Volume 12, Issue 1 (2024)
Health Educ Health Promot 2024, 12(1): 9-15 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Damayantie N, Ernawati E, Dewi M, Fahmi I. Nursing Education on Diabetes Through Smartphone Therapeutic Applications. Health Educ Health Promot 2024; 12 (1) :9-15
URL: http://hehp.modares.ac.ir/article-5-72139-en.html
URL: http://hehp.modares.ac.ir/article-5-72139-en.html
1- Department of Nursing, Health Polytecnic of Jambi, Jambi, Indonesia
Keywords: Diabetes Mellitus [Mesh], Health Belief Model [MeSH], Hypoglycemia [MeSH], Smartphone [MeSH]
Full-Text [PDF 630 kb]
(3489 Downloads)
| Abstract (HTML) (2032 Views)
Full-Text: (458 Views)
Introduction
In addition to managing blood sugar levels, the treatment also emphasized strategies for reducing multifactorial risks [1, 2]. The global prevalence of diabetes mellitus has reached 424.9 million people, with an estimated projection to increase to 628.6 million people by 2045. Approximately ninety percent (90%) of diabetes cases are classified as type 2 diabetes mellitus (T2DM), characterized by impaired insulin sensitivity and secretion [3].
Indonesia is ranked sixth globally in terms of the number of people with diabetes mellitus, currently at 10.3 million people, and this number is projected to rise to 16.7 million by 2045 [4]. The use of insulin or oral hypoglycemic agents in diabetes mellitus therapy often leads to hypoglycemic effects. This can be caused by inadequate insulin administration, excessive dosing, or the failure of counterregulatory mechanisms due to the long-standing diabetes mellitus disease process. To date, approximately 90% of diabetic patients receiving insulin therapy have experienced episodes of hypoglycemia [5].
The prevention of hypoglycemia involves improving blood glucose control and early detection, which includes educating individuals about the signs and symptoms of hypoglycemia, interim treatments, and other essential measures [6, 7]. Assessment of knowledge regarding self-monitoring of blood sugar can be conducted after specific training. Understanding hypoglycemia is crucial for recognizing its symptoms, interpreting early signs, and making informed decisions independently or with assistance. Knowledge of T2DM management and hypoglycemia symptoms positively impacts patients' self-awareness in detecting hypoglycemia [8, 9].
The continuous advancement of science and technology has encouraged new efforts in utilizing technological advancements within the learning process [10]. The emergence of new technologies has broadened the scope of specialist nurses, facilitating efficient and sustainable technology-based nursing practices. This involves identifying suitable technologies and application systems in accordance with the nursing plan and the condition of the DM patient [11, 12]. Multimedia refers to the presentation of material using text and images. Learners can achieve a better understanding when information is presented with both text and images compared to presentations using text alone [13]. The multimedia cognitive theory assumes that the human data processing system comprises multiple channels for visual and auditory processing. Each channel has a limited processing capacity, and active education entails the coordinated execution of a series of cognitive processes during learning [14].
Numerous studies have explored the use of smartphones as educational tools for managing diabetes mellitus and improving the quality of life. According to research by Bonoto, smartphone applications have shown promise in enhancing HbA1c control for patients with type 1 and 2 Diabetes Mellitus. These applications typically incorporate features such as storage and feedback for blood glucose data, dietary guidance, physical exercise tracking, dosage management, medication adherence, and access to healthcare professionals to facilitate better glycemic control. The findings also indicated that patients gained confidence in managing their diabetes, leading to an improved quality of life and a reduced fear of encountering potential hypoglycemic episodes [15, 16].
The diabetes education model was scientifically developed as a structured learning design presented in an academic text. It encompasses various development stages, including model conceptualization, product development, and field testing. Creating a diabetes education model involves analyzing the problem, context, and existing literature, followed by outlining and designing an initial prototype. This smartphone application is known as NEDTA (Nursing Education Diabetic Therapeutic Application).
The NEDTA enables individuals with T2DM to engage in independent learning through a user-friendly interface accessible on both IOS and Android platforms. The app's simple navigation allows for anytime usage, and its incorporation of images and videos enhances user engagement. Through problem-based learning and case studies, the app fosters critical thinking skills among its users. Additionally, the general public can utilize the app to raise awareness and prevent and manage early-stage hypoglycemia. Despite extensive exploration in previous research, researchers have not identified any similar applications.
This research holds significant importance as the development of a diabetes education model for T2DM patients could empower them to independently manage their health. Moreover, this study strongly aligns with the policies and initiatives of the Indonesian government, aiming to prevent and control diabetes by fostering community empowerment through the Non-Communicable Disease Prevention and Control Program. Leveraging smartphones as educational tools enables individuals to use information technology for the enhancement and maintenance of their health, underscoring the crucial significance of this research. The primary objective of this study was to develop a therapeutic education model for diabetes mellitus, focusing on enhancing the ability of T2DM patients to detect hypoglycemia.
Materials and Methods
Research Design
This research adopted a design and development approach, utilizing mixed methods [17]. The development stage primarily emphasized the qualitative aspects, focusing on the conceptual model, while the product development and trial stages incorporated a blend of qualitative and quantitative elements. During the trial stage, the quantitative aspect took precedence. The product design and development process followed the ADDIE framework across all stages [18], including analysis, design, development, implementation, and evaluation for the main stage, while the design stage of the intervention product used the dick and colleagues intervention design model [19]. The media for diabetes education, aimed at enhancing the ability to detect hypoglycemia in T2DM patients, was founded on the health belief model (HBM), encompassing perceived vulnerability, perceived severity, and perceived benefits. Additionally, the social cognitive theory was integrated, considering behavioral, personal, cognitive, and environmental factors. The development stages of the diabetes education model for improving hypoglycemia detection in T2DM patients were aligned with behavior change theory.
During its model development, diabetes education entailed analyzing the problem, context, and literature, followed by the outline and design of an initial prototype. The smartphone application was named NEDTA (Nursing Education Diabetic Therapeutic Application).
This prototype was a smartphone-based educational medium equipped with health education features focusing on diabetes mellitus, hypoglycemia identification, and initial hypoglycemia management. The intervention model underwent field testing through a quasi-experimental design, employing a two-group pre-test and post-test design with a control group.
