Volume 10, Issue 3 (2022)
Health Educ Health Promot 2022, 10(3): 565-570 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zainel I, Abdul-Ra'aoof H, Tiryag A. Mothers' Knowledge and Attitudes towards her Children with Neonatal Jaundice: A Cross-Sectional Study. Health Educ Health Promot 2022; 10 (3) :565-570
URL: http://hehp.modares.ac.ir/article-5-59471-en.html
URL: http://hehp.modares.ac.ir/article-5-59471-en.html
1- Adult Nursing Department, College of Nursing, University of Telafer, Telafer, Iraq
2- Community Health Nursing Department, College of Nursing, University of Basrah, Basrah, Iraq
3- Fundamental of Nursing Department, College of Nursing, University of Basrah, Basrah, Iraq
2- Community Health Nursing Department, College of Nursing, University of Basrah, Basrah, Iraq
3- Fundamental of Nursing Department, College of Nursing, University of Basrah, Basrah, Iraq
Keywords: Mothers [MeSH], Knowledge [MeSH], Attitudes [MeSH], Children [MeSH], Neonatal Jaundice [MeSH]
Full-Text [PDF 803 kb]
(5381 Downloads)
| Abstract (HTML) (2681 Views)
Conclusion
Most mothers who participated in this study had poor knowledge and attitudes about neonatal jaundice.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Zainel IH (First Author), Introduction Writer/ Main Researcher/Discussion Writer (40%); Abdul-Ra'aoof HH (Second Author), Assistant Researcher (20%); Tiryag AM (Third Author), Methodologist (20%)
Funding/Support: None declared.
Full-Text: (765 Views)
Introduction
Neonatal Jaundice (NNJ) is defined as yellowish discoloration of the skin and sclera of newborns because of a high bilirubin level in the body [1, 2]. A bilirubin level of more than 85mmol/l (5mg/dl) manifests as jaundice. In newborns, jaundice is discovered by watching the skin; neonate has an apparent icteric sclera and yellowing of the face expanding down to the chest. In the newborn, the jaundice of the dermis is first noted in the face, and with the bilirubin, increasing levels advance produce spread to the trunk and then to the limbs [3].
Neonatal Jaundice is the most common neonatal disorder requiring clinical evaluation and management worldwide [4]. It occurs in up to 60% of term newborns and 80% of preterms in the first week [3, 5]. NNJ has a major impact on neonatal morbidity and mortality in developing countries, including Iraq [6].
Gamaleldin et al. reported that forty-eight percent (48%) of the 1008 neonates admitted to the outborn unit of the neonatal intensive care unit (NICU) of Cairo University Children's Hospital, Egypt, from 2006 to 2008 had NNJ. When bilirubin raises immoderately more than 20 mg/dl in healthy and normal birth weight babies, it is a great concern because possible complications arising from unconjugated hyperbilirubinemia include acute bilirubin encephalopathy, neurotoxic, with long-term neurological consequences (kernicterus), seizures, cerebral palsy, mental retardation, deafness, death, and amongst others [7-9].
In newborn, jaundice trends progress because of two factors, the disintegration of fetal hemoglobin and the relatively immature hepatic metabolic pathways which are unable to conjugate and so excretion of bilirubin as quickly as an adult; this cause aggregation of bilirubin in the blood leading to appearance the clinical manifestation of jaundice. Other causes of hyperbilirubinemia in the newborn are large or small for gestation age, immaturity, trisomy syndrome, utilization of oxytocin in labor, presence of bruising cephalhematoma, and a family history of neonatal jaundice [10].
Delay in starting breastfeeding or inadequate feeding causes poor gut movement, which leads to poor bilirubin excretion, resulting in bilirubin buildup and hyperbilirubinemia. Insufficient milk leads to a delay in the passage of meconium. Passing the child through the vagina during birth activates the mother's milk formation. The milk excretion is slightly delayed when the baby is born by cesarean section. There will be pain and sedation for the mothers, so the feeding is delayed; these children are at greater risk for jaundice. Mothers should start breastfeeding as soon as feasible, whether they had a caesarian section or a normal delivery [11].
The short post-delivery hospital stay, delays in obtaining a post-discharge appointment, lack of post-discharge appointment for mothers delivering in unorthodox settings, lack of knowledge of risk factors for the development of significant hyperbilirubinemia in mothers, increased frequency of breastfeeding, lack of concern about high bilirubin levels in newborns among pediatric care providers and late recognition and commencement of effective therapy for NNJ are documented factors associated with the occurrence of kernicterus (A disorder that is due to severe jaundice in the newborn, with deposition of bilirubin in the brain that causes brain damage, potentially leading to cerebral palsy, hearing impairment, visual impairment, or dementia), also known as bilirubin encephalopathy [7, 12]. According to research, kernicterus has a 10% mortality and 70% morbidity rates [13]; the complications resulting from untreated or improperly managed unconjugated hyperbilirubinemia are mostly incurable but could be prevented by early disclosure and effective management of neonatal jaundice.
