Volume 10, Issue 3 (2022)
Health Educ Health Promot 2022, 10(3): 483-487 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kadhum Zeidan M, Hassoon S, Shatha Ahmed M. Polycystic Ovary Syndrome Risk Factors among Women in Baghdad: A Case-Control study. Health Educ Health Promot 2022; 10 (3) :483-487
URL: http://hehp.modares.ac.ir/article-5-62991-en.html
URL: http://hehp.modares.ac.ir/article-5-62991-en.html
1- Community Health Department, College of Health and Medical Technologies, Middle Technology University, Baghdad, Iraq
2- Medical Technical Institute, Al-Mansor University of Middle Technology
2- Medical Technical Institute, Al-Mansor University of Middle Technology
Full-Text [PDF 859 kb]
(4179 Downloads)
| Abstract (HTML) (1918 Views)
Full-Text: (5959 Views)
Introduction
PCOS, or polycystic ovarian syndrome, is a hormonal disorder that affects women of childbearing age and causes many physical and mental symptoms [1]. PCOS affects 5% to 10% of women throughout their reproductive years [2]. Although some women with PCOS have normal menstrual cycles, the majority of them suffer from monthly irregularities such as oligomenorrhea, amenorrhea, and prolonged irregular bleeding [3].
Women with PCOS frequently exhibit hyperandrogenism, infertility, and hirsutism as clinical symptoms [4, 5]. Also, acne is another marker of hyperandrogenism but is less specific than hirsutism. The prevalence of acne has been reported to be 15%–30% in PCOS adult women [6]. Moreover, 40% of women with PCOS have infertility [7]. Also, spontaneous abortion is observed more frequently in PCOS women [8].
Some metabolic changes of PCOS are blood lipids, insulin resistance, inflammation, obesity, increased oxidative stress, and changes in hormones [9]. Even though no one knows for sure what causes PCOS, it seems that both genetics and the environment play a role [9].
One of the risk factors of PCOS is obesity [10]. It is reported that increased weight often intensifies the development of PCOS [11]. Obese women had a 28.3% prevalence of PCOS [12]. A healthy lifestyle in women with PCOS results in decreased weight and abdominal fat, reduced testosterone, and improved insulin resistance [13]. PCOS increases the risk of type 2 diabetes, dyslipidemia, and heart disease in women [13]. PCOS women have four times the incidence of endometrial cancer, according to cohort research [14].
Another risk factor for PCOS is having a family history of the condition. Genetic factors can be seen in the increased frequency of PCOS or its symptoms among first-degree relatives [15]. Patients with PCOS are also more likely to develop dyslipidemia. An elevated triglyceride level and decreased (HDL-C), as well as increased (LDLC) levels, are all signs of lipid disorders (LDL-C) [16]. PCOS's economic impact on society is expected to be roughly $3.7 billion per year in 2020 based on the expenses of diagnosis and reproductive endocrine morbidities, but not pregnancy-related or long-term morbidities [17].
Treatment for women suffering from PCOS is based on the symptoms, although no specified treatment for PCOS is determined. Treatment options include dietary and exercise modifications, as well as weight loss [18]. An oral contraceptive pill may regulate menstruation and reduce hirsutism and acne. Metformin and antiandrogens also have a role in PCOS [19]. The majority of women with PCOS are overweight or obese, and metabolic issues associated with obesity typically coexist with PCOS, at least in part. It is still unclear, despite the substantial study, whether the polycystic ovarian syndrome is a risk factor for metabolic diseases and cardiovascular disease. Due to the lack of research identifying the risk factors of the polycystic ovarian syndrome in Baghdad, the purpose of this study was to determine the risk factors of polycystic ovary syndrome among women in Baghdad to inform judgments for early screening and preventative measures against PCOS.
Material and Methods
This case-control study was done on women referring to the hospitals of Baghdad from 1 Sep 2019 to 15 Dec 2019. The non-probability convenient approach was used to collect the samples. And the sample size was determined using Raosoft's sample size calculator:
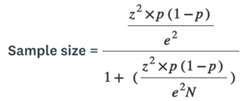
z= Standard critical of 95% confidence level = 1.96;
p= Probability of knowledge (0.5);
e = Margin of error (0.05);
N= Population size
Based on this computation, 170 people comprised the overall sample. We add 15% (25.5) to ensure compensation for the loss or refusal to participate by some respondents, so the total number becomes 25.5+170=195.5≈200 to more accurate. Participants were chosen from Baghdad Hospital in the medical city because it is the main hospital for provides services to patients with (PCOS). PCOS was diagnosed using the Rotterdam ESHRE/ASRM PCOS Consensus Workshop Group 2003. If two of the following conditions were met, PCOS was diagnosed: There are several clinical and biochemical symptoms of hyperandrogenism (hirsutism), including acne or alopecia, as well as an increased testosterone and/or androstenedione, as well as a polycystic ovaries (PCOS) diagnosis [20]. Inclusion criteria were all women of reproductive age referring to the Gynecology Clinic of the hospitals who had willing to participate in the study. Pregnant and postmenopausal women, those on hormone therapy, and those who refused to participate in the study due to their refusal were eliminated, as were individuals with cancerous tumors, cardiovascular illness, severe organic disease, and psychological disorders.
A paper-based questionnaire developed by a researcher was used to conduct an interview. The research questionnaire consisted of four parts which were distributed as follows:
Part I: Age, degree of education, and employment are socio-demographic variables.
Part II: Patients' lifestyle and biomedical factors which include physical activity (regular physical exercise), family history of PCOS; diet (unhealthy diet, for example, pickled food, coarse food, drink, and salty food), menstrual history (regular or irregular menstruation), a drug used (contraception drugs, cortisone, Clomid).
Part III: Anthropometric measures were taken, including body mass, height, and waist circumference (WC). Body weight (kg) and height (cm) were measured by standing position and without shoes, Anthropometric measurements for measuring height, and waist circumference, using the metric tape, and measuring weight utilizing an electronic scale. Classification of participants’ BMI according to World Health Organization (WHO) guidelines for Asian populations was as follow:(<18.5-22.5 kg/m2 underweight, 23-24.9 kg/m2 normal weight, 25-29.9 kg/m2 overweight and >30 kg/m2 obese) [21].
Part IV: Clinical symptoms of PCOS.
Ethical approval and all administrative agreements were obtained from the College of Health and Medical Technology/ Baghdad/ Community Health Department and the research committee at Middle Technical University. Protecting the participant's values and dignity is one of the most fundamental pre-collection concepts.
SPSS version 22 was used to analyze data, and the Chi-square test was applied to assess the data. The level of significance was fixed at P< 0.05. To assess the probability of PCOS, odds ratios and confidence intervals of 95% were calculated.
Findings
This research involved 200 women in total. Table 1 displays the socio-demographic data of the study's case and control populations. Table 1 showed that 46% of the case group and 45% of the control group were in the age group of 21-25 years. Poly Cystic Ovarian Syndrome was shown to be more common in women between the ages of 21 and 25. In terms of BMI, most of the patients with PCOS were overweight, while most of the control group had normal BMI. The results of the univariate analysis of risk factors for PCOS in Table 1 showed that age, BMI, educational level, occupational status, and waist circumference were all significantly related to PCOS.
The results of Table 2 showed that a high percentage of the case group had a family history of PCOS, while 8% of the control group reported a family history of PCOS (p<0.05). In addition, 46% of the case group had a diet, whereas only 23% of the control group did; this difference was statistically significant. However, there was no statistically significant difference between the two groups in terms of regular exercise or having children (p<0.05).
Table 1) Distribution of Socio-demographic characteristics, BMI, and Waist circumference in the case and control groups

Table 2) Results of the probability of PCOS in the case and control group

Discussion
The cause of PCOS is still unknown because of its complexity. PCOS is caused by the interplay of hereditary and environmental variables [22]. PCOS leads to changes in lifestyle, increased stress, and reduced cycle impairment. The most effective treatment for PCOS is to prevent its development and diagnose its risk factors to prevention of serious long-term complications [23]. The goal of this study was to find out what makes women in Baghdad more likely to get polycystic ovary syndrome.
The majority of women in both groups were between 21 and 25 years of age, demonstrating that age is a key risk factor for PCOS. Similar findings were observed in another study, which revealed that the majority of PCOS patients (34.2%) were between the ages of 21 and 25 [24]. A similar experiment in Bhopal had equivalent results [25].
The findings of the current investigation reflected that educational level is significantly related to PCOS which is consistent with the findings of the study in 2015 that reported educational level is a fundamental risk factor for PCOS [26], however in their study, most women had an educational level of primary school and in our study, most participants had an educational level of college and higher. This disparity is likely attributable to the fact that females in Iraq may not receive a PCOS diagnosis during their early pubertal years.
The findings of the current study indicated that housewives were a more risky group for PCOS; this result was confirmed in the study done in Pakistan [27]. This is because housewives women are more interested to diagnose the cause of delayed pregnancy or menstrual disorders. Moreover, a family history of PCOS was detected to be a highly significant risk factor for PCOS. Some studies reported similar findings [28-30].
According to the findings of the current study, an unhealthy diet including pickled food, coarse food, drink, and salty food was the other significant risk factor for PCOS (p=0.001). This finding was in agreement with the study conducted in China [31]. Unhealthy foods with high amounts of calories cause an imbalance of hormones which increases the weight.
Also, the present study showed that physical exercise was not a significant risk factor for the development of PCOS. This result is in agreement with the investigation performed in UAE [28]. Although the result was not consistent with the study's conclusion that a lack of physical activity was statistically related to PCOS [26]. Uneven distribution of body fat is caused by a lack of physical activity, which is a significant risk factor for central obesity. We observed that overweight and obese participants were riskier for the development of PCOS compared to normal BMI women. This result is following the study done in UAE [28], and the study done in Spain [12]. This is likely due to a lack of physical activity and bad eating habits. In addition to central obesity and overweight, an increased waist circumference is an additional risk factor for the development of PCOS. Our investigation displayed that PCOS was significantly associated with waist circumference (<80cm). This finding is in agreement with the investigation performed in UAE [28]. It is mostly caused to excessive intake of fast food, unhealthy eating habits, and a poor diet.
Irregular menstrual cycle and infertility are highly significant risk factors for PCOS. A high index for the diagnosis of PCOS in teens with irregular menstrual cycles was reported in Nicandri's study, which showed a similar outcome [32]. In the current study, there was a highly significant association between the use of Clomid and PCOS. The result is in agreement with the study done in the USA [33].
According to the results of this study, recommended to establish more health programs regarding early diagnosis, effective treatment, and follow-up of patients, use a different type of media to stimulate public awareness about the risk factors of PCOS, improve the programs of health education about maintaining a healthy weight, establish health educational programs about reducing high carbohydrates and low-fat foods, designing programs about regular physical activity, and regular follow-up.
One problem with this study is that it didn't look at some risk factors for PCOS, like being married or having a family history of diabetes. In the next study, we should make the project design even better.
Conclusion
Targeting the high-risk factors of age, educational level, occupational status, BMI, waist circumference, family history, diet, regular menstrual cycle, and Clomid used, we should perform early screening, diagnosis, and treatment of POCS and identify its risk factors to decrease the incidence of PCOS and progress its prognosis.
Acknowledgments: The authors like to express their gratitude to all of the women who participated in this study.
Ethical Permissions: The researchers conducted the necessary agreements ethics committee from the College of Health and Medical Technology/ Baghdad/ and then the researchers informed the participants that the responses will be used for the research purpose only.
Conflicts of Interests: There are no conflicts of interest.
Authors’ Contributions: Kadhum Zeidan MA (First Author), Introduction Writer/Methodologist/Main Researcher /Statistical Analyst/Discussion Writer (75%); Hassoon SM (Second Author), Assistant Researcher/Statistical Analyst (15%); Shatha Ahmed MA (Third Author), Introduction Writer/Assistant Researcher (10%)
Funding/Support: None declared.
PCOS, or polycystic ovarian syndrome, is a hormonal disorder that affects women of childbearing age and causes many physical and mental symptoms [1]. PCOS affects 5% to 10% of women throughout their reproductive years [2]. Although some women with PCOS have normal menstrual cycles, the majority of them suffer from monthly irregularities such as oligomenorrhea, amenorrhea, and prolonged irregular bleeding [3].
Women with PCOS frequently exhibit hyperandrogenism, infertility, and hirsutism as clinical symptoms [4, 5]. Also, acne is another marker of hyperandrogenism but is less specific than hirsutism. The prevalence of acne has been reported to be 15%–30% in PCOS adult women [6]. Moreover, 40% of women with PCOS have infertility [7]. Also, spontaneous abortion is observed more frequently in PCOS women [8].
Some metabolic changes of PCOS are blood lipids, insulin resistance, inflammation, obesity, increased oxidative stress, and changes in hormones [9]. Even though no one knows for sure what causes PCOS, it seems that both genetics and the environment play a role [9].
One of the risk factors of PCOS is obesity [10]. It is reported that increased weight often intensifies the development of PCOS [11]. Obese women had a 28.3% prevalence of PCOS [12]. A healthy lifestyle in women with PCOS results in decreased weight and abdominal fat, reduced testosterone, and improved insulin resistance [13]. PCOS increases the risk of type 2 diabetes, dyslipidemia, and heart disease in women [13]. PCOS women have four times the incidence of endometrial cancer, according to cohort research [14].
Another risk factor for PCOS is having a family history of the condition. Genetic factors can be seen in the increased frequency of PCOS or its symptoms among first-degree relatives [15]. Patients with PCOS are also more likely to develop dyslipidemia. An elevated triglyceride level and decreased (HDL-C), as well as increased (LDLC) levels, are all signs of lipid disorders (LDL-C) [16]. PCOS's economic impact on society is expected to be roughly $3.7 billion per year in 2020 based on the expenses of diagnosis and reproductive endocrine morbidities, but not pregnancy-related or long-term morbidities [17].
Treatment for women suffering from PCOS is based on the symptoms, although no specified treatment for PCOS is determined. Treatment options include dietary and exercise modifications, as well as weight loss [18]. An oral contraceptive pill may regulate menstruation and reduce hirsutism and acne. Metformin and antiandrogens also have a role in PCOS [19]. The majority of women with PCOS are overweight or obese, and metabolic issues associated with obesity typically coexist with PCOS, at least in part. It is still unclear, despite the substantial study, whether the polycystic ovarian syndrome is a risk factor for metabolic diseases and cardiovascular disease. Due to the lack of research identifying the risk factors of the polycystic ovarian syndrome in Baghdad, the purpose of this study was to determine the risk factors of polycystic ovary syndrome among women in Baghdad to inform judgments for early screening and preventative measures against PCOS.
Material and Methods
This case-control study was done on women referring to the hospitals of Baghdad from 1 Sep 2019 to 15 Dec 2019. The non-probability convenient approach was used to collect the samples. And the sample size was determined using Raosoft's sample size calculator:
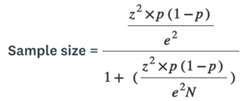
z= Standard critical of 95% confidence level = 1.96;
p= Probability of knowledge (0.5);
e = Margin of error (0.05);
N= Population size
Based on this computation, 170 people comprised the overall sample. We add 15% (25.5) to ensure compensation for the loss or refusal to participate by some respondents, so the total number becomes 25.5+170=195.5≈200 to more accurate. Participants were chosen from Baghdad Hospital in the medical city because it is the main hospital for provides services to patients with (PCOS). PCOS was diagnosed using the Rotterdam ESHRE/ASRM PCOS Consensus Workshop Group 2003. If two of the following conditions were met, PCOS was diagnosed: There are several clinical and biochemical symptoms of hyperandrogenism (hirsutism), including acne or alopecia, as well as an increased testosterone and/or androstenedione, as well as a polycystic ovaries (PCOS) diagnosis [20]. Inclusion criteria were all women of reproductive age referring to the Gynecology Clinic of the hospitals who had willing to participate in the study. Pregnant and postmenopausal women, those on hormone therapy, and those who refused to participate in the study due to their refusal were eliminated, as were individuals with cancerous tumors, cardiovascular illness, severe organic disease, and psychological disorders.
A paper-based questionnaire developed by a researcher was used to conduct an interview. The research questionnaire consisted of four parts which were distributed as follows:
Part I: Age, degree of education, and employment are socio-demographic variables.
Part II: Patients' lifestyle and biomedical factors which include physical activity (regular physical exercise), family history of PCOS; diet (unhealthy diet, for example, pickled food, coarse food, drink, and salty food), menstrual history (regular or irregular menstruation), a drug used (contraception drugs, cortisone, Clomid).
Part III: Anthropometric measures were taken, including body mass, height, and waist circumference (WC). Body weight (kg) and height (cm) were measured by standing position and without shoes, Anthropometric measurements for measuring height, and waist circumference, using the metric tape, and measuring weight utilizing an electronic scale. Classification of participants’ BMI according to World Health Organization (WHO) guidelines for Asian populations was as follow:(<18.5-22.5 kg/m2 underweight, 23-24.9 kg/m2 normal weight, 25-29.9 kg/m2 overweight and >30 kg/m2 obese) [21].
Part IV: Clinical symptoms of PCOS.
Ethical approval and all administrative agreements were obtained from the College of Health and Medical Technology/ Baghdad/ Community Health Department and the research committee at Middle Technical University. Protecting the participant's values and dignity is one of the most fundamental pre-collection concepts.
SPSS version 22 was used to analyze data, and the Chi-square test was applied to assess the data. The level of significance was fixed at P< 0.05. To assess the probability of PCOS, odds ratios and confidence intervals of 95% were calculated.
Findings
This research involved 200 women in total. Table 1 displays the socio-demographic data of the study's case and control populations. Table 1 showed that 46% of the case group and 45% of the control group were in the age group of 21-25 years. Poly Cystic Ovarian Syndrome was shown to be more common in women between the ages of 21 and 25. In terms of BMI, most of the patients with PCOS were overweight, while most of the control group had normal BMI. The results of the univariate analysis of risk factors for PCOS in Table 1 showed that age, BMI, educational level, occupational status, and waist circumference were all significantly related to PCOS.
The results of Table 2 showed that a high percentage of the case group had a family history of PCOS, while 8% of the control group reported a family history of PCOS (p<0.05). In addition, 46% of the case group had a diet, whereas only 23% of the control group did; this difference was statistically significant. However, there was no statistically significant difference between the two groups in terms of regular exercise or having children (p<0.05).
Table 1) Distribution of Socio-demographic characteristics, BMI, and Waist circumference in the case and control groups

Table 2) Results of the probability of PCOS in the case and control group

Discussion
The cause of PCOS is still unknown because of its complexity. PCOS is caused by the interplay of hereditary and environmental variables [22]. PCOS leads to changes in lifestyle, increased stress, and reduced cycle impairment. The most effective treatment for PCOS is to prevent its development and diagnose its risk factors to prevention of serious long-term complications [23]. The goal of this study was to find out what makes women in Baghdad more likely to get polycystic ovary syndrome.
The majority of women in both groups were between 21 and 25 years of age, demonstrating that age is a key risk factor for PCOS. Similar findings were observed in another study, which revealed that the majority of PCOS patients (34.2%) were between the ages of 21 and 25 [24]. A similar experiment in Bhopal had equivalent results [25].
The findings of the current investigation reflected that educational level is significantly related to PCOS which is consistent with the findings of the study in 2015 that reported educational level is a fundamental risk factor for PCOS [26], however in their study, most women had an educational level of primary school and in our study, most participants had an educational level of college and higher. This disparity is likely attributable to the fact that females in Iraq may not receive a PCOS diagnosis during their early pubertal years.
The findings of the current study indicated that housewives were a more risky group for PCOS; this result was confirmed in the study done in Pakistan [27]. This is because housewives women are more interested to diagnose the cause of delayed pregnancy or menstrual disorders. Moreover, a family history of PCOS was detected to be a highly significant risk factor for PCOS. Some studies reported similar findings [28-30].
According to the findings of the current study, an unhealthy diet including pickled food, coarse food, drink, and salty food was the other significant risk factor for PCOS (p=0.001). This finding was in agreement with the study conducted in China [31]. Unhealthy foods with high amounts of calories cause an imbalance of hormones which increases the weight.
Also, the present study showed that physical exercise was not a significant risk factor for the development of PCOS. This result is in agreement with the investigation performed in UAE [28]. Although the result was not consistent with the study's conclusion that a lack of physical activity was statistically related to PCOS [26]. Uneven distribution of body fat is caused by a lack of physical activity, which is a significant risk factor for central obesity. We observed that overweight and obese participants were riskier for the development of PCOS compared to normal BMI women. This result is following the study done in UAE [28], and the study done in Spain [12]. This is likely due to a lack of physical activity and bad eating habits. In addition to central obesity and overweight, an increased waist circumference is an additional risk factor for the development of PCOS. Our investigation displayed that PCOS was significantly associated with waist circumference (<80cm). This finding is in agreement with the investigation performed in UAE [28]. It is mostly caused to excessive intake of fast food, unhealthy eating habits, and a poor diet.
Irregular menstrual cycle and infertility are highly significant risk factors for PCOS. A high index for the diagnosis of PCOS in teens with irregular menstrual cycles was reported in Nicandri's study, which showed a similar outcome [32]. In the current study, there was a highly significant association between the use of Clomid and PCOS. The result is in agreement with the study done in the USA [33].
According to the results of this study, recommended to establish more health programs regarding early diagnosis, effective treatment, and follow-up of patients, use a different type of media to stimulate public awareness about the risk factors of PCOS, improve the programs of health education about maintaining a healthy weight, establish health educational programs about reducing high carbohydrates and low-fat foods, designing programs about regular physical activity, and regular follow-up.
One problem with this study is that it didn't look at some risk factors for PCOS, like being married or having a family history of diabetes. In the next study, we should make the project design even better.
Conclusion
Targeting the high-risk factors of age, educational level, occupational status, BMI, waist circumference, family history, diet, regular menstrual cycle, and Clomid used, we should perform early screening, diagnosis, and treatment of POCS and identify its risk factors to decrease the incidence of PCOS and progress its prognosis.
Acknowledgments: The authors like to express their gratitude to all of the women who participated in this study.
Ethical Permissions: The researchers conducted the necessary agreements ethics committee from the College of Health and Medical Technology/ Baghdad/ and then the researchers informed the participants that the responses will be used for the research purpose only.
Conflicts of Interests: There are no conflicts of interest.
Authors’ Contributions: Kadhum Zeidan MA (First Author), Introduction Writer/Methodologist/Main Researcher /Statistical Analyst/Discussion Writer (75%); Hassoon SM (Second Author), Assistant Researcher/Statistical Analyst (15%); Shatha Ahmed MA (Third Author), Introduction Writer/Assistant Researcher (10%)
Funding/Support: None declared.
Article Type: Original Research |
Subject:
Sexual Health Education/Promotion
Received: 2022/05/17 | Accepted: 2022/07/24 | Published: 2022/08/10
Received: 2022/05/17 | Accepted: 2022/07/24 | Published: 2022/08/10
References
1. Zhang J, Xu JH, Qu QQ, Zhong GQ. Risk of cardiovascular and cerebrovascular events in polycystic ovarian syndrome women: A meta-analysis of cohort studies. Front Cardiovasc Med. 2020;7:552421. [Link] [DOI:10.3389/fcvm.2020.552421]
2. Wang YY, Hao SL, Hou LH, Wu XK. Research progress on cardiovascular risk factors for polycystic ovarian syndrome. J Medl Res. 2013;42(7):11-3. [Link]
3. Hart R, Hickey M, Franks S. Definitions, prevalence and symptoms of polycystic ovaries and polycystic ovary syndrome. Best Pract ResClin Obstet Gynaecol. 2004;18(5):671-83. [Link] [DOI:10.1016/j.bpobgyn.2004.05.001]
4. Farquhar C, Brown J, Marjoribanks J. Laparoscopic drilling by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database System Rev. 2012(6). [Link] [DOI:10.1002/14651858.CD001122.pub4]
5. Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS): the Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97(1):28-38. [Link] [DOI:10.1016/j.fertnstert.2011.09.024]
6. Azziz R, Sanchez LA, Knochenhauer ES, Moran C, Lazenby J, Stephens KC, et al. Androgen excess in women: Experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004;89(2):453-62. [Link] [DOI:10.1210/jc.2003-031122]
7. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. [Link] [DOI:10.1186/1741-7015-8-41]
8. González F. Inflammation in polycystic ovary syndrome: Underpinning of insulin resistance and ovarian dysfunction. Steroids. 2012;77(4):300-5. [Link] [DOI:10.1016/j.steroids.2011.12.003]
9. Sarahian N, Sarvazad H, Sajadi E, Rahnejat N, Eskandari Roozbahani N. Investigation of common risk factors between polycystic ovary syndrome and Alzheimer's disease: A narrative review. Reprod Health. 2021;18:156. [Link] [DOI:10.1186/s12978-021-01203-x]
10. De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia FJ. Genetic, hormonal and metabolic aspects of PCOS: An update. Reprod Biol Endocrinol. 2016;14:38. [Link] [DOI:10.1186/s12958-016-0173-x]
11. Isikoglu M, Berkkanoglu M, Cemal H, Ozgur K. Polycystic ovary syndrome. Kent, UK: Anshan, Ltd; 2007. pp. 157-63. [Link]
12. Alvarez-Blasco F, Botella-Carretero JI, San Millán JL, Escobar-Morreale HF. Prevalence and characteristics of the polycystic ovary syndrome in overweight and obese women. Arch Inter Med. 2006;166(19):2081-6. [Link] [DOI:10.1001/archinte.166.19.2081]
13. Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011(7). [Link] [DOI:10.1002/14651858.CD007506.pub2]
14. Gottschau M, Kjaer SK, Jensen A, Munk C, Mellemkjaer L. Risk of cancer among women with polycystic ovary syndrome: A Danish cohort study. Gynecol Oncol. 2015;136(1):99-103. [Link] [DOI:10.1016/j.ygyno.2014.11.012]
15. Amato P, Simpson JL. The genetics of polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2004;18(5):707-718. [Link] [DOI:10.1016/j.bpobgyn.2004.05.002]
16. Wild RA, Rizzo M, Clifton S, Carmina E. Lipid levels in polycystic ovary syndrome: Systematic review and meta-analysis. Fertil Steril. 2011;95(3):1073-9. [Link] [DOI:10.1016/j.fertnstert.2010.12.027]
17. Riestenberg C, Jagasia A, Markovic D, Buyalos RP, Azziz R. Health care-related economic burden of polycystic ovary syndrome in the United States: pregnancy-related and long-term health consequences. J Clin Endocrinol Metab. 2022;107(2):575-85. [Link] [DOI:10.1210/clinem/dgab613]
18. Mortada R, Williams T. Metabolic Syndrome: Polycystic Ovary Syndrome. FP Essent. 2015;435:30-42. [Link]
19. National Institutes of Health. Treatments to relieve symptoms of PCOS [Internet]. Rockville: National Institutes of Health; 2015 [Cited 2021 Jun 1]. Available from: https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/treatments/relieve [Link]
20. Rotterdam ESHRE/ASRM‐Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long‐term health risks related to polycystic ovary syndrome (PCOS). Human Reprod. 2004;19(1):41-7. [Link] [DOI:10.1093/humrep/deh098]
21. Jih J, Mukherjea A, Vittinghoff E, Nguyen TT, Tsoh JY, Fukuoka Y, et al. Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prevent Med. 2014;65:1-6. [Link] [DOI:10.1016/j.ypmed.2014.04.010]
22. Aversa A, La Vignera S, Rago R, Gambineri A, Nappi RE, Calogero AE, et al. Fundamental concepts and novel aspects of polycystic ovarian syndrome: expert consensus resolutions. Front Endocrinol. 2020;11:516. [Link] [DOI:10.3389/fendo.2020.00516]
23. Shinde KS, Patil SS. Incidence and risk factors of polycystic ovary syndrome among women in reproductive age group attending a tertiary health care hospital in Western Maharashtra. Int J Reprod Contracept Obstet Gynecol. 2019;8(7):2804-10. [Link] [DOI:10.18203/2320-1770.ijrcog20193046]
24. Renatt C, Francis CI, Sajeeth Mini NM. Prevalence, risk factors, and treatment strategies of polycystic ovary syndrome at various hospitals, Palakkad: A prospective study. Int J Innov Res Med Sci. 2017;2:784-8. [Link]
25. Gupta M, Singh D, Toppo M, Priya A, Sethia S, Gupta P. A cross sectional study of polycystic ovarian syndrome among young women in Bhopal, Central India. Int J Community Med Public Health. 2018;5(1):95-100. [Link] [DOI:10.18203/2394-6040.ijcmph20175603]
26. Bronstein J, Tawdekar S, Liu Y, Pawelczak M, David R, Shah B. Age of onset of polycystic ovarian syndrome in girls may be earlier than previously thought. J Pediatr Adolesc Gynecol. 2011;24(1):15-20. [Link] [DOI:10.1016/j.jpag.2010.06.003]
27. Sidra S, Tariq MH, Farrukh MJ, Mohsin M. Evaluation of clinical manifestations, health risks, and quality of life among women with polycystic ovary syndrome. PloS One. 2019;14:e0223329. [Link] [DOI:10.1371/journal.pone.0223329]
28. Begum GS, Shariff A, Ayman G, Mohammad B, Housam R, Khaled N. Assessment of risk factors for development of polycystic ovarian syndrome. Diabetes. 2017;1(2). [Link]
29. Kahsar-Miller MD, Nixon C, Boots LR, Go RC, Azziz R. Prevalence of polycystic ovary syndrome (PCOS) in first-degree relatives of patients with PCOS. Fertil Steril. 2001;75(1):53-8. [Link] [DOI:10.1016/S0015-0282(00)01662-9]
30. Kahsar-Miller M, Azziz R. The development of the polycystic ovary syndrome: Family history as a risk factor. Trend Endocrinol Metab. 1998;9(2):55-8. [Link] [DOI:10.1016/S1043-2760(98)00021-6]
31. Du JY, Xu ZY, Feng JY. The relationship study between environmental factors in Weihai region and polycystic ovary syndrome. Chin J Healthy Birth Child Care. 2012;18(5):269-72. [Link]
32. Nicandri KF, Hoeger K. Diagnosis and treatment of polycystic ovarian syndrome in adolescents. Curr Opin Endocrinol Diabetes Obes. 2012;19(6):497-504. [Link] [DOI:10.1097/MED.0b013e32835a1a03]
33. Zain MM, Jamaluddin R, Ibrahim A, Norman RJ. Comparison of clomiphene citrate, metformin, or the combination of both for first-line ovulation induction, achievement of pregnancy, and live birth in Asian women with polycystic ovary syndrome: A randomized controlled trial. Fertil Steril. 2009;91(2):514-21. [Link] [DOI:10.1016/j.fertnstert.2007.12.002]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





