Volume 11, Issue 5 (2023)
Health Educ Health Promot 2023, 11(5): 701-706 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Putri T, Abdullah K, Ligita T, Nelwati N, Narullita D, Dewi V. Effect of COVID-19 Fearing on the Quality of Life of Pregnant Women. Health Educ Health Promot 2023; 11 (5) :701-706
URL: http://hehp.modares.ac.ir/article-5-72360-en.html
URL: http://hehp.modares.ac.ir/article-5-72360-en.html
1- Department of Nursing, Faculty of Medicine, Tanjungpura University, West Kalimantan, Indonesia
2- Department of Nursing, School of Medical and Life Sciences, Sunway University, Sunway, Malaysia
3- Department of Nursing, Faculty of Nursing, Andalas University, Padang, Indonesia
4- Department of Nursing, Institute Administration and Health, Muaro Bungo, Indonesia
5- Department of Nursing, Polytechnic of Health, Jambi, Indonesia
2- Department of Nursing, School of Medical and Life Sciences, Sunway University, Sunway, Malaysia
3- Department of Nursing, Faculty of Nursing, Andalas University, Padang, Indonesia
4- Department of Nursing, Institute Administration and Health, Muaro Bungo, Indonesia
5- Department of Nursing, Polytechnic of Health, Jambi, Indonesia
Full-Text [PDF 622 kb]
(2503 Downloads)
| Abstract (HTML) (868 Views)
Full-Text: (168 Views)
Introduction
During the years of the COVID-19 outbreak, the spread of the virus has experienced peaks and troughs. Although not as high as in the early stages of the outbreak, transmission of cases still occurs worldwide. Throughout 2022, there were still fluctuations in COVID-19 cases on a global scale. Pregnant women are a vulnerable group during an outbreak [1], triggered by long-term social restrictions and various problems during an outbreak [2]. Furthermore, a significant reduction in the use of maternal health services during the 2020 COVID-19 outbreak was found in most countries [3].
During an outbreak, pregnant women can experience obstetric high risks (preeclampsia, premature birth, and cardiovascular complications) [4, 5]. The level of fear of COVID-19 was associated with a reduction in infant weight of 192 grams, decreased gestational age at birth, food insecurity, ethnicity, geographic location, history of pre-pregnancy anxiety, having a chronic health condition, pre-pregnancy BMI, parity and stage of pregnancy at the time of enrolment in the study [6]. Others reported pregnant women can experience such as domestic violence [7-9], insomnia, post-traumatic stress disorder [10], stress, anxiety, depression [11, 12], and fear, which is the cause of psychological problems for many people with various health conditions that compound the impact of infectious diseases [13].
Fear is a strategy for dealing with situations in which something is considered a threat. Studies that developed a multifaceted fear model have concluded that a threat can be viruses and diseases that cause outbreaks [14]. Another study reported that pregnant women have a higher fear of COVID-19 infection compared to nursing students and the general public [15]. Nonetheless, other studies argue that fear is a triggering factor that manifests as protective and preventive behaviors to help avoid infection by following outbreak health instructions [14]. The incidence of mental disorders in pregnant women has been reported to be higher than before the outbreak [16]. When fear becomes chronic or inappropriate, it can be dangerous and contribute to the development of various mental disorders during pregnancy [17].
The problem of low mental well-being is related to fear of COVID-19, as a relationship has been reported with a decrease in quality of life (QoL) [18]. Measuring a woman's perceived QoL and the factors that influence it during pregnancy can help to identify unmet needs and predict future health problems [19]. World Health Organization (WHO) defined QoL as a form of general well-being that includes mental status, such as stress levels, sexual function, and perceived health status [20]. A few QoL-related factors, such as better sleep quality and physical exercise, are associated with increased QoL. In contrast, physical and psychological stressors are associated with a lower QoL [21]. Economic status can affect QoL, particularly during the COVID-19 outbreak [22], and a significant correlation exists between fear and QoL [23]. Fear of COVID-19 can increase anxiety and depression, factors that can reduce QoL, a negative correlation between the level of fear related to COVID-19 and QoL may explain the decrease in QoL in pregnant women [22]. Fear can be considered an independent contributor to reduced QoL in pregnant women [17, 24].
It has been reported during the outbreak of COVID-19, there was an increase in fear and anxiety among pregnant women, leading to a significant impact on mental health in this vulnerable population [25]. Identification of fears of COVID-19 during the outbreak will highlight the need for mental health services, possibly in other populations, in response to any psychological conditions due to fear [26].
Uncertainty about the outbreak's end can increase fear and affect the QoL of pregnant women, but it can also increase alertness. Therefore, it is important to understand how fear of COVID-19 affects the QoL of pregnant women.
Instrument and Methods
In this cross-sectional study, 12,576 pregnant women were studied in six health centers in West Kalimantan, Indonesia. Data collection was conducted from June to July 2022. Convenience and snowball sampling were employed to increase the sample size. Pregnant women in our study recruited other pregnant women with our selection criteria, including women >19 years of age, in the first, second, or third trimesters, not experiencing mental disorders, and willing to participate in the study. Respondents were excluded if they had been diagnosed with or suspected positive for COVID-19. Apart from using the questionnaire distributed directly, we simultaneously shared the questionnaire using Google Forms. Data collection was conducted directly, as not all participants knew how to use a smartphone. The online questionnaire link was sent to pregnant women who made antenatal visits to the public health centers, which were scattered in various areas of Pontianak, namely north, southeast, east, south, and west of the city and in the city itself. The online survey consists of sociodemographic questions, a fear scale, and a QoL questionnaire. Based on the sample determination table for a certain population developed by Issac and Michael, the required number of samples for an error rate of 1% was estimated at 647.
The sociodemographic questionnaire included questions about age, education, occupation, COVID-19 status, gestational age, and age parity. The Fear of COVID-19 Scale (FCV-19S) questionnaire was developed by [27], and it is a robust, reliable, and valid method for assessing fear of COVID-19. The Indonesian FCV-19S has very high internal consistency [28]. This instrument consists of seven items and uses a five-point Likert scale: ‘strongly disagree’ (Minimum score is 1) to ‘strongly agree’ (Maximum score is 5). The total score is calculated by adding up the score of each item from a minimum score of 7 to a maximum score of 35. The QoL gravidarum (QoL-GRAV) questionnaire was developed by [29]. QOL-GRAV Indonesia has very high internal consistency [30]. It contains nine questions that address women’s individual QoL during pregnancy. This instrument scoring is a scale of ‘never’ (Minimum score is 0) to ‘absolute’ (Maximum score is 4), and the total score for each item is 15 to 35. The questionnaire's last three questions (items 7, 8, and 9) were scored inversely. If the scale’s mean is lower, a person’s QoL was deemed better.
Each participant gave written consent voluntarily or online. The research was conducted in accordance with ethical principles and research regulations, as defined by the university ethics committee.
The study's data were analyzed using SPSS 23 software. The Shapiro-Wilk test assessed the normality of distributions. In a bivariate analysis, the Pearson correlation test tested an association between fear of COVID-19 and pregnancy-related QoL. In the multivariate analysis, a generalized linear model accounted for obstetric and sociodemographic variables.
Findings
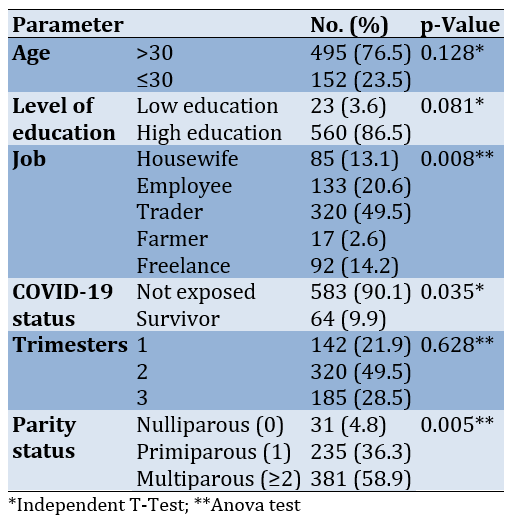
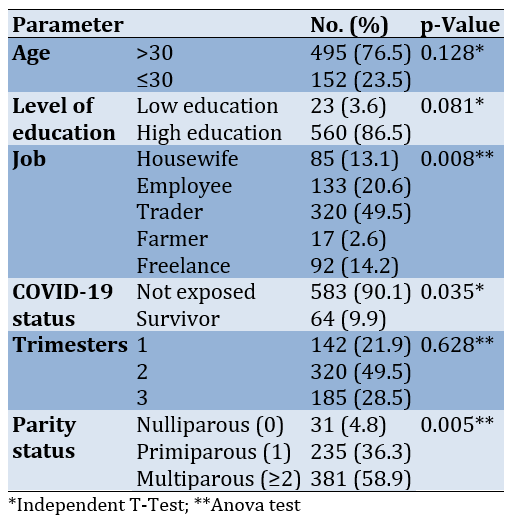
The average age of pregnant women was 28.0±3.9 years. The fear experienced by pregnant women had an average score of 21.6±9.6. The QoL average score was 25.0±8.7. There was no correlation between fear of COVID-19 and quality of life in pregnant women (p=0.056; Table 1).
Table 1. Comparing the socio-demographic, obstetric history, and COVID-19 status of the studies individuals
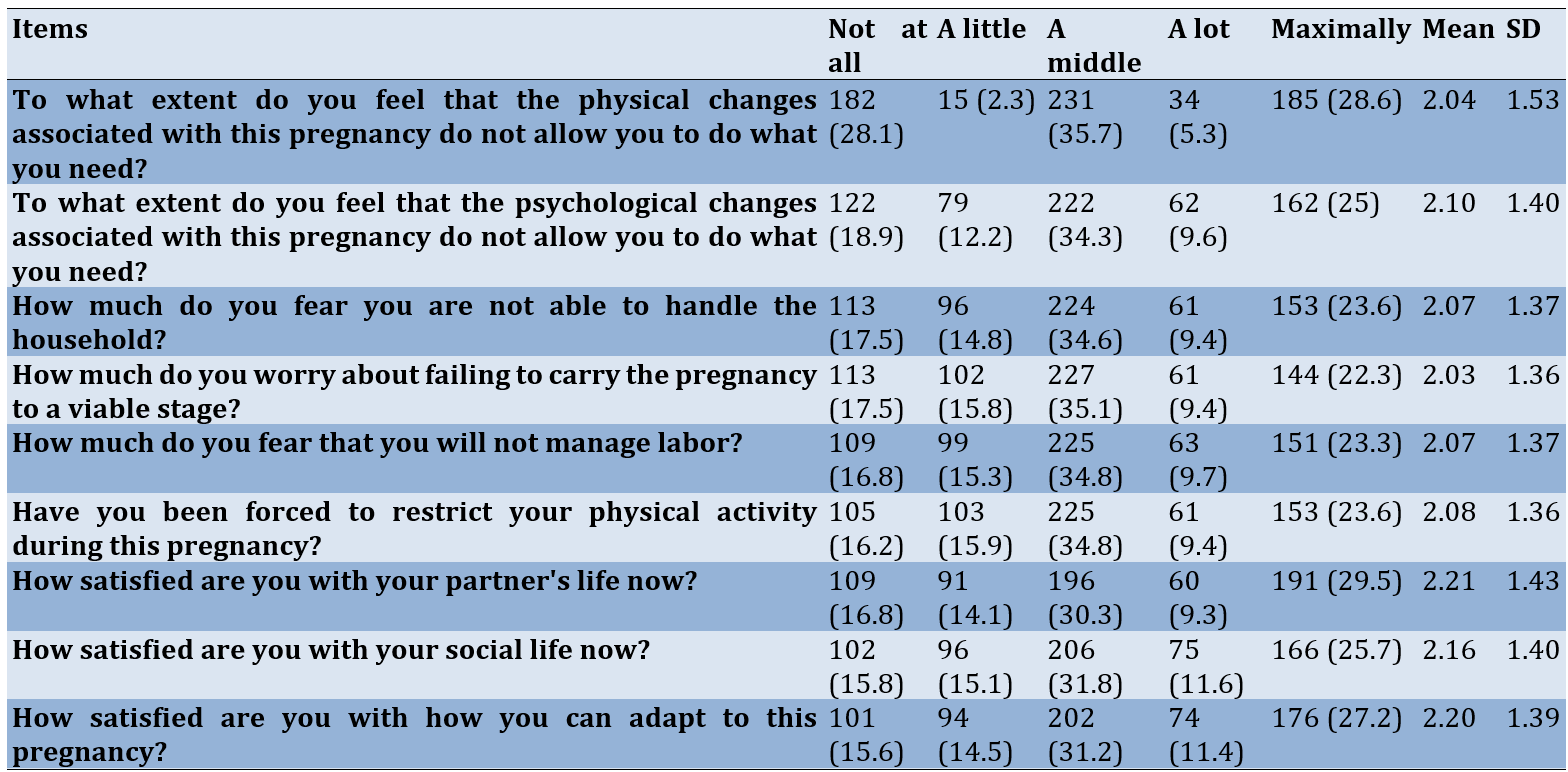
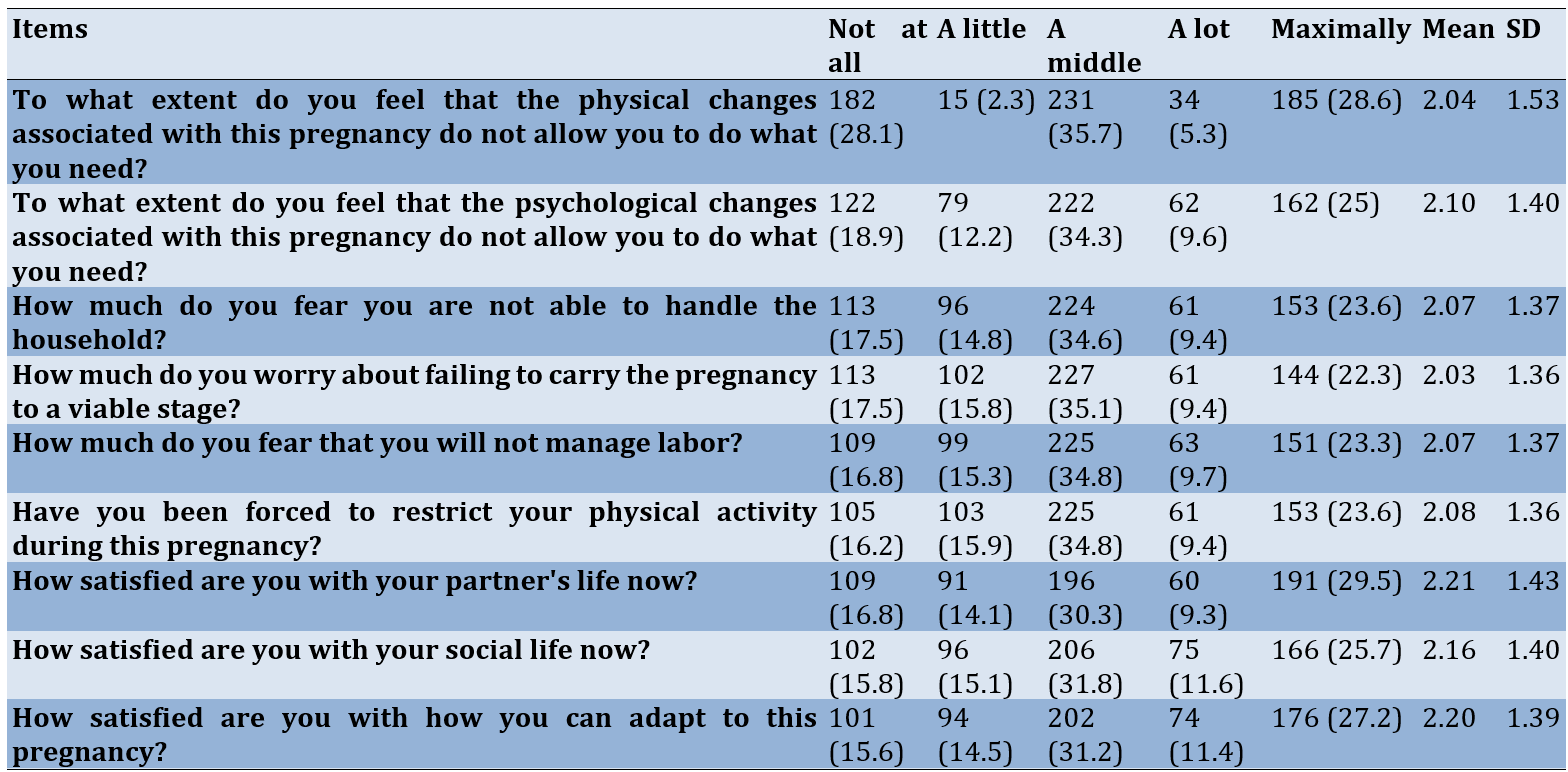
Most pregnant women chose option 3 (a middle) for all items of QoL-Grav, and the response score was highest in partner life satisfaction 2.21±1.43 (Table 2).
Table 2. Descriptive of each item QoL
The general linear model showed a dominant relationship between parity status (β=-0.083; t=-2.141; p=0.005) and job (β=-0.75; t=1.923; p=0.033) with QoL in pregnant women. COVID-19 had no significant relationship with QoL (β=-0.11; t=-2.809; p=0.055).
Discussion
Our survey suggested that the fear of COVID-19 experienced by pregnant women is from average to moderate. This result contrasts with other studies, which have reported that the average pregnant woman experiences moderate to high fear [6]. Pregnant women may fear COVID-19 because they are at high risk of being exposed to the virus, which continues to mutate, then contracting it and passing it on to their fetuses. Pregnant women also may fear contracting the COVID-19 virus, transmitting it from mother to baby, and not being able to breastfeed after giving birth [31].