Therefore, it becomes necessary to prepare mothers to recognize NNJ early and bring afflicted newborns to suitable health institutions by examining their knowledge, attitude, and practice about NNJ. Previous studies have revealed varying degrees of ignorance and deficiency in the knowledge of risk factors, presentation, complications, treatment, and attitude of family caregivers regarding neonatal jaundice in different areas of the world [14, 15].
Studies to evaluate mothers' knowledge regarding NNJ have not been conducted in Iraq, Telafer city. Since the mothers are beside the baby 24 hours a day, priority must be given to educating them. Therefore, the objective of this study was to examine mothers' knowledge and attitudes about newborn jaundice, including their awareness, recognition, knowledge of risk factors/causes, problems, treatment options, and the first measures to take when it is discovered. The information gathered might aid in the proper direction of health education in the community to reduce the occurrence, severity, and consequences of newborn jaundice.
On the other hand, any action taken by mothers is influenced by their knowledge and attitude about neonatal jaundice, so it is essential to assess mothers` knowledge and attitude toward Neonatal Jaundice.
As a significant public health information source, healthcare personnel has difficulties properly distributing information. Firstly, it has been reported that up to 42% of deliveries are either without prenatal care or with little antenatal care given in an inappropriate setting; hence the reach of the necessary information from health workers to women of childbearing age is limited [16] Secondly, it has been documented that significant proportion of healthcare workers on occasions display inadequate knowledge of certain aspects of health issues and are therefore predisposed to giving inadequate information to antenatal attendees [17]. As a result, healthcare professionals must be exposed to frequent seminars and workshops to refresh and update their knowledge. The often prolonged power outage could explain the low rate of population information through electronic media in most parts of this country and bad security in certain areas making the widespread, efficient dissemination of information and education through electronic media difficult. Increased effort should be made by knowledgeable medical personnel to make frequent appearances in electronic media for the health education of the citizenry, especially in areas where power supply and security are relatively stable.
This study aimed to assess mothers' knowledge and attitudes toward neonatal jaundice.
Instrument and Methods
A descriptive non-experimental study has been carried out to assess the knowledge and attitudes of mothers who have children with neonatal jaundice attending Telafer General Hospital-Iraq at Telafer District-Mousel Governorate in the north of Iraq over a period from December 1, 2021, to June 29, 2022. The study includes 200 mothers aged between 16 to 45 years representing the study sample; they were selected by random sampling. Mothers who refused to participate in the present study were excluded.
The instrument advanced and utilized to collect the data was based on the objectives. A semi-structured interview schedule was prepared, and based on the problem statement, a review of books and journals publicized was considered. The questionnaire has three sections: Section A: demographic variables, including age, occupation, educational level, delivery mode, and living nature. Section B: knowledge regarding neonatal jaundice consists of sixteen questions. Section C: Mothers' attitudes on managing babies with neonatal jaundice; the attitudes assessment consists of nine questions. We use the 3-Points Likert Scale ranging from (1 to 3). This scale is composed of 16 items, and these items were measured on a 3-point Likert scale, which ranged from 1 (=Don't know), 2 (=Uncertain), and 3 (=Know). The level of assessment for each item in the knowledge scales was estimated by calculating the cutoff point for the mean of the score and scored as follows: The researcher determined 1-1.66 for poor knowledge, 1.67-2.33 for moderate knowledge, and 2.34-3 for the high knowledge. Scoring Key for Attitude Statement: attitudes assessment scoring was prepared according to Likert's three-point Scale. Yes (=3), Don’t Know (=2), and No (=1). Experts were consulted about the tool's content validity, and their recommendations were implemented before data was collected.
Official approvals were obtained from the concerned authorities to conduct this study. The questionnaire was explained to the mothers, and we received oral consent from them. Each interview took 20 to 30 minutes; the researcher interviewed five participants in one day. A pilot study was done on 20 mothers, using the same setting and questionnaire to assess the feasibility of the revised study to remove ambiguities and clarify the questions. Professionals assessed its content validity.
The collected data were organized and tabulated in a master sheet as frequencies and percentages and were analyzed using the SPSS software version 26. Descriptive data analysis includes mean scores, with their standard deviation, and frequency. Inferential data analysis includes the chi-square.