Participants
This study involved 64 individuals with DM and was conducted between May and September 2023. The participants were randomly selected and met the inclusion criteria of having and currently experiencing DM, as well as possessing and being capable of using an Android cellphone.
Sample Size
A total of 64 students were calculated using Slovin's formula at α=0.05, and the total population was considered to be 75 people. According to Imas Masturoh and Nauri Anggita [20], the sample size was calculated using the Taro Yamane formula as follows:
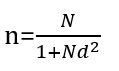
n=number of samples
N=statistical population
d=precision
Data Collection and Instrument
The authors independently compiled the questionnaire, which has been validated and deemed feasible. The questionnaire comprised 20 positive and negative statements, with answer options, including 'often,' 'sometimes,' and 'never'.
Statistical Analisis
In component 1 (analysis), qualitative data were obtained during the initial observation activities, precisely at the needs analysis stage. The subsequent analysis stage was constructed from the bottom up, also known as inductive analysis. Univariate analysis was performed on the quantitative data to determine the percentage or magnitude of the problem or indicators under scrutiny. The quantitative data, collected from individuals with DM during the needs analysis stage, were then subjected to descriptive statistical analysis. This process involved narration and interpretation to underscore its urgency for the practical resolution of the identified issues.
In the prototype development component, expert validation was presented qualitatively. During the field test, the data were presented descriptively, accompanied by the frequency distribution. Data were analyzed using descriptive analysis and inferential statistics. Numerical data were presented as mean, median, standard deviation, minimum, and maximum. The paired t-test was then utilized to assess the impact of product usage.
Findings
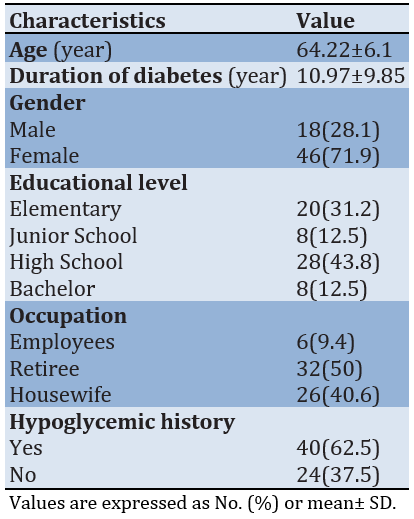
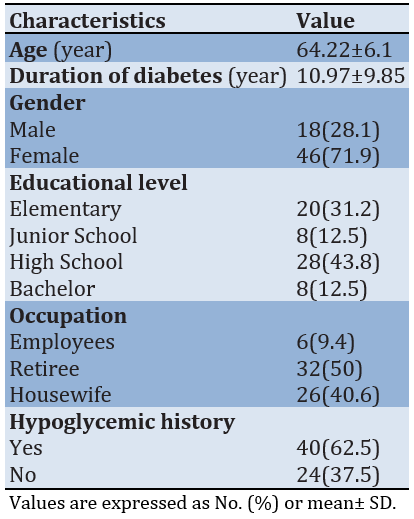
The majority of respondents were female, accounting for 71.9% of the total. Furthermore, 43.8% of participants had attained a high school education level, while 40.6% were identified as housewives. Additionally, a significant percentage of participants, approximately 62.5%, reported a history of hypoglycemia. Table 1 shows the characteristics of respondents.
Table 1. Characteristics of respondents
1- Problem Analysis
The author conducted an analysis of the issues that require attention and the objectives to be achieved through health education activities. Problem analysis served as the initial and crucial step in program planning and development. One notable gap in this context was that individuals with DM often attempted to reduce blood sugar levels using antidiabetic medication without being fully aware of the potential side effects, such as hypoglycemia.
The author conducted an interview with the person in charge of the non-communicable disease (NCD) program at the Jambi City health office. According to the NCD Coordinator, there was no specific program for DM as it falls under the category of non-communicable diseases. DM case identification was primarily conducted through screening procedures. Social media platforms such as Instagram were utilized, and all activities were integrated into the city Health Office website. There was no designated platform specifically catering to DM patients for obtaining information about their condition. The activities at the city Health Office predominantly revolved around non-communicable diseases. More specific initiatives were carried out at the public health center (PHC) level, serving as the technical implementer for the non-communicable disease prevention and control program.
To analyze the issues and assess the role of health services in providing health education to DM patients, an interview was conducted with the Head of PHC Simpang Empat Sipin. According to the interviewee, the management of diabetes mellitus primarily took place in the general clinic and elderly clinic, as a significant proportion of DM patients belong to the elderly demographic. Health workers at the PHC were unable to directly identify instances of hypoglycemia among individuals with DM. Typically, patients themselves conveyed information regarding hypoglycemic episodes after experiencing them at home.
Health services and education for DM patients were typically provided during the Elderly Program (Prolanis) activities in the form of counseling. Additionally, there was a collaboration with a private clinical laboratory (Prodia) for HbA1c testing and light exercise sessions for DM patients. However, there was no specific platform employed as a dedicated source of information for DM patients at PHC Simpang IV Sipin. The PHC Simpang IV Sipin operated Instagram and Facebook accounts, where they showcased implemented activities and those scheduled for the future.
The author identified the challenges faced by individuals with DM in preventing the recurrence of hypoglycemia. The initial survey results were based on five individuals with T2DM who had experienced hypoglycemia.
Some studies have highlighted that educating patients about the early symptoms of hypoglycemia served as the main strategy in controlling its occurrence. Health education played a crucial role in enhancing knowledge and understanding of hypoglycemia, including its recognition, interpretation of early symptoms, and decision-making regarding interventions, whether independently or with the assistance of others. Based on information gathered from five individuals with DM, it was discovered that all participants had previously experienced hypoglycemia. This history instilled concerns about the likelihood of recurrence, prompting them to pay closer attention to their health maintenance efforts. Due to the lack of glucometers among most respondents, they were unable to confirm a weakened physical state as an indication of reduced blood sugar levels. Consequently, they tend to consume sugary drinks as a habit when experiencing weakness and fatigue. All participants possessed smartphones, considering them as readily available communication tools that enabled easy access to information. This foundation presented an opportunity for patients to access applications tailored, specifically for DM patients, particularly aiding in recognizing hypoglycemia. Enhanced knowledge about DM and hypoglycemia, coupled with improved skills in utilizing applications to monitor hypoglycemic status, empowered DM patients to proactively prevent hypoglycemic episodes. In the future, this heightened awareness could enable early identification of hypoglycemia, allowing family members to promptly provide initial management at home.
2- Design and Construction
The design and development represented the embodiment of the conceptual framework stemming from the conducted problem analysis. This was manifested through the creation of a prototype for a health promotion model, aiming to enhance the self-detection of transmission risks among close contacts of tuberculosis patients. The device was meticulously designed and constructed, incorporating information technology that leveraged computer hardware and software resources, alongside the availability of an Internet network.
The design of the prototype should primarily emphasize message design, which entails careful consideration of aspects, such as word and language selection, visual design, and audio design. The entire construction of the message design was delineated in the storyboard, which served the crucial role of ensuring effective and efficient communication of each message component. Moreover, the storyboard facilitated the establishment of a well-defined interaction design.
3- Prototype Development
The prototype development stage materialized in the form of hypoglycemia prevention applications designed for DM patients. The website can be accessed through https://deteksihipoglikemia.com after completing the initial registration process. The prototype development proceeded through an evaluation or validation process conducted by experts or practitioners.
4- Expert Validation
The material validation instrument contained seven questions related to the content of hypoglycemic prevention material in DM patients.
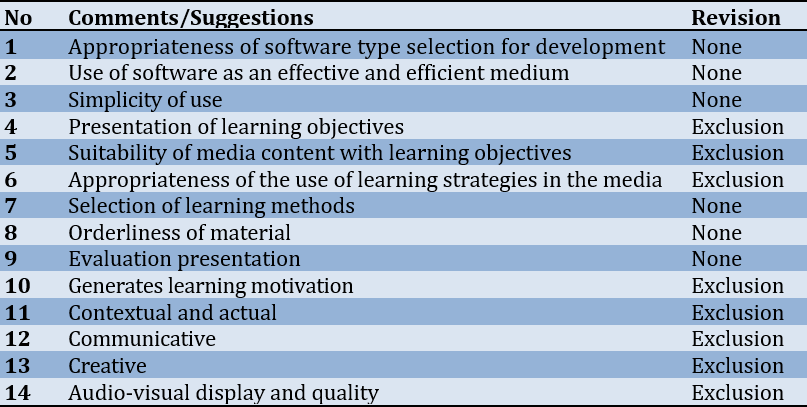
Table 2. Comments/suggestions on product validity by practitioner validators
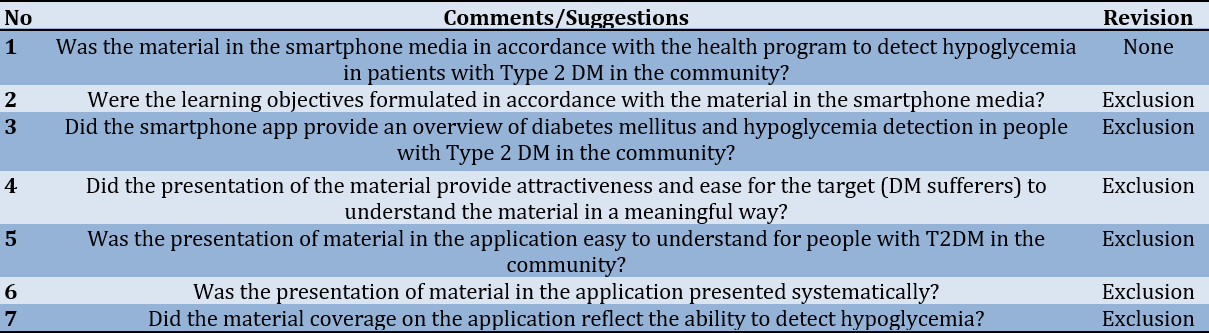
The results of material validation, conducted by expert validators of the health promotion material, indicated the necessity for several revisions in the academic paper. These revisions were essential to ensure that the content aligned with the material elements and was compatible with the ongoing prototype development. The expert validators had recommended the creation of an application user manual that offered a comprehensive explanation of the application/media's development process. Ultimately, the expert validators concluded that the educational media for preventing hypoglycemia in individuals with DM was viable for further trials, provided that the suggested revisions were incorporated.
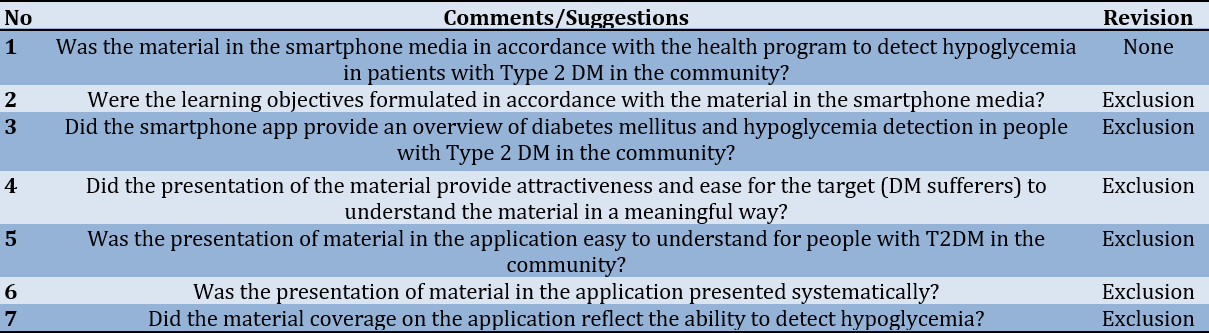
Table 3. Comments/suggestions on product validity by media expert validators
The results of material validation by multimedia expert validators suggested that the NEDTA was suitable for use by individuals with DM. The expert validators had recommended improvements in several areas. The conclusion drawn by the media expert validator was that the educational media for preventing hypoglycemia in patients with DM was considered feasible for a trial, provided that the suggested revisions were implemented.
5- Implementation and Evaluation Results (Field Trial)
Field trials were conducted on 35 respondents, all of whom were introduced to the application following the updated application instructions. The testing objective centered around evaluating the application's impact and effectiveness within the community.
The average patient's ability to prevent hypoglycemia was 45.13±4.02. After the intervention, the patient's ability increased by 3.21 to 48.34±4.04 (paired t-test p-value=0.0001), signifying a significant difference in the ability to detect hypoglycemia before and after the intervention.
Discussion
The present study aimed to develop a smartphone application-based DM therapy education model to enhance the ability to detect hypoglycemia in T2DM patients. The fundamental theories employed in this study for improving hypoglycemia detection among patients with T2DM include the HBM and social cognitive theory. The results indicated a significant difference in the ability to detect hypoglycemia before and after the intervention.
The HBM served as a conceptual framework used to assess health behaviors and understand the rationales behind compliance or non-compliance with recommended health management strategies. The HBM posits that individuals were likely to respond positively to health-related measures when they perceived the risk (perceived susceptibility), understood the severity of the risk (perceived severity), and recognized the potential benefits of behavioral changes (perceived benefit) [21]. They could remove barriers to health behavior (perceived barriers). On the other hand, self-efficacy refers to the belief in the ability to act, improve one's health behaviors, and withdraw behaviors that were detrimental to health [22]. The study conducted by Megawati et al. [23] on the impact of educational interventions based on the HBM in promoting self-care behavior among patients with T2DM, revealed an increase in the average values of vulnerability, severity, benefits, obstacles, self-efficacy, and attitudes. Notably, self-care showed a significant improvement [23-27].
Perceived susceptibility refers to an individual's belief regarding their vulnerability to a health condition, thereby motivating them to adopt healthier behaviors. On the other hand, perceived severity encompassed an individual's understanding of the gravity of the illness they might face. Furthermore, perceived severity could stem from an individual's perception of the severity of a particular ailment and its potential impact on their life [28, 29].
Perceived benefits exhibited a significant positive correlation with patient adherence to the correct insulin usage. The greater the patients' awareness of the benefits associated with adopting healthy behaviors, the more likely they were to adhere to using insulin at the appropriate time, place, and dosage.
Mobile apps were highly sought-after to facilitate the self-management of health, owing to their accessibility, portability, affordability, ease of use, and extensive reach. Statistics showed that at least 50% of smartphone users had employed one or more mobile health apps [30]. The incorporation of mobile health technology in diabetes education represented an innovative approach to learning that held the potential to actively involve patients and encourage positive health behaviors. Leveraging technology for the management of DM could enhance communication between nurses and patients, leading to effective information exchange and improving the quality of life for those affected [31, 32]. An important goal of treatment utilizing information technology is to maintain effective nurse-patient learning without interruption [32, 33].
The NEDTA offered individuals with T2DM the opportunity to engage in independent learning. Accessible on both IOS and Android platforms via a touchscreen interface, the user-friendly app incorporates engaging multimedia elements, such as images and videos, facilitating an immersive learning experience. Through problem-based learning and case studies, the app fostered critical thinking skills among users. Moreover, the app served as a tool for the general public to raise awareness, prevent, and manage early instances of hypoglycemia. Notably, despite extensive exploration in previous research, no similar applications had been identified by researchers [2, 34].
The limited number of samples served as a limitation in this study. Consequently, for future studies, it was imperative to assess the effectiveness of the next stage through randomized controlled trials (RCTs) involving a larger sample size.
Conclusion
Implementing the NEDTA diabetes education model relying on smartphone applications is effective in enhancing the ability to detect hypoglycemia in patients with T2DM.
Acknowledgments: We express our deepest gratitude to the director of Health Polytechnic of Jambi Indonesia for supporting this research.
Ethical Permissions: This study was approved by the Health Research Ethics Commission of the Ministry of Health, Jambi (LB.02.06/2/26/2023).
Conflicts of Interests: The authors report no conflict of interest.
Authors’ Contribution: Damayantie N (First Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Ernawati (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Dewi M (Third Author), Assistant Researcher/Statistical Analyst/Discussion Writer (25%); Fahmi I (Fourth Author), Introduction Writer/Methodologist/Discussion Writer (25%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
In addition to managing blood sugar levels, the treatment also emphasized strategies for reducing multifactorial risks [1, 2]. The global prevalence of diabetes mellitus has reached 424.9 million people, with an estimated projection to increase to 628.6 million people by 2045. Approximately ninety percent (90%) of diabetes cases are classified as type 2 diabetes mellitus (T2DM), characterized by impaired insulin sensitivity and secretion [3].
Indonesia is ranked sixth globally in terms of the number of people with diabetes mellitus, currently at 10.3 million people, and this number is projected to rise to 16.7 million by 2045 [4]. The use of insulin or oral hypoglycemic agents in diabetes mellitus therapy often leads to hypoglycemic effects. This can be caused by inadequate insulin administration, excessive dosing, or the failure of counterregulatory mechanisms due to the long-standing diabetes mellitus disease process. To date, approximately 90% of diabetic patients receiving insulin therapy have experienced episodes of hypoglycemia [5].
The prevention of hypoglycemia involves improving blood glucose control and early detection, which includes educating individuals about the signs and symptoms of hypoglycemia, interim treatments, and other essential measures [6, 7]. Assessment of knowledge regarding self-monitoring of blood sugar can be conducted after specific training. Understanding hypoglycemia is crucial for recognizing its symptoms, interpreting early signs, and making informed decisions independently or with assistance. Knowledge of T2DM management and hypoglycemia symptoms positively impacts patients' self-awareness in detecting hypoglycemia [8, 9].
The continuous advancement of science and technology has encouraged new efforts in utilizing technological advancements within the learning process [10]. The emergence of new technologies has broadened the scope of specialist nurses, facilitating efficient and sustainable technology-based nursing practices. This involves identifying suitable technologies and application systems in accordance with the nursing plan and the condition of the DM patient [11, 12]. Multimedia refers to the presentation of material using text and images. Learners can achieve a better understanding when information is presented with both text and images compared to presentations using text alone [13]. The multimedia cognitive theory assumes that the human data processing system comprises multiple channels for visual and auditory processing. Each channel has a limited processing capacity, and active education entails the coordinated execution of a series of cognitive processes during learning [14].
Numerous studies have explored the use of smartphones as educational tools for managing diabetes mellitus and improving the quality of life. According to research by Bonoto, smartphone applications have shown promise in enhancing HbA1c control for patients with type 1 and 2 Diabetes Mellitus. These applications typically incorporate features such as storage and feedback for blood glucose data, dietary guidance, physical exercise tracking, dosage management, medication adherence, and access to healthcare professionals to facilitate better glycemic control. The findings also indicated that patients gained confidence in managing their diabetes, leading to an improved quality of life and a reduced fear of encountering potential hypoglycemic episodes [15, 16].
The diabetes education model was scientifically developed as a structured learning design presented in an academic text. It encompasses various development stages, including model conceptualization, product development, and field testing. Creating a diabetes education model involves analyzing the problem, context, and existing literature, followed by outlining and designing an initial prototype. This smartphone application is known as NEDTA (Nursing Education Diabetic Therapeutic Application).
The NEDTA enables individuals with T2DM to engage in independent learning through a user-friendly interface accessible on both IOS and Android platforms. The app's simple navigation allows for anytime usage, and its incorporation of images and videos enhances user engagement. Through problem-based learning and case studies, the app fosters critical thinking skills among its users. Additionally, the general public can utilize the app to raise awareness and prevent and manage early-stage hypoglycemia. Despite extensive exploration in previous research, researchers have not identified any similar applications.
This research holds significant importance as the development of a diabetes education model for T2DM patients could empower them to independently manage their health. Moreover, this study strongly aligns with the policies and initiatives of the Indonesian government, aiming to prevent and control diabetes by fostering community empowerment through the Non-Communicable Disease Prevention and Control Program. Leveraging smartphones as educational tools enables individuals to use information technology for the enhancement and maintenance of their health, underscoring the crucial significance of this research. The primary objective of this study was to develop a therapeutic education model for diabetes mellitus, focusing on enhancing the ability of T2DM patients to detect hypoglycemia.
Materials and Methods
Research Design
This research adopted a design and development approach, utilizing mixed methods [17]. The development stage primarily emphasized the qualitative aspects, focusing on the conceptual model, while the product development and trial stages incorporated a blend of qualitative and quantitative elements. During the trial stage, the quantitative aspect took precedence. The product design and development process followed the ADDIE framework across all stages [18], including analysis, design, development, implementation, and evaluation for the main stage, while the design stage of the intervention product used the dick and colleagues intervention design model [19]. The media for diabetes education, aimed at enhancing the ability to detect hypoglycemia in T2DM patients, was founded on the health belief model (HBM), encompassing perceived vulnerability, perceived severity, and perceived benefits. Additionally, the social cognitive theory was integrated, considering behavioral, personal, cognitive, and environmental factors. The development stages of the diabetes education model for improving hypoglycemia detection in T2DM patients were aligned with behavior change theory.
During its model development, diabetes education entailed analyzing the problem, context, and literature, followed by the outline and design of an initial prototype. The smartphone application was named NEDTA (Nursing Education Diabetic Therapeutic Application).
This prototype was a smartphone-based educational medium equipped with health education features focusing on diabetes mellitus, hypoglycemia identification, and initial hypoglycemia management. The intervention model underwent field testing through a quasi-experimental design, employing a two-group pre-test and post-test design with a control group.
Participants
This study involved 64 individuals with DM and was conducted between May and September 2023. The participants were randomly selected and met the inclusion criteria of having and currently experiencing DM, as well as possessing and being capable of using an Android cellphone.
Sample Size
A total of 64 students were calculated using Slovin's formula at α=0.05, and the total population was considered to be 75 people. According to Imas Masturoh and Nauri Anggita [20], the sample size was calculated using the Taro Yamane formula as follows:
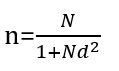
n=number of samples
N=statistical population
d=precision
Data Collection and Instrument
The authors independently compiled the questionnaire, which has been validated and deemed feasible. The questionnaire comprised 20 positive and negative statements, with answer options, including 'often,' 'sometimes,' and 'never'.
Statistical Analisis
In component 1 (analysis), qualitative data were obtained during the initial observation activities, precisely at the needs analysis stage. The subsequent analysis stage was constructed from the bottom up, also known as inductive analysis. Univariate analysis was performed on the quantitative data to determine the percentage or magnitude of the problem or indicators under scrutiny. The quantitative data, collected from individuals with DM during the needs analysis stage, were then subjected to descriptive statistical analysis. This process involved narration and interpretation to underscore its urgency for the practical resolution of the identified issues.
In the prototype development component, expert validation was presented qualitatively. During the field test, the data were presented descriptively, accompanied by the frequency distribution. Data were analyzed using descriptive analysis and inferential statistics. Numerical data were presented as mean, median, standard deviation, minimum, and maximum. The paired t-test was then utilized to assess the impact of product usage.
Findings
The majority of respondents were female, accounting for 71.9% of the total. Furthermore, 43.8% of participants had attained a high school education level, while 40.6% were identified as housewives. Additionally, a significant percentage of participants, approximately 62.5%, reported a history of hypoglycemia. Table 1 shows the characteristics of respondents.
Table 1. Characteristics of respondents
1- Problem Analysis
The author conducted an analysis of the issues that require attention and the objectives to be achieved through health education activities. Problem analysis served as the initial and crucial step in program planning and development. One notable gap in this context was that individuals with DM often attempted to reduce blood sugar levels using antidiabetic medication without being fully aware of the potential side effects, such as hypoglycemia.
The author conducted an interview with the person in charge of the non-communicable disease (NCD) program at the Jambi City health office. According to the NCD Coordinator, there was no specific program for DM as it falls under the category of non-communicable diseases. DM case identification was primarily conducted through screening procedures. Social media platforms such as Instagram were utilized, and all activities were integrated into the city Health Office website. There was no designated platform specifically catering to DM patients for obtaining information about their condition. The activities at the city Health Office predominantly revolved around non-communicable diseases. More specific initiatives were carried out at the public health center (PHC) level, serving as the technical implementer for the non-communicable disease prevention and control program.
To analyze the issues and assess the role of health services in providing health education to DM patients, an interview was conducted with the Head of PHC Simpang Empat Sipin. According to the interviewee, the management of diabetes mellitus primarily took place in the general clinic and elderly clinic, as a significant proportion of DM patients belong to the elderly demographic. Health workers at the PHC were unable to directly identify instances of hypoglycemia among individuals with DM. Typically, patients themselves conveyed information regarding hypoglycemic episodes after experiencing them at home.
Health services and education for DM patients were typically provided during the Elderly Program (Prolanis) activities in the form of counseling. Additionally, there was a collaboration with a private clinical laboratory (Prodia) for HbA1c testing and light exercise sessions for DM patients. However, there was no specific platform employed as a dedicated source of information for DM patients at PHC Simpang IV Sipin. The PHC Simpang IV Sipin operated Instagram and Facebook accounts, where they showcased implemented activities and those scheduled for the future.
The author identified the challenges faced by individuals with DM in preventing the recurrence of hypoglycemia. The initial survey results were based on five individuals with T2DM who had experienced hypoglycemia.
Some studies have highlighted that educating patients about the early symptoms of hypoglycemia served as the main strategy in controlling its occurrence. Health education played a crucial role in enhancing knowledge and understanding of hypoglycemia, including its recognition, interpretation of early symptoms, and decision-making regarding interventions, whether independently or with the assistance of others. Based on information gathered from five individuals with DM, it was discovered that all participants had previously experienced hypoglycemia. This history instilled concerns about the likelihood of recurrence, prompting them to pay closer attention to their health maintenance efforts. Due to the lack of glucometers among most respondents, they were unable to confirm a weakened physical state as an indication of reduced blood sugar levels. Consequently, they tend to consume sugary drinks as a habit when experiencing weakness and fatigue. All participants possessed smartphones, considering them as readily available communication tools that enabled easy access to information. This foundation presented an opportunity for patients to access applications tailored, specifically for DM patients, particularly aiding in recognizing hypoglycemia. Enhanced knowledge about DM and hypoglycemia, coupled with improved skills in utilizing applications to monitor hypoglycemic status, empowered DM patients to proactively prevent hypoglycemic episodes. In the future, this heightened awareness could enable early identification of hypoglycemia, allowing family members to promptly provide initial management at home.
2- Design and Construction
The design and development represented the embodiment of the conceptual framework stemming from the conducted problem analysis. This was manifested through the creation of a prototype for a health promotion model, aiming to enhance the self-detection of transmission risks among close contacts of tuberculosis patients. The device was meticulously designed and constructed, incorporating information technology that leveraged computer hardware and software resources, alongside the availability of an Internet network.
The design of the prototype should primarily emphasize message design, which entails careful consideration of aspects, such as word and language selection, visual design, and audio design. The entire construction of the message design was delineated in the storyboard, which served the crucial role of ensuring effective and efficient communication of each message component. Moreover, the storyboard facilitated the establishment of a well-defined interaction design.
3- Prototype Development
The prototype development stage materialized in the form of hypoglycemia prevention applications designed for DM patients. The website can be accessed through https://deteksihipoglikemia.com after completing the initial registration process. The prototype development proceeded through an evaluation or validation process conducted by experts or practitioners.
4- Expert Validation
The material validation instrument contained seven questions related to the content of hypoglycemic prevention material in DM patients.
Table 2. Comments/suggestions on product validity by practitioner validators
The results of material validation, conducted by expert validators of the health promotion material, indicated the necessity for several revisions in the academic paper. These revisions were essential to ensure that the content aligned with the material elements and was compatible with the ongoing prototype development. The expert validators had recommended the creation of an application user manual that offered a comprehensive explanation of the application/media's development process. Ultimately, the expert validators concluded that the educational media for preventing hypoglycemia in individuals with DM was viable for further trials, provided that the suggested revisions were incorporated.
Table 3. Comments/suggestions on product validity by media expert validators
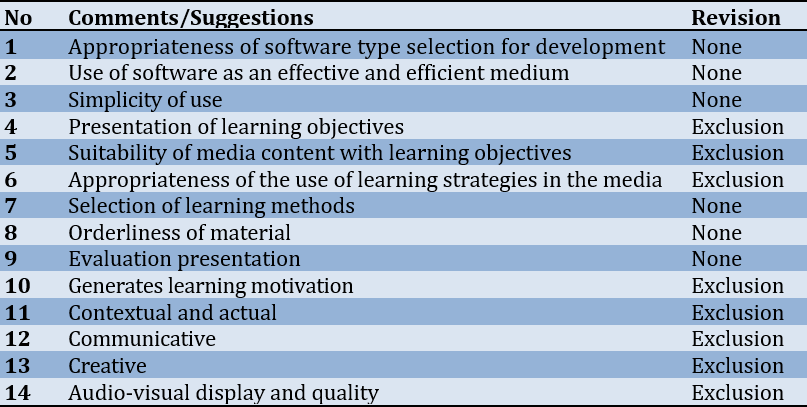
The results of material validation by multimedia expert validators suggested that the NEDTA was suitable for use by individuals with DM. The expert validators had recommended improvements in several areas. The conclusion drawn by the media expert validator was that the educational media for preventing hypoglycemia in patients with DM was considered feasible for a trial, provided that the suggested revisions were implemented.
5- Implementation and Evaluation Results (Field Trial)
Field trials were conducted on 35 respondents, all of whom were introduced to the application following the updated application instructions. The testing objective centered around evaluating the application's impact and effectiveness within the community.
The average patient's ability to prevent hypoglycemia was 45.13±4.02. After the intervention, the patient's ability increased by 3.21 to 48.34±4.04 (paired t-test p-value=0.0001), signifying a significant difference in the ability to detect hypoglycemia before and after the intervention.
Discussion
The present study aimed to develop a smartphone application-based DM therapy education model to enhance the ability to detect hypoglycemia in T2DM patients. The fundamental theories employed in this study for improving hypoglycemia detection among patients with T2DM include the HBM and social cognitive theory. The results indicated a significant difference in the ability to detect hypoglycemia before and after the intervention.
The HBM served as a conceptual framework used to assess health behaviors and understand the rationales behind compliance or non-compliance with recommended health management strategies. The HBM posits that individuals were likely to respond positively to health-related measures when they perceived the risk (perceived susceptibility), understood the severity of the risk (perceived severity), and recognized the potential benefits of behavioral changes (perceived benefit) [21]. They could remove barriers to health behavior (perceived barriers). On the other hand, self-efficacy refers to the belief in the ability to act, improve one's health behaviors, and withdraw behaviors that were detrimental to health [22]. The study conducted by Megawati et al. [23] on the impact of educational interventions based on the HBM in promoting self-care behavior among patients with T2DM, revealed an increase in the average values of vulnerability, severity, benefits, obstacles, self-efficacy, and attitudes. Notably, self-care showed a significant improvement [23-27].
Perceived susceptibility refers to an individual's belief regarding their vulnerability to a health condition, thereby motivating them to adopt healthier behaviors. On the other hand, perceived severity encompassed an individual's understanding of the gravity of the illness they might face. Furthermore, perceived severity could stem from an individual's perception of the severity of a particular ailment and its potential impact on their life [28, 29].
Perceived benefits exhibited a significant positive correlation with patient adherence to the correct insulin usage. The greater the patients' awareness of the benefits associated with adopting healthy behaviors, the more likely they were to adhere to using insulin at the appropriate time, place, and dosage.
Mobile apps were highly sought-after to facilitate the self-management of health, owing to their accessibility, portability, affordability, ease of use, and extensive reach. Statistics showed that at least 50% of smartphone users had employed one or more mobile health apps [30]. The incorporation of mobile health technology in diabetes education represented an innovative approach to learning that held the potential to actively involve patients and encourage positive health behaviors. Leveraging technology for the management of DM could enhance communication between nurses and patients, leading to effective information exchange and improving the quality of life for those affected [31, 32]. An important goal of treatment utilizing information technology is to maintain effective nurse-patient learning without interruption [32, 33].
The NEDTA offered individuals with T2DM the opportunity to engage in independent learning. Accessible on both IOS and Android platforms via a touchscreen interface, the user-friendly app incorporates engaging multimedia elements, such as images and videos, facilitating an immersive learning experience. Through problem-based learning and case studies, the app fostered critical thinking skills among users. Moreover, the app served as a tool for the general public to raise awareness, prevent, and manage early instances of hypoglycemia. Notably, despite extensive exploration in previous research, no similar applications had been identified by researchers [2, 34].
The limited number of samples served as a limitation in this study. Consequently, for future studies, it was imperative to assess the effectiveness of the next stage through randomized controlled trials (RCTs) involving a larger sample size.
Conclusion
Implementing the NEDTA diabetes education model relying on smartphone applications is effective in enhancing the ability to detect hypoglycemia in patients with T2DM.
Acknowledgments: We express our deepest gratitude to the director of Health Polytechnic of Jambi Indonesia for supporting this research.
Ethical Permissions: This study was approved by the Health Research Ethics Commission of the Ministry of Health, Jambi (LB.02.06/2/26/2023).
Conflicts of Interests: The authors report no conflict of interest.
Authors’ Contribution: Damayantie N (First Author), Introduction Writer/Main Researcher/Discussion Writer (25%); Ernawati (Second Author), Methodologist/Assistant Researcher/Statistical Analyst (25%); Dewi M (Third Author), Assistant Researcher/Statistical Analyst/Discussion Writer (25%); Fahmi I (Fourth Author), Introduction Writer/Methodologist/Discussion Writer (25%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Article Type: Original Research |
Subject:
Technology of Health Education
Received: 2023/10/26 | Accepted: 2023/11/11 | Published: 2024/01/5
Received: 2023/10/26 | Accepted: 2023/11/11 | Published: 2024/01/5
References
1. Arbiter B, Look H, McComb L, Snider C. Why download data: the benefits and challenges of more diabetes data. Diabetes Spectr. 2019;32(3):221-5. [Link] [DOI:10.2337/ds18-0099]
2. Bellfield EJ, Sharp LK, Xia Y, Gerber BS. Use of a mobile app to facilitate blood glucose monitoring in adolescents with type 1 diabetes: single-subject nonrandomized clinical trial. JMIR Diabetes. 2018;3(1):e3. [Link] [DOI:10.2196/diabetes.8357]
3. Simmons K, Riddley S. Diabetes and technology. Prim Care: Clin Office Pract. 2022;49(2):327-37. [Link] [DOI:10.1016/j.pop.2021.11.005]
4. Kemenkes RI. Hasil utama RISKESDAS 2018 [Internet]. Ministry of Health Health Research and Development Agency. Jakarta: Kemenkes RI; 2018- [cited 2022 June 20]. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf. [Indonesian] [Link]
5. Hariton A, Nita L, Cretu M. A web application for blood glucose monitoring using the iPhone advantages. 2012 International Conference and Exposition on Electrical and Power Engineering; 2012 Oct 25-27; New York :IEEE; 2012. pp. 505-8. [Link] [DOI:10.1109/ICEPE.2012.6463883]
6. Izahar S, Lean QY, Hameed MA, Murugiah MK, Patel RP, Al-Worafi YM, et al. Content analysis of mobile health applications on diabetes mellitus. Front Endocrinol. 2017;8:318. [Link] [DOI:10.3389/fendo.2017.00318]
7. Joaheer R, Nagowah SD. A big data framework for diabetes in Mauritius. 2017 International Conference on Infocom Technologies and Unmanned Systems (Trends and Future Directions; ICTUS); 2017 Dec 18-20; New York; IEEE; 2017. pp. 126-32. [Link] [DOI:10.1109/ICTUS.2017.8285991]
8. Grifantini K. Advances in management technology for diabetes: From personal reminders to digital doctors. IEEE Pulse. 2014;5(3):40-4. [Link] [DOI:10.1109/MPUL.2014.2309579]
9. Eng DS, Lee JM. The promise and peril of mobile health applications for diabetes and endocrinology. Pediatr Diabetes. 2013;14(4):231-8. [Link] [DOI:10.1111/pedi.12034]
10. Morrison C. Digital health and care institutes: Scottish diabetes policy and market report. Glasgow: University of Strathclyde; 2019. [Link]
11. Weinstock RS, Aleppo G, Bailey TS, Bergenstal RM, Fisher WA, Greenwood DA, et al. The role of blood glucose monitoring in diabetes management. Virginia: American Diabetes Association; 2020. [Link] [DOI:10.2337/db2020-31]
12. Yoo JH, Kim JH. Advances in continuous glucose monitoring and integrated devices for management of diabetes with insulin-based therapy: Improvement in glycemic control. Diabetes Metab J. 2023;47(1):27-41. [Link] [DOI:10.4093/dmj.2022.0271]
13. Salber P, Niksch A. Digital health tools for diabetes. J Ambul Care Manag. 2015;38(2):196-9. [Link] [DOI:10.1097/JAC.0000000000000080]
14. Stanger C, Kowatsch T, Xie H, Nahum-Shani I, Lim-Liberty F, Anderson M, et al. A digital health intervention (SweetGoals) for young adults with type 1 diabetes: Protocol for a factorial randomized trial. JMIR Res Protoc. 2021;10(2):e27109. [Link] [DOI:10.2196/27109]
15. Vashist SK, Luong JHT, Vashist SK. Point-of-care technologies enabling next-generation healthcare monitoring and management. Springer: New York; 2019. pp.117-32. [Link] [DOI:10.1007/978-3-030-11416-9_4]
16. Wang W, Seah B, Jiang Y, Lopez V, Tan C, Lim ST, et al. A randomized controlled trial on a nurse‐led smartphone‐based self‐management programme for people with poorly controlled type 2 diabetes: A study protocol. J Adv Nurs. 2018;74(1):190-200. [Link] [DOI:10.1111/jan.13394]
17. Creswell JW. Steps in conducting a scholarly mixed methods study. Lincoln: University of Nebraska; 2013. [Link]
18. Rusdi M. Educational treatment-based research. Jakarta: Rajawali Pers; 2020. [Indonesian] [Link]
19. Dick W, Carey L, Carey JO. The systematic design of instruction. 8th ed. London: Pearson; 2015. [Link]
20. Imas Masturoh SKM, Nauri Anggita T. Health Research Methodology. Jakarta: Rineka Cipta: Kementerian Kesehatan Republik Indonesia; 2018. [Indonesian] [Link]
21. Yudianti I, Nurhayati R. Health Belief Model (HBM) and Delay in Referral of Gynecological Cases. Matern Neonatal Health J. 2018;18-24. [Indonesian] [Link]
22. Crossen SS, Romero CC, Lewis C, Glaser NS. Remote glucose monitoring is feasible for patients and providers using a commercially available population health platform. Front Endocrinol. 2023;14:1063290. [Link] [DOI:10.3389/fendo.2023.1063290]
23. Megawaty I, Syahrul S. Educational interventions in diabetics with the use of health belief models: Literature review. Indonesian Contemporary Nurs J. 2019:4(1);1-10. [Link] [DOI:10.20956/icon.v4i1.5038]
24. Nurhidayati I, Suciana F, Zulcharim I. The relationship between health beliefs and medication adherence in people with Type 2 Diabetes Mellitus. JIlmu Community Nursing. 2019;2(2):27-34. [Indonesian] [Link] [DOI:10.32584/jikk.v2i2.412]
25. Muhlisa M, Amira BSA. Medication Compliance for Diabetes Mellitus Patients Based on the Health Belief Model (HBM) Theory at the Diabetes Center in Ternate City in 2017. Interest: Journal of Health Sciences. 2018;7(2):144-9. [Indonesian] [Link] [DOI:10.37341/interest.v7i2.23]
26. Marsim E, Prisma FA, Prianggi H. Meta analysis: Application of health belief model on the tertiary prevention of type 2 diabetes mellitus. J Health Promot Behav. 2021;6(4):284-97. [Link] [DOI:10.26911/thejhpb.2021.06.04.03]
27. Fitriani Y, Pristianty L, Hermansyah A. Health Belief Model (HBM) Approach to Analyze Compliance of Type 2 Diabetes Mellitus Patients in Using Insulin. J Farmasi Indonesia. 2019;16(2):167-77. [Indonesian] [Link] [DOI:10.30595/pharmacy.v16i2.5427]
28. Sukma FJ, Hidayati IR, Pristianty L. Behavioral factor analysis of the accuracy in using gastritis drugs at the Puskesmas Arjuno in Malang City with the Health Belief Model (HBM) approach. Farmasains: Jurnal Farmasi dan Ilmu Kesehatan. 2021;6(1):15-9. [Link]
29. Puspita RC, Tamtomo D, Indarto D. Health belief model for the analysis of factors affecting hypertension preventive behavior among adolescents in Surakarta. J Health Promot Behav. 2017;2(2):183-96. [Link] [DOI:10.26911/thejhpb.2017.02.02.08]
30. Böhm AK, Jensen ML, Sørensen MR, Stargardt T. Real-world evidence of user engagement with mobile health for diabetes management: Longitudinal observational study. JMIR Mhealth Uhealth. 2020;8(11):e22212. [Link] [DOI:10.2196/22212]
31. Cui L, Schroeder PR, Sack PA. Inpatient and outpatient technologies to assist in the management of insulin dosing. Clin Diabetes. 2020;38(5):462-73. [Link] [DOI:10.2337/cd20-0054]
32. Doyle-Delgado K, Chamberlain JJ. Use of diabetes-related applications and digital health tools by people with diabetes and their health care providers. Clin Diabetes. 2020;38(5):449-61. [Link] [DOI:10.2337/cd20-0046]
33. Clements M, Kaufman N, Mel E. Using digital health technology to prevent and treat disease. Diabetes Technol Ther. 2022;24(S1):S76-95. [Link] [DOI:10.1089/dia.2022.2505]
34. Bello GJ. Mobile Application For Diabetes Monitoring And Management. Murfreesboro: Dean College of Basic and Applied Science Location; 2019. [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |