Volume 10, Issue 4 (2022)
Health Educ Health Promot 2022, 10(4): 791-797 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadeqi-Arani A, Montazeralfaraj R, Sadeqi-Arani Z, Bahrami M, Rahati M, Askari R. Strategies for Improving the Standards of Health Promoting Hospitals: A case study in the Selected Hospitals in Iran. Health Educ Health Promot 2022; 10 (4) :791-797
URL: http://hehp.modares.ac.ir/article-5-64450-en.html
URL: http://hehp.modares.ac.ir/article-5-64450-en.html
1- Healthcare Management & Economics Department, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2- Management and Entrepreneurship Department, Humanities Faculty, University of Kashan, Kashan, Iran
3- Department of Healthcare Management, School of Management and Medical Informatics, Shiraz University of Medical Sciences, Shiraz, Iran
4- Healthcare Management Department, Faculty of Health, Kashan University of Medical Sciences, Kashan, Iran
2- Management and Entrepreneurship Department, Humanities Faculty, University of Kashan, Kashan, Iran
3- Department of Healthcare Management, School of Management and Medical Informatics, Shiraz University of Medical Sciences, Shiraz, Iran
4- Healthcare Management Department, Faculty of Health, Kashan University of Medical Sciences, Kashan, Iran
Full-Text [PDF 1687 kb]
(950 Downloads)
| Abstract (HTML) (1569 Views)


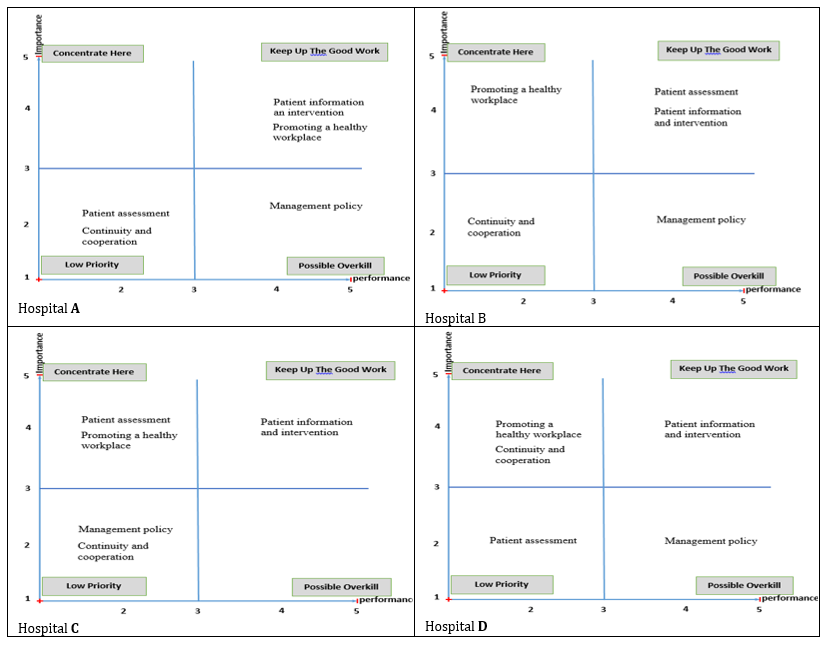
Figure 2) Importance-performance analysis matrix of the selected hospitals in Iran
Figure 2 reveals that the selected hospitals have critical and resource waste points.
According to the critical and resource waste points mentioned in Table 4, the focus group sessions were held, and improvement strategies were presented.
Regarding the critical points, the following solutions were presented based on the standards of HPHs:
1. Promoting a healthy workplace standard
• Holding educational courses on health promotion programs for staff
• Setting up diet and physical activity programs for staff
• Participation of staff in health promotion policies, evaluations, and decision making
2. Patient assessment standard
• Implementing guidelines on how to determine the status of smoking, nutrition, and mental and economic status of patients
• Preparing and implementing guidelines for assessing the health promotion needs of different groups of patients (patients with diabetes, asthma, chronic, surgery, rehabilitation, etc.)
• Assessing patients’ needs, such as cultural and social backgrounds
3. Continuity and cooperation standard
• Identifying and documenting the list of partners
(Partner Health Organizations)
• Establishing a schedule and regular sessions to meet partners
• Providing specific processes for information exchange with other partner organizations by the principles of confidentiality
The resource waste points occur in the following cases based on the standards of HPHs:
1. Management policy standard
• Expressing the concept of health promotion in the goals, missions, and programs of the hospital
• Participating in health promotion projects in line with the communication policies of the Ministry of Health
• Creating specific programs to evaluate the quality of health promotion activities in the hospital
Table 4) Critical and resource waste points in the importance-performance analysis matrix for the selected hospitals

Full-Text: (308 Views)
Introduction
The concept of health is very dynamic in that its scope and dimensions are increasing constantly [1]. The World Health Organization (WHO) defines health not only as the absence of disease or weakness but also as a complete physical, social, and mental condition [2].
Health promotion is a systematic approach to gaining control of variables that affect health, leading to population empowerment [3]. A health-promoting environment can have beneficial consequences for individuals, families, healthcare providers, and all communities [4]. Ways of disease prevention (prognosis) is one of the items in the field of patient information and education, which is important in the responsiveness of the health system [5].
From a health promotion perspective, hospitals are among the best platforms for providing health promotion and prevention services, so their most important mission is to change the treatment-oriented attitude to a health-oriented attitude [6]. A hospital is an integrated department of a social and medical organization, providing complete health care (both treatment and prevention) to the population [7].
The idea of Health-Promoting Hospitals (HPHs) was developed for the first time at the World Summit on Health Promotion in 1986 by the WHO [8].
The Network of Health Promoting Hospitals (HPH) was first established by the European Regional Office of the World Health Organization as a contextual approach for healthcare organizations to improve the quality of healthcare, the relationship between hospitals, society, and the environment and increase the satisfaction of patients, their families, and health workers [9].
In Iran, hospitals play only the traditional roles of diagnosis and treatment, and there are no defined structures to provide many health promotion services in hospitals and improve the health of the community and pursue sustainable and desirable results. The current state of health promotion in our country is unclear. However, some of these services, such as nutritional counseling, are limited to patients. But there is no defined structure for many services [8].
Health Promoting Hospitals (HPHs) seek to institutionalize the concept of prevention and health promotion among staff, empower patients in the hospital, and provide proper hospital interaction with the community, which improves the quality of services provided to people and communities [6]. Emphasizing the task of governments in providing public health, especially the vulnerable groups, is highly obvious [10]. In general, it is based on four dimensions, including 1) patient, 2) staff, 3) organization, and 4) community [7, 11]. According to the comprehensive framework to guide the strategic implementation of health promotion in hospitals and the further development of health standards, health promotion in hospitals is summarized in 18 key strategies. They consist of five standards including 1) management policy, 2) patient assessment, 3) patient information and intervention, 4) promoting a healthy workplace, and 5) continuity and cooperation [12-14].
One of the goals of HPHs is to provide the basis for quality management changes in hospitals. The results of establishing health promotion standards in hospitals include improving the usefulness and efficiency of the hospital, increasing the satisfaction and quality of life of patients and staff, reducing treatment complications, reducing frequent hospitalizations, decreasing treatment costs, reducing employee absenteeism, as well as improving clinical outcomes after treatment. It also reduces mortality, reduces personal satisfaction, reduces surgery complications, reduces the length of hospital stay, improves lifestyle, improves quality of health care, and increases the level of well-being of staff and patients [15].
Regarding the evaluation of health-promoting hospitals, many studies have been done with different tools [16-19]. There are different infrastructures in Iran to provide these services, such as human and legal infrastructures [20]. Therefore, the present study aims to investigate the strategies for improving the standards of HPHs in the selected hospitals in Iran using the Importance-Performance Analysis (IPA) matrix in 2021.
Instruments and Methods
The present study is a mixed-method study that involves tow quantitative and qualitative phases and was conducted in 2021. The first phase included two parts. First, the importance and performance of HPHs standards in the selected hospitals were evaluated using a questionnaire. The WHO questionnaire was used to assess HPH standards [21]. This questionnaire includes five standards with 40 questions, including management policy (9 questions), patient assessment (7 questions), patient information and intervention (6 questions), promoting a healthy workplace (10 questions), and continuity and cooperation (8 questions). The questions are scored based on a 5-point Likert scale (1 = very low, 2 = low, 3 = medium, 4 = high, 5 = very high). The reliability was measured based on Cronbach's alpha coefficient, which was 0.983. Then, the selected hospitals were compared based on the mean importance and performance of health-promoting standards using a one-way analysis of variance test. Finally, the importance-performance analysis matrix was plotted for each hospital, and critical points and resource waste were identified using the mean importance and performance of health-promoting standards. Importance-performance analysis matrix is a two-dimensional matrix, in which performance is located on the X-axis and importance on the Y-axis. When the mean score point of importance and the mean score point of performance meet, four connection areas are created. The first area (keep up the good work) is where the importance and performance are high. The second area (critical area) is where there is high importance and low performance. The third area (low priority) is where the importance and performance is low. The fourth area (resource waste) is where there is low importance and high performance.
In the second (qualitative) phase, according to the critical points and resource waste extracted from the importance-performance analysis matrix, solutions for improving these hospitals were presented using the focus group method. The statistical population of this study consisted of managers and officials of 4 selected hospitals in Iran, which were 65 people (using the census method), 61 people of whom participated in the study. The participants included chairman (n=3), manager (n=4), metron (n=4), quality improvement officer (n=4), quality improvement expert (n=1), patient safety expert (n=4), educational supervisor (n=4), expert providing patient education (n=4), head nurse (n=30), and environmental health expert (n=3). The selected hospitals included one government hospital and three non-government hospitals. The names of these hospitals are marked with letters A, B, C, and D due to confidentiality.
Importance-performance analysis matrix was performed as follows:
After extracting the critical points and resource waste points, an improvement solution was presented using the focus group method. Focus groups are organized discussion sessions, in which a group of people selected who can be considered as the focus of a thematic discussion. Then, these people represent their opinions and experiences through group interviews. The selection of focus group participants relies more on purposive sampling. Participants were selected based on the research design and their ability to cooperate. Given that the people completing the questionnaire were selected from the managers and officials of the hospital, the participants in the focus group were selected from the same people. Focus group sessions were conducted in three stages. The first stage was conceptualization. In this stage, the purpose of forming the group, the reason for implementing the focus group, the type of information in terms of their special importance, and the information requesting reference was explained to the participants. The second stage was the interview; the questions related to the interview were based on the critical points and resource waste extracted from the questionnaires, and the interviews were conducted accordingly. The third stage was data analysis and reporting. In this stage, the data were reviewed and analyzed, and improvement strategies were extracted. Figure 1 shows the working method of the article in the form of a flowchart.
Findings
The status of selected hospitals in terms of ownership, number of active beds, number of personnel, bed occupancy rate, and year of operation are presented in Table 1.

Figure 1) The method of providing an improvement solution
Table 1) The status of selected hospitals in terms of ownership, number of active beds, number of staff, bed occupancy rate, and year of operation

The mean performance scores of HPH standards in selected Iranian hospitals are presented in Table 2, which were significantly different from each other.
The mean importance scores of HPH standards in selected Iranian hospitals are presented in Table 3. The selected hospitals in Iran did not differ significantly in the mean score of the importance of patient management and evaluation policy standards. These hospitals were significantly different from other standards and general standards.
According to Tables 2 and 3, the importance-performance analysis matrix, critical points, and resource waste points of the selected hospitals are
presented in Figure 2.
The concept of health is very dynamic in that its scope and dimensions are increasing constantly [1]. The World Health Organization (WHO) defines health not only as the absence of disease or weakness but also as a complete physical, social, and mental condition [2].
Health promotion is a systematic approach to gaining control of variables that affect health, leading to population empowerment [3]. A health-promoting environment can have beneficial consequences for individuals, families, healthcare providers, and all communities [4]. Ways of disease prevention (prognosis) is one of the items in the field of patient information and education, which is important in the responsiveness of the health system [5].
From a health promotion perspective, hospitals are among the best platforms for providing health promotion and prevention services, so their most important mission is to change the treatment-oriented attitude to a health-oriented attitude [6]. A hospital is an integrated department of a social and medical organization, providing complete health care (both treatment and prevention) to the population [7].
The idea of Health-Promoting Hospitals (HPHs) was developed for the first time at the World Summit on Health Promotion in 1986 by the WHO [8].
The Network of Health Promoting Hospitals (HPH) was first established by the European Regional Office of the World Health Organization as a contextual approach for healthcare organizations to improve the quality of healthcare, the relationship between hospitals, society, and the environment and increase the satisfaction of patients, their families, and health workers [9].
In Iran, hospitals play only the traditional roles of diagnosis and treatment, and there are no defined structures to provide many health promotion services in hospitals and improve the health of the community and pursue sustainable and desirable results. The current state of health promotion in our country is unclear. However, some of these services, such as nutritional counseling, are limited to patients. But there is no defined structure for many services [8].
Health Promoting Hospitals (HPHs) seek to institutionalize the concept of prevention and health promotion among staff, empower patients in the hospital, and provide proper hospital interaction with the community, which improves the quality of services provided to people and communities [6]. Emphasizing the task of governments in providing public health, especially the vulnerable groups, is highly obvious [10]. In general, it is based on four dimensions, including 1) patient, 2) staff, 3) organization, and 4) community [7, 11]. According to the comprehensive framework to guide the strategic implementation of health promotion in hospitals and the further development of health standards, health promotion in hospitals is summarized in 18 key strategies. They consist of five standards including 1) management policy, 2) patient assessment, 3) patient information and intervention, 4) promoting a healthy workplace, and 5) continuity and cooperation [12-14].
One of the goals of HPHs is to provide the basis for quality management changes in hospitals. The results of establishing health promotion standards in hospitals include improving the usefulness and efficiency of the hospital, increasing the satisfaction and quality of life of patients and staff, reducing treatment complications, reducing frequent hospitalizations, decreasing treatment costs, reducing employee absenteeism, as well as improving clinical outcomes after treatment. It also reduces mortality, reduces personal satisfaction, reduces surgery complications, reduces the length of hospital stay, improves lifestyle, improves quality of health care, and increases the level of well-being of staff and patients [15].
Regarding the evaluation of health-promoting hospitals, many studies have been done with different tools [16-19]. There are different infrastructures in Iran to provide these services, such as human and legal infrastructures [20]. Therefore, the present study aims to investigate the strategies for improving the standards of HPHs in the selected hospitals in Iran using the Importance-Performance Analysis (IPA) matrix in 2021.
Instruments and Methods
The present study is a mixed-method study that involves tow quantitative and qualitative phases and was conducted in 2021. The first phase included two parts. First, the importance and performance of HPHs standards in the selected hospitals were evaluated using a questionnaire. The WHO questionnaire was used to assess HPH standards [21]. This questionnaire includes five standards with 40 questions, including management policy (9 questions), patient assessment (7 questions), patient information and intervention (6 questions), promoting a healthy workplace (10 questions), and continuity and cooperation (8 questions). The questions are scored based on a 5-point Likert scale (1 = very low, 2 = low, 3 = medium, 4 = high, 5 = very high). The reliability was measured based on Cronbach's alpha coefficient, which was 0.983. Then, the selected hospitals were compared based on the mean importance and performance of health-promoting standards using a one-way analysis of variance test. Finally, the importance-performance analysis matrix was plotted for each hospital, and critical points and resource waste were identified using the mean importance and performance of health-promoting standards. Importance-performance analysis matrix is a two-dimensional matrix, in which performance is located on the X-axis and importance on the Y-axis. When the mean score point of importance and the mean score point of performance meet, four connection areas are created. The first area (keep up the good work) is where the importance and performance are high. The second area (critical area) is where there is high importance and low performance. The third area (low priority) is where the importance and performance is low. The fourth area (resource waste) is where there is low importance and high performance.
In the second (qualitative) phase, according to the critical points and resource waste extracted from the importance-performance analysis matrix, solutions for improving these hospitals were presented using the focus group method. The statistical population of this study consisted of managers and officials of 4 selected hospitals in Iran, which were 65 people (using the census method), 61 people of whom participated in the study. The participants included chairman (n=3), manager (n=4), metron (n=4), quality improvement officer (n=4), quality improvement expert (n=1), patient safety expert (n=4), educational supervisor (n=4), expert providing patient education (n=4), head nurse (n=30), and environmental health expert (n=3). The selected hospitals included one government hospital and three non-government hospitals. The names of these hospitals are marked with letters A, B, C, and D due to confidentiality.
Importance-performance analysis matrix was performed as follows:
After extracting the critical points and resource waste points, an improvement solution was presented using the focus group method. Focus groups are organized discussion sessions, in which a group of people selected who can be considered as the focus of a thematic discussion. Then, these people represent their opinions and experiences through group interviews. The selection of focus group participants relies more on purposive sampling. Participants were selected based on the research design and their ability to cooperate. Given that the people completing the questionnaire were selected from the managers and officials of the hospital, the participants in the focus group were selected from the same people. Focus group sessions were conducted in three stages. The first stage was conceptualization. In this stage, the purpose of forming the group, the reason for implementing the focus group, the type of information in terms of their special importance, and the information requesting reference was explained to the participants. The second stage was the interview; the questions related to the interview were based on the critical points and resource waste extracted from the questionnaires, and the interviews were conducted accordingly. The third stage was data analysis and reporting. In this stage, the data were reviewed and analyzed, and improvement strategies were extracted. Figure 1 shows the working method of the article in the form of a flowchart.
Findings
The status of selected hospitals in terms of ownership, number of active beds, number of personnel, bed occupancy rate, and year of operation are presented in Table 1.

Figure 1) The method of providing an improvement solution
Table 1) The status of selected hospitals in terms of ownership, number of active beds, number of staff, bed occupancy rate, and year of operation

The mean performance scores of HPH standards in selected Iranian hospitals are presented in Table 2, which were significantly different from each other.
The mean importance scores of HPH standards in selected Iranian hospitals are presented in Table 3. The selected hospitals in Iran did not differ significantly in the mean score of the importance of patient management and evaluation policy standards. These hospitals were significantly different from other standards and general standards.
According to Tables 2 and 3, the importance-performance analysis matrix, critical points, and resource waste points of the selected hospitals are
presented in Figure 2.
Table 2) Performance scores (mean±SD) of HPHs standards in the selected hospitals in Iran

Table 3) Importance scores (mean±SD) of HPHs standards in the selected hospitals in Iran

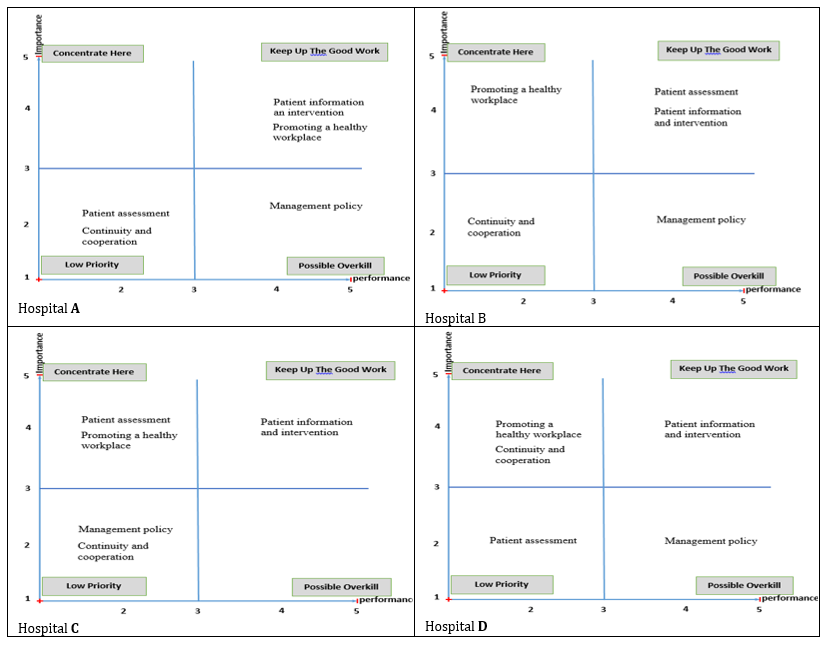
Figure 2) Importance-performance analysis matrix of the selected hospitals in Iran
Figure 2 reveals that the selected hospitals have critical and resource waste points.
According to the critical and resource waste points mentioned in Table 4, the focus group sessions were held, and improvement strategies were presented.
Regarding the critical points, the following solutions were presented based on the standards of HPHs:
1. Promoting a healthy workplace standard
• Holding educational courses on health promotion programs for staff
• Setting up diet and physical activity programs for staff
• Participation of staff in health promotion policies, evaluations, and decision making
2. Patient assessment standard
• Implementing guidelines on how to determine the status of smoking, nutrition, and mental and economic status of patients
• Preparing and implementing guidelines for assessing the health promotion needs of different groups of patients (patients with diabetes, asthma, chronic, surgery, rehabilitation, etc.)
• Assessing patients’ needs, such as cultural and social backgrounds
3. Continuity and cooperation standard
• Identifying and documenting the list of partners
(Partner Health Organizations)
• Establishing a schedule and regular sessions to meet partners
• Providing specific processes for information exchange with other partner organizations by the principles of confidentiality
The resource waste points occur in the following cases based on the standards of HPHs:
1. Management policy standard
• Expressing the concept of health promotion in the goals, missions, and programs of the hospital
• Participating in health promotion projects in line with the communication policies of the Ministry of Health
• Creating specific programs to evaluate the quality of health promotion activities in the hospital
Table 4) Critical and resource waste points in the importance-performance analysis matrix for the selected hospitals

Discussion
Based on our current knowledge about the importance of lifestyle-related factors in the treatment and prognosis of diseases, all hospitals should create policies, counseling services, education, and support for health promotion as an inseparable part of the patient's disease course as well as the staff [22].
The results of health promotion refer to the adjustment of personal, social, and environmental factors in improving people's control over health indicators (such as health awareness, activity and social impact, healthy society policy, and organizational culture). Intermediate outcomes refer to changes in health indicators (such as lifestyle, access to health services, and reduction of environmental hazards) [23].
This study indicated that in the management policy standard, the mean performance score of non-government hospitals was significantly higher than government hospitals, which is not in line with the studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25]. Moreover, in the patient assessment standard, the performance score of non-government hospitals was significantly higher than government hospitals, which is not consistent with the studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25]. In the patient information and intervention standard, the performance score of non-government hospitals was significantly higher than government hospitals. In studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25], the performance score of non-government hospitals in the patient information and intervention standard was higher than the government hospitals, which is consistent with the present study, but the difference was not significant, which is not in line with the present study.
The present study revealed that in promoting a healthy workplace standard, the mean performance score of non-government hospitals was significantly higher than government hospitals, which is not in line with the study by Yaghoubi and Javadi [24]. In their study, this difference was not significant, but it was in line with the study by Pezeshki et al. [25]. In their study, the performance score of non-government hospitals was significantly higher than government hospitals.
In the continuity and cooperation standard, the present study showed that the mean performance score of non-government hospitals was significantly higher than government hospitals, which is consistent with Yaghoubi and Javadi’s study but is not in line with Pezeshki et al.’s study [24, 25].
The study results indicate that in all standards of HPHs, the mean performance score of non-government hospitals was higher than government hospitals, which is consistent with the studies by Yaghoubi and Javadi and Pezeshki et al. [24, 25].
The researchers did not find any study on the importance of HPHs standards as well as in the field of importance-performance analysis matrix of HPHs standards.
In similar studies, only the performance of hospitals has been examined, but its importance has not been examined from the perspective of hospital managers and officials. However, in the present study, the importance and performance were examined, and in this regard, the present article is innovative. Furthermore, the improvement strategy was presented using the importance-performance analysis matrix, which has not been used in similar studies. The lack of related studies and insufficient sample size for statistical measurement were the most important limitations of this study. Investigating the factors affecting the implementation of health promotion hospital standards, also the impact of implementing the standards of health promoting hospitals to control the spread of the Covid-19 disease are suggested for further studies.
Given that the standards of continuity and cooperation, promoting a healthy workplace, and patient assessment were among the critical points of the studied hospitals, some cases are recommended, such as creating a list of partner health organizations and holding regular sessions with them to plan for providing the best patient care, setting up appropriate educational programs to promote staff’s health, staff participation in hospital policies and decision making, creating and reviewing guidelines on how to determine the status of smoking, nutrition, and mental and economic status of patients, and determining and evaluating the health promotion needs of different groups of patients. Considering that the management policy standard was one of the resource waste points of the studied hospitals, the most significant resource waste occurs in expressing the concept of health promotion in the goals and mission statement of the hospital and documentation in each department for regular audit of health promotion policy.
Conclusion
The standards of continuity and cooperation, promoting a healthy workplace, and patient assessment are the critical points of the studied hospitals. Also, the management policy standard is one of the resource waste points of the studied hospitals, and the most significant resource waste occurs in expressing the concept of health promotion in the goals and mission statement of the hospital and documentation in each department for regular audit of health promotion policy.
Acknowledgments: We are grateful to the leadership and management staff of hospitals A, B, C, and D for supporting the present study.
Ethical Permission: This research was approved by the ethics committee with the code IR.SSU.SPH.REC.1399.104.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Sadeqi-Arani A (First Author), Main Researcher (30%); Montazeralfaraj R (Second Author), Assistant Researcher/Methodologist (20%); Sadeqi-Arani Z (Third Author), Introduction Writer (10%); Bahrami MA (Fourth Author), Discussion Writer (10%); Rahati M (Fifth Author), Statistical Analyst (10%); Askari R (Sixth Author), Assistant Researcher (20%)
Funding: This research is the result of a master's thesis
Based on our current knowledge about the importance of lifestyle-related factors in the treatment and prognosis of diseases, all hospitals should create policies, counseling services, education, and support for health promotion as an inseparable part of the patient's disease course as well as the staff [22].
The results of health promotion refer to the adjustment of personal, social, and environmental factors in improving people's control over health indicators (such as health awareness, activity and social impact, healthy society policy, and organizational culture). Intermediate outcomes refer to changes in health indicators (such as lifestyle, access to health services, and reduction of environmental hazards) [23].
This study indicated that in the management policy standard, the mean performance score of non-government hospitals was significantly higher than government hospitals, which is not in line with the studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25]. Moreover, in the patient assessment standard, the performance score of non-government hospitals was significantly higher than government hospitals, which is not consistent with the studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25]. In the patient information and intervention standard, the performance score of non-government hospitals was significantly higher than government hospitals. In studies by Yaghoubi and Javadi [24] and Pezeshki et al. [25], the performance score of non-government hospitals in the patient information and intervention standard was higher than the government hospitals, which is consistent with the present study, but the difference was not significant, which is not in line with the present study.
The present study revealed that in promoting a healthy workplace standard, the mean performance score of non-government hospitals was significantly higher than government hospitals, which is not in line with the study by Yaghoubi and Javadi [24]. In their study, this difference was not significant, but it was in line with the study by Pezeshki et al. [25]. In their study, the performance score of non-government hospitals was significantly higher than government hospitals.
In the continuity and cooperation standard, the present study showed that the mean performance score of non-government hospitals was significantly higher than government hospitals, which is consistent with Yaghoubi and Javadi’s study but is not in line with Pezeshki et al.’s study [24, 25].
The study results indicate that in all standards of HPHs, the mean performance score of non-government hospitals was higher than government hospitals, which is consistent with the studies by Yaghoubi and Javadi and Pezeshki et al. [24, 25].
The researchers did not find any study on the importance of HPHs standards as well as in the field of importance-performance analysis matrix of HPHs standards.
In similar studies, only the performance of hospitals has been examined, but its importance has not been examined from the perspective of hospital managers and officials. However, in the present study, the importance and performance were examined, and in this regard, the present article is innovative. Furthermore, the improvement strategy was presented using the importance-performance analysis matrix, which has not been used in similar studies. The lack of related studies and insufficient sample size for statistical measurement were the most important limitations of this study. Investigating the factors affecting the implementation of health promotion hospital standards, also the impact of implementing the standards of health promoting hospitals to control the spread of the Covid-19 disease are suggested for further studies.
Given that the standards of continuity and cooperation, promoting a healthy workplace, and patient assessment were among the critical points of the studied hospitals, some cases are recommended, such as creating a list of partner health organizations and holding regular sessions with them to plan for providing the best patient care, setting up appropriate educational programs to promote staff’s health, staff participation in hospital policies and decision making, creating and reviewing guidelines on how to determine the status of smoking, nutrition, and mental and economic status of patients, and determining and evaluating the health promotion needs of different groups of patients. Considering that the management policy standard was one of the resource waste points of the studied hospitals, the most significant resource waste occurs in expressing the concept of health promotion in the goals and mission statement of the hospital and documentation in each department for regular audit of health promotion policy.
Conclusion
The standards of continuity and cooperation, promoting a healthy workplace, and patient assessment are the critical points of the studied hospitals. Also, the management policy standard is one of the resource waste points of the studied hospitals, and the most significant resource waste occurs in expressing the concept of health promotion in the goals and mission statement of the hospital and documentation in each department for regular audit of health promotion policy.
Acknowledgments: We are grateful to the leadership and management staff of hospitals A, B, C, and D for supporting the present study.
Ethical Permission: This research was approved by the ethics committee with the code IR.SSU.SPH.REC.1399.104.
Conflict of Interests: The authors declare no conflict of interest.
Authors’ Contribution: Sadeqi-Arani A (First Author), Main Researcher (30%); Montazeralfaraj R (Second Author), Assistant Researcher/Methodologist (20%); Sadeqi-Arani Z (Third Author), Introduction Writer (10%); Bahrami MA (Fourth Author), Discussion Writer (10%); Rahati M (Fifth Author), Statistical Analyst (10%); Askari R (Sixth Author), Assistant Researcher (20%)
Funding: This research is the result of a master's thesis
Article Type: Descriptive & Survey |
Subject:
Health Education and Health Behavior
Received: 2022/08/26 | Accepted: 2022/11/26 | Published: 2022/12/13
Received: 2022/08/26 | Accepted: 2022/11/26 | Published: 2022/12/13
References
1. Damari B, Nasehei A, Vosoogh Moghaddam A. What should we do for improving Iranian social health? Situational analysis, national strategies and role of ministry of health and medical education. J Sch Public Health Instit Public Health Res. 2013;11(1):45-58. [Persian] [Link]
2. Kumar S, Preetha G. Health promotion: an effective tool for global health. Indian J Community Med. 2012;37(1):5-12. [Link] [DOI:10.4103/0970-0218.94009]
3. Weiss D, Lillefjell M, Magnus E. Facilitators for the development and implementation of health promoting policy and programs-a scoping review at the local community level. BMC Public Health. 2016;16(140):15-1. [Link] [DOI:10.1186/s12889-016-2811-9]
4. Mahmoodi H, Shaghaghi A. Barriers and gateways to adapt standards of the Health Promoting Hospitals: a rigorous consolidation of the global research evidence. Int J Health Promot Educ. 2019;57(5):235-55. [Link] [DOI:10.1080/14635240.2019.1610025]
5. Askari R, Arab M, Rashidian A, Akbari-Sari A, Hosseini SM, Gharaee H. Designing Iranian model to assess the level of health system responsiveness. Iran Red Crescent Med J. 2016;20;18(3):e24527. [Link] [DOI:10.5812/ircmj.24527]
6. Estebsari F, Mostafaei D, Taghdisi M, Ghavami M. Health promoting hospitals: concepts, indexes and standards. Iran J Health Educ Health Promot. 2016;3(4):281-6. [Persian] [Link]
7. Groene O, Jorgensen S, Fugleholm AM, Møller L, Garcia‐Barbero M. Standards for health promotion in hospitals: development and pilot test in nine European countries. Int J of Health Care Qual Assur Inc Leadersh Health Serv. 2005;18(4-5):300-7. [Link] [DOI:10.1108/09526860510602569]
8. Askari R, Mir Hosseini R, Montazeral Faraj R, Jambarsang S. Evaluation of the effect of implementing health promoting hospitals program on the level of attitude of cardiac patients. Health Educ Health Promot. 2022;10(2):341-34. [Link]
9. Institute of Medicine (US) Committee on Quality of Health Care in America, Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: Building a safer health system. Washington (DC): National Academies Press (US); 2000. [Link]
10. Pakdaman M, Geravandi S, Askari R, Askarishahi M, Afzali HR. The effect of macroeconomic indicators on health-care expenditure in Iran. J Edu Health Promot 2019;8:123. [Link]
11. Yaghoubi M, Javadi M, Bahadori M. Designing a health promoting hospital: Case study Isfahan University of Medical Sciences. Health Inf Manage. 2014;10(7):1014-22. [Persian] [Link]
12. Groene O. Implementing health promotion in hospitals: manual and self-assessment forms [Internet]. Geneva: World Health Organization. Regional Office for Europe; 2006 [cited 2020 Sep 17]. Available from: https://apps.who.int/iris/handle/10665/107737 [Link]
13. Seif Rabiei MA, Khanlarzadeh E, Nikpajouh A, Doaee M, Sanaei Z. Evaluating health promotion standards at the Farshchian heart center of Hamadan, Iran. Hosp Pract. 2020;48(5):282-8. [Link] [DOI:10.1080/21548331.2020.1788819]
14. Al Aufa B. Management process of health promoting hospital in a private hospital, Lamongan, East Java. 3rd International Conference on Vocational Higher Education (ICVHE 2018). Atlantis Press; 2020. [Link] [DOI:10.2991/assehr.k.200331.154]
15. Naderi S, Amiri M, Riahi L. Effect of health promoting hospitals' standards on hospital performance A Case Study in Fatemieh Hospital in Shahrod. J Hosp. 2015;14(2):101-9. [Persian] [Link]
16. Onegh S, Vahdat S, Mahfozpour S. Determining the readiness of hospitals in Golestan Province in Terms of Management in Establishing Standards for Health Promotion Hospitals. J Healthcare Manag. 2018;8(4):29-38. [Persian] [Link]
17. Yaghoubi M, Javadi M, Bahadori M, Ravangard R. Health promoting hospitals model in Iran. Iran J Public Health. 2016;45(3):362-9. [Link]
18. Kozica SL, Lombard CB, Hider K, Harrison CL, Teede HJ. Developing comprehensive health promotion evaluations: a methodological review. MOJ Public Health. 2014;1(1):39-48. [Link] [DOI:10.15406/mojph.2014.01.00007]
19. Mansouri Z, Vahdat S, MasoudiAsl I, Hessam S, Mahfoozpour S, Mohammadi R. Developing and psychometrics "Evaluation criteria for health promoting hospitals scale". J Health Promot Manag. 2021;10(1):103-13. [Persian] [Link]
20. Heydarnia M, Abachzadeh K, Damari B, Azargashb E, Vosoughmoghaddam A. Study of expert opinion on health promotive services for patients at hospitals affiliated to Shahid Beheshti University of Medical Science. Pajoohande. 2009;14(4):183-90. [Persian] [Link]
21. Groene O, Alonso J, Klazinga N. Development and validation of the WHO self-assessment tool for health promotion in hospitals: results of a study in 38 hospitals in eight countries. Health Promot Int. 2010;25(2):221-9. [Link] [DOI:10.1093/heapro/daq013]
22. Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomized clinical trial. Lancet. 2002;359(9301):114-7. [Link] [DOI:10.1016/S0140-6736(02)07369-5]
23. Nutbeam D. Evaluating Health Promotion-Progress, Problems and solutions. Health Promot Int. 1998;13(1):27-44. [Link] [DOI:10.1093/heapro/13.1.27]
24. Yaghoubi M, Javadi M. Health promoting hospitals in Iran: How it is. J Educ Health Promot. 2013;2(41):1-5. [Link] [DOI:10.4103/2277-9531.115840]
25. Pezeshki MZ, Alizadeh M, Nikpajouh A, Ebadi A, Nohi S, Soleimanpour M. Evaluation of the health promotion standards in governmental and non-governmental hospitals in East-Azerbaijan. Med J Islam Repub Iran. 2019;33:113 [Link] [DOI:10.47176/mjiri.33.113]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