Findings
The mean of participants age was 25.03+6.27 years. Most of the mothers were housewives, had a high school education, had a natural vaginal delivery, and lived in cities (Table 1).
The majority of the mothers had poor knowledge about neonatal jaundice, and 7.5% of them have good knowledge (Table 2). There was a significant relationship between mothers' occupation and their knowledge of neonatal jaundice (p<0.05). Also, these findings show no significant relationship between mothers' age, level of education, delivery mode, and living nature and their knowledge about neonatal jaundice (p>0.05; Table 3).
Table 1) Frequency results of demographic data of the mothers
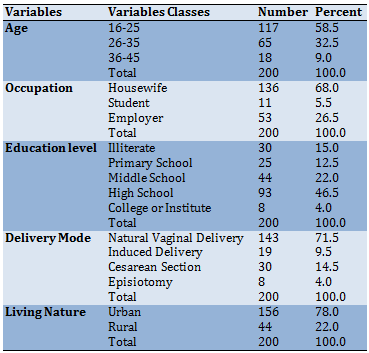
Table 2) Mothers' knowledge and attitude toward neonatal jaundice
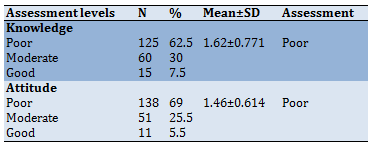
Table 3) Relationships of demographic variables with mothers' knowledge and attitude
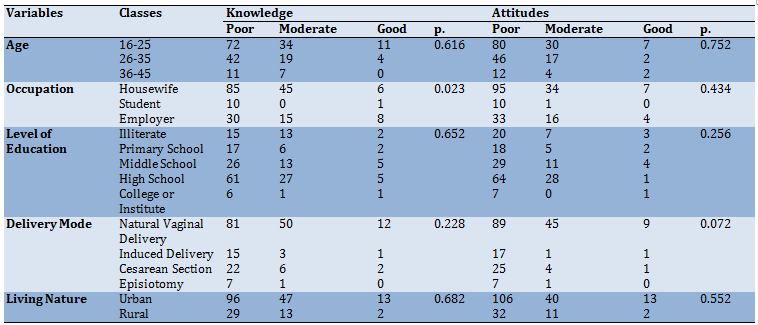
Also, the majority of the mothers had poor attitudes about neonatal jaundice, and 5.5% of them have good attitudes (Table 2). The findings showed no significant relationship between mothers' age, occupation, level of education, delivery mode, and living nature and their knowledge about neonatal jaundice (p>0.05; Table 3).
Discussion
In reviewing the above statistics, one can conclude that most mothers (58.5%) were from (16-25). This agrees with Dash [2] that the majority of respondents, 21 (42%), were in the age group of 21-25 years.
Regarding occupation, a high percentage of the mothers (68%) were housewives. This agrees with Rabiyeepoor et al. [18]. In contrast, most respondents, 159 (79.5%), were housewives. Also, concerning the level of education, most of them had a high school education (46.5%) agree with Onyearugha et al. [6] showing a high level of awareness in this study because a large percentage of the respondents (96.7%) having high school and above this explains the health education is very poor between peoples. Also, concerning the delivery mode, a high percentage of the mothers (71.5%)were natural vaginal delivery, and the majority of the mothers (78%) lived in urban (cities). This finding is consistent with a study conducted in Iran [18] that showed the natural vaginal delivery rate was 121 and 79 (n=200) had cesarean section; also, the majority of respondents, 130 (65%), were lived-in cities.
According to this study's results, most mothers (62.5%) have poor knowledge about neonatal jaundice. The researcher believes that mothers’ poor knowledge regarding neonatal jaundice might be due to many causes: Mothers did not study neonatal jaundice. Most mothers are housewives. The mothers do not update their knowledge continuously without educational and television programs about neonatal jaundice. Most mothers are young in the group age 16-25.
The results of this study agreed with a study [19]; the results showed that most mothers have poor knowledge (68.9%) of neonatal jaundice. Also, the results of this study agree with a study [6]; the results show that most mothers have low knowledge about neonatal jaundice. Also, the study's findings agreed with a study [20] that shows the majority of mothers have low knowledge regarding causes, danger signs, and effective treatment available for neonatal jaundice.
According to the findings of this study, there is a significant relationship between mothers' knowledge and their occupation. This may be due to the employers' mothers' higher education levels than housewives and students.
The results of this study agreed with a study [21], which reported a significant relationship between mothers' knowledge and occupation. According to the findings of this study, there is no significant relationship between mothers' knowledge and their demographic variables (age, level of education, delivery mode, and living nature). The results of this study agreed with a study [19]; that shows age and educational level did not show any statistically significant relationship with knowledge about neonatal jaundice (p<0.05).
According to this study's results, most mothers (69%) have poor attitudes about neonatal jaundice. The results of this study agreed with a study [22] conducted in Ghana on Neonatal jaundice in Ghanaian children: Assessing maternal knowledge, attitude, and perceptions reported that mothers had poor attitudes about neonatal jaundice. The results of this study agreed with a study conducted in Saudi Arabia by a study [22] on the Assessment of Knowledge, Attitude, and Practice of Saudi Parents towards Neonatal Jaundice (NNJ): A Cross-sectional Study reported that mothers had poor attitudes about neonatal jaundice. The results of this study agreed with a study conducted in Ethiopia by a study [23] Knowledge on neonatal jaundice and its associated factors among mothers in northern Ethiopia: a facility-based cross-sectional study reported that more than half of the mothers have unfavorable attitudes about neonatal jaundice.
According to the result of this study, there is no significant relationship between mothers' attitudes and their demographic characteristics (age, occupation, level of education, delivery mode, and living nature). The findings of this study agreed with a study conducted in Iran by a study [24] on Maternal Knowledge, Attitude, And Practice About Neonatal Jaundice In Jiroft, 2017 reported that there is no significant relationship between mothers' knowledge and demographic variables.
Recommendations were as follows:
Neonatal Jaundice (NNJ) is defined as yellowish discoloration of the skin and sclera of newborns because of a high bilirubin level in the body [1, 2]. A bilirubin level of more than 85mmol/l (5mg/dl) manifests as jaundice. In newborns, jaundice is discovered by watching the skin; neonate has an apparent icteric sclera and yellowing of the face expanding down to the chest. In the newborn, the jaundice of the dermis is first noted in the face, and with the bilirubin, increasing levels advance produce spread to the trunk and then to the limbs [3].
Neonatal Jaundice is the most common neonatal disorder requiring clinical evaluation and management worldwide [4]. It occurs in up to 60% of term newborns and 80% of preterms in the first week [3, 5]. NNJ has a major impact on neonatal morbidity and mortality in developing countries, including Iraq [6].
Gamaleldin et al. reported that forty-eight percent (48%) of the 1008 neonates admitted to the outborn unit of the neonatal intensive care unit (NICU) of Cairo University Children's Hospital, Egypt, from 2006 to 2008 had NNJ. When bilirubin raises immoderately more than 20 mg/dl in healthy and normal birth weight babies, it is a great concern because possible complications arising from unconjugated hyperbilirubinemia include acute bilirubin encephalopathy, neurotoxic, with long-term neurological consequences (kernicterus), seizures, cerebral palsy, mental retardation, deafness, death, and amongst others [7-9].
In newborn, jaundice trends progress because of two factors, the disintegration of fetal hemoglobin and the relatively immature hepatic metabolic pathways which are unable to conjugate and so excretion of bilirubin as quickly as an adult; this cause aggregation of bilirubin in the blood leading to appearance the clinical manifestation of jaundice. Other causes of hyperbilirubinemia in the newborn are large or small for gestation age, immaturity, trisomy syndrome, utilization of oxytocin in labor, presence of bruising cephalhematoma, and a family history of neonatal jaundice [10].
Delay in starting breastfeeding or inadequate feeding causes poor gut movement, which leads to poor bilirubin excretion, resulting in bilirubin buildup and hyperbilirubinemia. Insufficient milk leads to a delay in the passage of meconium. Passing the child through the vagina during birth activates the mother's milk formation. The milk excretion is slightly delayed when the baby is born by cesarean section. There will be pain and sedation for the mothers, so the feeding is delayed; these children are at greater risk for jaundice. Mothers should start breastfeeding as soon as feasible, whether they had a caesarian section or a normal delivery [11].
The short post-delivery hospital stay, delays in obtaining a post-discharge appointment, lack of post-discharge appointment for mothers delivering in unorthodox settings, lack of knowledge of risk factors for the development of significant hyperbilirubinemia in mothers, increased frequency of breastfeeding, lack of concern about high bilirubin levels in newborns among pediatric care providers and late recognition and commencement of effective therapy for NNJ are documented factors associated with the occurrence of kernicterus (A disorder that is due to severe jaundice in the newborn, with deposition of bilirubin in the brain that causes brain damage, potentially leading to cerebral palsy, hearing impairment, visual impairment, or dementia), also known as bilirubin encephalopathy [7, 12]. According to research, kernicterus has a 10% mortality and 70% morbidity rates [13]; the complications resulting from untreated or improperly managed unconjugated hyperbilirubinemia are mostly incurable but could be prevented by early disclosure and effective management of neonatal jaundice.