Fear of COVID-19 varied by gender, education, and income level, regardless of age [32]. A systematic review reported several risk factors that increased fear experienced by pregnant women, including unplanned pregnancy, poor support from partners, and intolerance of uncertainty [25]. A potential explanation for our finding of a tendency to lower fear of COVID-19 than other studies is that our research started in the third year of the outbreak, during which antenatal services were available, and there was a decrease in COVID-19 cases and deaths compared to previous years. Furthermore, vaccines have been distributed to vulnerable groups, such as pregnant women, the elderly, children over 12 years of age, and people with mental illness. Other studies also reported reduced levels of fear expressed by vaccinated individuals [33].
Pregnancy is a critical transition period involving important physical, emotional, hormonal, and physiological changes [34]. Our research found that, on average, pregnant women experienced a decrease in QoL. Indonesian pregnant women experienced moderate QoL during the 30. Fear of COVID-19 during pregnancy can indirectly affect mental health by influencing anxiety about pregnancy [35]. Women without a risk of depression have a better QoL than women who are at risk of experiencing depressive symptoms [36]. Recent studies report an increase in domestic violence experienced by pregnant women in Indonesia during the outbreak [9]. For unmarried women, adverse events experienced during the second trimester of pregnancy are negatively related to QoL [36]. It is important to note that it is not only the fear of COVID-19 that can cause a decrease in QoL, but pregnant women also experience other problems due to the impact of COVID-19.
Our study found no correlation between fear and QoL in pregnant women. Similarly, another study reported no correlation between fear of COVID-19 and quality of mental life in pregnant women. In contrast, others reported the more fear pregnant women experience, the lower the quality of their mental life [27], and still others find that, although negatively correlated with QoL, the patient's fear is at only a moderate level [37]. Other studies suggest that fear of COVID-19 has a significant impact on loneliness and report a correlation between fear of COVID-19 and QoL [38]. Our findings contrast another study that reported a negatively significant association between fear of COVID-19 and QoL related to pregnancy [17]. Recent studies report a negative correlation between fear of COVID-19 and women's quality of sexual experiences and scores of sexual satisfaction during the outbreak [39].
Nearly half of the women in this study were traders. Significant threats emerged as a pathway for the COVID-19 outbreak, especially in global economic and trade activities [40]. Not only have traders and entrepreneurs been threatened with a double impact during the pandemic apart from health, but their income has also decreased, leading to their welfare [41]. Low income will affect QoL [42], especially during pregnancy; conditions of loss of income have been identified as prenatal stress during a pandemic [43]. In addition, parity status can affect QoL in pregnant women in this study. Parity and mode of birth have an impact on the physical and mental health of women, including women who do not have children or only one child who has worse physical and mental health than women who have two children [44]. The finding in this study is that the highest parities are multipara. In the context of the COVID-19 outbreak, changes to prenatal care are common, including changes in the postpartum experience among postpartum women and difficulties in managing childcare among mothers with young children [45]. Those with parity status of more than two children (multiparous) may have school-going children, which added stress to the parents due to school closures during the pandemic. Fear of COVID-19 and various issues related to school closures are related to parenting stress and parental well-being [46]. Parents experience moderate to severe stress levels during school closures associated with longer media screen time [47].
Although the level of fear of COVID-19 among pregnant women is average to moderate, it was thought that additional antenatal care services are still needed to minimize the existing fear experienced by pregnant women and improve QoL. In addition, mental health and psychosocial support must continue to be provided during the outbreak, especially since fear has not decreased in pregnant women. Support needs to be maintained so that pregnant women's physical and mental well-being is not neglected and QoL can be improved. The current study had some limitations. First, this study was conducted in one part of Indonesia only. Therefore, the findings may not be generalizable to the other populations in which the severity and control measures for COVID-19 may differ. Moreover, the study design and convenience sampling were used, which could lead to the possibility of response biases. However, the study instruments FCV-19S [28] and QOL-GRAV Indonesia have very high internal consistency [30].
Conclusion
There is no correlation between fear of COVID-19 and quality of life, while job and parity influence the quality of life in pregnant women.
Acknowledgments: The authors would like to thank all participants in this study for their time and effort.
Ethical Permissions: This study received ethical approval from the Institutional Review Board (IRB) of the Faculty of Medicine, Tanjungpura University (No. 780/UN.22.9/PG/2022).
Conflicts of Interests The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: Putri TH (First Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (45%); Abdullah KL (Second Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (15%); Ligita T (Third Author), Introduction Writer/Discussion Writer/Statistical Analyst (10%); Nelwati N (Fourth Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (10%); Narullita D (Fifth Author), Assistant Researche/Statistical Analyst (10%); Dewi V (Sixth Author), Assistant Researcher/Statistical Analyst (10%)
Funding/Support: This work was supported by University of Tanjungpura, DIPA UNTAN in year 2022.
During the years of the COVID-19 outbreak, the spread of the virus has experienced peaks and troughs. Although not as high as in the early stages of the outbreak, transmission of cases still occurs worldwide. Throughout 2022, there were still fluctuations in COVID-19 cases on a global scale. Pregnant women are a vulnerable group during an outbreak [1], triggered by long-term social restrictions and various problems during an outbreak [2]. Furthermore, a significant reduction in the use of maternal health services during the 2020 COVID-19 outbreak was found in most countries [3].
During an outbreak, pregnant women can experience obstetric high risks (preeclampsia, premature birth, and cardiovascular complications) [4, 5]. The level of fear of COVID-19 was associated with a reduction in infant weight of 192 grams, decreased gestational age at birth, food insecurity, ethnicity, geographic location, history of pre-pregnancy anxiety, having a chronic health condition, pre-pregnancy BMI, parity and stage of pregnancy at the time of enrolment in the study [6]. Others reported pregnant women can experience such as domestic violence [7-9], insomnia, post-traumatic stress disorder [10], stress, anxiety, depression [11, 12], and fear, which is the cause of psychological problems for many people with various health conditions that compound the impact of infectious diseases [13].
Fear is a strategy for dealing with situations in which something is considered a threat. Studies that developed a multifaceted fear model have concluded that a threat can be viruses and diseases that cause outbreaks [14]. Another study reported that pregnant women have a higher fear of COVID-19 infection compared to nursing students and the general public [15]. Nonetheless, other studies argue that fear is a triggering factor that manifests as protective and preventive behaviors to help avoid infection by following outbreak health instructions [14]. The incidence of mental disorders in pregnant women has been reported to be higher than before the outbreak [16]. When fear becomes chronic or inappropriate, it can be dangerous and contribute to the development of various mental disorders during pregnancy [17].
The problem of low mental well-being is related to fear of COVID-19, as a relationship has been reported with a decrease in quality of life (QoL) [18]. Measuring a woman's perceived QoL and the factors that influence it during pregnancy can help to identify unmet needs and predict future health problems [19]. World Health Organization (WHO) defined QoL as a form of general well-being that includes mental status, such as stress levels, sexual function, and perceived health status [20]. A few QoL-related factors, such as better sleep quality and physical exercise, are associated with increased QoL. In contrast, physical and psychological stressors are associated with a lower QoL [21]. Economic status can affect QoL, particularly during the COVID-19 outbreak [22], and a significant correlation exists between fear and QoL [23]. Fear of COVID-19 can increase anxiety and depression, factors that can reduce QoL, a negative correlation between the level of fear related to COVID-19 and QoL may explain the decrease in QoL in pregnant women [22]. Fear can be considered an independent contributor to reduced QoL in pregnant women [17, 24].
It has been reported during the outbreak of COVID-19, there was an increase in fear and anxiety among pregnant women, leading to a significant impact on mental health in this vulnerable population [25]. Identification of fears of COVID-19 during the outbreak will highlight the need for mental health services, possibly in other populations, in response to any psychological conditions due to fear [26].
Uncertainty about the outbreak's end can increase fear and affect the QoL of pregnant women, but it can also increase alertness. Therefore, it is important to understand how fear of COVID-19 affects the QoL of pregnant women.
Instrument and Methods
In this cross-sectional study, 12,576 pregnant women were studied in six health centers in West Kalimantan, Indonesia. Data collection was conducted from June to July 2022. Convenience and snowball sampling were employed to increase the sample size. Pregnant women in our study recruited other pregnant women with our selection criteria, including women >19 years of age, in the first, second, or third trimesters, not experiencing mental disorders, and willing to participate in the study. Respondents were excluded if they had been diagnosed with or suspected positive for COVID-19. Apart from using the questionnaire distributed directly, we simultaneously shared the questionnaire using Google Forms. Data collection was conducted directly, as not all participants knew how to use a smartphone. The online questionnaire link was sent to pregnant women who made antenatal visits to the public health centers, which were scattered in various areas of Pontianak, namely north, southeast, east, south, and west of the city and in the city itself. The online survey consists of sociodemographic questions, a fear scale, and a QoL questionnaire. Based on the sample determination table for a certain population developed by Issac and Michael, the required number of samples for an error rate of 1% was estimated at 647.
The sociodemographic questionnaire included questions about age, education, occupation, COVID-19 status, gestational age, and age parity. The Fear of COVID-19 Scale (FCV-19S) questionnaire was developed by [27], and it is a robust, reliable, and valid method for assessing fear of COVID-19. The Indonesian FCV-19S has very high internal consistency [28]. This instrument consists of seven items and uses a five-point Likert scale: ‘strongly disagree’ (Minimum score is 1) to ‘strongly agree’ (Maximum score is 5). The total score is calculated by adding up the score of each item from a minimum score of 7 to a maximum score of 35. The QoL gravidarum (QoL-GRAV) questionnaire was developed by [29]. QOL-GRAV Indonesia has very high internal consistency [30]. It contains nine questions that address women’s individual QoL during pregnancy. This instrument scoring is a scale of ‘never’ (Minimum score is 0) to ‘absolute’ (Maximum score is 4), and the total score for each item is 15 to 35. The questionnaire's last three questions (items 7, 8, and 9) were scored inversely. If the scale’s mean is lower, a person’s QoL was deemed better.
Each participant gave written consent voluntarily or online. The research was conducted in accordance with ethical principles and research regulations, as defined by the university ethics committee.
The study's data were analyzed using SPSS 23 software. The Shapiro-Wilk test assessed the normality of distributions. In a bivariate analysis, the Pearson correlation test tested an association between fear of COVID-19 and pregnancy-related QoL. In the multivariate analysis, a generalized linear model accounted for obstetric and sociodemographic variables.
Findings
The average age of pregnant women was 28.0±3.9 years. The fear experienced by pregnant women had an average score of 21.6±9.6. The QoL average score was 25.0±8.7. There was no correlation between fear of COVID-19 and quality of life in pregnant women (p=0.056; Table 1).
Table 1. Comparing the socio-demographic, obstetric history, and COVID-19 status of the studies individuals
Most pregnant women chose option 3 (a middle) for all items of QoL-Grav, and the response score was highest in partner life satisfaction 2.21±1.43 (Table 2).
Table 2. Descriptive of each item QoL
The general linear model showed a dominant relationship between parity status (β=-0.083; t=-2.141; p=0.005) and job (β=-0.75; t=1.923; p=0.033) with QoL in pregnant women. COVID-19 had no significant relationship with QoL (β=-0.11; t=-2.809; p=0.055).
Discussion
Our survey suggested that the fear of COVID-19 experienced by pregnant women is from average to moderate. This result contrasts with other studies, which have reported that the average pregnant woman experiences moderate to high fear [6]. Pregnant women may fear COVID-19 because they are at high risk of being exposed to the virus, which continues to mutate, then contracting it and passing it on to their fetuses. Pregnant women also may fear contracting the COVID-19 virus, transmitting it from mother to baby, and not being able to breastfeed after giving birth [31].
Fear of COVID-19 varied by gender, education, and income level, regardless of age [32]. A systematic review reported several risk factors that increased fear experienced by pregnant women, including unplanned pregnancy, poor support from partners, and intolerance of uncertainty [25]. A potential explanation for our finding of a tendency to lower fear of COVID-19 than other studies is that our research started in the third year of the outbreak, during which antenatal services were available, and there was a decrease in COVID-19 cases and deaths compared to previous years. Furthermore, vaccines have been distributed to vulnerable groups, such as pregnant women, the elderly, children over 12 years of age, and people with mental illness. Other studies also reported reduced levels of fear expressed by vaccinated individuals [33].
Pregnancy is a critical transition period involving important physical, emotional, hormonal, and physiological changes [34]. Our research found that, on average, pregnant women experienced a decrease in QoL. Indonesian pregnant women experienced moderate QoL during the 30. Fear of COVID-19 during pregnancy can indirectly affect mental health by influencing anxiety about pregnancy [35]. Women without a risk of depression have a better QoL than women who are at risk of experiencing depressive symptoms [36]. Recent studies report an increase in domestic violence experienced by pregnant women in Indonesia during the outbreak [9]. For unmarried women, adverse events experienced during the second trimester of pregnancy are negatively related to QoL [36]. It is important to note that it is not only the fear of COVID-19 that can cause a decrease in QoL, but pregnant women also experience other problems due to the impact of COVID-19.
Our study found no correlation between fear and QoL in pregnant women. Similarly, another study reported no correlation between fear of COVID-19 and quality of mental life in pregnant women. In contrast, others reported the more fear pregnant women experience, the lower the quality of their mental life [27], and still others find that, although negatively correlated with QoL, the patient's fear is at only a moderate level [37]. Other studies suggest that fear of COVID-19 has a significant impact on loneliness and report a correlation between fear of COVID-19 and QoL [38]. Our findings contrast another study that reported a negatively significant association between fear of COVID-19 and QoL related to pregnancy [17]. Recent studies report a negative correlation between fear of COVID-19 and women's quality of sexual experiences and scores of sexual satisfaction during the outbreak [39].
Nearly half of the women in this study were traders. Significant threats emerged as a pathway for the COVID-19 outbreak, especially in global economic and trade activities [40]. Not only have traders and entrepreneurs been threatened with a double impact during the pandemic apart from health, but their income has also decreased, leading to their welfare [41]. Low income will affect QoL [42], especially during pregnancy; conditions of loss of income have been identified as prenatal stress during a pandemic [43]. In addition, parity status can affect QoL in pregnant women in this study. Parity and mode of birth have an impact on the physical and mental health of women, including women who do not have children or only one child who has worse physical and mental health than women who have two children [44]. The finding in this study is that the highest parities are multipara. In the context of the COVID-19 outbreak, changes to prenatal care are common, including changes in the postpartum experience among postpartum women and difficulties in managing childcare among mothers with young children [45]. Those with parity status of more than two children (multiparous) may have school-going children, which added stress to the parents due to school closures during the pandemic. Fear of COVID-19 and various issues related to school closures are related to parenting stress and parental well-being [46]. Parents experience moderate to severe stress levels during school closures associated with longer media screen time [47].
Although the level of fear of COVID-19 among pregnant women is average to moderate, it was thought that additional antenatal care services are still needed to minimize the existing fear experienced by pregnant women and improve QoL. In addition, mental health and psychosocial support must continue to be provided during the outbreak, especially since fear has not decreased in pregnant women. Support needs to be maintained so that pregnant women's physical and mental well-being is not neglected and QoL can be improved. The current study had some limitations. First, this study was conducted in one part of Indonesia only. Therefore, the findings may not be generalizable to the other populations in which the severity and control measures for COVID-19 may differ. Moreover, the study design and convenience sampling were used, which could lead to the possibility of response biases. However, the study instruments FCV-19S [28] and QOL-GRAV Indonesia have very high internal consistency [30].
Conclusion
There is no correlation between fear of COVID-19 and quality of life, while job and parity influence the quality of life in pregnant women.
Acknowledgments: The authors would like to thank all participants in this study for their time and effort.
Ethical Permissions: This study received ethical approval from the Institutional Review Board (IRB) of the Faculty of Medicine, Tanjungpura University (No. 780/UN.22.9/PG/2022).
Conflicts of Interests The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: Putri TH (First Author), Introduction Writer/Methodologist/Main or Assistant Researcher/Discussion Writer/Statistical Analyst (45%); Abdullah KL (Second Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (15%); Ligita T (Third Author), Introduction Writer/Discussion Writer/Statistical Analyst (10%); Nelwati N (Fourth Author), Introduction Writer/Methodologist/Discussion Writer/Statistical Analyst (10%); Narullita D (Fifth Author), Assistant Researche/Statistical Analyst (10%); Dewi V (Sixth Author), Assistant Researcher/Statistical Analyst (10%)
Funding/Support: This work was supported by University of Tanjungpura, DIPA UNTAN in year 2022.
Article Type: Descriptive & Survey |
Subject:
Quality of Life
Received: 2023/11/11 | Accepted: 2023/12/20 | Published: 2024/05/8
Received: 2023/11/11 | Accepted: 2023/12/20 | Published: 2024/05/8
References
1. Moore KM, Suthar MS. Comprehensive analysis of COVID-19 during pregnancy. Biochem Biophys Res Commun. 2021;538:180-6. [Link] [DOI:10.1016/j.bbrc.2020.12.064]
2. Lu X, Lin Z. COVID-19, economic impact, mental health, and coping behaviors: A conceptual framework and future research directions. Front Psychol. 2021;12:759974. [Link] [DOI:10.3389/fpsyg.2021.759974]
3. Manchia M, Gathier AW, Yapici-Eser H, Schmidt MV, De Quervain D, Van Amelsvoort T, et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur Neuropsychopharmacol. 2022;55:22-83. [Link] [DOI:10.1016/j.euroneuro.2021.10.864]
4. Briller JE, Aggarwal NR, Davis MB, Hameed AB, Malhamé I, Mahmoud Z, et al. Cardiovascular complications of pregnancy-associated COVID-19 infections. JACC Adv. 2022;1(3):100057. [Link] [DOI:10.1016/j.jacadv.2022.100057]
5. Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. Can Med Assoc J. 2021;193(16):E540-8. [Link] [DOI:10.1503/cmaj.202604]
6. Giesbrecht GF, Rojas L, Patel S, Kuret V, MacKinnon AL, Tomfohr-Madsen L, et al. Fear of COVID-19, mental health, and pregnancy outcomes in the pregnancy during the COVID-19 pandemic study: Fear of COVID-19 and pregnancy outcomes. J Affect Disord. 2022;299:483-91. [Link] [DOI:10.1016/j.jad.2021.12.057]
7. Kourti A, Stavridou A, Panagouli E, Psaltopoulou T, Spiliopoulou C, Tsolia M, et al. Domestic violence during the COVID-19 pandemic: A systematic review. Trauma Violence Abuse. 2023;24(2):719-45. [Link] [DOI:10.1177/15248380211038690]
8. Orpin J, Papadopoulos C, Puthussery S. The prevalence of domestic violence among pregnant women in Nigeria: A systematic review. Trauma Violence Abuse. 2020;21(1):3-15. [Link] [DOI:10.1177/1524838017731570]
9. Putri TH, Fujiana F. Domestic violence against pregnant women during the COVID-19 pandemic. Jurnal Keperawatan Jiwa (JKJ): Persatuan Perawat Nasional Indonesia. 2022;10(3):625-32. [Indonesian] [Link] [DOI:10.26714/jkj.10.2.2022.285-296]
10. Bastami M, Monibi H, Shahamati E, Yazdanpanah A. The impact of COVID-19 pandemic on quality of life and psychological outcomes associated home quarantine: A narrative study; 2022. [Link]
11. Kolker S, Biringer A, Bytautas J, Blumenfeld H, Kukan S, Carroll JC. Pregnant during the COVID-19 pandemic: An exploration of patients' lived experiences. BMC Pregnancy Childbirth. 2021;21:851. [Link] [DOI:10.1186/s12884-021-04337-9]
12. Mowbray H. In Beijing, coronavirus 2019-nCoV has created a siege mentality. BMJ. 2020;368:m516. [Link] [DOI:10.1136/bmj.m516]
13. Koçak O, Koçak ÖE, Younis MZ. The psychological consequences of COVID-19 fear and the moderator effects of individuals' underlying illness and witnessing infected friends and family. Int J Environ Res Public Health. 2021;18(4):1836. [Link] [DOI:10.3390/ijerph18041836]
14. Starcevic V, Schimmenti A, Billieux J. A model of multifaceted fear during the Covid-19 pandemic and balancing between overemphasising and neglecting the distinction between fear and anxiety: A reply to Heeren (2020). Clin Neuropsychiatry. 2020;17(4):255-9. [Link]
15. Koiwa K, Wakashima K, Ikuta M, Asai K, Takagi G. Fear of COVID-19 infection and related factors in Japan: A comparison of college students, pregnant women, hospital nurses and the general public. PLoS One. 2022;17(7):e0271176. [Link] [DOI:10.1371/journal.pone.0271176]
16. Koyucu RG, Karaca PP. The Covid 19 outbreak: Maternal mental health and associated factors. Midwifery. 2021;99:103013. [Link] [DOI:10.1016/j.midw.2021.103013]
17. Naghizadeh S, Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch Psychiatr Nurs. 2021;35(4):364-8. [Link] [DOI:10.1016/j.apnu.2021.05.006]
18. Alyami M, De Albuquerque JV, Krägeloh CU, Alyami H, Henning MA. Effects of fear of COVID-19 on mental well-being and quality of life among Saudi adults: A path analysis. Saudi J Med Med Sci. 2021;9(1):24-30. [Link] [DOI:10.4103/sjmms.sjmms_630_20]
19. Alzboon G, Vural G. Factors influencing the quality of life of healthy pregnant women in north Jordan. Medicina. 2019;55(6):278. [Link] [DOI:10.3390/medicina55060278]
20. Wu H, Sun W, Chen H, Wu Y, Ding W, Liang S, et al. Health-related quality of life in different trimesters during pregnancy. Health Qual Life Outcomes. 2021;19:182. [Link] [DOI:10.1186/s12955-021-01811-y]
21. Boutib A, Chergaoui S, Marfak A, Hilali A, Youlyouz-Marfak I. Quality of life during pregnancy from 2011 to 2021: Systematic review. Int J Womens Health. 2022;14:975-1005. [Link] [DOI:10.2147/IJWH.S361643]
22. Aksoy A, Abiç A, Değirmenci F, Vefikuluçay Yılmaz D. The relationship between quality of life and fear of Turkish individuals during the COVID-19 pandemic: A cross-sectional study. Arch Psychiatr Nurs. 2021;35(5):472-8. [Link] [DOI:10.1016/j.apnu.2021.06.003]
23. Yeni K, Tulek Z, Ozer A, Cavusoglu A, Inan GS, Baykan B, et al. The effect of fear of COVID-19 on quality of life in patients with epilepsy. Neurol Asia. 2022;27(1):109-16. [Link] [DOI:10.54029/2022jzi]
24. Dule A, Hajure M, Mohammedhussein M, Abdu Z. Health-related quality of life among Ethiopian pregnant women during COVID-19 pandemic. Brain Behav. 2021;11(4):e02045. [Link] [DOI:10.1002/brb3.2045]
25. Muñoz-Vela FJ, Rodríguez-Díaz L, Gómez-Salgado J, Fernández-Carrasco FJ, Allande-Cussó R, Vázquez-Lara JM, et al. Fear and anxiety in pregnant women during the COVID-19 pandemic: A systematic review. Int J Public Health. 2023;68:1605587. [Link] [DOI:10.3389/ijph.2023.1605587]
26. Quadros S, Garg S, Ranjan R, Vijayasarathi G, Mamun MA. Fear of COVID 19 infection across different cohorts: A scoping review. Front Psychiatry. 2021;12:708430. [Link] [DOI:10.3389/fpsyt.2021.708430]
27. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: Development and initial validation. Int J Ment Health Addict. 2022;20(3):1537-45. [Link] [DOI:10.1007/s11469-020-00270-8]
28. Nazari N, Safitri S, Usak M, Arabmarkadeh A, Griffiths MD. Psychometric validation of the Indonesian version of the fear of COVID-19 scale: Personality traits predict the fear of COVID-19. Int J Ment Health Addict. 2021;21(3):1348-64. [Link] [DOI:10.1007/s11469-021-00593-0]
29. Vachkova E, Jezek S, Mares J, Moravcova M. The evaluation of the psychometric properties of a specific quality of life questionnaire for physiological pregnancy. Health Qual Life Outcomes. 2013;11:214. [Link] [DOI:10.1186/1477-7525-11-214]
30. Putri TH, Priyono D, PH L, Narullita D, Agusthia M, Rahmaniza R. Quality of life in pregnancy woman during the COVID-19 pandemic. Jurnal Keperawatan Jiwa (JKJ): Persatuan Perawat Nasional Indonesia. 2022;10(3):615-24. [Indonesian] [Link]
31. Yeşilçinar İ, Güvenç G, Kinci MF, Bektaş Pardes B, Kök G, Sivaslioğlu AA. Knowledge, fear, and anxiety levels among pregnant women during the COVID-19 pandemic: A cross-sectional study. Clin Nurs Res. 2022;31(4):758-65. [Link] [DOI:10.1177/10547738221085662]
32. Demirbas N, Kutlu R. Effects of COVID-19 fear on society's quality of life. Int J Ment Health Addict. 2022;20(5):2813-22. [Link] [DOI:10.1007/s11469-021-00550-x]
33. Seddig D, Maskileyson D, Davidov E. Vaccination against COVID-19 reduces virus-related fears: Findings from a German longitudinal study. Front Public Health. 2022;10:878787. [Link] [DOI:10.3389/fpubh.2022.878787]
34. Alnuaimi K, Alshraifeen A, Aljaraedah H. Factors influencing quality of life among syrian refugees pregnant women in Jordan: A cross-sectional study. Heliyon. 2022;8(9):e10685. [Link] [DOI:10.1016/j.heliyon.2022.e10685]
35. Salehi L, Rahimzadeh M, Molaei E, Zaheri H, Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: A structural equation model. Brain Behav. 2020;10(11):e01835. [Link] [DOI:10.1002/brb3.1835]
36. Saridi M, Toska A, Latsou D, Chondropoulou MA, Matsioula A, Sarafis P. Assessment of quality of life and psycho-emotional burden in pregnant women in Greece. Eur J Midwifery. 2022;6:13. [Link] [DOI:10.18332/ejm/145963]
37. Akbaba A, Erünal M, Ozdamar H, Mert H, Dursun H, Kaya D. Determination of the fear of COVID-19 and the quality of life of patients with transcatheter aortic valve implants during the pandemic. Clin Nurs Res. 2022;31(8):1422-30. [Link] [DOI:10.1177/10547738221102275]
38. Ahorsu DK, Imani V, Lin CY, Timpka T, Broström A, Updegraff JA, et al. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: An actor-partner interdependence modelling. Int J Ment Health Addict. 2022;20(1):68-82. [Link] [DOI:10.1007/s11469-020-00340-x]
39. Gönenç IM, Öztürk Özen D, Yılmaz Sezer N. The relationship between fear of COVID-19, quality of sexual life, and sexual satisfaction of women in Turkey. Int J Sex Health. 2022;34(3):377-85. [Link] [DOI:10.1080/19317611.2022.2058145]
40. Yu Z, Li Y, Xie X. Long-term trade impact of epidemic outbreaks: Is it V-shaped?. Econ Anal Policy. 2021;71:16-40. [Link] [DOI:10.1016/j.eap.2021.04.003]
41. Xu Z, Jia H. The influence of COVID-19 on Entrepreneur's psychological well-being. Front Psychol. 2022;12:823542. [Link] [DOI:10.3389/fpsyg.2021.823542]
42. Rizal H, Said MA, Majid HA, Su TT, Pin TM, Ismail R, et al. Health-related quality of life of younger and older lower-income households in Malaysia. PLoS One. 2022;17(2):e0263751. [Link] [DOI:10.1371/journal.pone.0263751]
43. Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. 2020;266:113348. [Link] [DOI:10.1016/j.socscimed.2020.113348]
44. Davis DL, Wu C, Brown WJ, Nohr EA. Parity and mode of birth and their relationships with quality of life: A longitudinal study. PLoS One. 2022;17(9):e0273366. [Link] [DOI:10.1371/journal.pone.0273366]
45. Ghassabian A, Jacobson MH, Kahn LG, Brubaker SG, Mehta-Lee SS, Trasande L. Maternal perceived stress during the COVID-19 pandemic: Pre-existing risk factors and concurrent correlates in New York city women. Int J Public Health. 2022;67:1604497. [Link] [DOI:10.3389/ijph.2022.1604497]
46. Chen CYC, Byrne E, Vélez T. A preliminary study of COVID-19-related stressors, parenting stress, and parental psychological well-being among parents of school-age children. J Child Fam Stud. 2022;31(6):1558-69. [Link] [DOI:10.1007/s10826-022-02321-1]
47. Seguin D, Kuenzel E, Morton JB, Duerden EG. School's out: Parenting stress and screen time use in school-age children during the COVID-19 pandemic. J Affect Disord Rep. 2021;6:100217. [Link] [DOI:10.1016/j.jadr.2021.100217]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |