square test showed no significant relationship (Table 4).
Table 4. Relationship between hygiene practices and job compliance in angiocatheter placement and pre-suction procedures
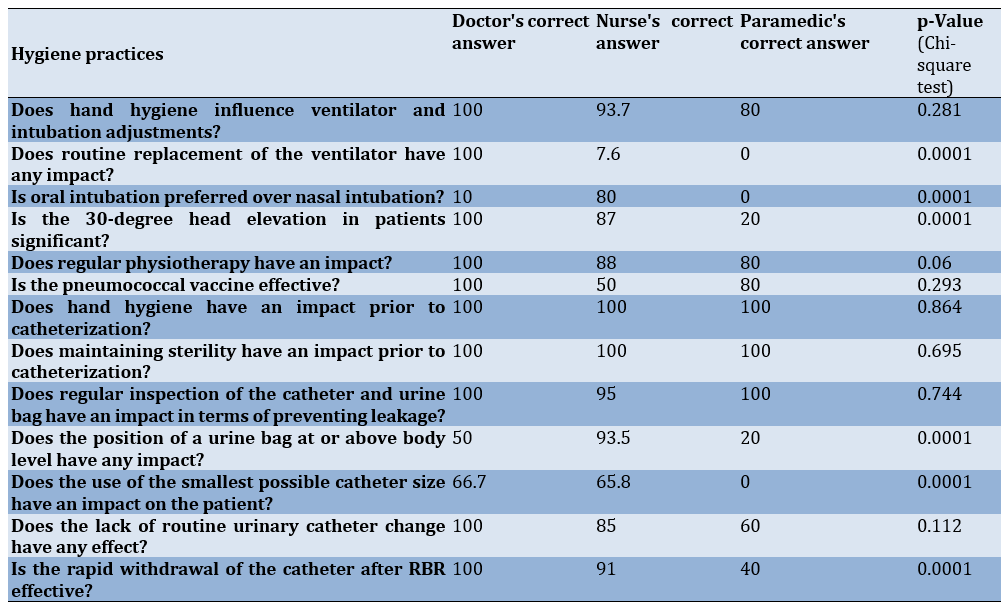
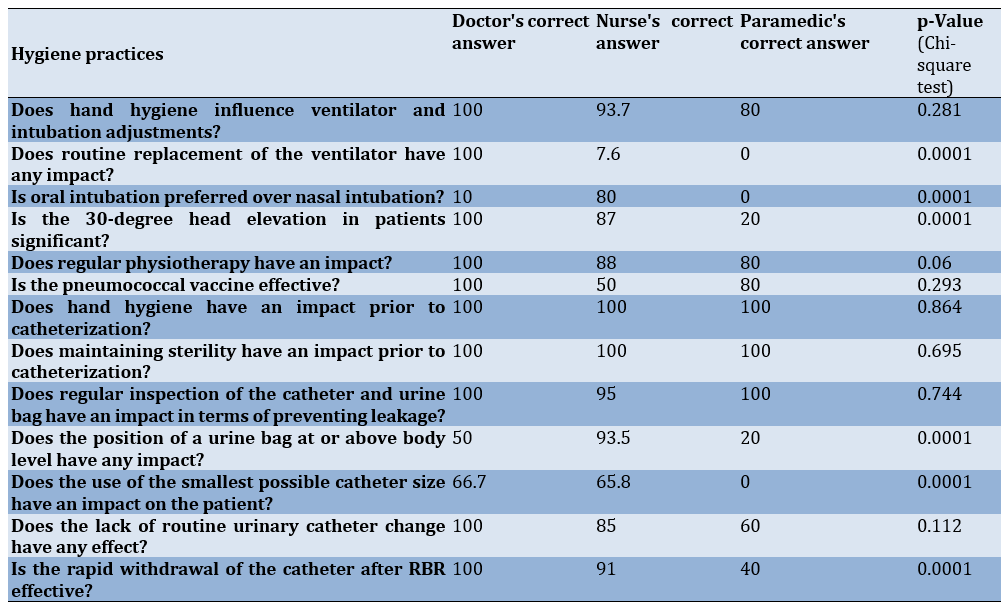
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between health compliance and occupation concerning awareness measures for ventilator-associated pneumonia by Chi-square test showed significant differences, with response rates of 100%, 7.6%, and 0%, respectively (p=0.0001). Preferences for oral over nasal intubation also varied significantly, with 10% of doctors, 80% of nurses, and 0% of paramedics preferring oral intubation, showing a statistically significant difference (p=0.0001). The importance of maintaining a 30-degree head elevation in patients also yielded statistically significant results (p=0.0001). Additionally, significant differences were observed in participant responses regarding not positioning the urine bag at the same level or higher than the body (p<0.0001; Table 5).
A significant difference was noted among doctors, nurses, and paramedics concerning the use of the smallest possible urinary catheter size for patients and avoiding routine urinary catheter changes, which was statistically significant (p<0.0001).
Table 5. Relationship between health compliance and occupation concerning awareness measures for ventilator-associated pneumonia (VAP)
Discussion
This study aimed to assess the knowledge, attitudes, and practices of nurses and patient-related staff within the special care units of Ghaem Hospital, Mashhad, focusing on the control and prevention of hospital-acquired infections.
Oral suction is conducted by medical, nursing, and paramedic teams. Adherence to hygiene practices such as hand washing, hand rubbing, or wearing gloves was maintained by less than 30% across all groups. However, 86% of nurses consistently used the correct suction technique, while only 65% of doctors did the same, indicating a need for additional training for doctors in this procedure.
Doctors and nurses are also tasked with adjusting ventilators. Maintaining hand hygiene is critical in preventing VAP, which can prolong hospital stays and increase the prevalence of antibiotic-resistant pathogens. Encouragingly, about 90% of doctors and nurses acknowledged the importance of hand washing before adjusting the ventilator or performing intubation.
To reduce the risk of VAP, it is advisable to maintain patients’ heads elevated at a 30-degree angle relative to the body. This practice helps minimize the likelihood of aspiration and the subsequent risk of pneumonia. Awareness of this measure was statistically significant, with all doctors and about 80% of nurses knowledgeable about it. However, awareness among paramedics was markedly lower, underscoring the need to educate all paramedic staff on this critical preventative measure.
The routine replacement of ventilator sets is known to increase the risk of pneumonia. All doctors understood this risk, but only approximately 7% of nurses and none of the paramedics were aware, indicating a significant gap in knowledge among these groups.
The role of respiratory physiotherapy for patients on ventilators is vital and must be prescribed by the attending physician. About 90% of doctors recognized the importance of this intervention.
The regular use of chlorhexidine mouthwash for ventilated patients is recommended, with about 80% of both doctors and nurses aware of this guideline.
Addressing the risk of infection during Foley catheterization is crucial. Urinary system infections can be mitigated by adhering to straightforward guidelines, including maintaining hand hygiene. Foley catheterization is performed by nurses, doctors, and occasionally paramedics. All doctors and nurses, and 90% of paramedics, demonstrated awareness of the importance of maintaining hand hygiene and sterility during this procedure. Positioning the catheter lower than the patient to prevent infection from ascending from the sac to the urinary tract is another vital practice. About 50% of doctors and 94% of nurses were aware of this critical positioning, but only 20% of paramedics knew of this measure, highlighting a significant disparity in knowledge.
Furthermore, the use of the smallest possible catheter size is essential to minimize discomfort and reduce the risk of urinary tract infections. This was understood by 67% of doctors and 65% of nurses, yet none of the paramedics were aware of this, which is concerning.
Once a patient is ready for release, the catheter should be removed if possible. All doctors and 90% of nurses were aware of this protocol, but only 40% of paramedics knew this, showing a statistically significant difference in knowledge.
Mertz and colleagues in 2011 assessed hand hygiene compliance in 13 public and private hospitals They have found adherence to hand hygiene relative frequency was 31.2%, a relatively low figure. It was a slightly lower value in the current study, with about 29%,. They Believe several factors may hinder healthcare staff’s ability to adhere to hand hygiene, including a lack of necessary equipment, cultural barriers, insufficient understanding, belief, and knowledge, time constraints, or substandard nurse-to-patient ratios. Numerous factors deter healthcare workers, such as doctors and nurses, from adhering to hand hygiene practices. These factors include working in specialized environments like surgical and anesthesia departments, staff shortages leading to low nurse-to-patient ratios, the need for wearing gowns or gloves, time constraints, lack of habit, carelessness, routine work, the absence of washing and drying equipment, busy departments, unsuitable washing materials, defects in the management system, poor understanding and awareness of the risk of infection transmission and its consequences, and low self-efficacy [12].
Another descriptive study by Najafi et al., conducted in Lorestan in 2011, evaluated the adherence of nurses and doctors to hand hygiene principles over a two-week period. In contrast to the current study, a higher rate of 34% of nurses have adhered to this hygiene practice. The compliance rate of doctors prior to patient contact is 33%, while it was slightly lower at 30%. Despite the availability of alcohol disinfectants, none of the employees use them for hand hygiene. Only 14.3% of interactions involving high-risk patients have reported they saw workers using gloves correctly. However, this value ranged from 35% to 57% [13].
In a 2016 study conducted by Yusefi et al. in Shiraz have reported a statistically significant correlation between adherence to health guidelines and the marital status and education level of the nurses. However, such correlation was not detected in Ghaem Hospital [14].
In a study by Yaghubi et al., 90% of the nurses wash their hands prior to any procedure. This figure is notably higher compared to 34% in our study. The rates of hand washing before dressing, inserting an angiocatheter, and administering intravenous injections are 82%, 70%, and 78%, respectively. In contrast, our study showed slightly higher rates at 86%, 77%, and 84% respectively, indicating a similar trend [15].
In a 2013 study by Al-Hussami and Darawad in Jordan, only 32% of nurses followed precautions to prevent infections [16].
In a study by Daneshmandi et al., 32% of hospital employees take hand hygiene practices into consideration. Hand hygiene practices have increased with the perceived risk of infection transmission. The rate of hand hygiene prior to patient contact was significantly lower than after patient contact (4% vs. 32%). The rate of hand hygiene was 34% before patient contact. However, after patient contact, this figure varied between 36% and 47% depending on the situation. The significant statistical difference in hand washing rates before and after patient contact in Daneshmandi et al.’s study is also reported[17].
Maintaining hygiene in hospitals is a basic but crucial aspect. To avoid the spread of hospital infections, medical staff are supposed to maintain the highest level of hygiene practical.
According to the findings, the Ministry of Health and related universities should prioritize familiarizing hospital staff with conventional infection control practices in accordance with global standards.
To eliminate errors associated with completing the questionnaire, in future studies, the behavior and performance of employees can be assessed in person, or by increasing the statistical population, the probability of questionnaire errors can be lowered to the greatest extent possible. Additionally, the definition of job-based training courses. To improve infection control, incentive programs based on the performance of treatment personnel must be developed, along with more effective supervision.
Most hospital employees had no sufficient knowledge and adherence to infection prevention practices. Unfortunately, this statistic has not shown significant improvement over the years. Among the staff, which includes doctors, nurses, and paramedics, none adhered fully to the recommended hygiene guidelines. One question that received the highest number of incorrect responses pertained to the routine replacement of the ventilator set. Many medical staff members mistakenly believed that this practice could prevent ventilator-associated pneumonia. There is a pressing need for the Ministry of Health and affiliated universities to intensify efforts to educate hospital staff about standard infection control precautions. These efforts should align with global standards and be tailored to the specific needs of each region. This could be achieved through academic courses, in-service training, as well as the development and enhancement of training programs. Additionally, it is crucial to establish and upgrade infection control units in emergency centers and improve working conditions. As the research was carried out through the use of a questionnaire, it is possible that the results might be distorted if the participants answer the questions on the questionnaires inaccurately
Conclusion
The majority of hospital employees lack sufficient knowledge and adherence to infection prevention practices.
Acknowledgments: Nothing declared by the authors.
Ethical Permissions: Nothing declared by the authors.
Conflicts of Interests: This study is approved with the ethical permission code of IR.MUMS.IRH.REC.1401.020.
Authors’ Contribution: Khodadadi B (First Author), Main or Assistant Researcher (25%); Sharafi M (Second Author), Methodologist (20%); Modarres Moghaddam M (Third Author), Statistical Analyst (20%); Fazli B (Fourth Author), Introduction Writer/ Discussion Writer/ (35%)
Funding/Support: Nothing declared by the authors.
Hospital infections are on the rise and significantly contribute to mortality rates among hospitalized patients. Research indicates that about 25% of hospital-acquired infections occur in intensive care units. Medical staff, particularly nurses and other personnel in direct contact with patients, play a crucial role in preventing and controlling these infections, underscoring the need for their continual education in this area [1, 2]. Additionally, a 24-hour point prevalence study conducted across 1,150 sites in 88 countries found that 54% of patients had suspected or confirmed infections, with 70% receiving at least one antibiotic for prophylactic or therapeutic purposes. The hospital mortality rate for these patients was 30% [3].
It is vital for relevant authorities to implement decisive educational initiatives in this field. While invasive medical procedures and equipment have been linked to a decrease in healthcare-associated infections over the past decade, many infections still penetrate intensive care units. This complicates treatment and jeopardizes patient outcomes, especially in the context of emerging infections. The COVID-19 pandemic is a prime example, highlighting the challenges of adapting prevention strategies to new pathogens and balancing the risk of exposure to caregivers with the provision of high-quality care [4].
Questionnaires are invaluable tools for assessing individuals' knowledge, attitudes, and behaviors. They are particularly significant due to their simplicity, cost-effectiveness, and flexibility, offering a time-efficient method for data collection.
Several studies in Iran have explored the knowledge, beliefs, and practices of medical staff regarding infection control, showing that these professionals generally demonstrate satisfactory knowledge and performance [5, 6]. However, other studies present conflicting results, particularly highlighting inadequate hand hygiene among nurses [7, 8]. Hand hygiene is critical in reducing hospital infections by 50%. Healthcare workers' hands are the primary vectors for transmitting microorganisms between patients, different areas of the same patient's body, and from contaminated environments to patients. Therefore, maintaining rigorous hand hygiene is crucial [9].
This study aimed to assess the knowledge, attitudes, and practices of nurses and patient-related staff within the special care units of Ghaem Hospital, Mashhad, focusing on the control and prevention of hospital-acquired infections.
Instrument and Methods
This descriptive-analytical study was conducted from 2022 to 2023 in the special care units of Ghaem Hospital, Mashhad. Using a census and convenience sampling method, all nurses, doctors, and paramedics working in the department were involved in the study. According to the study by Allah-Bakhshian et al. [11], with an alpha of 0.05, a beta of 0.2, and an error margin of 0.1 p, a population proportion (p) of 0.8 was calculated using the formula for estimating a ratio, resulting in a required sample size of 96 individuals.
Data collection tools included a researcher-designed questionnaire with 44 questions for gathering demographic information and separate questionnaires for assessing the knowledge, attitudes, and practices of nurses and patient-related staff regarding infection control methods. After preparing the checklist, the information was recorded in the respective file.
The validity of the questionnaire of “Measuring the knowledge attitude and performance of nurses and medical staff of ICU about infection control methods” was assessed through content validity, while reliability was determined by retesting for the knowledge and attitude sections and by bisecting for the performance section [10]. The content validity index (CVI) and content validity coefficient (CVC) for the entire questionnaire ranged from 0.8 to 1. The face validity of the questions was assessed at 3.35. Richardson’s coefficient for the knowledge section was 0.81, while Cronbach’s alpha coefficients for the attitude and performance sections were 0.71 and 0.83, respectively. The correlation coefficients were 0.9 for awareness, 0.85 for attitude, and 0.9 for performance, indicating favorable conditions. The responses on the Likert scale ranged from “I agree” to “I have no opinion” and “I disagree.”
Five questionnaires were developed based on standards from nursing reference books to assess general knowledge, precautions for intravenous injections and serum therapy, wound dressing precautions, procedures for inserting an angiocath, and suction techniques. Responses were categorized as “always,” “often,” “sometimes,” “rarely,” and “never.”
The study included nurses and patient care personnel in the intensive care unit, excluding those with less than a year’s experience in the unit and those working in other departments. Confidentiality principles were maintained, including omitting names from the database and publishing results in a generalized format. Eligible participants who were willing to participate were provided with informed consent forms. All questionnaires were administered anonymously, ensuring strict confidentiality of the results.
Upon collection, data were entered into SPSS 26. P-values less than 0.05 were considered statistically significant. Data were described using central and dispersion indices and frequency tables. The independent t-test or its non-parametric equivalent was utilized to compare the means of quantitative variables between two groups, while the Chi-squared test was applied to examine qualitative variables.
Findings
A total of 96 individuals (34 males and 62 females) participated in this study (Table 1).
Table 1. Frequency and percentage of participants' demographic information
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to health guidelines and profession regarding awareness by Chi-square test showed a statistically significant correlation between thorough hand washing, including fingernails, before procedures (p<0.001). However, no significant relationship was found in other categories (Table 2).
Table 2. Relationship between adherence to health guidelines and occupation regarding awareness
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to health guidelines and professional roles in pre-bandage procedures by Chi-square test showed a significant difference in the use of Betadine for wound cleansing, with 50% of doctors and 52% of nurses using it (p<0.001). No significant differences were found in other aspects (Table 3).
Table 3. Relationship between occupational roles and hygiene practices in pre-bandage procedures
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between adherence to hygiene practices during angiocatheter insertion and pre-suction procedures by Chi-square test showed no significant relationship (Table 4).
Table 4. Relationship between hygiene practices and job compliance in angiocatheter placement and pre-suction procedures
Comparing the relative frequency of Doctors, Nurses and Paramedics (n=96) according to the relationship between health compliance and occupation concerning awareness measures for ventilator-associated pneumonia by Chi-square test showed significant differences, with response rates of 100%, 7.6%, and 0%, respectively (p=0.0001). Preferences for oral over nasal intubation also varied significantly, with 10% of doctors, 80% of nurses, and 0% of paramedics preferring oral intubation, showing a statistically significant difference (p=0.0001). The importance of maintaining a 30-degree head elevation in patients also yielded statistically significant results (p=0.0001). Additionally, significant differences were observed in participant responses regarding not positioning the urine bag at the same level or higher than the body (p<0.0001; Table 5).
A significant difference was noted among doctors, nurses, and paramedics concerning the use of the smallest possible urinary catheter size for patients and avoiding routine urinary catheter changes, which was statistically significant (p<0.0001).
Table 5. Relationship between health compliance and occupation concerning awareness measures for ventilator-associated pneumonia (VAP)
Discussion
This study aimed to assess the knowledge, attitudes, and practices of nurses and patient-related staff within the special care units of Ghaem Hospital, Mashhad, focusing on the control and prevention of hospital-acquired infections.
Oral suction is conducted by medical, nursing, and paramedic teams. Adherence to hygiene practices such as hand washing, hand rubbing, or wearing gloves was maintained by less than 30% across all groups. However, 86% of nurses consistently used the correct suction technique, while only 65% of doctors did the same, indicating a need for additional training for doctors in this procedure.
Doctors and nurses are also tasked with adjusting ventilators. Maintaining hand hygiene is critical in preventing VAP, which can prolong hospital stays and increase the prevalence of antibiotic-resistant pathogens. Encouragingly, about 90% of doctors and nurses acknowledged the importance of hand washing before adjusting the ventilator or performing intubation.
To reduce the risk of VAP, it is advisable to maintain patients’ heads elevated at a 30-degree angle relative to the body. This practice helps minimize the likelihood of aspiration and the subsequent risk of pneumonia. Awareness of this measure was statistically significant, with all doctors and about 80% of nurses knowledgeable about it. However, awareness among paramedics was markedly lower, underscoring the need to educate all paramedic staff on this critical preventative measure.
The routine replacement of ventilator sets is known to increase the risk of pneumonia. All doctors understood this risk, but only approximately 7% of nurses and none of the paramedics were aware, indicating a significant gap in knowledge among these groups.
The role of respiratory physiotherapy for patients on ventilators is vital and must be prescribed by the attending physician. About 90% of doctors recognized the importance of this intervention.
The regular use of chlorhexidine mouthwash for ventilated patients is recommended, with about 80% of both doctors and nurses aware of this guideline.
Addressing the risk of infection during Foley catheterization is crucial. Urinary system infections can be mitigated by adhering to straightforward guidelines, including maintaining hand hygiene. Foley catheterization is performed by nurses, doctors, and occasionally paramedics. All doctors and nurses, and 90% of paramedics, demonstrated awareness of the importance of maintaining hand hygiene and sterility during this procedure. Positioning the catheter lower than the patient to prevent infection from ascending from the sac to the urinary tract is another vital practice. About 50% of doctors and 94% of nurses were aware of this critical positioning, but only 20% of paramedics knew of this measure, highlighting a significant disparity in knowledge.
Furthermore, the use of the smallest possible catheter size is essential to minimize discomfort and reduce the risk of urinary tract infections. This was understood by 67% of doctors and 65% of nurses, yet none of the paramedics were aware of this, which is concerning.
Once a patient is ready for release, the catheter should be removed if possible. All doctors and 90% of nurses were aware of this protocol, but only 40% of paramedics knew this, showing a statistically significant difference in knowledge.
Mertz and colleagues in 2011 assessed hand hygiene compliance in 13 public and private hospitals They have found adherence to hand hygiene relative frequency was 31.2%, a relatively low figure. It was a slightly lower value in the current study, with about 29%,. They Believe several factors may hinder healthcare staff’s ability to adhere to hand hygiene, including a lack of necessary equipment, cultural barriers, insufficient understanding, belief, and knowledge, time constraints, or substandard nurse-to-patient ratios. Numerous factors deter healthcare workers, such as doctors and nurses, from adhering to hand hygiene practices. These factors include working in specialized environments like surgical and anesthesia departments, staff shortages leading to low nurse-to-patient ratios, the need for wearing gowns or gloves, time constraints, lack of habit, carelessness, routine work, the absence of washing and drying equipment, busy departments, unsuitable washing materials, defects in the management system, poor understanding and awareness of the risk of infection transmission and its consequences, and low self-efficacy [12].
Another descriptive study by Najafi et al., conducted in Lorestan in 2011, evaluated the adherence of nurses and doctors to hand hygiene principles over a two-week period. In contrast to the current study, a higher rate of 34% of nurses have adhered to this hygiene practice. The compliance rate of doctors prior to patient contact is 33%, while it was slightly lower at 30%. Despite the availability of alcohol disinfectants, none of the employees use them for hand hygiene. Only 14.3% of interactions involving high-risk patients have reported they saw workers using gloves correctly. However, this value ranged from 35% to 57% [13].
In a 2016 study conducted by Yusefi et al. in Shiraz have reported a statistically significant correlation between adherence to health guidelines and the marital status and education level of the nurses. However, such correlation was not detected in Ghaem Hospital [14].
In a study by Yaghubi et al., 90% of the nurses wash their hands prior to any procedure. This figure is notably higher compared to 34% in our study. The rates of hand washing before dressing, inserting an angiocatheter, and administering intravenous injections are 82%, 70%, and 78%, respectively. In contrast, our study showed slightly higher rates at 86%, 77%, and 84% respectively, indicating a similar trend [15].
In a 2013 study by Al-Hussami and Darawad in Jordan, only 32% of nurses followed precautions to prevent infections [16].
In a study by Daneshmandi et al., 32% of hospital employees take hand hygiene practices into consideration. Hand hygiene practices have increased with the perceived risk of infection transmission. The rate of hand hygiene prior to patient contact was significantly lower than after patient contact (4% vs. 32%). The rate of hand hygiene was 34% before patient contact. However, after patient contact, this figure varied between 36% and 47% depending on the situation. The significant statistical difference in hand washing rates before and after patient contact in Daneshmandi et al.’s study is also reported[17].
Maintaining hygiene in hospitals is a basic but crucial aspect. To avoid the spread of hospital infections, medical staff are supposed to maintain the highest level of hygiene practical.
According to the findings, the Ministry of Health and related universities should prioritize familiarizing hospital staff with conventional infection control practices in accordance with global standards.
To eliminate errors associated with completing the questionnaire, in future studies, the behavior and performance of employees can be assessed in person, or by increasing the statistical population, the probability of questionnaire errors can be lowered to the greatest extent possible. Additionally, the definition of job-based training courses. To improve infection control, incentive programs based on the performance of treatment personnel must be developed, along with more effective supervision.
Most hospital employees had no sufficient knowledge and adherence to infection prevention practices. Unfortunately, this statistic has not shown significant improvement over the years. Among the staff, which includes doctors, nurses, and paramedics, none adhered fully to the recommended hygiene guidelines. One question that received the highest number of incorrect responses pertained to the routine replacement of the ventilator set. Many medical staff members mistakenly believed that this practice could prevent ventilator-associated pneumonia. There is a pressing need for the Ministry of Health and affiliated universities to intensify efforts to educate hospital staff about standard infection control precautions. These efforts should align with global standards and be tailored to the specific needs of each region. This could be achieved through academic courses, in-service training, as well as the development and enhancement of training programs. Additionally, it is crucial to establish and upgrade infection control units in emergency centers and improve working conditions. As the research was carried out through the use of a questionnaire, it is possible that the results might be distorted if the participants answer the questions on the questionnaires inaccurately
Conclusion
The majority of hospital employees lack sufficient knowledge and adherence to infection prevention practices.
Acknowledgments: Nothing declared by the authors.
Ethical Permissions: Nothing declared by the authors.
Conflicts of Interests: This study is approved with the ethical permission code of IR.MUMS.IRH.REC.1401.020.
Authors’ Contribution: Khodadadi B (First Author), Main or Assistant Researcher (25%); Sharafi M (Second Author), Methodologist (20%); Modarres Moghaddam M (Third Author), Statistical Analyst (20%); Fazli B (Fourth Author), Introduction Writer/ Discussion Writer/ (35%)
Funding/Support: Nothing declared by the authors.
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2023/11/22 | Accepted: 2024/04/8 | Published: 2024/05/20
Received: 2023/11/22 | Accepted: 2024/04/8 | Published: 2024/05/20
References
1. Jafari M, Fazeli F, Sezavar M, Khashkhashi S, Fazli B, Abdollahpour N, Sedaghat A. Role of procalcitonin in the prognosis of mortality in patients admitted to the Intensive Care Unit: A review study. Tanaffos. 2021;20(4):296-305. [Link]
2. Alrubaiee G, Baharom A, Faisal I, Shahar HK, Mohd Daud S, Basaleem H. Implementation of an educational module on nosocomial infection control measures: A randomised hospital-based trial. BMC Nurs. 2021;20:33. [Link] [DOI:10.1186/s12912-021-00551-0]
3. Vincent JL, Sakr Y, Singer M, Martin-Loeches I, Machado FR, Marshall JC, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323(15):1478-87. [Link] [DOI:10.1001/jama.2020.2717]
4. Blot S, Ruppé E, Harbarth S, Asehnoune K, Poulakou G, Luyt CE, et al. Healthcare-associated infections in adult intensive care unit patients: Changes in epidemiology, diagnosis, prevention and contributions of new technologies. Intensive Crit Care Nurs. 2022;70:103227. [Link] [DOI:10.1016/j.iccn.2022.103227]
5. Sedaghat A, Fazli B, Soheili V, Bagheri Moghadam A, Fazeli F, Mirzaei Faizabadi B. Antibiotic resistance pattern of bacteria isolated from specimens of cultures from Intensive Care Units. Medical Journal of Mashhad University of Medical Sciences. 2022; 65(5): 1915-25. [Persian] [Link]
6. Amerion A, Tavakoli R, Sanaeinasab H, Karimizarchi A. Knowledge of hospital infection control by supervisors in three selected military hospitals in Islamic Republic of Iran. Eur J Sci Res. 2010;44(4):660-5. [Link]
7. Nazari R, Haji Ahmadi M, Dadashzade M, Asgari P. Study of hand hygiene behavior among nurses in Critical Care Units. Iran J Crit Care Nurs. 2011;4(2):95-8. [Link]
8. Askarian M, Mirzaei K, Honarvar B, Etminan M, Araujo MW. Knowledge, attitude and practice towards droplet and airborne isolation precautions among dental health care professionals in Shiraz, Iran. J Public Health Dent. 2005;65(1):43-7. [Link] [DOI:10.1111/j.1752-7325.2005.tb02785.x]
9. Martín-Madrazo C, Cañada-Dorado A, Salinero-Fort MA, Abanades-Herranz JC, Arnal-Selfa R, García-Ferradal I, et al. Effectiveness of a training programme to improve hand hygiene compliance in primary healthcare. BMC Public Health. 2009;9:469. [Link] [DOI:10.1186/1471-2458-9-469]
10. Soleimani Z, Mosadeghrad AM, Abbasabadi M, Moradi M, Ashkani F, Asgari MR, et al. Developing and psychometric testing of a questionnaire to assess the knowledge, attitude and practice of paramedical staffs about nosocomial infections. Koomesh. 2021;23(4):530-9. [Persian] [Link] [DOI:10.52547/koomesh.23.4.530]
11. Allah-Bakhshian A, Moghaddasian S, Zamanzadeh V, Parvan K, Allah-Bakhshian M. Knowledge, attitude, and practice of ICU nurses about nosocomial infections control in teaching hospitals of Tabriz. Iran J Nurs. 2010;23(64):17-28. [Link]
12. Mertz D, Johnstone J, Krueger P, Brazil K, Walter SD, Loeb M. Adherence to hand hygiene and risk factors for poor adherence in 13 Ontario acute care hospitals. Am J Infect Control. 2011;39(8):693-6. [Link] [DOI:10.1016/j.ajic.2010.12.002]
13. Najafi Ghezeljeh T, Abbasnejad Z, Rafii F, Haghani H. Nurses' knowledge, beliefs and practices towards hand hygiene. J Hayat. 2015;21(1):79-93. [Persian] [Link]
14. Yusefi AR, Kavosi Z, Sadeghi A, Hadi Barhaghtalab R. Knowledge, attitude, and practice of nurses in affiliated hospitals of Shiraz University of Medical Sciences about infection control in 2016. Nurs Midwifery J. 2017;15(9):667-79. [Persian] [Link]
15. Yaghubi M, Sharifi S, Abbaspour H. Knowledge, attitude, and practice of intensive care units nurses about nosocomial Infections control in hospitals of Bojnurd in 2012. J North Khorasan Univ Med Sci. 2014;5(5):943-50. [Persian] [Link] [DOI:10.29252/jnkums.5.5.S5.943]
16. Al-Hussami M, Darawad M. Compliance of nursing students with infection prevention precautions: Effectiveness of a teaching program. Am J Infect Control. 2013;41(4):332-6. [Link] [DOI:10.1016/j.ajic.2012.03.029]
17. Daneshmandi M, Samadipour E, Salari MM. Hand hygiene practice in Sabzevar hospitals Iran. J Sabzevar Univ Med Sci. 2008;15(1):59-64. [Persian] [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