Therefore, it becomes necessary to prepare mothers to recognize NNJ early and bring afflicted newborns to suitable health institutions by examining their knowledge, attitude, and practice about NNJ. Previous studies have revealed varying degrees of ignorance and deficiency in the knowledge of risk factors, presentation, complications, treatment, and attitude of family caregivers regarding neonatal jaundice in different areas of the world [14, 15].
Studies to evaluate mothers' knowledge regarding NNJ have not been conducted in Iraq, Telafer city. Since the mothers are beside the baby 24 hours a day, priority must be given to educating them. Therefore, the objective of this study was to examine mothers' knowledge and attitudes about newborn jaundice, including their awareness, recognition, knowledge of risk factors/causes, problems, treatment options, and the first measures to take when it is discovered. The information gathered might aid in the proper direction of health education in the community to reduce the occurrence, severity, and consequences of newborn jaundice.
On the other hand, any action taken by mothers is influenced by their knowledge and attitude about neonatal jaundice, so it is essential to assess mothers` knowledge and attitude toward Neonatal Jaundice.
As a significant public health information source, healthcare personnel has difficulties properly distributing information. Firstly, it has been reported that up to 42% of deliveries are either without prenatal care or with little antenatal care given in an inappropriate setting; hence the reach of the necessary information from health workers to women of childbearing age is limited [16] Secondly, it has been documented that significant proportion of healthcare workers on occasions display inadequate knowledge of certain aspects of health issues and are therefore predisposed to giving inadequate information to antenatal attendees [17]. As a result, healthcare professionals must be exposed to frequent seminars and workshops to refresh and update their knowledge. The often prolonged power outage could explain the low rate of population information through electronic media in most parts of this country and bad security in certain areas making the widespread, efficient dissemination of information and education through electronic media difficult. Increased effort should be made by knowledgeable medical personnel to make frequent appearances in electronic media for the health education of the citizenry, especially in areas where power supply and security are relatively stable.
This study aimed to assess mothers' knowledge and attitudes toward neonatal jaundice.
Instrument and Methods
A descriptive non-experimental study has been carried out to assess the knowledge and attitudes of mothers who have children with neonatal jaundice attending Telafer General Hospital-Iraq at Telafer District-Mousel Governorate in the north of Iraq over a period from December 1, 2021, to June 29, 2022. The study includes 200 mothers aged between 16 to 45 years representing the study sample; they were selected by random sampling. Mothers who refused to participate in the present study were excluded.
The instrument advanced and utilized to collect the data was based on the objectives. A semi-structured interview schedule was prepared, and based on the problem statement, a review of books and journals publicized was considered. The questionnaire has three sections: Section A: demographic variables, including age, occupation, educational level, delivery mode, and living nature. Section B: knowledge regarding neonatal jaundice consists of sixteen questions. Section C: Mothers' attitudes on managing babies with neonatal jaundice; the attitudes assessment consists of nine questions. We use the 3-Points Likert Scale ranging from (1 to 3). This scale is composed of 16 items, and these items were measured on a 3-point Likert scale, which ranged from 1 (=Don't know), 2 (=Uncertain), and 3 (=Know). The level of assessment for each item in the knowledge scales was estimated by calculating the cutoff point for the mean of the score and scored as follows: The researcher determined 1-1.66 for poor knowledge, 1.67-2.33 for moderate knowledge, and 2.34-3 for the high knowledge. Scoring Key for Attitude Statement: attitudes assessment scoring was prepared according to Likert's three-point Scale. Yes (=3), Don’t Know (=2), and No (=1). Experts were consulted about the tool's content validity, and their recommendations were implemented before data was collected.
Official approvals were obtained from the concerned authorities to conduct this study. The questionnaire was explained to the mothers, and we received oral consent from them. Each interview took 20 to 30 minutes; the researcher interviewed five participants in one day. A pilot study was done on 20 mothers, using the same setting and questionnaire to assess the feasibility of the revised study to remove ambiguities and clarify the questions. Professionals assessed its content validity.
The collected data were organized and tabulated in a master sheet as frequencies and percentages and were analyzed using the SPSS software version 26. Descriptive data analysis includes mean scores, with their standard deviation, and frequency. Inferential data analysis includes the chi-square.
Findings
The mean of participants age was 25.03+6.27 years. Most of the mothers were housewives, had a high school education, had a natural vaginal delivery, and lived in cities (Table 1).
The majority of the mothers had poor knowledge about neonatal jaundice, and 7.5% of them have good knowledge (Table 2). There was a significant relationship between mothers' occupation and their knowledge of neonatal jaundice (p<0.05). Also, these findings show no significant relationship between mothers' age, level of education, delivery mode, and living nature and their knowledge about neonatal jaundice (p>0.05; Table 3).
Table 1) Frequency results of demographic data of the mothers
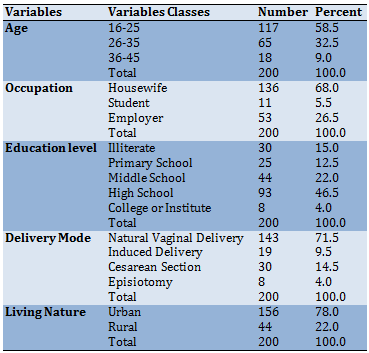
Table 2) Mothers' knowledge and attitude toward neonatal jaundice
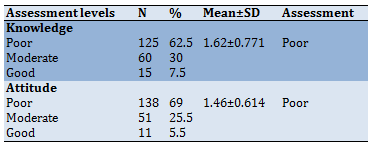
Table 3) Relationships of demographic variables with mothers' knowledge and attitude
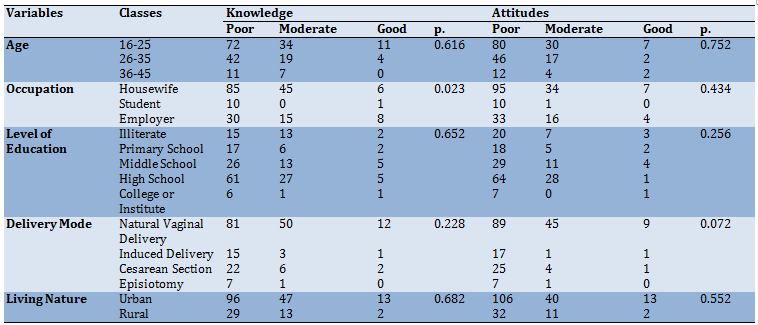
Also, the majority of the mothers had poor attitudes about neonatal jaundice, and 5.5% of them have good attitudes (Table 2). The findings showed no significant relationship between mothers' age, occupation, level of education, delivery mode, and living nature and their knowledge about neonatal jaundice (p>0.05; Table 3).
Discussion
In reviewing the above statistics, one can conclude that most mothers (58.5%) were from (16-25). This agrees with Dash [2] that the majority of respondents, 21 (42%), were in the age group of 21-25 years.
Regarding occupation, a high percentage of the mothers (68%) were housewives. This agrees with Rabiyeepoor et al. [18]. In contrast, most respondents, 159 (79.5%), were housewives. Also, concerning the level of education, most of them had a high school education (46.5%) agree with Onyearugha et al. [6] showing a high level of awareness in this study because a large percentage of the respondents (96.7%) having high school and above this explains the health education is very poor between peoples. Also, concerning the delivery mode, a high percentage of the mothers (71.5%)were natural vaginal delivery, and the majority of the mothers (78%) lived in urban (cities). This finding is consistent with a study conducted in Iran [18] that showed the natural vaginal delivery rate was 121 and 79 (n=200) had cesarean section; also, the majority of respondents, 130 (65%), were lived-in cities.
According to this study's results, most mothers (62.5%) have poor knowledge about neonatal jaundice. The researcher believes that mothers’ poor knowledge regarding neonatal jaundice might be due to many causes: Mothers did not study neonatal jaundice. Most mothers are housewives. The mothers do not update their knowledge continuously without educational and television programs about neonatal jaundice. Most mothers are young in the group age 16-25.
The results of this study agreed with a study [19]; the results showed that most mothers have poor knowledge (68.9%) of neonatal jaundice. Also, the results of this study agree with a study [6]; the results show that most mothers have low knowledge about neonatal jaundice. Also, the study's findings agreed with a study [20] that shows the majority of mothers have low knowledge regarding causes, danger signs, and effective treatment available for neonatal jaundice.
According to the findings of this study, there is a significant relationship between mothers' knowledge and their occupation. This may be due to the employers' mothers' higher education levels than housewives and students.
The results of this study agreed with a study [21], which reported a significant relationship between mothers' knowledge and occupation. According to the findings of this study, there is no significant relationship between mothers' knowledge and their demographic variables (age, level of education, delivery mode, and living nature). The results of this study agreed with a study [19]; that shows age and educational level did not show any statistically significant relationship with knowledge about neonatal jaundice (p<0.05).
According to this study's results, most mothers (69%) have poor attitudes about neonatal jaundice. The results of this study agreed with a study [22] conducted in Ghana on Neonatal jaundice in Ghanaian children: Assessing maternal knowledge, attitude, and perceptions reported that mothers had poor attitudes about neonatal jaundice. The results of this study agreed with a study conducted in Saudi Arabia by a study [22] on the Assessment of Knowledge, Attitude, and Practice of Saudi Parents towards Neonatal Jaundice (NNJ): A Cross-sectional Study reported that mothers had poor attitudes about neonatal jaundice. The results of this study agreed with a study conducted in Ethiopia by a study [23] Knowledge on neonatal jaundice and its associated factors among mothers in northern Ethiopia: a facility-based cross-sectional study reported that more than half of the mothers have unfavorable attitudes about neonatal jaundice.
According to the result of this study, there is no significant relationship between mothers' attitudes and their demographic characteristics (age, occupation, level of education, delivery mode, and living nature). The findings of this study agreed with a study conducted in Iran by a study [24] on Maternal Knowledge, Attitude, And Practice About Neonatal Jaundice In Jiroft, 2017 reported that there is no significant relationship between mothers' knowledge and demographic variables.
Recommendations were as follows:
1- A greater level of mothers' awareness is required of all aspects of neonatal jaundice, such as causes, side effects, signs and symptoms, and treatment because the mother is the first caregiver for the infant; as a result, they must recognize the color change and seek quick medical attention to avoid complications and save a life., in another hand the antenatal talks and regular TV programs can help to educate a large number of mothers.
2- As well, informing school and university students can be so helpful;
3- Also, healthcare providers should be encouraged to publish information on neonatal jaundice to the general population in communal and social gatherings on all different mass media and social media;
4- In addition, we are increasing the health staff's knowledge of various aspects of neonatal jaundice;
5- Special educational programs and the involvement of electronic media for mothers to increase their knowledge about neonatal jaundice;
6- Finally, a positive attitude should be improved in breastfeeding the child during neonatal jaundice as it is essential to prevent complications.
Conclusion
Most mothers who participated in this study had poor knowledge and attitudes about neonatal jaundice.
Acknowledgments: None declared.
Ethical Permissions: None declared.
Conflicts of Interests: None declared.
Authors’ Contributions: Zainel IH (First Author), Introduction Writer/ Main Researcher/Discussion Writer (40%); Abdul-Ra'aoof HH (Second Author), Assistant Researcher (20%); Tiryag AM (Third Author), Methodologist (20%)
Funding/Support: None declared.
Article Type: Original Research |
Subject:
Health Communication
Received: 2022/02/9 | Accepted: 2022/07/23 | Published: 2022/08/22
Received: 2022/02/9 | Accepted: 2022/07/23 | Published: 2022/08/22
References
1. Ogunfowora OB, Daniel OJ. Neonatal jaundice and its management, knowledge, attitude and practice of community health workers in Nigeria. BMC Public Health. 2006;6:19. [Link] [DOI:10.1186/1471-2458-6-19]
2. Dash M. A descriptive study to assess the knowledge and attitude on neonatal jaundice among the mothers in a selected village of Puducherry. Res Rev J Med Health Sci. 2013;2(3). among-the-mothers-in-a-selected-village-of-puducherry.php?aid=34657 [Link]
3. Jacob A. Comprehensive text book of midwifery. New Delhi: Jaypee Brothers Medical Pub; 2008. [Link]
4. Boo NY, Gan CY, Gian YW, Lim KSL, Lim MW, Krishna-Kumar H. Malaysian mothers' knowledge & practices on care of neonatal jaundice. Med J Malaysia. 2011;66(3):239-43. [Link]
5. Rodrigo BKNR, Cooray G. The knowledge, attitude & behavior on neonatal jaundice of postnatal mothers in provincial general hospital, Badulla. Sri Lanka J Child Health. 2011;40(4):164-8. [Link] [DOI:10.4038/sljch.v40i4.3842]
6. Onyearugha CN, Chapp-Jumbo A, George IO. Neonatal jaundice: evaluating the knowledge and practice of expectant mothers in Aba, Nigeria. J Health Sci Res. 2016;1(2):42-7. [Link] [DOI:10.18311/jhsr/2016/v1/i2/4918]
7. Habib H, Lohani M, Khan H, Khan MH. Infant morbidity leading to infant mortality. Gomal J Med Sci. 2009;7:2. [Link]
8. Gamaleldin R, Iskander I, Second IA, Aboraga H. Risk factors for neurotoxicity in newborns with severe neonatal hyperbilirubinemia. Pediatric. 2011;128(4):e925-31. [Link] [DOI:10.1542/peds.2011-0206]
9. Egube BA, Ofili AN, Isara AR, Onakewhor JU. Neonatal jaundice and its management: knowledge, attitude, and practice among expectant mothers attending antenatal clinic at University of Benin Teaching Hospital, Benin City, Nigeria. Nigerian J Clin Pract. 2013;16(2):188-94. [Link] [DOI:10.4103/1119-3077.110147]
10. Kliegman RM, Stanton B, St Geme JW, Felice Schor N, Behrman RE, Nelson WE. Nelson textbook of pediatrics e-book. Pennsylvania: Elsevier; 2007. [Link]
11. Semmalar R. A study to assess the effectiveness of Kangaroo mother care on responses among low birth weight neonates in the postnatal ward of Government Rajaji Hospital at Madurai [dissertation]. Madurai: Madurai Medical College; 2011. [Link]
12. Edmond KM, Zandoh C, Quigley MA, Amenga-Etego S, Owusu-Agyei S, Kirkwood BR. Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics. 2006;117(3):380-6. [Link] [DOI:10.1542/peds.2005-1496]
13. Maisels MJ. Neonatal hyperbilirubinemia and kernicterus-not gone but sometimes forgotten. Early Human Dev. 2009;85(11):727-32. [Link] [DOI:10.1016/j.earlhumdev.2009.09.003]
14. Ives K. Preventing kernicterus-A wake-up call. Arch Dis Child Fetal Neonat Ed. 2007;92(5):F330-1. [Link] [DOI:10.1136/adc.2006.112342]
15. Ogunlesi TA, Abdul A. Maternal knowledge and care-seeking behavior for newborn jaundice in Sagamu, Southwest Nigeria. Niger J Clin Pract. 2015;18(I):12-5. [Link]
16. Olayinka OO, Omolara AK, Odugbemi BA, Femi-Adebayo TT, Odusanya OO. Neonatal jaundice: knowledge, attitude, and practices of mothers in a community in Lagos, Nigeria. Niger Postgrad Med J. 2015;22(3):158-63. [Link] [DOI:10.4103/1117-1936.170741]
17. Macro ICF and National Population Commission. Nigeria demographic and health survey 2008 Abuja. Nigeria: National Population Commission and ICF Macro; 2009. [Link]
18. Rabiyeepoor S, Gheibi S, Jafari S. To study the knowledge and attitude of postnatal mothers on neonatal jaundice in Motahari Hospital, Iran. Clin Med Res. 2014;3(1):1-5. [Link] [DOI:10.11648/j.cmr.20140301.11]
19. Goodman OO, Kehinde OA, Odugbemi BA, Femi-Adebayo TT, Odusanya OO. Neonatal jaundice: knowledge, attitude and practices of mothers in Mosan-Okunola community, Lagos, Nigeria. Niger Postgrad Med J. 2015;22(3):158-63. [Link] [DOI:10.4103/1117-1936.170741]
20. Aggarwal B, Agrawal A, Chaudhary P, Gupta G, Rana S, Gupta S. Neonatal Jaundice: knowledge, attitude beliefs, and practices of postnatal mothers in a tertiary care hospital in Uttarakhand, India. Indian J Child Health. 2017;4(4):603-8. [Link] [DOI:10.32677/IJCH.2017.v04.i04.033]
21. Alfouwais NM, Seada LS, Alahmadi RY, Alassiri AA, Alenazi AA, Aljuaeed MS. Assessment of knowledge, attitude, and practice of Saudi parents towards neonatal jaundice (NNJ): A cross-sectional study. The Egyptian J Hospital Medicine. 2018;70(9):1686-94. [Link] [DOI:10.12816/0044688]
22. Seneadza NAH, Insaidoo G, Boye H, Ani-Amponsah M, Leung T, Meek J, et al. Neonatal jaundice in Ghanaian children: Assessing maternal knowledge, attitude, and perceptions. PLoS One. 2022;17(3):e0264694. [Link] [DOI:10.1371/journal.pone.0264694]
23. Demis A, Getie A, Wondmieneh A, Alemnew B, Gedefaw G. Knowledge on neonatal jaundice and its associated factors among mothers in northern Ethiopia: a facility-based cross-sectional study. BMJ Open. 2021;11(3):e044390. [Link] [DOI:10.1136/bmjopen-2020-044390]
24. Soltaninejad A, Dehdashti N. Maternal knowledge, attitude, and practice about neonatal jaundice in Jiroft, 2017. J Jiroft Univ Med Sci. 2020;6(2):204-13. [Persian] [Link]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |