Volume 12, Issue 1 (2024)
Health Educ Health Promot 2024, 12(1): 37-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fahri S, Suhermanto S. Enhancing Student Knowledge in Dengue Hemorrhagic Fever Control Through Educational Modeling. Health Educ Health Promot 2024; 12 (1) :37-42
URL: http://hehp.modares.ac.ir/article-5-72065-en.html
URL: http://hehp.modares.ac.ir/article-5-72065-en.html
1- Environmental Health Department, Health Polytechnic of Jambi, Jambi, Indonesia
Full-Text [PDF 578 kb]
(3195 Downloads)
| Abstract (HTML) (1721 Views)
Full-Text: (452 Views)
Introduction
Dengue hemorrhagic fever (DHF) results from an infection with the dengue virus, transmitted by the Aedes aegypti mosquito [1, 2]. Indonesia, due to its enduring prevalence in many regions, continues to grapple with the commonality of DHF. This mosquito-borne disease is endemic in numerous countries across Southeast and South Asia, the Pacific, and Latin America. Its hallmark characteristics include heightened vascular permeability, hypovolemia, and compromised clotting mechanisms. While primarily impacting children, adults are also vulnerable to its effects [3, 4].
In areas where dengue is endemic, significant outbreaks are often marked by an upsurge in cases. According to data provided by the Jambi Provincial Health Office, the incidence of dengue fever in 2018 was 831 cases per 100,000 people, which escalated to 2229 cases in 2019. Jambi City recorded the highest number of cases, with 668 individuals affected [5].
Epidemiological investigations involve the continual and systematic observation of disease patterns in a population, aiming to comprehend the history of the disease and gather foundational data for effective disease control and management [6, 7]. This includes identifying the prevalent Aedes spp. in a particular area or region. Aedes spp. mosquitoes serve as carriers of dengue fever. Various factors contribute to the spread and transmission of the disease, such as the burgeoning urban population, suboptimal awareness and knowledge regarding disease prevention, inadequate sanitation practices, compromised water supplies, and improper waste disposal [8, 9].
During increased rainfall in Jambi City, the management of DHF is primarily focused on eliminating mosquito breeding sites. This is achieved through the implementation of eradication of mosquito nests (EMN) and the 3M approach, which encompasses draining (and scrubbing) of containers, such as bathtubs and toilets, sealing off household water reservoirs, like crocks and drums, and disposal or destruction of discarded items, including garbage cans and tires [10, 11]. Regular landfill drainage, conducted at least once a week, is essential to prevent mosquito breeding in these areas. Additionally, the adoption of the extended 3M plus approach is gaining traction, contributing to an improved larval-free rate in community containers and households [12, 13].
Environmental management practices play a pivotal role in DHF control, emphasizing the maintenance of suitable humidity levels within homes and neighborhoods. This entails proper room ventilation, organized spaces, and the avoidance of storing items in dark and damp locations, which can serve as potential resting spots for Aedes aegypti mosquitoes [14-16].
Effective Aedes aegypti mosquito eradication relies on periodic larval inspections (PJB) performed by health center personnel and the routine calculation of the Breteau Index (ABf) on a monthly basis. Fidayanto, Susanto, Yohanan, and Yudhastuti's Dengue Fever Control Model serves as an indicator for detecting the presence of mosquito larvae in containers or households. When the larval-free rate is low, this signals an increased presence of larvae, necessitating vigorous vector control measures to curb the transmission of dengue disease [17-19].
Vector control, a pivotal strategy in managing diseases transmitted by disease vectors, like the Aedes aegypti mosquito, incorporates biological control methods. For instance, the use of natural predators, such as certain species of Copepoda or Cyclops, has demonstrated effectiveness in controlling DHF vectors [20]. Notably, the utilization of Mesocyclops aspericornis has shown promise in various research trials conducted in Vietnam, Tahiti, and at the Vector and Reservoir Research Center in Salatiga [21].
Chemical control, utilizing insecticides for Aedes aegypti eradication, encompasses larvacidation, which targets both larval and adult stages. Temephos, commonly used as a larvicide, is formulated as sand granules. The recommended dosage is 1ppm or 10g (equivalent to 1 flat tablespoon) per 100 liters of water, with a residual effect lasting up to three months. Insect growth regulators can also be employed for this purpose [22, 23].
However, the use of insecticides in dengue vector control poses potential side effects on the environment and public health, especially when factors, such as dosage, target, timing, and coverage of vector control are not meticulously managed.
Schools, characterized by clean water reservoirs and routine eating and drinking activities, generate waste that, if improperly managed during the rainy season, can serve as breeding grounds for mosquitoes. DHF poses a significant public health challenge in Indonesia, with the number of cases showing a rising trend and the geographical spread widening. Typically, areas experiencing outbreaks of DHF initially witness a surge in the number of cases within the region. Fernandez et al. [24] suggest that urban neighborhoods with a higher-income population are at a heightened risk of dengue fever transmission.
Socialization and promotional efforts aim to engage the educational community in collaborative endeavors to combat dengue fever through improved environmental hygiene practices, ultimately leading to a reduction in the incidence of dengue fever in junior high schools. The outcomes are measured by the rate of free flies and the decreased incidence of dengue fever.
This study aimed to analyze the impact of educational interventions on the control of DHF among students in Jambi City.
Materials and Methods
Study Design
This experimental research employed a non-equivalent control group with a pretest and a posttest design [25, 26].
Participants
The study was carried out between July and October 2022, encompassing nine junior high schools in Jambi City, Indonesia. A total of 225 students who met the inclusion criteria were randomly selected to participate. The inclusion criteria comprised students in grades seven to nine, proficient in reading, and with parental consent. The researcher provided a comprehensive explanation of the study's scope to both students and parents. Upon their agreement, both parties signed a research consent certificate.
Variables and Data Collection
The dependent variable was the students' knowledge of managing DHF in Jambi City, assessed through a questionnaire comprising ten questions with binary (yes/no) answer options. The Guttman scale was utilized to assign a score ranging from 10 to 100. Scores of 60 or higher categorized students' responses as positive, while scores below 60 classified them as negative.
The independent variable was the implementation of educational strategies, including lectures, leaflet dissemination, and interactive discussions. The educational material focused on enhancing students' comprehension of DHF management through the implementation of the draining, covering, and burying (3M) approach.
Before implementing the educational intervention, a pretest involving the distribution of questionnaires to students was conducted. After completing the pretest, educational materials were presented to the students, delivered over a 30-minute duration, followed by discussions aimed at reinforcing their understanding of dengue hemorrhagic fever control. Subsequently, a posttest was administered in the form of another questionnaire addressing the management of DHF.
Sample size
A total of 225 students were calculated using Slovin's formula at α=0.05, and the total population was considered to be 515 people. According to Masturoh and Anggita [27], the sample was calculated using the Taro Yamane formula as follows:
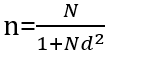
n=Number of samples
N=Number of populations
d=Precision
Statistical Analysis
The demographic data presentation involves providing a comprehensive overview by displaying the percentage distribution of variables. Additionally, numerical data is represented using mean values, standard deviation (SD), and the range of maximum and minimum values for each variable (both pre- and post-test). For data analysis, the non-parametric Wilcoxon test was employed due to the non-normal distribution of the data. This test was utilized to assess the impact of the intervention on students' behavior. All data analyses were conducted using SPSS version 16.0 software, with statistical significance determined at a p-value threshold of <0.05.
Ethical considerations
This research was approved by ethics code LB.02.06/2/574/2021 from Health Polytechnic of Jambi, Jambi Province, Indonesia.
Findings
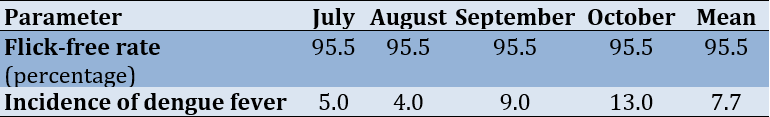
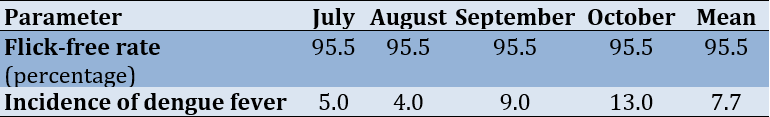
An overview of larval prevalence and the incidence of dengue fever in Jambi City, Indonesia, from July to October 2021, is presented in Table 1. Table 1 illustrates a monthly larva free rate of 95.5%, alongside a consistent occurrence of dengue fever every month from July to October, with an average of 7.7 incidents.
Table 1. Flick-free rate and incidence of dengue fever
According to the Kolmogorov-Smirnov test result (p=0.001>0.05), we rejected the null hypothesis (ineffectiveness of the intervention on students' knowledge regarding DHF) and concluded that the data were not normally distributed. The mean score of students' knowledge of controlling DHF through the 3M approach following the implementation of the intervention showed an increase from the pre-test (75.20±14.38) to the post-test (83.51±11.88) (p<0.05).
Discussion
Several factors influence the knowledge level, including counseling through videos, leaflets, socialization, and interactive Q&A sessions. This is evident in the noticeable improvement in respondents' knowledge from the pre-modeling phase to the post-modeling phase, facilitated by the use of videos, leaflets, socialization, and Q&A sessions. Modeling, which integrates various media, represents an effort to disseminate information effectively. As noted by Huthmaker et al. [27], increased exposure to information leads to broader knowledge.
Modeling serves as a valuable teaching aid, facilitating the explanation and presentation of materials. The use of video, leaflets, and socialization offers several advantages, including making the content more engaging through detailed explanations, illustrations, and various animated elements such as text, images, and photos. Visual information is particularly accessible, stimulating students to explore the significance of implementing the 3M movement in controlling dengue fever.
The observed increase in action is a result of the learning process among respondents, indicative of heightened sensitivity and readiness for assessment. Actions related to Dengue Fever occur subsequent to individuals' perception of specific stimuli, which is facilitated through sensory experiences like sight, hearing, smell, and touch. Notably, the use of video as an audio-visual medium aids in capturing students' attention and engagement.
Highlighting the benefits of utilizing media in teaching, emphasizes that it captures students' attention, thereby enhancing their motivation to learn. Additionally, instructional materials become clearer and more accessible, facilitating better understanding and mastery of learning objectives. Diversifying learning methods through multimedia not only prevents monotony but also enables effective communication beyond verbal instruction, ensuring that students remain actively engaged and enthusiastic throughout the learning process [22, 28]. Health counseling significantly impacts knowledge enhancement, as evidenced by the contrast between the pre-counseling (pretest) and post-counseling (posttest) stages. Prior to receiving health counseling, students exhibited limited knowledge, which notably improved after the counseling sessions [29].
Indications suggest that human retention solely through visual perception is limited to approximately 82%. Leaflets, as a visual medium, rely solely on visual perception for information absorption. Several factors contribute to the ineffectiveness of educational outreach, including unengaging leaflet design, accompanying imagery, less prominent color schemes, complex language unsuitable for the target audience, and the monotony of content delivery [30].
Health counseling is associated with predisposing, reinforcing, and enabling factors in educational diagnosis and evaluation, leading to behavioral changes that facilitate the achievement of desired objectives. Researchers emphasize that modeling in dengue fever control represents a crucial strategy for augmenting individuals' understanding of dengue fever, ultimately influencing behavioral changes in preventing DHF [31, 32].
Following the decision by local authorities, socialization activities will be conducted, with schools being visited and learning activities resuming. Students will be informed about the 3M Socialization plan. Regular surveys monitoring the presence of mosquito larvae are critical in supporting the control of dengue disease transmission. These surveys serve as crucial indicators to predict the risk of dengue fever transmission within an area. The larval-free rate is one of the key indicators frequently employed. An area with a larval free rate equal to or exceeding 95% is classified as a larval-free zone. While achieving the larval free rate in Jambi City does not guarantee complete immunity from the risk of dengue fever transmission, the evaluation of mosquito larvae density identified bathtubs as the primary reservoirs hosting larvae. This observation aligns with the findings from Sultana et al. [33], which identify bathtubs, pots, and barrels as the most common containers housing Aedes Sp. larvae.
Mosquito larvae surveys also serve to identify various types of water reservoirs, providing essential insights, such as the size of infected domestic water reservoirs, community awareness levels regarding dengue fever, health promotional activities, water hygiene conditions, and community engagement in eradicating mosquito breeding sites in endemic regions. The identification outcomes gleaned from these surveys prove invaluable in disrupting the life cycle of the Aedes aegypti mosquito [1, 2].
According to Pratama et al. [34], the presence of larvae in water reservoirs is attributed to the attitudes of respondents towards draining these reservoirs. Respondents are inclined to empty water reservoirs when they perceive the water to be unclean, odorous, or murky. Notably, the primary motivation for draining bathtubs is not necessarily to eliminate mosquito larvae or prevent these reservoirs from becoming breeding grounds for mosquitoes.
Conclusion
The modeling conducted in nine junior high schools in Jambi city indicated that educational modeling has a positive impact on enhancing students' knowledge in controlling dengue fever through the 3M movement in Jambi city.
Acknowledgments: We extend our sincere gratitude to the Chairperson of Jambi Health Polytechnic for their invaluable support in providing the necessary research facilities. Additionally, we would like to express our heartfelt appreciation to the Head of SMP Jambi City for their invaluable assistance in supplying the required data.
Ethical Permissions: his study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, with registration number: LB.02.06/2/574/2021.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors’ Contribution: Fahri S (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (50%); Suhermanto S (Second Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (50%).
Funding/Support: This research did not receive financial support from any party.
Dengue hemorrhagic fever (DHF) results from an infection with the dengue virus, transmitted by the Aedes aegypti mosquito [1, 2]. Indonesia, due to its enduring prevalence in many regions, continues to grapple with the commonality of DHF. This mosquito-borne disease is endemic in numerous countries across Southeast and South Asia, the Pacific, and Latin America. Its hallmark characteristics include heightened vascular permeability, hypovolemia, and compromised clotting mechanisms. While primarily impacting children, adults are also vulnerable to its effects [3, 4].
In areas where dengue is endemic, significant outbreaks are often marked by an upsurge in cases. According to data provided by the Jambi Provincial Health Office, the incidence of dengue fever in 2018 was 831 cases per 100,000 people, which escalated to 2229 cases in 2019. Jambi City recorded the highest number of cases, with 668 individuals affected [5].
Epidemiological investigations involve the continual and systematic observation of disease patterns in a population, aiming to comprehend the history of the disease and gather foundational data for effective disease control and management [6, 7]. This includes identifying the prevalent Aedes spp. in a particular area or region. Aedes spp. mosquitoes serve as carriers of dengue fever. Various factors contribute to the spread and transmission of the disease, such as the burgeoning urban population, suboptimal awareness and knowledge regarding disease prevention, inadequate sanitation practices, compromised water supplies, and improper waste disposal [8, 9].
During increased rainfall in Jambi City, the management of DHF is primarily focused on eliminating mosquito breeding sites. This is achieved through the implementation of eradication of mosquito nests (EMN) and the 3M approach, which encompasses draining (and scrubbing) of containers, such as bathtubs and toilets, sealing off household water reservoirs, like crocks and drums, and disposal or destruction of discarded items, including garbage cans and tires [10, 11]. Regular landfill drainage, conducted at least once a week, is essential to prevent mosquito breeding in these areas. Additionally, the adoption of the extended 3M plus approach is gaining traction, contributing to an improved larval-free rate in community containers and households [12, 13].
Environmental management practices play a pivotal role in DHF control, emphasizing the maintenance of suitable humidity levels within homes and neighborhoods. This entails proper room ventilation, organized spaces, and the avoidance of storing items in dark and damp locations, which can serve as potential resting spots for Aedes aegypti mosquitoes [14-16].
Effective Aedes aegypti mosquito eradication relies on periodic larval inspections (PJB) performed by health center personnel and the routine calculation of the Breteau Index (ABf) on a monthly basis. Fidayanto, Susanto, Yohanan, and Yudhastuti's Dengue Fever Control Model serves as an indicator for detecting the presence of mosquito larvae in containers or households. When the larval-free rate is low, this signals an increased presence of larvae, necessitating vigorous vector control measures to curb the transmission of dengue disease [17-19].
Vector control, a pivotal strategy in managing diseases transmitted by disease vectors, like the Aedes aegypti mosquito, incorporates biological control methods. For instance, the use of natural predators, such as certain species of Copepoda or Cyclops, has demonstrated effectiveness in controlling DHF vectors [20]. Notably, the utilization of Mesocyclops aspericornis has shown promise in various research trials conducted in Vietnam, Tahiti, and at the Vector and Reservoir Research Center in Salatiga [21].
Chemical control, utilizing insecticides for Aedes aegypti eradication, encompasses larvacidation, which targets both larval and adult stages. Temephos, commonly used as a larvicide, is formulated as sand granules. The recommended dosage is 1ppm or 10g (equivalent to 1 flat tablespoon) per 100 liters of water, with a residual effect lasting up to three months. Insect growth regulators can also be employed for this purpose [22, 23].
However, the use of insecticides in dengue vector control poses potential side effects on the environment and public health, especially when factors, such as dosage, target, timing, and coverage of vector control are not meticulously managed.
Schools, characterized by clean water reservoirs and routine eating and drinking activities, generate waste that, if improperly managed during the rainy season, can serve as breeding grounds for mosquitoes. DHF poses a significant public health challenge in Indonesia, with the number of cases showing a rising trend and the geographical spread widening. Typically, areas experiencing outbreaks of DHF initially witness a surge in the number of cases within the region. Fernandez et al. [24] suggest that urban neighborhoods with a higher-income population are at a heightened risk of dengue fever transmission.
Socialization and promotional efforts aim to engage the educational community in collaborative endeavors to combat dengue fever through improved environmental hygiene practices, ultimately leading to a reduction in the incidence of dengue fever in junior high schools. The outcomes are measured by the rate of free flies and the decreased incidence of dengue fever.
This study aimed to analyze the impact of educational interventions on the control of DHF among students in Jambi City.
Materials and Methods
Study Design
This experimental research employed a non-equivalent control group with a pretest and a posttest design [25, 26].
Participants
The study was carried out between July and October 2022, encompassing nine junior high schools in Jambi City, Indonesia. A total of 225 students who met the inclusion criteria were randomly selected to participate. The inclusion criteria comprised students in grades seven to nine, proficient in reading, and with parental consent. The researcher provided a comprehensive explanation of the study's scope to both students and parents. Upon their agreement, both parties signed a research consent certificate.
Variables and Data Collection
The dependent variable was the students' knowledge of managing DHF in Jambi City, assessed through a questionnaire comprising ten questions with binary (yes/no) answer options. The Guttman scale was utilized to assign a score ranging from 10 to 100. Scores of 60 or higher categorized students' responses as positive, while scores below 60 classified them as negative.
The independent variable was the implementation of educational strategies, including lectures, leaflet dissemination, and interactive discussions. The educational material focused on enhancing students' comprehension of DHF management through the implementation of the draining, covering, and burying (3M) approach.
Before implementing the educational intervention, a pretest involving the distribution of questionnaires to students was conducted. After completing the pretest, educational materials were presented to the students, delivered over a 30-minute duration, followed by discussions aimed at reinforcing their understanding of dengue hemorrhagic fever control. Subsequently, a posttest was administered in the form of another questionnaire addressing the management of DHF.
Sample size
A total of 225 students were calculated using Slovin's formula at α=0.05, and the total population was considered to be 515 people. According to Masturoh and Anggita [27], the sample was calculated using the Taro Yamane formula as follows:
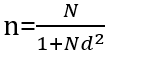
n=Number of samples
N=Number of populations
d=Precision
Statistical Analysis
The demographic data presentation involves providing a comprehensive overview by displaying the percentage distribution of variables. Additionally, numerical data is represented using mean values, standard deviation (SD), and the range of maximum and minimum values for each variable (both pre- and post-test). For data analysis, the non-parametric Wilcoxon test was employed due to the non-normal distribution of the data. This test was utilized to assess the impact of the intervention on students' behavior. All data analyses were conducted using SPSS version 16.0 software, with statistical significance determined at a p-value threshold of <0.05.
Ethical considerations
This research was approved by ethics code LB.02.06/2/574/2021 from Health Polytechnic of Jambi, Jambi Province, Indonesia.
Findings
An overview of larval prevalence and the incidence of dengue fever in Jambi City, Indonesia, from July to October 2021, is presented in Table 1. Table 1 illustrates a monthly larva free rate of 95.5%, alongside a consistent occurrence of dengue fever every month from July to October, with an average of 7.7 incidents.
Table 1. Flick-free rate and incidence of dengue fever
According to the Kolmogorov-Smirnov test result (p=0.001>0.05), we rejected the null hypothesis (ineffectiveness of the intervention on students' knowledge regarding DHF) and concluded that the data were not normally distributed. The mean score of students' knowledge of controlling DHF through the 3M approach following the implementation of the intervention showed an increase from the pre-test (75.20±14.38) to the post-test (83.51±11.88) (p<0.05).
Discussion
Several factors influence the knowledge level, including counseling through videos, leaflets, socialization, and interactive Q&A sessions. This is evident in the noticeable improvement in respondents' knowledge from the pre-modeling phase to the post-modeling phase, facilitated by the use of videos, leaflets, socialization, and Q&A sessions. Modeling, which integrates various media, represents an effort to disseminate information effectively. As noted by Huthmaker et al. [27], increased exposure to information leads to broader knowledge.
Modeling serves as a valuable teaching aid, facilitating the explanation and presentation of materials. The use of video, leaflets, and socialization offers several advantages, including making the content more engaging through detailed explanations, illustrations, and various animated elements such as text, images, and photos. Visual information is particularly accessible, stimulating students to explore the significance of implementing the 3M movement in controlling dengue fever.
The observed increase in action is a result of the learning process among respondents, indicative of heightened sensitivity and readiness for assessment. Actions related to Dengue Fever occur subsequent to individuals' perception of specific stimuli, which is facilitated through sensory experiences like sight, hearing, smell, and touch. Notably, the use of video as an audio-visual medium aids in capturing students' attention and engagement.
Highlighting the benefits of utilizing media in teaching, emphasizes that it captures students' attention, thereby enhancing their motivation to learn. Additionally, instructional materials become clearer and more accessible, facilitating better understanding and mastery of learning objectives. Diversifying learning methods through multimedia not only prevents monotony but also enables effective communication beyond verbal instruction, ensuring that students remain actively engaged and enthusiastic throughout the learning process [22, 28]. Health counseling significantly impacts knowledge enhancement, as evidenced by the contrast between the pre-counseling (pretest) and post-counseling (posttest) stages. Prior to receiving health counseling, students exhibited limited knowledge, which notably improved after the counseling sessions [29].
Indications suggest that human retention solely through visual perception is limited to approximately 82%. Leaflets, as a visual medium, rely solely on visual perception for information absorption. Several factors contribute to the ineffectiveness of educational outreach, including unengaging leaflet design, accompanying imagery, less prominent color schemes, complex language unsuitable for the target audience, and the monotony of content delivery [30].
Health counseling is associated with predisposing, reinforcing, and enabling factors in educational diagnosis and evaluation, leading to behavioral changes that facilitate the achievement of desired objectives. Researchers emphasize that modeling in dengue fever control represents a crucial strategy for augmenting individuals' understanding of dengue fever, ultimately influencing behavioral changes in preventing DHF [31, 32].
Following the decision by local authorities, socialization activities will be conducted, with schools being visited and learning activities resuming. Students will be informed about the 3M Socialization plan. Regular surveys monitoring the presence of mosquito larvae are critical in supporting the control of dengue disease transmission. These surveys serve as crucial indicators to predict the risk of dengue fever transmission within an area. The larval-free rate is one of the key indicators frequently employed. An area with a larval free rate equal to or exceeding 95% is classified as a larval-free zone. While achieving the larval free rate in Jambi City does not guarantee complete immunity from the risk of dengue fever transmission, the evaluation of mosquito larvae density identified bathtubs as the primary reservoirs hosting larvae. This observation aligns with the findings from Sultana et al. [33], which identify bathtubs, pots, and barrels as the most common containers housing Aedes Sp. larvae.
Mosquito larvae surveys also serve to identify various types of water reservoirs, providing essential insights, such as the size of infected domestic water reservoirs, community awareness levels regarding dengue fever, health promotional activities, water hygiene conditions, and community engagement in eradicating mosquito breeding sites in endemic regions. The identification outcomes gleaned from these surveys prove invaluable in disrupting the life cycle of the Aedes aegypti mosquito [1, 2].
According to Pratama et al. [34], the presence of larvae in water reservoirs is attributed to the attitudes of respondents towards draining these reservoirs. Respondents are inclined to empty water reservoirs when they perceive the water to be unclean, odorous, or murky. Notably, the primary motivation for draining bathtubs is not necessarily to eliminate mosquito larvae or prevent these reservoirs from becoming breeding grounds for mosquitoes.
Conclusion
The modeling conducted in nine junior high schools in Jambi city indicated that educational modeling has a positive impact on enhancing students' knowledge in controlling dengue fever through the 3M movement in Jambi city.
Acknowledgments: We extend our sincere gratitude to the Chairperson of Jambi Health Polytechnic for their invaluable support in providing the necessary research facilities. Additionally, we would like to express our heartfelt appreciation to the Head of SMP Jambi City for their invaluable assistance in supplying the required data.
Ethical Permissions: his study obtained ethical feasibility under the Health Research Ethics Commission of the Ministry of Health, Jambi, with registration number: LB.02.06/2/574/2021.
Conflicts of Interests: The authors declared no conflicts of interests.
Authors’ Contribution: Fahri S (First Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (50%); Suhermanto S (Second Author), Introduction Writer/Methodologist/Original or Assistant Researcher/Discussion Writer/Statistical Analyst (50%).
Funding/Support: This research did not receive financial support from any party.
Article Type: Original Research |
Subject:
Health Education and Health Behavior
Received: 2023/10/10 | Accepted: 2023/11/13 | Published: 2024/01/5
Received: 2023/10/10 | Accepted: 2023/11/13 | Published: 2024/01/5
References
1. Wong LP, AbuBakar S, Chinna K. Community knowledge, health beliefs, practices and experiences related to dengue fever and its association with IgG seropositivity. PLoS Negl Trop Dis. 2014;8(5):e2789. [Link] [DOI:10.1371/journal.pntd.0002789]
2. Wong LP, AbuBakar S. Health beliefs and practices related to dengue fever: A focus group study. PLoS Negl Trop Dis. 2013;7(7):e2310. [Link] [DOI:10.1371/journal.pntd.0002310]
3. Tosepu R, Susilawaty A, Asis MA. Relationship between Surveillance data and Google trends data for dengue hemorrhagic fever in Southeast Sulawesi, Indonesia. Higiene. 2023;9(1):51-7. [Indonesian] [Link]
4. Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176-84. [Link] [DOI:10.1111/j.1524-475X.2004.04006.x]
5. Dinkes Kota Jambi. Jambi City Health Profile [Internet]. Jambi: Dinkes Kota Jambi; 2021- [cited 2022 Jul 19]. Available from: http://dinkes.jambiprov.go.id/all_profil_kesehatan. [Indonesian] [Link]
6. Ajlan BA, Alafif MM, Alawi MM, Akbar NA, Aldigs EK, Madani TA. Assessment of the new World Health Organization's dengue classification for predicting severity of illness and level of healthcare required. PLoS Negl Trop Dis. 2019;13(8):e0007144. [Link] [DOI:10.1371/journal.pntd.0007144]
7. Al-Raddadi R, Alwafi O, Shabouni O, Akbar N, Alkhalawi M, Ibrahim A, et al. Seroprevalence of dengue fever and the associated sociodemographic, clinical, and environmental factors in Makkah, Madinah, Jeddah, and Jizan, Kingdom of Saudi Arabia. Acta Trop. 2019;189:54-64. [Link] [DOI:10.1016/j.actatropica.2018.09.009]
8. nAbd El-Ghany GM, Mahmoud SF. Effect of educational sessions about dengue fever on nurse's knowledge and attitude at Zagazig Fever hospital. Egypt Nurs J. 2018;15(3):281. [Link] [DOI:10.4103/ENJ.ENJ_18_18]
9. Adnyana I, Surya A. Strategy to control and eradicate dengue hemorrhagic fever vectors in Bali. Int J Public Heal Sci. 2023;12(1):196-202. [Link] [DOI:10.11591/ijphs.v12i1.22201]
10. Chaikoolvatana A, Singhasivanon P, Haddawy P. The development of an intelligent self-learning program in dengue mosquito and hemorrhagic fever surveillance. J Sci Technol Ubal Rajthani Univ. 2014;12(4):2553. [Link]
11. Chandra E, Zunidra Z, Ariyadi B, Ahyanti M. Trigger method in an effort to improve the culture of eradicating mosquito nests in the community. J Ilmiah Ilmu Kebidanan Kandungan. 2023;15(3):618-29. [Indonesian] [Link]
12. Arsin AA, Amiruddin R, Marzuki DS, Elisafitri R, Mallongi A, Yani A. Community empowerment with independent larva monitor in reducing the dengue hemorrhagic fever incidence, in Sidrap Regency. Pharmacognosy J. 2023;15(4):622-5. [Link] [DOI:10.5530/pj.2023.15.129]
13. Bakar AA, Kefli Z, Abdullah S, Sahani M. Predictive models for dengue outbreak using multiple rulebase classifiers. Proceedings of the 2011 International Conference on Electrical Engineering and Informatics; 2011 Jul 17-19. Bandung: IEEE; 2011. [Link] [DOI:10.1109/ICEEI.2011.6021830]
14. Desjardins MR, Casas I, Victoria AM, Carbonell D, Dávalos DM, Delmelle EM. Knowledge, attitudes, and practices regarding dengue, chikungunya, and Zika in Cali, Colombia. Health Place. 2020;63:102339. [Link] [DOI:10.1016/j.healthplace.2020.102339]
15. Díaz-González EE, Danis-Lozano R, Peñaloza G. Schools as centers for health educational initiatives, health behavior research and risk behavior for dengue infection in school children and community members: A systematic review. Health Educ Res. 2020;35(5):376-95. [Link] [DOI:10.1093/her/cyaa019]
16. Diaz-Quijano FA, Martínez-Vega RA, Rodriguez-Morales AJ, Rojas-Calero RA, Luna-González ML, Díaz-Quijano RG. Association between the level of education and knowledge, attitudes and practices regarding dengue in the Caribbean region of Colombia. BMC Public Health. 2018;18(1):143. [Link] [DOI:10.1186/s12889-018-5055-z]
17. El-Bahnasawy MMM, Megahed LA, Saleh HAA, Morsy TA. Training program for the nursing staff regarding the viral hemorrhagic fevers (VHFs) in a Fever Hospital. J Egypt Soc Parasitol. 2015;45(2):249-72. [Link] [DOI:10.21608/jesp.2015.89812]
18. Eldigail MH, Adam GK, Babiker RA, Khalid F, Adam IA, Omer OH, et al. Prevalence of dengue fever virus antibodies and associated risk factors among residents of El-Gadarif state, Sudan. BMC Public Health. 2018;18(1):921. [Link] [DOI:10.1186/s12889-018-5853-3]
19. Espinoza-Gómez F, Hernández-Suárez CM, Coll-Cárdenas R. Educational campaign versus malathion spraying for the control of Aedes aegypti in Colima, Mexico. J Epidemiol Community Health. 2002;56(2):148-52. [Link] [DOI:10.1136/jech.56.2.148]
20. Hsu JC, Hsieh CL, Lu CY. Trend and geographic analysis of the prevalence of dengue in Taiwan, 2010-2015. Int J InfectDis. 2017;54:43-9. [Link] [DOI:10.1016/j.ijid.2016.11.008]
21. Gamil MA, Eisa ZM, Eifan SA, Al-Sum BA. Prevalence of dengue fever in Jizan area, Saudi Arabia. J Pure Appl Microbiol. 2014;8(1):225-31. [Link]
22. Ibrahim NK, Abalkhail B, Rady M, Al Bar H. An educational programme on dengue fever prevention and control for females in Jeddah high schools. East Mediterr Health J. 2009;15(5):1058-67. [Link] [DOI:10.26719/2009.15.5.1058]
23. Huthmaker JW. Improving Dengue fever knowledge, attitude, and practices in primary school children in Florida through animation [Dissertation]. Minnesota: Capella University; 2015. [Link]
24. Fernandez S, Thomas SJ, De La Barrera R, Im-Erbsin R, Jarman RG, Baras B, et al. An adjuvanted, tetravalent dengue virus purified inactivated vaccine candidate induces long-lasting and protective antibody responses against dengue challenge in rhesus macaques. Am J Trop Med Hyg. 2015;92(4):698. [Link] [DOI:10.4269/ajtmh.14-0268]
25. Krishnan P. A review of the non-equivalent control group post-test-only design. Nurse Res. 2023;31(1). [Link]
26. Denny M, Denieffe S, Pajnkihar M. Using a non-equivalent control group design in educational research. California: SAGE Publications Ltd; 2017. [Link] [DOI:10.4135/9781526419156]
27. Imas Masturoh SKM, Imas Masturoh SKM, Nauri Anggita T, Nauri Anggita T. Health Research Methodology. Jakarta: Rineka Cipta: Ministry of Health of the Republic of Indonesia; 2018. [Indonesian] [Link]
28. Y, Abebe L, Alemayehu G, Sudhakar M, Birhanu Z. School-based social and behavior change communication (SBCC) advances community exposure to malaria messages, acceptance, and preventive practices in Ethiopia: a pre-posttest study. PLoS One. 2020;15(6):e0235189. [Link] [DOI:10.1371/journal.pone.0235189]
29. Khormi HM, Kumar L. Modeling dengue fever risk based on socioeconomic parameters, nationality and age groups: GIS and remote sensing based case study. Sci Total Environ. 2011;409(22):4713-9. [Link] [DOI:10.1016/j.scitotenv.2011.08.028]
30. Lennon JL, Coombs D. The utility of a board game for dengue hemorrhagic fever health education. Health Educ. 2001;107(3). [Link] [DOI:10.1108/09654280710742582]
31. Rahman MM, Khan SJ, Tanni KN, Roy T, Chisty MA, Islam MR, et al. Knowledge, attitude, and practices towards dengue fever among university students of Dhaka City, Bangladesh. Int J Environ Res Public Health. 2022;19(7):4023. [Link] [DOI:10.3390/ijerph19074023]
32. - Rahman MS, Karamehic-Muratovic A, Baghbanzadeh M, Amrin M, Zafar S, Rahman NN, et al. Climate change and dengue fever knowledge, attitudes and practices in Bangladesh: A social media-based cross-sectional survey. Trans R Soc Trop Med Hyg. 2021;115(1):85-93. [Link] [DOI:10.1093/trstmh/traa093]
33. Sultana A, Hasan S, Hossain M, Alim A, Al Mamun M, Bashar K. Larval breeding habitats and ecological factors influence the species composition of mosquito (Diptera: Culicidae) in the parks of Dhaka city, Bangladesh. Bangladesh J Zool. 2017;45(2):111-22. [Link] [DOI:10.3329/bjz.v45i2.35706]
34. Pratama IP, Handayani W, Setyono JS, Prayoga N. Community capacity building through an alternative approach based on participation in handling dengue hemorrhagic fever (DHF) in Semarang. J Reg City Plan. 2017;28(1):52-69. [Link] [DOI:10.5614/jrcp.2017.28.1.4]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







