Volume 11, Issue 4 (2023)
Health Educ Health Promot 2023, 11(4): 555-560 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kody M, Sukartiningsih M. Interventions to Accelerate Uterine Involution after Early Breastfeeding and Correct Breastfeeding Techniques in Primigravida Postpartum Mothers. Health Educ Health Promot 2023; 11 (4) :555-560
URL: http://hehp.modares.ac.ir/article-5-71796-en.html
URL: http://hehp.modares.ac.ir/article-5-71796-en.html
1- Nursing Department, Health Polytechnic of Ministry of Health Kupang, Kupang, Indonesia
Full-Text [PDF 607 kb]
(3743 Downloads)
| Abstract (HTML) (2426 Views)
Full-Text: (1421 Views)
Introduction
The process of restoring the uterus to its pre-pregnancy state after childbirth is referred to as involution. This process is driven by contractions of the uterine smooth muscles [1, 2]. Within the first day following childbirth, the size of the uterus is approximately equivalent to its size at 16 weeks of gestation with a weight of around 1000 g. Within 12 hours postpartum, the fundus typically reaches a position approximately 1 cm above the level of the umbilicus. Subsequently, over the next several days, involution progresses rapidly, with the fundus descending approximately 1-2 cm every 24 hours. By the sixth day postpartum, the normal uterine fundus reaches a position midway between the umbilicus and the pubic symphysis. Beyond the ninth day postpartum, the uterus cannot be palpated on the abdominal surface [3, 4].
At the site where the placenta implants in the uterus, there are blood vessels that remain open after the placenta is expelled, increasing the risk of postpartum bleeding. This occurs when the uterine muscles fail to contract adequately to constrict these blood vessels, a condition known as subinvolution. Subinvolution is characterized by the inability of the uterus to return to its normal, non-pregnant state, and it can transpire when uterine contractions are ineffective or even cease [5-7]. Postpartum bleeding is a critical risk factor that can exacerbate a mother's condition and may even lead to fatality. The placenta is firmly attached to the uterine wall, and during labor, it typically detaches as part of the normal process. Following childbirth, the uterus should contract effectively to minimize postpartum bleeding. However, in cases of weak or absent uterine contractions (such as in subinvolution), the risk of substantial postpartum bleeding, also known as hemorrhagic postpartum bleeding, significantly increases, heightening the risk of maternal mortality [8-10]. Alarming statistics reveal that 45% of maternal deaths due to heavy postpartum bleeding occur within the first 24 hours after childbirth, with 68-73% happening within one week and 82-88% within two weeks postpartum [11-13].
Indonesia continues to face a high maternal mortality rate compared to other ASEAN countries. In 2003, Indonesia reported a maternal mortality rate of 307 per 100,000 live births. Subsequently, in 2004, this rate decreased to 240 per 100,000 live births, followed by a slight increase to 262 per 100,000 live births in 2005. In 2006, this rate further decreased to 255 per 100,000 live births, and in 2007, it stood at 248 per 100,000 live births. The Millennium Development Goals (MDG) set a target for Indonesia to achieve a maternal mortality rate of 125 per 100,000 live births by the year 2015 [14].
The maternal mortality rate in NTT province exhibited fluctuations between 2006 and 2009. In 2006, there were 253 maternal deaths, translating to a rate of 269 per 100,000 live births. This rate declined in 2007 to 251 maternal deaths or 247 per 100,000 live births. However, it surged in 2008 to 312 maternal deaths or 332 per 100,000 live births, before decreasing once more in 2009 to 286 maternal deaths or 302 per 100,000 live births. Conversely, the under-five mortality rate experienced a significant reduction during the same period. In 2006, there were 862 child deaths, accounting for a rate of 9.1 per 1000 live births. By 2007, this rate dropped to 490 child deaths or 4.8 per 1000 live births. In 2008, it further decreased to 409 child deaths or 4.3 per 1000 live births, and in 2009, it reached 362 child deaths or 3.8 per 1000 live births. The high maternal and infant mortality rates in NTT stem from various factors, including limited healthcare infrastructure, geographical challenges, a shortage of healthcare professionals, and a predominant cause of maternal and infant deaths being related to bleeding, which often causes delays in treatment by medical teams [15].
The mentioned conditions and risks arise when the pregnancy-to-delivery process is not managed systematically and consistently. In reality, a typical postpartum recovery adheres to traditional practices but is presented in a contemporary manner, emphasizing early mobilization, rooming-in, and breastfeeding. When a mother effectively and sufficiently initiates breastfeeding after childbirth, it promotes proper uterine involution and can decrease the likelihood of bleeding complications [1, 16].
Breastfeeding offers numerous advantages for mothers. When the baby sucks on the mother's nipple, it triggers a response from the posterior pituitary gland, leading to the release of oxytocin. Oxytocin plays a crucial role by enhancing smooth muscle contractions in the milk glands' alveoli and the uterine muscles. This dual action yields benefits for both mother and baby. For mothers, the stimulation of oxytocin induces uterine contractions, which significantly reduce postpartum bleeding. Simultaneously, for babies, the stimulation of prolactin hormone secretion increases milk production, ensuring that the baby's nutritional needs are well met. Hence, early breastfeeding holds paramount importance for the health and well-being of both mother and baby [2, 17, 18].
The proper breastfeeding technique encompasses various aspects, including the positioning and attachment of both the mother and the baby. To achieve this, the baby's belly must be in contact with the mother's belly, the baby's face must be directed toward the mother's breast, and the baby's head must remain in a neutral position without excessive tilting toward the breast. The mother should ideally be in a comfortable sitting position, ensuring that the baby's ears and arms align in a straight line. In terms of correct attachment, the baby's chin must be snugly against the mother's breast, allowing most mammary areola to enter the baby's mouth. The baby's lower lip should be turned downward, and their mouth should be wide open. When these aspects of attachment are achieved, the baby can effectively suckle, stimulating optimal milk production by the pituitary gland. Additionally, it fosters a strong psychological bond and enhances the affectionate relationship between the mother and the baby [19-22].
Given this background, we examined the variation in uterine involution acceleration following early breastfeeding and the application of correct breastfeeding techniques among first-time mothers in the postpartum period.
Materials and Methods
Study Design
This research adopted an experimental approach utilizing a post-test design with a control group This study was conducted within the Kemuning room at the Umbu Rara Meha Regional General Hospital in Waingapu, located in East Sumba Regency, within the province of East Nusa Tenggara, Indonesia.
Participants
The participants were 100 randomly selected primigravida pregnant women referring to the Waingapu Regional General Hospital in East Sumba, NTT, Indonesia during January-May 2021. Inclusion criteria comprised mothers who had experienced a normal childbirth (without cesarean section) and were actively breastfeeding their babies while demonstrating willingness to participate in the study. Mothers who had encountered labor complications were excluded from the study.
Sample size
The number of samples involved was 134 participants who were chosen randomly. The sample was divided into an intervention group of 50 cases (early breastfeeding and practicing the correct breastfeeding technique) and 100 cases in the control group (not breastfeeding early and not practicing proper breastfeeding techniques). The sample size was calculated to be 134 people using the Slovin formula and considering d=0.05.
Variables and data collecting
The dependent variable was the pace of uterine involution among postpartum mothers, while the independent variables included the practice of early breastfeeding and the application of correct breastfeeding techniques. The "pace of uterine involution" was assessed using a checklist using the following procedure: The patient was placed in a lithotomy, and starting from the navel, the left hand was placed on it and began to palpate and move the fingers to find the fundus of the uterus. The position of the finger was measured as two fingers' width from the umbilicus. Simultaneously, the right hand palpated the uterus, assessing its roundness and firmness. Normal uterine fundal reduction was considered if it decreased by more than 2 cm daily. To evaluate the "early breastfeeding" variable, a questionnaire consisting of seven questions was utilized. The questions covered topics, such as the definition of early breastfeeding, the initiation process, its benefits, the required time, and colostrum. This variable was scored using a Guttman scale, assigning a score of two for "yes" answers and one for "no" responses. The "correct breastfeeding technique" was assessed through a checklist encompassing breastfeeding position, mother-infant attachment, and baby burping with questions scored using a Likert scale, with "Very Good" rated as four for a final value between 10-12, "Good" rated as three for a final value between 7-9, "Fair" rated as two for a final value between 4-6, and "Less" rated as one for a final value between 1-3. Before the intervention, the postpartum mothers in the intervention group received education on early breastfeeding and correct breastfeeding techniques, while the control group did not receive such education. Subsequently, both groups practiced early breastfeeding and applied correct breastfeeding techniques. Following the intervention, both groups were assessed using questionnaires, checklists, and measurements of uterine fundal reduction.
Ethical considerations
Prior to the implementation of measles immunization, the researcher asked the mother's willingness to provide informed consent. Then, the baby's mother signed the informed consent. No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki's ethical guidelines for clinical studies. This research was approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health (LB.02.01/6/91/2021).
Statistical analysis
Data are presented as numbers and percentages and mean and standard deviation (SD) values. Data analysis was done by bivariate analysis using the Wilcoxon test to determine the effect of early breastfeeding and correct breastfeeding techniques on uterine fundus reduction. Then, to analyze the differences between the intervention and control groups, the Mann-Whitney U test was used. The significance level was considered at p<0.05. Statistical analysis was performed using SPSS version 16.0.
Findings
The respondents’ characteristics can be seen in Table 1.
Table 1. Demographic characteristics of participants

Table 1 reveals that the majority of participants were in the age range of 20-30 years, primarily had primary school education, predominantly worked as housewives, and practiced the Catholic Christian religion.
Table 2 illustrates that regarding the early breastfeeding variable, both groups, specifically the intervention and control groups, predominantly initiated breastfeeding immediately after delivery. Regarding the correct breastfeeding technique, the intervention group displayed a stronger presence in the "good" category, while the control group was primarily categorized as "satisfactory". Concerning the acceleration of uterine involution, the intervention group exhibited dominance in the "fast" category, whereas the control group was more prevalent in the "slow" category.
Table 2. Frequency of research variables
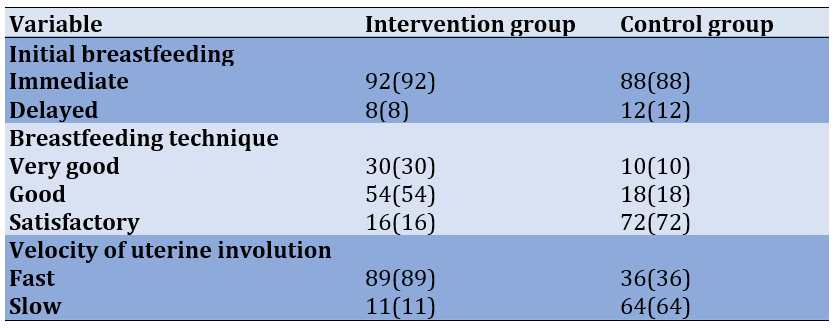
Table 2 illustrates that regarding the early breastfeeding variable, both groups, specifically the intervention and control groups, predominantly initiated breastfeeding immediately after delivery. Regarding the correct breastfeeding technique, the intervention group displayed a stronger presence in the "good" category, while the control group was primarily categorized as "satisfactory". Concerning the acceleration of uterine involution, the intervention group exhibited dominance in the "fast" category, whereas the control group was more prevalent in the "slow" category.
There was a significant difference in the outcomes of accelerated uterine involution between the intervention (1.89±0.31) and control (1.36±0.48) groups, as influenced by early breastfeeding and the application of correct breastfeeding techniques (p<0.0001).
Discussion
Involution refers to a retrogressive transformation occurring in the uterus, resulting in a reduction in its size. During the postpartum period, involution is specific to the uterus, while changes in other organs and structures are considered part of the puerperium. Uterine involution, often termed uterine shrinkage, is a mechanism, through which the uterus gradually returns to its pre-pregnancy state, typically weighing around 60 g. This process commences immediately following the expulsion of the placenta, driven by the contractions of the uterine smooth muscles. The term "involution" encompasses the overall changes occurring in the reproductive organs. The speed of involution signifies the process of uterine transformation and the gradual restoration of the uterus in postpartum mothers [22-24].
There are mothers who have received education on proper breastfeeding techniques but encounter challenges in applying this knowledge during their treatment. This issue is influenced by several factors, such as psychological factors. The psychological well-being of postpartum women plays a pivotal role in determining the success or failure of breastfeeding [25, 26]. For instance, mothers who excessively worry about their ability to breastfeed may struggle to do so effectively. Various factors contribute to this, including hormonal fluctuations, physical fatigue from pregnancy and childbirth, sleep deprivation, unfamiliar surroundings, anxiety related to the baby, spouse, or other children, and psychological changes occurring in the first two days postpartum. These psychological changes may manifest as a need for attention, passivity, self-focused behavior, dependence, a reluctance to engage with the baby, or a lack of awareness of the baby's needs [3, 4, 27].
In this study, the measurement target was set for the seventh day. The research team measured the height of the uterine fundus and observed that the reduction in the intervention group was notably more rapid, while in the control group, it predominantly progressed at a slower rate. The process of uterine involution is marked by a daily decrease in the height of the uterine fundus (TFU). On the first day, it typically measures two fingers below the umbilical center, and on the second day, it is approximately three fingers below the center. Correct breastfeeding involves the baby's suction, which triggers nerve impulses in the breast areola area. These impulses are then transmitted to the hypothalamus, subsequently reaching the hypophysis, which is located partially behind the brain. Oxytocin is released as a result of this process. One of the key functions of oxytocin is to stimulate the contraction of the uterine smooth muscles, thereby facilitating a faster uterine involution process.
In accordance with the theory presented by Gimpl and Fahrenholz [17], lactation involves a prolactin reflex that necessitates nerve impulses originating from the nipple. These impulses travel through the hypothalamus and posterior pituitary, ultimately leading to the release of oxytocin, which triggers smooth muscle contractions, facilitating the ejection of breast milk.
Aryani et al. [28] explored the correlation between breastfeeding and uterine involution in Delivery Room II at RSUD DR. SOETOMO Surabaya, involving 30 respondents. The research data revealed that 15 individuals who breastfed correctly exhibited normal uterine involution, while three individuals who breastfed incorrectly experienced fast uterine involution (which is considered normal). Additionally, four individuals who breastfed correctly encountered slow uterine involution (deemed abnormal), and eight individuals who breastfed incorrectly also had slow uterine involution (also considered abnormal).
Regarding early breastfeeding, there was scarcely any distinction between the two groups. This is largely attributed to the policy implemented at the Umbu Rara Meha Regional General Hospital in Waingapu, East Sumba Regency, East Nusa Tenggara Province, Indonesia, which advocates the immediate provision of breast milk to newborns right after birth. This policy significantly expedites the uterine involution process in postpartum mothers.
Immediate Maternal Delivery (IMD) emerges as one of the factors supporting uterine involution because providing breast milk promptly after birth induces contractions in uterine smooth muscles. While prolactin initiates milk production, the effective delivery of milk to the infant and the continuation of lactation hinge on mechanical stimulation of the nipple. Touch and suction of the mother's breast promote the release of oxytocin, which in turn triggers uterine contractions, aiding the expulsion of the placenta and preventing excessive bleeding. Oxytocin also stimulates other hormones that foster a sense of safety and comfort in the mother, facilitating the smooth flow of milk [29-31].
In studies carried out in both Indonesia and Egypt, it was discovered that immediate maternal delivery (IMD) can effectively reduce postpartum vaginal bleeding and promote the normalization of uterine size. These effects were observed both within 24 hours after delivery and up to seven days postpartum [16, 18].
Limitations
The process of involution is affected not only by breastfeeding but also by various factors, such as early mobilization, rest, pain, and anxiety, which were not examined in this study. Therefore, in future research, it would be beneficial to incorporate some of these additional variables for a more comprehensive analysis.
Conclusion
Regarding early breastfeeding, both the intervention and control groups exhibited a prevalent practice of providing breast milk immediately after delivery. Considering the correct breastfeeding technique, the intervention group displayed a higher prevalence in the "good" category, while the control group was predominantly categorized as "sufficient." Furthermore, a notable disparity was observed in the acceleration of uterine involution between the intervention and control groups.
Acknowledgments: We express our deepest gratitude to the director of Poltekkes Kupang Indonesia for supporting this research.
Ethical Permission: This research was approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health (LB.02.01/6/91/2021).
Conflict of Interest: The authors reported no conflicts of interests.
Authors’ contribution: Kody MM (First Author), Introduction Writer/Methodologist/Original Researcher/Discussion Writer/Statistical Analyst (70%); Endang Sukartiningsih MC (Second Author), Methodologist/ Assistant Researcher/Statistical Analyst (30%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The process of restoring the uterus to its pre-pregnancy state after childbirth is referred to as involution. This process is driven by contractions of the uterine smooth muscles [1, 2]. Within the first day following childbirth, the size of the uterus is approximately equivalent to its size at 16 weeks of gestation with a weight of around 1000 g. Within 12 hours postpartum, the fundus typically reaches a position approximately 1 cm above the level of the umbilicus. Subsequently, over the next several days, involution progresses rapidly, with the fundus descending approximately 1-2 cm every 24 hours. By the sixth day postpartum, the normal uterine fundus reaches a position midway between the umbilicus and the pubic symphysis. Beyond the ninth day postpartum, the uterus cannot be palpated on the abdominal surface [3, 4].
At the site where the placenta implants in the uterus, there are blood vessels that remain open after the placenta is expelled, increasing the risk of postpartum bleeding. This occurs when the uterine muscles fail to contract adequately to constrict these blood vessels, a condition known as subinvolution. Subinvolution is characterized by the inability of the uterus to return to its normal, non-pregnant state, and it can transpire when uterine contractions are ineffective or even cease [5-7]. Postpartum bleeding is a critical risk factor that can exacerbate a mother's condition and may even lead to fatality. The placenta is firmly attached to the uterine wall, and during labor, it typically detaches as part of the normal process. Following childbirth, the uterus should contract effectively to minimize postpartum bleeding. However, in cases of weak or absent uterine contractions (such as in subinvolution), the risk of substantial postpartum bleeding, also known as hemorrhagic postpartum bleeding, significantly increases, heightening the risk of maternal mortality [8-10]. Alarming statistics reveal that 45% of maternal deaths due to heavy postpartum bleeding occur within the first 24 hours after childbirth, with 68-73% happening within one week and 82-88% within two weeks postpartum [11-13].
Indonesia continues to face a high maternal mortality rate compared to other ASEAN countries. In 2003, Indonesia reported a maternal mortality rate of 307 per 100,000 live births. Subsequently, in 2004, this rate decreased to 240 per 100,000 live births, followed by a slight increase to 262 per 100,000 live births in 2005. In 2006, this rate further decreased to 255 per 100,000 live births, and in 2007, it stood at 248 per 100,000 live births. The Millennium Development Goals (MDG) set a target for Indonesia to achieve a maternal mortality rate of 125 per 100,000 live births by the year 2015 [14].
The maternal mortality rate in NTT province exhibited fluctuations between 2006 and 2009. In 2006, there were 253 maternal deaths, translating to a rate of 269 per 100,000 live births. This rate declined in 2007 to 251 maternal deaths or 247 per 100,000 live births. However, it surged in 2008 to 312 maternal deaths or 332 per 100,000 live births, before decreasing once more in 2009 to 286 maternal deaths or 302 per 100,000 live births. Conversely, the under-five mortality rate experienced a significant reduction during the same period. In 2006, there were 862 child deaths, accounting for a rate of 9.1 per 1000 live births. By 2007, this rate dropped to 490 child deaths or 4.8 per 1000 live births. In 2008, it further decreased to 409 child deaths or 4.3 per 1000 live births, and in 2009, it reached 362 child deaths or 3.8 per 1000 live births. The high maternal and infant mortality rates in NTT stem from various factors, including limited healthcare infrastructure, geographical challenges, a shortage of healthcare professionals, and a predominant cause of maternal and infant deaths being related to bleeding, which often causes delays in treatment by medical teams [15].
The mentioned conditions and risks arise when the pregnancy-to-delivery process is not managed systematically and consistently. In reality, a typical postpartum recovery adheres to traditional practices but is presented in a contemporary manner, emphasizing early mobilization, rooming-in, and breastfeeding. When a mother effectively and sufficiently initiates breastfeeding after childbirth, it promotes proper uterine involution and can decrease the likelihood of bleeding complications [1, 16].
Breastfeeding offers numerous advantages for mothers. When the baby sucks on the mother's nipple, it triggers a response from the posterior pituitary gland, leading to the release of oxytocin. Oxytocin plays a crucial role by enhancing smooth muscle contractions in the milk glands' alveoli and the uterine muscles. This dual action yields benefits for both mother and baby. For mothers, the stimulation of oxytocin induces uterine contractions, which significantly reduce postpartum bleeding. Simultaneously, for babies, the stimulation of prolactin hormone secretion increases milk production, ensuring that the baby's nutritional needs are well met. Hence, early breastfeeding holds paramount importance for the health and well-being of both mother and baby [2, 17, 18].
The proper breastfeeding technique encompasses various aspects, including the positioning and attachment of both the mother and the baby. To achieve this, the baby's belly must be in contact with the mother's belly, the baby's face must be directed toward the mother's breast, and the baby's head must remain in a neutral position without excessive tilting toward the breast. The mother should ideally be in a comfortable sitting position, ensuring that the baby's ears and arms align in a straight line. In terms of correct attachment, the baby's chin must be snugly against the mother's breast, allowing most mammary areola to enter the baby's mouth. The baby's lower lip should be turned downward, and their mouth should be wide open. When these aspects of attachment are achieved, the baby can effectively suckle, stimulating optimal milk production by the pituitary gland. Additionally, it fosters a strong psychological bond and enhances the affectionate relationship between the mother and the baby [19-22].
Given this background, we examined the variation in uterine involution acceleration following early breastfeeding and the application of correct breastfeeding techniques among first-time mothers in the postpartum period.
Materials and Methods
Study Design
This research adopted an experimental approach utilizing a post-test design with a control group This study was conducted within the Kemuning room at the Umbu Rara Meha Regional General Hospital in Waingapu, located in East Sumba Regency, within the province of East Nusa Tenggara, Indonesia.
Participants
The participants were 100 randomly selected primigravida pregnant women referring to the Waingapu Regional General Hospital in East Sumba, NTT, Indonesia during January-May 2021. Inclusion criteria comprised mothers who had experienced a normal childbirth (without cesarean section) and were actively breastfeeding their babies while demonstrating willingness to participate in the study. Mothers who had encountered labor complications were excluded from the study.
Sample size
The number of samples involved was 134 participants who were chosen randomly. The sample was divided into an intervention group of 50 cases (early breastfeeding and practicing the correct breastfeeding technique) and 100 cases in the control group (not breastfeeding early and not practicing proper breastfeeding techniques). The sample size was calculated to be 134 people using the Slovin formula and considering d=0.05.
Variables and data collecting
The dependent variable was the pace of uterine involution among postpartum mothers, while the independent variables included the practice of early breastfeeding and the application of correct breastfeeding techniques. The "pace of uterine involution" was assessed using a checklist using the following procedure: The patient was placed in a lithotomy, and starting from the navel, the left hand was placed on it and began to palpate and move the fingers to find the fundus of the uterus. The position of the finger was measured as two fingers' width from the umbilicus. Simultaneously, the right hand palpated the uterus, assessing its roundness and firmness. Normal uterine fundal reduction was considered if it decreased by more than 2 cm daily. To evaluate the "early breastfeeding" variable, a questionnaire consisting of seven questions was utilized. The questions covered topics, such as the definition of early breastfeeding, the initiation process, its benefits, the required time, and colostrum. This variable was scored using a Guttman scale, assigning a score of two for "yes" answers and one for "no" responses. The "correct breastfeeding technique" was assessed through a checklist encompassing breastfeeding position, mother-infant attachment, and baby burping with questions scored using a Likert scale, with "Very Good" rated as four for a final value between 10-12, "Good" rated as three for a final value between 7-9, "Fair" rated as two for a final value between 4-6, and "Less" rated as one for a final value between 1-3. Before the intervention, the postpartum mothers in the intervention group received education on early breastfeeding and correct breastfeeding techniques, while the control group did not receive such education. Subsequently, both groups practiced early breastfeeding and applied correct breastfeeding techniques. Following the intervention, both groups were assessed using questionnaires, checklists, and measurements of uterine fundal reduction.
Ethical considerations
Prior to the implementation of measles immunization, the researcher asked the mother's willingness to provide informed consent. Then, the baby's mother signed the informed consent. No economic incentives were offered or provided for participation in this study. The study protocol matched the Declaration of Helsinki's ethical guidelines for clinical studies. This research was approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health (LB.02.01/6/91/2021).
Statistical analysis
Data are presented as numbers and percentages and mean and standard deviation (SD) values. Data analysis was done by bivariate analysis using the Wilcoxon test to determine the effect of early breastfeeding and correct breastfeeding techniques on uterine fundus reduction. Then, to analyze the differences between the intervention and control groups, the Mann-Whitney U test was used. The significance level was considered at p<0.05. Statistical analysis was performed using SPSS version 16.0.
Findings
The respondents’ characteristics can be seen in Table 1.
Table 1. Demographic characteristics of participants

Table 1 reveals that the majority of participants were in the age range of 20-30 years, primarily had primary school education, predominantly worked as housewives, and practiced the Catholic Christian religion.
Table 2 illustrates that regarding the early breastfeeding variable, both groups, specifically the intervention and control groups, predominantly initiated breastfeeding immediately after delivery. Regarding the correct breastfeeding technique, the intervention group displayed a stronger presence in the "good" category, while the control group was primarily categorized as "satisfactory". Concerning the acceleration of uterine involution, the intervention group exhibited dominance in the "fast" category, whereas the control group was more prevalent in the "slow" category.
Table 2. Frequency of research variables
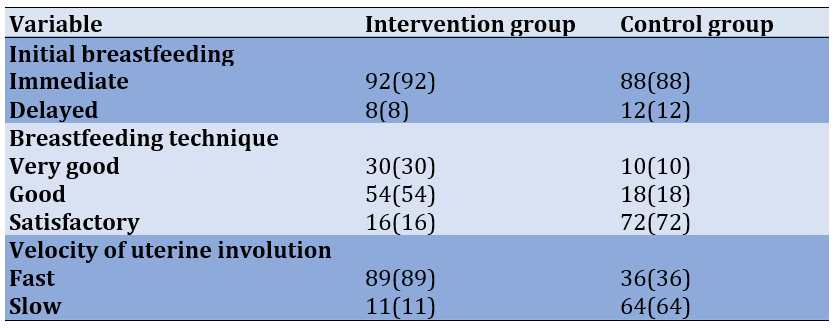
Table 2 illustrates that regarding the early breastfeeding variable, both groups, specifically the intervention and control groups, predominantly initiated breastfeeding immediately after delivery. Regarding the correct breastfeeding technique, the intervention group displayed a stronger presence in the "good" category, while the control group was primarily categorized as "satisfactory". Concerning the acceleration of uterine involution, the intervention group exhibited dominance in the "fast" category, whereas the control group was more prevalent in the "slow" category.
There was a significant difference in the outcomes of accelerated uterine involution between the intervention (1.89±0.31) and control (1.36±0.48) groups, as influenced by early breastfeeding and the application of correct breastfeeding techniques (p<0.0001).
Discussion
Involution refers to a retrogressive transformation occurring in the uterus, resulting in a reduction in its size. During the postpartum period, involution is specific to the uterus, while changes in other organs and structures are considered part of the puerperium. Uterine involution, often termed uterine shrinkage, is a mechanism, through which the uterus gradually returns to its pre-pregnancy state, typically weighing around 60 g. This process commences immediately following the expulsion of the placenta, driven by the contractions of the uterine smooth muscles. The term "involution" encompasses the overall changes occurring in the reproductive organs. The speed of involution signifies the process of uterine transformation and the gradual restoration of the uterus in postpartum mothers [22-24].
There are mothers who have received education on proper breastfeeding techniques but encounter challenges in applying this knowledge during their treatment. This issue is influenced by several factors, such as psychological factors. The psychological well-being of postpartum women plays a pivotal role in determining the success or failure of breastfeeding [25, 26]. For instance, mothers who excessively worry about their ability to breastfeed may struggle to do so effectively. Various factors contribute to this, including hormonal fluctuations, physical fatigue from pregnancy and childbirth, sleep deprivation, unfamiliar surroundings, anxiety related to the baby, spouse, or other children, and psychological changes occurring in the first two days postpartum. These psychological changes may manifest as a need for attention, passivity, self-focused behavior, dependence, a reluctance to engage with the baby, or a lack of awareness of the baby's needs [3, 4, 27].
In this study, the measurement target was set for the seventh day. The research team measured the height of the uterine fundus and observed that the reduction in the intervention group was notably more rapid, while in the control group, it predominantly progressed at a slower rate. The process of uterine involution is marked by a daily decrease in the height of the uterine fundus (TFU). On the first day, it typically measures two fingers below the umbilical center, and on the second day, it is approximately three fingers below the center. Correct breastfeeding involves the baby's suction, which triggers nerve impulses in the breast areola area. These impulses are then transmitted to the hypothalamus, subsequently reaching the hypophysis, which is located partially behind the brain. Oxytocin is released as a result of this process. One of the key functions of oxytocin is to stimulate the contraction of the uterine smooth muscles, thereby facilitating a faster uterine involution process.
In accordance with the theory presented by Gimpl and Fahrenholz [17], lactation involves a prolactin reflex that necessitates nerve impulses originating from the nipple. These impulses travel through the hypothalamus and posterior pituitary, ultimately leading to the release of oxytocin, which triggers smooth muscle contractions, facilitating the ejection of breast milk.
Aryani et al. [28] explored the correlation between breastfeeding and uterine involution in Delivery Room II at RSUD DR. SOETOMO Surabaya, involving 30 respondents. The research data revealed that 15 individuals who breastfed correctly exhibited normal uterine involution, while three individuals who breastfed incorrectly experienced fast uterine involution (which is considered normal). Additionally, four individuals who breastfed correctly encountered slow uterine involution (deemed abnormal), and eight individuals who breastfed incorrectly also had slow uterine involution (also considered abnormal).
Regarding early breastfeeding, there was scarcely any distinction between the two groups. This is largely attributed to the policy implemented at the Umbu Rara Meha Regional General Hospital in Waingapu, East Sumba Regency, East Nusa Tenggara Province, Indonesia, which advocates the immediate provision of breast milk to newborns right after birth. This policy significantly expedites the uterine involution process in postpartum mothers.
Immediate Maternal Delivery (IMD) emerges as one of the factors supporting uterine involution because providing breast milk promptly after birth induces contractions in uterine smooth muscles. While prolactin initiates milk production, the effective delivery of milk to the infant and the continuation of lactation hinge on mechanical stimulation of the nipple. Touch and suction of the mother's breast promote the release of oxytocin, which in turn triggers uterine contractions, aiding the expulsion of the placenta and preventing excessive bleeding. Oxytocin also stimulates other hormones that foster a sense of safety and comfort in the mother, facilitating the smooth flow of milk [29-31].
In studies carried out in both Indonesia and Egypt, it was discovered that immediate maternal delivery (IMD) can effectively reduce postpartum vaginal bleeding and promote the normalization of uterine size. These effects were observed both within 24 hours after delivery and up to seven days postpartum [16, 18].
Limitations
The process of involution is affected not only by breastfeeding but also by various factors, such as early mobilization, rest, pain, and anxiety, which were not examined in this study. Therefore, in future research, it would be beneficial to incorporate some of these additional variables for a more comprehensive analysis.
Conclusion
Regarding early breastfeeding, both the intervention and control groups exhibited a prevalent practice of providing breast milk immediately after delivery. Considering the correct breastfeeding technique, the intervention group displayed a higher prevalence in the "good" category, while the control group was predominantly categorized as "sufficient." Furthermore, a notable disparity was observed in the acceleration of uterine involution between the intervention and control groups.
Acknowledgments: We express our deepest gratitude to the director of Poltekkes Kupang Indonesia for supporting this research.
Ethical Permission: This research was approved by the Health Research Ethics Commission of the Health Polytechnic of the Jambi Ministry of Health (LB.02.01/6/91/2021).
Conflict of Interest: The authors reported no conflicts of interests.
Authors’ contribution: Kody MM (First Author), Introduction Writer/Methodologist/Original Researcher/Discussion Writer/Statistical Analyst (70%); Endang Sukartiningsih MC (Second Author), Methodologist/ Assistant Researcher/Statistical Analyst (30%)
Funding/Support: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Article Type: Original Research |
Subject:
Family Health Education/Promotion
Received: 2023/08/2 | Accepted: 2023/10/21 | Published: 2023/10/29
Received: 2023/08/2 | Accepted: 2023/10/21 | Published: 2023/10/29
References
1. Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs. 2012;41(1):114-21. [Link] [DOI:10.1111/j.1552-6909.2011.01313.x]
2. Weigert EML, Giuglian ERJ, França MCT, Oliveira LD de, Bonilha A, Espírito Santo LC do, et al. The influence of breastfeeding technique on the frequencies of exclusive breastfeeding and nipple trauma in the first month of lactation. J Pediatr. 2005;81:310-6. [Link] [DOI:10.2223/1367]
3. Anggraeni NPDA, Herawati L, Widyawati MN. The effectiveness of postpartum yoga on uterine involution among postpartum women in Indonesia. Int J Nurs Health Serv. 2019;2(3):124-34. [Link] [DOI:10.35654/ijnhs.v2i3.164]
4. Cholifah N, Siswanti H. Factors related to the speed of the uterus involution in post partum mothers. 8th International Conference on Public Health; 2021 Jul 29; Java, Indonesia Neliti. p.862-7. [Link] [DOI:10.26911/ICPHmaternal.FP.08.2021.25]
5. D'Alton ME, Rood KM, Smid MC, Simhan HN, Skupski DW, Subramaniam A, et al. Intrauterine vacuum-induced hemorrhage-control device for rapid treatment of postpartum hemorrhage. Obstet Gynecol. 2020;136(5):882-91. [Link] [DOI:10.1097/AOG.0000000000004138]
6. Wormer KC, Jamil RT, Bryant SB. Acute postpartum hemorrhage. Treasure Island: StatPearls Publishing; 2023. [Link]
7. Kandeel M, Sanad Z, Ellakwa H, El Halaby A, Rezk M, Saif I. Management of postpartum hemorrhage with intrauterine balloon tamponade using a condom catheter in an Egyptian setting. Int J Gynecol Obstet. 2016;135(3):272-5. [Link] [DOI:10.1016/j.ijgo.2016.06.018]
8. Bienstock JL, Eke AC, Hueppchen NA. Postpartum hemorrhage. N Engl J Med. 2021;384(17):1635-45. [Link] [DOI:10.1056/NEJMra1513247]
9. Newsome J, Martin JG, Bercu Z, Shah J, Shekhani H, Peters G. Postpartum hemorrhage. Tech Vasc IntervRadiol. 2017;20(4):266-73. [Link] [DOI:10.1053/j.tvir.2017.10.007]
10. Andrikopoulou M, D'Alton ME. Postpartum hemorrhage: Early identification challenges. Semin Perinatol. 2019;43(1):11-7. [Link] [DOI:10.1053/j.semperi.2018.11.003]
11. Sentilhes L, Merlot B, Madar H, Sztark F, Brun S, Deneux-Tharaux C. Postpartum haemorrhage: Prevention and treatment. Exp Rev Hematol. 2016;9(11):1043-61. [Link] [DOI:10.1080/17474086.2016.1245135]
12. Maswime S, Buchmann E. A systematic review of maternal near miss and mortality due to postpartum hemorrhage. Int J Gynaecol Obstet. 2017;137(1):1-7. [Link] [DOI:10.1002/ijgo.12096]
13. Butwick A, Lyell D, Goodnough L. How do I manage severe postpartum hemorrhage?. Transfusion. 2020;60(5):897-907. [Link] [DOI:10.1111/trf.15794]
14. Kementerian Kesehatan. Indonesian Health Profile [Internet]. Jakarta: Ministry of Health of the Republic of Indonesia; 2021- [cited 2023, September, 19]. Available from: https://www.kemkes.go.id/id/profil-kesehatan-indonesia-2021. [Indonesian] [Link]
15. Kemenkes RI. Main results of Riskesdas 2018 [Internet]. Jakarta: Ministry of Health Health Research and Development Agency; 2018- [cited 2023, August 12]. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf. [Indonesian] [Link]
16. Nurjanna, As'ad S, Idris I. Relationship between early breastfeeding initiation and involution uteri of childbirth mothers in nenemallomo regional public hospital and arifin nu'mang public regional hospital of sidenrengrappang regency in 2014. Indian J Public Health Res Dev. 2019;10(4):838. [Link] [DOI:10.5958/0976-5506.2019.00809.X]
17. Gimpl G, Fahrenholz F. The oxytocin receptor system: structure, function, and regulation. Physiol Rev. 2001;81(2):629-83. [Link] [DOI:10.1152/physrev.2001.81.2.629]
18. Yahya S, Al Sabati SY, Mousa O. Effect of early initiation of breastfeeding on the uterine consistency and the amount of vaginal blood loss during early postpartum period. Nurs Primary Care. 2019;3(3):2-7. [Link] [DOI:10.33425/2639-9474.1108]
19. Rinata E, Rusdyati T, Sari PA. T Breastfeeding Techniques: Position, Attachment and Effectiveness of Sucking - Study on Breastfeeding Mothers at Sidoarjo Hospital. Prosiding Sem Nat Int. 2016;18. [Indonesian] [Link]
20. Subekti R. Correct Breastfeeding Techniques in Wanaraja Village, Wanayasa District, Banjarnegara Regency. J Penelitian Dan Pengabdian Kepada Masyarakat UNSIQ. 2019;6(1):45-9. [Indonesian] [Link] [DOI:10.32699/ppkm.v6i1.550]
21. Ayu AEP, Septiani H, Dewi SWR, Nurherliyany M, Divilda M, Gumilar S, et al. Oxytocin massage and breastfeeding on demand in the uterine involution process. Genius Midwifery J. 2022;1(1):22-5. [Link] [DOI:10.56359/genmj.v1i1.104]
22. Rukmawati S, Astutik P, Retnoningrum AD. Method (Stimulation endorphin, oxytosin and sugestive) to increase the production of breast milk and involution of uters on postpartum. STRADA: J Ilmiah Kesehatan. 2020;9(2):1207-11. [Link] [DOI:10.30994/sjik.v9i2.310]
23. Wachsberg RH, Kurtz AB, Levine CD, Solomon P, Wapner RJ. Real‐time ultrasonographic analysis of the normal postpartum uterus: Technique, variability, and measurements. J Ultrasound Med. 1994;13(3):215-21. [Link] [DOI:10.7863/jum.1994.13.3.215]
24. Mohamed SS. Effect of eating palm date on breast feeding and uterine involution. Ain Shams University. 2012:1-7. [Link]
25. Shukri NHM, Wells J, Mukhtar F, Lee MHS, Fewtrell M. Study protocol: An investigation of mother-infant signalling during breastfeeding using a randomised trial to test the effectiveness of breastfeeding relaxation therapy on maternal psychological state, breast milk production and infant behaviour and growt. Int Breastfeed J. 2017;12:33. [Link] [DOI:10.1186/s13006-017-0124-y]
26. Nagel EM, Howland MA, Pando C, Stang J, Mason SM, Fields DA, et al. Maternal psychological distress and lactation and breastfeeding outcomes: A narrative review. Clin Ther. 2022;44(2):215-27. [Link] [DOI:10.1016/j.clinthera.2021.11.007]
27. Righard L, Alade MO. Sucking technique and its effect on success of breastfeeding. Birth. 1992;19(4):185-9. [Link] [DOI:10.1111/j.1523-536X.1992.tb00399.x]
28. Aryani Y, Alyensi F, Fathunikmah F. Buku Proses Laktasi dan Teknik Pijat Oksitosin. Pekanbaru: Malay Culture; 2021. [Link]
29. Nelwatri H. The Effect of Early Breastfeeding Initiation (IMD) on Uterine Involution in Maternity Women in BPS Padang City in 2013. JIpteks Terapan. 2014;8(3):83-7. [Indonesian] [Link] [DOI:10.22216/jit.2014.v8i3.2]
30. Wahyuni I, Daulay NM. The Effect of Early Breastfeeding Initiation (IMD) on Uterine Involution in Maternity Women in BPS Padang City in 2013. Indonesian Health Sci J. 2020;5(1):9-14. [Indonesian] [Link]
31. Sendra E, Indriani D. The relationship between breastfeeding and uterine involution in physiological postpartum mothers at RSIA Aura Syifa, Kediri Regency. J Ilmu Kesehatan. 2017;5(2):64-71. [Indonesian] [Link] [DOI:10.32831/jik.v5i2.136]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








