Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 715-721 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Amin Shokravi F, Sanaei Nasab H, Karimi Zarchi A, Nashwan A, Shahbazi H. Stigma Against Health Care Providers; Caring for COVID-19 Patients in Iran. Health Educ Health Promot 2023; 11 (5) :715-721
URL: http://hehp.modares.ac.ir/article-5-72508-en.html
URL: http://hehp.modares.ac.ir/article-5-72508-en.html
1- Department of Health Education & Health Promotion, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
2- Department of Health Education, Faculty of Health, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Department of Biostatistics, Faculty of Biostatistics, Baqiyatallah University of Medical Sciences, Tehran, Iran
4- Department of Nursing Education & Practice Development, Hazm Mebaireek General Hospital (HMGH), Hamad Medical Corporation (HMC), Doha, Qatar
2- Department of Health Education, Faculty of Health, Baqiyatallah University of Medical Sciences, Tehran, Iran
3- Department of Biostatistics, Faculty of Biostatistics, Baqiyatallah University of Medical Sciences, Tehran, Iran
4- Department of Nursing Education & Practice Development, Hazm Mebaireek General Hospital (HMGH), Hamad Medical Corporation (HMC), Doha, Qatar
Full-Text [PDF 656 kb]
(2732 Downloads)
| Abstract (HTML) (874 Views)
Full-Text: (180 Views)
Introduction
Healthcare providers (HCPs) have always been a common target of stigmatization during widespread infections particularly COVID-19 [1]. The declaration of COVID-19 as a pandemic in 2020 made it a priority for governments and healthcare systems worldwide. This disease has severe consequences in terms of morbidity, mortality, economic effects, and extensive social and cultural changes. The COVID-19 pandemic has created an unprecedented panic in the minds of people around the world [2]. Some people believe that healthcare workers are a potential source of infection. This baseless belief extends to drivers of ambulances, family members of COVID-19 patients, and the patients discharged from the hospital after the cure [2]. These consequences have caused most of the efforts to be made in the field of studying the disease, treating it, and responding to the economic consequences of the epidemic.
Also, the possibility of human-to-human transmission, the knowledge gap about the disease, the fear caused by uncertainty and ignorance, and the constant change of relevant laws and recommendations, caused the stigma associated with COVID-19. Stigma has many negative consequences, such as concealment of the disease, delay in receiving health services, refusal to take preventive behaviors, suffering caused by psychological tensions, and related social and economic consequences; Therefore, the necessary measures should be taken in this field and the spread of stigma should be prevented, especially through measures aimed at raising awareness and ensuring access to reliable information [2].
To address social stigma derived from COVID-19, the WHO speaks of creating an environment where open discussion among people and healthcare workers is possible. The WHO states, “How we communicate about COVID-19 is critical in supporting people to take effective action to help combat the disease and to avoid fueling fear and stigma”. “All efforts must be taken to destigmatize COVID-19 instead of statutory sermons by lawmakers, scientifically”, urges Sarkar. “Proper health education targeting the public appears to be the most effective method to prevent social harassment of healthcare workers and COVID-19 survivors” [3].
The epidemic of coronavirus disease is known as one of the most important challenges of the present era [4]. In addition to the physical effects of this disease, human society has also faced extensive mental effects. One of the psychological and social consequences of contracting COVID-19 is the patient's fear of social reactions, the stigma of the disease, and the fact that the disease is a transmission factor, which in turn can cause many psychological and behavioral disorders in these people and have a negative impact on them. Stigma can put people's mental and emotional health at risk and negatively affect people's and communities' communication and empathy [5].
However, the psychological consequences of the disease, including the stigma of COVID-19, have been neglected. At the same time, the stigma associated with the COVID-19 disease threatens different groups, including patients, recoveries, healthcare workers, and other groups at risk. Stigma means non-fulfillment of a prescribed social norm and an attack on a person's identity [6]. The definition of stigma deals with the distinction between the normative expectations of what a person should be and what a person is, and considers stigma as the result of the gap between these two types of identity. A gap with embarrassment between the actual and potential social identity of a person [7].
Stigma is an internal feeling about having an unwanted status, along with the fear of discrimination due to low status or lack of acceptance by society [8]. Because a stigmatized person is not considered a healthy person with the necessary sufficiency to be accepted in society, the fear of being stigmatized in the case of coronavirus is not an exception to this rule. The root of stigma is in social and interpersonal relationships, and when a person cultivates the same negative thoughts that others have about him or his situation, he experiences the internal stigma of self-stigma, which can be created in both individual and group ways [9]. Also, the results of a study conducted in 2019 on 312 nurses of medical training centers in Ardabil City showed that the decrease in stubbornness or motivation and impairment of mental health in the conditions of the COVID-19 epidemic led to an increase in stigma among HCWs [10].
Healthcare providers are faced with stigma, social isolation, and discrimination in the workplace and their social environment during some diseases pandemic. Which, negatively impacts their work and decreases the efficiency of making sufficient decisions [1]. The impact of such circumstances is not just limited to the psychological well-being of care providers; It can also affect their professional competencies to provide quality care to the population during the pandemic [1, 11].
Identifying and managing related stigmas' main factors can be considered in developing educational interventions to promote people's knowledge about diseases. As a result, it may prevent the creation of stigma in such critical situations. The purpose of this study was to investigate the prevalence of stigmatization during the COVID-19 pandemic among HCWs.
Instrument and Methods
This descriptive cross-sectional study was conducted in 2022 by a simple random sampling method and based on the sample size calculation formula on 527 people in a group of HCWs who had experiences caring for COVID-19 patients. The criteria for entering the study were interest and consent to participate in the study, not having mental or physical disease, and being in contact with patients with COVID-19. The exclusion criteria included Lack of consent to participate in the study and lack of contact with patients with COVID-19.
The questionnaire used in this project is a researcher-made questionnaire with 18 questions, from questions 1 to 6 related to the demographic section, and the rest of the questions measure the stigma of service providers towards patients with COVID-19. In this section, the validity and reliability of the questionnaire of the mentioned design were assessed with the cooperation of 10 experts. Psychometrics analysis of the instrument was performed as the second goal of this study. The validity of the questionnaire was determined by measuring the content validity ratio (CVR) and content validity index (CVI) including simplicity, relevance, and clarity, as well as face validity (FV). The reliability of the questionnaire was determined by measuring Cronbach's alpha and inter-rater coefficient as 0.88 and 0.86 respectively.
The survey was completed as a self-report. The questionnaires were placed in the employees' rest room to complete. The researcher was present at the site. When the health service workers who work in the Corona patient department and come to the rooms for rest are asked to complete the questionnaire if they agree to participate in the study. Because individuals who make up the subset of the larger group are chosen at random, each individual in the large population set has the same probability of being selected. This creates, in most cases, a balanced subset that carries the greatest potential for representing the larger group as a whole.
The data were reviewed by the research team, coded, and rechecked. The data will be stored for at least 5 years on the researcher's computer located in the study room at the Faculty of Medical Sciences of Tarbiat Modares University (the responsible researcher's workplace will be stored) and in terms of security with a username and password, it will only be available to the research team; After this period, the data will be deleted and after the end of the study, the connection between the code and the ID will be lost. Any participant who participates in the survey will be considered eligible. To improve the response speed, two reminders were sent to the participants. The data was analyzed by SPSS 25 software. Frequencies and means, Pearson’s correlation coefficients also, and linear regression analysis to predict the anxiety or fear of being affected were applied.
Findings
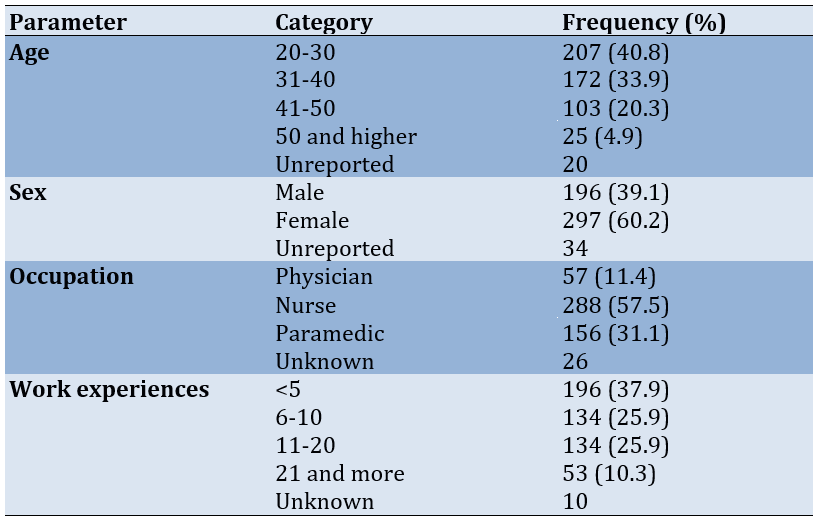
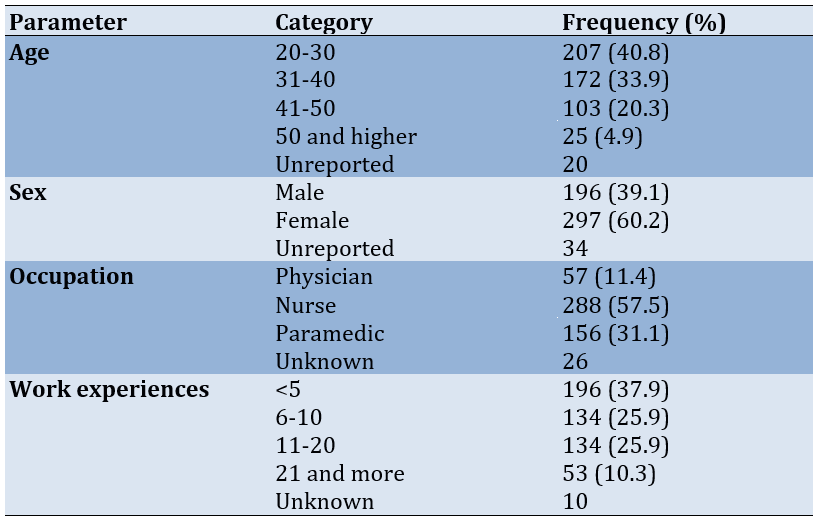
Most of the 527 participants were in the 20-30 age group (40.8%), 297 were female (60.2%), 288 were nurses (57.5%), and 196 had less than 5 years of work experience (37.9%; Table 1).
Table 1. Characteristics of the participants
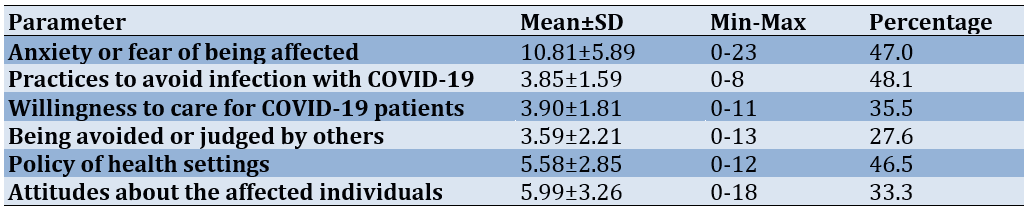
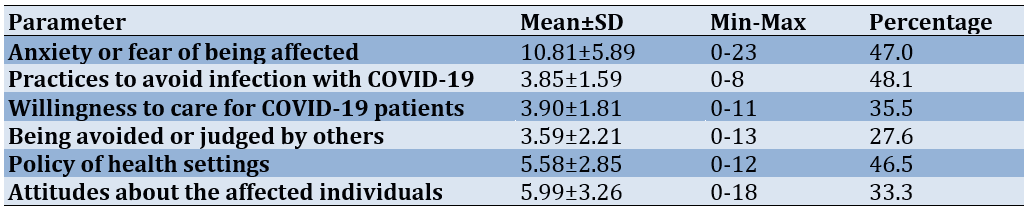
The highest percentage of the obtained score was assigned to the practices to avoid infection with COVID-19 (48.1%) and anxiety or fear of being affected (47%; Table 2).
Table 2. Mean score and standard deviation of domains of stigma in the study participants
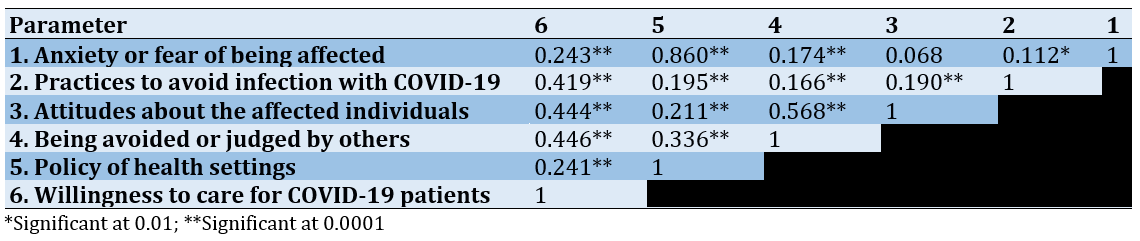
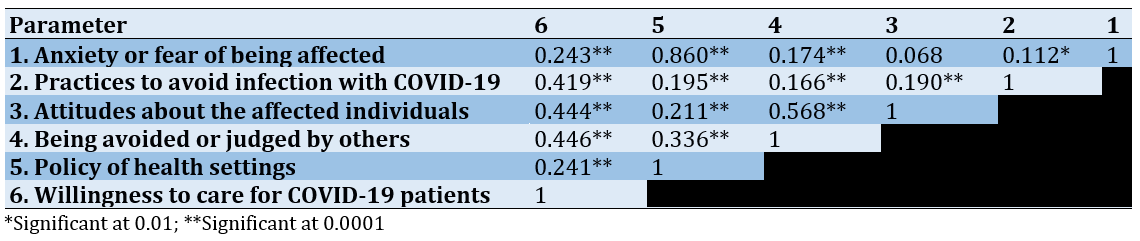
The correlations between the domains of stigma were all significant, except the correlation between anxiety and fear of being affected and attitudes about the affected individuals (p=0.118; Table 3).
Table 3. Pearson’s correlation coefficients between domains of stigma in the study participants
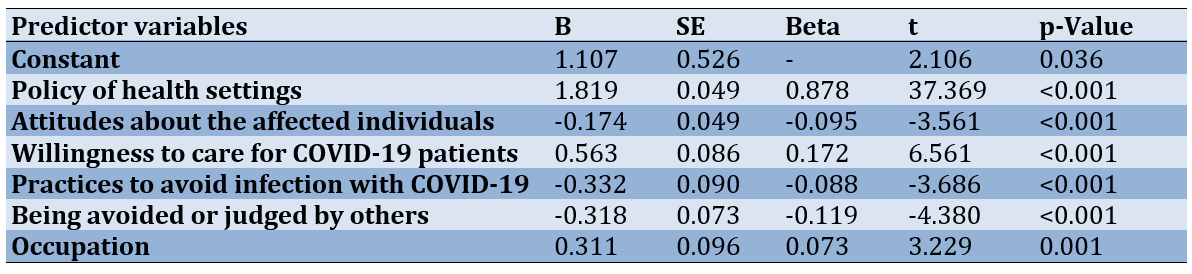
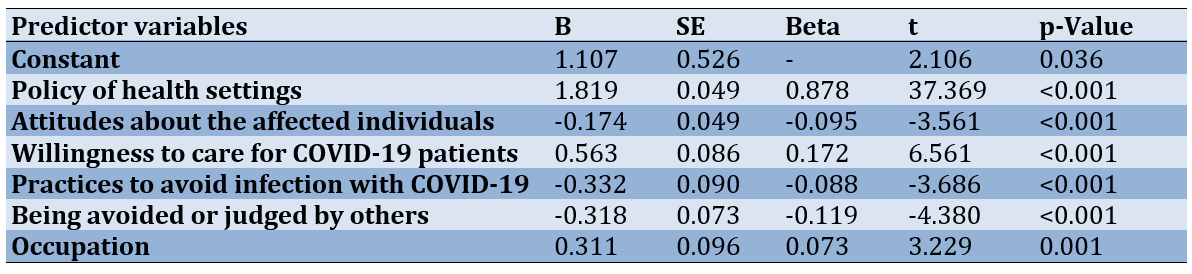
The step-by-step linear regression analysis has shown that among the domains of stigma, the most important predictor of anxiety or fear of being affected was the policy of health settings (R2=0.735). Other domains of stigma were entered into the equation, and finally, 77% predicted the variance of anxiety or fear of being affected (Table 4).
Table 4. Linear regression analysis to predict the anxiety or fear of being affected
The analysis of variance test (ANOVA) showed there were no statistically significant differences between the anxiety and fear of being affected by age and work experiences (p=0.377 and p=0.344 respectively), while there was a significant difference with occupation (p<0.001). Also, the results of the t-test test showed that there was a significant difference between the anxieties or fear of being affected and gender so the mean score of anxiety or fear of being affected was higher in females.
Discussion
In December 2019, for the first time in the city of Wuhan, China, a new type of coronavirus, called COVID-19, was identified by observing many people who experienced acute respiratory syndrome without any prior knowledge and quickly expanded. Additionally, the main characteristic of this disease was the ineffectiveness of the usual treatments [12, 13].
This contagious virus, which has common symptoms such as high fever, cough, body aches, and shortness of breath, quickly spread throughout the world. So far, it has infected more than 154 million people and caused the deaths of more than 3 million people worldwide. According to the World Health Organization, this epidemic has occurred faster than previous global epidemics and has affected more than 220 countries, including Iran. According to the statistics from the Ministry of Health, more than 7 million people have been infected with the COVID-19 virus in Iran and more than 140 thousand people have died. Stigma can undermine social cohesion and prompt possible social isolation of groups, which might contribute to a situation where the virus is more, not less, likely to spread. This can result in more severe health problems and difficulties controlling a disease outbreak. COVID-19 is closely associated with physical and mental health problems; However, little is known about the severity of the stigma caused by COVID-19 among its survivors. The level of stigma associated with COVID-19 is based on three main factors: 1) It is a disease that is new and for which there are still many unknowns, 2) We are often afraid of the unknown, and 3) It is easy to associate that fear with others [14-16].
In the present study, although the average score obtained for practice to avoid infection with COVID-19 was higher than other domains of stigma, about 48% of the essential practices to prevent COVID-19 were performed by HCWs. A range of studies have highlighted both the strengths and weaknesses in healthcare workers' adherence to infection prevention and control measures during the COVID-19 pandemic. Mustafa et al. [17] and Mohamad et al. [18] both underscore the need for improved IPC training and the establishment of institutional IPC teams to enhance HCWs' practices. Mk et al.'s study [19] at a tertiary care center found high adherence to IPC practices, particularly in the use of personal protective equipment (PPE) and environmental disinfection. However, Cobb et al.'s recommendations [20] for low- and middle-income countries emphasize the need for practical strategies, such as patient cohorts and visitor restrictions, to minimize nosocomial transmission. These findings collectively underscore the importance of continuous training, reinforcement of IPC guidelines, and tailored interventions to enhance HCWs' practices in preventing COVID-19 infections.
Healthcare workers caring for COVID-19 patients experience anxiety, fear, and stigma due to their frontline roles. Studies reveal that HCWs face stigmatization driven by the fear of infection [21], and they exhibit anxiety and depression [22, 23]. The fear experienced by HCWs is multifaceted, including insecurity, dread, and fear of proximity to death [24]. Additionally, the prevalence of anxiety and depression among HCWs during the pandemic is significant, with around one-third suffering from depression and more than one-third experiencing anxiety [25]. The impact of COVID-19 on HCWs' mental well-being is profound, leading to stress, burnout, and moderate depression, particularly affecting nurses and paramedics. In the current study, the examined healthcare workers expressed their anxiety and fear at 47% of the maximum score for this domain. In 2020, in an article entitled Stigma at the Time of the COVID-19 Pandemic in Clinical Microbiology and Infection, Villa et al. stated that public health and healthcare professionals need to address psychosocial distress faced by COVID-19 healthcare workers [11]. These findings underscore the urgent need for mental health support programs tailored to the unique challenges faced by HCWs on the frontlines of the pandemic.
The results of the present study showed there were no statistically significant differences between the anxiety or fear of being affected by age and work experiences, while there was a significant difference in occupation. Also, the results showed that there was a significant difference between the anxiety or fear of being affected and gender, so the mean score of anxiety or fear of being affected was higher in females. Bisht et al. [26] and Mertens et al. [27] found that fear of COVID-19 was independent of both gender and age. In Mertens et al. 's research, there is no significant difference between fear and age [26, 27]. Park et al. and Sreelatha & Arun, both highlighted the heightened anxiety and fear experienced by healthcare workers, particularly those involved in active COVID-19 duties and shift work [28, 29].
In this study, these were all significant, except for the correlation between anxiety and fear of being affected and attitudes about the affected individuals. Ahmed et al. discovered a positive correlation between fear of COVID-19 and health-related preventive practices [30]. Almarghlani et al. reported a significant relationship between infection-control knowledge, attitude, practice, and risk perception of occupational exposure to COVID-19 among dentists [31].
According to the results found in the present study, the most important predictor of anxiety or fear of being affected was the policy of health settings. We have not seen a similar study to compare these results. Still, these findings underscore the need for appropriate health policies and interventions to support the mental well-being of healthcare providers during the pandemic. Also, because of the different types of roles of the HCPs, there is a special source of stigma, like doctors’ fears of patients’ irresponsible behavior, which does not pay attention to infecting others. Also, doctors believe that patients must be ashamed of their feelings and report that the patients are guilty of their infection because of their irresponsibility.
Also, 77 people (14.9%) of the participants' attitudes toward COVID-19 patients were that they do not care about others getting infected, which was statistically significant. A study conducted in Finland by Lohiniva et al. in 2021 showed that perceived stigma among respondents was driven by fear and blame for infection. It manifested in various ways, leading to a reluctance to disclose their coronavirus status to others. Self-stigma developed from conflicting information and advice about coronavirus and COVID-19 led to difficulties interacting with others outside the house and reluctance to meet people after quarantine and isolation [32]. These results were consistent with our results.
In 2021, Yuan et al. reported COVID-19 survivors reported more overall stigma, and stigma in domains of social rejection, financial insecurity, internalized shame, and social isolation. Status as a COVID-19 survivor, having family members infected with COVID-19, economic loss during the COVID-19 pandemic, and depressive symptoms were positively associated with higher overall stigma levels [33]. The results of this research were in general agreement with our study. In 2020, Bagcchi announced that several incidents of stigmatization of healthcare workers, COVID-19 patients, and survivors have come up during this pandemic across the world. For instance, in Mexico, doctors and nurses were found to use bicycles, as they were reportedly denied access to public transportation and were subjected to physical assaults. Similarly, in Malawi, healthcare workers were reportedly disallowed from using public transport, insulted in the street, and evicted from rented apartments [2]. In 2020, Duan et al. reported that multinomial logistic regression analyses revealed that generally, people with a high level of education, like people working in hospitals and people with many obsession cases, have a high probability of being distributed into the stigma [34] which was consistent with our study. In 2020, Shokri et al. reported that the mean perceived stigma for COVID-19 was 5.50±2.24 out of a 10-point scale. The highest point was seen for perceived external stigma, 6.73±2.49, followed by disclosure stigma. Interestingly, self-employed were more concerned about disclosing their illness than those with government jobs and also had an overall higher stigma score [35]. In 2022, Hosseinzadeh et al. stated that Healthcare workers and their nuclear family members suffer from severe stigma, with mean stigma scores of 33.57 and 33.17, respectively [36]. Which was in agreement with our study. Therefore, it seems that in different communities and cultures, there are different types of stigma, and there needs to search on different eras to find out the relevant stigma and develop special educational interventions aimed at reducing the frequency of stigma between different HCWs and promoting the quality of the care for health services.
Self-report method of completing the questionnaire could cause over or under-estimation of the results and limit the results of the study. The experimental and control groups were blinded to the study. It is suggested to do an experimental design study with case and control groups to measure the effects of the educational intervention based on the results of the study to improve the quality of the care. Furthermore, these results highlight the necessity for suitable healthcare policies and measures to uphold the psychological welfare of healthcare professionals amid the pandemic.
Conclusion
Ongoing education, adherence to infection prevention and control protocols, and personalized strategies have the most significant role in improving healthcare workers' compliance in averting COVID-19 transmission.
Acknowledgments: The author would like to thank all the participants who sincerely participated in this study.
Ethical Permissions: All studies were conducted under the supervision of Tarbiat Modares University's ethics committee (IR.MODARES.REC.1399.205).
Conflicts of Interests: We have no conflicts of interest to declare.
Authors’ Contribution: Amin Shokravi F (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (70%); Sanaei Nasab H (Second Author), Introduction Writer (10%); Karimi Zarchi AA (Third Author), Statistical Analyst (5%); Nashwan AJ (Fourth Author), Methodologist (5%); Shahbazi H (Fifth Author), Statistical Analyst (10%)
Funding/Support: The cost of this study was provided by Tarbiat Modares University.
Healthcare providers (HCPs) have always been a common target of stigmatization during widespread infections particularly COVID-19 [1]. The declaration of COVID-19 as a pandemic in 2020 made it a priority for governments and healthcare systems worldwide. This disease has severe consequences in terms of morbidity, mortality, economic effects, and extensive social and cultural changes. The COVID-19 pandemic has created an unprecedented panic in the minds of people around the world [2]. Some people believe that healthcare workers are a potential source of infection. This baseless belief extends to drivers of ambulances, family members of COVID-19 patients, and the patients discharged from the hospital after the cure [2]. These consequences have caused most of the efforts to be made in the field of studying the disease, treating it, and responding to the economic consequences of the epidemic.
Also, the possibility of human-to-human transmission, the knowledge gap about the disease, the fear caused by uncertainty and ignorance, and the constant change of relevant laws and recommendations, caused the stigma associated with COVID-19. Stigma has many negative consequences, such as concealment of the disease, delay in receiving health services, refusal to take preventive behaviors, suffering caused by psychological tensions, and related social and economic consequences; Therefore, the necessary measures should be taken in this field and the spread of stigma should be prevented, especially through measures aimed at raising awareness and ensuring access to reliable information [2].
To address social stigma derived from COVID-19, the WHO speaks of creating an environment where open discussion among people and healthcare workers is possible. The WHO states, “How we communicate about COVID-19 is critical in supporting people to take effective action to help combat the disease and to avoid fueling fear and stigma”. “All efforts must be taken to destigmatize COVID-19 instead of statutory sermons by lawmakers, scientifically”, urges Sarkar. “Proper health education targeting the public appears to be the most effective method to prevent social harassment of healthcare workers and COVID-19 survivors” [3].
The epidemic of coronavirus disease is known as one of the most important challenges of the present era [4]. In addition to the physical effects of this disease, human society has also faced extensive mental effects. One of the psychological and social consequences of contracting COVID-19 is the patient's fear of social reactions, the stigma of the disease, and the fact that the disease is a transmission factor, which in turn can cause many psychological and behavioral disorders in these people and have a negative impact on them. Stigma can put people's mental and emotional health at risk and negatively affect people's and communities' communication and empathy [5].
However, the psychological consequences of the disease, including the stigma of COVID-19, have been neglected. At the same time, the stigma associated with the COVID-19 disease threatens different groups, including patients, recoveries, healthcare workers, and other groups at risk. Stigma means non-fulfillment of a prescribed social norm and an attack on a person's identity [6]. The definition of stigma deals with the distinction between the normative expectations of what a person should be and what a person is, and considers stigma as the result of the gap between these two types of identity. A gap with embarrassment between the actual and potential social identity of a person [7].
Stigma is an internal feeling about having an unwanted status, along with the fear of discrimination due to low status or lack of acceptance by society [8]. Because a stigmatized person is not considered a healthy person with the necessary sufficiency to be accepted in society, the fear of being stigmatized in the case of coronavirus is not an exception to this rule. The root of stigma is in social and interpersonal relationships, and when a person cultivates the same negative thoughts that others have about him or his situation, he experiences the internal stigma of self-stigma, which can be created in both individual and group ways [9]. Also, the results of a study conducted in 2019 on 312 nurses of medical training centers in Ardabil City showed that the decrease in stubbornness or motivation and impairment of mental health in the conditions of the COVID-19 epidemic led to an increase in stigma among HCWs [10].
Healthcare providers are faced with stigma, social isolation, and discrimination in the workplace and their social environment during some diseases pandemic. Which, negatively impacts their work and decreases the efficiency of making sufficient decisions [1]. The impact of such circumstances is not just limited to the psychological well-being of care providers; It can also affect their professional competencies to provide quality care to the population during the pandemic [1, 11].
Identifying and managing related stigmas' main factors can be considered in developing educational interventions to promote people's knowledge about diseases. As a result, it may prevent the creation of stigma in such critical situations. The purpose of this study was to investigate the prevalence of stigmatization during the COVID-19 pandemic among HCWs.
Instrument and Methods
This descriptive cross-sectional study was conducted in 2022 by a simple random sampling method and based on the sample size calculation formula on 527 people in a group of HCWs who had experiences caring for COVID-19 patients. The criteria for entering the study were interest and consent to participate in the study, not having mental or physical disease, and being in contact with patients with COVID-19. The exclusion criteria included Lack of consent to participate in the study and lack of contact with patients with COVID-19.
The questionnaire used in this project is a researcher-made questionnaire with 18 questions, from questions 1 to 6 related to the demographic section, and the rest of the questions measure the stigma of service providers towards patients with COVID-19. In this section, the validity and reliability of the questionnaire of the mentioned design were assessed with the cooperation of 10 experts. Psychometrics analysis of the instrument was performed as the second goal of this study. The validity of the questionnaire was determined by measuring the content validity ratio (CVR) and content validity index (CVI) including simplicity, relevance, and clarity, as well as face validity (FV). The reliability of the questionnaire was determined by measuring Cronbach's alpha and inter-rater coefficient as 0.88 and 0.86 respectively.
The survey was completed as a self-report. The questionnaires were placed in the employees' rest room to complete. The researcher was present at the site. When the health service workers who work in the Corona patient department and come to the rooms for rest are asked to complete the questionnaire if they agree to participate in the study. Because individuals who make up the subset of the larger group are chosen at random, each individual in the large population set has the same probability of being selected. This creates, in most cases, a balanced subset that carries the greatest potential for representing the larger group as a whole.
The data were reviewed by the research team, coded, and rechecked. The data will be stored for at least 5 years on the researcher's computer located in the study room at the Faculty of Medical Sciences of Tarbiat Modares University (the responsible researcher's workplace will be stored) and in terms of security with a username and password, it will only be available to the research team; After this period, the data will be deleted and after the end of the study, the connection between the code and the ID will be lost. Any participant who participates in the survey will be considered eligible. To improve the response speed, two reminders were sent to the participants. The data was analyzed by SPSS 25 software. Frequencies and means, Pearson’s correlation coefficients also, and linear regression analysis to predict the anxiety or fear of being affected were applied.
Findings
Most of the 527 participants were in the 20-30 age group (40.8%), 297 were female (60.2%), 288 were nurses (57.5%), and 196 had less than 5 years of work experience (37.9%; Table 1).
Table 1. Characteristics of the participants
The highest percentage of the obtained score was assigned to the practices to avoid infection with COVID-19 (48.1%) and anxiety or fear of being affected (47%; Table 2).
Table 2. Mean score and standard deviation of domains of stigma in the study participants
The correlations between the domains of stigma were all significant, except the correlation between anxiety and fear of being affected and attitudes about the affected individuals (p=0.118; Table 3).
Table 3. Pearson’s correlation coefficients between domains of stigma in the study participants
The step-by-step linear regression analysis has shown that among the domains of stigma, the most important predictor of anxiety or fear of being affected was the policy of health settings (R2=0.735). Other domains of stigma were entered into the equation, and finally, 77% predicted the variance of anxiety or fear of being affected (Table 4).
Table 4. Linear regression analysis to predict the anxiety or fear of being affected
The analysis of variance test (ANOVA) showed there were no statistically significant differences between the anxiety and fear of being affected by age and work experiences (p=0.377 and p=0.344 respectively), while there was a significant difference with occupation (p<0.001). Also, the results of the t-test test showed that there was a significant difference between the anxieties or fear of being affected and gender so the mean score of anxiety or fear of being affected was higher in females.
Discussion
In December 2019, for the first time in the city of Wuhan, China, a new type of coronavirus, called COVID-19, was identified by observing many people who experienced acute respiratory syndrome without any prior knowledge and quickly expanded. Additionally, the main characteristic of this disease was the ineffectiveness of the usual treatments [12, 13].
This contagious virus, which has common symptoms such as high fever, cough, body aches, and shortness of breath, quickly spread throughout the world. So far, it has infected more than 154 million people and caused the deaths of more than 3 million people worldwide. According to the World Health Organization, this epidemic has occurred faster than previous global epidemics and has affected more than 220 countries, including Iran. According to the statistics from the Ministry of Health, more than 7 million people have been infected with the COVID-19 virus in Iran and more than 140 thousand people have died. Stigma can undermine social cohesion and prompt possible social isolation of groups, which might contribute to a situation where the virus is more, not less, likely to spread. This can result in more severe health problems and difficulties controlling a disease outbreak. COVID-19 is closely associated with physical and mental health problems; However, little is known about the severity of the stigma caused by COVID-19 among its survivors. The level of stigma associated with COVID-19 is based on three main factors: 1) It is a disease that is new and for which there are still many unknowns, 2) We are often afraid of the unknown, and 3) It is easy to associate that fear with others [14-16].
In the present study, although the average score obtained for practice to avoid infection with COVID-19 was higher than other domains of stigma, about 48% of the essential practices to prevent COVID-19 were performed by HCWs. A range of studies have highlighted both the strengths and weaknesses in healthcare workers' adherence to infection prevention and control measures during the COVID-19 pandemic. Mustafa et al. [17] and Mohamad et al. [18] both underscore the need for improved IPC training and the establishment of institutional IPC teams to enhance HCWs' practices. Mk et al.'s study [19] at a tertiary care center found high adherence to IPC practices, particularly in the use of personal protective equipment (PPE) and environmental disinfection. However, Cobb et al.'s recommendations [20] for low- and middle-income countries emphasize the need for practical strategies, such as patient cohorts and visitor restrictions, to minimize nosocomial transmission. These findings collectively underscore the importance of continuous training, reinforcement of IPC guidelines, and tailored interventions to enhance HCWs' practices in preventing COVID-19 infections.
Healthcare workers caring for COVID-19 patients experience anxiety, fear, and stigma due to their frontline roles. Studies reveal that HCWs face stigmatization driven by the fear of infection [21], and they exhibit anxiety and depression [22, 23]. The fear experienced by HCWs is multifaceted, including insecurity, dread, and fear of proximity to death [24]. Additionally, the prevalence of anxiety and depression among HCWs during the pandemic is significant, with around one-third suffering from depression and more than one-third experiencing anxiety [25]. The impact of COVID-19 on HCWs' mental well-being is profound, leading to stress, burnout, and moderate depression, particularly affecting nurses and paramedics. In the current study, the examined healthcare workers expressed their anxiety and fear at 47% of the maximum score for this domain. In 2020, in an article entitled Stigma at the Time of the COVID-19 Pandemic in Clinical Microbiology and Infection, Villa et al. stated that public health and healthcare professionals need to address psychosocial distress faced by COVID-19 healthcare workers [11]. These findings underscore the urgent need for mental health support programs tailored to the unique challenges faced by HCWs on the frontlines of the pandemic.
The results of the present study showed there were no statistically significant differences between the anxiety or fear of being affected by age and work experiences, while there was a significant difference in occupation. Also, the results showed that there was a significant difference between the anxiety or fear of being affected and gender, so the mean score of anxiety or fear of being affected was higher in females. Bisht et al. [26] and Mertens et al. [27] found that fear of COVID-19 was independent of both gender and age. In Mertens et al. 's research, there is no significant difference between fear and age [26, 27]. Park et al. and Sreelatha & Arun, both highlighted the heightened anxiety and fear experienced by healthcare workers, particularly those involved in active COVID-19 duties and shift work [28, 29].
In this study, these were all significant, except for the correlation between anxiety and fear of being affected and attitudes about the affected individuals. Ahmed et al. discovered a positive correlation between fear of COVID-19 and health-related preventive practices [30]. Almarghlani et al. reported a significant relationship between infection-control knowledge, attitude, practice, and risk perception of occupational exposure to COVID-19 among dentists [31].
According to the results found in the present study, the most important predictor of anxiety or fear of being affected was the policy of health settings. We have not seen a similar study to compare these results. Still, these findings underscore the need for appropriate health policies and interventions to support the mental well-being of healthcare providers during the pandemic. Also, because of the different types of roles of the HCPs, there is a special source of stigma, like doctors’ fears of patients’ irresponsible behavior, which does not pay attention to infecting others. Also, doctors believe that patients must be ashamed of their feelings and report that the patients are guilty of their infection because of their irresponsibility.
Also, 77 people (14.9%) of the participants' attitudes toward COVID-19 patients were that they do not care about others getting infected, which was statistically significant. A study conducted in Finland by Lohiniva et al. in 2021 showed that perceived stigma among respondents was driven by fear and blame for infection. It manifested in various ways, leading to a reluctance to disclose their coronavirus status to others. Self-stigma developed from conflicting information and advice about coronavirus and COVID-19 led to difficulties interacting with others outside the house and reluctance to meet people after quarantine and isolation [32]. These results were consistent with our results.
In 2021, Yuan et al. reported COVID-19 survivors reported more overall stigma, and stigma in domains of social rejection, financial insecurity, internalized shame, and social isolation. Status as a COVID-19 survivor, having family members infected with COVID-19, economic loss during the COVID-19 pandemic, and depressive symptoms were positively associated with higher overall stigma levels [33]. The results of this research were in general agreement with our study. In 2020, Bagcchi announced that several incidents of stigmatization of healthcare workers, COVID-19 patients, and survivors have come up during this pandemic across the world. For instance, in Mexico, doctors and nurses were found to use bicycles, as they were reportedly denied access to public transportation and were subjected to physical assaults. Similarly, in Malawi, healthcare workers were reportedly disallowed from using public transport, insulted in the street, and evicted from rented apartments [2]. In 2020, Duan et al. reported that multinomial logistic regression analyses revealed that generally, people with a high level of education, like people working in hospitals and people with many obsession cases, have a high probability of being distributed into the stigma [34] which was consistent with our study. In 2020, Shokri et al. reported that the mean perceived stigma for COVID-19 was 5.50±2.24 out of a 10-point scale. The highest point was seen for perceived external stigma, 6.73±2.49, followed by disclosure stigma. Interestingly, self-employed were more concerned about disclosing their illness than those with government jobs and also had an overall higher stigma score [35]. In 2022, Hosseinzadeh et al. stated that Healthcare workers and their nuclear family members suffer from severe stigma, with mean stigma scores of 33.57 and 33.17, respectively [36]. Which was in agreement with our study. Therefore, it seems that in different communities and cultures, there are different types of stigma, and there needs to search on different eras to find out the relevant stigma and develop special educational interventions aimed at reducing the frequency of stigma between different HCWs and promoting the quality of the care for health services.
Self-report method of completing the questionnaire could cause over or under-estimation of the results and limit the results of the study. The experimental and control groups were blinded to the study. It is suggested to do an experimental design study with case and control groups to measure the effects of the educational intervention based on the results of the study to improve the quality of the care. Furthermore, these results highlight the necessity for suitable healthcare policies and measures to uphold the psychological welfare of healthcare professionals amid the pandemic.
Conclusion
Ongoing education, adherence to infection prevention and control protocols, and personalized strategies have the most significant role in improving healthcare workers' compliance in averting COVID-19 transmission.
Acknowledgments: The author would like to thank all the participants who sincerely participated in this study.
Ethical Permissions: All studies were conducted under the supervision of Tarbiat Modares University's ethics committee (IR.MODARES.REC.1399.205).
Conflicts of Interests: We have no conflicts of interest to declare.
Authors’ Contribution: Amin Shokravi F (First Author), Introduction Writer/Methodologist/Main Researcher/Discussion Writer/Statistical Analyst (70%); Sanaei Nasab H (Second Author), Introduction Writer (10%); Karimi Zarchi AA (Third Author), Statistical Analyst (5%); Nashwan AJ (Fourth Author), Methodologist (5%); Shahbazi H (Fifth Author), Statistical Analyst (10%)
Funding/Support: The cost of this study was provided by Tarbiat Modares University.
Article Type: Descriptive & Survey |
Subject:
Health Communication
Received: 2023/11/19 | Accepted: 2024/05/22 | Published: 2024/05/30
Received: 2023/11/19 | Accepted: 2024/05/22 | Published: 2024/05/30
References
1. Nashwan AJ, Valdez GFD, Sadeq AF, Al-Najjar H, Elamir H, Barakat M, et al. Stigma towards health care providers taking care of COVID-19 patients: A multi-country study. Heliyon. 2022;8(4):e09300. [Link] [DOI:10.1016/j.heliyon.2022.e09300]
2. Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20(7):782. [Link] [DOI:10.1016/S1473-3099(20)30498-9]
3. Rewerska-Juśko M, Rejdak K. Social stigma of patients suffering from COVID-19: Challenges for health care system. Healthcare. 2022;10(2):292. [Link] [DOI:10.3390/healthcare10020292]
4. Lin CY. Social reaction toward the 2019 novel coronavirus (COVID-19). Soc Health Behav. 2020;3(1):1. [Link] [DOI:10.4103/SHB.SHB_11_20]
5. UNICEF. Social stigma associated with the coronavirus disease (COVID-19). New York: UNICEF; 2020. [Link]
6. Rameshgar H, Nayebi H, Tabrizi M, Mohseni Tabrizi A. The evaluation of the effect of stigma unemployment on mental health of the unemployed. Soc Welf Q. 2017;17(67):203-31. [Persian] [Link]
7. Major B, O'brien LT. The social psychology of stigma. Annu Rev Psychol. 2005;56:393-421. [Link] [DOI:10.1146/annurev.psych.56.091103.070137]
8. Hall V, Foulkes S, Insalata F, Kirwan P, Saei A, Atti A, et al. Protection against SARS-CoV-2 after Covid-19 vaccination and previous infection. N Engl J Med. 2022;386(13):1207-20. [Link] [DOI:10.1056/NEJMoa2118691]
9. Zahraie S, Amini S, Saebi S. The relationship between illness perception, stigma and cognitive fusion with quality of life of the women with multiple sclerosis. Q J Psychol Stud. 2018;14(2):25-40. [Persian] [Link]
10. Mohamadi M, Mohtashami J, Arab Khangholi Z. Stigma towards patients with mental disorders. Iran J Syst Rev Med Sci. 2022;1(1):61-72. [Persian] [Link]
11. Villa S, Jaramillo E, Mangioni D, Bandera A, Gori A, Raviglione MC. Stigma at the time of the COVID-19 pandemic. Clin Microbiol Infect. 2020;26(11):1450-2. [Link] [DOI:10.1016/j.cmi.2020.08.001]
12. Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57(6):365-88. [Link] [DOI:10.1080/10408363.2020.1783198]
13. Shi Y, Wang G, Cai XP, Deng JW, Zheng L, Zhu HH, et al. An overview of COVID-19. J Zhejiang Univ Sci B. 2020;21(5):343-60. [Link] [DOI:10.1631/jzus.B2000083]
14. Bhanot D, Singh T, Verma SK, Sharad S. Stigma and discrimination during COVID-19 pandemic. Front Public Health. 2021;8:577018. [Link] [DOI:10.3389/fpubh.2020.577018]
15. Brodeur A, Gray D, Islam A, Bhuiyan S. A literature review of the economics of COVID‐19. J Econ Surv. 2021;35(4):1007-44. [Link] [DOI:10.1111/joes.12423]
16. Zolnikov TR, Furio F. Stigma on first responders during COVID-19. Stigma Health. 2020;5(4):375-9. [Link] [DOI:10.1037/sah0000270]
17. Mustafa ZU, Majeed HK, Latif S, Salman M, Hayat K, Mallhi TH, et al. Adherence to infection prevention and control measures among health-care workers serving in COVID-19 treatment centers in Punjab, Pakistan. Disaster Med Public Health Prep. 2023;17:e298. [Link] [DOI:10.1017/dmp.2022.252]
18. Mohamad N, Pahrol MA, Shaharudin R, Md Yazin NKR, Osman Y, Toha HR, et al. Compliance to infection prevention and control practices among healthcare workers during COVID-19 pandemic in Malaysia. Front Public Health. 2022;10:878396. [Link] [DOI:10.3389/fpubh.2022.878396]
19. MK Y, Benachinmardi K, Sura Anjanappa L. Compliance of health care workers with infection prevention and control practices in COVID-19 pandemic. SVU-Int J Med Sci. 2023;6(1):302-11. [Link] [DOI:10.21608/svuijm.2022.159283.1400]
20. Cobb N, Papali A, Pisani L, Schultz MJ, Ferreira JC. Pragmatic recommendations for infection prevention and control practices for healthcare facilities in low-and middle-income countries during the COVID-19 pandemic. Am J Trop Med Hyg. 2021;104(Suppl 3):25-33. [Link] [DOI:10.4269/ajtmh.20-1009]
21. Spruijt I, Cronin A, Udeorji F, Nazir M, Shehu S, Poix S, et al. Respected but stigmatized: Healthcare workers caring for COVID-19 patients. PLos One. 2023;18(7):e0288609. [Link] [DOI:10.1371/journal.pone.0288609]
22. Ramos FRS, Da Silva DMGV, Lima KJV, Monteiro WF, Sachett JdA, Monteiro W, et al. Path of fear: Experiences of health professionals in the fight against COVID‐19. Nurs Inq. 2023;30(4):e12578. [Link] [DOI:10.1111/nin.12578]
23. Łaskawiec-Żuławińska D, Wlazło M, Grajek M, Szlacheta P, Korzonek-Szlacheta I. Self-esteem, stress and anxiety among health care workers during the COVID-19 pandemic. J Educ Health Sport. 2023;20(1):78-89. [Link] [DOI:10.12775/JEHS.2023.20.01.009]
24. Sialakis C, Sialaki PA, Frantzana A, Iliadis C, Ouzounakis P, Kourkouta L. Prevalence of anxiety and depression of health care workers during COVID-19-a systematic review and meta-analysis. Med Pharm Rep. 2023;96(3):246-53. [Link] [DOI:10.15386/mpr-2579]
25. Rahman AU, Ejaz U, Ahtasm AD, Zartasha A, Zafar S, Asif N. Frequency of depression, anxiety and stress in health care workers serving in COVID-19 wards. Am J Health Med Nurs Pract. 2023;8(3):22-31. [Link] [DOI:10.47672/ajhmn.1458]
26. Bisht IP, Bisht RK, Sagar P. Effect of gender and age in fear and stress due to COVID-19. J Hum Behav Soc Environ. 2021;31(1-4):70-6. [Link] [DOI:10.1080/10911359.2020.1851844]
27. Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord. 2020;74:102258. [Link] [DOI:10.1016/j.janxdis.2020.102258]
28. Park S, Lee Y, Kim T, Jung SJ. Anxiety and COVID-19 related stressors among healthcare workers who performed shift work at four COVID-19 dedicated hospitals in Korea. J Occup Environ Med. 2021;63(10):875-80. [Link] [DOI:10.1097/JOM.0000000000002250]
29. Sreelatha P, Arun PVS. Fear and anxiety of COVID-19 in health care workers in a tertiary teaching hospital designated as COVID-19 19 hospital. Int J Indian Psychol. 2021;9(1):191-200. [Link]
30. Ahmed A, Nisar N, Gul A, Javed A, Abbas HB, Yasmin R. Fear of COVID-19 infection and its relationship with health-related preventive practices among patients having chronic ailments. Pak J Med Health Sci. 2021;15(9):2508-11. [Link] [DOI:10.53350/pjmhs211592508]
31. Almarghlani AA, Alshehri MA, Alghamdi AA, Sindi MA, Assaggaf MA, Al-Dabbagh N. Infection-control knowledge, attitude, practice and risk perception of occupational exposure to COVID-19 among dentists: A cross-sectional survey. Niger J Clin Pract. 2022;25(7):1029-37. [Link] [DOI:10.4103/njcp.njcp_1459_21]
32. Lohiniva A-L, Dub T, Hagberg L, Nohynek H. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS One. 2021;16(4):e0247962. [Link] [DOI:10.1371/journal.pone.0247962]
33. Yuan Y, Zhao YJ, Zhang QE, Zhang L, Cheung T, Jackson T, et al. COVID-19-related stigma and its sociodemographic correlates: A comparative study. Global Health. 2021;17(1):54. [Link] [DOI:10.1186/s12992-021-00705-4]
34. Duan W, Bu H, Chen Z. COVID-19-related stigma profiles and risk factors among people who are at high risk of contagion. Soc Sci Med. 2020;266:113425. [Link] [DOI:10.1016/j.socscimed.2020.113425]
35. Shokri A, Moradi G, Bolbanabad AM, Satary M, Shabrandi M, Sadeghkhani P, et al. Stigma and COVID-19 in Iran: A rapid assessment. Int J Hum Rights Healthc. 2020;14(1):4-9. [Link] [DOI:10.1108/IJHRH-04-2020-0025]
36. Hosseinzadeh R, Hosseini SM, Momeni M, Maghari A, Fathi-Ashtiani A, Ghadimi P, et al. Coronavirus disease 2019 (COVID-19) infection-related stigma, depression, anxiety, and stress in Iranian healthcare workers. Int J Prev Med. 2022;13:88. [Link] [DOI:10.4103/ijpvm.ijpvm_12_21]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |